This chapter motivates the study by setting the context and reviewing trends in the demand for skills in the health workforce across countries. It discusses how ongoing trends, such as the adoption of new technologies, are likely to change the type of tasks and skills that are required of the health workforce going forward. The chapter also presents an overview of the research methodology.
Equipping Health Workers with the Right Skills
1. Changing demand for skills in the health workforce
Abstract
Context
Most countries were unprepared for the sudden surge in demand for health services brought upon by the COVID-19 pandemic. Health workers were called upon to respond to the needs of COVID-19 patients during the various waves of the pandemic since early 2020. While some sectors of the economy contracted or shut down completely in response to pandemic-related policy measures, many workers in the health sector had to maintain or increase their workload, often under considerable additional pressure. More than two years into the pandemic, health workforces across countries are struggling with high rates of burnout due to the challenging working conditions (Leo et al., 2021[1]; The COVISTRESS network, 2021[2]; Prasad et al., 2021[3]). Moreover, the World Health Organization estimates that between 80 000 and 180 000 health and care workers could have died globally of COVID-19 as of May 2021 (WHO, 2021[4]). The pandemic has both highlighted the importance of the health workforce, as well as the need to strengthen its resilience.
Prior to the pandemic, health workforces in many countries across the world were already under strain, with shortages reported both in terms of numbers of professionals and in terms of the skills needed to work with new technologies and adapt to new tasks. Public health systems were already overburdened in many countries that faced challenges in recruiting, deploying, and retaining sufficiently well trained and motivated health workers (WHO, 2016[5]). In its 2016 report, the World Health Organization recognised health workforce challenges as critical barriers to achieving the Sustainable Development Goal of universal health coverage by 2030 (WHO, 2016[5]).
Changes in the demographic, epidemiological and socioeconomic profile of populations will continue to change the demand for health services going forward and are likely to put further pressure on the demand for health workers. For instance, population ageing will increase the overall demand for healthcare, while also shifting the type of care that is demanded. At the same time, population ageing could strain the supply of health workers, as the size of the working age population declines (ILO, 2019[6]). For some countries, particularly in low and medium-income countries (LMICs), climate change is likely to increase the frequency of new viruses and infectious diseases, putting further pressure on health workforces and increasing the likelihood of future global health crises. Changes in health service utilisation and care delivery models – including a shift towards more people-centred healthcare and preventative healthcare – are also likely to impact the future demand for health services.
Conversely, technological advances have the potential to mitigate shortages in health workforces, with new technologies able to perform some of the tasks currently undertaken by health service workers or increase the efficiency by which particular tasks can be carried out. Health workers will also need to learn new skills to work optimally alongside newly adopted technologies. Some new technologies, like artificial intelligence, may also alleviate health workers of time-consuming tasks such as administrative work, allowing them to spend more time performing tasks that draw upon their uniquely human skills, like empathy and communication skills required in direct patient contact. A European review of skill mix initiatives, including those to update the tasks and roles of health workers in light of new technologies, has shown such initiatives to be linked to improvements in patient outcomes (Maier et al., 2021[7]). Adoption of new technologies is likely to be uneven across countries, with OECD countries currently better prepared to harness their potential than low and medium-income countries.
Box 1.1. Defining the health workforce
In this report, the health workforce is defined as all people engaged in actions whose primary intent is to enhance health, or who are essential to the performance of health systems (WHO, 2006[8]; WHO, 2010[9]). That means that the health workforce includes:
all personnel trained in health occupations delivering clinical work in health facilities (such as medical doctors, nurses, or dentists);
all non-health professionals employed in the health sector, public and private, regardless of their occupation (such as managers, ambulance drivers, or teachers of health education); and
all those whose work supports the delivery of health services, even if they are employed by other sectors or industries (such as cleaning, catering, security or agency staff working in the health sector) (ILO, 2017[10]).
Identifying the health workforce using data is complicated by the fact that health-related occupations are spread across occupation groups under the International Standard Classification of Occupations (ISCO-08), and some of these occupations are not predominantly health-related. For simplicity, data presented in this report refer to the core occupations in the health workforce as defined by ISCO-08 (ILO, 2012[11]; WHO, 2010[9]). These include:
Health professionals: medical doctors, nursing and midwifery professionals, traditional and complementary medicine professionals, paramedical practitioners, and other health professionals such as dentists, pharmacists, nutritionists or speech therapists; and
Health associate professionals: medical and pharmaceutical technicians, nursing and midwifery associate professionals, traditional and complementary medicine associate professionals, and other health associate professionals such as medical records and health information technicians.
Broadly, the current and future supply of the health workforce is a function of the current stock of health workers and their behaviour, and the net impact of inflows and outflows to the health workforce (Ono, Lafortune and Schoenstein, 2013[12]). Sources of inflows include immigration and education, while outflows include retirements, attrition, and emigration.
Misalignment between the supply and demand for skills in the health workforce contributes to various forms of skills mismatches, including over- or under-qualification, skills gaps, and labour shortages. Skills gaps and labour shortages are particularly costly in the health workforce, since they can increase the length of patient waiting lists and waiting times and result in poor patient care, for instance due to increased burnouts and job dissatisfaction among medical staff (Kane et al., 2007[13]; Jun et al., 2021[14]). These costs come in addition to the negative economic consequences usually associated with skill mismatches and shortages in other sectors of the economy, including lost wages and lower productivity and growth (OECD, 2016[15]).
Addressing the skills mismatch challenge in the health workforce can improve healthcare provision and limit these negative economic effects. Countries have a number of policy tools at their disposal to improve the supply of skills to meet demand (OECD, 2016[16]). These include increasing the number of places available to train new health service workers, updating education and training curricula to respond to market needs, offering targeted career guidance for prospective students, altering migration flows, and facilitating the recognition of skills and qualifications of migrants. Improving wages and working conditions can also improve the future supply of health workers by increasing the inflow and reducing attrition rates.
However, such policy efforts require resources, and their impacts may not be immediate or may have adverse consequences. Building and developing skills supply in the health workforce requires forward planning, as it can take several years to train health professionals, particularly highly skilled health workers such as physicians. Further, the highly complex nature of clinical functions means that health workers who are trained in one specialisation cannot simply be redeployed to another to fill existing gaps. Migration flows of health service workers tend to consist of movements from lower-income to higher-income countries, where demand and capacity to pay for health services are higher (OECD, 2019[17]). Migration can provide flexibility for higher-income countries in responding to demand-side pressures and allow workers from lower-income countries to gain new skills abroad. However, this can also lead to a “brain drain” effect away from lower-income countries, which have invested resources to train the health workforce and may have a shortage of trained health workers themselves (ILO, 2017[18]).
Alternatively, other strategies can be deployed in a relatively short period by introducing new categories in the health workforce (such as community health workers), expanding the role of existing categories of health workers, or non-traditional programmes that enable fast entry into the health workforce (such as recruitment programmes for foreign trained health workers). While these types of strategies can offer a means to improve the availability of health workers in a relatively shorter period, they can also involve changes in the ways health services are provided and financed, and re-thinking regulations around scopes of practice, professional education, quality standards and accreditation practices.
Any policy response will only be effective if informed by accurate information about both current and future skill needs in the health workforce. Effective anticipation of future skills needs is crucial in this respect. Improving the resilience of the health workforce involves both increasing the size of the health workforce and equipping it with the relevant emerging skills. In response to these challenges, countries are already starting to assess future health workforce needs in terms of both numbers and skills.
Objective of this study
This study is a collaboration between the OECD and the International Labour Organization (ILO). The objective is to map the methods currently used by countries to anticipate health workforce needs – both in terms of numbers of workers and skill requirements. It aims to shed light on the strengths and weaknesses of different methods and highlight how skills intelligence is used to build more resilient health workforces, so that other countries may learn and refine their own approaches to anticipating skill and labour needs in the health workforce.
Past and changing demand for skills in the health workforce
The OECD and ILO Skills for Jobs databases provide internationally comparable measures of skills shortages and surpluses (Box 1.2), and Figure 1.1 highlights that health workforces in most countries are under strain. Most countries included in the OECD and ILO Skills for Jobs databases already experienced large shortages of health professionals and/or health associate professionals prior to the COVID-19 pandemic, suggesting that it was hard to find sufficient numbers of workers with the right skills in health services occupations. Shortages in health workforces are relatively large compared to other occupations, with only three occupations demonstrating larger shortages: teaching professionals, skilled forestry fishery and hunting workers, and street and related sales and service workers.
The greatest shortages of health professionals were found in Belgium, Thailand and Greece, and the greatest shortages of health associate professionals were found in Uruguay, France and Norway. Some countries, such as Finland, Spain, the Netherlands, and Denmark, show relatively large shortages for both groups of health services workers.
Figure 1.1. Shortages in the health workforce in 2019 (or nearest year)
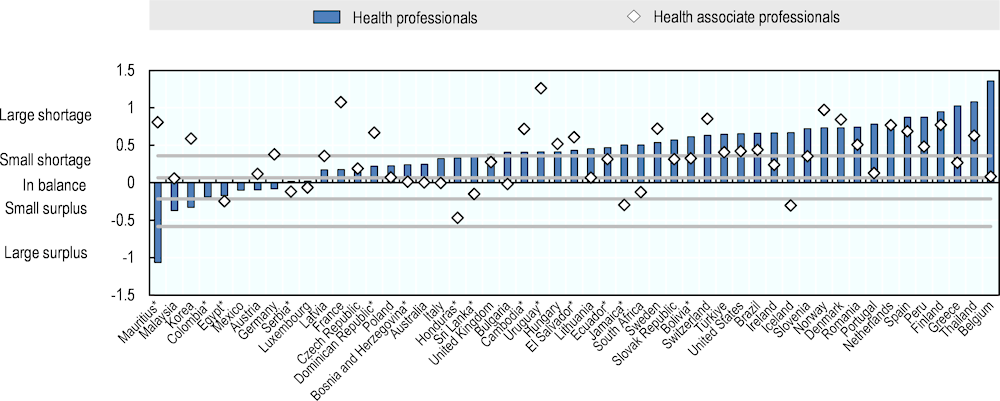
Note: Based on the re-weighted occupational imbalance indicator (see Box 1.2). Positive values indicate shortages, negative values indicate surpluses. The categorisation of small/large shortages and surpluses is based on the distribution of the OECD average of the composite occupational needs indicator across years. Within this distribution, the bottom 10% of the OECD average values across occupations are ‘large surpluses’ and the top 10% are ‘large shortages’. When shortages or surpluses are so small that they could be considered negligible (i.e. values in the middle 40% of the distribution of the OECD average, or the 30th to the 70th percentile) the occupation is considered ‘in balance’. These cut-off values are then applied to all countries. Data refer to 2019, with the following exceptions: they refer to 2021 for BIH, BOL, DOM, ECU, SLV, SRB, URY; 2020 for HND; 2018 for CHE, FRA, IRL, ITA, MUS, POL, THA; 2017 for DEU, GBR, KHM, KOR; 2016 for AUS; 2015 for BRA, TUR; 2014 for JAM; 2012 for ISL and SVN. Health professionals include veterinarians and health associate professionals include veterinary technicians and assistants – and none of these are part of the health workforce. The data for health associate professionals in Colombia and Mexico are suppressed from the graph due to insufficient data reliability.
Source: Elaborations based on the OECD Skills for Jobs database 2022; *Elaborations based on the ILO Skills for Jobs database.
Box 1.2. Skills for Jobs database
Originally launched in 2017, the OECD Skills for Jobs database is an internationally comparable index of skill needs (such as medicine, communication, or physical skills). The data indicate which skills are in shortage (hard-to-find) or surplus (easy-to-find) across countries. The indicator measuring skills shortages and surpluses is constructed following a two-step approach.
Step 1. An “occupational imbalance indicator” is a composite indicator of occupational imbalance that is calculated for occupation groups at the 2-digit ISCO-08 level. This calculation is based on labour market information from household surveys and consists of five sub-components: i) wage growth, ii) employment growth, iii) hours worked growth, iv) change in unemployment rate, and v) change in under-qualification rate. For every country, occupational group and sub-component, long-run trends are compared to the economy-wide trend. This standardisation sheds light on whether the specific occupational group is outperforming/underperforming the rest. When combining the standardised sub-components into the composite occupational imbalance indicator, each sub-component is weighted equally, except for employment growth, which has a lesser weight than the others.
Step 2. The composite occupational imbalance indicator is then linked to a mapping of skill requirements by occupation (for more information, see (OECD, 2022[19])). By aggregating the data by skill, using number of employed by occupation as a weight, a skill imbalance indicator is created for each country. For instance, if there are shortages of health professionals in a country, then there are likely to be shortages of medical knowledge (a skill), provided the health professional occupational group is relatively large, and that job postings for health professionals often mention knowledge of medicine. Conversely, large surplus occupations that require physical skills will contribute to surpluses of physical skills.
Extension of the OECD Skills for Jobs database for this report
Exceptionally for this report, some changes were made to the weighting scheme in Step 1. A lesser weight is given to the sub-components of wage growth and change in the under-qualification rate, while a greater weight is given to change in the unemployment rate. Wage growth may not be a reliable indicator of health workforce shortages in countries with large public healthcare systems. Similarly, due to a high degree of occupational licensing in the health workforce, hiring workers with a lower qualification than is required is not usually a viable option when labour is scarce. Unemployment rates of health services workers, on the other hand, appear to be sensitive to changing demand in the health workforce, which is why the weight for that sub-component is increased. The weights of the sub-components for employment and hours worked remain unchanged.
The ILO Skills for Jobs database extends the methodological approach used by OECD to low-and-middle income countries (for more information, see (ILO, 2021[20]).
Source: OECD Skills for Jobs database, https://www.oecdskillsforjobsdatabase.org; ILO Skills for Jobs database, https://www.ilo.org/skills/areas/skills-training-for-poverty-reduction/WCMS_835486/lang--en/index.htm.
Shortages in the health workforce are far from a new phenomenon. On average, most countries experienced large shortages of health service occupations persistently over the past 15 years (Figure 1.2). In some countries, shortages of health services workers not only persisted but also increased (Dominican Republic, Slovenia, the Slovak Republic, Peru, Ireland, and France). In other countries, large shortages emerged within the past 10 to 15 years (Türkiye, Uruguay, El Salvador, and Argentina). For some countries, surpluses of health services workers found in the past have since disappeared (Luxembourg and Malaysia). Shortages of health services workers decreased in size in countries such as New Zealand, South Africa, Austria, and Mauritius.
These developments, and the way in which they differ across countries, highlight the challenge of aligning the future supply of health workers to long-term demand correctly. For all countries, reforming training and employment strategies to better respond to changing skill and health needs can help meet demand. For OECD countries, this can also reduce reliance on foreign-trained health workers from low and medium-income countries, thereby promoting sustainable outcomes across countries (OECD, 2016[16]).
Figure 1.2. Average shortages in health service occupations, 2004 and 2019 (or nearest years)
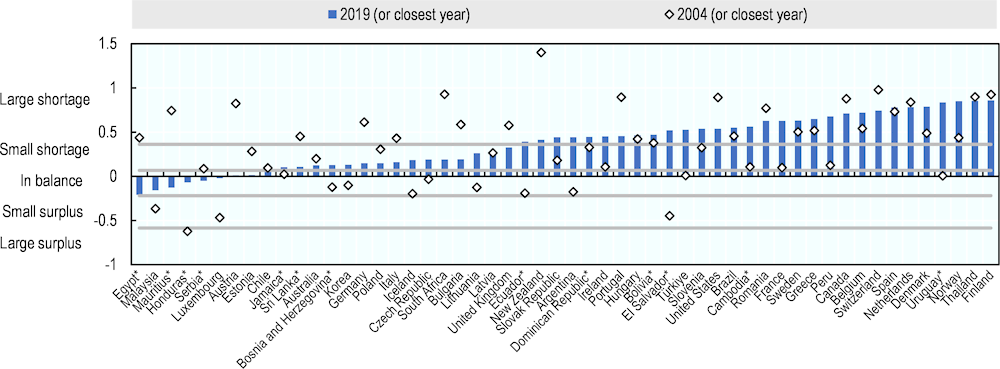
Note: Unweighted average across health professionals and health associate professionals. Based on the re-weighted occupational imbalance indicator (see Box 1.2). Positive values indicate shortages, negative values indicate surpluses. The first year refers to 2004, with the following exceptions: they refer to 1999 for KOR; 2001 for CAN, CHL; 2003 for BRA; 2005 for AUT, CZE, DEU, GBR, LTU, SVK, SVN, TUR; 2006 for ESP; 2007 for BGR, GRC, HUN, ITA, LVA, NOR, POL, PRT, ROU; 2008 for CHE, PER; 2009 for JAM, NLD; 2010 for EGY, KHM, NZL; 2011 for AUS, BIH, ZAF; 2012 for BOL, MUS, MYS, THA, URY; 2013 for SRB; 2014 for ECU, LKA, SLV; 2016 for DOM, HND. The final year refers to 2019, with the following exceptions: they refer to 2021 for BIH, BOL, DOM, ECU, SLV, SRB, URY; 2020 for HND; 2018 for CHE, FRA, IRL, ITA, MUS, POL, THA; 2017 for DEU, GBR, KHM, KOR; 2016 for AUS; 2015 for BRA, TUR; 2014 for JAM; 2012 for ISL and SVN.
Health associate professionals include veterinarians and veterinary technicians and assistants, who are not part of the health workforce. The data for Colombia and Mexico are suppressed from the graph due to insufficient data reliability for health associate professionals.
Source: Elaborations based on the OECD Skills for Jobs database 2022; *Elaborations based on the ILO Skills for Jobs database.
While shortages of skilled health workers are a serious and widespread problem, they affect LMICs especially severely. The size of the health workforce varies dramatically across the globe by region and income group (see Figure 1.3). From a regional perspective, Europe and North America perform significantly better than other regions in terms of physicians and nurses per 1 000 people, while the Middle East and North Africa, South Asia and particularly Sub-Saharan Africa perform worse. The contrast between high-, middle- and low-income countries is stark: high-income countries had 15.3 physicians and nurses per 1 000 people in 2017, while this figure was only 4.2 per 1 000 for middle-income countries, and 1.2 per 1 000 for low-income countries. It is evident that globally, millions more doctors and nurses need to be trained to meet the Sustainable Development Goals (SDGs) and global goals for universal health coverage, particularly in low and middle-income countries.
Figure 1.3. Physicians and nurses per 1 000 people, 2017
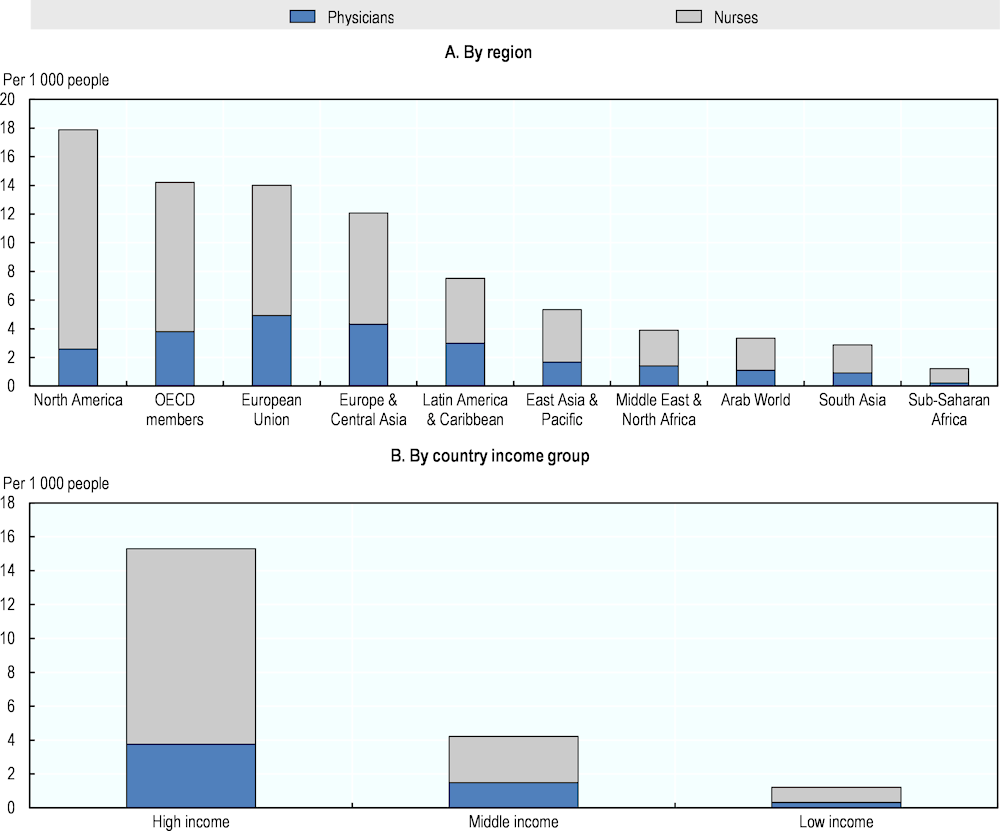
Note: For some countries, more recent data are available in the OECD Health Statistics 2022. These data show that, for most countries included in the database, the number of physicians and nurses per 1000 people increased over time (see https://stats.oecd.org/Index.aspx?ThemeTreeId=9#)
Source: World Bank Databank.
Compared to occupations in other sectors, qualification and field-of-study mismatches are relatively uncommon in the health workforce (Figure 1.4). Among health professionals and health associate professionals, about 13% are over-qualified for their occupation (compared to 15% on average across all occupations), 8% are under-qualified (compared to 18% across all occupations), and 15% have a qualification in a field-of-study that does not directly match their occupation (compared to 32% across all occupations). This reflects a high degree of occupational licensing in the health workforce, particularly in health service occupations. Occupational licensing ensures that health services workers meet minimum skill and knowledge requirements, which is important for ensuring patient safety. At the same time, occupational licensing reduces flexibility in task allocation and in recruitment, which complicates the response to reducing or preventing shortages. While over-qualification is relatively uncommon among native workers, it is more widespread amongst migrant workers, often due to strict qualification requirements and a lack of recognition of foreign qualifications. Coupled with “brain drain,” the emigration of highly qualified people, this contributes to an underutilisation of skilled labour at a national and global level.
Figure 1.4. Qualification mismatches in the health workforce in OECD countries, 2019
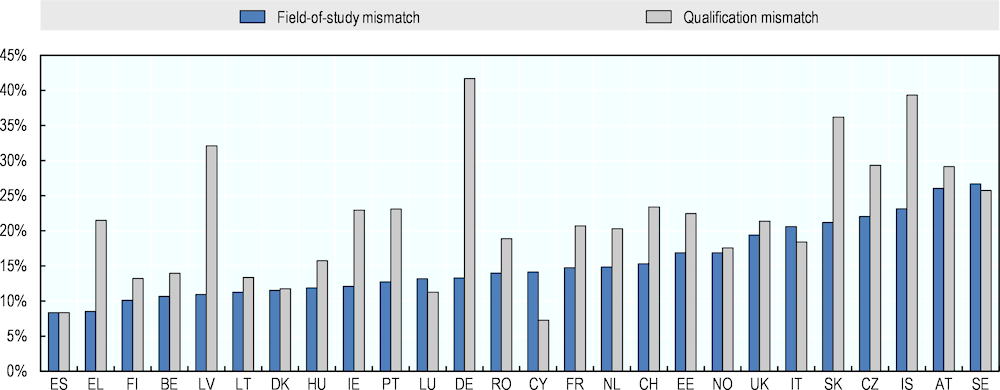
Note: Average across Medical doctors, Nursing and midwifery professionals, Traditional and Complementary Medicine Professionals, Paramedical Practitioners, Other Health Professionals, Medical and Pharmaceutical Technicians, Nursing and Midwifery Associate Professionals, Traditional and Complementary Medicine Associate Professionals, Other Health Associate Professionals, Personal Care Workers in Health Services, Professional Services Managers (incl. Health Services Managers and Aged Care Services Managers), Social and Religious Professionals (incl. Psychologists) and Administrative and Specialised Secretaries (incl. Medical Secretaries).
Source: OECD Skills for Jobs database 2022
Online job vacancies reveal change in the relative importance of some skills for health services occupations over time. Job-specific knowledge of psychology, therapy and counselling, and medicine and dentistry consistently show up as important in job vacancies for health service occupations (Figure 1.5). This reflects that the minimum qualification requirements of health service workers are relatively stable over time. That said, some skills have become more important for health services workers, while others have become less important over time. For instance, learning, judgment and decision making skills are becoming increasingly important for health services workers, while the relative importance of physical skills like psychomotor abilities is decreasing. This could reflect the increasing use of technology in health service delivery, which can lighten some of the physical burden on health service workers, while putting a greater emphasis on their social and decision-making skills.
Figure 1.5. Change in the relative importance of skills within health services occupations
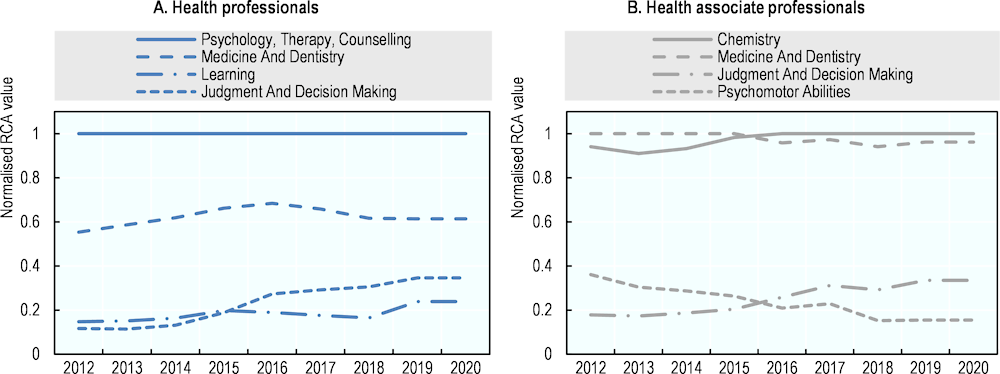
Note: A normalised Relative Comparative Advantage (RCA) value of 1 indicates the most important skills for a given occupation, compared to other skills; while a value of 0 indicates the least important skills. See OECD (2022[19]) for more details.
Source: Elaborations based on the OECD Skills for Jobs database 2022.
Future trends in the health workforce
A number of trends will affect the future supply and demand for health workers, and these must be taken into account when anticipating skill and labour needs. Three notable trends include technological change, demographic change and environmental change.
Adoption of new technologies in the health sector could increase the productivity of health workers, and potentially mitigate shortages, but automation in the sector remains limited. While new technologies may lead to the automation of some tasks, they are unlikely to fully replace health workers and are instead more likely to augment their capabilities. Figure 1.6 highlights that the health workforce – and health service occupations in particular – is less likely to be automated than other occupation groups. This is partly because healthcare professionals and technicians are highly dependent on customer- or patient-serving skills and interpersonal skills that cannot easily be routinised, substituted by digital technologies or offshored (Nedelkoska and Quintini, 2018[21]).
Figure 1.6. Risk of automation within and outside of the health workforce
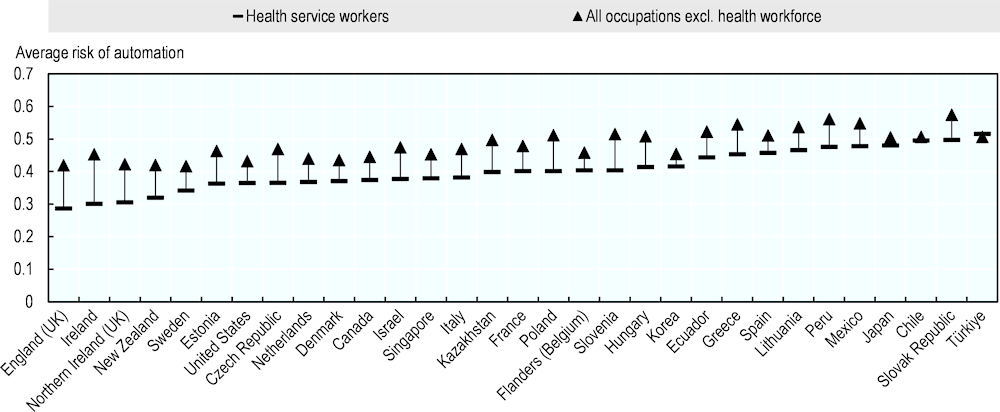
Note: Average risk of automation across 3-digit ISCO-08 occupations.
Source: OECD Survey of Adult Skills (2011/12, 2014/15, 2017/18).
An OECD report summarizing literature on the impact of artificial intelligence (AI) on the labour market concludes that it is likely to complement rather than substitute high-skilled workers and enable them to increase their productivity (Lane and Saint-Martin, 2021[22]). For instance, AI can support health service workers with administrative activities, freeing up their time for more direct patient contact or work that uses their specialised skills. With many highly skilled workers in the sector and ethical issues relating to the application of AI that are likely to slow widespread adoption, AI is unlikely to displace large numbers of health service workers (Davenport and Kalakota, 2019[23]). Potential ethical issues include the risk that using this technology may put patients’ digital security and privacy at risk or systematise human biases in diagnosis, among others (Salvi Del Pero, Wyckoff and Vourc’h, 2022[24]; WHO, 2021[25]). Policies will need to be put in place to mitigate these risks in the health sector. Meanwhile, uniquely human skills like empathy, persuasion and big-picture integration, alongside digital skills, are likely to be increasingly required in order to complement and operate new technologies as they are adopted. AI can support diagnosis and treatment recommendations, for instance, with several studies showing that algorithms are already outperforming radiologists in spotting malignant tumours (Davenport and Kalakota, 2019[23]). AI can also improve patient engagement and adherence with treatment plans via messaging alerts and personalised content.
Demographic changes, including ageing societies and population growth, will continue to influence the health sector and shape the future demand for workers. Ageing populations will create many challenges for health systems, including increased demand for healthcare, long-term care and end-of-life services. Furthermore, the health workforce itself is ageing in many countries. In 2019, 35% of all doctors in OECD countries were over 55 years of age, an increase from 20% in 2000 (see Figure 1.7). Ageing health workforces could affect the ratio of health workers to patients if a sufficient number of newly trained workers is not available to replace those who will retire and lead to further demand in OECD countries for trained health workers from LMICs that are projected to have younger populations (primarily in sub-Saharan Africa).
Figure 1.7. Share of doctors aged 55 and older, 2000 and 2019 (or nearest years)
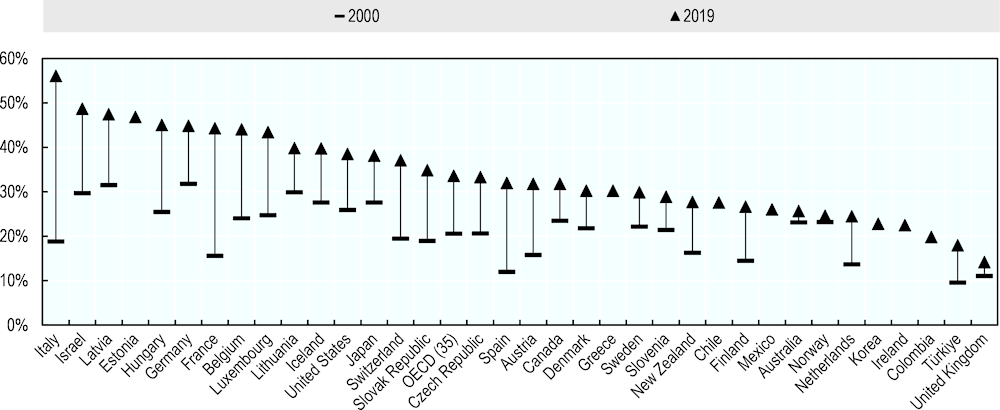
Source: OECD (2021[26]), Health at a Glance 2021: OECD Indicators, https://doi.org/10.1787/ae3016b9-en.
Environmental factors, including climate change and air pollution, will also affect the future demand for health services (ILO, 2019[6]). Climate change has been indirectly linked to an increased risk of vector-borne diseases and cholera and can increase the prevalence of diseases transmitted through food and water (Costello et al., 2009[27]). Among the conditions most likely to increase demand for health services are heat stress, dengue, malaria, and malnutrition, particularly in low and medium-income countries situated in warmer climates. Health issues related to climate change and environmental factors are likely to continue to impact both the demand for health services and the health workforce itself, including occupational safety and health of workers.
Research methodology
This study is based on three sources of data. First, it is based on a series of semi-structured interviews with institutions that are involved in developing or using skill needs assessments in the health workforce. Second, it is based on a review of the international literature on methods that countries use to anticipate future skill needs, in the health sector and more generally. Third, it draws from discussions during a virtual peer-learning workshop in June 2022 which brought together representatives from 20 countries to discuss the methods used to anticipate skill needs in the health workforce, and how the resulting skills intelligence is used in policymaking. The next sections describe how countries and institutions were selected for interviews and provides some additional information about the interviews themselves.
Selection of countries and institutions for interviews
A mix of high-income, middle-income, and low-income countries were selected for interviews to showcase a range of skill anticipation exercises with different resource requirements. Countries were selected based on desk research revealing that skill anticipation exercises were being carried out for the health workforce, and with an aim to have broad representation of different types of exercises. The following 16 countries participated in the study: Argentina, Australia, Bangladesh, Canada, Colombia, Ethiopia, Finland, Germany, Ghana, Ireland, Korea, the Netherlands, Norway, South Africa, Sweden, and the United States. Data collection for the United States focused on the use of skills anticipation exercises for policymaking and not on the development of the exercises. For this reason, Chapter 2 does not include the United States.
Respondents and semi-structured interviews
Respondents were typically individuals who were actively involved in conducting skill assessments for the health workforce within their respective institutions. The types of institutions that conduct skill assessments vary substantially. The institutions that participated in this study included ministries of education, ministries of employment/labour, health sector skills committees, workers’ unions, government-appointment committees, education and training institutions, and research institutions. Trade unions and employer representatives were invited to participate in the study via the OECD’s Trade Union Advisory Committee and the Business and Industry Advisory Committee. The ILO conducted its work in LMICs by carrying out interviews with tripartite constituents, consisting of respondents from relevant ministries, employers’ and workers’ organizations and consulting with sector skills bodies in the countries where they were in place. Consultants were hired in these countries who could carry out the interview in the respondent’s language.
As part of the semi-structured interviews, respondents were asked a series of open-ended questions about the methods they used to anticipate health workforce skill needs. An interview guide that was developed to support these interviews is included in the Annex. Interviews generally lasted one hour and were conducted over videoconference or face to face. They were informal in nature and not all questions in the interview guide were asked during each interview, as questions were selected according to the respondent’s interest or expertise. In cases of language or time constraints, the respondents were sent the interview guide following the interview and asked to provide further responses to the questions they felt equipped to answer.
References
[27] Costello, A. et al. (2009), “Managing the health effects of climate change”, The Lancet Commissions, Vol. 373, p. 1693, https://doi.org/10.1016/S0140-6736(09)60935-1.
[23] Davenport, T. and R. Kalakota (2019), “The potential for artificial intelligence in healthcare”, Future Healthcare Journal, Vol. 6/2, pp. 94-98, https://doi.org/10.7861/futurehosp.6-2-94.
[2] Gesser-Edelsburg, A. (ed.) (2021), “The major worldwide stress of healthcare professionals during the first wave of the COVID-19 pandemic – the international COVISTRESS survey”, PLOS ONE, Vol. 16/10, p. e0257840, https://doi.org/10.1371/journal.pone.0257840.
[20] ILO (2021), Methodological note, https://www.ilo.org/ilostat-files/Documents/skillsforjobs.html (accessed on 16 August 2022).
[6] ILO (2019), “The future of work in the health sector”, Working Paper, No. 325, International Labour Office, Geneva, https://www.ilo.org/sector/Resources/publications/WCMS_669363/.
[10] ILO (2017), Improving employment and working conditions in health services, International Labour Organization, Geneva, https://www.ilo.org/global/docs/WCMS_548288/.
[18] ILO (2017), Tripartite Meeting on Improving Employment and Working Conditions in Health Services: Conclusions on improving employment and working conditions in health services, International Labour Office, Geneva, https://www.ilo.org/sector/activities/sectoral-meetings/WCMS_508523/.
[11] ILO (2012), International Standard Classification of Occupations: ISCO-08, International Labour Office, Geneva.
[14] Jun, J. et al. (2021), “Relationship between nurse burnout, patient and organizational outcomes: Systematic review”, International Journal of Nursing Studies, Vol. 119, p. 103933, https://doi.org/10.1016/J.IJNURSTU.2021.103933.
[13] Kane, R. et al. (2007), “Nurse staffing and quality of patient care.”, Evidence Report/technology Assessment 151, pp. 1-115, http://europepmc.org/books/NBK38315 (accessed on 16 August 2022).
[22] Lane, M. and A. Saint-Martin (2021), “The impact of Artificial Intelligence on the labour market: What do we know so far?”, OECD Social, Employment and Migration Working Papers, No. 256, OECD Publishing, Paris, https://doi.org/10.1787/7c895724-en.
[1] Leo, C. et al. (2021), “Burnout Among Healthcare Workers in the COVID 19 Era: A Review of the Existing Literature”, Frontiers in Public Health, Vol. 9, https://doi.org/10.3389/fpubh.2021.750529.
[7] Maier, C. et al. (2021), Skill-mix Innovation, Effectiveness and Implementation: Improving Primary and Chronic Care, European Observatory on Health Systems and Policies, World Health Organization.
[21] Nedelkoska, L. and G. Quintini (2018), “Automation, skills use and training”, OECD Social, Employment and Migration Working Papers, No. 202, OECD Publishing, Paris, https://doi.org/10.1787/2e2f4eea-en.
[19] OECD (2022), Mapping skill requirements in occupations based on job postings data: An application to the Skills for Jobs database 2022, https://www.oecdskillsforjobsdatabase.org/data/S4J2022_methods.pdf.
[26] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[17] OECD (2019), Recent Trends in International Migration of Doctors, Nurses and Medical Students, OECD Publishing, Paris, https://doi.org/10.1787/5571ef48-en.
[15] OECD (2016), Getting Skills Right: Assessing and Anticipating Changing Skill Needs, Getting Skills Right, OECD Publishing, Paris, https://doi.org/10.1787/9789264252073-en.
[16] OECD (2016), Health Workforce Policies in OECD Countries: Right Jobs, Right Skills, Right Places, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/9789264239517-en.
[12] Ono, T., G. Lafortune and M. Schoenstein (2013), “Health Workforce Planning in OECD Countries: A Review of 26 Projection Models from 18 Countries”, OECD Health Working Papers, No. 62, OECD Publishing, Paris, https://doi.org/10.1787/5k44t787zcwb-en.
[3] Prasad, K. et al. (2021), “Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study”, EClinicalMedicine, Vol. 35, p. 100879, https://doi.org/10.1016/j.eclinm.2021.100879.
[24] Salvi Del Pero, A., P. Wyckoff and A. Vourc’h (2022), “Using Artificial Intelligence in the workplace : What are the main ethical risks?”, OECD Social, Employment and Migration Working Papers, No. 273, OECD Publishing, Paris, https://doi.org/10.1787/840a2d9f-en.
[25] WHO (2021), Ethics and Governance of Artificial Intelligence for Health: WHO guidance, http://apps.who.int/bookorders. (accessed on 14 November 2022).
[4] WHO (2021), The impact of COVID-19 on health and care workers: a closer look at deaths, World Health Organization, https://apps.who.int/iris/handle/10665/345300 (accessed on 22 July 2022).
[5] WHO (2016), “Global strategy on human resources for health: Workforce 2030”, https://www.observatoriorh.org/sites/default/files/webfiles/fulltext/2019/global_strategy_workforce2030_who.pdf (accessed on 25 July 2022).
[9] WHO (2010), Monitoring the building blocks of health systems: A handbook of indicators and their measurement strategies, https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf (accessed on 31 March 2022).
[8] WHO (2006), Working together for health, https://www.who.int/whr/2006/whr06_en.pdf (accessed on 31 March 2022).