In the LAC region, around one‑third of the deaths in the first year of life occur during the neonatal period (i.e. during the first four weeks of life or days 0‑27) and childhood diarrhoea and pneumonia are the leading infectious causes of childhood morbidity and mortality (PAHO, 2017[1]). Effective health systems can greatly limit the number of infant deaths, particularly by addressing life‑threatening issues during the neonatal and childhood period. Basic care for infants and children includes promoting and supporting early and exclusive breastfeeding (see indicator “Infant and young child feeding” in Chapter 4), identifying conditions requiring additional care and counselling on when to take an infant and young child to a health facility (Tomczyk et al., 2019[2]). Several cost-effective preventive and curative treatments exist, including zinc and vitamin A supplementations, vaccination, oral rehydration therapy (ORT) for diarrhoea, and appropriate antibiotic treatment for acute respiratory infection (ARI). Access to these services leads to better infant and child health.
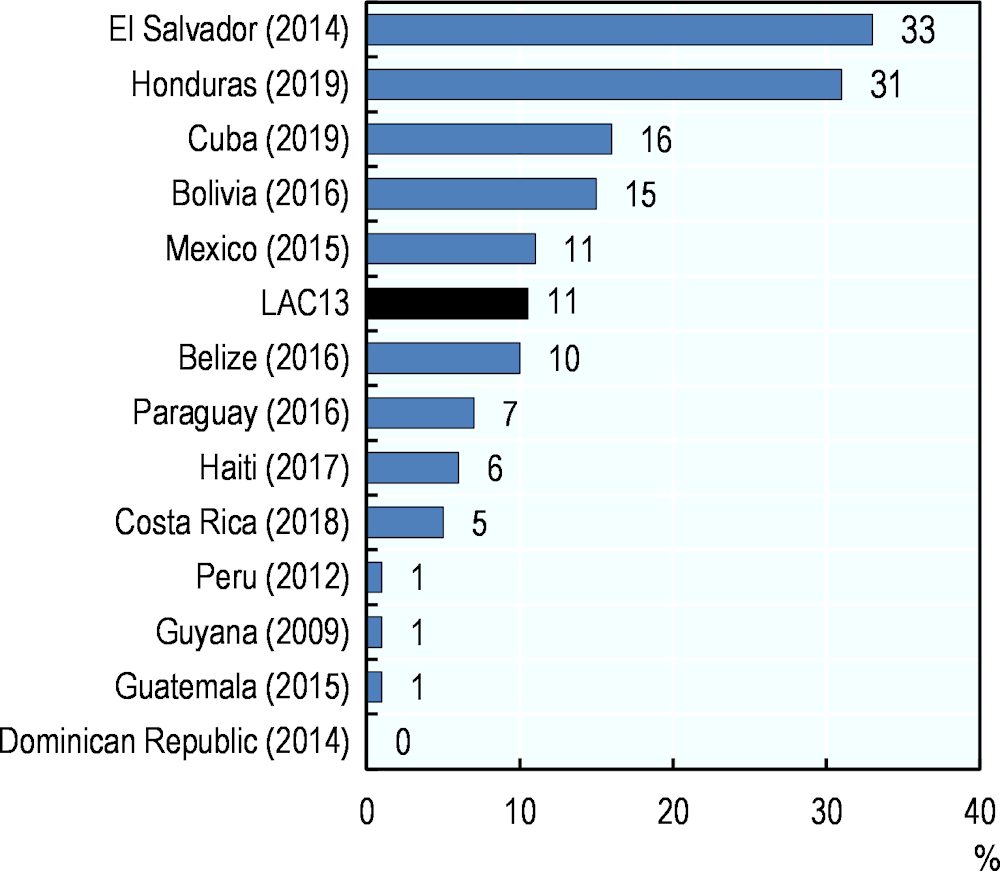
Appropriate treatment could also prevent deaths from diarrhoea and pneumonia. One of the effective treatments for childhood diarrhoea is zinc supplementation. According to data from 13 LAC countries, access to zinc supplementation for children aged under 5 years is markedly low in Peru, Guyana, Guatemala, and the Dominican Republic at 1% or less, while El Salvador and Honduras have coverage rates above 30%. The LAC13 average stands at 11% (Figure 5.14).
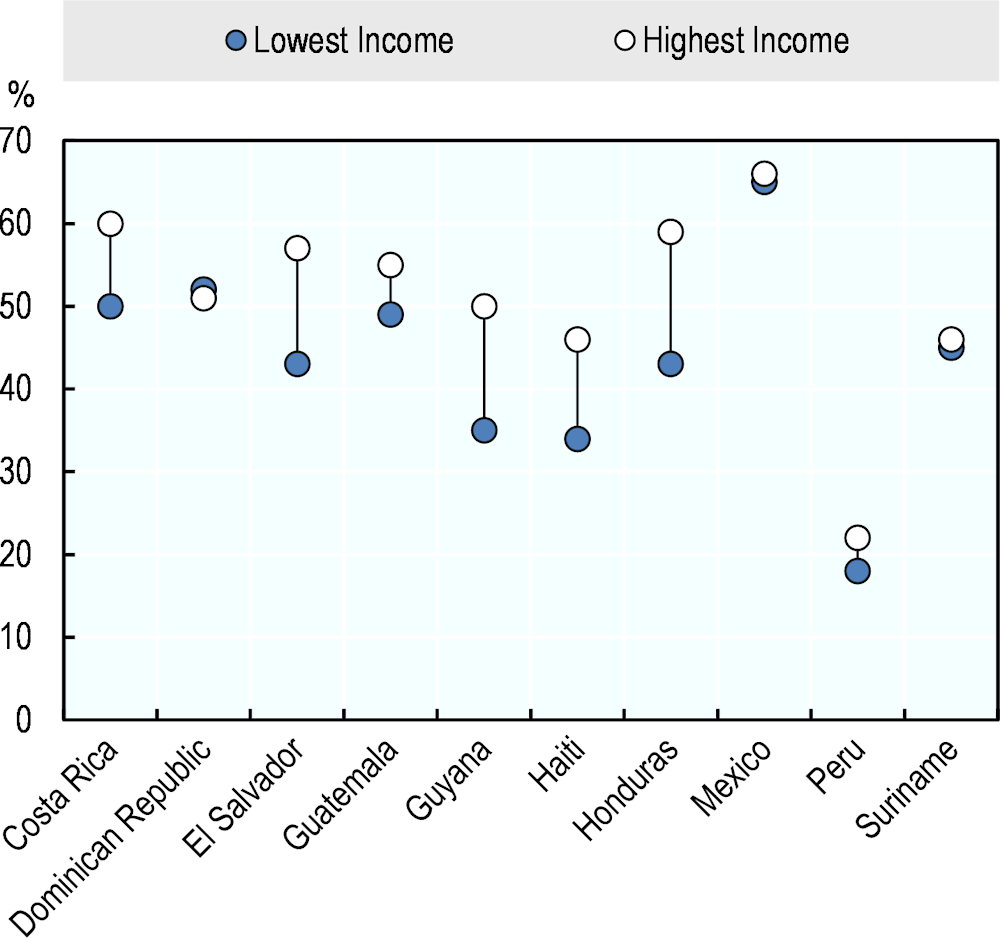
In addition, dehydration caused by severe diarrhoea can be easily treated with ORT. In average, less than half of children aged under 5 years with diarrhoea receive ORT in 22 LAC countries with data, with Argentina, Bolivia, Cuba, Guyana, Haiti, Paraguay, Peru and Venezuela having 40% or less. The coverage is the highest in Nicaragua, at 95%. Income inequalities are high in Honduras where 59% of children in the highest income quintile receive ORT when they need it, while only 43% of children in the lowest income quintile do (Figure 5.15). Notably, children in the lowest income group receive a higher coverage than in the highest income group in Bolivia and the Dominican Republic, which suggests that the health system can target the most vulnerable population.
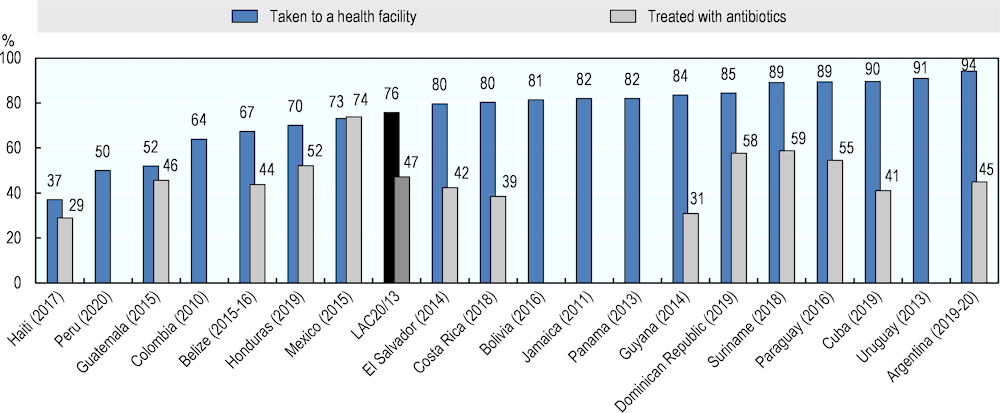
Access to appropriate medical care for children with ARI can also be improved in many countries in the region. Although on average more than three‑quarters of children with symptoms are taken to a health facility, less than half of them receive antibiotic treatment (Figure 5.16). It is important to stress the relevance of rational antibiotic use, both due to the health implications of antimicrobial resistance development and as a source of waste in health systems (OECD/The World Bank, 2020[3]).
There is a correlation between treatment coverage for diarrhoea and ARI. Antibiotic treatment for ARI is particularly low in Haiti and Guyana, where the treatment for diarrhoea is also low. This suggests an urgent need to further expand access to care to treat leading causes of child mortality in these countries.