Abstract
The coronavirus (COVID-19) pandemic highlights the need for a comprehensive and integrated approach to human health. Enhancing environmental health through better air quality, water and sanitation, waste management, along with efforts to safeguard biodiversity, will reduce the vulnerability of communities to pandemics and thus improve overall societal well-being and resilience. Exposure to ambient and indoor air pollution increases the risk of cardiovascular, respiratory and developmental diseases, as well as premature death, and makes individuals more vulnerable to COVID-19. Water access and quality and biodiversity protection are key to battling the spread of pandemics, while effective waste management is essential to minimise possible secondary impacts upon health and the environment.
1. The COVID-19 crisis has clearly demonstrated that societies need to strengthen their resilience to pandemics and other emergencies. Countries are concentrating, in the short term, on shoring up public health systems and addressing the immediate economic impacts of the crisis. But, in the medium to longer term, enhancing the environmental health of societies – i.e. aspects of human health and well-being that are determined by environmental factors – is a key component to the economic recovery and stimulus measures that governments are currently designing. Limiting people’s exposure to hazardous physical, chemical, and biological agents in air, water, soil, food, and other environmental media will reduce their vulnerability to future pandemics, increase their health and well-being, and provide an important complement to public health systems.
Limiting people’s exposure to air and water pollution will reduce vulnerability to future pandemics and contribute to enhancing health and well-being.
2. Many of today’s environmental challenges are responsible for adversely affecting the health and livelihoods of individuals and communities in both OECD and non-OECD countries, with vulnerable groups such as the elderly and less well-off segments of society being more impacted. Improving air quality reduces the incidence of cardiovascular and respiratory diseases that increase the vulnerability of individuals and communities to pandemics similar to COVID-19, and generates wider benefits for public health, well-being and resilience. Better access to clean water and sanitation can lower transmission of infectious diseases. Effectively addressing waste generation, management and recycling minimises health and environmental risks from poor handling of contaminated waste. Halting and reversing biodiversity loss protects people from the transmission of pathogens.
3. While the crisis is still unfolding around the world, and will continue to evolve for some time, empirical evidence on the links between environmental challenges and COVID-19 is still emerging. However, a better understanding of the role of environmental health as a crucial component of overall health priorities will help to inform policy responses in the recovery from the current pandemic and preparedness for future such shocks. Such an understanding will also generate significant co-benefits in terms of improving the overall health of communities and increasing the resilience of societies.
Improving air quality for well-being and resilience
4. Air pollution is the world’s single largest environmental health risk, accounting for an estimated 4.2 million premature deaths a year from outdoor pollution, and 3.8 premature deaths from indoor pollution. It is estimated that 9 out of 10 people breathe air containing high levels of pollutants (WHO, 2020[1]). Exposure to air pollution is associated with myriad adverse health outcomes in the short and long term, such as increased risks of cardiovascular, respiratory and developmental diseases, as well as a higher risk of overall mortality (WHO, 2018[2]). Improving air quality can help increase resilience against acute respiratory illnesses as well as generate wider societal benefits.
Improving air quality can help increase resilience against acute respiratory illnesses as well as generate wider societal benefits.
Air pollution can increase susceptibility to acute respiratory illnesses
5. People suffering from preconditions linked to air pollution are more vulnerable to the effects of the SARS-CoV-21. Health damages resulting from long-term exposure to air pollution can diminish the body’s ability to fend off respiratory infections. While the understanding of the epidemiology of COVID-19 is still evolving, a Harvard study2 conducted in the United States identified a large overlap between causes of deaths of COVID-19 patients and the diseases that are linked to long-term exposure to fine particulate matter (PM2.5). The research found that a person living for decades in a state in the US with high levels of fine particulate matter is 15% more likely to die from COVID-19 than someone in a region with one unit less of the fine particulate pollution (Wu et al., 2020[3]). These results are also consistent with findings that air pollution exposure dramatically increased the risk of death during the Severe Acute Respiratory Syndrome (SARS) outbreak in 2003, which was caused by another type of coronavirus (Cui, 2003[4]). However, empirical evidence on the link between air pollution concentrations and COVID-19 impacts is currently lacking from most other countries due to the emerging nature of the crisis and the absence of sufficiently granular data on COVID-19 cases and mortality.
6. Exposure to a major form of air pollution, fine particulate matter (PM2.5),3 is particularly harmful as it penetrates deep into the lungs and blood streams, causing heart and respiratory diseases, and premature death. Despite some progress since 2011 in OECD countries, exposure to PM2.5 remains high. The mean population exposure to PM2.5 in two out of three OECD countries exceeds the WHO guideline of 10 μg/m3, a value which is still associated with elevated levels of risk (Figure 1). The percentage of the population that exceeds the WHO guideline is significant in many OECD countries (Figure 2).
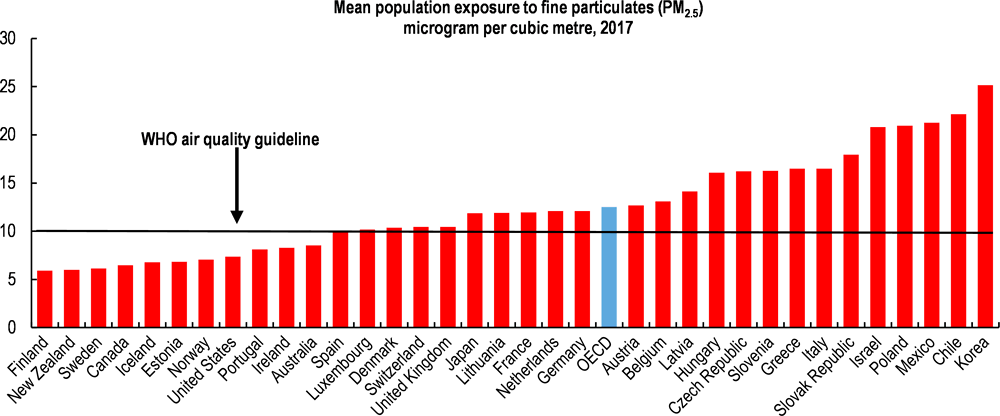
Note: The chart shows ambient (outdoor) PM2.5. In some countries, residential (indoor) pollution is an important factor (e.g. from burning biomass for heating and cooking). Data on other countries in the world, and on exposure to residential PM2.5 are available at OECD.Stat.
Source: OECD (2020) Environment at a Glance: Air quality, using estimates from Global Burden of Disease.
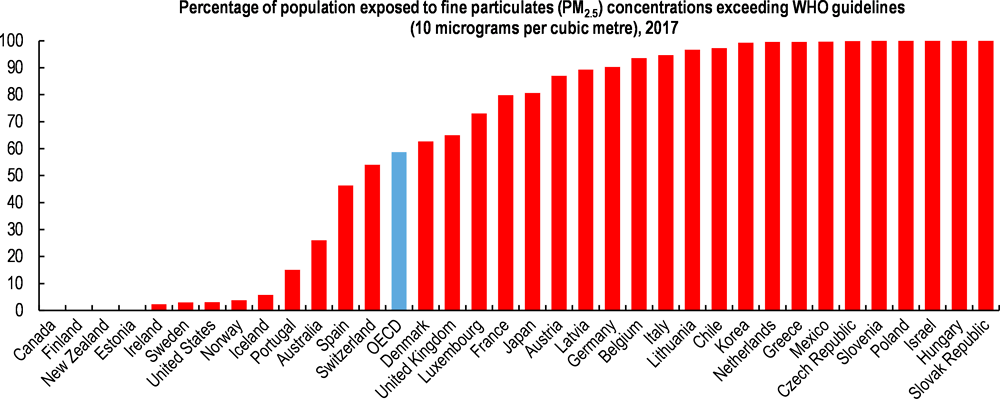
Note: The chart shows ambient (outdoor) PM2.5. In some countries, residential (indoor) pollution is an important factor (e.g. from burning biomass for heating and cooking). Data on other countries in the world, and on exposure to residential PM2.5 are available at OECD.Stat.
Source: OECD (2020) Environment at a Glance: Air quality, using estimates from Global Burden of Disease.
7. Globally, exposure to ambient PM2.5 is projected to lead to an estimated 6-9 million premature deaths a year in 2060, in the absence of better policies. In OECD countries, the welfare costs of premature mortality due to PM2.5 pollution are equivalent to about 3% of GDP on average. In the absence of stronger policy action, annual welfare costs from premature deaths are projected to more than double in OECD countries and increase tenfold in non-OECD economies by 2060 (OECD, 2016[5]).
8. While measures undertaken in response to the COVID-19 pandemic have seen a substantial improvement in outdoor air quality in many parts of the world, and will have saved lives as a result of improved outdoor air quality, these positive effects are likely to be only temporary. As economies begin to recover from the pandemic, resumptions in air travel, movements of people within and between cities, and production levels in factories will see an increase in outdoor air pollution (although it remains to be seen whether some of the travel-related behavioural changes induced by the pandemic response measures persist). At the same time, confinement measures can result in increased exposure to indoor air pollution. This is particularly relevant for developing countries where many people still rely on polluting fuels for cooking stoves and heating (Bannerji, 2020[6]). Furthermore, indoor air pollution is an issue for buildings and small shops lacking, or with poor, ventilation systems. Circulation of people in buildings with poor ventilation, including hospitals, can also facilitate the spread of COVID-19 and other viruses (Xu, 2020[7]).
Good air quality generates wide societal benefits
9. Available evidence indicates that efforts to improve air quality lead to rapid improvements in health, which have been noticed as little as one week following reduced exposure (Schraufnagel et al., 2019[8]). For example, reductions in air pollution leading up to the 2008 Olympic Games in Beijing resulted in lower biomarkers of inflammation and higher birthweights among residents. When pollution levels later rebounded, these indicators deteriorated (Mu, 2019[9]). This experience highlights the importance of maintaining air quality regulations during shocks such as COVID-19, despite pressures that may emerge to relax such regulations in the light of a temporary improvement in air quality or a push to reduce the compliance costs associated with such regulations.
10. Good air quality not only has the merit of potentially reducing the vulnerability of individuals and communities to pandemics similar to COVID-19, but also of generating wider benefits for public health, well-being and resilience. Reduced air pollution decreases damage to crops, forests, ecology and buildings. There is also a potential boost to efforts to tackle climate change, since air pollution and climate change are closely related. The main causes of greenhouse gas emissions (fuel combustion from electricity, industry and transport), are also major sources of air pollution. In turn, air pollutants contribute to the warming of the atmosphere4. In addition, there are significant economic benefits from improved air quality as a result of fewer air pollution-related illnesses, which means less money spent on medical treatments and reduced impact on work productivity through lower absenteeism from illness. The economic welfare benefits of cleaner air have been demonstrated to outweigh the costs by at least 30-to-1 in the case of the US, while they could be at least 14-to-1 in the case of Europe under tighter regulation (Amann, 2017[10]) (Sullivan, 2018[11]).
11. As economic activity picks up, the transport and industry sectors will continue to play crucial roles in efforts to improve air quality and enhance environmental health and resilience. In the transport sector, the pandemic could trigger a number of effects, including behavioural changes – such as more teleworking and teleconferencing and changes in business models – which could in turn translate in reductions of emissions from transport. On the other hand, there could be a shift away from public transport, driven by fear of contagion, and reliance on single-occupancy cars, which would significantly increase emissions. Stimulus packages should encourage cleaner vehicle fleets and avoid lock-in in the existing mobility paradigm based on private vehicle ownership and low-occupancy vehicle use. In the case of the industry sector, the immediate priorities will clearly be on restarting and revitalising production and jobs in the face of the significant demand shock that has been experienced around the world. At the same time, there is a recognition that cleaner production provides economic benefits to firms as well as the community and that broader sustainability considerations are essential to the future health of industry. Recovery and stimulus packages provide an opportunity to reinforce the need for cleaner production and continued reductions in air pollution emissions.
Continue to enforce existing air pollution regulations during the COVID-19 crisis and after the crisis.
Develop comprehensive strategies to achieve air quality objectives, including through better integration of land use planning, transport and environmental policies, implementing economic instruments to address pollution from mobile and stationary sources, and improving data collection and quality across monitoring networks.
Channel financial support measures to public transport providers to enhance capacity and quality (with focus on reducing crowding and promoting cleaner facilities).
Encourage companies to continue to develop cleaner production methods, in particular with respect to emissions of air pollutants, and strengthen the use of economic and regulatory instruments to support such developments.
Clearly communicate the need to ensure proper ventilation and indoor air quality during confinement, especially in areas heading into winter and those relying on wood burning. After the COVID-19 crisis, support the diffusion of cleaner heating and cooking systems to improve resilience to possible future epidemics.
Improving access to clean water and sanitation and ensuring financial sustainability of utilities
12. The spread of SARS-CoV-2 is closely related to water and sanitation. One of the key recommendations to prevent transmission of the virus and help people stay healthy is to regularly wash hands, which can be particularly challenging in many developing countries5. A significant share of the global population currently lacks access to water and sanitation services that support health and hygiene. Further, the health crisis and the associated economic crisis may reduce the ability of water utilities to provide essential services due to budgetary pressures. Wastewater could also provide useful information on the incidence of the virus within communities. Research suggests that screening for the SARS-CoV-2 at municipal wastewater plants can play an important role in following the evolution of the pandemic and even detecting outbreaks in advance (KWR, 2020[12]).
Handwashing is key to preventing transmission of the virus. Yet many people in developing countries currently lack access to water and sanitation services.
Access to clean water and sanitation services is key for public health and reducing transmission of infectious diseases
13. Globally, an estimated 2.2 billion people lack access to safely-managed drinking water services, and 4.2 billion people do not have safely-managed sanitation services (WHO and UNICEF, 2019[13]). For developing countries, improving access to these services should be a top priority, with a particular consideration for women, which are often responsible for gathering water and suffer most from inadequate access to sanitation.6 While a vast majority of households in developed countries have access to safe water services, this is not the case for vulnerable groups, including homeless people, people living in informal settlements and poor households.
14. Further, WHO and UNICEF estimate that globally 3 billion people lack hand hygiene facilities at home, including alcohol-based hand rubs as well as soap and water, and that two out of five health care facilities lack hand hygiene at points of care (WHO and UNICEF, 2019[14]). In addition, supply shortages due to the ongoing emergency, have made access to hand hygiene products more challenging.
15. Though providing universal access to safely-managed drinking water and sanitation services requires significant time and resources, short-term options can also be employed, such as providing hand hygiene products in the form of alcohol-based hand rubs. Where handwashing with water and soap is not possible, a liquid soap solution, mixing detergent with little water, can be used. In addition, safe water and hand hygiene products should be readily provided in healthcare centres, schools, transportation hubs, and other community buildings.
Affordability issues are expected to intensify
16. The economic impact of the health crisis will very likely affect average household income, increasing the pervasiveness of affordability issues for some households and for water and sanitation utilities. Reduced cash flows combined with pressures on municipal budgets can result in pressure on utilities’ finances, generating strain to continue to deliver essential services. The challenge is to secure revenues for utilities and to maintain capital investment and timely spending on maintenance, while guaranteeing access to households who cannot pay.
17. Direct support to households, which in some countries has been included in relief packages adopted in response to the COVID-19 pandemic, should account for affordability issues related to water bills wherever this is an issue in the context of overall burdens on households. More broadly, the best option is to apply tariffs that reflect the true cost of supplying water and sanitation services, and address affordability issues through targeted social measures to avoid undermining the financial viability of utilities delivering services. In countries that do not have the administrative capacity to identify households in need of financial support, social tariffs and adapted tariff structures can be considered. In the context of the current crisis, disconnection (or reduced access) due to lack of payment is particularly detrimental, potentially amplifying health risks and suffering for poor households. Where social measures reduce revenues of utilities, public support is required to ensure utilities have the financial resources to operate and continue to deliver safe water and sanitation services to their customers, now and in the future, in urban and rural environments alike.
18. In the longer term, stimulus packages should consider public support to invest in water infrastructure development and modernisation. Water supply and sanitation, mitigation of water risks (risk of shortage, excess water or polluted water) should feature high on global, national and local investment agendas, as water security contributes to sustainable growth and to mitigating risks of future epidemics, some of which are likely to be waterborne (including cholera, Ebola, and all diseases spread by mosquitoes grown in stagnating water).
Secure delivery of safe and reliable water and sanitation services to communities paying special attention to vulnerable groups, through for example public fountains and public water taps. Communicate clearly on the measures taken to improve water safety.
Provide access to hand hygiene stations (either for handwashing with soap or for hand rubbing with alcohol-based rubs) in all public buildings and transportation hubs.
Response and recovery efforts should address water affordability issues for households through targeted social measures (e.g. in the context of direct support to households) and shore up the financial viability of utilities delivering essential services as needed.
In the longer term, stimulus packages should consider public support to invest in water-related infrastructure development and modernisation, leveraging private sector investment where feasible.
Systematically screen and share information on SARS-CoV-2 in wastewater before treatment, as an early warning system on the health of the connected population and use the information to inform response measures such as quarantine of communities or increased and targeted monitoring.
Addressing waste generation, management and recycling
19. The current pandemic also raises challenges regarding waste generation, management and recycling practices. Governments need to treat waste management, including medical, household and other hazardous waste as an urgent and essential public service in order to minimise possible secondary impacts upon health and the environment.
Effective waste management is essential to minimise possible secondary impacts upon health and the environment from COVID-19.
Large amounts of medical and hazardous waste can hamper safe and environmentally sound treatment
20. Medical waste generation increases exponentially in an epidemic outbreak and it may, if improperly collected or treated, accelerate disease spread and pose a significant risk to medical staff, patients and waste collection and treatment staff. Medical and hazardous waste include infected masks, gloves and other personal protection equipment (PPE). The safe and environmentally sound handling, treatment and final disposal of this waste is therefore essential to prevent negative effects on human health and the environment.
21. During the height of the outbreak in Wuhan, for example, the city was dealing with 240 tons of medical waste a day, compared to around 40 tons a day before the outbreak (Zuo, 2020[15]). Medical waste facilities are also confronted with an influx from unusual sources, such as planes and cruise ships where passengers have tested positive and were quarantined.
22. Medical waste should be safely collected in designated containers and bags, then safely disposed of or treated, or both. Workers should be provided with appropriate PPE and be trained on how to correctly remove it to prevent contagion. Best practices include assigning responsibility at all governance levels and sufficient human and material resources to safely dispose of such waste (WHO, 2020[16]).
Managing household waste is critical to protect people
23. Household waste also needs to be properly managed during the COVID-19 emergency. Firstly, generation of cleaning and disinfecting waste has increased. At the same time, medical waste, including unused medication, and other items can easily become mixed with domestic garbage, while it should be treated and disposed of separately.
24. Initial research indicates that the SARS-CoV-2 can live on materials such as cardboard and plastic, for multiple hours, up to days, and could therefore be transmitted by touching a surface or object that has the virus on it and then touching their own mouth, nose or eyes (van Doremalen et al., 2020[17]). Therefore waste and recycling workers face a risk of exposure to the virus. This has prompted some municipalities to alter their collection policies, with instances in which they decided to stop collection and sorting of recyclables from household waste altogether. Reduced collection has also occurred in countries where deposit-refund-systems are in place, as a result of consumers not returning bottles due to social distancing and self-isolation. This can also lead to a reduction of supply in post-consumer bottles for recycling (Barrett, 2020[18]).
25. Longer-term impacts on people’s health can stem from improper management and recycling, rolling back plastic reduction and recycling measures that countries had in place before the crisis. The perceived role of and public attitudes to single-use-plastic (SUP) has changed during the crisis. Consumers are using more SUP than previously, for a number of reasons. They are perceived safer as reducing the risk of virus spread, plus they often represent the only option for restaurants and other operators that continue to serve during the crisis but are limited to take-out and delivery options. Following this logic, some countries have put in place waivers or delays of bans on usage of SUP bags, amid discussion that reusable bags are perceived as unsanitary.
Effectively manage biomedical and health-care waste through appropriate identification, collection, separation, storage, transportation, treatment and disposal in order to ensure the minimisation of impacts upon human health and the environment from these potentially hazardous waste stream.
Provide guidance and training to workers involved in both formal and informal waste collection and management systems.
Maintain plastic reduction and recycling measures.
In the longer term, use stimulus packages to strengthen the ability of waste management systems to address the challenges of highly contaminated waste.
Halting and reversing biodiversity loss
26. Humans have transformed the majority of the world’s ecosystems, destroying, degrading and fragmenting terrestrial, marine and other aquatic habitats, and undermining the services they provide. This interference – in particular, the destruction of natural habitat and wild animal trade – has altered the abundance of, and interaction between, hosts and vectors of infectious diseases. Natural habitat destruction and the increased contact with wildlife exposes humans to virus-carrying animals via zoonotic transfer. While the origin of the SARS-CoV-2 is yet to be fully established, it is clear that over-exploitation of habitats and wildlife trade can play an important role in disease propagation.
Threats to biodiversity exacerbate risks of future pathogen outbreaks
27. Human interference with biodiversity – such as deforestation, habitat degradation and fragmentation, agriculture intensification, wildlife trade, and climate change – helps to create the conditions for pathogens to leap from animals to humans. Scientists estimate that zoonotic diseases – that is, disease agents that transfer from animals to humans – account for three-quarters of new or emerging diseases in humans (CDC, 2017[19]). Many deadly pathogens in recent memory – Ebola, HIV, dengue, SARS, MERS, Zika, West Nile – have taken this interspecies leap.
28. Today’s COVID-19 global crisis is a stark reminder of the complex links between the transmission of infectious diseases and biodiversity. Biodiversity loss is associated with the transmission of a range of pathogens, while land conversion and wildlife trade bring more people into contact with potentially new diseases. Threatened species whose population is reduced due to overexploitation (for instance, through hunting and wild animal trade) or habitat loss (for example, landscape alteration such as forest fragmentation, development and conversion to cropland) have over twice as many zoonotic viruses compared to threatened species listed for other reasons (Johnson et al., 2020[20]).
29. The food system in particular, through its relationship between animals and the natural environment, has been a major potential factor of disease (e.g. the Creutzfeld-Jacob and H5N1 diseases). Land-use change, via agriculture expansion and intensification are key pressures on biodiversity. The homogeneity and concentration of crop and animal varieties also encourage the propagation of disease agents. The food system must therefore adapt in order to limit this risk, but also to ensure its resilience and food security.
30. The benefits biodiversity and ecosystem services provide are immense and go far beyond disease protection to include crop pollination, water purification, flood protection, carbon sequestration and clean air, the last of which can be important in reducing the risk of acute respiratory symptoms, frequently present with COVID-19 (see section above Improving air quality for well-being and resilience). The most comprehensive global estimate suggests that ecosystem services provide benefits of USD 125-140 trillion per year i.e. more than one and a half times the size of global GDP. The costs of inaction on biodiversity loss are high. Between 1997 and 2011, the world lost an estimated USD 4-20 trillion per year in ecosystem services owing to land-cover change and USD 6-11 trillion per year from land degradation (OECD, 2019[21]).
31. Effective biodiversity conservation and sustainable use, including to address deforestation, will limit the risk of zoonotic transfer while also helping to maintain the existing wealth ecosystem services. An ambitious and effectively implemented Post-2020 Global Biodiversity Framework under the United Nations Convention on Biological Diversity is one venue for policy change that can help mitigate future disease outbreaks. Governments must scale up the suite of policy instruments for biodiversity protection and get the economic incentives right to ensure biodiversity is better reflected in producer and consumer decision-making (OECD, 2019[21]). Governments should, for example, consider the cost of disease transmission from animals to humans when risking a disturbance to natural habitats.
32. Businesses and investors also depend on biodiversity and ecosystems services for the production of goods and services, yet businesses’ awareness of and commitment to biodiversity action remain too limitedNo source specified.. Businesses have a key responsibility to help protect biodiversity and the ecosystem services they provide. OECD provides recommendations and guidance to help companies ensure due diligence with respect to environmental risks across their operations, including throughout their supply chains.7
Support an ambitious and effective Post-2020 Global Biodiversity Framework under the United Nations Convention on Biological Diversity.
Scale up policy instruments to create the economic incentives to conserve and sustainably use biodiversity, such as forest protection, and to address illegal and poorly managed wildlife trade.
Mainstream biodiversity into economic sectors and reform subsidies harmful to biodiversity, including in the agricultural sector.
Integrate biodiversity factors in business and investment decisions, including through responsible supply chain management.
References
[10] Amann, M. (2017), Costs, benefits and economic impacts of the EU Clean Air Strategy and their implications on innovation and competitiveness, IIASA, https://ec.europa.eu/environment/air/pdf/clean_air_outlook_economic_impact_report.pdf.
[6] Bannerji, A. (2020), Has India’s ’airpocalypse’ put the poor more at risk from coronavirus?, https://news.trust.org/item/20200414122042-jc9jj/.
[18] Barrett, A. (2020), “Impact of Corona on European Recycling Industry”, Bioplastics News, https://bioplasticsnews.com/2020/03/24/impact-corona-european-recycling-industry (accessed on 16 April 2020).
[19] CDC (2017), Zoonotic Diseases, https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html (accessed on 16 April 2020).
[4] Cui, Y. (2003), Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study, https://doi.org/10.1186/1476-069x-2-15.
[20] Johnson, C. et al. (2020), “Global shifts in mammalian population trends reveal key predictors of virus spillover risk”, Proceedings of the Royal Society B: Biological Sciences, Vol. 287/1924, p. 20192736, http://dx.doi.org/10.1098/rspb.2019.2736.
[12] KWR (2020), What we learn about the Corona virus through waste water research, https://www.kwrwater.nl/en/actueel/what-can-we-learn-about-the-corona-virus-through-waste-water-research (accessed on 16 April 2020).
[9] Mu, L. (2019), Metabolomics Profiling before, during, and after the Beijing Olympics: A Panel Study of Within-Individual Differences during Periods of High and Low Air Pollution, http://dx.doi.org/doi: 10.1289/EHP3705.
[21] OECD (2019), Biodiversity: Finance and the Economic and Business Case for Action - report prepared for the G7 Environment Ministers’ Meeting.
[5] OECD (2016), The economic consequences of outdoor air pollution: Policy Highlights, OECD Publishing, https://www.oecd.org/environment/indicators-modelling-outlooks/Policy-Highlights-Economic-consequences-of-outdoor-air-pollution-web.pdf.
[8] Schraufnagel, D. et al. (2019), “Health Benefits of Air Pollution Reduction”, Annals of the American Thoracic Society, Vol. 16/12, pp. 1478-1487, http://dx.doi.org/10.1513/annalsats.201907-538cme.
[11] Sullivan, T. (2018), Air pollution success stories in the United States: The value of long-term observations, Environmental Science & Policy, https://doi.org/10.1016/j.envsci.2018.02.016.
[17] van Doremalen, N. et al. (2020), “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1”, New England Journal of Medicine, Vol. 382/16, pp. 1564-1567, http://dx.doi.org/10.1056/nejmc2004973.
[16] WHO (2020), Water, sanitation, hygiene, and waste management for the COVID-19 virus - Interim guidance, https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19 (accessed on 16 April 2020).
[1] WHO (2020), “WHO website”, https://www.who.int/.
[2] WHO (2018), Ambient (outdoor) air pollution, https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health.
[13] WHO and UNICEF (2019), Progress on household drinking water, sanitation and hygiene 2000-2017, https://www.who.int/water_sanitation_health/publications/jmp-report-2019/en/.
[14] WHO and UNICEF (2019), WASH in health care facilities - Global baseline report 2019, https://www.who.int/water_sanitation_health/publications/wash-in-health-care-facilities-global-report/en (accessed on 16 April 2020).
[3] Wu, X. et al. (2020), Exposure to air pollution and COVID-19 mortality in the United States, Cold Spring Harbor Laboratory, http://dx.doi.org/10.1101/2020.04.05.20054502.
[7] Xu, C. (2020), The 2019-nCoV epidemic control strategies and future challenges of building healthy smart cities, https://journals.sagepub.com/doi/10.1177/1420326X20910408.
[15] Zuo, M. (2020), “Coronavirus leaves China with mountains of medical waste”, South China Morning Post, https://www.scmp.com/news/china/society/article/3074722/coronavirus-leaves-china-mountains-medical-waste (accessed on 16 April 2020).
Notes
SARS-CoV-2 refers to the virus, while COVID-19 indicates the disease.
At the time of writing, the study is a working paper which has not yet undergone peer review.
Particulate matter (PM) is made up of tiny particles of chemicals (such as sulphur dioxides and nitrogen oxides), soil, smoke, dust or allergens. PM2.5 refers to fine inhalable particles, with diameters that are generally 2.5 micrometers and smaller.
A forthcoming OECD policy brief on climate change and COVID-19 will be released shortly.