Intimate partner violence (IPV) has long been characterised as a health crisis. As it is a common point of entry to social services for victims/survivors, the health sector offers meaningful opportunities to mainstream and integrate responses to IPV. This chapter explores how OECD countries have used integrated service delivery (ISD) based in health care to support women affected by IPV. It examines integrated responses in hospital and outpatient settings, as well as targeted mental health initiatives. While most health care systems in the OECD use referral protocols to link victims/survivors with specialised services, governments must ensure that sufficient specialised services exist and are better linked to meet victims/survivors’ needs.
Supporting Lives Free from Intimate Partner Violence

3. Integrated service delivery to support victims/survivors’ physical and mental health
Abstract
Key findings of this chapter
The health care sector is a common point of entry to social services for women experiencing gender-based violence (GBV), or more narrowly, intimate partner violence (IPV) – the focus of this report. Women affected by IPV often seek help from health care providers to address the physical or psychological consequences of their abuse, and in many ways the health sector is historically the most advanced in terms of offering an integrated, multisectoral response for victims/survivors.
Screening for IPV in health care settings is a helpful way to encourage women who experience violence to come forward, and it offers an opportunity to ensure that appropriate supports are provided.
While there is already evidence that health care facilities are central hubs for cross-sector co‑operation, co-location and referral pathways, more can be done to strengthen their central role in co‑operation – for instance, through more training for staff.
OECD member countries frequently report initiating integrated service delivery (ISD) out of hospitals, either based on co-location or referrals to local partners. These often play a dual role in that they help respond to crises in the immediate aftermath of violence and provide the infrastructure for longer-term health resources.
Victims/survivors of IPV often experience deep and long-term effects on their mental health, so mental-health services are crucial in helping women exposed to violence. Many OECD members have made integrated service delivery in the form of multidisciplinary counselling centres, often co‑ordinated at the national level, that help ensure that victims/survivors receive holistic support.
3.1. The health sector frequently encounters women experiencing IPV
The health sector is one of the most common points of entry to public services for help-seeking women affected by gender-based violence (GBV), and more specifically, intimate partner violence (IPV), the focus of this report. Most women access medical care at some point in their lives, and women experiencing IPV, in particular, are more likely to need repeated health care interventions than women who are not abused by their partner (Dillon et al., 2013[1]; Garcia-Moreno and Amin, 2019[2]; World Health Organization, 2009[3]). The health sector is therefore uniquely placed to offer safe and confidential spaces for women to receive support (World Health Organization, 2009[3]).
IPV presents numerous threats to women’s health (Box 3.1). Physical injuries can vary from superficial bruising to injuries that can require long-term rehabilitation, interrupt daily routines such as work attendance and social engagements, or leave women disfigured. Physical violence has also been shown to have (often undocumented) cognitive and neuropsychological consequences as a result of traumatic brain injuries caused by blows to the head (Valera et al., 2019[4]). Other physical health consequences include sexual and reproductive health issues in the wake of forced sexual activity, such as sexually transmitted infections, unintended pregnancies, and pregnancy complications (Oram et al., 2022[5]).
IPV can also severely affect women’s mental health and well-being. Mental health issues – such as depression, anxiety, post-traumatic stress disorder and suicidal ideation – frequently co‑occur alongside physical injuries, especially when these are inflicted by a known and (formerly) trusted individual like an intimate partner. IPV can and does also directly affect women’s mental health and well-being even in the absence of physical abuse/injury. Psychological and emotional abuse is also often directly deployed by perpetrators in an effort to control their partners (Oram et al., 2022[5]). Emotional and psychological abuse and coercive control can then in turn significantly impact mental health and well-being, with knock-on effects on physical health, social and economic participation, income.
Box 3.1. Substance use coercion complicates escape from a violent partner – and complicates treatment by service providers
The United States Department of Health and Human Services has elevated an important challenge that can accompany intimate partner violence: substance use coercion. Substance use coercion occurs “when perpetrators of intimate partner violence undermine and control their partners through substance‑use related tactics and actively keep them from meeting treatment and recovery goals”. Abusers who carry out substance use coercion may force or pressure their partner to use drugs, for instance, or sabotage recovery efforts. A survey of callers to the US National Domestic Violence Hotline found that at least four out of ten respondents had experienced some form of substance use coercion: a partner pressuring them to use substances, a partner threatening to report their substance use to the authorities, or the victim/survivor’s fear of calling the police because of their substance use (ibid).
Health care services are an important consideration in cases of substance use coercion by abusers. In addition to the potential physical and mental health consequences of substance abuse for the user, coercive substance abuse can also limit victims/survivors’ ability to engage with health services and treatment. In addition to the direct health-related impacts, substance use coercion can prevent victims/survivors from retaining custody of their children and becoming economically self-sufficient. These compounding issues heighten the importance of an integrated, holistic service delivery response.
3.2. Tools for detecting IPV should join up with a system of referrals in health
A major challenge to ending IPV is that much of the violence takes place in private. Although women experiencing IPV access health services more frequently than non-abused women, they may not be forthcoming about disclosing abuse (for more on barriers to disclosure, see Chapter 2). This greatly complicates the process of identifying and treating victims/survivors of IPV.
Health care professionals are well-placed to screen their clients for IPV. There is an ongoing debate about the benefits of two different approaches: universal screening versus routine enquiry for IPV among patients entering health services. Routine enquiry seeks to identify IPV through routine wellness questions, whereas universal screening entails an official and typically standardised screening tool1.
It has been argued that universal screening should be implemented particularly in settings that both perpetrators and victims/survivors come into contact with, such as family and couples therapy and nurse‑midwives (Todahl and Walters, 2011[8]; Paterno and Draughon, 2016[9]). For instance, at the first prenatal check-up appointment for pregnant women in Chile, women are screened using the abbreviated psychosocial risk scale (EPsA) (OECD QISD-GBV, 2022, see Annex A). The WHO recommends the routine enquiry approach, but a recent survey of country policies finds that only about one‑quarter of countries regularly apply this approach in their health care systems. Around 10% of countries apply universal screening, while the rest do not have a standard approach to identifying IPV (World Health Organization, 2021[10]).
Although both methods of screening can be effective in increasing identification of women experiencing IPV, studies are inconclusive as to whether they substantively improve health outcomes following identification by health care practitioners. This is due, at least in part, to a dearth of measured outcomes, post-screening follow-up and programme evaluation. Currently, rates of referral act as the primary measurable outcome of screening in research studies, as opposed to whether or not referrals are successful in securing safety for help-seeking women (Sprague et al., 2016[11]; World Health Organization, 2013[12]).
As a minimum standard, the WHO highlights the need for a standardised operating procedure to ensure first-line support for women who do disclose violence. In addition to an official protocol, first-line support through health services should include training for health professionals to learn how to ask about and discern IPV, with particular emphasis on being able to do so in a private setting that ensures confidentiality (World Health Organization, 2013[12]). The WHO highlights the importance of effective responses when IPV is revealed, otherwise women may find repeated enquiry difficult, particularly if no action is taken (World Health Organization, 2013[12]).
Screening is most fruitful when support services can be offered after the disclosure of violence. Good ways of establishing channels of communication regarding IPV cases include cross-agency partnering, set referral pathways, and co-location. However, a recent literature review of studies evaluating screening processes found that out only a minority of those screened who had experienced IPV were referred to follow-up psycho-social services. According to the review, part of the issue is that a lack of referral services undermines the effectiveness of screening processes in obtaining positive outcomes in health care, notably due to insufficient cross-sectoral collaborations with IPV-service advocates (Miller et al., 2021[13]). Simply put, providers had few places to send women who revealed abuse and needed support outside of the immediate health care environment.
More evaluations will be helpful to determine how best to implement screening tools, and how other services, referral pathways and training can be joined-up to provide immediate support for those who disclose. Future research could focus on measuring different outcomes, and especially longer-term results.
Some countries have prioritised strengthening health systems’ capacity to respond to IPV through the national health care system. For example, Spain has published national guidelines aimed at healthcare practitioners to help them actively look out for warning signs of IPV, confirm suspected cases, and when detected, to determine their nature and severity (Escribá Agüir et al., 2009[14]). Similarly, in the United Kingdom, national-level guidance has been issued on how the National Health Service (NHS) can respond to violence against women and children (Taskforce on the Health Aspects of Violence Against Women and Children, 2010[15]; Department of Health, 2017[16]). This has included official guidance to support health care professionals following disclosures of IPV. It notes the importance of risk assessments and referring women to related health professionals or external resources like multi‑agency risk assessment conferences known as “MARACs” (Chapter 2) (Department of Health, 2017[16]). The United Kingdom also provides a so-called “Quality Standard” to help improve the quality of care for services related to domestic violence and abuse (National Institute for Healthcare Excellence, 2016[17]; Macdonald, 2021[18]). Of course, these kinds of national guidelines are most useful when accompanied with the necessary funding to ensure that providers can in fact act upon the guidelines.
Strategic planning for IPV responses in health care settings have also been observed at the subnational level. For example, in New South Wales, Australia, the recent strategy (2021‑26) for preventing and responding to domestic violence also outlines six strategic directions including improving identification protocols to enhance early interventions and providing integrated responses for people experiencing domestic violence (NSW Health, 2021[19]).
3.3. Developing integrated responses to IPV via health systems
Health care offers governments a significant opportunity to form policy recommendations and delineate minimum services to respond to IPV. Indeed, the World Health Organization has encouraged policy makers to strengthen health systems in promoting a multi-sectoral response to violence against women since 2009. In 2014, a resolution was put forward calling on countries to integrate GBV-specific responses better within the health care system, including through standardised procedures for the identification and referral of GBV cases (World Health Organization, 2014[20]).
In light of the relatively frequent contact between health care professionals and women experiencing IPV, the sector has in many ways been more advanced, historically, than other sectors in integrating targeted service delivery. Indeed, in a 2021 review, the WHO found that 81% of countries have multi-sectoral policies that aim to prevent and/or respond to violence against women. The health sector is most frequently involved in multi-sectoral policies: out of surveyed countries with multi-sectoral policies to address violence against women, 86% include the health sector, while only 61% include the police (World Health Organization, 2021[10]).
3.3.1. Integrated service delivery in health care settings can take a variety of forms
There is a variety of definitions of how integrated service delivery takes shape in the health care sector. One literature review on the definitions identified over 150 overlapping definitions of integrated care (Armitage et al., 2009[21]). Variation in definitions and mechanisms hampers the comparability of integrated care initiatives across countries and its expected outcomes. Terms such as integrated care, co‑ordination of care, continuing care, care pathway and seamless care are used interchangeably, while different views are reflected in these definitions, including those from patients, providers and policy makers.
The literature often refers to some broad considerations when conceptualising common models of service delivery. First, it is valuable to note the breadth of services available, ranging from offering a package of preventive health interventions, acute crisis response and post-crisis continuity of care. Second, models of integration will be characterised by the time‑span of the continuity of care, since integration can be oriented towards a specific episode of care (e.g. postnatal follow-up), stages in a person’s life cycle (e.g. maternity) or adopting a life‑course approach. Third, the intensity of integration is relevant, and range from partial integration, with non-binding linkages or ties between two sectors, to full integration, involving process of integrating health and social sectors into a new organisational model (Barrenho et al., 2022[22]).
This chapter considers three common models of service delivery are common to facilitate integrated responses to IPV against women through an entry point in the health care secto (Colombini, Mayhew and Watts, 2008[23]):
Provider integrated: The same provider offers several services during the one single consultation. For example, “a nurse in accident and emergency is trained and resourced to screen for domestic violence, treat her client’s injury, provide counselling and refer her to external sources of legal advice”.
Facility integrated (co-located): All services are available in one facility, though are not delivered by a sole provider. For example, “a nurse in accident and emergency may be able to treat a woman’s injury, but may not be able to counsel a woman who discloses domestic violence, and may need instead to refer the woman to the hospital medical social worker for counselling.” This is in line with the “co-located delivery” model discussed in Chapter 1.
Systems-level integrated (referral pathways): A coherent referral system exists between facilities in different locations. For example, “a family-planning client who discloses violence can be referred to a different facility (possibly at a different level) for counselling and treatment”.
Systems-level integrated service delivery to treat IPV in health care settings is often based on case management, MARACs, or referrals (Chapter 2). Figure 3.1. illustrates how a woman with physical or mental-health care needs brought about by experiences of IPV could present herself at a primary care doctor, clinic, or hospital and then be referred to resources in the social and justice sectors – or vice versa. Alternatively, a woman could be introduced to a case manager who helps her navigate this system. Where case‑relevant information can be shared along with a referral or by the case manager, support might be more efficiently provided (see Chapters 1 and 6 for more).
Figure 3.1. Example of a GBV referral network in health care
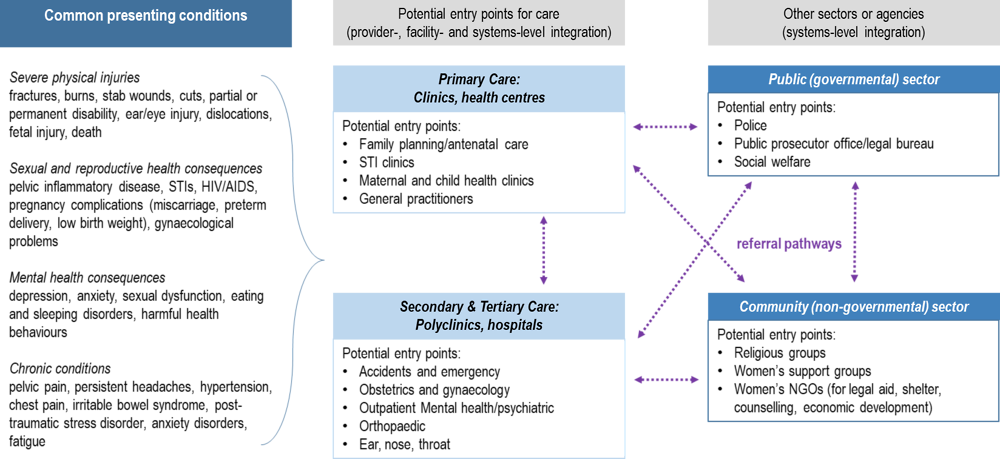
Source: Adapted from original model in Colombini, Mayhew and Watts (2008, p. 639[23]), “Health-sector responses to intimate partner violence in low- and middle-income settings: a review of current models, challenges and opportunities”, https://doi.org/10.2471/BLT.07.045906.
3.3.2. Lack of training can hamper responses by health care providers
Time and resource constraints, especially where health services are overstretched, limit the capacity to respond effectively to disclosures of violence (World Health Organization, 2013[12]). Inadequate funding, in particular, is a commonly-cited challenge across government and non-government providers (Chapter 6). Reliable and adequate funding for everyone involved is crucial to allow different agencies to build relationships and referral pathways.
Lack of implementation guidance and training have also been cited as hindering integration of IPV and health care services. Article 15 of the Istanbul Convention suggests that parties provide or strengthen training initiatives across sectors for relevant professionals dealing with victims/survivors of GBV. This includes training on issues such as gender equality and mutual respect, as well as co‑ordinated multi‑agency co‑operation (Council of Europe, 2022[24]). For example, in a recent cross-national review of IPV-specific support services, GREVIO – the monitoring arm of the Istanbul Convention – highlights the introduction of graduate programmes dedicated to studying violence against women in Spain, as well as the introduction of men’s violence against women as a compulsory subject for university students in Sweden (Council of Europe, 2022[24]).
While the obligation to provide training around IPV is crucially important for the health sector, in particular, countries have not always managed to implement this successfully. In 2017, a survey of 24 of the UK’s 34 medical schools showed that 21 institutions delivered some education around domestic violence. However, 15 of these schools providing some training still felt the training was inadequate, and 11 of the schools providing some training reported that their contact hours on the topic were two hours or less over the five‑year course (Potter and Feder, 2018[25]).
One potentially promising approach is to embed IPV experts from community organisations or other sectors within existing health care institutions. This was the strategy used in the successful Themis and Pathfinder pilots carried out in the United Kingdom (Box 3.2). Since these efforts often target victims/survivors in relatively severe situations, it should be noted that such initiatives should be combined with preventative strategies and provisions for early intervention, as discussed in Chapter 2.
Box 3.2. Piloting Independent Domestic Violence Advisors (IDVA) throughout the UK health sector
On the ground, a series of promising pilots in England appointed Independent Domestic Violence Advisers (IDVAs) across National Health Service sites to act as case managers for women experiencing IPV. Since the pilots ended in 2020, IDVAs have remained co-located in some sites, and have even emerged in hospitals not originally included in the pilots. Importantly, Pathfinder is one of the few ISD initiatives for which academics have carried out impact analyses. Studies of the Pathfinder Project find that self-reported well-being improved among users who had gone through the programme – users who may not have been identified at all, had the programme not been deployed (Chapter 1). The model was since adopted as a best practice, and a toolkit was developed to support health leaders in delivering the model, though it is unclear how much progress has been made since 2020 given that its implementation does not appear to be mandatory.
Themis pilot, 2012‑15
In collaboration with SafeLives, a national charity whose mission is to end domestic violence, the UK Government launched Themis, a pilot project which co-located IDVAs in select hospital emergency and maternity wards. The role of IDVAs was multidimensional:
1. provide training to health care workers to better identify cases of GBV;
2. provide immediate support to survivors in the form of safety planning;
3. provide in-hospital referrals, for example, to mental health practitioners;
4. provide off-site referrals, for example to emergency housing, substance use counselling, social workers and police.
Service uptake increased annually throughout the pilot, which delivered services to cis-gendered women and men, as well as to the LGBTI+ community.
Pathfinder pilot, 2017‑20
With the help of a Consortium of non-governmental partners, the Pathfinder Project also saw the co‑location of IDVAs at eight other hospital sites between 2017 and 2020. Over the course of three years, 633 individuals took up domestic abuse services after referral from health care under the Pathfinder project, including some who might otherwise have gone unassisted. According to the technical report conducted by Melendez-Torres and colleagues for SafeLives on the outcomes of the pilot, Health Pathfinder sites had an average quarter-on-quarter increase in referrals of around 10% in each quarter.
With Pathfinder, IDVAs also participated in weekly multi‑agency risk assessment conferences (MARACs) held at the local police station prior to the COVID‑19 pandemic, moving to daily remote (telephone) meetings during lockdowns. Survey evidence from 2019‑20 published by the Consortium indicate that self-reported well-being had increased for users exiting services, with 91% reporting feeling safer and 95% reporting improved well-being. Respondents also report that the abuse was reduced or stopped in many cases, especially when the abuse was physical.
3.4. Hospitals are important sites for an integrated policy response
Medical practitioners in a variety of settings are well-placed to assist individuals experiencing IPV. Alongside efforts to promote early identification and support, health care providers play a critical role in providing physical and mental health support related to experiences of IPV, and hospitals are often a victim/survivor’s first stop in the wake of a violent crisis. Assistance can also be provided during unrelated or routine visits to medical practitioners. This was especially true during COVID‑19, when social-distancing rules limited the number of people allowed to accompany a help-seeking individual in waiting and consultation rooms – thereby increasing women’s privacy during medical appointments.
3.4.1. Member countries have successfully integrated IPV-related services in hospitals
Within wider health care systems, hospitals have been shown to be one important hub for ISD, particularly related to support for victims/survivors of severe violence. There are a few reasons for this. First, hospitals play a critical role in providing acute crisis support; second, they can conduct comprehensive assessments of health and social needs, and develop a plan of interventions and services required to meet needs; and finally, they can sign-post and co‑ordinate access to the services and specialists needed. Countries with publicly-funded health care systems are also well-placed to co‑ordinate responses nationally to implement integrated GBV supports, integrating hospital care with care in other parts of the health care system.
Co-located case management and referral models to support victims/survivors are reported throughout the OECD (Table 3.1) and play an important role over time: they help respond to crises in the immediate aftermath of violence, while also providing infrastructure for certain longer-term health resources. The joined-up service provision can help ensure that resources are used appropriately, with each actor playing a specialised role in a larger system of care, support and prevention.
In Austria, for example, hospitals are legally obliged to establish multidisciplinary protection groups to support adults who disclose instances of domestic violence. In Korea, more care is provided within hospitals, which often provide multidisciplinary centres that offer medical support in addition to psychotherapy and legal counselling for both the immediate victims and their family members.
In Italy, a national directive applied at the subnational level seeks to ensure timely and integrated support for women who disclose violence through a standardised assessment deployed in the health care sector. In the United Kingdom, Independent Domestic Violence Advisers at NHS sites refer clients to related services, though these services are not usually co-located (Box 3.2). And in France, the co-located service provision site Maison des Femmes, in the suburbs of Paris, was founded by a women’s health provider; this model is now being rolled out in new physical sites throughout France (Chapter 6).
Table 3.1. Integrated, hospital-based responses to GBV
|
Country |
Nature of Integration |
Description of services delivered |
|---|---|---|
|
Austria |
Referral pathways |
Through the federal hospital act in Austria, all hospitals are obliged by law to establish “victim protection groups for adult victims of domestic violence” since 2011. The Groups are responsible for facilitating early detection and prevention of domestic violence through awareness raising among hospital colleagues. More importantly, out of recognition that domestic violence requires solutions borne of inter-institutional and inter-disciplinary co‑operation, the main goal of the Group is to establish a network of cross-sectoral actors, including police, shelters, social workers and helpline operators which can then be mobilised to support help-seeking individuals. The Group aims to identify individuals experiencing domestic violence among hospital clients, and to refer them to the nearest “violence protection facility”, or to network contacts (or both), where they can receive a broad spectrum of support. Relatedly, the Groups are responsible for collecting and reporting administrative data on domestic violence according to a specialised scheme. |
|
Finland |
Co-located |
In 2017, the Seri Support Centre was established in the Helsinki Women’s Hospital Department of Obstetrics and Gynaecology with the support of the National Institute for Health and Welfare. The Centre is accessible 24‑hour per day for individuals of any gender aged 16 and older to seek assistance related to experiences of sexual violence occurring less than one month from their visit, without necessarily having to make a police report. The Centre offers crisis care and support, forensic medical examinations, access to psychologists and social workers, medications, vaccinations or emergency contraception, treatment follow-up plans and a referral service to psychiatrists and third sector or municipal officials. The Centre can also make referrals where help-seeking individuals are under the age of 16 or have experienced sexual violence more than one month prior to their visit. There are now 21 SERI Support Centres in Finland, and three more are planned to be established by the end of 2023. |
|
Ireland |
Provider-integrated |
Via the Department of Health, the Health Service Executive directly provides 83 specialised staff in hospitals to respond to GBV cases that are flagged. |
|
Italy |
Referral pathways |
In 2017, the “Pathways for women subjected to violence” was adopted into the National Guidelines for Health Authorities via Prime Ministerial Decree. The programme, which is left to regional authorities to implement, seeks to ensure timely and integrated support for women through the health sector. The Pathway is initiated following an emergency code assessment for which health professionals are trained to deploy. Consenting women are then referred to dedicated regional supports, such as local anti-violence centres, to develop safety planning, access advocates and other resources. The most recent National Strategic Plan on Male Violence Against Women (2021‑23) prioritises improving the effectiveness of the Pathways initiative, including developing monitoring mechanisms in conjunction with the National Statistical Institute of Italy (ISTAT). |
|
Korea |
Co-located |
In 2004, MOGEF began to establish “Sunflower Centres” across the country to provide rapid, inter-disciplinary responses in cases of sexual assault, domestic violence or sex trafficking; over 30 exist nation-wide, many of which are located in hospitals. Twelve of these Centres deploy a “one‑stop service centre” (OSC) model, where all services are available in one location. The one‑stop Centres employ a permanent, multidisciplinary team of 25 specialists to provide medical treatment for injuries, including forensic examinations, as well as counselling and psychotherapy for both the immediate victim and their family members; legal counselling, advice and case‑building support. Support staff is also available to facilitate travel to and from Sunflower Centres. |
|
Norway |
Co-located |
Operating in existing health care settings, such as clinics and hospitals, 23 sexual assault reception centres offer medical care and counselling to help-seeking individuals. Of the 23 centres, six (26%) also accept individuals experiencing domestic violence. |
|
United Kingdom |
Co-located |
The Secretary of State for Health, via the National Health Service (NHS) England, commissions 47 sexual assault referral centres (SARCs) which provide acute health care and psychosocial support, as well as direct access or referral to an Independent Sexual Violence Adviser (ISVA) who acts as a case manager. Though not yet nationally streamlined, Independent Domestic Violence Advisers (IDVAs) are similarly available in hospital settings (see Box 3.2). |
Note: This table presents a non-exhaustive list of ISD practices in health care settings for survivors of violence in the OECD. MOGEF in Korea had recently been abolished and the funding resolution is uncertain.
Source: OECD QISD-GBV 2022 (Annex A); (UNDP, 2019[33]; Austrian Ministry of Social Affairs, 2022[34]).
Hospitals are well-placed to co‑ordinate responses to IPV where there is a need for very acute or crisis care, but that does not necessarily mean they should be hubs for all forms of co‑ordination. It is important to note that hospital care is relatively costly, so to use existing resources most effectively, other settings within the health care system (e.g. those equipped with screening tools (Section 3.2)) might be better placed to support victims/survivors who are not in need of acute physical care. For instance, care can and ought to be co‑ordinated and integrated across settings to maximise the potential of primary health care and mental health services. Indeed, such co‑ordination can help ensure better outcomes for people in vulnerable circumstances, including people with chronic diseases and mental health issues, both of which are common among victims/survivors of IPV (OECD, 2021[35]; OECD, 2020[36]). Where the aim of services is to prevent violence and provide non-acute support for victims/survivors to live lives free of violence, community-based care (Chapter 6) could also serve as good hubs of co‑ordination.
For instance, community-based care is recognised as the preferred approach for most mental health care (discussed in the next section). All OECD countries either already deliver the majority of mental health services outside of hospitals or have prioritised the transition to community-based care models. Community-based care has the potential to deliver care that is less costly than inpatient care, more in line with service users’ preferences, and better integrated with other public services. This could be reflected in ISD responses to broader health needs related to IPV in coming years (OECD, 2021[35]).
3.5. Mental health care support is a critical part of an integrated response to violence
Experiencing physical or psychological violence of any kind can have negative and long-term consequences on a person’s mental health and well-being. These consequences can be exacerbated in situations where violence is perpetrated by a known, trusted or loved individual.
The Lancet Psychiatry Commission lists a range of mental health disorders that are more common among people who have experienced IPV than those who have not, including “anxiety, depression, substance use disorder, post-traumatic stress disorder (PTSD), personality disorders, psychosis, self-harm, and suicidality” (Oram et al., 2022[5]). The Commission also underscores the cyclical and intergenerational relationship between violence and mental ill-health: “Exposure to IPV in childhood or adulthood increases the likelihood of developing a range of mental health problems, suicidal ideation, and attempting suicide. The presence of mental health problems also makes individuals more vulnerable to experiencing IPV. Children who are exposed to IPV […] greatly increase the risk of both experiencing and perpetrating IPV as an adult” (Oram et al., 2022[5])
Countries are working to extend access to dedicated mental health support for victims/survivors of IPV. Responses to OECD QISD-GBV 2022 illustrate policies which integrate mental health support and social support. At the local level in Denmark, for example, since 2020, municipal governments are obligated to offer up to ten hours of free, psychological counselling to women who are staying – or who have stayed – at a shelter as a result of domestic violence. Municipalities are also obligated to offer at least four, and up to ten, hours of psychological support to children accompanying women in this context. Sessions can be used both during and after shelter stays (OECD QISD-GBV, 2022).
Other OECD countries have integrated mental health with other support through multidisciplinary counselling centres co‑ordinated at the national level (Table 3.2). In Costa Rica, for example, the National Institute of Women operates regional units which provide multidisciplinary supports, including psychosocial support, to women experiencing IPV. Similarly, in Greece, the Ministry of Labour and Social Affairs funds a number of dedicated counselling centres which provide targeted mental health services for women experiencing IPV. And in Japan, the national and subnational governments jointly fund and operate several spousal violence counselling and support centres which respond to women’s mental health needs and accompany them to related medical appointments.
Table 3.2. Some counselling centres link mental health care with other social and health services
|
Country |
Description of services delivered |
|---|---|
|
Austria |
The central and regional governments jointly fund a constellation of over 350 multidisciplinary women’s counselling centres, including specialised branches to support women affected by female genital mutilation and forced marriage. Specialised centres also exist which provide family counselling, and men’s counselling, including perpetrator counselling. |
|
Costa Rica |
The National Institute of Women (INAMU) operates 5 Regional Units, as well as the Women’s Delegation in the capital, which provide psychological care to women experiencing violence. Both also provide access to specialised social workers and legal experts. |
|
Greece |
Via the Ministry of Labour & Social Affairs, the Research Centre for Gender Equality (KETHI, https://www.kethi.gr/en/counseling-centers) operates 14 counselling centres which provide mental health services to women suffering from violence or multiple discriminations through multidisciplinary teams that include psychologists, social workers and legal advisors. |
|
Japan |
The Cabinet Office and Prefectures jointly fund and operate over 100 Spousal Violence Counselling and Support Centres (https://www.gender.go.jp/policy/no_violence/e-vaw/soudankikan/01.html) which provide mental health services, as well as referral and accompaniment to medical appointments. |
|
Korea |
As of early 2022, the Ministry of Gender Equality and Family (MOGEF) jointly funded and operated, with municipal governments, counselling centres for sexual violence and domestic violence cases |
|
Mexico |
External Care Centres provide psychological services to women and their children. In 2021, nearly 62 000 women received mental health services from External Care Centres |
Note: This table presents a non-exhaustive list of ISD practices related to mental health for survivors of violence in the OECD. At the time of this reports publication, MOGEF in Korea had recently been abolished and the funding resolution is uncertain.
Source: OECD QISD-GBV 2022 (Annex A).
References
[21] Armitage, G. et al. (2009), “Health systems integration: State of the evidence”, International Journal of Integrated Care, Vol. 9/2, https://doi.org/10.5334/IJIC.316/METRICS/.
[34] Austrian Ministry of Social Affairs (2022), Toolbox OSG, https://toolbox-opferschutz.at/ (accessed on 15 December 2022).
[22] Barrenho, E. et al. (2022), “International comparisons of the quality and outcomes of integrated care: Findings of the OECD pilot on stroke and chronic heart failure”, OECD Health Working Papers, No. 142, OECD Publishing, Paris, https://doi.org/10.1787/480cf8a0-en.
[23] Colombini, M., S. Mayhew and C. Watts (2008), “Health-sector responses to intimate partner violence in low- and middle-income settings: a review of current models, challenges and opportunities”, Bulletin of the World Health Organization, Vol. 86/8, pp. 635-642, https://doi.org/10.2471/BLT.07.045906.
[24] Council of Europe (2022), Mid-term horizontal review of GREVIO baseline evaluation reports, Council of Europe, https://rm.coe.int/prems-010522-gbr-grevio-mid-term-horizontal-review-rev-february-2022/1680a58499 (accessed on 4 October 2022).
[16] Department of Health (2017), Responding to domestic abuse: A resource for health professionals, UK Department of Health, https://www.basw.co.uk/resources/responding-domestic-abuse-resource-health-professionals.
[26] Dheensa, S. et al. (2020), ““From taboo to routine”: a qualitative evaluation of a hospital-based advocacy intervention for domestic violence and abuse”, BMC Health Services Research, Vol. 20/1, p. 129, https://doi.org/10.1186/s12913-020-4924-1.
[1] Dillon, G. et al. (2013), “Mental and Physical Health and Intimate Partner Violence against Women: A Review of the Literature”, International Journal of Family Medicine, Vol. 2013, pp. 1-15, https://doi.org/10.1155/2013/313909.
[31] Elvey, R., T. Mason and W. Whittaker (2022), “A hospital-based independent domestic violence advisor service: demand and response during the Covid-19 pandemic”, BMC Health Services Research, Vol. 22/1, pp. 1-12, https://doi.org/10.1186/S12913-022-08183-Z/TABLES/5.
[14] Escribá Agüir, V. et al. (2009), Protocolo para la atención sanitaria de la violencia de género (PDA), Dirección General de Salud Pública, https://violenciagenero.igualdad.gob.es/profesionalesInvestigacion/protocolosAmbitoAutonomico/sanitario/docs/Protocolo_atencion_sanitaria_Valencia.pdf (accessed on 30 January 2023).
[2] Garcia-Moreno, C. and A. Amin (2019), “Violence against women: where are we 25 years after ICPD and where do we need to go?”, Sexual and Reproductive Health Matters, Vol. 27/1, pp. 346-348, https://doi.org/10.1080/26410397.2019.1676533.
[37] Gerberding, J. et al. (2007), Intimate Partner Violence and Sexual Violence Victimization Assessment Instruments for Use in Healthcare Settings, CDC, https://www.cdc.gov/violenceprevention/pdf/ipv/ipvandsvscreening.pdf (accessed on 14 December 2022).
[28] Halliwell, G. et al. (2019), “Cry for health: a quantitative evaluation of a hospital-based advocacy intervention for domestic violence and abuse”, BMC Health Services Research, Vol. 19/1, p. 718, https://doi.org/10.1186/s12913-019-4621-0.
[6] HHS Family and Youth Services Bureau (2020), Understanding Substance Use Coercion as a Barrier to Economic Stability for Survivors of Intimate Partner Violence: Policy Implications, United States Department of Health and Human Services, Washington, DC, https://aspe.hhs.gov/reports/understanding-substance-use-coercion-barrier-economic-stability-survivors-intimate-partner-violence.
[30] IRISi (2020), Pathfinder Toolkit: New Model Launched to Transform Health System’s Response to Domestic Abuse - IRISi, IRISi, https://irisi.org/pathfinder-toolkit-new-model-launched-to-transform-health-systems-response-to-domestic-abuse/ (accessed on 4 January 2023).
[18] Macdonald, M. (2021), The role of healthcare services in addressing domestic abuse, House of Commons Library, http://www.parliament.uk/commons-library|intranet.parliament.uk/commons-library|papers@parliament.uk|@commonslibrary.
[29] Melendez-Torres, G. et al. (2021), Health Pathfinder: Full Technical Report, SafeLives, https://safelives.org.uk/sites/default/files/resources/Health%20Pathfinder%20Full%20Technical%20Report%20-%20March%202021.pdf.
[13] Miller, C. et al. (2021), “Screening for intimate partner violence in healthcare settings: An implementation-oriented systematic review”, Implementation Research and Practice, Vol. 2, p. 263348952110398, https://doi.org/10.1177/26334895211039894.
[17] National Institute for Healthcare Excellence (2016), Domestic violence and abuse: Quality standard, National Institute for Healthcare Excellence, http://www.nice.org.uk/guidance/qs116.
[19] NSW Health (2021), NSW Health Strategy for Preventing and Responding to Domestic and Family Violence 2021-2026, NSW Health, https://www.health.nsw.gov.au/parvan/DV/Publications/dfv-stratgy-2021-2026.PDF (accessed on 15 December 2022).
[35] OECD (2021), A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill-Health, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/4ed890f6-en.
[36] OECD (2020), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en.
[5] Oram, S. et al. (2022), “The Lancet Psychiatry Commission on intimate partner violence and mental health: advancing mental health services, research, and policy”, The Lancet Psychiatry, Vol. 9/6, pp. 487-524, https://doi.org/10.1016/S2215-0366(22)00008-6.
[9] Paterno, M. and J. Draughon (2016), Screening for Intimate Partner Violence, Journal of Midwifery & Women’s Health, https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/jmwh.12443 (accessed on 26 January 2023).
[25] Potter, L. and G. Feder (2018), “Domestic violence teaching in UK medical schools: a cross-sectional study”, The Clinical Teacher, Vol. 15/5, pp. 382-386, https://doi.org/10.1111/tct.1270610.1111/tct.12706.
[27] SafeLives (2020), Pathfinder Key Findings Report, SafeLives, https://avaproject.org.uk/wp-content/uploads/2020/06/Pathfinder-Key-Findings-Report_Final.pdf.
[32] SafeLives (2016), A Cry for Health Why we must invest in domestic abuse services in hospitals, SafeLives, https://safelives.org.uk/sites/default/files/resources/SAFJ4993_Themis_report_WEBcorrect.pdf (accessed on 3 February 2023).
[11] Sprague, S. et al. (2016), “A Scoping Review of Intimate Partner Violence Screening Programs for Health Care Professionals”, PLOS ONE, https://doi.org/10.1371/JOURNAL.PONE.0168502.
[15] Taskforce on the Health Aspects of Violence Against Women and Children (2010), Responding to violence against women and children: The role of the NHS, The Health Foundation, https://www.health.org.uk/sites/default/files/RespondingtoViolenceAgainstWomenAndChildrenTheRoleofTheNHS_guide.pdf (accessed on 2 December 2022).
[8] Todahl, J. and E. Walters (2011), “Universal screening for intimate partner violence: A systematic review”, Journal of Marital and Family Therapy, Vol. 37/3, pp. 355-369, https://doi.org/10.1111/J.1752-0606.2009.00179.X.
[33] UNDP (2019), Sunflower Center Resource Book | United Nations Development Programme, UNDP, https://www.undp.org/policy-centre/seoul/publications/sunflower-center-resource-book (accessed on 15 December 2022).
[4] Valera, E. et al. (2019), “White Matter Correlates of Mild Traumatic Brain Injuries in Women Subjected to Intimate-Partner Violence: A Preliminary Study”, Journal of Neurotrauma, Vol. 36, https://doi.org/10.1089/neu.2018.5734.
[7] Warshaw, C. et al. (2020), Substance use coercion as a barrier to safety, recovery, and economic stability: Implications for policy, research and practice, National Center on Domestic Violence, Trauma, and Mental Health, http://www.nationalcenterdvtraumamh.org/wp-content/uploads/2020/10/Substance-Use-Coercion-Meeting-Report.pdf (accessed on 15 December 2022).
[10] World Health Organization (2021), Addressing violence against women in health and multisectoral policies: a global status report, World Health Organization, https://www.who.int/publications/i/item/9789240040458 (accessed on 15 December 2022).
[20] World Health Organization (2014), Strengthening the role of the health system in addressing violence, in particular against women and girls, and against children, World Health Organization, https://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_ACONF1Rev1-en.pdf.
[12] World Health Organization (2013), Responding to intimate partner violence and sexual violence against women, World Health Organization, http://www.who.int/reproductivehealth (accessed on 13 December 2022).
[3] World Health Organization (2009), Health-sector responses to violence against women, World Health Organization, https://apps.who.int/iris/bitstream/handle/10665/44456/9789241500630_eng.pdf?sequence=1&isAllowed=y.
Note
← 1. For examples, see those listed in (Gerberding et al., 2007[37]).