As Latvia is facing various health challenges while working with a limited health care budget, a well-functioning public health system is crucial. This chapter will explore the public health picture in Latvia, and describe the public health system tasked with addressing these challenges. It looks at the organisational structure, leadership and governance, partnerships and collaborations, financial resources, knowledge development and workforce.
OECD Reviews of Public Health: Latvia

1. The Public Health System in Latvia
Abstract
1.1. Introduction
Public health issues have gained importance across OECD countries in recent years. Aging populations and rising prevalence of chronic diseases, combined with limited health care budgets, mean that governments are looking for ways to prevent disease and ill-health. Latvia is no exception to this trend. This chapter gives an overview of the public health picture in Latvia and the structure of the health system. It aims to provide a summary of the strengths and weaknesses of Latvia’s public health system, and make recommendations to strengthen this system. The description of public health policies in this chapter is structured according to a framework for analysing public health capacity (Figure 1.1).
Figure 1.1. Appraising Latvia’s public health capacity – analytical framework
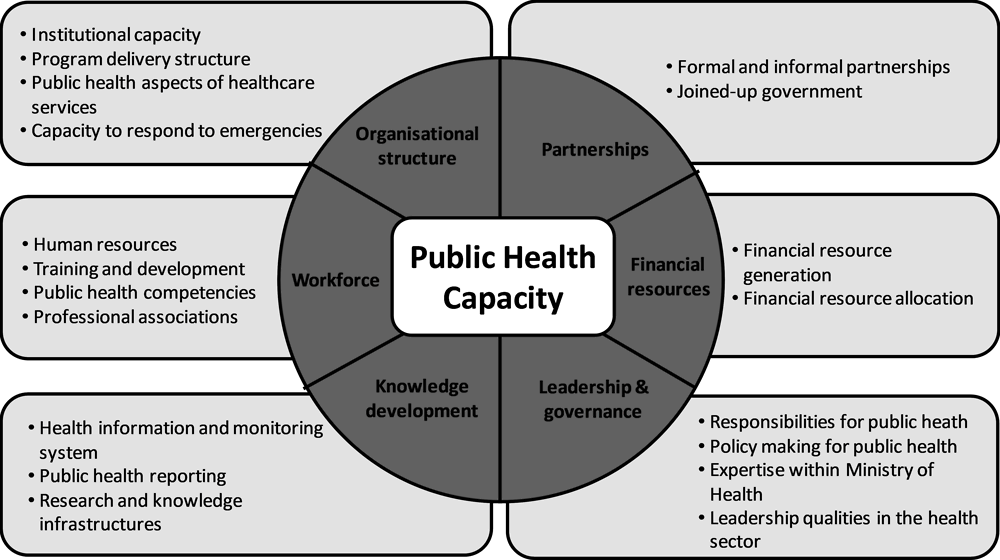
Source: OECD analysis.
1.2. The public health picture in Latvia
1.2.1. Health status of the Latvian population
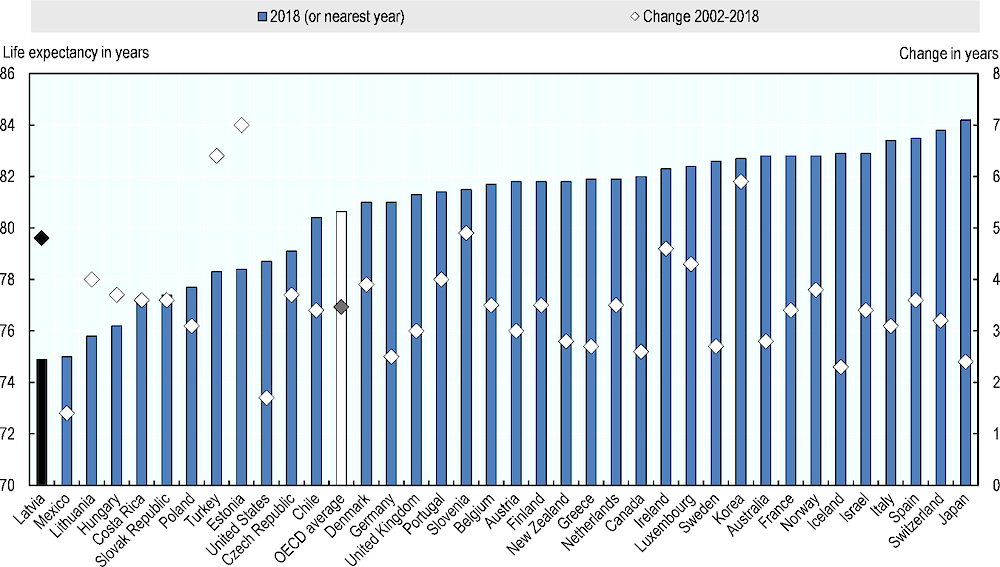
Latvia faces a number of public health challenges – some similar to the other OECD countries, some more pressing. To start with, Latvia has the lowest life expectancy in the OECD, at 74.9 years versus the OECD average of 80.6 years (Figure 1.2). However, Latvia has seen one of the greatest increases in life expectancy over the past 15 years. Between 2002 and 2018, life expectancy in Latvia increased by 4.8 years, while the OECD average increased by 3.5 years.
Figure 1.2. Life expectancy
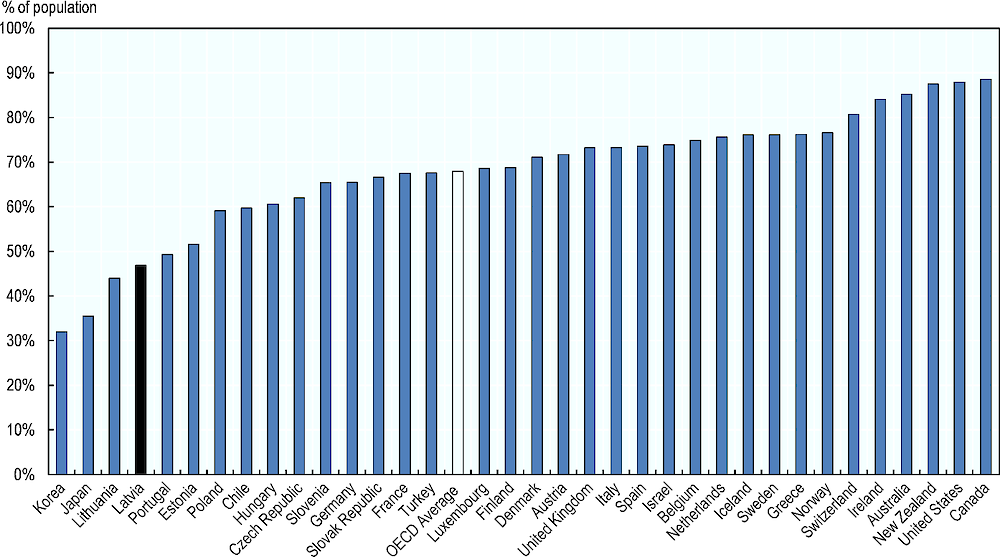
People in Latvia have a lower perceived health status than most other OECD countries. Only 47% of people in Latvia would rate their health status as “good” or “very good”, compared to 68% of people in the OECD on average (Figure 1.3). Women are less likely to rate their health status highly, with 42% reporting “good” or “very good” health, compared to 52% of men (OECD, 2020[1]).
Figure 1.3. Perceived health status
1.2.2. Burden of disease
Like in other OECD countries, non-communicable diseases (NCDs) are the leading cause of mortality in Latvia. Cardiovascular disease is one of the main contributors to the disease burden in Latvia: in 2019, ischaemic heart disease and stroke were the first and second most common cause of both overall deaths and premature deaths (Institute for Health Metrics and Evaluation, 2020[2]). When compared to the OECD average, Latvia sees higher mortality due to diseases of the circulatory system: 58% versus 36% on average (Figure 1.4). Other OECD countries see a relatively larger share of deaths due to cancers. However, in absolute terms, cancer mortality is higher in Latvia: 303 deaths per 100 000 population are due to cancer, compared to 231 per 100 000 in the OECD on average (OECD, 2020[1]).
Figure 1.4. Causes of mortality in Latvia¹
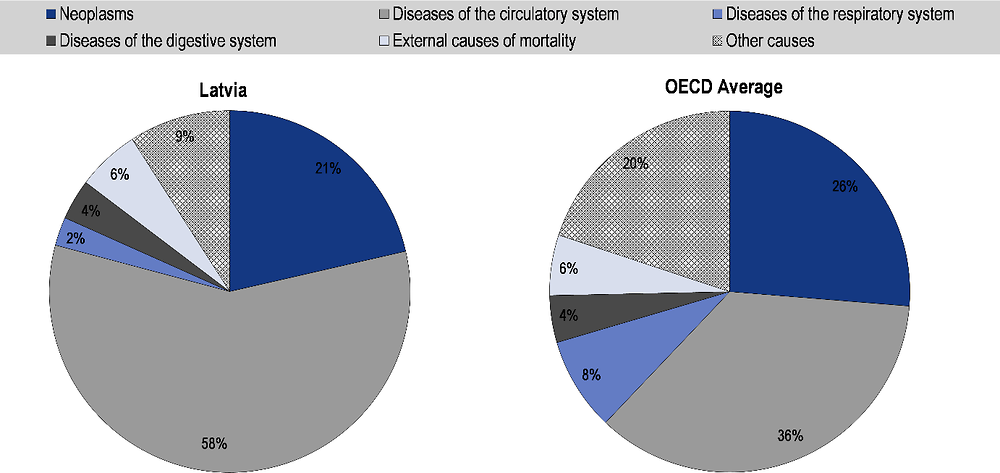
Note: ¹Data for Latvia is 2015.
Source: OECD (2020[1]), OECD Health Statistics 2020, https://doi.org/10.1787/health-data-en.
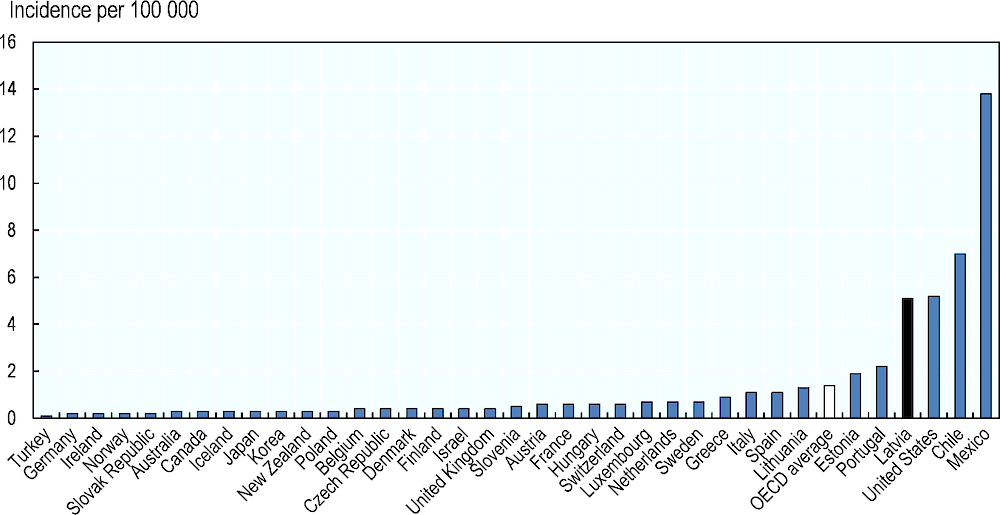
Latvia has a higher than average incidence of acquired immunodeficiency syndrome (AIDS) (Figure 1.5). In 2018, Latvia saw 5.1 cases per 100 000 population, compared to an OECD average of 1.4 per 100 000, based on rates age-standardised to the OECD population. Late diagnosis of human immunodeficiency virus (HIV) infection is an issue in Latvia, as approximately 30% of all new HIV cases are identified at the AIDS stage. In addition, there is a challenge around HIV and tuberculosis (TB) co-infection: according to data from the Latvian CDPC, approximately 10.8% of all TB patients also have HIV, and approximately 10% of all HIV/TB co-infections are multi-drug-resistant forms of TB (Latvia Centre for Disease Control and Prevention, 2017[3]).
HIV/AIDS, as well as other infectious diseases such as hepatitis B and C and TB, are a public health priority for Latvia, and are addressed in the Action Plan for the Prevention of HIV, Sexually Transmitted Infections and Hepatitis B and C for 2018‑20. HIV prevention points (HPPs) provide information and counselling, rapid testing, and supplies (such as syringes, needles, condoms). In 2015, there were 19 HIV prevention points, of which 16 were located in cities and three mobile units that serviced seven other cities (Grāmatiņa, 2015[4]). In 2019, HPPs were visited by 7 010 people, of whom 2 466 were intravenous drug users and 4 544 non-intravenous drug users.
Figure 1.5. Incidence of acquired immunodeficiency syndrome (AIDS)
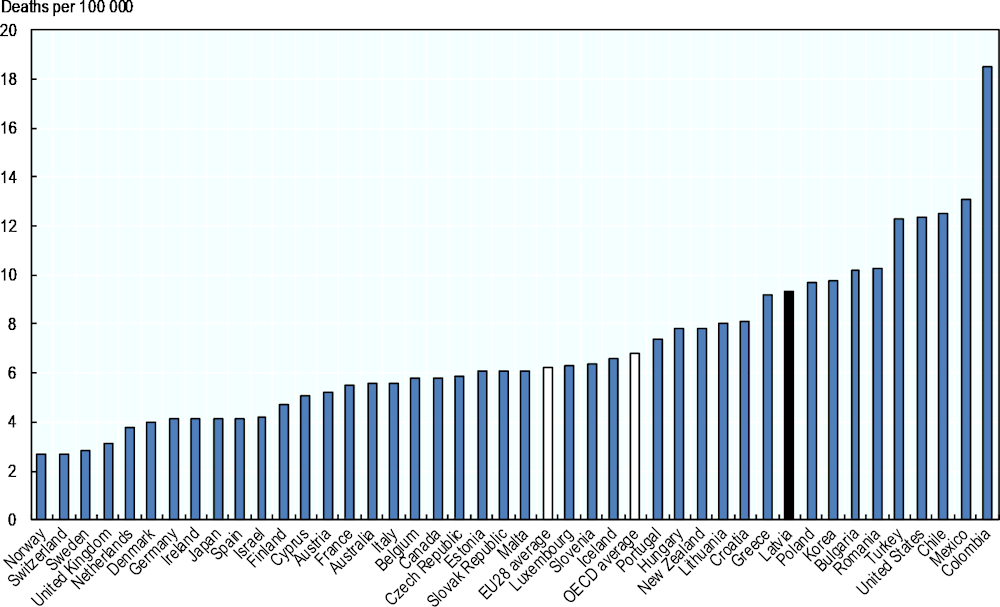
Latvia has one of the highest rates of mortality from suicide: the age-standardised rate in Latvia is 18.1 deaths per 100 000 population, compared to an OECD average of 11.5 per 100 000 (Figure 1.6). However, this rate has decreased considerably over the last two decades, as it was 36.7 per 100 000 in 1997.
The Latvian Mental Health Care Access Improvement Plan 2019‑20 highlighted the importance of addressing mental health (Legislation of the Republic of Latvia, 2019[5]). The Plan identifies a number of key issues to address, including the high rate of suicide, the low rate of consultation for mental health problems in primary care settings, and high rates of bullying in schools. Particular weaknesses identified in the mental health system include under-use of multi-disciplinary teams in inpatient care, weak links between primary and specialist care, insufficient availability of psychotherapy, and shortages in human resources.
The Plan set out by Latvia to address these weaknesses aims to provide the population with evidence-based, up-to-date, high-quality and appropriate access to mental health care through mental health promotion, disease prevention programs and by promoting the early diagnosis of mental illness, early treatment and medical rehabilitation. The most important aspects of the plan are raising public awareness of mental health issues, reducing stigma against mental illness, promoting and improving help options for people with mental health problems, suicide prevention, and promoting cross-sectoral and team cooperation in the field of mental health. Increased education for family doctors and nurses, as well as medical practitioners working in prisons, is also planned. Latvia is also looking to make changes to the regulatory framework to increase the amount of funding for the multi-professional teams.
Figure 1.6. Mortality from intentional self-harm
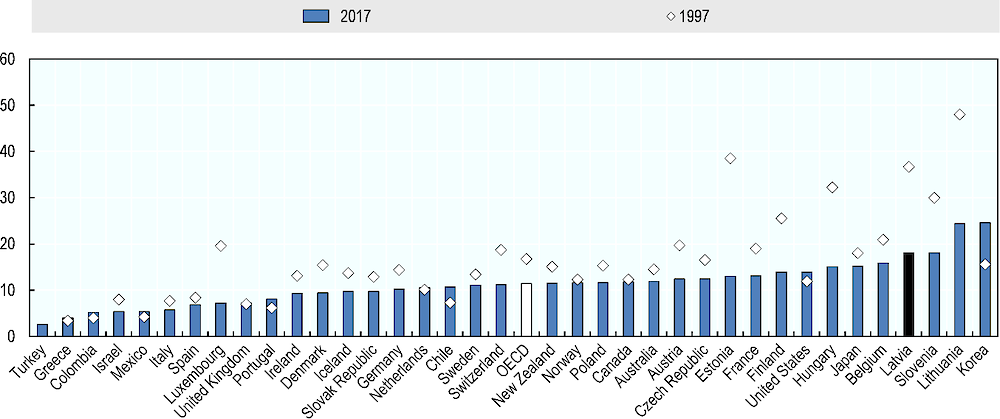
Note: ¹Most recent OECD data for Latvia is from 2015.
Source: OECD (2020[1]), OECD Health Statistics 2020, https://doi.org/10.1787/health-data-en.
In Latvia, mortality from road traffic accidents is also higher than in most OECD and EU countries. The mortality rate in Latvia is 9.3 per 100 000 population per year – which is about 50% higher than the averages for the EU28 (6.2 per 100 000) (Figure 1.7). The rate in Latvia is also higher than in Lithuania (8.0 per 100 000) and Estonia (6.1 per 100 000). To address this issue, Latvia has a road traffic safety programme that spans the years 2014‑20, with recent activities focusing on high risk sites treatment and reduced speed limits at dangerous locations (European Road Safety Observatory, 2017[6]). Latvia’s National Action Plan on the Consumption of Alcoholic Beverages and Limitation of Alcoholism 2020‑22 will explore whether it is possible to reduce the legal blood alcohol concentration for all drivers from 0.5% to 0.2%.
Figure 1.7. Mortality from road traffic accidents
1.2.3. Health risk factors
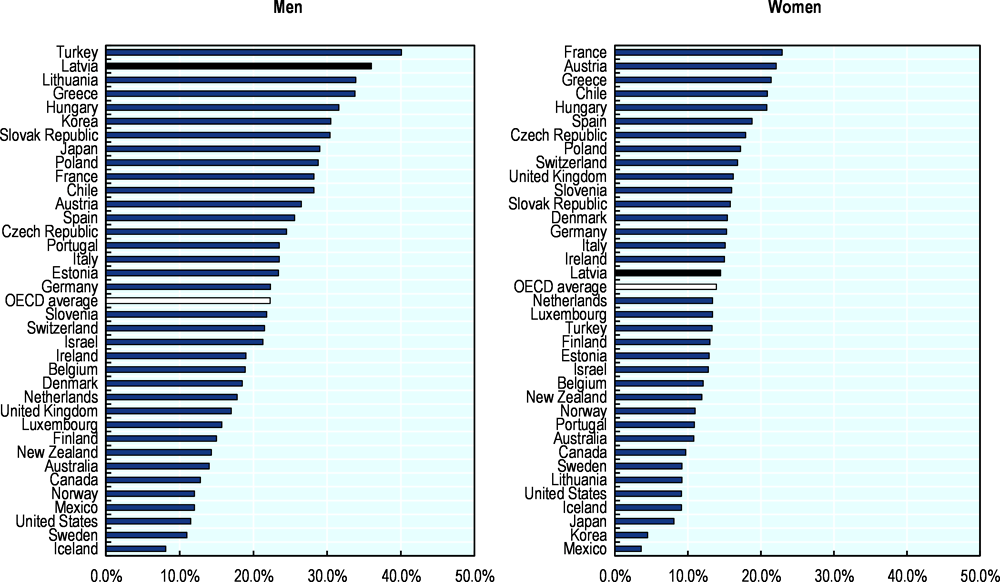
While tobacco consumption among Latvian women is around the OECD average (14.5% in Latvia in 2014, when latest data is available, versus 13.9% in the OECD), tobacco consumption among Latvian men is among the highest in the OECD (Figure 1.8). In Latvia, 36.0% of men over the age of 15 smoke daily, compared to 22.3% on average in the OECD. On the other hand, smoking in men has decreased considerably in recent years (from 46% in 2008), while the smoking prevalence in women has stayed roughly the same albeit with a slight increase, up from 13% in 2008 (OECD, 2020[1]).
To reduce the smoking rate, a range of policies have been implemented. Latvia taxes tobacco products, with the tax accounting for 80% of the retail price (World Health Organization, 2019[8]). This is above the WHO recommended guideline of 75% (World Health Organization, 2014[9]). Since 2008, the affordability of cigarettes (as measured as the share of per capita GDP needed to purchase 100 packs) has not changed (World Health Organization, 2019[8]).
In addition to taxation, Latvia has put in place a wide range of measures: people under the age of 18 are not allowed to purchase tobacco products, all types of tobacco advertising is banned (including sponsorship) as is smoking in most public places, and products need to have a health warning that takes up 50% or more of the package. Smoking is not allowed on the balconies of apartment buildings, nor is smoking in the presence of a child.
In addition, there are public campaigns and educational activities in schools. These policies form a comprehensive package and cover nearly the entire WHO Framework on Tobacco Control, but one element that had been currently missing was a ban on the display of tobacco products at points of sales (WHO FCTC Implementation Database, 2018[10]). This changed on 1 October 2020, as Latvian retailers are now required to put tobacco out of view of consumers.
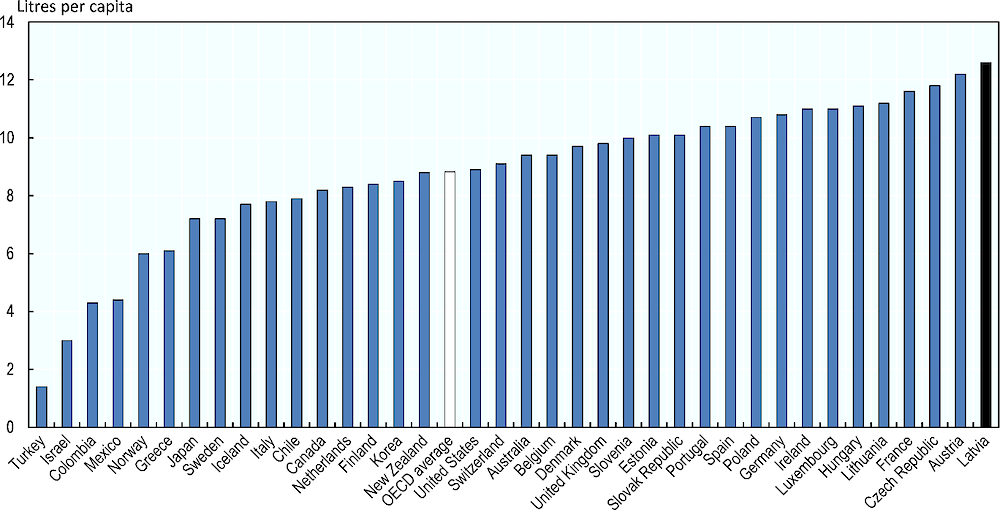
Figure 1.8. Tobacco consumption per capita
Latvia has a relatively high alcohol consumption, at 12.6 litres per capita per year, compared to 8.8 litres in the OECD on average in 2018 (Figure 1.9). This is equal to about two and a half bottles of wine per week, or ten pints of beer. In addition, Latvia has a high prevalence of heavy episodic or “binge” drinking (drinking at least 60 grammes of pure alcohol at a single occasion). In Latvia, 59% of the population reported binge drinking in the 30 days prior, compared to 43% on average in the OECD (World Health Organization, 2019[11]).
Figure 1.9. Alcohol consumption per capita
A comprehensive policy package is needed to address harmful alcohol consumption, and Latvia already has a number of policies in place. These include taxation on alcohol products, a ban on sales to people younger than 18 years, a ban on the off-trade sale of alcoholic beverages between 10pm and 8am, educational campaigns and some advertising restrictions. Advertising restrictions include a requirement that 10% of the product is covered with a warning label. However, there are important limitations to the current regulations. For example, currently beer and wine are exempt from the restrictions on television and radio advertising.
Moreover, while Latvia does have a tax on alcohol, the level of the tax has historically been low – driving alcohol tourism from nearby countries such as Finland and Estonia. The revenue from this cross-border trade means that there is a financial incentive for Latvia to keep taxes on alcohol low. When Estonia decreased the tax on alcoholic drinks by 25% in 2019, Latvia responded by reducing their tax on strong alcoholic drinks by 15% (Reuters, 2019[12]).
The Ministry of Health is in the process of exploring more extensive regulations (Latvian Ministry of Health, 2020[13]). The National Action Plan on the Consumption of Alcoholic Beverages and Limitation of Alcoholism 2020‑22 was adopted by the Cabinet of Ministers on 30 July 2020 and calls for stricter restrictions on the advertising and availability of alcoholic beverages (Box 1.1). It includes a ban on television, radio and internet advertising of special offers (sales and discounts) for all alcohol products, and on trade promotion activities such as two‑for-one sales. However, the plan does not include any changes to the tax on alcohol products, which falls under the responsibility of the Ministry of Finance.
Box 1.1. National Action Plan on the Consumption of Alcoholic Beverages and Limitation of Alcoholism 2020-22
On 30 July 2020 Latvia’s National Action Plan on the Consumption of Alcoholic Beverages and Limitation of Alcoholism 2020‑22 was adopted by the Cabinet of Ministers. Under this plan, a number of policies will be implemented:
Labelling of alcoholic beverages with warnings against drinking while pregnant and when driving, as well as nutrient labels that include the energy content;
Exploring whether it is possible to reduce the legal blood alcohol concentration limit for all drivers 0.2%;
Exploring the possibility of reviewing the sales hours of alcoholic beverages, taking into account the experience of other countries;
Prohibiting the trade promotion activities (like discounts, sales, for buying multiple alcoholic beverages at the same time or purchase of alcoholic beverages together with other products or services with a discount);
Prohibiting TV, radio, and internet advertising of special offers (sales and discounts) for all alcohol products;
Exploring whether it is possible to prohibit the sale of alcoholic beverages with over 22% alcohol-by-volume packaged as a single serving intended for immediate consumption;
The plan also suggests exploring the potential for setting up a public health promotion fund, earmarking 0.5% of excise tax revenue on alcohol, tobacco and gambling and lottery taxes.
Source: Latvian Ministry of Health (2020[13]), Order of the Cabinet of Ministers No. 412 – Action Plan for Reducing Alcohol Consumption and Limiting Alcoholism 2020‑22, https://likumi.lv/ta/id/316448-par-alkoholisko-dzerienu-paterina-mazinasanas-un-alkoholisma-ierobezosanas-ricibas-planu-20202022-gadam
Another major risk factor in Latvia is obesity and overweight: 26% of the Latvian population is obese and 58% is overweight (World Health Organization, 2020[14]). Moreover, over a fifth of children is overweight. This is driven by both diet and physical inactivity. A large proportion of the Latvian population does not get physical activity through recreational activities, sports or fitness: only 40% of the population does some form of sports at least once a week (see figure 2.4 in Chapter 2). On the other side of the energy balance, calorie availability has increased in Latvia in the last two decades. More details on obesity and the policies to tackle it can be found in Chapter 2.
Latvia also has to manage the higher health needs that come with an aged population. In Latvia, 22% of the population is currently aged 65 years or older (Figure 1.10). This is higher than the OECD average of 18%. However, Latvia will see less of an increase in the coming 30 years. As a result, by 2050 in Latvia 28%, and in the OECD on average 25%, will be 65 years old or older.
Figure 1.10. Population ageing – 2019 and 2050
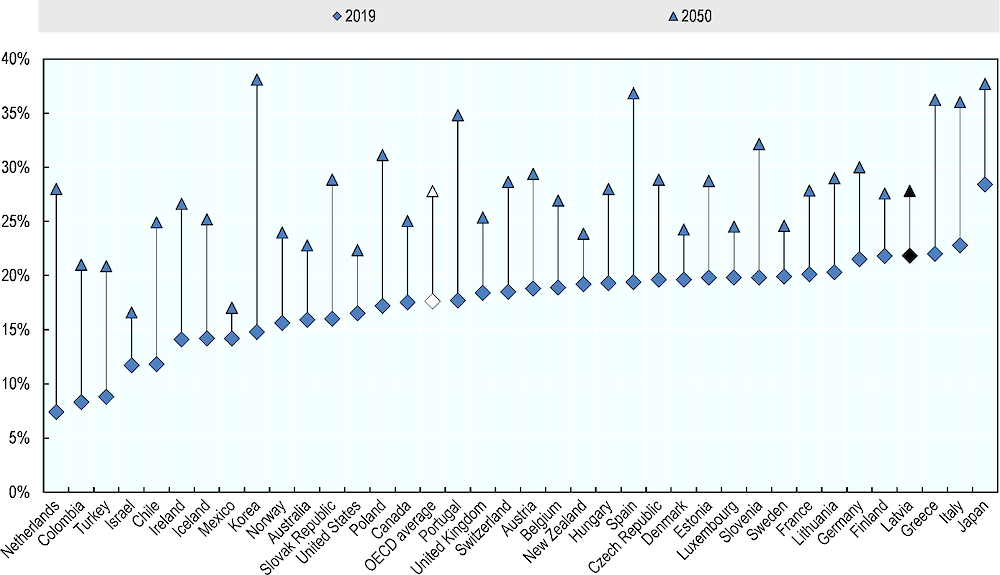
Source: the United Nations (2019[15]), World Population Prospects, https://population.un.org/wpp/Download/Standard/Population/ OECD (2020[1]), OECD Health Statistics 2020, https://doi.org/10.1787/health-data-en.
In terms of natural disasters that could create public health emergencies, Latvia is exposed to both (small) earthquakes and floods, with the latter posing the greatest risk (World Bank, 2016[16]). One such flooding event occurred in 2017, when heavy rain in late summer and autumn led to flash floods (European Parliament, 2018[17]). However, while there was substantial damage to crops and infrastructure, the impact on public health was very limited and there were no casualties.
1.3. Organisational structure
Since regaining independence in 1991, Latvia has undergone a number of health system reforms (OECD, 2016[18]). Currently, Latvia has single-purchaser national health system, funded by general tax revenues, which offers universal health coverage. This coverage provides access to a relatively full range of health care services, delivered by both public and private providers, although out-of-pocket payments are high. This section describes the organisation of the health system in Latvia.
1.3.1. Primary care
A strong, well-established primary care sector is one of the Latvian health system’s key attributes (OECD, 2016[18]). Primary care services commissioned by the National Health Service (NHS) are provided mostly by private general practitioners (GPs) (OECD, 2019[19]). While registration is voluntary, most people are signed up with a GP practice. As in many other OECD countries, GPs act as a gatekeeper to secondary care. They are paid through a range of different mechanisms, including a capitated budget, fixed monthly bonuses (for example for serving rural areas), payments for specific medical procedures (including vaccination and preventive check-ups) and, since 2013, a pay-for-performance scheme (Behmane et al., 2019[20]).
In recent years, Latvia has worked to improve the role of primary care in prevention and public health. The Primary Health Care Development Plan 2014‑16 aimed to position primary health care as the most accessible, effective and comprehensive level of care (OECD, 2016[18]). In addition to increasing the availability of primary care, this plan aimed to increase the role of primary health care in prevention diagnostics and treatment.
As a result, GPs now play an important role in national screening programs. They inform and remind patients to use screening services, offer intestinal screening services, and perform health checks for specific chronic diseases (see Chapter 3 for more information). Patients who have not visited a GP in over a year are supposed to be contacted for a prophylactic visit, during which BMI, vision, blood pressure and vaccination coverage are checked. For this activity, doctors receive EUR 2 (for patients under 65 years of age) or EUR 1 (for patients over 65 years of age).
To encourage more prevention activities in primary care, practices with more than 1 200 patients or 600 patients under the age of 18 patients are given funding for a second practice nurse, whose primary focus is supposed to be prevention (OECD, 2016[18]). In reality though, the time of the additional practice nurse is often spent on activities other than prevention due to the heavy workload that many GP practices experience, though GP practices are left to arrange their own time and workflow arrangement.
1.3.2. Secondary care
Despite the investments in primary care, Latvia’s health system remains hospital centric (OECD, 2019[19]). To remedy this, recent reforms have focused on concentrating specialised care in fewer hospitals and shifting other care to the ambulatory setting. In-hospital care is paid through a combination of fixed budgets (for emergency care and observational wards), case payments, payments for bed-days and diagnosis-related group (DRG) (Behmane et al., 2019[20]).
Most hospitals are publicly owned by the municipalities (OECD, 2016[18]). However, due to an uneven distribution of public health care services, long waiting times and high co-payment rates, the demand for private hospital care has increased in recent years. Between 2000 and 2016, the proportion of private hospital beds increased from 3% to 10% (OECD, 2019[19]).
The role of secondary care in public health and prevention is very limited. In some cases, patients will need to go to a hospital for prevention activities such as an examination of cytological smears from the cervix and posterior vault (Leishman – Nohta combined microscopy of stained preparation), further, depending on screening results women receive a human papillomavirus (HPV) test or biopsy for cervical cancer, and some tertiary prevention and disease management is done by specialists (see Chapter 3 for more information). There are also isolated examples of prevention programmes organised within hospitals, such as the weight loss programme run in the Children’s University Hospital in Riga (see Chapter 2 for more information).
1.3.3. Delivery of essential public health operations in Latvia
Vaccination programmes
The vaccination programme is governed by Cabinet Regulation No.330, introduced on 26 September 2000, and last revised in March 2019 (Likumi.lv, 2000[21]) (Likumi.lv, 2019[22]). These Vaccine Regulations define a list of mandatory vaccinations. For children, these include tuberculosis, diphtheria, tetanus, pertussis, polio, measles, rubella, mumps, Haemophilus influenzae type b infection, hepatitis B, chickenpox, pneumococcal infection, rotavirus infection, and human papillomavirus infection. These vaccines are provided free of cost for the patient. Other vaccines deemed mandatory, such as diphtheria and tetanus for adults, rabies for people who may have contracted this disease, and flu for pregnant women, tick-borne encephalitis (children from one year to 18 years declared place of residence is in a tick-borne encephalitis endemic area) are also covered in full by the state budget.
It is important to note that the term “mandatory” applies to state institutions and vaccination providers, not the public (Walkinshaw, 2011[23]). In other words, it is mandatory for the state to provide these vaccines free of cost, but people can decline vaccination. In this case, doctors are required to obtain a written and signed refusal statement.
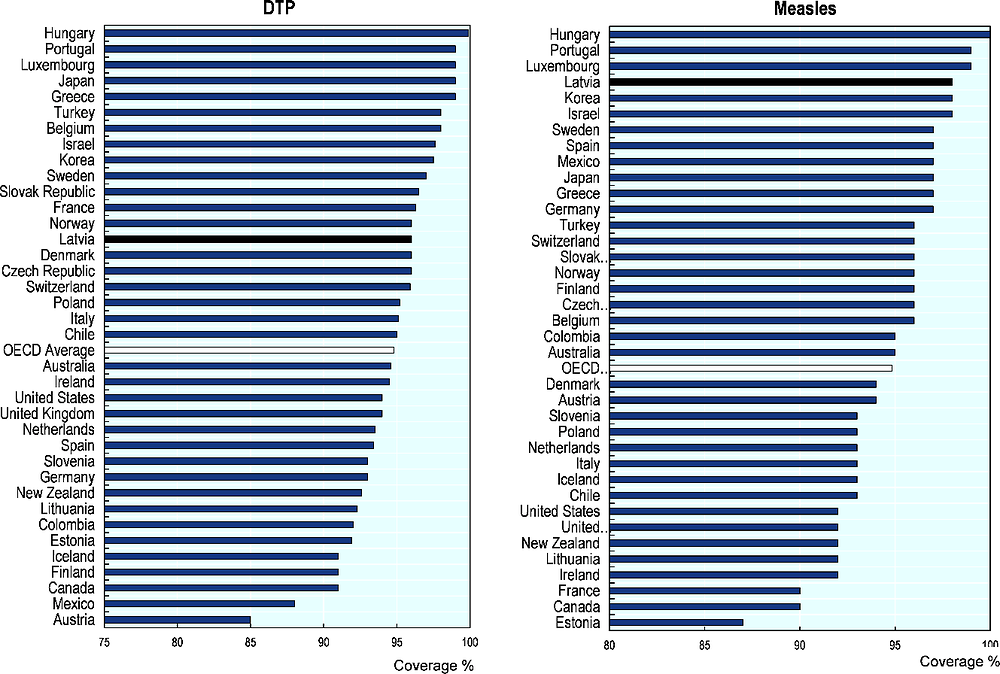
Vaccines are generally provided by the GPs, who also monitor the childhood vaccination schedule for their patients. Coverage in Latvia is high compared to the OECD average: 96% of children receive their diphtheria tetanus toxoid and pertussis (DTP) vaccination, compared to 95% on average in the OECD (Figure 1.11). The coverage of the first dose of measles vaccine is even higher, at 98%, compared to an OECD average of 95%.
Figure 1.11. Childhood immunisation rates
The Centre for Disease Prevention and Control (CDPC) is in charge of planning, coordinating and monitoring the implementation of the state immunisation programme. In 2017, the CDPC launched a programme of educational activities for medical professionals about HPV vaccination. Seminars were organised in five regions of Latvia and in total 360 medical practitioners were trained. This was followed-up in 2018 with a public awareness campaign to explain the need to vaccinate girls against HPV infection, aimed at the parents of girls aged 12 to 18.
Tackling Antimicrobial resistance (AMR)
Systematic surveillance of AMR was introduced in Latvia in 2006. More recently, the Ministry of Health has developed a short-term policy planning document – the Antimicrobial Resistance Limiting and Proper Antibiotic Use Action Plan “One Health” for 2019‑20 – which is the first policy document in Latvia that has defined the problem of AMR (Ministry of Health, 2019[24]) (see Box 1.2). This “one health” approach was developed together with the Ministry of Agriculture.
Box 1.2. Antimicrobial Resistance Limiting and Proper Antibiotic Use Action Plan “One Health” for 2019-20
The Latvian action plan on AMR covers several different areas (Ministry of Health, 2019[24]):
Improving AMR monitoring
Improving the use and tracking of antimicrobials
Improving surveillance, control and prevention of communicable diseases
Limiting the spread of multi-drug-resistant tuberculosis (MDR-TB)
Strengthening inter-institutional cooperation on AMR
Promoting science and research in AMR
Building the capacity of laboratories
Improving specialist education, training and public awareness on AMR in public health
Improving education and public awareness on AMR in animal health
Source: Ministry of Health (2019[24]), On the Antimicrobial Resistance Control and Precautionary Antibiotic Use Plan “One Health” 2019‑20, https://likumi.lv/ta/id/308758-par-antimikrobialas-rezistences-ierobezosanas-un-piesardzigas-antibiotiku-lietosanas-planu-viena-veseliba-2019-2020-gadam
To raise awareness, the CDPC runs public education initiatives about the prudent use of antibiotics each year on European Antibiotic Awareness Day. The CDPC disseminates information for the general public, for health care specialists and other stakeholders about the AMR threat to public health and the importance of prudent antibiotic use.
The largest university hospitals have implemented stewardship programmes to encourage better prescription of antibiotics. The Ministry of Health is now working on the implementation of an EU Structural Reform Support programme in collaboration with the Swedish Public Health Agency, to facilitate the development of stewardship programmes in other hospitals and health care institutions.
Food safety
The Food and Veterinary Service, which falls under the Ministry of Agriculture, is responsible for food safety in Latvia (Behmane et al., 2019[20]). The Food and Veterinary Service carries out control of compliance with safety, quality, and other specific requirements for food products, and they are in charge of food labelling activities, including the Bordeaux and Green Spoon front-of-pack labels (see Chapter 2 for more details). Eleven regional boards provide veterinary surveillance and food control throughout Latvia, while the central office is in charge of strategic planning and providing methodological assistance to regional boards. (Ministry of Agriculture, 2020[25]).
1.4. Leadership and governance
1.4.1. Key actors in the Latvian health system
The Ministry of Health is the leading government authority in the health sector and is responsible for public health, health care and pharmaceutical care. The Ministry of Health plays an important role in the health system, as it develops the national health policy, as well as coordinating and monitoring its implementation. The Ministry of Health also oversees important executive organisations, such as the NHS, the State Agency for Medicines and the CDPC. The Ministry’s budget, as well as that of the NHS, are approved by the parliament (Saeima) (Figure 1.12).
Figure 1.12. The Latvian Health System (simplified)
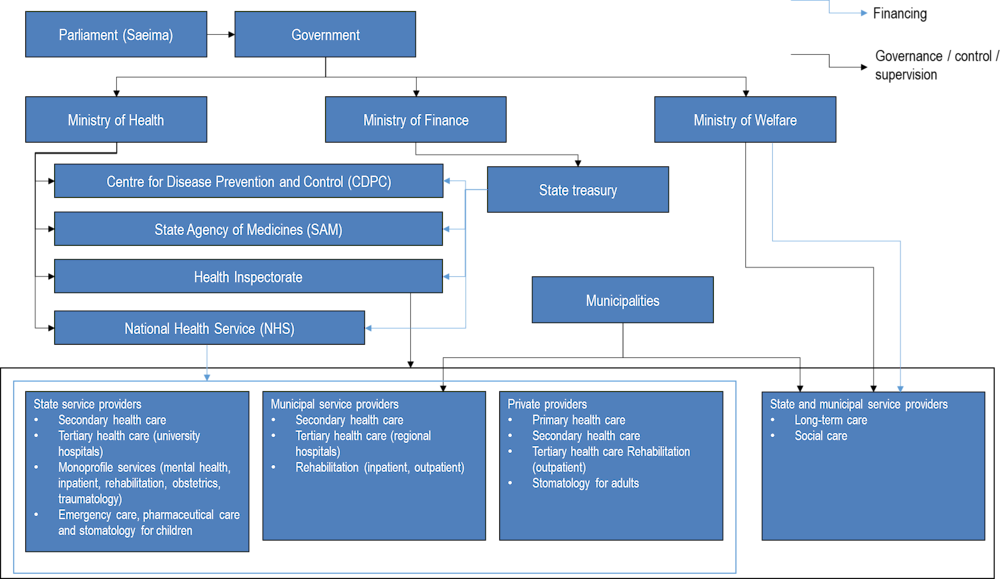
Source: Adapted from Behmane et al. (2019[20]), Latvia: Health system review. Health Systems in Transition, https://apps.who.int/iris/bitstream/handle/10665/331419/HiT-21-4-2019-eng.pdf.
Other ministries are in charge of certain aspects of health (Behmane et al., 2019[20]). The Ministry of Finance, through the State Treasury, is in charge of the financial flows from the state budget to the health care system. The Ministry of Welfare oversees social rehabilitation and home help (for instance hygiene support, help with household tasks, in the home or in institutional settings), disabled and impaired individuals. The Ministry of Agriculture oversees food safety, and the Ministry of Education and Science manages several educational facilities in the health sector. The Ministry of Defence, Interior and Justice finances health services for specific population groups (e.g. armed forces, inmates).
The National Health Service (NHS) is an administrative institution subordinate to the Ministry of Health. The aim of the NHS is to allocate the state budgetary funds for health care and to contract care from providers (Behmane et al., 2019[20]). The NHS agrees contracts with providers, determining the range of services, number of patients and funding. It is also tasked with implementing the state policy for the planning of health care services and ensuring rational and effective use of the state budget for health. The NHS has five territorial branches that contract health care providers for their populations.
The Centre for Disease Prevention and Control (CDPC), also an administrative institution subordinate to the Ministry of Health, implements public health policy in the areas of epidemiological safety and disease prevention, health care quality, and health promotion. In addition to disease monitoring, it also implements various policies of the Ministry. For example, the CDPC is main coordinator and budget holder of HIV prevention points (HPP) network; it produces and disseminates health information campaigns; and it works with municipalities to support them in their health promotion and disease prevention activities (see Chapter 2 for more information).
Local municipal governments are responsible for ensuring accessibility of health care services and health promotion, and depending on budget and local priorities, they maintain hospitals and long-term social care facilities. They also are also charged with local health promotion activities, including promoting healthy lifestyles, controlling alcoholism, and protecting vulnerable groups. While the municipalities are in charge of health promotion, they receive support and oversight from the Ministry and the CDPC to accomplish this task (Box 1.3).
Box 1.3. Balancing local and central government
After Latvia regained independence, a push was made towards a decentralised system that relied more on the municipalities for managing and implementing health policy (OECD, 2016[18]). However, partially due to the small size of the municipalities and the country in general, the system shifted back to a more centralised model.
Local Governments do still participate in health policy and governance. The Union of Local Governments of Latvia has a separate Health and Social Affairs Committee, which actively operates and solves various issues related to the health sector and often participates in the Ministry’s discussions. Section 15 of Part 2 of the Local Government Law stipulates that the Local Administration is to ensure the availability of health care, as well as to promote a healthy lifestyle and sports for the population.
Currently there are 119 municipalities, with populations ranging from just over 1 000‑36 000 people (Centrālā statistikas pārvalde, 2011[26]). The expertise and capabilities of these municipalities are equally variable, resulting in inequalities in access to health services and health promotion (Behmane et al., 2019[20]). To address this, the system is being reorganised, and a reduction to 43 larger municipalities is expected in 2021.
The State Agency for Medicines is in charge of registering medical drugs, devices and treatment methods. While until recently health technology assessment (HTA) was under the remit of the NHS, it has recently moved to the State Agency for Medicines (see Chapter 4 for more information).
The Health Inspectorate performs audits of health care providers to ensure compliance with the conditions of service provision determined in NHS contracts, as well as adherence to the mandatory requirements of health care institutions (Behmane et al., 2019[20]).
The State Emergency Medical Service implements a unified national policy for emergency and disaster medicine, organises and provides pre-hospital emergency medical care, stores state medical stockpiles and organises trainings in first aid.
Voluntary private health insurance accounts for a minor share of financing of health care in Latvia, and the role of private insurers therefore is limited (Behmane et al., 2019[20]).
1.4.2. Management of public health emergencies and the COVID‑19 crisis
In a case of a public health emergency, the State Disaster Medicine Plan (SDMP) and the Hospital Disaster Medicine Plans are activated to manage and coordinate the disaster response. Both were developed according regulation of Cabinet of Ministers No. 948 “Roles of organisation of Disaster medical system”. The SDMP describes coordination mechanism for emergencies caused by biological, chemical, radioactive agents, climatic impact on health, mass casualties and pandemic preparedness. Based on the type of threat each SDMP annex consists of the list of points of contact relevant to exchange and receive information (including health and non-health sectors, for example, police, fire and rescue service, environmental health services). Each annex also describes key functions and tasks attributed to all involved actors. At the level of Ministry of Health emergency situations are coordinated and leading decisions are accepted by State Operational Medical comity (SOMC).
The CDPC is responsible for the monitoring and prevention of communicable and noncommunicable diseases. Its nine regional offices, in Rīga, Daugavpils, Rēzekne, Valmiera, Gulbene, Jelgava, Jēkabpils, Liepāja and Ventspils, are responsible for epidemiological surveillance and monitoring, outbreak investigation of infectious diseases, and emergency management of epidemics (Behmane et al., 2019[20]).
Like all other OECD countries, in the Spring of 2020 Latvia was confronted with the outbreak of the new coronavirus COVID‑19 which demanded a whole-of-government response. At the time of writing in early September 2020, Latvia recorded a peak of COVID‑19 cases in March 2020 with a daily high of 71 cases (Our World in Data, 2020[27]). Since June daily recorded cases have fluctuated around 0‑19 per day. As of the week of 8 September 2020 new daily confirmed cases were at 2.5 per million population, well below the European Union average of 51.95. As of early September 2020 Latvia had recorded 35 deaths from COVID‑19, a rate of 18.56 per million population, significantly below both the European Union average of 317.42 per million population and below neighbouring Estonia (48.25 per million population) and Lithuania (31.59 per million population) (Our World in Data, 2020[27]).
Latvia recorded its first case of COVID‑19 in March 2020, and begun introducing a series of containment measures from mid-March. Containment measures included limits on public gatherings, closure of schools, limits to international travel, and a requirement that Latvians practice social distancing both inside and outside (OECD, 2020[28]). After initial boarder closures, from May free movement was allowed between Latvia, Lithuania and Estonia as part of a so-called “Baltic Bubble”. At the beginning of September 2020, as average daily cases in Estonia (16.91 per million population) and Lithuania (10.18 per million population) were rising Latvia was considering tightening travel restrictions on these countries (BBC News, 2020[29]; Our World in Data, 2020[27]).
Like other OECD countries, at the beginning of the crisis Latvia also took steps to prepare for the health system impact of the COVID‑19 outbreak. In Latvia this included using medical equipment from the private sector, stockpiling and procuring additional protective equipment and pharmaceuticals (OECD, 2020[28]). Special new structures include mobile testing points of the Emergency medical service and drive-throughs (public and private) were set up, and the capacity of COVID‑19 laboratory testing capacity was increased. To increase health care capacity overtime working hours are allowed in excess of the maximum overtime hours prescribed by the Labor Law, but not exceeding 60 hours per week for medical practitioners working in the Emergency medical service, in-patient institutions, as well as for epidemiologists working in the CDPC. the government also increased a financial bonus for health workers, amounting to an additional 20‑50% of the monthly salary for March, April and May (OECD, 2020[28]).
The primary research phase of this review was undertaken in late 2019, prior to the start of the major COVID‑19 outbreak in Europe. The review was finalised in late 2020, as the COVID‑19 crisis continued to evolve.
1.5. Partnerships and collaboration
1.5.1. Ministries that have a role in public health policy
Along with the Ministry of Health, which leads public health governance and policy setting in Latvia, numerous other Ministries contribute to the delivery of health promotion and disease prevention efforts in different ways. The Ministries of Welfare, of Agriculture, and of Environmental Protection and Regional Development in particular play a role in public health activities.
The Ministry of Welfare is the leading institution of the state administration in the areas of labour, social security, children’s and family rights as well as equal rights for people with disability and gender equality. The Ministry of Welfare has responsibility for vulnerable populations, nursing care and social care services – although these are usually organised by local authorities – and promoting healthy work places. In addition, the Ministry of Welfare is implementing a ‘healthy aging’ project with the support of the European Union, which aims to extend and improve the working life of the population, and identify evidence-based strategies to promote active ageing.
Latvia’s Ministry of Agriculture is the main governmental institution responsible for the sector of agriculture, food, forestry and fisheries. The Ministry’s main responsibilities are to assure sustainable systems in these areas, including assuring food safety and animal welfare. In addition, the Ministry of Agriculture, in collaboration with the Ministry of Health, works on the topic of antimicrobial resistance in order to improve the quality and analysis of data on antimicrobial resistance and antibiotic use, to improve the prevention and monitoring of communicable diseases in both public and animal health, and to raise awareness among professionals and the general public of responsible and prudent use of antibiotics in humans and animals.
The Ministry of Agriculture, in collaboration with the Ministry of Health, is responsible for the food nutrition labelling and food safety. The Ministry of Education and Science is the main governmental institution responsible for education, sports, youth, state language policies. It is also involved in the anti-doping policy implementation in cooperation with the Ministry of Health and the National Anti-Doping Agency. The Ministry of Education and Science in collaboration with the Ministry of Health and other organisations have established the draft of The Sports Policy Guidelines 2021–2027. This draft aims to promote physical activity for all, including youth, paralympic and elite sports, including the preparation of athletes within the competitive programmes; improve disabled people`s access to sports; and promote the development of the sports infrastructure. The policy of the Ministry of Education and Science of Latvia has developed the Education Development Guidelines 2020–2030, which addresses the integration of physical activity in education. This includes general (primary and secondary) education, along with higher education, and focuses on ethnic minorities, low socio-economic groups, and children and youth. Health education in Latvia has been integrated in the general education programmes for all education levels (preschool, primary and secondary, as well as vocational) and the Ministry of Health was involved in the development of the content of subjects like biology, chemistry, natural science, social sciences, sports, where health themes are included.
More broadly, there is ongoing collaboration across Ministries for issues related to health. This includes co-operation of the Ministry of Health with the Ministry of Welfare around agreements for prescribing and paying for sick-leave certificates, or collaboration with the Ministry of Education and Science on, for instance, issues such as exempting students from state tests because of health; first aid and health care in educational institutions; requirements for children’s camps; integration of children with disabilities in educational institutions, and so on.
1.5.2. Public involvement in policy making for public health
Latvia takes some steps to involve the public in health care planning, both through general public consultation or through engagement with Non-Governmental Organisations, some of which are required by law. The 2013 ‘Procedures for the Public Participation in the Development Planning Process’ requires that certain procedures for public participation in the development planning process of the government and state institutions are followed (Republic of Latvia, 2013[30]). Opportunities for public participation includes participation in the planning of legal acts, opportunities to review planning documents, participation in inter-institutional working groups and advisory councils, and involvement in public discussions and consultations.
The Ministry of Health has established long-term cooperation with various Non-Governmental Organisations (NGOs), involving them in the development and implementation of health care policy. NGOs are also involved in several commissions and councils established in public administration. Inter-sectoral policies affecting the health sector are dealt with in ad-hoc inter-ministerial working groups where NGOs are also involved. Interdisciplinary commissions within the Ministry of Health in which NGOs are engaged include the Anti-microbial Resistance Limitation Commission, the National Anti-Smoking Committee and the Nutrition Council and others (see Chapter 2). Advisory groups on specific topics bring in expertise from a range of Ministries, as well as stakeholders from outside of government. A Human Biomonitoring Council established in 2016, for example, brings together expertise from the Ministry of Health and related public health institutions, from the Ministries of Environmental Protection and Regional Development, of Agriculture, of Education and Science, of Welfare, as well as input from Riga Stradiņš University, the Latvian Medical Association and the Environmental Consultative Council.
There is also active engagement with a range of professional associations, for example the Latvian Public Health Association, Latvian Physicians’ Association, the Health Care Employers’ Association, the Latvian Family Physicians’ Association, the Latvian Midwives’ Association, the Latvian Nurses’ Association, and the Latvian Pharmacists’ Association. Some professional groups have been assigned regulatory tasks, for example around licensing and education.
There is also engagement between the Latvian Ministry of Health and a number of patient groups. For example, with the Latvian Haemophilia Society, Latvian Cystic Fibrosis Society, or the Oncological Patient Support Association ‘Tree of Life’. Some patient associations receive EU funding to support their activities, and some associations receive funding from pharmaceutical companies.
Overall the relationship between the Ministry of Health and patient representatives seemed to be a positive one. It appeared that patient groups were regularly consulted with, even if their demands are not always met, and there are frustrations with the capacity of the current Latvian health system.
1.5.3. Engagement with representatives of industry
Engagement between the Ministry of Health and representatives of industry, notably food, appears to be positive in Latvia. Voluntary marketing regulations on soft drinks were introduced in 2011, notably a voluntary commitment from industry to limit advertising of soft drinks to children. The Nutrition Council, set up by the Ministry of Health, convenes several times a year and includes the participation of the Latvian Food Business Federation, Latvian Hotel and Restaurant Association (for more information see also Chapter 2). The Latvian Confederation of Employers – the largest employers organisation of Latvia, representing 42% of all employees in Latvia – and the Foreign Investors Council in Latvia – a non-governmental organisation that brings together the largest companies from various countries and sectors that have made significant investments in Latvia – also engage with the government in policy discussions.
As Chapter 2 sets out, there is scope for stronger engagement of industry with promoting healthier lifestyles for Latvians, following some of the practices that can be found in other OECD countries. For example, as detailed in the Chapter 2, both in Spain and the United Kingdom the food and beverage industry has been pushed to take the lead in voluntary reformulation of certain foods, followed by evaluations to assess whether a voluntary approach is delivering effective changes. Latvia is working on this, as the Ministry of Health of Latvia is planning to sign a Memorandum of Cooperation with industry aiming to improve the composition of food products by implementing reformulation.
1.6. Financial resources
1.6.1. The case for investing in health promotion and disease prevention
When invested in the right way, spending on public health and prevention activities can be highly cost-effective, reducing health care expenditure, reducing years of life lost, and increasing participation in the labour market. A 2014 analysis of investment in public health services and capacity at the European level found that spending on prevention can be cost-effective and provide good value-for-money in both the short and longer term (World Health Organization, 2014[31]). National analyses, for example from England, have found that many public health interventions are either cost-saving or cost-effective (Owen et al., 2012[32]; Owen and Fischer, 2019[33]). The OECD’s economics of public health analysis has identified interventions across a range of public health areas, and in particular with regards to reducing non-communicable diseases, which are represent excellent investments in population health.
The effectiveness of spending on public health depends on the policies and interventions where investments are made. Many of the interventions that represent the best value-for-money are population-level investments that target broad health improvements, for example reducing obesity or harmful alcohol consumption. The WHO ‘best buy’ interventions also includes several ‘prevention’ interventions that are highly cost effective, including tobacco and alcohol legislation, reducing salt, and increasing physical activity (World Health Organization, 2014[31]; World Health Organization, 2011[34]). A significant number of interventions – including vaccinations, mental health promotion, violence prevention, and road traffic injury prevention – are investments that can give returns on investment within 1‑2 years (World Health Organization, 2014[31]). Other public health interventions – including those discussed in the other chapters of this Review – are also be cost-effective when well-implemented, for example cancer screening or chronic disease management programmes as discussed in Chapter 3.
OECD analysis has identified cost-effective public health policies and policy packages, in particular in terms of reducing the burden of obesity and reducing harmful alcohol consumption (OECD, 2019[35]; OECD, 2015[36]). For example, across OECD countries, each USD 1 invested in reducing overweight and obesity, up to USD 5.6 will be returned in economic benefits through reduced health care costs, and increased labour market participation. By helping to tackle overweight and obesity regulation of advertising, and menu labelling, would save USD 5.6 and USD 4.8 respectively in GDP benefits, for each dollar invested (OECD, 2019[35]).
1.6.2. Latvia had one of the lowest levels of health spending in the OECD
Latvia had one of the lowest levels of health spending in the OECD in 2019, both in terms of per capita expenditure – USD 1 924 (adjusted for purchasing power parity, or PPP) in Latvia compared to the OECD average of USD PPP 4 170– and as a percentage of GDP – 6.2% in Latvia, compared to the OECD average of 8.9% (OECD, 2020[1]) (Figure 1.13, Figure 1.14).
Figure 1.13. Health expenditure per capita, 2019 (or nearest year)
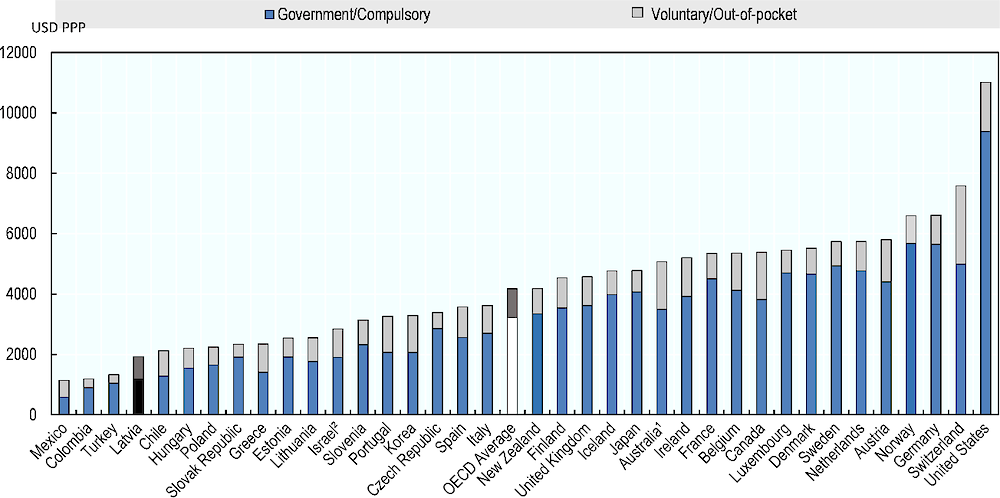
Note: 1. Australian expenditure estimates exclude all expenditure for residential aged care facilities in welfare (social) services.
1. Includes investments.
Source: OECD (2020[1]), OECD Health Statistics 2020, https://doi.org/10.1787/health-data-en, World Health Organization (2020[37]) Global Health Expenditure Database, https://apps.who.int/nha/database.
Figure 1.14. Health expenditure as a share of GDP, 2019 (or nearest year)
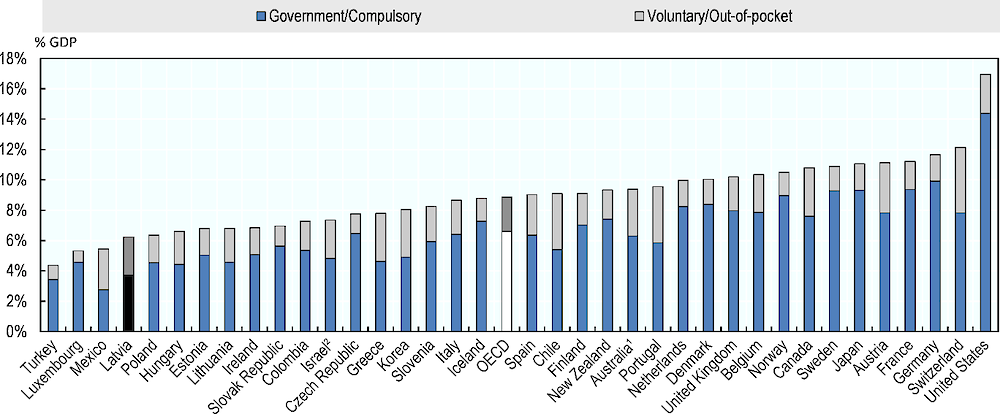
Note: Expenditure excludes investments, unless otherwise stated. 1. Australian expenditure estimates exclude all expenditure for residential aged care facilities in welfare (social) services. 2. Includes investments.
Source: OECD (2020[1]), OECD Health Statistics 2020, https://doi.org/10.1787/health-data-en, World Health Organization (2020[37]) Global Health Expenditure Database, https://apps.who.int/nha/database.
However, in recent years the Latvian Government has been looking to increase health spending. Additional funding of EUR 190.07 million was allocated in 2018 compared to 2017, followed by EUR 142.51 million in 2019 compared to 2018, and additional EUR 78.19 million in 2020 compared to 2019. This additional investment had been initially financed from a mix of budget reallocation, a budget deficit increase allowed by the European Commission, and revenues raised by an increase in social contributions.
1.6.3. High levels of cost-sharing reduces access to health care
Household out-of-pocket payments represented 39.2% of total health spending in Latvia in 2018, compared to the OECD average of 20.1% (OECD, 2019[38]; OECD, 2019[19]). In 2014, 34.7% of Latvians reported having foregone care because of affordability, and in 2013 15.2% of Latvian households experienced catastrophic health spending (households spending 40% or more of total household resources on health care) (OECD, 2019[38]). In 2017 out-of-pocked spending represented 4.2% of Latvian household spending on average, higher than the OECD average of 3.3%, and higher than neighbouring countries such as Lithuania (3.3%), Estonia (3.1%), and Poland (2.6%) (ibid.). Some key public health functions – for example breast and cervical cancer screening, and vaccinations – are available with no out-of-pocket payments. However, if Latvians are foregoing health care for cost reasons it may be making the population less likely to proactively seek health care, consult early in the case of health concerns, or even engage actively in the management of a chronic disease.
Additionally, Latvia has relatively limited mechanisms in place to protect the population from catastrophic health spending and/or protecting poorer populations from foregoing health care due to cost. During the financial crisis period from 2008‑10 Latvia introduced exemptions for cost-sharing for vulnerable and low-income groups, and in 2016 the OECD encouraged Latvia to consider re-introducing some or all of these exemptions (OECD, 2016[39]). Exemptions to co-payments remain extremely limited. For example, co-payment exemptions for financial need are applied only if an individual’s average monthly income during the last three months does not exceed a set threshold, and if the individual does not own monetary accumulations, securities or property. The total annual contribution for inpatient and outpatient treatment is also relatively high (excluding the purchasing of outpatient medicines, spectacles and dental services) (WHO, 2017[40]) (see also Chapter 4).
As of 2020 Latvia introduced changes to co-payment for different health care services and patient categories, primarily to protect elderly persons over age 65 from risk of catastrophic health expenditure, which is a welcome development. Children under age 18 are already exempt from co-payments for general practitioner visits, and all Latvians can attend a GP visit once a year for a general preventive health check-up. Mandatory vaccines are purchased centrally and provided free of charge. Employees whose workplace means that they need additional vaccinations, for example yellow fever or hepatitis B, should have the cost of this vaccine borne by their employer. Additional vaccines for patients with chronic or acute disease are compensated at 50% by State budget resources. Flu vaccines are also covered in full for children aged 6‑23 months, for children up to the age of 18 with health risks, and at 50% for people aged over 65 and adults with certain health risks. During 2020 flu vaccinations were fully covered (100%) for over 65s and adults with certain health risks, as part of efforts to reduce pressure on the health system given the COVID‑19 outbreak.
1.6.4. Spending on health promotion and prevention is low but increasing, but funding sources may not be sustainable
Latvia’s health system is, in general, stretched for resources, and the public health sector is no exception. As a percentage of current expenditure on health, Latvia spends less than the OECD average on prevention; in 2018 Latvia spent 2.2% of the total health budget on prevention, compared to the OECD average of 2.7% (OECD, 2020[1]) (see Figure 1.15). Latvia also spent less on prevention as a percentage of GDP than the OECD average; in 2018 Latvia spent 0.16% of GDP on prevention, compared to the OECD average of 0.25% (OECD, 2020[1]).
Figure 1.15. Spending on prevention as a percentage of current expenditure on health, 2018 (or nearest year)
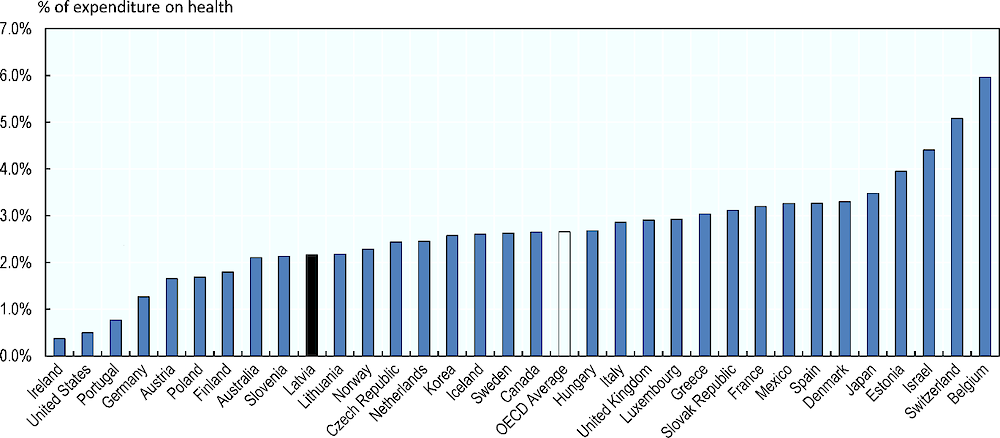
Source: OECD (2020[1]), OECD Health Statistics 2020, https://doi.org/10.1787/health-data-en, World Health Organization (2020[37]) Global Health Expenditure Database, https://apps.who.int/nha/database.
Spending on public health is spread across a range of different functions in Latvia, for example centralised purchasing of vaccines, funding for cancer and newborn screening, and prevention activities in primary care delivered by General Practitioners. In 2018, total government spending on prevention was 44.7 EUR million (excluding municipal spending and EU funds) was split across health condition monitoring programmes (49%), immunisation programmes (21%), early disease detection programmes (15%), epidemiological surveillance and risk and disease control programmes (8%), information, education and counselling programmes (7%) (Central Statistical Bureau of Latvia, 2018[41]). A further EUR 3.4 million was spent on health promotion with multi-sectoral approach (ibid.).
However, when it comes to targeted health promotion and prevention programmes, for example national campaigns, efforts to support weight loss or increased physical activity, smoking cessation programmes, Latvia appears to be highly reliant upon funding from the European Union. For example, Latvia’s Public Health Strategy for 2014‑20 has been primarily funded by EU funds (OECD, 2016[39]), and EU funding which runs until 2023 has been used to pay for municipalities to develop their own local health promotion plans, overseen by the Ministry of Health. There is a risk that too much reliance on EU funding for impedes building a sustainable set of health promotion and prevention programmes, if funding in priority areas cannot be assured over the longer term.
In terms of municipal public health programmes, these local efforts should be tailored to local needs, but focus on areas such as physical activity, nutrition, alcohol, tobacco, mental health, and sexual and reproductive health. The expectation of the central government appears to have been that municipalities would receive start-up capital from these EU funds, but then be expected to cover the ongoing costs of these programmes out of local budgets from 2023. As of 2020 the projected central budget did not include provisions to continue to support municipalities, nor was there a mechanism to ensure that municipalities continued to fund public health programmes out of their own budget.
1.7. Knowledge development
1.7.1. Most public health information is centralised and analysed by the CDPC
The principal institutions responsible for health data collection in Latvia are the CDPC, the NHS, and the Central Statistical Bureau (CSB). The CDPC is responsible for collecting and summarising all health-related statistical data in Latvia, including data collected by the NHS and the CSB. The CDPC is also responsible for complying with international obligations by submitting certain data to WHO and Eurostat.
All statistical reports consist of aggregated data and do not include personal identifiers. The CDPC collects cause of death statistics and the NHS all data related to state-paid health services, service provision and payment information received from all contracted providers (such as for instance hospitals, health centres or GPs). The NHS data system also contains information on all services provided for individual patients, including patient personal data, diagnoses, procedure codes (according to a national coding system), and a provider identifier. The CSB collects statistical information on some key health indicators, for example, the use of emergency medical services or population morbidity. The CSB is in charge of communications with the OECD and also Eurostat for some indicators (Behmane et al., 2019[20]).
1.7.2. Latvia is developing its eHealth system but further progress is needed
The current eHealth system intents to provide a secure system to record and exchange medical and patient information. The use of the central electronic system is voluntary for medical institutions; however, since January 2018 electronic sick leave certificates and prescriptions for outpatient pharmaceuticals reimbursed by the NHS have been mandatory.
In practice, the eHealth system consists of two parts, one for the public and one for authorised health care professionals. The public section, accessible through the eHealth portal, provides information on the health care system, healthy lifestyles, databases, etc. After authentication, patients can view their basic health data, check current prescriptions or sick leave certificates. Health care professionals are able to enter and process patient data and prescribe medications, as well as sick leave certificates, while pharmacists can access prescriptions for the patient and mark their delivery to the pharmacy.
The NHS is responsible for the implementation of the national eHealth strategy and the establishment of the necessary infrastructure and running of the eHealth support service. However, it is up to health care providers to equip themselves with the necessary IT material (Behmane et al., 2019[20]).
Latvia could still stand to increase use of real-world health care data to inform biomedical research and evaluation. A “learning health care system” based on electronic health records and other routinely collected data holds large promises for facilitating medical research and improving effective and efficient use of medicines, is at an early stage in Latvia, although mechanisms for data access for research are in place (OECD, 2021 (forthcoming)[42]). The Centre for Disease Prevention and Control evaluates researchers’ and research institutions’ applications for the use of identifiable patient data recorded in the medical documents in specific research under Cabinet Regulation No. 446 which covers cases where it is not possible to obtain informed consent from the patient. If approved, data for research from different sources is provided/available on a person level with a direct identifier (personal ID, etc.). Requests for a data extraction from the public monitoring system for health care quality and efficiency are approved by a special project council consisting of representatives from the Centre for Disease Prevention and Control, National Health Service, State Emergency Medical Service and Health Inspectorate. In this case, approved applicants’ access pseudonymised data (OECD, 2019[43]).
Latvia has developed a Health System Performance Assessment Framework (including health care quality, patient safety and efficiency indicators). Within this framework, principles and procedures for data provision, data linkage, health data protection, and access for research are set out (OECD, 2019[43]).
1.7.3. Heath information to citizens increased substantially in recent years but health literacy remains low
Public health information available to citizens has increased in Latvia. The Ministry of Health developed a portal called “Your Health”, where citizens may obtain information on their rights and responsibilities, health care organisation, how to apply for health care services, health prevention, healthy lifestyle, special recommendations for specific patient groups etc. The Ministry of Health uses this support to also inform patients about regulatory issues, planned reforms and provides links to other national and international institutions.
Other public institutions share online information regarding their activities and responsibilities: the NHS for instance provides information on the financing of health services, tariffs and access to contracted health care providers; the CDPC information on health promotion, infectious disease control, epidemiological data and other health statistics; and the SAM on responsible medicines utilisation and medicines shortages (among others) (Behmane et al., 2019[20]).
Yet, despite these recent improvements the health literacy of the Latvian population appears to be rather limited; there have been no recent studies of health literacy in Latvia, although in 2020 “Study on the knowledge and skills of the Latvian population in the field of health or health literacy” has been put out for procurement. Digital Transformation Guidelines are currently being developed in Latvia, which also includes health literacy, and health education is promoted through the Public Health Guidelines, while the education sector promotes children’s health education. However, given how important good health literacy is for person-centredness in health systems, for supporting chronic disease management, and for promoting healthy habits in the population, Latvia could still follow other OECD countries in introducing targeted efforts to increase health literacy (see Box 1.4).
Box 1.4. Increasing health literacy
Health literacy supports individuals become partners in the co-production of health. When individuals are educated and empowered on health information, they will be able to make informed decisions about the care that they, or others, receive. It also encourages individuals to take more responsibility for own health. It is thus a key element in the move towards people-centred health systems. Evidence shows it can improve patient experience, support self-care practices and may contribute to improve certain health outcomes.
The proportion of a population seeking health information in the internet is one of the indicators used to measure health literacy. Half of all EU residents sought health information on line in 2017, a figure that has almost doubled since 2008. The highest proportions were in the Netherlands and Finland (about 70%). Latvia reported among the lowest levels, with only 43% of people seeking health information on line in 2017.
Austria, Australia, Germany or New-Zealand have all developed health literacy programmes. In Austria for instance, the national government has structured its health literacy approach into three areas of intervention: (i) improving the organisational health literacy of the health care system, i.e. health literacy becomes a quality dimension of health care organisations and of the health system, (ii) improve personal health literacy with a focus on information, education and training, and (iii) improve health literacy in the consumer and service sector with specific attention to the quality of information that supports decision on product purchasing or service utilisation. For each sub-goal, a number of interventions has been defined and are subject to a monitoring process focusing on progress of interventions. Another area of future action focus digital health literacy which is slowly gaining relevance.
Source: Moreira (2018[44]), Health Literacy for People-Centred Care: Where do OECD countries stand?, http://www.oecd.org/els/health-systems/health-working-papers.htm, OECD (2018[45]), Health at a Glance: Europe 2018, https://ec.europa.eu/health/sites/health/files/state/docs/2018_healthatglance_rep_en.pdf.
1.8. Workforce
1.8.1. Latvia reports fewer health professionals than the OECD average
While the number of practising doctors in Latvia is slightly below the OECD average, at 3.2 doctors per 1 000 population (3.5 in OECD countries), the number of nurses is nearly half the OECD average (4.6 per 1 000 vs. 8.8, see Figure 1.16). While the number of doctors per 1 000 population has been continuously increasing since 2001, the number of nurses has been decreasing since 2010 and the nurse-to-population ratio is currently one of the lowest among OECD countries (1.4 nurses per physician in 2016) (Behmane et al., 2019[20]).
Figure 1.16. Doctors and nurses numbers in OECD countries, 2017 or nearest year
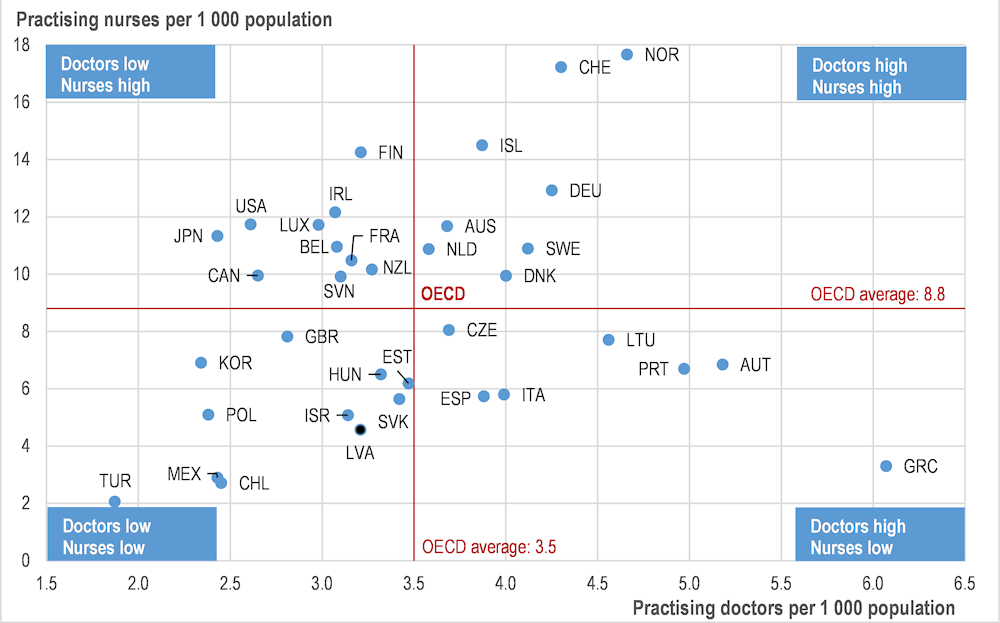
Note: In Portugal and Greece, data refer to all doctors licensed to practice, resulting in a large overestimation of the number of practising doctors (e.g. of around 30% in Portugal). In Austria and Greece, the number of nurses is underestimated as it only includes those working in hospital.
Source: OECD (2020[1]), OECD Health Statistics 2019, https://doi.org/10.1787/health-data-en.
Since 2000, Latvia has witnessed an increase in the overall number of graduates of health-related study and training. In particular, the number of medical graduates increased more than four times between 2000 and 2015 (Behmane et al., 2019[20]). However, many of them choose to work in different professions or move abroad and consequently the health authorities continue to grapple with important health workforce shortages, more particularly in rural areas.
1.8.2. The regional repartition of the health workforce is very imbalanced
There is considerable variation in the distribution of doctors across regions in Latvia. Physician density across the country reveals a clear divide between urban and rural areas that constitutes an important access barrier for many Latvians living outside major urban centres. In 2018, the ratio of practising medical doctors per population was more than three times higher in the Riga area than in rural regions such as Zemgale or Kurzeme. (OECD, 2019[19]). While population density is far higher in Riga and other cities than rural areas of Latvia, securing geographical access to health care can nonetheless be a concern in less populated areas. The age composition of the currently practising GP workforce is a further concern, as the retirement of substantial numbers of GPs is anticipated in the next few years, foreshadowing the development of additional shortages of primary care physicians.
In light of these issues, the Latvian authorities have begun taking steps to increase the supply of physicians in rural areas. For example, since April 2015 medical universities are required to give priority to applicants who have agreed to practise in a rural area on completion of their training. the government has also raised salaries for all groups of health professionals and increased the number of student places in nursing schools. Also, since 2018 an EU-funded project has provided financial incentives to attract medical practitioners to work in regions outside Riga. In 2020, EU funding will also be used to try to attract physicians to public health care services in Riga, in parallel with these measures to attract practitioners to rural areas. As of July 2019, 315 medical practitioners have received such financial support. Beneficiaries include doctors of various specialties, as well as medical assistants, nurses, midwives and physiotherapists (OECD, 2019[19]).
1.8.3. GPs are a strong feature of the Latvian primary health care system
Primary care is provided by a network of GP practices, mostly private entrepreneurs, and few employed by health centres. Registration with a family doctor is voluntary but most Latvians choose to sign up with one practice.
GPs act as health-system gatekeepers, providing referrals for patients to visit most specialists (some specialists such as gynaecologists do not require to be referred to by a GP though). Most GPs work in solo practices, conversely to what has been reported in many OECD countries where there has been a shift towards larger teams in recognition of the economic and communal benefits of working with peers (OECD, 2016[18]). GPs are paid using a mix of capitation, fee for service, fixed practice allowances (capitation) and, since 2013, payments on quality indicators. The family medicine curricula was introduced as a new specialty in 1990 in Latvia (Behmane et al., 2019[20]).
Continuous medical education is offered and organised by universities and medical professional associations, under different formats. Proof of having participated and validated a certain number of continuous medical courses (credits) is required for recertification every 5 years, regardless of the type of health care institution in which doctors work (Behmane et al., 2019[20]).
1.8.4. Training of public health professionals in Latvia is well-established
Since 1997, Riga State University has offered a 4‑year Bachelor programme in public health, training approximately 20 students every year. After their Bachelor’s degree, graduates as well as other health professionals (physicians, nurses, etc.) can engage in a 2‑year Master’s programme in Public Health, after which they may pursue a doctoral degree (Behmane et al., 2019[20]). From 2020 the University of Latvia is offering a Master’s Programme in Epidemiology and Statistics.
In 2014, RSU and Riga International School of Economics and Business Administration (RISEBA) established a joint full-time Professional Master’s degree in Health Management and a professional Business Establishment Executive, which lasts 1.5‑2 years (Behmane et al., 2019[20]).
Other public health professionals include:
Public health physicians: these are physicians who undertook a 4 years residency specialisation in public health (the other medical specialties that include a substantial amount of training in public health are general medicine, infectiology and sport medicine).
Nutritionists, who receive a four‑years dedicated training.
In addition, nurses’ training has been revised in 2019 and the curricula now includes more focus on public health matters (environmental health, prevention, social determinants of health, etc.) and the possibility for them to further specialise. Also, as mentioned previously, to encourage more prevention activities in primary care, practices with more than 1 200 adult patients or 600 patients under the age of 18 on their patient list are given funding for a second practice nurse, whose primary focus is supposed to be more on prevention.
1.9. Conclusion
When it comes to the overall Latvian public health system architecture, Latvia’s Ministry of Health is clearly turning attention to prevention and promotion activities. However, despite noticeable improvements over the last decades, Latvia is facing a considerable public health challenge: life expectancy is low, the burden of non-communicable and infectious diseases is high, and risk factors such as smoking, alcohol consumption and obesity are prevalent.
To address these issues, Latvia has a centralised health system controlled by the Ministry of Health. The role of local governments in public health is limited, but this may change after the municipalities are reorganised, and the local government role in public health has grown in recent years. Most preventive care falls under the remit of primary care, however this sector is under-resourced and overloaded. GP and municipalities are expected to play a key role and both appear over-stretched and over-loaded. Latvia should consider allowing other health system actors to take on some GP tasks – such as pharmacists offering routine health checks – as well as looking to introduce more capacity in the system by giving additional support to GPs, especially tied to incentives to undertake prevention activity. Municipalities, too, could likely be stronger public health actors through more strategic planning, especially in light of the instability of financing for programmes such as municipality-level group fitness classes or healthy eating education, which are currently mainly paid for with EU funding. This could mean using funding that is currently available to pay for training for staff in health promotion, so that the expertise in this area remains within the municipality beyond the horizon of the current programmes. There is also scope for Latvia to strengthen regulation around harmful alcohol consumption, continuing to pursue the tighter regulations on availability and marketing of alcoholic beverages planned for 2020‑22.
There is scope for Latvia to make better use of existing resources, such giving pharmacists a more significant role in public health education and prevention activities, but it remains that Latvia has one of the lowest levels of health spending in the OECD, and high levels of cost-sharing reduces access to health care. While spending on health promotion and prevention is low but increasing, funding sources may not be sustainable. Latvia would be well-placed to maintain the commitment made in recent years to increasing health spending, and focus on investing in public health interventions that represent good value-for-money, including those examples given in this chapter which include a comprehensive policy package to reduce harmful alcohol consumption, strengthening the health information infrastructure, and promoting health literacy.
References
[29] BBC News (2020), Coronavirus: Baltic states open a pandemic ’travel bubble’ - BBC News, https://www.bbc.com/news/world-europe-52673373 (accessed on 8 September 2020).
[20] Behmane, D. et al. (2019), Latvia: Health system review. Health Systems in Transition, https://apps.who.int/iris/bitstream/handle/10665/331419/HiT-21-4-2019-eng.pdf (accessed on 1 April 2020).
[41] Central Statistical Bureau of Latvia (2018), Health care expenditure (based on SHA methodology), https://www.csb.gov.lv/en/statistics/statistics-by-theme/tables/metadata-health-care-expenditure-based-sha-methodology (accessed on 18 November 2020).
[26] Centrālā statistikas pārvalde (2011), Population and Housing Census 2011: Resident population on 1 March 2011 by territorial unit and sex, https://data1.csb.gov.lv/pxweb/en/iedz/iedz__tautassk__demogr__tsk2011/TSG11-01.px/table/tableViewLayout1/?rxid=dcc30576-1e14-481f-a372-9698956b3f68 (accessed on 5 March 2020).
[17] European Parliament (2018), MEPs approve €17.7 million in EU aid after intense floods in Latvia, https://www.europarl.europa.eu/news/en/press-room/20181105IPR18262/meps-approve-EU17-7-million-in-eu-aid-after-intense-floods-in-latvia (accessed on 15 May 2020).
[6] European Road Safety Observatory (2017), Road Safety Country Overview - Latvia.
[4] Grāmatiņa, L. (2015), Hepatitis prevention in the context of HIV prevention point work in Latvia.
[2] Institute for Health Metrics and Evaluation (2020), Latvia Country Profile, http://www.healthdata.org/latvia (accessed on 5 March 2020).
[3] Latvia Centre for Disease Control and Prevention (2017), Registered TB / HIV cases in Latvia, 1998-2017 per year, https://www.spkc.gov.lv/lv/tuberkuloze-1/7_tb_hiv_20171.pdf (accessed on 17 November 2020).
[13] Latvian Ministry of Health (2020), Order of the Cabinet of Ministers No. 412 - Action Plan for Reducing Alcohol Consumption and Limiting Alcoholism 2020-2022, https://likumi.lv/ta/id/316448-par-alkoholisko-dzerienu-paterina-mazinasanas-un-alkoholisma-ierobezosanas-ricibas-planu-20202022-gadam (accessed on 17 November 2020).
[5] Legislation of the Republic of Latvia (2019), Mental health care access improvement plan 2019-2020 [Psihiskās veselības aprūpes pieejamības uzlabošanas plāns 2019.–2020] - Order of the Cabinet of Ministers No. 299, https://likumi.lv/ta/id/307701 (accessed on 3 November 2020).
[22] Likumi.lv (2019), Amendments to the Cabinet Regulations No. 330: Vaccination Regulations, https://likumi.lv/ta/id/305718 (accessed on 5 March 2020).
[21] Likumi.lv (2000), Cabinet Regulation No. 330: Vaccine Regulations, https://likumi.lv/ta/en/en/id/11215 (accessed on 5 March 2020).
[25] Ministry of Agriculture (2020), Food and Veterinary Service - About us, https://www.zm.gov.lv/en/partikas-un-veterinarais-dienests/statiskas-lapas/startpage?nid=2913#jump (accessed on 15 May 2020).
[24] Ministry of Health (2019), On the Antimicrobial Resistance Control and Precautionary Antibiotic Use Plan “One Health” 2019-2020, https://likumi.lv/ta/id/308758-par-antimikrobialas-rezistences-ierobezosanas-un-piesardzigas-antibiotiku-lietosanas-planu-viena-veseliba-2019-2020-gadam (accessed on 5 March 2020).
[44] Moreira, L. (2018), Health Literacy for People-Centred Care: Where do OECD countries stand?, http://www.oecd.org/els/health-systems/health-working-papers.htm (accessed on 29 April 2020).
[28] OECD (2020), OECD COVID-19 Health Systems Response Tracker, https://www.oecd.org/health/COVID19-OECD-Health-System-Response-Tracker.xlsx (accessed on 8 September 2020).
[1] OECD (2020), OECD Health Statistics 2020, http://dx.doi.org/10.1787/health-data-en.
[38] OECD (2019), Health at a Glance 2019: OECD Indicators, OECD Publishing, Paris, https://dx.doi.org/10.1787/4dd50c09-en.
[19] OECD (2019), Latvia: Country Health Profile 2019, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels, https://dx.doi.org/10.1787/b9e65517-en.
[43] OECD (2019), Monitoring the Adoption of the Council Recommendation on Health Data Governance - Results of the 2019 survey and next steps (DELSA/HEA(2019)18).
[35] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/67450d67-en.
[45] OECD (2018), Health at a Glance: Europe 2018, https://ec.europa.eu/health/sites/health/files/state/docs/2018_healthatglance_rep_en.pdf.
[18] OECD (2016), OECD Reviews of Health Systems Latvia, OECD Publishing, Paris.
[39] OECD (2016), OECD Reviews of Health Systems: Latvia 2016, OECD Reviews of Health Systems, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264262782-en.
[36] OECD (2015), Tackling Harmful Alcohol Use: Economics and Public Health Policy, OECD Publishing, http://http//dx.doi.org/10.1787/9789264181069-en.
[42] OECD (2021 (forthcoming)), OECD Review of Digital Transformation for Latvia.
[27] Our World in Data (2020), Coronavirus Pandemic (COVID-19), https://ourworldindata.org/coronavirus (accessed on 8 September 2020).
[33] Owen, L. and A. Fischer (2019), “The cost-effectiveness of public health interventions examined by the National Institute for Health and Care Excellence from 2005 to 2018”, Public Health, Vol. 169, pp. 151-162, http://dx.doi.org/10.1016/j.puhe.2019.02.011.
[32] Owen, L. et al. (2012), “The cost-effectiveness of public health interventions”, Journal of Public Health, Vol. 34/1, pp. 37-45, http://dx.doi.org/10.1093/pubmed/fdr075.
[30] Republic of Latvia (2013), Procedures for the Public Participation in the Development Planning Process, https://likumi.lv/ta/en/en/id/197033-procedures-for-the-public-participation-in-the-development-planning-process (accessed on 26 March 2020).
[12] Reuters (2019), Latvia fires next salvo in Baltic booze battle, https://www.reuters.com/article/us-estonia-latvia-alcohol/latvia-fires-next-salvo-in-baltic-booze-battle-idUSKCN1U321V (accessed on 15 May 2020).
[15] United Nations (2019), World Population Prospects, https://population.un.org/wpp/Download/Standard/Population/ (accessed on 6 March 2020).
[23] Walkinshaw, E. (2011), “Mandatory vaccinations: The international landscape.”, Canadian Medical Association journal, Vol. 183/16, pp. E1167-E1168, http://dx.doi.org/10.1503/cmaj.109-3993.
[40] WHO (2017), Financial protection in high-income countries: a comparison of the Czech Republic, Estonia and Latvia, http://www.who.int/health_financing/events/who_europe_uhc_day_report_web.pdf.
[10] WHO FCTC Implementation Database (2018), Latvia Factsheet, https://untobaccocontrol.org/impldb/latvia/ (accessed on 6 March 2020).
[16] World Bank (2016), Europe and Central Asia Country Risk Profiles for Floods and Earthquakes, http://documents.worldbank.org/curated/en/958801481798204368/pdf/111015-REVISED-WP-ECA-Country-risk-profiles-PUBLIC.pdf (accessed on 15 May 2020).
[37] World Health Organization (2020), Global Health Expenditure Database, https://apps.who.int/nha/database (accessed on 18 November 2020).
[7] World Health Organization (2020), Global Health Observatory Database, WHO, Geneva, https://www.who.int/data/gho (accessed on 18 November 2020).
[14] World Health Organization (2020), Obesity and overweight - Fact sheet, https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 24 February 2020).
[8] World Health Organization (2019), Country profile Latvia Summary of MPOWER measures in Latvia.
[11] World Health Organization (2019), WHO Global Information System on Alcohol and Health (GISAH), http://apps.who.int/gho/data/node.main.GISAH?lang=en (accessed on 12 November 2019).
[9] World Health Organization (2014), Fact Sheet - Tobacco Taxation, https://www.euro.who.int/__data/assets/pdf_file/0007/250738/140379_Fact-sheet-Tobacco-Taxation-Eng-ver2.pdf (accessed on 15 May 2020).
[31] World Health Organization (2014), The Case for Investing in Public Health, WHO, Copenhagen.
[34] World Health Organization (2011), From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low-and Middle-Income Countries, WHO, Geneva, http://www.who.int (accessed on 18 November 2020).