Wouter De Tavernier
Andrew Reilly
Hervé Boulhol

Wouter De Tavernier
Andrew Reilly
Hervé Boulhol
This chapter first examines the lack of recognition of long-term care workers and its origins and presents measures countries have taken to boost social recognition of these workers. It then moves to gender issues within the LTC sector including the over-representation of women and the gender wage gap. The chapter finally explores the role of migrant workers in the LTC sector, and shows that they are filling employment gaps in particular as live‑in carers, making them vulnerable to abuse.
The ease with which sectors can fulfil vacancies depends not only on the characteristics of the job advertised, but also on the available workforce that would be interested in taking on the job in question. While Chapters 2 and 3 deal with working conditions of long-term care (LTC) jobs, this chapter looks into the characteristics of the LTC workforce and how these workers are perceived by society. In addition to working conditions such as wages and the working environment, people can be motivated to select a certain job in a given occupation by the recognition it receives from others in society, as it may give them a sense that the work they envisage is considered valuable. In the initial stages of the COVID‑19 pandemic, the applause for care workers was a clear expression of recognition of their hard work and sacrifice. However, as the applause faded, questions have emerged how to improve recognition of healthcare and LTC work in a sustainable way. This chapter discusses social recognition, the forms it can take and the forms of recognition care workers currently experience as lacking.
The LTC workforce is highly female and has an above‑average share of workers with a migration background. Both women and immigrants often occupy disadvantaged positions in the labour market in general, in particular as they more often work in less-well-paid jobs. This chapter analyses in detail the composition of the LTC workforce in terms of gender and migration background, looks into the root causes of the overrepresentation of women and migrants in LTC and explores how this may impact working conditions and recognition of LTC work.
This chapter consists of three sections. The first section goes into recognition of LTC workers, examines the sources of LTC workers’ feeling of not being properly recognised and details initiatives OECD countries have recently undertaken to improve the recognition of these workers. The second section explores the gender imbalance in the LTC workforce and its causes. The final section presents the increasing reliance on migrant workers in LTC, documents OECD countries’ efforts to attract foreign workers and compares their working conditions to those of native‑born workers.
Studies from Australia and the Nordic countries show that LTC workers feel recognised by care recipients and by their colleagues, but much less so by their managers, politicians and the wider society. This feeling of low recognition is related to poor working conditions including wages and low status.
Social recognition refers to the acknowledgement of a worker’s contribution to the community and can take the form of gratitude, good status or high enough remuneration. While care work has repeatedly been described as “undervalued”, meaning that the market value of care would be below its social value for the community or society, it is not clear what the social value of LTC is. Gendered care norms downplay the skills needed to provide LTC and the wage levels required to attract skilled and motivated workers to the LTC sector, undermining recognition and valuation of care work.
To go Beyond Applause and sustainably improve LTC workers’ position in society necessitates better recognising their work in terms of increased status and remuneration and tackling gendered care norms.
OECD countries’ initiatives to improve the social recognition of LTC workers include increased remuneration, fighting gender discrimination, recognition of LTC experience in education, increased training requirements for LTC workers and public information campaigns.
LTC professions are among those where women are most over-represented, accounting for more than 85% of LTC employment. The only other sectors with such an over-representation of women are cleaners and helpers as well as general and keyboard clerks.
The gender pay gap among technical and semi/low-skilled workers in the healthcare and care sector, which cover most LTC workers, is much smaller than for similar workers in other sectors. Yet, in a sector where women are so numerous, women are paid significantly less than men for workers with otherwise similar characteristics, by about 7‑8%. In particular, women are not well represented in management positions.
The over-representation of women in LTC is due to two main factors. First, LTC jobs offer opportunities for part-time or flexible working hours, and the share of healthcare and care workers working part-time among women is twice that among men (32% and 16%), with both rates being higher than in the total economy. Second, stereotypes learned in childhood and persistent gender biases in unpaid care work at home play a key role; girls are two to three times more likely to pursue health-related studies than boys, and women tend to be seen as a more natural “fit” for paid care work.
Reaching a more gender-balanced LTC workforce may increase economic performance, job status and wages for all workers in the sector.
Foreign-born workers account for 26% of the LTC workforce on average across OECD countries, compared to 20% of all workers.
Over the past decade, there has been a large increase in the employment share of foreign-born workers in the LTC sector in virtually every European country, with an average increase of more than 5 percentage points of their share in total employment. The reliance on migrant workers to fill the employment gaps in the LTC sector is likely to increase further due to population ageing.
Foreign-born workers represent a large proportion of live‑in carers and the monitoring of their employment conditions is generally very poor, making them vulnerable to abuse.
Only Canada, Israel and Japan in the OECD have so far been identified as having specific legal labour migration channels for care workers.
During the initial stages of the COVID‑19 pandemic, people applauded those working on the front lines in caring for infected patients around the globe. The applause was an expression of the general public’s acknowledgement and appreciation – that is, the recognition – of the work done and sacrifices made by doctors and nurses as well as personal care workers in long-term care (LTC). As the first lockdowns ended and the clapping faded, discussions emerged on how to revalue the work of care workers and recognise their contribution to society more sustainably.
Recognition refers to the acknowledgement and approval of individuals or social groups and the work they do for the broader community (Austen et al., 2016[1]). Recognising other people means to see and treat them as full members of society. A lack of recognition, or misrecognition, can then be understood either as a form of psychological harm at the individual level, entailing disrespect and undermining the person’s self-esteem, or as a form of social subordination at the societal level, and thus an expression of social hierarchy and exclusion (Elstad and Vabø, 2021[2]).
Studies indicate that the recognition of LTC work (or at least its perception) is low in the general public, although it is high among care recipients. Generally, LTC workers themselves feel recognised by the care recipients and their families, but much less so by their managers, policy makers and the wider community (Table 4.1). One Australian study (Austen et al., 2016[1]) found that one in five LTC workers felt not at all recognised by their managers and a similar share felt not recognised by the community.1 At the same time, very few felt misrecognised by care recipients or their family members. A similar picture emerges in a Nordic study (Elstad and Vabø, 2021[2]): while the vast majority (nine in ten) of LTC workers felt valued by colleagues and care recipients, one in three felt not at all recognised by municipal leaders. The feeling of not at all being recognised by mass media ranged from 19% in Norway to 36% in Denmark, and the feeling of not at all being valued by the general public from 7% in Finland and Norway to 21% in Denmark. A similar outcome was found in France (Baret, Recotillet and Kornig, 2021[3]).2
The Australian and Nordic studies show that intentions to quit LTC work are related to the feeling of misrecognition. In the Australian study recognition by the community, especially, was associated with turnover intentions. In the Nordic countries, where local authorities play an important role in the organisation of LTC provision, LTC workers’ experience of misrecognition from municipal leaders was an important driver of intentions to quit. Hence, misrecognition can seriously hamper care supply as four in ten Nordic LTC workers had seriously considered quitting over the last year (Elstad and Vabø, 2021[2]).
Share of LTC workers “not at all” feeling valued by the specific stakeholder
|
|
Managers |
Municipal officials and politicians |
Mass media |
General public1 |
Clients |
Colleagues |
|---|---|---|---|---|---|---|
|
Australia |
21% |
18% |
<2% |
|||
|
Denmark |
34% |
36% |
21% |
0% |
1% |
|
|
Finland |
34% |
23% |
7% |
0% |
1% |
|
|
Norway |
19% |
7% |
0% |
0% |
||
|
Sweden |
33% |
32% |
17% |
0% |
1% |
1. In the Australian study, LTC workers were asked about feeling valued by their local community. The Australian sample consisted of approximately 4 000 female LTC workers aged 45+ surveyed in 2011‑12; the Nordic samples consisted of unionised LTC workers surveyed in 2015, with samples ranging from approximately 750 in Sweden to around 1 000 in Denmark and Finland.
Source: Austen et al. (2016[1]), “Recognition: applications in aged care work”, https://www.doi.org/10.1093/cje/bev057 for Australia; Elstad and Vabø (2021[2]), “Lack of recognition at the societal level heightens turnover considerations among Nordic eldercare workers: a quantitative analysis of survey data”, https://www.doi.org/10.1186/s12913-021-06734-4 for Denmark, Finland, Norway and Sweden.
LTC workers’ feelings of misrecognition by the society are likely driven by a negative perception of the job itself and the skills required. These feelings were related to the community’s perception of their work as being “dirty”, reducing the job to its physical aspects and overlooking its emotional and communicative aspects (Austen et al., 2016[1]). Overlooking these aspects then results in a lack of recognition of the emotional and psychological competences required to care for vulnerable people (Bailly, Devetter and Horn, 2013[4]). The feeling of misrecognition by managers and policy makers is likely connected to poor working conditions and low remuneration, for which LTC workers hold these leaders responsible. Half of Australian LTC workers considered their earnings not at all satisfactory in the light of the estimated importance of their work for society (Austen et al., 2016[1]).
One study analysing the perceptions of LTC workers among service users and their close relatives shows that they both value the interactive aspects of care work and workers’ social skills (Manthorpe et al., 2017[5]); indeed, interactions with LTC workers often make up a large part of the care recipient’s day-to-day social contacts. Both also value more professional characteristics, including a strong work ethic, reliability and an individualised approach to care work.
Recognition can be expressed in the form of payments or in non-monetary forms. Expressions of gratitude are a form of recognition, for instance through applause recognising care workers’ sacrifices to help others under difficult circumstances during the initial stages of the COVID‑19 pandemic. Recognition can also take the form of status.
Health professionals feel very appreciated by care recipients and their families (Aparicio et al., 2019[6]). While care recipients and their family members are grateful for health professionals’ technical skills, the expression of gratitude is particularly linked to their interactive skills: taking time to give information and advice, listening to care recipients’ and their family members’ experiences and grievances, providing emotional support at difficult moments. The applause for care workers during the initial stages of the pandemic was an expression of gratitude for the efforts care workers made as well as for the outcomes of their work in terms of care provided and lives saved (Day et al., 2021[7]). Expressions of gratitude towards health professionals provide a range of benefits, including increased satisfaction, well-being and work motivation, and might reduce burnout in care staff (Aparicio et al., 2019[6]).
Status, or standing, reflects the desirability of an occupation in a given society, and the extent to which the occupation fulfils a role that is considered valuable. Overall, care work has low occupational standing, but it has higher standing than other occupations with similar educational requirements and job characteristics such as strain, repetitiveness and autonomy (Magnusson, 2009[8]).3 Moreover, personal care work is among the least desired occupations among younger people (OECD, 2019[9]).
Remuneration can be interpreted as a manifestation of recognition, although both could separately affect socio‑economic positions. On the one hand, low pay can be experienced as a lack of recognition, particularly from managers and policy makers. On the other hand, remuneration and recognition can be two separate, although mutually reinforcing, mechanisms producing social hierarchy (Fraser, 1997[10]). While remuneration shapes social hierarchies financially, recognition does so culturally: individuals can feel treated as inferior if their contribution to society is not recognised by others. Cultural and socio‑economic inequalities mutually reinforce each other, with cultural inequalities legitimising socio‑economic differences and differences in material conditions reproducing one’s place in the cultural hierarchy. Hence, for a social group to sustainably improve its position in society, both its cultural and its economic position should ameliorate. Specifically, sustainably improving the position of personal care workers entails tackling the gendered care norms, which treat care as a less respectable occupation, recognising the inherent hardness of personal care workers’ jobs, and improving their earnings – that is, to go Beyond Applause.
Increased remuneration can boost workers’ motivation if it is perceived as a form of recognition. If a financial reward is perceived as supportive and an acknowledgement of the person’s performance – that is, recognising the individual’s competence and contribution – it boosts self-determination and self-esteem, and fosters intrinsic motivation. Other working conditions also play a role in whether or not care workers feel recognised. A French study on working conditions and employee recognition in the healthcare sector stresses the importance of employee autonomy, managerial support and being provided with sufficient resources to deliver quality care (Baret, Recotillet and Kornig, 2021[3]).
Recognition depends on the assessment of the work one does for the community or the society. This implies that devaluing the contribution to society made by a certain occupational group leads to misrecognition of that group (Elstad and Vabø, 2021[2]). Care work has repeatedly been described as “undervalued”, although it is often not clarified what is meant by this. Much attention has been paid to measuring the value of unpaid care work for instance in terms of the amount of paid care it substituted (OECD, 2021[11]), but few efforts have been made to assess the social value of paid care work.
It is sometimes argued that if left to the forces of supply and demand, care work would not be valued properly (Barry and Jennings, 2021[12]; ILO, 2018[13]; Folbre, 1995[14]), implying that care work has “social value” as different from market value. “Social value” thus refers in that case to care work having some value other than its market value for the community or society. However, what this social value exactly entails is rather vague, let alone measurable. It is reminiscent of the concept of positive externalities in economics, referring to others reaping some benefits from a good or a service beyond the buyer and the seller themselves of that good or service. While examples of positive externalities include getting a vaccination to limit the spread of a virus, the decision to stop smoking to avoid passive smoking, opting for public transport or cars that are less polluting, etc., it is much less clear how personal care work produces benefits for the wider community beyond those for the care recipients and their families.
The lack of a clear understanding of what social value exactly is, does not mean that personal care work cannot be undervalued in the labour market. Indeed, there appears to be a wage penalty to being a personal care worker compared to other occupations with similar characteristics (Chapter 2). In particular, gender norms may play a role in wages being lower for personal care workers than for comparable occupations.
In the traditional gendered division of labour, care is considered women’s work and the skills required for performing care work are assumed to occur “naturally” in women. In the male‑breadwinner model, home care is not part of income‑producing activities and is thus not valued in monetary terms.
In a society adhering to or still replicating some forms of the traditional division of labour, the crowding of women in the care sector could result in undervaluation of care work. This crowding of the LTC sector by women could be theorised as the result of discrimination against women in other sectors (i.e. a preference among employers for male workers), or as the result of women’s own preferences, whether they are “naturally” occurring in women or shaped by norms setting non-monetary rewards for performing care work (Folbre, 1995[14]).
The women’s work devaluation thesis asserts that work is undervalued if it is done primarily by women (England, Budig and Folbre, 2002[15]). This is due to gender bias, for instance because the skills required might be perceived as being “natural” in women and therefore not requiring specific training or compensation (England and Folbre, 1999[16]; England, Budig and Folbre, 2002[15]; Austen et al., 2016[1]) – this perception overlooks that in child raising, girls are more likely to be stimulated to take up care tasks at home. At the same time, the idea that the skills required for care work are “natural” in women can undermine willingness to pay for care services particularly if families think they are able to provide the required services themselves (Bailly, Devetter and Horn, 2013[4]). The blurring of care and domestic work and cash-for-care schemes, allowing that family members are paid to provide care, further contribute to the perception that personal care work does not require specific skills (Le Bihan and Sopadzhiyan, 2018[17]). However, low-status jobs are typically highly gendered rather than specifically female, and occupational standing of care work may not be exceptionally low compared to other occupations requiring similar training levels and displaying similar job characteristics (Magnusson, 2009[8]; García-Mainar, Montuenga and García-Martín, 2018[18]).
Some institutionalist thinkers furthermore argue that it is the necessity of the work – testifying to its high value – that causes its low pay. As care is a socially necessary activity, norms assigning caregiver roles to a specific social group, in particular women, could make care provision, a highly time‑intensive activity, significantly cheaper or even free in the case of informal care (Folbre, 1995[14]). Indeed, the provision of LTC often happens in a context of inequality between the caregiver and the care recipient, whether this inequality is shaped by income differences, gender norms or precariousness due to migration (De Tavernier and Draulans, 2018[19]). Female care norms, linked to the idea of care as work done “for love” rather than “for money” (see below), therefore contribute to ensuring an affordable supply of LTC for older people. The same applies to care work carried out by immigrants, who often occupy weaker positions in the labour market – such as having a higher likelihood to be employed in non-standard work (OECD, 2018[20]) – and have less leverage to bargain for higher wages (Cools, Finseraas and Bergli Rasmussen, 2020[21]; Kranendonk and de Beer, 2016[22]). One specific issue of recognition in relation to immigrants is the lack of recognition of previously acquired qualifications. About one‑quarter of economy-wide immigrant workers are formally overqualified for their jobs (OECD, 2017[23]), which in the case of LTC often entails nurses and other healthcare professionals working as personal care workers (IOM, 2010[24]). Formal procedures may prevent the recognition of previously acquired degrees and skills abroad even though managers may appreciate both the skill level (Atanackovic and Bourgeault, 2013[25]) and the flexibility offered by migrant care workers (Näre, 2013[26]).
Wages may be low if non-monetary rewards of work – or amenities, see Chapter 2 – are high, following the concept of compensating wage differentials, so that employers could offer lower wages for work that is intrinsically motivating (England, Budig and Folbre, 2002[15]; Palmer and Eveline, 2012[27]). Good-quality care entails not only performing certain activities (“caring for”) but it may also require a certain emotional connection (“caring about”). Some have even argued that higher wages would draw in less intrinsically motivated people for whom care is not a “vocation”, resulting in a weaker emotional connection and therefore a lower quality of care – that is, they argue that care work would be better if performed “for love” rather than “for money” (Brekke and Nyborg, 2010[28]; Heyes, 2005[29]). Hence, for proponents of this approach, good care requires a certain self-sacrifice of care workers. Some studies have documented cases of employers in the LTC sector subscribing to the idea that care workers should not be motivated by money (Palmer and Eveline, 2012[27]; Franzosa and Tsui, 2020[30]; Austen et al., 2016[1]). Socialising women into the idea that motivations for care should be altruistic results in women being more likely to accept emotional over financial rewards (Hebson, Rubery and Grimshaw, 2015[31]).
The idea that the quality of care would somehow be better thanks to low wages for LTC workers makes little sense for several reasons. This makes even less sense in the light of care shortages that cannot be solved by relying solely on LTC workers for whom care is a “vocation”. First, low wages in the LTC sector may result in skilled and motivated workers choosing to work in other sectors, which could undermine the quality of LTC provision (Fedele, 2018[32]; Austen et al., 2016[1]). Second, workers who feel that the remuneration and other amenities they receive are not in proportion to their performance may seek to rebalance by reducing performance, resulting in lower-quality care. LTC workers feeling unfairly compensated are for instance less involved in their work (Heponiemi et al., 2011[33]) and more likely to want to retire (Sulander et al., 2016[34]). Third, choosing to become a care worker for the sake of making an income does not necessarily imply providing impersonal care. Intrinsic (liking the nature of the work) and extrinsic motivations (financial incentives) are by no means mutually exclusive: not only extrinsically motivated people are concerned about having a high enough income, also care workers who are strongly intrinsically motivated would want to have a better lifestyle for themselves and their families (Folbre and Nelson, 2000[35]). Fourth, it puts too much emphasis on the emotional skills of care workers and tends to disregard other skills and competences that contribute to providing good-quality care (Nelson and Folbre, 2006[36]). And finally, self-sacrifice may even undermine good care as nurses who are more motivated by altruistic feelings tend to experience higher job turnover and are more likely to face health problems including burnout (Dill, Erickson and Diefendorff, 2016[37]).
The bottom line is that workers could be altruist, brave and generous and still expect not to receive undervalued wages to do their job well. As summarised by the Royal Commission into Aged Care Quality and Safety (2020[38]), “aged care workers do not need to be told they are heroes. They need better wages and conditions and enough colleagues to be able to complete their work safely and to the standard that they consider is appropriate. That is how their work can be properly respected and acknowledged”.
OECD countries recognise the need to improve the social recognition of LTC workers and have taken measures to boost social recognition through three different means (Table 4.2). Sixteen OECD countries have aimed to improve the remuneration of LTC workers either through permanent wage increases or through bonuses or temporary wage increases in relation to COVID‑19. Ten countries have taken initiatives in the area of education and training: eight countries recognise previous work experience in LTC by awarding course credits in education programmes, and two have strengthened training requirements for LTC staff. Finally, five countries have aimed to improve the public image of LTC workers through organising or supporting public information campaigns.
Several countries have permanently increased wages of LTC workers since the outbreak of the COVID‑19 pandemic and before the inflation surge. While the impact of these increases may have been significantly mitigated by high recent inflation, they still result in an increase in the relative income of LTC workers compared to workers in other sectors.
Hungary (20%), Slovenia (up to 16%) and Lithuania (8% or 13% depending on level of education) have noted the biggest increases in salaries. Wages in the LTC sector were also increased in Belgium, where those working in institutional care settings gained 6% and those working in home care 4.5%, in Japan, where wages of LTC workers in institutional care were increased by around 3%, in Luxembourg, where all LTC workers received a real-wage increase of 2%, and in the Netherlands, where wages for nurses and some groups of personal care workers were increased by 1.5% in addition to an increase of 2.5% of all wages in the care sector.
France significantly increased care workers’ wages, especially for low-wage earners as it opted for flat-rate supplements. Australia opted to increase the minimum wage for LTC workers by 15% in 2023 and set up an expert panel to examine whether supplementary increases in wages are required in the sector. Similarly, Germany increased the minimum wage for LTC workers by around 10% in 2022 with some variation depending on qualification levels; there are plans to increase it further by around 4% in 2023. Latvia adjusted minimum and maximum wages for LTC workers employed by municipalities, as part of a wider reform of wages for public sector workers.4
Most countries that provided permanent wage increases to LTC workers also implemented temporary wage increases or bonuses in response to the COVID‑19 pandemic. In addition to those countries, bonuses were paid to LTC workers in Japan as well as, albeit indirectly, in Austria, Canada and the United States. In Austria, the federal states are temporarily provided with additional financing from the government in order to improve the income situation in the LTC sector. Similarly, as Canadian federal government has no jurisdiction over care workers’ wages, it provided funding to the Provinces and Territories to temporarily top up the wages of low-income “essential workers”, including LTC workers.5 In 2021, the US federal government reserved a supplementary budget of around 8% of public LTC spending for states to improve home and community-based services over a 12‑month period, which several states used to provide bonuses to LTC workers.
Luxembourg provided LTC workers with extra holidays, which in effect entails an increase in hourly earnings. Nurses and personal care workers in LTC are entitled to one extra day of leave per year, and in 2021 they received an additional bonus in the form of two extra days of leave. In addition, a guarantee of 20 work-free weekends per year was introduced to improve work-life balance in the sector.
|
Permanent wage increase |
Bonus or temporary wage increase |
Obligatory education and training |
Recognition of experience in education and training |
Public information campaign |
|
|---|---|---|---|---|---|
|
Australia |
● |
● |
|||
|
Austria |
● |
● |
|||
|
Belgium |
● |
● |
|||
|
Canada |
● |
||||
|
Chile |
|||||
|
Colombia |
|||||
|
Costa Rica |
|||||
|
Czech Republic |
● |
||||
|
Denmark |
● |
||||
|
Estonia |
|||||
|
Finland |
|||||
|
France |
● |
● |
|||
|
Germany |
● |
● |
● |
||
|
Greece |
|||||
|
Hungary |
● |
● |
|||
|
Iceland |
|||||
|
Ireland |
● |
||||
|
Israel |
|||||
|
Italy |
|||||
|
Japan |
● |
● |
● |
● |
|
|
Korea |
● |
● |
|||
|
Latvia1 |
●a |
● |
|||
|
Lithuania |
● |
● |
|||
|
Luxembourg |
● |
● |
● |
||
|
Mexico |
|||||
|
Netherlands |
● |
● |
|||
|
New Zealand |
|||||
|
Norway |
● |
||||
|
Poland |
|||||
|
Portugal |
● |
||||
|
Slovak Republic |
|||||
|
Slovenia |
● |
● |
|||
|
Spain |
|||||
|
Sweden |
● |
||||
|
Switzerland |
● |
||||
|
Türkiye |
|||||
|
United Kingdom |
● |
||||
|
United States2 |
● |
● |
1. In Latvia, wages for LTC workers are set by the municipalities, although within a range determined by the law and government regulations. As part of a wider reform of wages of public sector workers gradually taking effect over the period 2022‑27, the maximum wage for LTC workers is substantially increased and a minimum wage is introduced. However, it is unclear to what extent LTC workers’ wages will effectively be impacted.
2. In the United States, the federal government did not provide bonus payments to LTC workers in response to COVID‑19, but several states did (Denny-Brown et al., 2020[39]; Tyler et al., 2021[40]).
Source: Information provided by countries.
Interventions in terms of education and training include both increasing training requirements and valorising previous work experience in LTC by awarding course credits in education programmes. Training programmes for LTC workers improve the quality of care delivered and can in addition ameliorate the public image of LTC jobs (Fujisawa and Colombo, 2009[41]). In Belgium, completion of a formal training programme and at least two days of additional training every year are obligatory for all LTC workers. Ireland assesses the quality of LTC providers which includes educational requirements of the provider’s care staff. LTC workers have to complete certain trainings or refresher programmes depending on the needs of the persons they are caring for. This approach allows for an incremental build-up of knowledge and competences tied to improving care quality.
Experience in personal care work can also be valorised in the form of course credits for education and training programmes. In most countries, it is left to education providers to determine whether certain work experiences can replace (part of) the training programme. In Denmark and Norway, university colleges providing programmes in nursing can award study credits for relevant work experience. Usually, such credits are awarded for internships intended to build practical experience as part of the study programme, although in principle also credits for theoretical parts of the curriculum could be awarded for work experience. In Sweden, Switzerland, the United Kingdom and the United States, prior work experience can replace courses in vocational training programmes in LTC. In Switzerland, even the entire training for some health and social care workers can be replaced by recognised work experience.6 Japan and Portugal take a national approach to the valorisation of work experience. Japan provides a qualification as certified personal care worker to people passing a national exam. To enter the exam, people need to have work experience as a personal care worker and should have gone through an advanced training course. Portugal has a national system to register qualifications built up through training or experience, also covering qualifications in the area of social services.
Information campaigns can be used to try to change the public image of LTC workers and can contribute to LTC workers feeling more valued by the media and the general public. Australia launched its multi-media campaign “A Life Changing Life” in 2021 to attract more workers to the LTC sector, with testimonies illustrating the importance of LTC workers for care recipients. Austria has developed aired television commercials picturing the everyday working lives of people working in care professions. The aim of this 2020 campaign was to improve the public image of these occupations and make them more attractive. Germany ran a campaign between 2019 and 2021 under the tagline “Make a career as a human!” (“Mach Karriere als Mensch!”) to entice young people to choose a career in care. A new campaign running from 2022 to 2025 similarly aims to increase the number of young people choosing to study for a caring profession, and in addition is supposed to boost the public standing of care work. Similarly, Luxembourg launched an information campaign at the end of 2022 with the same dual purpose. The campaign primarily targets younger people through social media and provides information on working in different occupations in healthcare and LTC among others through video testimonies. The Japanese Government has not organised public campaign itself but has provided support to private initiatives intended to improve the public image of LTC workers. Projects receiving support include among others a programme in which LTC workers visited high schools to talk about their work and how to interact with older people; a series of virtual tours of LTC institutions showing the variety of jobs they offer; and, a scheme in which media personalities visited LTC providers and talked to workers to broaden their knowledge about the work so that it would be promoted and depicted more attractively on TV and in newspaper reports. While these information campaigns may be good examples for other OECD countries, there are no evaluations of their impact in either of these countries.
In all OECD countries, the LTC workforce is predominantly female. On average across countries, women account for the vast majority of workers, ranging from 78% in Japan to 95% in Korea among the 25 countries for which data is available (Figure 4.1). Having such a gender-related imbalance raises a host of issues related to wage levels, discrimination, social stereotypes, valuation of the work, well-being at work and economic performance.
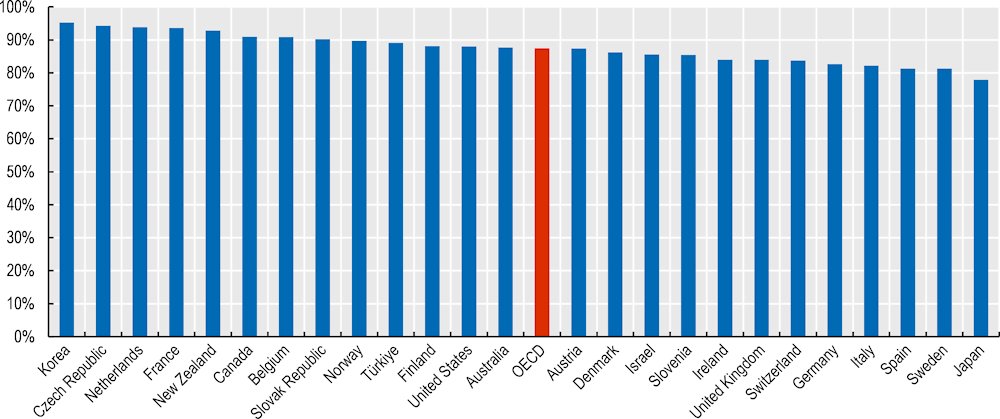
Note: The OECD data point is the unweighted average of the 25 OECD countries shown in the chart. Data are based on ISCO 3‑digit and NACE 2‑digit codes. Data for the Czech Republic, France, the Slovak Republic and Slovenia should be treated with caution as they fall below the “b” limit for reliability. Data is 2016 for Australia, Canada and Japan, 2019 for New Zealand and 2020 for Korea and the United States.
Source: EU-Labour Force Survey; ASEC-CPS for the United States; Census 2016 for Canada; LFS for Israel; Survey on Long-term Care Workers 2016 for Japan; OECD estimates based on national sources for Australia and New Zealand.
This section builds upon the analysis of social recognition discussed in the preceding section. It begins by investigating the employment levels by gender across occupations before concentrating on part-time work in LTC. Attention then turns to earnings and gender pay gaps across sectors. Why most LTC workers are women is then explored before discussing whether attracting more men to the LTC sector may be an interesting avenue to pursue.
Women represent 88% of all personal care workers, over 75% of health associate professionals and 70% of health professionals (Figure 4.2).7 The only other sectors with such a large proportion of female workers are cleaners and helpers as well as general and keyboard clerks. By contrast. men represent over 90% of workers in manual labour professions, such as builders or electricians, as well as in the armed forces. Overall, based on the ISCO‑08 two‑digit classification, about half of professions8 have a workforce that is at least 60% male; by contrast, less 20% of occupations have a workforce that is over 60% female including food preparation assistants and other clerical workers on top of the aforementioned occupations.
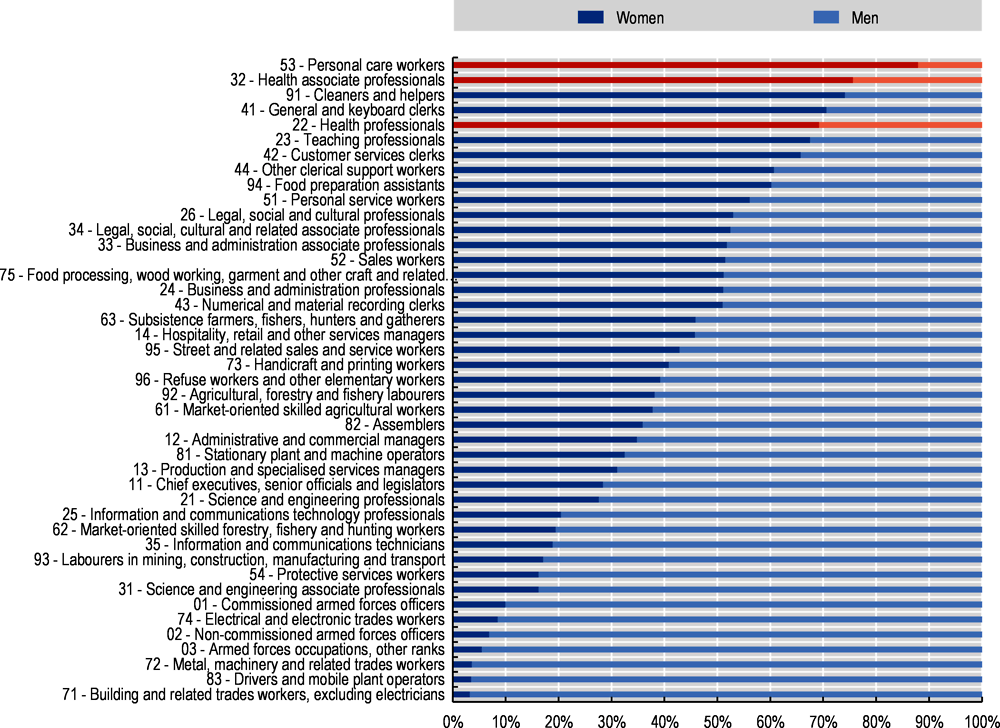
Note: The weighted average is not a global figure. It is based on available data for 121 countries, which represent 63% of global employment. Data for China and India were not available. For ease of reading professions with less than 60% for both genders have been excluded.
Source: ILOSTAT.
Despite the fact that the LTC sector has such a predominantly female workforce, women are not as well represented in senior positions. Only 20% of the managerial roles in the LTC sector in the United States, for example, are filled by women; this women’s share in management levels is similar in LTC to that in many other professions, as men dominate managerial roles in general. Similar results have been found in other countries. For example, in England, despite representing only around 17% of the LTC workforce, men filled 32% of senior management roles (Hussein, Ismail and Manthorpe, 2014[42]).
However, over the last few decades, there may have been a change in the perception of “female” and “male” jobs, with men now more likely to be employed in traditionally female‑perceived occupations. The latest data from the National Aged Care Workforce Census in Australia indicates that since 2012 the share of male staff working in aged-care‑related work has increased from 10% to 13%. In the United States, more men are moving to jobs that have been predominantly seen as a female domain. An analysis of census data showed that between 2000 and 2010, almost one‑third of all job growth by men were in occupations that were more than 70% female, double the share of the previous decade; it also finds that in Texas the number of male registered nurses doubled over the same period and men accounted for 10.5% of all nurses, up from 8.4% a decade earlier (Dewan and Gebeloff, 2012[43]).
The gender composition within sectors seems to influence wage differences across sectors for workers with similar characteristics (Chapter 2). For example, sectors in which 90% of workers are men are estimated to pay 14% more per working hour for similar workers (age, education, tenure, etc.) of the same sex than those with equal gender shares in employment. The gap is even larger, at 18%, when comparing sectors with 90% male employment to those with 90% female employment. This provides some support to the idea that, by having a primarily female workforce, the LTC sector as a whole may have been devalued.
However, results differ when comparing across occupations (e.g. nurses, managers, cooks, etc.) rather than across sectors (e.g. healthcare, social care, construction etc.). Chapter 2 did not find similar significant effects of the gender proportions on wage differences across occupations for workers with similar characteristics. However, there has been some evidence in the United States of a large negative impact of the increase in the share of female workers over time in a given occupation on the average wage of both men and women in that occupation (Harris, 2022[44]).9
Gender pay gaps within the healthcare and care sector are compared with those within all other sectors. The gender pay gap is defined as the difference in average earnings between men and women who are engaged in paid employment, as a ratio of male earnings. Data are from ILO and WHO estimates based on national survey data from WHO (2022[45]). Data are grouped by three occupational categories within sectors: professional, technical and semi/low-skilled. The professional category in the healthcare and care sector includes nurse professionals, while nurse associates are part of the technical worker category and semi/low-skilled covers auxiliary healthcare workers and personal care workers. Hence, almost all LTC workers are included in the technical and semi/low-skilled categories while the professional category is mainly relevant for the healthcare sector.
In the LTC sector where women represent more than 85% of employment, gender pay gaps are pervasive whatever the occupational category. While this could be due to more part-time work and fewer working hours, the in-depth analysis conducted in Chapter 2 based on microdata shows that the gender difference in the hourly wage among LTC workers in similar jobs and with similar characteristics is also significant and estimated at about 8%. That is, even in a sector with such a large share of women, men with similar characteristics having similar jobs earn significantly more. Table 4.3 provides the summary results which are detailed and discussed below in Figure 4.3. The gender pay gap in the professional category is much larger in the healthcare and care sector than overall in other sectors, at 23% versus 17%. These occupations include doctors who are predominantly male and highly paid. There is considerable country variation with virtually no gender gap in Canada and Luxembourg among the professional health and care workers, while it is over 40% in Chile and Lithuania (Figure 4.3, Panel A).
Pay gap between men and women within each occupational classification and sector, in percentage
|
Healthcare and care sector |
Other sectors |
|
|---|---|---|
|
Professional |
23.1 |
17.4 |
|
Technical |
6.8 |
14.7 |
|
Semi/low-skilled |
8.2 |
13.2 |
Note: Professionals cover ISCO codes 1**** and 2****. Technical workers are 3**** and semi/low-skilled are 4**** to 9****. Armed forces (code 0****) are not included.
Reading note: For professional workers within the healthcare and care sector, women earn 23.1% less than men, whilst for other sectors women in the professional category earn 17.4% less than men.
Source: WHO/ILO (2022[45]), The gender pay gap in the health and care sector: A global analysis in the time of COVID‑19, https://apps.who.int/iris/handle/10665/358057.
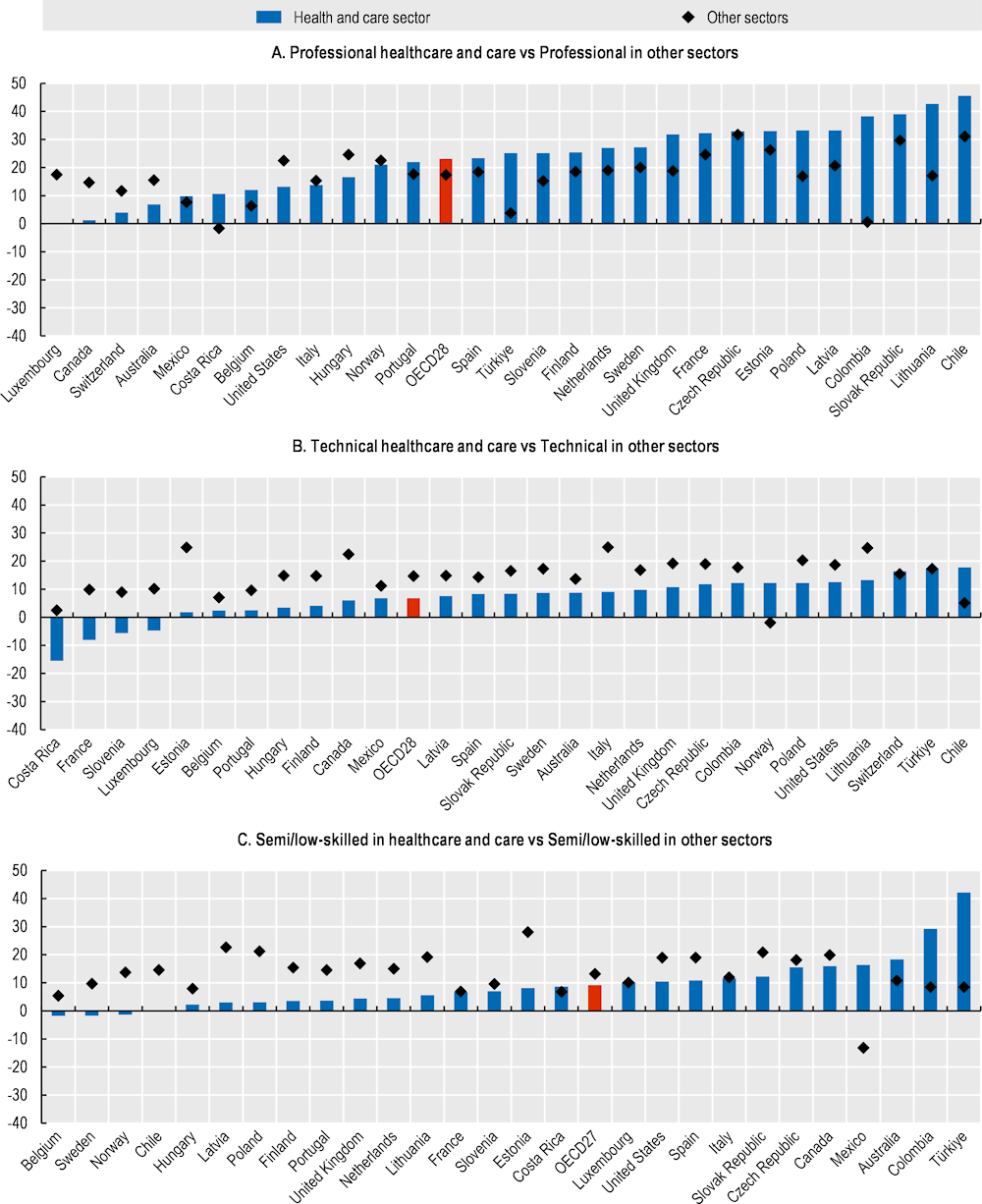
Note: Professionals cover ISCO codes 1**** and 2****. Technical workers are 3**** and semi/low-skilled are 4**** to 9****. Armed forces (code 0****) are not included. Switzerland is not included due to very small sample size.
Source: WHO/ILO (2022[45]), The gender pay gap in the health and care sector: A global analysis in the time of COVID‑19, https://apps.who.int/iris/handle/10665/358057.
Within healthcare and care, the gender pay gap is also much higher for professionals than for both technical and semi/low-skilled where average wages are also lower overall. The much lower gender gaps for latter categories than in the whole economy is consistent with smaller gender gaps generally found in low-wage occupations, partly due to the wage compressing role of minimum wages.
For the technical occupations, the gender gap is 7% for healthcare and care workers, much lower than 15% for other sectors (Figure 4.3, Panel B). In four countries, Costa Rica, France, Luxembourg and Slovenia, women earn more than men working in technical occupations in the healthcare and care sector, i.e. the gender gap is actually negative. Conversely, the gender gap among technical workers in the sector is over 15% for workers in Chile, Switzerland and Türkiye.
The gender gap for the semi/low-skilled healthcare and care workers, which include most LTC workers, is 8%, significantly lower than 13% for the other sectors on average (Figure 4.3, Panel C). The gap is under 5%, in many countries and even negative in Belgium, Chile, Norway and Sweden; conversely, it is positive and large at 15‑20% in Australia, Canada, the Czech Republic and Mexico and about 30% in Colombia and about 40% in Türkiye.
Historically, some sectors or industries have been predominantly comprised of one gender – a phenomenon known as horizontal segregation (OECD, 2021[46]). Gender segregation in the occupations of interest in the current report is extreme.
The causes of horizontal gender segregation are plentiful. First, inherently, LTC jobs offer part-time opportunities. As women provide most unpaid work at home, they are more likely to take up part-time work or a job with flexible working hours in order to reconcile work and family responsibilities (Mas and Pallais, 2017[47]; OECD, 2019[48]). Among healthcare and care workers, a higher proportion of women than men are working part-time (Figure 4.4, Panel A). On average across countries 32% of the female and 16% of the male workers are working part-time. In Austria, Belgium, Germany, Iceland, the Netherlands and Switzerland at least 50% of the female workers are working part-time. By comparison, only 25% of the male workers in these countries are working part-time.
Care work naturally provides part-time opportunities as there are peak periods of activity during the working day, primarily early morning and evenings. Whilst these working times may be beneficial for some, they are harder for others with caring responsibility for children, for example. In the majority of countries, both female and male healthcare and care workers have a higher tendency to work part-time than workers of the respective sex in other sectors (Figure 4.4, Panel B). The difference is actually larger for men than for women, but from a lower level as men work much less part-time than women in the overall economy. More precisely, on average the prevalence of part-time work is 7 percentage points higher for men and 4 percentage points higher for women in healthcare and care compared to other workers.
The data used in Figure 4.4 refer to all workers within the healthcare and care sector, rather than specifically identifying LTC workers. This enables more countries to be included in the analysis as with the gender pay gap analysis above. The specific gender analysis of part-time LTC workers in Chapter 3 (Figure 3.11) indicates that both male and female part-time employment are high compared to other sectors. Comparing the above absolute numbers with reported figures in Chapter 3 implies that the level of part-time work in LTC is higher than more broadly within the health and care sector confirming that part-time work is more widespread in LTC work.
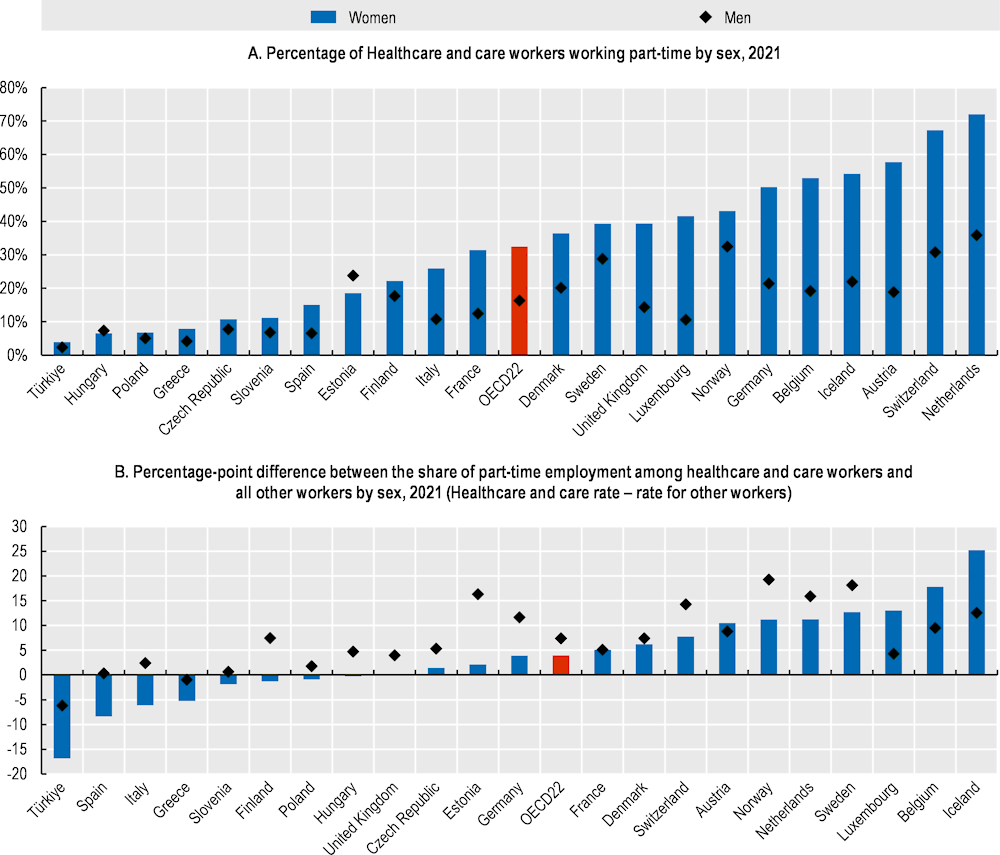
Note: Data are based on ISCO 3‑digit and NACE 2‑digit codes. Data is 2020 for Türkiye and 2019 for the United Kingdom. Data for the Czech Republic, Estonia, Poland and Slovenia should be treated with caution as they fall below the “b” limit for reliability.
Source: EU-Labour Force Survey.
Second, some factors explaining horizontal segregation are rooted in stereotypes learned in childhood and early schooling. Seehuus (2021[49]) suggests that the persistent gender segregation in the labour market is the result of men and women initiating and continuing to pursue different educational paths. OECD PISA finds that 15‑year‑old girls are two to three times more likely to pursue health-related studies than boys, with the percentage of girls who stated that they expect to work in the healthcare sector growing significantly in most countries, whilst that for boys has been stable (OECD, 2017[50]). As a result, the gender gap in the percentage of students expecting to work in the healthcare sector has grown in most countries.
Moreover, the pervasiveness of gender biases in unpaid care work at home has repercussions on the labour market for formal care as women may be seen as a more natural “fit” for paid care work (Hay et al., 2019[51]). Globally, women bear the disproportionate responsibility for unpaid care work: over 75% of the world’s total unpaid care work, including childcare, is done by women (OECD, 2019[52]).
Based on responses to the 2021 Gender Equality Questionnaire sent to OECD member countries, the attitude towards men having a role in caregiving has progressed (Figure 4.5). Three‑quarters of the governments that responded answered either somewhat or very much improved in response to the question, whilst about one‑fifth answered that the position is unchanged.10 The results are very similar when looking at the attitude towards women working whilst having a family, with 77% of countries answering somewhat improved or very much improved, though there is still a wide margin for further progress in many countries given the large remaining gender differences.
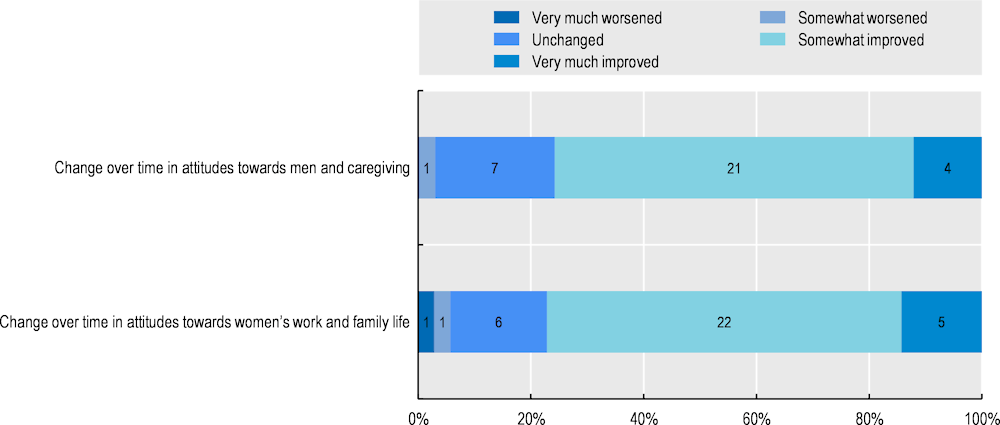
Note: Out of the 38 OECD member countries, 33 responded to the question regarding “attitudes towards men and caregiving”, and 35 to the question on “women”s work and family life’. Number of countries marked.
Source: 2021 Gender Equality Questionnaire (2021 GEQ).
A Handbook chapter has found women to be more empathetic than men (Marianne, 2011[53]), providing both push and pull factors11 to LTC work. Greenberg et al. (2022[54]) find that women are better at empathising with others than men no matter where they live in the world or what their cultural or family influences, in their study covering over 300 000 individuals in 57 countries. Burbano, Padilla and Meier (2020[55]) also highlight that women have a higher tendency than men to move into jobs that help others; they also find that while financial preferences are similar between men and women, women tend to draw more personal reward from work that provides wider benefits, whether to individuals or to communities.
There is of course nothing inherently female about the skills required to be a good carer. Skills that may be required include managing medication, preparing food, assisting with personal care and helping people to move about, as well as empathy and commitment. Social norms may assign some of these skills, such as being a sensitive person or managing personal care, more commonly to women. But others, such as helping a person move around or lifting somebody from a chair or bed, are skills that rely on characteristics more generally associated with men, such as body strength. Thus, it is time to combat prejudice and recognise that excellent care can be provided by both men and women, and that there is nothing inherently female about the skills needed and tasks undertaken in the care profession.
The devaluation of LTC work can be an important barrier to recruitment. The LTC sector has long suffered from a lack of social recognition, as discussed in Section 4.1. This is likely to make it more difficult to attract young people as well as men who may traditionally regard LTC jobs as “women’s work” (OECD, 2020[56]). Overcoming recruitment difficulties is one key objective to tackle current and future shortages of workers in the sector, which are analysed in Chapter 5.
Better gender balance helps to improve economic performance (OECD, 2008[57]). In Australia, a better gender balance has been identified as a way to increase organisational performance, enhance the ability of companies to attract talent and retain employees, and improve organisational reputation (WGEA, 2022[58]). In a recent survey in the United States, about three‑quarters of job seekers said that a diverse workforce is an important factor when evaluating companies and job offers (Glassdoor, 2021[59]). There are more male applicants to jobs typically thought of as “female jobs” if the vacancy presents the job as more challenging and indicates that skills and performance are rewarded (Delfino, 2021[60]). However, the majority of campaigns or recruitment programmes in OECD countries are just designed to get more workers into the sector irrespective of who they are rather than directly tackling gender imbalances.
Some patients may prefer to have a male carer, and employing more men may solve some sensitive issues. There is a multitude of reasons why a male care worker may be preferred, ranging from privacy issues, to being able to relate more easily or even religious beliefs. Being able to accommodate these requests would provide a better experience for the patient. According to Care England – a trade organisation for independent adult social care providers -, with men living longer, more male workers will be needed to provide support, as some older men prefer to be looked after by men (BBC, 2015[61]).
Norway and the United Kingdom have implemented positive discrimination programmes that were specifically targeted at getting more men into the sector to try and redress the gender imbalance. The Norwegian Menn i helse (Men in health) programme was targeted at unemployed men aged 26‑55 years providing an apprenticeship certificate for men, enabling them to work in the health social care sectors. It has produced more than 400 successful graduates since 2010 (Nordregio, 2021[62]). In the United Kingdom, Skills for Care – a development and planning body for adult social care -commissioned the Men into Care Programme to attract more men into the LTC workforce. This programme actively encourages more men to study healthcare‑related subjects to help increase the level of future employment. Coventry University, for example, announced in 2017, a fund of GBP 30 000 to help ten men in subjects where they are under-represented including nursing, occupational therapy, physiotherapy, midwifery operating department practice, and dietetics. Similarly, Queen’s University Belfast, alongside a private housing and care provider, have been running campaigns to encourage more men into care work including targeting all-boys’ schools.
A significant proportion of the LTC workforce are migrants in many countries, and this phenomenon is likely to increase in the coming decades to help deal with population ageing. The large number of migrant LTC workers, in some countries, has been influencing the nature of LTC provision by enabling many more people in need to remain at home rather than having to go to institutions. At the same time, with the migration of care workers, shortages can easily develop in the countries of origin, both within the formal sector and the immediate family. Whilst most less-developed countries still have favourable demographics, they are expected to age rapidly. Therefore, demand for care workers will also increase in those countries.
This section begins by comparing the share of LTC migrants across countries before highlighting specific legal channels to recruit foreign care workers in some OECD countries or laws in place to facilitate their recruitment. Whether LTC migrant workers are treated fairly is then investigated.
Migrant workers represent a higher proportion of LTC workers than among all workers. In the OECD on average, 26% of LTC workers are foreign-born compared to 20% across all employment sectors.12 In Israel, over 70% of LTC workers are foreign-born, and around 40% in Luxembourg, Sweden and Switzerland (Figure 4.6). By contrast, this share is below 3% in the Czech Republic. Only in a few countries (Australia, Ireland and Luxembourg) is the share of foreign-born workers higher across all workers than for LTC workers only.

Note: Data are based on ISCO 3‑digit and NACE 2‑digit codes. Data is 2019 for the United Kingdom, 2016 for Australia, Canada, Israel, New Zealand and the United States. Data for the Czech Republic and Slovenia should be treated with caution as they fall below the “b” limit for reliability.
Source: EU-Labour Force Survey; ASEC-CPS for the United States; Census 2016 for Canada; LFS for Israel; OECD estimates based on national sources for Australia and New Zealand.
Over the past decade, there has been a large increase in the employment share of foreign-born workers in the LTC sector in virtually every country for which data is available, with an average increase of more than 5 percentage points of their share in total employment, larger than amongst all workers on average and in particular in Norway and Sweden (Figure 4.7). The increases can at least be partly explained by Bulgaria and especially Romania joining the European Union in 2007 and being granted freedom of movement across all countries in the years thereafter (OECD, 2015[63]). As OECD countries continue to age rapidly, the increasing demand for LTC workers from abroad is likely to be a long-term phenomenon.
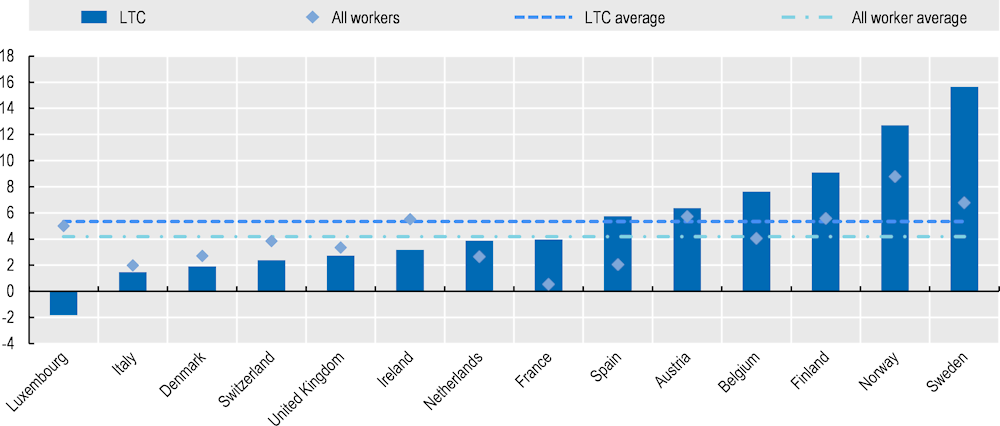
Note: Data are based on ISCO 3‑digit and NACE 2‑digit codes. Data for Finland and France for LTC workers should be treated with caution as they fall below the “b” limit for reliability in 2011 data.
Source: EU-Labour Force Survey.
Migrant workers can help shift the structure of the LTC sector from residence‑based to home‑based services. A recent study in the United States has shown that having a higher proportion of less-educated migrants in the local community decreases the probability of institutionalisation amongst the older population. A 10 percentage point increase in the number of less-educated migrants is estimated to reduce the probability of someone aged 65 or over living in a nursing home or other institution by 29%, and by 26% for those aged 80 or over (Butcher, Moran and Watson, 2022[64]). The study found that areas with higher levels of immigration have lower wages among the less-educated workforce and higher levels of employment of health and nursing aides. This abundance of relatively cheap carers thereby reduces the cost of ageing within the community setting.
There is a clear distinction in the role of LTC migrant workers between countries or even regions of destination. In Northern and Western Europe, the majority of LTC workers are usually employed by specific LTC organisations, therefore having more formal employment provisions. Conversely, in Central and Eastern Europe and in Southern Europe, workers are predominantly hired by the person in need of care or their families (Scheil-Adlung, 2015[65]). In that case, employment is more likely to be informal in nature.
Globally, Southeast Asia is a major origin of immigrants employed in the LTC sector, with some moving to both Japan and Korea as well as many more going further afield to Canada, the United Kingdom and the United States, for example. China is also beginning to supply workers in the LTC sector, particularly in Korea, for example. Parreñas (2015[66]) suggests that low-skilled workers remain within the Asian region in terms of destination countries, whilst those with higher skills migrate intercontinentally.
Many LTC workers are recruited after having migrated and commonly find employment in the informal sector (King-Dejardin, 2019[67]). However, some countries have been proactive in trying to recruit migrant workers to the LTC sector, through various legal channels or less commonly with specific recruitment campaigns. Only five OECD countries, Canada, Germany, Israel, Japan and the United Kingdom, have so far been identified as having specific legal labour migration channels for care workers.
In Canada, the Home Support Worker Pilot (HSWP), launched in 2019, is the latest in a long line of migration schemes covering care workers. HSWP is designed to safeguard against problems associated with the old Live‑in Caregiver Programme (LCP) as applicants now immediately apply for permanent residency. Previously, workers recruited under LCP could only apply for permanent residency after having worked in the programme for two years. Workers were therefore vulnerable to employer abuse, poor working conditions and low wages, with limited opportunity to complain as they were not permitted to work for more than one employer and feared repatriation. For permanent residency, foreign candidates must meet language proficiency requirements in either English or French and have at least one year of Canada‑equivalent post-secondary education. After working 24 out of 36 months in a qualifying adult social care occupation, participants are automatically granted permanent residence.
Germany has a growing need for both health and LTC workers, with ageing leading to a shortage of workers. To help address the employment needs, a specialist agency for skilled labour in health and care occupations, DeFa (Deutsche Fachkräfteagentur für Gesundheits und Pflegeberufe) was established in 2019 to specifically recruit workers from abroad. It is the first point of contact for health and care providers and helps with visa applications and work permits as well as the recognition of professional qualifications and also organises the selection of applicants and offers language courses (Eurofund, 2020[68]).
In Israel, the Foreign Care Worker programme allows those in need, who have obtained a permit from the Ministry of Industry, Trade and Labour, to hire a foreign care worker. International recruitment must occur through a licensed recruitment agency. The permit obtained is temporary (limited to five years or the death of the person cared for, whichever is longer), with no pathway to permanent residence. The cost of employing a foreign care worker is approximately NIS 4 500– NIS 5 500 per month (34%‑42% of average wage). The families are expected to provide an adequate living space for the caregiver, three meals a day and one day off per week. Agreements were signed with Morocco in June 2022 to permit nurses to emigrate to Israel and 2000 workers from Nepal are due to arrive to work in retirement homes. The programme covers over 70 000 workers in Israel, representing about 2% of total employment, but more workers are still needed.
In Japan, there are several schemes allowing foreigners to work as care workers. The Care Work visa route (“Nursing care” Status of Residence) started in 2017. In order to acquire this status, foreign workers must have become certified Care Workers. If they acquire the “Nursing Care” Status of Residence, there is no limit on the number of times they can extend the period of stay, and they can bring their family with them.
There are three other schemes in Japan, two systems and one covering partnership agreements. The two systems are the Specified Skilled Worker System and the Technical Intern Training Programme which cover nursing care work. The third scheme is the Economic Partnership Agreements (EPAs) that have been in place since 2008 with several countries. The first EPA was signed with Indonesia in 2008, followed by the Philippines in 2009 and Viet Nam in 2014 (ERIA, 2022[69]). A component of the agreement permits care workers to work in Japan, but the scheme is limited to just 300 individuals per year from each country. Foreign care workers are required to meet certain requirements such as having a nursing diploma or college degree with being certified as a care giver, be recruited through the Japanese accepting agency (Japan International Corporation of Welfare Services, JICWELS), and be employed only by eligible care facilities. In order to continue to work in Japan after completing the EPA programme, they have to become certified care workers within four years after they started working in Japan and pass a national exam. EPA workers are protected by the Labour Standards Act and guaranteed working conditions at least equivalent to those of Japanese care workers.
The United Kingdom has had to adapt its policy towards LTC workers in recent years. Between January and April 2019, migrants accounted for 5.2% of all new entrants into the LTC sector in the United Kingdom, whereas it was only 1.8% from January to April 2021. Duval et al., (2022[70]) suggest that the pandemic may have accelerated a process already set in motion by “Brexit,” which eliminated free movement for employment from the EU, speeding up the decline in the employment rate of foreigners and contributing to pockets of labour shortages in low-skilled professions, such as care workers. It was virtually impossible for care workers to meet the 70‑points threshold of the points-based immigration system introduced in January 2021, because of both low wages and the low-skilled classification of the job. However, since February 2022, care workers have been added to both the Shortage Occupation List (SOL) and the Health and Care Worker visa programme, meaning that employers can now sponsor employees from abroad to fill vacancies, though there are fees involved with this process, even though they are much lower than for most other sectors (MAC, 2022[71]). Senior care workers have been on the SOL since inception in December 2020 and on the visa programme since January 2021. Being added to these programmes has resulted in over 23 000 applications (95% granted) for senior care workers and over 40 000 for care workers or home carers (86% granted) in 2022, with health and care visa applications nearly 150% higher than in 2021.
LTC workers may be eligible to use general labour migration channels. In a number of countries recruitment of LTC workers from abroad is exempt from labour market tests as they appear on the list of occupations identified as having labour market shortages (OECD, 2020[56]). In Korea, an ancestry-based mixed migration route – the H‑2 Working Visit Permit for ethnic Koreans whose ancestors emigrated or were deported to foreign countries, mostly China, before 1945 – has served as the main route for the recruitment of foreign workers into adult social care roles. The Working Visit Permit allows a pathway to permanent residence.
Other OECD countries, including Australia and New Zealand have had routes for adult social care workers through their general employment migration schemes. All of these schemes have become more selective over time and now generally apply only to highly skilled occupational sectors, whilst most care jobs are classified as low skilled. Yet, in Australia there is a Carer Visa category which lets individuals live in Australia permanently and provide care for their relatives who are suffering from a long-term or permanent medical condition. Also, there are some agreements with the LTC sector which allow aged care facilities to sponsor foreign-born individuals with the required skills to care for the elderly, even though the occupation of the aged care workers is not on the list of eligible occupations.
The European Care strategy has called for more co‑ordinated efforts to recruit foreign LTC workers through the proposed action “Map the current admission conditions and rights of long-term care workers from non-EU countries and explore the feasibility of developing EU-level schemes to attract care workers” (European Commission, 2022[72]). In addition, the strategy is also concerned about the working conditions with the action “Review the application of EU standards governing working conditions”. Legislation for fair working conditions is set out in both the European Pillar of Social Rights and the Charter of Fundamental Rights of the European Union. Under these legislations workers are guaranteed a maximum regular working week of 48 hours with guaranteed rest and break periods and extra protection for night work. Member States though have the option to opt out of these rules for specific categories of workers or employment sectors. Individual employees can also opt out of the maximum working hours as long as it is a free choice without pressure from employers. This section now turns to examine the overall treatment and working conditions for migrant LTC workers.
Migrant workers represent a large proportion of live‑in care workers (Figure 4.8). In Italy, Spain and Switzerland, more than half of live‑in carers are foreign-born, a much higher share than in residential or non-residential care. However, reliable data on personal care workers in live‑in care positions are scarce as sample sizes are small; such statistics are available for only eight countries. The actual number of live‑in foreign-born personal care workers is likely to be higher than what is reported as migrant workers are less likely to participate in data collection, due to, for example, undeclared work.
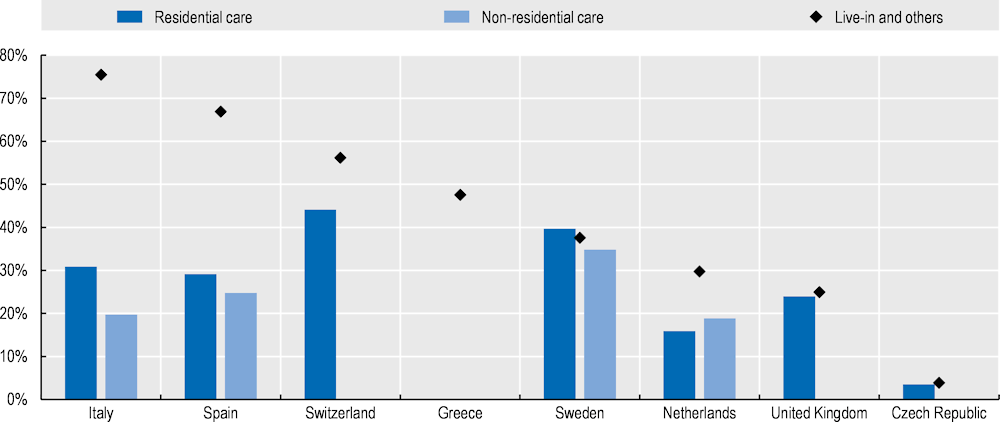
Note: Data are based on ISCO 3‑digit code 532, representing “Personal Care Workers in Health Services”. Live‑in and others excludes NACE codes 38, 55, 56, 84‑88 and 96 (see EUROPA – Competition – List of NACE codes, https://ec.europa.eu/competition/mergers/cases/index/nace_all.html). Data for “Live‑in and others” in the Netherlands, Sweden, Switzerland and the United Kingdom should be treated with caution as they fall below the “b” limit for reliability, meaning that the sample size is small.
Source: EU Labour Force Survey.
In countries with widespread live‑in caregiver programmes, individuals can more easily remain in their own home benefitting from 24‑hour on-call personalised support for routine activities and health-related needs. However, in most cases, having 24‑hour in-home support is unaffordable and is only possible because care workers have to work much longer hours without additional payments for this overtime (Horn et al., 2019[73]).
There is a lower level of labour regulation and a lower – if any – frequency of labour inspections for in-home care compared with other employment settings and sectors. Exploitation of workers can be more commonplace when permission to remain in the country is dependent on remaining with their employer (Arat-Koç, 2001[74]). This employment precariousness and isolation, as well as risks of having to leave the country, makes undeclared LTC workers more vulnerable to physical and sexual abuse.
One‑third of domestic workers working in private households globally, a group which includes live‑in care workers, are completely excluded from employment legislation (King-Dejardin, 2019[67]). Furthermore, even when legislation is introduced to protect care workers, the rules covering those privately employed are typically less favourable or even non applicable to them. For example, in the United States, under the 2013 Department of Labour regulations, individuals employed as a live‑in carer are not covered by federal overtime protection when they are privately paid (Goldberg, 2015[75]).
In Israel, many employment laws do not cover foreign workers who are employed as live‑in care providers; 87% of Israel’s elderly who are eligible for LTC benefits live in the community (Hasson and Buzaglo, 2019[76]). As foreign workers are living in the same home, they are effectively on call 24 hours a day. However, their working hours are not regulated by law with labour courts having ruled that Israel’s Work and Rest Hours Law does not apply to them, though they are entitled to 25 hours a week of rest (Hasson and Buzaglo, 2019[76]).
In Germany, the Federal Labour Court issued a judgement in June 2021 stating that the minimum wage needs to be paid for not only the hours working, but also for those hours effectively on call. Therefore, someone ensuring live‑in care overnight, for example, should now be paid for the hours spent in the home overnight, even if no direct care is actually provided.
Many OECD countries have had immigration arrangements with a particular country to cover their employment shortages across numerous sectors, but the supplier country can change over time. For example, until the early 2000s foreign LTC workers in Japan and Korea came mainly from the Philippines, while Indonesia and Viet Nam have now become the main countries of supply as these workers tend to be cheaper to employ (Peng, 2017[77]).
Within international labour laws, there are mechanisms to protect migrant workers and give them the same rights as the national population. However, within the LTC sector only 13 OECD countries (35 countries worldwide) have ratified ILO Convention 189, which provides standards for decent working conditions of domestic workers, including live‑in carers. Non-ratification of Convention 189 does not imply that countries are not pursuing alternative routes to better protect domestic workers, but adopting it is a recommendation of the recent European Care Strategy. As migrant workers often represent a significant proportion of the workforce in these sectors, they often work either as undeclared or as false self-employed and have very low wages. They are sometimes denied basic labour rights, such as adequate rest periods (European Commission, 2022[78]).
Improving the working conditions of migrant care workers is therefore a key issue to address. Introducing training programmes to make the adaption to the destination country easier is an option as has been done with language courses in Japan. Alternatively, countries could make applications for permanent residency more straightforward, as in Canada.
The analysis presented in Chapter 2 found no significant difference in the level of wages between migrant workers and those born in the country having similar individual characteristics. However, this covers only formal workers within the LTC sector, whereas many migrant workers, particularly those providing in-home care are in the informal economy (King-Dejardin, 2019[67]). The disadvantages faced by undeclared migrant workers in the LTC sector highlighted above extend to lower earnings (Doyle and Virpi, 2009[79]; Jönson and Giertz, 2013[80]). Home‑care positions are often less well paid than institutional employment and commonly not fully covered by employment legislation.
When looking more globally and including undeclared workers, migrant LTC workers are predominantly low-paid, middle‑aged women, with qualifications often higher than is strictly necessary for the job (ILO, 2013[81]). In Canada, for example, foreign workers account for a large proportion of home‑care providers. Many are qualified as nurses in their country of origin with higher education degrees in healthcare, but they cannot work as nurses in Canada due to issues with recognising their qualifications; over 40% of those starting employment among home childcare providers and home support workers are overqualified (CBOC, 2021[82]). In most European countries, the share of migrants reporting that they are overqualified for the work they do is greater in the LTC sector than in the overall economy (OECD, 2020[56]). Removing overqualified foreign nurses from less-developed countries raises ethical concerns when some of these countries also face population ageing challenges (Kotschy and Bloom, 2022[83]).
[6] Aparicio, M. et al. (2019), “Gratitude between patients and their families and health professionals: A scoping review”, Journal of Nursing Management, Vol. 27/2, pp. 286-300, https://doi.org/10.1111/jonm.12670.
[74] Arat-Koç, S. (2001), Caregivers Break the Silence: A Participatory Action Research on the Abuse and Violence, Including the Impact of Family Separation, Experienced by Women in the Live-In Caregiver Program, Intercede, Toronto.
[25] Atanackovic, J. and I. Bourgeault (2013), “The Employment and Recruitment of Immigrant Care Workers in Canada”, Canadian Public Policy / Analyse de Politiques, Vol. 39/2, pp. 335-350, https://www.jstor.org/stable/23594748.
[1] Austen, S. et al. (2016), “Recognition: applications in aged care work”, Cambridge Journal of Economics, Vol. 40/4, pp. 1037-1054, https://doi.org/10.1093/cje/bev057.
[4] Bailly, F., F. Devetter and F. Horn (2013), “Can working and employment conditions in the personal services sector be improved?”, Cambridge Journal of Economics, Vol. 37/2, pp. 299-321, https://doi.org/10.1093/cje/bes071.
[3] Baret, C., I. Recotillet and C. Kornig (2021), “Which characteristics of working conditions affect employee recognition? Case study of a French teaching hospital”, Communication at the 20th EURAM conference, Dublin, Ireland, December 4-6, 2020, https://halshs.archives-ouvertes.fr/halshs-03213237.
[12] Barry, U. and C. Jennings (2021), “Gender equality: Economic value of care from the perspective of the applicable EU funds”, Study, No. PE 694.784, European Parliament, Policy Department for Citizens’ Rights and Constitutional Affairs, Brussels.
[61] BBC, R. (2015), More male care workers needed, says providers’ chief, BBC, https://www.bbc.com/news/uk-34103302.
[28] Brekke, K. and K. Nyborg (2010), “Selfish bakers, caring nurses? A model of work motivation”, Journal of Economic Behavior & Organization, Vol. 75/3, pp. 377-394, https://doi.org/10.1016/j.jebo.2010.05.008.
[55] Burbano, V., N. Padilla and S. Meier (2020), Gender Differences in Preferences for Meaning at Work, IZA Discussion Papers, No. 13053, Institute of Labour Economics (IZA), Bonn, https://www.econstor.eu/bitstream/10419/216365/1/dp13053.pdf.
[64] Butcher, K., K. Moran and T. Watson (2022), “Immigrant labor and the institutionalization of the U.S.‐born elderly”, Review of International Economics, Vol. 30/5, pp. 1375-1413, https://doi.org/10.1111/roie.12607.
[82] CBOC (2021), Valued workers, valuable work: The current and future role of (im)migrant talent, The Conference Board of Canada, https://www.conferenceboard.ca/temp/bef358cd-1f54-4438-aac7-c668645a2042/11354_impact-paper_valued-workers_immigrant-talent.pdf.
[84] Cohen, R. (2016), What Programming’s Past Reveals About Today’s Gender-Pay Gap, The Atlantic, https://www.theatlantic.com/business/archive/2016/09/what-programmings-past-reveals-about-todays-gender-pay-gap/498797/.
[21] Cools, S., H. Finseraas and M. Bergli Rasmussen (2020), “The Immigrant‐Native Gap in Union Membership: A Question of Time, Sorting, or Culture?”, LABOUR, Vol. 35/1, pp. 24-51, https://doi.org/10.1111/labr.12186.
[7] Day, G. et al. (2021), “An outbreak of appreciation: A discursive analysis of tweets of gratitude expressed to the National Health Service at the outset of the COVID‐19 pandemic”, Health Expectations, Vol. 25/1, pp. 149-162, https://doi.org/10.1111/hex.13359.
[19] De Tavernier, W. and V. Draulans (2018), “Negotiating informal elder care, migration and exclusion: the case of a Turkish immigrant community in Belgium”, International Journal of Ageing and Later Life, Vol. 12/2, pp. 89-117, https://doi.org/10.3384/ijal.1652-8670.18404.
[60] Delfino, A. (2021), Breaking Gender Barriers: Experimental Evidence on Men in Pink-Collar Jobs, IZA Institute of Labour Economics, https://docs.iza.org/dp14083.pdf.
[39] Denny-Brown, N. et al. (2020), COVID-19 intensifies nursing home workforce challenges, Mathematica, Cambridge, MA, http://resource.nlm.nih.gov/101775124.
[43] Dewan, S. and R. Gebeloff (2012), More Men Enter Fields Dominated by Women, New York Times, https://www.nytimes.com/2012/05/21/business/increasingly-men-seek-success-in-jobs-dominated-by-women.html.
[37] Dill, J., R. Erickson and J. Diefendorff (2016), “Motivation in caring labor: Implications for the well-being and employment outcomes of nurses”, Social Science & Medicine, Vol. 167, pp. 99-106, https://doi.org/10.1016/j.socscimed.2016.07.028.
[79] Doyle, M. and T. Virpi (2009), “The different faces of care work: understanding the experiences of the multi-cultural care workforce”, Ageing and Society, Vol. 29/3, pp. 337-350, https://doi.org/10.1017/s0144686x08007708.
[70] Duval, R. et al. (2022), Labor Market Tightness in Advanced Economies, International Monetary Fund, https://www.imf.org/-/media/Files/Publications/SDN/2022/English/SDNEA2022001.ashx.
[2] Elstad, J. and M. Vabø (2021), “Lack of recognition at the societal level heightens turnover considerations among Nordic eldercare workers: a quantitative analysis of survey data”, BMC Health Services Research, Vol. 21/1, https://doi.org/10.1186/s12913-021-06734-4.
[15] England, P., M. Budig and N. Folbre (2002), “Wages of Virtue: The Relative Pay of Care Work”, Social Problems, Vol. 49/4, pp. 455-473, https://doi.org/10.1525/sp.2002.49.4.455.
[16] England, P. and N. Folbre (1999), “The Cost of Caring”, The Annals of the American Academy of Political and Social Science, Vol. 561, pp. 39-51, https://doi.org/10.1177/000271629956100103.
[68] Eurofund (2020), Long-term care workforce: Employment and working conditions, Publications Office of the European Union, Luxembourg.
[72] European Commission (2022), European Care Strategy, European Commission, https://www.alzheimer-europe.org/news/european-commission-launches-european-care-strategy.
[78] European Commission (2022), SWD(2022) 440 final, European Commission, https://ec.europa.eu/info/law/better-regulation/have-your-say/initiatives/13298-European-care-strategy_en.
[32] Fedele, A. (2018), “Well-paid nurses are good nurses”, Health Economics, Vol. 27/4, pp. 663-674, https://doi.org/10.1002/hec.3623.
[14] Folbre, N. (1995), ““Holding hands at midnight”: The paradox of caring labor”, Feminist Economics, Vol. 1/1, pp. 73-92, https://doi.org/10.1080/714042215.
[35] Folbre, N. and J. Nelson (2000), “For Love or Money—Or Both?”, Journal of Economic Perspectives, Vol. 14/4, pp. 123-140, https://doi.org/10.1257/jep.14.4.123.
[30] Franzosa, E. and E. Tsui (2020), “Professional, friend or family? How home care companies sell emotional care”, Journal of Women & Aging, Vol. 32/4, pp. 440-461, https://doi.org/10.1080/08952841.2020.1763894.
[10] Fraser, N. (1997), Justice Interruptus: Critical Reflections on the “Postsocialist” Condition, Routledge, New York.
[41] Fujisawa, R. and F. Colombo (2009), “The Long-Term Care Workforce: Overview and Strategies to Adapt Supply to a Growing Demand”, OECD Health Working Papers, No. 44, OECD Publishing, Paris, https://doi.org/10.1787/225350638472.
[18] García-Mainar, I., V. Montuenga and G. García-Martín (2018), “Occupational Prestige and Gender-Occupational Segregation”, Work, Employment and Society, Vol. 32/2, pp. 348-367, https://doi.org/10.1177/0950017017730528.
[59] Glassdoor (2021), What Job Seekers Really Think About Your Diversity and Inclusion Stats, https://www.glassdoor.com/employers/blog/diversity/.
[75] Goldberg, H. (2015), “The long journey home: The contested exclusion and inclusion of domestic workers from federal wage and hour protections in the United States, Conditions of Work and Employment Series No. 58”, Conditions of Work and Employment Series, No. 58, Inernational Labour Office, Geneva, https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---travail/documents/publication/wcms_396235.pdf.
[54] Greenberg, D. et al. (2022), “Sex and age differences in “theory of mind” across 57 countries using the English version of the “Reading the Mind in the Eyes” Test”, Proceedings of the National Academy of Sciences, Vol. 120/1, https://doi.org/10.1073/pnas.2022385119.
[44] Harris, J. (2022), “Do wages fall when women enter an occupation?”, Labour Economics, Vol. 74, p. 102102, https://doi.org/10.1016/j.labeco.2021.102102.
[76] Hasson, Y. and N. Buzaglo (2019), The care deficit in Israel: What it means and how it can be reduced, Adva Center, https://adva.org/en/care-deficit/.
[51] Hay, K. et al. (2019), “Disrupting gender norms in health systems: making the case for change”, The Lancet, Vol. 393/10190, pp. 2535-2549, https://doi.org/10.1016/s0140-6736(19)30648-8.
[31] Hebson, G., J. Rubery and D. Grimshaw (2015), “Rethinking job satisfaction in care work: looking beyond the care debates”, Work, Employment and Society, Vol. 29/2, pp. 314-330, https://doi.org/10.1177/0950017014556412.
[33] Heponiemi, T. et al. (2011), “The effects of ownership, staffing level and organisational justice on nurse commitment, involvement, and satisfaction: A questionnaire study”, International Journal of Nursing Studies, Vol. 48/12, pp. 1551-1561, https://doi.org/10.1016/j.ijnurstu.2011.05.015.
[29] Heyes, A. (2005), “The economics of vocation or ‘why is a badly paid nurse a good nurse’?”, Journal of Health Economics, Vol. 24/3, pp. 561-569, https://doi.org/10.1016/j.jhealeco.2004.09.002.
[73] Horn, V. et al. (2019), “Live-in migrant care worker arrangements in Germany and the Netherlands: motivations and justifications in family decision-making”, International Journal of Ageing and Later Life, Vol. 13/2, pp. 83-113, https://doi.org/10.3384/ijal.1652-8670.18410.
[42] Hussein, S., M. Ismail and J. Manthorpe (2014), “Male workers in the female-dominated long-term care sector: evidence from England”, Journal of Gender Studies, Vol. 25/1, pp. 35-49, https://doi.org/10.1080/09589236.2014.887001.
[13] ILO (2018), Care work and care jobs for the future of decent work, International Labour Office, Geneva, https://www.ilo.org/global/publications/books/WCMS_633135.
[81] ILO (2013), Domestic Workers Across the World: Global and Regional Statistics and Extent of Legal Protection, International Labour Office, Geneva, https://www.ilo.org/global/publications/books/WCMS_173363/lang--en/index.htm.
[24] IOM (2010), The Role of Migrant Care Workers in Ageing Societies: Report on Research Findings in the United Kingdom, Ireland, Canada and the United States, International Organization for Migration, Geneva, https://publications.iom.int/system/files/pdf/mrs41.pdf.
[80] Jönson, H. and A. Giertz (2013), “Migrant Care Workers in Swedish Elderly and Disability Care: Are They Disadvantaged?”, Journal of Ethnic and Migration Studies, Vol. 39/5, pp. 809-825, https://doi.org/10.1080/1369183x.2013.756686.
[67] King-Dejardin, A. (2019), The social construction of migrant care work: At the intersection of care, migration and gender, International Labour Organization, https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---migrant/documents/publication/wcms_674622.pdf.
[83] Kotschy, R. and D. Bloom (2022), A comparative perspective onlong-term care systems, National Bureau of Economic Research, https://www.nber.org/system/files/working_papers/w29951/w29951.pdf.
[22] Kranendonk, M. and P. de Beer (2016), “What Explains the Union Membership Gap between Migrants and Natives?”, British Journal of Industrial Relations, Vol. 54/4, pp. 846-869, https://doi.org/10.1111/bjir.12192.
[17] Le Bihan, B. and A. Sopadzhiyan (2018), “The development of an ambiguous care work sector in France”, in Christensen, K. and D. Pilling (eds.), The Routledge Handbook of Social Care Work Around the World, Routledge, Abingdon, https://doi.org/10.4324/9781315612805-8.
[71] MAC (2022), Adult Social Care and Immigration: A Report from the Migration Advisory Committee, Her Majesty’s Stationery Office, https://www.gov.uk/government/publications/review-of-adult-social-care-2022.
[8] Magnusson, C. (2009), “Gender, Occupational Prestige, and Wages: A Test of Devaluation Theory”, European Sociological Review, Vol. 25/1, pp. 87-101, https://doi.org/10.1093/esr/jcn035.
[5] Manthorpe, J. et al. (2017), “Doing, Being and Becoming a Valued Care Worker: User and Family Carer Views”, Ethics and Social Welfare, Vol. 11/1, pp. 79-91, https://doi.org/10.1080/17496535.2016.1247904.
[53] Marianne, B. (2011), “New Perspectives on Gender”, in Handbook of Labor Economics, Elsevier, https://doi.org/10.1016/s0169-7218(11)02415-4.
[47] Mas, A. and A. Pallais (2017), “Valuing Alternative Work Arrangements”, American Economic Review, Vol. 107/12, pp. 3722-3759, https://doi.org/10.1257/aer.20161500.
[85] Mavromaras, K. et al. (2017), The Aged Care Workforce, 2016, Australian Government Department of Health, https://gen-agedcaredata.gov.au/www_aihwgen/media/Workforce/The-Aged-Care-Workforce-2016.pdf.
[26] Näre, L. (2013), “Ideal Workers and Suspects: Employers’ Politics of Recognition and the Migrant Division of Care Labour in Finland”, Nordic Journal of Migration Research, Vol. 3/2, p. 72, https://doi.org/10.2478/v10202-012-0017-5.
[36] Nelson, J. and N. Folbre (2006), “Why a well-paid nurse is a better nurse”, Nursing Economics, Vol. 24/3, pp. 127-130, https://pubmed.ncbi.nlm.nih.gov/16786826/.
[62] Nordregio (2021), Recruitment and retention in the welfare sector: Nordic good practice, Nordregio, https://doi.org/10.6027/pb2021:1.2001-3876.
[11] OECD (2021), Bringing Household Services Out of the Shadows: Formalising Non-Care Work in and Around the House, Gender Equality at Work, OECD Publishing, Paris, https://doi.org/10.1787/fbea8f6e-en.
[46] OECD (2021), Pay Transparency Tools to Close the Gender Wage Gap, Gender Equality at Work, OECD Publishing, Paris, https://doi.org/10.1787/eba5b91d-en.
[56] OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/92c0ef68-en.
[9] OECD (2019), Good Practice for Good Jobs in Early Childhood Education and Care, OECD Publishing, Paris, https://doi.org/10.1787/64562be6-en.
[48] OECD (2019), Part-time and Partly Equal: Gender and Work in the Netherlands, Gender Equality at Work, OECD Publishing, Paris, https://doi.org/10.1787/204235cf-en.
[52] OECD (2019), Why you should care about unpaid care work, Development Matters, OECD, Paris, https://oecd-development-matters.org/2019/03/18/why-you-should-care-about-unpaid-care-work.
[20] OECD (2018), The Future of Social Protection: What Works for Non-standard Workers?, OECD Publishing, Paris, https://doi.org/10.1787/9789264306943-en.
[23] OECD (2017), Making Integration Work: Assessment and Recognition of Foreign Qualifications, Making Integration Work, OECD Publishing, Paris, https://doi.org/10.1787/9789264278271-en.
[50] OECD (2017), The Pursuit of Gender Equality: An Uphill Battle, OECD Publishing, Paris, https://doi.org/10.1787/9789264281318-en.
[63] OECD (2015), International Migration Outlook 2015, OECD Publishing, Paris, https://doi.org/10.1787/migr_outlook-2015-en.
[57] OECD (2008), “Gender and Sustainable Development: Maximising the economic, social and environmental role of women”, OECD, Paris, https://www.oecd.org/greengrowth/40881538.pdf.
[27] Palmer, E. and J. Eveline (2012), “Sustaining Low Pay in Aged Care Work”, Gender, Work & Organization, Vol. 19/3, pp. 254-275, https://doi.org/10.1111/j.1468-0432.2010.00512.x.
[66] Parreñas, R. (2015), Servants of Globalization, Stanford University Press, https://doi.org/10.1515/9780804796187.
[77] Peng, I. (2017), Elderly Care Work and Migration: East and Southeast Asian Contexts, https://www.un.org/development/desa/ageing/wp-content/uploads/sites/24/2017/11/Peng-UN-Expert-Group-Meeting_Dec-5-7-final-Paper_4Dec.pdf.
[38] Royal Commission into Aged Care Quality and Safety (2020), Royal Commission into Aged Care Quality and Safety Council Assisting’s Final Submissions, https://agedcare.royalcommission.gov.au/sites/default/files/2021-02/RCD.9999.0541.0001_1.docx.
[65] Scheil-Adlung, X. (2015), Extension of Social Security, Long-term care protection for older persons: A review of coverage deficits in 46 countries, ILO, https://www.social-protection.org/gimi/RessourcePDF.action?id=53175.
[49] Seehuus, S. (2021), “Gender differences and similarities in work preferences: Results from a factorial survey experiment”, Acta Sociologica, p. 000169932110602, https://doi.org/10.1177/00016993211060241.
[34] Sulander, J. et al. (2016), “Does Organizational Justice Modify the Association Between Job Involvement and Retirement Intentions of Nurses in Finland?”, Research in Nursing & Health, Vol. 39/5, pp. 364-374, https://doi.org/10.1002/nur.21740.
[40] Tyler, D. et al. (2021), COVID-19 intensifies home care workforce challenges, RTI International, https://aspe.hhs.gov/reports/covid-19-intensifies-home-care-workforce-challenges.
[58] WGEA, W. (2022), What is workplace gender equality?, Australian Government, https://www.wgea.gov.au/about/workplace-gender-equality.
[45] WHO/ILO (2022), The gender pay gap in the health and care sector: A global analysis in the time of COVID-19, World Health Organisation, https://apps.who.int/iris/handle/10665/358057.
[69] Yuko O. Hirano, O. (ed.) (2022), Agents of Care Technology Transfer, Trends and Challenges of Migration Care Workers Across Borders, https://www.eria.org/publications/agents-of-care-technology-transfer-trends-and-challenges-of-migration-care-workers-across-borders/.
← 1. Another study found that Australian LTC workers are generally rather satisfied with the support they receive from their supervisors (Mavromaras et al., 2017[85]), although receiving support does not necessarily entail being recognised.
← 2. Healthcare workers in one French hospital felt to some extent recognised by patients, co-workers and supervisors, but felt very little recognition from management (Baret, Recotillet and Kornig, 2021[3]).
← 3. Occupational standing is measured through survey research in which people are asked how prestigious they consider a specific occupation to be. The findings are very stable over time and across countries.
← 4. Municipalities are free to set wages of LTC workers, albeit within the boundaries set by the law and government regulations. While previously no specific minimum wage existed for LTC workers, occupation-specific minimum wages were introduced in 2022 and will fully take effect as of 2027. The maximum wage for LTC workers set by the law was substantially increased, by 50% to 80% depending on the specific occupation and connected responsibilities. At the same time, a target wage for average LTC workers was introduced, which exceeds the previous maximum wage for all LTC occupations.
← 5. Canada has a list of “essential services and functions” which comprises services and functions that are critical to ensure the health, safety, and economic well-being of the population.
← 6. This applies if the evaluation of prior work experience demonstrates that all the required competencies have been acquired.
← 7. This is consistent with Figure 4.1 based on a different dataset.
← 8. 22 out of a total of 43.
← 9. Likewise, there is other evidence suggesting that when men start to enter an occupation both the perception of the job and the remuneration improve. For, example, the initial programmers in the computing industry were women in the 1970s, when wages were generally low. According to Cohen (2016[84]), over the last 50 years it has now become a predominantly male profession with both compensation and esteem having risen substantially.
← 10. One country responded that it has somewhat worsened.
← 11. Employers are more likely to recruit women because of perceived empathy (pull), which also draws women towards a career that provides help to individuals (push).
← 12. LTC workers are identified in the Labour Force Survey data based on NACE classification codes 87 and 88 (see Chapter 2).