Mental health is a vital component of people’s well-being, and measuring it is essential to monitor what ultimately matters to people. The aim of this report is to encourage official data producers to collect data on population mental health outcomes more frequently and in an internationally harmonised manner. Considering all aspects of mental health, ranging from mental ill-health (which may or may not include a diagnosed mental health condition) to positive mental states, can provide new avenues for a proactive rather than reactive design of mental health systems and services, and it can open up space for policy to focus on both reducing illness and promoting people’s flourishing. Collecting data on mental ill-health and positive mental health in household, social and health surveys would yield a more complete picture of mental health and help to better understand the drivers and policy levers for improving it.
Measuring Population Mental Health

1. What is population mental health and why should we measure it?
Abstract
Good mental health is a vital component of people’s well-being. Good mental health enables individuals to realise their own potential, cope with the stresses of life, work productively and make a positive contribution to their communities (World Health Organization, 2019[1]). Mental ill-health on the other hand accounts for one of the largest and fastest-growing categories of the burden of disease worldwide; its economic costs, including investment in the mental health system and lower employment and productivity, are estimated at more than 4% of GDP in OECD countries (Rehm and Shield, 2019[2]; OECD, 2021[3]). In 2016, already well before the COVID-19 pandemic, deaths of despair (due to suicide, acute alcohol abuse or drug overdose) were one of the largest causes of preventable deaths in OECD countries, six times higher on average than deaths due to homicide, and three times higher than road deaths (OECD, 2020[4]). Over the period 2016‑18, one in eight people living in OECD countries experienced more negative than positive emotions during a typical day (OECD, 2020[4]).
Mental health has come to the forefront of the public debate during COVID-19. Besides the direct effect of the pandemic in terms of the high number of lives lost, social isolation, loss of work and financial insecurity all led to a significant worsening of people’s mental health, with more than a quarter of people in 15 OECD countries experiencing symptoms of anxiety or depression by late 2020 (OECD, 2021[3]; OECD, 2021[5]). Populations living in vulnerable situations, including women, young people, those in precarious employment and financial situations, racial and ethnic minorities, and people living with existing mental health conditions and substance use disorders, have been particularly affected.
While it is clear that mental health matters for people’s well-being, and that substantial parts of the population are living with and affected by mental ill-health, discussion so far have not focused sufficiently on how governments should best monitor it at the broader population level, and on how to consider both mental ill-health and positive mental states. This also requires a conversation about what exactly is meant by “mental health” and about which outcomes are most relevant for policy makers responsible for treatment, prevention and promotion strategies.
This chapter first makes the case for why regular measures of population-level mental health outcomes should be collected. It then presents how different components of mental health, including mental ill-health and positive mental health, have been distinguished in research and practice.1 This provides the basis for a common understanding and terminology used throughout this report, including in the subsequent chapters on available measurement tools and current measurement activities in OECD countries (Chapter 2) and on what is known about their statistical quality and measurement practice (Chapter 3).
The importance of focusing on population mental health outcomes
The OECD has a long record of collating international health statistics and promoting a society-wide response to improving mental health. This includes the 2015 OECD Recommendation on Integrated Mental Health, Skills and Work Policy and its follow-up report, Fitter Minds, Fitter Jobs, as well as the recent publication A New Benchmark for Mental Health Systems, which sets out a framework for understanding mental health performance and assesses whether countries are delivering the policies and services that matter for health system performance (OECD, 2021[3]; OECD, 2015[6]; OECD, 2021[7]). Preventing mental illness, promoting mental well-being and taking a multisectoral approach to mental health are amongst the key principles of the OECD’s New Benchmark framework, and a number of population-level outcomes indicators are included under these principles (life satisfaction, suicide rate and inequalities in mental distress by education and employment status). In addition, the OECD How’s Life? reports (which assess well-being, inequality and sustainability in over 40 member and partner countries, see Box 1.1) also feature a range of outcome indicators relevant to mental health. However, several of these are produced irregularly, only cover a subset of OECD countries and in some cases are drawn from non-official sources.2
Box 1.1. Measuring people’s well-being
The OECD Well-being Framework is a broad outcome-focused tool to measure human and societal conditions and assess whether life as a whole is getting better for people living in OECD countries (OECD, 2020[4]). It includes both current well-being in the “here and now”, which focuses on living conditions at the individual, household and community levels, and systemic resources needed to sustain well-being in the future.3 The Well-being Framework underpins the OECD How’s Life? report series and a wide range of other OECD work related to well-being (for an overview, see https://www.oecd.org/wise/).
Figure 1.1. The OECD Well-being Framework
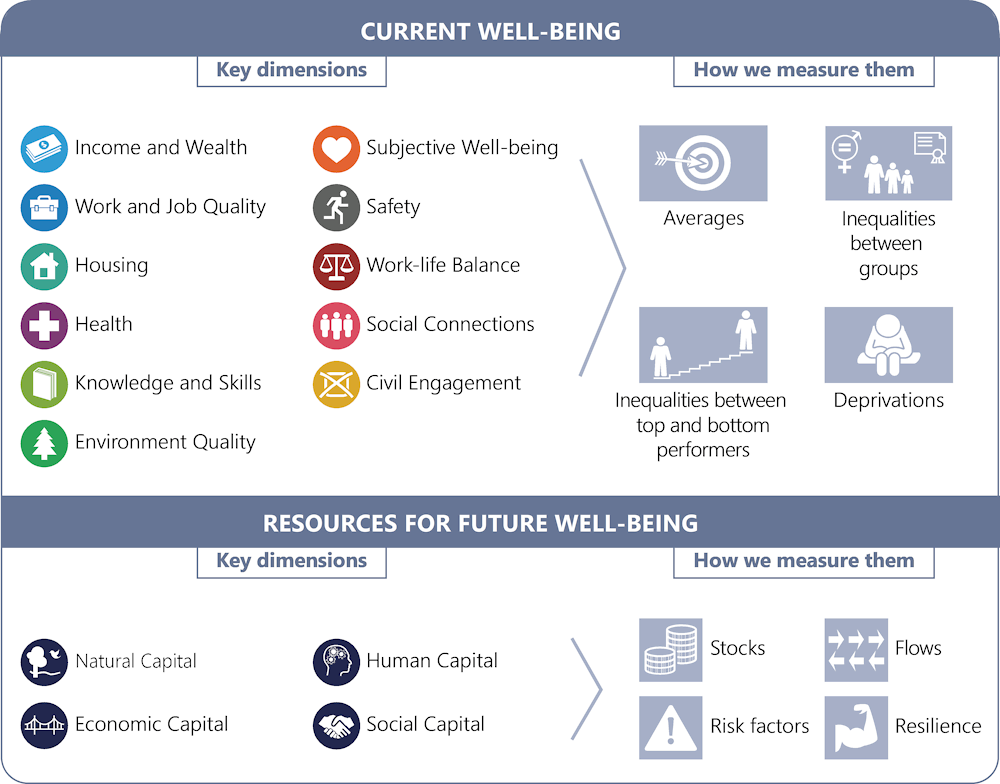
Source: OECD (2020[4]), How’s Life? 2020: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/23089679.
Mental health is not explicitly identified as a separate dimension of well-being in the framework, but mental health outcomes are relevant to several dimensions:
First, and foremost, the broad “health” dimension of the Framework encompasses both mental and physical health. For example, two indicators of mental ill-health (deaths from suicide, acute alcohol abuse and drug overdose, and the share of people at risk of depression) were included in the OECD How’s Life? 2020 report under this dimension.
Second, the “subjective well-being” dimension encompasses elements of good psychological functioning, notably eudaimonia and positive and negative affect. People’s own evaluation of their lives (e.g. life satisfaction) is also included here.
Last, “Human capital”, included under resources for future well-being, refers to “the knowledge, competencies, skills and health status of individuals, which are viewed here from the perspective of their contribution to future well-being” and includes indicators such as premature mortality and obesity prevalence (OECD, 2020[4]).4
In addition, several aspects of positive functioning that are often included in broad definitions of positive mental health, such as social connections, financial security (income and wealth), and knowledge and skills, are captured by separate dimensions within the OECD Well-being Framework.
The aim of this report is to encourage official data producers to collect data on population-level mental health outcomes more frequently and in an internationally harmonised manner. This is in line with a well-being approach that assesses what ultimately matters to people themselves and their capabilities to live a life of their choosing (in this case, feeling mentally healthy and free of mental distress) (OECD, 2020[4]). Moreover, several well-being drivers measured by more frequently available input or output indicators may be imperfectly correlated with such outcomes (e.g. mental health expenditure is a poor proxy of mental health status if the health care system is inaccessible; similarly, the number of drugs prescribed says little about people’s (mental) health conditions) (OECD, 2011[8]).
Collecting data on mental health status for the entire population, rather than only for people diagnosed or treated by health care professionals, is important for a number of reasons. First, measures focusing on the numbers diagnosed might only reflect how accessible and developed a country’s health care system is, and how likely people (and certain population groups) are to seek treatment. Second, strategies to prevent mental ill-health would benefit from identifying at-risk groups early on. So, they necessitate tracking outcomes prior to, and following, engagement with the health system. Third, positive mental health is a foundational asset for the population, and as such, is valuable to track in its own right Linking mental health with the broader risk and resilience factors typically also collected in population (survey) statistics, such as people’s material conditions, quality of life and social relationships (and inequalities in these), can equally support mental health strategies.
Concepts of mental health: From illness to wellness
Previous OECD work on mental health has adopted the widely accepted definition of mental health by the World Health Organisation (WHO): “a state of well-being in which the individual realises his or her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” (OECD, 2021[3]; OECD, 2015[6]). This definition explicitly states that mental health is not the absence of illness and encompasses multiple aspects of psychosocial functioning (World Health Organization, 1948[9]).5
Various theories about what mental health entails have been developed over the past decades. These range from those focusing on symptoms of mental illness either being present or not (“binary model”), to those conceiving of mental health as a spectrum of experience (“single-continuum model”), all the way to viewing mental ill-health and positive mental health as related but distinct experiences (“dual-continuum model”) (Figure 1.2). Each of these models carries different implications for which mental health outcomes need to be tracked in order in order to capture the concept in its entirety.
Figure 1.2. Models of mental health
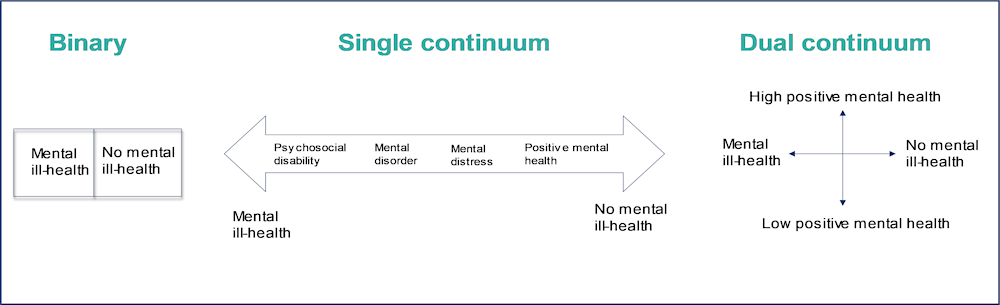
Source: Adapted from Iasiello et al. (2020[10]), “Mental Health and/or Mental Illness: A Scoping Review of the Evidence and Implications of the Dual-Continua Model of Mental Health”, Evidence Base, 10.21307/eb-2020-001.; Keyes, C. (2005[11]), “Mental illness and/or mental health? Investigating axioms of the complete state model of health”, Journal of Consulting and Clinical Psychology, 73(3): 539.
The binary model
Clinical psychology, psychiatry and research more generally have historically focused on the reduction of mental illness symptoms, or psychopathology, in order to improve mental health. In this “disease-centred” perspective, mental illness (in the form of conditions defined by psychiatric classification systems) is the focal concept, and the goal of intervention is primarily to help reduce the associated symptomatology, rather than to support people into wellness. In this perspective, an individual is capable of experiencing one of two alternative states: either being diagnosed as mentally ill or being presumed mentally healthy (Routledge et al., 2016[12]; Keyes, 2005[11]; Trent, 1992[13]).
Binary categorisations of mental illness can be useful, for instance, when a person is trying to access appropriate health care or other support services or for defining guidelines and treatment pathways to manage diagnosed conditions. However, practitioners and researchers have criticised the reductionist nature of this model, i.e. the notion of an arbitrary point where illness transitions to full health and the presumed impossibility of “gaining” more mental health once the threshold of no diagnosable condition is crossed (Herron and Trent, 2000[14]).
Mental health as a continuum
An alternative approach is to characterise mental health as a continuum of experience, from severe mental ill-health, on one end of the spectrum, through to positive mental health (high levels of emotional and psychological well-being) on the other (Patel et al., 2018[15]; Payton, 2009[16]; Greenblat, 2000[17]). This view is rooted in a “salutogenic” approach that focuses on factors that support health and well-being, beyond the traditional focus on risks, symptoms and problems. It acknowledges a wider breadth of people’s experiences (which are different for someone who might feel worried or has trouble sleeping compared to a person experiencing a full-blown episode of major depression).
In this model, “everyone has mental health”, and an individual can move up and down the spectrum throughout their life (including up to a daily or weekly basis) depending on the context they find themselves in, the challenges they face and the internal and external resources available to them. Some researchers have used the metaphor of a river, rather than a linear continuum, to express this constant process and the fluidity of different states between acute mental ill-health and positive mental health (Figure 1.3 (Koushede and Donovan, 2022[18])
Figure 1.3. The mental health continuum as a river
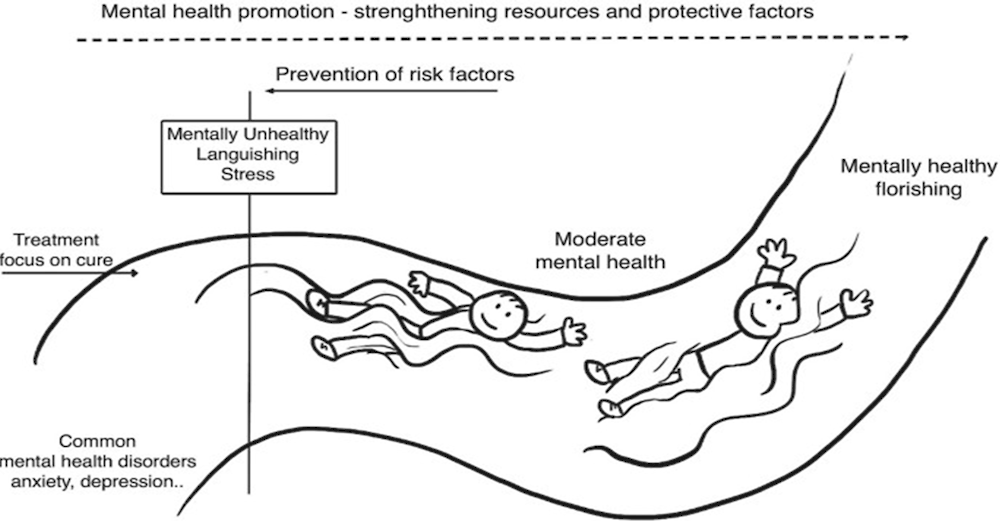
Source: Koushede, V. and R. Donovan (2022[18]), “Applying Salutogenesis in Community-Wide Mental Health Promotion”, The Handbook of Salutogenesis. Springer, Cham. https://doi.org/10.1007/978-3-030-79515-3_44.
From a policy perspective, considering the full spectrum between mental ill-health and positive mental health carries implications for both targeting and designing interventions and can provide new avenues for proactive rather than reactive system and service design. The single-continuum model adds value vis-à-vis the binary perspective by providing the space for mental health strategies to focus not just on “curing” (diagnosed) illness or reducing the associated symptoms, but also on preventing people in the middle of the spectrum from doing worse and on promoting mentally healthy populations.
Mental ill-health and positive mental health as a dual continuum
A third conceptual view, increasingly considered by international players such as the World Health Organisation, several public health agencies, national statistical offices and other government departments, more clearly differentiates between mental ill-health, on one side, and positive mental health, on the other (Statistics Canada, n.d.[19]; Australian Early Development Census, 2012[20]; Swiss Health Observatory, n.d.[21]; Government of Western Australia Mental Health Commission, 2021[22]; Queensland Government, 2015[23]) (World Health Organization, 2022[24]). This “dual-continuum” model characterises mental ill-health and positive mental states as related but distinct experiences (placing them on two different but intersecting continua), rather than as extreme ends of a single spectrum.6
Mental ill-health and positive mental health, or high levels of emotional and psychological well-being, are closely interconnected. Gains in good mental health at the population level imply declines in average mental disorders over time, while experiencing positive mental health decreases the risk of developing a mental disorder, can help recovery once it has been developed and is thus considered an important resilience factor (Keyes, Dhingra and Simoes, 2010[25]; Robinson, 2012[26]; Santini et al., 2022[27]).
Proponents of the dual-continuum model, however, argue that the association between ill-health and positive mental health is not linear, as the single-continuum model might suggest: the mere absence of clinically significant symptoms of mental ill-health, or diagnosed conditions, does not always imply a thriving mental state. Conversely, a person could have symptoms of a mental disorder and associated distress and disability, but also be satisfied with their life as a whole and achieving their potential (Galderisi et al., 2015[28]). This view, which aims to acknowledge the full diversity of human experiences, is also often echoed by people with lived experience of mental health conditions (New Zealand Initial Mental Health and Wellbeing Commission, 2020[29]).
The majority of research supporting a dual continuum has relied on confirmatory factor analysis (CFA) to compare whether survey data best fit a single- or dual-continuum model. Keyes (2005[11])measured aspects of emotional, psychological and social well-being7 and some common forms of mental illness (presence of a major depressive episode, generalised anxiety disorder, panic disorder, or alcohol dependence in the past year) in a nationally representative sample of US adults. He then used CFA to highlight the existence of two correlated but separate latent factors. Additional studies of non-US populations using a variety of measurement tools for both positive mental health and mental illness have further supported the notion of the dual-continuum model. A recent review identified 83 peer-reviewed empirical articles, including cross-sectional, longitudinal and intervention studies, which provided support for the superior explanatory power of dual-continuum models of mental health over a single-continuum model (Iasiello, van Agteren and Cochrane, 2020[10]; Routledge et al., 2016[12]).8
The typical visualisation of two completely orthogonal axes in the dual-continuum model can, however, be misleading. Several studies classify individuals into separate groups around the model’s quadrants, using variations of categories such as “complete mental health” (no mental illness, high positive mental health), “vulnerable” (low mental illness, low positive mental health), “symptomatic but content” (high mental illness, high positive mental health) and “struggling” (high mental illness, low positive mental health) (Iasiello, van Agteren and Cochrane, 2020[10]). Distributions within these categories, however, strongly suggest that levels of positive mental health and mental ill-health are highly related and that mental health conditions bring significant impairments for emotional and psychological well-being. For instance, a study of Australian schoolchildren shows that only around 5% of children experience either high levels of positive mental health but also mental ill-health, or low levels of positive mental health but no mental ill-health (Figure 1.4). Similarly, while in a study by Keyes only one in five people who had no diagnosed mental health condition in the past year recorded high positive mental health, even fewer respondents with a mental disorder were likely to do so (Table 1.1) (Keyes, 2005[11]).
In the same study, experiences of positive mental health also vary strongly according to the type of psychological disorder experienced in the past year (and its severity at the time of the survey), ranging from only 2% for those with generalised anxiety disorder to 8% for those who were alcohol-dependent (Table 1.1). Nevertheless, the share of respondents with a high degree of mental ill-health who can attain some degree of positive mental health is not insignificant. Lesser-known interlinkages between various aspects of emotional and psychological well-being and different, even severe, mental health conditions are also possible: some studies suggest that, compared to psychologically-healthy adults, people with depression might react to negative events with less distress, while people with bipolar disorder experience greater positive emotions during mania, people with schizophrenia can construct meaning from their hallucinations and delusions, and trauma survivors can live meaningful lives upon coping with their stressful experiences (Goodman, Doorley and Kashdan, 2018[30]).
Figure 1.4. The dual continuum of mental health in Australian children
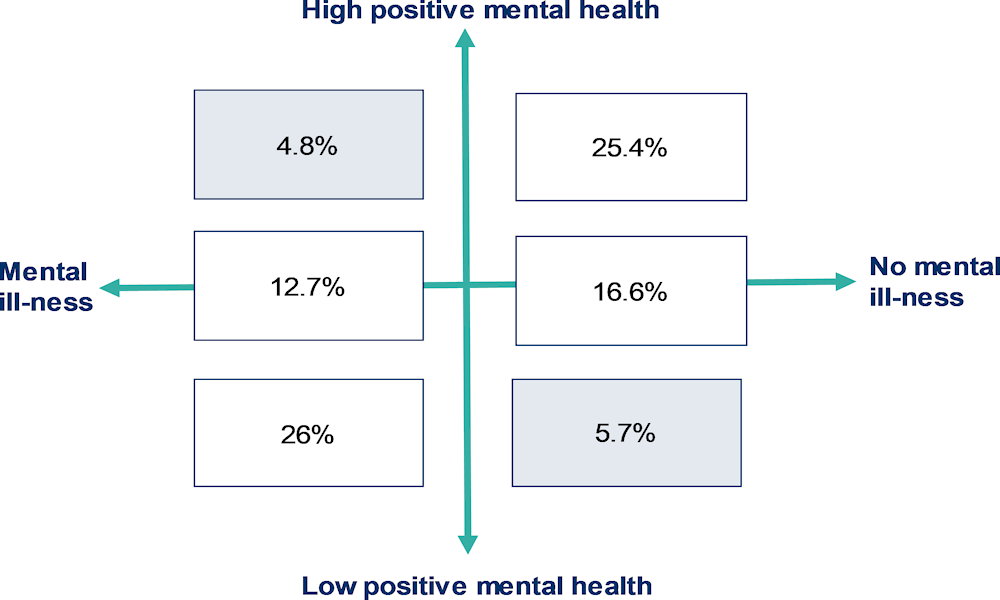
Note: Data are drawn from the 2012 national Australian Early Development Index, and responses about children were provided by their school teachers. Darker shaded fields refer the share of children who have either low positive mental health but no mental illness or those who experience mental illness but also high positive mental health. The original source termed these categories as mental health difficulties (e.g. anxiety disorders, depression, behavioural problems) and mental health competency (e.g. healthy psychosocial functioning).
Source: Australian Early Development Census (2012[20]), The mental health of Australian children: A dual continuum, https://www.aedc.gov.au/resources/detail/the-mental-health-of-australian-children-a-dual-continuum.
Table 1.1. Different mental health conditions influence the extent to which positive mental health is achievable
Share of adults with a mental health condition in the past 12 months that report low, moderate or high positive mental health, United States, 1994-95
|
Low positive mental health (languishing) |
Moderate positive mental health |
High positive mental health (flourishing) |
|
|---|---|---|---|
|
Overall sample (n=3032) |
16.9% |
65.1% |
18% |
|
Major depressive episode (n=422) |
33.9% |
60.2% |
6.2% |
|
Generalised anxiety disorder (n=98) |
55.1% |
41.8% |
2% |
|
Panic disorder (n=204) |
39.2% |
58.3% |
2.5% |
|
Alcohol dependence (n=194) |
24.7% |
69.1% |
7.7% |
|
Comorbidity (n=193) |
43.5% |
55.4% |
2.1% |
Note: Data are drawn from the “Midlife in the United States” study. Mental disorders were measured by the Composite International Diagnostic Interview Short Form (CIDI-SF) scale. Flourishing (languishing) was defined as an individual exhibiting high (low) levels on one of two questions about positive affect and high (low) levels on six of 11 questions about positive functioning (per Ryff’s scales of psychological well-being and Keyes’ scales of social well-being). All other respondents were categorised within moderate positive mental health. Comorbidity refers to the experience of more than one mental health condition, regardless of in which combination.
Source: Keyes, C. (2005[11]), “Mental illness and/or mental health? Investigating axioms of the complete state model of health”, Journal of Consulting and Clinical Psychology, 73(3): 539.
By distinguishing between mental ill-health and positive mental health, the dual-continuum model also implicitly suggests that the relative importance of their respective drivers differs. This is important for policy and clinical practice, as the same strategies for preventing mental illness might not be sufficient for enhancing positive mental states, and vice versa. Evidence on this is still emerging. Some population-based studies from Denmark and England have suggested that deprivations in people’s material conditions and quality of life (such as low income and educational attainment, lack of employment and financial insecurity) predict outcomes at the tail-end of each continuum (i.e. both mental ill-health and low levels of positive mental health). These same socio-economic factors did not play an equally strong role in determining high levels of positive mental health (Stewart-Brown et al., 2015[31]; Nielsen et al., 2016[32]; Santini et al., 2020[33]). However, population-based data from Canada and Slovenia suggests that higher financial security and household income are indeed associated with increased odds of psychological well-being (Varin et al., 2020[34]; Vinko et al., 2022[35]). By contrast, relational factors such as greater social connectedness, improved family relations and participation in recreational activities have been associated with both reduced risk of mental health conditions as well as higher positive mental health in the majority of studies (Van Lente et al., 2012[36]; Santini et al., 2020[33]; Santini et al., 2017[37]; Solin et al., 2019[38]; Thoits, 2011[39]).
The value-add of the dual-continuum model (over the single continuum) is that it more explicitly communicates that both mental ill-health and good mental states impact people’s lives. From a measurement perspective, the dual-continuum model suggests that collecting data on both mental health and positive functioning in population surveys and health assessments would yield a more complete picture of mental health. This would also help to identify the factors, and by extension policy levers, associated with the dual goals of improving positive mental health and reducing mental illness. This report hence considers the two constructs separately where possible and defines each in more detail in the following sections.
Mental ill-health
The term mental ill-health refers to diagnosable mental and behavioural conditions, as well as the transdiagnostic characteristic of psychological distress.
Mental health conditions
The terms “conditions” or “disorders” are used in this report to describe symptoms reaching the clinical threshold of a diagnosis according to psychiatric classification systems such as the World Health Organization International Classification of Disease (ICD) or the American Psychiatric Association Diagnostic and Statistical Manual (DSM).9 There are more than one hundred separate diagnoses and disorders featured in these classification systems, including mild or moderate anxiety and depression, drug and alcohol use disorders, and severe disorders such as severe depression, bipolar disorders and schizophrenia, each with their own specific symptoms, age of onset and trajectory (Box 1.2). The experience of mental health conditions can be highly fluid both over the life-course and over much shorter periods of several weeks – e.g. an individual experiencing a moderate depressive episode can worsen so that the condition becomes severe, just as a severe episode can be stabilised with the symptoms lessened or alleviated (OECD, 2021[3]).
It is estimated that half of the population will experience a mental health condition in their lifetime and about one in five people in any given year (OECD, 2019[40]). The data currently available from population-based surveys often focus on experiencing symptoms of anxiety and depression (see Chapter 2). Pre-COVID-19 point estimates from the Institute for Health Metrics and Evaluation (IHME) suggest that the most common mental disorder in EU countries is anxiety disorder, with an estimated 25 million people (or 5.4% of the population) living with this condition in 2016, followed by depressive disorders, which affected over 21 million people (or 4.5% of the population). An estimated 11 million people across EU countries (2.4%) have drug and alcohol use disorders. Severe mental illnesses such as bipolar disorders affected almost 5 million people (1% of the population), while schizophrenic disorders affected 1.5 million people (0.3%) (OECD/European Union, 2018[41]).10
Box 1.2. Examples of mental health conditions and their symptoms
According to the DSM, a mental health condition is a syndrome characterised by a clinically significant disturbance in an individual's cognition, emotion regulation or behaviour that reflects a dysfunction in the psychological, biological or development processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational or other important activities (American Psychiatric Association, 2013[42]). Comorbidity of mental disorders and physical illnesses and multiple mental health problems is common. The most recent version, DSM-5, was published in 2013 and lists a total of 157 diagnoses and close to 300 disorders. Some of the most common clusters of disorders featured include:
Mood/affective disorders
Mood disorders, or affective disorders, are characterised by a disturbance of the general emotional state that interferes with an individual’s ability to function. Various forms of mood disorders exist: for instance, a major depressive disorder is characterised by persistent periods of low mood, low self-esteem and loss of interest in usually pleasurable activities lasting at least two weeks. Physical symptoms such as fatigue, headaches or digestive problems are also common. Bipolar disorder is characterised by alternating periods of depression and periods of mania (pathologically elevated mood, arousal and energy levels).
Anxiety disorders
Anxiety disorders are characterised by excessive and uncontrollable feelings of anxiety and fear. Specific symptoms depend on the type of anxiety disorder present. The most common anxiety disorders are generalised anxiety disorder, panic disorder and social anxiety disorders. In addition, various specific phobias (a fear of specific objects or situations) exist, like intense fear of heights or of flying.
Substance use disorders
Substance use disorder is a condition characterised by an uncontrollable intake of substances despite adverse consequences, and it is often accompanied by emotional, physical and behavioural problems and an inability to stop consuming despite several attempts. For instance, alcohol use disorder is a type of substance abuse disorder and includes frequent and heavy alcohol use.
Adjustment disorders
An adjustment disorder is characterised by a maladaptive emotional or behavioural reaction to a psychosocial stressor. Adjustment disorders occur when individuals have significant difficulties to adjust or cope with a stressful life event. For example, post-traumatic stress disorder (PTSD) usually develops due to exposure to traumatic life events or threatening situations, such as war, sexual assault or child abuse. Symptoms can range from sleeping difficulties, difficulty concentrating or irritability to hypervigilance and an exaggerated startle response.
Psychotic disorders
Psychotic disorders are severe mental health conditions with delusions and hallucinations as common symptoms. The most common psychotic disorder is schizophrenia, in which people interpret and experience reality abnormally and which is characterised by a combination of hallucinations, delusions and extremely disordered thinking and behaviour that impairs daily functioning.
Personality disorders
Personality disorders are characterised by long-term maladaptive patterns of behaviour, cognition and inner experience that differ significantly from the cultural-social norm. They are associated with difficulties in cognition, emotiveness, interpersonal functioning or impulse control. Three clusters of personality disorders exist: odd or eccentric disorders; dramatic, emotional or erratic disorders; and anxious or fearful disorders.
Somatoform and dissociative disorders
Somatoform disorders are disorders causing physical symptoms that might not be traceable to a somatic cause. Dissociative disorders include problems with memory, awareness, perception or identity; people experiencing dissociative disorder might feel disconnected from their body or develop different identities.
Eating disorders
An eating disorder is characterised by abnormal eating behaviours that affect physical and/or mental health. Various types of eating disorders exist, the most common being bulimia nervosa, anorexia nervosa and binge eating disorder. Eating disorders are often comorbid with anxiety disorders, depression and substance abuse.
Obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental and behavioural disorder characterised by intrusive, reoccurring thoughts or mental images (obsessions) that generate feelings of anxiety, disgust or discomfort, which in turn elicit an urge to perform a certain task or routine, such as hand washing, counting, cleaning or arranging things, in order to relieve this discomfort (compulsions).
Psychological distress
The term “psychological distress” is used in this report to refer to non-specific symptoms of negative affect (such as sadness, anguish, restlessness), sometimes combined with somatic symptoms (such as inability to sleep or loss of appetite) that do not reach the clinical threshold of a diagnosis within psychiatric classification systems.
There is some debate about whether psychological distress and mental conditions form conceptually distinct phenomena. Some researchers have argued that they are qualitatively distinct: psychological distress should only be considered as part of a pathological psychological process and a marker of a mental health condition if it is persistent and in excess of an “expectable response” to adverse events and other stressors. However, this is difficult to determine in practice and may depend on an individual’s socio-economic and overall life conditions (Horwitz, 2007[44]; Phillips, 2009[45]; Payton, 2009[16]; Roger T. Mulder, 2008[46]; Wakefield et al., 2007[47]). The DSM-5 does not provide any criteria for determining when distress becomes clinically significant; an assessment is usually made based on the degree of impairment to functioning produced by the distress, rather than its “appropriateness”.
Many of the tools developed to assess psychological distress in individuals, as documented in Chapter 2 of this report, are able to reliably distinguish cases of serious mental health conditions from non-serious cases. This suggests that mental disorder and distress, as a transdiagnostic characteristic of most mental health conditions, are indeed closely related (Barlow and Durand, 2009[48]). Moreover, even if the experience of psychological distress were to be temporary, it can imply significant suffering and hardship of individuals and deserves attention in its own right.
Positive mental health
Positive mental health covers psychological, emotional, and in some cases also social, relational and spiritual well-being (Huppert, 2005[49]; Keyes, 2005[11]; Steger et al., 2006[50]; Reis and Gable, 2003[51]).11
The concept of positive mental health is closely related to that of subjective well-being, which refers to “good mental states, including all of the various evaluations, positive and negative, that people make of their lives, and the affective reactions of people to their experiences” (OECD, 2013[52]). In 2013, the OECD published Guidelines on Measuring Subjective Well-being that identified three broad aspects of subjective well-being (and proposed measures for data collectors):
Life evaluation – a reflective self-assessment of a person’s life as a whole, or some specific aspect of it (e.g. life satisfaction measures; satisfaction with financial situation)
Affect – a person’s feelings, emotions or states, typically measured with reference to a particular point in time (e.g. measures about experiences of happiness, worry, pain, tiredness)
Eudaimonia – a sense of meaning and purpose in life, or good psychological functioning (e.g. measures of feeling that the things you do in life are worthwhile).
The strongest overlap between positive mental health and subjective well-being tends to be in the area of affect (where common mental health measures emphasise persistent experiences of certain affective states, such as worry, pain or tiredness) and eudaimonia (where many measures were explicitly developed to capture positive mental health). Additional concepts sometimes featured in measures of positive mental health, such as autonomy, optimism, resilience or environmental mastery, are not explicitly referenced in the OECD definition of subjective well-being provided above (Davydov et al., 2010[53]; Snow, 2019[54]; Peterson and Seligman, 2004[55]; Conversano et al., 2010[56]; Ryff and Keyes, 1995[57]). Although these concepts are sometimes included in some (long-form) measures of eudaimonia and psychological functioning that are discussed in the aforementioned OECD Guidelines (see Annex 1 and Module D), appraisal styles such as optimism and other character traits are considered mediating factors that influence a person’s affective reactions to life circumstances, rather than final well-being outcomes to strive for (OECD, 2013[52]).
The area of greatest conceptual difference between subjective well-being and positive mental health concerns life evaluation measures, which provide a very broad assessment of a person’s life in all its dimensions, rather than assessing only their mental health. Nevertheless, in practical terms, life evaluation measures are often included in research on (positive) mental health, since they are valuable as broad outcome measures that reflect a person’s perception of their well-being as a whole.
Chapter 2 reviews current data collection practice in OECD countries for the three aspects of subjective well-being mentioned above, as well as for positive mental health summary scales (mostly stemming from positive psychology) that cover aspects of emotional, psychological and social well-being. Chapter 3, which discusses the statistical quality of mental health tools, focuses only on the latter, since the OECD Guidelines have already considered in-depth the issue measuring life evaluations, affect and eudaimonia (OECD, 2013[52]). The topic of measuring affect and eudaimonia specifically will also continue to be explored in future OECD workstreams on subjective well-being. Extremely broad definitions of positive mental health that include domains such as physical and sexual health, financial security, or academic and occupational performance (which are covered elsewhere in the OECD Well-being Framework) are not considered in this publication (Fusar-Poli and Santini, 2022[58]; Fusar-Poli et al., 2020[59]; Harvard Center for Health and Happiness, n.d.[60]).
Conclusion
Measuring mental health is important to fully assess the well-being outcomes that matter to people’s lives. The aim of this report is to encourage official data producers to collect population-level data on mental health status more frequently and in an internationally harmonised manner, in order to understand how all societal groups, rather than only those in touch with the health care system, are faring, and to address a topic that is increasingly recognised as public policy challenge.
Mental health is a multifaceted concept that extends beyond a binary distinction between mental illness either being present or not. Considering all aspects of mental health can provide new avenues for the proactive rather than reactive design of mental health systems and services, draw attention to the importance of caring about positive mental health in its own right, and open up the space for policy to focus on both reducing illness and promoting good mental states. Collecting data on both aspects in household, social and health surveys would yield a more complete picture of mental health and help to better understand the drivers and policy levers needed for improving it.
References
[64] American Psychiatric Association (2022), Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR™), https://www.appi.org/dsm (accessed on 6 April 2022).
[42] American Psychiatric Association (2013), Diagnostic statistical manual of mental disorder (5th ed.).
[20] Australian Early Development Census (2012), The mental health of Australian children: a dual continuum, https://www.aedc.gov.au/resources/detail/the-mental-health-of-australian-children-a-dual-continuum (accessed on 17 May 2022).
[48] Barlow, D. and V. Durand (2009), Abnormal Psychology: An Integrative Approach, Cengage Learning, https://books.google.com/books/about/Abnormal_Psychology_An_Integrated_Approa.html?id=Mo_q4zFVNo4C (accessed on 7 February 2022).
[56] Conversano, C. et al. (2010), “Optimism and Its Impact on Mental and Physical Well-Being”, Clinical Practice & Epidemiology in Mental Health, Vol. 6/1, pp. 25-29, https://doi.org/10.2174/1745017901006010025.
[53] Davydov, D. et al. (2010), “Resilience and mental health”, Clinical Psychology Review, Vol. 30/5, pp. 479-495, https://doi.org/10.1016/j.cpr.2010.03.003.
[61] Exton, C. and L. Fleischer (2023), The future of the How’s Life? dashboard, OECD Publishing.
[63] Finnish Institute for Health and Welfare (n.d.), Positive mental health, https://thl.fi/en/web/mental-health/mental-health-promotion/positive-mental-health (accessed on 7 April 2022).
[59] Fusar-Poli, P. et al. (2020), “What is good mental health? A scoping review”, European Neuropsychopharmacology, Vol. 31, pp. 33-46, https://doi.org/10.1016/j.euroneuro.2019.12.105.
[58] Fusar-Poli, P. and Z. Santini (2022), “Promoting good mental health in the whole population: The new frontier”, European Neuropsychopharmacology, Vol. 55, pp. 8-10, https://doi.org/10.1016/j.euroneuro.2021.09.010.
[28] Galderisi, S. et al. (2015), “Toward a new definition of mental health”, World Psychiatry, Vol. 14/2, pp. 231-233, https://doi.org/10.1002/wps.20231.
[30] Goodman, F., J. Doorley and T. Kashdan (2018), “Well-being and Psychopathology: A Deep Exploration into Positive Emotions, Meaning and Purpose in Life, and Social Relationships”, in Diener, E., S. Oishi and L. Tay (eds.), Handbook of well-being, DEF Publishers, Salt Lake City.
[62] Government of Canada (n.d.), Positive Mental Health Surveillance Indicator Framework (PMHSIF), https://health-infobase.canada.ca/positive-mental-health/Index (accessed on 8 September 2022).
[22] Government of Western Australia Mental Health Commission (2021), Western Australian Mental Wellbeing Framework, https://www.mhc.wa.gov.au/mental-wellbeing-framework/ (accessed on 14 March 2022).
[17] Greenblat, L. (2000), “Understanding Health as a Continuum”, Schizophrenia Bulletin, Vol. 26/1, pp. 243-245, https://doi.org/10.1093/oxfordjournals.schbul.a033444.
[60] Harvard Center for Health and Happiness (n.d.), Repository of Positive Psychological Well-Being Scales, https://www.hsph.harvard.edu/health-happiness/repository-of-positive-psychological-well-being-scales/ (accessed on 7 April 2022).
[14] Herron, S. and D. Trent (2000), “Mental Health: A Secondary Concept to Mental Illness”, Journal of Public Mental Health, Vol. 2/2, pp. 29-38, https://doi.org/10.1108/17465729200000014.
[44] Horwitz, A. (2007), “Distinguishing distress from disorder as psychological outcomes of stressful social arrangements”, Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine, Vol. 11/3, pp. 273-289, https://doi.org/10.1177/1363459307077541.
[49] Huppert, F. (2005), “Positive mental health in individuals and populations”, in The Science of Well-Being, Oxford University Press, https://doi.org/10.1093/acprof:oso/9780198567523.003.0012.
[10] Iasiello, M., J. van Agteren and E. Cochrane (2020), “Mental Health and/or Mental Illness: A Scoping Review of the Evidence and Implications of the Dual-Continua Model of Mental Health”, Evidence Base, Vol. 2020/1, pp. 1-45, https://doi.org/10.21307/eb-2020-001.
[11] Keyes, C. (2005), “Mental Illness and/or Mental Health? Investigating Axioms of the Complete State Model of Health.”, Journal of Consulting and Clinical Psychology, Vol. 73/3, pp. 539-548, https://doi.org/10.1037/0022-006X.73.3.539.
[25] Keyes, C., S. Dhingra and E. Simoes (2010), “Change in Level of Positive Mental Health as a Predictor of Future Risk of Mental Illness”, American Journal of Public Health, Vol. 100/12, pp. 2366-2371, https://doi.org/10.2105/AJPH.2010.192245.
[18] Koushede, V. and R. Donovan (2022), “Applying Salutogenesis in Community-Wide Mental Health Promotion”, in The Handbook of Salutogenesis, Springer International Publishing, Cham, https://doi.org/10.1007/978-3-030-79515-3_44.
[29] New Zealand Initial Mental Health and Wellbeing Commission (2020), Developing a Mental Health and Wellbeing Outcomes Framework Summary of what we heard through the co-define phase, https://www.mhwc.govt.nz/assets/Outcomes-framework/Co-define-Report-on-Responses_Online-Version.pdf (accessed on 1 June 2022).
[32] Nielsen, L. et al. (2016), “High and low levels of positive mental health: are there socioeconomic differences among adolescents?”, Journal of Public Mental Health, Vol. 15, pp. 37-49.
[3] OECD (2021), A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill-Health, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/4ed890f6-en.
[5] OECD (2021), COVID-19 and Well-being: Life in the Pandemic, OECD Publishing, Paris, https://doi.org/10.1787/1e1ecb53-en.
[7] OECD (2021), Fitter Minds, Fitter Jobs: From Awareness to Change in Integrated Mental Health, Skills and Work Policies, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/a0815d0f-en.
[4] OECD (2020), How’s Life? 2020: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9870c393-en.
[40] OECD (2019), Health at a Glance 2019: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/4dd50c09-en.
[6] OECD (2015), 2015 OECD Recommendation on Integrated Mental Health, Skills and Work Policy, https://www.oecd.org/els/emp/Flyer_MHW%20Council%20Recommendation.pdf (accessed on 13 March 2022).
[52] OECD (2013), OECD Guidelines on Measuring Subjective Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9789264191655-en.
[8] OECD (2011), How’s Life?: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9789264121164-en.
[41] OECD/European Union (2018), Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris/European Union, Brussels, https://doi.org/10.1787/health_glance_eur-2018-en.
[15] Patel, V. et al. (2018), “The Lancet Commission on global mental health and sustainable development”, The Lancet, Vol. 392/10157, pp. 1553-1598, https://doi.org/10.1016/S0140-6736(18)31612-X.
[16] Payton, A. (2009), “Mental Health, Mental Illness, and Psychological Distress: Same Continuum or Distinct Phenomena?”, Journal of Health and Social Behavior, Vol. 50/2, pp. 213-227, https://doi.org/10.1177/002214650905000207.
[55] Peterson, C. and M. Seligman (2004), Character Strengths and Virtues: A Handbook and Classification, American Psychological Association.
[45] Phillips, M. (2009), “Is distress a symptom of mental disorders, a marker of impairment, both or neither?”, World psychiatry : official journal of the World Psychiatric Association (WPA), Vol. 8/2, pp. 91-2.
[23] Queensland Government (2015), The dual continuum of mental health and mental illness, https://cspm.csyw.qld.gov.au/practice-kits/mental-health/overview-of-mental-health-1/the-dual-continuum-of-mental-health-and-mental-ill (accessed on 17 May 2022).
[2] Rehm, J. and K. Shield (2019), “Global Burden of Disease and the Impact of Mental and Addictive Disorders”, Current Psychiatry Reports, Vol. 21/2, p. 10, https://doi.org/10.1007/s11920-019-0997-0.
[51] Reis, H. and S. Gable (2003), “Toward a positive psychology of relationships.”, in Flourishing: Positive psychology and the life well-lived., American Psychological Association, Washington, https://doi.org/10.1037/10594-006.
[26] Robinson, P. (2012), “Deep phenotyping for precision medicine”, Human Mutation, Vol. 33/5, pp. 777-780, https://doi.org/10.1002/humu.22080.
[46] Roger T. Mulder (2008), “An Epidemic of Depression or the Medicalization of Distress?”, Perspectives in Biology and Medicine, Vol. 51/2, pp. 238-250, https://doi.org/10.1353/pbm.0.0009.
[12] Routledge, K. et al. (2016), “Shared versus distinct genetic contributions of mental wellbeing with depression and anxiety symptoms in healthy twins”, Psychiatry Research, Vol. 244, pp. 65-70, https://doi.org/10.1016/j.psychres.2016.07.016.
[57] Ryff, C. and C. Keyes (1995), “The structure of psychological well-being revisited.”, Journal of Personality and Social Psychology, Vol. 69/4, pp. 719-727, https://doi.org/10.1037/0022-3514.69.4.719.
[27] Santini, Z. et al. (2022), “Higher levels of mental wellbeing predict lower risk of common mental disorders in the Danish general population”, Mental Health & Prevention, Vol. 26, p. 200233, https://doi.org/10.1016/j.mhp.2022.200233.
[37] Santini, Z. et al. (2017), “The protective properties of Act-Belong-Commit indicators against incident depression, anxiety, and cognitive impairment among older Irish adults: Findings from a prospective community-based study”, Experimental Gerontology, Vol. 91, pp. 79-87, https://doi.org/10.1016/j.exger.2017.02.074.
[33] Santini, Z. et al. (2020), “Predictors of high and low mental well-being and common mental disorders: Findings from a Danish population-based study”, European Journal of Public Health, Vol. 30/3, pp. 503-509, https://doi.org/10.1093/eurpub/ckaa021.
[54] Snow, N. (2019), “Positive psychology, the classification of character strengths and virtues, and issues of measurement”, The Journal of Positive Psychology, Vol. 14/1, pp. 20-31, https://doi.org/10.1080/17439760.2018.1528376.
[38] Solin, P. et al. (2019), “Predicting high and low levels of positive mental health among people living alone in the Lapland region of Finland”, Journal of Public Mental Health, Vol. 18, pp. 214-223.
[19] Statistics Canada (n.d.), Positive mental health and mental illness, https://www150.statcan.gc.ca/n1/pub/82-003-x/2014009/article/14086-eng.htm (accessed on 17 May 2022).
[50] Steger, M. et al. (2006), “The meaning in life questionnaire: Assessing the presence of and search for meaning in life.”, Journal of Counseling Psychology, Vol. 53/1, pp. 80-93, https://doi.org/10.1037/0022-0167.53.1.80.
[31] Stewart-Brown, S. et al. (2015), “Socioeconomic gradients and mental health: implications for public health”, British Journal of Psychiatry, Vol. 206/6, pp. 461-465, https://doi.org/10.1192/bjp.bp.114.147280.
[21] Swiss Health Observatory (n.d.), Psychischer Gesundheitszustand [Mental Health Status], https://www.obsan.admin.ch/de/gesundheitsthemen/psychische-gesundheit/psychischer-gesundheitszustand (accessed on 17 May 2022).
[39] Thoits, P. (2011), “Mechanisms Linking Social Ties and Support to Physical and Mental Health”, Journal of Health and Social Behavior, Vol. 52/2, pp. 145-161, https://doi.org/10.1177/0022146510395592.
[13] Trent, D. (1992), “The promotion of mental health: fallacies of current thinking”, in Trent, D. and C. Reeds (eds.), Promotion of Mental Health, Aldershot, Avebury.
[36] Van Lente, E. et al. (2012), “Measuring population mental health and social well-being”, International Journal of Public Health, Vol. 57/2, pp. 421-430, https://doi.org/10.1007/s00038-011-0317-x.
[34] Varin, M. et al. (2020), “At-a-glance - An update on positive mental health among adults in Canada”, Health Promotion and Chronic Disease Prevention in Canada, Vol. 40/3, pp. 86-91, https://doi.org/10.24095/hpcdp.40.3.04.
[35] Vinko, M. et al. (2022), “Positive mental health in Slovenia before and during the COVID-19 pandemic”, Frontiers in Public Health, Vol. 10, https://doi.org/10.3389/fpubh.2022.963545.
[47] Wakefield, J. et al. (2007), “Extending the Bereavement Exclusion for Major Depression to Other Losses”, Archives of General Psychiatry, Vol. 64/4, p. 433, https://doi.org/10.1001/archpsyc.64.4.433.
[24] World Health Organization (2022), World mental health report: Transforming mental health for all, https://www.who.int/publications/i/item/9789240049338 (accessed on 7 December 2022).
[43] World Health Organization (2021), International Classification of Diseases - ICD -11 for Mortality and Morbidity Statistics.
[1] World Health Organization (2019), Mental health, https://www.who.int/news-room/facts-in-pictures/detail/mental-health (accessed on 16 May 2022).
[9] World Health Organization (1948), WHO Constitution Preamble, https://www.who.int/about/governance/constitution (accessed on 5 April 2022).
Notes
← 1. As described later, mental ill-health in this report refers to diagnosable mental and behavioural conditions, as well as the transdiagnostic characteristic of general psychological distress. This terms mental health condition and mental disorder are used interchangeably in this report to refer to clinically significant symptoms of mental ill-health. Positive mental health covers psychological, emotional, and in some cases also social, relational and spiritual well-being. This report mainly focuses on the areas of positive mental health that have a strong overlap with the related concept of subjective well-being and that have been covered in-depth in the 2013 OECD Guidelines of Subjective Well-being, which define it as “good mental states, including all of the various evaluations, positive and negative, that people make of their lives, and the affective reactions of people to their experiences” (OECD, 2013[52]).
← 2. For instance, the share of people at risk of depression in How’s Life? 2020 was reported only for European countries covered by the European Health Interview Survey (which is conducted only every five to six years), and information on negative affect balance (the share of the population reporting more negative than positive feelings and states) is currently sourced from the Gallup World Poll. Similarly, several of the surveys used to analyse inequalities in mental distress featured in the 2021 A New Benchmark for Mental Health Systems and Fitter Minds, Fitter Jobs workstreams were conducted before 2015 and use a variety of different (non-harmonised) instruments to measure distress.
← 3. Current well-being is comprised of 11 dimensions: they relate to material conditions that shape people’s economic options (income and wealth, housing, work and job quality) and quality-of-life factors that encompass how well people are (and how well they feel they are), what they know and can do, and how healthy and safe their places of living are (health, knowledge and skills, environmental quality, subjective well-being, safety). Quality of life also encompasses how connected and engaged people are, and how and with whom they spend their time (work-life balance, social connections, civic engagement). Resources for future well-being are expressed in terms of a country’s investment in (or depletion of) different types of capital resources that last over time but that are also affected by the decisions taken (or not taken) today, and these include economic capital (man-made and financial assets), natural capital (stocks of natural resources, land cover, species biodiversity, as well as ecosystems and their services), human capital (skills and the future health of individuals) and social capital (social norms, shared values and institutional arrangements that foster cooperation) (OECD, 2020[4]).
← 4. The indicator dashboard accompanying the OECD Well-being Framework differentiates between current well-being and the resources needed to sustain it, relying on different indicators for the two domains – hence, only premature mortality and obesity prevalence are included in the human capital indicator set (Exton and Fleischer, 2023[61]). However, people’s physical and mental health, which are covered in other dimensions, influence their opportunities in later life and are conceptually within the scope of human capital.
← 5. His broad view is also mirrored in the WHO’s definition of health more broadly as “complete physical, mental and social well-being and not merely the absence of disease and infirmity".
← 6. Various names for dual-continua models have been proposed, including the dual-factor model, two-factor, two-continua, the complete state model and complete mental health.
← 7. Prevalence of mental health, or flourishing, was defined here as both symptoms of hedonia and positive functioning, and it is measured by six questions about positive affect, Ryff’s scales of psychological well-being and Keyes’ scales of social well-being (Keyes, 2005[11]).
← 8. These studies were performed in clinical and non-clinical populations, over the entire life-course, and in Western and non-Western populations, and included studies specifically recruiting minority and at-risk groups.
← 9. Both the Diagnostic and Statistical Manual of Mental Disorders (DSM) of the American Psychiatric Association and the WHO International Classification of Diseases (ICD) list a set of criteria that are needed for a diagnosis of a specific mental health condition to be met (World Health Organization, 2021[43]; American Psychiatric Association, 2013[42]). These criteria, which vary depending on the specific disorder, specify the nature and number of symptoms and the level of distress or impairment required, and are used to exclude cases where symptoms can be directly attributed to general medical conditions, such as a physical injury, or an expectable or culturally approved response to a common stressor or loss, such as the death of a loved one. Mainly used and developed in the United States by American psychiatry experts, the DSM is a specified classification system for mental disorders only, while the ICD is an overarching joint classification system for both physical and mental disorders. The first version of the DSM was published in 1952 and included 106 specific diagnoses. It has since been revised several times with the latest version (DSM-5) having been published in 2013, listing a total of 157 diagnoses and close to 300 disorders. A text revision (DSM-5-TR) was released in March 2022 that includes among other things updated diagnostic criteria and diagnostic codes, Prolonged Grief Disorder as new mental health condition, and considerations of the impact of racism and discrimination on mental disorders (American Psychiatric Association, 2022[64]). The ICD has a chapter (chapter F) devoted specifically to psychiatric disorders and is also regularly updated, with version 11 published in 2019. Although the two systems present minor differences, they are based on similar sets of rules and assumptions.
← 10. The Institute for Health Metrics and Evaluation’s burden of disease estimates for these mental health disorders are based on a wide variety of data sources and a set of complex assumptions regarding prevalence of a given disorder or risk factor and the relative harm it causes to quality of life and premature mortality.
← 11. The way positive mental health is conceived, sometimes with greater focus and sometimes more broadly, is apparent in the way different government agencies across the OECD have operationalised the concept: the Canadian Positive Mental Health Surveillance Indicator Framework defines it as “a state of well-being that allows us to feel, think, and act in ways that enhance our ability to enjoy life and deal with the challenges we face” (Government of Canada, n.d.[62]), whereas the Finnish Institute for Health and Welfare describes it as “various levels of emotional (feelings), psychological (positive actions), social (relationships with others and society), physical (physical health and fitness) and spiritual (the sense that life has a meaning) wellbeing” (Finnish Institute for Health and Welfare, n.d.[63]).