This annex describes the key organisational structures in the governance of the Estonian health system and their roles in health policy. In its second part, data submitted by Estonia to international databases for the purposes of international benchmarking are described. Finally, key national policy priorities that were considered in the HSPA development process are addressed.
Health System Performance Assessment Framework for Estonia
Annex B. Policy context and health system governance structures relevant to the Estonian HSPA
Roles and responsibilities of stakeholders across the Estonian health system
Aligning a new implementation process with existing health system and health data governance structures allows the process to leverage established channels of communication, roles, and responsibilities. It can promote efficiency and effectiveness as stakeholders are following the process based on their expertise, authority, and organisational position, maintaining stability and continuity in the governance processes. Drawing from this rationale, the governance of the HSPA (see Section 4.1) was embedded into existing frameworks arising from the roles and responsibilities of stakeholders across the health system. Figure A B.1 depicts key health system stakeholders in Estonia relevant for the HSPA and its governance.
Figure A B.1. Key stakeholders relevant to the HSPA

Source: (OECD, 2022[2]), The Development of the Estonian Health System Performance Assessment Framework: Situational Analysis Report, https://www.oecd.org/health/Development-of-Estonian-Health-System-Performance-Assessment-Framework.pdf.
The Ministry of Social Affairs (MoSA) is responsible for policy making in health. Organisations within its governance include the Health Board, the State Agency of Medicines (SAM), the National Institute for Health Development (NIHD), and the Health and Welfare Information Systems Centre (HWISC).
The Health Board holds responsibilities related to the organisation and surveillance in healthcare. It keeps records on medical licenses and registered health workers and is additionally responsible for the surveillance, prevention, and control of communicable diseases, environmental health, chemical safety, and safety of medical devices.
Activities in the jurisdiction of the State Agency of Medicines resemble those of the Health Board but are specific to medicinal products. SAM’s responsibilities are to ensure that medicinal products authorised in Estonia to prevent, treat, and diagnose human and animal diseases are effective, of high quality, and safe. Additionally, SAM maintains records about availability and sales of medicinal products in Estonia as well as activity licenses for handling of medicinal products, mediation of medical devices, and procurement of cells, tissues, and organs.
The National Institute for Health Development is a research and development institution for the health sector. One of its responsibilities is to collect, compute and compile health statistics on the premise that evidence‑based information influences behaviour, policies, and the environment. NIHD also submits data into international databases, following internationally determined definitions and ensuring the comparability of Estonia’s health statistics at the international level. Six core national databases and medical registries fall under the responsibility of the NIHD.
The Health and Welfare Information Systems Centre is responsible for the technical implementation of information and communication technology (ICT) services in healthcare, social care, and labour domains. It manages the Estonian National Health Information System (ENHIS). Additionally, HWISC prepares strategies and development plans; publishes standards and classifications.
Officially outside of the immediate jurisdiction of MoSA, the Estonian Health Insurance Fund (EHIF) remains a key relevant stakeholder in policy making. EHIF operates the national mandatory health insurance scheme, ensures the payment of health insurance benefits, contracts service providers, pays for the provision of health services, ensures that services are accessible, and performs selected quality assurance activities.
Figure A B.1 depicts the organisations with key roles in health policy, their key roles and responsibilities in the organisation, governance and assessment of health status and healthcare. However, the health information system in Estonia is broader than the policy making stakeholders described in the mentioned figure. Many other stakeholders have input into the field and keep the goals of National Health Plan in mind. These stakeholders include clinical specialists, patients, higher education providers, etc (Figure A B.2).
Figure A B.2. Other stakeholders
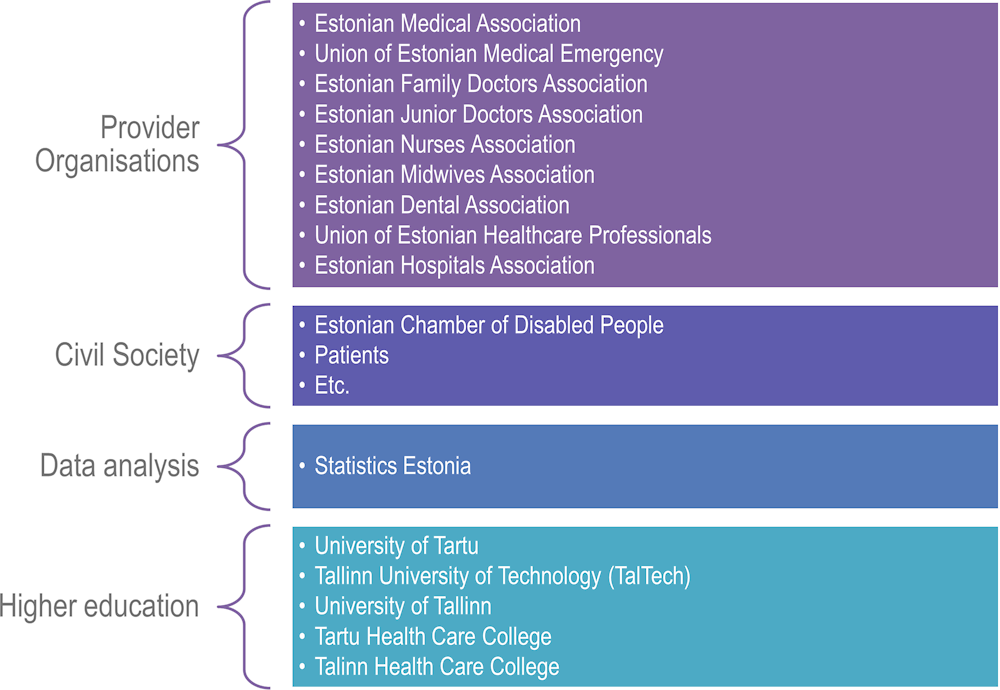
Source: The Estonian HSPA framework project.
Estonian health data infrastructure
Given the high level of digitalisation across the health system landscape in Estonia, a substantial amount of data is collected through both passive and active reporting. The data collection is often derived from the tasks assigned to each data collector by law. Thus, all databases are structured to allow the collecting authority to perform tasks assigned to them. Key data sources for health statistics are listed in Table A B.1 and detailed further in the Situational Analysis Report (OECD, 2022[2]).
Table A B.1. Sources of data for health statistics
|
Health registers and databases |
Surveys |
Other national registers and databases |
Statistical reports submitted by healthcare providers |
|---|---|---|---|
|
Registers located in the NIHD |
Nutrition Study |
Population Register |
11 different forms: outpatient visits and home visits; hospitals; dentists; infant breast feeding; mental and behavioural disorders; day care; economy; healthcare facilities; healthcare personnel; blood centres Collected annually; 10 aggregate, one individual level |
|
Estonian National Health Information System |
Health Behaviour of Adult Population survey |
Business Register |
|
|
Estonian Health Insurance Fund database |
Health Behaviour in School-age Children (HBSC) survey |
Working Register |
|
|
Registries located in the Health Board |
Childhood Obesity Surveillance Initiative (COSI) |
Work environment Register |
|
|
Registries located in the State Agency of Medicines |
European School Survey Project on Alcohol and Other Drugs (ESPAD) |
Traffic Register |
|
|
Myocardial Infarction Register |
Etc. |
Etc. |
International benchmarking
Estonia submits data to the OECD, WHO, EUROSTAT and other international databases for the purposes of international benchmarking. The majority of this data submissions for international purposes are in the responsibility of the NIHD. Table A B.2 outlines the categories in which data is shared internationally.
Table A B.2. Internationally submitted data by categories
|
EUROSTAT – WHO – OECD |
WHO |
OECD |
ECDC |
|---|---|---|---|
|
|
|
|
Source: OECD and NIHD.
Some indicators requested in international data collections are not currently submitted. The main reason for not submitting is that the required data are not collected, or there are differences in the methodology of calculating specific indicators. More specific descriptions for the indicators mentioned in this section can be found in the Annexes of the Situational Analysis Report (OECD, 2022[2]).
Key national priorities considered for HSPA development
National Health Plan 2020‑30
The National Health Plan (NHP) 2020‑30, co‑ordinated in the Ministry of Social Affairs, is the central strategy document that sets targets in the healthcare field for a decade (Ministry of Social Affairs, 2021[4]). The NHP operates on a ten‑year cycle, setting specific objectives and priorities in health. The plan is split into three core parts: healthy choices, health-supportive environment, and person-centred healthcare. Altogether, 114 indicators are used to measure progress, five of which are considered as central to the development of the population’s health in Estonia (Figure A B.3). Progress on objectives is assessed every two years through dedicated reports that contain updates on key indicators. A full list of the indicators included in the plan can be found in the Situational Analysis Report (OECD, 2022[2]).
Key objectives of NHP 2020‑30 are the following:
The average life expectancy of Estonian people increases by 2030: to 78.0 years for men and 84.0 years for women. Healthy life years increases to 62.0 and 63.0 years for men and women, respectively.
The increase in healthy life years exceeds the increase in life expectancy – people live a larger proportion of their lives without experiencing limitations caused by their health.
Health inequalities between genders, regions, and levels of education are reduced. By 2030, life expectancy in any county is not more than two years lower than the Estonian average. People with a basic level of education do not fall behind the average life expectancy of people with higher education by more than eight years.
Figure A B.3. Key Indicators of the Estonian National Health Plan 2020‑30
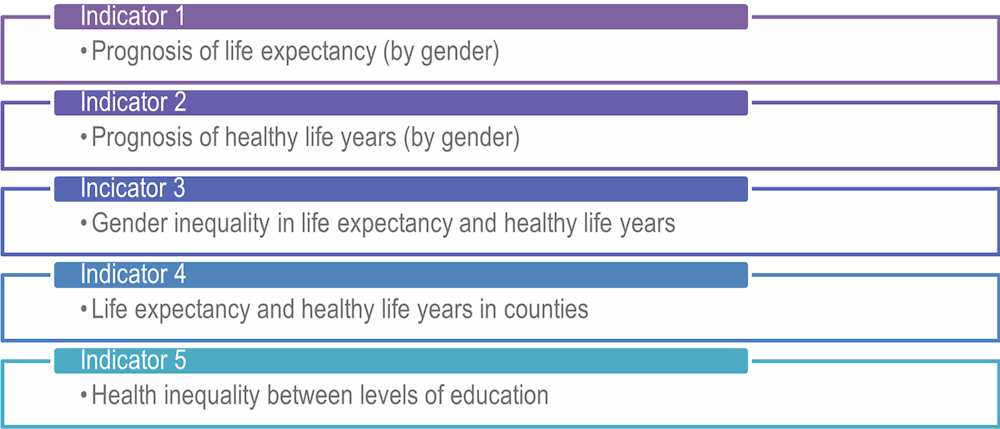
Source: (Ministry of Social Affairs, 2021[4]), National Health Plan 2020‑30, https://www.sm.ee/media/3054/download.
Other strategies and priorities
Several strategies and priority reforms have been formulated to reach the objectives set forth in the NHP 2020‑30. For instance, comprehensive reforms of healthcare services are underway, including developing and strengthening the model of primary care, modernising nursing care and renewing the health information system infrastructure through the New Generation Health Information System (UpTIS) reform. To ensure access to high-quality and person-centred specialist care for everyone, health infrastructure is renewed and different types of care are further integrated through the Hospital Master Plan (Ministry of Social Affairs, 2023[10]). Finally, due to poor performance on key indicators, good mental health throughout the life course is a key priority for Estonia and was given special consideration in the HSPA.