Abstract
Pandemic preparedness and response are quintessential “global public goods”: unless the new coronavirus is controlled everywhere, the risk of pandemic resurgence remains. This paper presents the key role of development finance in helping developing countries’ health systems prepare and respond to outbreaks. Yet, the global architecture is proving insufficient – and the risk is great that developing countries will be deeply affected by the direct consequences of the outbreak.
Development finance for health requires a shift in support towards more focused investments in transnational activities. It also needs to move from targeted support to specific communicable diseases, to more systemic resources to prevent chronic diseases and meeting the challenge of universal health coverage.
Development co-operation for health on the frontlines
Financing the health sector is a long-standing development challenge. The World Health Organization (WHO) estimates that an additional USD 370 billion per year are needed for primary health care to achieve the SDG targets on universal health care (UHC) in low- and middle-income countries (WHO, 2019[2]). Development co-operation continues to play an important role in this sector, with official development assistance (ODA) to health reaching USD 26 billion in 2018. Development assistance to health represented 12% of total health spending in lower middle-income countries, and 29% for low-income countries. As countries transition and reach higher levels of income, their dependency on external financing declines, but differences in health coverage remain.
Despite increased mobilisation after the 2014-2016 Ebola crisis, investment in pandemics preparedness and response has been insufficient. In light of the “global public good” nature of such spending, it is in countries’ own interest to spend more and better on pandemic preparedness in other countries. Setting up systems to track such flows can help to do so much more effectively.
Global mobilisation to fight the health consequences of COVID-19 has been impressive but more should be done. Development co-operation has a key role to play to limit the spread of the disease in low and middle-income countries. In addition to raising more funds, it can focus on creating and spreading knowledge of solutions, and promote best practices in the response.
The current crisis engulfs health systems as a whole, especially in low-income countries where they are most fragile. Health It is important to step up support to universal health coverage and avoiding the disruption in other critical healthcare provision (maternal and child care, other communicable and non-communicable diseases).
Development co-operation will be on the frontline of the COVID-19 battle in developing countries. As the economic and public health crises progressively hit developing countries, including the most in need, domestic resources will be strained, and external financing will be further solicited. It will be important to ensure that immediate responses to the crisis are put in place, and health systems are consolidated to build resilience to future shocks. There are other aspects where development finance will play a major role, in particular as a financial safety net, but this note focuses on aspects specific to the health sector.
The international community was prompt to respond with a number of statements calling for action. On 9 April 2020, the OECD Development Assistance Committee (DAC) issued a statement calling for “sustained action by many actors to address the immediate public health and humanitarian crisis and simultaneous support for economic, environmental and social resilience” (DAC/OECD, 2020[3]). The G20 Leaders on 26 March 2020 agreed that they “consider that consolidating Africa’s health defence is key for the resilience of global health. We will strengthen capacity building and technical assistance, especially to at-risk communities,” and that they stood “ready to mobilise development and humanitarian financing.”1
Will development co-operation be up to the COVID-19 challenge? The immediate global response from multilateral and bilateral providers of development co-operation – including both health-related measures and broader support to economic activity – is estimated at around USD 250 billion (ODI, 2020[4]). Humanitarian funding led by the United Nations (UN) system aimed to raise more than USD 2 billion for immediate needs, in addition to a request for funding of USD 625 million for the World Health Organization. Multilateral development banks also readied large amounts of resources with about USD 120 billion in loans and grants. The World Bank mobilised USD 2 billion in early April specifically directed to health, and committed to additional USD 160 billion over the next 15 months.
Bilateral donors also responded, with for example the European Union redirecting over EUR 15 billion to tackle the virus, and the French Development Agency (AFD) providing EUR 1.5 billion including technical support on epidemiological surveillance and response plans, and general support for health systems. In the longer run, there is a risk that the collapse of gross domestic product (GDP) growth in advanced economies could strain ODA budgets. This would be damaging, especially as all other inflows are collapsing. The OECD (2020[5]) highlights that ODA has proven to be a key countercyclical resource and was stable during the financial crisis of 2008 before declining slightly in 2011 and 2012. During the current crisis, only a strong political commitment to global solidarity would safeguard and even increase ODA.
Given the global emergency, development co-operation should focus on identified “quick wins” and successful models while also ensuring that funds are not diverted from essential services that need continued support and cannot be delayed, such as maternal health. Official development assistance can provide essential resources to fight the devastating effects of the crisis, and should serve as a catalyst of other sources of financing. Members of the DAC and other development partners can take steps to promote those solutions including:
Better monitor and address gaps in pandemic preparedness. It will be important to improve tracking of financing for pandemic preparedness, for example by including it as a separate item under the Creditor Reporting System of the OECD. This would facilitate holding development partners accountable for the commitments they make. DAC members and other development partners can also support pandemic preparedness by using the Joint External Evaluation mechanism (JEE) or other preparedness indicators as one of the criteria to guide donor funding, or by providing technical support to help countries improve preparedness.
Use and share technical expertise on “fixed-cost” items, including epidemiological modelling, support to the response, both at the country- and region-levels of intervention.
Promote best practices in financing policy and financial responses to the crisis. The DAC could provide one venue to discuss sectors of intervention where development finance providers could identify synergies in fighting the impacts of COVID-19 and strengthening existing development efforts. This could include investing in urban infrastructure with more distance between people, providing WASH facilities, developing contactless payments, etc. Those solutions should be identified, shared, and disseminated.
Use all available channels: Bilateral donors have the advantage of being able to rely on a variety of networks: foundations, civil society and community groups, research centres, etc., which can provide entry points in disseminating best practices. Development finance institutions should also play a role as responsible investors – adopting best practices in companies they invest in to slow the spread of the virus.
Investing in the “first line of defence”, or preparedness, is not enough. Development co-operation should also invest in the “second line of defence” – health systems. The COVID-19 crisis is a threat to domestic health systems that are already short of resources in many developing countries. The COVID-19 crisis may overwhelm health systems and challenge their capacity to handle basic functions, and it could also lead countries to shift their resources away from efforts to tackle other diseases and services.
In light of the nexus between COVID-19 and other diseases, it is important that international support to address COVID-19, including from the DAC, is delivered in a way that protects and reinforces existing health priorities, and does not divert attention and resources. For instance, disruptions to essential health services and access to food could lead to large increases in child and maternal mortality which had also been observed during the Ebola crisis in Guinea, Liberia and Sierra Leone (Davies and Bennett, 2016[7]) and (Roberton et al., 2020[6]) for a modelling study on COVID‑19 specifically. Health security efforts for prevention, alert, and response to disease outbreaks such as COVID-19 need to be pursued in parallel with health system strengthening, as part of a mutually reinforcing approach to developing resilient health systems. Lockdown policies can also reduce the use of healthcare services, and require enhanced monitoring of vulnerable populations. Synergies notably exist between achieving universal health coverage and enhancing health security. For example, universal health coverage secures against outbreaks through high immunisation coverage, provides early alert by facilitating access to healthcare for the entire population, women and men, and better response thanks to reliable infrastructure and healthcare workforce.
Tackling coronavirus (COVID-19): Was development co-operation sufficiently prepared and responsive?
The threat of pandemics had been highlighted by a number of public voices for years. The frequency of pandemic events has increased in the past decades (Ross et al., 2015[8]) and a number of major actors and observers of international health development co-operation, such as Bill Gates, repeatedly expressed their concern that “we are not prepared for the next epidemics”. In 2017, an article by Duke Global Health Institute and the Coalition for Epidemics Preparedness Innovations (CEPI) pointed out to the unfortunate dynamics: “The global pandemic response has typically followed cycles of panic followed by neglect. We are now, once again, in a phase of neglect, leaving the world highly vulnerable to massive loss of life and economic shocks from natural or human-made epidemics and pandemics” (Yamey et al., 2017[8]).
SDG 3, target D, outlines the responsibility of the international community to prepare for pandemics. It calls for the strengthening of “the capacity of all countries, in particular developing countries, for early warning, risk reduction, and management of national and global health risks”. The Ebola crisis of 2014-2016 helped change the international community’s apprehension of global health crises, with a myriad of new funds and facilities. For example, total concessional disbursements per year from DAC members for infectious diseases (excluding Tuberculosis and Malaria) increased from USD 861 million in 2014 to USD 1.36 billion in 2017, an increase by almost 58%. Using a broader measure including ODA and additional international spending on product development for diseases of poverty, Schäferhoff et al. (2019[10]) find a larger increase of 25% between 2013 and 2015, to USD 7.3 billion. However, current financing efforts remain insufficient to respond to crises of the magnitude of COVID-19 that has drastically impacted both developed and developing countries.
Financing will be one major force of the war against COVID-19. With scarce resources, the effectiveness of responses and spending will matter even more to maximise the impact of scarce resources like official development assistance – hence the need for greater co-operation across development actors and local health systems. The multilateral system and forums for co-ordination of development assistance, such as the OECD-DAC, will be central for the design and implementation of a better co-ordinated and more efficient response to the crisis, pooling of resources and avoiding duplication of efforts. Each country’s needs will differ and require different solutions to be decided and implemented in partnership with local actors.
Was the international development co-operation community sufficiently prepared for the COVID-19 crisis? Not quite…
The 2014-16 Ebola crisis was a major factor for increased awareness of the risks of pandemics in the international community. It both triggered the creation of innovative initiatives for global health issues, and contributed to raising commitments of bilateral development co-operation providers (especially the United States) and multilateral actors in favour of global health security.
How global health security was reformed in the wake of the Ebola crisis
Being prepared is the most time and cost-effective way to handle global health risks. Estimates place the expected annual loss from pandemics risk at 0.6% of global GDP, or about USD 500 billion per year (Fan, Jamison and Summers, 2018[11]).2 The economic and social costs of Ebola were estimated at USD 53 billion, most of which represents lives lost (Huber, Finelli and Stevens, 2018[12]), and early estimates of output losses over 2020 and 2021 from COVID-19 reach USD 12.5 trillion globally (Gopinath, 2020[13]).
Taking precautionary measures to manage and pre-empt these recurring risks is important. This would allow faster responses to crises, by unlocking resources in a more streamlined way: humanitarian aid can be slow to mobilise, as was the case during the Ebola outbreak. In its aftermath, a number of rapid response mechanisms were established (Box 2.1), which contributed to improve preparedness.
The World Bank uses four main facilities to finance the reaction to pandemics, three of which were pre-existing disaster financing mechanisms that were extended after 2015 to include health-related events.
The Pandemics Emergency Financing Facility (PEF) aims to provide surge funding before humanitarian assistance can be mobilised. It has two windows of disbursement:
The cash window is funded by traditional donor contributions, and disburses when an outbreak meets certain thresholds, subject to independent expert advice;
The insurance window, also known as “pandemic bonds”, is an innovative attempt to define a high-yielding financial instrument to attract private investors, disbursing according to predetermined thresholds. Investors lose part of their principal when those are crossed.
Catastrophe Deferred Drawdown Options (Cat-DDOs) provide rapid liquidity in cases of catastrophes – including public health-related events since 2016. Their size is limited at the minimum of USD 250 million or 0.5% of GDP for International Development Association (IDA) countries; and USD 500 million or 0.25% of GDP for IBRD countries. Eight countries have health-related triggers in their Cat-DDOs.
Contingency Emergency Response Components (CERC): A CERC of the immediate response mechanism provides access to a country’s undisbursed IDA allocation to respond to an emergency, embedded to a project, which avoids the need for restructuring.
The Crisis Response Window (CRW) provides IDA countries with resources to respond to emergencies. In the case of health events, it is triggered when countries declare a national public health emergency and the WHO declares that the outbreak is of potential international importance.
The World Health Organization has also dedicated funds for pandemics preparedness and response:
Health Emergency Programs is the umbrella for all preparedness and response activities of the WHO – including technical assistance to countries for preparedness, humanitarian financing (for example health programmes during refugee crises), etc. The budget is of about USD 500 million, funded by the general WHO budget.
Contingency Fund for Emergencies (CFE) has an objective of enabling the WHO to take rapid action after an outbreak – sometimes within 24 hours. Between 2015 and 2019, it funded 78 emergency allocations, for a budget of about USD 120 million
The International Monetary Fund (IMF) also expended its Catastrophe Containment and Relief Trust (CCRT) to include health emergencies as well as natural disasters.
Source: World Bank Group (2019[13]), “Pandemic Preparedness Financing – Status Update”, September, https://apps.who.int/gpmb/assets/thematic_papers/tr-4.pdf
In the aftermath of the Ebola crisis, the international community launched a number of initiatives to better assess epidemics preparedness. The Joint External Evaluation mechanism (JEE), launched in 2016 by the WHO provides an effective mechanism for conducting a systematic evaluation of a country’s preparedness capabilities and infrastructure, enabling clear identification of gaps and areas for improvement. More than 90 countries were evaluated as part of the JEE process by 2020, revealing important gaps in preparedness. Most worryingly in the current context, 25 countries in Africa were deemed “not ready” in the synthetic score developed by the organisation Prevent Epidemics using JEE data for the subcategory “emergency response operations”, and 16 with “work to do”, and 1 “better prepared (4 had no JEE).
However, progress has remained limited. While the JEE index has been widely applied in many countries, little has been done when gaps were identified. Often, there was no costing of the necessary investment suggested by the JEE, nor robust financing plans attached to it, whether domestic or external. In a recent report, the Global Pandemics Monitoring Board showed that there was no progress in 3 of the 6 preparation areas, all linked to financing: countries have rarely integrated a domestic revenue mobilisation strategy to preparedness, external financing remains limited and poorly targeted, and those indicators are not used in monitoring by multilateral banks and other financing organisations (World Bank Group, 2019[13]).
Pandemic preparedness is prone to a “panic-neglect cycle”, where health donors and national policy-makers rush to allocate emergency funding, which soon ebbs out once a disease seems to be under control, despite risks of resurgence (Yamey et al., 2020[14]). Therefore, mechanisms need to be put in place to incentivise domestic stakeholders to keep investing in pandemic preparedness.
Given the rapidity with which diseases cross borders, recent initiatives have stressed the need for co-ordination capacities at the regional level. Both in Africa and in Asia, regional initiatives have recorded significant support after 2015. The African CDC was launched officially in 2017, with support from the World Bank and the People’s Republic of China among others, and is playing an important co-ordination role in the current coronavirus crisis. IDA also funded the large REDISSE3 programme in West Africa, a USD 400 million project (over five years) to provide co-ordination in health security, surveillance, early-warning systems, and technical capacity to test, in collaboration with the Institut Pasteur. In Asia, the Indo-Pacific Centre for Health Security, supported by Australia with AUD 200 million, is also based on the regional model. These initiatives highlight the gains associated with co-ordination at regional level.
Innovations led to more financing after 2015, but impetus had since slowed down
The aforementioned efforts improved the ability of international institutions to respond to major public health crises, but never managed to reach the levels of ambition needed. Moreover, the global health security system remains fragmented,4 and not well integrated in countries’ planning initiatives. The response mechanisms in place have been subject to criticism.
The World Bank’s “Pandemic Emergency Funding” has not offered the flexibility it was aiming for. Its cash window is relatively limited and the insurance window (so-called “Pandemics Bonds”) was too slow and complex to trigger. This criticism has been made especially in the context of the Ebola re-emergence in the Democratic Republic of Congo in 2019,5 when the requirements to trigger the bond were not met. Indeed, even for the COVID-19 crisis, bonds were triggered only on 19 April, well after countries sought to purchase necessary equipment, undermining the flexibility of the instrument. By mid-May, the World Bank’s emergency operations including through its COVID-19 fast track facility and other forms of finance had been extended to 100 developing economies (World Bank, 2020[16]).
The WHO Contingency Fund for Emergencies has a capitalisation target of USD 100 million in windows of three months that should be replenished through flexible voluntary contributions, but remains underfunded. The situation improved recently, but as of March 2019, only 77% of the WHO Health Emergencies Programme was funded – a shortfall of over USD 100 million. There is also a relative narrowness of the donor base for major preparedness programmes: three donors support the majority of the WHO CFE (Japan, Germany, and the United Kingdom) and, there are only three donors for the World Bank’s PEF (Japan, Germany, and Australia).
Finally, although progress has been made in raising awareness about preparedness through the JEE exercise, countries’ responsiveness to filling the gaps has been limited. One area of important reform could be to make pandemics preparedness a part of macroeconomic surveillance. The current COVID-19 crisis clearly shows that pandemics have both health health-related and economic dimensions. Putting this risk on the radar of finance ministers, for example in IMF (in countries’ Article IV reports) or World Bank Systematic Country Diagnostics, would reinforce the impetus for investing in health security.
Shortcomings are not only at individual country level: Development co-operation in support of epidemics control is difficult to track. There are widely divergent estimates of commitments to global health security in developing countries, varying from USD 240 million to USD 11.1 billion (Global Pandemics Monitoring Board, 2019[18]). A key issue is the definition of preparedness – which varies from a narrow lens on “epidemics prevention and response” to a much broader concept of “whole-of-government readiness”; with the sectoral approach “robust health systems” in between. The following chapter takes the latter perspective by analysing how development assistance can help strengthen health systems as a whole. The OECD Creditor Reporting System provides one possible – though imperfect – estimate of development finance, both official and private. Using the “infectious disease control” category, a relatively “narrow” field (excluding HIV, Tuberculosis, and Malaria), financing increased sharply after 2014: official and private development finance increased from USD 2.2 billion in 2014 to USD 3.2 billion in 2015 and reached USD 3.7 billion in 2017 (Figure 2.1). According to the International Working Group (2017[17]), accounting for different sources yields to total financing of USD 4 billion, with USD 2.5 billion for preparedness and USD 1.5 billion for research and development. Better tracking those different estimates, including better identification of activities beyond “infectious disease control”, would help identify how much is spent, and how much is needed to fill the gap.
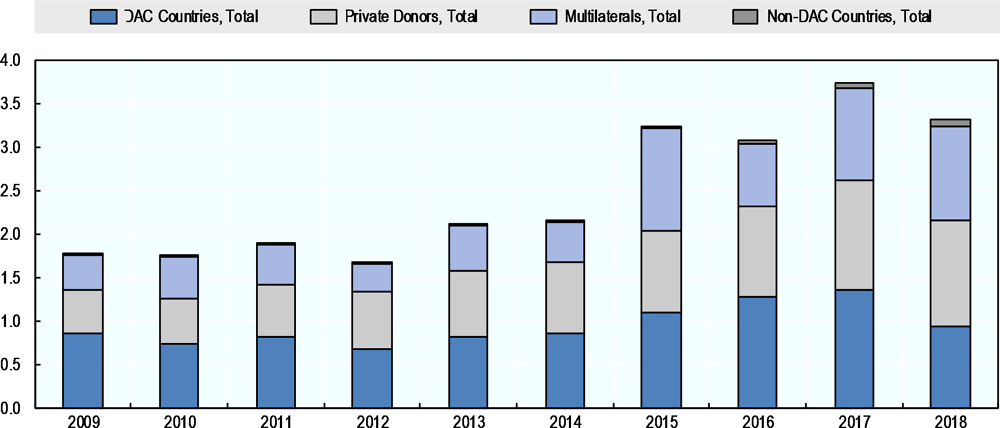
Note: Excluding official development finance to HIV/AIDS, Tuberculosis and Malaria. Infectious disease control refers to aid classified under purpose code 12250.
Source: OECD (2020[18]), Creditor Reporting System (database), https://stats.oecd.org/Index.aspx?DataSetCode=crs
As of 2018, the multilateral system, DAC members, and private foundations (mainly the Bill & Melinda Gates Foundation) each finance a third of the expenses related to epidemics control6. However, 2018 witnessed the first major decline in financing for epidemics control in years. The United States, which emerged as the major funder for preparedness after the Ebola crisis, especially through technical assistance by the Centre for Disease Control (CDC), reduced its international funding by USD 450 million in 2018. While it represented more than half of bilateral funding in 2015-2017, its share fell to 24% in 2018.
Increasing the global mobilisation
Global mobilisation: timely but still insufficient
As of May the multilateral system has mobilised strongly against COVID-19 in support of developing countries: the WHO set-up a “Strategic Preparedness and Response Plan (SPRP)” in February 2020, which outlined the main operational needs to fight the epidemics. It then estimated the funding needs for this plan at USD 675 million, requested through the Contingency Fund for Emergencies (CFE). The DAC strongly responded to this call, with above USD 125 million of funds provided. For the period starting in April, the WHO launched a “Coronavirus Response Fund” and estimates its total funding requirement for WHO’s COVID-19 response at USD 1.7 billion until the end of 2020 (WHO, 2020[19]). The UN Secretary General has launched a UN framework for the immediate socio-economic response to COVID-19, outlining the UN Development System’s social and economic support during the pandemic (UN, 2020[20]).The humanitarian response is co-ordinated at the level of the United Nations and guided by UN OCHA’s Global Humanitarian Response Plan (GHRP), pooled between several of international organisations and NGOs (WHO, UNICEF, WFP, etc.) (UNOCHA, 2020[21]). The GHRP initially called for USD 2 billion targeting fragile settings but given the burdens of the virus spread total requirements have risen to USD 6.71 billion (UNOCHA, 2020[22]). In early May, only 13% of the GHRP funding appeal had been received. The Global Fund against AIDS, Malaria and Tuberculosis has allowed recipient countries to reallocate parts of its grants to the current pandemics.
The global effort to prevent, treat, and test has received a major boost with EU support, bilateral and private donors. Relaying the call for action by several global health organisations, the Access to COVID19 Tools Accelerator raised EUR 7.4 billion on 4 May 2020.7 It includes a commitment for equal access to vaccines or therapeutics, which will allow the rapid distribution to developing countries. The initiative made clear that more will be needed: this sum meets initial needs, but will not be sufficient to manufacture and deliver solutions.
Multilateral development banks are responding both to the health emergency, and the economic shock. While figures are changing rapidly, the largest commitments so far stemmed from international financial institutions. The IMF raised its emergency lending capacity to USD 100 billion magnitude targeting shortfalls in low and middle-income countries (IMF, 2020[23]). The World Bank Group’s total emergency commitment is of USD 16 billion, through IDA (USD 1.3 billion) and the IBRD (USD 2.7 billion), as well as the IFC (USD 12 billion), but aims at deploying about USD 160 billion over the next year and a half (World Bank, 2020[24]). Regional development banks8 are estimated to have redeployed about USD 120 billion.
DAC members have a role in supporting the international effort, both through the multilateral system and their field operations. The global interventions outlined above have the advantage of scale, and rapid mobilisation. Supporting the global efforts should be a priority, to avoid fragmentation of effort. This is especially the case for procurement of goods that have become scarce – personal protective equipment, ventilators, etc. – where fragmentation would increase the already destructive market disruption. However, DAC members as bilateral donors should adapt their operations to the ongoing pandemic. The French Development Agency (AFD) announced that it would raise about EUR 1.5 billion to support countries in sub-Saharan Africa through expertise and direct support to health systems through grants and loans, and the German development ministry announced USD 1.2 billion in support. The EU prepared a EUR 15.6 billion to address both the immediate health impact and economic disruption. Other DAC members have also stepped up – Netherlands with USD 114 million, mostly for Africa, and Canada with USD 100 million.
Philanthropy and private sector actors have also made commitments. Jack Ma of Alibaba has provided equipment to African countries, Jack Dorsey of Twitter pledged USD 1 billion, while the Bill & Melinda Gates foundation, already a major funder of both multilateral initiatives, research, and evidence, has released USD 100 million in early February for Africa and South Asia, before most global organisations had begun to mobilise.9 During emergencies, philanthropic organisations can be more nimble and try untested solutions (see Box 2.2 on the role of the BMGF R&D), and increase their commitments. Corporations have also contributed to the effort of shifting certain production lines to production of essential medical supplies such as hydro-alcoholic gels and medical masks.
Given the massive loss of lives, the social returns of a cure or a vaccine to COVID-19 would be very large. The cost of decreased economic activity is also immense. Yet, the complexity of financing vaccines makes it difficult to adequately fund privately, especially for low-income countries where demand can only be met at subsidised rates. This box presents some related initiatives.
Research efforts on COVID-19 started as soon as the virus was discovered, and were global from the onset. As a global public good, co-ordinated funding and research is necessary. However, this increase of resources towards research and development is not necessarily counted as official development assistance, which only includes the share going to developing countries. Looking at experience from past crises, Schäferhoff et al. (2019[10]) identify an initial increase in global R&D allocated to pandemics in 2015 after Ebola, but a decline in the two subsequent years.
Developed in the aftermath of Ebola, the main co-ordinating body of global research is the WHO R&D Blueprint: a global strategy and preparedness plan that allows the rapid activation of R&D activities during epidemics. Its aim is to fast-track the availability of effective tests, vaccines, and medicines that can be used to save lives and avert large scale crises.
The Coalition for Epidemics Preparedness Innovations (CEPI) was founded and launched in 2017, with funding from the Gates Foundation, the Wellcome Trust, and a consortium of DAC members. Its goal is to provide funding to accelerate research – from an average of 10 years to develop a vaccine to 12 months. Following the COVID-19 outbreak, it called for a mobilisation of USD 2 billion, to which several countries and foundations have responded. It will be a recipient of the Access to COVID19 Tools Accelerator initiative.
Philanthropy can play a catalytic role: research is by definition uncertain and governments can hesitate to make large financial bets on untested solutions. The Bill & Melinda Gates Foundation10 announced on 6 April 2020 that it would start building plants for each of the seven potential vaccines identified as promising.11 The Wellcome Trust announced on 7 April 2020 that it would seek to gather USD 8 billion in funding to R&D from businesses.12
For distribution, GAVI, the Vaccine Alliance, is present in 73 countries where it supplies 600 million doses a year. It developed the IFFim model, which could be adapted to the case of the coronavirus, as proposed by Weintraub, Yadav and Berkley (2020[25]), GAVI would emit a bond, backed by donors, which allows the organisation to obtain immediate funding to develop logistics chains in hardest-hit countries, purchase and distribute a vaccine or a cure. Donor countries thus spread the cost over a longer period – about 20 years. The third generation of GAVI replenishment took take place in early June 2020 and exceeded its funding target of USD 7.4 billion by raising over USD 8.8 billion from bilateral donors, the private sector and organisations.
A second innovation against the coronavirus is the Advanced Market Commitments (AMC). AMC was initially developed to fund new vaccines for diseases prevalent in low-income countries, and applied to the pneumococcal vaccine (with the support of several DAC members). Recently, its model was extended to adapt to “markets for capacity” (Kremer, Levin and Snyder, 2020[26]) for a case study): not accelerating R&D, but raising production capacity to make sure the vaccine is available for all as early as possible. The device commits donor countries to buy an agreed number of doses at a given price, thus providing incentives for potential producers below that price. With donor support, GAVI has launched the ODA-supported Advance Market Commitment for COVID-19 Vaccines (Gavi Covax AMC) in June 2020, giving manufacturers confidence to invest in scale-up of manufacturing capacity for COVID vaccine candidates in advance of their licensure and create economies of scale.
Responding efficiently, preparing wisely
Given the emergency, development co-operation should focus on identified “quick wins” and successful models. Official development assistance should serve as a catalyst of other sources of financing. Chalkidou and Krubiner (2020[27]) of the Centre for Global Development provide useful recommendations to strengthen health systems. For the immediate response, they propose to establish a list of “best-buys”, working through existing institutions: the African CDC for example has been an important platform for the continent. Interventions should focus on public goods, and investments should be made to improve understanding of the disease. Supporting epidemiologic models and sharing knowledge can help manage the response. The cost-effectiveness approach to evaluate various treatments as well as other medical investments is important to adopt. In general, mobilising evidence is a first order priority.
This should not be limited to medical or epidemiological questions. Social science can and should inform the response – for example on how to best isolate vulnerable populations – and answers will need to be tailored to the cultural context. Researching and evaluating evidence on “what works” – through partnerships with universities and local institutions is essential. Reviewing lessons of various outbreaks, as well as experiments and randomised controlled trials can help. Collecting data, assessing value-for-money for medicines or public-health intervention, and using this evidence for policy making is a difficult undertaking for governments with limited resources, but which could be funded by external donors.
Some experts warned against applying the same solutions that proved efficient in higher income countries to lower income countries without taking into consideration local contexts. Donors should target achievable immediate actions: providing personal protective equipment to hospitals and medical staff to protect them in the front line,13 ensuring clean water facilities to allow hand-washing in dense places – markets, urban slums, etc. and adapting social distancing to the circumstances.14
This includes taking into account the role of gender in the response. A study in 104 countries show that women form 70% of workers in the health and social sector (Boniol et al., 2019[28]).Women are nurses, midwives and community health workers. However, globally women remain least represented at the top of the “medical hierarchy”, among health ministers and physicians and hold positions of lesser authority across the bulk of the formal system (Hay K, 2019[31]). Bilateral donors can ensure that both women and men are included in decision making around health systems and priorities.
Development co-operation providers should bear fixed-costs investment and assist countries in mobilising finance for preparedness and crisis-response. Examples of successful establishments of national CDCs – including the African CDC, but also the Nigerian CDC, which managed to contain the Lassa fever outbreak of 2018 – provide a useful financing model, where external donors would bear fixed-costs investment such as setting up institutions, and countries would mobilise domestic resources for recurrent costs. This approach yields a variety of co-financing options:
The Centre for Global Development proposed a “challenge fund” where countries and donors would co-finance improvements of epidemics preparedness (Glassman, 2020[28]), with the option of reimbursing countries’ investment upon meeting targets. This would reinforce domestic buy-in while providing an incentive structure. A dedicated fund would have the advantage of having a clear target – similar to other health funds (the Global Fund, Gavi, etc.) and would require high-level political buy-in.
Another financing possibility would be to provide “buy-downs”: loans to reach specific preparedness targets, and turn the loans into grants in case of success. Again, this model has the advantage of providing incentives to domestic governments while avoiding for them to pay upfront costs.
The private sector should be implicated in preparedness and crisis-response. Companies bear direct costs from pandemics, and can invest in better preparation and response, including while the outbreak is ongoing, by adopting safe labour practices, improving their hygiene environment, etc. They, or their investors, could allow partly paid furlough while the pandemic is spreading. Development co-operation actors could also step in to put in place measures such as temporary unemployment schemes in areas affected by sudden value chain disruptions, e.g. the garment sector in Bangladesh. These social measures would add to other measures aimed at building the resilience of trade and value chains in times of crisis. Development partners as well as development finance institutions could lead in adopting COVID‑19 safety procedures during the crisis. The private sector can also leverage innovation – technical and social – such as e-health, trackers, as well as social networks.
The DAC has an important role to play, and could take several steps in promoting those solutions:
Better monitor and address gaps in pandemics preparedness and response. In particular, the International Working Group (2017[17]) proposed that a discussion be initiated on including preparedness as an individual item in the Creditor Reporting System database. This would improve tracking of financing for pandemic preparedness, and facilitate holding development partners accountable for the commitments they make and create a forum for regular discussion of preparedness financing issues among stakeholders. DAC members can support pandemic preparedness by using JEE or other preparedness indicators as one of the criteria to guide donor funding, or by providing technical support to help countries improve preparedness.
Increase technical and financial assistance to support partner countries respond to the COVID-19 health challenges and medical innovation, including to maintain basic and critical health services in all health areas, treatment of COVID-19 patients, and support measures to contain the virus including testing and tracing.
Use and share technical expertise on “fixed-cost” items, including epidemiological modelling, support to the response, both at the country- and region-levels of intervention
Discuss and promote among DAC members best practices in financing policy and financial responses to the crisis. There are many sectors of intervention of development finance providers where they can identify “COVID-19 synergies”. This could include investing in urban infrastructure with more distance between people, providing WASH facilities, developing contactless payments, etc. Those solutions should be identified, shared, and disseminated.
Use all the channels available: Bilateral donors have the advantage of relying on a variety of networks: foundations, NGOs, research centres, which can be entry points in disseminating best practices. Development finance institutions should also play a role as responsible investors – adopting best practices in companies they invest in to slow the spread of the virus.
Beyond coronavirus (COVID-19): How could development co-operation build the resilience of health systems?
Health systems have been strengthened in developing countries in the past. This is in part due to support from the international development co-operation community and other (external) actors. Better health technology and hygiene as well as nutrition have allowed life expectancy to rise across countries, irrespective of income. Vaccines have eradicated infectious diseases that caused millions of deaths just a few decades ago. The COVID-19 crisis will be a setback for many countries. While there are still many unknowns, life expectancy in lower income countries could be threatened, as was the case with the HIV/AIDS virus two decades ago.
However, investing in “the first line of defence” – preparedness – is not enough. Development co-operation should also invest in the “second line of defence” – health systems. From the financing point of view, the central commitment is SDG target 3.8, universal health coverage,15 which states “that all people have access to needed health services (including prevention, promotion, treatment, rehabilitation and palliation) of sufficient quality to be effective while also ensuring that the use of these services does not expose the user the financial hardship.”
This implies the need for development co-operation to shift from disease-focused actions to a “systems” approach. The COVID-19 crisis is a threat to domestic health systems that are already short of resources in many developing countries. First, the COVID-19 crisis could overwhelm health systems and ultimately challenge their capacity to handle basic functions. Second, it may lead countries to shift their resources away from tackling other diseases or services that cannot be delayed or reprogrammed such as maternal health services.
The following section reviews existing evidence and possible solutions in order for development co-operation to better build resilience of health systems in response to the COVID-19 crisis.
Pandemics can overwhelm health systems and have ripple effects on other diseases
Development co-operation has helped fight infectious diseases and promote health through various channels
Development co-operation promotes health in a variety of ways, both directly through health-targeted programmes, and indirectly through programmes targeting water, sanitation and hygiene (WASH) or nutrition. Official development finance to the health sector has mainly supported programmes targeting specific infectious diseases (Figure 3.1). Between 2014 and 2017, for instance, around 53% of official development assistance commitments to health targeted the control of sexually transmitted diseases (including AIDS/HIV), infectious disease control, malaria and tuberculosis. The creation of various so-called “vertical funds” in the early 2000s and the large-scale engagement of private philanthropic foundations underscores this focus on specific disease intervention. Vertical funds target specific programmes and disease interventions and often channel support through private, non-public systems. In the meantime, development finance towards health policy and health systems more generally has increased from USD 5.2 billion to USD 8.6 billion between 2010 and 2018, representing an increase from 26% to almost 33% as a share of total development assistance to health.
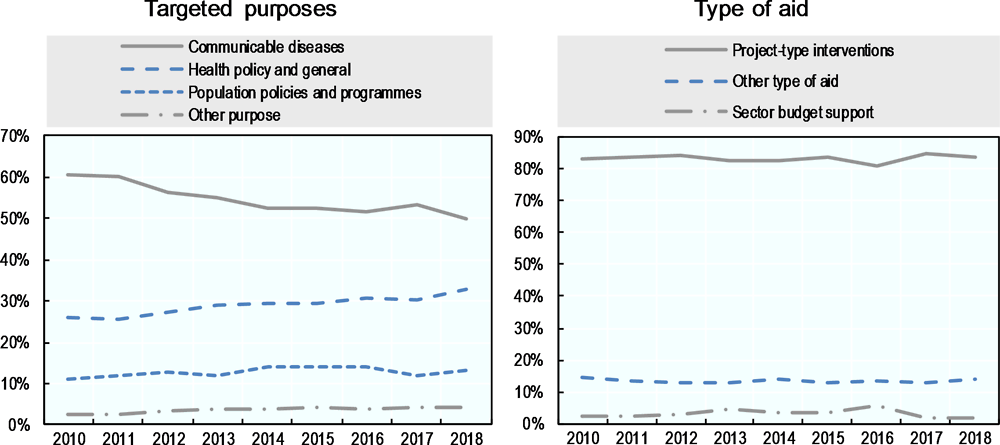
Note: Bilateral allocable aid including bilateral DAC and non-DAC donors, multilateral donors and philanthropic development finance. Detailed methodological notes in the footnote at the end of the paper.
Source: OECD (2020[18]), Creditor Reporting System (database), https://stats.oecd.org/Index.aspx?DataSetCode=crs
The importance of financial support to health systems will increase along with the disease burden in low- and lower-middle income countries and the risk of recurring epidemics and pandemics. For example, responding to the ongoing COVID-19 pandemic largely depends on the medical infrastructure and the ability of the health sector as a whole to respond to the emergency. This depends on the number of medical personnel and personnel protective equipment, intensive care units, and equipment such as ventilators, which all depend on adequate financing. Testing and tracing of infected persons is critical to stop chains of infections.
Risks associated with the COVID-19 crisis are associated with trade-offs as much as general disruptions of health systems
While the response to COVID-19 is pushing healthcare systems to and beyond their limits, global efforts to end other communicable diseases such as HIV, TB and malaria risk are being severely affected. The DAC has been a key supporter of the fight against these diseases and provided USD 6 billion in ODA for infectious disease control (including malaria and tuberculosis) in 2018. As such, this is a clear priority for bilateral donors, and the DAC should play a role in helping to minimise the disruption to this agenda and to ensure continued progress.
Risk of co-infection: While medical research into COVID-19 is still ongoing, people already infected with other communicable diseases such as HIV and TB could be among the most vulnerable. (GBC Health, 2020[29]) As the virus seems to have a more severe impact on people with underlying health conditions, there might be specifically high vulnerability throughout parts of the world with a high incidence of HIV, TB and malaria which puts Africa notably, at high risk.
Disruption to health systems: COVID-19 could derail progress on other diseases, through disruptions in treatment or other interventions, or disruptions in supply chains of critical medicines and medical supplies. The latter could also be amplified by measures taken in higher income countries to ban exports of essential supplies in response to their own shortage of supplies in times of pandemics. A recent study estimated the indirect effects of the pandemic on maternal and child mortality in LMICs, and found that COVID-related disruptions to the health system can cause an increase of 9.8–44.7% in under-5 child deaths, and an 8.3–38.6% increase in maternal deaths per month. (Roberton et al., 2020[30])
With local health systems under stress, countries will lack the resources and capacity to cater to patents of other infectious diseases. People with a medical condition may not be able to be treated due to hospital occupancies being reached, and health workers focusing on the treatment of patients infected by COVID-19. Experience from the 2015 Ebola outbreak in West Africa suggests that additional deaths from existing diseases such as malaria could be comparable to or even greater than those from the outbreak itself.
The 2014–15 Ebola crisis in West Africa was the most extensive and deadliest outbreak of Ebola recorded, with profound and multifaceted consequences. It began in rural Guinea in December 2013 and spread to neighbouring countries and urban centres becoming widespread and intense in Sierra Leone, Guinea, and Liberia. After reaching peak levels between August and December 2014, incidence decreased over time until the outbreak was declared over in January 2016, although sporadic cases have arisen since.
Over 28 000 people were infected by Ebola and over 11 000 died. The impact however was not confined to morbidity and mortality directly caused by Ebola. The health system was severely compromised due to overwhelming demand, healthcare workers deaths, resource diversion, and closure of health facilities. The surge of EVD (Ebola virus disease) cases rapidly overwhelmed health facilities, there was a severe lack of treatment beds, lack of supplies and essential medicines. In Liberia, the impact on the health system appeared more substantial with WHO reporting that 62% of health facilities were closed at some point and that two-thirds of healthcare services had ceased to function in August 2014.
Healthcare workers were among the first to encounter cases of EVD and were unprepared and vulnerable, lacking training and personal protective equipment. It has been estimated that 10.7%, 10.3%, and 2.7% of the healthcare workforce were infected by Ebola in Sierra Leone, Liberia, and Guinea, respectively and that 6.9%, 8.1%, and 1.5% of the workforce died from EVD.
Access to healthcare was compromised. Substantial reductions in healthcare utilisation were reported, including over 80% reductions in maternal delivery care in Ebola-affected areas, and 40% national reductions in malaria admissions among children under five years. Vaccination campaigns and community vaccination activities were suspended in all three countries over safety concerns.
Source: Elston et al. (2017[31]), “The health impact of the 2014–15 Ebola outbreak” https://doi.org/10.1016/j.puhe.2016.10.020
Supply chain disruptions caused by the pandemic and countries’ response can affect the ongoing fight against infectious diseases through procurement delays and long stock outs of drugs and other commodities. With many health commodities being produced in East and Southeast Asia, the production of pharmaceutical and other health-related products has significantly slowed down, in some cases even coming to a halt. China is the dominant global supplier of pharmaceuticals, and Wuhan, where the virus originated, is significant centre of the biotechnology and pharmaceutical industry. With factories in Asia on lockdown due to quarantines to contain the spread of COVID-19, many commodities are being produced and shipped late. (GBC Health, 2020[29]) While some high-income countries are struggling to ensure the adequate supply of medical equipment, the situation is exacerbated in countries where there are already supply chain issues.
Development co-operation should take into consideration the potential collateral damage of COVID-19 in designing its response to the crisis. Diversion of resources from other essential forms of support to targeted disease programmes, nutrition or health systems at large could amplify the death toll from COVID-19. Possible solutions to minimise health system disruptions are currently being discussed. Examples include the expansion of telemedicine, better primary healthcare, etc. Donors can actively encourage this discussion by investing in research and integrating the solutions in their health programmes.
Financing gaps in the health sector give rise to a trade-off between health security and other priorities
In many countries, existing financing gaps in the health sector challenge the objective of universal quality healthcare. The gap is even wider in developing countries. There can be an inherent trade-off in providing support to the fight against COVID-19 in developing countries and ensuring continued support for other health needs.
In light of the nexus between COVID-19 and other diseases, it is important that international support to address the current crisis, including from the DAC, is delivered in a way that protects and reinforces existing health priorities, and does not divert attention and resources. The focus of the support should be on assisting the most vulnerable. In this context, the WHO issued two statements regarding the importance of ensuring the continuity of malaria and TB services during the COVID-19 pandemic, urging countries to “not scale back […] planned malaria prevention, diagnostic and treatment activities” in the face of the pandemic, and highlighted the importance of keeping health workers safe in the face of these infectious diseases (WHO, 2020[32]) (WHO, 2020[33]). So far, however, evidence of previous crisis management shows that the DAC members have respected the additionality principle, and financing creation effects have prevailed over diversion effects.
Many countries including a rising number of low-income countries increasingly face a double burden: lasting infectious diseases and the growth of non-communicable diseases. The WHO estimates that 53% of deaths in low-income countries in 2016 were due to communicable diseases.16 But non-communicable diseases such as cardiovascular disease, cancer, chronic respiratory disease, and diabetes have caused around 37% of all deaths in low-income countries in 2016 – up from about 23% in 2000. This shift towards non-communicable diseases – while infectious, maternal, perinatal, and nutritional conditions still pose major challenges – puts additional strain on already scarcely resourced health systems. At the same time, communicable diseases still present a significant health challenge for lower middle-income countries, causing 30% of deaths compared to 67% for non-communicable diseases.
Development partners finance and support the health sector in low- and lower middle-income countries
A variety of sources are available to finance healthcare including domestic and international, private and public resources. In 2017, global spending on health amounted to USD 7.8 trillion, representing about 10% of the world’s GDP (WHO, 2019[2]). While representing less than 1% of global health spending, aid represented 29% of health spending in low-income countries and 12% in lower middle-income countries. This clearly demonstrates the important role of development co-operation and finance to support these countries responding to the COVID-19 pandemic. In total, development assistance to health more than quadrupled since 1990, and amounted to more than USD 26 billion in 2018 (OECD, 2020[18]). Within this total spending, members of the DAC provided USD 14.6 billion; in addition to USD 8.3 billion from multilateral donors, USD 3.1 billion from private philanthropic donors, and USD 0.4 billion from bilateral non-DAC donors.
Non-communicable diseases present a growing threat to countries supported by the DAC, but they remain under-prioritised. Even as global epidemics have been top priority of the global health agenda, there is an array of urgent health needs in developing countries that remain underfunded and under-prioritised. One of these is the response to non-communicable diseases and injuries, which are on the rise globally, and are especially burdensome for low- and lower middle-income countries. In 2016, non-communicable diseases (NCD) such as cardiovascular disease, cancer, chronic respiratory disease, and diabetes accounted for 73% of global deaths (40 million people), of which 75% (30 million) were in low-income and middle-income countries. (Hatefi and Allen, 2018[34]) In low-income countries, the share of total deaths caused by NCDs rose from 23% in 2000 to 37% in 2016. As observed during the COVID-19 crisis, those non-communicable diseases could also be a factor of vulnerability to pandemics.
Despite the growing urgency, NCD response attracts only a limited amount of external resources, especially from DAC members. In 2018, support for NCDs represented a mere 0.1% of ODA disbursements from DAC members targeting the health sector.17 Only a limited number of donors provide assistance to cope with NCDs, and the bulk of the funding comes from three private foundations (World Diabetes Foundation, Wellcome Trust, Bill and Melinda Gates Foundation) rather than from official providers. Of DAC members, 12 countries report their support for NCDs, with Germany, New Zealand, Norway and Switzerland being among the largest.
The mobilisation of funds for the COVID-19 response should not divert funds from support for the fight against NCDs. In the medium to long-term, calls for more funding for pandemic preparedness in developing countries will likely rise, as an important prerequisite to ensuring the global public good of health security. However, while the importance of global health security cannot be contested, experience shows that a narrow targeting of development assistance for health risks could be unsustainable, and could have negative side effects. A forthcoming OECD paper on health sector financing explores how countries who receive development assistance run the risk of sliding back on their progress in health outcomes as they become wealthier and lose access to external resources. For example, after graduating from the Global Fund in 2010, Romania saw a rapid rise in HIV prevalence among persons who inject drugs. The HIV prevalence among this group, estimated at 1.1% in 2009 increased to 6.9% in 2012 and spiked at 53% in 2013 (ICASO, 2016[36]).
Assistance to address the consequences and prevent a resurgence of COVID-19 and similar epidemics need to be carefully and smartly designed. If donors target narrowly confined objectives related to the control of COVID-19 and pandemic preparedness, the gains and progress achieved with their support could be quickly reversed.
Investing in stronger health systems is critical to managing this trade-off
Health security efforts for prevention, alert, and response to disease outbreaks such as COVID-19 need to be pursued in parallel with health system strengthening, as part of the same mutually reinforcing approach to developing resilient health systems. Health system strengthening aims to ensure that the individual building blocks of the health system (i.e. service delivery; health workforce; information; medical products, vaccines, and technologies; financing; and leadership and governance) function smoothly and interact well with each other. Universal health coverage, which allows everyone to access affordable and quality health services, is an important element of a strong health system (WHO, 2007[37]).
Donor support for health system strengthening is rather limited. In 2018, the categories “general health” and “other basic health”, which would include health system strengthening made up 15.8% and 16.7%, respectively, of overall development assistance targeting the health sector. During emergency responses, this percentage is also likely to decline, although crises could also be a wake-up call and benefit support to health programmes at large.
A strong health system is critical to ensure effective crisis response and prevention. Successfully functioning health systems underpin countries’ ability to detect and respond to disease threats. To improve developing countries’ resilience to health crises, donors need to invest in stronger health systems. (Wenham et al., 2019[38]) By focusing their post-COVID support on health system strengthening activities, DAC members and other donors could also help to address the tension between competing health priorities. There is a strong link between universal health coverage and NCD control, as enabling access to affordable healthcare could allow more people to be diagnosed and treated early. Similarly, support for health system strengthening should integrate concerns for gender inequalities in order to ensure that the entire population is able to access services. Over the past decade, the share of DAC members’ ODA in the health sector that integrated gender equality has never surpassed 50%. In 2017-18 the figure was 42%, which seems surprisingly low. In the area of infectious disease control, only 24% of aid focussed on gender equality and women’s empowerment in 2017-18.
Health system strengthening is often focused on upstream support for governance and policy making; however, downstream projects can be designed in a way that is conducive to strengthening. Assistance for specific diseases, for instance, can also be used in order to maximise systemic benefits. For example, Ethiopia and Malawi have channelled HIV funding to train health workers who can manage multiple conditions, to build primary health care centres, develop monitoring and evaluation systems, and strengthen supply chain management to improve patient outcomes for a range of diseases. In sub-Saharan Africa, TB programmes have provided suitable platforms to introduce screening and scale up management of NCDs such as chronic respiratory diseases. (Atun et al., 2013[40])
Synergies especially exist between achieving universal health coverage and enhancing health security. For example, universal health coverage supports health security by preventing outbreaks through high immunisation coverage, providing early alert by facilitating access to healthcare for the entire population, better response thanks to reliable infrastructure and healthcare workforce. At the same time, effective prevention and response to health crises is key to achieving universal health care. Health crises tend to divert resources to focus on crisis response and lowers trust in the health system. Therefore, they cause barriers to accessing healthcare. By avoiding and better managing such health crises, countries can ensure that patients have access to healthcare. (Kluge et al., 2018[41])
Summary and conclusions
The quick spread of the COVID-19 crisis challenges the achievement of SDG 3, which aims at “Ensuring healthy lives and promote well-being for all at all ages”. Depending on the response to the crisis, and its potential collateral effects on health systems and their financing, the world could experience major development setbacks, threatening progress towards the SDGs and the achievement of the 2030 Agenda.
This report suggests that development partners take two perspectives: in the short term, strengthen the response by focusing on global and regional public goods, producing high-quality evidence on mitigating and containing the disease, and providing incentives for preparedness for future outbreaks. But health systems are also at risk, as trade-offs between budget choices and damaging interaction between communicable diseases can worsen the outcome.
Pandemics require a “whole-of-government” approach, and ODA is no different: all its roles and potential benefits should be explored. Three aspects in particular have been highlighted across this note.
The contribution of ODA to global public goods should be more explicitly defined and managed
Given the “public good” characteristics of the response, donors have mobilised to support the multilateral system, which is more responsive to raise finance and disburse funds where they are most needed. However, as previous crises have shown, humanitarian funding tends to lack the needs. It is thus important to monitor the response from donors and from international organisations.
Adequate financing for pandemic preparedness and response also requires that it is more explicitly included in the definition of global public goods, and in the corresponding institutional mandates of development organisations (Yamey, Ogbuoji and McDade, 2018[42]). Current definitions of global public goods are rather narrow, referring to more traditional activities such as the generation and sharing of knowledge, the setting of international health norms and standards, or the sharing of intellectual property. Going forward the understanding and financing of health GPGs would need to also include the active management of negative cross-border externalities that arise through pandemics and epidemics.
Another aspect that has attracted concerted effort is the development of a cure and/or vaccines. Increasing and sustaining global R&D effort will require both financial and organisational commitments. It has been complemented by the objective of an equitable distribution, going beyond pure market principles. Organisations with the ability to distribute eventual cures or vaccines, such as GAVI or the Global Fund, help to ensure that they reach the most vulnerable as early as possible.
Prevention also comes from better modelling of the disease. This sort of expertise, also in short supply, can be pooled at the regional or global level, for example through the support of epidemiologic models and other forms of knowledge sharing. These models have been successful when donors have borne the fixed costs of building institutions, while supporting domestic resource mobilisation by recipient countries to finance recurrent expenses.
Development finance providers have the capacity to gather and organise information across sectors
At a more granular level, development co-operation can help gather and share “best practices”. Through their health operations, they can collect data, share knowledge, and ultimately assess the value-for-money for medicines and public-health intervention. This could lead to establish a list of “best-buys” – solutions able to maximise the numbers of lives saves – adapted to country and regional contexts. For example, procurement and distribution of personal protective equipment for medical personnel is an urgent need for frontline workers.
This does not stop at only health projects: all sectors can contribute in adapting their programmes to a COVID-19 affected world. For example, setting up better WASH facilities in crowded places, or reviewing urban infrastructure in the context of the pandemic. The current crisis revealed the importance of developing investment strategies to promote sectors with “pandemic preparedness co-benefits”.
The DAC can track development finance going to pandemic preparedness and response. It can also leverage its resources to identify domestic resources going to global health security, better capturing national contributions to a major global public good. Development finance providers can also include preparedness in their macroeconomic monitoring: as the COVID-19 crisis has revealed, pandemics should be on the radar of finance ministers.
Health systems are the second line of defence and cannot be ignored
A possible risk in seeking to limit the spread of the virus is to paralyse health systems for other chronic or acute diseases or services. It is also important to consider damages of COVID-19 on systems and broader populations, and monitor risks for vulnerable populations already susceptible to or infected with other diseases.
This policy note has sought to highlight the complementarities between strengthening health systems, and in particular primary health, and the mobilisation against pandemics. Returns on investment in stronger health systems are even higher – whether on personnel or infrastructure. This approach would strengthen the implementation of global commitments to universal health coverage.
References
[40] Atun, R. et al. (2013), “Improving responsiveness of health systems to non-communicable diseases”, Lancet, Vol. 381/9867, pp. 690-697, https://doi.org/10.1016/S0140-6736(13)60063-X.
[45] Bill and Melinda Gates Foundation (2020), Bill & Melinda Gates Foundation Dedicates Additional Funding to the Novel Coronavirus Response (press release), https://www.gatesfoundation.org/Media-Center/Press-Releases/2020/02/Bill-and-Melinda-Gates-Foundation-Dedicates-Additional-Funding-to-the-Novel-Coronavirus-Response.
[3] DAC/OECD (2020), Joint Statement by the Development Assistance Committee (DAC) on the covid-19 global pandemic, OECD Publishing, Paris, http://www.oecd.org/dac/development-assistance-committee/DAC-Joint-Statement-COVID-19.pdf.
[7] Davies, S. and B. Bennett (2016), “A gendered human rights analysis of Ebola and Zika: locating gender in global health emergencies”, International Affairs, Vol. 92/5, pp. 1041-1060, https://doi.org/10.1111/1468-2346.12704.
[27] Development, C. (ed.) (2020), What COVID-19 Should Teach Us About Smart Health Spending in Developing Countries, https://www.cgdev.org/blog/what-covid-19-should-teach-us-about-smart-health-spending-developing-countries.
[31] Elston, J. et al. (2017), “The health impact of the 2014–15 Ebola outbreak”, Public Health, Vol. 143, pp. 60-70, https://doi.org/10.1016/j.puhe.2016.10.020.
[11] Fan, V., D. Jamison and L. Summers (2018), “Pandemic risk: How large are the expected losses?”, Bulletin of the World Health Organization, Vol. 96/2, pp. 129-134.
[43] Garrett, L. (2019), The World Bank has the money to fight Ebola but won’t use it (column), Foreign Policy, https://foreignpolicy.com/2019/07/22/the-world-bank-has-the-money-to-fight-ebola-but-wont-use-it/.
[29] GBC Health (2020), “Beyond COVID-19: Ripple Effects of a Pandemic”, http://gbchealth.org/beyond-covid-19-ripple-effects-of-a-pandemic/.
[35] GHRF Commission (2015), The Neglected Dimension: A Framework to Counter Infectious Disease Crises, https://nam.edu/wp-content/uploads/2016/01/Neglected-Dimension-of-Global-Security.pdf.
[28] Glassman, A. (2020), A Global Health Security Challenge Fund, https://www.cgdev.org/blog/call-global-health-security-challenge-fund.
[42] Glassman, A., B. Datema and A. McClelland (2018), Financing Outbreak Preparedness: Where Are We and What Next? (blog), Center for Global Development, https://www.cgdev.org/blog/financing-outbreak-preparedness-where-are-we-and-what-next.
[44] Gross, A. (2020), Waiting game continues for pandemic bonds payour (news article), Financial Times, https://www.ft.com/content/cbd8ade4-69e1-11ea-800d-da70cff6e4d3.
[34] Hatefi, A. and L. Allen (2018), “Donors, non-communicable diseases and universal health coverage to high-quality healthcare: an opportunity for action on global functions for health”, J Epidemiol Community Health, Vol. 72, pp. 665-667, https://jech.bmj.com/content/jech/early/2018/05/21/jech-2018-210605.full.pdf.
[39] Hay, K. et al. (2019), “Disrupting gender norms in health systems: making the case for change”, The Lancet - Gender equality, norms and health, Vol. 393/10190, pp. 2535-2549, https://doi.org/10.1016/S0140-6736(19)30648-8.
[12] Huber, C., L. Finelli and W. Stevens (2018), “The Economic and Social Burden of the 2014 Ebola Outbreak in West Africa.”, The Journal of infectious diseases, Vol. 218/suppl_5, pp. S698-S704.
[36] ICASO (2016), The impact of transition from Global Fund support to governmental funding on the sustainability of harm reduction programs, http://icaso.org/wp-content/uploads/2016/10/Romania-case-study.pdf.
[23] IMF (2020), Coronavirus Economic Planning: Hoping for the Best, Prepared for the Worst, International Monetary Fund, Washington D.C., https://blogs.imf.org/2020/03/12/coronavirus-economic-planning-hoping-for-the-best-prepared-for-the-worst/.
[17] International Working Group (2017), From Panic and Neglect to Investing in Health Security.
[41] Kluge, H. et al. (2018), “Strengthening global health security by embedding the International Health Regulations requirements into national health systems”, BMJ Global Health, Vol. 3/e000656., http://dx.doi.org/10.1136/bmjgh-2017-000656.
[26] Kremer, M., J. Levin and C. Snyder (2020), Advance Market Commitments: Insights from Theory and Experience, http://dx.doi.org/10.3386/w26775.
[4] ODI (2020), Donor responses to the coronavirus, Overseas Development Institute (ODI), London, https://set.odi.org/wp-content/uploads/2020/05/Donor-responses_as-of-30April-2020.pdf.
[18] OECD (2020), Creditor Reporting System (CRS) (database), https://stats.oecd.org/Index.aspx?DataSetCode=crs.
[5] OECD (2020), Six decades of ODA: insights and outlook in the COVID-19 crisis, OECD Publishing, Paris, https://doi.org/10.1787/5e331623-en.
[6] Roberton, T. et al. (2020), “Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study”, The Lancet Global Health, Vol. 8/7, pp. e901-e908, https://doi.org/10.1016/S2214-109X(20)30229-1.
[30] Roberton, T. et al. (2020), “Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study”, Lancet Global Health, Vol. 8, pp. 901-908, https://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(20)30229-1.pdf.
[8] Ross, A. et al. (2015), “Planning for the Next Global Pandemic”, International Journal of Infectious Diseases, Vol. 38, pp. 89-94, http://dx.doi.org/10.1016/j.ijid.2015.07.016.
[10] Schäferhoff, M. et al. (2019), “International Funding for Global Common Goods for Health: An Analysis Using the Creditor Reporting System and G-FINDER Databases”, Health Systems & Reform, Vol. 5/4, pp. 350-365, http://dx.doi.org/10.1080/23288604.2019.1663646.
[20] UN (2020), A UN framework for the immediate socio-economic response to COVID-19, United Nations, https://unsdg.un.org/resources/un-framework-immediate-socio-economic-response-covid-19.
[1] UNCTAD (2014), World Investment Report 2014: Investing in the SDGs: An Action Plan, United Nations Publications, Geneva, https://unctad.org/en/PublicationsLibrary/wir2014_en.pdf.
[21] UNOCHA (2020), Global Humanitarian Response Plan to COVID-19, United Nations, https://www.unocha.org/sites/unocha/files/Global-Humanitarian-Response-Plan-COVID-19.pdf.
[22] UNOCHA (2020), Global Humanitarian Response Plan to COVID-19 (May update), United Nations, https://www.unocha.org/sites/unocha/files/GHRP-COVID19_May_Update.pdf.
[25] Weintraub, R., P. Yadav and S. Berkley (2020), A Covid-19 Vaccine Will Need Equitable, Global Distribution, https://hbr.org/2020/04/a-covid-19-vaccine-will-need-equitable-global-distribution.
[38] Wenham, C. et al. (2019), “Global health security and universal health coverage: from a marriage of convenience to a strategic, effective”, BMJ Global Health, Vol. 4/e001145., http://dx.doi.org/10.1136/bmjgh-2018-001145.
[19] WHO (2020), COVID-19 WHO appeal, World Health Organization, Geneva, https://www.who.int/publications/m/item/covid-19-who-appeal.
[33] WHO (2020), “WHO urges countries to ensure the continuity of malaria services in the context of the COVID-19 pandemic”, https://www.who.int/news-room/detail/25-03-2020-who-urges-countries-to-ensure-the-continuity-of-malaria-services-in-the-context-of-the-covid-19-pandemic.
[32] WHO (2020), “World Health Organization (WHO) Information Note”, https://www.who.int/tb/COVID_19considerations_tuberculosis_services.pdf.
[2] WHO (2019), Global Spending on Health: A World in Transition, World Health Organization, Geneva, https://www.who.int/health_financing/documents/health-expenditure-report-2019/en/.
[46] WHO (2018), Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016., World Health Organization, Geneva, http://, https://www.who.int/healthinfo/global_burden_disease/estimates/en/.
[37] WHO (2007), Everybody’s business: Strengthening health systems to improve health outcomes, WHO Press, Geneva, Switzerland, https://www.who.int/healthsystems/strategy/everybodys_business.pdf.
[24] World Bank (2020), World Bank Group Increases COVID-19 Response to $14 Billion To Help Sustain Economies, Protect Jobs (press release), World Bank Group, Washington D.C., https://www.worldbank.org/en/news/press-release/2020/03/17/world-bank-group-increases-covid-19-response-to-14-billion-to-help-sustain-economies-protect-jobs.
[15] World Bank (2020), World Bank Group Launches First Operations for COVID-19 (Coronavirus) Emergency Health Support, Strengthening Developing Country Responses (press release), World Bank Group, Washington D.C., https://www.worldbank.org/en/news/press-release/2020/04/02/world-bank-group-launches-first-operations-for-covid-19-coronavirus-emergency-health-support-strengthening-developing-country-responses.
[16] World Bank (2020), World Bank Group’s Operational Response to COVID-19 (coronavirus) – Projects List (press release), World Bank Group, https://www.worldbank.org/en/about/what-we-do/brief/world-bank-group-operational-response-covid-19-coronavirus-projects-list.
[13] World Bank Group (2019), Pandemic Preparedness Financing - Status Update, https://apps.who.int/gpmb/assets/thematic_papers/tr-4.pdf.
[9] Yamey, G. et al. (2017), “Financing of international collective action for epidemic and pandemic preparedness”, thelancet.com.
[14] Yamey, G. et al. (2020), “Preparing for pandemics such as coronavirus—will we ever break the vicious cycle of panic and neglect?”, https://www.brookings.edu/blog/future-development/2020/02/11/preparing-for-pandemics-such-as-coronavirus-will-we-ever-break-the-vicious-cycle-of-panic-and-neglect/.
Annex 1.A. Methodological notes
Methodological notes for Figure 3.1.
Bilateral allocable aid refers to the CRS aid types A02, B01, B03, B04, C01, D01, D02 and E01. Broadly speaking, these are the projects donors can allocate to sectors (e.g. not including general budget support). Development finance to health includes CRS purpose codes 12XXX and 13XXX. Left: ‘communicable diseases’ include CRS purpose codes 12250, 12262, 12263 and 13040, ‘population policies and programmes’ includes 130, 13010, 13030 and 13020, ‘health policy and general’ includes 120, 121, 12110, 12181, 12182, 12191, 12196, 122, 12220, 12230, 12261, 12281, 13081, 13096, ‘other purpose’ includes all other purposes. Right: ‘project-type interventions’ includes CRS aid type C02, ‘sector budget support’ A02 and ‘other type of aid’ includes all other aid types.
Contact
Martin KESSLER (✉ martin.KESSLER@oecd.org)
Jieun KIM (✉ jieun.KIM@oecd.org)
Konstantin POENSGEN (✉ konstantin.POENSGEN@oecd.org)
Notes
G20 Leaders Communiqué, 26 March 2020, https://g20.org/en/media/Documents/G20_Extraordinary%20G20%20Leaders%E2%80%99%20Summit_Statement_EN%20(3).pdf
Pandemics are “fat-tailed events”: low frequency but high cost. On any given year, the cost is small or close to 0 but in some years – such as the COVID 19 events – it can be very high.
"Renforcement du système régional de surveillance des maladies". Bilateral donors were also partners of this initiative : US CDC, Canada, BMGF.
The shortcomings are pointed out by Glassman, Datema and McClellan (2018[42]), https://www.cgdev.org/blog/financing-outbreak-preparedness-where-are-we-and-what-next
More than the initial concept, the design of the instrument is at fault, argues for example Garrett (2019[43]), quoting Larry Summers, one of the intellectual advocates of the concept, but who criticised the way it was designed in practice.
Non-DAC members reporting to CRS have a quantitatively minor contribution. Other non-DAC members’ contributions that are not reporting to the OECD CRS are difficult to assess, but China had an important role in funding the African CDC, which has become the most prominent African institution in managing the COVID-19 outbreak
As often, there is some ambiguity around whether those sums correspond to “new” money raised or repurposing of already-committed financing
Asian Development Bank, Inter-American Development Banks, Islamic Development Bank and others.
Bill and Melinda Gates Foundation (2020[45]), https://www.gatesfoundation.org/Media-Center/Press-Releases/2020/02/Bill-and-Melinda-Gates-Foundation-Dedicates-Additional-Funding-to-the-Novel-Coronavirus-Response
According to the WHO, “Universal health coverage is defined as ensuring that all people have access to needed health services (including prevention, promotion, treatment, rehabilitation and palliation) of sufficient quality to be effective while also ensuring that the use of these services does not expose the user the financial hardship.”
Numbers based on: WHO (2018[46]), Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016. https://www.who.int/healthinfo/global_burden_disease/estimates/en/
It should be noted that these figures are prone to underestimate the donors engaged in NCD response and the amounts they are providing. NCD support has only become a separate reporting item in the OECD’s Creditor Reporting System in 2016. A significant portion of funding that potentially addresses NCDs is likely categorised as ‘health sector support’ and ‘other’.