Abstract
The COVID‑19 pandemic and its associated government measures to limit mobility impacted patterns and places of alcohol consumption. While the path to recovery remains long and difficult, this crisis also increases the risk that individuals engage in harmful drinking to cope with stress. During the COVID‑19 pandemic, there has been an increase in domestic violence, for which harmful alcohol consumption is a risk factor.
Harmful alcohol consumption damages health, causes diseases and injuries, weakens response to COVID‑19, and leads to significant economic and societal costs. Comprehensive policy packages built on a PPPP approach including Pricing policies, Policing to counter drink-driving, Primary care‑based counselling for heavy drinkers, and regulating alcohol Promotion activities, improve health, and support a stronger economic and social recovery in the aftermath of the pandemic.
During the COVID‑19 pandemic, people have significantly changed drinking habits, shifting places of consumption from bars and restaurants to home. For many people, alcohol is part of their social life, a life that has been significantly disrupted by COVID‑19. Overall, most people did not change how much they drank but, among those who did, a larger proportion of people drank more. Looking at preliminary government tax receipt data, alcohol sales increased by 3% to 5% in Germany, the United Kingdom and the United States in 2020 compared to 2019. Sales of alcohol in bars and restaurants plummeted, severely affecting this sector, while off-premise sales, such as e‑commerce and retail stores, grew significantly. For example, in the United States, online sales increased by up to 234%.
Some of the problems associated with harmful alcohol consumption were intensified by the crisis, even though the long-term impacts of COVID‑19 on alcohol consumption are uncertain. During the COVID‑19 lockdowns, women, parents of young children, people with higher income and those with anxiety and depressive symptoms reported the highest increase in alcohol consumption, for instance in Australia, Belgium, France, the United Kingdom and the United States. Emergency calls about domestic violence, for which harmful alcohol consumption is a risk factor, rose by 60% in EU countries. There is also a risk that COVID‑19 causes an increase in problematic drinking in the medium term, given that excessive alcohol consumption is common after traumatic events as a response to high stress levels.
Harmful alcohol consumption takes a heavy toll on people, the economy and the society. Over the next 30 years and on average across OECD countries, diseases and injuries caused by drinking more than 1 drink per day for women and 1.5 drinks per day for men – corresponding to lower-risk thresholds specifically used for the simulation – will cause life expectancy to be 0.9 years shorter than it otherwise would be; they will be also responsible for about 2.4% of total health expenditure; while GDP will be 1.6% lower than otherwise due to reduced workforce participation and productivity.
Governments have at their disposal a battery of policy interventions to tackle harmful alcohol consumption and prevent related diseases. A policy package based on a “PPPP” approach including Policing to counter drink-driving, strengthening Primary care‑based counselling for heavy drinkers, regulation on Promotion, including a ban on alcohol advertising to children, and Pricing policies particularly to target cheap alcohol has the potential to prevent diseases and injuries, increase life expectancy and generate savings that are greater than the implementation costs.
Preventing alcohol-related diseases and injuries has a triple dividend. First, reducing alcohol use helps individuals cope with infections and develop immunity after vaccination. Second, preventing alcohol use and its associated diseases reduces pressure on health care services – which are already under heavy strain from COVID‑19. Third, with prevention of harmful alcohol consumption, a healthier and more productive population will better help restart economic activities and social life in the aftermath of the pandemic. Investing in protecting children and people with problematic drinking is particularly important during the pandemic. Primary care‑based counselling for heavy drinkers, regulation on advertising or promoting alcoholic beverages on TV, the Internet and social media targeting children, and minimum unit price policies targeting cheap alcohol, are particularly well suited to address some of the priority areas in alcohol policy during the COVID‑19 pandemic.
The COVID‑19 pandemic has significantly changed people’s lifestyles, including drinking habits
The COVID‑19 pandemic has changed people’s lifestyles, including their drinking habits. Governments’ often stringent policies to contain the spread of the virus have generally been effective in keeping people at home. For example, 39% of workers in the OECD shifted to teleworking (OECD, 2020[1]) and millions of children switched to online learning and home schooling. Leisure time was also affected with, for example, a sharp increase in time spent online. Drinking habits – quantity, frequency and place of drinking – have also changed. Specifically, the latest data suggests that:
Overall, most people did not change their drinking amount but among those who did, a larger proportion of them increased consumption. Findings from a survey1 carried out in Australia, Austria, Brazil, France, Germany, Ireland, the Netherlands, New Zealand, Switzerland, the United Kingdom and the United States between May and June 2020 (Winstock et al., 2020[2]) show that 36% of individuals increased their consumption of alcohol, 22% decreased their consumption and 42% reported no change in the quantity drunk.
A small increase in alcohol purchases is also observed in government data monitoring sales, at least in countries for which data are available. For example, in the United Kingdom, the total alcohol duty receipts showed a 4.5% increase in the period April to October 2020, compared to the same period in the previous year (data not adjusted for inflation) (HM Revenue and Customs, 2020[3]). Similarly, US data from 15 states suggest a 4% increase in the quantity of alcohol sold in the period January to August 2020, compared to the same period in 2019 (National Institute on Alcohol Abuse and Alcoholism, 2020[4]). German data show an increase in alcohol tax revenues of 3.3% in 2020, compared to 2019 (Bundesministerium der Finanzen, 2021[5]). Stockpiling in the early phases of the pandemic may have also contributed to these trends.
People increased their drinking frequency, but binge drinking frequency was not greatly modified. In the 11 countries for which data are available, 43% of individuals reported an increased drinking frequency, compared to a quarter of adults who decreased their drinking frequency. The probability of binge drinking – drinking more than 80% of a bottle of wine or 1.5 litres of beer per drinking occasion – did not change for nearly half of the population. About 29% of the respondents reported binge drinking less frequently, though 23% said they binge drank more frequently.
While the hospitality sector, such as hotels, bars and restaurants, was severely hit by the crisis, other sectors such as retail stores and e‑commerce saw increasing sales. Alcohol sales in bars, pubs, restaurants and nightclubs plummeted because of the lockdowns. But alcohol consumption increased at home, with a significant increase in sales in retail or online stores. For instance, off-premise sales in Belgium, Spain and the United States showed a significant growth (Eurocare, 2020[6]; Nielsen, 2020[7]). Alcohol e‑commerce has increased in Australia, Brazil, Canada, China, Colombia, France, Germany, India, Italy, Japan, Mexico, Poland, the Russian Federation, South Africa, Spain, Thailand, Turkey, the United Kingdom, and the United States (IWSR, 2020[8]), with a +234% growth in the case of the United States (Nielsen, 2020[7]).
The crisis intensified some of the harms and problems arising from harmful alcohol use
Some population groups increased alcohol consumption more than others
Harmful patterns of alcohol consumption such as underage drinking, heavy drinking, or binge drinking are highly prevalent in some population groups, and the COVID‑19 restrictions have intensified this tendency. Prior to the COVID‑19 crisis, monthly binge drinking – that corresponds to drinking more than 80% of a bottle of wine, or 1.5 litres of beer in a single occasion – was a habit for one in three adults on average in OECD countries, with women with higher education and people with the lowest and the highest incomes particularly at risk (OECD, 2021[9]). In addition, alcohol is disproportionately consumed by a minority: people who drink heavily – that corresponds to men and women consuming more than 40 grammes and 20 grammes of pure alcohol per day, respectively – make up 4% to 14% of the population, depending on the country, but they consume between a third and half of all alcohol consumed, according to an analysis of six OECD countries (OECD, 2021[9]).
During the COVID‑19 lockdowns, women, parents of young children, middle‑age people, people with higher income and individuals with depressive and anxiety symptoms reported the highest increase in alcohol consumption, for example in Australia, Belgium, France, the United Kingdom and the United States (Gisle et al., 2020[10]; Santé Publique France, 2020[11]; Sallie et al., 2020[12]; Pollard, Tucker and Green, 2020[13]; Tran et al., 2020[14]). Looking at the future, there is a risk that COVID‑19 causes an increase in problematic drinking in the medium term. Increased alcohol use is common after traumatic events, and excessive alcohol consumption can be a response to high stress levels. Undoubtedly, COVID‑19 has disrupted people and communities across the world, creating the conditions for long-term physical and mental distress, increasing the risk of high levels of alcohol consumption, even after the crisis ends.
Domestic violence incidents increased
Harmful alcohol use is responsible for injuries, including road traffic crashes and violence, and it is a risk factor for intimate partner violence and child maltreatment, among others. The Preventing Harmful Alcohol Use report shows that drinking more than 1 drink per day for women and 1.5 drinks per day for men – corresponding to a lower-risk threshold – causes 37 million cases of injuries over the next 30 years in 52 countries, representing 4% of all injuries occurring in these countries (OECD, 2021[9]). In terms of treatment costs, such drinking will be responsible for about 4% of all the expenditure to treat injuries.
While road traffic crashes dropped (OECD/ITF, 2020[15]), lockdowns and stay at home orders have exacerbated some of the negative behaviours associated with harmful alcohol consumption, such as domestic violence. Nearly one in three women will have experienced physical and/or sexual violence by an intimate partner in their lifetime, and one‑in-three children experience some form of violence by parents or other family members (WHO, 2021[16]). During the pandemic, there has been an increase in the number of emergency calls to helplines to report domestic violence in countries such as Austria, Italy, Mexico, Spain and the United Kingdom, to name a few (Silverio-Murillo, Balmori de la Miyar and Hoehn-Velasco, 2020[17]). Across EU countries, there has been a 60% rise in emergency calls about domestic violence (Mahase, 2020[18]).
Harmful alcohol drinking damages health and causes significant economic and societal cost
For many people, alcohol consumption is an enjoyable part of their social life. During lockdowns and restrictions introduced to tackle COVID‑19, social life has been significantly disrupted and the hospitality sector has been severely affected. However, harmful patterns of alcohol consumption remain dangerous for the health of people and costly for societies, as shown by the recent OECD report Preventing Harmful Alcohol Use (OECD, 2021[9]).
Lower life expectancy
Alcohol consumption is a major risk factor for chronic diseases such as alcohol dependence, liver cirrhosis, diabetes, cardiovascular diseases, cancers, and injuries. OECD estimates (pre‑dating COVID‑19) suggest that drinking more than 1/1.5 drinks per day contributes to about 1.1 billion new cases of alcohol dependence (88% of all the cases), 37 million cases of injury (4%), 5 million cases of cirrhosis (38%) and 10 million cases of cancer related to alcohol (4%) and millions of cases of other diseases over the next 30 years in 52 countries.
Alcohol-related diseases and injuries cause life expectancy to be cut short by almost 1 year than it otherwise would be over the next 30 years, on average in OECD and EU countries (Figure 1). For comparison, over the last 30 years, life expectancy in OECD countries has increased by about 6.7 years (World Bank, 2020[19]). Alcohol consumption is only one determinant of population health, but drinking less than 1/1.5 drinks per day would contribute about 13% of the total life expectancy gain recorded over a similar period of time in the past. The largest reductions in life expectancy are predicted in Central and Eastern European countries.
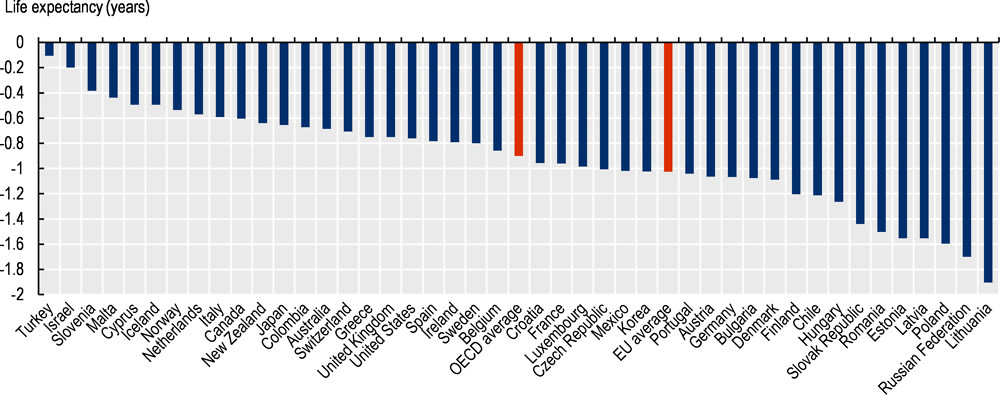
Note: These results are obtained from the comparison of a scenario where alcohol consumption is capped at 1/1.5 drinks per day and binge drinking is non-existent, against a business-as-usual scenario in which volume and patterns of alcohol consumption remain the same as today, over 2020‑50.
Source: OECD (2021[9]), Preventing Harmful Alcohol Use, https://doi.org/10.1787/6e4b4ffb-en.
Higher health spending
Diseases and injuries caused by alcohol drinking beyond 1/1.5 drinks per day imply treatment cost of about 2.4% of total health expenditure on average across OECD countries. In total, this is equal to USD 138 billion (in PPP) per year in 52 countries, or the equivalent of the current health spending in Australia, for instance, or more than twice the current health spending in Belgium. In EU member states, the impact on health spending is estimated at 2.6%. Most of this cost is to treat alcohol dependence, followed by expenditure to treat alcohol-related cancers, cardiovascular diseases, liver diseases and injuries. This estimate varies widely across OECD countries – from 0.1% in Turkey to 4.2% in Lithuania – which reflects both the level of alcohol consumption, the associated level of the burden of diseases in each country and the cost of providing health care services (Figure 2). In absolute terms, the largest spending is predicted to happen in countries where the cost of medical treatment is the highest, such as the United States, Luxembourg and Germany.
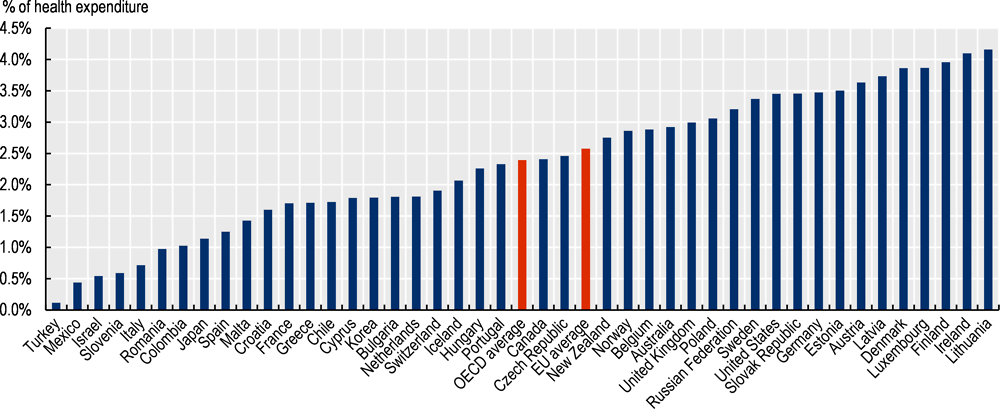
Note: These results are obtained from the comparison of a scenario where alcohol consumption is capped at 1/1.5 drinks per day and binge drinking non-existent, against a business-as-usual scenario in which volume and patterns of alcohol consumption remain the same as today, over 2020‑50.
Source: OECD (2021[9]), Preventing Harmful Alcohol Use, https://doi.org/10.1787/6e4b4ffb-en.
Lower educational outcomes
One‑in-five adolescents, on average, experienced drunkenness at least twice in their life in 2017‑18, in 26 OECD countries (Inchley et al., 2020[20]). Adolescents who reported frequent drunkenness are twice as likely as those who had always abstained from alcohol to display antisocial behaviours with their classmates, although a causal link cannot be asserted. They also show lower life satisfaction and report poorer performance at school.
Harmful drinking in adolescence reduces educational attainment. The analysis of longitudinal datasets from New Zealand, the Russian Federation, the United Kingdom and the United States suggests that, in the long term, students with harmful patterns of alcohol consumption have lower educational performance and lower educational attainment, particularly in the case of girls (OECD, 2021[9]). In the longer term, lower education outcomes affect the formation of human capital, economic growth, social welfare, and worsen inequalities.
Reduced employment and work productivity
Individuals with chronic diseases are more likely to be unemployed or miss days of work. When they are at work, they are also less productive than individuals in good health – a phenomenon also known as presenteeism. Findings from the OECD Preventing Harmful Alcohol Use report suggest that employment would be 0.33% lower each year over the period 2020‑50 due to diseases and injuries caused by drinking more than 1/1.5 drinks per day, in the working-age population (ages 18‑65) across all OECD countries. There are significant regional variations in this effect; the labour markets in Central and Eastern Europe suffer the most, with up to 0.67% employment reduction in Latvia. In addition, 0.11% of labour force productivity is lost annually because of sickness-related absences, while 0.24% is lost due to reduced productivity at work in the form of presenteeism, on average across OECD countries.
Detrimental economic impact
Combining all the effects on life expectancy, health spending, and labour market participation and productivity, GDP could be 1.6% lower than it would be otherwise over the next 30 years due to diseases and injuries caused by drinking more than 1/1.5 drinks per day, on average in OECD countries. Lithuania would be the hardest hit, with GDP expected to be lower by nearly 4%. The GDP impact in 24 EU countries is similar, at 1.9%. The loss across all the 48 countries included in the analysis totals USD 1.6 trillion (in PPP) per year in the period 2020‑50, which is similar to the average annual GDP of Canada or Spain (OECD, 2021[9]).
To cover the increased fiscal pressure caused by alcohol-related diseases, individuals effectively pay a tax of USD 232 (in PPP) per capita per year in OECD countries. This amount varies across OECD countries, from less than USD 40 (in PPP) in Turkey, the Netherland, Mexico and Italy, to more than USD 400 (in PPP) per capita in Finland, Sweden, Austria, the United States and Ireland.
Preventing alcohol-related diseases and injuries has a triple dividend
First, alcohol use weakens the immune system and, during the pandemic, preventing harmful alcohol use helps individuals cope with infections (WHO Europe, 2020[21]). In addition, there is some evidence that drinking alcohol, especially regular heavy drinking, could hinder the development of immunity in response to vaccination (Zimmermann and Curtis, 2019[22]).
Second, preventing harmful alcohol use reduces pressure on health care services. Hospitals and health care workers are already under enormous strain to provide care to patients with COVID‑19. Reducing health system utilisation for preventable alcohol-related conditions helps doctors focus both on patients with COVID‑19 and on patients requiring urgent care for other conditions. For example, South Africa experienced a 65% drop in utilisation of emergency rooms for trauma-related cases linked to alcohol use during the pandemic, following the implementation of an alcohol ban (EyeWitness News, 2021[23]).
Third, a healthier and more productive population will better help restart economic activities and social life in the aftermath of the pandemic. OECD analyses show that a comprehensive PPPP approach – which include actions to protect children from alcohol Promotion; Policing to limit alcohol-related injuries and violence; Primary care to help patients with harmful patterns of alcohol consumption; and Pricing policies to limit the affordability of cheap alcohol – is both effective and cost-effective to tackle harmful alcohol consumption. Namely, investing in such a policy package will:
Save 4.6 million life years annually across the 48 countries included in the analysis; which broadly corresponds to the total life years lost due to lung cancer in the United States each year, or the total life years lost due to cardiovascular diseases in Germany;
Save about USD 28 billion (in PPP) annually in health expenditures across 48 countries, broadly equivalent to 0.5% of total health spending. This is equivalent to the current health spending in Israel or half the current health spending in Sweden; and
Generate savings that are greater than the implementation costs. For every dollar invested in a comprehensive policy package, up to USD 16 are returned in economic benefits.
Investing in protecting children and people with problematic drinking is particularly important during the pandemic
The PPPP policy package includes a comprehensive set of policies which would effectively and efficiently tackle harmful alcohol consumption. While it is worthwhile for countries to upscale investments on the whole package, the COVID‑19 pandemic makes three policies of the package particularly suitable.
Protecting young people from alcohol promotion, particularly through the use of media such as TV, the Internet and social media. During the pandemic, children have increased screen time by 50% including TV and social media, on-demand and online video (Axios, 2021[24]). These children are likely to have increased their exposure to alcohol advertising, which is correlated to the probability of experimenting with drinking for the first time (Jernigan et al., 2017[25]). Yet only a handful of countries have strong legislation to protect children from online alcohol advertising on social media (WHO, 2020[26]).
Strengthening primary care to help patients with harmful patterns of alcohol consumption. It is estimated that less than 10% of patients with harmful patterns of alcohol consumption receive support from health care services in Europe and in the United States (Sugarman and Greenfield, 2021[27]). If, as seems conceivable, the number of individuals with harmful patterns of alcohol consumption and alcohol use disorders will increase in the aftermath of the pandemic, health services need to be ready to meet the challenge.
Tackling cheap alcohol, which is disproportionately consumed by individuals with harmful patterns of alcohol consumption, including among young people, through minimum unit price (MUP) policies. MUP has a double advantage: first, it specifically limits the affordability of cheap alcohol. Second, it may have a positive impact on bars and restaurants that are among the sectors most hit by economic crisis caused by the pandemic, given that the increased income from MUP remains with the industry.
Measures to tackle harmful alcohol consumption will always imply complex trade‑offs
Alcohol production and trade represent a significant part of the economy in a number of OECD countries. While alcohol industry revenues are affected by policy measures, in either profitable or unprofitable ways, countermeasures exist to minimise additional costs for industry. Comprehensive, well-designed policy packages assorted with approaches to mitigate consequences for the alcohol industry can get the expected health gains without major negative impact on the economy. For instance, regulation or price policies trigger adaptation costs such as those to develop a new strategy or new products, but the new products can create new revenues. In addition, the evidence shows that savings from a decreased expenditure on alcohol products, following the implementation of alcohol policies, may be used for other discretionary goods, with restaurants, hotels and recreation and culture among the economic sectors most likely to be recipients of this expenditure. Similarly, evidence from Australia, the United Kingdom and the United States suggest that reductions in employment in the alcohol industry can be partially or fully offset by an increase in employment in other sectors (OECD, 2021[9]).
Measures to tackle harmful alcohol consumption will always imply complex trade‑offs, for instance, regarding their impact on the economy and the labour market, as well as which type of consumer the policy aims to target. For example, interventions targeting all consumers are highly effective and efficient but they affect those who drink at low to moderate levels as well as those who consume alcohol heavily. On the other hand, interventions targeting only people who engage in risky drinking have a significant short-term to medium-term impact on those people, but a lower impact at the population level and tend to have higher implementation costs.
References
[24] Axios (2021), Kids’ screen time sees a big increase during pandemic - Axios, https://www.axios.com/kids-screen-time-pandemic-112650a6-743c-4c15-b84a-7d86103262bb.html (accessed on 8 April 2021).
[5] Bundesministerium der Finanzen (2021), Steuereinnahmen 2020.
[6] Eurocare (2020), Alcohol Consumption in Times of COVID-19, Eurocare, Brussels, https://www.eurocare.org/cares.php?sp=alcohol-and-health&ssp=alcohol-consumption-in-times-of-covid-19 (accessed on 10 November 2020).
[23] EyeWitness News (2021), WC Health Dept: Trauma-related cases on NYE dropped by 65% due to alcohol ban, https://ewn.co.za/2021/01/08/wc-health-dept-trauma-related-cases-on-nye-dropped-by-65-due-to-alcohol-ban (accessed on 8 April 2021).
[10] Gisle, L. et al. (2020), Deuxième Enquête de Santé COVID-19: Résultats préliminaires, Sciensano, Brussels, https://www.sciensano.be/en/biblio/deuxieme-enquete-de-sante-covid-19-resultats-preliminaires (accessed on 10 November 2020).
[3] HM Revenue and Customs (2020), National Statistics: Alcohol Bulletin Commentary (August to October 2020), HM Revenue and Customs, London, https://www.gov.uk/government/publications/alcohol-bulletin/alcohol-bulletin-commentary (accessed on 8 February 2021).
[20] Inchley, J. et al. (eds.) (2020), Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. International report. Volume 2. Key data, WHO Regional Office for Europe, Copenhagen, https://www.euro.who.int/en/health-topics/Life-stages/child-and-adolescent-health/health-behaviour-in-school-aged-children-hbsc/publications/2020/spotlight-on-adolescent-health-and-well-being.-findings-from-the-20172018-health-behaviour-in-school-aged-children-hbsc-survey-in-europe-and-canada.-international-report.-volume-2.-key-data (accessed on 20 July 2020).
[8] IWSR (2020), Beverage alcohol in 2020 performs better than expected - IWSR, https://www.theiwsr.com/beverage-alcohol-in-2020-performs-better-than-expected/ (accessed on 5 March 2021).
[25] Jernigan, D. et al. (2017), Alcohol marketing and youth alcohol consumption: a systematic review of longitudinal studies published since 2008, http://dx.doi.org/10.1111/add.13591.
[18] Mahase, E. (2020), “Covid-19: EU states report 60% rise in emergency calls about domestic violence”, BMJ (Clinical research ed.), Vol. 369, p. m1872, http://dx.doi.org/10.1136/bmj.m1872.
[4] National Institute on Alcohol Abuse and Alcoholism (2020), Alcohol Sales During the COVID-19 Pandemic, Surveillance Report #115, https://pubs.niaaa.nih.gov/publications/surveillance-covid-19/COVSALES.htm (accessed on 15 March 2021).
[7] Nielsen (2020), Rebalancing the “COVID-19 Effect” on Alcohol Sales, Nielsen, Chicago, Il, https://nielseniq.com/global/en/insights/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/ (accessed on 10 November 2020).
[9] OECD (2021), Preventing Harmful Alcohol Use, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/6e4b4ffb-en.
[1] OECD (2020), OECD Employment Outlook 2020: Worker Security and the COVID-19 Crisis, OECD Publishing, Paris, https://dx.doi.org/10.1787/1686c758-en.
[15] OECD/ITF (2020), Road Safety Annual Report 2020, OECD/ITF, Paris.
[13] Pollard, M., J. Tucker and H. Green (2020), “Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US”, JAMA Network Open, Vol. 3/9, p. e2022942, http://dx.doi.org/10.1001/jamanetworkopen.2020.22942.
[12] Sallie, S. et al. (2020), “Assessing international alcohol consumption patterns during isolation from the COVID-19 pandemic using an online survey: Highlighting negative emotionality mechanisms”, BMJ Open, Vol. 10/11, http://dx.doi.org/10.1136/bmjopen-2020-044276.
[11] Santé Publique France (2020), Tabac, Alcool: Quel impact du confinement sur la consommation des Français?, Santé Publique France, Paris, https://www.santepubliquefrance.fr/presse/2020/tabac-alcool-quel-impact-du-confinement-sur-la-consommation-des-francais (accessed on 10 November 2020).
[17] Silverio-Murillo, A., J. Balmori de la Miyar and L. Hoehn-Velasco (2020), “Families under Confinement: COVID-19, Domestic Violence, and Alcohol Consumption”, SSRN Electronic Journal, http://dx.doi.org/10.2139/ssrn.3688384.
[27] Sugarman, D. and S. Greenfield (2021), “Alcohol and COVID-19: How Do We Respond to This Growing Public Health Crisis?”, Journal of General Internal Medicine, Vol. 36/1, pp. 214-215, http://dx.doi.org/10.1007/s11606-020-06321-z.
[14] Tran, T. et al. (2020), “Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia”, Journal of Affective Disorders, Vol. 277, pp. 810-813, http://dx.doi.org/10.1016/j.jad.2020.09.012.
[16] WHO (2021), Violence against women, https://www.who.int/news-room/fact-sheets/detail/violence-against-women (accessed on 7 May 2021).
[26] WHO (2020), Global Information System on Alcohol and Health (GISAH), https://apps.who.int/gho/data/node.gisah.GISAHhome?showonly=GISAH (accessed on 24 June 2020).
[21] WHO Europe (2020), Alcohol and COVID-19: what you need to know, World Health Organization Regional Office for Europe, https://www.euro.who.int/__data/assets/pdf_file/0010/437608/Alcohol-and-COVID-19-what-you-need-to-know.pdf (accessed on 8 April 2021).
[2] Winstock, A. et al. (2020), GDS COVID-19 Special Edition: Key Findings Report | Global Drug Survey, https://www.globaldrugsurvey.com/gds-covid-19-special-edition-key-findings-report/ (accessed on 10 November 2020).
[19] World Bank (2020), DataBank: The World Bank, World Bank Open Data, https://databank.worldbank.org/.
[22] Zimmermann, P. and N. Curtis (2019), Factors that influence the immune response to vaccination, American Society for Microbiology, http://dx.doi.org/10.1128/CMR.00084-18.
Contact
Stefano SCARPETTA (✉ stefano.scarpetta@oecd.org)
Mark PEARSON (✉ mark.pearson@oecd.org)
Francesca COLOMBO (✉ francesca.colombo@oecd.org)
Michele CECCHINI (✉ michele.cecchini@oecd.org)
Marion DEVAUX (✉ marion.devaux@oecd.org)
Note
The Global Drug Survey (GDS) Special Edition on COVID‑19 gathers 55 811 responses from 11 countries. The majority of participants tend to be young, experienced with the use of illicit drug, and employed or in education. GDS data is not representative of the wider population.