Yasna Palmeiro
The World Bank, Santiago, Chile
Tomas Plaza Reneses
The World Bank, Washington, DC
Edit V. Velenyi
The World Bank
Cristian A. Herrera
The World Bank, Washington, DC

Yasna Palmeiro
The World Bank, Santiago, Chile
Tomas Plaza Reneses
The World Bank, Washington, DC
Edit V. Velenyi
The World Bank
Cristian A. Herrera
The World Bank, Washington, DC
The COVID‑19 pandemic has highlighted the importance of building the resilience and adaptability of health systems to cope with shocks and rapidly changing conditions. As countries slowly emerge out of this crisis, they are at an opportunity to strengthen their capacity to mitigate and adapt to a changing climate, which is expected to increasingly affect the health of the population in a number of ways. This chapter examines LAC countries current level of health systems resilience to climate change, identifying trends in the region and providing key considerations for policy actions that countries can implement to strengthen this resilience. The chapter is organised following the six building blocks of the World Health Organization Operational Framework for Building Climate Resilient Health Systems and uses them to explore LAC countries along several dimensions.
As introduced in Chapter 1, the COVID‑19 pandemic has shocked Latin America and the Caribbean (LAC) in terms of health, economic and social impacts (Jaramillo, 2022[1]; OECD, 2020[2]). As countries slowly transition out of this crisis, they also have the opportunity to improve their preparedness and response capacity of their health systems to deal with concurrent threats to population health, including those associated with a changing climate which are expected to increasingly affect the health of the population.
Climate change hazards (e.g. heatwaves, heavy precipitation events, sea level rise) along with social vulnerabilities (e.g. weak climate governance and intersectoral policies) threaten the development of populations in every country. In particular, LAC faces overlapping climatic, social, economic, and political challenges that may have serious consequences to health systems and population health (Yglesias-González et al., 2022[3]), as well as for other health-determining sectors, such as energy, transport, and agriculture, among others. The interacting effects of climate hazards, high social vulnerability, and lack of preparedness might result in disruption of daily activities, direct damage to critical infrastructure, economic burden, higher mortality and morbidity rates, and the exacerbation of social inequities.
Health systems in LAC are already under great pressure not only because of the COVID‑19 pandemic, but also because of low health expenditure, high out-of-pocket spending, low quality of care, limited access to health services, and health inequities between different demographic and socio-economic groups (OECD/The World Bank, 2020[4]). Therefore, to face the added challenges of climate change, health systems should be strengthened to continue protecting the population’s health and well-being.
In order to mitigate the potential damages of climate hazards and promote better health for all populations, multiple and complementary actions should be taken. The first key step is to analyse the state of health systems and their preparation and resilience to face climate change challenges.
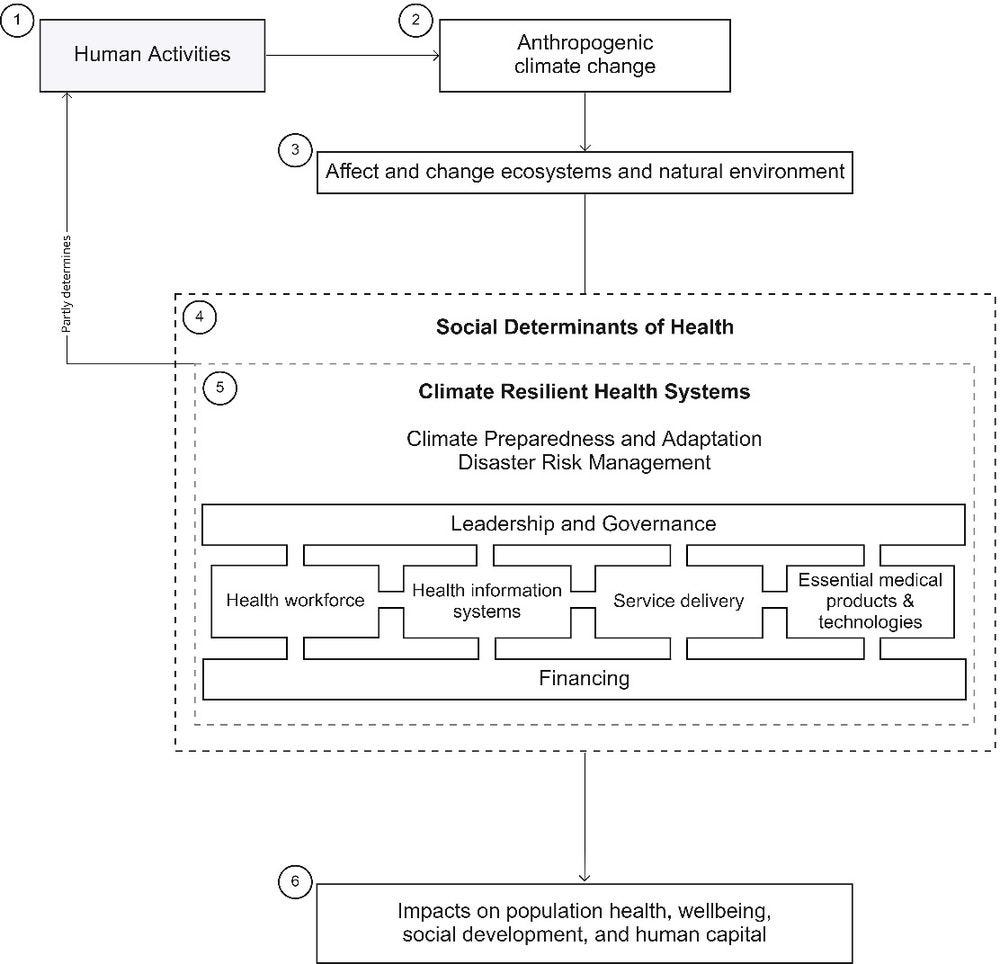
This chapter examines health systems resilience to climate change in LAC, identifying trends and providing key considerations for policy actions that countries can implement. The chapter also includes relevant best practices from OECD countries that are also in the process of strengthening their climate change resilience. To comprehensively analyse this information, this chapter is organised following the building blocks of the World Health Organization (WHO) Operational Framework for Building Climate Resilient Health Systems, composed of six building blocks, with leadership/governance and financing vital for an adequate health workforce, health information systems, essential medical products and technologies, and service delivery (WHO, 2015[5]).
The increase in atmospheric “heat-trapping” greenhouse gases (GHGs) has led to global warming and subsequent changes in the climate. Although LAC countries have not historically emitted a large amount of GHGs into the atmosphere (Friedlingstein et al., 2022[6]; Global Carbon Project, 2021[7]), the effects of a changing climate are global and affect every region and country in the world.
In LAC, the near-surface mean temperature has continue warming, being 0.78°C warmer in 2021 respect to 1961‑90 period (WMO, 2022[8]). Hot extremes have become more frequent and severe, and rainfall patterns have changed with an increase in drought events in some countries (Brazil, Bolivia, Chile and Paraguay) and heavy precipitation events in others (Uruguay and Argentina) (IPCC, 2021[9]; WMO, 2022[8]). Glaciers have shrunk dramatically since 1980s, losing between 30% and 50% of their mass in the Andes (WMO, 2022[8]), affecting water use for human consumption, agricultural purposes, and hydroelectric power. Finally, sea level rise poses high risks to low lying areas, especially small islands in the Caribbean and coastal cities (WMO, 2022[8]).
The LAC region has already experienced and continues to experience several climate related health crises. For example, prolonged dry spells and excessive rains have affected crops in the Dry Corridor of Central America, leaving farmers and their families prone to hunger and malnutrition. Warming temperatures, changing weather conditions and more extreme weather from torrential rains to drought can fuel outbreaks of dengue, which have affected countries such as Nicaragua, El Salvador, Brazil, Paraguay, Colombia and Belize. The Caribbean region is particularly exposed to hurricanes, storms and similar extreme weather events, which have caused extensive damage to health infrastructure and killed and injured significant numbers of people. For example, Hurricane Mitch caused 11 374 fatalities in Central America in 1998, and over 10 000 people have died as a direct result of tropical cyclones in the Caribbean in the last 20 years.
As these impacts are strongly mediated by social vulnerabilities and adaptive capacity, adequate and timely responses to rapid- and slow-onset climate hazards are key. Low governance and limited policies on disaster risk management and climate preparedness and adaptation, coupled with deep social inequities, high levels of poverty and informality (CEPAL, 2022[10]; OECD/The World Bank, 2020[4]), and impoverished health systems are important factors that might determine devastating impacts of climate change on population health.
Impacts on human systems would disrupt the daily lives of populations, affecting their health, well-being, social development, and human capital. Some examples of negative impacts include excess mortality and a higher incidence of cardiovascular and respiratory diseases, heat-related illnesses, vector-, water-, and food borne diseases, and mental health disorders (Romanello et al., 2022[11]). It has been estimated that between 20% (Argentina) and 75% (Colombia, Ecuador, Guatemala and Peru) of all heat-related mortality might be attributed to human-induced climate change (Vicedo-Cabrera et al., 2021[12]).
A health system is an interconnected set of organisations, institutions, infrastructure, resources, people, and activities, together with collaborations with other sectors and entities. Regardless of their specific structure, health systems aim to improve the health of populations (WHO, 2010[13]) while being responsive and efficient, and providing social and financial risk protection (WHO, 2007[14]).
As health systems are challenged by a changing climate, they need to be prepared and resilient to face rapid-onset hazards or shocks (e.g. heatwaves) and slow-onset hazards or stresses (e.g. droughts) to protect gains and continue making progress towards universal health coverage (UHC). In this regard, a climatic preparedness perspective should be integrated into health systems functioning to build climate resilient health systems, which should be “capable to anticipate, respond to, cope with, recover from and adapt to climate‑related shocks and stress, so as to bring sustained improvements in population health, despite an unstable climate” (WHO, 2015[5]).
As shown in Figure 2.1, climate resilient health systems, along with other social determinants of health, play an important role in modulating the impacts of climate change on population health, well-being, social development, and human capital. Policies and actions to strengthen climate resilient health systems are anchored in the WHO six core building blocks of climate resilient health systems.
Building climate resilience generally involves different actors and sectors at the national, regional, and local levels. In this sense, intersectoral policies should focus on reducing overall social vulnerabilities by reducing poverty and social inequities, and providing universal access to essential services (e.g. health, education, clean water, nutritious food, safe transport). At the same time, specific policies in the health sector should strengthen health governance and leadership, promote climate‑smart infrastructure, improve surveillance systems considering climate information, among other measures.
If governments take a whole‑system approach, the efforts and investment in climate resilient health systems are expected to have several benefits, not only to improve climate resilience, but also to strengthen health systems as a whole, improve overall population health, promote universal health coverage and primary healthcare for all.
This section presents the analysis of the status and trends of climate resilience of health systems in LAC under each of the six WHO climate resilient health systems.
Strong governance, political leadership, collaboration, and accountability are essential for managing climate‑related hazards that affect health systems and health-determining sectors. The objectives and actions are focused on strengthening governance within the ministry of health; integrating climate change into health policies and programmes, and supporting cross-sectoral collaboration to promote health and well-being (WHO, 2015[5]).
Based on the identification of social vulnerabilities and opportunities for climate adaptation, national strategies on climate change and health should be planned and implemented to strengthen health systems and protect the health of the population. The National Adaptation Plan (NAP) process was established under the Cancun Adaptation Framework (UNFCCC, 2011[15]) and facilitates the identification of adaptation needs to subsequently guide the development and implementation of strategies to address them.
Based on the United Nations Framework Convention on Climate Change (UNFCCC) NAP portal, NAPs from 12 LAC countries have been published (UNFCCC, 2022[16]) and, in most of the documents, the health sector has been identified as a vulnerable sector to climate change; however, the degree of details and the integration between existing health sectorial plans, also called HNAPs, and the overarching NAP vary across the countries (WHO, 2021[17]). Four countries have developed national health and climate plans (NHCP) or HNAPs, and 14 are still developing them (Office of Climate Change, Government of Guyana, 2019[18]; WHO, 2021[19]; WHO, 2021[20]). Complementing NAPs, NHCPs, and HNAPs, there are other initiatives in the region that acknowledge the action on climate change and health; for example, the Caribbean Action Plan on Health and Climate Change was approved by Caribbean countries and territories in 2019 with the aim of strengthening co‑operation, capacities, and resources to face the effects of climate change on health (PAHO, 2019[21]). Table 2.1 shows a summary of published NAPs, NHCPs, HNAPs, and other documents and initiatives by country.
|
Country |
NAP submitted to UNFCCC*† |
NHCP‡ or HNAP |
Other documents |
||
|---|---|---|---|---|---|
|
Developed |
Under Development |
No / No participant |
|||
|
Antigua and Barbuda |
✓ |
||||
|
Argentina |
✓ |
✓a |
|||
|
Bahamas |
✓ |
||||
|
Barbados |
✓ |
||||
|
Belize |
✓ |
||||
|
Bolivia |
✓ |
✓b |
|||
|
Brazil |
✓ (2016) |
✓ |
|||
|
Chile |
✓ (2017) |
✓ |
|||
|
Colombia |
✓ (2018) |
✓ |
|||
|
Costa Rica |
✓ (2022) |
✓ |
|||
|
Cuba |
✓ |
||||
|
Dominica |
✓ |
||||
|
Dominican Republic |
✓ |
||||
|
Ecuador |
✓ |
||||
|
El Salvador |
✓ |
||||
|
Grenada |
✓ (2019) |
✓ |
|||
|
Guatemala |
✓ (2019) |
✓ |
|||
|
Guyana |
✓ |
✓ |
|||
|
Haiti |
✓ |
||||
|
Honduras |
✓ |
||||
|
Jamaica |
✓ |
||||
|
Mexico |
✓ |
||||
|
Nicaragua |
✓ |
||||
|
Panama |
✓ |
||||
|
Paraguay |
✓ (2022) |
✓ |
|||
|
Peru |
✓ (2021) |
✓ |
|||
|
Saint Kitts and Nevis |
✓ |
||||
|
Saint Lucia |
✓ (2018) |
✓ |
|||
|
Saint Vincent and the Grenadines |
✓ (2019) |
✓ |
|||
|
Suriname |
✓ (2020) |
✓ |
|||
|
Trinidad and Tobago |
✓ |
||||
|
Uruguay |
✓ (2019) |
✓ |
|||
|
Venezuela |
✓ |
||||
* Submitted up to August 2022 (UNFCCC, 2022[22]); † In brackets is the year of posting; ‡ from 2021 WHO HCCGS (WHO, 2021[19]); a Action plan on health and climate change that includes several adaptation measures (Ministerio de Salud y Desarrollo Social, Argentina, 2019[23]) and in it has announced the creation of a specific programme for climate change and health (Chesini and Orman, 2021[24]); b National adaptation mechanism that includes adaptation measures for the health sector (Ministerio de Planificación del Desarrollo, 2007[25]).
Overall, LAC countries have been working to develop climatic plans and strategies; however, it appears that the pace of climate change is faster than their development and implementation. Although countries recognise that the health sector is highly vulnerable to climate change, there is less evidence on concrete and context-specific policies and plans that integrate adaptation actions to strengthen health systems.
A key area priority for the future is the monitoring and evaluation of past and/or current NAPs, strategies, or action plans. Over the coming years, several NAPs and HNAPS will need to be updated, representing an opportunity to evaluate what was done, what was partially done, and what needs to be improved to build climate‑resilient health systems.
Under the UNFCCC, the appointment of national focal points aims to enhance countries’ engagement and participation in UNFCCC relevant activities (UNFCCC, 2016[26]). By 2022, all LAC countries have designated at least one UNFCCC focal point, similar to OECD countries which have between one and five focal points (Table 2.2) (UNFCCC, 2022[22]). Most of the official national focal points are from the Ministry of Environment or Ministry of Foreign Affairs, but none are from the Ministry of Health. At the national level, most of the LAC countries have designated a climate change and health focal point within the Ministry of Health (WHO, 2021[19]), which can play an important role in cross-collaboration and intersectoral policies.
|
Countries |
Number of focal points |
||||
|---|---|---|---|---|---|
|
1 |
2 |
3 |
4 |
More than 4 (n) |
|
|
Antigua and Barbuda |
✓ |
||||
|
Argentina |
✓ |
||||
|
Bahamas |
✓ |
||||
|
Barbados |
✓ |
||||
|
Belize |
✓ |
||||
|
Bolivia |
✓ (8) |
||||
|
Brazil |
✓ |
||||
|
Chile |
✓ |
||||
|
Colombia |
✓ |
||||
|
Costa Rica |
✓ |
||||
|
Cuba |
✓ |
||||
|
Dominica |
✓ |
||||
|
Dominican Republic |
✓ |
||||
|
Ecuador |
✓ |
||||
|
El Salvador |
✓ |
||||
|
Grenada |
✓ |
||||
|
Guatemala |
✓ |
||||
|
Guyana |
✓ |
||||
|
Haiti |
✓ |
||||
|
Honduras |
✓ |
||||
|
Jamaica |
✓ |
||||
|
LAC average |
✓ |
||||
|
Mexico |
✓ |
||||
|
Nicaragua |
✓ |
||||
|
OECD average |
✓ |
||||
|
Panama |
✓ (10) |
||||
|
Paraguay |
✓ |
||||
|
Peru |
✓ |
||||
|
Saint Kitts and Nevis |
✓ |
||||
|
Saint Lucia |
✓ |
||||
|
Saint Vincent and the Grenadines |
✓ |
||||
|
Suriname |
✓ |
||||
|
Trinidad and Tobago |
✓ |
||||
|
Uruguay |
✓ |
||||
|
Venezuela |
✓ |
||||
Source: UNFCCC (2022[22]), National focal points, https://unfccc.int/process/parties-non-party-stakeholders/parties/national-focal-point.
A co‑ordinated and strong relationship between the health sector and health-determining sectors (e.g. agriculture, energy, and transport) is vital because several measures and actions that affect population health and well-being rely outside the health sector. The health sector should be a leading voice in ensuring that policies within health-determining sectors protect population health and well-being, as well as promote climate‑resilient health systems. Joint Memorandums of Understanding (JMU) promote intersectoral collaboration and help articulate intersectoral policies that build climate resilient health systems.
Overall, the health sector in LAC have limited JMU with other sectors (Table 2.3). Cuba and Nicaragua have recognised having JMU with almost all the sectors under analysis, except for social services (WHO, 2021[19]).
|
Sectors |
Yes |
No |
Unknown / Not applicable |
|---|---|---|---|
|
Agriculture |
2: Cuba, Nicaragua |
18 |
4 |
|
Education |
2: Cuba, Nicaragua |
18 |
4 |
|
Energy |
2: Cuba, Nicaragua |
18 |
4 |
|
Environment |
5: Bahamas, Brazil, Cuba, Grenada, Nicaragua |
15 |
4 |
|
Meteorological |
3: Brazil, Cuba, Nicaragua |
18 |
3 |
|
Social Services |
0 |
19 |
5 |
|
Transportation |
1: Cuba |
18 |
5 |
|
Urban Development and Housing |
1: Cuba |
18 |
5 |
|
Water, Sanitation, and Hygiene |
2: Cuba, Jamaica, Nicaragua |
18 |
4 |
Source: WHO (2021[19]), 2021 WHO health and climate change global survey report, https://apps.who.int/iris/handle/10665/348068.
When analysing the experiences of OECD countries, the situation is similar to that of LAC. However, Germany, the Netherlands, Israel, Portugal and Sweden stand out in having JMU with several health-determining sectors, especially national meteorological and hydrological services (WHO, 2021[19]). This intersectoral collaboration has allowed them to build capacity, establish climate‑informed programmes, and enhance surveillance and climate‑informed health early warning systems, among other measures (WHO, 2008[27]).
Overall, LAC countries have been working to improve leadership and governance at the intersection of climate and health; however, there are still many opportunities for improvement, especially regarding intersectoral collaboration to strengthen climate‑resilient health systems. Strengthening this building block is fundamental because it is the basis to strengthen all other building blocks.
A skilled health workforce is essential to promote health, achieve better health outcomes, and build climate‑resilient health systems. Health personnel are in direct contact with vulnerable populations during normal times and during emergencies, planning, organising, and implementing public health activities; developing public health policies; collaborating with other sectors, among other activities. They are a cornerstone of health systems. Therefore, in a changing climate, the health workforce needs to understand the challenges posed by climate change and be able to prepare for and act in the face of climate‑related events that affect the functioning of health systems. By training health personnel, developing adequate organisational capacities, and improving communication and awareness of climate change challenges, countries build climate‑resilient health systems.
Having an adequate density of health workers underpins the provision of adequate health services, and consequently leads to better population health, which is even more important during health emergencies. On average, there are 2 medical doctors and 3.4 nursing and midwifery personnel per 1 000 population in LAC countries, which is well below the average in OECD countries (3.5 medical doctors and 9.7 nursing and midwifery personnel per 1 000 population). Chapter 8 of this publication contains detailed information on health worker density in the LAC region (WHO, 2022[28]).
When a shock hits, the entire provision of health services is significantly affected and there a surge of demand, which requires sufficient health personnel to be available. Unfortunately, LAC countries are inadequately prepared when it comes to medical countermeasures and personnel deployment during emergencies. Based on the 2021 Global Health Security Index (GHSI), LAC countries scored very low, with an average score of 9.09 out of 100, which is well below the average score of 30.26 (out of 100) in the OECD countries (Bell and Nuzzo, 2021[29])
Training and inclusion of modules on climate change and health in LAC countries is limited. An analysis of 161 universities in 20 LAC countries showed that only one university in Brazil deliberately included and published one optative module on “climate change and health” in undergraduate medicine and nursing curricula (Palmeiro-Silva et al., 2021[30]). It is possible that the topic itself might have been included as individual lessons in other modules, such as public health and epidemiology; however, this information is not publicly available. Another international survey that considered members of the Global Consortium on Climate and Health Education showed that 63% of the respondents (n=84) offer climate‑health education; however, only six members were from LAC at that time (Palmeiro-Silva et al., 2021[30]; Shea, Knowlton and Shaman, 2020[31]).
Over the last few years, several educational opportunities organised by academic institutions and non-governmental organisations from LAC and supported by the Pan American Health Organisation (PAHO) have been launched. For example, the Global Consortium on Climate and Health Education from Columbia University along with the Inter-American Institute (IAI) and the PAHO organised a free 5‑weeks course called “Climate and Health Responder Course for Latin America” and focused on academic and research health communities in the region (Columbia University, 2022[32]). The 10‑week “Caribbean Climate and Health Responders Course” was organised by the Global Consortium on Climate and Health Education, Earth Medic/Earth Nurse, and the Caribbean Institute of Meteorology and Hydrology, with focus on healthcare professionals, climate leaders and students (Columbia University, 2022[33]). Finally, the University of the West Indies with support from PAHO, Caribbean Community (CARICOM), and the European Union (EU) have launched a “The Climate Change and Health Leaders” fellowship training programme focused on intersectoral and multidisciplinary leaders from the Caribbean (The University of West Indies, 2022[34]).
More broadly in LAC, the PAHO and other academic institutions have organised different open online courses on climate change and health, aimed at increasing awareness among professionals in the region (PAHO-VCPH, 2022[35]). The IAI has organised a massive open online course called “Cambio Climático y Global en América Latina” (“Climate and global change in Latin America”) which introduces audiences to climatic sciences, mitigation, adaptation, and sustainability in LAC (IAI, 2020[36]). Another open course called “Communicating Climate Change Effectively” was launched in 2020 by CDKN, which was focused on professionals from different disciplines (CDKN, 2022[37]). Two open courses on planetary health which include the topic on climate change and health have also been prepared. One was organised by a partnership between the Institute of Advanced Studies of the University of São Paulo, TelessaúdeRS, Sociedade Brasileira de Medicina de Família e Comunidade and the Planetary Health Alliance (TelessaudeRS, 2020[38]). The second course was organised by the Chilean Society of Planetary Health (Sochisap, 2022[39]).
At the international level, the One United Nations (UN) Climate Change Learning Partnership has made several open courses on climate change, including its intersection with health. These are generally short courses, some of which are available in Spanish, Portuguese, and French (UNCCELEARN, 2022[40]). The World Bank has also organised an open course called “From Climate Science to Action” and includes regional information on sectoral impacts, and mitigation and adaptation measures (World Bank, 2022[41]).
The number of individuals that have benefitted from these initiatives is unknown and formal training has rarely been integrated into undergraduate or postgraduate health curricula, which highlights the need for additional investments and attention to this topic.
Communication of essential information during public health emergencies is vital to maximising efforts, facilitating and supporting decision making, and limiting the potential damage of the hazard (WHO, 2018[42]). Expedite, accurate, and clear communication with health personnel is therefore vital to protect population health and health systems during an emergency.
According to the 2021 GHSI on communications with healthcare workers during a public health emergency, LAC countries have an average score of 10.6 out of 100, while OECD countries scored an average of 31.6 out of 100. The best prepared LAC countries are Argentina, Peru, Chile, Mexico, and Saint Vincent and the Grenadines, while Australia, Belgium, Denmark, Finland, and the United States are the best prepared within OECD countries. This low score in LAC countries increases the risk of inadequate functioning and co‑ordination of actors during an emergency, both vertically (e.g. from ministries of health to local health centres) and horizontally (e.g. health staff in a health centre). The resulting effects would range from a loss of trust, delayed critical decisions, inadequate resource allocation, misunderstandings and conflicts, and increased morbidity and mortality.
LAC countries need to improve their risk communication with health personnel and citizens to battle disinformation, gain public trust (OECD, 2020[43]), and strengthen their health systems. Risk communication that is accurate, clear, assertive, quick, and puts people at the centre is part of enhancing disaster risk management and resilience building, helping to engage actors in collective response. The experience of the COVID‑19 pandemic showed that several countries had to implement practical strategies to improve public communication. For example, Chile and Korea had daily briefings to timely and consistently communicate essential information; in Belgium, Chile, Portugal and the United States public briefings were delivered by scientists and/or public health experts to support data and interventions on evidence (OECD, 2020[43]); and Canada, Chile and the United Kingdom built specific websites where daily statistics were presented to simplify data understanding (Bangdiwala et al., 2021[44]).
Health information systems (HISs) are a central element of health systems because they “enable decision-makers to identify problems and needs, make evidence‑based decisions on health policy, and allocate scarce resources optimally” (WHO, 2008[45]). To face the challenges and impacts of a changing climate and protect population health, decision-makers and health personnel should understand critical information related to climate hazards, the location of vulnerable populations, and the range of resources to implement adaptation measures.
HISs are intrinsically linked to all health system building blocks, particularly new health technologies (Section 3.4) and service delivery (Section 3.5). For example, innovative platforms for service delivery would require robust health governance and integral health policies that allow for systems interoperability and security. At the same time, health personnel should be properly trained to maximise the benefits of new technologies and optimise healthcare delivery according to patients’ characteristics and needs. The integration of a climate and health perspective to HISs would strengthen patient-centred healthcare delivery and reduce climate risks (e.g. minimising disruption to services during emergencies) (Rozenberg et al., 2021[46]).
One of the first steps in building climate‑resilient health systems is to understand: i) which populations are most vulnerable to different climate‑related health hazards, ii) the responsiveness of the health system to manage potential impacts on populations, iii) main vulnerabilities of the health system before and during an extreme event, and iv) the resources available for effective adaptation. Vulnerability and adaptation (V&A) assessments are vital for collecting and analysing data, conducting continuous situational analyses, and informing adequate action plans. The information from V&A assessments aims to inform and develop national adaptation plans, including sectorial ones.
Based on the 2021 WHO Health and Climate Change Global Survey (HCCGS) (WHO, 2021[19]), only seven LAC countries (out of 25 participating in the survey) have conducted climate change and health V&A assessments. Other national analyses on vulnerability to climate change have been performed by several countries, although sometimes they do not meet all the requirements to be considered formal assessments. Table 2.4 shows a summary of LAC countries that have declared or published their V&A documents.
|
Country |
V♦●■erabi●ity a■d Adaptio■ Assessme■t‡ |
Other assessments |
||
|---|---|---|---|---|
|
Performed† |
Under Development |
No / No participant |
||
|
Antigua and Barbuda |
✓ |
✓a |
||
|
Argentina |
✓ |
✓a |
||
|
Bahamas |
||||
|
Barbados |
✓ |
|||
|
Belize |
✓ |
✓b |
||
|
Bolivia |
✓ |
✓a ✓c |
||
|
Brazil |
✓(2020) |
|||
|
Chile |
✓ |
|||
|
Colombia |
✓ |
✓a ✓b |
||
|
Costa Rica |
✓ |
✓a ✓b |
||
|
Cuba |
✓ (2020) |
|||
|
Dominica |
✓ (2017) |
✓a |
||
|
Dominican Republic |
✓ |
✓b |
||
|
Ecuador |
✓ |
✓a |
||
|
El Salvador |
✓ |
✓a ✓b |
||
|
Grenada |
✓ (2016) |
|||
|
Guatemala |
✓ (2020) |
✓a ✓b |
||
|
Guyana |
✓ |
|||
|
Haiti |
✓ |
✓a |
||
|
Honduras |
✓ |
✓a ✓b |
||
|
Jamaica |
✓ |
|||
|
Mexico |
✓ |
✓b |
||
|
Nicaragua |
✓ |
✓a ✓b |
||
|
Panama |
✓ |
✓a ✓b |
||
|
Paraguay |
✓ |
✓a |
||
|
Peru |
✓ |
✓a |
||
|
Saint Kitts and Nevis |
✓ |
|||
|
Saint Lucia |
✓ (no date) |
|||
|
Saint Vincent and the Grenadines |
✓ |
|||
|
Suriname |
✓ |
|||
|
Trinidad and Tobago |
✓ (2019) |
|||
|
Uruguay |
✓ |
|||
|
Venezuela |
✓ |
|||
‡ from 2021 WHO HCCGS (WHO, 2021[19]); † i■ brackets: comp●etio■ of ●atest assessme■t; a V&A performed through The Regional Getaway for Technology Transfer and Climate Change Action for Latin America and the Caribbean (REGATTA) (UNEP-REGATTA, 2022[47]); b V&A performed through The Inter-American Development Bank (IADB, 2010[48]); c The document “Avances en el conocimiento: Cambio climático y el desafío de la salud en Bolivia” (“Advances in knowledge: Climate change and the health challenge in Bolivia”) includes some areas of V&A (Providas, 2013[49]).
Small Island Developing States (SIDS) in the Caribbean, with support from the PAHO, have been working on strengthening their capacities, including the implementation of V&A assessments. They established the Caribbean Community Climate Change Centre in 2004, the Caribbean Public Health Agency in 2013, and the Caribbean Health Climatic Bulletin, among other initiatives, and are also part of the Special Initiative on Climate Change and Health in Small Island Developing States, which aims to ensure that by 2030 all SIDS health systems are resilient to climate variability and change (PAHO, 2019[21]). Combined efforts have led to Antigua and Barbuda, Bahamas, Barbados, Belize, Dominica, Grenada, Guyana, Haiti, Jamaica, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, and Trinidad and Tobago being awarded the 5‑year EU/CARIFORUM Climate Change and Health Project, which enabled them to prepare climate change and health V&A assessments and the subsequent adaptation plans (PAHO, 2021[50]). Finally, Saint Lucia has shown great leadership by co-founding the initiative “Adaptation Action Coalition Health” which aims to adapt and build resilience to the impacts of climate change (WHO, 2021[51]). Nonetheless, more formal processes for V&A assessments are needed to inform subsequent measures and policies.
Other countries in the region, including Chile (Ministerio del Medio Ambiente, 2017[52]), Costa Rica (Ministerio de Ambiente y Energía, 2022[53]), Peru (Ministerio del Ambiente, 2022[54]), Dominican Republic (Presidencia de la República Dominicana, 2016[55]), Uruguay (MVOTMA, 2010[56]), and Venezuela (MINEA, 2017[57]) have named several vulnerability factors in their NAPs, nationally determined contributions (NDCs), or national communications, but they are not linked to previous V&A assessments or systematically analysed.
Overall, most LAC countries are carrying out or have performed formal or preliminary V&A assessments; however, some of them need to be updated in accordance with new challenges and further integrate health as the main area of examination. The completion of assessments that include context-specific and systematic evaluations of vulnerable populations and vulnerabilities of the health system helps decision-makers focus actions and resources on climate adaptation and resilience.
The UNFCCC has compiled a training package on methods and tools for V&A assessments in English and Spanish that can be used by countries to develop their own assessments, including a chapter on human health (UNFCCC, 2007[58]). Also, Canada, the Czech Republic, Estonia, Germany, Lithuania, the Netherlands, Sweden, and the United States have performed specific climate change and health V&A assessments that can be used as methodological models. Particularly, the Government of Canada has specifically developed a workbook on climate change and health V&A assessment where different steps are described on how to analyse main vulnerabilities and identify measures to increase climate resilience of health systems; it is available in English and French (Health Canada, 2022[59]).
Argentina has also developed a document called “Manual: Vulnerabilidad y Adaptación al Cambio Climático para la Gestión y Planificación Local” (“Guidelines: Vulnerability and Adaptation to Climate Change for Local Management and Planning”), which guides the evaluation of main risks and vulnerabilities associated with climate change (Dirección de Cambio Climático de la Secretaría de Ambiente y Desarrollo Sustentable de la Nación Argentina, 2011[60]).
The World Bank has been supporting countries across the globe with the implementation of Climate and Health Vulnerability Assessments (CHVAs), Climate and Health Economic Valuations (CHEVs) and other related analytics. In LAC, the Haiti CHVA was completed in 2022.
Although climate change hazards may be similar globally, the impacts are different because of the differential exposure and vulnerability factors within the populations. In general, vulnerability assessment includes three components: the analysis of the exposure of the population to hazards, the degree of susceptibility (or to what extent people are affected), and the capacity to adapt or respond to hazards. Vulnerable populations are at a higher risk of suffering the negative effects of climate hazards, not only because of their effects on livelihoods and daily life, but also because of the cascading impacts on income, poverty, and poor health. In this regard, the identification of vulnerable populations is key to reducing the damage caused by climate hazards by intervening in any of the three vulnerability components.
People who live in areas with weak climatic policies, limited access to basic services, marginalised and poor communities, indigenous people, women, people above 65 and below 1 year of age, and outdoor workers are generally considered vulnerable populations (IPCC, 2022[61]). A particular concern in LAC countries is the combination of poor urban planning and rapid urbanisation rates of cities (Ezquiaga Arquitectura, Sociedad y Territorio S.L., 2015[62]), which increases the risk of adverse health effects from climate change hazards.
At the national level, the WHO and World Meteorological Organisation (WMO) have published an atlas of health and climate that identifies countries or areas with a high risk of negative climate‑sensitive health outcomes, including malaria, dengue, and respiratory illnesses. In this document, most LAC countries are recognised as vulnerable to climatic and environmental changes, especially due to social vulnerabilities (WHO and WMO, 2012[63]). Complementary to this, the Lancet Countdown has estimated an increase in the exposure of vulnerable populations to heatwaves globally, and LAC countries have not been the exception. The number of heatwave exposure events in people over 65 years of age has increased across all LAC countries, especially in Colombia, Venezuela, Brazil, Bolivia, Paraguay, Suriname and Guyana (Romanello et al., 2021[64]; 2022[11]). Additionally, almost all countries in LAC have a significant number of people exposed to sea level rise (SLR), with Brazil and Ecuador having the highest absolute number of people exposed (Romanello et al., 2021[64]). It has been estimated that more than 27% of the LAC population live in coastal areas and 8% of them are at high or very high risk of being affected by coastal hazards, including SLR (WMO, 2022[8]); however, proportionally and geographically, SIDS in the Caribbean are at a particularly high risk of SLR (Giardino et al., 2020[65]; IPCC, 2022[66]).
Because of the intertwined elements between climate‑sensitive health outcomes and social vulnerability, countries have the opportunity to multiply the positive health effects of climate preparedness, build climate resilience, and reduce poverty and social inequities. In this sense, the health sector in collaboration with other health-determining sectors, such as housing and social services, might map and identify vulnerable populations allowing better prioritisation and focalisation of resources and efforts. It is also important to identify vulnerabilities within health systems, including weak communication processes or critical infrastructure that may be damaged due to climate hazards.
Mexico has published an online interactive atlas called “Atlas Nacional de Vulnerabilidad ante el Cambio Climático” (“National Atlas of Vulnerability to Climate Change” in English), where the degree of vulnerability to mudslides, dengue, floods, and tropical cyclones has been analysed and identified at the municipal level to inform local development strategies. The sensitivity index includes indigenous people, food poverty, individual characteristics (e.g. weight), and other agricultural factors (Gobierno de México/INECC, 2022[67]).
Similarly, Chile has also developed and published an online atlas of climatic risks called “Atlas de Riesgos Climaticos” (“Atlas of Climatic Risks”) that explores different sectors, including agriculture, health and well-being, forests, tourism, and energy at the municipal level. In particular for health and well-being, it identifies the risks of floods, premature mortality due to temperature changes and heat, effects of heatwaves and coldwaves on human health, and water security by analysing the hazard, degree of exposure, and sensitivity of the population. This atlas supports national and regional governments in prioritising actions and focalising resources (Ministerio del Medio Ambiente, 2020[68]).
Panama has performed an spatial analysis of vulnerability to climate change, including an index on access to health centres at the corregimientos level (Calderón, Francisco and López, 2021[69]).
Ecuador also has analysed exposure and vulnerability maps and identified risks at the canton level. Although this is a very useful document, it should be updated according to new emerging vulnerabilities (D’Ercole and Trujillo, 2003[70]). Argentina has proposed the development of a national health and climate observatory to support adaptation policies related to population health; however, it is still unpublished (Ministerio de Salud, 2018[71]).
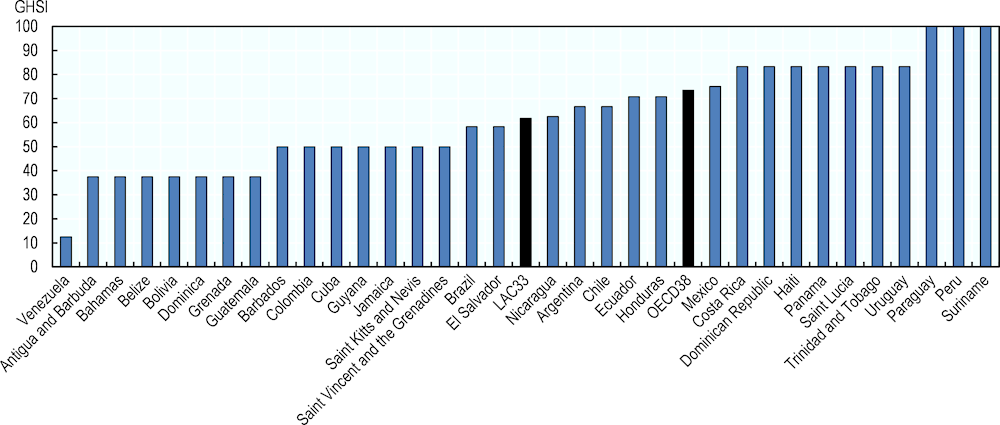
From a general perspective, surveillance systems in LAC have improved over time, but show important differences across countries. According to the WHO International Health Regulations (IHR) capacity score for surveillance, the average score for LAC countries in 2020 was 79.6 out of 100, with a minimum score of 40 (Belize and Trinidad and Tobago) and a maximum of 100 (Brazil, El Salvador, Guyana, Mexico and Paraguay). This average score was close to but below the average score of OECD countries, which reached 87.6 out of 100 (Figure 2.2) (WHO, 2022[72]).
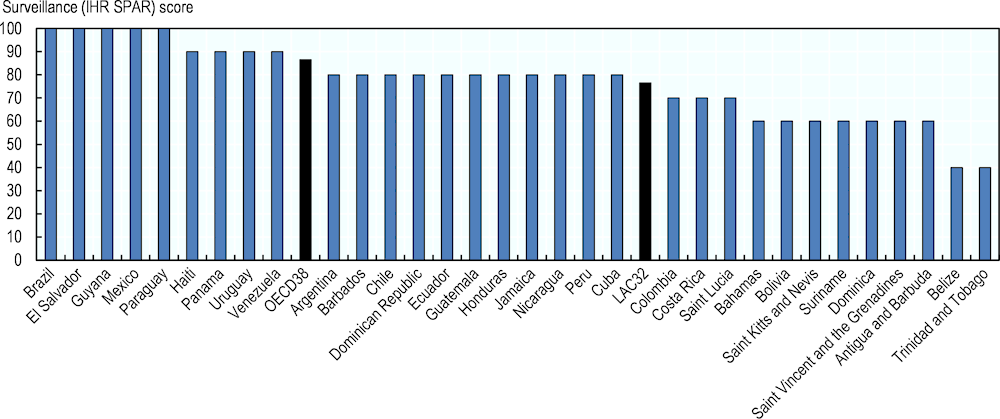
Source: WHO (2022[72]), Surveillance (IHR SPAR), https://www.who.int/data/gho/data/indicators/indicator-details/GHO/surveillance-ihr-spar.
More detailed information on the existence of surveillance systems for climate‑related diseases was collected by the 2021 WHO HCCGS. It shows that most participating LAC countries (n=25) have surveillance systems for non-communicable diseases (92%), vector-borne diseases (92%), malnutrition and foodborne diseases (83.3%), water-borne diseases (83.3%), zoonoses (83.3%), and airborne and respiratory illnesses (71%); however, fewer countries have surveillance systems for mental and psychosocial health (65.2%), injury and mortality from extreme weather events (33.3%), and heat-related illness (8.3%) (WHO, 2021[19]).
In terms of laboratory services, the average IHR score for LAC countries is 77.8 out of 100, with Brazil, Cuba, El Salvador, and Guyana being the top countries. However, most of the LAC countries are well below the OECD countries average of 90.3 out of 100 (Figure 2.3) (WHO, 2022[72]). Of particular interest is the laboratory capacity to perform analyses related to vector-borne diseases, especially dengue and malaria which are two diseases of special public health concern in LAC due to their endemic behaviour and their projections under climate change scenarios. Figure 2.4, left-hand chart, shows that 30 countries reported cases of dengue but only 15 confirmed the serotype (DENV‑1, DENV‑2, DENV‑3 and DENV‑4) in 2021 (PAHO, 2022[73]). The analysis and confirmation of the serotype is relevant for public health purposes because of the associated clinical outcomes within the population and subsequent measures (Aguas et al., 2019[74]). Complementary, malaria is a life‑threatening parasitic disease which should be diagnosed and treated quickly after suspicion to prevent high mortality rate. An important aspect to analyse in Figure 2.4, right-hand chart, is the significant gap between the suspected and the confirmed incidence rates in 2020, which could indicate the limited laboratory capacity to perform rapid diagnostic tests or microscopy analyses in some countries (WHO, 2022[75]; WHO, 2022[76]).
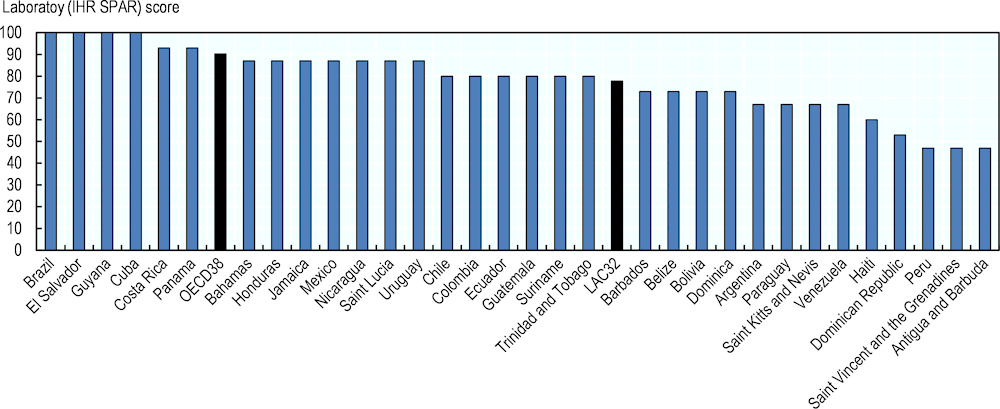
Source: WHO (2022[72]), Surveillance (IHR SPAR), https://www.who.int/data/gho/data/indicators/indicator-details/GHO/surveillance-ihr-spar.
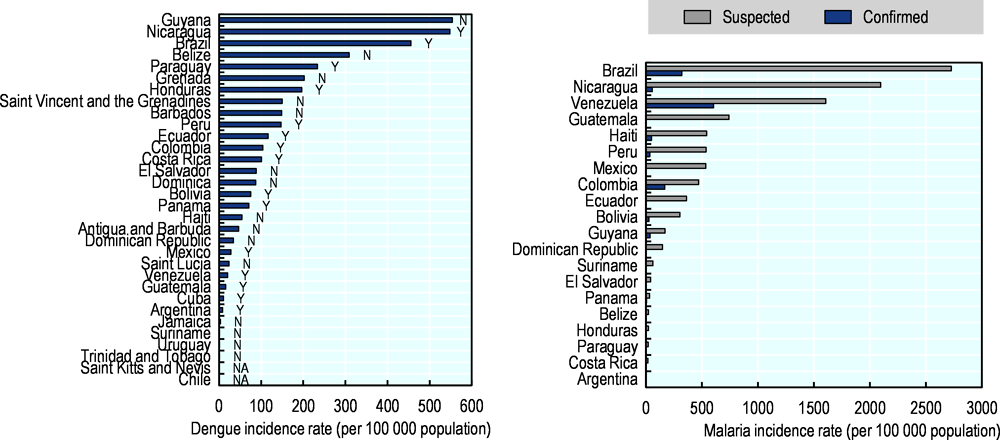
Left-hand chart shows dengue incidence rate per 100 000 population and serotype confirmation (Y: Yes, N: No, NA: Not applicable). Right-hand chart shows malaria incidence rate per 100 000 population: Totals for suspected (grey) and confirmed by rapid diagnostic test or microscopy (blue).
Source: PLISA Health Information Platform for the Americas (PAHO/WHO, 2023[77]) and WHO Global Health Observatory (WHO, 2022[75]; 2022[76]; 2022[78]).
Early warning systems applied to health surveillance and preparedness are also a key tool when anticipating to climate‑hazards and prevent damages (Box 2.2). In this regard, climate‑informed health early warning systems (C-HEWS) in place are less common in LAC countries. Only six participating countries in 2021 WHO HCCGS have informed a current C-HEWS for vector-borne diseases (26.1%) and five for airborne and respiratory illnesses (21.7%). Very few countries have informed C-HEWS for heat-related illness (17.4%), injury and mortality from extreme weather events (13%), non-communicable diseases (8.7%), infectious diseases (8.7%), malnutrition and foodborne diseases (8.7%), water-borne diseases (8.7%), zoonoses (5%), and mental and psychosocial health (4.3%) (WHO, 2021[19]).
Important advances in C-HEWS have been done in several countries, although there is still great variability across them. For example, the EuroHEAT is an online tool that displays daily forecasts of heatwave probability (0‑100%), informing about the upcoming ten days (EuroHEAT, 2022[79]). Similarly, the United Kingdom, through the UK Health Security Agency (UKHSA) and based on Met Office forecasts, provides the Heat-Health Alert Service from June to September. This service aims to help healthcare professionals cope through periods of extreme temperature or heatwaves by informing possible five response levels (Levels 0‑4). Each level is associated with a series of actions, detailed in the Heatwave Plan for England, and include long-term planning, summer and heatwave preparedness and action, and a major national emergency (MetOffice, 2021[80]; UK Health Security Agency, 2022[81]). Another tool is promoted by the European Aeroallergen Network (EAN) and it forecasts pollen and fungal spore data for the European region (EAN, 2022[82]). In LAC, the Servicio Meteorologico Nacional in Argentina has launched an early warning system for heatwaves based on the impacts on population health. The SAT-OCS (Sistema de Alerta Temprana por Olas de Calor y Salud, in Spanish) has four levels of alert – green (no effect), yellow, orange, and red (extreme danger) – each of one indicating the potential effects of heatwaves on populations health (SMN Argentina, 2022[83]).
The COVID‑19 pandemic demonstrated the importance of clear and adequate risk communication with the general public as well as with the health personnel. The lack of rapid and clear information left people looking for answers to several questions in a stressful context, where disinformation and rumours were commonly found on social media, threatening the effectiveness and compliance with the emergency measures being enacted against the pandemic (OECD, 2020[43]).
Based on the 2021 GHSI for risk communication, the best prepared countries in LAC were Paraguay, Peru and Suriname, while the countries that need to improve their risk communication planning are Antigua and Barbuda, Bahamas, Belize, Bolivia, Dominica, Grenada, Guatemala and Venezuela. The average GHSI for LAC countries was 61.73 out of 100, below the score of OECD countries which reached 73.46 out of 100 (Figure 2.5). In this case, Australia, Canada, Portugal, Slovenia and the United Kingdom led the group (Bell and Nuzzo, 2021[29]).
Source: Bell and Nuzzo (2021[29]), Global Health Security Index: Advancing Collective Action and Accountability Amid Global Crisis, https://www.ghsindex.org/.
Complementarily, the risk communication plans specific to public health emergencies should also be improved in LAC countries. The average 2021 GSHI score for the region was 54.54 out of 100, where Argentina, Brazil, Chile, Costa Rica, Dominican Republic, Ecuador, El Salvador, Haiti, Honduras, Mexico, Nicaragua, Panama, Paraguay, Peru, Saint Lucia, Suriname, Trinidad and Tobago, and Uruguay led the region as well-prepared countries. In the case of OECD countries, most of them are well-prepared, having an average score of 82.21 (Bell and Nuzzo, 2021[29]).
As activities derived from healthcare services and delivery contribute to GHGs emissions, it is essential that health systems incorporate sustainable practices and reduce their carbon emissions and environmental footprint (WHO, 2015[5]). Also, climate resilient health systems consider response protocols under climate risk conditions to adequately provide essential medical products and services, including new technology that could help health service response (e.g. eHealth).
Although all actions from health systems are critical to improving population health and well-being, they have associated an important carbon and environmental footprint, which paradoxically threatens population health. It is estimated that between 4% and 10% of global GHG emissions come from the health sector; however, these estimates could vary significantly between countries and health centres. Globally, the main emitters of GHG in the health sector are the United States of America, China, and all countries from the European Union, which together represent approximately 56% of total emissions of the sector (HCWP/ARUP, 2019[84]).
International estimates show a strong association between the health expenditure per capita and the GHG emissions from the health sector per capita (Figure 2.6). OECD countries could double or even triple the health expenditure per capita (in PPP) as well as the total GHG emissions from the health sector compared to LAC countries (Lenzen et al., 2020[85]; WHO, 2022[86]). This information urgently calls for transformation in health services in the coming decades (Box 2.3). Some interventions to reduce the carbon and environmental footprint include passive solar heating and cooling strategies, energy efficiency, natural model ventilation, reducing water consumption, reducing general waste and waste anaesthetic gases, among others (World Bank, 2017[87]).
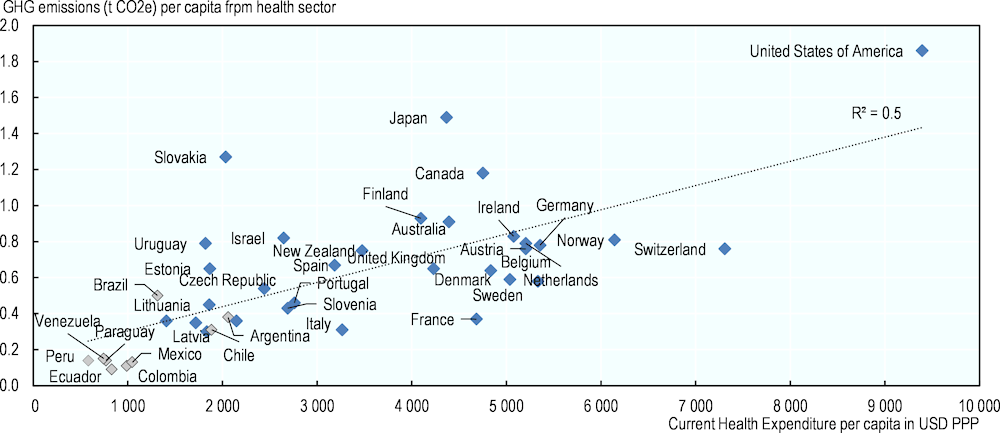
Source: WHO (2022[86]), “NHA Indicators”, WHO Global Health Expenditure Database, https://apps.who.int/nha/database/ViewData/Indicators/en and Lenzen et al. (2020[85]), “The environmental footprint of health care: a global assessment”, https://www.doi.org/10.1016/s2542-5196(20)30121-2.
The estimation of carbon or environmental footprints of health centres allows the identification of areas or activities responsible for large amounts of carbon emissions, as well as the subsequent planning of more sustainable health centres. For example, the Hospital General de Agudos Enrique Tornú de la Ciudad Autónoma de Buenos Aires in Argentina in 2015 found that of the total GHG CO2e emissions, 43% were from direct activities, 29% from energy consumption, and 29% from other indirect emissions (Rodriguez-Smith and Titto, 2018[88]). Also, the Hospital Base de Puerto Montt in Chile found that from the total CO2e emissions in 2016, 46% were from electricity consumption, 29% from the generation of residues, and 10% from clinical gas consumption, of which sevoflurane was the greatest contributor (Balkenhol et al., 2018[89]).
The Global Green and Healthy Hospitals (Red Global de Hospitales Verdes y Saludables) in Spanish, and Projeto Hospitais Saudáveis in Portuguese) is an international network of healthcare institutions that aims to transition to sustainable and climate‑smart healthcare. Under a standardised framework and roadmap, participating institutions and organisations act upon ten interconnected sustainability goals to promote sustainable healthcare, including leadership, safer chemicals, reducing waste, better transport and buildings, and green purchasing (HCWH, 2022[90]). Several healthcare facilities from LAC have joined the initiative, including Brazil (37 facilities), Chile (29 facilities), Colombia (20 facilities), Argentina, Costa Rica, Ecuador, and Mexico. Among these centres, the most shared goals are waste, leadership, and energy. In relation to hospitals, Chile leads the group with 180 hospitals, followed by Colombia (178 hospitals), Brazil (176 hospitals), and Mexico (80 hospitals), then fewer hospitals have joined from Argentina, Costa Rica, Ecuador, Dominican Republic, Peru, Guatemala, Uruguay, Honduras, and Panama. The most common area to focus on is energy, waste, and leadership (HCWH, 2022[90]). The voluntary nature of this membership demonstrates the awareness of the responsibility that health centres have on GHGs emissions, as well as the leadership of health institutions to become more sustainable, greener, and healthier.
Specific initiatives have emerged from the network. For example, in 2019, the first Latin America Huellatón was co‑organised by the Chilean Ministry of Health in collaboration with the Healthcare Without Harm Latin America team. The aim of this activity was to support hospitals in calculating and mitigating their carbon footprint (HCWH Europe, 2019[91]). Another initiative is called “Menos huella, más salud” (less footprint, more health), which aims to support hospitals and health centres in reducing their environmental footprint. For example, the Hospital San Rafael de Pasto in Colombia has reduced its environmental and water footprint by installing low consumption sinks and promoting composting to reduce waste. Similarly, the Dr. Rafael Angel Calderon Guardia hospital in Costa Rica has also reduced its water consumption and environmental footprint by installing water saving devices (HCWH and GGHH, 2021[92]).
From the COVID‑19 pandemic, several lessons can be learnt to strengthen technologies in the health sector, including digitalisation of health records for timely analyses, mobile applications, and telehealth consultations. These initiatives should also be accompanied by strengthening digital governance and processes for digitalisation, better digital security and interoperability, effective training of health personnel, and promotion of digital and health literacy within the population, among other barriers to overcome. Investments in digital health must also weighed against potential negative impacts such as the increase of GHG emissions or the generation of technological waste that can be challenging to manage, such as forever chemicals.
Health technologies may range from basic technologies that facilitate the access to healthcare services to more modern technologies, including telehealth. Nowadays, universal access to pre‑hospital care via telephone seems to be a basic service health systems provide, and it has helped improve the delivery of care, efficiency of resources, and visit success rates (Sheffield University, 2010[93]; Wray et al., 2022[94]). In 2016, 75% of the LAC countries had access to pre‑hospital care through national telephone numbers, while 21.42% (Argentina, Bolivia, Colombia, Dominican Republic, Panama and Paraguay) had partial coverage, and only one (Guatemala) had no coverage. In OECD countries, this situation improves, where more than 80% of countries had universal access, 13.2% had partial coverage and 2.6% had no coverage at all (WHO, 2020[95]).
A more modern approach to new health technologies might be seen in several LAC and OECD countries, from telehealth to artificial intelligence. A digital transformation process would strengthen climate resilience if health systems included a climatic preparedness and disaster risk approach across all building blocks and health policies. The number of OECD countries that have implemented electronic medical records (EMRs) have increased over time, where on average, 93% of primary care practices use EMRs across 24 OECD countries in 2021. Additionally, most patients are able to view and interact with their information on EMRs as well as to access to teleconsultations or video-conferencing (OECD, 2021[96]). From the start of the COVID‑19 pandemic, the proportion of adults who reported teleconsultations (online or by phone) increased considerably, from 30% in mid‑2020 to approximately 50% in early 2021 (OECD, 2021[96]).
Access to technological devices and the Internet is critical for the digitalisation of health systems and HISs (Box 2.4). Figure 2.7 shows that the percentage of people using the Internet in OECD and LAC countries has steadily increased from 1990 to 2020 but significantly varies across countries. In LAC, this percentage in 2020 was, on average, 66.7%, with Haiti showing the lowest proportion (34.5%) and Chile the largest (88.3%). The situation in OECD countries is quite different, where the average in 2020 was 88%, with Colombia having the lowest proportion (69.8%) and Iceland the largest (99%) (ITU, 2022[97]; World Bank, 2022[98]; WHO, 2022[72]). Access should increase to enable the digitalisation of health systems in the region, which would improve the access to care by shortening geographical barriers and facilitate communications with the general public and with the health personnel during routine activities and emergencies.
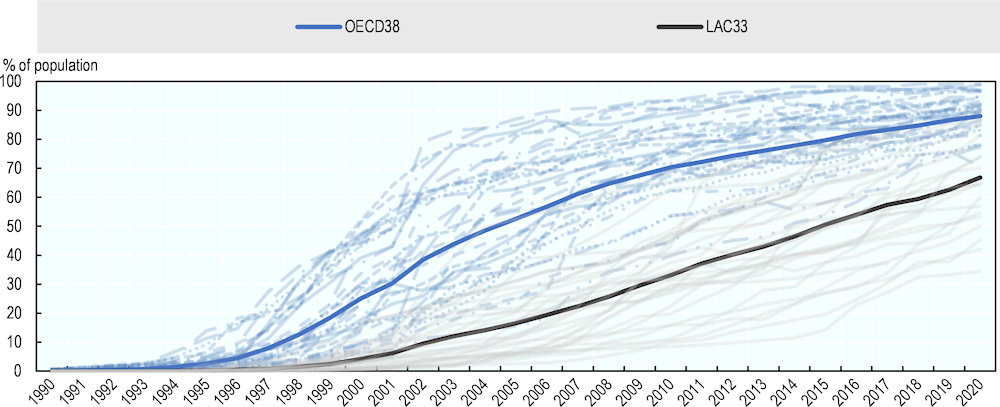
Source: ITU (2022[97]), Core indicators on access to and use of ICT by households and individuals, https://www.itu.int:443/en/ITU-D/Statistics/Pages/stat/default.aspx; Word Bank (2022[98]), Individuals using the Internet (% of population), https://data.worldbank.org/indicator/IT.NET.USER.ZS; WHO (2022[72]), Surveillance (IHR SPAR), https://www.who.int/data/gho/data/indicators/indicator-details/GHO/surveillance-ihr-spar.
Although very scarcely, there have been several initiatives to incorporate new technologies in LAC countries prior to the COVID‑19 pandemic (PAHO, 2019[99]). Brazil has expanded its telemedicine activities by using artificial intelligence and launching Telessaude Brazil programme focused on teleconsultations in primary healthcare, resulting in optimising waiting lists and expanding the access to healthcare (Haddad and Messina, 2021[100]). Uruguay and Costa Rica have implemented EHRs for patients (Bagolle et al., 2022[101]). Jamaica has launched the mobile health app “Jamaica Moves” that aims to track health status and promote healthier lifestyles (Bagolle et al., 2022[101]). Additionally, Chile has launched Hospital Digital, which is associated with a new healthcare model and aims to transform and modernise the public health system by offering digital services, such as Saludablemente and Yo me Vacuno (Ministerio de Salud - Chile, 2021[102]).
To support countries, the digital assessment toolkit guide, provided by the World Bank, gives a framework on how to assess different quantitative indicators, areas of digitalisation, and plan future digital health roadmap strategy and interventions (World Bank, 2021[103]). Complementary, the PAHO has launched a plan of action for strengthening information systems for health with the objective to “strengthen the activities of Member States aimed at upgrading health systems through the use of interconnected and interoperable information systems” (PAHO, 2019[99]).
The health challenges associated with climate change require the adoption of new health innovations and technologies either to provide better health services, be responsive during emergencies, or reduce the carbon or environmental footprints. However, these innovations sometimes may have important implications for health systems that should be identified and addressed appropriately. In this sense, health technology assessments (HTAs) allow a systematic evaluation of the consequences of the technologies to be introduced (Box 2.5).
HTAs are carried out in 15 of the responding LAC countries (Argentina, Belize, Brazil, Chile, Colombia, Costa Rica, Ecuador, El Salvador, Guyana, Jamaica, Mexico, Paraguay, Peru, Trinidad and Tobago, and Uruguay), and their scope and coverage vary significantly across countries. Only a few LAC countries use HTA systematically (Belize, Brazil, Jamaica, Mexico, Paraguay, Trinidad and Tobago, and Uruguay) to make coverage decisions and no country reported to use HTA to determine reimbursement levels (Lorenzoni et al., 2019[104]).
Considering health systems as a whole, the National Health Service (NHS) in the United Kingdom has committed to be become more environmentally sustainable and net-zero by 2040 (NHS England, 2022[105]). The NHS is responsible for 4% of the country’s GHG carbon emissions and the largest publicly funded health system in the world (Tennison et al., 2021[106]). Since 2008, the NHS has been working according to the UK Climate Change Act, conducting carbon footprints regularly and aiming to be the world’s first net zero national health service. From 1990 to 2019, the CO2e emissions have been reduced by 26%; however, there is still work to do up to 2040 and beyond. The NHS has a adopted a 4‑steps analytical process to inform the targets and trajectories for net-zero, including current estimates of NHS carbon footprint, modelled projected scenarios, carbon reductions available across the system, and modelled interventions and carbon reductions. This approach would allow to have a clear understanding of the current situation of the system and what the potential future scenarios and interventions would be possible to follow to achieve net-zero (NHS England, 2022[105]).
For health systems to be climate resilient, they should transform their traditional biomedical health models and integrate social and environmental determinants that mediate the effects of climate change on population health. Surveillance and management of these determinants are essential, particularly through collaborative and intersectoral public health programmes in which the health sector provides evidence, monitors health effects of climate change, defines regulatory standards, and co‑ordinates health risk management. Climate‑informed health programmes and preparedness and emergency plans contribute to resilient health systems and protect population health.
Strategic public health emergency preparedness frameworks are key to supporting, organising, and enabling the responsibilities and activities of health systems during an emergency, optimising their functions, effectiveness, and the analysis of the resources needed.
In terms of having a clear national health emergency framework (NHEF), LAC countries have improved over time; however, there are still significant differences across countries. Between 2019 and 2020, the IHR score in LAC countries was, on average, 74.6 out of 100, with Cuba, El Salvador, Guatemala, Guyana and Nicaragua being the most prepared countries and Argentina the least prepared. In contrast, OECD countries, the average was 84 out of 100, with a minimum of 33 and maximum of 100 (Figure 2.8) (WHO, 2022[107]).
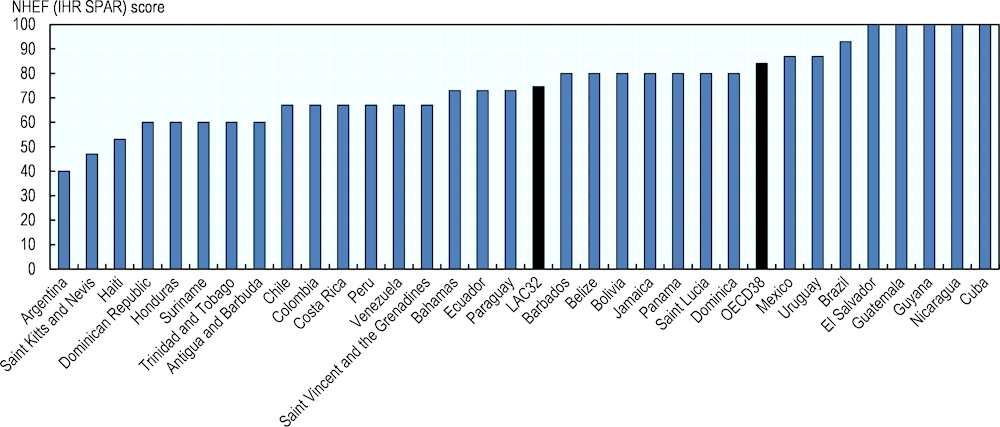
Source: WHO (2022[107]), National Health Emergency Framework (IHR SPAR), https://www.who.int/data/gho/data/indicators/indicator-details/GHO/national-health-emergency-framework.
Health systems, at national or local levels, are responsible for developing health programmes that address climate‑sensitive health risks (e.g. heat-related illnesses, vector- and water-borne diseases), as well as the health response during extreme weather events. National health plans or strategies and health programmes should progressively include critical information on climatic hazards and vulnerabilities as these affect the final health outcomes on the population (Box 2.6).
According to the 2021 WHO HCCGS, the proportion of countries that are developing or already developed climate‑informed health programmes in LAC ranges from 4.2% to 29.2%, while in OECD this range goes from 0% to 54.6%. The three top areas which most countries are focusing on are health-related illnesses, injuries and mortality from extreme weather events, and vector-borne diseases (Figure 2.5) (WHO, 2021[19]).
|
Area |
LAC countries |
OECD countries |
|---|---|---|
|
Airborne and respiratory illnesses |
17.4% |
27.3% |
|
Heat-related illness |
4.6% |
54.6% |
|
Injury and mortality from extreme weather events |
13% |
50% |
|
Malnutrition and foodborne diseases |
4.2% |
0% |
|
Mental and psychosocial health |
4.4% |
20% |
|
Noncommunicable diseases |
4.2% |
27.3% |
|
Vector-borne diseases |
29.2% |
25% |
|
Waterborne diseases and other water-related health outcomes |
16.7% |
18.2% |
|
Zoonoses |
13% |
10% |
Source: WHO (2021[19]), WHO health and climate change global survey report, https://apps.who.int/iris/handle/10665/348068.
As a national strategy, Health Canada has developed HealthADAPT, which is a multi-year capacity-building programme that aims to help the health sector and communities to prepare for and respond to the impacts of climate change. Several projects focus on understanding the health vulnerabilities to climate change and developing adaptive capacity of health systems to limit the damage from climate change (Health Canada, 2022[108]).
Learning from the catastrophic event of 2003 heatwaves in Europe (Robine et al., 2008[109]), Austria, Belgium, Croatia, France, Germany, Greece, Hungary, Italy, the Netherlands, Portugal, Slovenia, Spain, Sweden and Switzerland have developed national or subnational health-heat action plans (HHAP) (European Climate Adaptation Platform, 2021[110]; WHO, 2008[27]). Germany, for example, has even included climate change in the strategic plan of the Ministry of Health, leading to some extent to an inclusion of the topic across all health programmes (WHO, 2015[111]). In 2022, Chile also included climate change as a topic in the national strategic plan up to 2030 (Ministerio de Salud, Chile, 2022[112]).
All plans, programmes, and activities to strengthen climate resilient health systems require financial resources. Climate finance capacity varies significantly between and within countries and, in general, the most vulnerable countries are often the least able to obtain sufficient financing support to implement adaptation and resilience actions.
Funding mechanisms, either at an international or national level, have to be implemented to support policies that boost the resilience of health systems as well as other sectors through activities oriented to improve health infrastructure, train health personnel, implement monitoring and emergency systems, and ensure food security, sanitation, and water supply (WHO, 2015[5]). Internationally, the UNFCCC, the Kyoto Protocol and the Paris Agreement call for financial assistance from Parties with more financial resources to those that are less well-endowed and more vulnerable. Nationally, countries should perform V&A assessments and promote adaptation capacities to allocate, apply for, and prioritise climate‑smart healthcare investments. Several funds have been established to help countries with limited financial capacity to prepare and cope with climatic hazards and strengthen health systems.
The World Bank is engaging with international partners to develop innovations and policy action in this agenda, under the umbrella term Green Health Financing (GHF). These engagement seeks to strengthen all three health financing functions (resource mobilisation, risk pooling and strategic purchasing) with a focus on climate.
In LAC, several international funding bodies have supported a wide range of adaptation projects. From the Adaptation Fund (AF), established under the Kyoto Protocol, 27 adaptation projects have been funded in LAC (up to August 2022), including projects focused on multiple sectors as well as agriculture, coastal management, disaster risk reduction, food security, rural development, and water management. On average, the grant amount per project is USD 5 403 755, with a minimum of USD 10 000 and a maximum of USD 13 248 121. In general, the projects across all countries are mostly focused on enhancing adaptation and resilience and reducing vulnerability (Adaptation Fund, 2022[113]). The Global Facility for Disaster Reduction and Recovery (GFDRR) have funded 34 projects in LAC aiming at reducing disaster risk or enhancing resilience. The average granted amount per project is USD 509 654 (minimum of USD 49 943 and maximum of USD 1 833 744). The most common funding source is the Japan-World Bank Program for Mainstreaming Disaster Risk Management in Developing Countries, followed by the European Union (EU) – African, Caribbean and Pacific (ACP) Region Disaster Reduction Partnership Trust Fund (GFDRR, 2022[114]). None of the projects, either from the AF or the GFDRR is specifically focused on health systems or public. Figure 2.6 shows the recipients and number of projects awarded from the Adaptation Fund and the GFDRR.
|
Country |
Projects under the AF |
Projects under the GFDRR |
||||
|---|---|---|---|---|---|---|
|
1 |
2 |
3 or more |
1 |
2 |
3 or more |
|
|
Antigua and Barbuda |
✓ (3) |
|||||
|
Argentina |
✓ |
|||||
|
Bahamas |
||||||
|
Barbados |
||||||
|
Belize |
✓ |
|||||
|
Bolivia |
✓ |
|||||
|
Brazil |
✓ (3) |
|||||
|
Central America |
✓ |
|||||
|
Chile |
✓ |
|||||
|
Colombia |
✓ |
|||||
|
Costa Rica |
✓ (5) |
|||||
|
Cuba |
✓ |
|||||
|
Dominica |
✓ |
✓ |
||||
|
Dominican Republic |
✓ (3) |
✓ |
||||
|
Ecuador |
✓ |
|||||
|
El Salvador |
✓ |
✓ |
||||
|
Grenada |
||||||
|
Guatemala |
✓ |
|||||
|
Guyana |
||||||
|
Haiti |
✓ |
✓ (3) |
||||
|
Honduras |
✓ (3) |
✓ |
||||
|
Jamaica |
✓ |
|||||
|
LAC |
✓ (3) |
|||||
|
Mexico |
✓ |
✓ |
||||
|
Nicaragua |
✓ |
|||||
|
Panama |
✓ |
|||||
|
Paraguay |
✓ |
|||||
|
Peru |
✓ (3) |
✓ (4) |
||||
|
Saint Kitts and Nevis |
||||||
|
Saint Lucia |
✓ |
✓ |
||||
|
Saint Vincent and the Grenadines |
✓ |
|||||
|
Suriname |
✓ |
|||||
|
The Caribbean |
✓ (9) |
|||||
|
Trinidad and Tobago |
✓ |
|||||
|
Uruguay |
✓ |
|||||
|
Venezuela |
||||||
Sources: Adaptation Fund (2022[113]), Projects Table View, https://www.adaptation-fund.org/projects-programmes/project-information/projects-table-view/ and GFDRR (2022[114]), GFDRR grants, https://www.gfdrr.org/en/grants?title=&field_grant_region_target_id=14&field_country_target_id=All&field_topics_term_target_id=All&field_sendai_tag_value=All&field_status_value=All&field_completion_date_value&field_start_date_value&page=1.
Focusing on health, food, and water security, the Green Climate Fund (GCF) have approved 17 projects of which 7 are focused on adaptation and 11 are cross-cutting projects in LAC. Most projects are related to new technologies applied to coral reefs, forest restoration, the agricultural sector, water management, and financial systems; however, none is focused on health systems. On average, the grant amount is USD 284 710 000 and includes Bahamas, Barbados, Belize, Brazil, Chile, Colombia, Costa Rica, Dominican Republic, Ecuador, El Salvador, Grenada, Guatemala, Honduras, Jamaica, Mexico, Nicaragua, Panama, and Trinidad and Tobago.
The GFC Readiness Programme, which provides resources to strengthen the institutional capacities of National Designated Authorities/focal points, has awarded four projects to LAC countries related to strengthening climate resilience of health systems. The project “Developing a climate resilient health system in The Bahamas” was awarded to Bahamas in 2020; the project “Increasing health sectors capacities and strengthening co‑ordination on climate action in Argentina at national and subnational levels” was awarded to Argentina in 2020; the project “Enhancing climate change resilience of health systems in the Caribbean” was awarded to Jamaica, Guyana, Saint Kitts and Nevis, Saint Lucia, Haiti, Trinidad and Tobago, and Belize in 2020; and the project “Building climate resilience into Trinidad and Tobago Healthcare System” was awarded to Trinidad and Tobago in 2020 (Green Climate Fund, 2022[115]). The outcomes of these projects are still unpublished, and it is probable that standardised mechanisms of impact evaluation would be needed.
Other funds have also supported different adaptation projects, ranging from building resilience in agriculture, water management, ecosystems, coastal cities. Almost all countries in LAC have received funding from the Global Climate Change Alliance Plus (GCCA+) from the EU, Global Environment Facility (GEF), Least Developed Countries Fund (LDCF), MDG Achievement Fund, Pilot Program for Climate Resilience (PPCR) and the Special Climate Change Fund (SCCF). Unfortunately, from the title of the projects, none is focused on strengthening climate resilience of health systems. One mitigation project has been approved by the Clean Technology Fund (CFT) in Honduras and is titled “GESP: Innovative Energy Solutions for Health Service Delivery in Honduras” (Climate Funds Update, 2022[116]). The World Bank Group has also been one of the largest multilateral financier of climate action in developing countries, delivering record USD 31.7 billion in climate finance in fiscal year 2022 (World Bank, 2022[117]).
Complementary, based on the 2021 WHO HCCGS, 36% (n=9) of the participating countries have declared the Ministry of Health is currently receiving international funds to support climate and change work and plans. These countries are Bahamas, Belize, Colombia, Grenada, Guatemala, Guyana, Jamaica, Peru, and Saint Kitts and Nevis (WHO, 2021[19]).
There is no doubt that strengthening climate resilient health systems requires adequate and sustained financing. On one hand, and according to the principle of “common but differentiated responsibility”, international support should be provided to countries that need it the most; however, every country needs to strengthen its own financial capacity to improve its climate resilience and prioritise resources according to its own vulnerabilities and capacities. Adequate strategic planning and strong intersectoral collaboration would optimise institutional efforts and financial resources by multiplying positive effects in different sectors as well as in all building blocks of health systems.
This chapter has examined the level of resilience of the health systems of the LAC countries to climate change, identifying trends in the region and providing key considerations for policy actions that countries can implement to strengthen this resilience.
LAC countries have a great opportunity to overcome the health and economic crises caused by the COVID‑19 pandemic, as well as to build forward better considering the challenges imposed by the climate change. To promote climate resilient health systems as LAC countries recover from the COVID‑19 crisis, they should focus on:
Leadership and governance: The health sector should lead a positive transformation towards climate resilience within health systems and support other health-determining sectors. Health policies and programmes should integrate a climate resilient and disaster risk management perspective to strengthen health systems for current and future shocks and stresses. Specific collaborative agendas between the Ministry of Health and health-determining sectors, such as meteorological services or social services, should be carried out to better understand the effects of climate hazards on population health and be able to prepare for them, as well as identify the most vulnerable populations to better protect them. Some specific recommendations to strengthen leadership and governance are:
Designate a team on climate change and health within the health sector with leadership capacity, financial resources and links with other health-determining sectors. This team would be responsible for ensuring that intersectoral collaboration, policies, and activities are adequately performed.
Define and track key performance indicators that allow quantification of progress toward building climate resilience of health systems, including those indicators related to accountability.
Health workforce: Formal development and training opportunities on climate change and health should be established through collaboration between institutions to enhance the technical and professional capacity of health personnel. Instances of formal education should be supported by academic institutions, and legally and financially recognised by ministries of education, health, and finance of each country. Some specific recommendations to strengthen the health workforce are:
Create an educational and training framework on climate change and health supported by a national committee that integrates ministries of health and education, as well as academic institutions and health centres. This framework would standardise training instances according to context-specific needs.
Apply this framework to establish risk communication protocols with the general public and health personnel before, during, and after extreme climatic events.
Health information systems: LAC countries need to formalise and systematise their V&A assessments to better integrate climatic information into health programmes, surveillance systems and implement early warning systems. Countries should focus on risk communication as the basis of these efforts. Some specific recommendations to strengthen health information systems are:
Perform V&A assessments at the municipal level including spatial identification of vulnerable populations, which can be supported by community health workers.
Establish working groups between the health sector and the meteorological and environmental sectors in order to inform health programmes about climate hazards, integrate climate into surveillance systems and develop early warning systems for health risks.
Essential medical products and technologies: Transitioning towards the sustainable and climate‑smart transformation of health systems would strengthen leadership of the health sector in promoting better health for all, decrease disruptions during climate shocks and stresses, and reduce the environmental footprint of healthcare services. Some specific recommendations to strengthen essential medical products and technologies are:
Promote digitalisation of health systems and invest in interoperability and cybersecurity.
Develop a national framework that standardises the evaluation of sustainability of health centres, as well as guides improvement of buildings, optimisation energy and water consumption, and improve green waste management.
Strengthen PHC to ensure that climate‑related health risks are addressed, and that health emergency response systems are climate resilient and adopt low carbon, climate‑resilient service delivery: LAC countries should strengthen their national health emergency frameworks, including climate emergency preparedness and response planning. To build climate resilience, LAC countries should emerge actively promote collaboration with health-determining sectors to include climate and social determinants of health in health programmes. Health emergency plans should be in full co‑ordination with national and local emergency plans, which means that community-based preparedness and response are critical to protect health during emergencies. Complementarily, to reduce the current and future impacts of climate and environmental hazards, health programmes should integrate climatic information from design to implementation. Some specific recommendations to strengthen service delivery are:
Develop a national policy on disaster risk management that includes climate hazards and allows rapid articulation with regional and local circumstances.
Implement awareness campaigns on climate change and health targeted to the general public as well as health personnel.
Reduce air pollution by progressively incorporating clean cooking and heating systems, as well as improving public transport and creating cyclable and walkable cities and promoting low carbon diets. These actions would benefit health beyond climate change impacts, as they can help promote healthier food habits and physical activity.
Strengthen PHC to ensure that climate‑related health risks are addressed (e.g. heatstroke), and that health emergency response systems are prepared to provide essential services despite climate‑related hazards and risks.
Financing: Countries should allocate more resources to prepare health systems for the impact of climate change and capitalise on synergies with other areas (e.g. pandemic preparedness) and sectors. Equally important, LAC countries should strengthen collaboration between them, as well as with diverse stakeholders, to obtain international financial support. Some areas to strengthen financing are:
Increase public spending for core public health services that protect the population from climate change.
Establish transdisciplinary working groups that can seek international funding to analyse public health problems and design and implement evidence‑based policies.
LAC countries are in the process of strengthening the climate preparedness and resilience of their health systems; however, this chapter has highlighted some of remaining gaps. LAC countries have the potential to successfully build more equitable, accessible, and climate resilient health systems, but they need to adopt a proactive, holistic and collaborative approach, taking into account the important role of health-determining sectors, stakeholders, and international institutions, as well as health sector actors across all levels.
[113] Adaptation Fund (2022), Projects Table View, https://www.adaptation-fund.org/projects-programmes/project-information/projects-table-view/.
[74] Aguas, R. et al. (2019), “Cross-serotype interactions and disease outcome prediction of dengue infections in Vietnam”, Scientific Reports, Vol. 9/1, https://doi.org/10.1038/s41598-019-45816-6.
[101] Bagolle, A. et al. (2022), La gran oportunidad de la salud digital en América Latina y el Caribe, Inter-American Development Bank, https://doi.org/10.18235/0004153.
[89] Balkenhol, M. et al. (2018), “Huella de carbono en el Hospital Base de Puerto Montt”, Revista médica de Chile, Vol. 146/12, pp. 1384-1389, https://doi.org/10.4067/s0034-98872018001201384.
[44] Bangdiwala et al. (2021), Statistical Considerations when Communicating Health Risks: Experiences from Canada, Chile, Ecuador and England Facing COVID-19.
[29] Bell, J. and J. Nuzzo (2021), Global Health Security Index: Advancing Collective Action and Accountability Amid Global Crisis, https://www.ghsindex.org/.
[69] Calderón, A., N. Francisco and R. López (2021), Indice de vulnerabilidad al cambio climatico de la Republica de Panama, https://dcc.miambiente.gob.pa/wp-content/uploads/2021/07/Indice_de_Vulnerabilidad_al_Cambio_Climatico.pdf.
[37] CDKN (2022), Curso: Comunicando el cambio climático de manera efectiva,” Climate & Development Knowledge Network, https://cdkn.org/es/page/comunicando.
[10] CEPAL (2022), Panorama Social de América Latina, CEPAL, https://hdl.handle.net/11362/48518.
[24] Chesini, F. and M. Orman (2021), Politica de salud en la agenda climatica Argentina, Ministerio de Salud de la Nación.
[116] Climate Funds Update (2022), Climate Funds Update, https://climatefundsupdate.org/data-dashboard/themes/.
[33] Columbia University (2022), Caribbean Climate and Health Responders Course, https://www.publichealth.columbia.edu/research/global-consortium-climate-and-health-education/caribbean-climate-and-health-responders-course.
[32] Columbia University (2022), Climate and Health Responder Course for Latin America, https://www.publichealth.columbia.edu/research/global-consortium-climate-and-health-education/climate-and-health-responder-course-latin-america.
[70] D’Ercole, R. and M. Trujillo (2003), Amenazas, vulnerabilidad, capacidades, y riesgos en el Ecuador, https://horizon.documentation.ird.fr/exl-doc/pleins_textes/divers11-03/010032419.pdf.
[60] Dirección de Cambio Climático de la Secretaría de Ambiente y Desarrollo Sustentable de la Nación Argentina (2011), Manual: Vulnerabilidad y Adaptación al Cambio Climático para la Gestion y Planificación Local.
[82] EAN (2022), Pollen Info, https://www.polleninfo.org/country-choose.html.
[79] EuroHEAT (2022), EuroHEAT - Forecasts, http://www.euroheat-project.org/dwd/index.php.
[110] European Climate Adaptation Platform (2021), National heat-health warning systems and action plans, https://climate-adapt.eea.europa.eu/en/observatory/evidence/national-and-sub-national-warning-systems.
[62] Ezquiaga Arquitectura, Sociedad y Territorio S.L. (2015), The Experience of Latin America and the Caribbean in Urbanization: Knowledge Sharing Forum on Development Experiences: Comparative Experiences of Korea and Latin America and the Caribbean.
[6] Friedlingstein, P. et al. (2022), “Global Carbon Budget 2021”, Earth System Science Data, Vol. 14/4, pp. 1917-2005, https://doi.org/10.5194/essd-14-1917-2022.
[114] GFDRR (2022), GFDRR Grants, https://www.gfdrr.org/en/grants?title=&field_grant_region_target_id=14&field_country_target_id=All&field_topics_term_target_id=All&field_sendai_tag_value=All&field_status_value=All&field_completion_date_value&field_start_date_value&page=1.
[65] Giardino et al. (2020), Assessing the impact of sea level rise and resilience potential in the Caribbean. Revisiting Resilience in the Caribbean: a 360-degree approach.
[7] Global Carbon Project (2021), Supplemental data of Global Carbon Project 2021, https://doi.org/10.18160/gcp-2021.
[67] Gobierno de México/INECC (2022), Atlas Nacional de Vulnerabilidad al Cambio Climático, https://atlasvulnerabilidad.inecc.gob.mx/page/index.html#zoom=8&lat=31.7613&lon=-115.2253&layers=1.
[115] Green Climate Fund (2022), Green Climate Fund - Projects & Programmes, https://www.greenclimate.fund/countries.
[100] Haddad, A. and L. Messina (2021), La Telemedicina y la Telesalud integradas en el ecosistema de salud digital, https://www.paho.org/ish/.
[90] HCWH (2022), Global Green and Healthy Hospitals, Health Care without Harm, https://greenhospitals.org/about.
[92] HCWH and GGHH (2021), Hospitales que curan el planeta. Informe sobre el trabajo de los miembros de la red global de hospitales verdes y saludables en America Latina, https://saludsindanio.org/informe-2022.
[91] HCWH Europe (2019), Annual Report 2019, Health Care without Harm, https://noharm-europe.org/documents/annual-report-2019.
[84] HCWP/ARUP (2019), Health care’s climate footprint: How the health sector contributes to the global climate crisis and opportunities for action, Health Care without Harm, https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf.
[59] Health Canada (2022), Climate change and health vulnerability and adaptation assessment: Workbook for the Canadian health sector.
[108] Health Canada (2022), HealthADAPT: Program descriptions, https://www.canada.ca/en/health-canada/programs/health-adapt.html.
[48] IADB (2010), Vulnerabilidad y adaptación al cambio climatico: Diagnóstico inicial, avances, vacíos y potenciales líneas de acción en Mesoamérica, https://publications.iadb.org/es/vulnerabilidad-y-adaptacion-al-cambio-climatico-diagnostico-inicial-avances-vacios-y-potenciales.
[36] IAI (2020), Cambio Climático y Global en América Latina: Curso masivo en línea, https://cclatam.iai.int/.
[61] IPCC (2022), Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change, (H.-O. Pörtner et al., Eds.), Cambridge University Press.
[9] IPCC (2021), Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change, Cambridge University Press.
[97] ITU (2022), Core indicators on access to and use of ICT by households and individuals, https://www.itu.int:443/en/ITU-D/Statistics/Pages/stat/default.aspx.
[1] Jaramillo, C. (2022), In 2022, Latin America and the Caribbean Must Urgently Strengthen the Recovery, World Bank, https://www.worldbank.org/en/news/opinion/2022/02/07/latin-america-and-the-caribbean-must-urgently-strengthen-the-recovery.
[85] Lenzen, M. et al. (2020), “The environmental footprint of health care: a global assessment”, The Lancet Planetary Health, Vol. 4/7, pp. e271-e279, https://doi.org/10.1016/s2542-5196(20)30121-2.
[104] Lorenzoni, L. et al. (2019), “Health systems characteristics: A survey of 21 Latin American and Caribbean countries”, OECD Health Working Papers, No. 111, OECD Publishing, Paris, https://doi.org/10.1787/0e8da4bd-en.
[80] MetOffice (2021), Heat-Health Alert, https://www.metoffice.gov.uk/public/weather/heat-health/?tab=heatHealth&season=normal.
[57] MINEA (2017), Segunda Comunicación Nacional ante la CMNUCC., Venezuela, http://www.minea.gob.ve/wp-content/uploads/2015/10/Segunda-Comunicaci%C3%B3n-sobre-Cambio-Clim%C3%A1tico-V.pdf.
[53] Ministerio de Ambiente y Energía (2022), Plan Nacional de Adaptación al Cambio Climático., Costa Rica, https://cambioclimatico.go.cr/wp-content/uploads/2022/04/NAP_Documento-2022-2026_VC.pdf.
[25] Ministerio de Planificación del Desarrollo (2007), Mecanismo Nacional de Adaptación al Cambio Climático, https://www.bivica.org/file/view/id/1415.
[71] Ministerio de Salud (2018), Observatorio Nacional de Salud y Clima, Cambio climático y salud,” Cambio climático y salud, Argentina.
[102] Ministerio de Salud - Chile (2021), ¿Qué es Hospital Digital? - Hospital Digital, Chile, https://www.hospitaldigital.gob.cl/hospital-digital/que-es-hospital-digital.
[23] Ministerio de Salud y Desarrollo Social, Argentina (2019), Plan de Acción de Salud y Cambio Climático, https://www.argentina.gob.ar/sites/default/files/infoleg/res447-6.pdf.
[112] Ministerio de Salud, Chile (2022), Estrategia Nacional de Salud para los Objetivos Sanitrios al 2030, https://www.minsal.cl/wp-content/uploads/2022/03/Estrategia-Nacional-de-Salud-2022-MINSAL-V8.pdf.
[54] Ministerio del Ambiente (2022), Plan Nacional de Adaptación al Cambio Climático del Perú: Un insumo para la actualización de la Estrategia Nacional ante el Cambio Climático., Peru, https://cdn.www.gob.pe/uploads/document/file/2827898/220214_Resumen%20Ejecutivo%20del%20Plan%20Nacional%20.
[68] Ministerio del Medio Ambiente (2020), Atlas de Riesgos Climaticos (ARCLIM), Chile.
[52] Ministerio del Medio Ambiente (2017), Plan de Acción Nacional de Cambio Climático 2017-2022., Santiago, Chile, https://mma.gob.cl/wp-content/uploads/2017/07/plan_nacional_climatico_2017_2.pdf.
[56] MVOTMA (2010), Plan nacional de respuesta al cambio climatico. Diagnostico y lineamientos estrategicos., Uruguay, https://www.gub.uy/ministerio-ambiente/politicas-y-gestion/planes/plan-nacional-respuesta-cambio-climatico.
[105] NHS England (2022), Delivering a ‘Net Zero’ National Health Service, Queen’s Printer of Acts of Parliament, https://www.legislation.gov.uk/ukpga/2022/31/contents/enacted.
[96] OECD (2021), “Digital health”, in Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/08cffda7-en.
[2] OECD (2020), “COVID-19 in Latin America and the Caribbean: Regional socio-economic implications and policy priorities”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/93a64fde-en.
[43] OECD (2020), “Transparency, communication and trust: The role of public communication in responding to the wave of disinformation about the new Coronavirus”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/bef7ad6e-en.
[4] OECD/The World Bank (2020), Health at a Glance: Latin America and the Caribbean 2020, OECD Publishing, Paris, https://doi.org/10.1787/6089164f-en.
[18] Office of Climate Change, Government of Guyana (2019), Office of Climate Change - Guyana - NAP, https://climatechange.gov.gy/en/index.php/component/tags/tag/nap.
[73] PAHO (2022), PLISA Health Information Platform for the Americas - Dengue Fever in The Americas: Number of reported cases.
[50] PAHO (2021), EU CARIFORUM Climate Change and Health Project, https://www.paho.org/en/eu-cariforum-climate-change-and-health-project.
[21] PAHO (2019), Caribbean Action Plan on Health and Climate Change. No. PAHO/CDE/19-007.
[99] PAHO (2019), Plan of action for strengthening information systems for health 2019-2023, https://iris.paho.org/handle/10665.2/51617.
[77] PAHO/WHO (2023), “Dengue incidence rate”, PLISA Health Information Platform for the Americas, Pan American Health Organization, https://www3.paho.org/data/index.php/en/mnu-topics/indicadores-dengue-en/dengue-nacional-en/254-dengue-incidencia-en.html.
[35] PAHO-VCPH (2022), Virtual Classroom of Massive Open Online Courses of Public Health, https://mooc.campusvirtualsp.org/.
[30] Palmeiro-Silva, Y. et al. (2021), “Cambio climático y salud ambiental en carreras de salud de grado en Latinoamérica”, Revista de Saúde Pública, Vol. 55, p. 17, https://doi.org/10.11606/s1518-8787.2021055002891.
[66] Pörtner, H. et al. (eds.) (2022), Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change, Cambridge University Press, http://doi:10.1017/9781009325844.
[55] Presidencia de la República Dominicana (2016), Plan Nacional de Adaptación para el cambio climático en la República Dominicana.
[49] Providas (2013), Avances en el conocimiento: Cambio climático y el desafío de la salud en Bolivia., Bolivia, https://www.undp.org/sites/g/files/zskgke326/files/migration/bo/undp-bo-salud-2014.pdf.
[109] Robine, J. et al. (2008), “Death toll exceeded 70,000 in Europe during the summer of 2003”, Comptes Rendus Biologies, Vol. 331/2, pp. 171-178, https://doi.org/10.1016/j.crvi.2007.12.001.
[88] Rodriguez-Smith, M. and E. Titto (2018), Hospitales sostenibles frente al cambio climático: Huella de carbono de un hospital público de la ciudad de Buenos Aires, Revista Argentina de Salud Pública.
[11] Romanello, M. et al. (2022), “The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels”, The Lancet, Vol. 400/10363, pp. 1619-1654, https://doi.org/10.1016/s0140-6736(22)01540-9.
[64] Romanello, M. et al. (2021), “The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future”, The Lancet, Vol. 398/10311, pp. 1619-1662, https://doi.org/10.1016/s0140-6736(21)01787-6.
[46] Rozenberg et al. (2021), 360° Resilience: A Guide to Prepare the Caribbean for a New Generation of Shocks, The World Bank, Washington, D.C.
[31] Shea, B., K. Knowlton and J. Shaman (2020), “Assessment of Climate-Health Curricula at International Health Professions Schools”, JAMA Network Open, Vol. 3/5, p. e206609, https://doi.org/10.1001/jamanetworkopen.2020.6609.
[93] Sheffield University (2010), Building the evidence base in pre-hospital urgent and emergency care: a review of research evidence and priorities for future research.
[83] SMN Argentina (2022), Estado del Sistema de Alerta Temprana por Olas de Calor y Salud (SAT-OCS) | Servicio Meteorologico Nacional, https://www.smn.gob.ar/smn_alertas/olas_de_calor.
[39] Sochisap (2022), SoChiSaP, https://www.sochisap.org/.
[38] TelessaudeRS (2020), Cursos ead com inscrições abertas no Moodle do TelessaúdeRS, https://www.ufrgs.br/telessauders/noticias/inscricoes-abertas-para-cursos-de-estomatologia-animais-peconhentos-climaterio-e-nutricao-na-aps/.
[106] Tennison, I. et al. (2021), “Health care’s response to climate change: a carbon footprint assessment of the NHS in England”, The Lancet Planetary Health, Vol. 5/2, pp. e84-e92, https://doi.org/10.1016/s2542-5196(20)30271-0.
[34] The University of West Indies (2022), Climate Change and Health Leaders Fellowship Program, https://sta.uwi.edu/cchsrd/empowering-caribbean-action-climate-and-health-each.
[81] UK Health Security Agency (2022), Heatwave plan for England: Protecting health and reducing harm from severe heat and heatwaves, https://www.gov.uk/government/publications/heatwave-plan-for-england.
[40] UNCCELEARN (2022), One UN Climate Change Learning Partnership, https://unccelearn.org.
[47] UNEP-REGATTA (2022), Vulnerabilidad, impacto y adaptación - UNEP-REGATTA, https://cambioclimatico-regatta.org/index.php/es/vulnerabilidad.
[16] UNFCCC (2022), National Adaptation Plans, https://www4.unfccc.int/sites/NAPC/Pages/national-adaptation-plans.aspx.
[22] UNFCCC (2022), National focal points, UN Climate Change, https://unfccc.int/process/parties-non-party-stakeholders/parties/national-focal-point.
[26] UNFCCC (2016), Report of the Subsidiary Body for Scientific and Technological Advice on its forty-fourth session, held in Bonn from 16 to 26 May 2016. No. FCCC/SBSTA/2016/2.
[15] UNFCCC (2011), Report of the Conference of the Parties on its sixteenth session, held in Cancun from 29 November to 10 December 2010. Addendum: Part Two: Action taken by the Conference of the Parties at its sixteenth session. No. FCCC/CP/2010/7/Add.1., https://unfccc.int/resource/docs/2010/cop16/eng/07a01.pdf#page=4.
[58] UNFCCC (2007), “Vulnerability & Adaptation,” Non Annex I Training Package (CD ROM), https://unfccc.int/resource/cd_roms/na1/v_and_a/.
[12] Vicedo-Cabrera, A. et al. (2021), “The burden of heat-related mortality attributable to recent human-induced climate change”, Nature Climate Change, Vol. 11/6, pp. 492-500, https://doi.org/10.1038/s41558-021-01058-x.
[78] WHO (2022), “Estimated number of malaria cases”, The Global Health Observatory. Explore a world of health data, World Health Organization, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/estimated-number-of-malaria-cases.
[28] WHO (2022), “Indicators index”, The Global Health Observatory, World Health Organization, https://www.who.int/data/gho/data/indicators/indicators-index.
[107] WHO (2022), “National Health Emergency Framework (IHR SPAR)”, The Global Health Observatory, World Health Organization, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/national-health-emergency-framework.
[86] WHO (2022), “NHA Indicators”, Global Health Expenditure Database, World Health Organization, https://apps.who.int/nha/database/ViewData/Indicators/en.
[75] WHO (2022), “Number of confirmed malaria cases”, The Global Health Observatory, World Health Organization, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/number-confirmed-malaria-cases.
[76] WHO (2022), “Number of suspected malaria cases”, The Global Health Observatory, World Health Organization, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/number-of-suspected-malaria-cases.
[72] WHO (2022), “Surveillance (IHR SPAR)”, The Global Health Observatory, World Health Organization, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/surveillance-ihr-spar.
[51] WHO (2021), Adaptation Action Coalition Health Launch: Building climate resilient health systems, World Health Organization, https://www.who.int/news-room/events/detail/2021/05/06/default-calendar/adaptation-action-coalition-health-launch.
[17] WHO (2021), Health in National Adaptation Plans: Review, World Health Organization, https://apps.who.int/iris/handle/10665/340915.
[20] WHO (2021), WHO global strategy on health, environment and climate change: the transformation needed to improve lives and well-being sustainably through healthy environments, World Health Organization, https://apps.who.int/iris/handle/10665/358754.
[19] WHO (2021), WHO health and climate change global survey report, World Health Organization, https://apps.who.int/iris/handle/10665/348068.
[95] WHO (2020), “Existence of a universal access telephone number for pre-hospital care”, The Global Health Observatory, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/existence-of-a-universal-access-telephone-number-for-pre-hospital-care.
[42] WHO (2018), Communicating risk in public health emergencies, World Health Organization, https://apps.who.int/iris/handle/10665/259807.
[111] WHO (2015), Implementing the European Regional Framework for Action to protect health from climate change, World Health Organization, Regional Office for Europe, https://apps.who.int/iris/handle/10665/162057.
[5] WHO (2015), Operational framework for building climate resilient health systems, World Health Organization, https://apps.who.int/iris/handle/10665/189951.
[13] WHO (2010), Monitoring the Building Blocks of Health Systems: A handbook of indicators and their measurements strategies, World Health Organization, https://apps.who.int/iris/handle/10665/258734.
[45] WHO (2008), Health information systems: Toolkit on monitoring health systems strengthening, World Health Organization, https://www.who.int/publications/m/item/health-information-systems.
[27] WHO (2008), Protecting health in Europe from climate change, World Health Organization, Regional Office for Europe, https://apps.who.int/iris/handle/10665/107262.
[14] WHO (2007), Everybody’s Business: Strengthening health systems to improve health outcomes: WHO’s Framework for action, World Health Organization, https://apps.who.int/iris/handle/10665/43918.
[63] WHO and WMO (2012), Atlas of health and climate, World Health Organization, https://apps.who.int/iris/handle/10665/76224.
[8] WMO (2022), State of the Climate in Latin America and the Caribbean 2021, World Metereological Organization, https://public.wmo.int/en/our-mandate/climate/wmo-statement-state-of-global-climate/LAC.
[41] World Bank (2022), From Climate Science to Action, https://www.coursera.org/learn/climate-science.
[98] World Bank (2022), Individuals using the Internet (% of population), https://data.worldbank.org/indicator/IT.NET.USER.ZS.
[117] World Bank (2022), World Bank Group Delivers Record $31.7 Billion in Climate Finance in Fiscal Year 2022, https://www.worldbank.org/en/news/press-release/2022/09/07/world-bank-group-delivers-record-31-7-billion-in-climate-finance-in-fiscal-year-2022.
[103] World Bank (2021), Digital Health Assessment Toolkit Guide, World Bank, https://doi.org/10.1596/36547.
[87] World Bank (2017), Climate-Smart Healthcare: Low-Carbon and Resilience Strategies for the Health Sector, http://hdl.handle.net/10986/27809.
[94] Wray, C. et al. (2022), “Assessing the Impact of a Pre-visit Readiness Telephone Call on Video Visit Success Rates”, Journal of General Internal Medicine, Vol. 38/1, pp. 252-253, https://doi.org/10.1007/s11606-022-07627-w.
[3] Yglesias-González, M. et al. (2022), “Code Red for Health response in Latin America and the Caribbean: Enhancing peoples’ health through climate action”, The Lancet Regional Health - Americas, Vol. 11, p. 100248, https://doi.org/10.1016/j.lana.2022.100248.