A variety of tools are available for monitoring population mental health, ranging from administrative data to different types of survey questions. Although many OECD countries began collecting new or additional mental health data during COVID-19, official data producers were already active in this space well before the pandemic started. However, there is room for improvement by increasing the frequency of (survey) data collection, diversifying the types of indicators used to cover the full spectrum of mental health, and expanding the international harmonisation of existing measures. Here, data collectors could: (1) beyond screening tools focusing on symptoms of depression, expand use to those including symptoms of anxiety as outcome measures; (2) move towards collecting harmonised information on affective and eudaimonic aspects of positive mental health; and (3) explore using single-item questions on general mental health status across surveys.
Measuring Population Mental Health

2. Measuring population mental health: Tools and current country practice
Abstract
The frequent collection of population-level data on mental health outcomes is important for identifying populations at-risk for mental ill-health, for determining which socio-economic and other factors shape (and are shaped by) people’s mental health, and for designing effective prevention and promotion strategies. As outlined in Chapter 1, mental health is a multifaceted concept and exists beyond a binary distinction between the presence or absence of mental illness. Collecting data on both mental ill-health and positive mental health in population surveys and mental health assessments would yield a more complete picture of people’s overall mental health and help to better understand the drivers and policy levers associated with improving it.
However, the current lack of (internationally) standardised data on population mental health makes it difficult to assess the efficacy of different policy approaches across disparate contexts; standardising outcome measures is the first step in facilitating such analysis. This chapter outlines the tools available to data collectors, gives an overview of current data collection practices across OECD countries and offers suggestions for which outcomes to prioritise in international harmonisation efforts.
An analysis of responses to a questionnaire sent to official data producers in OECD countries in 2022 shows that all member states that answered are already active in this space. Prior to the pandemic, almost all OECD members were already collecting information on mental health outcomes in both health interviews and general household surveys, as well as via administrative data. COVID-19 has sparked additional interest in measuring population mental health, with many public agencies and statistical offices adding items to both new and existing surveys.
These existing data collections demonstrate the interest in, and relevance of, population mental health outcomes in a national statistics context. Yet there is room for improvement in several areas: the frequency of data collection; greater data availability across the full spectrum of both negative and positive mental health outcomes; and better harmonisation of measures across countries to improve international comparability.
Indeed, prior to the pandemic most mental health data were collected by countries on surveys that ran every four to ten years. While many introduced high-frequency surveys with mental health modules in the first two years of COVID-19, it is currently unclear whether these surveys will continue to be implemented moving forward. Further, although all statistical offices collect data on mental ill-health – with a particular focus on common mental disorders – general psychological distress and depressive symptoms tend to be captured through standardised screening tools, whereas measures of experiencing anxiety are less harmonised across countries. Data collection efforts for other mental conditions – such as post-traumatic stress disorder (PTSD), bipolar disorder, eating disorders, etc. – and for other aspects of mental health – such as suicidal ideation and mental health-related stigma – remain very uneven across countries. When it comes to positive mental health, cross-country comparative data are mainly limited to measures of life evaluation. Other aspects, such as affect and eudaimonia, are much less frequently collected as outcome measures, and when they are, the tools used are less likely to be standardised across countries.
The results of the OECD questionnaire suggest that existing data collection efforts are not capturing the full range of mental health outcomes – missing aspects of both mental ill-health as well as positive mental health. In order to capture these outcomes and collect frequent information on mental health, data collectors in OECD member countries could: (1) beyond screening tools focusing on symptoms of depression, expand use to those including symptoms of anxiety as outcome measures; (2) move towards collecting harmonised information on affective and eudaimonic aspects of positive mental health; and (3) explore using single-item questions on general mental health status across surveys.
Which tools are available for measuring population mental health?
While Chapter 1 focused on relevant types of outcomes (covering both mental ill-health as well as positive mental health) for data collectors interested in mental health, this chapter focuses mainly on the types of tools that can be used to measure these.
The broad tool types discussed in this chapter – some of which are sourced from administrative data, but the bulk of which come from household surveys – range from long survey modules to a battery of question items to single questions. Some tools can be used to capture aspects of either mental ill-health or positive mental health, while others are used only for specific types of outcomes. Each type of tool has its own advantages and disadvantages, requiring data collectors to select among them, depending on the needs and constraints of their specific contexts. The different tools are described below in order to provide a common understanding of the categorisation used in this report.
The chapter annexes contain in-depth information for readers interested in further details. Annex 2.A provides an overview of which specific tools are collected by each country, along with sample question framing and answer options. Annex 2.B lists full details, including question wording and scoring recommendations, for the most commonly used standardised instruments. More detailed reflections on the statistical quality of mental health survey measures are addressed in Chapter 3.
Tools sourced from administrative data
Administrative data can contain information on the use of mental health services, diagnoses of mental disorders in clinical settings, as well as cause of death data from suicide and substance abuse (i.e. drug overdoses and alcohol abuse).
While all of these can be considered objective (i.e. not self-reported) and easy-to-collect proxies of mental ill-health, measurement challenges remain. For instance, measures of service use and medical diagnoses do not capture population outcomes, but rather only those who are willing and able to access health care services. Such measures can overestimate comparative levels or incidence rates in countries with good (and affordable) medical systems, awareness programmes and less stigma, where people are more likely to both seek and receive treatment. In addition, preventing ill-health necessitates tracking outcomes prior to, and following, engagement with the service sector. This report does not consider administrative statistics related to health care further, referring readers to (OECD, 2021[1]).
Data on causes of death due to suicide or substance abuse (which are commonly referred to as “deaths of despair” (Case and Deaton, 2017[2])) do capture mental ill-health outcomes at the population level. These measures can act as proxies for severe mental illness and addiction. While there are social and cultural reasons affecting suicidal behaviours – meaning that not all suicides are the direct result of a mental ill-health – living with mental health conditions does substantially increase the risk of dying by suicide (OECD, 2021[1]). However, the registration of suicide deaths is a complex procedure, affected by factors such as how intent is ascertained, who completes the death certificate, and prevailing norms and stigma around suicide, all potentially affecting the cross-country comparability of mortality records (OECD, 2021[1]).
A general limitation for all types of administrative data is that the additional socio-demographic data collected alongside are often limited to the age, sex, geographic region and potentially the race/ethnicity of the deceased. This constrains the ability to delve into the drivers of mental health and to identify relevant socio-economic, environmental and relational risk and resilience factors.
Tools sourced from household surveys
In contrast to administrative data, population surveys generally contain information on respondents’ material conditions (e.g. income, wealth, labour market outcomes, housing quality), quality of life (e.g. physical health, educational attainment, environmental quality) and relationships (e.g. social connections, trust, safety). Population surveys can have a specific content focus, such as a health survey, or a more general scope, such as general social surveys. These surveys are conducted at the household level, with more in-depth modules on employment, health (including mental health), education, etc., administered to selected household members. Having a full range of well-being covariates is important to understand how mental health is impacted by, and how it in turn influences, other areas of people’s life. Furthermore, tracking (and eventually achieving) equity in mental health outcomes requires disaggregation by important socio-demographic categories.
Tools that have been included in household surveys to assess specific mental health outcomes range from single-item questions to standardised batteries of items. A brief description of each can be found below, with full details in Annex 2.A and Annex 2.B.
Questions about previous diagnoses – This refers to single-item questions about whether an individual has been diagnosed with a mental health disorder (e.g. major depressive disorder, generalised anxiety disorder, or other mental health conditions) by a health care worker, either in the past 12 months or over the course of his/her lifetime. These questions typically have yes/no answers and are not standardised across countries. For full details, see Table 2.6. Examples include:
“Have your mental health problems ever been diagnosed as a mental disorder by a professional (psychiatrist, doctor, clinical psychologist)? Yes / No”.
“Have you EVER been told by a doctor or other health professional that you had ...Any type of depression? Read if necessary: Some common types of depression include major depression (or major depressive disorder), bipolar depression, dysthymia, post-partum depression, and seasonal affective disorder. Yes / No”.
Questions about experienced symptoms – This refers to single-item questions about symptoms of mental disorders experienced in the past 12 months or over the course of an individual’s lifetime, without explicitly referring to a diagnosis by a medical professional. These questions typically have yes/no answers and are not standardised across countries. For full details, see Table 2.7. Examples include:
“During the past 12 months, have you had any of the following diseases or conditions? Depression (“Yes / No”).
“Have you ever suffered from chronic anxiety? ("Yes / No").
“Do you have a mood disorder? Yes / No”.
Questions about suicidal ideation and suicide attempts – These are (usually) single-item questions about a respondent’s experience of suicidal ideation, self-harm behaviours or suicide attempts. These questions typically have yes/no answers and are not standardised across countries. Recall periods refer to an individual’s lifetime, the last 12 months, the past two weeks, or “during COVID”. For full details, see Table 2.8. Examples include:
“Have you seriously contemplated suicide since the COVID-19 pandemic began? Yes/No”.
“Sometimes people harm themselves on purpose but they do not mean to take their life. In the past 12 months, did you ever harm yourself on purpose but not mean to take your life? Yes/No”.
“Have you ever attempted suicide? Yes/No”.
“Did you stay in a hospital overnight or longer because you tried to kill yourself? Yes/No”.
Questions about general mental health status – These refer to single-item questions on how respondents rate their mental health overall, and thus capture both components of ill-health and positive mental health. Questions are not standardised across countries and differ in terms of question wording, response options and recall period. For full details, see Table 2.9. Examples include:
“In general, how is your mental health? Excellent / Very good / Good / Fair / Poor”.
“Has your mental health/well-being been affected by the Covid-19 pandemic during the last 12 months?”
“On a scale from 1 to 10 can you indicate to what extent you are satisfied with your mental health? A score of 1 refers to completely dissatisfied and a 10 to completely satisfied”.
“Does your mental state interfere with your daily life at work? your family life? Yes / No”.
Positive mental health indicators – This refers to questions pertaining to the various aspects of positive mental health: life evaluation, affect (summary affect scales, and batteries of questions on positive, negative or mixed affect), eudaimonia (questions about quality of life, whether life is worthwhile or meaningful), as well as standardised positive mental health composite scales (combining different dimensions of positive mental health, prioritising positive over negative affect, and sometimes adding a social well-being component). In some instances, positive mental health indicators are single-item questions that vary across countries and surveys, while in others they are standardised batteries of questions. Standardisation across countries varies, with only life evaluation questions and positive mental health composite scales being consistently phrased. For full details, see Table 2.10. Specific question item phrasing and scoring suggestions for standardised composite scales can be found in Annex 2.B.
Screening tools – These refer to multi-item instruments designed to screen respondents for symptoms (rather than for diagnoses) of mental health conditions. These tools were initially developed in clinical settings to screen for common mental disorders to identify individuals who may be at risk and to flag them for further screening and potential diagnosis. They can be interviewer-led or self-administered and focus either on general psychological distress or on specific mental health conditions such as major depressive disorder, generalised anxiety disorder (and sometimes a combination of the two), alcohol use disorder, post-traumatic stress disorder, eating disorders and so on. These tools are considered “validated” in that they have been psychometrically tested for their validity (against the gold standard of structured interviews or diagnoses), sensitivity (the probability of correctly identifying a patient with the condition) and reliability (the measures produce consistent results when an individual is interviewed under a given set of circumstances) (refer to Chapter 3 for an extended discussion of statistical quality). A wide variety of screening tools are available, ranging from very short screeners of two items to longer instruments covering 20 items or more. The focus of questions varies between screening tools: all cover the frequency of experiencing (mostly negative) affect (i.e. feeling low, feeling nervous, feeling worthless), with some also including somatic symptoms (i.e. changed appetite, trouble sleeping) and/or functional impairment due to emotional distress (e.g. disturbance in daily activities, not being able to concentrate, not being able to stop worrying). Screening tools also differ in terms of reference period for symptoms, ranging from the past week to the past month; however, none are able to measure lifetime prevalence. Given these differences between screening tools, they are therefore not always directly comparable and should not be used interchangeably for international comparisons. Item scores are typically summarised in a summary index, with the final score being used either as a continuous measure of mental ill-health or to assess the risk of a common mental health conditions using a validated cut-off score. For full details, refer to Table 2.5. Exact question item wording and scoring recommendations for the most frequently used screening tools can be found in Annex 2.B.
Structured interviews – Structured interviews are considered the gold standard for measuring mental disorders (often both on a lifetime and 12-month basis). They provide a standardised assessment based on the internationally agreed definitions and criteria of recognised psychiatric classification systems and have strong diagnostic reliability and psychometric properties to determine whether or not a respondent has the condition of interest (Mueller and Segal, 2015[3]; Burger and Neeleman, 2007[4]).1 They are administered by trained interviewers, with close-ended and fully scripted questions and standardised scoring of responses (Ruedgers, 2001[5]). Structured interviews approximate assessments conducted by mental health professionals and in this way can identify populations at risk for mental health conditions even if these individuals have not been diagnosed by a health care professional. For additional information on the most commonly used structured interview, the Composite International Diagnostic Interview (CIDI), see Table 2.4 and Annex 2.B.
Additional mental-health related topics – This category refers to questions on any other relevant topics, including the use of mental health medication and services, the mental health of children and young people in the household, loneliness and stress, resilience and self-efficacy, attitudes towards mental health including stigma and literacy, and questions on unmet needs. For additional information, see Table 2.11.
Trade-offs between tool types
All tools imply trade-offs in terms of response burden/ease and cost of data collection, accuracy and coverage (Figure 2.1, Table 2.1). Response burden is a direct function of how much time an individual needs to spend to provide information on their mental health status and how much stress is caused by providing this information. Accuracy refers to the sensitivity of a tool in correctly identifying a person with a mental health condition, whereas coverage entails whether the measure in question is applied to the full (adult) population.
By way of illustration, administrative data have a low response burden: they do not require answers from individual respondents and are routinely collected within a country’s data infrastructure. Yet statistics on deaths of despair focus only on the extreme end of mental ill-health and are further complicated by the fact that not all deaths of despair may be the culmination of a mental disorder. Furthermore, unlike household surveys, only those who were in contact with the health care system are captured by administrative records of diagnoses in a clinical setting.2
For household surveys, both the response burden and accuracy increase the longer and more specific a tool is: whereas single questions about experienced symptoms or a person’s general mental health status are short and easy to answer, they do not consider the nature or severity of symptoms, or the type of mental health condition, and have not been benchmarked against diagnostic criteria. Screening tools have been validated against the gold standard of structured interviews and are, depending on the specific tool used and the number of items covered, still relatively low cost in terms of response burden. However, they do not constitute a diagnosis from a health care professional and can only identify people likely at risk of disorders. Screening tools are validated against clinical diagnoses, and are thus designed to maximise likeness to diagnostic interviews to the extent possible. Still, when calibrating tools and cut-off scores, there is a trade-off between sensitivity (correctly identifying the presence of a mental health condition) and specificity (correctly noting the absence of a mental health condition), and researchers often prioritise the former rather than the latter, leading to slight overestimates by design (see Box 3.3 and Section 3.3.1 for a more detailed discussion). Finally, the majority of tools included in both household surveys and administrative data focus on mental ill-health; the only exceptions are household survey questions about general mental health and positive mental health.
The difference in question framing and item length – between structured interviews, screening tools and single-item questions on experienced symptoms or received diagnoses – can lead to different estimates of prevalence for the same reported outcome measure (Box 2.1). This speaks to the need for the standardisation of tool type (and transparency about which tool was used) when comparing outcomes across countries, over time and across population groups: i.e. mixing types of tools when commenting on outcomes like “share at risk for depression” or “share at risk for psychological distress” can lead to different estimates because of measurement differences, rather than because of differences in underlying mental health status (refer to Chapter 3 for an extended discussion of these themes).
Figure 2.1. Trade-off between response burden and accuracy for mental health measurement tools
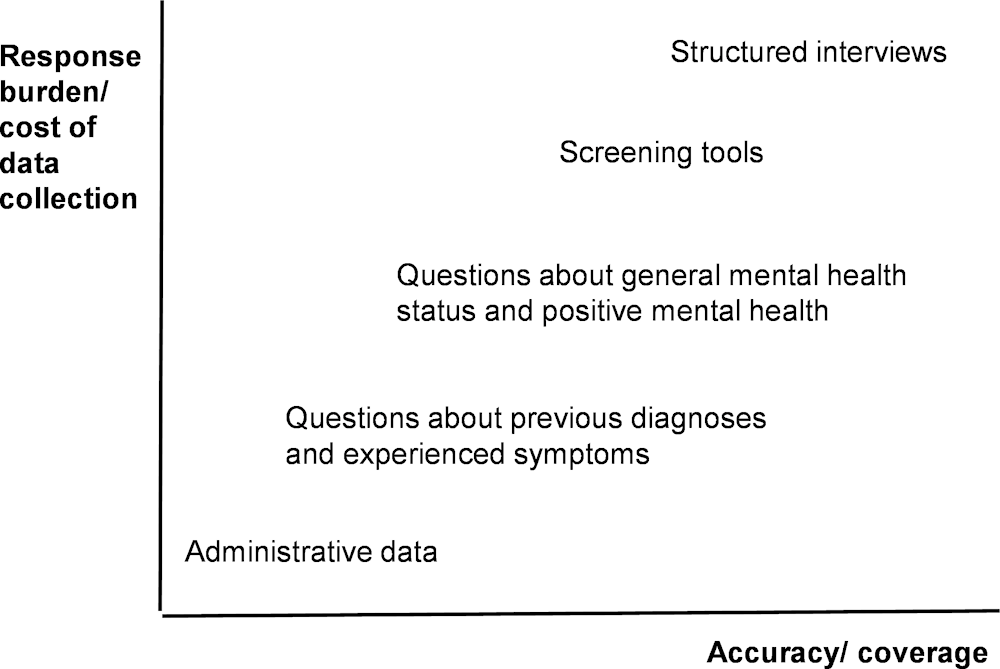
Source: Adapted from a presentation given by Statistics Canada at the OECD conference “Well-being and mental health – towards an integrated policy approach” in December 2021.
Table 2.1. Advantages and limitations of different tools to measure mental health
|
Tool |
Advantages |
Limitations |
|---|---|---|
|
Administrative data (deaths of despair from suicide, drug overdose, alcohol abuse; diagnoses of common mental disorders in clinical care settings) |
• No response burden for individuals • Possibility to link across other administrative data (e.g. health system quality) • Less costly and more readily available than other types of data • Clinical care data can provide some insight into lifetime and specific time period (e.g. past 12 months) prevalence estimates for a range of ill-health conditions when other data sources are not available |
• Captures only those who sought treatment, were correctly coded by a health professional and are part of the reporting database • “Cause of death” data need to be correctly coded, do not account for suicide attempts or substance abuse not leading to death, and only capture the extreme end of mental ill-health • Often difficult, or even impossible, to interpret (without supplemental information) whether changes in diagnostic rates are driven by changes in underlying prevalence of mental health conditions or by other factors such as changes to affordability or accessibility of care, changes in help-seeking behaviour, etc. • Limited contextual information on well-being covariates |
|
Household surveys: questions about previous diagnoses |
• Relatively easy to understand for respondents • Minimal response burden (usually a single binary question) • Can provide both lifetime and specific time period (e.g. past 12 months) prevalence estimates for a range of ill-health conditions |
• Captures only those who sought treatment and were diagnosed by a health professional • Evidence that these questions lead to social desirability bias and higher rates of refusal and non-response (see Chapter 3) • Limited contextual information on the nature and severity of symptoms |
|
Household surveys: questions about experienced symptoms of mental health conditions |
• Minimal response burden (usually a single binary question) • Can provide both lifetime and specific time period (e.g. past 12 months) prevalence estimates for a range of ill-health conditions |
• Potential for confusion for respondents in terms of whether the question refers to an actual diagnosis or their self-assessment, though evidence suggests this type of tool is closely related to questions about previous diagnoses by health professionals • Limited contextual information on the nature and severity of symptoms |
|
Household surveys: questions on general mental health status |
• Relatively easy to understand for respondents • Minimal response burden (usually a single question) • Captures a respondent’s global evaluation of their mental state, and hence both ill-health and positive aspects |
• Over-reporting of true prevalence – not a complete assessment or an actual diagnosis, does not consider symptoms • Has not been validated against structured interviews or other diagnostic tools, no established threshold in the tools as to what constitutes at-risk respondents • Generally less of an existing evidence base, though available studies suggest this to be a useful measure • Limited contextual information on the nature and severity of symptoms or the type of mental health condition |
|
Household surveys: indicators of positive mental health |
• Relatively easy to understand for respondents • Minimal response burden (usually single or limited-item questions) • Focus on psychological and emotional well-being or flourishing • International measurement guidance exists (e.g. OECD Guidelines on Measuring Subjective Well-being) |
• No reference point of what (true and/or desired) prevalence should be • Recall period for questions typically ranges from day prior to past 4 weeks; cannot provide lifetime estimates |
|
Household surveys: screening tools |
• Easy to administer and reduced response burden compared to structured interviews • Have been validated against structured interviews or other diagnostic tools • Can capture undiagnosed conditions |
• Over-reporting of true prevalence – not a complete assessment or an actual diagnosis • Recall period for questions typically ranges from day prior to past 4 weeks; cannot provide lifetime estimates |
|
Household surveys: structured interviews |
• Approximates true prevalence – near gold standard • Can capture undiagnosed conditions • Extensive contextual information of the respondents’ lives can be taken into account |
• Very complex to develop and administer, including interviewer training • Many questions for people who have symptoms • Lack of survey measurement tools available to map to most up-to-date diagnostic guidelines (DSM-5) |
Source: Adapted from a presentation given by Statistics Canada at the OECD conference “Well-being and mental health – towards an integrated policy approach” in December 2021.
Box 2.1. Prevalence rates vary depending on the measurement tool used
Prevalence rates for specific mental health conditions will vary – at times substantially – depending on the type of tool used to create the estimate. Screening tools are likely to overstate population level prevalence of mental disorders by design. They were developed in clinical settings to identify individuals at risk for common mental disorders, who can then be flagged for further observation and actual diagnoses – some of whom may not end up being diagnosed or needing further treatment (National Academies of Sciences Engineering and Medicine, 2021[6]; Topp et al., 2015[7]). In contrast, questions that require individuals to report whether they have been diagnosed with a mental disorder by a health care professional in the past, or currently live with a specific disorder, focus on those in touch with the health care system and are therefore likely to understate population prevalence.
On the first point, Figure 2.2 below shows that screening tools may overestimate population prevalence as compared to structured interviews. The figure shows national estimates of the same outcome measure – prevalence for major depressive disorder (MDE) – in three OECD countries as measured by CIDI, a structured interview, and by the Patient Health Questionnaire (PHQ), a screening tool. (The version of the PHQ varies by country: PHQ-9 in Canada and Korea, PHQ-2 in the United States. Refer to Annex 2.B for the specific items included in each iteration.) While both the CIDI and screening tools are used in different surveys within each country, implying that care should be taken in making direct comparisons, generally prevalence of MDE as measured by the CIDI is lower than that measured through screening tools. The exception is the United States, which also shows the smallest difference between the estimates. This may be in part because many mental health survey tools were first developed, and subsequently extensively validated, in the United States, making the calibrations between different tools more precise.
Figure 2.2. Screening tools typically show greater prevalence of major depressive disorder than do structured interviews
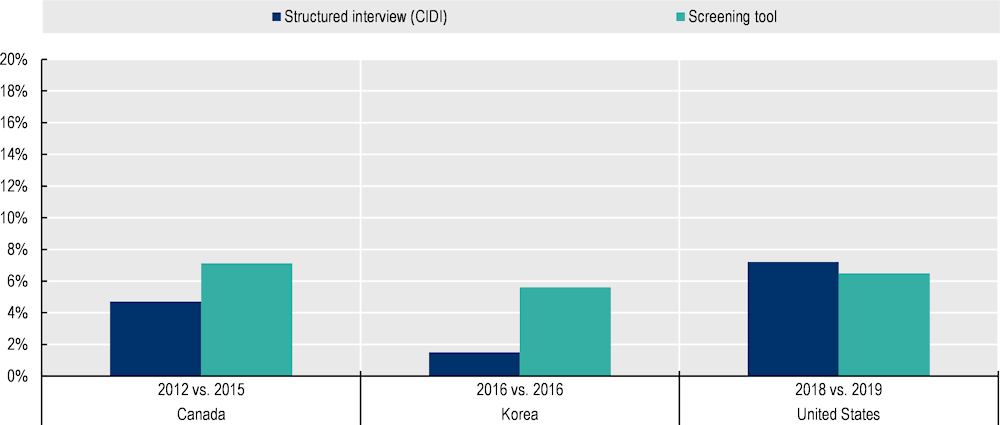
Note: For all three countries, the structured interview used is the CIDI, which is used to measure the prevalence of Major Depressive Episodes (MDE) over the past 12 months. In Korea, these estimates are adjusted for age and sex. In Canada and the United States, these estimates are nationally representative for the 15+ and 18+ population, respectively. The validated screening tool used by Canada is the PHQ-9 (MDE defined as having a score >= 10); the PHQ-9 is used by Korea (being at risk for depression is defined as having a score >= 10; although not described by KOSIS, Korea’s statistical service, as a risk for MDE, this same scoring convention is used by Canada to measure MDE); and the PHQ-2 is used by the United States (symptoms of a depressive disorder are defined as having a score >= 3). The PHQ-9 and PHQ-2 both have a reference period of the past 2 weeks. For the United States, the PHQ-2 measures the share with symptoms of a depressive disorder, rather than experience of MDE. Refer to Annex 2.B for more information on individual screening tools.
Source: Structured interview data for Canada come from Statistics Canada (2013[8]), Canadian Community Health Survey: Mental Health, 2012, The Daily, https://www150.statcan.gc.ca/n1/daily-quotidien/130918/dq130918a-eng.htm; PHQ-9 data for Canada are derived from Dobson, K. et al. (2020[9]), “Trends in the prevalence of depression and anxiety disorders among Canadian working-age adults between 2000 and 2016”, Health Reports, Vol. 31/12, pp. 12-23, https://doi.org/10.25318/82-003-X202001200002-ENG; Structured interview data for Korea come from KOSIS (n.d.[10]), Annual prevalence of mental disorders (adjusted for sex and age) (database), Korean Statistical Information Service, https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=TX_117_2009_HB027&conn_path=I2; PHQ-9 data for Korea come from KOSIS (KOSIS, n.d.[11]), Depressive disorder prevalence (database), National Health and Nutrition Survey, Korean Statistical Information Services, https://knhanes.kdca.go.kr/knhanes/sub01/sub01_05.do#none; Structured interview data for the United States come from SAMHSA (2019[12]), Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (database), Substance Abuse and Mental Health Services Administration, Rockville, MD, https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf; PHQ-2 data for the United States come from the National Center for Health Statistics (2021[13]), Estimates of Mental Health Symptomatology, by Month of Interview: United States, 2019 (database), U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, https://www.cdc.gov/nchs/data/nhis/mental-health-monthly-508.pdf.
On the second point, Figure 2.3 shows that, based on answers to screening tools, the share of the population reporting ever having received a diagnosis for a given mental disorder is much lower than the share deemed to be at risk for poor mental health conditions; this is often a function of affordability and access to health care, along with stigma and mental health illiteracy affecting health-seeking behaviours. The left-hand side of the figure displays the share of respondents who are at risk for psychological distress or low levels of positive mental health, including: (1) those at risk for depression, as defined by a scoring convention of the Short Form-12 mental health summary component (SF-12); those at risk for a probable common mental disorder, as measured by the General Health Questionnaire-12 (GHQ-12); and (3) those who have poor mental well-being, as defined by a scoring convention of the Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS). (Refer to Table 2.5 and Table 2.10, along with Annex 2.B, for more information on the three tools.) The right-hand side of the figure shows the share of respondents who report having ever received a diagnosis for a range of specific mental health conditions.
Figure 2.3. The share of those reporting a diagnosis of a mental health condition is much lower than the share identified as experiencing psychological distress by screening tools
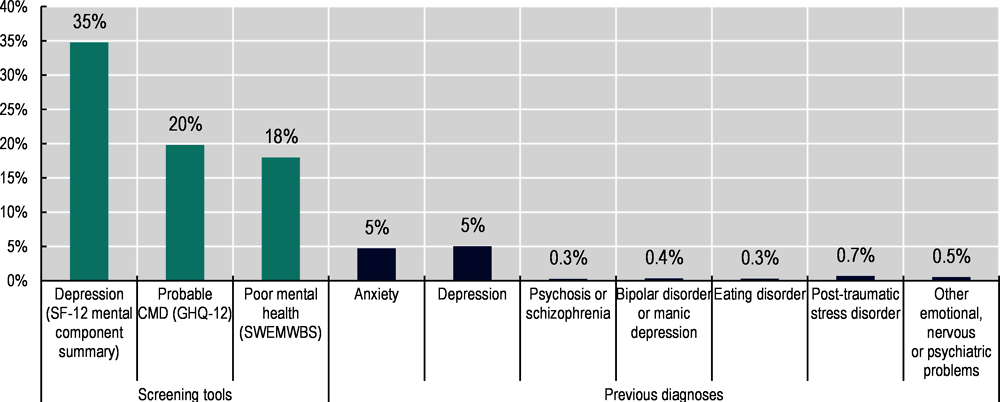
Note: Scoring information for each of the screening tools included: risk for depression is defined as having a score <= 45 on the transformed SF-12 mental health component composite scale, where 0 indicates worst mental health and 100 best possible mental health; risk for a probable common mental disorder (CMD) is defined as having a score >= 4 on the GHQ-12, as used in (Woodhead et al., 2012[14]); poor mental health is defined as having a SWEMWBS score more than one standard deviation below the sample average. Refer to Annex 2.B for more information on individual screening tools.
Source: OECD calculations based on University of Essex, Institute for Social and Economic Research (2022[15]), Understanding Society: Waves 1-11, 2009-2020 and Harmonised BHPS: Waves 1-18, 1991-2009 (database), 15th Edition, UK Data Service, SN: 6614, http://doi.org/10.5255/UKDA-SN-6614-16, from wave 10 only (Jan 2018 – May 2020).
Which population mental health data are OECD countries already collecting?
In February and March of 2022, 37 of 38 OECD countries provided answers to a questionnaire designed by the OECD Secretariat to better understand what OECD countries are doing in terms of measuring mental health outcomes.3 The questionnaire covers the statistical tools used (questions about diagnoses, experienced symptoms, screening tools and structured interviews) and outcomes covered (mental ill-health, positive mental health and other related topics, including loneliness, stress, attitudes towards mental health, etc.). A discussion of mental health data related to service use and access to care is set out in A New Benchmark for Mental Health Systems (OECD, 2021[1]), and this new round of surveying seeks to build upon existing work by primarily focusing on mental health outcomes, rather than on service use or access to care, and in particular on outcomes that could be measured through household surveys rather than administrative data.
All OECD countries already collect both administrative and survey data on population mental health
All OECD countries collect mortality statistics on causes of death, including from suicides rates as well as deaths from alcohol and drug overdoses. Statistics on causes of deaths are typically collected by hospitals or health care providers, while police authorities report deaths from suicides. The OECD already regularly publishes statistics for its member countries on both deaths from suicide and other types of deaths of despair (OECD, 2020[16]; OECD, 2021[17]).4
Administrative data on mental health go beyond death records. Hospital discharge registries that, depending on the country, may cover the length of hospitalisation and discharges by field of medical specialisation were mentioned by a number of countries, including Canada, Chile, Hungary, Italy, Slovenia, Switzerland and Türkiye. Some countries, including Spain and the United Kingdom, collect care or clinical care data to measure prevalence and incidence of specific behavioural disorders. The Swedish Social Insurance Agency also collects data on causes of work absences, with a special category for sick leave following a psychiatric diagnosis. Finally, a handful of countries collect administrative data on psychiatric medication. For example, in France the Agence nationale de sécurité du médicament (ANSM) publishes data on psychotropic drugs delivered to outpatients; Statistics Netherlands provides data on dispensed medicines, including those related to mental health conditions as determined by ATC (anatomical therapeutic chemical) coding; Australia collects administrative data on dispensed medications covered under the Pharmaceutical Benefits Scheme; and the Slovenian National Institute of Public Health (NIJZ) hosts data on prescription drug claims, including for mental health-related drugs.
In addition, all OECD countries that responded to the questionnaire reported collecting population-wide data on mental health outcomes through household surveys, already prior to the COVID-19 pandemic. While much of these data are collected through health interviews, 89% of countries reported also collecting mental health data in general social surveys (Figure 2.4). Some data on mental health are also collected through labour force surveys and special modules of the national census. Some countries also reported collecting mental health data in special surveys that focus on sub-populations, including Indigenous peoples, those in the criminal justice system and young people (see Box 2.2 for more information on the latter).
Figure 2.4. The majority of OECD countries report measuring population mental health in both health and general social surveys
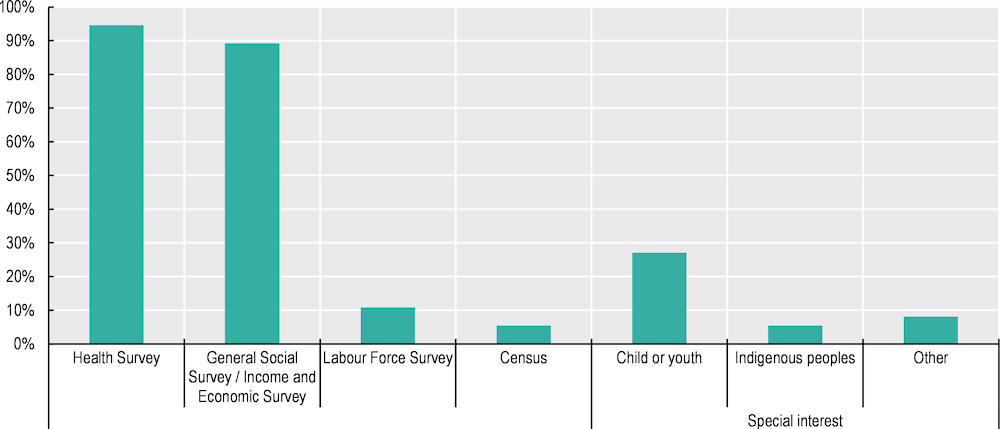
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Many countries have launched surveys with mental health content since the onset of COVID-19, but it is unclear whether these will continue in the future
The pandemic has put mental health high on the national agenda for many OECD countries. As a result, most countries that answered the OECD questionnaire reported having ramped up data collection efforts on mental health in the months and years since March 2020. Around 68% of OECD countries reported collecting additional mental health data during the pandemic, either through new stand-alone surveys (43%) or by adding mental health and COVID-19 modules to existing surveys (35%) (see Table 2.3).5 Many of these new surveys are high-frequency, interviewing respondents weekly, biweekly, monthly or quarterly. However, it is unclear whether these surveys will continue in the future, or continue with the same frequency. Indeed, some COVID-specific surveys have already been discontinued by countries, while others that started off as weekly or monthly have since become less frequent (biweekly or quarterly).
Before 2020, only 22% of countries collected mental health data on surveys that ran annually or more frequently, and 11% on surveys that ran every two to three years. Returning to business as usual prior to the pandemic would mean that over half (51%) of countries collect mental health data every four to ten years. Such large gaps between survey rounds make it more difficult to track changes at the population-level (which as has been seen during the COVID-19 pandemic were sensitive to periods of intensifying COVID‑19 deaths and strict confinement measures) and craft policy interventions accordingly.
Figure 2.5. Many OECD countries collect mental health data infrequently, with over half reporting four-to-ten-year lags between survey rounds
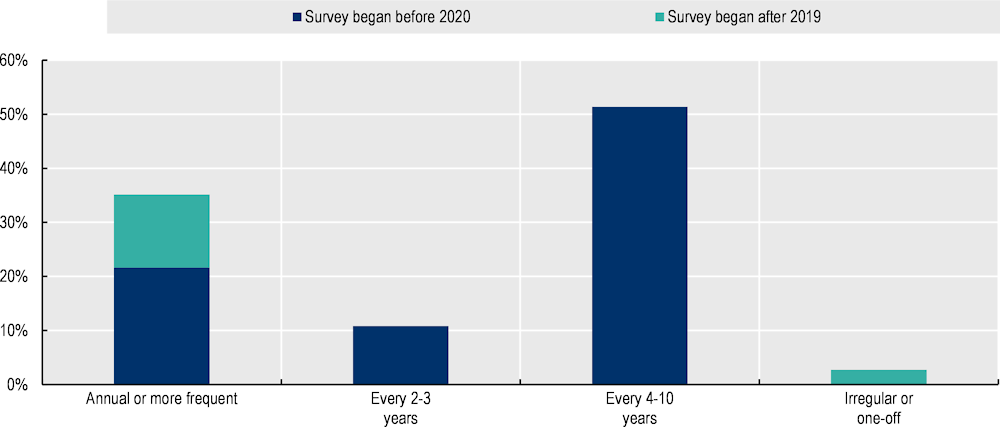
Note: This figure considers only the most frequently run survey per country, rather than the full set of surveys containing mental health data that countries report. It thus shows the highest degree of frequency for which mental health are available, per country. Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Box 2.2. Initiatives to collect data on mental health for children and youth
The mental health of young people suffered dramatically during the COVID-19 pandemic (OECD, 2021[18]; OECD, 2021[19]), and a number of OECD countries launched campaigns focusing on youth mental health in 2021 and 2022 to help combat increasing rates of suicide, reported anxiety, depression and general psychological stress (HHS, 2021[20]; Chile, 2021[21]; Santé Publique France, 2021[22]). The results from the OECD questionnaire show that, although the pandemic may have underscored the importance of focusing on young people, many OECD countries were already implementing child or youth-specific surveys with mental health modules (Table 2.2).
The measurement of child and youth mental health differs from that of adults in several ways. Some surveys use the same tools for children and adults – questions about previous diagnoses, standardised composite scales such as the WHO-5, negative affect questions – however, there are also some youth-specific validated screening tools. A number of countries answering the OECD questionnaire reported using the Strengths and Difficulties Questionnaire (SDQ), a behavioural screening tool for children and youth aged three to 16, or the Development and Well-Being Assessment (DAWMA), to screen for psychiatric diagnoses for children starting at age of two. Child and youth surveys often include modules covering behavioural and emotional issues, adverse childhood experiences, positive childhood experiences and substance use/abuse, and can contain questions that are posed to children, parents or teachers (Table 2.11). Some surveys also cover previous diagnoses of attention deficit hyperactivity disorder (ADHD) or autism spectrum disorder (ASD).
Table 2.2. Many countries have introduced child and youth surveys, or survey modules, with a mental health focus
|
Country |
Survey |
|---|---|
|
Australia |
Australian Child and Adolescent Survey of Mental Health and Wellbeing |
|
Canada |
Canadian Health Survey of Children and Youth (CHSCY) |
|
Germany |
Study on the Health of Children and Adolescents in Germany (KiGGS) |
|
Italy |
Quality of Life in Children and Adolescents* |
|
Luxembourg |
Youth Survey Luxembourg |
|
United Kingdom |
Mental Health of Children and Young People Surveys |
|
United States |
Youth Risk Behavior Survey (YRBS) National Health Interview Survey (NHIS)† |
|
Denmark, Ireland, Italy, Latvia, Luxembourg, Slovenia, Sweden |
Health Behaviour in School-Aged Children (HBSC) |
Note: The HBSC is a school-based survey, not a household survey. * indicates the survey was introduced following the start of the pandemic (post-March 2020). † The NHIS includes the Strengths and Difficulties Questionnaire (SDQ) in the child component of the rotating core module. Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.3. Over half of OECD countries reported increasing the collection of mental health data during the COVID-19 pandemic
|
Country |
Stand-alone COVID survey |
COVID module added to existing survey |
Any COVID-related survey |
|---|---|---|---|
|
Australia |
● |
● |
|
|
Austria |
|||
|
Belgium |
● |
● |
|
|
Canada |
● |
● |
|
|
Chile |
● |
● |
|
|
Colombia |
● |
● |
|
|
Costa Rica |
● |
● |
|
|
Czech Republic |
|||
|
Denmark |
|||
|
Finland |
● |
● |
|
|
France |
● |
● |
● |
|
Germany |
● |
● |
● |
|
Greece |
|||
|
Hungary |
|||
|
Iceland |
● |
● |
|
|
Ireland |
● |
● |
|
|
Israel |
● |
● |
|
|
Italy |
● |
● |
|
|
Japan |
|||
|
Korea |
● |
● |
|
|
Latvia |
|||
|
Lithuania |
|||
|
Luxembourg |
● |
● |
|
|
Mexico |
● |
● |
|
|
Netherlands |
● |
● |
|
|
New Zealand |
● |
● |
|
|
Norway |
● |
● |
|
|
Poland |
|||
|
Portugal |
|||
|
Slovak Republic |
|||
|
Slovenia |
● |
● |
|
|
Spain |
● |
● |
|
|
Sweden |
● |
● |
● |
|
Switzerland |
● |
● |
|
|
Türkiye |
|||
|
United Kingdom |
● |
● |
|
|
United States |
● |
● |
● |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
The focus of household surveys is mainly on mental ill-health
All OECD countries collect data on both mental ill-health and positive mental health outcomes. For the former, there is much variety in terms of both the tools used and outcomes measured, whereas for the latter cross-country comparative data are mainly limited to measures of life evaluation (Figure 2.6); 59% of countries reported collecting data on affect, and only 24% on eudaimonia.
Figure 2.6. All OECD countries reported collecting data on mental ill-health and positive mental health, with the latter mostly focused on life evaluation
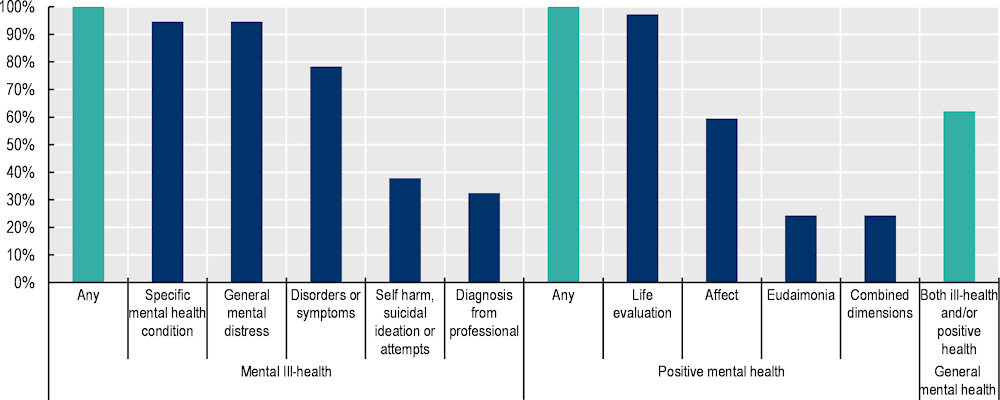
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Note that the question collected during the EU-SILC 2013 ad hoc well-being module, on the extent to which respondents feel that their life is worthwhile, was not included in this figure given that the question was removed from subsequent well-being modules.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Mental ill-health outcome measures are captured through a variety of tools. The two tools most often reported by countries are screening tools and questions about experienced symptoms or disorders (either general or specific), with 97% and 78% of countries reporting using these types of tools in household surveys, respectively (Figure 2.7). Over half of countries (62%) ask single questions about people’s general mental health status. Many fewer countries report collecting data on previous diagnoses in household surveys (30%) or in structured interviews (16%).
Figure 2.7. Screening tools and questions about experience of symptoms and disorders are the most common mental ill-health tools reported by countries
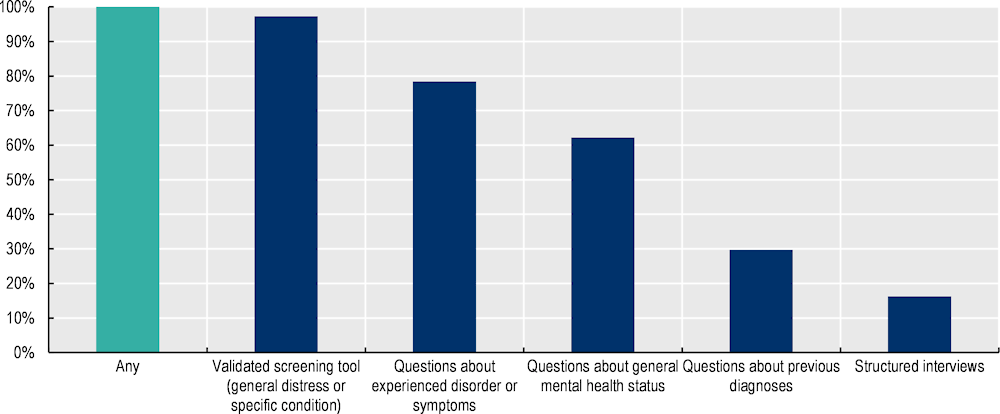
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
General psychological distress and symptoms of depression tend to be captured by standardised screening tools, whereas measures of experiencing anxiety are often not harmonised across countries
Within the continuum of mental ill-health, existing measurement initiatives focus more on some forms of mental health issues than on others. Anxiety and depressive disorder are the most common mental health conditions affecting people in OECD countries (OECD/European Union, 2018[23]).While 86% of countries (32 out of 37) have a dedicated validated screening tool for measuring symptoms of depression, and 95% have one for general psychological distress (35 out of 37), only 41% rely on a screening tool for symptoms of anxiety (15 out of 37) (Figure 2.8). Screening tools used by countries vary widely in terms of item length, ranging from two to 40 questions (see Table 2.5).
Variants of the PHQ are the most common screening tool for measuring symptoms of depression, used by 84% (31 out of 37) of countries. The MHI-5 is the most common screening tool for general psychological distress, used by 76% of countries (28 out of 37). In both instances, this is largely driven by Eurostat, which harmonises the data collection efforts of European Union member countries: 26 of the 28 countries that rely on the MHI-5 participate in Eurostat, all but Australia and Israel.6 The PHQ-8 has been included in Eurostat’s European Health Interview Survey (EHIS), which is conducted every five to six years. Variants of the PHQ are also used by a number of non-European OECD countries (see Table 2.5).
Figure 2.8. Screening tools capturing general psychological distress and symptoms of depression are more commonly used than those for symptoms of anxiety or other disorders
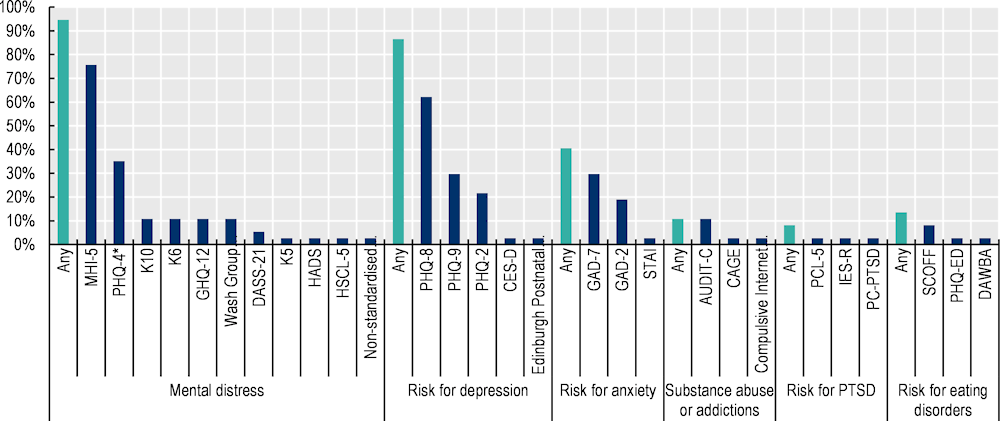
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Note that the MHI-5 and PHQ-8 findings are partly driven by Eurostat, although a number of other non-European OECD countries also use these, especially the PHQ-8. The MHI-5 will not be repeated in future EU-SILC ad hoc well-being modules, which will reduce the share of countries regularly collecting it.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
OECD countries also collected data on symptoms of anxiety, although often through country-specific tools rather than validated screening tools (Figure 2.9). 70% of countries report capturing anxiety outcomes, through some combination of structured interviews, questions about previous diagnoses or about experience of anxiety disorders, affect data or validated screening tools. Considering all measurement tools included in surveys, more countries indicated using them primarily for measuring symptoms of depression. The only exceptions are questions about negative affect, for which usage is evenly divided: 30% of countries reported using negative affect to measure both anxiety (feeling nervous, anxious) and depression (feeling low, downhearted).
The focus of measurement initiatives on depressive and anxiety disorders reflects the fact that they are some of the most prevalent mental health conditions (OECD/European Union, 2018[23]), and that they contribute highly to the disease burden globally and in OECD countries (Santomauro et al., 2021[24]). Data collection efforts for other specific mental conditions – such as PTSD, bipolar disorder, eating disorders, etc. – remain very uneven across OECD countries (Figure 2.8).
Figure 2.9. Countries do capture anxiety data, but often with non-standardised measures
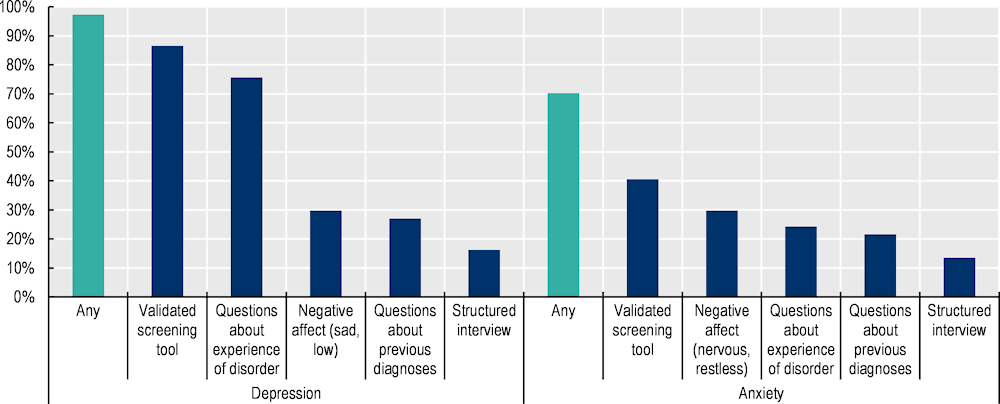
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Most countries collect comparative data on life evaluation, but less so on affect and eudaimonia
Almost all OECD countries collect some data on life evaluation, primarily through a question on self-reported life satisfaction. Other aspects of positive mental health – affect and eudaimonia – are much less frequently covered by surveys undertaken by OECD countries; even when they are, the tools used are less standardised across countries (Figure 2.10). Measures of affect are more commonly collected than of eudaimonia; 59% of countries collect some form of affect data, through a combination of standardised composite scales and non-harmonised questions, while only 24% collect data on eudaimonia. In terms of standardised tools for measuring positive mental health outcomes, the SF-12 (and the SF-36 sub-component on energy and vitality, EVI), WHO-5 and either WEMWBS or its shorter form SWEMWBS are the three most common instruments; however, their overall use is still low: 30%, 16% and 19% of countries reported using each scale in a household survey, respectively.
Figure 2.10. Affect data are more commonly collected than eudaimonic data, but OECD countries are not aligned in the tools used to collect data on positive mental health beyond life satisfaction
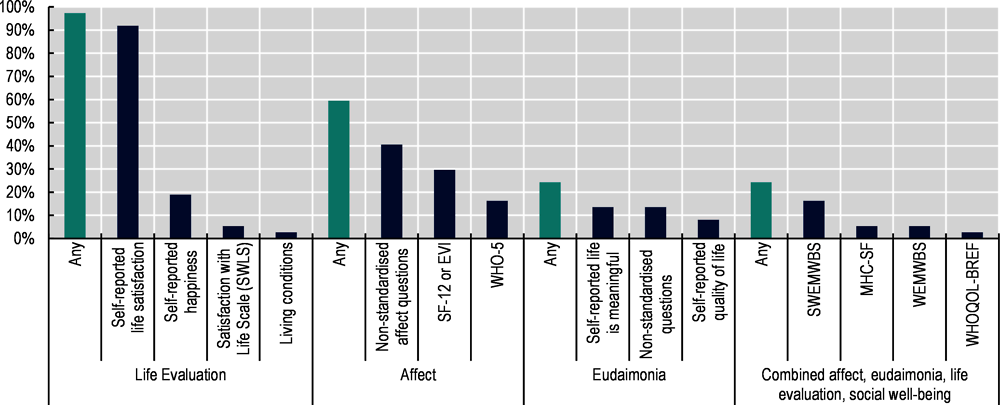
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Note that the question collected during the EU-SILC 2013 ad hoc well-being module, on the extent to which respondents feel that their life is worthwhile, was not included in this figure given that the question was removed from subsequent well-being modules.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
There are interesting recent developments in topics such as data collection on mental health awareness
Overall, data collection efforts on additional mental-health related topics (e.g. use of mental health medication and services; mental health of children and young people in the household; loneliness and stress; resilience and self-efficacy; attitudes towards mental health, including stigma and literacy; and questions on unmet needs) are also uneven across countries (see Table 2.11). Many of these issues are not yet well-defined conceptually, with few internationally standardised tools available. For instance, only 30% of countries reported collecting (very different) indicators covering the topics of mental health stigma, discrimination, literacy and knowledge of mental health issues and resources.7 However, some countries have recently launched new survey efforts – and developed new methods – given increased interest in mental health awareness. For instance, in 2021 Sweden’s Public Health Agency conducted an online population survey, covering more than 10 000 respondents, on knowledge and attitudes about mental illness and suicide (Public Health Agency Sweden, 2022[25]). After systematically reviewing more than 400 existing instruments for measuring mental health stigma and conducting cognitive testing, the Public Health Agency concluded that the overwhelmingly negative tone of existing measures was in itself stigmatising and focused mostly on examples of severe mental illness. They hence decided to develop their own survey: the final questionnaire included items that were designed as semantic differentials (word pairs) that captured both positive and negative perceptions of mental illness and focused on all forms of mental illness, including more common experiences of depression, anxiety and stress-related conditions (Public Health Agency Sweden, 2022[25]).
Conclusion and ways forward
Measuring population mental health outcomes is not a new field for producers of official data in OECD countries, and many national statistical offices and health agencies were already collecting relevant data well before COVID-19. Nevertheless, it is also clear that there is room for improvement moving forward.
First, some aspects of mental health are measured more frequently than others, and there is scope for better cross-country harmonisation. The results of the OECD questionnaire to official data producers suggest that existing data collection efforts are not capturing the full range of mental health outcomes – missing aspects of both mental ill-health as well as positive mental health. While 86% of countries use a screening tool for symptoms of depression, and 95% for general psychological distress, only 41% use a standardised screening tool for symptoms of anxiety – and generalised anxiety disorder, along with mood disorders, is one of the most common mental health conditions affecting people in OECD countries. Data collection efforts for other specific mental conditions – such as post-traumatic stress disorder, bipolar disorder, eating disorders, etc. – remain very uneven across countries. When it comes to positive mental health, almost all countries gather some form of life evaluation data, but information about affect and eudaimonia is much less frequently collected (by 59% and 24% of countries, respectively), and often not in a standardised manner. Data producers could hence as a first step expand their use of screening tools to those that include symptoms of anxiety, as well as depression, and move towards more harmonisation for affective and eudaimonic aspects of positive mental health.
Second, it will be important to measure mental health outcomes regularly, and to keep up some of the momentum provided by the high frequency surveys with mental health modules initiated during the first two years of the pandemic. Given the trade-offs between response burden and accuracy that data producers face when choosing between different tools to measure mental health outcomes, adding a single question about people’s general mental health status to frequently conducted population surveys could be a way to gather this information regularly and help link data across surveys. Over half of countries (62%) already include such single items in surveys, though question wording varies widely. Canada has been an early leader in developing single-item self-reported mental health (SRMH) indicators, and its question formulation has already been adopted by Chile and Germany, which could make it a useful model for other countries moving forward. While questions about previous diagnoses received by health care professionals are also short, evidence suggests that they focus mostly on people who have been in touch with the health system and hence are better placed in health surveys only.
Chapter 3 reviews the available evidence on the statistical quality of these recommended tools in further detail and provides suggestions for three concrete measures that countries could adapt to maximise international harmonisation and minimise response burden.
Lastly, whichever results are communicated to policy makers or the general public, it is essential to be transparent as to which exact aspect of mental health is being measured, including which areas a specific tool covers and does not cover (e.g. only previous diagnosis? only affect, or also somatic symptoms, and if so, which ones?). This information is important to contextualise findings and to provide transparency as to any limitations that might impact the interpretation of results.
Annex 2.A. Mental health survey measures by country
Table 2.4. Overview of structured interviews to monitor mental health conditions
|
Focus |
Tool |
Abbreviation |
Number of items |
Frame of reference |
Time to complete |
Already collected by |
|---|---|---|---|---|---|---|
|
Diagnosis of mental condition according to ICD-10 and DSM-IV |
Composite International Diagnostic Interview |
CIDI |
More than 300 symptom questions but because of skip rules not all of them are asked to every respondent |
75 mins |
Australia, Canada, Chile, Germany, Korea, United States (depressive symptoms only) |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. For more details on the tool, see Annex 2.B.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.5. Overview of validated screening tools to monitor both general mental ill-health and risk for specific mental health conditions
|
Focus |
Covers |
Tool |
Abbreviation |
Number of items |
Frame of reference |
Already collected by country |
|---|---|---|---|---|---|---|
|
Psychological distress |
Negative and positive affect |
Mental Health Inventory -5 |
MHI-5 |
5 |
Past month |
Australia, Austria, Belgium, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, Netherlands, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Türkiye, United Kingdom |
|
Psychological distress |
Negative affect, functional impairment |
Kessler Scale 10 |
K10 |
10 |
Past 4 weeks |
Australia, Canada, Netherlands, New Zealand |
|
Psychological distress |
Negative affect |
Kessler Scale 6 |
K6 |
6 |
Past 4 weeks |
Australia, Japan, Sweden, United States |
|
Psychological distress |
Negative and positive affect, somatic symptoms, functional impairment |
General Health Questionnaire |
GHQ-12 |
12 |
Recently |
Australia, Belgium, Finland, Spain, United Kingdom |
|
Symptoms of depression and anxiety |
Negative affect, anhedonia, functional impairment |
Patient Health Questionnaire -4 |
PHQ-4 |
4 (2 depression, 2 anxiety) |
Past 2 weeks |
Australia, Belgium, Canada, Chile, Finland, France, Germany, Iceland, Korea, Slovenia, Switzerland, United Kingdom, United States |
|
Symptoms of depression and anxiety |
Negative and positive affect, anhedonia |
Hospital Anxiety and Depression Scale |
HADS |
14 (7 depression, 7 anxiety) |
Past week |
France |
|
Symptoms of depression and anxiety |
Negative affect |
Hopkins Symptom Checklist |
HSCL-5 |
5 |
Past week |
Norway |
|
Symptoms of depression and anxiety |
Negative affect, anhedonia, somatic symptoms, functional impairment |
Depression, Anxiety and Stress Scale |
DASS-21 |
21 (7 depression, 7 anxiety, 7 chronic non-specific stress) |
Past week |
Australia, Italy |
|
Symptoms of depression and anxiety among the general and disabled population |
Negative affect, functional impairment |
Washington Group on Disability Statistics Short Set on Functioning – Enhanced |
WG-SS Enhanced |
12 (2 depression, 2 anxiety) |
General |
Australia, Canada, New Zealand, United States |
|
Symptoms of depression and anxiety among the general and disabled population |
Negative affect, functional impairment |
Washington Group Extended Set on Functioning |
WG-ES |
37 (3 depression, 3 anxiety) |
General |
United States |
|
Depressive symptoms |
Negative affect, anhedonia, somatic symptoms, functional impairment (matched to major depressive disorder per DSM-IV and DSM-5 criteria) |
Patient Health Questionnaire -8 |
PHQ-8 |
8 |
Past 2 weeks |
Austria, Czech Republic, Denmark, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Netherlands, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Türkiye, United Kingdom, United States |
|
Depressive symptoms |
Negative affect, anhedonia, somatic symptoms, functional impairment (matched to major depressive disorder per DSM-IV and DSM-5 criteria) |
Patient Health Questionnaire -9 |
PHQ-9 |
9 (PHQ-8 + question on suicidal ideation) |
Past 2 weeks |
Australia, Belgium, Canada, Finland, France, Germany, Italy, Korea, Slovenia, Switzerland, United States |
|
Depressive symptoms |
Negative affect, anhedonia |
Patient Health Questionnaire -2 |
PHQ-2 |
2 |
Past 2 weeks |
Australia, Canada, Chile, Finland, Germany, Italy, Norway, United States |
|
Depressive symptoms |
Negative and positive affect, anhedonia, somatic symptoms, functional impairment, interpersonal challenges |
Center for Epidemiological Studies Depression Scale |
CES-D |
20 |
Past week |
Mexico |
|
Symptoms depression among recent mothers |
Negative and positive affect, anhedonia, functional impairment |
Edinburg Post-natal Depression Scale |
EPDS |
6 |
Past week |
Italy |
|
Symptoms of anxiety |
Negative affect, somatic symptoms, functional impairment |
Generalised Anxiety Disorder-7 |
GAD-7 |
7 |
Past 2 weeks |
Australia, Belgium, Canada, Finland, France, Germany, Iceland, Korea, Slovenia, Switzerland, United States |
|
Symptoms of anxiety |
Negative affect, functional impairment |
Generalised Anxiety Disorder-2 |
GAD-2 |
2 |
Past 2 weeks |
Australia, Canada, Chile, Germany, Mexico, United Kingdom, United States |
|
Symptoms of anxiety |
Negative affect,(including panic-like anxiety), functional impairment, subjective well-being |
The State and Trait Anxiety Scale |
STAI |
40 (20 state anxiety, 20 trait anxiety) |
State anxiety: “in this moment”, trait anxiety: “generally” |
Italy |
|
Symptoms of panic disorder |
Presence and severity of anxiety attacks, somatic symptoms |
Patient Health Questionnaire-Panic Disorder |
PHQ-PD |
15 |
Past 4 weeks |
Germany, Switzerland |
|
Symptoms of post-traumatic stress disorder (PTSD) |
Presence and severity of PTSD symptoms (matched to DSM-5 criteria) |
PTSD Checklist for DSM-5 |
PCL-5 |
20 |
Past 4 weeks |
Canada |
|
Symptoms of PTSD |
Presence and severity of PTSD symptoms (matched to DSM-5 criteria) |
Primary Care PTSD Screen for DSM-5 |
PC-PTSD-5 |
5 |
Past 4 weeks |
Switzerland |
|
Symptoms of PTSD |
Presence and severity of PTSD symptoms (matched to DSM-IV criteria) |
Impact of Event Scale – revised |
IES-R |
22 |
Past week |
Italy |
|
Symptoms of agoraphobia |
Presence and severity of anxiety related to different aspects of everyday life |
Angstbarometer |
Angstbarometer |
12 |
Past year |
Switzerland |
|
Symptoms of social anxiety disorder |
Presence and severity of symptoms of social anxiety disorder |
Mini-Social Phobia Inventory |
Mini-SPIN |
3 |
Past week |
Finland, Switzerland |
|
Symptoms of substance abuse or addiction |
Presence and severity of symptoms of alcoholism |
CAGE Substance Abuse Screening Tool |
CAGE |
4 |
No specific recall period |
Belgium |
|
Symptoms of substance abuse or addiction |
Presence and severity of symptoms of alcoholism |
Alcohol Use Disorders Identification Test-Concise |
AUDIT-C |
3 |
No specific recall period |
Chile, Sweden |
|
Symptoms of substance abuse or addiction |
Presence and severity of symptoms of alcoholism |
Alcohol Use Disorders Identification Test |
AUDIT |
10 |
No specific recall period |
France, Spain |
|
Symptoms of substance abuse or addiction |
Presence and severity of Internet addiction and compulsive, pathological, or problematic online behaviours (matched to DSM-IV criteria for substance addiction and pathological gambling) |
Compulsive Internet Use Scale |
CIUS |
14 |
No specific recall period |
Switzerland |
|
Symptoms of eating disorders |
Presence and severity of symptoms of anorexia nervosa and bulimia nervosa |
SCOFF |
SCOFF |
5 |
Past 3 months |
Belgium, Finland, Germany |
|
Symptoms of eating disorders |
Presence and severity of symptoms of binge eating disorder, bulimia nervosa and recurrent binge eating |
Patient Health Questionnaire-Eating Disorder Module |
PHQ-ED |
6 |
Past 3 months |
France |
|
Symptoms of eating disorders in 7-17 year-olds |
Presence and severity of symptoms of eating disorders |
Screening questions from the Development and Wellbeing Assessment – Eating Disorder Module |
DAWBA |
5 |
No specific recall period |
United Kingdom |
Note: Countries in italics are those that have explicitly stated that they no longer collect the measure in question. Countries in bold did not report collecting the instrument in their official questionnaire submission, however, it was added by the OECD Secretariat based on the country’s participation in the European Health Interview Survey (EHIS), which contains the PHQ-8 as a core module. The PHQ-4 country practice was added in by the Secretariate for countries collecting both the PHQ and GAD (from which the PHQ-4 pulls its indicators), regardless of individual country reporting on the PHQ-4 itself. Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations. For details of the tools collected by at least two OECD countries, see Annex 2.B.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.6. Overview of questions about previous diagnoses
|
Category |
Example question framing |
Answer options |
Frame of reference |
Already collected by country |
|---|---|---|---|---|
|
Received diagnosis of any mental health condition |
Have you been told by a doctor or nurse that you have any of these long-term health conditions? List: Mental health condition (including depression or anxiety) (AUS) Have your mental health problems ever been diagnosed as a mental disorder by a professional (psychiatrist, doctor, clinical psychologist)? (SVN) |
Yes / No |
Lifetime |
Australia, Slovenia |
|
Received diagnosis of any mood disorder (including depression) |
Have you ever in your life been diagnosed by a doctor with any of the following health problems or illnesses? In the event that you have been diagnosed any of them, have you received or are you undergoing medical treatment? Depression or anxiety (CHL) During your life, has a doctor ever told you that you had a psychiatric or psychological disorder or an addiction? Depression or depressive episode (FRA) |
Yes / No |
Lifetime, last 12 months, or during COVID |
Australia, Austria, Canada, Chile, Costa Rica, France, New Zealand, Slovenia, Spain, United States |
|
Received diagnosis of anxiety disorder |
Have you ever been told by a doctor, nurse or other health professional that you have any of these conditions? Anxiety (AUS) Has a health professional ever told you that you have…? Chronic anxiety (CRI) During your life, has a doctor ever told you that you had a psychiatric or psychological disorder or an addiction? Anxiety disorder (generalised anxiety, phobia, obsessive compulsive disorder, etc.) (FRA) |
Yes / No |
Lifetime, during COVID |
Australia, Chile, Costa Rica, France, New Zealand, Slovenia, Spain, United States |
|
Received diagnosis of bipolar disorder or mania |
Have you ever been told by a doctor that you have bipolar disorder, which is sometimes called manic depression? (NZL) |
Yes / No |
Lifetime, during COVID |
Australia, France, New Zealand, Slovenia |
|
Received diagnosis of post-traumatic stress disorder (PTSD) |
Have you ever been diagnosed with PTSD? (CAN) |
Yes / No |
Lifetime |
Australia, Canada |
|
Received diagnosis of obsessive compulsive disorder (OCD) |
Have your mental health problems ever been diagnosed as a mental disorder by a professional (psychiatrist, doctor, clinical psychologist)? Obsessive compulsive disorder (SVN) |
Yes / No |
Lifetime |
Australia, Slovenia |
|
Received diagnosis of schizophrenia or other psychotic disorders |
During your life, has a doctor ever told you that you had a psychiatric or psychological disorder or an addiction? Schizophrenia (FRA) |
Yes / No |
Lifetime, during COVID |
France, Slovenia |
|
Received diagnosis of personality disorder |
During your life, has a doctor ever told you that you had a psychiatric or psychological disorder or an addiction? borderline personality disorder (FRA) |
Yes / No |
Lifetime, during COVID |
France |
|
Received diagnosis of agoraphobia or social disorder |
Were you told by a doctor, nurse or other health professional that you had [...] mental health condition? Agoraphobia (AUS) |
Yes / No |
Lifetime |
Australia |
|
Received diagnosis of addictive disorder or substance abuse problems |
Have you ever been told by a doctor, nurse or other health professional that you have any of these conditions? Harmful use or dependence on alcohol or drugs (AUS) During your life, has a doctor ever told you that you had a psychiatric or psychological disorder or an addiction? Addiction or addictive disorder (FRA) |
Yes / No |
Lifetime, during COVID |
Australia, France |
|
Received diagnosis of an eating disorder |
Have your mental health problems ever been diagnosed as a mental disorder by a professional (psychiatrist, doctor, clinical psychologist)? Eating disorder (SVN) |
Yes / No |
Lifetime, during COVID |
France, Slovenia |
|
Received diagnosis of conduct disorder or behavioural / emotional problems |
Have you ever been told by a doctor, nurse or other health professional that you have any of these conditions? Behavioural or emotional problems (AUS) Have you ever been diagnosed with conduct disorders by a medical professional? (ESP) |
Yes / No |
Lifetime |
Australia, Spain |
|
Neurodiversity: received diagnosis of attention deficit hyperactivity disorder (ADHD) |
Have [you/name] ever been told by a doctor or other health professional that {you/he/she} had attention deficit hyperactivity disorder (ADHD) or attention deficit disorder (ADD)? (USA) |
Yes / No |
Lifetime |
Germany, United States |
|
Neurodiversity: received diagnosis of autism spectrum disorder (ASD) |
Have you ever been diagnosed with autism by a medical professional? (ESP) |
Yes / No |
Lifetime |
Spain |
|
Received diagnosis of any other mental health condition |
Do you have any other long-term physical or mental health condition that has been diagnosed by a health professional? (CAN) Have your mental health problems ever been diagnosed as a mental disorder by a professional (psychiatrist, doctor, clinical psychologist)? (SVN) |
Yes / No |
Lifetime, last 12 months, or during COVID |
Australia, Canada, Chile, Costa Rica, France, Slovenia |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.7. Overview of questions about experienced symptoms and mental health conditions
|
Category |
Example question framing |
Answer options |
Frame of reference |
Already collected by country |
|---|---|---|---|---|
|
Self-reported mental health problems |
Have you suffered from psychological stress or an acute illness in the last three months? (ISR) Are you currently facing mental health problems? (SVN) Do you have your own experience with mental illness? (SWE) Do you think you ever had a problem with your own mental health? (USA) |
Yes / No |
Lifetime, last 12 months, last 3 months |
Hungary, Israel, Slovenia, Sweden, United States |
|
Self-reported mood disorder (depression, etc.) or mood disorder symptoms |
During the past 12 months, have you had any of the following diseases or conditions? Depression (European OECD countries participating in EHIS) Do you have a mood disorder? (CAN) Next I will ask you some questions related to different chronic diseases or health conditions that you may currently have. Chronic diseases are those of long duration and usually evolve slowly. Do you have chronic depression? (CRI) |
Yes / No |
Lifetime, last 12 months, current |
Australia, Austria, Belgium, Canada, Costa Rica, Czech Republic, Denmark, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Netherlands, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Türkiye, United Kingdom, United States |
|
Self-reported anxiety disorder, or anxiety symptoms |
Do you have an anxiety disorder? (CAN) During the last 12 months did you have or do you have any of the chronic diseases / diseases that are listed: Anxiety disorders (e.g. panic attacks, anxiety) (GRC) Have you ever suffered from chronic anxiety? (ESP) |
Yes / No |
Lifetime, last 12 months, last 3 months, current |
Australia, Canada, Costa Rica, Greece, Hungary, Norway, Slovenia, Spain, Sweden |
|
Self-reported bipolar disorder or mania |
Do you have any of these conditions? Bipolar disorder (AUS) Do you have a mood disorder such as depression, bipolar disorder, mania or dysthymia? (CAN) |
Yes / No |
Lifetime |
Australia, Canada |
|
Self-reported PTSD |
Do you currently experience symptoms of PTSD? (CAN) |
Yes / No |
Lifetime |
Australia, Canada |
|
Self-reported OCD |
Do you have any of these conditions? Obsessive-compulsive disorder (OCD) (AUS) |
Yes / No |
Lifetime |
Australia |
|
Self-reported schizophrenia or other psychotic disorders |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Schizophrenia (AUS) [Do you have] Schizophrenia, schizotypal and delusional disorders (HUN) |
Yes / No |
Lifetime or last 12 months |
Australia, Hungary |
|
Self-reported agoraphobia or social disorder |
Do you have any of these conditions? Agoraphobia (AUS) |
Yes / No |
Lifetime |
Australia |
|
Self-reported addictive disorder or substance abuse problems |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Dependence on alcohol; Dependence on drugs; Harmful use or dependence on medicinal, prescription drugs (AUS) |
Yes / No |
Lifetime or last 12 months |
Australia, Hungary |
|
Self-reported eating disorder |
In the past 12 months, how often have you done the following things? a. Been preoccupied with a desire to be thinner b. Vomited to lose weight c. Changed your eating habits in order to manage your weight (CAN) |
Never / A few times / Monthly / Weekly / Daily |
Last 12 months |
Canada |
|
Self-reported conduct disorder or behavioural / emotional problems |
Have you suffered from conduct disorders in the last 12 months? (ESP) |
Yes / No |
Lifetime or last 12 months |
Australia, Spain |
|
Self-reported ADHD |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Attention Deficit Hyperactivity Disorder (ADHD) (AUS) |
Yes / No |
Lifetime |
Australia |
|
Self-reported ASD |
Have you suffered from autism in the last 12 months? (ESP) |
Yes / No |
Lifetime or last 12 months |
Australia, Spain |
|
Self-reported dementia |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Dementia, including Alzheimer's Disease (AUS) |
Yes / No |
Lifetime |
Australia |
|
Self-reported intellectual impairment |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Intellectual impairment, mental retardation (AUS) |
Yes / No |
Lifetime |
Australia |
|
Self-reported learning disorder |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Learning difficulties, including dyslexia (AUS) |
Yes / No |
Lifetime |
Australia |
|
Self-reported other mental disorder |
(Apart from any conditions you have told me about) do you have any other mental health, behavioural or cognitive conditions, such as these? Any other mental or behavioural condition (AUS) |
Yes / No |
Lifetime or last 12 months |
Australia, Costa Rica, Hungary |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.8. Overview of questions about suicidal ideation and suicide attempts
|
Category |
Example question framing |
Answer options |
Frame of reference |
Already collected by country |
|---|---|---|---|---|
|
Suicidal ideation |
Final question of the PHQ-9 |
Not at all / Several days / More than half the days / Nearly every day |
Last 2 weeks |
Australia, Belgium, Canada, Finland, France, Germany, Italy, Korea, Slovenia, Switzerland, United States |
|
Suicidal ideation |
Have you seriously contemplated suicide since the COVID-19 pandemic began? (CAN) Have you had this experience [seriously considering suicide] in the last 12 months? (CHL) In the last 12 months, have you thought about committing suicide? (FRA) Have you ever been in a situation where you seriously considered taking your own life? (SWE) |
Yes / No |
Lifetime, last 12 months, during COVID |
Australia, Belgium, Canada, Chile, Finland, France, Korea, Mexico, Slovenia, Sweden, Switzerland, United States |
|
Self-harm behaviours |
Sometimes people harm themselves on purpose but they do not mean to take their life. In the past 12 months, did you ever harm yourself on purpose but not mean to take your life? (CAN) During the past 2 weeks, how often did you have thoughts of hurting yourself? (GRC) |
Yes / No Not at all/ Several days/ More than half the days/ Nearly every day |
Lifetime, last 12 months, last 2 weeks |
Australia, Canada, Finland, Greece, Mexico |
|
Suicide attempts |
Did you attempt to commit suicide in the last 12 months? (BEL) Have you attempted to actually commit suicide over the last 12 months? (KOR) Have you ever attempted suicide? (LUX) |
Yes / No |
Lifetime, last 12 months, during COVID |
Australia, Belgium, Canada, Chile, Finland, France, Korea, Luxembourg, Sweden, United States |
|
Suicide attempt led to hospitalisation or required medical care |
Did you stay in a hospital overnight or longer because you tried to kill yourself? (USA) |
Yes / No |
Lifetime or last 12 months |
Australia, United States |
|
Received counselling following suicidal thoughts or suicide attempt |
Following your thoughts of suicide, did you talk to anyone? (CHE) During the past 12 months, did you get medical attention from a doctor or other health professional as a result of an attempt to kill yourself? (USA) |
Yes / No |
Lifetime or last 12 months |
France, Switzerland, United States |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.9. Overview of questions about general mental health status
|
Category |
Example question framing |
Answer options |
Frame of reference |
Already collected by country |
|---|---|---|---|---|
|
Self-reported general mental health status |
In general, how is your mental health? (CAN, CHL, DEU) How is your mental state, usually? (ISR) |
Excellent / Very good / Good / Fair / Poor (AUS, CAN, CHL, DEU) Very good / good / not so good / Not good at all (ISR) |
Current or last 4 weeks |
Australia, Canada, Chile, Costa Rica, Finland, Germany, Iceland, Israel, Slovenia, Switzerland, United States |
|
Self-reported number of mentally healthy days |
During the past 30 days, how often was your mental health not good? (USA) |
[Number of days] |
Last 30 days |
United States |
|
Self-reported recovery |
At this time do you consider yourself to be in recovery or recovered from your own mental health problem? (USA) |
Yes / No |
General assessment |
United States |
|
Self-reported satisfaction with mental health status |
On a scale from 1 to 10 can you indicate to what extent you are satisfied with your mental health? (NLD) How satisfied are you with your mental health? (NOR) |
0 (completely dissatisfied) to 10 (completely satisfied) |
General assessment |
Netherlands, Norway |
|
Self-reported mental health status and COVID-19 |
Compared to before the pandemic started, how would you say your mental health is now? (CAN) Has your mental health/well-being been affected by the COVID-19 pandemic during 2020 / during the last 12 months? (DNK, LVA, PRT, SVK, SVN, TUR) How has your morale been affected by the pandemic? (CHE) During the periods of confinement, have there been times when you have felt so discouraged that nothing could cheer you up? (FRA) |
Much better now / Somewhat better now / About the same / Somewhat worse now / Much worse now (CAN) 1. Yes, has been negatively affected 2. Yes, has been positively affected 3. No, has not been affected (DNK, LVA, PRT, SVK, TUR) 0 (much worse) - 10 (much better) (CHE) Yes / No (FRA) |
During COVID-19 |
Canada, Denmark, Finland, France, Germany, Israel, Japan, Latvia, Netherlands, Portugal, Slovak Republic, Slovenia, Switzerland, Türkiye |
|
Mental health interferes with daily activities (impairment-days) |
Does your mental state interfere with your daily life at work? With family? (ISR) Have you felt very sad or hopeless for more than two weeks over the last 12 months to a degree that you have experienced disruptions in your daily life? (KOR) During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities? (USA) |
Yes / No |
Varies from past 12 months to past 4 weeks |
Australia, Canada, Hungary, Israel, Korea, Spain, United States |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.10. Overview of indicators of positive mental health
|
Components |
Tool |
Abbreviation |
Number of items |
Frame of reference |
Already collected by country |
|---|---|---|---|---|---|
|
Positive affect |
WHO-5 Wellbeing Index |
WHO-5 |
5 |
Last 2 weeks |
France, Hungary, Italy, Latvia, New Zealand, Slovenia |
|
Positive and negative affect, functional impairment (Mental Health Component Summary) |
Short Form Health Status |
SF-12 |
12 |
Last 4 weeks |
Chile, Italy, Netherlands, New Zealand, Spain, United States |
|
Positive and negative affect, functional impairment |
SF-36 |
SF-36 |
36 |
Last 4 weeks |
Australia, Germany |
|
Positive and negative affect |
SF-36 vitality sub-scale |
EVI |
4 |
Last 4 weeks |
Australia, Belgium, Italy, Switzerland |
|
Positive or negative affect |
Non-standardised affect questions Example questions: During the day yesterday, did you feel happy? (FRA) During this period [last 12 months], to what extent did you experience the following feelings? Stress and anxiety (ISR) Now, I am going to mention a series of emotions or feelings. How often have you felt… during the last two weeks? Angry Optimistic Worried Happy Sad Calm Tired Useful (CHL) |
NA 0 (least happy) – 10 (happiest) (FRA) To a large extent / Certain / Not so much / Not at all (ISR) Never, almost never sometimes, almost always or always (CHL) |
Varies from 1 to 8 |
Varies from yesterday to last year |
Chile, Costa Rica, Finland, France, Ireland, Israel, Italy, Japan, Latvia, Netherlands, New Zealand, Norway, Slovenia, Sweden, United Kingdom |
|
Eudaimonia |
Self-reported feeling that life is worthwhile or meaningful Example questions: Do you feel that what you do in your life has meaning, value? Answer on a scale of 0 (no meaning) to 10 (full of meaning) (FRA) How would you usually describe yourself? Would you say: 1: Happy and interested in life 2: Somewhat happy 3: Somewhat unhappy 4: Unhappy with little interest in life 5: So unhappy that life is not worthwhile (CAN) |
NA |
1 |
General assessment |
Australia, Austria, Belgium, Canada, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Japan, Latvia, Lithuania, Luxembourg, Netherlands, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Türkiye, United Kingdom |
|
Eudaimonia |
Self-reported quality of life Example question: Would you rate your quality of life as... ? 1: Excellent 2: Very good 3: Good 4: Fair 5: Poor (CAN) |
NA |
1 |
General assessment |
Canada, Costa Rica, Finland, Switzerland |
|
Eudaimonia |
Self-reported satisfaction with self Example question: How satisfied are you with...… yourself? (CRI) |
1 Very satisfied, 2 Satisfied, 3 Moderately satisfied, 4 Dissatisfied, 5 Very dissatisfied |
1 |
General assessment |
Costa Rica, Finland |
|
Eudaimonia |
Self-reported sense of purpose, accomplishment or achievement of goals Example questions: So far, I have achieved the goals that are important to me in life (MEX) My life has a clear sense of purpose (USA) Most days I feel a sense of accomplishment from what I do (USA) |
NA |
1 |
General assessment |
Mexico, United States |
|
Eudaimonia |
Self-reported sense of being a beneficial participant of society Example question: How do you feel about yourself being an important and beneficial participant of the society? (HUN) |
NA |
1 |
General assessment |
Hungary |
|
Life evaluation |
Self-reported life satisfaction Example question: Overall, how satisfied are you with life as a whole these days? Please answer on a scale from 0 to 10. 0 means “not at all satisfied” and 10 means “completely satisfied”. (European OECD countries participating in EU-SILC well-being modules) |
NA |
1 |
General assessment |
Australia, Austria, Belgium, Canada, Chile, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Korea, Latvia, Lithuania, Luxembourg, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Türkiye, United Kingdom, United States |
|
Life evaluation |
Satisfaction with Life Scale (SWLS) |
SWLS |
5 |
General assessment |
Norway, Slovenia |
|
Life evaluation |
Self-reported happiness Example question: Overall, how happy do you think you are? Please check one box on a scale of 1- 10 where 1 means very unhappy and 10 very happy. (ISL) |
NA |
1 |
General assessment |
Chile, France, Iceland, Japan, Netherlands, Switzerland, United States |
|
Life evaluation |
Self-reported living conditions Example question: Currently the living conditions in your household are: 1. Very good; 2. Good; 3. Fair; 4. Bad (COL) |
NA |
1 |
General assessment |
Colombia |
|
Positive affect, eudaimonia, life satisfaction, social well-being |
Mental Health Continuum Short Form |
MHC-SF |
14 |
Past month |
Canada, Slovenia |
|
Positive affect, eudaimonia, social well-being |
Warwick- Edinburgh Mental Well-Being Scale |
WEMWBS |
14 |
Last 2 weeks |
Finland, Norway* |
|
Positive affect, eudaimonia, social well-being |
Short Warwick- Edinburgh Mental Well-Being Scale |
SWEMWBS |
7 |
Last 2 weeks |
Canada, Finland, Germany, Iceland, Sweden, United Kingdom |
|
Positive and negative affect, eudaimonia, self-esteem, concentration |
WHO Quality of Life-BREF psychological health domain |
WHOQOL-BREF |
6 |
Last 2 weeks |
Chile |
Note: *Norway does not currently collect WEMWBS but indicated that the tool may be included in future rounds of the National Survey on Quality of Life. Countries in italics are those that have explicitly stated that they no longer collect the measure in question. Countries in bold did not report collecting the instrument in their official questionnaire submission, however, it was added by the OECD Secretariat based on the country’s participation in the European Union Statistics on Income and Living Conditions (EU-SILC), which contained the question "Overall, to what extent do you feel that the things you do in your life are worthwhile?" in the 2013 ad-hoc module focusing on well-being; the measure was not included again in 2018. Countries in bold and italics did not report collecting the instrument in their official questionnaire, however, it was added by the OECD Secretariat based on the country’s participation in a 2016 OECD questionnaire on subjective well-being measures. Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations. For details of the tools collected by at least two OECD countries, see Annex 2.B.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Table 2.11. High-level overview of additional mental health-related topics collected by countries
|
Topic Area |
Types of Tools Used |
Types of Indicators Collected |
Already collected by country |
|---|---|---|---|
|
Access to / use of mental health services |
Self-reported non-standardised questions |
Sought care from a mental health professional (psychologist, psychiatrist, etc.) |
Australia, Canada, Chile, Colombia, Finland, France, Ireland, Japan, Korea, Luxembourg, New Zealand, Slovenia, United States |
|
Medication prescribed or taken (anti-depressants, anxiolytics) |
Belgium, Canada, Chile, Finland, France, Germany, Norway, Slovenia, Spain |
||
|
Mental health of children and young people |
Standardised screening tools, diagnoses and experienced symptoms |
Strengths and Difficulties Questionnaire (SDQ); KIDSCREEN-27 and KIDSCREEN-10; Screen for Child Anxiety and Related Emotional Disorders (SCARED); Short Moods and Feelings Questionnaire (SMFQ) |
Australia, Belgium, Finland France, Germany, Italy, Slovenia, Spain, United Kingdom, United States |
|
Diagnostic and reported experience of conduct disorders, behavioural and emotional issues, positive and adverse early childhood experiences, and substance use/abuse behaviours |
Canada, Italy, Spain, Türkiye, United States |
||
|
Loneliness and stress |
Standardised screening tools, non-standardised self-reported indicators |
Loneliness and social connections: UCLA Loneliness Scale, Oslo Social Support Scale; Multidimensional Scale of Perceived Social Support; non-standardised indicators |
Australia, Austria, Belgium, Canada, Colombia, Costa Rica, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Latvia, Lithuania, Luxembourg, Netherlands, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, United States, United Kingdom |
|
Stress: Cohen Perceived Stress Scale (PSS); non-standardised indicators |
Canada, Colombia, Iceland, Israel, Italy, Korea, Latvia, Slovenia, Sweden |
||
|
Resilience, optimism and self-efficacy |
Standardised composite scales, non-standardised self-reported indicators |
Pearlin and Schooler’s Mastery Scale, General Self-Efficacy Scale, Brief Resilient Coping Scale, Short Sense of Coherence Questionnaire, Connor-Davidson Resilience Scale (CD RISC-10), Single Item Self-esteem Scale; non-standardised indicators |
Australia, Canada, Germany, Italy, Norway, Slovenia, Switzerland |
|
Attitudes towards mental health |
Standardised composite scales, non-standardised self-reported indicators |
Non-standardised indicators covering topics of stigma, discrimination, literacy and knowledge of mental health issues and resources |
Costa Rica, Hungary, Italy, Japan, Korea, Mexico, New Zealand, Norway, Slovenia, Sweden |
|
Mental health literacy: Depression and Anxiety Literacy questionnaire (D-Lit; A-Lit) |
Slovenia |
Note: Results are shown for all OECD countries except Estonia, which did not participate in the questionnaire. Data for the United Kingdom include only surveys carried out by the Office for National Statistics on mental health and do not include the data collected by devolved administrations. Countries in bold did not report collecting the instrument in their official questionnaire submission, however, it was added by the OECD Secretariat based on the country’s participation in the European Health Interview Survey (EHIS), which contained the Oslo Social Support Scale (OSS-3) in waves 2 and 3.
Source: Responses to an OECD questionnaire sent to national statistical offices in January 2022.
Annex 2.B. Details on standardised survey tools to measure mental health
Mental ill-health
Mental health conditions: Structured interviews
Composite International Diagnostic Interview (CIDI): The Composite International Diagnostic Interview (CIDI) is a comprehensive, fully-structured interview designed to be used by trained lay interviewers for the assessment of mental disorders according to the definitions and criteria of ICD-10 and DSM-IV (Kessler and Bedirhan Üstün, 2006[26]). A computer-assisted version of the interview is available along with a direct data entry software system that can be used to keypunch responses to the paper-and-pencil version of the interview. The CIDI is intended for use in epidemiological and cross-cultural studies as well as for clinical and research purposes. It allows investigators to measure the prevalence of lifetime and 12-month mental conditions, the severity and courses of these disorders, their impact on home management, work life, relationships and social life, and service and medications use. Several versions of the CIDI exist, but the latest version is the World Health Organization’s Composite International Diagnostic Interview (WHO-CIDI) V3.0 (Harvard Medical School, n.d.[27]). In total, the CIDI consists of a screening module and 40 sections, 22 of which are diagnostic sections to assess mood (two sections), anxiety (seven sections), substance abuse (two sections), childhood (four sections) and other disorders (seven sections). The remaining sections assess functioning and physical comorbidity, risk factors, socio-demographic information and the treatment of mental disorders. The screening module, which includes a series of introductory questions about the respondent’s general health before delving into the diagnostic stem questions, has been shown to increase the accuracy of diagnostic assessments by reducing the effects of respondent fatigue and unwillingness to disclose on stem question endorsement (Harvard Medical School, n.d.[27]).
Symptoms of mental ill-health: Screening tools
The public health tools presented in this section focus mainly on royalty-free instruments, since fees and copyright restrictions might present a barrier to use.
Mental Health Inventory (MHI-5): The Mental Health Inventory-5 (MHI-5) is a five-item scale to screen for symptoms of psychological distress. It is drawn from the 38-item Mental Health Inventory (MHI) and included in the 20-item and 36-item versions of the Short Form Health Survey (SF-20 and SF-36) (Berwick et al., 1991[28]; Kelly et al., 2008[29]). The questions tap into both negative and positive affect, with three items focusing on low/depressed mood and two on nervousness/anxiety (although the tool itself is not used to present these aspects separately). The MHI-5 has been found to be a reliable measure of mental health status and has been validated against both depressive and, to a lesser degree, also anxiety disorders (including generalised anxiety and panic disorder) in general population and patient samples in a range of countries (Yamazaki, Fukuhara and Green, 2005[30]; Hoeymans et al., 2004[31]; Elovanio et al., 2020[32]; Gill et al., 2007[33]; Rumpf et al., 2001[34]; Strand et al., 2003[35]; Thorsen et al., 2013[36]). There is some evidence that removing the two anxiety-related items does not reduce the effectiveness of the MHI in detecting depression, although this has not been examined in studies in which a formal diagnosis according to clinical criteria was used as a gold standard (Yamazaki, Fukuhara and Green, 2005[30]).
Table 2.12. MHI-5 Questionnaire with scoring breakdown
|
All of the time |
Most of the time |
A good bit of the time |
Some of the time |
A little of the time |
None of the time |
|
|---|---|---|---|---|---|---|
|
During the past month, how much of the time: |
||||||
|
1. Have you been a happy person? (reverse coded) |
1 |
2 |
3 |
4 |
5 |
6 |
|
2. Have you felt calm and peaceful? (reverse coded) |
1 |
2 |
3 |
4 |
5 |
6 |
|
3. Have you been a very nervous person? |
1 |
2 |
3 |
4 |
5 |
6 |
|
4. Have you felt downhearted and blue? |
1 |
2 |
3 |
4 |
5 |
6 |
|
5. Have you felt so down in the dumps that nothing could cheer you up? |
1 |
2 |
3 |
4 |
5 |
6 |
Note: All items are added together to provide a total score from 5 to 30, which is then transformed into a variable ranging from 0-100 using a standard linear transformation. Higher values indicate better mental health, with the following cut-off points for various degrees of psychological distress: 68 or less mild, moderate or severe, 60 or less moderate or severe, 52 or less severe.
Source: Kelly, M.J. et al. (2008[29]), “Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: A comparison of five different methods”, BMC Psychiatry Vol. 8/10, https://doi.org/10.1186/1471-244X-8-10.
The Short-Form Health Survey (SF-12): The Short-Form Health Survey (SF-12) is a tool to measure health-related quality of life. It was developed as a shorter alternative to the SF-36 questionnaire to be used in the general population and in large surveys and contains up to two items for each of the SF-36’s eight dimensions: general mental health, energy and fatigue, bodily pain, general health perceptions, limitations on physical activity due to health, limitations on social activity due to physical or emotional conditions, limitations on day-to-day activities due to physical health, and limitations on day-to-day activities due to emotional health (Ware et al., 2002[37]). A number of questions in both the SF-12 and SF-36 are taken directly from the Mental Health Inventory (MHI), which also features the MHI-5 free-standing scale in its own right (see above) (RAND, n.d.[38]). Two summary scores, the Physical Component Summary (PCS) and the Mental Component Summary (MCS), can be derived from the SF-12, and a range of scoring methods have been validated against both active and recent depressive disorders and to a lesser degree also anxiety disorders in general population samples (Ware et al., 2002[37]; Gill et al., 2007[33]; Vilagut et al., 2013[39]). Some evidence suggests that the association between the SF-12’s physical health dimensions might be more strongly related with mental health in low-income settings, with implications for context-specific weights (Ohrnberger et al., 2020[40]). The SF-12 is subject to copyright restrictions and can thus not be republished in this report (Quality Metric, n.d.[41]).
Kessler Scale (K10/ K6): The Kessler psychological distress scale, which is most often used in its 10-item (K10) and 6-item (K6) form, is a screening tool for identifying adults with significant levels of psychological distress. The questions focus on somatic symptoms and negative affect, particularly on both low-depressed mood and nervousness/anxiety. While these aspects are usually not presented separately and a total score for distress is usually used, factor analysis has established depression and anxiety as distinct clusters in the K10 (Brooks, Beard and Steel, 2006[42]). Indeed, although it is often applied in primary clinical settings as well, it was designed for use in the general population, and sensitivity and specificity analysis support both K6 and K10 as screening instruments to identify likely community cases of anxiety and depression (Slade, Grove and Burgess, 2011[43]). Furthermore, they have been extensively validated, including in cross-cultural settings, against diagnostic interview evaluations of anxiety and affective disorders, with lesser but significant associations with other mental disorder categories and with the presence of any current mental disorder (Andrews and Slade, 2001[44]). There is also some evidence that the Kessler scales can be used successfully (with lower cut-off scoring criteria) to capture individuals struggling with more moderate psychological distress that nonetheless warrants mental health intervention (Prochaska et al., 2012[45]).
Table 2.13. Kessler Scale 10/6 Questionnaire with scoring breakdown
|
None of the time |
A little of the time |
Some of the time |
Most of the time |
All of the time |
|
|---|---|---|---|---|---|
|
During the last 30 days, about how often did you feel: |
|||||
|
1. Tired out for no good reason? |
1 |
2 |
3 |
4 |
5 |
|
2. Nervous? |
1 |
2 |
3 |
4 |
5 |
|
3. So nervous that nothing could calm you down? |
1 |
2 |
3 |
4 |
5 |
|
4. Hopeless? |
1 |
2 |
3 |
4 |
5 |
|
5. Restless or fidgety? |
1 |
2 |
3 |
4 |
5 |
|
6. So restless you could not sit still? |
1 |
2 |
3 |
4 |
5 |
|
7. Depressed? |
1 |
2 |
3 |
4 |
5 |
|
8. That everything was an effort? |
1 |
2 |
3 |
4 |
5 |
|
9. So sad that nothing could cheer you up? |
1 |
2 |
3 |
4 |
5 |
|
10. Worthless? |
1 |
2 |
3 |
4 |
5 |
Note: All items are added together to provide a total score, where higher values indicate worse mental health. However, different scoring methods for both K10 and K6 scales have been used depending on the country and institutional context. For instance, in the United States, answers are coded from 0-4 (leading to a maximum possible score of 40 for the K10 and 24 for the K6), whereas in Australia, 1-5 as shown in the table above have been used (leading to a maximum possible score of 50 for the K10 and 30 for the K6). The K10 scoring used in Australian health surveys have typically been as follows: 10-5 low, 16-21 moderate, 22-29 high, 30-50 very high psychological distress. For the K6 scoring, respondents with scores of 13 (in the 0-4 coding)/ 19 (in the 1-5 coding) or higher are typically classified as having a probable serious mental illness. Cut-off scores in other contexts might vary.
Source: ABS (2007[46]), Information Paper: Use of the Kessler Psychological Distress Scale in ABS Health Surveys, Australian Bureau of Statistics, https://www.abs.gov.au/ausstats/abs@.nsf/lookup/4817.0.55.001chapter92007-08; Kessler, R. et al. (2010[47]), “Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO World Mental Health (WMH) survey initiative”, International Journal of Methods in Psychiatric Research, Vol. 19/S1, pp. 4-22, https://doi.org/10.1002/mpr.310.
General Health Questionnaire (GHQ-12): The 12-item General Health Questionnaire (GHQ-12) is a measure to detect psychological distress by focusing on affect (negative and positive), somatic symptoms and the functional impairment of respondents. The GHQ-12 has been translated into many languages and extensively validated in general and clinical populations worldwide (particularly against depression and anxiety disorders), including among adolescent samples (Hankins, 2008[48]; Gilbody, 2001[49]; Baksheev et al., 2011[50]). Originally intended as a unidimensional measure, there is some debate about the dimensionality of the GHQ-12, with many factor-analytical studies supporting a range of multidimensional structures (e.g. anxiety and depression, social dysfunction, loss of confidence) (Gao et al., 2004[51]). However, more recent evidence points to these results likely being an expression of method-specific variance caused by item wording, supporting the notion that treating the scale as a unitary construct would minimise bias (Hystad and Johnsen, 2020[52]). The GHQ-12 is subject to copyright restrictions and can thus not be republished in this report.
Patient Health Questionnaire (PHQ-9/ PHQ-8): The full Patient Health Questionnaire (PHQ) contains 59 questions, with modules focusing on mood, anxiety, alcohol, eating and somatoform disorders. The PHQ-9 is a nine-question survey designed to detect the presence and severity of depressive symptoms, and it directly maps onto the DSM-IV and DSM-5 symptom criteria for major depressive disorder. The PHQ-8 questionnaire removes the final question regarding suicidal ideation. While a one-factor structure for both the PHQ-8/9 has been identified, more recent studies support a two-factor model composed of affective and somatic factors (Sunderland et al., 2019[53]). Both instruments have shown acceptable diagnostic screening properties across various population and clinical settings, age groups, and cultures/ ethnicities, in addition to being also a reliable and valid measure of depression severity (Manea, Gilbody and McMillan, 2012[54]; Moriarty et al., 2015[55]; Kroenke et al., 2009[56]; Huang et al., 2006[57]; Kroenke, Spitzer and Williams, 2001[58]; Richardson et al., 2010[59]). The close alignment between the PHQ-8/9 and the DSM make it subject to the same criticism, including a potentially Western-focused construct of depression, relative to longer self-reported scales with less constrained symptom sets (Zimmerman et al., 2012[60]; Haroz et al., 2017[61]).
Table 2.14. PHQ-9/8 questionnaire with scoring breakdown
|
Not at all |
Several days |
More than half the days |
Nearly every day |
|
|---|---|---|---|---|
|
Over the last two weeks, how often have you been bothered by any of the following problems: |
||||
|
1. Little interest or pleasure in doing things |
0 |
1 |
2 |
3 |
|
2. Feeling down, depressed or hopeless |
0 |
1 |
2 |
3 |
|
3. Trouble falling or staying asleep, or sleeping too much |
0 |
1 |
2 |
|
|
4. Feeling tired or having little energy |
0 |
1 |
2 |
3 |
|
5. Poor appetite or overeating |
0 |
1 |
2 |
3 |
|
6. Feeling bad about yourself – or that you are a failure or have let yourself or your family down |
0 |
1 |
2 |
3 |
|
7. Trouble concentrating on things, such as reading the newspaper or watching television |
0 |
1 |
2 |
3 |
|
8. Moving or speaking so slowly that other people could have noticed. Or the opposite – being so fidgety or restless that you have been moving around a lot more than usual |
0 |
1 |
2 |
3 |
|
9. Thoughts that you would be better off dead or of hurting yourself in some way |
0 |
1 |
2 |
3 |
Note: The last item in italics is the question on suicidal ideation that is added for the PHQ-9. Scoring can be done in two ways: (1) via an “algorithm diagnosis” of either major depression or other depression; or (2) via summing all items and applying different cut-off scores for depression severity. In the algorithm diagnosis that adheres to DSM definitions, the first or second item (depressed mood or anhedonia) have to present at least “more than half the days” and, combined with at least 5 of the total symptoms or 2 to 4 symptoms also present at this frequency, constitutes major depression or other depression, respectively. In the second form of categorisation, all items are added together to provide a total score of depression severity, with scores ranging from 0-24 for the PHQ-8 and 0-27 for the PHQ-9: 0-4 none, 5-9 mild depression, 10-14 moderate depression, 15-19 moderately severe depression, 20-24/27 severe depression. A score of ≥10 indeed typically represents clinically significant depression regardless of diagnostic status.
Source: Kroenke, K. et al. (2009[56]), “The PHQ-8 as a measure of current depression in the general population”, Journal of Affective Disorders, Vol. 114/1-3, pp. 163-173, https://doi.org/10.1016/j.jad.2008.06.026; Kroenke, K. et al. (2001[58]), “The PHQ-9: Validity of a brief depression severity measure”, Journal of General Internal Medicine, Vol. 16/9, pp. 606-613, http://dx.doi.org/10.1046/j.1525-1497.2001.016009606.x.
The Generalised Anxiety Disorder Questionnaire (GAD-7/GAD-2): The Generalised Anxiety Disorder Questionnaire (GAD-7) comprises seven questions about the frequency of broad anxiety-related problems in the past two weeks. It was developed for screening and severity assessment of Generalised Anxiety Disorder, and the items cover most but not all (symptoms of this disorder listed in the DSM-IV and 5 (excessive worry, difficulty to control the worry, restlessness and irritability but not e.g. fatigue, muscle tension, sleep disturbance). Research supports a unidimensional structure for the scale (Sunderland et al., 2019[53]). The GAD-7 has demonstrated good internal consistency, convergent validity, and sensitivity to change in both patient and population samples (Löwe et al., 2008[62]; Beard and Björgvinsson, 2014[63]). While the scale has been successfully translated into multiple languages and local dialects, more research on potential cross-cultural bias of the tool needs to be conducted (Parkerson et al., 2015[64]; Sunderland et al., 2019[53]). The scale focuses on general symptoms of anxiety and was not developed to assess the presence of other anxiety disorders, such as Social Anxiety Disorder. However, some researchers have argued that it can be used across different anxiety disorders, given the scale’s emphasis on the transdiagnostic process of worry and the fact that Generalised Anxiety Disorder has a high degree of comorbidity (Johnson et al., 2019[65]). The GAD-2 shorter version of this scale focuses only on the first two items (worry and difficulty to control the worry), i.e. the core criteria of generalised anxiety per the DSM. Available evidence has indicated support for its psychometric properties and validity in a range of settings (Byrd-Bredbenner, Eck and Quick, 2021[66]; Hughes et al., 2018[67]; Luo et al., 2019[68]; Ahn, Kim and Choi, 2019[69]).
Table 2.15. GAD-7/GAD-2 Questionnaire with scoring breakdown
|
Not at all |
Several days |
More than half the days |
Nearly every day |
|
|---|---|---|---|---|
|
Over the last two weeks, how often have you been bothered by any of the following problems: |
||||
|
1. Feeling nervous, anxious or on edge |
0 |
1 |
2 |
3 |
|
2. Not being able to stop or control worrying |
0 |
1 |
2 |
3 |
|
3. Worrying too much about different things |
0 |
1 |
2 |
3 |
|
4. Trouble relaxing |
0 |
1 |
2 |
3 |
|
5. Being so restless that it is hard to sit still |
0 |
1 |
2 |
3 |
|
6. Becoming easily annoyed or irritable |
0 |
1 |
2 |
3 |
|
7. Feeling afraid as if something awful might happen |
0 |
1 |
2 |
3 |
Note: Items in italics represent the 2-item shorter version of the scale (GAD-2). All items are added together to provide a total score ranging from 0-21 for the GAD-7, with higher scores indicating the presence of more anxiety symptomatology: 0-4 none, 5-9 mild anxiety, 10-14 moderate anxiety, 15-21 severe anxiety. For the GAD-2, a score of 3 points is the suggested cut-off for identifying possible cases for which further diagnostic evaluation for generalised anxiety disorder is warranted.
Source: Spitzer, R. et al. (2006[70]), “A brief measure for assessing generalized anxiety disorder: The GAD-7”, Archives of Internal Medicine, Vol. 166/10, pp. 1092-1097, http://dx.doi.org/10.1001/ARCHINTE.166.10.1092.
Patient Health Questionnaire (PHQ-4): The PHQ-4 screening tool is a short, four-question tool to identify the presence and severity of core symptoms of both depression and anxiety, given that these are two of the most prevalent illnesses among the general population and often comorbid. The PHQ-4 pulls the two core depression-related questions from the PHQ-9/8 (which together are called the PHQ-2) plus two core anxiety-related questions from GAD-7 (which are called the GAD-2). Thus, the PHQ-4 is a combination of the PHQ-2 and GAD-2, which have independently been shown to be good, brief screening tools with construct and criterion validity (see above). Available evidence supports the PHQ-4’s psychometric properties, reliability and validity in studies focused on the general population, intervention, and workers and college students (Stanhope, 2016[71]; Khubchandani et al., 2016[72]; Löwe et al., 2010[73]).
Table 2.16. PHQ-4 Questionnaire with scoring breakdown
|
Not at all |
Several days |
More than half the days |
Nearly every day |
|
|---|---|---|---|---|
|
Over the last two weeks, how often have you been bothered by any of the following problems: |
||||
|
1. Feeling nervous, anxious or on edge |
0 |
1 |
2 |
3 |
|
2. Not being able to stop or control worrying |
0 |
1 |
2 |
3 |
|
3. Feeling down, depressed or hopeless |
0 |
1 |
2 |
3 |
|
4. Little interest or pleasure in doing things |
0 |
1 |
2 |
3 |
Note: All items are added together to provide a total score of psychological distress ranging from 0-12, with higher scores indicating the presence of more symptomatology: 0-2 normal, 3-5 mild, 6-8 moderate, 9-12 severe. A total score greater than or equal to 3 for the first two items (GAD-2) indicates that the respondent is at risk for anxiety. A total score greater than or equal to 3 for the final two items (PHQ-2) indicates that the respondent is at risk for depression.
Source: Kroenke, K. et al. (2009[74]), “An ultra-brief screening scale for anxiety and depression: The PHQ-4”, Psychosomatics, Vol. 50/6, pp. 613-621, http://dx.doi.org/10.1176/APPI.PSY.50.6.613.
Washington Group on Disability Statistics Short Set on Functioning – Enhanced (WG-SS): The Washington Group Short Set on Functioning – Enhanced (WG-SS Enhanced) was developed by the Washington Group on Disability Statistics, which is composed of representatives from National Statistics Offices, as well as UN agencies, international non-governmental organisations and organisations for people who are disabled, to capture not only the presence but also the type and severity of a respondent’s disability for use in population and special interest surveys (Washington Group on Disability Statistics, 2020[75]). Its focus is on functioning in the areas of seeing, hearing, walking or climbing stairs, remembering or concentrating, self-care, communication, upper body activities, as well as affect. The four questions on the latter focus on symptoms of depression and anxiety, though the questionnaire is not typically used in its subcomponent parts. Regardless, the focus on overall functioning might carry important ways forward for capturing transdiagnostic symptoms of mental ill-health.
Table 2.17. WG-SS Enhanced Questionnaire
|
No difficulty |
Some difficulty |
A lot of difficulty |
Cannot do at all |
||
|---|---|---|---|---|---|
|
Do you have difficulty: |
|||||
|
1. Seeing, even when wearing your glasses? |
|||||
|
2. Hearing, even when using a hearing aid(s)? |
|||||
|
3. Walking or climbing steps? |
|||||
|
4. Using your usual language, communicating, for example understanding or being understood? |
|||||
|
5. Remembering or concentrating? |
|||||
|
6. With self-care, such as washing all over or dressing? |
|||||
|
7. Raising a 2-liter bottle of water or soda from waist to eye level? |
|||||
|
8. Using your hands and fingers, such as picking up small objects, for example, a button or pencil, or opening or closing containers or bottles? |
|||||
|
Daily |
Weekly |
Monthly |
A few times a year |
Never |
|
|
9.How often do you feel worried, nervous or anxious? |
|||||
|
A little |
A lot |
Somewhere in between a little and a lot |
|||
|
10. Thinking about the last time you felt worried, nervous or anxious, how would you describe the level of these feelings? |
|||||
|
Daily |
Weekly |
Monthly |
A few times a year |
Never |
|
|
11. How often do you feel depressed? |
|||||
|
A little |
A lot |
Somewhere in between a little and a lot |
|||
|
12. Thinking about the last time you felt depressed, how depressed did you feel? |
Note: Different domain-specific identifiers of functioning (and the severity of its impairment) can be calculated for an overall disability identifier. The recommended level of inclusion is: “a lot of difficulty” or “cannot do at all” for at least one of the first six questions, severity levels 3 or 4 for the two upper-body mobility questions, and severity level 4 for the anxiety or depression indicators. Items in italics represent the 6-item shorter version of the scale (Washington Group on Disability Statistics Short Set on Functioning), which excludes questions on mental health and upper body functioning.
Source: Washington Group on Disability Statistics (2020[75]), The Washington Group Short Set on Functioning: Enhanced (WG-SS Enhanced), The Washington Group Data Collection Tools and their Recommended Use (washingtongroup-disability.com).
Alcohol Use Disorders Identification Test/Concise (AUDIT/ AUDIT-C): The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item alcohol screen developed by the WHO from the 1980s onwards that can help identify respondents or patients who are hazardous drinkers or have active alcohol use disorders (including alcohol abuse or dependence). Its validity has been demonstrated in settings beyond primary care, such as inpatient hospital wards, emergency departments, universities, workplaces, outpatient settings and psychiatric services (Berner et al., 2007[76]). Its short version of 3 items, designed to be integrated into routine patient interviews, has been found to have similar accuracy to the full-scale version and has been validated primarily in primary-care settings, as well as increasingly in more general population samples, including adults seeking online help with drinking (Bush et al., 1998[77]; Khadjesari et al., 2017[78]).
Table 2.18. AUDIT/ AUDIT-C Questionnaire with scoring breakdown
|
Never |
Monthly or less |
2-4 times a month |
2-3 times a week |
4 or more times a week |
|
|---|---|---|---|---|---|
|
1. How often do you have a drink containing alcohol? |
0 |
1 |
2 |
3 |
4 |
|
1 or 2 |
3 to 4 |
5 to 6 |
7 to 9 |
10 or more |
|
|
2. How many standard drinks containing alcohol do you have on a typical day? |
0 |
1 |
2 |
3 |
4 |
|
Never |
Less than monthly |
Monthly |
Weekly |
Daily or almost daily |
|
|
3. How often do you have six or more drinks on one occasion? |
0 |
1 |
2 |
3 |
4 |
|
4. How often during the last year have you found that you were not able to stop drinking once you had started? |
0 |
1 |
2 |
3 |
4 |
|
5. How often during the last year have you failed to do what was normally expected from you because of drinking? |
0 |
1 |
2 |
3 |
4 |
|
6. How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session? |
0 |
1 |
2 |
3 |
4 |
|
7. How often during the last year have you had a feeling of guilt or remorse after drinking? |
0 |
1 |
2 |
3 |
4 |
|
8. How often during the last year have you been unable to remember what happened the night before because you had been drinking? |
0 |
1 |
2 |
3 |
4 |
|
No |
Yes, but not in the last year |
Yes, during the last year |
|||
|
9. Have you or someone else been injured as a result of your drinking? |
0 |
2 |
4 |
||
|
10. Has a relative or friend or a doctor or another health worker been concerned about your drinking or suggested you cut down? |
0 |
2 |
4 |
Note: Items in italics represent the 3-item shorter version of the scale (AUDIT-C). All items are added together to provide a total score ranging from 0-40 (0-12 for the AUDIT-C), with higher scores indicating higher likelihood that a person’s drinking is affecting his or her safety. For the AUDIT, scores of 8 or more are recommended as indicators of hazardous and harmful alcohol use, as well as possible alcohol dependence. Since the effects of alcohol vary with average body weight and differences in metabolism, establishing the cut-off point for all women and men over age 65 one point lower at a score of 7 will increase sensitivity for these population groups. For the AUDIT-C, in men (women), a score of 4 (3) or more is considered as identifying symptoms of hazardous drinking or active alcohol use disorders.
Source: Bush, K. et al. (1998[77]), “The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking”, Archives of Internal Medicine, Vol. 158/16, https://doi.org/10.1001/archinte.158.16.1789; WHO (2001[79]), AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care, World Health Organization, https://www.who.int/publications/i/item/audit-the-alcohol-use-disorders-identification-test-guidelines-for-use-in-primary-health-care.
Positive mental health
Core questions from the OECD Guidelines on Measuring Subjective Well-being: The OECD Guidelines on Subjective Well-being propose a minimal set of measures of subjective well-being covering both life evaluation and (short-term) affect that could be included in household surveys (OECD, 2013[80]). The core measures included are the ones which have the strongest evidence when it comes to validity and relevance, and for which international comparability is the most important. An experimental measure of an aspect of eudaimonic well-being is also included.
Table 2.19. OECD core questions on subjective well-being
|
0-10 |
|
|---|---|
|
The following question asks how satisfied you feel, on a scale from 0 to 10. Zero means you feel “not at all satisfied” and 10 means you feel “completely satisfied”. |
|
|
1. Overall, how satisfied are you with life as a whole these days? |
|
|
The following question asks how worthwhile you feel the things you do in your life are, on a scale from 0 to 10. Zero means you feel the things you do in your life are “not at all worthwhile”, and 10 means “completely worthwhile”. |
|
|
2. Overall, to what extent do you feel the things you do in your life are worthwhile? |
|
|
The following questions ask about how you felt yesterday on a scale from 0 to 10. Zero means you did not experience the feeling “at all” yesterday while 10 means you experienced the feeling “all of the time” yesterday. I will now read out a list of ways you might have felt yesterday. |
|
|
3. How about happy? |
|
|
4. How about worried? |
|
|
5. How about depressed? |
Note: The three questions on affect (3-5) should be included as a group and are intended to provide a minimal set of questions required to characterise the affective state of the respondent on the previous day.
Source: OECD (2013[80]), OECD Guidelines on Measuring Subjective Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9789264191655-en.
WHO-5 Well-being index (WHO-5): The World Health Organization Well-Being Index (WHO-5) is a short questionnaire of 5 items that focus on a respondent’s positive affect. The questionnaire, adapted from the longer WHO/ICD-10 Depression Diagnosis and DSM-IV Depression scale by selecting a subset of positively phrased items, has first been used in a project on well-being measures in primary health care by the WHO Regional Office in Europe in 1998 and since then has been translated into more than 30 languages (World Health Organization, 1998[81]; Topp et al., 2015[7]). The WHO-5 has been applied as a generic scale for well-being across a wide range of study fields and countries, as a sensitive screening tool for depression as well as an outcome measure in clinical trials (Topp et al., 2015[7]). Studies of younger and elderly persons indicated a unidimensional structure for this scale (Topp et al., 2015[7]).
Table 2.20. WHO-5 questionnaire with scoring breakdown
|
All of the time |
Most of the time |
More than half the time |
Less than half the time |
Some of the time |
At no time |
|
|---|---|---|---|---|---|---|
|
Over the past two weeks… |
||||||
|
1. I have felt cheerful and in good spirits |
5 |
4 |
3 |
2 |
1 |
0 |
|
2. I have felt calm and relaxed |
5 |
4 |
3 |
2 |
1 |
0 |
|
3. I have felt active and vigorous |
5 |
4 |
3 |
2 |
1 |
0 |
|
4. I woke up feeling fresh and rested |
5 |
4 |
3 |
2 |
1 |
0 |
|
5. My daily life has been filled with things that interest me |
5 |
4 |
3 |
2 |
1 |
0 |
Note: All items are added together to provide a total score from 0 to 25, which is then multiplied by 4 to normalise to a 0 (worst possible well-being) to 100 (best possible well-being) score. A cut-off score of less than or equal to 50, or less than or equal to 52 (Sándor et al., 2021[82]),is often used as indicative of reduced well-being, which has been validated in studies using the WHO-5 for the screening of depression and for predicting patient mortality.
Source: Topp, C. et al. (2015[7]), “The WHO-5 well-being index: A systematic review of the literature”, Psychotherapy and Psychosomatics, Vol. 84/3, pp. 167-176, https://doi.org/10.1159/000376585.
SF-36 Energy/Vitality subscale: The 4-item vitality subscale of the larger SF-36 measure (see above) is a general measure of energy/fatigue. It has been validated in clinical settings and performed well compared to longer scales (e.g. for cancer-related fatigue) (Brown et al., 2011[83]).
Table 2.21. SF-36 vitality subscale questionnaire with scoring breakdown
|
All of the time |
Most of the time |
A good bit of the time |
Some of the time |
A little of the time |
None of the time |
|
|---|---|---|---|---|---|---|
|
How much of the time during the past 4 weeks… |
||||||
|
1. Did you feel full of pep? |
1 |
2 |
3 |
4 |
5 |
6 |
|
2. Did you have a lot of energy? |
1 |
2 |
3 |
4 |
5 |
6 |
|
3. Did you feel worn out? |
1 |
2 |
3 |
4 |
5 |
6 |
|
4. Did you feel tired? |
1 |
2 |
3 |
4 |
5 |
6 |
Note: Standardised scores range from 0-100, with lower scores indicating greater fatigue. Scores ≤45 have been established as representing clinically significant fatigue.
Source: Ware, J. et al. (1993[84]), SF-36 Health Survey: Manual and Interpretation Guide, The Health Institute, New England Medical Center Hospitals, https://www.researchgate.net/profile/John-Ware-6/publication/313050850_SF-36_Health_Survey_Manual_Interpretation_Guide/links/594a5b83aca2723195de5c3d/SF-36-Health-Survey-Manual-Interpretation-Guide.pdf (accessed on 22 January 2023); Donovan, K. et al. (2008[85]), “Identifying clinically meaningful fatigue with the Fatigue Symptom Inventory”, Journal of Pain and Symptom Management, Vol. 36/5, pp. 480-487, https://doi.org/10.1016/j.jpainsymman.2007.11.013.
Satisfaction with Life Scale (SWLS): The Satisfaction with Life Scale was developed to assess people’s satisfaction and evaluation of their lives as a whole, rather than focusing on specific life domains. Early studies have found it to show good convergent validity with other types of subjective well-being, while being distinct from affective well-being measures (Pavot et al., 1991[86]; Pavot and Diener, 1993[87]).
Table 2.22. SWLS questionnaire with scoring breakdown
|
Strongly agree |
Agree |
Slightly agree |
Neither agree nor disagree |
Slightly disagree |
Disagree |
Strongly disagree |
|
|---|---|---|---|---|---|---|---|
|
1. In most ways my life is close to my ideal. |
7 |
6 |
5 |
4 |
3 |
2 |
1 |
|
2. The conditions of my life are excellent. |
7 |
6 |
5 |
4 |
3 |
2 |
1 |
|
3. I am satisfied with my life. |
7 |
6 |
5 |
4 |
3 |
2 |
1 |
|
4. So far I have gotten the most important things I want in life. |
7 |
6 |
5 |
4 |
3 |
2 |
1 |
|
5. If I could live my life over, I would change almost nothing. |
7 |
6 |
5 |
4 |
3 |
2 |
1 |
Note: All items are added together to provide a total score from 5 to 35, where higher values indicate higher life satisfaction: 5-9 extremely dissatisfied, 10-14 dissatisfied, 15-19 slightly dissatisfied, 20-24 slightly satisfied, 25-29 satisfied, 30-35 extremely satisfied.
Source: Diener, E. et al. (1985[88]), “The Satisfaction with Life Scale”, Journal of Personality Assessment, Vol. 49/1, pp. 71-75, https://doi.org/10.1207/s15327752jpa4901_13.
The Mental Health Continuum Short-Form (MHC-SF): The MHC-SF is a 14-item scale developed by Keyes to capture positive mental health in his dual-continuum model (Keyes, 2002[89]). It was derived from the 40-item Mental Health Continuum Long Form (MHC-LF), and consists of separate subscales: three “emotional well-being” items (reflecting affective well-being plus life satisfaction), five “social well-being” items, and six “psychological well-being” items (which when combined reflect eudaimonic well-being) (Lamers et al., 2011[90]). Studies have shown high internal and moderate test-retest reliability for the MHC-SF and confirmed the 3-factor structure of the subscales, which also show convergent validity with corresponding aspects of well-being and functioning (Lamers et al., 2011[90]).
Table 2.23. MHC-SF questionnaire with scoring breakdown
|
Never |
Once or twice |
About once a week |
Two or three times a week |
Almost every day |
Every day |
|
|---|---|---|---|---|---|---|
|
How often in the past month did you feel … |
||||||
|
Emotional well-being (affect) |
||||||
|
1. Happy? |
0 |
1 |
2 |
3 |
4 |
5 |
|
2. Interested in life? |
0 |
1 |
2 |
3 |
4 |
5 |
|
3. Satisfied with your life? |
0 |
1 |
2 |
3 |
4 |
5 |
|
Social well-being (eudaimonic) |
||||||
|
4. That you had something important to contribute to society? (social contribution) |
0 |
1 |
2 |
3 |
4 |
5 |
|
5. That you belonged to a community (like a social group, your neighbourhood, your city, your school)? (social integration) |
0 |
1 |
2 |
3 |
4 |
5 |
|
6. That our society is becoming a better place for people like you? (social growth) |
0 |
1 |
2 |
3 |
4 |
5 |
|
7. That people are basically good? (social acceptance) |
0 |
1 |
2 |
3 |
4 |
5 |
|
8. That the way our society works makes sense to you? (social coherence) |
0 |
1 |
2 |
3 |
4 |
5 |
|
Psychological well-being (eudaimonic) |
||||||
|
9. That you liked most parts of your personality? (self-acceptance) |
0 |
1 |
2 |
3 |
4 |
5 |
|
10. Good at managing the responsibilities of your daily life? (environmental mastery) |
0 |
1 |
2 |
3 |
4 |
5 |
|
11. That you had warm and trusting relationships with others? (positive relationship with others) |
0 |
1 |
2 |
3 |
4 |
5 |
|
12. That you had experiences that challenged you to grow and become a better person? (personal growth) |
0 |
1 |
2 |
3 |
4 |
5 |
|
13. Confident to think or express your own ideas and opinions? (autonomy) |
0 |
1 |
2 |
3 |
4 |
5 |
|
14. That your life has a sense of direction or meaning to it? (purpose in life) |
0 |
1 |
2 |
3 |
4 |
5 |
Note: All items are summed, yielding a total score ranging from 0 to 70, with higher scores indicating greater levels of positive mental health. Subscale scores range from 0 to 15 for emotional well-being, from 0 to 25 for social well-being and from 0 to 30 for psychological well-being. “Flourishing” is defined by reporting ≥ 1 of 3 emotional signs and ≥ 6 of 11 eudaimonic signs (social and psychological subscales combined) experienced “every day” or “almost every day”. “Languishing” is defined by reporting ≥ 1 of 3 emotional signs and ≥ 6 of 11 eudaimonic signs experienced “never” or “once or twice”. Individuals who are neither flourishing nor languishing are categorised as “moderately mentally healthy”.
Source: Lamers, S. et al., (2011[90]), “Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF)”, Journal of Clinical Psychology, Vol. 67/1, pp. 99-110, https://doi.org/10.1002/jclp.2074.
The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): The 14-item WEMWBS scale was developed with funding from NHS Health Scotland in 2005 to measure mental well-being (conceived of as “both feeling good and functioning well”), taking the Affectometer 2 instrument as the starting point (Warwick Medical School, 2021[91]). Some studies confirmed a unidimensional structure for WEMWBS, while others identified three residual factors relating to affective well-being, psychological functioning or eudaimonia, and social relationships (Shannon et al., 2020[92]; Koushede et al., 2019[93]). A shorter, 7-item version of the scale, SWEMWBS, is also available, focusing slightly less on affect (Stewart-Brown et al., 2009[94]). (S)WEMWBS has been validated in various populations and among different subgroups, including adolescents, clinical samples and ethnic minority samples, and has been translated into more than 25 languages and validated in Norwegian, Swedish, Italian, Dutch, Danish, German, French and Spanish. Both scales have been shown to be sensitive to changes that occur in mental well-being promotion and mental illness treatment and prevention projects (Koushede et al., 2019[93]). Both instruments can distinguish mental well-being between subgroups, but SWEMBS has been found to be less sensitive than the longer version to gender differences (Koushede et al., 2019[93]; Ng Fat et al., 2017[95]).
Table 2.24. (S)WEMWBS questionnaire with scoring breakdown
|
None of the time |
Rarely |
Some of the time |
Often |
All of the time |
|
|---|---|---|---|---|---|
|
Over the last two weeks… |
|||||
|
1. I’ve been feeling optimistic about the future |
1 |
2 |
3 |
4 |
5 |
|
2. I’ve been feeling useful |
1 |
2 |
3 |
4 |
5 |
|
3. I’ve been feeling relaxed |
1 |
2 |
3 |
4 |
5 |
|
4. I’ve been feeling interested in other people |
1 |
2 |
3 |
4 |
5 |
|
5. I’ve had energy to spare |
1 |
2 |
3 |
4 |
5 |
|
6. I’ve been dealing with problems well |
1 |
2 |
3 |
4 |
5 |
|
7. I’ve been thinking clearly |
1 |
2 |
3 |
4 |
5 |
|
8. I’ve been feeling good about myself |
1 |
2 |
3 |
4 |
5 |
|
9 I’ve been feeling close to other people |
1 |
2 |
3 |
4 |
5 |
|
10. I’ve been feeling confident |
1 |
2 |
3 |
4 |
5 |
|
11 I’ve been able to make up my own mind about things |
1 |
2 |
3 |
4 |
5 |
|
12 I’ve been feeling loved |
1 |
2 |
3 |
4 |
5 |
|
13 I’ve been interested in new things |
1 |
2 |
3 |
4 |
5 |
|
14 I’ve been feeling cheerful |
1 |
2 |
3 |
4 |
5 |
Note: Items in italics represent the 7-item shorter version of the scale (SWEMWBS). For the 14-item scale, all items are summed, yielding a total score ranging from 14-70. For the 7-item scale, raw scores are transformed into a 7-35 metric score (see conversion table here: https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/using/howto/swemwbs_raw_score_to_metric_score_conversion_table.pdf). For both scales, higher scores indicate greater levels of positive mental health. (S)WEMWBS scores approximate to a normal distribution, permitting parametric analysis. For categorical scoring, cut-off points for high, average and low mental well-being can be generated using two approaches: (1) a statistical approach putting the cut-off point at +/- one standard deviation, placing approximately 15% of the sample into high well-being and 15% into low well-being categories; or (2) a benchmarking approach against validated measures of depression, e.g. a score of 41-44 as indicative of possible/mild depression and a score of >41 as indicative of probable clinical depression, using the Center for Epidemiologic Studies Depression Scale (CES-D) as a benchmark. WEMWBS is protected by copyright. Those wishing to use WEMWBS can obtain a licence to do so. Please go to https://warwick.ac.uk/wemwbs/using for information on the type of licence you will require and details on how to apply. A free-of-charge “non-commercial” licence is available to public sector organisations, charities and registered social enterprises, as well as to researchers employed in Higher Education Institutions. Any further enquiries can be directed to wemwbs@warwick.ac.uk.
Source: Warwick-Edinburgh Mental Well-being Scale (WEMWBS) © NHS Health Scotland, University of
Warwick and University of Edinburgh, 2006, all rights reserved; Warwick Medical School (2021[91]), The Warwick-Edinburgh Mental Wellbeing Scales (WEMWBS), https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/.
References
[46] ABS (2007), Information Paper: Use of the Kessler Psychological Distress Scale in ABS Health Surveys, Australian Bureau of Statistics, https://www.abs.gov.au/ausstats/abs@.nsf/lookup/4817.0.55.001chapter92007-08.
[69] Ahn, J., Y. Kim and K. Choi (2019), “The psychometric properties and clinical utility of the Korean version of GAD-7 and GAD-2”, Frontiers in Psychiatry, Vol. 127/10, https://doi.org/10.3389/fpsyt.2019.00127.
[44] Andrews, G. and T. Slade (2001), “Interpreting scores on the Kessler Psychological Distress Scale (K10)”, Australian and New Zealand Journal of Public Health, Vol. 25/6, pp. 494-497, https://doi.org/10.1111/j.1467-842X.2001.tb00310.x.
[50] Baksheev, G. et al. (2011), “Validity of the 12-item General Health Questionnaire (GHQ-12) in detecting depressive and anxiety disorders among high school students”, Psychiatry Research, Vol. 187/1-2, pp. 291-296, https://doi.org/10.1016/j.psychres.2010.10.010.
[63] Beard, C. and T. Björgvinsson (2014), “Beyond generalized anxiety disorder: Psychometric properties of the GAD-7 in a heterogeneous psychiatric sample”, Journal of Anxiety Disorders, Vol. 28/6, pp. 547-552, https://doi.org/10.1016/j.janxdis.2014.06.002.
[76] Berner, M. et al. (2007), “The Alcohol Use Disorders Identification Test for Detecting At-Risk Drinking: A Systematic Review and Meta-Analysis”, Journal of Studies on Alcohol and Drugs, Vol. 68/3, pp. 461-473, https://doi.org/10.15288/jsad.2007.68.461.
[28] Berwick, D. et al. (1991), “Performance of a five-item mental health screening test”, Medical Care, Vol. 29/2, pp. 169-176, https://doi.org/10.1097/00005650-199102000-00008.
[42] Brooks, R., J. Beard and Z. Steel (2006), “Factor structure and interpretation of the K10”, Psychological Assessment, Vol. 18/1, pp. 62-70, https://doi.org/10.1037/1040-3590.18.1.62.
[83] Brown, L. et al. (2011), “Comparison of SF-36 vitality scale and Fatigue Symptom Inventory in assessing cancer-related fatigue”, Supportive Care in Cancer, Vol. 19/8, pp. 1255-1259, https://doi.org/10.1007/s00520-011-1148-2.
[4] Burger, H. and J. Neeleman (2007), “A glossary on psychiatric epidemiology”, Journal of Epidemiology and Community Health, Vol. 61/3, pp. 185-189, https://doi.org/10.1136/jech.2003.019430.
[77] Bush, K. et al. (1998), “The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking”, Archives of Internal Medicine, Vol. 158/16, https://doi.org/10.1001/archinte.158.16.1789.
[66] Byrd-Bredbenner, C., K. Eck and V. Quick (2021), “GAD-7, GAD-2, and GAD-mini: Psychometric properties and norms of university students in the United States”, General Hospital Psychiatry, Vol. 69, pp. 61-66, https://doi.org/10.1016/j.genhosppsych.2021.01.002.
[2] Case, A. and A. Deaton (2017), Mortality and Morbidity in the 21st Century, Brookings Papers on Economic Activity, http://brookings.edu/wp-content/uploads/2017/08/casetextsp17bpea.pdf.
[21] Chile, G. (2021), Saludable Mente [Healthy Mind], https://www.gob.cl/saludablemente/.
[88] Diener, E. et al. (1985), “The Satisfaction with Life Scale”, Journal of Personality Assessment, Vol. 49/1, pp. 71-75, https://doi.org/10.1207/s15327752jpa4901_13.
[9] Dobson, K. et al. (2020), “Trends in the prevalence of depression and anxiety disorders among Canadian working-age adults between 2000 and 2016”, Health Reports, Vol. 31/12, pp. 12-23, https://doi.org/10.25318/82-003-X202001200002-ENG.
[85] Donovan, K. et al. (2008), “Identifying clinically meaningful fatigue with the fatigue symptom inventory”, Journal of Pain and Symptom Management, Vol. 36/5, pp. 480-487, https://doi.org/10.1016/j.jpainsymman.2007.11.013.
[32] Elovanio, M. et al. (2020), “General Health Questionnaire (GHQ-12), Beck Depression Inventory (BDI-6), and Mental Health Index (MHI-5): Psychometric and predictive properties in a Finnish population-based sample”, Psychiatry Research, Vol. 289, p. 112973, https://doi.org/10.1016/j.psychres.2020.112973.
[51] Gao, F. et al. (2004), “Does the 12-item General Health Questionnaire contain multiple factors and do we need them?”, Health and Quality of Life Outcomes, Vol. 2/1, p. 63, https://doi.org/10.1186/1477-7525-2-63.
[49] Gilbody, S. (2001), “Routinely administered questionnaires for depression and anxiety: systematic review”, BMJ, Vol. 322/7283, pp. 406-409, https://doi.org/10.1136/bmj.322.7283.406.
[33] Gill, S. et al. (2007), “Validity of the mental health component scale of the 12-item Short-Form Health Survey (MCS-12) as measure of common mental disorders in the general population”, Psychiatry Research, Vol. 152/1, pp. 63-71, https://doi.org/10.1016/j.psychres.2006.11.005.
[48] Hankins, M. (2008), “The reliability of the twelve-item general health questionnaire (GHQ-12) under realistic assumptions”, BMC Public Health, Vol. 8/1, p. 355, https://doi.org/10.1186/1471-2458-8-355.
[61] Haroz, E. et al. (2017), “How is depression experienced around the world? A systematic review of qualitative literature”, Social Science & Medicine, Vol. 183, pp. 151-162, https://doi.org/10.1016/j.socscimed.2016.12.030.
[27] Harvard Medical School (n.d.), About the WHO WMH-CIDI, https://www.hcp.med.harvard.edu/wmhcidi/about-the-who-wmh-cidi/ (accessed on 31 May 2022).
[20] HHS (2021), U.S. Surgeon General Issues Advisory on Youth Mental Health Crisis Further Exposed by COVID-19 Pandemic, United States Department of Health and Human Services (HHS), https://www.hhs.gov/about/news/2021/12/07/us-surgeon-general-issues-advisory-on-youth-mental-health-crisis-further-exposed-by-covid-19-pandemic.html.
[31] Hoeymans, N. et al. (2004), “Measuring mental health of the Dutch population: A comparison of the GHQ-12 and the MHI-5”, Health and Quality of Life Outcomes, Vol. 2/23, https://doi.org/10.1186/1477-7525-2-2.
[57] Huang, F. et al. (2006), “Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients”, Journal of General Internal Medicine, Vol. 21/6, pp. 547-552, https://doi.org/10.1111/j.1525-1497.2006.00409.x.
[67] Hughes, A. et al. (2018), “Diagnostic and clinical utility of the GAD-2 for screening anxiety symptoms in individuals with multiple sclerosis”, Archives of Physical Medicine and Rehabilitation, Vol. 99/10, pp. 2045-2049, https://doi.org/10.1016/j.apmr.2018.05.029.
[52] Hystad, S. and B. Johnsen (2020), “The Dimensionality of the 12-Item General Health Questionnaire (GHQ-12): Comparisons of Factor Structures and Invariance Across Samples and Time”, Frontiers in Psychology, Vol. 11, https://doi.org/10.3389/fpsyg.2020.01300.
[65] Johnson, S. et al. (2019), “Psychometric properties of the General Anxiety Disorder 7-Item (GAD-7) scale in a heterogeneous psychiatric sample”, Frontiers in Psychology, Vol. 10, https://doi.org/10.3389/fpsyg.2019.01713.
[29] Kelly, M. et al. (2008), “Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: A comparison of five different methods”, BMC Psychiatry, Vol. 8/10, https://doi.org/10.1186/1471-244X-8-10.
[26] Kessler, R. and T. Bedirhan Üstün (2006), “The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI)”, International Journal of Methods in Psychiatric Research, Vol. 13/2, pp. 93-121, https://doi.org/10.1002/mpr.168.
[47] Kessler, R. et al. (2010), “Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative”, International Journal of Methods in Psychiatric Research, Vol. 19/S1, pp. 4-22, https://doi.org/10.1002/mpr.310.
[89] Keyes, C. (2002), “The mental health continuum: From languishing to flourishing in life”, Journal of Health and Social Behavior, Vol. 43/2, pp. 207-222, https://doi.org/10.2307/3090197.
[78] Khadjesari, Z. et al. (2017), “Validation of the AUDIT-C in adults seeking help with their drinking online”, Addiction Science & Clinical Practice, Vol. 12/1, p. 2, https://doi.org/10.1186/s13722-016-0066-5.
[72] Khubchandani, J. et al. (2016), “The psychometric properties of PHQ-4 depression and anxiety screening scale among college students”, Archives of Psychiatric Nursing, Vol. 30/4, pp. 457-462, https://doi.org/10.1016/j.apnu.2016.01.014.
[10] KOSIS (n.d.), Annual prevalence of mental disorders (adjusted for sex and age) (database), Korean Statistical Information Service, https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=TX_117_2009_HB027&conn_path=I2 (accessed on 16 May 2022).
[11] KOSIS (n.d.), Depressive disorder prevalence (database), National Health and Nutrition Survey, Korean Statistical Information Service, https://knhanes.kdca.go.kr/knhanes/sub01/sub01_05.do#none (accessed on 31 August 2022).
[93] Koushede, V. et al. (2019), “Measuring mental well-being in Denmark: Validation of the original and short version of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS and SWEMWBS) and cross-cultural comparison across four European settings”, Psychiatry Research, Vol. 271, pp. 502-509, https://doi.org/10.1016/j.psychres.2018.12.003.
[58] Kroenke, K., R. Spitzer and J. Williams (2001), “The PHQ-9: Validity of a brief depression severity measure”, Journal of General Internal Medicine, Vol. 16/9, https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
[74] Kroenke, K. et al. (2009), “An ultra-brief screening scale for anxiety and depression: The PHQ-4”, Psychosomatics, Vol. 50/6, pp. 613-621, https://doi.org/10.1176/APPI.PSY.50.6.613.
[56] Kroenke, K. et al. (2009), “The PHQ-8 as a measure of current depression in the general population”, Journal of Affective Disorders, Vol. 114/1-3, pp. 163-173, https://doi.org/10.1016/j.jad.2008.06.026.
[90] Lamers, S. et al. (2011), “Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF)”, Journal of Clinical Psychology, Vol. 67/1, pp. 99-110, https://doi.org/10.1002/jclp.20741.
[62] Löwe, B. et al. (2008), “Validation and standardization of the Generalized Anxiety Disorder screener (GAD-7) in the general population”, Medical Care, Vol. 46/3, pp. 266-274, https://doi.org/10.1097/mlr.0b013e318160d093.
[73] Löwe, B. et al. (2010), “A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population”, Journal of Affective Disorders, Vol. 122/1-2, pp. 86-95, https://doi.org/10.1016/j.jad.2009.06.019.
[68] Luo, Z. et al. (2019), “Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: A validation study and meta-analysis”, General Hospital Psychiatry, Vol. 60, pp. 50-56, https://doi.org/10.1016/j.genhosppsych.2019.07.008.
[54] Manea, L., S. Gilbody and D. McMillan (2012), “Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis”, Canadian Medical Association Journal, Vol. 184/3, pp. E191-E196, https://doi.org/10.1503/cmaj.110829.
[55] Moriarty, A. et al. (2015), “Screening and case finding for major depressive disorder using the Patient Health Questionnaire (PHQ-9): A meta-analysis”, General Hospital Psychiatry, Vol. 37/6, pp. 567-576, https://doi.org/10.1016/j.genhosppsych.2015.06.012.
[3] Mueller, A. and D. Segal (2015), “Structured versus Semistructed versus Unstructured Interviews”, in Cautin, R. and S. Lilienfeld (eds.), The Encyclopedia of Clinical Psychology, John Wiley & Sons, Inc, https://www.researchgate.net/profile/Daniel-Segal-6/publication/313966231_Structured_versus_Semistructured_versus_Unstructured_Interviews/links/599a13bcaca272e41d3ec727/Structured-versus-Semistructured-versus-Unstructured-Interviews.pdf (accessed on 30 March 2022).
[6] National Academies of Sciences Engineering and Medicine (2021), Mental Health, Substance Use, and Wellbeing in Higher Education: Supporting the Whole Student, The National Academies Press, Washington, D.C., https://doi.org/10.17226/26015.
[13] National Center for Health Statistics (2021), Estimates of Mental Health Symptomatology, by Month of Interview: United States, 2019 (database), U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, https://www.cdc.gov/nchs/data/nhis/mental-health-monthly-508.pdf (accessed on 16 May 2022).
[95] Ng Fat, L. et al. (2017), “Evaluating and establishing national norms for mental wellbeing using the short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS): Findings from the Health Survey for England”, Quality of Life Research, Vol. 26/5, pp. 1129-1144, https://doi.org/10.1007/s11136-016-1454-8.
[1] OECD (2021), A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill-Health, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/4ed890f6-en.
[18] OECD (2021), COVID-19 and Well-being: Life in the Pandemic, OECD Publishing, Paris, https://doi.org/10.1787/1e1ecb53-en.
[17] OECD (2021), Health at a Glance, OECD Publishing, Paris, https://doi.org/10.1787/19991312.
[19] OECD (2021), Supporting young people’s mental health through the COVID-19 crisis, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://www.oecd.org/coronavirus/policy-responses/supporting-young-people-s-mental-health-through-the-covid-19-crisis-84e143e5/.
[16] OECD (2020), How’s Life? 2020: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9870c393-en.
[80] OECD (2013), OECD Guidelines on Measuring Subjective Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9789264191655-en.
[23] OECD/European Union (2018), Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris/European Union, Brussels, https://doi.org/10.1787/health_glance_eur-2018-en.
[40] Ohrnberger, J. et al. (2020), “Validation of the SF12 mental and physical health measure for the population from a low-income country in sub-Saharan Africa”, Health and Quality of Life Outcomes, Vol. 18/78, https://doi.org/10.1186/s12955-020-01323-1.
[64] Parkerson, H. et al. (2015), “Cultural-based biases of the GAD-7”, Journal of Anxiety Disorders, Vol. 31, pp. 38-42, https://doi.org/10.1016/j.janxdis.2015.01.005.
[87] Pavot, W. and E. Diener (1993), “Review of the Satisfaction With Life Scale.”, Psychological Assessment, Vol. 5/2, pp. 164-172, https://doi.org/10.1037/1040-3590.5.2.164.
[86] Pavot, W. et al. (1991), “Further validation of the Satisfaction with Life Scale: evidence for the cross-method convergence of well-being measures”, Journal of Personality Assessment, Vol. 57/1, pp. 149-161, https://doi.org/10.1207/s15327752jpa5701_17.
[45] Prochaska, J. et al. (2012), “Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization”, International Journal of Methods in Psychiatric Research, Vol. 21/2, pp. 88-97, https://doi.org/10.1002/mpr.1349.
[25] Public Health Agency Sweden (2022), Synen på psykisk ohälsa och suicid, https://www.folkhalsomyndigheten.se/publicerat-material/publikationsarkiv/s/synen-pa-psykisk-ohalsa-och-suicid-/?pub=105538#105580.
[41] Quality Metric (n.d.), The SF-12v2 PRO Health Survey, https://www.qualitymetric.com/health-surveys-old/the-sf-12v2-health-survey/ (accessed on 10 May 2022).
[38] RAND (n.d.), Mental Health Inventory Survey, https://www.rand.org/health-care/surveys_tools/mos/mental-health.html (accessed on 10 May 2022).
[59] Richardson, L. et al. (2010), “Evaluation of the Patient Health Questionnaire-9 item for detecting major depression among adolescents”, Pediatrics, Vol. 126/6, pp. 1117-1123, https://doi.org/10.1542/peds.2010-0852.
[5] Ruedgers, R. (2001), Handbook of diagnositc and structured interviewing, Guilford Press, https://psycnet.apa.org/record/2001-05047-000.
[34] Rumpf, H. et al. (2001), “Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard”, Psychiatry Research, Vol. 105/3, pp. 243-253, https://doi.org/10.1016/S0165-1781(01)00329-8.
[12] SAMHSA (2019), Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (database), Substance Abuse and Mental Health Services Administration, Rockville, MD, https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf (accessed on 16 May 2022).
[82] Sándor, E. et al. (2021), Impact of COVID-19 on young people in the EU, Publications Office of the European Union, https://www.eurofound.europa.eu/publications/report/2021/impact-of-covid-19-on-young-people-in-the-eu#:~:text=COVID%2D19%20pandemic.-,Young%20people%20were%20more%20likely%20than%20older%20groups%20to%20experience,home%20requirements%20and%20school%20closures.
[22] Santé Publique France (2021), La santé mentale au temps de la COVID-19 : En parler, c’est déjà se soigner [Mental health in the time of COVID-19: Talking about it is already treating yourself], Santé Puique France, https://www.santepubliquefrance.fr/presse/2021/la-sante-mentale-au-temps-de-la-covid-19-en-parler-c-est-deja-se-soigner.
[24] Santomauro, D. et al. (2021), “Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic”, The Lancet, Vol. 398/10312, pp. 1700-1712, https://doi.org/10.1016/S0140-6736(21)02143-7.
[92] Shannon, S. et al. (2020), “Testing the factor structure of the Warwick-Edinburgh Mental Well-Being Scale in adolescents: A bi-factor modelling methodology”, Psychiatry Research, Vol. 293, https://doi.org/10.1016/j.psychres.2020.113393.
[43] Slade, T., R. Grove and P. Burgess (2011), “Kessler Psychological Distress Scale: Normative Data from the 2007 Australian National Survey of Mental Health and Wellbeing”, Australian & New Zealand Journal of Psychiatry, Vol. 45/4, pp. 308-316, https://doi.org/10.3109/00048674.2010.543653.
[70] Spitzer, R. et al. (2006), “A brief Measure for assessing Generalized Anxiety Disorder: The GAD-7”, Archives of Internal Medicine, Vol. 166/10, pp. 1092-1097, https://doi.org/10.1001/ARCHINTE.166.10.1092.
[71] Stanhope, J. (2016), “Patient Health Questionnaire-4”, Occupational Medicine, Vol. 66/9, pp. 760-761, https://doi.org/10.1093/occmed/kqw165.
[8] Statistics Canada (2013), Canadian Community Health Survey: Mental Health, 2012, The Daily, https://www150.statcan.gc.ca/n1/daily-quotidien/130918/dq130918a-eng.htm (accessed on 16 May 2022).
[94] Stewart-Brown, S. et al. (2009), “Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish Health Education Population Survey”, Health and Quality of Life Outcomes, Vol. 7/1, p. 15, https://doi.org/10.1186/1477-7525-7-15.
[35] Strand, B. et al. (2003), “Measuring the mental health status of the Norwegian population: A comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36)”, Nordic Journal of Psychiatry, Vol. 57/2, pp. 113-118, https://doi.org/10.1080/08039480310000932.
[53] Sunderland, M. et al. (2019), “Self-Report Scales for Common Mental Disorders”, in The Cambridge Handbook of Clinical Assessment and Diagnosis, Cambridge University Press, https://doi.org/10.1017/9781108235433.019.
[36] Thorsen, S. et al. (2013), “The predictive value of mental health for long-term sickness absence: the Major Depression Inventory (MDI) and the Mental Health Inventory (MHI-5) compared”, BMC Medical Research Methodology, Vol. 13/115, https://doi.org/10.1186/1471-2288-13-115.
[7] Topp, C. et al. (2015), “The WHO-5 well-being index: A systematic review of the literature”, Psychotherapy and Psychosomatics, Vol. 84/3, pp. 167-176, https://doi.org/10.1159/000376585.
[15] University of Essex, Institute for Social and Economic Research (2022), Understanding Society: Waves 1-11, 2009-2020 and Harmonised BHPS: Waves 1-18, 1991-2009 (database), 5th Edition. UK Data Service., https://doi.org/10.5255/UKDA-SN-6614-16 (accessed on 10 June 2022).
[39] Vilagut, G. et al. (2013), “The mental component of the Short-Form 12 health survey (SF-12) as a measure of depressive disorders in the general population: Results with three alternative scoring methods”, Value in Health, Vol. 16/4, pp. 564-573, https://doi.org/10.1016/j.jval.2013.01.006.
[84] Ware, J. et al. (1993), SF-36 Health Survey: Manual and Interpretation Guide, The Health Institute, New England Medical Center Hospitals, https://www.researchgate.net/profile/John-Ware-6/publication/313050850_SF-36_Health_Survey_Manual_Interpretation_Guide/links/594a5b83aca2723195de5c3d/SF-36-Health-Survey-Manual-Interpretation-Guide.pdf (accessed on 22 January 2023).
[37] Ware, J. et al. (2002), How to score SF-12 items: How to score version 2 of the SF-12 Health Survey, https://www.researchgate.net/publication/291994160.
[91] Warwick Medical School (2021), The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS), https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/.
[75] Washington Group on Disability Statistics (2020), The Washington Group Short Set on Functioning: Enhanced (WG-SS Enhanced), https://www.washingtongroup-disability.com/fileadmin/uploads/wg/Documents/Washington_Group_Questionnaire__3_-_WG_Short_Set_on_Functioning_-_Enhanced.pdf.
[14] Woodhead, C. et al. (2012), “Impact of exposure to combat during deployment to Iraq and Afghanistan on mental health by gender”, Psychological Medicine, Vol. 42/9, pp. 1985-1996, https://doi.org/10.1017/S003329171100290X.
[79] World Health Organization (2001), AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care, World Health Organization, https://www.who.int/publications/i/item/audit-the-alcohol-use-disorders-identification-test-guidelines-for-use-in-primary-health-care.
[81] World Health Organization (1998), Wellbeing measures in primary health care/the DepCare Project: Report on a WHO meeting, World Health Organization, https://apps.who.int/iris/handle/10665/349766.
[30] Yamazaki, S., S. Fukuhara and J. Green (2005), “Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan”, Health and Quality of Life Outcomes, Vol. 3/1, pp. 1-7, https://doi.org/10.1186/1477-7525-3-48/FIGURES/1.
[60] Zimmerman, M. et al. (2012), “How can we use depression severity to guide treatment selection when measures of depression categorize patients differently?”, Journal of Clinical Psychiatry, Vol. 73/10, pp. 1287-1291, https://doi.org/10.4088/JCP.12m07775.
Notes
← 1. Of course, this implies that diagnoses reached through clinical interviews are only as valid as the classification system they are based on (Mueller and Segal, 2015[3]) (see also Box 3.4 in Chapter 3).
← 2. Of course, the coverage of household surveys is also not complete and includes only those sampled. Typically, people living in institutional settings as well as the homeless (who are likely to have higher prevalence of mental ill-health than the general population) are not taken into account.
← 3. The following countries responded to the questionnaire: Australia, Austria, Belgium, Bulgaria, Canada, Chile, Colombia, Costa Rica, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Korea, Latvia, Lithuania, Luxembourg, Mexico, the Netherlands, Norway, New Zealand, Poland, Portugal, Slovenia, the Slovak Republic, Spain, Sweden, Switzerland, Türkiye, the United Kingdom and the United States.
← 4. The OECD also publishes administrative data on mental health service provision, such as the number of psychiatrists, psychologists or mental health professionals per 100 000 population; the number of hospital beds devoted to mental health care; spending on mental health services; etc. (OECD, 2021[17]). As these are not considered population-level mental health outcomes, they are not further considered for the purposes of this project.
← 5. Percentages do not add up to 68% because some countries did both: introduced new stand-alone surveys and added mental health modules to existing surveys.
← 6. Furthermore, it is worth noting that while the MHI-5 appeared in the well-being ad hoc modules for the 2013 and 2018 European Union Statistics on Income and Living Conditions (EU-SILC) survey administered by Eurostat, in future well-being modules the tool has been removed. Therefore, future use of the MHI-5 may be significantly diminished, although some individual member states may elect to keep the measure in their own national health and/or well-being surveys.
← 7. For an extended discussion of surveys used to measure attitudes and stigma towards mental health, refer to Table 6.2 in (OECD, 2021[1]).