This annex outlines the process of developing the conceptual framework for the Estonian HSPA, including consecutive refinements to the core structure, visualisation, areas, and domains of the framework. The definition of each of the 18 domains in the HSPA is provided alongside a visualisation of the final HSPA framework for Estonia.
Health System Performance Assessment Framework for Estonia
Annex A. Development process of the Estonian HSPA framework
International expertise and best practices
The determined scope and purpose of a national HSPA provides guidance on defining domains and indicators that will be used to populate the HSPA framework. In international practice, common functions relate to accountability and monitoring of performance, evaluation of policies and strategy development, assessment of specific sectors or programs, and providing a platform for accountability to the government or general public. Together, these objectives balance reporting and assessment with learning and improvement functions. Figure A A.1 outlines most common domains that have been used frequently in existing HSPA frameworks in the European region.
Figure A A.1. Examples of common domains used in HSPA frameworks in Europe
Source: (Fekri, Macarayan and Klazinga, 2018[8]), Health system performance assessment in the WHO European Region: which domains and indicators have been used by Member States for its measurement?, https://apps.who.int/iris/bitstream/handle/10665/326260/9789289053044-eng.pdf?sequence=3&isAllowed=y.
The consultative process of developing a shared HSPA framework
HSPA framework development workshops
Having reached a consensus on the scope and purpose of the Estonian HSPA in winter 2022, HSPA framework development workshops were held on 24‑25 May 2022 in Tallinn. More than 30 participants representing key governmental institutions as well as external stakeholders came together to establish the framework structure and begin to identify indicators that would be used in measuring key domains of the Estonian HSPA. The OECD team was also in person in Tallinn. Following a summary of international approaches to HSPA domain definition, participants were asked to write down 4‑8 potential themes to be addressed in the HSPA on separate post-it notes in the colour corresponding to their organisation. Workshop participants then added their post-it notes to posters identifying broad areas of potential domains. In total, 111 themes were identified (see Figure A A.2).
Figure A A.2. 111 potential themes identified via the HSPA consensus building process
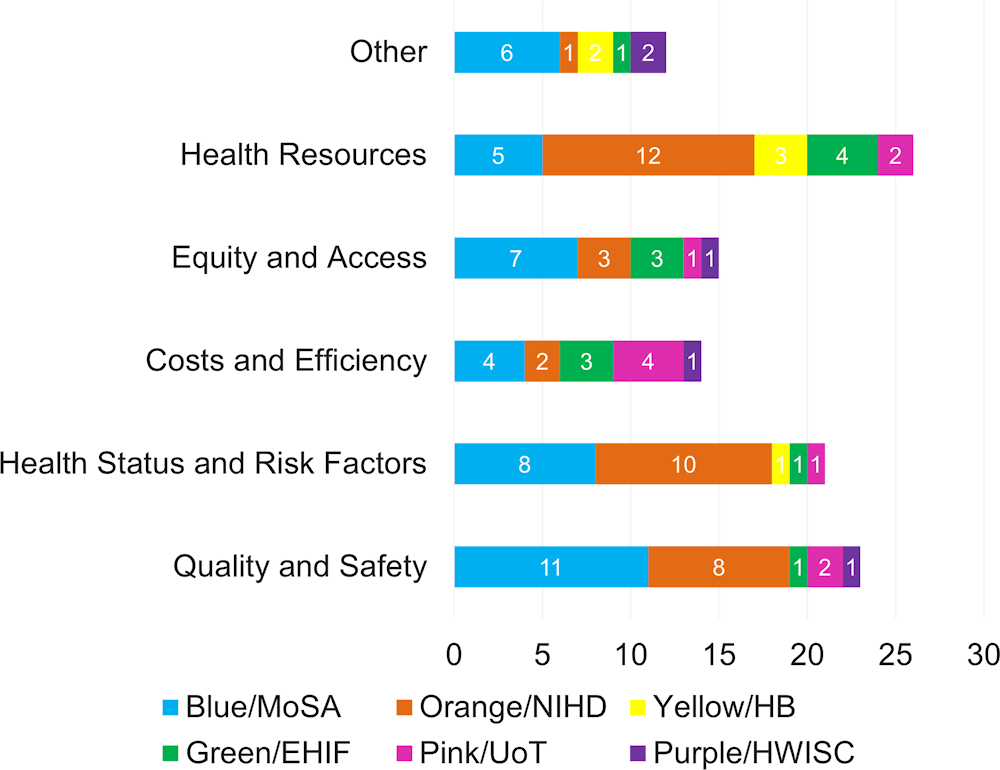
Source: The Estonian HSPA framework project, May 2022.
Following the exercise to generate themes, participants of the workshop took part in moderated sessions to summarise the post-it notes and identify common themes, while clarifying any ambiguous or unclear notes. The consolidation process aligned the 111 proposed domains into 22 cohesive themes. In order to prioritise the themes for representation in the HSPA, participants assigned allocated votes to themes they considered most important. Votes were given to 16 of the 22 themes. Notably, the top five themes encompassed access, data and digitalisation, health literacy, resilience, and quality (see Figure A A.3).
Figure A A.3. Results of the voting process on the importance of each of the 22 themes
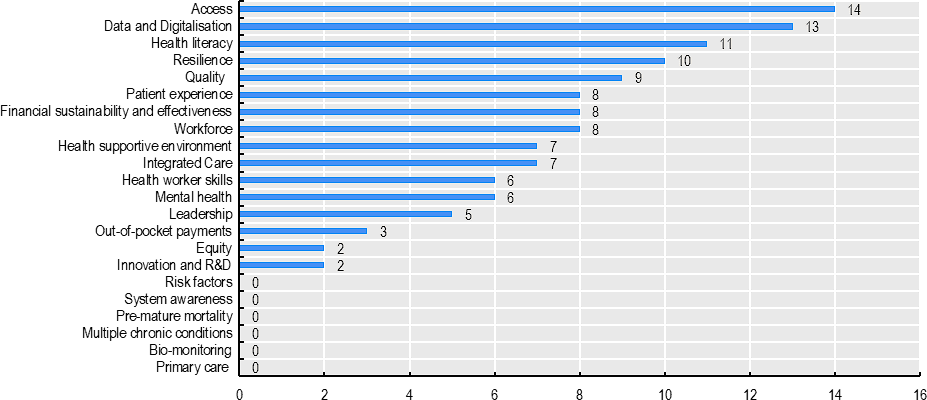
Source: The Estonian HSPA framework project, May 2022.
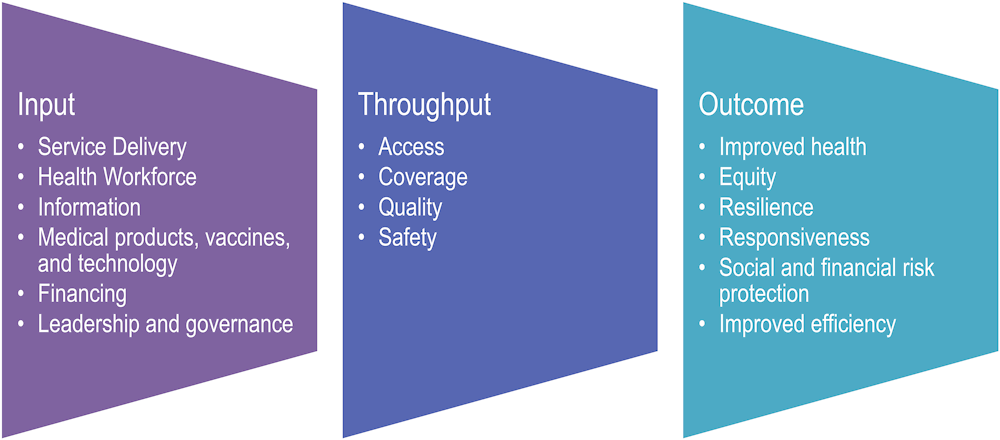
After the voting exercise, the domains were organised into an initial draft framework by the project management team. Themes were cross-referenced between the previous Estonian HSPA framework (see Figure A A.4) as well as the Avedis Donabedian model for assessing care quality (Donabedian, 1966[9]). The draft framework was then presented to workshop participants for validation and feedback. Following the incorporation of comments from the working group participants, the draft framework was revised to the version presented in Figure A A.5.
Figure A A.4. The 2009 Framework for assessing health system performance in Estonia
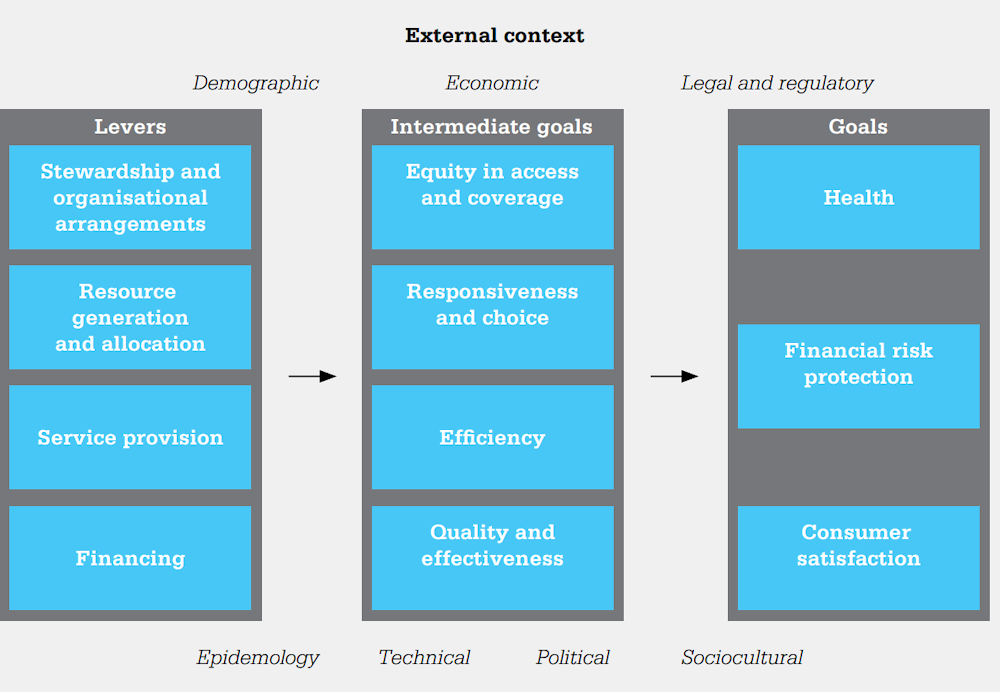
Source: (World Health Organization, 2010[1]), Estonia Health System Performance Assessment: 2009 Snapshot, https://www.sm.ee/sites/default/files/content-editors/Ministeerium_kontaktid/Uuringu_ja_analuusid/Tervisevaldkond/estonia_hspa.pdf.
Figure A A.5. Draft Estonian HSPA framework developed during the May 2022 HSPA development workshops
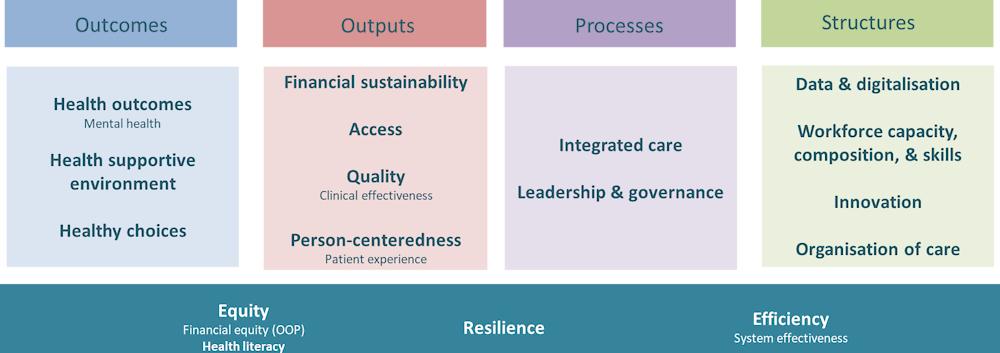
Source: The Estonian HSPA framework project, May 2022.
Further refinements to the HSPA framework
The structure and format of the initial draft were revised in winter 2022‑23 (see Figure A A.6). This iteration included 5 indicator areas and 17 domains. Indicator areas remained the same as in the initial framework, but some domains were reorganised. Notably, health literacy was moved from the cross-cutting area to the outcomes area. Structures area got one new domain called organisation of care. Cross-cutting area was reduced to three domains: equity, resilience, and efficiency.
The new visualisation aimed to emphasise interaction and flow between the themes instead of the initial draft with separate standing pillars. Therefore, areas were presented in a circular arrangement and arrows to show interaction were added. The cross-cutting indicator area was highlighted more as an influence on all other indicator areas.
Figure A A.6. Second working draft of the Estonian HSPA Framework
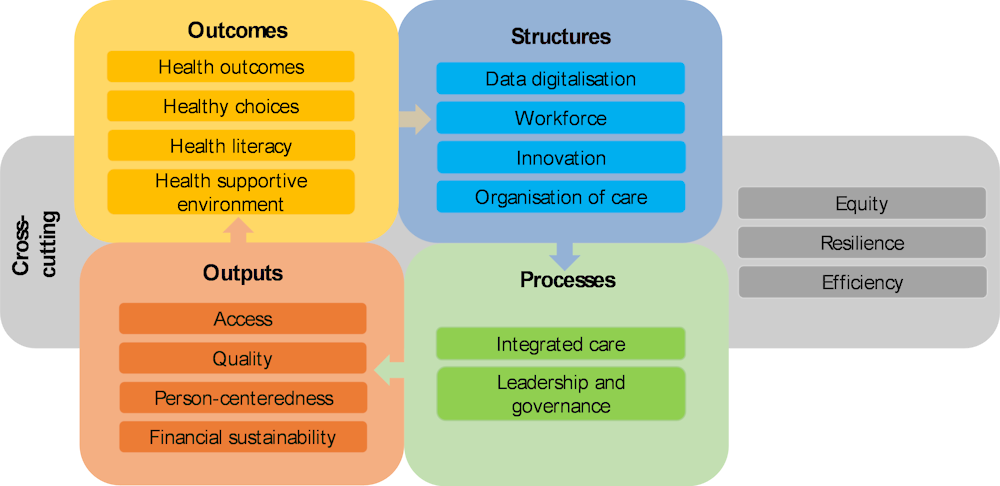
Source: The Estonian HSPA framework project, December 2022.
Simultaneously, a core working group led by MoSA met regularly to work on the input from the working group, advisory board, and other relevant experts. The members of this core working group were representatives of NIHD and EHIF. They worked to refine the framework and choose possible indicators derived from the suggestions from various experts. The group suggested a significant modification to the framework by merging the areas of outcomes and outputs due to a lack of clear distinction between these two concepts in the Estonian language. Consequently, some domains were rearranged between the indicator areas (e.g. financing from the outputs to structures cluster; health literacy and person-centredness to processes etc.). Organisation of care was renamed as health infrastructure. Furthermore, mental health, initially treated as a separate domain, was divided between different areas to ensure the framework follows a more coherent structure while maintaining emphasis on its importance.
Following the merge, the final visualisation of the HSPA framework was modified to display 18 domains in total: 14 domains are grouped by the key indicator areas of processes, outcomes, and structures as a circle. The domain of health status, highlighting the people in the centre of the visualisation, is placed in the centre of the circle while 3 cross-cutting domains of equity, resilience and efficiency encircle the visual. The final visualisation highlights the main policy direction of the Estonian health system to become more person-centred, and embeds equity, efficiency, and resilience into all domains.
Figure A A.7. The final Estonian HSPA framework
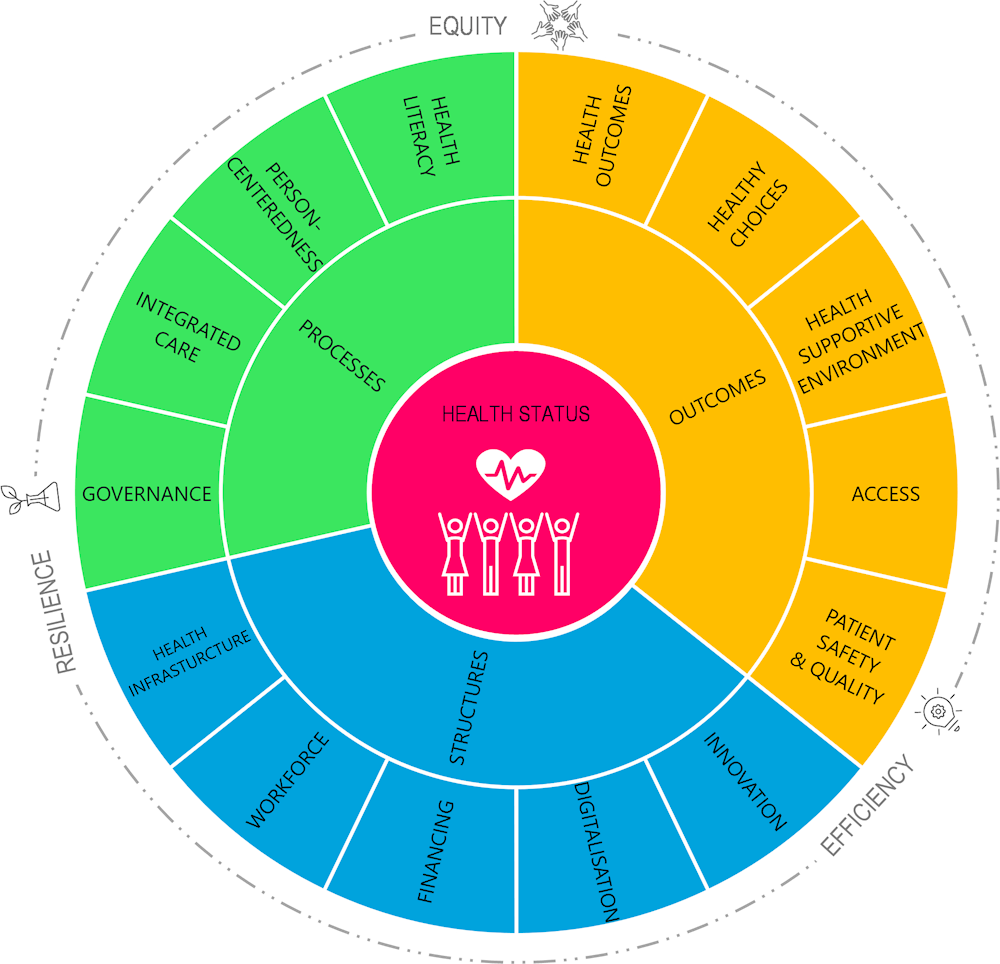
Source: The Estonian HSPA framework project, April 2023.
Description of the Estonian HSPA framework domains
Health Status – the state of health of a person or population assessed by subjective or objective indicators – healthy life expectancy, life expectancy and self-reported health status.
Health Outcomes – describes changes in well-being, morbidity, and mortality (health status) that result from health behaviour, provision of healthcare or other health services.
Healthy Choices – describes health risk factors (balanced diet and exercise, smoking, alcohol and drug consumption, etc.) that a person can or should be able to manage to promote their health, reduce risk behaviour and improve their health status.
Health Supportive Environment – focuses on the conditions surrounding the living environment (home, study, work and leisure environment), including socio‑economic, psychosocial, natural and artificial environment, which affect or can affect population health and well-being.
Access – includes ensuring timely and affordable access to evidence‑based and effective health services, medicines and medical equipment when needed.
Patient Safety and Quality – describes the purposeful actions to prevent the risk of unnecessary harm associated with the provision of healthcare services and adopting an evidence‑based approach to the effective delivery of healthcare services to patients.
Health Literacy – relates to general education and information literacy and includes people’s knowledge, motivation, and skills to seek, understand, evaluate and use health information in order to make decisions related to health promotion, prevention and use of healthcare services with the aim of maintaining or improving the quality of life throughout life.
Person-centredness – a way of thinking and acting, where a person is viewed holistically and as an equal partner with whom co‑operation is carried out to find suitable solutions both in maintaining and improving health and in coping with diseases, while considering the person’s preferences, social and cultural background.
Integrated Care – health services are provided in a co‑ordinated manner between the levels of the health system and care providers, as well as in co‑operation with parties outside the health system, taking into account the needs of the person throughout life. This includes continuous health promotion, disease prevention, diagnosis, treatment and management of disease, and access to rehabilitation and palliative services as needed.
Governance – the way rules, norms and actions are prioritised, structured, sustained, regulated, and taken accountability for the field of health.
Health Infrastructure – availability of facilities, equipment and furnishings that meets established requirements to provide health services according to the population needs.
Workforce – describes the training, volumes, availability, workload, and migration of qualified and professionally educated healthcare service providers (doctors, dentists, nurses, midwives, pharmacists, etc.) and other health professionals participating in health service provision.
Financing – addresses the amount of financial resources at different levels that are invested in the provision of health services and the use of health products that contribute to the health and well-being of the population.
Digitalisation – the development and use of digital health technologies, programs, and software in the health system, which comprehensively support a person and their family members, members of the health network (incl. healthcare workers and specialists participating in the provision of health services), secondary data users, and the information system interoperability and comprehensiveness.
Innovation – development, piloting, and implementation of new solutions (incl. ICT solutions) in the health system.
Equity – describes disparities in health that are associated with socio‑economic (e.g. region, income, education level) factors, are not only unnecessary and avoidable but also considered unfair.
Efficiency – describes the extent to which best possible value has been achieved in the use of health services and available resources (incl. financial resources).
Resilience – a proactive capacity of the health system organisations, units, teams, and people to be prepared and quickly adapt to changes and potential challenges, rather than resist them, ensuring resilience, continuity, and quality of service delivery.