Abstract
The mental health of young people has been significantly impacted by the COVID‑19 crisis. Prevalence of symptoms of anxiety and depression has risen dramatically among young people and remains higher than pre‑crisis levels even with the partial re‑opening of the economy, and compared to other age groups, even as economies partially re-open. The worsening of mental health can be attributed to disruptions to access to mental health services, the wide‑ranging impacts of school closures, and a labour market crisis that is disproportionately affecting young people. With adequate support and timely intervention, young people experiencing mental distress may be able to bounce back as we recover from the COVID‑19 crisis. This will require a scaling up of existing mental health support in education systems, workplaces and health systems, and comprehensive policies to support young people to remain in education, or to find and keep a job.
The COVID‑19 crisis has turned into a mental health crisis for young people:
Young people’s (15‑24 year‑olds) mental health has worsened significantly in 2020‑21. In most countries, mental health issues among this age group have doubled or more. With adequate support and timely intervention, young people may be able to bounce back as we recover from the COVID‑19 crisis, but there is a risk that the consequences of the COVID‑19 crisis continue to cast a shadow over the lives of young people and their mental health;
The uncertainties and broad impacts of COVID‑19 have not affected all people to the same degree: young people were 30% to 80% more likely to report symptoms of depression or anxiety than adults in Belgium, France and the United States in March 2021. Higher levels of loneliness are also being reported by young people;
Mental health support for young people – notably in schools, universities and workplaces – has been heavily disrupted. Young people are turning to platforms such as mental health hotlines and youth centres for support, often enabled by online tools, while mental health services are offering teleconsultations and remote forms of care to maintain continuity of services;
Closures of educational institutions at all levels have contributed to weakening of protective factors, including daily routine and social interactions that help maintain good mental health. Young people from disadvantaged backgrounds are particularly affected by school closures;
The impact of COVID‑19 on labour markets is disproportionately affecting young people, reducing opportunities for part-time work and work-based learning for students, and leaving soon-to-be graduates and recent graduates facing an uphill task to find and keep a job, putting them at elevated risk of experiencing mental health issues throughout the life course.
An integrated policy response is needed, as called for by the OECD Recommendation on Integrated Mental Health, Skills, and Work Policy, to protect young people’s mental health, both now and on a long-term basis:
Additional mental health support – through information dissemination, phone or online services, and easier access to in-person services – should be a priority for young people, and where mental health support services in schools and universities cannot be resumed, alternatives must be found with urgency;
Support for young people at risk of early school leaving, including young people with experience of mental health issues, should be prioritised to avoid disruptions in learning having a long-term impact on young people’s labour market outcomes and overall well-being;
Unemployment is a major risk factor for poor mental health: supporting young people in finding, keeping and staying in work must be an economic, social, and public health policy priority. Training line managers in the workplace in mental health can also promote better mental health among young adults already in work.
The terms “young people” and “youth” in this brief refers primarily to 15‑24 year‑olds. The brief looks at the mental health impacts of the COVID‑19 crisis and provides policy considerations for three broad groups: young people in upper-secondary education and above (ISCED 3 and above); young people in work; and young people not in education, employment or training.
The terms “mental health conditions” and “mental health issues” are used interchangeably in this brief, while the terms “mental illness” and “mental disorder” are largely avoided. This is to align language with ongoing efforts to raise awareness and address stigma, and to ensure, where possible, language is person-centred, strengths-based, and recovery-focused, and reflects the differing experiences of mental health issues from individual-to‑individual.
Data on population mental health, and especially age‑stratified data, remains limited in coverage. This brief primarily uses prevalence symptoms of anxiety and depression – the two most common forms of mental health issues – estimated through surveys as a barometer of mental health. Where possible, surveys using validated instruments – such as General Anxiety Disorder (GAD‑7) for anxiety and Patient Health Questionnaire‑9 (PHQ‑9) for depression – are used. Instruments used to estimate population mental health, including age groups, differ across surveys, and samples are not necessarily representative, limiting the possibility for cross-country comparisons. As symptoms are self-reported, increase in prevalence may partially reflect changes in awareness or levels of (self-)stigma against mental health issues.
Young people’s mental health has declined significantly since the onset of the COVID‑19 crisis
The COVID‑19 crisis has significantly affected the lives of young people (15‑24 year‑olds), and available evidence points to an alarming surge in mental health issues among this age group. In Belgium, France and the United States, based on data from March 2021, the share of young people experiencing symptoms of anxiety and depression was more than twice as high than the most recent data available from before the crisis (U.S. Census Bureau, 2021[1]; Sciensano, 2021[2]; Santé Publique France, 2021[3]). In the United States, as of March 2021, 43% of 18‑29 year‑olds were reporting symptoms of anxiety, up significantly from the 10% of 18‑34 year‑olds in January to June 2019 (NCHS, 2019[4]). Similar patterns are also evident with depression. In Belgium, the share of 16‑24 year‑olds experiencing symptoms of depression stood at 29% in April 2020, representing a threefold increase among young women and a fourfold increase among young men compared to 2018 (Sciensano, 2020[5]). In the United Kingdom, whereas 11% of 16‑39 year‑olds reported having some form of depression from July 2019 to March 2020, this number had surged to 31% in June 2020 (ONS, 2020[6]).
Self-reported mental health issues are also more prevalent among young people compared to other age groups across many OECD countries. The same data from Belgium, France and the United States shows that prevalence of symptoms of anxiety and depression is around 30% to 80% higher among young people than the general population as of March 2021. In Canada, a survey in May 2020 found that 27% of 15‑24 year‑olds were experiencing moderate to severe symptoms of anxiety, significantly above the 19% share among 25‑64 year‑olds (Statistics Canada, 2020[7]). In Japan, a survey in July 2020 found 31% of 20‑29 year‑olds were experiencing symptoms of depression, compared to 18% of the general population (Fukase et al., 2021[8]). In Italy, a survey in March to May 2020 estimated that 24% of 16‑24 year‑olds were experiencing symptoms of depression, almost double the share among adults aged 25 and above (13%) (Delmastro and Zamariola, 2020[9]). The higher share of young people experiencing anxiety and depression is not consistent with data from recent years, and indicates that the mental health of young people has been disproportionately affected during the COVID‑19 crisis. In the European Union, the proportion of 15‑24 year‑olds reporting chronic depression was estimated at 3.6% in 2014, much lower than among the general population (6.9%) (Eurostat, 2014[10]). In Belgium, 18‑29 year‑olds were the age group least likely to report symptoms of anxiety or depression in 2018, but since the onset of the pandemic, they have become the age group most likely to report symptoms of anxiety or depression (Sciensano, 2021[2]).
In some countries, including Belgium, France and the United States, surveys have followed the trend in the share of the population reporting symptoms of anxiety and depression by age group regularly throughout the COVID‑19 crisis. In the United States, 18‑29 year‑olds have been more likely to report symptoms of anxiety and depression than the general population throughout the crisis, and on average, by 11.5 and 12.3 percentage points respectively in the period from April 2020 to March 2021 (U.S. Census Bureau, 2021[1]) In France, as shown by Figure 1, the prevalence of anxiety and depression has been higher among 18‑24 year‑olds than in the general population throughout March 2020 to March 2021 with only a few exceptions (Santé Publique France, 2021[3]). In mid-February 2021, the prevalence of anxiety and depression among 18‑24 year‑olds stood at 39% and 32% respectively, the highest level since the onset of the pandemic, before declining to 31% and 26% in March 2021. Similar trends have also been recorded in Belgium, where the share of 18‑29 year‑olds reporting symptoms of anxiety and depression increased significantly between September and December 2020. Latest data from March 2021 points to only minor changes in the share reporting symptoms of anxiety (34%) and depression (38%) compared to December 2020 (Sciensano, 2021[2]). These data indicate that the COVID‑19 crisis continues to cast a shadow over young people’s lives.
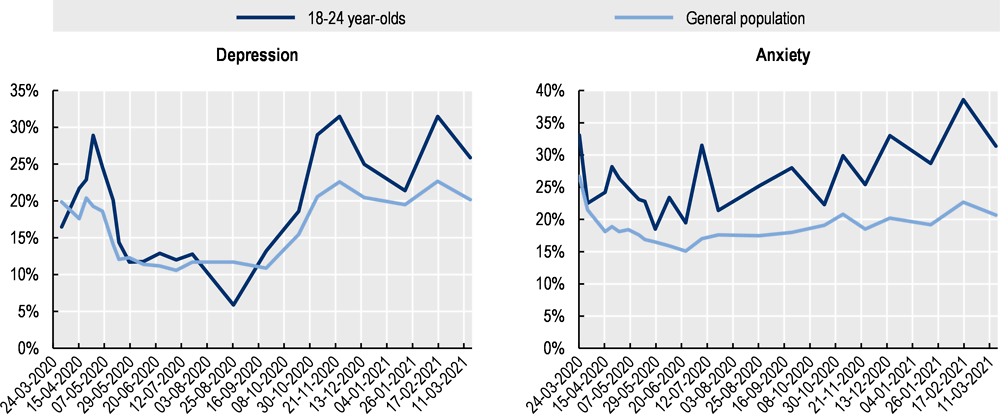
Note: General population is the adult population aged 18 and above.
Source: Santé Publique France, Enquête CoviPrev, https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-COVID-19.
Gender differences in the prevalence of anxiety and depression among young people appear to have persisted or widened in some OECD countries. Anxiety and depression, the two most common forms of mental health conditions, are more prevalent among young women based on self-reported measures (Van Droogenbroeck, Spruyt and Keppens, 2018[11]), whereas for conditions such as schizophrenia, prevalence is higher among young men. A study in the United Kingdom found that the prevalence of a serious mental health condition was highest in April 2020 among 16‑24 and 25‑34 year‑old women, at 35% and 36% respectively, and that the estimated effect of the pandemic on mental health had been the largest for women in these age groups (Xu and Banks, 2020[12]). Based on longitudinal data from 2015‑19, in the absence of the pandemic, it is estimated that the prevalence for the same groups would have been 18% and 14% respectively. By comparison, the prevalence of a serious mental health condition among 16‑24 year‑old men stood at 30% in April 2020. In Belgium, trend data shows a widening of gender differences in anxiety prevalence, but less so for depression. Symptoms of anxiety were already more common among young women before the crisis, but have increased significantly more among young women since the onset of the pandemic: in 2018, the gender differences in the share reporting symptoms of depression among 15‑24 year‑olds was 2.5 percentage points; in March 2021, the difference among 18‑29 year‑olds stood at almost 15 percentage points. For depression, in the period from June to December 2020, young men were more likely to report symptoms, although this trend was reversed in the latest survey from March 2021, which found that young women were more than 5 percentage points more likely to be reporting symptoms of depression (Sciensano, 2021[2]).
Particular attention should be given to the impact of the crisis on young people with pre‑existing mental health conditions or substance use disorders, individuals from lower income backgrounds and/or ethnic minority backgrounds, individuals who identify themselves as LGBT+ or gender diverse, as well as young carers. In a survey of 18‑30 year‑olds in the United States covering the period from April to June 2020, respondents identifying as sexual and gender minorities were more likely to report symptoms of depression than those not identifying as sexual and gender minorities (Kamal et al., 2021[13]). Similarly in the United Kingdom, among 11‑18 year‑olds, LGBTI+ respondents were more than twice as likely to report symptoms of depression as non-LGBTI+ respondents (Just Like Us, 2021[14]). Differences by ethnicity appear to follow a less clear trend. In the United Kingdom, a study of under-18 users of Kooth, a digital mental health support service, found that in March to May 2020, ethnic minority young people were significantly more likely to report symptoms of anxiety or depression and have suicidal thoughts than their white counterparts. The proportion of minority ethnic young users reporting symptoms of anxiety increased 11% year-on-year, significantly higher than the 3% increase among white young users (Kooth, 2021[15]). In contrast, in the United States, in a survey of 18‑30 year‑olds, Asian Americans were less likely to report mental health symptoms than White respondents, and Hispanic and Latinx respondents were less likely to report symptoms of severe anxiety than their White counterparts (Liu et al., 2020[16]).
Loneliness, a risk factor for poor mental health, is a particular burden for young people. Young people were already at high risk of loneliness pre‑crisis, but the situation has worsened, with containment measures continuing to limit in-person social interaction, especially for those living alone. Eurofound surveys show that 18‑34 year‑olds in the EU‑27 were the most likely to report feeling lonely “more than half of the time”, “most of the time” or “all of the time” in both April/May 2020 (32%) and June/July 2020 (28%), considerably above the general population share of 26% and 21% respectively (Eurofound, 2020[17]). In a survey in the United States in October 2020, almost 61% of 18‑25 year‑olds reported feeling lonely “frequently” or “almost all the time or all the time,” nearly double the average of 36% among all respondents (Weissbourd et al., 2021[18]). In New Zealand, prolonged loneliness among young people rose from 5.8% before the crisis to 20.8% during the lockdown, and decreased only slightly to 17.7% in July 2020 after the lockdown ended. This was the highest among all age groups and four times higher than the share experiencing post-lockdown loneliness among those aged 65 and above (Loneliness New Zealand, 2020[19]).
Factors that increase suicide risk such as chronic mental health conditions, social isolation, and financial difficulties, have also been exacerbated by the COVID‑19 crisis. Although evidence points to no increase in suicide rates in the early months of the pandemic, findings stratified by age are not widely available and longer-term impacts are still unclear (Pirkis et al., 2021[20]). One study in Japan found that the suicide rate among under 20‑year‑olds increased from July to October 2020 (Tanaka and Okamoto, 2021[21]), which runs counter to the trend of declining suicide rates among 15‑19 year‑olds in recent years across many OECD countries including Japan (Choi, 2018[22]). Survey results from Belgium, France and the United Kingdom also show suicidal ideation (i.e. suicidal thoughts) has increased significantly among young people (Wise, 2020[23]; Sciensano, 2021[2]; Santé Publique France, 2021[3]). Countries should continue to monitor rates of suicide stratified by age, as suicide is one of the leading causes of death among young people in many OECD countries, and continue to invest in suicide prevention policies targeting young people (OECD/European Union, 2020[24]).
Mental health services have seen heavy disruptions and increases in demand
Mental health services and support for children and adolescents have been heavily disrupted by the COVID‑19 crisis. A WHO survey in June‑August 2020 found that in more than three‑quarters of countries globally school mental health programmes were completely or partially disrupted, while in over 70% of countries child and adolescent mental health services experienced disruptions (WHO, 2020[25]). Workplace‑based mental health services saw a similarly high degree of disruption.
Young people experiencing mental health conditions in the United Kingdom have been reporting difficulty accessing mental health services during the pandemic, while demand for mental health services appears to be rising. A survey of 13‑25 year‑olds in the United Kingdom with a history of mental health needs conducted in January and February 2021 found that among those who expressed a need for support during the pandemic, only 54% had received some mental health support. Almost one-in-four (24%) reported having looked for support but not accessing any, in some cases due to barriers to accessing support online, and 22% reported having not looked for support (YoungMinds, 2021[26]). Monthly referrals to children and young people’s mental health services have also surged in England (United Kingdom) since the summer of 2020, up 72% in September 2020 compared to September 2019 after a fall in referrals in April 2020 (Children’s Commissioner, 2021[27]).
Other types of mental health services are also reporting increased usage across many OECD countries, with young people overrepresented among users and callers to mental health hotlines. While this may partially reflect a willingness of young people to interact online or over the phone, in part due to high levels of awareness, trends are consistent with the disproportionate impact the COVID‑19 crisis is having on young people’s mental health. In France, under 25‑year‑olds are the most common age group calling mental health hotlines such as SOS Amitié, with the organisation reporting a notable increase in young callers at the beginning of 2021, while in Colombia, around a third of callers to the COVID‑19 mental health hotline from April 2020 to March 2021 were 15‑29 year‑olds. Youth-specific hotlines and services are also reporting a surge in demand. In Ireland, the youth mental health charity ‘Jigsaw’ saw a 50% increase in demand for services in August 2020 compared to August 2019, and a 400% increase in traffic to the charity’s e‑mental health platform in the first six months of 2020.
Mental health services for children and adolescents moved swiftly to remote consultations in a number of countries to ensure continuity of treatment. In England (United Kingdom), in April 2020, 84% of child and adolescent mental health services were delivered in non-face‑to-face formats, compared to only 23% in 2019‑20; as of February 2021, 67% of child and adolescent mental health services were still being delivered in non-face‑to-face formats (NHS Benchmarking Network, 2021[28]). In a survey in Australia in June 2020 of users of ‘headspace’ centres, which provide mental health support for 12‑25 year‑olds, 78% agreed or strongly agreed that the mode of service they received had been appropriate for their needs, and around half indicated they would like to use telehealth again in the future (Headspace, 2020[29]). While not all young people have been comfortable using digitally-enabled services for support, for many young people, it has played an important role in ensuring service continuity.
Disruptions to schooling affect young people’s mental health
The lives of young people continue to be severely disrupted by many of the measures put in place to limit the spread of the virus. By the end of March 2020, 35 of 38 OECD countries had put in place some form of school closures, including nationwide closures in 31 countries (Figure 2). While OECD countries have sought to minimise school closures, 28 OECD countries still had partial or full closures in place at the end of March 2021. As much as two‑thirds of an academic year of in-person education has already been lost on average worldwide due to school closures. The duration of closure of educational institutions has also often differed across age groups and grades, with countries tending to prioritise reopening in-person schooling for younger students, whereas education for older students has more likely remained online.
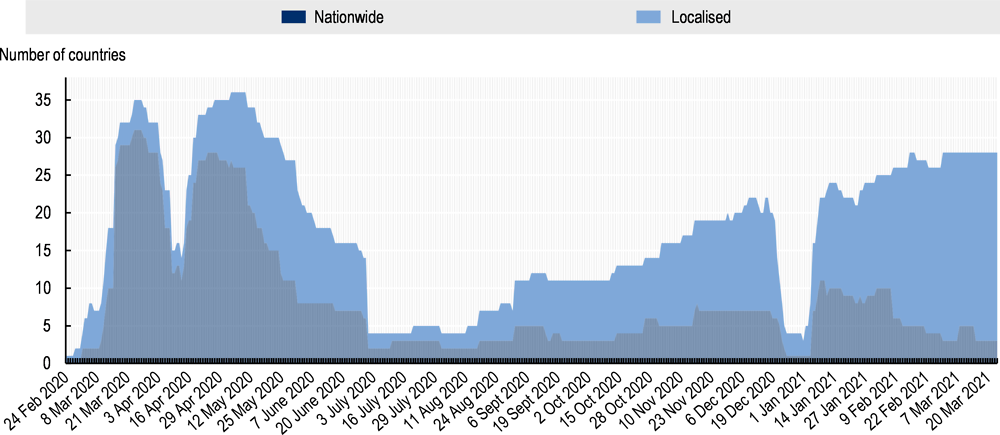
Note: This figure covers educational institutions from early childhood education to tertiary education. Localised school closure refers to school closures of some levels of education only and/or for some subnational entities. The low number of closures in early April 2020 and end December 2020 to January 2021 is the result of holidays, which are not categorised as closures. Information on data for Israel: https://oe.cd/israel-disclaimer
Source: UNESCO (2021[30]), Global School Closures COVID‑19, https://data.humdata.org/dataset/global-school-closures-COVID-19.
School closures have had significant implications for the mental health of young people as schools are not just places where students develop and progress their academic skills. The shift to remote learning has resulted in an erosion of many protective factors that attending school offers, including daily routines, social contact, social and emotional support from teachers, sense of belonging to a community, and access to physical exercise. While many young people have been able to maintain connection with peers through digital means, the loss of in-person interaction resulting from school closures could have long-term negative consequences for mental health.
The impacts of school closures are disproportionately falling on young people from disadvantaged backgrounds. While not directly comparable, school holidays can partially replicate the implications of prolonged periods of disrupted schooling that have resulted from the crisis. Evidence from the United States suggests summer holidays contribute to a widening of learning gaps, while a study in Wales found that young people from lower-income backgrounds are more likely to experience increases in isolation, hunger and sedentary behaviour during summer holidays (Morgan et al., 2019[31]), all risk factors that could contribute to a deterioration of mental health. While schools quickly turned to remote learning, wide disparities continue to exist in access to internet and digital devices, as well as to a quiet place to study, all prerequisites for online learning. Recognising the unequal effects of school closures, in some countries, such as in Austria or the United Kingdom, measures were put in place to ensure children of essential workers or in vulnerable situations could continue to physical attend school even during periods of closure.
The closure of schools and educational institutions has also meant mental health issues among young people risk going unidentified. Schools serve as a primary point of access to mental health services and promotion for many young people, and front-line actors such as teachers are often well-placed to identify early symptoms of mental health issues such as repeated absence and truancy, difficulty concentrating and behavioural changes in day-to-day school activities. School closures have already disrupted access to mental health services as referrals from schools are an important pathway to child and adolescent mental health services, while in other cases, teachers may encourage parents to seek mental health support for their children. For example, child and adolescent mental health services in England (United Kingdom) received far fewer referrals when schools were closed: 53% fewer referrals in April 2020 compared to 2019, and still 10‑24% lower referrals when schools were closed in January and February 2021 (NHS Benchmarking Network, 2021[28]).
A bleak labour market is putting more pressure on young people’s mental health
Young people are being disproportionately affected by the labour market impacts of the COVID‑19 crisis, which could have significant mental health consequences as long-term unemployment is a risk factor for poor mental health throughout the life course. After a decade of decline, the OECD total unemployment rate among 15‑24-year-olds rose sharply from 11.3% in February 2020 to 18.9% in May 2020, and while it has recovered somewhat since, remains above pre-crisis levels at 13.3% as of March 2021. This increase is driven both by young people in employment being more likely to lose their jobs, and new entrants to the labour market finding it difficult to secure entry-level jobs with hiring rates down. Young workers generally hold less secure jobs and make up a large proportion of jobs in customer-facing industries such as accommodation, tourism, and food services – the sectors strongly affected by the crisis – while also often being the first to be let go as they tend to have shorter tenure and less company-specific skills (OECD, forthcoming[32]). Training pathways that help connect young people to work such as internships, apprenticeships, and temporary work have also often been suspended by struggling companies, placing additional pressures on the school-to-work transition. Joblessness has also resulted in significant income losses, resulting in financial insecurity, another risk factor for poor mental health. These pressures have also affected students, such as those reliant on part-time work to fund their education and living costs.
A mental health-in-all policies response to the youth mental health crisis
Addressing the emerging youth mental health crisis requires a mental-health-in-all policies approach that considers the interlinkages of mental health with other policy areas including education, youth and employment policies outlined in the OECD Recommendation on Integrated Mental Health, Skills, and Work Policy. Ensuring and maintaining access to quality education and work for young people should be seen as a public health priority and an economic necessity. At the same time, expanding availability of mental health services is an immediate priority, as well as embedding mental health support in educational and workplace settings, in public employment services and in the social protection system.
Supporting students to remain in school and in education should be a priority
As disruptions to learning due to the COVID-19 crisis drag on, students are at growing risk of becoming disengaged and leaving education altogether. Early school leavers are at increased risk of poor mental health, just as young people with mental health conditions tend to have poorer educational outcomes. UNESCO projected in June 2020 that 24 million learners from pre‑primary to tertiary levels of education were at risk of dropping out of school, or not having access to schooling for the rest of the year (UNESCO, 2020[33]). In Italy, a survey commissioned by Save the Children found that around 28% of students had claimed that at least one of their classmates had stopped attending classes, which could result in the equivalent of around 34 000 students leaving school early (Save the Children, 2021[34]).
Even from before the crisis, students experiencing mental health conditions were at elevated risk of early school leaving. It is crucial that policies are put in place to ensure such students are supported through to the end of their education including by resuming school-based mental health services and providing mental health training to teachers. Keeping young people in school also protects against poor mental health, and brings benefits for both the individual and society in terms of improved long-term employment prospects. There are concerns that even if students can remain in school, learning loss could result in students repeating years or grades. Across OECD countries, students indicating mental distress are 35% more likely to have repeated a grade and remain at elevated risk of early school leaving (OECD, forthcoming). A number of countries have loosened requirements for examinations and progression to the next grade to support young people in continuing their education. As schools reopen and mental distress remains elevated, schools could consider emphasising resilience‑building in curricula, including the development of social and emotional skills, and implement a whole‑of-school approach to promoting good mental health among students (Burns and Gottschalk, 2019[35]). In Canada, School Mental Health Ontario prepared guides targeted at educators, students, and parents on how to promote mental health and well-being in school reopening measures, which was incorporated into the region’s strategy for reopening schools ahead of the 2020‑21 academic year.
Given that around half of young adults pursue post-secondary education across OECD countries, tertiary educational institutions are also well-placed to promote mental health and provide timely support. Even before the pandemic, it was widely reported in a number of countries, including the United Kingdom, Canada, and the United States, that students in tertiary education faced difficulties accessing mental health support. In a few OECD countries, governments have taken action to increase mental health support in universities. In France, the government has increased the capacity of integrated mental health and education support available to university students, and is accelerating the rollout of mental health first aid programmes in universities. In the United Kingdom, while the legal responsibility to support students with mental health conditions lies primarily with the tertiary institutions (Hubble and Bolton, 2020[36]), the government also funds Student Space, launched in June 2020 to provide online mental health services and support for university students in Wales and England.
Employment, workplace and social protection policies can cushion the mental health impact of the crisis for young people
Young people are bearing a disproportionate burden of the labour market impacts of the crisis, and countries must take swift action to prevent a youth unemployment crisis. Governments across many OECD countries have put in place wage subsidies targeted at entry-level jobs and apprenticeships (OECD, forthcoming[32]). As employment can protect against poor mental health, policies to promote hiring of young jobseekers can contribute to better mental health outcomes for young people today and throughout the life course. An area for further action is job quality for young people. While it is well-known that meaningful work contributes positively to mental health, there are often few initiatives to improve quality of jobs available to young people in youth employment strategies (OECD/ILO, 2020[37]).
Policies in the workplace also have a key role in promoting better mental health for young people. Beyond the challenge of transitioning from learning-to‑earning, young workers often experience longer working hours, less autonomy over work organisation and lower job security, all of which can contribute to deteriorating mental health. Investment in awareness-raising campaigns and the promotion of mental health training for line managers and executives should be considered as policy options to promote better mental health among all workers, and especially young workers, as effective management can reduce risk factors for poor mental health and form the foundation of mentally healthy work environments. For young people, working remotely may pose additional challenges for mental health such as managing work-life balance and elevated risk of isolation, which need to be addressed with new approaches to workplace mental health protection (OECD, 2021[38]).
Reinforcing mental health services within public employment services should also be a priority, and proactive outreach in collaboration with local stakeholders will be necessary as young people often do not get in touch with public employment services upon falling out of education or the labour market. All EU countries have already agreed to the reinforced Youth Guarantee in October 2020, which commits them to ensuring that young people under age 30 receive a good quality offer of employment, continued education, apprenticeship or training within four months of leaving the education system or labour market. While supporting people back into employment should remain a priority, participation in active labour market programmes can also replicate some aspects of employment and cushion the impact of unemployment on mental health (OECD, 2021[38]). Access to integrated mental health and employment support for young people experiencing mental health issues must be urgently expanded within public employment services. Even prior to the crisis, despite evidence that integrated employment and mental health support is effective at promoting employment of young jobseekers experiencing mental health issues, access to such support was lacking across most OECD countries.
Increasing mental health support to young people amidst the pandemic
Mental health hotlines, often newly set up in response to the COVID‑19 crisis, are playing an important role in providing emergency support to young people and should be maintained. Most OECD countries have introduced or expanded existing mental health support phone hotlines (OECD, forthcoming[39]). Many hotlines are operated by the non-profit sector, and would benefit from increased public investment to allow them to continue through the immediate COVID‑19 crisis, and beyond.
Youth centres are well-placed to offer integrated support to young people to support their mental health, but need to be adequately resourced. In Australia, ‘headspace’ centres provide integrated support for 100 000 people aged 12‑25 each year with an emphasis on mental health interventions, while in Finland, the government is expanding its programme to provide low-threshold psychosocial support through one‑stop Ohjaamo youth centres. Youth organisations already recognise that supporting the mental health of young people should be a key priority. When asked about the impacts of the COVID‑19 crisis in an OECD survey in April 2020, youth organisations expressed greatest concern about mental health followed by employment and disposable income (OECD, 2020[40]).
Governments have also sought to increase access to mental health support specifically for young adults through one‑off schemes. France introduced the “chèque psy” scheme in February 2021, which allows university students to receive up to three consultations with a mental health specialist for free, which was later followed in April 2021 by a scheme offering up to 10 free sessions from a mental health specialist for 3‑17 year‑olds. The United Kingdom also recently dedicated GBP 13 million in funding to provide tailored mental health services for 18-25‑year‑olds that bridge the gap between child and adolescent mental health services and adult mental health services and to support young adults through the pandemic.
Supporting young people’s mental health needs to be part of a cross-sectoral policy response to tackle the mental health impacts of the COVID-19 crisis, as discussed in the policy brief on “Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response” (OECD, 2021[38]). The importance of strengthening mental health support in youth support systems will also be highlighted in the OECD’s Youth Action Plan, which is currently being updated.
Acknowledgements
This policy brief was prepared by Shunta Takino, Emily Hewlett, Yuka Nishina and Christopher Prinz. Valuable comments were provided by various colleagues from the OECD, including especially Monika Queisser, Veerle Miranda, Stefano Scarpetta, Mark Pearson, Tracey Burns, Francesca Gottschalk, Elettra Ronchi, Andras Molnar, Gráinne Dirwan, Lara Fleischer, Olivier Thévenon and Masato Hayashikawa.
For more details on the data sources and the measurement methodology, as well as further policy analysis of countries’ responses to the mental health impact of the COVID‑19 crisis, please see the forthcoming OECD Working Paper on ‘Tackling the mental health impact of the COVID‑19 crisis through an integrated whole‑of-society response’.
References
[35] Burns, T. and F. Gottschalk (eds.) (2019), Educating 21st Century Children: Emotional Well-being in the Digital Age, Educational Research and Innovation, OECD Publishing, Paris, https://dx.doi.org/10.1787/b7f33425-en.
[27] Children’s Commissioner (2021), The state of children’s mental health services 2020/21, Children’s Commissioner for England, https://www.childrenscommissioner.gov.uk/wp-content/uploads/2021/01/cco-the-state-of-childrens-mental-health-services-2020-21.pdf (accessed on 4 May 2021).
[22] Choi, A. (2018), “Emotional well-being of children and adolescents: Recent trends and relevant factors”, OECD Education Working Papers, No. 169, OECD Publishing, Paris, https://dx.doi.org/10.1787/41576fb2-en.
[9] Delmastro, M. and G. Zamariola (2020), “Depressive symptoms in response to COVID-19 and lockdown: a cross-sectional study on the Italian population”, Scientific Reports, Vol. 10/1, http://dx.doi.org/10.1038/s41598-020-79850-6.
[17] Eurofound (2020), Living, working and COVID-19 series, Publications Office of the European Union.
[10] Eurostat (2014), European Health Interview Survey Wave 2.
[8] Fukase, Y. et al. (2021), “Depression, risk factors, and coping strategies in the context of social dislocations resulting from the second wave of COVID-19 in Japan”, BMC Psychiatry, Vol. 21/1, http://dx.doi.org/10.1186/s12888-021-03047-y.
[29] Headspace (2020), Young people’s experience of telehealth during COVID-19, https://headspace.org.au/assets/Uploads/Telehealth-Client-Experience-FINAL-8-10-20.pdf.
[36] Hubble, S. and P. Bolton (2020), Support for students with mental health issues in higher education in England, https://commonslibrary.parliament.uk/research-briefings/cbp-8593/.
[14] Just Like Us (2021), LGBT+ young people twice as likely to experience depression, anxiety and panic attacks, https://www.justlikeus.org/single-post/lgbt-young-people-twice-likely-depression-anxiety-panic-attacks (accessed on 29 April 2021).
[13] Kamal, K. et al. (2021), “Psychiatric impacts of the COVID-19 global pandemic on U.S. sexual and gender minority young adults”, Psychiatry Research, Vol. 299, p. 113855, http://dx.doi.org/10.1016/j.psychres.2021.113855.
[15] Kooth (2021), Week 14: How Covid-19 is Affecting the Mental Health of Young People in the BAME Community, https://xenzone.com/wp-content/uploads/2020/06/BAME_infographic_June-2020_WEB-v2.pdf (accessed on 1 May 2021).
[16] Liu, C. et al. (2020), “Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health”, Psychiatry Research, Vol. 290, p. 113172, http://dx.doi.org/10.1016/j.psychres.2020.113172.
[19] Loneliness New Zealand (2020), Prolonged loneliness in New Zealand before, during, and after lockdown, https://loneliness.org.nz/wp-content/uploads/2020/07/Prolonged-loneliness-in-New-Zealand-1-Aug-2020.pdf.
[31] Morgan, K. et al. (2019), “Socio-Economic Inequalities in Adolescent Summer Holiday Experiences, and Mental Wellbeing on Return to School: Analysis of the School Health Research Network/Health Behaviour in School-Aged Children Survey in Wales”, International Journal of Environmental Research and Public Health, Vol. 16/7, p. 1107, http://dx.doi.org/10.3390/ijerph16071107.
[4] NCHS (2019), National Health Interview Survey, https://www.cdc.gov/nchs/data/nhis/earlyrelease/ERmentalhealthbyage-508.pdf.
[28] NHS Benchmarking Network (2021), Covid 19 Monthly Tracker Mental Health, Learning Disability & Autism Services February 2021.
[38] OECD (2021), “Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/0ccafa0b-en.
[40] OECD (2020), “Youth and COVID-19: Response, Recovery and Resilience”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/c40e61c6-en.
[32] OECD (forthcoming), “Supporting young people through the COVID-19 crisis and beyond”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris.
[39] OECD (forthcoming), “Tackling the mental health impact of the COVID-19 crisis through an integrated whole-of-society response”, OECD Health Working Papers, OECD Publishing, Paris.
[24] OECD/European Union (2020), Health at a Glance: Europe 2020: State of Health in the EU Cycle, OECD Publishing, Paris, https://dx.doi.org/10.1787/82129230-en.
[37] OECD/ILO (2020), Helping Disadvantaged Youth: Progress and Policy Action towards the Antalya G20 Youth Goal, https://www.ilo.org/wcmsp5/groups/public/---dgreports/---ddg_p/documents/publication/wcms_742291.pdf.
[6] ONS (2020), Coronavirus and depression in adults, Great Britain: June 2020, https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusanddepressioninadultsgreatbritain/june2020.
[20] Pirkis, J. et al. (2021), “Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries”, The Lancet Psychiatry, http://dx.doi.org/10.1016/s2215-0366(21)00091-2.
[3] Santé Publique France (2021), CoviPrev : une enquête pour suivre l’évolution des comportements et de la santé mentale pendant l’épidémie de COVID-19, https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-covid-19 (accessed on 19 February 2021).
[34] Save the Children (2021), Rapporto sui primi sei mesi di attivita’: Dove sono gli adolescenti? La voce degli studenti inascoltati nella crisi [Report on the first six months: Where are the teenagers? The voice of unheard students in the crisis].
[2] Sciensano (2021), Sixième enquête de santé COVID-19, https://doi.org/10.25608/j877-kf56.
[5] Sciensano (2020), Première enquête de santé COVID-19, https://doi.org/10.25608/ydnc-dk63.
[7] Statistics Canada (2020), Mental health of Canadians during the COVID-19 pandemic, https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2020039-eng.htm (accessed on 1 April 2021).
[21] Tanaka, T. and S. Okamoto (2021), “Increase in suicide following an initial decline during the COVID-19 pandemic in Japan”, Nature Human Behaviour, http://dx.doi.org/10.1038/s41562-020-01042-z.
[1] U.S. Census Bureau (2021), Indicators of Anxiety or Depression Based on Reported Frequency of Symptoms During Last 7 Days, https://data.cdc.gov/NCHS/Indicators-of-Anxiety-or-Depression-Based-on-Repor/8pt5-q6wp (accessed on 29 March 2021).
[30] UNESCO (2021), Global School Closures COVID-19, https://data.humdata.org/dataset/global-school-closures-covid19 (accessed on 25 March 2021).
[33] UNESCO (2020), How many students are at risk of not returning to school?, https://unesdoc.unesco.org/ark:/48223/pf0000373992 (accessed on 5 March 2021).
[11] Van Droogenbroeck, F., B. Spruyt and G. Keppens (2018), “Gender differences in mental health problems among adolescents and the role of social support: results from the Belgian health interview surveys 2008 and 2013”, BMC Psychiatry, Vol. 18/1, http://dx.doi.org/10.1186/s12888-018-1591-4.
[18] Weissbourd, R. et al. (2021), Loneliness in America: How the Pandemic Has Deepened an Epidemic of Loneliness and What We Can Do About It, https://static1.squarespace.com/static/5b7c56e255b02c683659fe43/t/6021776bdd04957c4557c212/1612805995893/Loneliness+in+America+2021_02_08_FINAL.pdf.
[25] WHO (2020), The impact of COVID-19 on mental, neurological and substance use services, https://www.who.int/publications/i/item/978924012455 (accessed on 3 December 2020).
[23] Wise, J. (2020), “Covid-19: Suicidal thoughts increased in young adults during lockdown, UK study finds”, BMJ, p. m4095, http://dx.doi.org/10.1136/bmj.m4095.
[12] Xu, X. and J. Banks (2020), The mental health effects of the first two months of lockdown and social distancing during the Covid-19 pandemic in the UK, The IFS, http://dx.doi.org/10.1920/wp.ifs.2020.1620.
[26] YoungMinds (2021), Coronavirus: Impact on young people with mental health needs, https://youngminds.org.uk/media/4350/coronavirus-report-winter.pdf (accessed on 6 March 2021).
Contact
Stefano SCARPETTA (✉ stefano.scarpetta@oecd.org)
Mark PEARSON (✉ mark.pearson@oecd.org)
Shunta TAKINO (✉ shunta.takino@oecd.org)