Abstract
COVID‑19 hit the long-term care sector hard. This brief looks at mortality rates in care homes, as well as the policy responses undertaken during the pandemic. The brief assesses the emergency preparedness of the sector and highlights the lessons learned, including policies to reduce isolation, testing strategies, care workforce and co‑ordination with the health care sector.
The long-term care (LTC) sector was generally ill-prepared to tackle a health emergency: just over half of OECD countries had guidelines on infection controls in LTC before the pandemic. Deaths in the sector account for 40% of total COVID‑19 deaths. Early intervention has been key to contain the number of fatalities: the greater the time lapse between the first COVID‑19 case and the implementation of guidelines on tackling COVID‑19 in LTC, the higher the number of LTC deaths per million population among people aged 80 and over.
Most OECD countries banned visitors to LTC facilities and reduced group activities especially during the early months of the outbreak. Such restrictions of visitors and group activities had a toll on resident’s well-being.
Access to testing and personal protective equipment (PPE) in the initial phases of the pandemic was not sufficiently prioritised in the sector: more than 20% of workers did not use PPE in the third quarter of 2020. Correct identification of symptoms among residents in care homes and staff was limited due to lack of initial knowledge on screening, insufficient access to health professionals and testing availability. Ensuring more robust infection control training will also reduce preventable safety failures in the future.
High population density in LTC facilities has often been associated with worse outcomes. Shared rooms and other organisational hurdles rendered isolation of cases challenging. Alternative solutions for intermediate care, such as for example the emergency centres in Chile, and appropriate co‑ordination with health care professionals to ensure medical presence 24/7, as in Italy and Luxembourg, need to be put in place much more quickly in the event of future health crises.
A higher LTC staffing rate was strongly associated with lower infection and LTC death rates across countries in early 2020. Reducing staff movements between facilities has contributed to reducing viral spread, as workers have often been one of the key vectors for introducing the virus into facilities. Rapid recruitment and retention of staff remains challenging without addressing more structural issues in the sector, linked to pay adequacy and job quality. More efforts to support the physical and mental health of staff is also required, with three‑quarters of countries recognising COVID‑19 as an occupational disease. In the Netherlands, LTC workers could get additional mental health coaching while France organised support groups.
Only seven OECD countries generated guidelines for better integration of care services with hospitals and only six improved access to palliative care. Lack of good co‑ordination with the health system had a negative impact on providing appropriate medical care to LTC recipients at times when hospitals and primary care were under pressure. Ensuring appropriate medical monitoring and enhancing the availability of respiratory therapy services in LTC is an alternative when transfer to hospital is delayed or not possible.
Nearly all OECD countries have prioritised the sector for the rollout of COVID‑19 vaccination. Across OECD countries, high vaccination rates are associated with reductions in deaths and hospitalisations of LTC recipients and among the older people overall.
Going forward, improving LTC preparedness requires an assessment of preparedness at the level of LTC facilities with detailed knowledge of human and material resources and regular actualisation of protocols for different scenarios. In addition, enhancing LTC response to emergencies requires co‑ordination channels between public health authorities and the social sector, but also adequate follow-up mechanisms on the strategies undertaken with standardised data on infections and characteristics of facilities and residents.
The long-term care sector has proven particularly vulnerable during the COVID‑19 pandemic
COVID‑19 has disproportionately hit older people who are at higher risk of developing severe disease and death due to COVID‑19 because of being frail and having underlying medical conditions. The rate of COVID‑19 deaths1 among older people has been high with 4 500 deaths per million people aged over 60 while deaths among older people represent 90% of total COVID‑19 deaths (Figure 1). Residents of long-term care (LTC) facilities have been particularly impacted: across the OECD, 40% of total COVID‑19 deaths come from long-term care. The rate of LTC deaths in the older population is about 6 000 LTC deaths per million people aged over 80 on average, with LTC deaths ranging from under 2000 to over 15 000 deaths per million (Rocard, Sillitti and Llena-Nozal, 2021[1]).

Note: Data on cumulative deaths up to early May 2021, except for Canada, Italy and the United Kingdom (late April); the Czech Republic, Ireland, Japan, Lithuania and Slovenia (late February). Cross-country differences in coding and reporting affects comparability of results.
Data refer to those aged 65 and over and 85 and over for Austria, Belgium, Slovenia and the United States (65+ and 85+). The United Kingdom refers to England and Wales.
Source: COVID‑19 INED (2020[2]), “Demographics of COVID‑19 deaths”, https://dc-covid.site.ined.fr/en/, complemented with 2021 OECD Questionnaire on COVID‑19 and LTC. Eurostat (2021[3]), “Life expectancy by age and sex”, https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_mlexpec&lang=en, and OECD (2021[4]), “OECD Health Statistics”, https://doi.org/10.1787/health-data-en, for data on demographics (2018).
Emergency preparedness in long-term care was insufficient
At the onset of the COVID‑19 crisis, most OECD countries’ overall pandemic preparedness and response systems were not fully prepared to face the pandemic. Where emergency preparedness systems existed, they often lacked follow-up to update existing measures, hampering an adequate and timely reaction. In most cases, the existing pandemic preparedness plans did not focus on or prioritise the LTC sector and in some instances, never mentioned LTC facilities. In eight countries (Australia, Austria, France, Germany, Iceland, Ireland, Italy and Slovenia), despite the existence of emergency preparedness systems for the health care sector in general, specific measures for LTC were missing prior to 2020.
Fifteen countries had issued guidelines for infection control in LTC facilities and seven countries had specific emergency preparedness plans for the LTC sector. For instance Estonia performed crisis management exercises prior to the pandemic to test the country’s ability to react in case of emergency, while Japan had a Disaster Management bureau as well as a task force which could be activated when a large scale disaster takes place. Similarly, other countries had specific institutes for the management of emergencies, like Australia, Finland, the Netherlands and Belgium.
Since the start of the COVID‑19 pandemic, the percentage of OECD countries with public national guidelines on infection control in LTC rose from 53% prior to 2020, to 84%. Seven OECD countries that did not include the LTC sector in their emergency preparedness systems prior to 2020 developed new LTC-specific measures like guidelines, webpages, task forces and rapid response teams.
Early intervention limited the spread of COVID‑19 in LTC
At the early stage of the pandemic, a greater number of days between the first case and the first guidelines was related to a higher number of LTC deaths.2 Learning from the countries first hit by COVID‑19 helped other countries to improve preparedness and buffer the impact of the pandemic. More stringent social distancing had a key role on reducing mortality in communities and hospitals and also affected community transmission into the LTC sector. In Austria the share of LTC deaths was dramatically lower in regions where regional governments applied more screening and stricter visit restrictions in LTC facilities (Leichsenring, Schmidt and Staflinger, 2020[5]).
The strong focus on containment was initially hampered by lack of prioritisation of the sector for testing and shortage of equipment
The initial priority to reduce interactions was plagued by organisational hurdles
Initial guidance for the sector concentrated on containment and mitigation strategies in LTC, aiming to minimise the risk of transmission of infections and to slow down the spread of the virus. Restrictions to shelter residents within facilities have been very common, with 32 OECD countries implementing such measures. A number of countries initially banned visitors in early 2020, except for emergency reasons, and later reinstituted visitor access. The Czech Republic initially banned visits and afterwards permitted them, providing visitors adhered to hygiene standards and underwent testing. Estonia and Hungary allowed visits in LTC facilities after use of PPEs and adherence to 2 metres social distancing and if possible, in special meeting rooms or outdoors. Large group activities such recreational activities were heavily restricted. In 17 countries, it was also recommended that meals be eaten in bedrooms on a regular basis. Other countries kept such activities as usual, although encouraging distance among residents. In Demark, for instance, joint activities and meals were done in small groups.
Prior to the pandemic, different studies had indicated that outbreaks of infectious diseases occurred in the sector because of suboptimal infection control practices. For example, in Belgium, a small survey showed that about 15% of nursing homes did not have virucidal products and 19% did not disinfect appropriately medical devices at the early stage of the pandemic (Médecins Sans Frontières, 2020[6]). Conversely, Japan, which had well-established routine protocols of infection prevention and control, and effective communication channels between the regulatory authorities and the LTC facilities after SARS, was well prepared at the onset of the pandemic. Despite the importance of heightened hygiene to prevent and control COVID‑19 infection, about 90% of surveyed countries did not take any specific measure to recruit cleaners and other non-care workers in LTC facilities.
There were also challenges linked to organisational features in LTC facilities. Congregate living, whereby persons share common spaces, played a role in explaining higher mortality rates in LTC facilities. A study in Ontario, Canada, showed that higher population density in LTC facility was associated with higher incidence of COVID‑19 infection and mortality (Brown et al., 2020[7]). Evidence from Spain suggests that mortality rates were associated with the median size of the nursing homes and the occupation rate across regions (Fundación de Estudios de Economía Aplicada, 2020[8]).
Not only did multiple occupancy rooms facilitate the spread of infection, but it also hindered the implementation of isolation measures of suspected or infected cases. In Austria, complete isolation was almost impossible in nursing homes in part because of the presence of double occupancy rooms for residents. Certain countries, like Japan, followed strict isolation protocols transferring cases to other facilities. In Chile, the design of strict hygiene and safety protocols teamed with isolation often in outside facilities (intermediate care), together with proactive and reactive testing of residents and caregivers helped saving 411 lives of older people by September 2020, and averted 1 468 infections among care home residents and 857 hospitalisations in critical care beds (Singer, 2020[9]).
Challenges in balancing safety and well-being remain
Many containment strategies made LTC recipients even more socially isolated, with significant repercussions for residents’ mental health in some cases. Many LTC residents experienced severe functional and cognitive decline, deterioration in physical health, severe loneliness and social isolation, while evidence suggests an increased use of psychotropic medications and physical restraints (Stall et al., 2020[10]).
The trade‑off between security and freedom in LTC facilities has long been a challenge that COVID‑19 has exacerbated. A study from the Netherlands showed that when one visitor per resident was allowed and nursing homes followed national guidelines, no new COVID‑19 infections were reported in surveyed nursing homes (Verbeek et al., 2020[11]). In-person visits with family have the potential to improve mental health outcomes. In Australia, some providers implemented a concierge service to co‑ordinate and screen visitors, as well as dedicated communications teams within facilities to improve co‑ordination between residents and their families. These initiatives were dependent upon adequate additional staffing and therefore required extra funding.
Disruptions in care were partly addressed by boosting telehealth
In most OECD countries, all day care centres closed during the initial months at the national level. Closure of all day care centres and pausing the provision of LTC at home at the national level had a massive impact. For example, over 545 000 older people did not receive community-based LTC in Colombia during the first wave, while closure of day care centres affected an estimated 21 000 older people in the Czech Republic and 25 000 older people in Greece. Moreover, home care decreased in 18 OECD countries. Care disruption also placed additional burdens on informal carers.
Many older people receiving home care had to forgo care for fear of infection, or were asked to postpone it during July-August 2020 (Figure 2). One particular concern in terms of care continuity has been access to physiotherapy, rehabilitation and all types of physical activity among LTC recipients. Some countries undertook targeted efforts to prevent such concerns. For instance, in Navarre, Spain, 85% of nursing homes organised physical activity exercises and emotion management (Fresno, 2020[12]). In Chile, special isolation facilities for those infected by COVID‑19 were coupled with an additional budget for rehabilitation and reablement.
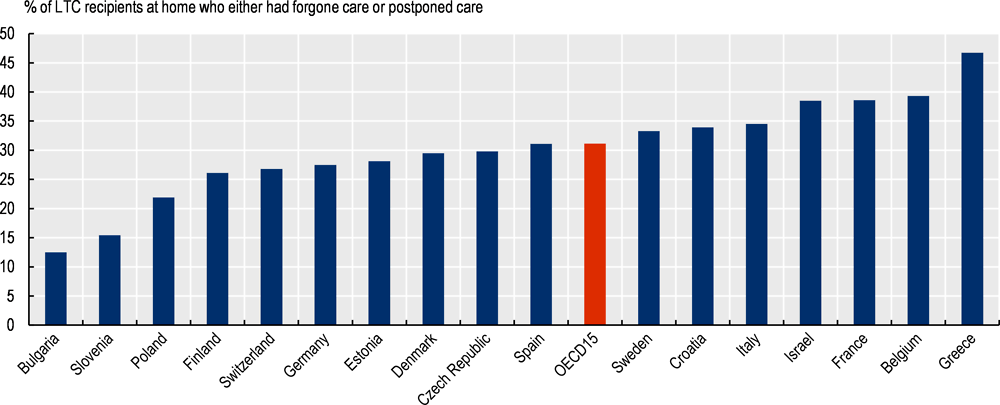
Note: LTC recipients refer to those aged 65 years old receiving regularly home care who reported ADL or IADL limitations in SHARE wave 7 (2017). Question on forgone care is “Since the outbreak of Corona, did you forgo medical treatment because you were afraid to become infected by the corona virus?” and the question on postponed care is “Did you have a medical appointment scheduled, which the doctor or medical facility decided to postpone due to Corona?”
Source: SHARE‑COVID‑19 wave 8 (data refer to June and August 2020).
In most countries, one key measure to ensure care continuity for older people was the scaling-up of digital technology. Over half of surveyed OECD countries did not have programmes or guidelines on the development of telehealth services in LTC before the outbreak. Since then, 21 OECD countries expanded the use of telehealth services to allow remote consultations between patients and the health care sector and to keep LTC residents in touch with their relatives outside the facilities. Six countries (Belgium, Denmark, France, Hungary, Ireland and Norway) set up coverage rates or fee‑for-consultation of telehealth services. Two-thirds of surveyed countries developed teleservices to maintain contact between the LTC recipients and their relatives, for example through tablets. Over 40% of surveyed countries use more remote management, data-sharing and monitoring technologies. In Hungary, digital teleservices included teleconsultations as well as triage before hospital admission. In Australia, home‑based recipients received support to use tablets and digital technology was also used to connect LTC facilities with doctors.
Limited testing and personal protective equipment prevailed in the early phases
The LTC sector was typically not prioritised for PPE and testing across many OECD countries at the onset of the pandemic, with some exceptions. In a ranking from 1 (not an issue) to 5 (extremely challenging), countries defined access to PPE as 3 and access to testing as 4. Korea, a country that took particularly swift measures, developed a strategy to avoid shortages of PPE from March 2020. It established a working group to manage supplies and an IT system to distribute 5.46 million public masks for 770 000 employees via long-term care providers in a timely manner. Across OECD countries, there was also an initial lack of clarity with respect to PPE, as physical distancing was initially perceived as sufficient in some countries and not all LTC workers wore PPE when caring for older people in the second and third quarter of 2020 (Figure 3).

Note: LTC recipients refer to those aged 65 years old receiving regularly home care who reported ADL or IADL limitations in SHARE wave 7 (2017). Question is “Did the people who cared for you wear protective devices such as masks or gloves?”
Source: SHARE‑COVID‑19 wave 8 (data refer to June and August 2020).
All surveyed OECD countries have learnt from initial PPE shortages and stockpiled PPEs in 2021, although recommendations on the minimum stockpiles varied across countries. For example, in Lithuania, the stockpile of each LTC provider should be sufficient for 30 days and the national level stockpile is sufficient for 60 days. In Norway, municipalities order PPEs with the help of a web-calculator made available by national authorities.
In most cases, national or local governments funded the supply of PPE to LTC facilities. Among surveyed countries, only in Colombia and the Czech Republic did workers contribute to the purchase of PPE, and only in Lithuania did LTC recipients at home pay for their own PPE among surveyed countries. There are also some hybrid systems, such as Japan, where each LTC facility pays for PPEs, but when there is a surge in the use of PPE, the national or sub-national government provides PPE for free. In addition, national subsidies for PPE purchase are available to LTC facilities.
In the wake of the COVID‑19 crisis, insufficient testing in nursing homes slowed effective detection and isolation of confirmed cases. Since then, 21 of the surveyed OECD countries implemented measures to increase testing capacity for LTC workers and residents. In 13 countries, LTC facilities received support that included training and equipment for staff; 11 countries set up mobile teams to facilitate testing in facilities; and 10 countries provided extra funding to facilities to finance testing. In the overwhelming majority of countries, the government covered the cost of testing for workers and residents. Other measures to improve testing capacity also existed, as in Germany, where the federal government supplied and financed volunteers and Armed Forces personnel to support testing in LTC facilities; while in Greece, starting from February 2021, new legislation allowed hospitals to provide LTC facilities with free rapid tests.
By March 2021, most OECD countries had policies to test LTC workers and residents with COVID-like symptoms and when they have been in contact with a confirmed or suspected COVID‑19 case. This can still be problematic because of asymptomatic cases: a Spanish study screened people in nursing homes in April 2020 and showed that about 24% of residents and 15% of staff were positive and that, among them, 70% of residents and 56% of staff were asymptomatic (Borras-Bermejo et al., 2020[13]). Routine testing of residents and workers is less frequent among OECD countries, but it is often compulsory to test new residents before admitting them to the facility.
Despite efforts to boost staff, workforce challenges persist
Task forces and mobile teams supported rapid responses and LTC workers
During the COVID‑19 pandemic, OECD countries have often established task forces as part of their response. These consist of groups of experts organised at the national, local or facility level with the aim of managing and co‑ordinating responses to the COVID‑19 crisis. Almost half of the countries created specific task forces for LTC. In countries where there was no LTC-specific task force, 35% of these countries included experts of the sector in the task forces’ boards (Australia, Denmark, France, Germany, Greece, Hungary, Korea, the Netherlands, Portugal). Some countries have permanent task forces that intervene when a crisis takes place (Denmark, Korea). In some countries, the task force provided direct support to the LTC facilities. This is the case of Finland, where municipalities created local task forces composed by the head of the LTC facility and the physician responsible for LTC facility together with the physician responsible for communicable diseases and other relevant actors that operated alongside a national task force.
Around 90% of surveyed countries prepared rapid response teams, either at the national or subnational level, to counteract staff shortages. Rapid response teams have supported continuity of care in LTC facilities during the crisis by providing help to overwhelmed facilities. Most countries deployed rapid response teams constituted by workers from different sectors or from geographical areas less hit by the crisis. This was the case in Italy; with home care workers deployed into LTC facilities in case of staff shortages. Similarly, in Australia, experienced aged care workers have been called to move from areas without transmission of the virus to areas where the emergency had caused personnel’s shortages. In at least four countries, the army deployed personnel to the facilities in need (Canada, the Czech Republic, Estonia, Germany).
Insufficiently skilled workers hamper the effectiveness of policies
The number of staff was curtailed by sickness and isolation during the pandemic. LTC workers were at higher risk of being infected: in Portugal, workers in LTC facilities accounted for about a third of COVID‑19 related sick leave (European Trade Union Institute, 2021[14]). Numerous OECD countries have now recognised the risk of LTC workers being infected by COVID‑19 in the workplace. Almost three‑quarters of OECD countries have labelled COVID‑19 as an occupational disease or in a few cases as an accident at work but compensation rules vary widely across EU countries (ILO, 2021[15]).
Facilities with lower numbers of LTC workers were associated with higher infection rates. The sector suffers from structural challenges to recruit and retain workers and, during the pandemic, over half of surveyed countries provided financial help to LTC facilities for recruitment. About 40% of surveyed countries supported the recruitment of LTC students through financial help. In Belgium, Canada (some provinces), Estonia, France, Luxembourg, the Netherlands and Finland (some municipalities), a pool of volunteers was available for emergencies and activated to boost LTC staff. Portugal hastened the accreditation of foreign diplomas; Luxembourg signed short-term contracts with foreign workers; and in Australia, international students were temporarily allowed to work. In four OECD countries (Greece, Germany, Luxembourg and Norway), the maximum number of working hours were increased or lifted.
Many countries decided to reward LTC workers for their exceptional efforts and improve their working conditions. About 40% of surveyed OECD countries provided a one‑off bonuses to reward LTC workers for their exceptional efforts. Four countries also improved wages permanently following the start of the pandemic (Czech Republic, Germany, France, and Korea). Additional measures are likely to be needed in the long-term, possibly through the use of collective bargaining to promote stable employment relationships.
Staff ratios became a renewed source of debate in many surveyed OECD countries since the beginning of the COVID‑19 pandemic. Since the onset, four countries introduced guidelines on staff ratios (Japan, Lithuania, the Netherlands, and Slovenia). In Ontario, Canada, the provincial government announced in November 2020 a commitment to increase the minimum number of hours of direct care to an average of four hours per resident by 2024‑25. Colombia is in the process of adopting a regulation to set a staff ratio by LTC facility varying between one staff member for every 12 residents to one staff member for every 20 residents depending on the degree of LTC needs of older people. In Finland, under the Older Person’s Care Act, staffing ratio will be gradually increased from 0.5 to 0.7 by 2023 and will vary depending on LTC needs’ assessments.
During the pandemic, several countries made efforts to provide exceptional training to LTC workers to implement infection protocols or other prevention and care activities. Among surveyed countries, 17 countries provided additional training on infection control, 16 countries on use of PPE, and 12 countries on other safety procedures. In addition, eight countries offered exceptional training on palliative care during the pandemic and six countries on physical and mental well-being. Going forward, it remains critical that countries continue to offer infectious disease training, as well as to set up health and safety structures.
The pandemic has also negatively affected the mental health of LTC workers. Given the unprecedented nature of COVID‑19 outbreaks in LTC facilities, a number of countries have offered support on mental well-being to LTC workers. Among surveyed countries, 15 countries provided LTC workers access to a free phone line as part of psychological support during the acute phases of the pandemic. Another 12 countries offered LTC workers access to specialist consultations as part of a psychological support package.
Reducing staff movement helped to limit containment
LTC workers represent (along with visitors) potential transmission vectors. For example, a study in New Zealand found in three out of five affected facilities, that the outbreak originated from a staff member (Ministry of Health, New Zealand, 2020[16]). In a number of countries – including the Czech Republic, England, Estonia, and Norway – the weekly share of positive LTC residents often mirrored that of LTC workers, with generally larger peaks among LTC residents than LTC staff during outbreaks.
A prevalent challenge in the containment strategy is restricting the movement of staff between long-term care facilities, as many LTC workers work multiple part-time jobs. In 12 countries, policies included the creation of COVID‑19 wards. Ten countries introduced policies to reduce multiple‑site work. Ten countries initiated policies to reduce staff rotation within LTC facilities. Single‑site policies were introduced in only seven countries while staying-on site policies was uncommon. In France, centres where staff remained voluntarily confined with residents saw a much lower infection rate than others (0.4% versus 4.4%) as well as lower mortality (Belmin et al., 2020[17]).
Evidence suggests that limiting the mobility of staff is important in limiting transmission. In Canada, multiple provinces implemented emergency single‑site measures. In Ontario, Canada, a study found that mobility between nursing homes fell by 70% after the emergency order by the Ontario Government restricted long-term care staff to a single nursing home (Jones et al., 2021[18]).
Ensuring good co‑ordination with health care should remain a priority
COVID‑19 has magnified the impact of poor care integration when attempting to protect care recipients. Poor co‑ordination between primary and long-term care is a long-standing issue in LTC. In 2019, between 36% and 88% of the primary care providers in 11 OECD countries reported not co‑ordinating care frequently with social care or other community care services (Doty et al., 2020[19]). This generated particular challenges in LTC residences in places where transfer to hospital was not forthcoming, especially during the early phase of the pandemic.
Since the outbreak, 24 OECD countries reported having implemented measures to improve care co‑ordination (e.g. deployment of medical staff to LTC facilities to treat residents with COVID‑19, covering the extra-cost of COVID‑19 residents in facilities and co‑ordination plans across health settings). Approaches to organising a response in the LTC sector have differed between OECD countries, in terms of responsibilities for guidelines, implementation and enforcement. Ten OECD countries reported having guidelines or legislation on the integration of long-term care and primary care before the outbreak. Eight OECD countries have introduced new measures to foster multi-disciplinary teams, with the aim to integrate more primary care in LTC facilities. In France, a new financial incentive is provided to incentivise primary care doctors visiting LTC residents. Italy and Luxembourg have required nursing homes to have a 24/7 medical presence to ensure follow-up care of ill LTC residents (WHO/European Observatory on Health Systems and Policies, 2020[20]). In Korea, a recent initiative ensured that LTC facilities receive at least one doctor visit twice a week to improve continuity of care by introducing more medical care in nursing homes.
Since the outbreak, seven countries have introduced new guidelines on the integration of long-term care and care in hospital. In general, these guidelines aim to minimise transfer from nursing homes to hospitals, as well as to share expertise, especially from the geriatric units of hospitals to staff within nursing homes. For example, in Upper Austria, hygiene specialists from hospitals went to LTC facilities at the beginning of the crisis to monitor hygiene standards and support possible improvements (Leichsenring, Schmidt and Staflinger, 2020[5]). Belgium presented in April 2020 a framework for hospitals to provide expertise, transfer staff, help with equipment or products, and provide support in the screening process to the LTC sector.
Despite the growing number of guidelines for the LTC sector during the COVID‑19 crisis, guidelines rarely mentioned palliative care. Only 6 out of 29 countries mentioned palliative care needs and guidelines included, for instance, the management of the transfer of people at the end of life across settings and/ or the activation of helplines for health care workers to receive counselling on the provision of palliative care. In the United Kingdom, there has been increased uptake of the Electronic Palliative Care Co‑ordination System (EPaCCS), a local initiative of palliative care shared records that enables different health and care organisations to share information about a patient’s end of life preferences and care plans (Crouch, 2020[21]).
Effective vaccination campaigns have shown initial positive results
When vaccination became available, the 28 countries for which data are available prioritised care home residents and staff at the first stage of the vaccination rollout, and all older people were included in a second stage or in parallel. In order to facilitate the vaccine’s administration, the COVID‑19 vaccines for LTC recipients were provided through mobile teams or through the LTC doctors and nurses in most OECD countries. In some cases, people receiving home care could receive the vaccine from the GPs and could be accompanied to the vaccine’s site by home care personnel (e.g. Australia). In other cases, such as in Denmark and the United Kingdom, housebound people can receive the vaccine in their homes.
Determining the vaccines’ impact in reducing COVID‑19 cases and/or deaths is challenging due to the plethora of measures currently in place to decrease the virus transmission but early evidence has emerged among older people. Evidence of vaccination’s effectiveness has emerged from the LTC sector. In Chile, the death rate for the LTC population declined from 20% to 7% following the vaccination campaign. A study carried out by the American Health Care Association indicated that LTC facilities with vaccinated residents and staff experienced a decline in cases of 48% among residents and 33% among staff three weeks after vaccination, compared to respectively 21% and 18% in LTC facilities without vaccine rolled out (Domi et al., 2021[22]). In Spain, between the 4 January and 4 April 2021, the number of positive cases registered in LTC facilities plummeted from 2 807 to 56 and the number of deaths decreased from 365 to 2 (IMSERSO, 2021[23]).
Studies revealed that older people and LTC recipients tend to develop a weaker antibody reaction after receiving the vaccine (Brockman et al., 2021[24]). These results have led to discussion around the possibility to administer a third vaccine dose to people aged 60 or older. Israel was the first country to announce this measure on the 1 August 2021 and highlights that those with the third dose were 11.3 times less likely to be infected with the Delta variant (Bar-On et al., 2021[25]). The FDA and the EMA (together with the ECDC) approved the possibility of a booster shot for people aged 60 or older respectively on the 12 August 2021 and on the 6 September 2021. Following on, a number of countries, including, France, Germany, Italy, Spain, the United Kingdom and the United States started to administer third doses to vulnerable populations in September 2021.
References
[25] Bar-On, Y. et al. (2021), “Protection of BNT162b2 Vaccine Booster against Covid-19 in Israel”, New England Journal of Medicine, http://dx.doi.org/10.1056/nejmoa2114255.
[17] Belmin, J. et al. (2020), “Coronavirus Disease 2019 Outcomes in French Nursing Homes That Implemented Staff Confinement With Residents”, JAMA Network Open, Vol. 3/8, p. e2017533, http://dx.doi.org/10.1001/jamanetworkopen.2020.17533.
[13] Borras-Bermejo, B. et al. (2020), “Asymptomatic SARS-CoV-2 Infection in Nursing Homes, Barcelona, Spain, April 2020”, Emerging Infectious Diseases, Vol. 26/9, pp. 2281-2283, http://dx.doi.org/10.3201/eid2609.202603.
[24] Brockman, M. et al. (2021), Weak humoral immune reactivity among residents of long-term care facilities following one dose of the BNT162b2 mRNA COVID-19 vaccine, Cold Spring Harbor Laboratory, http://dx.doi.org/10.1101/2021.03.17.21253773.
[7] Brown, K. et al. (2020), “Association Between Nursing Home Crowding and COVID-19 Infection and Mortality in Ontario, Canada”, JAMA Internal Medicine, http://dx.doi.org/10.1001/jamainternmed.2020.6466.
[2] COVID-19 INED (2020), Demographics of COVID-19 deaths, https://dc-covid.site.ined.fr/en/ (accessed on 26 July 2021).
[21] Crouch, H. (2020), Electronic system to improve patients’ end of life care shared nationally, Digital Health, https://www.digitalhealth.net/2020/11/electronic-system-to-improve-patients-end-of-life-care-shared-nationally (accessed on 9 December 2020).
[22] Domi, M. et al. (2021), Nursing Home Resident and Staff Covid-19 Cases After the First Vaccination Clinic, http://www.CHPE-LTC.org.
[19] Doty, M. et al. (2020), “Primary Care Physicians’ Role In Coordinating Medical And Health-Related Social Needs In Eleven Countries”, Health Affairs, Vol. 39/1, pp. 115-123, http://dx.doi.org/10.1377/hlthaff.2019.01088.
[14] European Trade Union Institute (2021), Covid-19 as occupational disease: the need for European homogenisation, https://www.etui.org/news/covid-19-occupational-disease-need-european-homogenisation (accessed on 5 May 2021).
[3] Eurostat (2021), “Eurostat Database”, Life expectancy by age and sex, https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_mlexpec&lang=en (accessed on 19 May 2021).
[12] Fresno, J. (2020), Estudios propios, Auditoría de los centros residenciales en Navarra ante la crisis de la Covid-19. Observatorio de la Realidad Social de Navarra, Observatorio de la Realidad Social,, https://www.observatoriorealidadsocial.es/es/estudios/auditoria-de-los-centrosresidenciales-en-navarra-ante-la-crisis-de-la-covid-19/es-556293/# (accessed on 15 April 2021).
[8] Fundación de Estudios de Economía Aplicada (2020), La asistencia residencial en España y COVID-19, https://www.fedea.net/la-asistencia-residencial-en-espana-y-covid-19/ (accessed on 15 April 2021).
[15] ILO (2021), State practice to address COVID-19 infection as a work-related injury, https://www.ilo.org/global/topics/geip/publications/WCMS_768009/lang--en/index.htm (accessed on 4 May 2021).
[23] IMSERSO (2021), Actualización nº 6. Enfermedad por coronavirus (COVID-19) en Centros Residenciales. 4/4/2021, https://www.imserso.es/InterPresent2/groups/imserso/documents/binario/inf_resid_20210404.pdf.
[18] Jones, A. et al. (2021), “Impact of a Public Policy Restricting Staff Mobility Between Nursing Homes in Ontario, Canada During the COVID-19 Pandemic”, Journal of the American Medical Directors Association, Vol. 22/3, pp. 494-497, http://dx.doi.org/10.1016/j.jamda.2021.01.068.
[5] Leichsenring, K., A. Schmidt and H. Staflinger (2020), The second wave has hit Austria harder – also in care homes, LTCcovid, https://ltccovid.org/2020/11/27/the-second-wave-has-hit-austria-harder-also-in-care-homes/ (accessed on 9 December 2020).
[6] Médecins Sans Frontières (2020), Les laissés pour compte de la réponse au Covid-19, Partage d’expérience sur l’intervention de Médecins Sans Frontières dans les maisons de repos de Belgique,, https://www.msf-azg.be/sites/default/files/imce/Rapport_MaisonsDeRepos/MSF_lessons%20l.
[16] Ministry of Health, New Zealand (2020), Independent Review of COVID 19 Clusters in Aged Residential Care Facilities, https://www.health.govt.nz/publication/independent-review-covid-19-clusters-aged-residential-care-facilities (accessed on 30 June 2020).
[4] OECD (2021), OECD Health Statistics, OECD Publishing, Paris, https://doi.org/10.1787/health-data-en.
[1] Rocard, E., P. Sillitti and A. Llena-Nozal (2021), “COVID-19 in long-term care: impact, policy responses and challenges”, OECD Health Working Papers, OECD Publishing, Paris.
[9] Singer, M. (2020), Performance of Care Homes for the Elderly in Chile against Covid-19, Pontificia Universidad Católica de Chile.
[10] Stall, N. et al. (2020), “Finding the Right Balance: An Evidence-Informed Guidance Document to Support the Re-Opening of Canadian Nursing Homes to Family Caregivers and Visitors during the Coronavirus Disease 2019 Pandemic”, Journal of the American Medical Directors Association, Vol. 21/10, pp. 1365-1370.e7, http://dx.doi.org/10.1016/j.jamda.2020.07.038.
[11] Verbeek, H. et al. (2020), “Allowing Visitors Back in the Nursing Home During the COVID-19 Crisis: A Dutch National Study Into First Experiences and Impact on Well-Being”, Journal of the American Medical Directors Association, Vol. 21/7, pp. 900-904, http://dx.doi.org/10.1016/j.jamda.2020.06.020.
[20] WHO/European Observatory on Health Systems and Policies (2020), What measures have been taken to protect care homes during the COVID-19 crisis? – Cross-Country Analysis, https://analysis.covid19healthsystem.org/index.php/2020/06/08/what-measures-have-been-taken-to-protect-care-homes-during-the-covid-19-crisis/ (accessed on 30 April 2021).
Contact
Francesca COLOMBO (✉ francesca.colombo@oecd.org)
Ana LLENA-NOZAL (✉ ana.llenanozal@oecd.org)
Paola SILLITTI (✉ paola.sillitti@oecg.org)
Eileen ROCARD (✉ eileen.rocard@oecd.org)
Notes
Comparability of COVID‑19 deaths differs across countries because of differences in recording, registration and coding practices across countries, especially at the beginning of the pandemic when availability of diagnostic tests varied.
OECD analysis not shown here based on a regression analysis between the number of days between the first case and the first guidelines on COVID‑19 in LTC and included in Rocard, Sillitti and Llena-Nozal (2021[1]).