This chapter discusses the public and private financing of end-of-life care. It highlights that there are gaps in public coverage of certain services, leading to high out-of-pocket (OOP) expenses for families and a heavy burden on informal carers. Current models of care can also result in heavy hospital use and potentially higher costs. Avenues for improvement discussed include more prioritisation of cost-effective interventions, especially community and home‑based palliative care and adapting payment mechanisms to incentivise more integrated care (between curative and palliative care). Finally, better support for informal or family carers in terms of combining work and care is essential to avoid high societal costs.
Time for Better Care at the End of Life

5. Ensuring that end-of-life care is appropriately financed
Abstract
Introduction
End-of-life care1 (EOLC) refers to the health and social care provided to persons who are very ill and most likely will die in the near term from their illness. Such care involves acute care provided in the days or months prior to death and/or palliative care, which focuses on relieving the patient’s suffering and improving quality of life. Costs of care at the end of life can be paid by public social protection schemes, but individuals also often have significant out-of-pocket payments or might rely on private health care insurance in some countries. Even where family members or others close to the person needing end-of-life care may also provide an important part of the care, some individuals fail to have their needs met because of inadequate financing, leading to unnecessary suffering at the end of life.
Expenses at the end of life have also raised concerns about their high costs for public budgets. Several studies have highlighted that the bulk of per capita health care costs are concentrated in the last years of life, as more health services are needed and therefore more is spent on an individual close to death (Lorenzoni et al., 2019[1]).There is evidence of high variability in the costs of dying, related to the type of illness but also to the location and type of services provided. For instance, increases in spending at the end of life are driven primarily by increases in emergency rather than planned treatment (Lee and Stoye, 2019[2]). Evidence from several countries shows that in the last three months of life, more than 80% of the total health and social costs were attributable to hospital care. In contrast, the cost of palliative care amounted to 10% (Yi et al., 2020[3]).
As countries prepare for increasingly ageing populations and more individuals with chronic conditions who require complex care before dying (see Chapter 1), there will likely be substantial increases in the need for high quality end-of-life care services, and consequently more sustainable financing solutions for such services. A central policy question is whether to expand the role of the government in providing support to individuals and families to assist with end-of-life care. Equitable financing of end-of-life care services means that care will be affordable and adequate, as well as the care burden being fairly shared and not unduly burdensome upon relatives and other informal carers.
The remainder of the chapter is organised as follows. Section 5.1 highlights the principles of appropriately financed end-of-life care. Section 5.2 illustrates the consequences of not having appropriate financing for end-of-life care. Section 5.3 explores policies and best financing practices to ensure adequate and effective care, whose cost is fairly shared, and without undue financial burden on family and informal caregivers.
Key findings
In most countries end-of-life care services are publicly funded, mostly through health benefits or insurance (in 70% of countries), but public funding varies widely across settings of care. Medical spending in the 12 months prior to death ranges from 8.5% of aggregate spending in the United States to 11% in Denmark. Public funding of end-of-life care services is more predominant in hospitals which could influence the place of death and have an upward impact on public expenses. Across OECD countries, hospital expenditure constitutes 32% to 67% of end‑of-life care expenditures across countries.
Public social protection systems do not cover some of the health and social care expenses to alleviate symptoms at the end of life. Partial coverage of expenses occurs in a third of the countries for some services such as opioids and other forms of pain management, for nutrition support and for medication to alleviate vomiting and nausea. This can lead to substantial out-of-pocket medical expenses, which amount to a mean of EUR 3 200 in a year for households.
Gaps in public coverage can lead to an overreliance on informal and family carers. Currently, two‑thirds of individuals receive informal care at the end of life. Informal carers can face a heavy burden which can generate additional societal indirect costs because of reduced employment and financial costs, especially because one‑third of countries do not provide financial support for carers.
Policy options
Modifying payment systems for end-of-life care should focus on ensuring sustainable funding given growing demand. While more, more stable, and predictable funding would allow for better planning of care, only 7 out of 25 countries have policies in place to control the budget on EOLC. In Australia, England and Switzerland, the amount of reimbursement received per patient is being set to vary by performance status, phase of illness, care setting and age to ensure that payments are more adequately reflecting needs. Countries also need to find a balance between sustainable funding and affordable care. Belgium, France, Germany, and Korea have put in place policies to reduce out-of-pocket expenditures for end-of-life care.
Incentivising early access to palliative care services is paramount as palliative care is found to be cost-effective, improving quality of life and reducing length of hospital stays, re‑admissions, and visits to intensive care units. Improving care co‑ordination can incentivise earlier access to palliative care, but current funding schemes do little to incentivise care models that improve co‑ordination. Bundled payments have been suggested as an alternative option to integrate curative and palliative care. The United States are moving towards value‑based payments which might favour more palliative care, while the United Kingdom has applied pay-for-performance systems incentivising GPs to identify and manage palliative care needs.
Incentivising the use of palliative care outside hospitals can lead to better cost-effectiveness and higher quality of end-of-life care. Evidence from Australia, Belgium, Canada, the United States and the United Kingdom showed cost-effectiveness of palliative care at home, and evidence on the cost-effectiveness of palliative care in nursing homes has started to emerge. France has increased funding for out-of-hours palliative care and increased mobile teams with the aim of promoting palliative care at home, while Australia has announced increased funding for home palliative care. Furthermore, Luxembourg has started to allow medical devices in nursing homes, while France has implemented a hospital at home protocol to avoid the transfer of people from nursing homes to the hospital.
Supporting informal or family carers who provide end-of-life care remains an essential element of overall end-of-life care policy. This includes appropriate training, information services, the provision or adequate benefits and sufficient leave for keeping carers in employment. Flexible work arrangements can also support caregivers by allowing them to balance professional and caring responsibilities. Norway and the United States for instance provide opportunities for training and counselling, while in Denmark, employees have the statutory right to leave for the care of someone close dying, and there is no fixed time limit for the leave. Furthermore, in Belgium informal caregivers can obtain part time work arrangements for up to five years and in Norway people who care for a dying person can work from home.
5.1. Why is it important for end-of-life care to be appropriately financed?
Good end-of-life care has an enormous impact on the quality of a person’s last weeks or months of life, by reducing unnecessary suffering and providing a supportive, caring environment. End-of-life care should therefore be a right afforded to everyone equally. This requires adequate financing of services so that people can receive the care they need, both specialist and non-specialist, irrespective of their background and where they live. Palliative care and hospice services need to be affordable to families, without resulting in excessive out-of-pocket costs. Timely access is also critical. Palliative care teams connected to every hospital helps minimise waiting times and ensure access across different localities. In many countries, given demographic changes, without more resources for social, community and home care, it will remain challenging to respect people’s preferences to die at home and for care to be of high-quality.
Informal carers are an important source of care in many countries. They constitute the foundation of care for many relatives and friends, can help contain the overall costs to the health system but also suffer from financial costs themselves, especially because of the time invested. Without proper support, informal carers often struggle to combine caring with work and other personal commitments. Informal carers need both financial and non-financial support, including sufficient formal care to ensure that the burden is fairly shared. Respite care, initial training and provision of equipment, and bereavement care are all critical support components for informal carers and the person they are caring for.
From a financial and human perspective, it is also important for end-of-life care to be (cost) effective. Concern about high cost at the end of life raise ethical dilemmas about how to balance appropriate interventions and spending. This is fundamentally challenging because it remains difficult to predict the timing of mortality. Individuals with high likelihood of dying account for only a small share of total spending- less than 5% of spending (Einav et al., 2018[4]). Ensuring an appropriate balance of treatments with curative and palliative care and avoiding inappropriate treatments is likely to be not only desirable for patients and families in terms of quality of life but also cost-effective. This requires accessible, high quality palliative care home care teams, including knowledgeable palliative nurses and palliative care physicians who can advise other professionals on appropriate treatment and psychological support (Service Publique Fédéral Santé Publique, 2020[5]). Investing in palliative care knowledge among staff in nursing homes should also contribute to have more palliative care delivered in such institutions without the need to transfer patients.
5.2. The consequences of inadequate financing at the end of life
5.2.1. Inadequate models of care can lead to high expenditures, with detrimental impacts on government budgets and households
The cost of end-of-life care has received a great deal of attention and there have been concerns about the high level of public expenditures for people at the end of life. Such focus started with the publication that in the United States 5% of people on Medicare represent patients in the last year of life while they amount to 25% of the costs of Medicare (Banarto et al., 2004[6]). More recent cross‑country analysis has confirmed that EOLC spending is substantial on a per capita basis, yet expenditures as share of public health spending appear to be much lower than 25. In the United States, average medical spending from all payers was USD 80 000 in the last 12 months of life (in 2011, measured in 2014 US dollars), and the share of medical spending in the 12 months prior to death ranges from 8.5% of aggregate spending in the United States to 11% in Denmark (French et al., 2017[7]). Such spending appears to be driven by the high costs of managing chronic conditions prior to death since a country’s medical spending in the last three years of life usually exceeds 2% of its GDP and spending in the last three years of life accounted for as much as 24.5% of overall costs (French et al., 2017[7]).
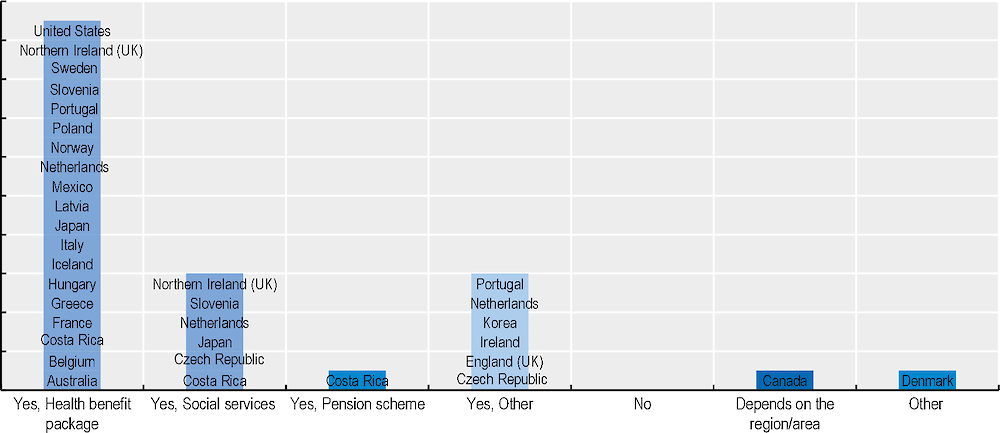
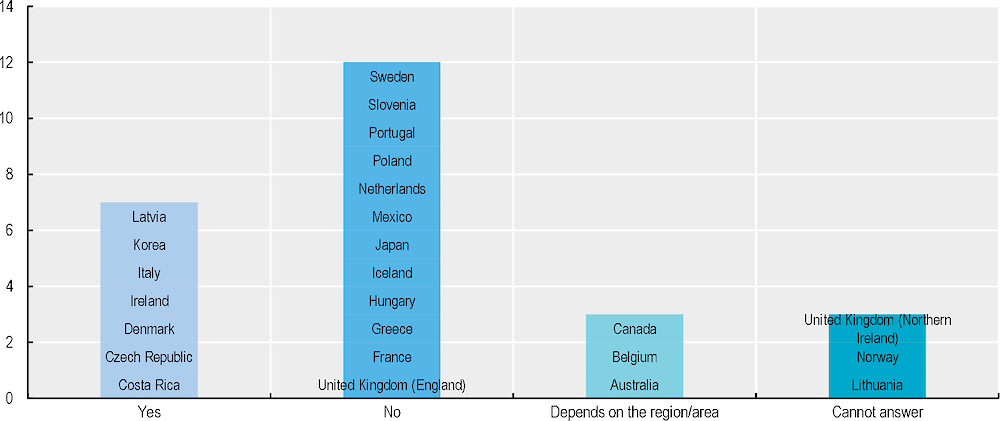
End-of-life care costs benefit from public funding across all OECD countries. In 18 out of 25 countries which provided data, services are funded in part through health benefits and in 5 of these countries or regions the funding comes from both health and social care packages (Figure 5.1). In most countries, there is a dedicated palliative care budget, but the funding system is mixed (Groeneveld EI, 2017[8]). In Costa Rica, funding is covered through health care social insurance, government budget, and special sources such as lottery revenue. Several countries pointed to other sources of funding. For instance, in England (United Kingdom), EOLC is funded through the National Health System (NHS) or in hospices through a mix of NHS and charitable funding. In the Czech Republic, a significant part of the funding is coming from social services, funded through municipalities but there is also an important share of expenditure from families. In Australia, the budget is shared between the Department of Health and the Treasury. In Denmark, all health and social services, including EOLC, are financed by general taxes and are supported by a system of central government block grants, reimbursements, and equalisation schemes (OECD, 2020-2021[9]).
Figure 5.1. EOLC services are covered in part by health and social security schemes
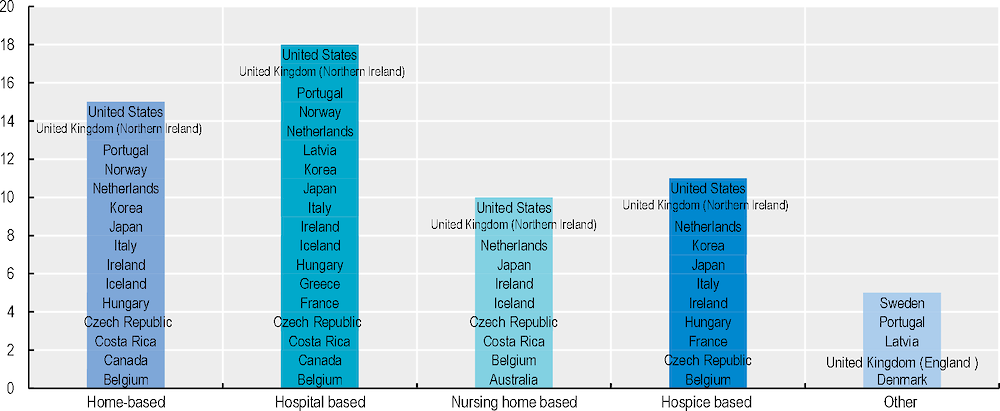
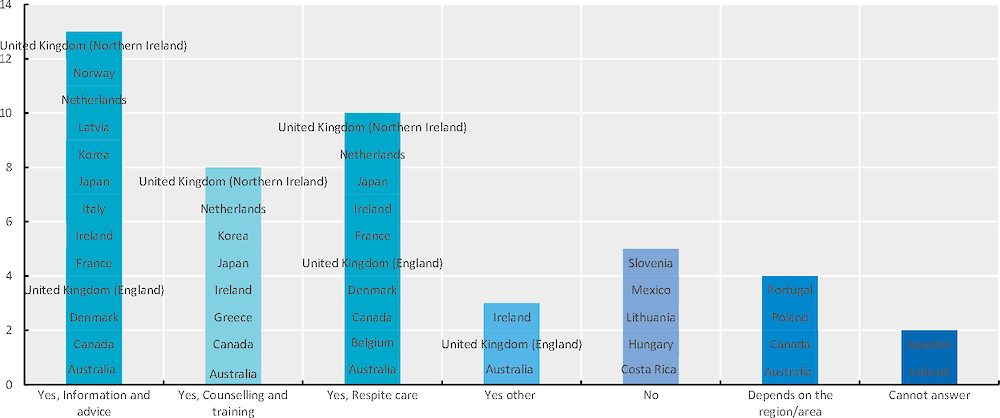
Public funding for end-of-life care varies by setting, affecting place of death. Most OECD countries provide funding for end-of-life care in hospitals (18 out of 25), but an important share (14) has home‑based care financing (Figure 5.2). Hospice‑based care is publicly financed in less than half of countries. In the United Kingdom, between 25 to 40% of hospice funding comes from the government (UK Hospice, 2021[10]). Hospices also rely heavily on volunteers. In the United States, hospice care is covered for the elderly through Medicare but there are usually some capped co-payments for medication, for respite care inpatient and board and lodging is not covered if live in a facility, while it is an optional plan for people on Medicaid who need to select it and wave other cure or treatment. Nursing home end-of-life care funding is less widely available and overall use of long-term care is subject to high out-of-pocket costs in several OECD countries. Exceptions include, for instance, Luxembourg, where it is legislated that nursing homes need to have certain share of personnel with palliative care expertise at different levels. In Poland, there is insufficient end-of-life care in long-term care (LTC), both for institutions and home care as specialist hospice palliative care services by law are excluded from LTC facilities (Krakoviaw, 2020[11]). This can have unintended consequences on the quality of EOLC and on place of death. There is also, for instance, an association between high levels of public financing and organisation of long-term and lower hospitalisations and a higher share of out-of-hospital deaths (Orlovic, Marti and Mossialos, 2017[12]).
Figure 5.2. Public funding for EOLC services is predominantly hospital-based
Hospital care, especially acute care, is an important component of end-of-life care expenditures. This represents 67% of expenditures in the last 12 months of life in France, 58% in Germany and Denmark, 44% in the United States but 32% in the Netherlands where expenditures from long-term care represent the most important item (French et al., 2017[7]). An international study revealed that more than 80% of the costs in the last three months of life were attributable to hospital acute care while the costs of palliative care were only close to 10% (Yi et al., 2020[3]). However, not all of hospital care is necessary or appropriate. Differences in medical culture could influence patterns of treatment intensity as shown by the variation in hospital admissions across countries in the last year of life. Similarly, variability in end-of-life health care is dependent on a range of patient characteristics, including gender, age and the type of disease or chronic conditions and the presence of limitations, with one of the most consistently important factors is age at death) illustrated by the fact that those being 60+ are less likely to be hospitalised (see Chapter 3). OECD data in Chapter 3 also finds that men and individuals with cancer are more likely to be hospitalised at the end of life and data from the United Kingdom confirms that this results in higher costs for those groups (Luta et al., 2020[13]).
Similarly, several studies have highlighted regional variation in the use of inpatient care and in costs at the end of life. This suggests that the high cost of EOL may also be partially the result of a failure of community-based services to support the person at home (Luta et al., 2020[13]). Evidence from the literature suggests more than one‑third (33% to 38%) of older patients with advanced irreversible diseases hospitalised near the end of life received interventions unlikely to provide either survival or palliation benefit (Cardona-Morrel et al., 2016[14]). Regional variation in surgical interventions and other treatments suggest that treatment is influenced by external factors such as the number of hospital beds per head and availability of local practices (Kelley, 2011[15]). A ten‑year Canadian study has indicated that early specialist palliative care exposure reduces the risk of hospital-based acute care, including Intensive Care Unit (ICU) admission, in the last 30 days of life for all chronic disease groups except dementia (Earp et al., 2021[16]).
5.2.2. Not all service costs are covered, leading to gaps and high expenses for families
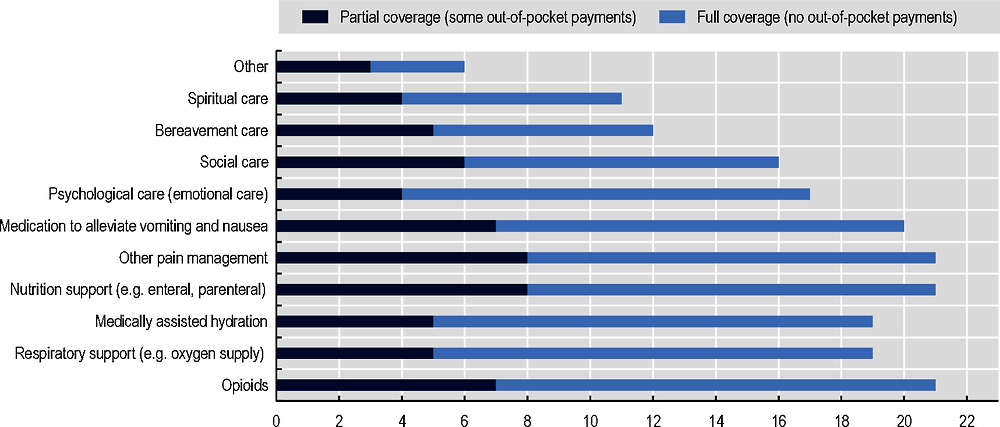
Public social protection for EOLC does not cover all health and social care expenses. Across counties, partial coverage occurs in a third of the countries for some services such as opioids and other forms of pain management, similarly to nutrition support and for medication to alleviate vomiting and nausea (Figure 5.3). This is the case for instance in Australia, Belgium, Hungary, Iceland, Ireland, Japan, Korea, and Portugal. Australia, Belgium, Ireland, Japan, and Korea do not fully cover respiratory support nor medically assisted hydration. Six countries do not fully cover social care nor bereavement support. In Poland, the reimbursement rate from the National Health Insurance fund covers between 50% and 75% of all drug purchases and so the hospices must find additional funds to ensure access to all essential medicines (Pawłowska et al., 2016[17]).
Figure 5.3. Certain EOLC services are not fully covered
In addition, the financing mechanisms designed to reimburse palliative and end-of-life care impact how palliative care is delivered and can lead to insufficient care and/or inequalities. A review of funding mechanisms across 14 OECD countries found that payment mechanisms for palliative care often maintained inequalities in access to palliative care, and often did not structure reimbursement models to deliver on the needs of individual patients (Groeneveld EI, 2017[8]). In some countries, statutory funding does not always appear to lead to sustainable funding for the services and funding meeting population needs. In the United Kingdom, researchers found a limited correlation between the palliative care needs of the population and the budget allocated to palliative care services while more than two‑thirds of hospices had their statutory funding frozen or reduced in recent years (Ryan, 2018[18]).
There are sizeable reimbursement limits in some countries which can lead to gaps. In the United States, there are limitations on reimbursements related to the timing of treatments or interventions, which can only be reimbursed in the last six months of life. This can constrain access to end-of-life care for those with conditions that are more difficult to identify the end-of-life phase, such as dementia, or who require palliative care services towards the end of life for more than the reimbursed period (OECD, 2018[19]). For instance, in Hungary, palliative care is restricted to 150 visits. In addition, in Hungary, outpatient palliative care services do not receive government funding and rely on funding to be made available from the general hospital budgets. Home and community-based care services in some countries rely to a certain extent on contributions by the charitable sector (Groeneveld EI, 2017[8]).
In addition to partial coverage, other regulations such as prescription drug caps might affect access to symptom management services across countries. For instance, due to the large increase in opioid in some OECD countries, efforts to curb the opioid abuse are also having an unintended effect of reducing access to pain medication for terminally ill cancer patients in the United States, among other countries (Andrea C. Enzinger, 2021[20]). In the Unites States, while Medicare appears to cover 80% of those at the end of life, for those on Medicaid, states can choose whether to include a hospice benefit at all and some do not cover hospice while some can limit the number of prescriptions for Medicaid patients, impacting pain management and other symptoms (Wachterman and Sommers, 2021[21]). In France, there are restrictions to provide midazolam outside hospital settings, making long and continuous sedation outside hospitals very rare (Senat, 2021[22]).
If public social protection does not cover all end-of-life costs, families can face significant costs at the end-of-life. Out-of-pocket health care expenses at the end of life for elderly households represent a substantial amount. According to comparative data, the mean out-of-pocket medical expenses in OECD countries can be significant at around EUR 3 200, ranging from around EUR 300 per year in the Slovak Republic, to more than EUR 13 000 per year in Switzerland (Figure 5.4). The amount of out-of-pocket spending depends on whether EOLC financing is predominantly private or public, the type of cost-sharing arrangement and the financial protection mechanisms in place (such as caps on patients’ out-of-pocket contributions). In the Slovak Republic for instance, 40‑60% of the cost of inpatient palliative care is paid for by patients and families, as the health insurance companies do not consider hospices to be necessary medical facilities while for outpatient care, patients must contribute to the cost of medications (Krizanova and Skripekov, 2015[23]).
Figure 5.4. Summary of OOP expenditure in the last year of life, 2008‑17
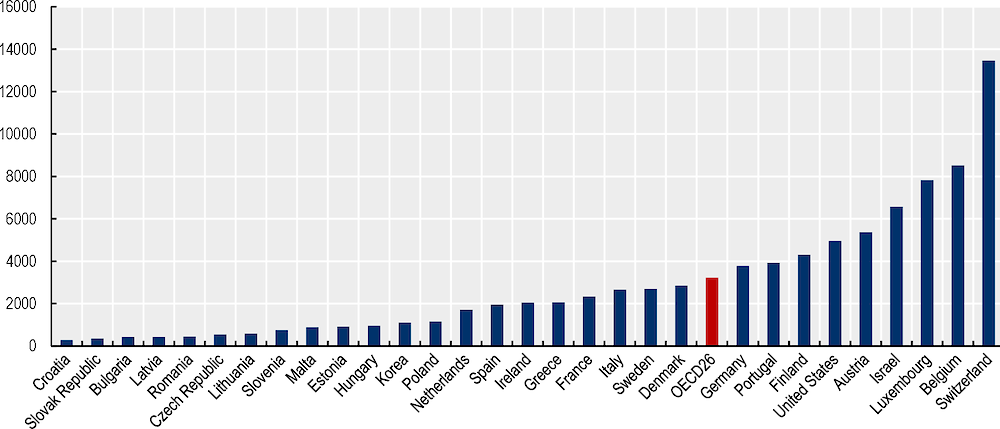
Note: Mean Health Expenditures (Normalised to a Twelve‑Month Period). Values are in 2010 Euros computed based on the CPI for country and year of death. For details, refer to the codebook for SHARE EoL dataset.
Source: Analysis based on data from SHARE EoL wave 2‑7 interview (SHARE, the Survey of Health, Ageing and Retirement in Europe, 2020[24]), HRS (wave 8‑14), KLoSA (wave 2‑7).
Overall out-of-pocket expenditures are highly related to the place of death, the financing of long-term care and the availability of informal care support (Orlovic, Marti and Mossialos, 2017[12]). Previous analysis shows that the largest expenditure item at the end of life tends to be hospital care, especially in the last months, and long-term care (French et al., 2017[7]; De Nardi et al., 2016[25]; Marshall, McGarry and Skinner, 2010[26]). Indeed, some end-of-life expenditures on formal medical services are reasonably well covered by public systems while, by contrast, the extent of coverage and cost-sharing for long-term care (LTC) varies substantially. Data from the last year of life from the Survey of shows that it represents 30% on average of out-of-pocket expenditures. Data for Israel focusing on cancer patients highlights that 84% have out-of-pocket expenditures and that such expenditures represent mostly spending on medicines and private caregivers (USD 5 800 and USD 10 800 respectively during the last half-year of life) (Tur-Sinai et al., 2022[27]).
In addition to expenditures to meet health needs, many people with terminal illnesses need other social services such as long-term care, housing adaptation and technical aids. People at the end of life may need help with support with daily living such as washing, dressing, and preparing meals which represent long-term care. OECD analysis shows that the reported total costs of LTC represent between one‑half to as much as five times the median disposable income of individuals of retirement age or older and that even for as little as 6.5 hours of care per week for people with low needs, the total costs of home LTC services would represent more than half of the disposable income of an older person with a low income. In seven jurisdictions, older people with severe needs receiving care at home would face out-of-pocket costs that are higher than the median income among elderly people (Oliveira Hashiguchi and Llena-Nozal, 2020[28]).
High out-of-pocket medical and long-term care expenditures at the end of life may strain the finances of households. Data from the United Kingdom shows that two‑third of households affected by terminal illness experience financial strain and that the cost of additional expenses can amount to 98% of income for disadvantaged families (Marie Curie, 2019[29]). An international study based on information from GPs reported that 43% of patients and families in Italy, 36% in The Netherlands, 14% in Belgium and 8% in Spain had difficulties in covering the costs of care at the end of life (Pivodic et al., 2014[30]). High expenses at the end of life may even influence the capacity to pay other expenses, and people might need to use their savings or assets. Data from several studies points out that households can struggle to pay important living expenses or choose to forgo or delay treatment (Marie Curie, 2019[29]). It can also drain a couple’s assets when one spouse gets sick and leaving little for the other spouse later in life. Data from the United States show that for 25% of households the total out-of-pocket spending over the last 5 years of life exceeds total household assets and for 40% it exceeds their financial assets (Kelley and al., 2010[31]).Older households appear to save in order to use their financial wealth in the last years of life when there is insufficient public support for long-term care (Nakajima and Telyukova, 2018[32]).
5.2.3. Overreliance on informal carers can generate high societal costs
Because of both public funding and service delivery gaps, much of the burden of providing EOLC falls on informal carers. Two-thirds of all people dying at age 65+ received informal care (Table 5.1), ranging from 46% in Switzerland to 86% in Finland. A high proportion of people dying at age 65 or over received some form of informal care. Moreover, a relative, most often children or grandchildren, provides most of the informal care. These data are in line with sources estimating that informal caregivers provide 75‑90% of home‑based care for people who are near the end of life (Gardiner et al., 2020[33]). In Canada, there are about 1.5 to 2 million end-of-life informal caregivers (Lung et al., 2021[34]).
Table 5.1. Proportion of deceased who died at age 65 or over who received informal care, 2008‑20
|
Country |
Received Informal Care |
Relationship to the Deceased |
|||
|---|---|---|---|---|---|
|
Spouse |
Children/ Grandchildren |
Relative |
Non-relative |
||
|
Austria |
62.95 |
31.13 |
48.19 |
8.81 |
13.87 |
|
Germany |
61.54 |
40.85 |
54.13 |
4.35 |
12.60 |
|
Sweden |
48.24 |
24.03 |
43.39 |
5.75 |
9.11 |
|
Netherlands |
59.09 |
42.56 |
45.08 |
9.26 |
9.94 |
|
Spain |
69.10 |
26.75 |
62.77 |
10.31 |
14.13 |
|
Italy |
72.00 |
25.80 |
67.27 |
8.73 |
10.36 |
|
France |
63.43 |
37.23 |
45.62 |
8.47 |
11.11 |
|
Denmark |
59.64 |
25.75 |
52.34 |
7.33 |
11.39 |
|
Greece |
69.61 |
24.78 |
67.47 |
10.98 |
12.77 |
|
Switzerland |
45.96 |
31.96 |
36.96 |
5.78 |
8.86 |
|
Belgium |
71.88 |
39.00 |
54.88 |
8.45 |
12.28 |
|
Israel |
57.49 |
28.07 |
45.10 |
3.52 |
5.05 |
|
Czech Republic |
66.99 |
33.95 |
67.99 |
5.37 |
14.78 |
|
Poland |
67.95 |
32.49 |
78.45 |
7.51 |
8.31 |
|
Ireland |
59.77 |
16.57 |
73.46 |
23.38 |
0.00 |
|
Luxembourg |
73.01 |
26.65 |
52.81 |
12.97 |
9.62 |
|
Hungary |
71.52 |
28.23 |
70.30 |
8.66 |
14.64 |
|
Portugal |
66.23 |
24.01 |
65.10 |
14.83 |
5.79 |
|
Slovenia |
73.03 |
33.43 |
71.23 |
8.92 |
10.84 |
|
Estonia |
66.78 |
30.43 |
48.39 |
7.83 |
11.20 |
|
Croatia |
68.79 |
24.90 |
71.81 |
8.49 |
16.04 |
|
Lithuania |
71.21 |
32.71 |
58.96 |
11.68 |
17.83 |
|
Bulgaria |
56.38 |
29.55 |
63.12 |
5.74 |
7.99 |
|
Cyprus |
70.55 |
24.49 |
51.63 |
0.00 |
12.12 |
|
Finland |
86.47 |
41.45 |
53.25 |
11.30 |
2.18 |
|
Latvia |
65.96 |
53.07 |
38.60 |
4.49 |
14.32 |
|
Malta |
62.98 |
34.44 |
66.26 |
0.00 |
6.36 |
|
Romania |
65.12 |
35.68 |
53.90 |
13.45 |
18.09 |
|
Slovak Republic |
82.64 |
41.69 |
73.05 |
7.37 |
3.62 |
|
United States |
81.39 |
31.28 |
52.97 |
10.38 |
14.01 |
|
Korea |
54.83 |
35.21 |
47.23 |
3.68 |
5.66 |
Note: Weighted using cross-sectional weight from last core interview. Data not available for SHARE Wave 5. It is possible that the deceased received informal care from multiple sources.
Source: Analysis based on data from SHARE (EoL wave 2‑4, 6‑8 interview), HRS (wave 3‑14), MHAS (wave 2‑5), KLoSA (wave 2‑7).
Not only do informal caregivers provide the bulk of care, but they might also influence the end-of-life experience (e.g. the place of death). According to the Survey of Health, Ageing and Retirement in Europe (SHARE), the Mexican Health and Aging Study (MHAS), the Korean Longitudinal Study of Aging (KLoSA) and the Health and Retirement Study (HRS) on the United States, in most countries people who receive informal care are slightly more likely to die at home (36% versus 33% see Figure 5.5).
Figure 5.5. Older people who received informal care are more likely to die at home
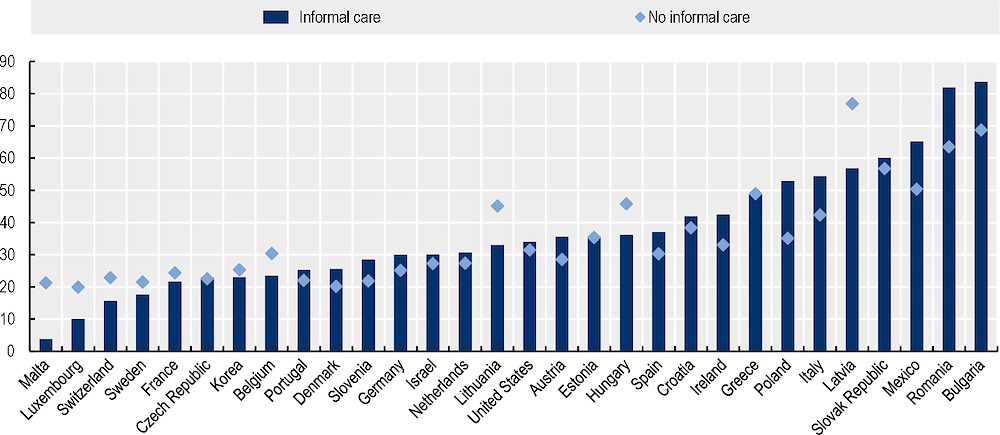
Note: Data weighted using cross-sectional weight from last core interview.
Source: Analysis based on data from SHARE (EoL wave 2‑8 interview), HRS (wave 3‑14), MHAS (wave 2‑5), KLoSA (wave 2‑7).
The financial costs of informal caring for a person approaching the end of life can be substantial. Such costs stem from three main areas: work-related costs (due to stopping work or reducing hours), carer time costs (cost related to time investment required by carers) and out-of-pocket costs. Caregivers can incur a number of out-of-pocket costs which include the cost of special food, travel expenses, additional care supplies and medication, and extra household costs to support the care recipient and this can represent 7%–13% of total caregiver costs (Coumoundouros et al., 2019[35]). Estimates suggests that the overall cost of caregiving ranges across countries from 26.6% to 80% of total costs at the end of life (Gardiner et al., 2014[36]). In the United Kingdom, 43% of people caring for someone at the end of life struggle financially and average out of pocket costs are GBP 3 300 per patient and GBP 1 500 per carer, every year (Marie Curie, 2019[29]).
Households experience high indirect costs from end of life due to the heavy burden of care undertaken by family carers. There is limited evidence on the impact of caregiving at the end of life on employment, but some studies report that caregivers have reported giving up work, reducing hours of work, or using up annual or sick leave to cope with the demands of caregiving. Data from Korea shows that those caring for someone with a terminal illness were 2.4 times more likely to be not working compared with the general population (Kim et al., 2013[37]). Changing jobs and accepting a low-paid occupation which might be more compatible with caregiving can also occur, as can early retirement. Caring for terminally ill loved ones often results in diminished lifetime earnings (O’Brien, Yang and Jankauskaite, 2020[38]) and/or reduced retirement savings (Girgis et al., 2013[39]). Even when caregivers could combine work and care, the situation could still be demanding, especially with the progression of illness leading to unpredictable care needs and work interruptions (Bijnsdorp et al., 2021[40]). Scheduling can become challenging when dealing with doctor’s appointments. More than half of the caregivers had one employment transition (between full-time employment, part-time, on-leave and not employed) and 29% had three or more over a period ranging between 2.6 and 6.4 months (Guerriere et al., 2020[41]). All employment changes and challenges accumulate and result in difficulties for career advancement (O’Brien, Yang and Jankauskaite, 2020[38]). Employment changes can result in an income loss which adds to other expenses. For instances, studies of cancer patients found that it was associated with an income loss of 1 000 per year for the spouse (Coumoundouros et al., 2019[35]).
Time spent on informal or family caregiving is especially intense in the last three months of life: caregivers of cancer patients provided an average of 70 hours per week of informal care (Rowland and al., 2017[42]). A study from Ireland, the United Kingdom and the United States found that when considering the hours that informal carers were on duty and valuing them average hourly wages and unit costs for nursing care, the costs to informal carers are larger than those to formal care services (health, social and voluntary combined) for people in the last three months of life. Costs of informal carers represent 58% of total societal costs (Higginson et al., 2020[43]). Costs are higher when death occurs at home: informal care costs at home were found to be USD 6 144 per month compared to USD 4 168 per month in the hospital (Yu, Guerriere and Coyte, 2015[44]).
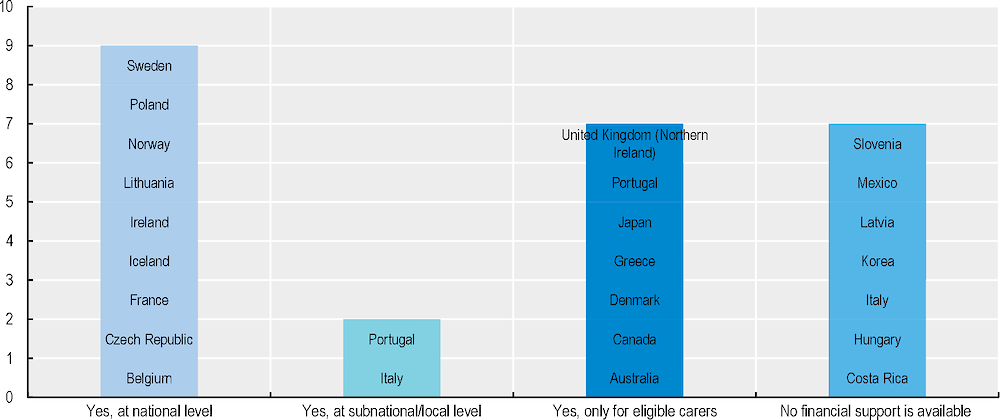
Limited support is provided to informal carers at the end of life. In particular, Figure 5.6 shows that not all countries provide financial support for carers. Yet, a Eurobarometer survey had found that financial remuneration was perceived as the most important support to informal caregivers (Gardiner et al., 2019[45]). Furthermore, when financial support is available, informal caregivers report difficulties navigating the bureaucratic application process to obtain such support. Eligibility criteria consider the hours of care provided, the income and employment status, as well as the relationship with the person cared for. According to a survey covering 6 OECD countries (Australia, Canada, Ireland, New Zealand, the United Kingdom, and the United States), eligibility criteria and application processed tend to discourage people from applying. This results in eligible people not receiving such benefits. For instance, only 12% of Canadian caregivers have used financial benefits. A further issue consists in people not defining themselves as caregivers and thus not applying for benefits they would be eligible to (Gardiner et al., 2019[45]).
Figure 5.6. Not all countries provide financial support for carers
Caregiving takes a toll on the physical and mental health of caregivers which is particularly prominent for those accompanying someone at the end of life. Several studies report on the emotional strain of caregiving at the end of life and the great deal of loss and grief experienced by caregivers (Williams, Wang and Kitchen, 2013[46]). A Canadian study comparing EOL caregivers with those providing short-term care and those providing long-term care to someone with an illness or dependency, found EOL caregivers are more negatively impacted by the often‑additional role of caregiving, financially, in terms of employment and especially in terms of their health.
5.3. How can countries improve the financing of end-of-life care?
5.3.1. Ensuring sufficient funding for end-of-life care
A stable and predictable funding that allows end-of-life services to be planned and developed in a coherent way is needed. A growing demand will place a challenge on the sustainability of funding in most countries for not having a policy to control the budget on end-of-life care (see Figure 5.7) This can create pressure on budgets as additional resources may still be required. Funding such investments requires finance and health ministries to agree solutions that combine raising additional funding with efforts to free up current resources by reducing wasteful spending in health systems. Such solutions require forward-looking, multi-year commitments (OECD, 2015[47]). They are also likely to involve a trade‑off with other priorities, especially in terms of exploring the possibility of reallocation and allocating possible additional resources to this specific area of health.
A more effective public financing should improve the alignment of EOLC services with EOLC needs. This requires budgets or reimbursement mechanisms that adequately fund priority EOLC services. Critical in this regard is better pricing, so that provider payments are set at accurate levels to cover the costs of service provision. Yet in some cases, payments are set below the average costs of service provision for palliative care patients. For examples, studies of palliative care wards in Poland show that payments from the national health system cover only 60% of the costs incurred by the units – thereby providing insufficient incentives for promoting such palliative care wards for providers (Ciałkowska-Rysz et al., 2016[48]). Changing the reimbursement amount of palliative care services by the National Health Insurance is likely to promote access to palliative care. As well as pricing, reimbursement rules are also important. For example, in Hungary, a single payment is received for each day on which the community-based palliative care team visits the patient, irrespective of the number or length of visits (Groeneveld EI, 2017[8]). As previously discussed, funding for each patient is limited to 150 visits over a longer period, but approximately 5% of patients require more than 150 days of care. In England, to improve the pricing of palliative care and reduce variation in funding, the NHS tested the introduction of a national “currency” for Specialist Palliative Care Providers. A “currency” is used to describe a consistent unit of health care, that is, interventions that are carried out in a health care setting and the complexity of the patients that are using that care, which may also be used as the basis for payment (NHS England, 2017[49]).
Figure 5.7. Most countries do not have a policy to control the budget on EOLC
With strong pressures to increase public spending, some governments have considered if the private sector can absorb some of such increases in health spending needing for end-of-life care. Currently options for private insurance in this area are limited. In the United States, most private insurance companies have a hospice benefit which covered 12% of end-of-life care expenditures (Raphael, Ahrens and Fowler, 2001[50]). An interesting example in severe disability in old age was Eldershield in Singapore where citizens were automatically enrolled at the age of 40, unless they explicitly chose to opt out and was provided by private insurers (this was replaced by a new system CareShield in 2020 which is now mandatory for recent cohorts).
Because cost-sharing appears to be sizeable, countries need to find an appropriate balance between the financial sustainability and the affordability of end-of-life care. Countries could consider target universal care benefits where needs are the highest, especially for those with low-income. Caps and exemption for those with low income might be relevant while considering some degree of means-testing to ensure that those with higher income contribute more. It would be important that thresholds set by public social protection systems are close to or above relative poverty levels to prevent that economically vulnerable care recipients are not eligible for increased public support. Some countries have introduced policies to limit out-of-pocket costs. Korea adopted a new insurance system from 15 July 2015, based on diagnosis-related groups (DRG) and per diem payment to support patients through a multidisciplinary approach and lighten their economic burden. Out-of-pocket expenses for patients decreased in the new payment system while length of stay is similar and there is no negative effect on quality of life (Lee et al., 2018[51]). Belgium and Germany have policies to decrease the out-of-pocket costs of GPs, physiotherapists, nursing home visits and/or pharmaceuticals. In Belgium people can obtain the legal palliative status, in which case they are not charged any out-of-pocket cost, while people with chronic diseases who are care‑dependent and live at home can fulfil the criteria to obtain EUR 130 per month. In Germany out-of-pocket is fixed to 1% of the annual household income for care dependent people. In France such policies are not in place, but the French health care system fixes an annual cap of EUR 50 for out-of-pocket expenditure per person (Maetens et al., 2017[52]).
5.3.2. Prioritising the most cost-effective interventions
Firstly, palliative care interventions have been associated with improvements in patient quality of life and symptom burden. Several studies have supported that palliative care reduces symptom burden, improves quality of life and mood and in some cases increased longevity or survival rates (Institute of Medicine, 2015[53]). A meta‑analysis of randomised control trials further provided robust evidence of quality of life and symptom improvement (Kavalieratos et al., 2016[54]). In addition, specialist palliative care has been shown to bring further benefits for patients, including a reduction in the likelihood of costly and often aggressive treatments such as chemotherapy in the last days of life (Hunter, 2018[55]).
Secondly, evidence from several countries shows that the introduction of better access to palliative care can result in more cost-effective outcomes (Public Health England, 2017[56]). A literature review including studies from nine OECD countries (Belgium, Canada, France, Greece, Israel, Italy, Spain, the United Kingdom and the United States) performed over ten years and with different characteristics has found consistent results on the cost-effectiveness of palliative care across settings (Smith et al., 2013[57]). Evidence from the United States found that transferring people into inpatient palliative care units resulted into 25% cost reduction (Isenberg et al., 2017[58]). Hospital palliative care teams can be cost-effective, for instance, especially with early introduction and integrated with other treatments, such as oncology (KMPG, 2020[59]). Care co‑ordination at the end of life is also important to manage care transitions and avoid discontinuities in care. Preventable hospital readmissions are frequently a consequence of poorly managed transitions. Care managers should be of prime importance at the end of life (Institute of Medicine, 2015[53]).
Comparing the costs of end-of-life care in hospital with the cost of equivalent care outside
Several studies have found that palliative care outside inpatient settings can enhance patient satisfaction, improve symptom control and quality of life, and reduce health care costs (Public Health England, 2017[56]). Some studies also show that hospice enrolment and care in nursing homes results in better quality at the end of life with lower public health expenditures (Abernathy et al., 2011[60]). An analysis of people at the end of life living with dementia found that being cared for in nursing homes seems to reduce the likelihood of using hospital care and ICU at the end of life, with same spending levels (Nicholas et al., 2014[61]). Evidence from Australia suggests that specialist palliative care in nursing homes reduced hospital admissions (KMPG, 2020[59]).
Several studies from Australia, Canada, the United Kingdom and the United States found that providing palliative care at the person’s home can be cost effective (Luta et al., 2021[62]; Higginson et al., 2003[63]; Gomes et al., 2013[64]), while additional literature has also found that palliative care in nursing homes can reduce costs and hospital use, as well as increasing the quality of life (Abernathy et al., 2011[60]). Evidence has shown that home care is cost-effective and provides potential benefits for people receiving care and their relatives, together with lower health care costs (Luta et al., 2021[62]; Higginson et al., 2003[63]; Gomes et al., 2013[64]). The effectiveness of palliative care stems mainly from reducing length of hospital stays, re‑admissions, and visits to intensive care units (Hodgson, n.d.[65]). In Belgium, for instance, patients using palliative home care support had lower ICU and emergency visits (Maetens et al., 2019[66]).
Home‑based palliative care appears to have a sizeable impact on expenditures, depending on the country. In the United States, a proactive, community‐based palliative care programme engaged participants several months before death, resulted in dramatically lower hospital usage and lower health care expenditures, achieved with modest programme costs (Cassel and al., 2016[67]). In Ontario, Canada, an in-home palliative team care was cost-effective; it increased the chance of dying at home by 10%, increased the average number of days at home (6 days) and quality-adjusted lifedays (0.5 days), and it reduced costs by approximately USD 4 400 per patient (Pham and Kram, 2014[68]). An analysis on the effectiveness of the Australian Palliative Care Extended Packages at Home (PEACH) pilot found that it increased at-home stay by one day. The mean direct cost of PEACH was AUD 3 489 per patient, which was largely offset by cost savings amounting to AUD 2 450. Although a lower share of people died at home when receiving care as part of the pilot compared to usual care (McCaffrey et al., 2013[69]), in 79% of cases this was in line with their wishes (Agar et al., 2022[70]). A study from the United Kingdom found that the estimated cost of a day of community care at the end of life is GBP 145 compared to the cost of GBP 425 for a specialist palliative care bed day in hospital. Overall, a meta‑analysis concluded that home‑based palliative care may contribute to an improvement in quality of care by reducing medicalisation at the end of life and therefore reducing costs (Luta et al., 2021[62]). This indicates that changing the setting of care of a patient at the end of life has the potential to reduce the daily cost by GBP 280 (Marie Curie, 2012[71]). At the same time, the extent of cost-savings cannot be determined with confidence because many studies did not consider the additional community costs and informal cost to carers (Hunter, 2018[55]).
The literature has also explored the potential cost savings at the end of life linked to the use of advance care planning, showing mixed results. A literature review including studies from Canada, Singapore, the United Kingdom, and the United States found that around half of the studies showed cost savings attributable to the use of advance care planning. The studies showing a reduction in health care costs linked to advance care planning also reported reductions in the use of hospital care and acute care (e.g. ICU) at the end of life. Further analysis of the potential cost savings – and cost effectiveness – linked to advance care planning may be beneficial (Dixon, 2015[72]).
5.3.3. Adapting health financing mechanisms to incentivise a more appropriate mix of end-of-life care services
Improving provider payments
While countries use a variety of payment systems, better linking provider payments to population needs will be important. In most countries, a mix of activity-based and non-activity-based payment exists for EOLC. In the United States, Medicare payment for hospices has a fixed per diem rate. In England, Ireland, New Zealand and Norway, block contracts are often used to pay for services, while Spain uses capitation-based resource allocation (Groeneveld EI, 2017[8]). In Germany, experts in clinical care and health care financing identified weaknesses in both reimbursement mechanisms used for palliative care, per-diem payments and payments based on the diagnosis-related group (DRG) (Schildmann et al., 2019[73]). DRGs do not sufficiently classify palliative care and may fail to fully account for the unique needs of the individual patient, instead looking at the broader definitions around their official disease diagnosis (Schildmann et al., 2019[73]). In an analysis of patients who received palliative care in two German hospitals, researchers found that existing DRG categories did not sufficiently capture the true costs of palliative care, with the cost of the extra health care staff time needed to provide quality palliative care, in particular, not reflected in existing DRGs (Vogl et al., 2018[74]) In contrast, in Australia, a patient characteristic-based payment model has been rolled out nationally. The amount of reimbursement received per patient varies by performance status, phase of illness, care setting and age (Groeneveld EI, 2017[8]). Similar patient-characteristic payment models are currently being explored in England and Switzerland.
Different funding streams between curative care and palliative care can impede early access to palliative care. Designing funding to recognise the complementarity of different care services and their integration would be beneficial. Currently, payment systems do little to support new care models that for instance improve care co‑ordination as health service provision is predominantly financed in a “silo”. For instance, it has been found that in Canada, acute‑care beds are substantially more expensive than hospice or in-patient palliative‑care beds, long-term care (LTC) beds or homecare and, if budgets were global, then efficiencies would be found by increasing capacity in lower-cost settings to reduce backlogs in higher-cost settings (Kieran Quinn, 2021[75]). Frequently, this results in fragmentation of care with poor patient experience and poor health outcomes.
Recommendations for improved funding in end-of-life care include thinking about integrated funding – with some form of bundling of the palliative and curatively oriented components of care (Duckett, 2018[76]). Bundled payments have been used for specific diseases but are complex to implement, particularly in setting tariffs (OECD, 2016[77]). Yet, a bundled payment for those with a diagnosis of advanced illness may provide strong incentives to provide care in teams, thereby reducing fragmentation. It would be important to signal that choosing palliative care should not necessarily mean giving up on seeking a cure but rather on improving quality of life and possibly, even living longer. Medicare is testing a new model of care –Medicare Choices – that would allow patients to continue receiving curative care once they enter hospice care – an option that has been unavailable until now (May et al., 2021[78]).
In the United States, there has been progress towards value‑based payments which might favour more palliative care. In general, the use of fee‑for-service payment might encourage providers to have more curative care instead of palliative care which requires more time‑intensive care. Medicare has seen growth in Medicare Advantage (MA) which pays private insurers a risk-adjusted fee to administer bundled inpatient, outpatient and typically prescription drug benefits to Medicare beneficiaries who opt into these plans and makes providers likely to gain financially from promoting palliative care as it has been shown to reduce overall expenditures. It also promotes Medicare’s hospice benefit because the MA plan is no longer responsible for the expenses, but costs are borne by original Medicare under the hospice benefit. Medicare also has moved toward value‑based care that is more consistent with palliative care through the growth of accountable care organisations (ACOs) and other special payment models in original Medicare. These models provide incentives for co‑ordinated care by investing in data infrastructure and offering providers a share in any savings (and increasingly in any loss) to Medicare relative to projected targets and subject to meeting quality guidelines. Nevertheless, evidence of the effectiveness of ACOs is mixed. One of the issues related to their use consists in the difficulty to define when a person is likely to die. People whose likelihood to die soon is easy to predict only represent a small share of the total number of people who are nearing the end of their life (Gilstrap et al., 2018[79]).
Quality measures related to end-of-life care are needed to transform the payment system to a system where there is payment for quality or value. In England (United Kingdom) there are pay-for-performance systems to incentivise GPs to identify and manage palliative care needs. For instance, the Quality and Outcome Framework incentivised GPs to keep a register of patients who need palliative care and to have regular multidisciplinary reviews where the cases of people in need of palliative care are discussed.
Incentivising care outside hospitals
Given the evidence pointing to cost- effectiveness of palliative care outside hospitals, rethinking payment systems to incentive such care might be useful. In this sense, it is important to avoid uncapped funding for hospital-based palliative care while home‑based care is capped. Similarly, separate funding for different places of death can create negative incentives and would require funding to be aligned for services in different locations. Allowing the benefits to follow the patient would ease problems with transitions and give patients a broader range of options. Improving the adequacy of payment levels for health care in nursing homes might contribute to more desirable outcomes overall, and at the end of life, although further cost-effectiveness analysis would be beneficial.
Several countries have introduced funding changes to incentivise the use of home‑based palliative care. England has introduced personal health budgets for end-of-life in five areas with the goal of having more personalised care (HSJ solutions, 2017[80]). The use of personal health budgets has resulted in 82% of people dying in their preferred place while allowing people to purchase services which were not previously available and resulting in a cost neutral or reduced cost compared with the traditionally commissioned care. A personal health budget is in place in The Netherlands as well (persoonsgebonden budget (PGB)), for people who need help at home due to illness or disability or for palliative care needs (Government of the Netherlands, 2022[81]). France has introduced as part of the action plan on end of life in 2022 additional funding for out-of-hours palliative care and a reinforcement of mobile teams to promote palliative care at home. Mobile palliative care teams (EMSP) are funded by global budgets. The price is set by the Regional Health Office (ARS) according to the number of full-time‑equivalent persons working in the team and considers the travel costs. The payment also includes a contribution to the structural costs of the hospital that the team is attached to. The amount of payment for organisational costs may be assessed by the ARS based on hospital accounting data (WHO/OECD, 2021[82]). The Australian Government has announced in December 2021 an investment of AUD 56 million to improve the provision of palliative care at home. AUD 37 million will be invested in scaling up the Greater Choice for At Home Palliative Care programme – which has so far been successful as a pilot programme to improve access to palliative care at home (Department of Health and Aged Care, 2021[83]). Since 2007 in Germany GPs can refer people to specialised outpatient palliative care services (SAPV), which include medical, nursing, and psychological services. The SAVOIR project analysed people’s satisfaction regarding SAPV services and found a general positive attitude towards SAPV across the country, despite regional differences in the characteristics of the services provided (Gemeinsamer Bundesausschuss, 2019[84]).
Countries are also implementing policies to improve the provision of end-of-life care in nursing homes. In Luxembourg, for instance, up until now nursing homes were not allowed to have medical devices onsite (like stocks operated by pharmacists). As of end of 2022, new legislation to allow stocks operated by pharmacists in nursing homes has passed and its implementation is foreseen in January 2023. The impact of such change on hospital admissions will be monitored. In France, to avoid hospitalisations and improve the quality of care at the end of life, the hospital at home (HAH) protocol is available in nursing homes so that nursing homes can provide palliative treatments that require material and medical services that are not normally available. The palliative care in HAH, is paid by an activity-based payment scheme using palliative care DRGs (WHO/OECD, 2021[82]). As part of the AUD 56 million investment for end-of-life care in Australia, the government has announced an investment of AUD 19 million on improving end-of-life care in residential aged care (Department of Health and Aged Care, 2021[83]). Furthermore, the European Union has funded the Palliative Care for Older People in Care and Nursing homes in Europe (PACE) project in six countries (Belgium, Finland, Italy, the Netherlands, Poland, and the United Kingdom). The project aims at producing toolkits and guidelines for governments to improve the provision of palliative care in nursing homes.
5.3.4. Countries need to find a better balance between supporting and relying on family carers
Policies to support informal carers such as cash benefits, respite care, leave and training heavily influence the availability and burden of informal cares. Such policies are particularly important in case of a shift towards more home EOLC which may also have unintended consequence on caregivers, especially if formal home services are insufficient. Indeed, informal caregivers of patients dying at home spent more than twice as much time on unpaid caregiving compared with those caring for patients dying in hospital (Gardiner et al., 2020[33]).
Because financial issues are often a major barrier in the provision and receiving of palliative home care, specific allowances, or other financial incentives to both patients and informal caregivers are important. As mentioned in Section 5.3.3, several countries do not provide such benefits for carers. Cash benefits could help to expand the supply of otherwise unpaid carers, but there are also important trade‑offs for both carers and care recipients which need to be considered. It is important that cash benefits are not used to substitute the formal care providers, thereby impacting the quality of care. They are an adequate tool to prevent poverty and social exclusion and should be made more widely available but should not trap family carers into a low-paid unwanted role. For instance, in Belgium informal caregivers can receive EUR 786.76 per month. Informal caregivers who work in the Flanders are also entitled to the Flemish encouragement allowance for up to two years (EUR 123.95 per month), which serves as an incentive to remain attached to the labour market and return to their jobs. Furthermore, 82% of Flemish municipalities offer an allowance of an additional EUR 30 per month on average. In France, people who are accompanying a relative to death can receive a daily allowance of around EUR 56 for up to 21 days per year. Parisian residents are also entitled to an additional allowance of up to EUR 610 per month for up to 3 months (12 months if the terminally ill is a child) (Maetens et al., 2017[52]).
The design of the eligibility criteria for carers’ allowance should be carefully weighted to ensure an adequate trade‑off between the generosity of the cash benefit and the size of the eligible population. Typically, such cash allowances involve several eligibility requirements with a view to define an eligible carer, the level of care effort, and the relationship between the carer and the care recipient (e.g. certain relatives, co-residency). Countries also use very different compensation and eligibility conditions. Two main approaches, discussed below, emerge: i) countries providing remuneration to family carers who are formally employed; and ii) countries with means-tested allowances. In most Nordic countries, remuneration is subject to a contract with the carer and can last a maximum amount of time. For instance, in Denmark, the eligibility requirements specify that the caree receives palliative care and is expected to die in 3‑6 months. In English-speaking countries, allowances are subject to means-testing and eligibility conditions may result in disincentives to work as there are often not combined with several work hours.
Caregiving may have detrimental effects on the health and well-being, especially at the end of life. Likewise, bereavement may be associated with excess risk of mortality, a decline in health and higher rates of medical use and hospitalisation. Integrating relative and family in end-of-life care decisions and increasing understanding of the end-of-life process appears to be beneficial for both the patient experience and the psychological recovery of the relatives. Addressing emotional strain by providing coping strategies such as self-care, stress management, problem-solving and decision-making guidance are fruitful avenues to reduce caregiver stress and improve quality of care (Brimblecombe et al., 2018[85]). Such policies are likely to have a financial impact as well as there is evidence that counselling results in lower health care utilisation for caregivers and that assisting caregivers can reduce their productivity losses (KMPG, 2020[59]).
Yet, while information and advice are available in just over half of the countries, only 8 counties provide counselling and training (Figure 5.8). Availability of training services is often fragmented across OECD countries. Most training is typically provided through local initiatives and relies heavily on the voluntary sector. In Luxembourg, an NGO Omega 90 is providing follow-up support for informal carers after bereavement. In some countries, training is tied to a cash benefit specific to informal carers. In Norway, municipalities have the obligation to deliver training to caregivers providing intense care, under specific conditions, while in the Netherlands both volunteers and informal carers receive training on end-of-life care through a well-established national programme (OECD interviews, 2021). In the United States, there is a broad programme for all type of carers for the elderly, the National Family Caregiver Support Program (NFCSP). It is administered by the Administration for Community Living of the US Department of Health and Human Services. States and territories receive funding based on the proportion of their population age 70 and older and are required to offer various core services in partnership with local public centres (“Area Agencies on Aging”) and local service providers, including individual counselling, support groups, and caregiver training.
Figure 5.8. Support is focused on information, but specific counselling and training is lacking
Respite care, which is designed to offer caregivers a break from their regular duties, is viewed as a policy that helps carers to overcome some of the physical and psychological challenges from their caregiving role. It is often perceived as the most important and common form of support to alleviate caregiving burden (COFACE, 2017[86]). A review covering 11 OECD countries (Austria, Belgium, Czech Republic, Denmark, France, Germany, Luxembourg, Slovenia, Spain, Sweden, and Switzerland) found respite care to be the most effective support measure to improve the mental well-being of in-house informal caregivers (Calvó-Perxas et al., 2021[87]). Carers of people with advanced and terminal illnesses face considerable uncertainty over the length of time for which they are committing themselves to care, and what may be involved in delivering that care. Respite care could be provided as inpatient care, for instance in hospices, as day care or at home. In the United Kingdom, several types of respite care are available, including day care centres, homecare from a paid carer, short stays in care homes, respite holidays and sitting services. Respite care in the United Kingdom can be paid out-of-pocket or its cost can be covered by a charity or public funding. In the last case, both the person in need of care and their informal caregiver must undergo a needs assessment to qualify for the funding (NHS, 2019[88]). Often, there is restricted availability of respite care at home but there is some limited evidence that the service appears to be associated with better quality home care (Ingleton et al., 2003[89]). Yet, respite care is not always fully funded or available. In Belgium, respite care centres are reimbursed only for caregivers of terminally ill minors (Maetens et al., 2017[52]). In Germany, respite care is available for up to four weeks per calendar year if the caregiver is temporarily unavailable to provide home care and accommodation and food costs are paid by the patient or their family (Maetens et al., 2017[52]).
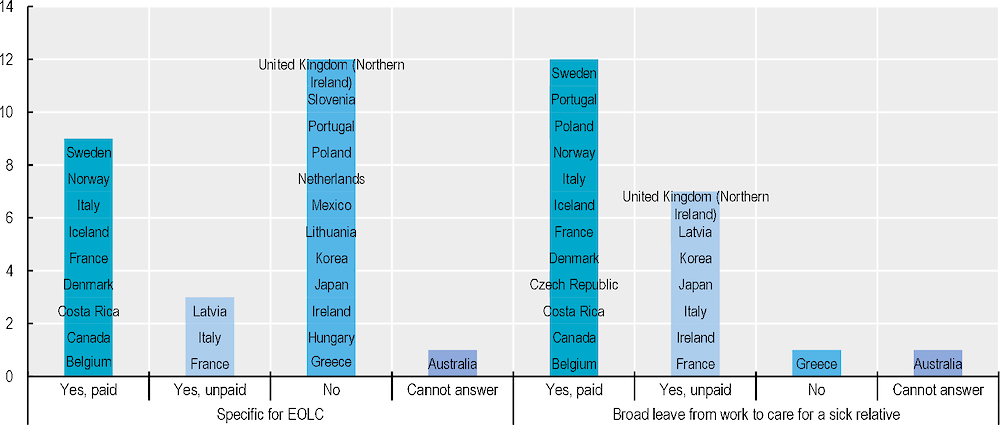
Across OECD countries, there is growing commitment to support informal carers combining work and caring but paid leave is not widely available, especially for terminal illness. Among EU countries, this is well exemplified by the Work-life Balance Directive, which entered into force in 2019 and must be adopted by member states within three years. The directive includes a carers’ leave: workers providing personal care or support to a relative will be entitled to five days of leave per year. Three‑quarters of OECD countries (30 countries) provide some rights to leave to care for a family member – either paid or unpaid – up from two‑thirds of countries 10 years ago (Rocard and Llena-Nozal, 2022[90]), while 12 OECD countries have specific care leave for end-of-life care, 9 of which have paid leave (Figure 5.9). In the future, countries need to find a way of promoting a better work-life balance care leave because it allows employees to provide care without having to worry about income loss or job security. Currently, leave entitlements vary starkly across countries in terms of duration, eligibility criteria and degree of compensation.
Figure 5.9. Only half of OECD countries have a special statutory leave from work for EOLC
Several countries have a more generous duration for palliative care paid leave. This is the case for Denmark, where employees have the statutory right to leave for the care of someone close dying, according to the Act on Leave from work due to Special Family reasons (March 2006) and there is no fixed time limit for the leave. In France since 2 March 2010 Law, family solidarity leave is available for three months (renewable once), but financial support for palliative care is only available for a maximum of 21 days. Sweden allows both family and relatives of a dying person to obtain leave for up to 100 days (Observatory for Sociopolitical Developments in Europe, 2016[91]), while 60 days of paid leave are available in Norway for informal caregivers (OECD interviews, 2021). Furthermore, the employer had a legal obligation to ensure the return to work after palliative care leave. Canada implemented in 2004 the Compassionate Care Benefit, which allows family caregivers to obtain up to six weeks of leave from work to care for a relative at the end of life. During the leave, informal caregivers receive up to 55% of their average earnings with a fixed cap of CAN 435 per week (Crooks and Williams, 2008[92]). Although such leave is generous in terms of weeks off, the halving of salary is likely to represent an issue for informal carers who need to provide care for a prolonged time. In Belgium, there is a palliative care leave for up to 3 months, but employees might also benefit from a time credit (part-time or full-time career break) from one year to up to five years leave full or part-time. In Japan, while employers are not obligated to offer paid leave to informal carers, there is a public system in place that provides financial support equivalent to 67% of the number of usual wages to those who meet certain requirements.
Yet, some other countries have much less generous leave arrangements, such as Luxembourg, where the “congé d’accompagnement de fin de vie” is for five working days at a time and per year. The Netherlands only allows employees to receive care leave, while this is not available for self-employed carers. Care leave has a cap of 240 hours per year and is unpaid. In some cases, financial support can be received based on collective bargaining agreements or working arrangements. In the Czech Republic, relatives of dependent persons are entitled to a right to work part-time, which is de facto rarely granted by employers (Observatory for Sociopolitical Developments in Europe, 2016[91]). Moreover, in many countries there is no specific leave to take care of a relative with terminal illness nor broad care leave (e.g. Croatia, Greece, Hungary, Portugal) or only unpaid broad care leave (e.g. Korea). Even for broad entitlement to leave for care, only about half of countries offer some form of paid leave for caring and it tends to be restricted to a short duration.
Flexible working arrangements can also support informal caregivers balancing personal and professional responsibilities with care needs. A study from the United States found that flexible working hours increased by 50% the likelihood that women caregivers would still be employed after two years of caregiving (Pavalko and Henderson, 2006[93]). Evidence from the United Kingdom also shows similar results, with supportive employers and flexible working arrangements being listed as the most relevant factors to retain employees with caregiving responsibilities (Gardiner et al., 2019[45]). Furthermore, the literature reports that informal caregivers value their job and that their workplace represents a way for them to obtain some respite from the caregiving (Bijnsdorp et al., 2021[40]). Allowing flexible work arrangement would thus benefit caregivers and would likely have a stronger impact on women, who are more likely to quit the labour market due to caregiving responsibilities. Across OECD countries, on average more than half of employees have their working hours set by their employer without possibility for change, with this share ranging from over 30% in Sweden to around 75% in Lithuania (Rocard and Llena-Nozal, 2022[90]). In some countries, together with paid leave, informal caregivers have the possibility of obtaining flexible working arrangements such as part time jobs. In Germany people can reduce their working hours to 15 hours per week for a maximum of two years. During the two years, part of the salary lost can be received in the form of a loan to be repaid without interests after the person returns to work full time, in the form of salary reductions (Maetens et al., 2017[52]). As mentioned above, in Belgium carers can negotiate part-time work arrangements or a break from work from 1 to 5 years. Furthermore, in Norway, people caring for a dying relative can work from home (OECD interviews, 2021). The pandemic has boosted the use of flexible working arrangements. The number of people working from home has increased substantially in OECD countries, by one‑third on average, and has been particularly high among women (Rocard and Llena-Nozal, 2022[90]).
5.4. Conclusions
This chapter shows that, despite the concern about high cost at the end of life, very few countries have data which is comparable on the topic and on the drivers of end-of-life care expenditures. Similarly, countries do not tend to have a policy to control end-of-life care budgets, even though needs and expectations are growing. International evidence conveys that end-of-life spending comprises only a modest fraction of aggregate expenditures, because the fraction of the population that dies in any given year is small, but projections on the number of people dying forecast an increase in those numbers and this will have an upward impact on costs (French et al., 2017[7]). Countries will need to make sure that end-of-life care is adequately funded in a sustainable manner to address future needs.
Yet the focus on costs should not overshadow the importance of ensuring that financing of end-of-life care is appropriate and provides high-quality people‑centred care in the last days or months of life. Currently, end-of-life care is publicly funded in most OECD countries, but public coverage is often partial and varies across settings of care. Partial public coverage leads to people relying heavily on informal support, with half of people currently receiving informal care before dying. Overreliance on informal care, without adequate public support for informal carers, generates indirect societal costs linked to the reduced employment and financial costs that can affect informal carers. Similarly, many patients do not receive palliative care to manage their pain and other symptoms, and financing should be redesigned in a way that there are more incentives for promoting palliative care and cost-effective interventions outside of hospitals, as well as ensuring better end-of-life planning with a view to reducing unplanned hospital costs.
References
[60] Abernathy, A. et al. (2011), “Death service ratio: a measure of hospice utilization and cost impact. 2011”, J Pain Symptom Manage, Vol. 41, pp. 5-6.
[70] Agar, M. et al. (2022), “Factors Associated With Mode of Separation for People With Palliative Diagnoses With Preference for Home Death Receiving Care From a Nurse-Led End of Life (Palliative Extended and Care at Home) Program”, Journal of Hospice & Palliative Nursing, Vol. Publish Ahead of Print, https://doi.org/10.1097/njh.0000000000000841.
[20] Andrea C. Enzinger, K. (2021), “US Trends in Opioid Access Among Patients With Poor Prognosis Cancer Near the End-of-Life”, Journal of Clinical Oncology, pp. 2948-2958.
[6] Banarto, A. et al. (2004), “Trends in Inpatient Treatment Intensity among Medicare Beneficiaries at the End of Life”, Health Serv Res, Vol. 39/2, pp. 363-376, https://doi.org/10.1111/j.1475-6773.2004.00232.x.
[40] Bijnsdorp, F. et al. (2021), “Combining paid work and family care for a patient at the end of life at home: insights from a qualitative study among caregivers in the Netherlands”, BMC Palliative Care, Vol. 20/1, https://doi.org/10.1186/s12904-021-00780-9.
[85] Brimblecombe, N. et al. (2018), “Review of the international evidence on support for unpaid carers”, Journal of Long-Term Care, Vol. 0/0, p. 25, https://doi.org/10.31389/jltc.3.
[87] Calvó-Perxas, L. et al. (2021), “A longitudinal study on public policy and the health of in-house caregivers in Europe”, Health Policy, Vol. 125/4, pp. 436-441, https://doi.org/10.1016/j.healthpol.2021.02.001.
[14] Cardona-Morrel, M. et al. (2016), “Non-beneficial treatments in hospital at the end”, International Journal for Quality in Health Care, Vol. 28/4, pp. 456-469, https://doi.org/10.1093/intqhc/mzw060.
[67] Cassel and E. al. (2016), “Effect of a Home-Based Palliative Care Program on Healthcare Use and Costs”, Journal of the American Geriatrics Society.
[48] Ciałkowska-Rysz, A. et al. (2016), “How much does care in palliative care wards cost in Poland?”, Archives of Medical Science, Vol. 2, pp. 457-468, https://doi.org/10.5114/aoms.2016.59272.
[86] COFACE (2017), Study on the challenges and needs of family carers in Europe | COFACE, http://www.coface-eu.org/resources/publications/study-challenges-and-needs-of-family-carers-in-europe/ (accessed on 29 August 2020).
[35] Coumoundouros, C. et al. (2019), “The direct and indirect financial costs of informal cancer care: A scoping review”, Health & Social Care in the Community, https://doi.org/10.1111/hsc.12808.
[92] Crooks, V. and A. Williams (2008), “An evaluation of Canada’s Compassionate Care Benefit from a family caregiver’s perspective at end of life”, BMC Palliative Care, Vol. 7/1, https://doi.org/10.1186/1472-684x-7-14.
[25] De Nardi, M. et al. (2016), “Medical spending on the U.S. elderly”, Fiscal Studies, Vol. 37/3-4, pp. 327-344.
[83] Department of Health and Aged Care (2021), $56 million to improve end of life care for Australians, https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/56-million-to-improve-end-of-life-care-for-australians#:~:text=The%20Australian%20Government%20will%20invest,and%20palliative%20care%20for%20Australians.&text=The%20Morrison%20Government%20wil.
[72] Dixon, J. (2015), “The economic evidence for advance care planning: systematic review of evidence”, Palliative medicine.
[76] Duckett, S. (2018), “Aligning policy objectives and payment design in palliative care”, BMC Palliat Care.
[16] Earp, M. et al. (2021), “Hospital-based acute care in the last 30 days of life among patients with chronic disease that received early, late or no specialist palliative care: A retrospective cohort study of eight chronic disease groups”, BMJ Open, Vol. 11/3, https://doi.org/10.1136/bmjopen-2020-044196.
[4] Einav, E. et al. (2018), “Predictive modeling of U.S. health care spending in late life”, Science, Vol. 360/6396, pp. 1462-1465, https://doi.org/10.1126/science.aar5045.
[7] French, E. et al. (2017), “End-Of-Life Medical Spending In Last Twelve Months Of Life Is Lower Than Previously Reported”, Health Affairs, Vol. 36/7, pp. 1211-1217, https://doi.org/10.1377/hlthaff.2017.0174.
[36] Gardiner, C. et al. (2014), “Exploring the financial impact of caring for family members receiving palliative and end-of-life care: a systematic review of the literature”, Palliative Medicine, Vol. 28/5, pp. 375-90, https://doi.org/10.1177/0269216313510588.
[33] Gardiner, C. et al. (2020), “Equity and the financial costs of informal caregiving in palliative care: a critical debate”, BMC Palliat Care.
[45] Gardiner, C. et al. (2019), “Comparison of financial support for family caregivers of people at the end of life across six countries: A descriptive study”, Palliative Medicine, Vol. 33/9, pp. 1189-1211, https://doi.org/10.1177/0269216319861925.
[84] Gemeinsamer Bundesausschuss (2019), SAVOIR – Evaluation of the SAPV Guideline: Outcomes, Interactions, Regional Differences, https://innovationsfonds.g-ba.de/projekte/versorgungsforschung/savoir-evaluierung-der-sapv-richtlinie-outcomes-interaktionen-regionale-unterschiede.5.
[79] Gilstrap, L. et al. (2018), “Changes In End-Of-Life Care In The Medicare Shared Savings Program”, Health Affairs, Vol. 37/10, pp. 1693-1700, https://doi.org/10.1377/hlthaff.2018.0491.
[39] Girgis, A. et al. (2013), “Physical, Psychosocial, Relationship, and Economic Burden of Caring for People With Cancer: A Review”, Journal of Oncology Practice, Vol. 9/4, pp. 197-202, https://doi.org/10.1200/jop.2012.000690.
[64] Gomes, B. et al. (2013), “Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers”, Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.cd007760.pub2.
[81] Government of the Netherlands (2022), Applying for a personal budget, https://www.government.nl/topics/care-and-support-at-home/applying-for-a-personal-budget.
[8] Groeneveld EI, C. (2017), “Funding models in palliative care: Lessons from international experience”, Palliative Medicine, pp. 296-305.
[41] Guerriere, D. et al. (2020), “Transitions in Labour Force Participation over the Palliative Care Trajectory”, Healthcare Policy | Politiques de Santé, Vol. 16/2, pp. 25-40, https://doi.org/10.12927/hcpol.2020.26355.
[63] Higginson, I. et al. (2003), “Is There Evidence That Palliative Care Teams Alter End-of-Life Experiences of Patients and Their Caregivers?”, Journal of Pain and Symptom Management, Vol. 25/2, pp. 150-168, https://doi.org/10.1016/s0885-3924(02)00599-7.
[43] Higginson, I. et al. (2020), “Associations between informal care costs, care quality, carer rewards, burden and subsequent grief: the international, access, rights and empowerment mortality follow-back study of the last 3 months of life (IARE I study)”, BMC Medicine, Vol. 18/1, https://doi.org/10.1186/s12916-020-01768-7.
[65] Hodgson, C. (n.d.), Cost-effectiveness of palliative care: A review of the literature.
[80] HSJ solutions (2017), CG provides support and enables patients to co-design and personalise their end of life care, resulting in 82% of people dying in their preferred place of care, https://solutions.hsj.co.uk/story.aspx?storyCode=7019244&preview=1&hash=873501F51809621AFA3084F98EB5E354.
[55] Hunter, O. (2018), End of Life Care briefing, IPPR.
[89] Ingleton, C. et al. (2003), “Respite in palliative care: A review and discussion of the literature”, Palliative Medicine, https://doi.org/10.1191/0269216303pm803ra.
[53] Institute of Medicine (2015), Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life, National Academy of Sciences.
[58] Isenberg, S. et al. (2017), “Impact of a New Palliative Care Program on Health System Finances: An Analysis of the Palliative Care Program Inpatient Unit and Consultations at Johns Hopkins Medical Institutions”, Journal of Oncology Practice, Vol. 13/5, pp. e421-e430, https://doi.org/10.1200/jop.2016.014860.
[54] Kavalieratos, D. et al. (2016), “Association Between Palliative Care and Patient and Caregiver Outcomes: A Systematic Review and Meta-analysis”, JAMA.
[15] Kelley, A. (2011), “Treatment intensity at end of life-time to act on the evidence”, Lancet, pp. 1364–5.
[31] Kelley, A. and al. (2010), “Out-of-Pocket Spending in the Last Five Years of Life”, Natl Bur Econ Res Bull Aging Health, Vol. 2, pp. 3-4.
[75] Kieran Quinn, S. (2021), Expensive Endings:Reining In the High Cost of End-of-Life Care in Canada.
[37] Kim, S. et al. (2013), “Employment Status and Work-Related Difficulties among Family Members of Terminally Ill Patients Compared with the General Population”, Asian Pacific Journal of Cancer Prevention, Vol. 14/1, pp. 373-379, https://doi.org/10.7314/apjcp.2013.14.1.373.
[59] KMPG (2020), Investing to Save: The economics of increased investment in palliative care in Australia.
[11] Krakoviaw, P. (2020), “Gaps in end-of-life care and lack of support for family carers in Poland and Central Eastern Europe”, Palliative Care & Social Practice, pp. 1-10.
[23] Krizanova, K. and A. Skripekov (2015), “Palliative care in Slovakia has come a long way since the 1990s”, European Journal of palliative care.
[2] Lee, T. and G. Stoye (2019), Variation in end-of-life hospital spending in England: Evidence from linked survey and administrative data.
[51] Lee, Y. et al. (2018), Effects of a new medical insurance payment system for hospice patients in palliative care programs in Korea. 2018.
[1] Lorenzoni, L. et al. (2019), “Health Spending Projections to 2030: New results based on a revised OECD methodology”, OECD Health Working Papers, No. 110, OECD Publishing, Paris, https://doi.org/10.1787/5667f23d-en.
[34] Lung, E. et al. (2021), “Informal Caregiving for People With Life-Limiting Illness: Exploring the Knowledge Gaps”, Journal of Palliative Care, Vol. 37/2, pp. 233-241, https://doi.org/10.1177/0825859720984564.
[13] Luta, X. et al. (2020), “Healthcare trajectories and costs in the last year of life: a retrospective primary care and hospital analysis”, BMJ Supportive & Palliative Care, pp. bmjspcare-2020-002630, https://doi.org/10.1136/bmjspcare-2020-002630.
[62] Luta, X. et al. (2021), “Evidence on the economic value of end-of-life and palliative care interventions: a narrative review of reviews”, BMC Palliative Care, Vol. 20/1, https://doi.org/10.1186/s12904-021-00782-7.
[66] Maetens, A. et al. (2019), “Impact of palliative home care support on the quality and costs of care at the end of life: A population-level matched cohort study”, BMJ Open, https://doi.org/10.1136/bmjopen-2018-025180.
[52] Maetens, A. et al. (2017), “Policy Measures to Support Palliative Care at Home: A Cross-Country Case Comparison in Three European Countries”, Journal of Pain and Symptom Management, Vol. 54/4, pp. 523-529.e5, https://doi.org/10.1016/j.jpainsymman.2017.07.022.
[29] Marie Curie (2019), “The cost of dying”, https://www.mariecurie.org.uk/globalassets/media/documents/policy/policy-publications/2019/00962-cost-of-dying_financial-impact-report.pdf (accessed on 2022).
[71] Marie Curie (2012), Understanding the cost of end of life care in different settings.
[26] Marshall, S., K. McGarry and J. Skinner (2010), “The Risk of Out-of-Pocket Health Care Expenditure at End of Life”, NBER.
[78] May, P. et al. (2021), Advancing the Economics of Palliative Care: The Value to Individuals and Families, Organizations, and Society, USC Schaeffer.
[69] McCaffrey, N. et al. (2013), “Is home-based palliative care cost-effective? An economic evaluation of the Palliative Care Extended Packages at Home (PEACH) pilot”, BMJ Supportive & Palliative Care, Vol. 3/4, pp. 431-435, https://doi.org/10.1136/bmjspcare-2012-000361.
[32] Nakajima, M. and I. Telyukova (2018), Medical expenses and saving in retirement: The case of U.S..
[88] NHS (2019), Carers’ breaks and respite care, https://www.nhs.uk/conditions/social-care-and-support-guide/support-and-benefits-for-carers/carer-breaks-and-respite-care/.
[49] NHS England (2017), Developing a new approach to Palliative Care Funding: final report, https://www.england.nhs.uk/wp-content/uploads/2017/03/developing-new-approach-palliative-care-funding-testing.pdf.
[61] Nicholas, L. et al. (2014), “Advance Directives And Nursing Home Stays Associated With Less Aggressive End-Of-Life Care For Patients With Severe Dementia”, Health Affairs, Vol. 33/4, pp. 667-674, https://doi.org/10.1377/hlthaff.2013.1258.
[38] O’Brien, K., N. Yang and G. Jankauskaite (2020), “Women’s Experiences of Managing Work and End-of-Life Care: Challenges, Rewards and Recommendations for Vocational Psychologists”, Journal of Career Assessment, Vol. 29/1, pp. 3-17, https://doi.org/10.1177/1069072720933556.
[91] Observatory for Sociopolitical Developments in Europe (2016), Leave and financial support for family caregivers in EU member states.
[19] OECD (2018), Care Needed: Improving the Lives of People with Dementia, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/9789264085107-en.
[77] OECD (2016), Better Ways to Pay for Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/9789264258211-en.
[47] OECD (2015), Fiscal Sustainability of Health Systems: Bridging Health and Finance Perspectives, OECD Publishing, Paris, https://doi.org/10.1787/9789264233386-en.
[9] OECD (2020-2021), OECD policy and data questionnaires.
[28] Oliveira Hashiguchi, T. and A. Llena-Nozal (2020), “The effectiveness of social protection for long-term care in old age: Is social protection reducing the risk of poverty associated with care needs?”, OECD Health Working Papers, No. 117, OECD Publishing, Paris, https://doi.org/10.1787/2592f06e-en.
[12] Orlovic, M., J. Marti and E. Mossialos (2017), “Analysis Of End-Of-Life Care, Out-Of-Pocket Spending, And Place Of Death In 16 European Countries And Israel”, Health Affairs, Vol. 36/7, pp. 1201-1210, https://doi.org/10.1377/hlthaff.2017.0166.
[93] Pavalko, E. and K. Henderson (2006), “Combining Care Work and Paid Work”, Research on Aging, Vol. 28/3, pp. 359-374, https://doi.org/10.1177/0164027505285848.
[17] Pawłowska, I. et al. (2016), “Pharmacoeconomic considerations regarding hospice and palliative care according to pharmacists and hospice managers”, Eur J Hosp Pharm. 23(4):, pp. 239-240.
[68] Pham and Kram (2014), End-of-Life Care Interventions:An Economic Analysis, Health Quality Ontario.
[30] Pivodic, L. et al. (2014), “Burden on family carers and care-related financial strain at the end of life: a cross-national population-based study”, European Journal of Public Health, Vol. 24/5, pp. 819-826, https://doi.org/10.1093/eurpub/cku026.
[56] Public Health England (2017), Cost-effective commissioning of end of life care: Understanding the health economics of palliative and end of life care.
[50] Raphael, C., J. Ahrens and N. Fowler (2001), “Financing end-of-life care in the USA”, J R Soc Med., pp. 94(9):458-61.
[90] Rocard, E. and A. Llena-Nozal (2022), “Supporting informal carers of older people: Policies to leave no carer behind”, OECD Health Working Papers, No. 140, OECD Publishing, Paris, https://doi.org/10.1787/0f0c0d52-en.
[42] Rowland, C. and E. al. (2017), “The contributions of family care-givers at end of life: A national post-bereavement census survey of cancer carers’ hours of care and expenditures”, Palliative Medicine, Vol. 31/4, pp. 346–355, https://doi.org/10.1177/0269216317690479.
[18] Ryan, T. (2018), “What is the cost of palliative care in the UK? A systematic review”, BMJ Supportive & Palliative Care, pp. 250-257.
[73] Schildmann, J. et al. (2019), “Ethical case interventions for adult patients”, Cochrane Database of Systematic Reviews, Vol. 2019/7, https://doi.org/10.1002/14651858.cd012636.pub2.
[22] Senat (2021), Pour des Soins Palliatifs Accessibles à Tous : Former, Anticiper, Accompagner, https://www.senat.fr/rap/r20-866/r20-866-syn.pdf (accessed on 2022).
[5] Service Publique Fédéral Santé Publique (2020), Rapport d’évaluation de soins palliatifs.
[24] SHARE, the Survey of Health, Ageing and Retirement in Europe (2020), SHARE - Survey of Health, Ageing and Retirement in Europe waves 2-7.
[57] Smith, S. et al. (2013), “Evidence on the cost and cost-effectiveness of palliative care: A literature review”, Palliative Medicine, Vol. 28/2, pp. 130-150, https://doi.org/10.1177/0269216313493466.
[27] Tur-Sinai, A. et al. (2022), “Understanding out-of-pocket spending and financial hardship among patients who succumb to cancer and their caregivers”, Israel Journal of Health Policy Research, Vol. 11/1, https://doi.org/10.1186/s13584-021-00511-8.
[10] UK Hospice (2021), https://www.hospiceinfo.org/uk-hospice-facts-and-figures/.
[74] Vogl, M. et al. (2018), “Redefining diagnosis-related groups (DRGs) for palliative care – a cross-sectional study in two German centres”, BMC Palliative Care, Vol. 17/1, https://doi.org/10.1186/s12904-018-0307-3.
[21] Wachterman, M. and B. Sommers (2021), “.Dying Poor in the US—Disparities in End-of-Life Care.”, JAMA. 325(5), pp. 423–424.
[82] WHO/OECD (2021), Pricing long term care for older persons Case study: France, https://extranet.who.int/kobe_centre/sites/default/files/OECD_2021_France.pdf (accessed on 2022).
[46] Williams, A., L. Wang and P. Kitchen (2013), “Differential impacts of care‐giving across three caregiver groups in Canada”, Health & Social Care in the Community, Vol. 22/2, pp. 187-196, https://doi.org/10.1111/hsc.12075.
[3] Yi, D. et al. (2020), “Drivers of care costs and quality in the last 3 months of life among older people receiving palliative care: A multinational mortality follow-back survey across England, Ireland and the United States”, Palliative Medicine, Vol. 34/4, pp. 513-523, https://doi.org/10.1177/0269216319896745.
[44] Yu, M., D. Guerriere and P. Coyte (2015), “Societal costs of home and hospital end-of-life care for palliative care patients in Ontario, Canada”, Health and Social Care in the Community, 23(6), pp. 605–618.
Note
← 1. This report conceptualises end-of-life care as the care provided to people who are in the last 12 months of life. It refers to the terminal stage of palliative care, as well as including some elements of curative care and help with mobility limitations. Chapter 1 of this report provides a more detailed definition of EOLC.