[77] Abdel-Razeq, H. et al. (2019), “Intensity of Cancer Care Near the End of Life at a Tertiary Care Cancer Center in Jordan”, Journal of Pain and Symptom Management, Vol. 57/6, pp. 1106-1113, https://doi.org/10.1016/j.jpainsymman.2019.02.016.
[41] Aoun, S. et al. (2020), “The Compassionate Communities Connectors model for end-of-life care: a community and health service partnership in Western Australia”, Palliative Care and Social Practice, Vol. 14, p. 263235242093513, https://doi.org/10.1177/2632352420935130.
[17] Arias-Casais, N. et al. (2019), EAPC Atlas of Palliative Care in Europe 2019, EAPC Press, http://dadun.unav.edu/handle/10171/56787 (accessed on 16 October 2019).
[102] Auriemma, C. et al. (2016), “Public Opinion Regarding Financial Incentives to Engage in Advance Care Planning and Complete Advance Directives”, American Journal of Hospice and Palliative Medicine®, Vol. 34/8, pp. 721-728, https://doi.org/10.1177/1049909116652608.
[59] Bajwah, S. et al. (2021), “Specialist palliative care services response to ethnic minority groups with COVID-19: equal but inequitable—an observational study”, BMJ Supportive & Palliative Care, pp. bmjspcare-2021-003083, https://doi.org/10.1136/bmjspcare-2021-003083.
[6] Bamford, C. et al. (2018), “What enables good end of life care for people with dementia? A multi-method qualitative study with key stakeholders”, BMC Geriatrics, Vol. 18/1, https://doi.org/10.1186/s12877-018-0983-0.
[101] Barnato, A. et al. (2017), “Financial Incentives to Increase Advance Care Planning Among Medicaid Beneficiaries: Lessons Learned From Two Pragmatic Randomized Trials”, Journal of Pain and Symptom Management, Vol. 54/1, pp. 85-95.e1, https://doi.org/10.1016/j.jpainsymman.2017.02.016.
[21] Bélanger, E., C. Rodríguez and D. Groleau (2011), “Shared decision-making in palliative care: A systematic mixed studies review using narrative synthesis”, Palliative Medicine, Vol. 25/3, pp. 242-261, https://doi.org/10.1177/0269216310389348.
[68] Bostwick, D. et al. (2017), “Comparing the Palliative Care Needs of Those With Cancer to Those With Common Non-Cancer Serious Illness”, Journal of Pain and Symptom Management, Vol. 53/6, pp. 1079-1084.e1, https://doi.org/10.1016/j.jpainsymman.2017.02.014.
[7] Brighton, L. and K. Bristowe (2016), Communication in palliative care: Talking about the end of life, before the end of life, https://doi.org/10.1136/postgradmedj-2015-133368.
[63] Buck, J. et al. (2020), “Persistent inequalities in Hospice at Home provision”, BMJ Supportive and Palliative Care, Vol. 10/3, https://doi.org/10.1136/bmjspcare-2017-001367.
[74] Bylicki, O. et al. (2019), Lung cancer and end-of-life care: A systematic review and thematic synthesis of aggressive inpatient care, BMJ Publishing Group, https://doi.org/10.1136/bmjspcare-2019-001770.
[87] Centre national des soins palliatifs et de la fin de vie (2021), Fin de vie - Soins palliatifs, https://www.parlons-fin-de-vie.fr/qui-sommes-nous/le-centre-et-ses-missions/.
[12] Centre National Fin de Vie Soins Palliatifs (2018), La fin de vie, et si on en parlait ?, https://www.parlons-fin-de-vie.fr/je-minteresse-a-la-fin-de-vie/la-fin-de-vie-et-si-on-en-parlait/ (accessed on 2022).
[62] CIHI (2018), Access to Palliative Care in Canada, https://www.cihi.ca/sites/default/files/document/access-palliative-care-2018-en-web.pdf.
[50] Clark, K. and J. Phillips (2010), “End of life care – the importance of culture and ethnicity”.
[106] Commonwealth Fund (2022), Improving Care at the End of Life, https://www.commonwealthfund.org/publications/newsletter-article/improving-care-end-life.
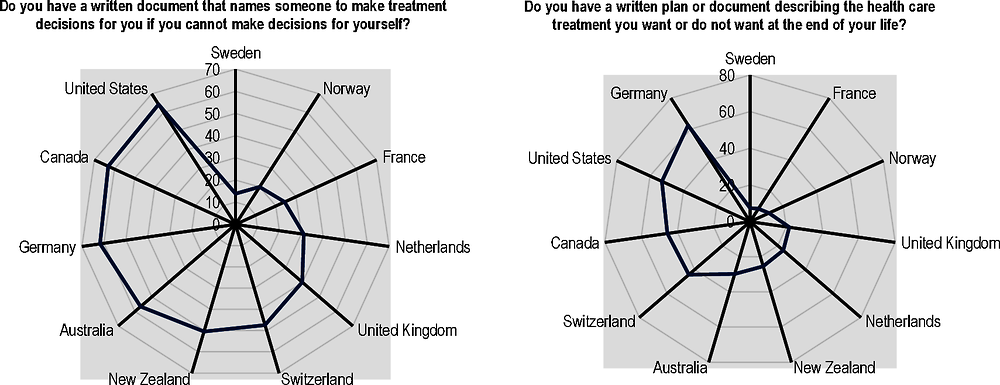
[33] Commonwealth Fund (2021), 2017 Commonwealth Fund International Health Policy Survey of Older Adults.
[95] Compassionate Communities UK (2022), , https://www.compassionate-communitiesuk.co.uk/ (accessed on 2022).
[57] Connolly, A., E. Sampson and N. Purandare (2012), “End-of-Life Care for People with Dementia from Ethnic Minority Groups: A Systematic Review”, Journal of the American Geriatrics Society, Vol. 60/2, pp. 351-360, https://doi.org/10.1111/j.1532-5415.2011.03754.x.
[56] Crist, J. et al. (2018), “Knowledge Gaps About End-of-Life Decision Making Among Mexican American Older Adults and Their Family Caregivers: An Integrative Review”, Journal of Transcultural Nursing, Vol. 30/4, pp. 380-393, https://doi.org/10.1177/1043659618812949.
[113] Cruz-Oliver, D. et al. (2017), “Evaluation of a Video-Based Seminar to Raise Health Care Professionals’ Awareness of Culturally Sensitive End-of-Life Care”, Journal of Pain and Symptom Management, Vol. 54/4, pp. 546-554, https://doi.org/10.1016/j.jpainsymman.2017.07.023.
[73] Das, M. (2019), “High-intensity end-of-life cancer care for young patients”, The Lancet Oncology, Vol. 20/5, p. e249, https://doi.org/10.1016/s1470-2045(19)30219-0.
[69] De Korte-Verhoef, M. et al. (2014), “Reasons for hospitalisation at the end of life: Differences between cancer and non-cancer patients”, Supportive Care in Cancer, Vol. 22/3, pp. 645-652, https://doi.org/10.1007/s00520-013-2019-9.
[36] Duke, G. and S. Thompson (2013), “Knowledge, attitudes and practices of nursing personnel regarding advance directives”, International Journal of Palliative Nursing, Vol. 13/3, https://doi.org/10.12968/ijpn.2007.13.3.23272 (accessed on 18 August 2020).
[4] Ejem, D. et al. (2019), “Reducing Disparities in the Quality of Palliative Care for Older African Americans through Improved Advance Care Planning: Study Design and Protocol”, Journal of Palliative Medicine, Vol. 22/S1, pp. S-90-S-100, https://doi.org/10.1089/jpm.2019.0146.
[110] ELDAC (2022), Supporting Inclusive End of Life Care Companion Guides, https://www.eldac.com.au/tabid/7513/Default.aspx#item6_1.
[94] End of life care research group (2022), Democratizing caring, dying and grieving: participation, action, understanding and evaluation, https://www.endoflifecare.be/sites/default/files/atoms/files/PHPCI2022Programme.pdf.
[14] Evans, N. et al. (2012), A critical review of advance directives in Germany: Attitudes, use and healthcare professionals’ compliance, https://doi.org/10.1016/j.pec.2011.10.004.
[27] Evenblij, K. et al. (2019), “Are care staff equipped for end-of-life communication? A cross-sectional study in long-term care facilities to identify determinants of self-efficacy”, BMC Palliative Care, Vol. 18/1, https://doi.org/10.1186/s12904-018-0388-z.
[30] Fin de vie soins palliatifs - centre national (2019), Les directives anticipées en mai 2019 : situation générale et dans les EHPAD en particulier, https://www.parlons-fin-de-vie.fr/wp-content/uploads/2019/07/Etude_BVA_directives_anticipees_2019.pdf (accessed on 2022).
[25] GAO (2019), ACP Selected States’ Efforts to Educate and Address Access challenges, https://www.gao.gov/assets/gao-19-231.pdf.
[82] Gott, M., T. Morgan and L. Williams (2020), “Gender and palliative care: a call to arms”, Palliative Care and Social Practice, Vol. 14, p. 263235242095799, https://doi.org/10.1177/2632352420957997.
[107] Government of Canada (2019), Framework on Palliative Care in Canada, https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/palliative-care/framework-palliative-care-canada.html#appc (accessed on 2022).
[37] Hafid, A. et al. (2022), “Assessing the application of continuity of care indices in the last year of life: a retrospective population-based study.”, Big data, https://doi.org/10.1370/afm.20.s1.2751.
[43] Hall, A., C. Rowland and G. Grande (2019), “How Should End-of-Life Advance Care Planning Discussions Be Implemented According to Patients and Informal Carers? A Qualitative Review of Reviews”, Journal of Pain and Symptom Management, Vol. 58/2, pp. 311-335, https://doi.org/10.1016/j.jpainsymman.2019.04.013.
[88] Hansford, L., F. Thomas and K. Wyatt (2022), “Poverty, choice and dying in the UK: a call to examine whether public health approaches to palliative care address the needs of low-income communities”, Mortality, pp. 1-17, https://doi.org/10.1080/13576275.2022.2044299.
[28] Harasym, P. et al. (2020), “Barriers and facilitators to optimal supportive end-of-life palliative care in long-term care facilities: a qualitative descriptive study of community-based and specialist palliative care physicians’ experiences, perceptions and perspectives”, BMJ Open, Vol. 10/8, p. e037466, https://doi.org/10.1136/bmjopen-2020-037466.
[8] Henderson, A. et al. (2018), “Interventions for interpersonal communication about end of life care between health practitioners and affected people”, Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.cd013116.
[85] Hoerger, M. et al. (2017), “Does educating patients about the Early Palliative Care Study increase preferences for outpatient palliative cancer care? Findings from Project EMPOWER.”, Health Psychology, Vol. 36/6, pp. 538-548, https://doi.org/10.1037/hea0000489.
[86] Hospice UK (2021), Community Grants Programme, https://www.hospiceuk.org/dying-matters-community-grants-programme.
[66] HSE (2017), palliative care services three year development framework (2017-2019), https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/palliative-care-services-development-framework.pdf (accessed on 2022).
[98] Hubert, S. et al. (2019), “Advance directives in France: Do junior general practitioners want to improve their implementation and usage? A nationwide survey”, BMC Medical Ethics, Vol. 20/1, https://doi.org/10.1186/s12910-019-0358-x.
[78] Hui, D. et al. (2013), “Targeted agent use in cancer patients at the end of life”, Journal of Pain and Symptom Management, Vol. 46/1, pp. 1-8, https://doi.org/10.1016/j.jpainsymman.2012.07.007.
[117] Hutchinson, R. et al. (2020), “What is Quality End‐of‐Life Care for Patients With Heart Failure? A Qualitative Study With Physicians”, Journal of the American Heart Association, Vol. 9/18, https://doi.org/10.1161/jaha.120.016505.
[91] IAHPC (2022), Global Directory of Palliative Care Institutions and Organizations, https://hospicecare.com/global-directory-of-providers-organizations/listings/details/2191/ (accessed on 2022).
[109] IPEPA (2022), What is IPEPA?, https://pepaeducation.com/about-ipepa/.
[65] Irish Department of Health, Social Services and Public Services (2010), Living matters, dying matters, https://www.health-ni.gov.uk/sites/default/files/publications/dhssps/living-matters-dying-matters-strategy-2010.pdf.
[121] Irish Hospice Foundation (2016), Have your say series launched, https://hospicefoundation.ie/public-engagement/have-your-say-series-launched/ (accessed on 2022).
[54] Isaacson, M. and A. Lynch (2017), “Culturally Relevant Palliative and End-of-Life Care for U.S. Indigenous Populations: An Integrative Review”, Journal of Transcultural Nursing, Vol. 29/2, pp. 180-191, https://doi.org/10.1177/1043659617720980.
[19] Khairuddin, N. et al. (2020), “Implementing advance care planning: A qualitative exploration of nurses’ perceived benefits and challenges”, Journal of Nursing Management, Vol. 28/5, pp. 1080-1087, https://doi.org/10.1111/jonm.13056.
[3] Kleiner, A. et al. (2019), “Advance care planning dispositions: The relationship between knowledge and perception”, BMC Geriatrics, Vol. 19/1, https://doi.org/10.1186/s12877-019-1113-3.
[29] Kononovas, K. and A. McGee (2017), “The benefits and barriers of ensuring patients have advance care planning”, Nursing Times, Vol. 113/1, pp. 41-44, https://www.nursingtimes.net/clinical-archive/end-of-life-and-palliative-care/the-benefits-and-barriers-of-ensuring-patients-have-advance-care-planning-03-01-2017/ (accessed on 27 July 2020).
[60] Kumar, B. et al. (2021), “Reducing the impact of the coronavirus on disadvantaged migrants and ethnic minorities”, European Journal of Public Health, Vol. 31/Supplement_4, pp. iv9-iv13, https://doi.org/10.1093/eurpub/ckab151.
[103] Kuosmanen, L. et al. (2021), “Patient participation in shared decision‐making in palliative care – an integrative review”, Journal of Clinical Nursing, Vol. 30/23-24, pp. 3415-3428, https://doi.org/10.1111/jocn.15866.
[58] Laguna, J. et al. (2012), “Racial/Ethnic Minority Access to End-of-Life Care: A Conceptual Framework”, Home Health Care Services Quarterly, Vol. 31/1, pp. 60-83, https://doi.org/10.1080/01621424.2011.641922.
[13] Lane, T., D. Ramadurai and J. Simonetti (2019), Public Awareness and Perceptions of Palliative and Comfort Care, Elsevier Inc., https://doi.org/10.1016/j.amjmed.2018.07.032.
[89] Last Aid (2022), Last Aid, https://www.letztehilfe.info/.
[75] Levinsky, N. et al. (2001), “Influence of age on Medicare expenditures and medical care in the last year of life”, Journal of the American Medical Association, Vol. 286/11, pp. 1349-1355, https://doi.org/10.1001/jama.286.11.1349.
[104] Lisa Jane Brighton, J. (2017), “A Systematic Review of End-of-Life Care Communication Skills Training for Generalist Palliative Care Providers: Research Quality and Reporting Guidance”, Journal of Pain and Symptom Management, Vol. 54/3, pp. 417-425, https://doi.org/10.1016/j.jpainsymman.2017.04.008 (accessed on 18 August 2020).
[26] Luna-Meza, A. et al. (2021), “Decision making in the end-of-life care of patients who are terminally ill with cancer – a qualitative descriptive study with a phenomenological approach from the experience of healthcare workers”, BMC Palliative Care, Vol. 20/1, https://doi.org/10.1186/s12904-021-00768-5.
[53] Marie Curie Cancer Care (2014), Improving access to palliative care services for people from Black, Asian and Minority Ethnic backgrounds in South East Cardiff.
[118] Mark Pfeifer, M. (2018), “Which Critical Communication Skills Are Essential for Interdisciplinary End-of-Life Discussions?”, AMA Journal of Ethics, Vol. 20/8, pp. E724-731, https://doi.org/10.1001/amajethics.2018.724.
[47] Martina Orlovic, K. (2019), “Racial and ethnic differences in end-of-life care in the United States: Evidence from the Health and Retirement Study (HRS)”, SSM - population health, https://doi.org/10.1016/j.ssmph.2018.100331 (accessed on 18 August 2020).
[79] Mathew, A. et al. (2017), “Prevalence and determinants of end-of-life chemotherapy use in patients with metastatic breast cancer”, Breast Journal, Vol. 23/6, pp. 718-722, https://doi.org/10.1111/tbj.12905.
[32] Meeussen, K. et al. (2011), Advance care planning in Belgium and the Netherlands: A nationwide retrospective study via sentinel networks of general practitioners, https://doi.org/10.1016/j.jpainsymman.2011.01.011.
[76] Menec, V. et al. (2007), “Health care use at the end of life among older adults: Does it vary by age?”, Journals of Gerontology - Series A Biological Sciences and Medical Sciences, Vol. 62/4, pp. 400-407, https://doi.org/10.1093/gerona/62.4.400.
[15] Mirage (2021), New campaign launches to challenge perceptions about palliative care, https://www.miragenews.com/new-campaign-launches-to-challenge-perceptions-564844/ (accessed on 2022).
[18] Murray, S. (2015), “The 2015 Quality of Death Index Ranking palliative care across the world”, The Economist Report, https://doi.org/10.1136/bmjspcare-2012-000211.
[46] Natalia Calanzani, D. (2013), Palliative and end of life care for Black, Asian and Minority Ethnic groups in the UK, https://www.mariecurie.org.uk/globalassets/media/documents/policy/policy-publications/june-2013/palliative-and-end-of-life-care-for-black-asian-and-minority-ethnic-groups-in-the-uk.pdf (accessed on 18 August 2020).
[52] Nelson-Becker, H. and T. Moeke-Maxwell (2020), “Spiritual diversity, spiritual assessment, and maori end-of-life perspectives: Attaining ka ea”, Religions, Vol. 11/10, pp. 1-16, https://doi.org/10.3390/rel11100536.
[116] NHCPO (2020), Position Paper: COVID-19 and Supporting Black Communities at the End of Life, National Hospice and Palliative Care Organization.
[49] NHPCO (2022), NHCPO webpage, https://www.nhpco.org/.
[115] NHPCO (2021), NHPCO seeks to increase access to hospice and palliative care services within diverse communities, https://www.nhpco.org/education/tools-and-resources/diversity/ (accessed on 2022).
[112] NHS (2022), Universal Principles for Advance Care Planning, https://www.england.nhs.uk/wp-content/uploads/2022/03/universal-principles-for-advance-care-planning.pdf (accessed on 2022).
[92] NHS UK (2021), Renewing our ambitions for palliative and end of life care, https://www.england.nhs.uk/blog/renewing-our-ambitions-for-palliative-and-end-of-life-care/ (accessed on 2022).
[114] Northam, H. et al. (2015), “Developing graduate student competency in providing culturally sensitive end of life care in critical care environments – A pilot study of a teaching innovation”, Australian Critical Care, Vol. 28/4, pp. 189-195, https://doi.org/10.1016/j.aucc.2014.12.003.
[100] NSW government (2021), End of Life Care and Decision-Making, https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2021_004.pdf (accessed on 2022).
[22] Ó Coimín, D. et al. (2019), “Dying in acute hospitals: voices of bereaved relatives”, BMC Palliative Care, Vol. 18/1, https://doi.org/10.1186/s12904-019-0464-z.
[2] OECD (2021), Health for the People, by the People: Building People-centred Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/c259e79a-en.
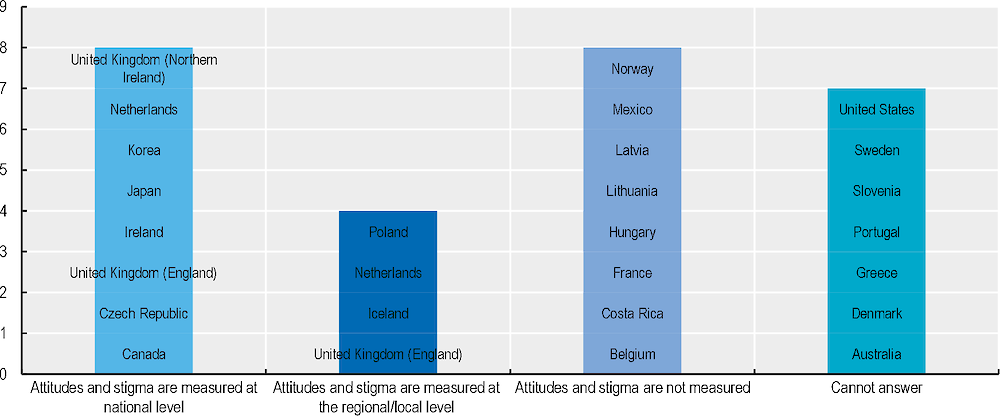
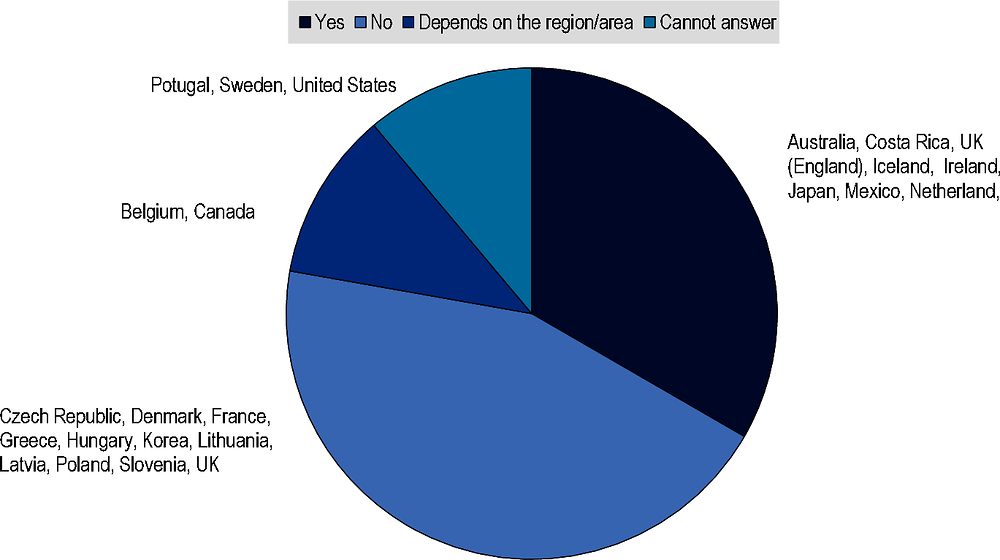
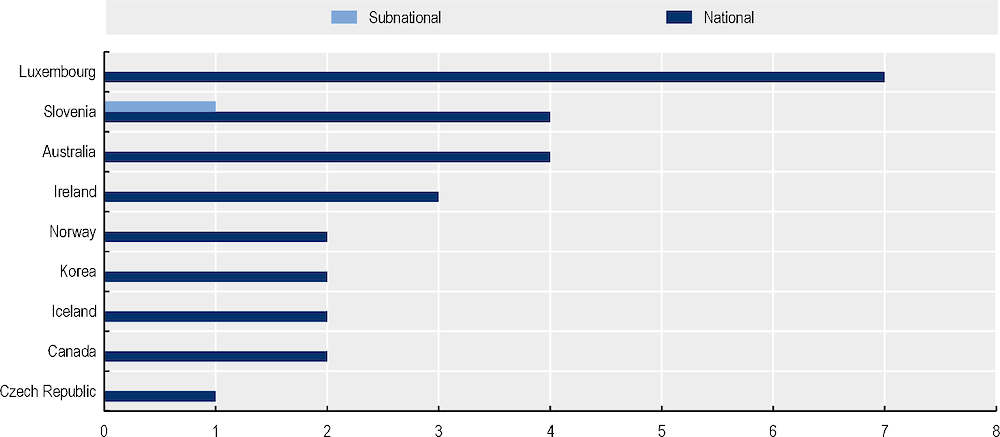
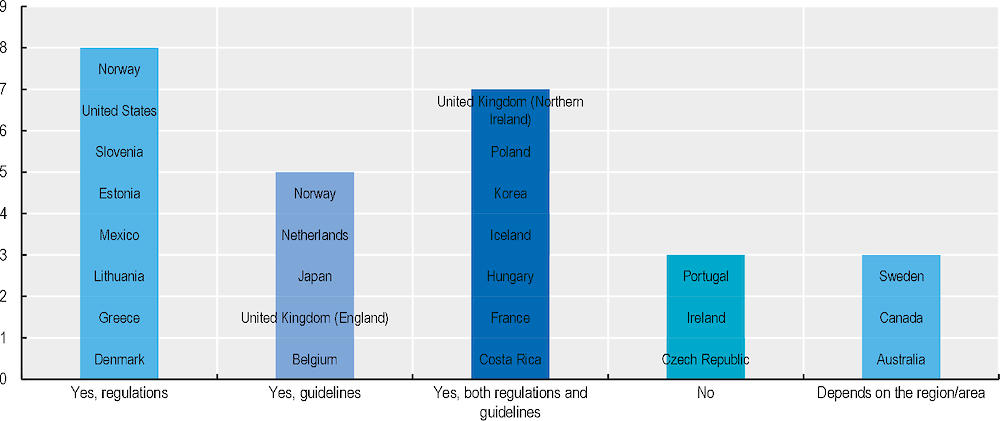
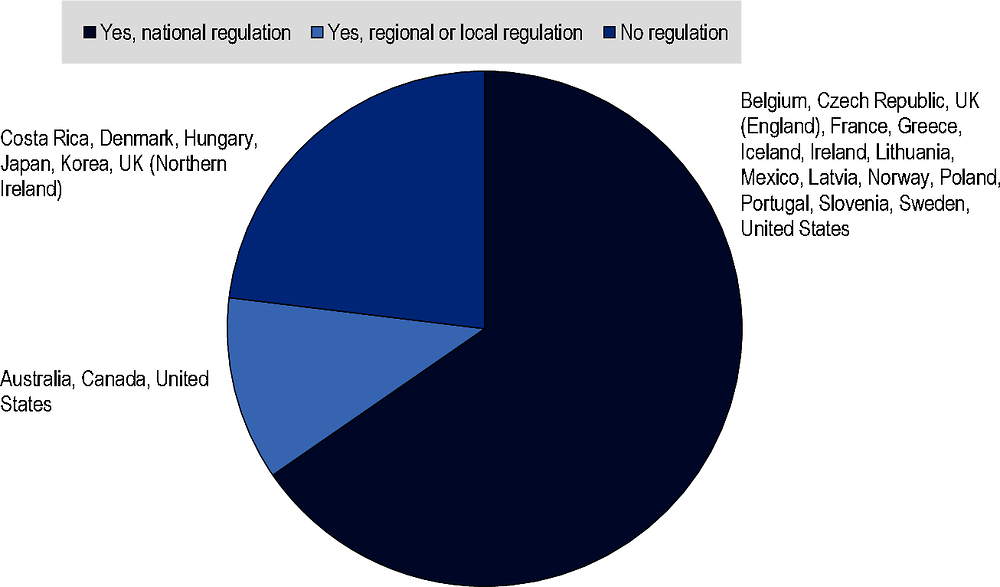
[16] OECD (2020-2021), OECD policy and data questionnaires.
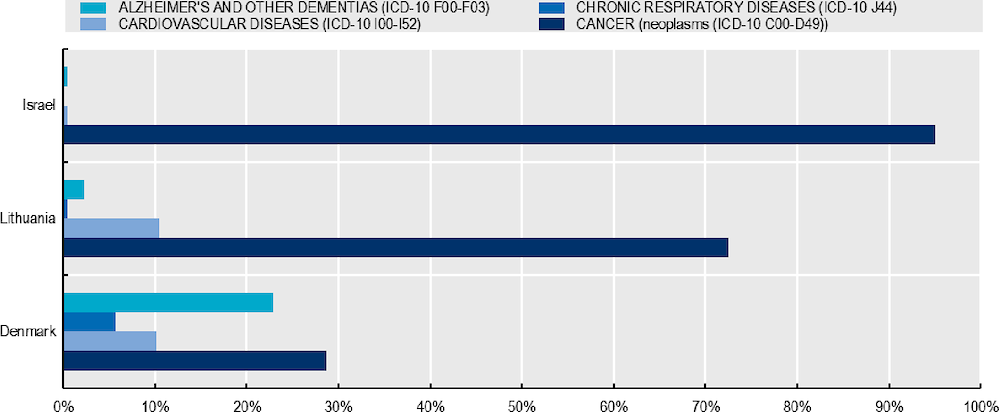
[71] OECD HCQO-EOLC pilot (2021), OECD HCQO-EOLC pilot data collection.
[24] ONS (2016), National Survey of Bereaved People (VOICES): england 2015, https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/bulletins/nationalsurveyofbereavedpeoplevoices/england2015.
[55] Orlovic, M., K. Smith and E. Mossialos (2019), “Racial and ethnic differences in end-of-life care in the United States: Evidence from the Health and Retirement Study (HRS)”, SSM - Population Health, Vol. 7, p. 100331, https://doi.org/10.1016/j.ssmph.2018.100331.
[23] O’Sullivan, A. (2021), Bereaved family members’ VOICES of support and care during the last three months of life for people with advanced illness, https://www.diva-portal.org/smash/get/diva2:1547812/FULLTEXT01.pdf.
[96] Pallium Canada (2022), Compassionate communities, https://www.pallium.ca/compassionate-communities/ (accessed on 2022).
[72] Parr, J. et al. (2010), “The Influence of Age on the Likelihood of Receiving End-of-Life Care Consistent with Patient Treatment Preferences”, Journal of Palliative Medicine, Vol. 13/6, pp. 719-726, https://doi.org/10.1089/jpm.2009.0337.
[35] Peicius, E. (2017), “Are advance directives helpful for good end of life decision making: a cross sectional survey of health professionals”, BMC medical ethics, Vol. 18/40, https://doi.org/10.1186/s12910-017-0197-6 (accessed on 18 August 2020).
[93] PHPCI (2022), Compassionate Cities, https://www.phpci.org/cities.
[42] Quintiens, B. et al. (2022), “Area-Based Compassionate Communities: A systematic integrative review of existing initiatives worldwide”, Palliative Medicine, Vol. 36/3, pp. 422-442, https://doi.org/10.1177/02692163211067363.
[80] Randén, M. et al. (2013), “Treatment decisions and discontinuation of palliative chemotherapy near the end-of-life, in relation to socioeconomic variables”, Acta Oncologica, Vol. 52/6, pp. 1062-1066, https://doi.org/10.3109/0284186X.2012.758872.
[31] Reid, K. et al. (2020), “VOICES: South Island pilot survey of bereaved people”, Vol. 133, https://journal.nzma.org.nz/journal-articles/voices-south-island-pilot-survey-of-bereaved-people.
[111] ReSPECTprocess (2022), What is ReSPECT, https://learning.respectprocess.org.uk/wp-content/uploads/2017/06/What-is-ReSPECT-download.pdf (accessed on 2022).
[119] Rietjens, J. et al. (2017), “Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care”, The Lancet Oncology, Vol. 18/9, pp. e543-e551, https://doi.org/10.1016/s1470-2045(17)30582-x.
[39] Rumbold, B. and S. Aoun (2021), “Palliative and End-of-Life Care Service Models: To What Extent Are Consumer Perspectives Considered?”, Healthcare, Vol. 9/10, p. 1286, https://doi.org/10.3390/healthcare9101286.
[83] Saeed, F. et al. (2018), “Preference for Palliative Care in Cancer Patients: Are Men and Women Alike?”, Journal of Pain and Symptom Management, Vol. 56/1, pp. 1-6.e1, https://doi.org/10.1016/j.jpainsymman.2018.03.014.
[90] Sánchez-Cárdenas, M. et al. (2021), “The Development of Palliative Care in Colombia: An Analysis of Geographical Inequalities Through the Application of International Indicators”, Journal of Pain and Symptom Management, Vol. 62/2, pp. 293-302, https://doi.org/10.1016/j.jpainsymman.2020.12.010.
[38] Sharma, G. et al. (2009), “Continuity of Care and Intensive Care Unit Use at the End of Life”, Archives of Internal Medicine, Vol. 169/1, p. 81, https://doi.org/10.1001/archinternmed.2008.514.
[20] Silveira, M. (2022), “Advance care planning and advance directives”, https://www.uptodate.com/contents/advance-care-planning-and-advance-directives.
[84] Singh, T. et al. (2017), “Palliative Care for Hospitalized Patients With Stroke”, Stroke, Vol. 48/9, pp. 2534-2540, https://doi.org/10.1161/strokeaha.117.016893.
[120] Sinuff, T. et al. (2015), “Improving End-of-Life Communication and Decision Making: The Development of a Conceptual Framework and Quality Indicators”, Journal of Pain and Symptom Management, Vol. 49/6, pp. 1070-1080, https://doi.org/10.1016/j.jpainsymman.2014.12.007.
[61] Sleeman, K. et al. (2015), “The changing demographics of inpatient hospice death: Population-based cross-sectional study in England, 1993–2012”, Palliative Medicine, Vol. 30/1, pp. 45-53, https://doi.org/10.1177/0269216315585064.
[105] Smith, M. et al. (2018), “The Use of Simulation to Teach Nursing Students and Clinicians Palliative Care and End-of-Life Communication: A Systematic Review”, American Journal of Hospice and Palliative Medicine®, Vol. 35/8, pp. 1140-1154, https://doi.org/10.1177/1049909118761386.
[10] Sonja McIlfatrick, F. (2013), “Public awareness and attitudes towards palliative care in Northern Ireland”, BMC Palliative Care, Vol. 12/34, https://doi.org/10.1186/1472-684X-12-34.
[45] Stats NZ (2019), New Zealand’s population reflects growing diversity, https://www.stats.govt.nz/news/new-zealands-population-reflects-growing-diversity (accessed on 27 Jan 2021).
[64] Stiel, S. et al. (2015), “Comparison of terminally ill cancer-vs. non-cancer patients in specialized palliative home care in Germany-A single service analysis”, BMC Palliative Care, Vol. 14/1, https://doi.org/10.1186/s12904-015-0033-z.
[5] Swerissen, H. (2014), Dying well, https://grattan.edu.au/wp-content/uploads/2014/09/815-dying-well.pdf (accessed on 2022).
[34] Tamiya, J. (2018), “Current Practice of Advance Care Planning Among Doctors and Nurses: Results from a National Survey in Japan”, Journal of Pain and Symptom Management, Vol. 56/6, https://doi.org/10.1016/j.jpainsymman.2018.10.460.
[97] The Choice in End of Life Care Programme Board (2015), What’s important to me? A review of choice in end of life care, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/407244/CHOICE_REVIEW_FINAL_for_web.pdf (accessed on 24 August 2020).
[40] The Economist Intelligence Unit (2015), The 2015 Quality of Death Index Ranking palliative care across the world.
[1] Thomas K, G. (2018), Population-based, person-centred end-of-life care: time for a rethink, pp. 116–7.
[9] Travers, A. and V. Taylor (2016), What are the barriers to initiating end-of-life conversations with patients in the last year of life?, https://doi.org/10.12968/ijpn.2016.22.9.454.
[48] United States Census Bureau (2019), Population estimates 2019, https://www.census.gov/quickfacts/fact/table/US/PST045219 (accessed on 17 september 2021).
[70] Vestergaard, A. et al. (2020), “Hospitalisation at the end of life among cancer and non-cancer patients in Denmark: a nationwide register-based cohort study”, BMJ Open, Vol. 10/6, p. e033493, https://doi.org/10.1136/bmjopen-2019-033493.
[108] VitalTalks (2022), VitalTalk makes communication skills for serious illness learnable., https://www.vitaltalk.org/.
[67] Wachterman, M. et al. (2016), “Quality of End-of-Life Care Provided to Patients With Different Serious Illnesses”, JAMA Internal Medicine, Vol. 176/8, p. 1095, https://doi.org/10.1001/jamainternmed.2016.1200.
[99] Waldrop, D. and M. Meeker (2012), “Communication and advanced care planning in palliative and end-of-life care”, Nursing Outlook, https://doi.org/10.1016/j.outlook.2012.08.012.
[11] Westerlund, C. et al. (2018), “Public awareness of palliative care in Sweden”, Scandinavian Journal of Public Health, Vol. 46/4, pp. 478-487, https://doi.org/10.1177/1403494817751329.
[44] Wilson, T. et al. (2020), “Past and projected growth of Australia’s older migrant populations”, Genus, Vol. 76/1, https://doi.org/10.1186/s41118-020-00091-6.
[51] Yarnell, C. et al. (2020), “Association between Chinese or South Asian ethnicity and end-of-life care in Ontario, Canada”, Canadian Medical Association Journal, Vol. 192/11, pp. E266-E274, https://doi.org/10.1503/cmaj.190655.
[81] Zhu, Y. et al. (2018), “End-of-life chemotherapy is associated with poor survival and aggressive care in patients with small cell lung cancer”, Journal of Cancer Research and Clinical Oncology, Vol. 144/8, pp. 1591-1599, https://doi.org/10.1007/s00432-018-2673-x.