Implementing and sustaining policies that simultaneously improve mental health and well-being outcomes require resources, incentives and working arrangements that enable all relevant stakeholders to contribute to the shared goal of tackling the social, economic, relational and environmental determinants of mental health upstream. Using key characteristics of well-being policy practice, this chapter reviews how selected mental health initiatives across the OECD have been aligning action across government agencies; redesigning policy formulation to address the joint determinants of mental health; refocusing efforts towards the promotion of positive mental health; and connecting with societal stakeholders beyond government, including those with lived experience, youth, civil society and researchers. Cross-cutting lessons point to the importance of clearly defining mental health goals, allocating sufficient time and resources to build partnerships, using strategic grantmaking to fund non-health activities, and systematically building in provisions for evaluation.
How to Make Societies Thrive? Coordinating Approaches to Promote Well-being and Mental Health

5. Realigning, redesigning, refocusing and reconnecting for better outcomes: Practical lessons
Abstract
The previous three chapters of this report have highlighted the strong interlinkages between people’s mental health and their experiences in other components of their economic, social, environmental and relational well-being. An extensive body of literature shows the important role that different government agencies, beyond health, have in improving population mental health alongside the other well-being outcomes that fall within their policy remit. The wide range of possible “win-win” policy examples that are showcased in Chapters 2-4, and that in some cases have already been put in place in OECD countries, exemplify the potential for such co-benefits.
However, despite their potential, systematically implementing such win-win policies is often difficult in practice. The mental health policy arena may be particularly challenging, in that better integrating service provision and tackling the social, economic and relational determinants of mental health upstream, require continuous cross-agency collaboration. Indeed, while almost three-quarters of countries responding to the OECD Mental Health Benchmarking Policy Questionnaire in 2020 reported having in place national programmes or strategies for integrated and cross-governmental approaches to mental health governance, there is room for improvement (OECD, 2021[1]). A recent review of progress made five years after the adoption of the 2015 OECD Recommendation on Integrated Mental Health, Skills and Work Policy, which focuses on the key areas of health care, youth support and education, workplace and welfare policy, found that OECD countries continue to see not only mental health treatment but also mental health prevention and promotion as first and foremost an issue for the health system (OECD, 2021[2]). Indeed, up to now integration with other sectors, particularly when it comes to linking mental health with welfare and employment services, is limited and often not scaled (OECD, 2021[2]). There tends to be even less systematic integration when it comes to other areas that impact mental health – beyond the key domains addressed in the Recommendation – such as the environment (see Chapter 3), neighbourhood design (see Chapters 2, 3 and 4), social connectedness, safety or work-life balance (see Chapter 4).
Successful strategy and policy formulation and implementation hence need to be supported by a broader ecosystem that provides resources, incentives and working arrangements that enable all relevant stakeholders to contribute to the shared goals of tackling the determinants of mental health upstream. To illustrate some of the challenges and opportunities of integrated approaches to mental health policy, following the characteristics of well-being policy approaches more generally (Box 5.1), this chapter examines nine different initiatives from eight OECD countries as case studies, with information gathered from mid-2022 until early 2023 (Table 5.1).1
The case studies vary in terms of focus: some include an overarching mental health strategy (e.g. in Sweden and Finland), others centre on an agency focusing on mental health and well-being (e.g. in New Zealand), and some concern specific programmatic activities (e.g. in Canada, Norway, Western Australia, and for the Act Belong Commit Programme). The findings of this chapter hence do not reflect a comprehensive stocktake that is representative of all OECD countries or of the included countries’ entire mental health portfolio, nor do they imply that there are no interesting approaches elsewhere.
In addition, the evidence base on the impact of the initiatives varied widely. In some cases, extensive evaluations including in peer-reviewed journals were published, while other initiatives were only launched at the time of writing this report and their inclusion here is based more on what has not worked well in previous strategies. Furthermore, since the case studies do not represent individual interventions (but rather supporting mechanisms that enable the programmes listed as examples in the previous chapters), they have not been subject to a typical best-practice evaluation for public health interventions (OECD, 2022[3]). Nevertheless, the experiences of these initiatives point to useful insights about the different elements of policy ecosystems that can help realise well-being and mental health co-benefits. They hence enlarge the evidence base on how countries are trying to align mental health action across government agencies; design policy formulation to address the joint determinants of mental health; refocus efforts towards the promotion of positive mental health; and connect with societal stakeholders beyond government, including those with lived experience, youth, civil society and researchers.
Table 5.1. Selected mental health initiatives featured as case studies
|
Initiative |
Country |
Agencies interviewed |
|---|---|---|
|
Act Belong Commit (the ABCs of mental health) Programme |
Australia (Western Australia), Denmark, Faroe Islands, Finland, Norway |
Trøndelag Public Health Alliance in Norway; Finnish Institute for Health and Welfare; Board of Public Health in the Faroe Islands; Copenhagen University |
|
Western Australian Mental Wellbeing Guide |
Australia (Western Australia) |
Western Australia Mental Health Commission |
|
Mental Health Promotion Innovation Fund & Positive Mental Health Surveillance Indicator Framework |
Canada |
Health Canada; Public Health Agency of Canada |
|
National Mental Health Strategy and Programme for Suicide Prevention 2020-30 |
Finland |
Finland Ministry of Social Affairs and Health, Finnish Institute for Health and Welfare, MIELI Mental Health Finland |
|
Mental Health and Wellbeing Commission (Te Hiringa Mahara) |
New Zealand |
New Zealand Mental Health and Wellbeing Commission (Te Hiringa Mahara) |
|
Programme for Public Health Work in Municipalities |
Norway |
Norway Directorate of Health |
|
Upcoming National Policy for Mental Health and Suicide Prevention |
Sweden |
Public Health Agency of Sweden |
|
Public Service Boards & the North Wales Public Service Lab and Insight Partnership |
Wales |
Flintshire and Wrexham Public Services Board, Wrexham University |
Box 5.1. Characteristics of well-being policy approaches applied to mental health
In recent years, practitioners in the field of public health have increasingly emphasised its role as provider of public goods to society more broadly, highlighting its important contributions to and interlinkages across sectors such as education, employment and social participation. This approach has also been conceptualised as moving away from a reactive focus on reducing disease, towards the proactive promotion of good well-being outcomes and new collaborative ways of working jointly with other departments, stakeholders and citizens (Table 5.2) (Von Heimburg et al., 2022[4]).
Table 5.2. Moving from a traditional public health approach to a well-being approach
Assumptions, practices and roles in framing public goods as well-being
|
Traditional public health |
Well-being |
|
|---|---|---|
|
Assumptions |
||
|
Goals |
Reduce incidence and prevalence of disease |
Promote well-being for all |
|
Scope |
Physical and mental health |
Multiple domains of well-being |
|
Responsibility |
Health sector |
All sectors |
|
Function of power and privilege* |
Invisible |
Visible |
|
Practices |
||
|
Capabilities |
Deficit orientation |
Strength orientation |
|
Ecological focus |
Individual |
Community |
|
Timing of interventions |
Reactive |
Proactive |
|
Disciplinary approach |
Health and epidemiology |
Transdisciplinary |
|
Roles |
||
|
Role of citizen |
Passive recipient of services |
Co-creators of public good |
|
Role of professionals |
Experts |
Facilitators |
|
Role of settings and institutions |
Service providers |
Arenas for co-creation of public good |
|
Role of government |
Fund health sector |
Convene and coordinate all sectors |
Source: Von Heimburg et al. (2022[4]), “From public health to public good: Toward universal wellbeing”, Scandinavian Journal of Public Health, Vol. 50, Issue 7, pages 1062-1070, https://journals.sagepub.com/doi/10.1177/14034948221124670.
Note: * This point both acknowledges the role different power structures, including structural discrimination, play in determining health outcomes, and views citizens as active, resourceful contributors to society.
The OECD has previously summarised well-being policy approaches in terms of four “R’s”: realigning policy practice across government silos, redesigning policy content from a more multidimensional perspective, refocusing policies towards the outcomes that matter most to people, and reconnecting people with the public institutions that serve them (OECD, 2021[5]). For this report, these principles have been adapted to reflect the goals of population mental health prevention and promotion strategies, and to point out the common challenges and success factors for achieving them (Figure 5.1).
Figure 5.1. Principles of well-being policy approaches in the case of mental health
|
REALIGN: WHOLE-OF-GOVERNMENT APPROACH |
REDESIGN: WELL-BEING DETERMINANTS FOR PREVENTION AND PROMOTION |
REFOCUS: EMPHASIS ON POSITIVE MENTAL HEALTH |
RECONNECT: BUILDING BROAD PARTNERSHIPS |
|---|---|---|---|
|
Involve collaborations across multiple government departments |
Reflect the (joint) social, economic, environmental and relational determinants of mental health in policy content |
Both address deprivations in mental health and promote human flourishing |
Collaborate with people with lived experience, communities and non-governmental actors |
5.1. Realign: Whole-of-government approach
Many (mental) health inequities are influenced by policies outside of the health sector, and it has long been recognised that intersectoral collaboration is needed to tackle them. Indeed, such efforts have often been described as Health in All Policies (HiAP), meaning that health considerations are systematically integrated into policymaking across sectors, alongside other objectives (CDC, 2016[6]; WHO, 2013[7]). Examples of existing coordination mechanisms between mental health and non-health sectors include joint service planning (often through inter-departmental coordinating committees or advisory groups); single multi-agency care plans; formal interagency collaborative agreements; joint training or cross-training of mental health and other staff to ensure shared understanding; sharing of information systems; blended funding initiatives; and joint service provision through multidisciplinary, multi-agency teams (Whiteford et al., 2014[8]; Diminic et al., 2015[9]).
However, turning a whole-of-government approach into reality, and sustaining it over time, is not easy. HiAP has often remained unrealised in practice, partly because the asymmetry built into the concept makes coalition-building difficult: it has often focused on wins for the health sector and often seems to imply that other sectors should adjust their priorities accordingly (National Collaborating Centre for Healthy Public Policy, 2022[10]; WHO and European Observatory on Health Systems and Policies, 2023[11]; Lundberg, 2020[12]). Indeed, a review of how municipal governments in Denmark, Norway and Sweden (all of which prioritised an HiAP approach over the last decade) implemented HiAP points to challenges related to insufficient political commitment to health equity goals outside of the health sector and inadequate budgetary prioritisation (Scheele, Little and Diderichsen, 2018[13]). In addition – in many countries and not limited to health topics – inter-departmental groups and task forces can be time-limited, tend to have no formal authority over other departments, and, without proper resourcing, rely on motivated individuals (outside of their day job) rather than formalised structures to push forward a collaborative agenda (Mondal, Van Belle and Maioni, 2021[14]; Fujisaki et al., 2016[15]; Karré, Van der Steen and Van Twist, 2013[16]; Kokkinen et al., 2017[17]; Tooher et al., 2016[18]).
Broader multidimensional frameworks can provide the mandate for agencies to contribute to common goals
One way to engage other sectors in promoting (mental) health outcomes and to strenghten their ownership over these topics is to emphasise broader, shared concepts such as sustainability and well-being. The various multidimensional well-being frameworks developed across OECD countries can provide a common understanding of the wide range of outcomes that matter to people (see Figure 5.2 for the OECD Well-being Framework as an illustration). This can be a starting point to support alignment across government departments towards objectives for which they share joint responsibility, and since outcomes right across government are included, it can resonate more strongly with a wider range of internal stakeholders compared to a narrower focus on health equity (Scheele, Little and Diderichsen, 2018[13]; OECD, 2023[19]).2
Figure 5.2. The OECD Well-being Framework
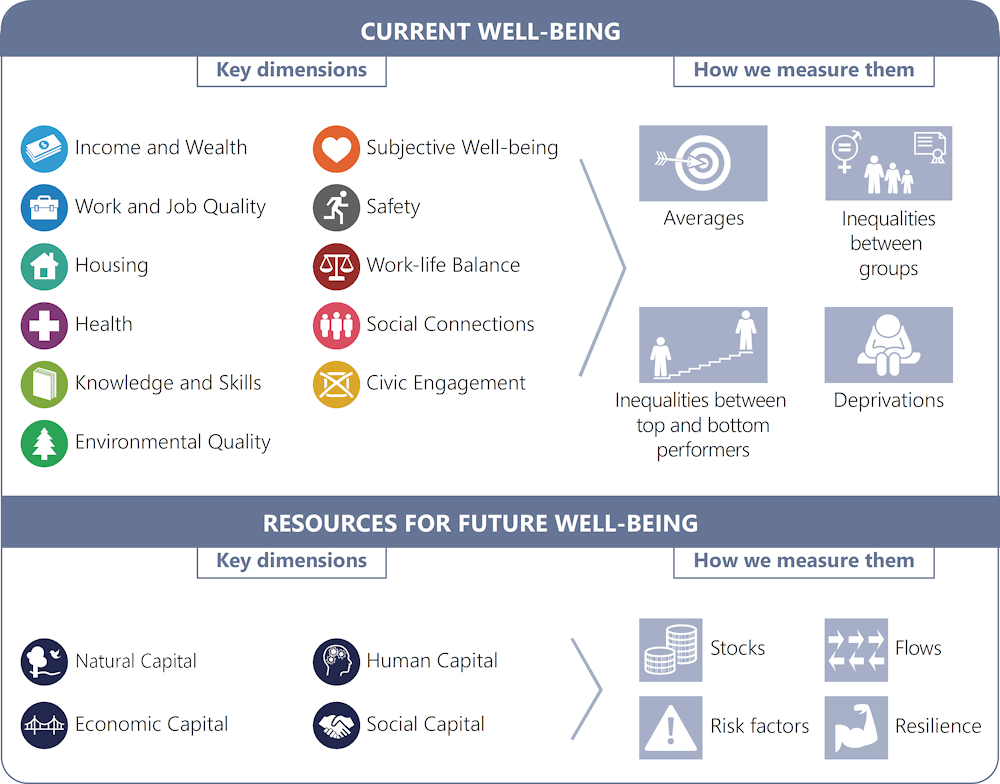
Source: OECD (2020[20]), How’s Life? 2020: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/23089679.
Anchoring such well-being frameworks in legislation has provided incentives for new, long-term ways of working together. For instance, in Wales, the 2015 Wellbeing of Future Generations Act sets out seven national well-being goals (encompassing health but also prosperity, resilience, equality, cohesion, culture/language and global responsibility). The Act requires public bodies to consider the long-term impact of their decisions, to work more closely with the public, communities and each other, and to address persistent problems such as poverty, health inequalities and climate change (Future Generations Commissioner for Wales, 2023[21]).3 Under this Act, each local authority established a Public Services Board (PSB) to improve joint work across all public services; each PSB has a member from the local health board alongside other authorities. In some cases, the PSBs have joined together across local authorities to realise the benefits of subregional and regional collaboration. The boards must carry out a well-being assessment, outlining the state of different aspects of well-being and expected future trends in the local area, which is then used to support a local well-being plan (formulated every five years) that sets out how PSBs will meet their responsibilities under the Act (Welsh Government, n.d.[22]; The Future Generations Commissioner for Wales, 2023[23]).
Oftentimes, mental health, and its connection to other areas of public policy, is identified as a priority area in both well-being assessments and plans. For instance, the Wrexham County Borough 2022 Well-being Assessment highlighted that access to the natural environment is associated with positive mental health outcomes, and that almost 20% of children aged 10+ in North Wales experience mental health problems (higher than the Welsh average of 14%) (Wrexham PSB, 2022[24]). Accordingly, the resulting 2023-28 Well-being Plan of the Flintshire and Wrexham Public Services Board agreed to “innovate with communities to build good mental health and wellbeing” as one of its six well-being priorities (Figure 5.3). The overarching well-being objectives under the Welsh Future Generations Act have thus facilitated a regular space for collaboration and coordination among public bodies, rather than setting up multiple inter-departmental task forces (e.g. on substance use, on suicide, on mental health) that can face overlapping issues and similar upstream determinants.
Figure 5.3. Example of well-being outcomes and objectives, including mental health, in a Public Services Board Well-being Plan in Wales
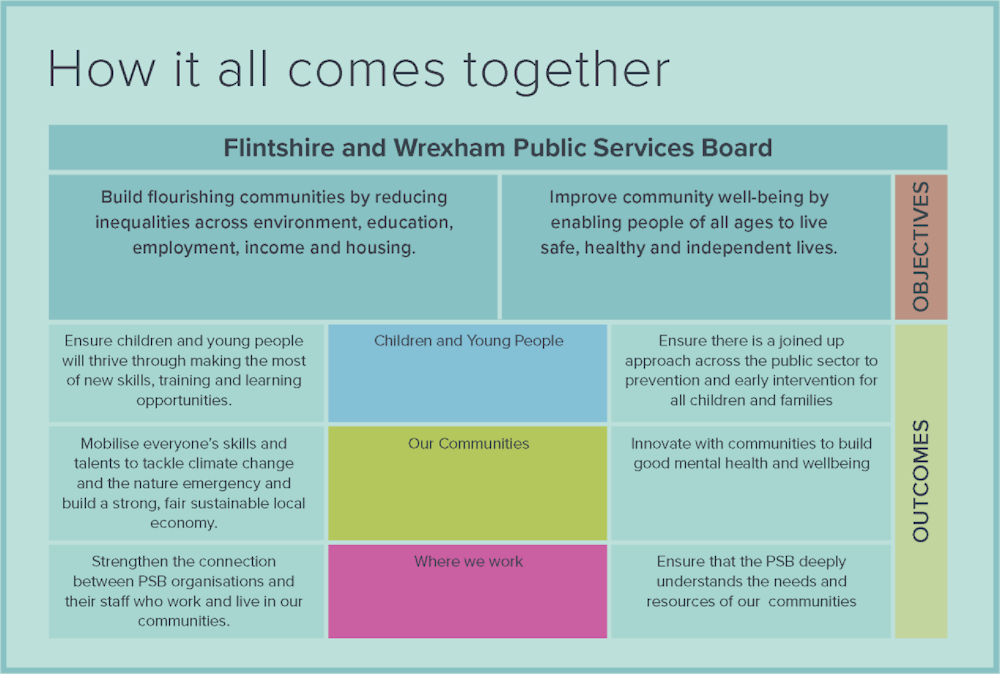
Source: Flintshire and Wrexham Public Services Board (2023[25]), Flintshire and Wrexham’s Wellbeing Plan 2023-2028, https://www.wrexhampsb.org/well-being-assessment/.
Also in cases where HiAP remains the central guiding principle, a recognised broader framework can provide non-health agencies with an official mandate (and thus the agency) to engage with health goals. Sweden’s Parliament endorsed a national public health policy in 2018, stating that “public health is a shared responsibility for all sectors at all levels” (Folkhälsomyndighete, 2021[26]). The policy’s eight target areas reflect the multidimensionality also inherent in many well-being frameworks, and highlight the social determinants of health (conditions in early life; knowledge, skills, and education/training; work, working conditions, and work environment; income and economic resources; housing and neighbourhood conditions; health behaviours; control, influence, and participation; an equitable and health-promoting health and medical service) (Figure 5.4). It also covers cross-cutting areas of focus, including human rights, national minorities, disability policy, child and youth rights policy, equality and discrimination policy.
Figure 5.4. The eight target areas of the Swedish public health policy

Source: Folkhälsomyndighete (2021[26]), Towards a Good and Equitable Health, Public Health Agency of Sweden, https://www.folkhalsomyndigheten.se/contentassets/bb50d995b033431f9574d61992280e61/towards-good-equitable-health.pdf.
Sweden is currently in the process of creating a new national strategy on mental health and suicide prevention. In doing this, the Ministry of Health and Social Affairs requested that the new strategy comprehensively address the need for “good, equal and gender-equitable mental health for the entire population” and be based on the national public health policy framework (Folkhälsomyndighete, 2020[27]; 2023[28]; Becker, 2023[29]). In this way, the framework was instrumental in bringing together 26 delivery agencies in 2020, under the lead of the National Board of Health and Welfare and the Swedish Public Health Agency, to draft a proposal for a strategy with goals, priorities and indicators for follow-up.4 The proposal, titled “It’s about life”, was submitted to the Ministry of Health and Social Affairs in September 2023 for consideration and eventual adoption (Folkhälsomyndighete, 2023[30]). By contrast, the previous Government’s Strategy for Mental Health 2016-20, while also emphasising the importance of whole-of-society approaches to population mental health promotion and prevention,5 was created before the establishment of the national public health policy framework and did not include clearly assigned areas of responsibility and targets (by government) for agencies. In retrospect, this led to a certain lack of ownership and engagement in several national agencies, and external evaluators have noted that it left especially regional and municipal governments with the responsibility for addressing the structural determinants of mental health (Fjellfeldt, 2023[31]; Becker, 2023[29]). In addition, a government inquiry strongly recommended that more comprehensive intersectoral efforts were needed to develop the 2016-20 Strategy’s follow-up in order to achieve sustainable progress on mental health (Government of Sweden, 2019[32]).
Implementation plans that address intersectoral collaboration, alongside performance evaluation metrics, can concretely support delivery
The high-level mental health strategies published by government departments often focus on the overall vision and opportunities for synergies, without explicitly spelling out the steps needed for their implementation and roll-out at the delivery level. Aspects such as funding and accountability, or plans for the monitoring and evaluation of partnerships, can also be absent from high-level strategy-setting documents (Diminic et al., 2015[9]). In some of the case studies, such as in Finland, these aspects have been or are planned to be supported by separate implementation plans.
In Finland, the current National Mental Health Strategy and Programme for Suicide Prevention was passed in February 2020, to cover the ten-year period ending in 2030 (Ministry of Social Affairs and Health, 2020[33]). The plan is housed in the Ministry of Social Affairs and Health but also involves nine other ministries.6 To facilitate inter-agency cooperation, an Interministerial Cooperation Group meets multiple times a year to foster cross-ministry connections and workshop how each could contribute to the promotion of mental health and well-being (the National Strategy does not provide lines of funding to different government agencies to develop programmes that touch on mental health). In order to support the implementation of the Strategy, a separate Draft Resolution on Mental Health Promotion was published in 2023, concretely outlining planned cross-cutting measures for mental health promotion and suicide prevention for 2023-27, and how these are reflected in the strategies and programmes of other ministries (Ministry of Health and Social Affairs, 2023[34]).7 The Draft Resolution will be updated in line with the forthcoming Government Programme (following a change in the Finnish Government in April 2023), and then lead to a separate implementation plan.
In addition, Finland has made the process of intersectoral collaboration itself an explicit goal of mental health policy. The National Mental Health Strategy and Programme for Suicide Prevention has five priority areas, which include: (1) mental health as a capital, (2) the mental health of children and young people, (3) mental health rights, (4) services to effectively meet all peoples’ needs and (5) good (integrated) management of mental health (Ministry of Social Affairs and Health, 2020[33]). While the first four priority areas capture improved mental health outcomes and service delivery, the fifth, “good management”, focuses specifically on the ability to effectively implement the strategy across administrative sectors and levels of government. Measures taken under this area, and also outlined in the Draft Resolution on Mental Health Promotion, include the development of mental health impact assessments (see section on “redesign” below), and regular assessments of municipal performance in promoting well-being and health, focusing on preconditions for effective management (Table 5.3). In addition, the good management priority of the National Strategy highlights that “models for inter-agency collaboration will be developed, describing the role of actors, cost-sharing and management of activities” (Ministry of Social Affairs and Health, 2020[33]).
Table 5.3. Areas of assessment for municipal management performance in health and welfare promotion in Finland
Health promotion capacity building framework (TEA)
|
Indicator |
Details |
|---|---|
|
Commitment |
The organisation's commitment to health and welfare promotion based on strategy documents as well as the use of national programmes |
|
Management |
How health and welfare promotion are organised, defined and implemented |
|
Monitoring and needs assessment |
How health and welfare determinants in the population are monitored, how the needs of different population groups are assessed and how the results are reported to the management and elected officials |
|
Resources |
The resourcing of health and welfare promotion based on staffing types and skills |
|
Participation |
Residents' opportunities to take part in development and assessment of activities |
Note: Indicators are scored from 0 (low result) to 100 (high result) for each municipality. Information is collected every two years.
Source: THL (2023[35]), Health and Welfare Promotion, Finnish Institute for Health and Welfare, https://thl.fi/en/web/thlfi-en/statistics-and-data/statistics-by-topic/health-and-welfare-promotion.
Successful cross-sectoral collaboration requires sufficient resources, but can facilitate participation and relationship building
Despite the increasing awareness of the importance of mental health and its economic and societal costs, mental health policies have historically seen a chronic shortage of investment. For instance, among OECD countries for which data are available, mental health spending as a proportion of total health spending largely remained unchanged between 2009 and 2019, when it stood at just under 7% – even though the costs of mental ill-health are estimated at more than 4% of GDP across the OECD (OECD, 2021[1]). While some OECD members, such as Australia, Austria, Canada, Chile, Latvia, Lithuania and the United Kingdom announced new funding for mental health care in response to the COVID-19 pandemic, this was not the case for most countries (OECD, 2023[36]).
Constraints on resources are also among the most commonly cited barriers to intersectoral linkages between mental health and other sectors (Whiteford et al., 2014[8]). Indeed, the OECD has previously highlighted the key role that financial incentives can play in encouraging stakeholders to develop more integrated mental health strategies and services, and the need for budgets to be allocated to ministries other than health (OECD, 2021[2]). However, responses to the 2020 OECD Mental Health Benchmarking Policy Questionnaire showed that most countries do not have such non-health budgets in place (and many countries had difficulty in identifying whether a dedicated mental health budget existed) (OECD, 2021[1]). A systematic review of mental health policy documents from jurisdictions in Australia, New Zealand, the United Kingdom, Ireland and Canada also found there to be little discussion of intersectoral financing arrangements at the strategy stage; and an accompanying report in support of the upcoming Irish Mental Health Promotion Plan stressed that while cross-sectoral integration will increase value for money and reduce erroneous spending, commitment in terms of additional investment and resources is crucial if implementation success (Diminic et al., 2015[9]; Barry, Keppler and Sheridan, 2023[37]).
Providing resources to all delivery agencies can support deeper engagement and commitment, as is shown by the development of the aforementioned proposal for the new national strategy on mental health and suicide prevention in Sweden. The drafting of the proposal was jointly led by the National Board of Health and Welfare and the Swedish Publish Health Agency and involved 24 additional agencies. While coordinated approaches are not new in Sweden, it is rare that over twenty agencies have been tasked with policy co-development. For each of the three years of the development phase, the government provided SEK 5 000 000 (around USD 480 000) to each of the two lead agencies, and SEK 1 000 000 (around USD 98 000) to all the other participating agencies to fund their involvement in strategy development. The funding was used flexibly depending on each agency’s needs; some (especially larger) agencies used the funds to pay internal staff costs, while others hired external consultants to drive this work.
Beyond funding, time to develop partnerships is another essential resource for collaboration. The time provided for co-development in Sweden – three years from 2020-23 – was viewed as an unusually long process by participants, but allowed for co-creation and exploratory idea development (Becker, 2023[29]). The first deliverable each agency was tasked with submitting was an analysis of the current relationship of mental health to their area of expertise, along with what they anticipate as long-term needs (Folkhälsomyndighete, 2020[27]).8 During the first year, meetings between the 26 agencies were held on a monthly basis and primarily consisted of knowledge sharing. As the strategy development continued, the work became more open and less prescriptive, as no pre-defined roles were given to agencies beyond the two leads. The flexibility of this co-creative process was perceived by participants to be at times difficult, especially given the number of views in the room, but also allowed for new perspectives to be developed.9
This exercise revealed how little agencies knew about one another’s work and ways of operating. In fact, many participants perceived the collaborative implementation process to be even more important than the actual content discussed and understood this assignment as a potential foundation for more cooperation in the future (Becker, 2023[29]). It is too early to judge whether such an extensive collaborative exercise is realistic for frequent or time-sensitive policymaking needs in the future, and what will happen to the recommendations in the draft proposal after submission to the Ministry of Health and Social Affairs. However, this experience points to the importance of continuously investing in building intersectoral relationships and trust, to start shifting (often hierarchical) organisational cultures to open learning (Mondal, Van Belle and Maioni, 2021[14]).
Independent oversight agencies and funding for broader well-being activities at the local level represent new models for realigning
Several case studies are employing models for realigning across government that go beyond the more traditional examples of joint service provision and interagency task forces. These include creating independent agencies to evaluate the efforts of other stakeholders, and redirecting funding to support broader mental health and well-being activities at the local level.
A model for creating a separate body to assess progress on mental health and well-being, and relevant efforts across sectors has been established in New Zealand through the Mental Health and Wellbeing Commission (Te Hiringa Mahara). The Commission, established in 2021 as an independent crown entity, provides system oversight on activities related to mental health and well-being and plays an advocacy role of amplifying community voices in policy processes (Mental Health and Wellbeing Commission, 2022[38]).10 The Mental Health and Wellbeing Commission has four main strategic priorities: (1) advancing mental health and well-being outcomes, (2) achieving health equity, with a special focus on priority populations, (3) advocating for a people-centred mental health and addiction service system, and (4) addressing the wider determinants of well-being. These goals are supported by workstreams on monitoring and reporting, and advocacy and engagement. While the Commission does not itself implement or fund mental health programmes, it serves as a watchdog that comments on both the activities of agencies tasked with providing mental health and addiction services and the population-level outcomes these policies are designed to target, by providing publicly available reporting on trends and strategies, by advocating for improvement and by placing relevant issues in the public debate.
The Commission’s monitoring reports have so far focused on publicly funded mental health and addiction services. Since one of the Commission’s strategic priorities is to address the wider determinants of well-being, it not only monitors services but has also built relationships with other commissions and government agencies – including the Ministry of Business, Innovation and Employment; the Ministry of Social Development; the Ministry of Justice; and the Ministry for Children (Oranga Tamariki). It should be noted, however, that other government agencies are not mandated to respond to the Commission’s recommendations. In addition, despite its broad remit for system oversight, its funding is relatively small.11
An interesting model for vertical realignment (i.e. between different levels of government) for mental health comes from the Norwegian Ministry of Health and Care Service’s Programme for Public Health Work in Municipalities. Vertical coordination is particularly relevant for countries in which local governments hold principal responsibility for public health implementation, as is the case in several Scandinavian countries that are following an HiAP approach. Indeed, insufficient vertical support and lack of alignment between the national, regional and local levels have been cited as some of the challenges of implementing HiAP in practice (Scheele, Little and Diderichsen, 2018[13]).
The Programme for Public Health Work in Municipalities is a 10-year strategic grantmaking initiative, launched in 2017 by the Ministry of Health and Care Services, the Norwegian Directorate of Health, the Norwegian Institute of Public Health and the Norwegian Association of Local and Regional Authorities (KS). Coordinated by the Directorate of Health, the Programme’s main goal is to increase the capacity of municipalities to establish systematic and long-term public health work that promotes mental health and prevents substance abuse among children and adolescents.12 It provides funding for innovative projects in municipalities that are based on local needs assessments and the involvement of the local population (Helsedirektoratet, 2023[39]). Funds are provided by the Norwegian Directorate of Health to county governments, who run their own competitive process to award municipality proposals. The selection process is overseen by regional advisory boards, which vary county by county, but typically comprise university and research actors, members from NGOs, youth council representatives and municipality stakeholders themselves.
Aside from the Programme’s engagement with different levels of government, it is innovative in various other ways: for instance, it pooled existing smaller government grants on mental health into a larger fund, and followed calls from the KS to move away from short-term, one year projects. In its first year, the Programme distributed grants totalling NOK 42 million (around USD 4 million); it gave out NOK 70 million (around USD 6.5 million) in the second year, and it has budgeted NOK 77 million (around USD 7 million) for grants every year since 2019. Each initiative is funded for over one year, but for less than five years, to strike a balance between effective long-term planning and enabling more agile policy making to better respond to evolving constituent needs. Indeed, a 2022 mid-term evaluation of the Programme found that municipalities singled out the long-term nature of the programme as an important success factor (Gotaas, Bergsli and Danielsen, 2022[40]).
The Programme employs an open definition of “innovation” – the only criteria being that projects must have a universal focus13 and be a new activity, or extend an existing activity to a new target group or a new setting within the municipality. This has allowed municipalities to use funds flexibly in accordance with their needs, which in many cases has meant that funding has been allocated to activities that would not have fallen under the traditional remit of health (e.g. school or kindergarten-based programmes, increasing participation in recreational activities, creating public meeting spaces, developing integrated welfare services for parents with financial difficulties, funding activities strengthening youth participation such as youth councils).
Lastly, the Programme has provided a platform for learning for what works by enabling and expanding knowledge sharing between municipalities (which often do not have broad oversight over what their counterparts are doing in other parts of the country). Both the county governments and the Directorate of Health have served as a conduit for different local actors to learn from one another’s innovations and adapt successful projects from other municipalities to their own local context (e.g. by organising a series of meetings and webinars on local public health work, and by launching a web portal featuring all funded projects) (Helsedirektoratet, 2021[41]). In addition, knowledge sharing has also been enabled to some degree with researchers – while there was no specific budget line provided for project evaluation, municipalities are required to document their initiatives and encouraged to collect impact data on interventions. In some cases, this led to increased collaboration with universities (see section on “reconnect” below).
Evaluations of the overall Programme’s outcomes so far have been positive. An initial survey commissioned by the Directorate of Health was conducted at the start to provide a baseline for mental health outcomes for children and young people in Norway, as well as for existing efforts at the municipal level to improve well-being, prevent mental ill-health, and diminish drug and alcohol use (Helgesen, Abebe and Schou, 2017[42]). The baseline report found that just under 20% of youth across municipalities reported feeling lonely in the past month and close to 13% reported symptoms of depression. 72% of municipalities reported that they had established cross-sectoral groups to address public health issues, showing that prior to the Programme’s implementation there were some coordination channels in place. A mid-term evaluation in 2022 (which focused on ways of working in the municipalities rather than repeating the baseline outcomes survey) provided an overall positive assessment: the Programme had increased collaborative relationships and municipalities' competencies for public health work (Gotaas, Bergsli and Danielsen, 2022[40]). Indeed, almost all of the municipalities surveyed stated that the initiative has led to them to conduct activities that they would not have prioritized within ordinary operations, and many felt that they would integrate these into existing workstreams after the grant period ended. Recommendations for further improvement included strengthening the role of counties as intermediaries between the Directorate of Health and municipalities; providing municipalities with greater support and training in research design; better engagement with municipalities that have not yet voluntarily participated in the programme; and acknowledging and addressing tensions between the need to implement evidence-based policies (the evaluations of which take significant time and resources) and the desire to roll out new, innovative programmes (which may be so novel as to not have as robust an evidence base) (Gotaas, Bergsli and Danielsen, 2022[40]).14
5.2. Redesign: Well-being determinants for mental health prevention and promotion
In contrast with “realign”, redesigning refers not to cross-government collaboration per se, but to how the development of policy content within individual government departments can better acknowledge how programmes affect people’s mental health.15 The previous three chapters, by highlighting policy examples that provide co-benefits for both mental health and well-being outcomes, have already outlined what redesigning might look like for different sectors (Box 5.2).
Box 5.2. Win-win policy examples to improve mental health and other aspects of well-being
Chapters 2-4 of this report have used the OECD’s Well-being Framework to better understand the interactions between mental health outcomes and our material conditions, quality of life factors and determinants of the quality of relationships. Each section culminates with a box outlining policy examples that address mental health and the given well-being outcome: these serve to provide evidence-based options to improve population-level outcomes, showcase existing programmes implemented by OECD countries and provide new examples on topics studies far less up to now, such as the nexus of climate change, civic engagement or social connections, and mental health.
A selection of such policy examples are listed below:
Material conditions, covering income and wealth; economic capital; work and job quality; and housing:
Increase access to social assistance programmes, while decreasing the cognitive burden of enrolment (Box 2.1)
Encourage employers to prioritise mental flourishing at work (Box 2.2)
Create supportive and inclusive neighbourhoods to promote connectedness and psychological well-being (Box 2.3)
Quality of life aspects, covering physical health; knowledge and skills; educational attainment and human capital; environmental quality and natural capital:
Better integrate physical and mental health care (Box 3.1)
Encourage physical activity to promote good mental health (Box 3.1)
Incorporate social and emotional learning into curricula (Box 3.2)
Promote life-long learning (Box 3.2)
Expand options to engage in ecotherapy and green social prescribing (Box 3.3)
Highlight the mental health costs of climate change, and the benefits of climate action, in environmental accounting and cost benefit analyses (Box 3.3)
Quality of relationships, covering safety; work-life balance; social connections and social capital; and civic engagement:
Tackle the roots of discrimination and racism (Box 4.1)
Value unpaid work (Box 4.2)
Prioritise social connectedness in policy (Box 4.3)
Ease participation and representation of those with lived experience of mental ill-health in politics (Box 4.4)
Detailed information on each policy can be found in Chapters 2 through 4; additionally, Table 1.2 provides an overview of all policies recommended in this report along with the government agencies that are involved in their design and implementation – highlighting the reach of these initiatives beyond the health sector.
Concrete examples of redesigned mental health programmes across the case studies
Each of the case studies featured in this chapter have very different structures and working processes, however all include a focus on integrated approaches to mental health policy design and implementation, resulting in redesigned programmes that target outcomes beyond mental health.
Both Canada and Norway have experimented with distributing funds to sponsor innovative programmes that approach the improvement of mental health in different ways. In Canada, the Mental Health Promotion Innovation Fund (described in greater detail in the subsequent section on “refocus”), aims to address issues related to health equity by financing community-based initiatives that support mental health (Government of Canada, 2023[43]). Examples include providing psychosocial and education support to children, especially those in families that have newly arrived in Canada (KDE Hub, 2023[44]) (see Box 3.2, for a discussion of policies to introduce socio-emotional learning skills in curricula); providing cooking, nutrition and food-focused lessons to promote healthy relationships with one’s self and one’s body, to thereby improve mental health (KDE Hub, 2023[45]) (see Box 3.1 for policies to promote healthy behaviours and more physical activity); offering arts-based mental health, sexual health and trauma-processing services, and doing so in a way that promotes cultural identity and the development of coping skills (KDE Hub, 2023[46]) (see Chapter 4 for a discussion of safety and mental health, and Box 3.2 for an illustration of how life-long learning – including courses in art and music – can improve mental health); and developing training courses for peers, parents and partnering organisations to better understand transphobia and transmisogyny, to better support trans, non-binary or gender-exploring youth (KDE Hub, 2023[47]) (see Chapter 4 for a discussion of discrimination and mental health). In Norway, the aforementioned Programme for Public Health Work in Municipalities has distributed funding to counties, which then receive applications from municipalities for their proposals for new approaches to mental health improvement. By way of example, the Kongsvinger municipality has rolled out a plan to provide loans to low-income families to ensure their children have stable housing and live in safe, clean environments. The programme does not aim just to improve housing outcomes, but by doing so, also hopes to improve the social inclusion of children and young people to enable them to participate in community events and activities, thereby improving their socio-emotional development and mental health (Forebygging, 2023[48]). In the Trondheim municipality, kindergartens have changed their initiation processes, so instead of three intense introductory days, they now host visits during parental leave in combination with a minimum of five less stressful introductory days later on, in order to better support not only children’s cognitive development but also the parents’ work-life balance (NTNU, 2023[49]).
In the case of national mental health strategies, such as in Finland, the overarching document may identify specific policies that will be funded under the national strategy. For example, the Finnish National Mental Health Strategy and Programme for Suicide Prevention 2020-30 includes Individual Placement Programmes (IPS) as a means to promote the inclusion of people experiencing mental ill-health into the labour market, and more broadly, to facilitate the social inclusion of those with mental health conditions (see Box 2.2 for a longer discussion of IPS programmes, which have been piloted in eight OECD countries thus far. Refer also to OECD (2021[2]) for more information on IPS programmes and on OECD recommendations for their implementation). The IPS programme in Finland was initially rolled out in 2020 in five regional projects, and from 2023-24 will be expanded to six new regions (THL, 2023[50]; 2023[51]). The Mental Health at Work Programme is another example of a policy implemented under the National Mental Health Strategy and Programme for Suicide Prevention 2020-30, and includes a toolkit for employers that recommends concrete steps to promote mental health at work (Finnish Institute of Occupational Health, 2023[52]). The toolkit includes a “recovery calculator” to ensure that business processes and workloads promote employee recovery and resilience, guidance for managers for building safe spaces, and advice for substance abuse programmes at the workplace (see Box 2.2 for other examples of how governments can encourage employers to prioritise mental flourishing at work).
The Public Services Boards in Wales each develop their own initiatives at a local level. One of the efforts of the Wrexham and Flintshire PSB focuses on building a community of practice around social prescribing to improve social connectedness and shore up resilience to mental ill-health (refer to Chapter 4 for a longer discussion of social connections and mental health, and Box 4.3 for policy examples relating to social prescribing). The Wrexham and Flintshire PBS have also developed an initiative called the Children’s University, in partnership with Wrexham University, to instill a love of learning in children from a young age. The programme is not school-based, but rather invites participation in extra-curricular activities including volunteering, sports, art, culture and outdoor learning (Wrexham PSB, 2022[24]; Wrexham University, n.d.[53]) (see Box 3.2 for a discussion of the importance of life-long learning for mental health, and Chapter 4 for more references on the way leisure activities and civic engagement – including volunteering – impact mental health).
The Act Belong Commit (the ABCs of mental health) Programme is a mental health promotion campaign that multiple countries have adopted – some at the national or local level – while in other countries non-governmental organisations, such as universities, have taken up the programme (see Box 5.3 for more information).16 The ABCs encourage people to do something active (Act), to do something with someone (Belong) and to do something meaningful (Commit). Some national ABC initiatives have created an activity bank to provide people with ideas for ways they can enact each of the pillars and for communal activities they can join. For example, the Faroe Islands ABC programme hosted a walking excursion for unemployed individuals, to enable them to interact with one another in nature, destress, and gain energy and inspiration from one another and the beautiful surroundings (Mentally Healthy WA, 2019[54]) (see Box 3.3 for examples of nature-based therapy, including green social prescribing). In Western Australia, ABC has been brought to the public school system through Mentally Healthy Schools: primary and secondary schools have integrated ABC messaging into classrooms, the school environment and the whole school community (Mentally Healthy WA, 2023[55]) (see Box 3.2 for school-based interventions; see also OECD (2021[1]) for more examples).
And finally, in New Zealand the Mental Health and Wellbeing Commission cannot enact policy in its own right, given its role as an independent agency, but it does advocate for the introduction or expansion of good practices. As one example, the Commission has called for increasing the use of peer support workers in mental health and addiction services to better address the needs of those experiencing mental ill-health or substance use issues (Mental Health and Wellbeing Commission, 2023[56]) (see Box 3.1 for policy examples relating to community-based health services, and the de-institutionalisation of mental health care; see also OECD (2021[2]) for a longer discussion of this topic).
Mental health and broader well-being impact assessments can help agencies to think about the impacts of their policies, but need to be designed in a user-friendly manner
In order to think about potential co-benefits, as well as trade-offs when deciding between different policy options, impact assessments (IAs) are a common tool for identifying the broader impacts of specific policies ex-ante, and Finland has been developing targeted mental health IAs to capture policy impacts on mental health specifically.
Municipalities in Finland are legally obliged to conduct IAs in decision-making, although implementation remains uneven in practice. The 2021 Acts on the Organisation of Social Welfare and Health Care, and on Wellbeing Services Counties, place a duty on local bodies to "assess in advance and take into account the impact of their decisions on the well-being and health of people by population group" (FINLEX, 2021[57]).17 The government has grouped a wide range of different types of IAs (e.g. related to children, gender, health, social impact, equality and linguistic impact) under the broader category of Human Impact Assessments, and public agencies are encouraged to combine the components as needed alongside other assessments (e.g. related to the environment, land use planning, economic and business impacts) (THL, 2023[58]) (Table 5.4). According to a 2022 survey commissioned by the Finnish Institute for Health and Welfare (THL), ex-ante evaluation was perceived as improving services and enabling a holistic review of important issues. However, while around 60% of municipalities that responded were using prospective IAs in their work “at least sometimes”, one-third did not have any IA process in place and many expressed difficulty in describing impacts of single decisions.18 When it comes to mental health, 93% of municipalities reported not having taken mental health impacts into account in their ex-ante assessments, and they expressed a desire for guidance on concrete approaches and working methods, training, networking and clear, easy-to-use indicators (Rotko et al., 2022[59]).
Table 5.4. A human impact assessment form used in municipal and county-level decision-making in Finland
|
Impacts (short and long term) |
Alternative 0 (current situation continues) |
Alternative 1 |
Alternative 2 |
|---|---|---|---|
|
Population (including by gender, age, income, level of education, residential area) |
|||
|
Organising services |
|||
|
Staff |
|||
|
Environment |
Source: Adapted from the Finnish Institute for Health and Welfare (THL).
Because mental health, and in particular positive mental health, has not yet been included among the existing suite of IAs for municipalities, the Finnish National Mental Health Strategy 2020-30 recommended the development of a specific mental well-being impact assessment (MIVA) tool to guide mental health management in support of its HiAP approach (Ministry of Social Affairs and Health, 2020[33]). As a first step in creating this tool, the Finnish Institute for Health and Welfare (THL) and MIELI Mental Health Finland conducted a systematic review of existing mental health and well-being impact evaluation frameworks that have been used in international settings, and highlighted both opportunities and challenges related to their practical implementation (Cresswell-Smith et al., 2022[60]) (Table 5.5). In early 2023, guidance that clarifies terms and supports a harmonised approach to MIVA for municipalities and wellbeing service counties was released, featuring examples of good practice (THL, 2023[61]). For instance, the City of Jyväskylä Council evaluated a proposed initiative to reduce operating fees for after-school activities for low-income families. After gathering input from service providers, children and parents, the evaluation identified positive psychosocial effects of different types of after-school activities on children, including on their social relationships and their opportunities for hobbies (THL, 2023[61]). Going forward, it will be important to ensure integration with other IAs (something municipalities stressed as important to them) in order to avoid duplication of work and the creation of multiple, potentially overlapping processes.
Table 5.5. Opportunities and challenges when implementing mental well-being impact assessments
|
Opportunities |
Challenges |
|---|---|
|
Listening to and involving a wide range of stakeholders, including people with lived experience and mental health organisations |
Impact assessment takes time and financial resources are essential – long-term monitoring in particular requires permanent resources |
|
An opportunity to explore both positive and negative effects on mental health |
Heterogeneous definitions cause confusion |
|
The purpose of IA is to facilitate evaluation, but it can also be a tool for advocacy, raising awareness and capacity building for mental health |
Impact assessment needs to be user-friendly and designed to be used by laypeople in a variety of sectors – it is important to avoid jargon and unnecessarily complex terminology |
|
Advocacy work is needed to raise awareness and improve the approach in different sectors |
|
|
There can be a tendency for a rapid process IA with subsequent reports lacking in-depth details and documentation |
Source: Adapted from Cresswell-Smith et al. (2022[60]), “Mental health and mental wellbeing impact assessment frameworks – A systematic review”, International Journal of Environmental Research and Public Health, https://www.mdpi.com/1660-4601/19/21/13985.
5.3. Refocus: Emphasis on positive mental health
Several countries have refocused their mental health activities so that in addition to addressing the incidence of clinical mental health conditions, efforts are simultaneously made to promote positive mental health outcomes at the population level. This is closely related to the field of mental health promotion, which focuses on strengthening protective factors for good mental health, enhancing supportive environments and enabling access to skills, resources and life opportunities that promote the mental health and well-being of individuals and populations (Barry et al., 2019[62]). Besides the value of positive mental health in itself, there is an argument to be made that mental health promotion is something other sectors beyond health are more likely to recognise as their responsibility: for instance, in Finland, the 2022 survey of municipalities mentioned in the previous section showed that only 29% of respondents had a mental health strategy in place (and 28% could not say whether their municipality has a strategy), whereas almost all (95%) were implementing mental health promotion activities (Rotko et al., 2022[59]).19
Publishing data on positive mental health can help to put it on the agenda
Investing in the development of indicators on positive mental health and regularly collecting monitoring data can help to foster a common understanding of its components across agencies and society, help assess the mental health impacts of shocks (e.g. COVID-19) in a timely manner and evaluate high-level progress on whether mental well-being is improving.
In Canada, the 2012 national mental health strategy Changing Directions, Changing Lives highlighted that while surveillance systems on mental health conditions have been established, data suitable for monitoring positive mental health across the Canadian population remained scarce (Mental Health Commission of Canada, 2012[63]). In response to this need for better data, the Government of Canada funded the Public Health Agency of Canada (PHAC) to develop the Positive Mental Health Surveillance Indicator Framework (PMHSIF), launched in 2016, to monitor population positive mental health and its determinants and to inform policies for mental health promotion (Orpana et al., 2016[64]). The underlying conceptual framework uses the PHAC’s definition of positive mental health as a “state of well-being that allows us to feel, think, and act in ways that enhance our ability to enjoy life and deal with the challenges we face. It is a positive sense of emotional and spiritual well-being that respects the importance of culture, equity, social justice, interconnections and personal dignity” (Government of Canada, 2014[65]). The PMHSIF contains five positive mental health outcome indicators across three domains (emotional, psychological and social well-being) and 24 indicators for capturing associated risk and protective factors across the individual, family, community and societal level (Figure 5.5).
The PHAC’s work on monitoring and evaluating the indicators of the PMHSIF (at the national level, for adults, youth and disaggregated according to a variety of demographic and socioeconomic variables) via an online platform has contributed to their routine inclusion in briefings to the Ministers of Health and Mental Health and Addictions, and to their mainstreaming into other health surveillance products (Public Health Agency of Canada, 2023[66]). For instance, the PMHSIF has informed municipal surveillance efforts around Canada, such as in the 2018 Status of Mental Health Report of the city of Ottawa in the province of Ontario which used the PMHSIF as its basis (Public Health Ottawa, 2018[67]). In addition, the PMHSIF’s outcome measure on self-rated mental health has been added to the health indicators dashboard of the Chief Public Health Officer of Canada, and psychological well-being is one of the PHAC’s high-level performance indicators in the departmental results reports (Government of Canada, 2023[68]; 2022[69]).20 Canada’s Quality of Life framework, originally developed by the Department of Finance in 2021, also includes three outcome indicators from the PMHSIF as headline indicators (intended to provide high-level assessments of overall quality of life): life satisfaction, self-rated mental health indicator (under the Health domain), and social well-being (i.e. sense of belonging to the local community (under the Society domain) (Statistics Canada, 2023[70]). For the last few years, the Quality of Life framework has been integrated into the budgeting process via budget impact reports: each budget measure lists the anticipated quality-of-life impacts it is expected to advance. By way of example, in the 2022 budget impact report, diverse budget measures ranging from “Long-Term Supports to End Homelessness” to “First Nations Water and Community Infrastructure” to “Fighting and Managing Wildfires” all highlighted self-reported mental health improvement as a potential impact (Government of Canada, 2022[71]).
Increasing data availability on positive mental health, including now annual statistics on self-rated mental health, life satisfaction and sense of belonging to one’s community, also made it possible to assess the impacts of the COVID-19 pandemic on mental health in Canada, including on different population groups (Capaldi et al., 2022[72]; Capaldi, Liu and Dopko, 2021[73]; Government of Canada, 2022[74]; 2022[75]; Ooi et al., 2023[76]). Such evidence is essential for informing the focus of strategies and taking wider governmental action to address mental health inequalities between population groups on an ongoing basis, including in the aftermath of shocks and during recovery periods.
Figure 5.5. The Canadian Positive Mental Health Surveillance Indicator Framework
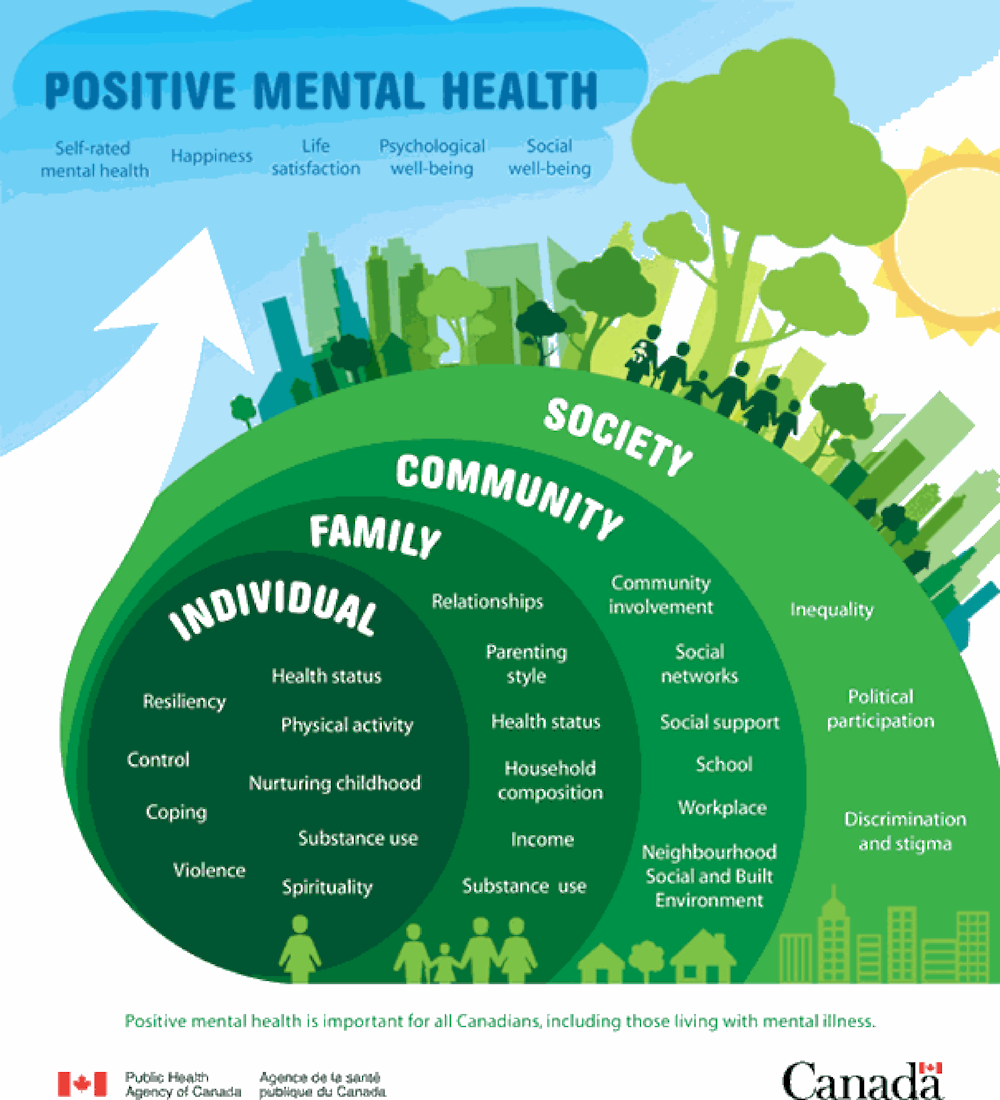
Source: Orpana et al. (2016[64]), “Monitoring positive mental health and its determinants in Canada: The development of the Positive Mental Health Surveillance Indicator Framework”, Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, https://doi.org/10.24095/hpcdp.36.1.01.
Strategies and funding mechanisms can and are increasingly explicitly targeting mental health promotion
Multiple governments have endorsed positive mental health as an explicit policy goal in recent years, as can be seen in several of the case studies conducted for this report (in Canada, Finland, Wales and Western Australia), as well as in additional OECD countries (e.g. in Ireland, where the Department of Health is currently developing a Mental Health Promotion Plan) (Department of Health Ireland, 2023[77]; Walsh, Sheridan and Barry, 2023[78]; Barry, Keppler and Sheridan, 2023[37]). Concretely, this has resulted in both bespoke guidance on how to improve mental well-being for agencies as well as innovative funding mechanisms that target resilience factors for health promotion.
In Australia, the Western Australia Mental Health Commission’s Mental Health Promotion, Mental Illness, Alcohol and Other Drug (AOD) Prevention Plan 2018-2025 (Prevention Plan) already included information about both risk and resilience factors for mental health, as well as references to promotion activities (Mental Health Commission, 2018[79]). However, since its release in 2018, there has been increasing awareness of the importance of promoting mental well-being (which is how the Commission refers to positive mental health) specifically, as well as developments in research and evidence about cost-effective mental health promotion over the life course (Carbone, 2021[80]). To better define and strengthen the mental well-being and mental health promotion components of the Prevention Plan, the Commission is developing a supplementary Mental Wellbeing Guide that will be published in 2023 (Mental Health Commission, 2023[81]). The Guide will clarify the term “mental well-being” and how it impacts and interacts with both mental health and physical health, identify the factors that influence mental well-being, and provide practical examples of activities to improve well-being for state and local government agencies, communities, non-governmental and private organisations. One of the Guide’s goals will also be to encourage other actors to include relevant measures in impact evaluations in order to further strengthen the evidence base on good practice.
In Canada, the PHAC has been experimenting for more than a decade with new models of strategic grantmaking for health promotion to encourage social innovation. Through the 2009-20 Innovation Strategy, long-term funding was provided to community-based organisations across Canada in over 1 700 communities that addressed complex health challenges by focusing on their broader social and economic determinants and inequities (Government of Canada, 2023[82]). The Innovation Strategy had two key objectives: to test and evaluate new, community-based approaches to promote health for individuals, families and communities; and to apply the results to impact policy and programme development, to ultimately support deep and sustainable systems change.21 The Innovation Strategy focused on two priority areas: “Equipping Canadians – Mental Health throughout Life” and “Achieving Healthier Weights in Canada's Communities”. The next, current iteration of the funding programme, started in 2019 and providing up to nine years of funding, has been renamed the Mental Health Promotion Innovation Fund and, as its name suggests, focuses on mental health promotion (Government of Canada, 2023[43]).
Two of the key elements for success of the Innovation Strategy (that have been retained in the current Mental Health Promotion Innovation Fund) are first, a multiyear commitment to funding that allows for meaningful project and partnership development (see section on reconnecting below).22 And, second, a phased approach to funding that allows for social innovation (all projects received funding for 12-18 months to design and test programmes, with the most promising approaches being selected for follow-up funding of up to four years for full implementation and evaluation, with an additional three years of funding for the final phase to scale up the successful programmes into other communities, populations and systems). At the end of the three phases of funding, the Innovation Strategy led to over 1 400 partnerships established by community-led organisations across multiple sectors with more than CAD 30 million (around USD 23 million) of leveraged funds through matched financing from project partners (e.g. the private sector, impact investors, other government departments or other community organisations), and all funded projects reported improvements in protective factors for project participants by the end of the programme (Bradley Dexter et al., 2021[83]).
A range of programme design components have also been updated in the Mental Health Promotion Innovation Fund following learnings from the Innovation Strategy. These include the creation of a dedicated Knowledge Development and Exchange Hub for Mental Health Promotion to facilitate knowledge sharing on what works for achieving scale-up and systems change (see section on reconnecting below (KDE Hub, 2023[44])), and a stronger focus on building protective factors for mental health into programme activities, especially at the early stages of life (infants to youth) (Figure 5.6). In addition, experiences from the Innovation Strategy showed that while funded projects targeted multiple determinants of health, there was a great emphasis on individual behaviour and personal skills, rather than on system level factors (Salmond and Mahato, 2021[84]). The Mental Health Promotion Innovation Fund hence created a Health Equity Indicator Tool (HEIT) pilot and invited funded projects to participate, with the aim of supporting them to define the priority determinants of health alongside equity considerations, as well as the opportunities to tackle these issues more upstream. Lastly, the Mental Health Promotion Innovation Fund moved from a traditional, detailed, long-term workplan to a “Programme of Work” approach that highlights key milestones rather than detailed activities so as to provide projects with greater flexibility to make mid-course corrections based on implementation and evaluation.
Figure 5.6. Promoting mental health and well-being for children and youth in Canada: Protective factors
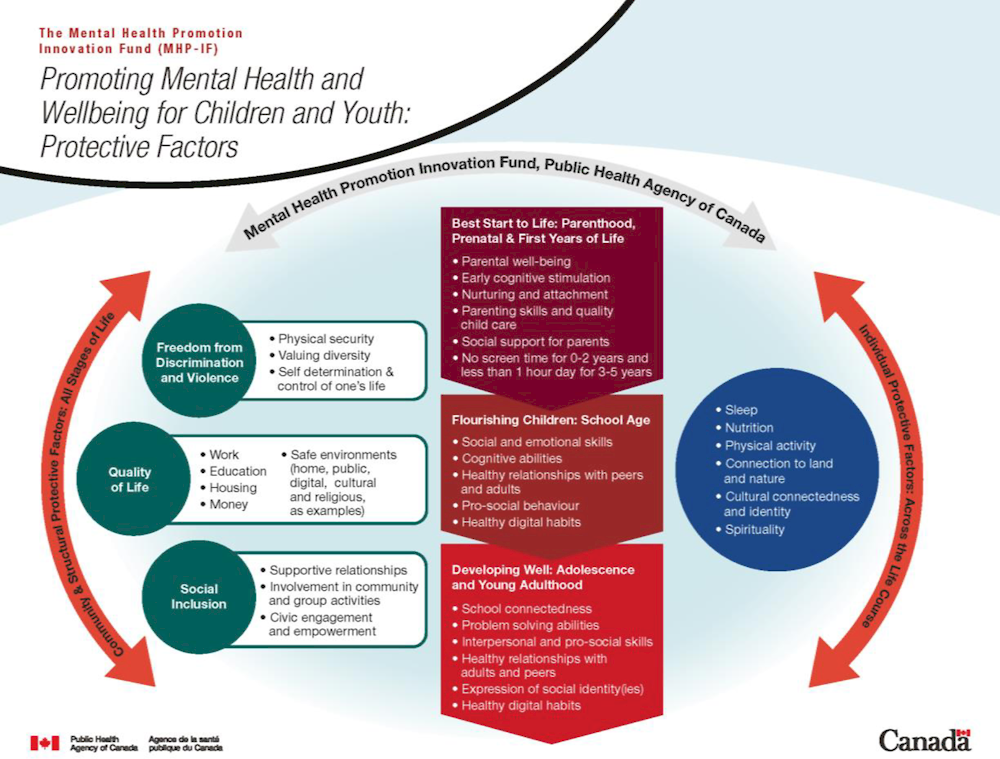
Source: Government of Canada (2023[85]), Public Health Agency of Canada (PHAC) Mental Health Promotion Innovation Fund, https://www.canada.ca/en/public-health/services/publications/diseases-conditions/infographic-mental-health-wellbeing-children-youth-protective-factors.html.
5.4. Reconnect: Building broad partnerships
Communities play an essential role in mental health promotion. Strengthening connections between central and local government policy makers and a diverse array of community associations, advocacy groups and civil society organisations is hence key to help build a joint understanding of what mental health prevention and promotion means and how it can be cultivated at the population level.
The majority of mental health strategies have a participatory element, and ideally this continues beyond the planning stage
Participatory approaches, to various degrees, have been a part of all studies covered in this chapter. Consultations in the course of strategy development have included people with lived experience, young people and where relevant Indigenous populations. In order for this participation to be meaningful to the consulted groups, their involvement should also be prioritised during implementation.
For example, the development of the Western Australian Mental Wellbeing Guide has been supported by two rounds of State-wide consultation: its initial development in 2021 was informed by consultation with 780 individuals via a series of 92 face-to-face interviews, 29 online focus groups and an online survey; a literature review of 333 published papers and grey literature relating to well-being; and an expert reference group. This was followed in 2023 by targeted consultation on the draft Mental Wellbeing Guide, with responses received from State government and non-governmental, private and community organisations, and people with lived experience (Mental Health Commission, 2023[81]). In New Zealand, the 2018 Government Inquiry into Mental Health and Addiction (He Ara Oranga) that recommended the establishment of the Mental Health and Wellbeing Commission consulted stakeholders widely and drew on over 5 000 submissions, 400 meetings and 26 public community forums (New Zealand Government, 2018[86]). The Mental Health and Wellbeing Commission itself has developed frameworks for assessing both mental health systems (He Ara Āwhina) and well-being outcomes (He Ara Oranga) for involved which public consultations, with a particular focus on reaching people with lived experience of mental distress – were conducted (Mental Health and Wellbeing Commission, 2023[87]; New Zealand Government, 2022[88]). People with lived experience continue to be represented through positions on the Commission’s board at the governance level, and dedicated lived experience roles at the operational level.
Depending on the country context, Indigenous populations and their views have been given special priority, as has been the case in New Zealand, Sweden and Canada. In New Zealand, the prioritisation of Māori and upholding of the Treaty of Waitangi (New Zealand’s founding document between Māori and the Crown) are mandated in the establishment legislation for the Mental Health and Wellbeing Commission (Parliamentary Council Office, 2022[89]). The He Ara Oranga well-being outcomes framework of New Zealand’s Commission, mentioned above, draws on existing New Zealand government work in monitoring outcomes (for example, the Treasury’s Living Standards Framework) (Mental Health and Wellbeing Commission, 2022[90]). However, it combines both a specific te ao Māori (a Māori worldview) and a “shared” (universal) perspective on what matters for good lives, unlike other well-being work in New Zealand which usually has treated these through separate frameworks (Figure 5.7). Through this framework, the Commission is reflecting te ao Māori views by emphasising less individualistic aspects and the relational well-being of whānau (roughly translated as extended family or community).
Figure 5.7. The He Aro Oranga Wellbeing Outcomes Framework
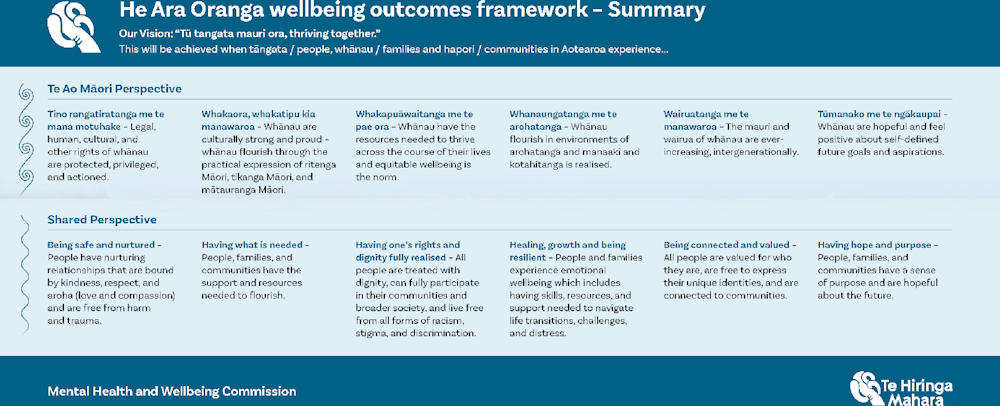
Source: Mental Health and Wellbeing Commission, (2022[90]), He Ara Oranga te tarāwaho putanga toiora / He Ara Oranga wellbeing outcomes framework, https://www.mhwc.govt.nz/our-work/he-ara-oranga-wellbeing-outcomes-framework/.
In Sweden, the Sámi Parliament is one of the agencies involved in drafting the new mental health and suicide prevention plan, the first time the needs of the Sámi people have been explicitly addressed in a mental health strategy (Schreiber, 2020[91]). Throughout the drafting process, the Sámi Parliament has argued for the importance of keeping a separate mention of issues and needs specific to the Sámi people, rather than mainstreaming these throughout the plan (the latter approach has been taken with other groups, e.g. by gender, children and young people, those with disabilities, those with existing mental health conditions). It is important to note that the needs of the Sámi are highlighted not because they are particularly vulnerable to mental ill-health in the way of other at-risk groups highlighted by the government mandate, but instead based on a discrimination and rights-based approach: their right to practice their own culture and speak their own language, and the acknowledgement that a denial of those rights historically has had impacts on (physical and mental) health.
And, in Canada, insights from National Indigenous Organisations were sought during the design process of the Mental Health Promotion Innovation Fund to inform more inclusive programme design and increase the number of Indigenous-led organisations successfully applying for funding. Following informal meetings with National Indigenous Organisations, through a PHAC-led consultation process to inform wider programming objectives, the application process was updated to include the use of culturally safe language, acknowledged the impact of ongoing colonisation on mental health, and reflected the language and wellness frameworks developed by Indigenous organisations; application opportunities were shared directly via key contacts for Indigenous organisations across the country. In addition, a chairperson with cultural safety expertise was recruited for the grantee assessment process, and specific support for projects with a connection to land was provided (e.g. through adjusted timing and project design requirements throughout the funding cycle).
Lastly, many of the mental health case studies in this chapter recognise young people as a priority group for mental health prevention and promotion, and in some cases are actively involving them in policy formulation. For instance, the Norwegian Programme for Public Health Work in Municipalities specifically focuses on mental health and well-being programmes targeting children and youth, and requires the participation of young people (and of other target groups, depending on the intervention funded) in programme development. This has taken different forms in practice, for instance through oral consultations, interviews, drawing or making cardboard models (Table 5.6). However, a qualitative study of young people’s experiences co-creating these programmes in four municipalities showed that the adolescents expressed feelings of resignation and dissatisfaction with the process in practice – they felt that implementation took a long time (so long that they themselves would not benefit from the intended projects anymore as they moved through school) and that while their views were gathered during the initial planning stages, their involvement was stopped shortly after (Sylte et al., 2023[92]). These findings are consistent with the broader literature on engaging children and adolescents in public projects, in that simply being consulted is not sufficient for young people to view their participation as meaningful, and that continuous engagement and clear and regular feedback on decisions made can help build ownership and set expectations (Cele and van der Burgt, 2015[93]; Freire et al., 2022[94]; Council of Europe, 2016[95]; Sylte, Lillefjell and Anthun, 2023[96]). Of course, this more extensive form of co-creation requires additional time and resources, and it should be noted that the COVID-19 pandemic coincided with the start of the projects in the four municipalities that were examined, placing constraints on physical meetings and introducing delays and changes in planning (Sylte et al., 2023[92]).
Table 5.6. Types of young people’s participation in municipal projects in Norway
Examples of young people’s participation in four projects funded under the Norwegian Programme for Public Health Work in Municipalities
|
Project funded |
Types of young people’s participation |
|---|---|
|
Schoolyard renovation |
Brainstorming day at school |
|
Schoolyard renovation |
The student council was consulted by the project leader; students in lower secondary school were involved in creative activities during classes (carpentry, painting, etc.); students in primary and lower secondary school took part in a drawing competition; students were consulted by an architect and researchers (interviews and GPS registration of schoolyard activities); adolescents and adult stakeholders took part in an activity night with image scraping |
|
Establishment of a youth club |
Student council members were represented in the project group; 8th graders were involved in creative activities during classes (cardboard modelling, image scraping, room sketching, etc.); prioritising challenges and brainstorming with students in lower secondary school using digital tools |
|
Schoolyard renovation |
5th-10th graders were involved in an activity night with adult stakeholders; 5th-10th graders were consulted by the project leader during school hours; the student council was occasionally consulted by the project leader |
Source: Sylte et al., (2023[92]), “Nothing gets realised anyway’: Adolescents’ experience of co-creating health promotion measures in municipalities in Norway”, Societies 2023, 13, 89, https://doi.org/10.3390/soc13040089.
Knowledge brokering is an essential part of reconnecting
Supporting non-governmental stakeholders and communities in their efforts to improve population mental health has been a key element of government approaches – as documented by the case studies reviewed here – and this has involved different ways of knowledge sharing and exchange. These include providing concrete guidance and toolkits for action, dedicated peer-learning and knowledge platforms, and partnering with academia for evaluation.
One approach is to provide easy-to-access information and guidance on the kinds of contributions community organisations can make. The Act Belong Commit campaign synthesises evidence on what contributes to living a mentally healthy life into a lifestyle framework with three main pillars. The ABCs encourage people to be physically, mentally, spiritually and socially engaged by doing something active (Act), doing something with someone (Belong) and doing something meaningful (Commit). The easy-to-remember acronym enables people to understand the goals of the programme and recall the protective and promotive steps they can take to cultivate and improve their mental health. In this way, the programme can be seen as a practical framework for mental health promotion that can be applied at all levels: in a clinical setting; in schools, workplaces or community organisations; or at the population level (Donovan and Anwar-McHenry, 2014[97]; Donovan et al., 2021[98]). Originally developed by researchers funded by the Western Australian Health Promotion Foundation (Healthway) in the early 2000s, the ABCs have been adopted by a range of other actors worldwide including schools, universities and community organisations, and the programme has received government funding in Australia, Denmark, the Faroe Islands, Finland and Norway (Donovan and Anwar-McHenry, 2015[99]; Elon University, n.d.[100]) (Box 5.3).23,24 One of the programme’s components is a dedicated partnership strategy to connect with community groups, local governments, health organisations, advocacy groups and schools to provide them with guidance and practical examples in mental health promotion strategies. In addition, regular meetings with partnering organisations (e.g. municipalities, sports organisations, scouts and guides, and volunteering groups such as the Red Cross) contribute to continued knowledge exchange and the refinement of tools. For instance, in Australia as of 2022, the campaign had worked with 270 community organisations in Western Australia, and several more in other Australian states, in addition to collaborating with international partners (Act Belong Commit Western Australia, 2022[101]; Koushede and Donovan, 2022[102]). A recent process evaluation of ABC in Denmark highlighted that it provided relevant knowledge on mental health promotion to stakeholders and fostered intersectoral and interprofessional collaborations. However, the evaluation also pointed out that its bottom-up approach requires time and resources, as well as a continuous deliberate balancing between local adaptability and concrete guidance when engaging implementers (Hinrichsen et al., 2020[103]).
Box 5.3. Act Belong Commit (the ABCs of mental health) across different OECD countries
ABC has been implemented in a variety of OECD settings now, with involved organisers from different countries regularly meeting online (and also in person, for example at the 17th World Congress on Public Health in Rome in 2023) to share knowledge and experiences.
Western Australia
The ABCs were initially developed in Western Australia. In the early 2000s, the Western Australian Health Promotion Foundation (Healthway) funded a team of researchers to conduct focus groups to better understand how the general public understood concepts of mental health and well-being. The findings from this work informed the conclusion that mental health promotion campaigns should use the term “mentally healthy” to neutralise the negative connotations surrounding the term “mental health”. This led to the Mentally Healthy Western Australia campaign that, following a six-month consultation period, was piloted in six communities in Western Australia from 2005 to 2007. The project team developed the ABC slogan at this time, wanting to find a way to communicate the goals of the programme clearly (Donovan et al., 2006[104]).
The success of the pilot led to ABC being fully launched in Western Australia in 2008. It is still active, making it the longest running mental health promotion campaign in Australia. The programme is now based in Curtin University, but it is publicly funded by the Government of Western Australia. The programme has a dedicated partnership strategy to connect with community groups, local governments, health organisations, advocacy groups and schools, and it provides them with free guidance in mental health promotion strategies. This helps to extend the reach of the ABC message to particularly to hard-to-reach populations, and directs people to opportunities for engagement. The programme website hosts a variety of publicly available tools, including a mental well-being self-assessment quiz and an activity finder (Act Belong Commit Western Australia, 2022[101]; Koushede and Donovan, 2022[102]).
Denmark
Denmark began its involvement with the ABC programme in 2014, when a research team comprising the Danish National Institute of Public Health, the Danish Healthy Cities Network, the Danish School of Media and Journalism, Public Health Copenhagen and the Red Cross Copenhagen obtained funding from the Danish Ministry of Health to pilot Act Belong Commit in Denmark (Koushede and Donovan, 2022[102]). The pilot focused primarily on understanding whether the Australian programme could be successfully adapted to the Danish context; the final evaluation supported this finding, and showed that Danes intuitively grasped the drivers of good mental health in a way that was consistent with the messaging of ABC campaign materials (Nielsen et al., 2017[105]). When implementing the ABCs, the team translated the core messaging to Danish, while retaining the “ABC” branding (ABC for Mental Sundhed, and the programme pillars of “do something”, “do something with someone” and “do something meaningful” are each translated to Danish).1 Following receipt of its initial grant, the programme has been awarded subsequent rounds of funding by the Nordea Foundation to enable it to continue to present day.
The programme is now led and administered through a research team in the Department of Psychology at the University of Copenhagen (UCPH) and as of 2022 has developed partnerships with more than 70 organisations including 23 (out of a total of 98) municipalities in Denmark. Organisations involved in the work include sports clubs, employee associations, evening schools, the Scouts and Guides association, mental health foundations and the Centre for Prevention in Practice which is a part of the National Association of Municipalities, among others. Although at a surface level the organisational structure appears similar to the ABC programme in Australia – in that a university serves as programme lead – the Danish iteration of the programme is more decentralised, with partnering organisations participating in programme development and taking turns to host quarterly programme meetings (Koushede and Donovan, 2022[102]).
In 2022, the Danish Government announced a multi-party agreement on a ten-year plan for addressing issues relating to psychiatry and mental health. The plan outlines 19 goals, with a series of recommended indicators to track progress in each area. A priority area for the government is to address stigma surrounding mental health and to increase the public’s knowledge of how to promote their mental health. From 2024, ABC for Mental Sundhed will receive funding through this plan to expand its mental health promotion campaign (Ministry for the Interior and Health, 2022[106]; Meilstrup et al., 2022[107]).
Faroe Islands
The Faroese Board of Public Health in the Faroe Islands became interested in ABC in 2016 and began developing its programme the subsequent year. Programme organisers worked closely with their Danish counterparts initially but first prioritised translating the messaging into Faroese. To develop the programme and bring onboard additional stakeholders, the Board of Public Health began by inviting all municipalities in the Faroe Islands to a presentation on ABC. The first partner to join was an umbrella organisation for all municipalities; following the presentation, additional municipalities and other agencies (including the Red Cross) agreed to join. As of early 2023, nine (of a total of 29) municipalities in the Faroe Islands have joined ABC, along with 26 partners, including Christian organisations, mental health visitors (an interest group for people experiencing mental ill-health) and (soon) also community partners that will include dance and walking groups. As a concrete example of how ABC messaging has influenced the programme design of partners, a partner school has created courses around the concepts of “togetherness” and “meaning”. As in Denmark, the ABC programme meets with participating organisations four times a year. Funding for ABC in the Faroe Islands has now been enshrined in the Public Finance Act.
Finland
In Finland, the Finnish Institute of Health and Welfare (THL) is piloting and studying the implementation of the ABCs of mental health in four municipalities in 2023-24.2 The programme development and research are supported financially by the Finnish Ministry of Social Affairs and Health. This experience will inform the potential expansion of the programme to the national level.
Norway
In 2022 the Ministry for Health and Care Services announced the launch of a two-year ABC pilot programme in the Trøndelag region, with the intention to prepare potential expansion to the national level (Ministry of Labour and Social Inclusion, 2022[108]). This decision was informed by an ongoing initiative of the Trøndelag Public Health Alliance, an association of volunteers and public partners who had already adopted ABC in their public health collaboration. In order to tailor the programme to the Norwegian context, the initial organising team for ABC in Norway, which also included the WHO Network of Health Promoting Hospitals, met with a professional marketing team to translate the name, which after a recent consultation with the Ministry for Health and Care Services is now ABC for god psykisk helse – ein folkehelsekampanje, or, ABC for Good Mental Health – A Public Health Campaign (the three pillars are also translated).3 Partners in Trøndelag have now adopted ABC to varying degrees, including the psychiatric community, which has been exploring how ABC can be implemented in clinical practice, to aid those currently experiencing, or in recovery from, chronic mental ill-health and addiction (ABC for Mental Sunnhet, n.d.[109]).
Notes:
1. Gør noget aktivt, Gør noget sammen, Gør noget meningsfuldt.
2. Translated as Mielen hyvinvoinnin ABC in Finnish.
3. Act: Gjer noko aktivt; Belong: Gjer noko saman; Commit: Gjer noko meiningsfillet.
Beyond providing guidance, Canada’s Innovation Strategy and its Mental Health Promotion Innovation Fund, as described above, have directly financed the work of community organisations targeting the social determinants and protective factors of health. Evaluation and peer learning have also been strong components: grant recipients are required (and receive funding) to evaluate progress on the protective factors of health that they are targeting, as well as on their policy impact (Government of Canada, 2023[43]). This information feeds into deciding which initiatives receive follow-up funding for scale. In addition, the Mental Health Promotion Innovation Fund now includes the aforementioned dedicated Knowledge Development and Exchange Hub for Mental Health Promotion (the KDE hub) to create new knowledge across funded projects in a timely fashion, build community and capacity amongst the projects and others who share their interests, and strengthen systemic supports for sustaining and scaling up promising approaches (KDE Hub, 2023[44]). Examples of KDE Hub activities include toolkits relevant to planning, implementing, evaluating and sharing new knowledge, regular webinars and an annual symposium. For instance, a research study was conducted to gather key insights from adapting project delivery to virtual and hybrid settings during the COVID-19 pandemic, including for different audiences (new immigrants, youth and 2SLGBTQI+) have been synthesised and shared in various ways, including in a peer-reviewed journal and on the KDE Hub’s website (KDE Hub, 2023[44]; Riley et al., 2022[110]).
A third way to improve knowledge development on mental health more broadly is to actively engage with academia. For instance, in Wales, the North Public Service Lab, enabled by Wrexham University, provides a space for systems leadership capacity building in relation to the Future Generations Act (through a programme of masterclasses, events, cafes and workshops), and Canada’s KED Hub is located at the University of Waterloo (KDE Hub, 2023[44]; Wrexham University, 2023[111]). Similarly, while the ABC programme in Western Australia is publicly funded by the Government of Western Australia, it is now based in Curtin University. Indeed, the ABC programme was not only initially developed by researchers, but it has also been continuously evaluated over the past decades through a large number of impact evaluations. Evaluations of the work in Australia, where the programme was developed and first piloted, found that it reduces the stigma surrounding mental ill-health, increases openness around discussing mental health issues, and increases the help-seeking behaviours of participants (Anwar-McHenry et al., 2012[112]; Drane et al., 2023[113]). Research in other contexts has shown that indicators relating to the three pillars of ABC are predictive of lessened risk both for the onset of depression and anxiety and for cognitive impairment among the elderly, a decreased likelihood of problematic alcohol consumption, improved self-reported (mental) health and life satisfaction, and increased help-seeking behaviour including talking to family and friends about mental health (Santini et al., 2017[114]; 2017[115]; Ekholm, Juel and Bonde, 2016[116]; Haug et al., 2021[117]; Santini et al., 2022[118]). Finally, in the Norwegian Programme for Public Health Work in Municipalities, some of the most successful municipal innovations involved increased cooperation between university-affiliated researchers who assisted with evaluation, although this was not a programme requirement (NTNU, 2020[119]; Forebygging, 2022[120]; Hope et al., 2021[121]; Berg and Johansen, 2023[122]). In turn, researchers also changed their way of working once they found out which questions were of actual interest to local policy makers, and they have since been integrated into larger research programmes (NTNU, 2023[49]; Lillefjell et al., 2018[123]; Lillefjell and Maass, 2021[124]; Lillefjell et al., 2022[125]). Going forward, the Programme could consider how to further incentivise and formalise this component.
The depth of partnerships matters for impact
Canada’s Innovation Strategy has yielded important insights about what it means to build effective partnerships (and how to evaluate them). At the end of the programme, 90% of projects and partnership networks had a sustained impact on policy and public health practice by the final phase of funding, and 82% of projects continued to operate afterward by obtaining funding from other sources or by integrating into an existing system through scale up (Government of Canada, 2023[82]). On the one hand, the long-term and flexible nature of the Strategy’s funding allowed for organic partnership development to take place, and on the other hand, partnership building itself was an explicit goal, which grantees were provided resources for and were evaluated on (alongside other key factors) throughout the project phases in order to assess readiness for scale-up and decide on funding extensions (Bradley Dexter et al., 2021[126]).25
The Strategy’s assessment of the partnerships that the grantees were building points to some common key characteristics of successful “vested” partnerships, including that they were diverse in character, shared a clear agenda on which social determinants matter, aligned and adapted through dialogue and shared activities, and intentionally pooled and leveraged resources and assets across partners (Table 5.7). It also indicated that there is a trade-off between project scale-up at the beginning (e.g. reaching a higher number of regions with a programme) and slower but deeper partnership development that ultimately resulted in higher impact (Lee and Salmond, 2021[127]).
Table 5.7. Key elements of successful vested partnerships
Assessment of partnership elements for projects funded through the Canadian Innovation Strategy 2009-20 (focusing on the two priority areas of mental health and obesity)
|
Element |
Example |
|
|---|---|---|
|
Diversity of partners |
Intentional multi-sectoral partnerships representing diversity across the sector (system) aiming to change Local partners and leaders ground the diversity and hold different stakeholders accountable to the long term |
One project demonstrated a mix of partners, schools, non-profits, stores and health food stores. The diversity represented the range of partners able to influence the food system Across the projects, strong community partners and local leaders and Elders helped the project adapt methods to the local culture as well as ensure continuity going forward |
|
Clear agenda on social determinants of health that includes sectoral change |
Changes in access to resources, material conditions and services Changes in attitudes, behaviour, skills, mental health, self-efficacy Upstream changes in policies, laws or budgets Changes in societal norms, attitudes and behaviours |
Community infrastructure as a part of the wider physical environment (ovens, freezers, gardens, community tables) were examples of building local assets and service provision. In addition, they also provided critical points of connection, as did events and festivals that supported social networks, belonging, and connecting cultural practices past and present Improved coping strategies for school children Demonstrated influence on First Nations and Inuit Health Branch; changes in school policies Changes in stigma related to mental health issues |
|
Partner alignment |
Deeper and ongoing dialogue and analysis of goals and issues across partners Backbone agencies or groups helped to broker learning and action and align partner interests and incentives Acknowledge differences in partners but aligned incentives and mutually reinforcing activities |
One project mentioned that a key lesson was that partnerships needed to be “fewer, deeper, stronger”. Time and dialogue are needed to bring partners to a shared understanding of the problem and shared solutions, and to align incentives Food networks developed a “backbone” agency, which was crucial to the health of the partnership network—even more so than the funding recipient/lead agency One project had interventions that connected multiple programs, services and sectors |
|
Brand pooling and leveraging assets |
Intentional business/governance strategy that involved aligning partner incentives and examining market and subsidy opportunities in the system Able to leverage investment and funding through evidence Able to institutionalise the strategies |
In one project, though led by a non-profit organisation, the presence of a private sector partner helped the partnership be savvy in assessing the market for local foods. This business savvy also supported sustained funding and a governance base. They were able to identify specifically where smart subsidy could be used (to address financial barriers of hunters) For one highly rated mental health promotion project, being able to quantify social return on investment was a good substitute for trying to earn income through the partnership and to attract investors and funders. They could demonstrate that every CAN 1 spent on the project would generate CAN 17.96 in social benefits Institutional strategies included schools, mental health centres, friendship centres, government health agencies, retail stores, universities, health food stores and e-commerce sites |
Source: Lee and Salmond, (2021[127]), “Monitoring vested health partnerships”, Canadian Journal of Public Health, Vol.112/S2, pp. 231-245, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8360250/.
5.5. Conclusion
This chapter has reviewed selected mental health initiatives in OECD countries to better understand which structures, working arrangements and practices can facilitate tackling the social, economic, relational and environmental determinants of mental health upstream. The resulting findings have illustrated that all case study countries, to different degrees, are currently trying to align action across sectors, redesign and propose interventions that bring co-benefits for mental health and other well-being outcomes, increasingly prioritise positive mental health as goal in strategies and funding, and connect and collaborate with stakeholders across society. All of these actions, or principles of well-being practice more generally, are important for the practice of good mental health policy.
Beyond the lessons already pointed out in each section, several cross-cutting insights are noteworthy. First, explicitly defining what it is that should be improved, and who can contribute, can help different agencies and stakeholders to focus action. This has been the case, at a broader level, when using multidimensional frameworks to inform mental health plans and point out the interlinkages with other sectors, when formulating concrete implementation plans, or when defining and monitoring positive mental health. Second, intersectoral collaboration, partnership building and knowledge brokering, whether between different government agencies or different levels of government, or when supporting community actors, takes resources, including time, to do well. In several of the case studies, such as during the development of a new mental health strategy in Sweden or when funding municipal and community programmes in Norway and Canada, there was a conscious move away from short-term project cycles to multi-year processes, in order to allow for relationships to form, for management capacity to be built and for experimentation with programme design. Third, strategic grant making by a public health agency, as in Norway and Canada, seems to be a promising approach to channel funds into activities that target (mental) health determinants and that take local needs into account, including in areas not necessarily under the traditional remit of the health sector. And, lastly, with a few exceptions, all case studies could benefit from integrating impact evaluations into their design from the outset, in order to build the evidence base on what works for improving ecosystems that are conducive to mental health, and to move from the partly descriptive approach of this chapter to a quantitative comparative assessment. Close cooperation with academia, as has already been started in several of the featured initiatives, could be a promising avenue.
Going forward, the approach of this chapter, in examining country efforts around realigning, redesigning, refocusing and reconnecting, could be extended beyond the small sample of case studies to all OECD countries, both to the area of population mental health improvement as well as to other policy areas that can benefit from an integrated approach.
References
[109] ABC for Mental Sunnhet (n.d.), Act-Belong-Commit in Recovery, https://www.abcmentalsunnhet.no/wp-content/uploads/ABC-in-recovery.pdf (accessed on 6 June 2023).
[101] Act Belong Commit Western Australia (2022), Act Belong Commit, https://www.actbelongcommit.org.au/.
[112] Anwar-McHenry, J. et al. (2012), “Impact evaluation of the Act-Belong-Commit mental health promotion campaign”, Journal of Public Mental Health, Vol. 11/4, pp. 186-194, https://doi.org/10.1108/17465721211289365.
[62] Barry, M. et al. (eds.) (2019), Implementing Mental Health Promotion, Springer International Publishing, Cham, https://doi.org/10.1007/978-3-030-23455-3.
[37] Barry, M., T. Keppler and A. Sheridan (2023), Development of the National Mental Health Promotion Plan: Report prepared for the Department of Health, Ireland, Health Promotion Research Centre, University of Galway, https://www.universityofgalway.ie/hprc/ (accessed on 5 September 2023).
[29] Becker, L. (2023), Intersectoral Collaboration in the Development of a National Policy for Mental Health and Suicide Prevention in Sweden, Lund University.
[122] Berg, A. and O. Johansen (2023), Oppstart av ungdomsklubber i kommunene Leka og Lierne som lokale tiltak knyttet til Program for folkehelsearbeid i Trøndelag, Nord Universitet, https://nordopen.nord.no/nord-xmlui/bitstream/handle/11250/3071702/FoURapport952023.pdf?sequence=1&isAllowed=y.
[83] Bradley Dexter, S. et al. (2021), “The art and science of a strategic grantmaker: The experience of the Public Health Agency of Canada’s Innovation Strategy”, Canadian Journal of Public Health, Vol. 112/S2, pp. 186-203, https://doi.org/10.17269/s41997-021-00512-9.
[126] Bradley Dexter, S. et al. (2021), “Readiness for scale-up: Lessons learned from the Public Health Agency of Canada’s Innovation Strategy”, Canadian Journal of Public Health, Vol. 112/S2, pp. 204-219, https://doi.org/10.17269/s41997-021-00517-4.
[73] Capaldi, C., L. Liu and R. Dopko (2021), “Positive mental health and perceived change in mental health among adults in Canada during the second wave of the COVID-19 pandemic”, Health Promotion and Chronic Disease Prevention in Canada, Vol. 41/11, pp. 359-377, https://doi.org/10.24095/hpcdp.41.11.05.
[72] Capaldi, C. et al. (2022), “Self-rated mental health, community belonging, life satisfaction and perceived change in mental health among adults during the second and third waves of the COVID-19 pandemic in Canada”, Health Promotion and Chronic Disease Prevention in Canada, Vol. 42/5, pp. 218-225, https://doi.org/10.24095/hpcdp.42.5.05.
[80] Carbone, S. (2021), What Works to Promote Mental Wellbeing and Prevent the Onset of Mental Health Conditions? A review of the latest research evidence, Prevention United, https://www.mhc.wa.gov.au/media/3940/wa-mhc-literature-review-final.pdf.
[6] CDC (2016), Health in All Policies, Centers for Disease Control and Prevention, https://www.cdc.gov/policy/hiap/index.html#:~:text=Health%20in%20All%20Policies%20(HiAP,of%20all%20communities%20and%20people.
[93] Cele, S. and D. van der Burgt (2015), “Participation, consultation, confusion: Professionals’ understandings of children’s participation in physical planning”, Children’s Geographies, Vol. 13/1, pp. 14-29, https://doi.org/10.1080/14733285.2013.827873.
[95] Council of Europe (2016), Child Participation Assessment Tool, https://www.coe.int/en/web/children/child-participation-assessment-tool.
[60] Cresswell-Smith, J. et al. (2022), “Mental health and mental wellbeing impact assessment frameworks: A systematic review”, International Journal of Environmental Research and Public Health, Vol. 19/21, https://doi.org/10.3390/IJERPH192113985.
[77] Department of Health Ireland (2023), Healthy Ireland Policies, https://www.gov.ie/en/policy-information/706608-healthy-ireland-policies/#mental-health-promotion-plan.
[9] Diminic, S. et al. (2015), “Intersectoral policy for severe and persistent mental illness: Review of approaches in a sample of high-income countries”, Global Mental Health, Vol. 2, p. e18, https://doi.org/10.1017/gmh.2015.16.
[99] Donovan, R. and J. Anwar-McHenry (2015), “Promoting mental health and wellbeing in individuals and communities: The ‘Act-Belong-Commit’ campaign”, in Wymer, W. (ed.), Innovations in Social Marketing and Public Health Communication Improving the Quality of Life for Individuals and Communities, Springer Cham, https://doi.org/10.1007/978-3-319-19869-9_11.
[97] Donovan, R. and J. Anwar-McHenry (2014), “Act-Belong-Commit: Lifestyle medicine for keeping mentally healthy”, American Journal of Lifestyle Medicine, Vol. 10/3, pp. 193-199, https://doi.org/10.1177/1559827614536846.
[104] Donovan, R. et al. (2006), “Implementing mental health promotion: The Act-Belong-Commit mentally healthy WA campaign in Western Australia”, International Journal of Mental Health Promotion, Vol. 8/1, https://www.abcmentalsunnhet.no/wp-content/uploads/abc-mental-sunnhet/Implementing_Act-Belong-Commit.pdf.
[98] Donovan, R. et al. (2021), “Twenty-one reasons for implementing the Act-Belong-Commit – ‘ABCs of Mental Health’ campaign”, International Journal of Environmental Research and Public Health, Vol. 18/21, p. 11095, https://doi.org/10.3390/ijerph182111095.
[113] Drane, C. et al. (2023), “Impact of the Act-Belong-Commit campaign on mental health help-seeking behaviour”, Health Promotion Journal of Australia, Vol. 34/1, pp. 232-236, https://doi.org/10.1002/HPJA.605.
[116] Ekholm, O., K. Juel and L. Bonde (2016), “Associations between daily musicking and health: Results from a nationwide survey in Denmark”, Scandinavian Journal of Public Health, Vol. 44/7, pp. 726-732, https://doi.org/10.1177/1403494816664252.
[100] Elon University (n.d.), ABC Framework for a Mentally Healthy Elon, https://www.elon.edu/u/wellness-initiative/ (accessed on 5 June 2023).
[57] FINLEX (2021), Laki sosiaali- ja terveydenhuollon järjestämisestä, Finlex Data Bank, https://www.finlex.fi/fi/laki/ajantasa/2021/20210612.
[52] Finnish Institute of Occupational Health (2023), The Mental Health Toolkit, https://hyvatyo.ttl.fi/en/mental-health-toolkit (accessed on 1 September 2023).
[31] Fjellfeldt, M. (2023), “Developing mental health policy in Sweden: A policy analysis exploring how a complex societal challenge was consigned to individual citizens to solve”, Nordic Social Work Research, Vol. 13/1, pp. 4-20, https://doi.org/10.1080/2156857X.2021.1899968.
[25] Flintshire and Wrexham PSB (2023), Flintshire and Wrexham’s Wellbeing Plan 2023-2028, https://www.wrexhampsb.org/well-being-assessment/.
[28] Folkhälsomyndighete (2023), Nationell strategi för psykisk hälsa och suicidprevention, Public Health Agency of Sweden, https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/psykisk-halsa-och-suicidprevention/psykisk-halsa/nationell-strategi/.
[30] Folkhälsomyndighete (2023), Nationell strategi för psykisk hälsa och suicidprevention, https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/psykisk-halsa-och-suicidprevention/nationell-strategi/ (accessed on 5 September 2023).
[26] Folkhälsomyndighete (2021), Towards a Good and Equitable Health, Public Health Agency of Sweden, https://www.folkhalsomyndigheten.se/contentassets/bb50d995b033431f9574d61992280e61/towards-good-equitable-health.pdf.
[27] Folkhälsomyndighete (2020), Uppdrag att inkomma med underlag inför en kommande nationell strategi inom området psykisk hälsa och suicid-prevention, Public Health Agency of Sweden, https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/psykisk-halsa-och-suicidprevention/psykisk-halsa/nationell-strategi/#:~:text=Regeringen%20har%20gett%20Folkh%C3%A4lsomyndigheten%20och,flera%20andra%20akt%C3%B6rer%20i%20uppdraget.
[48] Forebygging (2023), Kongsvingermodellen – Bolig som grunnlag for psykisk helse hos barn og unge, https://www.forebygging.no/tiltak-i-program-for-folkehelsearbeid-i-kommunene/Kongsvingermodellen-Bolig-som-grunnlag-for-psykisk-helse-hos-barn-og-unge/.
[120] Forebygging (2022), SAMMEN i oppvekstfellesskapet. Samskaping Av Mobiliserende Møteplasser og voksEnNettverk i oppvekstfellesskapet, https://www.forebygging.no/tiltak-i-program-for-folkehelsearbeid-i-kommunene/SAMMEN-i-oppvekstfellesskapet-Samskaping-Av-Mobiliserende-Moteplasser-og-voksEnNettverk-i-oppvekstfellesskapet/.
[94] Freire, K. et al. (2022), “Engaging with children and adolescents: A systematic review of participatory methods and approaches in research informing the development of health resources and interventions”, Adolescent Research Review, Vol. 7/3, pp. 335-354, https://doi.org/10.1007/s40894-022-00181-w.
[15] Fujisaki, T. et al. (2016), “Does REDD+ ensure sectoral coordination and stakeholder participation? A comparative analysis of REDD+ national governance structures in countries of Asia-Pacific region”, Forests, Vol. 7/9, p. 195, https://doi.org/10.3390/f7090195.
[21] Future Generations Commissioner for Wales (2023), Well-being of Future Generations (Wales) Act 2015, https://www.futuregenerations.wales/about-us/future-generations-act/.
[40] Gotaas, N., H. Bergsli and O. Danielsen (2022), Midtveisevaluering av Program for folkehelsearbeid i kommunene 2017-2027, The Institute for Urban and Regional Research (NIBR), https://www.oslomet.no/om/nibr/publikasjoner.
[68] Government of Canada (2023), Health of People in Canada Dashboard, Public Health Agency of Canada, https://health-infobase.canada.ca/health-of-people-in-canada-dashboard/.
[43] Government of Canada (2023), Mental Health Promotion Innovation Fund, Public Health Agency of Canada, https://www.canada.ca/en/public-health/services/funding-opportunities/mental-health-promotion-innovation-fund.html.
[85] Government of Canada (2023), Public Health Agency of Canada (PHAC) Mental Health Promotion Innovation Fund, https://www.canada.ca/en/public-health/services/publications/diseases-conditions/infographic-mental-health-wellbeing-children-youth-protective-factors.html.
[82] Government of Canada (2023), Public Health Agency of Canada’s Innovation Strategy: A Strategic Funding Model, Public Health Agency of Canada, https://www.canada.ca/en/public-health/services/innovation-strategy.html.
[71] Government of Canada (2022), Budget 2022 Impacts Report, Department of Finance, https://www.budget.canada.ca/2022/report-rapport/gdql-egdqv-02-en.html.
[128] Government of Canada (2022), Chief Public Health Officer of Canada’s Report on the State of Public Health in Canada 2022, Public Health Agency of Canada, https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/state-public-health-canada-2022/report.html#appa.
[74] Government of Canada (2022), Inequalities in the Mental Health of Adults before and during the COVID-19 Pandemic: Data Tool, https://health-infobase.canada.ca/covid-19/mental-health-inequalities/index.html.
[75] Government of Canada (2022), Map of Canadian Mental Health during the COVID-19 Pandemic, https://health-infobase.canada.ca/covid-19/mental-health/.
[69] Government of Canada (2022), Public Health Agency of Canada 2021-22 Departmental Results Report, Public Health Agency of Canada, https://www.canada.ca/en/public-health/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022.html.
[65] Government of Canada (2014), Mental Health Promotion, https://www.canada.ca/en/public-health/services/health-promotion/mental-health/mental-health-promotion.html.
[32] Government of Sweden (2019), För att börja med något nytt måste man sluta med något gammalt, https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2019/01/sou-201890/.
[117] Haug, M. et al. (2021), “ABC (Act-Belong-Commit) for bedre psykisk helse hos voksne i Norge. En HUNT-studie”, Tidsskrift for psykisk helsearbeid, Vol. 18/2, pp. 175-187, https://doi.org/10.18261/ISSN.1504-3010-2021-02-05.
[42] Helgesen, M., D. Abebe and A. Schou (2017), Oppmerksomhet mot barn og unge i folkehelsearbeidet: Nullpunktsundersøkelse for Program for folkehelsearbeid settes i verk, https://www.helsedirektoratet.no/tema/folkehelsearbeid-i-kommunen/program-for-folkehelsearbeid-i-kommunene/Oppmerksomhet%20mot%20barn%20og%20unge%20i%20folkehelsearbeidet%20-%20Rapport%20NIBR%20NOVA%202017.pdf/_/attachment/inline/6d05dd13-60dc-4c31-85d3-a.
[39] Helsedirektoratet (2023), Program for folkehelsearbeid i kommunene, Norwegian Directorate of Health, https://www.helsedirektoratet.no/tema/folkehelsearbeid-i-kommunen/program-for-folkehelsearbeid-i-kommunene#bakgrunnforprogrammet.
[41] Helsedirektoratet (2021), Webinarer om folkehelsearbeid i kommunen, Norwegian Directorate of Health, https://www.helsedirektoratet.no/tema/folkehelsearbeid-i-kommunen/program-for-folkehelsearbeid-i-kommunene/webinarer-om-folkehelsearbeid-i-kommunen#lanseringavveiviserforpsykiskhelseoglivskvalitet%E2%80%93april.
[129] Helsedirektoratet (2017), The Norwegian Public Health Act: And a new initiative on well-being and drug prevention, Norwegian Directorate of Health, https://www.sm.ee/sites/default/files/content-editors/eesmargid_ja_tegevused/Norra_toetused/Rahvatervise_programm/the_norwegian_public_health_act.pdf.
[103] Hinrichsen, C. et al. (2020), “Implementing mental health promotion initiatives – Process evaluation of the ABCs of mental health in Denmark”, International Journal of Environmental Research and Public Health, Vol. 17/16, p. 5819, https://doi.org/10.3390/ijerph17165819.
[121] Hope, S. et al. (2021), “Abstracts presented at the Norwegian Public Health conference, October 27-29, 2021, Trondheim, Norway”, Scandinavian Journal of Public Health, Vol. 49/S1, pp. 1-28, https://doi.org/10.1177/14034948211046925.
[16] Karré, P., M. Van der Steen and M. Van Twist (2013), “Joined-up government in the Netherlands: Experiences with program ministries”, International Journal of Public Administration, Vol. 36/1, pp. 63-73, https://doi.org/10.1080/01900692.2012.713295.
[44] KDE Hub (2023), Enhanced Wellness of Newcomer Children, Youth, and Families, Knowledge Development and Exchange (KDE) Hub, https://kdehub.ca/projects/mhp-if/enhance-wellness-of-refugee-children-youth-and-families-2/.
[47] KDE Hub (2023), Families in TRANSition, Knowledge Development and Exchange (KDE) Hub, https://kdehub.ca/projects/mhp-if/families-in-transition-fit-2/.
[46] KDE Hub (2023), FOXY Mental Health Intervention, Knowledge Development and Exchange (KDE) Hub, https://kdehub.ca/projects/mhp-if/foxy-mental-health-intervention-building-resiliency-coping-skills-and-strengthening-mental-health-among-youth-in-the-northwest-territories-through-the-arts-2/.
[45] KDE Hub (2023), Mind Your Food, Knowledge Development and Exchange (KDE) Hub, https://kdehub.ca/projects/mhp-if/mind-your-food-2/.
[17] Kokkinen, L. et al. (2017), “Taking health into account in all policies: Raising and keeping health equity high on the political agenda”, Journal of Epidemiology and Community Health, Vol. 71/8, pp. 745-746, https://doi.org/10.1136/jech-2016-207736.
[102] Koushede, V. and R. Donovan (2022), “Applying salutogenesis in community-wide mental health promotion”, in The Handbook of Salutogenesis, Springer International Publishing, Cham, https://doi.org/10.1007/978-3-030-79515-3_44.
[127] Lee, N. and K. Salmond (2021), “Monitoring vested health partnerships”, Canadian Journal of Public Health, Vol. 112/S2, pp. 231-245, https://doi.org/10.17269/s41997-021-00515-6.
[125] Lillefjell, M. et al. (2022), “A salutogenic, participatory and settings-based model of research for the development and evaluation of complex interventions: The Trøndelag model for public health work”, in Global Handbook of Health Promotion Research, Vol. 1, Springer International Publishing, Cham, https://doi.org/10.1007/978-3-030-97212-7_26.
[130] Lillefjell, M. et al. (2023), “Planning for health equity: How municipal strategic documents and project plans reflect intentions instructed by the Norwegian Public Health Act”, Societies, Vol. 13/3, p. 74, https://doi.org/10.3390/soc13030074.
[124] Lillefjell, M. and R. Maass (2021), “Involvement and Multi-Sectoral Collaboration: Applying Principles of Health Promotion during the Implementation of Local Policies and Measures – A Case Study”, Societies, Vol. 12/1, p. 5, https://doi.org/10.3390/soc12010005.
[123] Lillefjell, M. et al. (2018), “Governance for public health and health equity: The Tröndelag model for public health work”, Scandinavian Journal of Public Health, Vol. 46/22, pp. 37-47, https://doi.org/10.1177/1403494818765704.
[132] Lumell Associates (2021), Analys Av Svenska Styrdokument Som Berör Området Psykisk Hälsa Och Suicidprevention, Lumell Associates, Stockholm, https://lumell.se/wp-content/uploads/2021/10/Analys-av-svenska-styrdokument-som-beror-omradet-psykisk-halsa-och-suicidprevention.pdf.
[131] Lumell Associates (2021), Internationell Utblick: Andra Länders Och Internationella Organisationers Strategier För Psykisk Hälsa Och Suicidprevention, Lumell Associates, Stockholm, https://lumell.se/wp-content/uploads/2021/10/Internationell-utblick-Andra-landers-och-internationella-organisationers-strategier-for-psykisk-halsa-och-suicidprevention.pdf.
[12] Lundberg, O. (2020), “Next steps in the development of the social determinants of health approach: The need for a new narrative”, Scandinavian Journal of Public Health, Vol. 48/5, pp. 473-479, https://doi.org/10.1177/1403494819894789.
[107] Meilstrup, C. et al. (2022), “The Act-Belong-Commit ‘ABCs of Mental Health’ campaign for mental health promotion”, Open Access Government, Vol. 36/1, pp. 182-183, https://doi.org/10.56367/OAG-036-10437.
[56] Mental Health and Wellbeing Commission (2023), Bigger Role for Mental Health and Addiction Peer Support Workforce Called For, https://www.mhwc.govt.nz/news-and-resources/bigger-role-for-mental-health-and-addiction-peer-support-workforce-called-for/.
[87] Mental Health and Wellbeing Commission (2023), He Ara Āwhina (Ngā ara Tautoko) te tarāwaho / He Ara Āwhina (pathways to support) framework, https://www.mhwc.govt.nz/our-work/assessing-and-monitoring-the-mental-health-and-addiction-system/.
[90] Mental Health and Wellbeing Commission (2022), He Ara Oranga te tarāwaho putanga toiora / He Ara Oranga wellbeing outcomes framework, https://www.mhwc.govt.nz/our-work/he-ara-oranga-wellbeing-outcomes-framework/.
[38] Mental Health and Wellbeing Commission (2022), Strategy on a Page 2022-2026, https://www.mhwc.govt.nz/assets/Strategy-on-a-Page/THM-Strategy-English-version.pdf.
[133] Mental Health and Wellbeing Commission (2022), Te Hiringa Mahara Annual Report 2021/22, https://www.mhwc.govt.nz/assets/Annual-Reports/2021/22/Te-Hiringa-Mahara-Annual-Report-2022-PDF.pdf.
[81] Mental Health Commission (2023), Western Australian Mental Wellbeing Guide, Government of Western Australia, https://www.mhc.wa.gov.au/about-us/major-projects/mental-wellbeing-guide/.
[79] Mental Health Commission (2018), Western Australian Mental Health Promotion, Mental Illness, Alcohol and Other Drug Prevention Plan 2018-2025, Government of Western Australia, https://www.mhc.wa.gov.au/about-us/strategic-direction/the-western-australian-mental-health-promotion-mental-illness-alcohol-and-other-drug-prevention-plan-2018-2025/.
[63] Mental Health Commission of Canada (2012), Changing Directions, Changing Lives: The Mental Health Strategy for Canada, https://www.mentalhealthcommission.ca/wp-content/uploads/drupal/MHStrategy_Strategy_ENG.pdf.
[55] Mentally Healthy WA (2023), Mentally Healthy Schools, Act Belong Commit, https://www.actbelongcommit.org.au/programs-initiatives/mentally-healthy-schools/.
[54] Mentally Healthy WA (2019), ABC for Mental Health in the Faroe Islands, Act Belong Commit, https://www.actbelongcommit.org.au/news/abc-for-mental-health-in-the-faroe-islands/.
[106] Ministry for the Interior and Health (2022), Bred aftale om en 10-årsplan for psykiatrien og mental sundhed, Ministry for the Interior and Health, Copenhagen, https://sum.dk/nyheder/2022/september/bred-aftale-om-en-10-aarsplan-for-psykiatrien-og-mental-sundhed.
[134] Ministry of Health and Care Services (2011), The Norwegian Public Health Act, https://www.regjeringen.no/globalassets/upload/hod/hoeringer-fha_fos/123.pdf.
[34] Ministry of Health and Social Affairs (2023), Draft Resolution on Mental Health Promotion Published, Government of Finland, https://stm.fi/en/-/draft-resolution-on-mental-health-promotion-published.
[108] Ministry of Labour and Social Inclusion (2022), Government launches new public health campaign focusing on mental health, Government of Norway, https://www.regjeringen.no/en/aktuelt/government-launches-new-public-health-campaign-focusing-on-mental-health/id2912322/.
[33] Ministry of Social Affairs and Health (2020), National Mental Health Strategy and Programme for Suicide Prevention 2020-2030, Government of Finland, https://julkaisut.valtioneuvosto.fi/handle/10024/162234.
[14] Mondal, S., S. Van Belle and A. Maioni (2021), “Learning from intersectoral action beyond health: A meta-narrative review”, Health Policy and Planning, Vol. 36/4, pp. 552-571, https://doi.org/10.1093/heapol/czaa163.
[10] National Collaborating Centre for Healthy Public Policy (2022), Wellbeing Budgeting: A Critical Public Health Perspective Invited Commentary, https://ccnpps-ncchpp.ca/docs/2022-Wellbeing-Budgeting-A-Critical-Public-Health-Perspective.pdf.
[88] New Zealand Government (2022), Mental Health and Wellbeing Commission, https://www.mhwc.govt.nz/.
[86] New Zealand Government (2018), He Ara Oranga: Report of the Government Inquiry into Mental Health and Addiction, https://mentalhealth.inquiry.govt.nz/inquiry-report/he-ara-oranga/.
[105] Nielsen, L. et al. (2017), “’Mental health is what makes life worth living’: An exploration of lay people’s understandings of mental health in Denmark”, International Journal of Mental Health Promotion, Vol. 19/1, pp. 26-37, https://doi.org/10.1080/14623730.2017.1290540.
[49] NTNU (2023), Liten og ny i barnehagen: Folkehelseprosjekt i Trondheim kommune 2018-2023, Norwegian University of Science and Technology (NTNU), https://litenogny.com/information-in-english/.
[119] NTNU (2020), Delrapport for folkehelseprosjektet “Liten og ny i barnehagen” Evaluering 2020, Norwegian University of Science and Technology (NTNU), https://litenogny.com/wp-content/uploads/2021/06/Delrapport-for-folkehelseprosjektet-Liten-og-ny-i-barnehagen-Evaluering-2020_med-omslag.pdf.
[19] OECD (2023), Economic Policy Making to Pursue Economic Welfare: OECD Report for the G7 Finance Ministers and Central Bank Governors, OECD Publishing, Paris, https://www.oecd.org/economy/G7_Beyond_GDP_Economic_policy_making_to_pursue_economic_welfare_2023.pdf.
[36] OECD (2023), Ready for the Next Crisis? Investing in Health System Resilience, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/1e53cf80-en.
[3] OECD (2022), Guidebook on Best Practices in Public Health, OECD Publishing, Paris, https://doi.org/10.1787/4f4913dd-en.
[1] OECD (2021), A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill-Health, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/4ed890f6-en.
[5] OECD (2021), COVID-19 and Well-being: Life in the Pandemic, OECD Publishing, Paris, https://doi.org/10.1787/1e1ecb53-en.
[2] OECD (2021), Fitter Minds, Fitter Jobs: From Awareness to Change in Integrated Mental Health, Skills and Work Policies, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/a0815d0f-en.
[20] OECD (2020), How’s Life? 2020: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9870c393-en.
[76] Ooi, L. et al. (2023), “Social isolation, loneliness and positive mental health among older adults in Canada during the COVID-19 pandemic”, Health Promotion and Chronic Disease Prevention in Canada, Vol. 43/4, pp. 171-181, https://doi.org/10.24095/hpcdp.43.4.02.
[64] Orpana, H. et al. (2016), “Monitoring positive mental health and its determinants in Canada: The development of the Positive Mental Health Surveillance Indicator Framework”, Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, Vol. 36/1, pp. 1-10, https://doi.org/10.24095/HPCDP.36.1.01.
[89] Parliamentary Council Office (2022), Mental Health and Wellbeing Commission Act 2020, Government of New Zealand, https://www.legislation.govt.nz/act/public/2020/0032/latest/whole.html#LMS281167.
[66] Public Health Agency of Canada (2023), Positive Mental Health Surveillance Indicator Framework, Public Health Agency of Canada, Centre for Surveillance and Applied Research, https://health-infobase.canada.ca/positive-mental-health/Index.
[67] Public Health Ottawa (2018), Status of Mental Health in Ottawa, https://www.ottawapublichealth.ca/en/reports-research-and-statistics/resources/Documents/mental_health_report_2018_en.pdf.
[110] Riley, B. et al. (2022), “Pause, re-think, go virtual … Pandemic adaptations from 20 diverse mental health promotion intervention projects across Canada”, Mental Health & Prevention, Vol. 26, p. 200235, https://doi.org/10.1016/j.mhp.2022.200235.
[59] Rotko, T. et al. (2022), “Mielenterveysstrategian ja mielenterveysvaikutusten ennakkoarvioinnin nykytila Suomessa ja maailmalla”, Research in Focus, No. 59, National Institute for Heath and Welfare (THL), https://www.julkari.fi/handle/10024/145616.
[84] Salmond, K. and S. Mahato (2021), “Linking to and addressing the determinants of health: A review of the Innovation Strategy experience”, Canadian Journal of Public Health, Vol. 112/S2, pp. 220-230, https://doi.org/10.17269/s41997-021-00518-3.
[114] Santini, Z. et al. (2017), “The protective properties of Act-Belong-Commit indicators against incident depression, anxiety, and cognitive impairment among older Irish adults: Findings from a prospective community-based study”, Experimental Gerontology, Vol. 91, pp. 79-87, https://doi.org/10.1016/j.exger.2017.02.074.
[118] Santini, Z. et al. (2022), “Impact evaluation of the “ABCs of Mental Health” in Denmark and the role of mental health-promoting beliefs and actions”, Mental Health and Social Inclusion, Vol. 26/3, pp. 271-291, https://doi.org/10.1108/MHSI-03-2022-0014.
[115] Santini, Z. et al. (2017), “The association between Act-Belong-Commit indicators and problem drinking among older Irish adults: Findings from a prospective analysis of the Irish Longitudinal Study on Ageing (TILDA)”, Drug and Alcohol Dependence, Vol. 180, pp. 323-331, https://doi.org/10.1016/J.DRUGALCDEP.2017.08.033.
[13] Scheele, C., I. Little and F. Diderichsen (2018), “Governing health equity in Scandinavian municipalities: The inter-sectorial challenge”, Scandinavian Journal of Public Health, Vol. 46/1, pp. 57-67, https://doi.org/10.1177/1403494816685538.
[91] Schreiber, M. (2020), “Sweden’s new mental health strategy will include Sámi for the first time”, ArcticToday, https://www.arctictoday.com/swedens-new-mental-health-strategy-will-include-sami-for-the-first-time/.
[70] Statistics Canada (2023), Infosheet: Quality of Life Framework for Canada, https://www160.statcan.gc.ca/infosheet-infofiche-eng.htm.
[92] Sylte, M. et al. (2023), “‘Nothing gets realised anyway’: Adolescents’ experience of co-creating health promotion measures in Municipalities in Norway”, Societies, Vol. 13/4, p. 89, https://doi.org/10.3390/SOC13040089.
[96] Sylte, M., M. Lillefjell and K. Anthun (2023), “Co-creating public health measures with adolescents in municipalities: Municipal actors’ views on inhibitors and promoters for adolescent involvement”, Scandinavian Journal of Public Health, pp. 1-9, https://doi.org/10.1177/14034948231170430.
[23] The Future Generations Commissioner for Wales (2023), Public Services Boards, https://www.futuregenerations.wales/work/public-service-boards/.
[35] THL (2023), Health and Welfare Promotion, Finnish Institute for Health and Welfare, https://thl.fi/en/web/thlfi-en/statistics-and-data/statistics-by-topic/health-and-welfare-promotion.
[58] THL (2023), Human Impact Assessment, Finnish Institute for Health and Welfare, https://thl.fi/en/web/management-of-health-and-wellbeing-promotion/management-of-wellbeing/practices/human-impact-assessment.
[50] THL (2023), IPS – Individual Placement and Support Project, Finnish Institute for Health and Welfare, https://thl.fi/en/web/thlfi-en/research-and-development/research-and-projects/ips-individual-placement-and-support-project.
[61] THL (2023), Mielenterveysvaikutusten ennakkoarviointi, https://thl.fi/fi/web/mielenterveys/mielenterveysvaikutusten-ennakkoarviointi (accessed on 1 September 2023).
[51] THL (2023), Työkyvyn ja työllistymisen tuki, Finnish Institute for Health and Welfare, https://thl.fi/fi/tutkimus-ja-kehittaminen/tutkimukset-ja-hankkeet/suomen-kestavan-kasvun-ohjelma-rrp-/tyokyvyn-ja-tyollistymisen-tuki.
[18] Tooher, R. et al. (2016), “Intersectoral collaboration to implement school-based health programmes: Australian perspectives”, Health Promotion International, Vol. 32/2, pp. 312-321, https://doi.org/10.1093/heapro/dav120.
[4] Von Heimburg, D. et al. (2022), “From public health to public good: Toward universal wellbeing”, Scandinavian Journal of Public Health, Vol. 50/7, pp. 1062-1070, https://doi.org/10.1177/14034948221124670.
[78] Walsh, O., A. Sheridan and M. Barry (2023), “The process of developing a mental health promotion plan for the Irish health service”, Advances in Mental Health, Vol. 21/2, pp. 1-14, https://doi.org/10.1080/18387357.2022.2161402.
[22] Welsh Government (n.d.), Public Services Boards, https://www.gov.wales/public-services-boards (accessed on 5 July 2023).
[8] Whiteford, H. et al. (2014), “System-level intersectoral linkages between the mental health and non-clinical support sectors: A qualitative systematic review”, Australian & New Zealand Journal of Psychiatry, Vol. 48/10, pp. 895-906, https://doi.org/10.1177/0004867414541683.
[7] WHO (2013), What You Need to Know about Health in All Policies, World Health Organization, https://www.who.int/social_determinants/publications/health-policies-manual/key-messages-en.pdf.
[11] WHO and European Observatory on Health Systems and Policies (2023), Making Health for All Policies: Harnessing the co-benefits of health, World Health Organization and the European Observatory on Health Systems and Policies, https://eurohealthobservatory.who.int/publications/i/making-health-for-all-policies-harnessing-the-co-benefits-of-health#:~:text=Health%20for%20All%20Policies%20complements,bring%20other%20sectors%20on%20board.
[24] Wrexham PSB (2022), An Assessment of Well-being: Wrexham County Borough, Wrexham Public Services Board, https://www.wrexhampsb.org/well-being-assessment/.
[111] Wrexham University (2023), North Wales Public Service Lab, https://glyndwr.ac.uk/about/civic-mission/leadership-and-whole-systems-working/.
[53] Wrexham University (n.d.), Children’s University, https://glyndwr.ac.uk/childrens-university/ (accessed on 5 July 2023).
Notes
← 1. The respective initiatives were selected from a larger initial list of mental health activities that was presented to the OECD Working Party on Social Policy in early 2022, based on country interest to be featured. The Secretariat in some instances actively reached out to programmes that applied specific aspects of a well-being policy approach to mental health in an innovative way.
← 2. In Ireland, the Department of Health is currently developing a Mental Health Promotion Plan. While this activity is not a case study featured in depth in this chapter, an independent report carried out by the Health Promotion Research Centre at the University of Galway in support of the Mental Health Promotion Plan recommended the Well-being Framework for Ireland, launched by the Government in 2022, could provide an overarching structure for integrating cross-sectoral policy actions that address the structural determinants of population of mental health and well-being (Barry, Keppler and Sheridan, 2023[37]).
← 3. The Future Generations Act also mandates public bodies to adhere to “five ways of working”, or principles they must demonstrate in their decision making to show that they are acting in accordance with sustainable development. They are collaboration (acting in collaboration with any other person or different parts of the body itself that could help the body to meet its well-being objectives), integration (considering how the public body’s well-being objectives may impact upon each of the well-being goals, on their other objectives, or on the objectives of other public bodies), involvement (the importance of involving people with an interest in achieving the well-being goals and ensuring that those people reflect the diversity of the area which the body serves), long-term (the importance of balancing short-term needs with the need to safeguard the long-term needs), and prevention (how acting to prevent problems occurring or getting worse may help public bodies meet their objectives) (Future Generations Commissioner for Wales, 2023[21]).
← 4. Aside from the leading agencies, other government agencies involved in the strategy include: The Swedish Work Environment Authority, the Public Health Agency of Sweden, the Swedish Research Council for Health, Working Life and Welfare (Forte), the Swedish Social Insurance Agency, the Health and Social Care Inspectorate (IVO), the Swedish Gender Equality Agency, the Swedish Prison and Probation Service, the Medical Products Agency, the Swedish Migration Agency, the Swedish Agency for Work Environment Knowledge, the Swedish Agency for Participation (MFD), the Swedish Agency for Family Law and Parenthood Support (MFoF), the Swedish Civil Contingencies Agency (MSB), the Swedish Agency for Youth and Civil Society (MUCF), the Swedish Police Authority, The National Board of Forensic Medicine, the Sámi Parliament, the National Board of Health and Welfare, the National Agency for Special Needs Education (SPSM), the Swedish Agency for Medical and Social Evaluation (SBU), the National Board of Institutional Care (SIS), the Swedish Media Council, the National Agency for Education, the Swedish Transport Administration, the Swedish Research Council, Vinnova (Folkhälsomyndighete, 2023[28]).
← 5. This plan shifted mental health efforts in the country towards prevention and promotion at the population level, moving away from a narrower focus on severe mental ill-health and clinical care that shaped earlier efforts.
← 6. Ministries include: the Ministry of Defence, Ministry of Transport and Communications, Ministry of Finance, Ministry of Economic Affairs and Employment, Ministry of Justice, Ministry of Education and Culture, Ministry of the Interior, Ministry of Agriculture and Forestry and the Ministry of the Environment. Only one government ministry – the Ministry for Foreign Affairs – is not engaged in the work.
← 7. Compared to the National Mental Health Strategy, the Draft Resolution on Mental Health Promotion further emphasises the importance of the climate and the environment in mental health promotion, which is a topic also included in different ministries’ strategies and plans (Ministry of Health and Social Affairs, 2023[34]).
← 8. Separately, the National Board of Health and Welfare and the Public Health Agency commissioned two studies to map the existing knowledge base of health strategy development best practice. The first looks at previous experiences with policy and legislation relating to mental health and suicide prevention in Sweden (Lumell Associates, 2021[132]); the second looks at other countries’ (or international organisations’) experiences in drafting national strategies, pulling lessons from Denmark, Finland, England, Scotland, the Netherlands Canada, Australia, New Zealand, the EU and the WHO (Lumell Associates, 2021[131]).
← 9. In addition to the 26 government agencies involved, the two leading agencies held twice annual consultations with other government and/or external stakeholders, including local authorities and civil society organisations. Some agencies involved in the development process have expressed a desire for these entities to have been consulted with more frequently, given the depth of knowledge of many in the civil society, and the fact that regional and municipal authorities are concurrently developing a regional mental health strategy.
← 10. The Commission’s work builds off previous government strategies on mental health. In 2018 the New Zealand government launched an official inquiry into mental health and addiction: Pathway to Wellbeing (He Ara Oranga) (New Zealand Government, 2018[86]). It concluded with 40 recommendations to improve New Zealand’s policy approaches to mental health: one such recommendation was the establishment of an independent Mental Health and Wellbeing Commission to provide independent system leadership. While the Commission was being set up, a ministerial advisory committee – operating within the Ministry of Health – was created in 2020 to begin monitoring and reporting on the Government’s response to the He Ara Organa commission report, develop an outcomes framework to measure mental health and well-being, and support the establishment of the eventual independent Commission. The latter was officially inaugurated 14 months later, in February 2021.
← 11. In 2021-22, the Commission had 23 staff in permanent and fixed-term roles (Mental Health and Wellbeing Commission, 2022[133]). Per comparison, this is less than half the staff of the Human Rights Commission, another independent crown entity.
← 12. The 2012 Norwegian Public Health Act tasked municipalities with the promotion of health, well-being and their social determinants in local planning and service provision (Ministry of Health and Care Services, 2011[134]). Under the Public Health Act and following an HiAP approach, responsibility for public health work was transferred to municipalities to enables them to integrate public health considerations into all local development and planning, administration and the provision of services (Helsedirektoratet, 2017[129]). The central health authority remains involved in health promotion but takes a supporting role. A recent review of how four municipalities have reflected the Public Health Act in municipal plans and project-planning documents indicates awareness of public health work as a whole-of-municipality responsibility, but also shows public health process goals (e.g. cross-sectoral governance and working groups) have so far received more attention than outcomes (e.g. health equity) (Lillefjell et al., 2023[130]).
← 13. Although the majority of projects are indeed universal (meaning they are non-clinical strategies directed at an entire population that address generic mental health risk and protective factors), based on local needs, some projects may also target specific groups.
← 14. A final evaluation is also planned (Helsedirektoratet, 2023[39]).
← 15. Of course, realigning and redesigning are not mutually exclusive, in that the former is a precondition for the latter.
← 16. Forthcoming (2024) OECD work on best practices in mental health promotion and prevention will also include an evaluation of the ABC programme in terms of effectiveness, efficiency and equity, and assess its potential for transferability.
← 17. Wellbeing services counties in Finland are 21 public bodies separate from municipalities established under the 2021 reform of healthcare, social welfare and rescue services. Since January 2023, the responsibility for these services was transferred from municipalities to the wellbeing services counties.
← 18. Child and environmental IAs were most commonly used (reported by around 50% of municipalities), followed by IAs on land use and construction (43%) and business (33%). Gender and rural IAs were used by only around 5% of municipalities (Rotko et al., 2022[59]).
← 19. In several municipalities, mental health promotion and mental well-being strengthening activities are included in the welfare report municipalities are required by law to prepare every council term (FINLEX, 2021[57]).
← 20. The PMHSIF was also listed as an example of a public health surveillance activity related to addressing climate change in the 2022 Chief Public Health Officer of Canada’s Report on the State of Public Health (Government of Canada, 2022[128]).
← 21. Examples of systems change achieved through the Innovation Strategy projects included the redistribution of resources within family service centres to support mental health promotion programming as a core activity; changes in practice both within and outside of the health sector due to knowledge generated through Innovation Strategy projects; and the addition of mental health promotion programming and resources to the school curriculum. It should be noted that the “systems” are quite different across funded projects (e.g. the education system, the health system, the justice system, the local community), and each project defines their system and the key players within.
← 22. In the case of the Mental Health Promotion Innovation Fund, the long-term nature and flexibility of the funding model also allowed for a 1 year “pandemic extension” to provide projects the time to adapt and pivot to delivering online programming during the various stages of the COVID-19 pandemic.
← 23. Since 2016, the Western Australian Health Promotion Foundation (Healthway) is a statutory board under the Western Australian Health Promotion Foundation Act 2016.
← 24. Despite its name (“ABC”) being grounded by an English acronym, the programme has been successfully translated into other languages and cultural contexts, including Danish, Faroese, Norwegian, Swedish, Finnish and Japanese.
← 25. The Innovation Strategy created and applied a Scale-up Readiness Assessment Tool (SRAT) to assess the level of scale-up readiness of a funded project. The SRAT includes identifying predictors of success for the scale-up of effective population health interventions, organized into eight common characteristics: Intervention evidence and evaluation, reach and scale, organizational capacity, partnership development, system readiness, community context, cost factors, knowledge development and exchange (Bradley Dexter et al., 2021[126]).