Patrizio SICARI
OECD
Douglas SUTHERLAND
OECD

Patrizio SICARI
OECD
Douglas SUTHERLAND
OECD
Overall, the health of the Irish population has improved substantially during recent decades and is quite good compared with other OECD countries. However, spending is elevated, partly reflecting a system that is strongly based on hospitals. Population ageing is exacerbating spending pressures. In addition, the health sector is dealing with past underspending, particularly in capital outlays in the years following the global financial crisis, that have constrained service delivery, contributing to substantial waiting lists and heavy pressure on staff. The government has initiated wide-ranging reforms, termed Sláintecare, with the aim of broadening the coverage of universal care, decentralising provision and enhancing the integration of primary, community and hospital care. The reforms are complicated, reflecting a healthcare system that is complex and at times opaque. This is particularly the case with the interaction of the public and private parts of the system in which private patients enjoy easier access to care, leading to concerns about a two-tier healthcare system. The creation of new regional health areas is set to support more decentralised decision-making, but information systems to track spending and reform implementation need an overhaul. The COVID-19 pandemic has diverted policy-making attention just as the reforms got underway, but stepping up the efforts to address legacy issues and move forward on the reforms is now key to meet the coming challenges while using resources effectively.
The health of the Irish population improved considerably during recent decades. In comparison with other OECD countries, the population’s self-reported health status was amongst the best before the pandemic (Figure 2.1). Life expectancy at birth, in particular, rose to 80.8 years for men and 84.7 years for women in 2019 (among the highest in the OECD) and 6.8 and 5.5 years above their levels in 2000, respectively (Figure 2.2). In addition, the share of the working age population reporting moderate or more severe levels of depression decreased to 4.8% by 2019, 40% lower than in 2014, and somewhat below the EU average (Eurostat, 2019). Ireland’s population is thus relatively healthy, but differences in health status remain significant across income groups.
Share of the population aged 15 and older with good/very good health, 2019
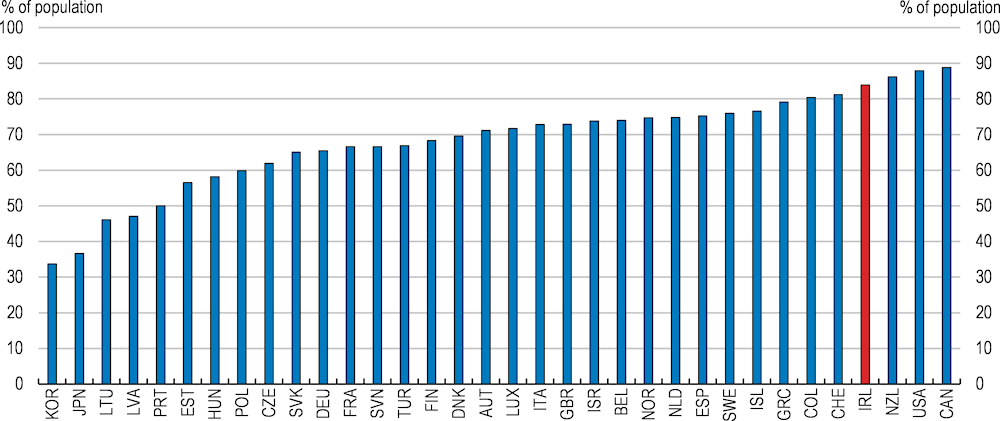
Note: Results for Canada, Colombia, New Zealand and the United States are not directly comparable due to methodological differences in the survey questionnaire resulting in a bias towards a more positive self-assessment of health.
Source: OECD, Health Statistics database.
The share of deaths caused by cancer in overall mortality was higher than the EU average before COVID-19, while pre-pandemic estimates of Ireland’s cancer incidence rate – the number of new cases registered in a given year normalised by the population – put it as the highest in the European Union in 2020 (OECD, 2021a). This suggests cancer prevention and care will represent priority areas, especially after COVID-19. Relatively high cancer morbidity is partly driven by behavioural risk factors, e.g., smoking, binge drinking and unhealthy dietary habits. Whilst smoking rates have decreased significantly in recent decades, adult overweight and obesity rates are of growing concern, together with alcohol abuse. More than one fifth of Irish adults reported regular heavy alcohol consumption in 2019, but evidence suggests that heavy drinking among 15-year-olds is less widespread in Ireland than across the European Union. Efforts to reduce alcohol consumption could be reinforced by the recent strengthening of alcohol control policies, including the introduction of minimum unit pricing.
Life expectancy at birth
Quality of care is generally good, as suggested by age-standardised mortality rates somewhat below the OECD average for both preventable and treatable causes (OECD, 2021a). However, there are widespread inefficiencies. The COVID-19 crisis highlighted significant weaknesses in the public health system, affecting its resources as well as its organisation. This came on top of a degree of dissatisfaction about a de facto two-tier system, emphasised by extremely long waiting lists for hospital inpatient and outpatient consultations. Healthcare is largely funded by the State, which accounted for 78.3% of total current health expenditures in 2021 (3.8 percentage points above 2019), while the remaining part is roughly equally covered by household out-of-pocket payments and voluntary private insurance schemes. Buyers of voluntary private health insurance (PHI), though, enjoy faster access to several public hospital healthcare services than lower-income individuals eligible for free care (Medical cardholders). At the same time, rising costs of specialist consultations and specific treatments have resulted in increased unmet care needs among low-income households and younger age cohorts with weak PHI coverage. These adverse outcomes stress the need to balance the trade-off between efficiency and equity, while reforming Ireland’s complex health system. For instance, measures resulting in increased public spending should avoid providing incentives to free-ride subsidised public care to those who could bear a greater share of its costs. Conversely, if not well-designed, policies shifting part of the burden of costly healthcare onto the private sector, such as through higher out-of-pocket payments, could undermine the broader objective of ensuring more vulnerable households have timely access to care.
The pandemic has likely aggravated shortcomings and heightened the risk of poorer health outcomes, as access to care for non-COVID related health conditions was limited. Additionally, though decreasing considerably in 2020, most likely due to patients avoiding – when possible – hospitalisation for fear of contagion, avoidable hospital admissions remain relatively high for conditions like asthma and Chronic Obstructive Pulmonary Disease (COPD), which are largely treatable in primary care. Reforms to foster primary care, expand the medical staff and the provision of integrated services, combined with measures to address the main drivers of avoidable deaths (Healthy Ireland Initiative), are currently being outlined and implemented in the context of the ten-year Sláintecare strategy (see below).
The Irish population’s self-assessment of unmet healthcare needs is somewhat lower than in the average of European OECD countries (Figure 2.3). However, waiting times in Ireland have grown, notably for outpatients, and implicitly affect a much larger share of the population (Figure 2.4). The pandemic has seen outpatient waiting lists increase further, particularly for those waiting for over 18 months. For inpatient and day cases, the numbers waiting for short periods has declined, probably reflecting patients deferring medical assistance. However, like in other OECD countries during the pandemic, the numbers waiting for longer periods has risen, reversing some success during the late 2010s in reducing the numbers of those waiting for over six months.
Unmet needs for medical examination by income quintile, 2021 or latest available year
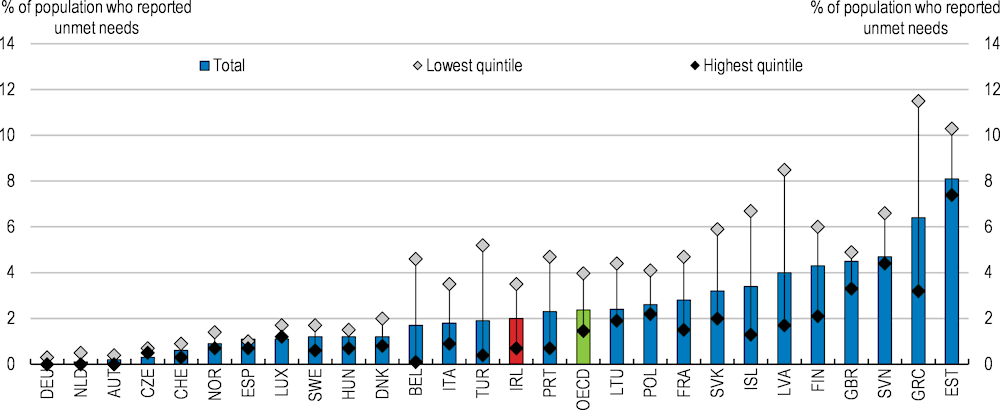
Note: Includes unmet needs due to financial, geographic, or waiting time reasons. Data for Norway, Slovenia, Switzerland, and Türkiye refer to 2020; data for Iceland and the United Kingdom refer to 2018.
Source: Eurostat, EU-SILC database.
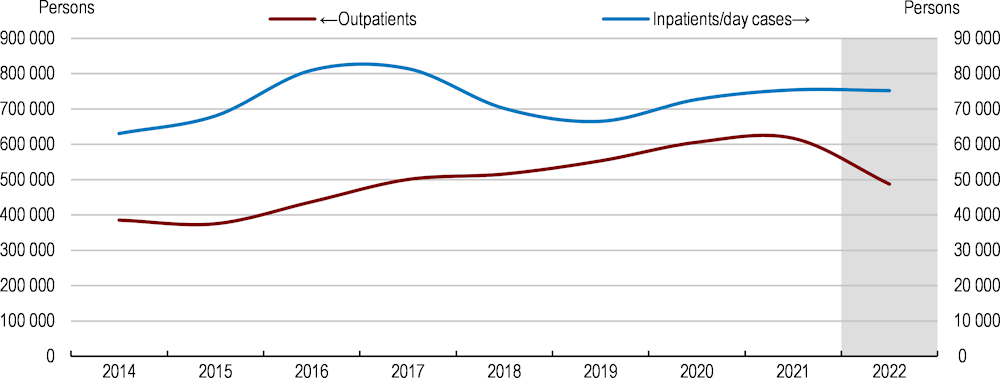
Note: The shaded area corresponds to the government’s projection for 2022.
Source: Department of Health, The 2022 Waiting List Action Plan.
Comparing waiting times across countries is difficult as like-for-like data are often not available. Furthermore, Ireland’s relatively weak digital infrastructure complicates matters. Key national healthcare datasets are in the custody of nine different institutions, which adopt different patient unique identifiers and have no linkage at the national level (Oderkirk, 2021). Besides, there are no national electronic health records, except for some specific clinical populations or systems (Walsh et al., 2021). Tracking patients from General Practitioner (GP) referral to discharge is thus not always possible in Ireland, also due to inadequate reporting standards and the incomplete coverage of the Individual Health Identifier, whose adoption accelerated in the context of COVID-19 vaccination programmes. The official measures identify waiting times as the period between the patients’ registration in the waiting list for a specified procedure (following specialist assessment) and a designated cut-off date. According to this metric, across 13 OECD countries with comparable data for seven public elective procedures, mean and median patient waiting times in Ireland rank in the middle: below most Eastern European countries, but well above those in the United Kingdom, Sweden and New Zealand (OECD Health Statistics, 2022).
Waiting list measures based on the number of patients registered at a certain point in time may be unreliable gauges of pressures due to the impossibility of identifying patients opting to use the private sector or opting out of the treatment altogether. In addition, patients may die while still waiting. Estimated waiting times from specialist assessment to treatment across comparable official data from other OECD countries for cataract surgery and hip and knee replacement procedures suggest Ireland ranks poorly, e.g., third or fourth longest waiting times out of 17 countries (Brick and Connolly, 2021).
When the COVID-19 pandemic struck in early 2020, Ireland’s health system was relatively ill-prepared to cope with its consequences. Highly centralised and largely relying on expensive hospital-based care services, the health system suffered several imbalances. Mostly a legacy of the procyclicality of health spending, such as the cuts after 2008 and of weak capital investment in health infrastructure up to the 1990s (Hennessy et al., 2021), the existing capacity constraints included understaffing, outdated hospital infrastructure, low numbers of hospital beds associated with inpatient bed occupancy rates well above international safety standards and, finally, weak ICU facilities (Figure 2.5; Humphries et al., 2021; Shine and Hennessy, 2022; Kennelly et al., 2020).
Ireland’s pandemic response prioritised ring-fencing the sustainability of hospital care services from the systemic risk posed by surging COVID-19-related admissions. This objective shaped the authorities’ decisions to promptly impose social distancing – coupled with contact tracing – and mobility restrictions to limit the diffusion of the virus. This included the repeated introduction of strict national lockdowns in March, October and late December 2020 (Humphries et al., 2021), when evidence of a rising number of infections suggested heightened risks of marked deteriorations in hospitalisation patterns.
Swift reorganisation of processes and resources prevented hospitals from being overwhelmed by the successive waves of COVID-19 variants. Early in the pandemic, the government established free universal care at the point of delivery for all COVID-19-related diagnosis and care services. In addition, it temporarily suspended all routine and non-essential health and social care services, which added further strain on already stretched waiting lists for diagnostics, elective non-urgent surgery or inpatient consultations. This allowed the concerned staff to be mobilised and redeployed in COVID-19 care units (Burke et al., 2021). On specific occasions, staff redeployment even exceeded the boundaries of the public sector. Indeed, the Health Service Executive (HSE), the publicly-funded national provider of health and personal social services, allowed its staff, particularly nurses and healthcare assistants, to be relocated – if willing – in private nursing homes, to assist them in tackling COVID-19. That was justified by the need to address nursing homes’ severe staff shortages due to illness, which made it hard to ensure patients were properly cared for. At the same time, GPs supported the process by assuming the role of first point of contact for individuals with suspected symptoms, which was mainly performed via phone or video consultations (Kennelly et al., 2020). Moreover, as part of the efforts towards enhanced surge-based capacity, hospitals often reconverted anaesthetic rooms or post-operatory beds into ICU stations, while mobilising recently retired workforce and setting up training modules for redeployed non-ICU staff.
2019 or latest year available
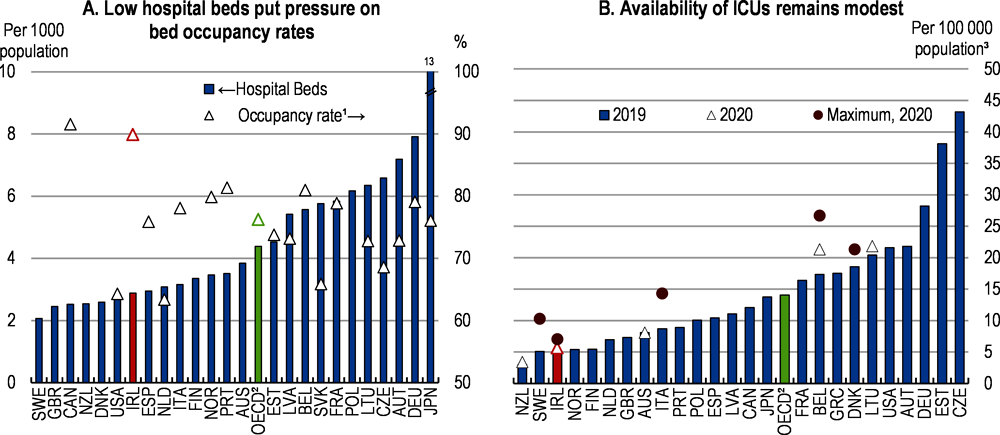
1. Occupancy rate of curative (acute) care beds.
2. Unweighted average across 27 countries with available data in Panel A; 33 countries in Panel B.
3. Data for Ireland cover critical care beds only; data for Slovenia include neonatal and paediatric ICU beds; data for the United Kingdom refer to England only.
Sources: OECD, Health Statistics database; and OECD, Health at a Glance 2021.
The involvement of private hospitals took some of the pressure off the public system, even though only part of their capacity was actually activated. In order to boost public acute care capacity, in March 2020, the government temporarily placed private hospitals under HSE’s governance. According to the agreement, the HSE had access to private hospitals’ capacity for a period of three months, for a payment of €287 million. During this period, no private work was allowed in private hospitals, although continuity of – essential – care to existing private patients was ensured. Based on this ‘safety net’ agreement, public patients gained access to 2 300 beds and 47 ICUs in 18 private hospitals, for an overall number of about 50 000 procedures (Committee of Public Accounts, 2021). Concretely, the scheme never used more than 45% of private hospitals’ capacity, which raised some cost-effectiveness concerns, especially considering that, based on the agreement’s terms, some private patient treatments, ordinarily funded by private insurances, were paid through the public purse (Houses of the Oireachtas, 2020). Moreover, the agreement, which was not initially negotiated with representatives of hospital staff (Mercille et al., 2021), excluded about 600 fully private practitioners, who were unable to continue the care relationship with their patients and were only offered the one-way solution of accepting temporary public-only hospital contracts, with no real clarity on their indemnities.
In light of the lessons learnt with the first agreement, and to prepare for a second wave of the pandemic, the government changed tactics and prioritised additional capacity based on specific needs. HSE entered into bilateral agreements with individual private hospitals to generate surge capacity via increased competition in streamlined public tenders, to be issued whenever the sustainability of public acute care was put at risk by rising infections. In its September 2020 Winter Plan, the HSE clearly outlined private hospitals’ key role in supporting public patients’ enhanced access to elective care via reduced waiting lists and providing essential ongoing care. This was formalised in the Safety Net II agreement, at the beginning of the third wave in January 2021, which, while allowing for ongoing treatment of private patients, foresaw private hospitals supporting the health system by making available a fixed 30% of their own capacity, plus an additional share negotiable on an as-needed basis. Later on, effective containment of new infections allowed the HSE to gradually release most of the private hospitals involved from the revised scheme.
Initiatives to significantly step up hospital bed capacity are ongoing. Since 2020, more than 2 000 acute, critical and community beds have been added, while the last two budgets allocated funding to deliver 250 additional beds in 2023 (Government of Ireland, 2022). In 2021-22, €77 million of additional funding was earmarked to increase national critical care capacity – currently at around 320 ICUs – to 340 beds by 2023, while the recruitment of skilled critical care staff was prioritised (HSE, 2022a). These efforts are welcome and achieving the objective of 446 ICUs by 2031 (Shine and Hennessy, 2022), established in the 2020 Strategic Plan for Critical Care, should be prioritised.
Overall, spending on health is high, particularly in light of a relatively young population. At the same time, health care is expensive in comparison with other European countries (Lorenzoni and Dougherty, 2022). The standard metric of spending as a share of GDP is complicated by the multinational nature of the Irish economy. When using the measure of national income that adjusts for the multinational sector, Ireland is one of the high spenders (Figure 2.6, Panel A). Spending on health accounts for one fifth of total public spending (Panel B). This partly reflects the fact that Ireland, in contrast to many other OECD countries and OECD System of Health Accounts guidelines (OECD, 2018; Wren and Fitzpatrick, 2020), includes some of the social care components of long-term care expenditure (assistance services that enable a patient to live independently, payments to family care givers or home-care services expenditures) in health spending. Providing an estimate of health-related social expenditure, as currently under discussion, would improve financial reporting in the health sector.
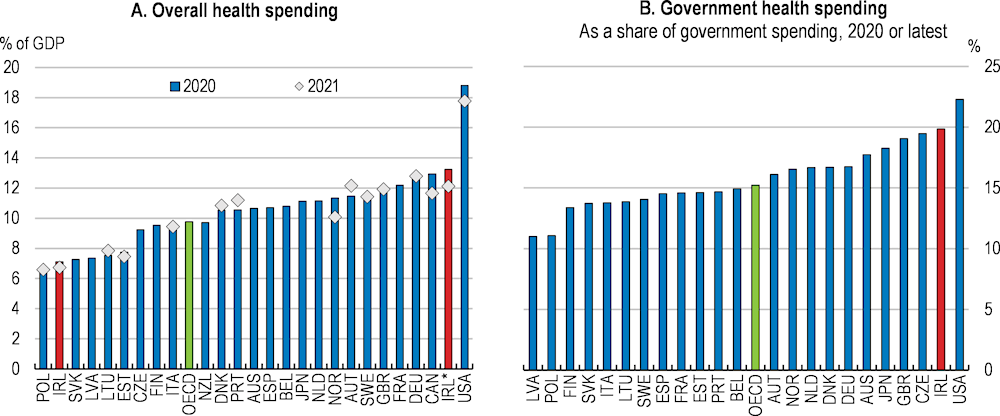
Note: IRL* denotes health spending for Ireland as a share of modified gross national income (GNI*).
Source: OECD, Health Expenditure and Financing database; and OECD, National Accounts database.
Health spending is subject to cost pressures largely stemming from ageing and death-related costs, the costs of new technologies (including pharmaceuticals), and increased demand as incomes rise. For example, at present, there are relatively few alternatives to staff spending time with elderly patients, particularly those with dementia. As average incomes rise across the economy, attracting staff into the long-term care sector requires higher salaries, pushing up health spending without necessarily seeing compensating productivity gains. In Ireland, the global market for trained personnel is another factor bidding up salaries, on the back of pay costs already accounting for about one third of HSE’s current expenditures in recent years (HSE, 2022b). At the same time, the COVID-19 pandemic emphasised the need for enhanced investment in machinery and equipment, which was close to the OECD average but below that of several European peers before the pandemic (OECD, 2021a). As a result of these pressures, health care costs in Ireland are relatively elevated, notably in hospitals (Lorenzoni and Dougherty, 2022), and compensation is quite high for some groups (Figure 2.7).
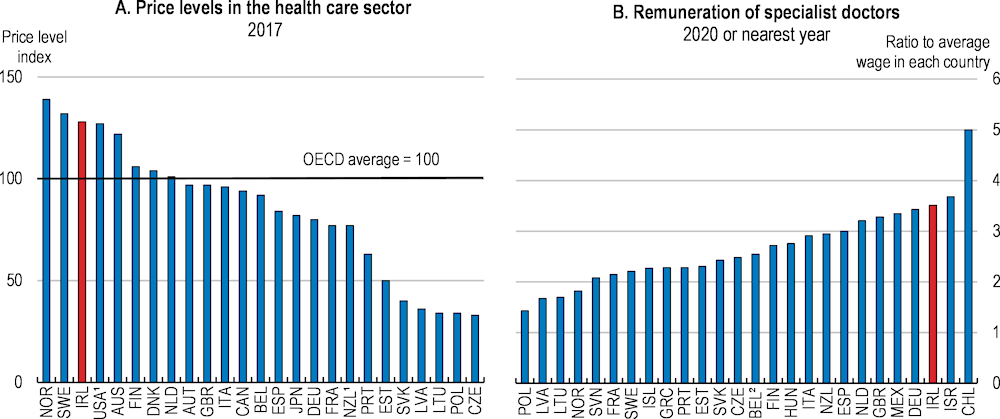
1. For hospitals, PPPs are estimated predominantly by using salaries of medical and non-medical staff (input method).
2. Estimate for Belgium includes practice expenses, which results in an over-estimation.
Source: OECD, Health at a Glance 2021; and OECD, Health Statistics database.
Spending has been relatively volatile in recent decades, reflecting the retrenchment of government outlays following the 2008 global financial crisis (Figure 2.8). The squeeze on spending was not uniform. Recognising an imbalance between higher numbers of nurses relative to doctors and other health professionals, the spending squeeze was mainly felt by nurses and midwives (Figure 2.9). In addition, in line with a more general trend across government functions, public capital spending on health was sharply cut back until recently (Figure 2.10). Besides its impact on the system’s capacity, the significant pro-cyclicality of spending has triggered concerns about equity in access and the well-being of poorer households during downturns (Nolan et al., 2014).
The private health insurance contribution to financing current health spending rose in the wake of the 2008 global financial crisis. The government, in a drive to rein in public spending, introduced prescription charges for medical card holders, while curtailing their dental care benefits, and increased user charges for several outpatient consultations and treatments. As a result, the share of the private sector in the financing of health expenditure peaked at about 30% in 2013 (Figure 2.11, Panel A), before dropping by 4 percentage points by 2019 with the economic recovery. Household out-of-pocket payments grew at an average nominal annual rate of less than 1% in the five years preceding the pandemic, remaining among the lowest in the OECD (Panel B). The leading role of the state during the pandemic further reduced the share of private health financing.
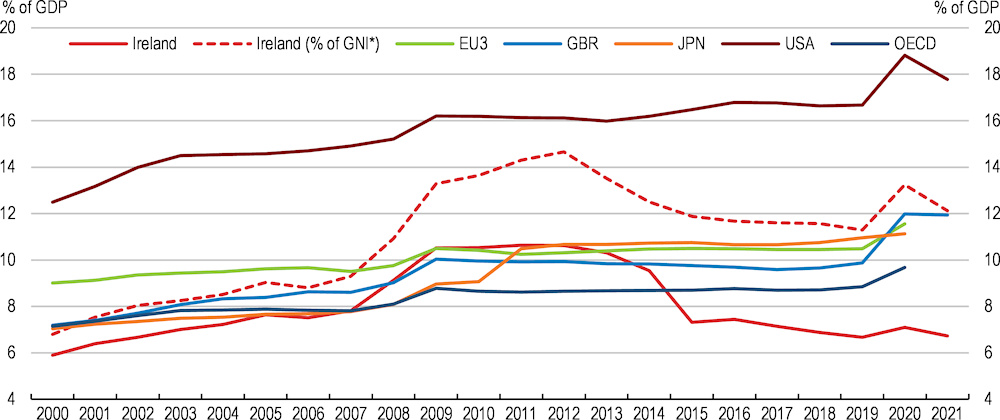
Note: GNI* represents modified Gross National Income at current market prices. EU3 stands for Germany, France and Italy. EU3 and OECD represent unweighted averages for composing countries. The system of Health Accounts was implemented in 2011, resulting in a methodological break in 2011.
Source: OECD, Global Health Expenditure database.
Persons aged 15-89 in employment
Growth rate of government health expenditure
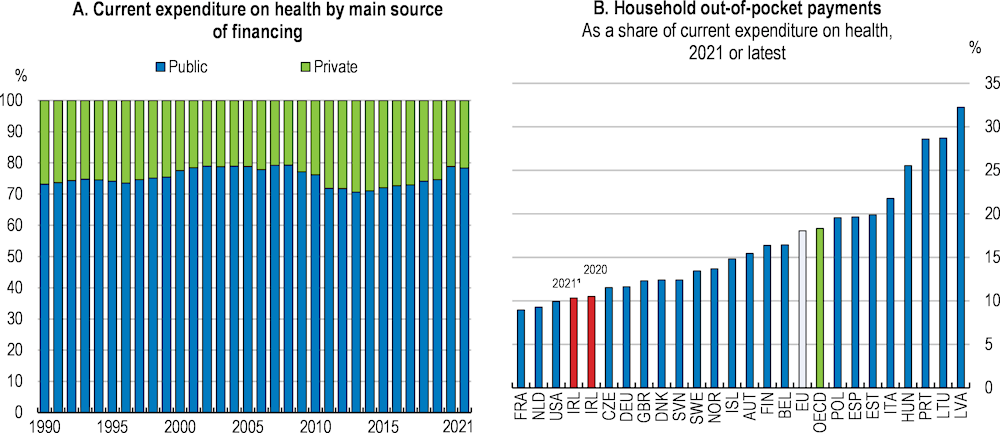
Note: In Panel A, private health care financing includes voluntary health care payment schemes and household out-of-pocket payments, while Panel B includes only household out-of-pocket payments. 1. Provisional estimate.
Source: OECD, Health Statistics database.
Past projections of health spending growth in Ireland, from even just about a decade ago, have erred on the downside, even though they used GDP rather than gross national income as the denominator. More recent projections suggest higher health spending levels than earlier ones (de Biase et al., 2022), notably due to the rise in long-term care costs (European Commission, 2021). Given Ireland’s current youthful population, rapid expected ageing and relatively high long-term care costs, the projected increases in spending are substantial. Incorporating health spending projections alongside pension projections into the OECD’s long-term model reveals that Ireland is facing some of the largest pressures on public spending to 2060 (Figure 2.12).
Projected change in expenditures from 2021 to 2060
Reforms underway suggest a movement of resources from acute towards non-acute care. However, so far, staff recruitment at primary- and community-level has not yet picked up markedly, in contrast with the larger staff gains in acute settings since 2014 (Fleming et al., 2022). As such, the locus of spending growth will change. More granular recent projections to 2035 suggest that spending growth outside the hospital sector will be pronounced, particularly in long-term residential care, home support and the high-tech community pharmaceutical scheme (Walsh et al., 2021). Earlier interventions outside the hospital setting can reduce overall costs. For example, some evidence suggests that primary care interventions to detect and treat frailty can delay or reverse it (Travers et al., 2019). As frailty is associated with heightened risks of illness, falls, disability, poorer outcomes after surgery and dependency and institutionalisation, effective primary care interventions are likely to reduce pressure on acute hospitals and long-term care facilities, reducing both health care use and spending (OECD, 2020a). Likewise, effective promotion and prevention programmes have the potential to contain the long-term costs of mental ill-health. In particular, the adoption of e-health solutions, combined with parenting and educational interventions (to help prevent anxiety disorders in young people) and well-being programmes in the workplace have generated significant savings in Australia and England (OECD, 2021b).
While spending projections are an important tool to assess pressures on public spending, they rely on a number of simplifying assumptions. Countries have been pursuing a number of options to slow spending growth. Public per capita spending growth on health had been slowing in a number of other OECD countries (including Ireland) before the pandemic, particularly following the 2008 global financial crisis. This was notable in curative and rehabilitative care and, to a lesser extent, medical goods (Lorenzoni et al., 2017). In many countries, including Ireland, the pandemic has spurred greater use of telemedicine, which offers potential to raise efficiency in the delivery of some services. Greater use of digitalisation, backed by the scaling-up of the needed digital infrastructure, can support health care workers and reduce pressure. For example, in Japan, the use of robots and remote sensors in long-term residential care settings allows medical staff to prioritise the patients most in need of interventions. Similarly, larger use of generics may help contain rapidly increasing spending on pharmaceuticals (see below). Against this background, efforts to boost efficiency could help offset spending pressures.
Significant gains in life expectancy, combined with a larger incidence of chronic conditions, partly because of rapid population ageing, exert significant pressures on health spending. At the same time, technological and treatment development translate into higher demand for new services, which are usually more expensive. In light of these and other structural fiscal challenges (pensions, housing, green and digital transitions), enhancing the efficiency of public spending will be key in ensuring adequate access to healthcare for all whilst preserving fiscal sustainability.
Recent OECD calculations, following Dutu and Sicari (2020) – and updating results from the OECD Economic Surveys of Switzerland and the Slovak Republic (OECD, 2015a and OECD, 2017a) ̶ use a non-parametric approach to measure the efficiency of healthcare expenditures (Box 2.1). Based on a restricted sample of OECD countries whose health systems are relevant benchmarks for Ireland, and subject to the caveats highlighted in Box 2.1, the results point to potential efficiency gains in healthcare spending between 2004 and 2019, which would have moved Ireland from the “least efficient” group towards the middle of the distribution (Figure 2.13). Estimated potential efficiency gains are larger across the input dimensions, suggesting that Ireland could in theory save up to 15% of its current expenditure on health, while maintaining the life expectancy of the population unchanged, if it were able to fully exploit the efficiency gains of frontier countries – again subject to the caveats in Box 2.1. The potential for similar gains along the output dimension seem more limited. Adjusting the composition of healthcare spending to OECD best practice, while keeping its level constant, may increase life expectancy by around 1%.
Restricted sample
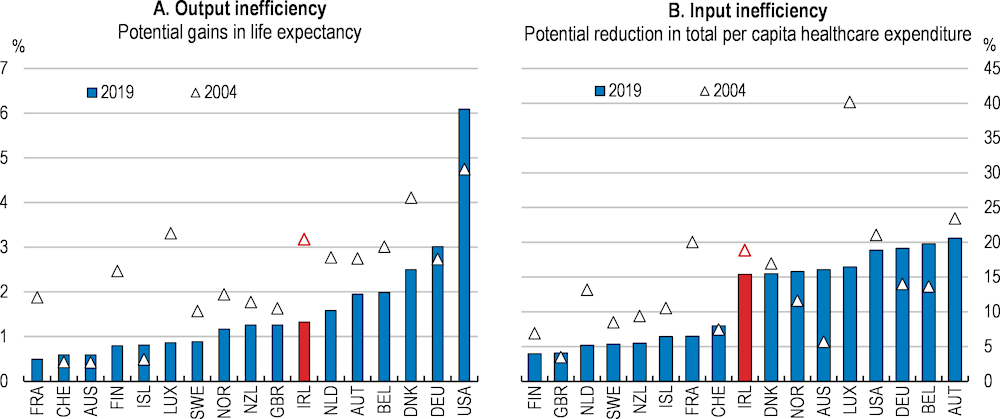
Note: The restricted sample is obtained by excluding Eastern and Southern European OECD countries from the sample, as well as all non-European ones, with the exception of Australia, New Zealand and the United States.
Source: OECD Secretariat calculations using R’s FEAR package, as made available in Wilson (2008).
Data envelopment analysis (DEA) is a nonparametric statistical technique which uses linear programming of input-output data combinations to construct a frontier of best practice countries. It then interprets each deviation from the latter as an inefficient input-output pair (Charnes et al., 1978), without requiring the specification of any underlying functional form. The DEA-estimated frontier thus ‘envelops’ all available observations and a country’s vertical (horizontal) distance along the Y-axis (X-axis) represents the measure of achievable output (input) efficiency gains while keeping input (output) constant. To limit the bias which occurs when a large number of inputs and/or outputs are used relative to a limited number of decision units (small sample), estimates are based on a “two input – one output” model structure.
The model uses life expectancy at birth as a proxy of the health system’s outcomes. Life expectancy is used due to its high levels of reliability and international comparability. As for inputs, the monetary value variable (average 5-year total per capita health expenditure) is complemented by a composite indicator capturing the effects of socio-economic environment and life-style factors. The purpose of the composite variable is to control for factors that influence the outcome variable but are not directly related to the health system. As such, it includes GDP per capita, adult educational attainment, nitrogen oxide emissions and, finally, consumption of fruit and vegetables, as well as of alcohol and tobacco (all lagged by ten years). The results are broadly confirmed by a sensitivity check using GNI* per capita for Ireland.
Life expectancy is influenced by health spending and a large set of non-health determinants whose full effects are hard to control for. Hence, its use as outcome variable comes with some caveats, including largely overlooking the effects of spending on the quality-of-life dimension of care. Furthermore, DEA estimates of relative efficiency are sensitive to the choice of indicators. Therefore, these estimates should not be taken at face value, but rather as measures providing a ranking of how countries’ health systems perform in terms of broad input and output efficiency.
To limit potential issues of the frontier being defined by health systems that are not relevant for Ireland, the sample includes 17 relevant OECD benchmark countries, i.e., northern European countries, Australia, New Zealand and the United States. Estimates assume non-increasing returns to scale and apply bootstrapping to DEA efficiency scores, following Simar and Wilson (2005), in order to obtain unbiased confidence intervals around the point estimates.
To shed more light on the exact nature of the estimated potential efficiency gains, Malmquist productivity indices are computed across the 17 countries, with reference to the input efficiency dimension. By identifying changes in the frontier of best currently known input-output combinations over a specific period of time, the Malmquist index allows a decomposition of overall productivity growth (efficiency gains) into technical efficiency gains and technological improvements (Färe et al., 1993). The former captures the catching-up of each health system towards the corresponding efficiency frontier and the latter takes into account the upward shift of the efficiency frontier itself, due to technological improvements during the period considered.
Source: OECD Secretariat calculations based on Dutu and Sicari (2020).
Efficiency gains are largely driven by technological change. The Malmquist productivity index, computed with reference to the input dimension, suggests that the Irish health system registered (macro-level) productivity growth of 40% over the period from 2004 to 2019, second only to Australia’s 44% growth and more than double the average productivity growth across the other 16 countries in the sample (18%). When looking at the decomposition components, though, productivity gains in the Irish health sector result almost entirely from technological change, rather than outright technical efficiency gains. This, however, is far from being a condition peculiar to Ireland, as upward shifts in the frontier are the main driver of efficiency improvements in all the sample countries.
In contrast with other EU countries, Ireland’s population does not benefit from universal coverage of primary care. Access to public health services, on the contrary, is differentiated across groups of individuals. Families with lower incomes are eligible for the Medical Card, which entitles them to largely free primary, community and public hospital care and examinations, as well as to lower prescription charges. Medical cardholders are generally identified as “Category I” users of publicly financed health services. Enrolment in the Medical Card system, which is largely not automatic, also ensures a relatively more generous coverage of dental, optical and aural services, as well as access to an array of ancillary services (maternity and infant care, public health nursing and social work services). In addition, the package also includes some relevant non-health related benefits, including a reduced rate of the Universal Social Charge income tax, plus an exemption from school transport charges and state exam fees in public second-level schools (Citizen Information, 2021).
Entitlement to the medical card is means-tested. This explains the peak in the number of Medical Card holders at 40% of the population in 2012, when the unemployment rate surged above 14%, and the gradual decrease thereafter as the economy recovered. Medical Card holders accounted for 31.8% of the population at the end of 2020 (Department of Health, 2021a), with the highest degree of coverage concentrated at the extremes of the age distribution (Figure 2.14). Means-testing thresholds depend on age, with higher levels of allowable income applied to applicants older than 70. Duly completed on-line applications for Medical Cards are normally treated within 15 days, while a longer wait might apply for forms filed through GPs or local health offices. So-called discretionary cards may be granted to applicants with income levels above the eligibility threshold, provided their circumstances would result in financial hardship without it. They account for around 11% of the total. Overall, the Medical Card constitutes the closest approach to the application of universal health coverage principles in Ireland, albeit restricted to lower income groups and individuals with the highest healthcare needs (Keane et al., 2021). In addition, Medical Card holders are more likely to use preventive care services, such as cancer screening (Connolly and White, 2019).
GP Visit Cards, established in 2005 and entitling holders to most GP visits for free, including through the GP Out of Hours Service, add to the system’s complexity. Extended free of charge, since 2015, to children under the age of six, as well as to people aged 70 and over, eligibility for GP Visit Cards is means-tested for all other categories, with an income threshold more than 60% higher than for Medical Cards, in the case of people aged under 70 (Nolan, 2017). Moreover, assessment of the entitlement to GP Visit Cards is automatic for applicants who were found ineligible to the Medical Card. About 10.6% of the population held a GP Visit Card at the end of 2020 (Figure 2.15, Panel A; HSE, 2021a), with around 7.4% of existing cards being discretionary. The extension of eligibility to the GP Visit Card to children aged six and seven, already announced in previous budgets, was restated in Budget 2023, with a commitment to implement it by end-2022. Budget 2023 also committed to extend the GP Visit Card to individuals with earnings at or below the median income by early 2023. These measures are set to increase the population eligible for GP Visit Cards by about 420 000 individuals. Were 80% of the latter to actually take up a GP Visit Card, the benefit’s coverage rate would be pushed up to about 17% of the population. Budget 2023 also committed funding to support GP capacity.
As a percentage of the population
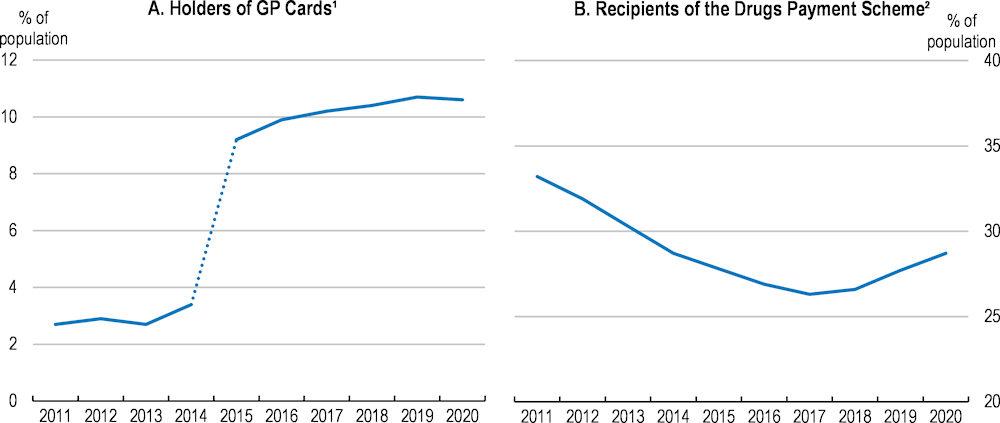
1. In 2015, eligibility was extended automatically to children under the age of six and adults aged 70 and over.
2. Under the Drug Payment Scheme, households may cap monthly out-of-pocket payments for prescribed medicines.
Source: DOH (2021a), Health in Ireland: Key Trends 2021, Department of Health.
The remainder of the population have so far been entitled to subsidised in-patient services in public hospitals (Category II users), subject to a maximum co-payment of €800 in 12 consecutive months (the standard charge for in-patient/day public services being currently at €80), although charges are not applied to maternity services and treatments involving children younger than 17 or related to infectious diseases. However, in compliance with Sláintecare’s objective to expand universal care, Budget 2023 includes the abolition of all in-patient hospital charges from 1st April 2023, which will support access to affordable acute services. Moreover, under the Drugs Payment Scheme, individuals or households regularly residing in Ireland may cap out-of-pocket monthly payments for prescribed medicines at a defined threshold (Figure 2.15, Panel B), recently lowered to €80 per household, from €114 at the beginning of 2021. At the same time, whilst non-medical cardholders enjoy access to out-patient specialist and diagnostic assessments in public hospitals without fees, provided they are backed by a GP referral, they are mostly required to pay the full cost of GP consultations – usually in the €45-65 range, as well as dental and ophthalmic treatments. Only a small fraction of these costs are covered by private health insurance, though, as the bulk of insurance plans are focused on in-patient (mainly semi-private) treatments (Health Insurance Authority, 2022). Finally, about one fifth of persons aged 15 and over did not hold any medical or GP visit card, nor any private insurance in 2021 (DOH, 2021a), and are thus subject to heavy user charges for many health care services.
In recent decades, several reforms have made way for organisational changes in the Irish healthcare system. At present, the governance of public healthcare services involves three main bodies: the Department of Health (DOH), the Health Service Executive (HSE) and the Health Information and Quality Authority (HIQA).
The key mission of the DOH is to improve the health and well-being of Ireland’s population by ensuring the required delivery of high-quality health services and the best effective use of the system’s resources. Consequently, the DOH advises the Minister and the Government on the health system’s strategic development.
Established in 2005, the HSE is tasked with the delivery of health and social care services. These services are provided either directly or by third parties under contract with the HSE (private healthcare providers, community organisations or self-employed health professionals) (Nolan, 2017; Government of Ireland, 2021; Citizens Information, 2021).
HIQA is an independent authority established in 2007 with the aim to define higher standards for health and social care services and ensure their monitoring. It is also responsible for inspecting residential services for children, older persons and people with disabilities, as well as for health technology assessments. Notwithstanding recent law proposals, and with the only exception of regulations on medical exposures to ionising radiations, HIQA does not currently have the legal remit to regulate or monitor providers of private healthcare services (Nolan, 2017; HIQA, 2021).
Current health system imbalances largely stem from spending cuts in the wake of the 2008 global financial crisis. In order to rapidly shore up public finances, the government reduced HSE’s financial envelope by 22% between 2009 and 2013 (Thomas et al., 2014), with the objective of cutting hospital beds and staff levels by more than 10%. As a result, Ireland’s health sector delivered 43% of total public sector staff cuts. Between 2008 and 2014, job reductions affected mostly support, administrative and management staff (-18.5%). Frontline staff numbers decreased by 3%, largely driven by a contraction in the number of non-specialised nurses (Williams and Thomas, 2017). In addition to staff reductions, the Government legislated across-the-board public sector pay cuts in both 2009 and 2010, via the Financial Emergency Measures in the Public Interest. At the same time, it introduced a public service moratorium on recruitment and promotions, with some exceptions, to be lifted only in 2015. Furthermore, the salaries and benefits of new entrants were reduced.
The public sector pay cuts and staff freezes have reduced the relative attractiveness of health professions in public hospitals. Due to the combined effect of the Pension Related Deduction and outright pay cuts, for instance, nurses faced salary reductions in the range of 5% to 20%, depending on their qualifications and income, as well as increased working hours since 2013 (Wells and White, 2014), which were reversed only recently. Similarly, the starting and top points of the salary scale of consultants – the most senior grade of hospital doctors – dropped by about 20% (IMO, 2017). At the same time, significant salary reductions were legislated for new hirings - from October 2012, accompanied by the lengthening of career progression scales (Public Service Pay Commission, 2018).
Although partly reversed in the recovery phase, cutbacks weighed on the system. The combined effect led to a deterioration in working conditions and mounting dissatisfaction with job quality. Salary and working conditions perceived as less favourable than in other healthcare systems have hindered recruitment and retention in the sector and contributed to outward migration among health care workers (IMO, 2017; IGEES, 2019). Unfilled consultant posts have emerged as a recurrent feature of recruitment drives, although some appear to be sector- and location-specific (HSE, 2016).
The shortage of specialists/consultants is in stark contrast to medical education in universities. In 2019, Ireland had close to 25 medical graduates per 100 000 population, 10 more than in the mid-2000s and almost twice the OECD average – the area’s record high (Figure 2.16, Panel A). In addition, Irish medical schools attract a large number of international students, who face no numerus clausus policy and accounted for about 45% of students in recent years (OECD, 2021a). However, only a limited share of these international students remain in Ireland after graduation, partly due to constrained access to postgraduate specialty training places, mostly reserved to domestic and EU students (Heffron and Socha-Dietrich, 2019). Hence, international recruitment was needed to meet domestic demand, with foreign-trained doctors making up about 41% of doctors in 2019 (Panel B), suggesting limited inflows from the large intakes of medical students in Irish medical schools. Similarly, the relative lack of postgraduate education opportunities may also help explain the system’s difficulty in retaining domestically-trained nurses (INMO, 2021), who accounted for 53% of all nurses in 2021. Recent regulatory reforms providing Irish trained non-EU doctors an equal footing as their EU peers, when applying for specialised training, and easing conditions for foreign-trained doctors’ access to visas are welcome.
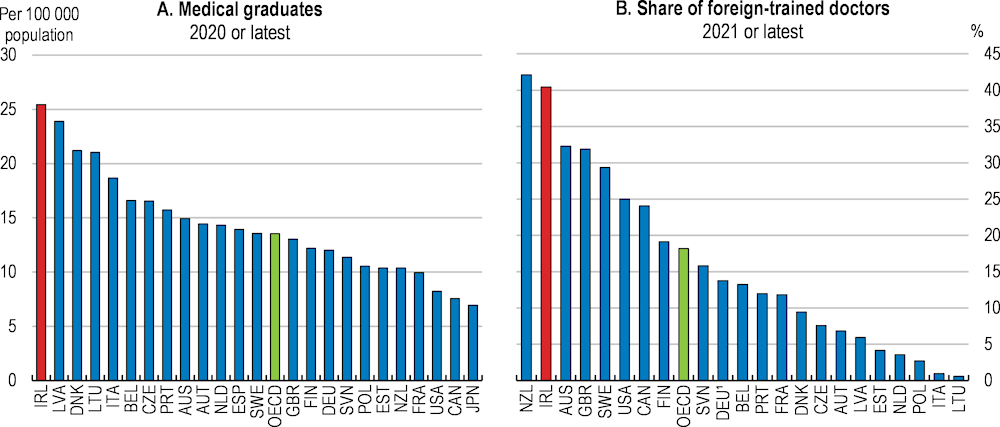
1. For Germany, data are based on nationality rather than on the place of training.
Source: OECD, Health Statistics database.
Persistent inefficiencies and unequal access to care services, in the face of relatively high spending, cemented consensus around the need for significant structural reforms in the health system. In particular, policymakers converged on the desirability of a system centred on care needs rather than on patients’ ability to pay. In 2011, the government committed to end two-tier access to hospital care and introduce universal free GP care at the point of use, which involved a shift towards compulsory universal health insurance. The proposal was abandoned in 2015 on the grounds of cost, as the system of price competition between insurers, adopted by the Netherlands in 2006 and taken as reference by the authorities, was deemed unsuitable for Ireland’s low-density and dispersed population (Connolly and Wren, 2019). However, the idea of universal health care remained central in the context of the 2016 elections. This led the ensuing coalition government to establish an all-party parliamentary committee with the aim of agreeing on a ten-year strategic plan for health reforms. The committee published its final report (Sláintecare) in May 2017, which stressed the need to establish a universal, single-tier and high-quality health system, in which patients are treated solely based on health need, while also reorienting emphasis towards primary and social care (Burke et al., 2018).
The strategy relied on a gradual expansion of health care entitlements, backed by organisational reforms and capacity building aimed at gradually shifting away from a hospital-based care model towards community-based services integrating health and social care. At the same time, emphasis was laid on fostering prevention and health promotion, as well as on e-health as a key tool to ensure more timely access to care (Box 2.2).
To ensure access to care is based on clinical need, rather than ability to pay, the Sláintecare Report also recommended dropping all user charges for GP, primary and public hospital care and reducing prescription charges for outpatients. In addition, phasing private care out of public hospitals, while empowering public-only consultants and attracting them with a newly agreed contract, was identified as a key step to achieving streamlined care services. This was seen as a way to reduce waiting lists for inpatient diagnostics and treatments. In addition, the proposed introduction of waiting time guarantees would further reinforce timely access to healthcare. On the funding side, the Report recommended anchoring financing of the targeted single-tier health system in a newly established National Health Fund, combining general taxation revenues and receipts from earmarked taxes, levies and charges – an approach broadly consistent with recent OECD analysis (Dougherty et al., 2022). This funding would support multi-year financial stability, integration of services and accountability. The multi-party Committee on the Future of Healthcare estimated the additional cost triggered by the proposed reforms at about €2.8 billion by year ten, plus €3 billion of transitional funding arrangements, over six years, aimed at making up for the country’s historical under-investment in health.
The Government launched its Sláintecare Implementation Strategy in 2018. Since then, improvements have been mainly concentrated on the organisational side, e.g., with the establishment of the Sláintecare Implementation Office, converted into a senior leadership team led by the Department of Health at end-2021, and a new independent Board for the HSE. Furthermore, a new contract enabled GPs to refer patients directly to community diagnostic services and extended their responsibility to chronic disease management, while a Sláintecare Integration Fund was set up to fund pilot projects in the area of integrated services. Progress on extending entitlements and lowering access costs, though, has been relatively limited.
The strategy adopted careful sequencing of reforms, involving the frontloading of reforms that were easier to implement and delaying more costly and contentious measures, e.g., universal access to GP/primary care or the removal of private care from public hospitals. Phasing in a set of entitlement expansions, especially when accompanied by reductions in cost barriers, could entail risks to the system’s integrity, were perverse incentives to build up and lead patients to seek care at the wrong entry point (Thomas et al., 2021). In addition, Sláintecare’s rights-based approach might represent an important step towards stronger accountability in the system. By establishing a legal entitlement to free care, as opposed to the current focus on eligibility (which depends on individual characteristics like age, means and residency), patients could appeal against those responsible for non-delivery and require corrective actions (Thomas et al., 2021).
The Oireachtas Committee on the Future of Healthcare published its final report, known as Sláintecare, in May 2017. It set out a ten-year, costed, policy roadmap to deliver systemic reform and achieve universal healthcare in Ireland. The report rested on eight fundamental principles (Table 2.1).
|
Engagement |
Create a modern, responsive, integrated public health system, comparable to other European countries, through building long-term public and political confidence in the delivery and implementation of this plan |
|
Nature of integrated care |
All care planned and provided so that the patient is paramount (ensuring appropriate care pathways and seamless transition backed-up by full patient record and information) |
|
Timely access to all health and social care according to medical need |
|
|
Care provided free at point of delivery, based entirely on clinical need |
|
|
Patients accessing care at the most appropriate, cost-effective service level with a strong focus on prevention and public health |
|
|
Enabling environment |
The health service workforce is appropriate, accountable, flexible, well-resourced, supported and valued |
|
Public money is only spent in the public interest/for the public good (ensuring value for money, integration, oversight, accountability and correct incentives) |
|
|
Accountability, effective organisational alignment and good governance are central to the organisation and functioning of the health system |
The Sláintecare Report laid out an agreed definition of universal healthcare and explicitly identified the set of healthcare entitlements that should be covered under it. It stipulated that a universal healthcare system should provide preventive, primary, curative, rehabilitative and palliative health and social care services to Ireland’s entire population, ensuring timely access to quality, effective, integrated services on the basis of clinical need. Accordingly, a range of services from health promotion, self-management and screening to rehabilitation, social, palliative and long-term care would come under the remit of universal healthcare. According to the Sláintecare report, the latter would also cover dental, ophthalmic and aural care, as well as drugs, mental healthcare and counselling. Moreover, special emphasis is laid on enhancing public health and prevention, as well as on the shift from hospital delivered care to primary and social care delivered in the community, especially with reference to the management of chronic diseases and the delivering of integrated care.
Despite significant improvements in life expectancy over the last decades, health outcomes continue to vary considerably between social, economic, regional and age groups. At the same time, a growing but rapidly ageing population would trigger increased demand for chronic disease management and other care services. The Report acknowledged that, in order to cope effectively with these challenges, health services should be delivered in an efficient, integrated manner at the lowest level of complexity, while the role of health prevention should be enhanced. Likewise, specific whole-of-government policy actions would need to address the social determinants of health, in order to reduce the inequality of health outcomes.
A significant phased expansion – backed by legislation – in the entitlements to primary and social care services, was envisaged, through the similarly phased introduction of a health card (the Cárta Sláinte), providing all residents with access to a comprehensive range of services based on need. Within a preferred model delivering the vast majority of healthcare at community level, the expansion in entitlements must be accompanied by the strengthening of the system’s capacity to deliver better and fairer access to primary, general practice and public hospital care services. To this end, the Report foresaw the gradual elimination of private care in public hospitals, alongside the removal or reduction of out-of-pocket payments from households, which may be a considerable barrier to equitable access to healthcare. The Committee estimated the additional cost triggered by the expansion in entitlements and capacity at about € 2.8 billion over ten years, excluding other likely increases due to demographic pressures and medical inflation.
Ireland’s rapid population ageing heightens the demand for a more complex set of clinical and social care services, especially in light of the growing prevalence of chronic diseases. In order to meet these needs, a new model integrating health and social care is required, in which the person is put at the centre of system design, and delivery occurs at the appropriate level of clinical complexity, within a reasonable period of time, with little if any charge at the point of access. This will be backed by newly established regional executive bodies, responsible for resource allocation and tasked with implementing integrated care services at the subnational level via enhanced coordination across the territorially relevant Hospital Groups and Community Health Organisations. Achieving effective integrated care, though, will depend on the system’s capacity to channel significant investments towards expanding diagnostic services out of hospitals. This, coupled with the imposition of time guarantees, would also help address exceedingly long waiting lists for access to essential diagnosis, treatment and elective care.
After having appraised various possible options, based also on lessons from international experience, the Sláintecare Report proposed to fund the desired single-tier health system through general taxation revenues and the earmarking of some taxes, levies or charges, all combined into a newly established single National Health Fund. The latter, as opposed to several purchasing mechanisms, would help incentivise integration of services and accountability. Over time, this would imply a diminishing role for private sector payments, as a larger share of the overall health budget would come from public, pooled resources. Moreover, in addition to the €2.8 billion expansion of the health budget over ten years, to meet the increase in spending led by the expansion in entitlements, the Report recommended the implementation of transitional funding arrangements totalling €3 billion over six years, in order to make up for the country’s historical under-investment in health. In the Committee’s proposal, these funds were meant to be deployed to enhance capital expenditure, training capacity and reinvestment into one-off system changing measures, as well as to enable a full roll-out of the eHealth strategy.
The Report’s final section included a series of provisions aimed at ensuring that the high level of political consensus attained in the Committee, concerning the need to pursue an ambitious programme to reform Ireland’s health system, is effectively carried over into implementation of its recommendations. These provisions included the request for a rapid establishment of an Implementation Office reporting directly to the Minister of Health, but placed under the authority of the Taoiseach. Adequately resourced and staffed, the Implementation Office should also set up a cabinet sub-committee tasked with the ongoing and effective monitoring and evaluation of the implementation programme.
Source: Committee on the Future of Healthcare (2017), Sláintecare Report, Houses of the Oireachtas, Dublin; Burke et al. (2018), “Sláintecare – A ten-year plan to achieve universal healthcare in Ireland”, Health Policy, Vol. 122.
Ireland’s healthcare consists of a publicly funded system, run by the HSE, and a private system that operates alongside it. Take-up of private health insurance is supported by public subsidies, in the form of a relatively sizeable tax relief. With about 46% of the population covered in 2020, private health insurance plays a prominent role in Ireland’s healthcare (Figure 2.17, Panel A). Overall, the share of the population covered by private health insurance rose only moderately from its 2014 trough, with the trend increase in take-up more evident across groups younger than 40 and older than 70 (Department of Health, 2021a). However, the coverage rate remained well below its levels in the mid-2000s, when it had peaked above 50% (Panel B; HIA, 2021).
At its core, the country’s health system is designed to provide comprehensive publicly-funded health services to low-income groups, coupled with universal public hospital coverage. Whilst open to medical and GP visit cardholders, private health insurance is thereby mainly taken out by individuals excluded from a significant part of public coverage, essentially to finance private or semi-private care provided in both public and private hospitals (Connolly and Wren, 2019; Nolan, 2017). As a consequence, over recent decades, policy-makers have supported the development of private health insurance as a way to provide greater choice over providers, while funding cost-sharing and services not covered by the public system (Colombo and Tapay, 2004). In particular, to shore up plummeting private health insurance coverage in the wake of the financial crisis (Figure 2.17, Panel B), the government introduced a tax relief equal to 20% of the cost of insurance premiums, which, in 2013, was capped at €1 000 per adult and €500 per children under 21 years of age. While the limited gains in private insurance coverage after the 2014 trough – despite the subsequent economic recovery– may justify the government’s decision to keep the tax relief in place, some form of means-testing would lower equity concerns. In 2015, a financial penalty on new policies subscribed by the over-35s was put in place, with the aim to incentivise early take-up of health insurance by younger generations.
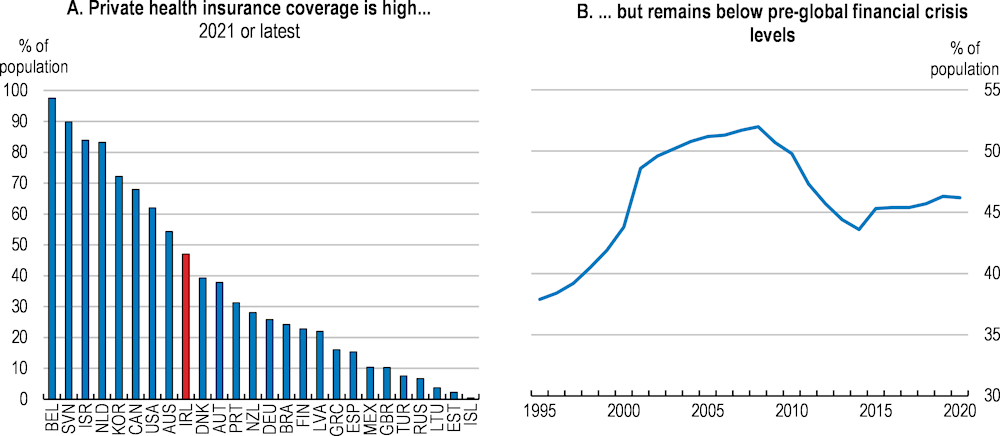
Note: Panel A only refers to voluntary private health insurance.
Source: OECD, Health Statistics database.
The peculiar role of private health insurance in the country’s health system raises equity concerns. Irish private health insurance subscribers, to a large extent, do so to acquire coverage for services that are essentially already made available in the public sector, either for free or in a highly subsidised form, but whose timely delivery is constrained by excess demand. Private health insurance ensures faster access to scheduled hospital treatments or services to people who can afford to pay for it (Turner and Smith, 2020). Besides, the duplicative nature of private insurance in Ireland is further emphasised by major private health insurers increasingly offering some limited coverage for primary care expenses. This contrasts with many other EU countries, where the role of private health insurance is largely to cover any cost sharing left after basic coverage (complementary, as in Belgium, Germany or Slovenia), or to ensure access to additional services (strictly supplementary, as in Austria and the Netherlands).
Private health insurance is thus at the core of a two-tier system in which public hospitals also provide beds and care services of a purely private nature to patients who can afford voluntary insurance coverage, thereby entailing the risk of differentiating quality in access to care based on patients’ ability to pay, rather than on their actual needs. Increased evidence of mounting barriers, affecting specific categories’ timely access to health care services, corroborates such concerns. Longer waiting lists for hospital-based and key diagnostic services weigh, in particular, on Medical Card holders (The Irish Times, 2021), while reduced take-up of primary health care, due to cost, emerged even among households in income groups well above the Medical Card’s eligibility threshold (Schneider and Devitt, 2018), and this may have deteriorated further during the pandemic. In addition, the adopted mixture of a universal public health service and a fee-based private system may lead people legitimately eligible to the benefits granted by the Medical Card to forego entitlement (Keane et al., 2021).
Rules managing entitlement to publicly-financed health services are extremely complex and limit the system’s transparency. In principle, eligibility is based on residence, but entitlement to several public health benefits is actually dependent on meeting additional criteria, including income, age and – to a more limited extent – payment of social contributions. At the same time, co-payments by Medical Card holders (for medical prescriptions), as well as some by non-medical cardholders (hospital in-patient services and the use of emergency departments if not referred there by a GP) are capped at monthly or annual amounts that vary across services. Not means-tested and with varying units of reference, either single individuals or households, these caps have often been set at lower levels for older people. In the wake of the 2008 global financial crisis, in particular, rapidly increasing user fees, imposed on non-medical cardholders for most inpatient and outpatient services, led to substantial upward revisions of annual caps on payments in 2013, which, once the economy recovered and fiscal consolidation concerns eased, were only partly reversed. Similarly, individuals aged over 70, who enjoyed automatic eligibility to the medical card since 2001, saw means testing reinstated in 2009 and a lowering of the relative income threshold four years later. Moreover, fees for some specific services (i.e., dental care or GP visits without a GP Visit Card) are not capped, which may weigh on low-income patients’ access to care. The variety of entitlement requirements and their relatively frequent adjustments create uncertainty for recipients whose income hovers around legislated eligibility thresholds, as even modest adjustments in one of the required parameters can affect their entitlement to public health benefits. At the same time, cuts in health spending and personnel lengthened waiting lists for many essential consultations and treatments, especially for Medical Card holders.
The public health system features widespread consultant involvement in private care. The characteristics of this involvement, however, depend on the type of contract held by consultants (Box 2.3). As of 2020, more than 80% of consultants held contracts allowing for some form of private practice (HSE/NDTP, 2021; Figure 2.18), a share found to be higher in public acute hospitals (IRG, 2019).
In this context, in December 2019, the Government proposed a new Sláintecare consultant contract as a key pillar to attract and retain staff via enhanced job satisfaction in the public health sector. Reserved for specialists working exclusively in the public health system, in line with current Type-A contracts, the proposed instrument is an integral part of the Sláintecare strategy to improve working conditions in public hospitals by removing private care services from their premises (HSE, 2021b). In a context of limited capacity, public hospital involvement in private care has resulted in long waiting lists for many services, creating equity concerns of access by poorer households entirely dependent on public care services. By freeing up public capacity and staffing, gradually reduced engagement in private care is expected to help move towards a need-based public health system (Independent Review Group, 2019). The restored resources, for instance, could lower bed occupancy rates or shorten waiting lists. However, the move would result in a limitation of patients’ right to choose the preferred service provider, not to mention the revenue losses faced by public hospitals.
The 2008 Consultant Contract granted public hospital consultants pay increases in exchange for higher restrictions to their private practice, with the objective – largely unattained – of increasing the number of consultants treating public patients only. While introducing a 39-hour working week, the 2008 agreement established three different types of contracts varying according to the extent of private practice allowed:
Type-A: public-only contract (consultants practising exclusively in public health services).
Type-B: consultants are free to engage in private practice on the public site or in a co-located site, but only up to 20% of their total clinical or patient output.
Type-C: consultants can also engage in off-site private practice, but private patient treatment should not exceed 20% of the consultant’s clinical workload.
These contracts have so far coexisted with more flexible alternatives, still linked to the previous 1997 Consultant Contract that allowed freer in- and off-site private practice in the context of a 37-hour working week. They include:
Type-B* contracts: extended to holders of the 1997 Consultant Contract whose public-to-private practice ratio was greater than 20%; they could retain a higher ratio under the 2008 Contract, subject to an overriding maximum of 70:30.
Old 1997 Category 1 and Category 2 contracts, with the former entitling holders only to limited off-site private practice, relative to more flexible Category 2 contracts.
Number of active consultants by type of contract, 2020
According to the Government’s first proposal, incumbent consultants will be offered the opportunity to opt into the new contractual framework, which, instead, will automatically apply to newly hired consultants. Even so, in a bid to lure more experienced health professionals into a fully public health system, the Government enhanced the new contract’s attractiveness by committing to raise pay levels to between €210 000 and €252 000 over a six-point scale. This implies a return to pre-2012 pay rates, i.e., before the wage cuts of about 30% imposed on higher-earning public sector staff in the aftermath of the 2008 crisis. Efforts have also been made in other OECD countries to improve the attractiveness of working conditions (Box 2.4).
The French authorities have recently introduced new reforms for public hospital practitioners and specialists, as a means to foster the attractiveness of public hospital medical careers. The measures built on the 2018 “Ma Santé 2022” plan, which, following long consultations involving the French Hospitals Federation, trade unions and various associations of healthcare professionals, set out a strategy to improve practitioners’ working conditions in public health venues.
The authorities merged three pre-existing categories of fixed-term contracts into the single status of contract practitioner, thereby simplifying human resource management. This was also accompanied by measures improving career support mechanisms and ensuring a better recognition of non-clinical activities within the framework of practitioners’ service obligations and their working time.
In order to respond to increased requests for new ways to deliver care, the new measures eased the conditions limiting dual practice among public hospital practitioners. This occurred in the context of public hospital doctors’ modest involvement in private practice and the absence of significant concerns over waiting lists. In particular, the minimum amount of working time for a public hospital practitioner was set at five half-days. The possibility to combine hospital employment with an off-site private activity was extended to all physicians whose public practice covers between 50% and 90% of their working time, with the only condition being to declare this activity – and its relative terms – to the employing institution. This was previously only granted to part-time practitioners with 40% to 60% public hospital time.
Similarly, while on-site private activity was formerly reserved to full-time hospital practitioners, the new rules open such opportunity to every physician with at least 80% public practice, including practitioners still in their probationary period. On-site private activities may be carried out on two separate sites within the same territorial hospital group.
Source: Ministère des Solidarités et de la Santé (2022), “Attractivités des carrières médicales à l’hôpital : l’exercice et les statuts de tous les praticiens sont réformés”.
Notwithstanding the proposed salary hikes, the new contract has so far failed to be agreed by medical representative bodies. Although in line with the policy objective to rebalance the health system towards public patients’ care by removing private care services from public hospitals, the contract’s ban on dual practice for new public sector specialists, even if partly compensated by higher pay, will add to existing contractual fragmentation during the foreseen transition phase. Additionally, the overall proposal appears to be perceived as including a strong top-down component with limited scope for flexible arrangements that are key to attract and nurture talent. In this regard, anecdotal evidence about the emigration of Irish-trained doctors to Australia in recent years suggests that their decision to leave is driven in part by the possibility over there to more easily combine clinical hours with research or management tasks, based on personal skills and interests (thejournal.ie, 2022; Humphries et al., 2019). Recent survey data suggest doctors in specialist training and fellowships – thereby still barred from private practice – have serious concerns about the proposed contract’s rigid approach with respect to patient advocacy, mobility policies, intellectual property rights and the implementation of future contract changes, which would result in reduced professional autonomy and stifled incentives for innovation (Croghan et al., 2021).
Dual practice of inpatient specialists is relatively common, but its regulation and organisation vary considerably across OECD countries. Canada is the only country not allowing public staff specialists to practice privately, whereas they are entitled to do so only outside of public hospital premises in Spain and Portugal. Dual practice is instead allowed within public hospitals – as well as outside – in Australia, France, Ireland, Italy and the United Kingdom, although with differences in the type of services provided to private patients, which may include treatments that are part of public benefit packages (Müller and Socha-Dietrich, 2020). In Ireland, as in the United Kingdom, private patients can in fact be treated alongside public patients but pay all related charges and fees themselves, either out-of-pocket or through private health insurance. Australia and France, instead, allow the public purse to partially cover the costs of private treatment. The high incidence of dual practice among Irish specialists, second only to Austria’s (Garrattini and Padula, 2018), has also had a significant impact on the financial management of public hospitals. Revenues from private practice, excluding consultant fees, have in fact grown to account for about 10% of public hospitals’ income, which helped stabilise health care provision in periods of volatile public spending (Müller and Socha-Dietrich, 2020).
The net effects from reducing dual practice in public hospitals depend on various country-specific factors, but institutional quality is likely to play a key role. On the one hand, dual practice within public care settings is often associated with conflicts of interests and competition for time, which reduce care responsiveness for public patients, distort the use of public resources and erode public trust in the health system (Ferrinho et al., 2004; Müller and Socha-Dietrich, 2020). The adoption of specific institutional arrangements and public sector governance frameworks, though, may help curtail these risks. Clearly outlined and effectively enforced public employment terms and conditions, combined with regulation enabling equal access to care for equal needs, could go a long way in balancing health workers’ incentives with the right to quality and timely care for all (Araujo et al., 2016).
On the other hand, if not accompanied by effective complementary measures to improve health professionals’ working environment, reducing dual practice opportunities in public hospitals would likely weigh on their capacity to attract more qualified physicians. The latter may thus look for jobs in the private sector or opt for practising abroad (Müller and Socha-Dietrich, 2020). The ensuing staff reductions would end up frustrating the objective to redirect freed resources towards tackling lengthy waiting lists and improving public patients’ access to care, unless the recruitment of new specialists is adequately stepped up. On the positive side, ceasing any involvement in private care services should simplify public hospitals’ administrative processes. At the same time, public hospitals might require higher public transfers to neutralise the income losses from reduced activity and preserve their financial stability.
Policy changes aimed at restricting dual practice opportunities should avoid accentuating the system’s rigidities. In light of this, close consultation with hospital practitioners and other relevant stakeholders, in both design and implementation stages, would help smooth the policy’s introduction. Moreover, approaches foreseeing the complete separation of public and private specialist practice should be complemented by regulatory changes aimed at removing any significant constraint on inter-sectoral mobility. Routine elective surgery currently represents the main operational focus of private hospitals, whereas more complex acute care is provided within public hospitals. As private practice in public settings is phased out, as planned, private hospitals may have stronger incentives to widen their range of services by investing in more advanced clinical and technological capacity. In this context, ensuring specialists can easily alternate public- and private-sector professional spells, along their entire careers would help support the enhancement of skills across the whole system.
Pressures contributing to waiting lists stem from a lack of specialists and past under-investment including in specialist diagnostic equipment. The share of generalists in the health system is comparatively large and there is room to expand hospitals’ clinical staff (Figure 2.19). In this regard, plans to expand the cadre of specialists are welcome. Similarly, ensuring Advanced Practice nurses and other specific clinical professionals may, under a consultant’s supervision or independently, assess patients that are deemed non-urgent based on referral information, could help streamline waiting lists for specialist appointments (Delamaire and Lafortune, 2010; Fennelly et al., 2018). The long period of under-investment in the health sector until recently has also resulted in a somewhat lower than average availability of some diagnostic technologies (CT scanners, MRI units and PET scanners) in comparison with other OECD countries (OECD, 2021a). However, this is being addressed and current plans include expanding elective capacity in a number of specialist units in Cork, Galway and Dublin (HSE, 2022c). These should expand the capacity for outpatient consultations to perform diagnostic procedures and some minor operations.
Some pressure stems from insufficient bed availability. Bed occupancy rates are elevated and amongst the highest in the OECD (Figure 2.5 above). Such rates are difficult to sustain and generally greater safety margins are advisable (the pressure on beds contributed to the limited capacity of the system to respond to the COVID-19 pandemic). However, elevated bed occupancy rates have been a chronic feature of acute hospitals in Ireland for some time. In part, this reflects the pressure on hospitals due to limited community care and long-term care provision providing alternative healthcare options (see below). For example, admissions of patients suffering from asthma and chronic obstructive pulmonary disorders are elevated when compared with other health systems (Figure 2.20). The pressure on beds also leads to pre-emptive blocking for patients who may have treatments scheduled after their admission date.
2021 or latest available year
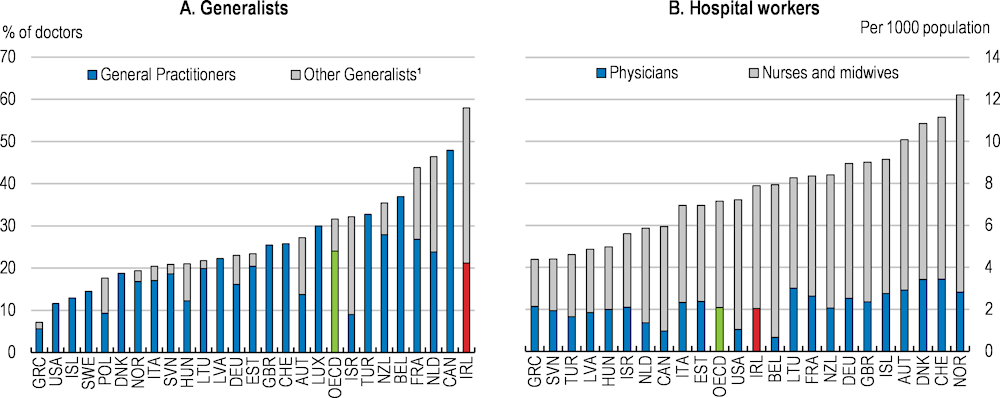
1. Includes non-specialist doctors working in hospitals and recent medical graduates who have not yet started post-graduate specialty training.
Source: OECD, Health Statistics database.
Around 400 000 outpatient appointments annually are missed due to people not attending. This is about 12% of all appointments and more than 30% above the corresponding rate in England, where more than 5 million hospital appointments annually are classified as ‘did not attend’ (NHS Quarterly Hospital Activity Data). This hinders the efforts to reduce waiting lists and complicates resource management. In some cases, it also leads to greater subsequent use of hospitals and increased mortality risk (Williamson et al., 2021). Improving existing methods of communication can reduce did not attends (DNAs). For instance, the use of behavioural science to redesign existing communications with the Better Letter Initiative had a positive impact in randomised control trials. A redesign of inpatient appointment offer letters increased confirmed intention to attend rates from 66% to 75%, and reduced DNA rates by 50% in one hospital (Murphy et al., 2020). Modifying, as intended, the technology developed during COVID-19 for vaccination and test and trace to improve bi-directional communication with patients and care givers could help reduce non-attendance. Sending SMS reminders to patients before an appointment or using electronic records to predict those patients most likely to miss appointments and contacting them in advance, appears to be effective in reducing non-attendance (Murphy and Taaffe, 2019; Valero-Bover et al., 2022). A national DNA Strategy is planned as part of the Action Plan for Waiting Lists.
Asthma and COPD hospital admissions in adults, 2010 and 2019
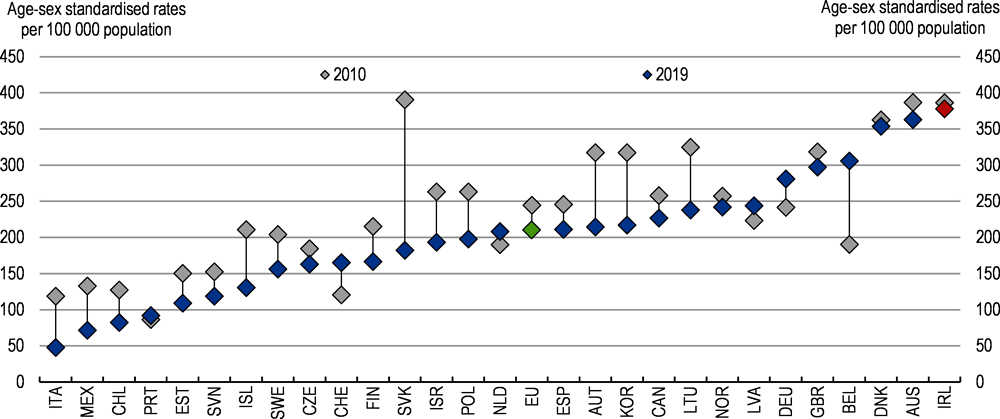
Note: The EU average is unweighted. COPD refer to chronic obstructive pulmonary disorders.
Source: OECD, Health at a Glance 2021.
Hospital overcrowding with patients spending time on trolleys has also developed alongside waiting lists. Overcrowding in emergency departments is a phenomenon in many countries. At an average of 12 hours, the waiting times in emergency departments (EDs) from registration to admission appear very long in Ireland, particularly for older patients, with hundreds each day spending time on trolleys waiting for beds to become available. Prolonged durations of stay in EDs (above six hours) are associated with poorer patient outcomes and increased mortality, while longer waiting times have adverse outcomes for discharged patients. In part, the relative underdevelopment of primary and long-term care has put pressure on hospitals (INMO, 2022). However, at 6.2 days, the average length of stay in hospital was among the lowest in the European Union in 2019 and well below the OECD average of 7.6 days, although the average time spent in hospital was comparably longer in case of diseases of the digestive and genitourinary system or neoplasms (OECD, 2021a). Pressure on emergency rooms also arises from under-provision of step-down beds, which would allow patients to move out of emergency rooms but still receive a higher level of care than in a general ward.
Previous expansions of the health sector did reduce waiting lists for a number of procedures prior to the onset of the global financial crisis in 2008 (Siciliani, Moran and Borowitz, 2014). However, expanding supply to address waiting lists can be expensive and, in some cases, induce higher demand (OECD, 2020b). OECD countries have tended to address waiting lists with a multi-pronged approach. These include setting maximum waiting times, which nonetheless need to be set in relation to what is feasible, and guarantees for patients, which may include the option to use different providers if waiting times exceed the maximum. In the United Kingdom, the waiting list maxima were gradually tightened, met partly by greater activity but also better demand management.
Ensuring adequate supply to meet demand cannot be achieved through a short-term boost to spending. Rather care is needed to identify priorities and ensure that efficiency is maximised. In some cases, a second layer of gatekeeping is helpful in preventing inappropriate or misdirected referrals clogging the system. For example, policies in Costa Rica, Finland and Poland coordinate primary and secondary care to use resources efficiently and minimise waiting lists. Finland plans specialist consultations in a primary care setting to reduce the need for unnecessary hospital referrals, particularly for patients with chronic conditions. An alternative approach, such as in Australia, New Zealand and Norway, uses clinical prioritisation to ensure that those most in need of care encounter shorter waiting lists (OECD, 2020b). Countries tend to prioritise treatments for life-threatening conditions (Siciliani, Moran and Borowitz, 2014). This is the case in Ireland, where cancer patients have fast-track pathways to care, given that delay is potentially life threatening.
A number of waiting list time targets have been set in Ireland, which are long in comparison with other OECD countries (OECD, 2020b). These include that 90% of patients wait less than 15 months for an elective procedure and that 85% of patients will be seen for their first outpatient appointment within 52 weeks. The Sláintecare implementation strategy also set waiting time targets, such as ten weeks for an outpatient appointment and 12 weeks for day and inpatient treatments. The first Waiting List Action Plan in 2021 saw some success in reducing numbers. The 2022 plan attempts to achieve further gains, allocating €350 million to increase activity, particularly initially for a number of procedures. For example, the National Treatment Purchase Fund will organise care for these procedures in the public or private sector, where prices are reasonable. Further work in the forthcoming multi-annual Waiting List Reform Programme will need to build a proper information base to monitor progress.
There is room to move some diagnosis and care from hospitals to primary and community care. The Waiting List Plan, besides funding for increased activity, also includes changes to cut waiting times in the future (HSE, 2022c). One initiative is Modernised Scheduled Care Pathways that are consistent with Sláintecare ambitions to move care out of the hospitals and into the community setting and should be implemented immediately. For example, not all patients use the most appropriate health pathways, either being referred to specialists that are not the correct ones or presenting themselves to emergency rooms to get diagnostic tests. Allowing diagnosis and care to be delivered in primary care and community care settings when appropriate (such as for minor operations) can reduce some of the pressures on waiting lists. Providing support and advice to medical professionals outside the acute hospital sector can help them direct patients to appropriate primary or community care instead of hospitals.
The COVID-19 pandemic had a severe impact on the long-term residential care sector. Nursing homes became an epicentre of contagion at the beginning of the pandemic, leading to marked increases in mortality among their residents. Nursing home deaths accounted for about 56% of Ireland’s total COVID-19-related deaths in mid-2020, one of the highest shares in Europe. However, the rate decreased to 36% in early 2022, a level below the average of European Union countries with available data (ECDC, 2022), thanks to improved infection prevention and control protocols and prioritised vaccinations (DOH, 2021b; Comas-Herrera et al., 2021). Outbreaks in residential facilities, though, led to disruptions of non-essential care and stringent visit restrictions (Rocard et al., 2021).
Overall disruptions in home care services because of COVID-19 were relatively limited, like in many other OECD countries (Rocard et al., 2021). In April 2020, the HSE temporarily suspended the provision of low-priority personal care services and referred recipients to alternative voluntary and community support. The HSE introduced detailed guidelines on infection prevention and control measures in home care settings, as well as an array of related training opportunities for home care providers, while ensuring the latter had continued access to facemasks and other appropriate PPE material. This resulted in extremely limited numbers of registered COVID-19 outbreaks in home care settings (DOH/HSE, 2021a). At the same time, a relatively low number of home care workers were redeployed to residential care services, when the policy emphasis was on preserving their essential staff capacity during pandemic peaks (DOH/HSE, 2021a).
Demand for home care support is rising. In 2019, publicly funded home-care, which is provided free of charge – up to the level of funded services, considerably exceeded the corresponding supply of services, resulting in long waiting lists (Smith et al., 2019). Mismatches between supply and demand led to untimely delivery, which, in turn, discouraged potential recipients from seeking home support and may have diverted part of demand from public towards private care provision, particularly at older ages (Figure 2.21). In addition, constrained access to home care favoured the use of residential care (Walsh and Lyons, 2021). At the regional level, lower supply of home care support correlates with longer hospital inpatient stays (Walsh et al., 2020).
In recent years, the government has increased the financing of home care services, to enhance community-based support and improve quality of life among the frail elderly (Table 2.2). In 2021, the authorities pledged to increase home support for people aged 65 or over by five million hours and committed to finalise the establishment of a new statutory scheme for the financing and regulation of home support services (Walsh and Lyons, 2021). Open to seniors who are unable to continue to live at home without support, due to illness, disability or, temporarily, following a hospital stay, the scheme – which is still under development by the Department of Health – will seek to ensure that, according to their needs, recipients can live in their own homes for as long as possible, and, thereby, reduce the number of those entering long-term residential care.
Home support receipt rates among the elderly by sex, age and type of provider; share of the population, 2019
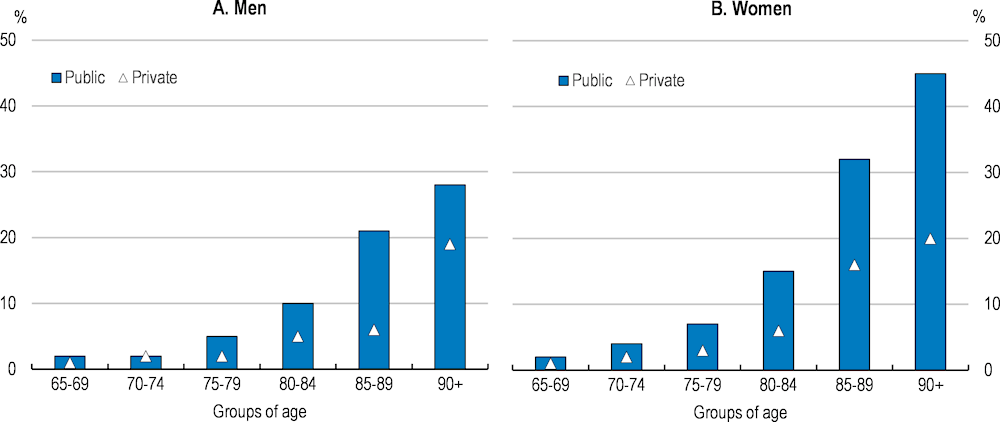
Note: Includes recipients of Home Help, Home Care Packages and Personal Care Attendant schemes; analysis based on data from TILDA Waves 2-4 Research Microdata File, collected between 2012 and 2016.
Source: Walsh and Lyons (2021), “Demand for the Statutory Home Support Scheme”, Research Series, No. 122, Economic and Social Research Institute, Dublin.
|
|
Budget (€ million) |
Home support hours (target, million hours) |
Budget (annual % increase) |
Home support hours (annual % increase) |
|---|---|---|---|---|
|
2017 |
380.4 |
16.7 |
||
|
2018 |
416.9 |
17.5 |
+9.6 |
+4.5 |
|
2019 |
445.7 |
18.3 |
+6.9 |
+4.6 |
|
2020 |
487.0 |
19.3 |
+9.3 |
+5.1 |
|
2021 |
632.0 |
24.3 |
+29.8 |
+26.0 |
|
Δ 2021-2017 |
+251.6 |
+7.6 |
+66.1 |
+45.0 |
Source: Department of Health and Health Service Executive (2021).
International studies tend to associate home care with lower societal costs, when compared with residential care (Kok et al., 2014; VanderBent and Kuchta, 2010). While home care is generally cheaper than residential care, its appropriateness and cost-effectiveness might be questioned for users requiring round the clock care and supervision or who reside in remote areas with limited access to caregiving services (Colombo et al., 2011). Evidence from a quasi-experimental study among a population of 65 years and over, eligible for permanent nursing home admission in the Netherlands, for instance, suggests that substituting nursing home care with home care might actually not save costs for patients with relatively severe medical needs. Nursing home care is expensive in the Netherlands but paid for by mandatory social insurance, which usually covers room and board costs as well. Albeit still relatively generous, social insurance coverage of home care is less pervasive because of its less structured nature. This, together with the more limited scope for economies of scale, might explain why individuals giving up nursing home care may end up using an almost equally expensive amount of home care (Bakx et al., 2020). These context-specific results, which do not consider the positive impact of home care on the individual’s well-being, echo recent OECD estimates of the average cost of long-term home care for over-65s with different levels of needs, across 24 OECD jurisdictions (OECD, 2022a). The latter highlighted that, independently from personal income levels, the total costs of long-term home care for over-65s with severe needs, measured as a share of their disposable income, were significantly higher than in the case of institutional long-term care (LTC). This is despite the overestimation of nursing home costs, which include food and accommodation, in contrast to home care costs (Figure 2.22, Panel A). Such results, however, do not seem to hold for Ireland, where the total costs associated with home care, in case of severe care needs, are well below those of institutional alternatives (Panel B), which are the sample’s second highest, after Finland’s. A review of funding for home support and its sustainability is currently in progress, which can help guide ongoing reforms.
Due to their qualitative nature, many benefits ensuing from expanded home support services are difficult to capture with standard quality-of-life metrics, which makes performing meaningful cost-effectiveness analysis more complicated (Moran and Halpin, 2021). In this context, identifying specific cost thresholds – resulting from a comprehensive assessment of the patient’s medical needs and well-being – above which a shift from home to institutional care settings may be considered could help enhance the cost effectiveness of long-term care spending (Bakx et al., 2020). Ideally, the quantification of the optimal provision of home care services should also build on a clear understanding of their implications for the health, well-being and labour supply of informal caregivers, who usually complement formal providers. In practice, however, these costs are hard to determine due to limited data availability.
Home care schemes’ cost-effectiveness partly depends on an adequate identification of needs. This would require effective integration of home care with other community-based health, long-term care and social services. Integrated funding and delivery of services, on the backdrop of combined management and information systems, would help ensure a service user moves through a continuum of care, eventually culminating with admission to long-term residential care.
The implementation of the Single Assessment Tool (SAT) at the national level would support better planning and allocation of LTC and strengthen integration across providers. SAT is a digital standardised assessment – based on the international interRAI framework – of the health and social care needs of frail older persons or people with disabilities applying for either home or nursing home support schemes (HSE, 2022d). The comprehensive assessment, which is set to replace a paper-based procedure, takes into account a broad set of information across several dimensions. These range from the individual’s (physical and mental) health status, functional performance and well-being to more detailed aspects of daily life, like medication management, physical activities, dietary habits and social interactions. Progress is already underway. The evaluation of the outcomes of four pilot projects of a reformed model of home support services – based on the use of SAT – is expected to inform the design of the new statutory home support scheme. Recruitment for 128 Care Needs Facilitator posts has commenced.
Total costs of LTC as a share of over-65s’ disposable income for different levels of needs
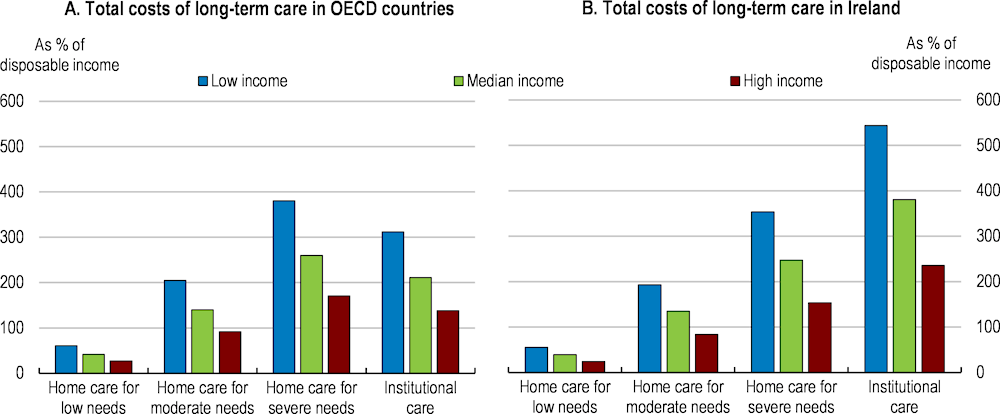
Note: OECD aggregate shows averages for 24 jurisdictions in the OECD in Panel A. Low income refers to the upper boundary of the 20th percentile, and high income to the upper boundary of the 80th percentile. Low, moderate and severe needs correspond to 6.5, 22.5 and 41.25 hours of care per week, respectively. The costs of institutional care include the provision of food and accommodation, so are overestimated relative to home care. The OECD average is computed across jurisdictions’ latest available observations (from 2016 to 2020). The reference year is 2016 for Ireland.
Source: OECD analyses based on the Long-Term Care Social Protection questionnaire and the OECD Income Distribution Database.
The implementation of the SAT at the national level should be accelerated and prioritised. Better identification of individual needs can enable better planning, effective and tailored person-centred care, improved clinical decisions, and less duplication of records. At the same time, the standardised nature of the assessment would make access to LTC support more equitable, by avoiding assessor bias (Walsh and Lyons, 2021). Moreover, when integrated with other relevant healthcare datasets or aggregated, SAT individual data could also support decision-making at the population level through more effective benchmarking and monitoring, for instance by improving screening of target priority groups.
The government has also committed to overhaul home-support regulations. Ongoing work to establish a professional licensing framework for public and private home-support providers, outline minimum license requirements and define national standards for home-support services is welcome. These regulations can also help address the sector’s skill shortages (The Irish Examiner, 2022; Houses of the Oireachtas, 2022a) by strengthening the professional status of formal home carers. The Strategic Work Advisory Group, an interdepartmental body established in March 2022 to identify challenges affecting the workforce in home-support and nursing home sectors – from recruitment and training to pay, career progression and retention – can also help.
Health care is largely funded by the public purse. Public spending for health is a “voted” expenditure in the budgetary framework that sets a ministerial ceiling as part of Ireland’s medium-term expenditure framework. In comparison with other OECD countries, spending has been relatively centralised (Beazley et al., 2019). Other revenue sources include out-of-pocket payments to general practitioners that the majority of the population face. In addition, public hospitals have been able to charge private patients.
The Irish Fiscal Advisory Council noted persistent overshooting of spending allocations in the past (IFAC, 2015). The overruns were pronounced for hospitals and primary care reimbursement services. In part, unrealistic budgetary allocations contributed to this outcome. For example, maintaining spending at existing service and staffing levels given expected inflation would cost more than budgetary allocations by some margins. As a result, inability to meet spending objectives softened the intended spending discipline of maintaining tight spending limits.
Some assessments have noted poor planning and a lack of modelling (European Commission, 2019). Furthermore, the Comptroller and Auditor General has identified problems in public procurement in the health sector, in particular non-competitive allocation of contracts. To some extent, the data needed to make better projections of health expenditure exist. For example, the Primary Care Reimbursement Service has collected pharmacy prescription claims since 1998 to track pharmaceutical spending and use. These, particularly following the recent centralisation of data processes, could feed into making better forecasts of likely spending evolutions (OECD, 2019a). Putting in place systems to prevent adverse outcomes includes establishing rules to identify malpractice and using analytical techniques to identify anomalies and predict where problems may emerge (OECD, 2017b).
In other cases, effective decision making is undermined by limitations in the governance of healthcare information systems. For example, so-called section 38 hospitals, which are funded by the HSE, have resisted providing more than aggregated data for their activities. Therefore, cost comparisons across hospitals are complicated. Furthermore, the limited take-up of digitalisation in the sector, combined with the lack of direct linkages across the existing key health-relevant datasets, make following-up of patient interventions difficult. Hence, fragmented governance frameworks, as well as lack of sufficient resources and technical capacity to process data and make them accessible across the system (Oderkirk, 2021), hamper authorities’ capability to reap the information potential of anonymised patients’ data. Finally, updated costing of Sláintecare implementation has not been fully released, making it difficult to assess progress (Casey and Carroll, 2021).
Besides financial reporting, performance budgeting can help ensure better service delivery but also creates challenges. Putting too much emphasis on financing can have adverse consequences for health care delivery. The authorities are sensitive to this risk and the HSE has implemented a Balanced Scorecard Approach to performance management since 2008 (Mesabbah and Arisha, 2016). This approach takes into account a wider set of indicators than relying solely on a financial perspective. Similarly, since 2020, a Balanced Scorecard Approach is used by the Department of Health to monitor the implementation of HSE’s national service plan and other reform measures. Overall, the national scorecard establishes key performance indicators and associated targets grouped in four sections: quality and safety; access and integration; finance, governance and compliance; and workforce (HSE, 2020). The use of available patient-level datasets to regularly report on health system performance or health care quality, however, remains limited (Oderkirk, 2021). Performance on the eve of the pandemic reveals a mixed picture with targets being met or approached in a number of areas, such as mental health services, whereas progress in meeting targets was uneven in others (industrial action affected some, such as outpatient waiting times). A lack of spending control can lead to outcomes where funds are allocated to other purposes than anticipated. In 2019, the Health Budget Oversight Group was created to monitor health spending and staffing, provide early warnings for any emerging deviation from annual budget allocations and help bring spending under control.
With the implementation of the Sláintecare reforms and the rebalancing of health care provision from hospitals to general practitioners and home care, budgets may come under pressure from unanticipated sources. As such, maintaining budgetary discipline will require strengthening oversight (see below). Learning from the recent experience will be important in that regard, but lessons from other countries may also help. Other OECD countries use performance management systems to facilitate the monitoring of the quality of service delivery, the extent to which national standards are being met, and of productivity and efficiency within the sector (Beazley et al., 2019). As reforms are implemented, they should be rigorously evaluated to ensure value for money, including through a formal spending review of all health spending.
Total public pharmaceutical spending is estimated to have amounted to €2.6 billion in 2021, up by 47% since 2014. A large majority of this spending is covered or subsidised through State pharmaceuticals arrangements administered by the DOH and the HSE. The bulk of State pharmaceuticals expenditure occurs centrally via the HSE Primary Care Reimbursement Service, which runs four separate reimbursement schemes that depend on the illness or type of drug. A remaining part is procured and paid for by hospitals and other health services. In addition, a small fraction (€80 million, according to 2020 estimates) is channelled through remaining health areas (for instance mental health). The complexity and the fact that payments are spread across different possible actors make the actual tracking of total pharmaceuticals spending complicated.
Spending performance diverged considerably across State pharmaceutical arrangements. Expenditure savings were only registered in the General Medical Scheme (GMS), which covers pharmaceutical spending of Medical Card holders, and the Drugs Payment Scheme (DPS), reimbursing households whose expenditure on drugs exceeds a given threshold. The former saw spending decreasing by 4% per annum on average between 2012 and 2020, largely driven by the fall-off in Medical Card numbers in the latter part of the 2010s, versus a 2% average decline for the latter, as a consequence of gradual increases in the expenditure threshold following the financial crisis. In contrast, the Long-Term Illness and the High-Tech Drug schemes are the arrangements registering the strongest average annual expansion in spending during that period (around 10% for both).
High-Tech Drug arrangement spending increased by 2.1 times from 2012 to 2020, from €380 million to €790 million (just under €1 billion in 2021, according to estimates). This is largely because this arrangement covers categories of medicines that treat serious, complex or chronic conditions and are associated with the larger cost increases. The rising patient headcount is an additional explanation, as it has grown at an annual average rate of 6.5% between 2012 and 2019. Moreover, the scheme is devoted to advanced medicines, which are based on technologies that are likely to remain under patent longer, resulting in higher prices due to the lack of competition.
Incentives to lower pharmaceutical prices could be strengthened. As pricing arrangements in place with industry prohibit upward adjustments, producers have incentives to set higher prices for new medicines coming to market to achieve a desired return to investment. This implies that cost pressures result from changes over time in the basket of pharmaceuticals purchased towards more expensive ones. Each medicinal product, though, is potentially subject to a downward annual price realignment based on the evolution of average ex-factory prices across 14 European comparator countries, for the same product. However, these benchmark prices are likely to be overestimated, as they may not take into account the “actual” price paid based on more favourable, but confidential, agreements. Whilst External Reference Pricing based on average pharmaceutical prices is quite common in the European Union, Italy, Spain and Hungary have moved their reference unit to the lowest price, whereas Greece, the Czech Republic and Slovakia consider an average of the lowest prices in their country baskets (Holtorf et al., 2019). Considering a similar move may help ease the price pressures weighing on Ireland’s pharmaceutical bill.
Recognizing the trade-off between ensuring fair access to healthcare and preserving the system’s sustainability, many countries have set up systems of Health Technology Assessment to determine what medical interventions should be funded through state expenditure (OECD, 2015b). In Ireland, this is carried out by the National Centre for Pharmacoeconomics (NCPE) in collaboration with the HSE Corporate Pharmaceutical Unit. While the benefits of new medications can be diverse, the NCPE establishes a standardised assessment of any new drug application based on an Incremental Cost-Effectiveness Ratio. This summary measure of cost-utility divides the incremental costs implied by the new drug, net of the estimated potential savings provided due to reduced use of healthcare resources – i.e., costly existing treatments avoided or reduced odds of hospitalisation, by a measure of the health improvement offered (incremental health effect) in terms of Quality Adjusted Life Years (“QALY”). A QALY incorporates both the additional years of life provided by a drug, and the quality of life provided during those extra years. For example, one QALY constitutes one year of life at perfect health, or two or more years of life at less than perfect health. The obtained measure of cost per QALY gained, thus, enables a comparison of the cost effectiveness of all drugs independent of the specific illness they treat (Prior et al., 2021). The NCPE recommendations are based around a threshold for cost effectiveness, in general recommending for reimburseable drugs that offer benefits of one QALY per €45 000 of spending or less (HIQA, 2020).
With the 2013 Health Act, Ireland adopted a system of reference pricing – applying common reimbursement prices to branded and generic medicines considered interchangeable – and enabled pharmacists to provide clients with a generic alternative whenever a more expensive (interchangeable) branded product was prescribed. As a result, the share of generics in the total pharmaceutical market rose to 40% in volume terms. This remains much lower than in other OECD countries (Figure 2.23), which is surprising given that part of domestic pharmaceuticals production is precisely in this segment of the market.
Enhanced competition in the off-patent drug market could increase the penetration of generics and ensure greater savings (OECD, 2020c). Currently, loss of exclusivity clauses, included in the existing industry agreement between the government and pharmaceutical producers, imposes mandatory price reductions on originator medicines (once their patent is expired) upon the launch of a non-generator alternative (Prior et al., 2021). These reductions amount to 40% of the generator’s price upon the launch of an alternative generic – 63% for the launch of a biosimilar one (IPHA, 2021), which suggests the generator drug may still remain less costly than the alternative and dominate the market despite the loss of exclusivity. The economic incentive to invest in the introduction of a new generic or biosimilar is thus significantly reduced, with negative effects on the system’s competition and productivity. However, the authorities’ capability of assessing the extent to which mandatory price reductions in generator drugs crowd out generic alternatives is hindered by limited information. Drug-level data comparing the utilisation and prices of branded medications and their generic alternatives are lacking and increased policy efforts to remedy such information gaps should be considered.
Action is being taken to strengthen the take-up of biosimilar medicines. The Department of Health has stepped up efforts in public consultation and awareness-enhancing activities to support greater biosimilar utilisation. In 2017, as part of its Acute Hospitals Drug Management Programme, the HSE adopted an operational biosimilar strategy aimed at making inroads in prescribing practices, via the introduction of targeted minimum prescribing rates and a collaborative approach with hospital pharmacists and clinical teams. This was accompanied by strong information support on the benefits of biosimilar medications, through targeted presentations to clinicians and hospitals (Prior et al., 2021). Overall, the programme led to marked increases in the prescribing rates of specific biosimilar drugs, particularly those treating rheumatoid and psoriatic arthritis, which, in their originator version, account among the costlier. The trend was further reinforced by the HSE in 2019, through the introduction of a gain-sharing system to incentivise the prescribing of identified best-value biological medicines. By the end of 2020, the new scheme had successfully widened access to biosimilar treatments for the most disabling forms of arthritis, yielding large savings relative to HSE’s corresponding spending on branded alternatives. Following official confirmation that biosimilar medicines approved in the European Union are interchangeable with their reference drug, recently released by the European Medicines Agency, the authorities could envisage legislative changes to bring the interchangeability of biosimilars on par with the current one on generics. More frequent updates of the list of interchangeable medicines managed by the Health Products Regulatory Authority can also support competition and increase the utilisation of lower cost non-originator products.
Share of generics in total pharmaceutical market, 2020 or latest available, %
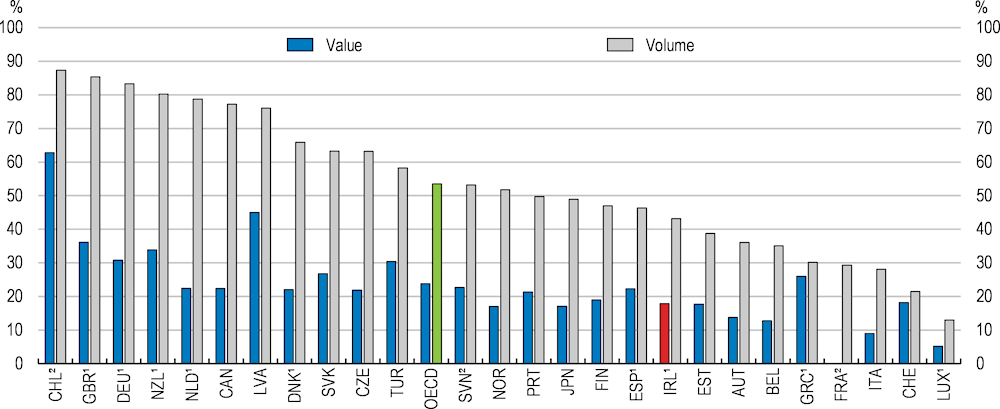
1. Reimbursed pharmaceutical market refers to the sub-market in which a third-party payer reimburses medicines.
2. Community pharmacy market.
Source: OECD, Health Statistics database.
Available international data on biosimilar alternatives for tumour necrosis factor inhibitors or erythropoietins (used, respectively, to treat a range of autoimmune disorders and anaemia) reveal a mixed picture. Biosimilars’ share in the Irish accessible market for these two types of medicines, on average, is below 25%, which is low compared to the majority of European countries and results from the relatively dominant presence of originator products with market exclusivity. Consequently, savings in drug prices following biosimilar market entry are limited, although not negligeable. Focusing on erythropoietins, Ireland achieved price reductions of 36%, well below the 76% price reductions in Portugal and Spain, obtained, respectively from biosimilar market shares of 29% and 75%, or Poland’s -61% with a 90% share of biosimilars in its accessible market (OECD, 2021a).
Ireland’s health system, as a result of the 2005 reform establishing the HSE as a single national body managing healthcare, counts among the most heavily centralised in the OECD. According to recent OECD estimates, the country’s central government accounted for about 60% of decision-making power (Figure 2.24, Panel A). The remaining 40% were accounted for by private health insurance funds and public and private service providers. Ireland’s health system stands out for its marginalisation of the country’s local authorities in decision-making processes (Panel B), although this reflects the small scale of the country and the uneven territorial distribution of its population. According to recent OECD work, across a sample of 26 member countries, a moderate degree of decentralisation is generally associated with lower public spending on health care and gains in life expectancy, but the direction of these relationships reverts when the degree of decentralisation becomes high (Dougherty et al., 2019).
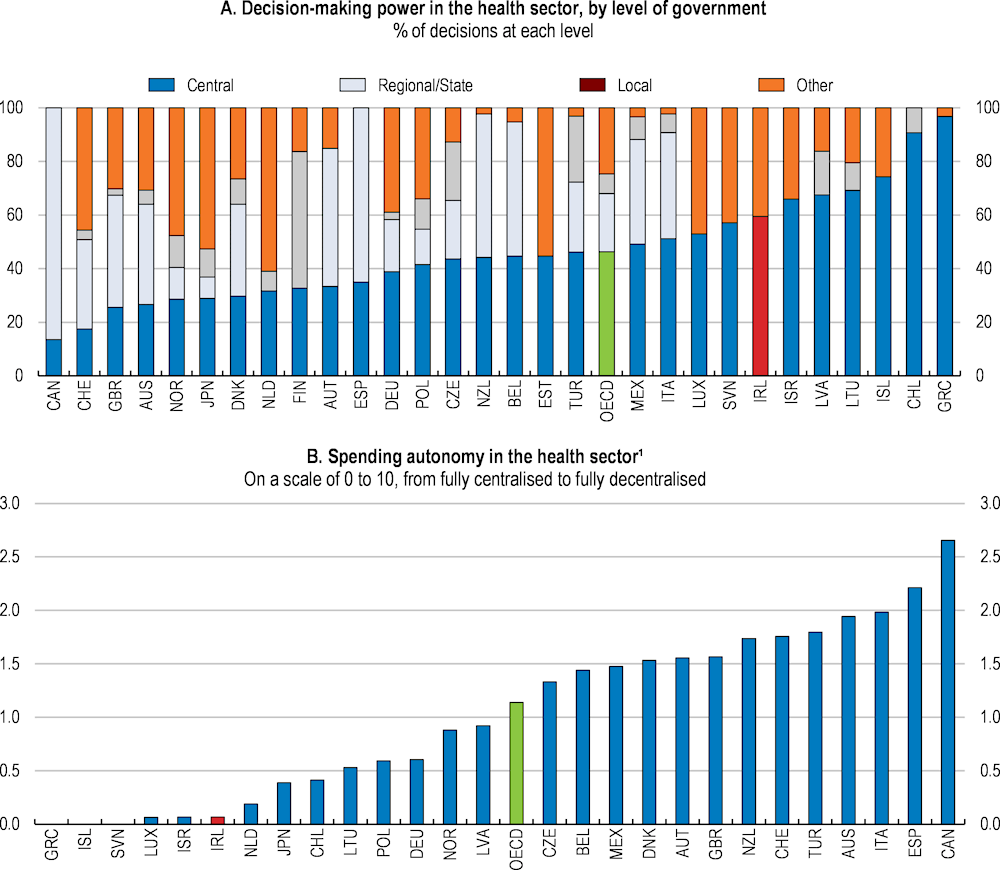
1. The spending autonomy of subnational governments measures the extent to which subnational entities exert influence over rules and regulations in different policy areas and whether they are free from constraints imposed by upper-level governments. Spending autonomy is considered across four different categories of rules and regulations: policy, budget, inputs and output and monitoring autonomy.
Source: OECD (2022), Fiscal Federalism 2022: Making Decentralisation Work, OECD Publishing, Paris; OECD (2022), OECD Fiscal Decentralisation Statistics (database).
Notwithstanding the centralised nature of the system, governance structures are fragmented and hamper the strategic planning of healthcare service delivery. There are 16 delivery structures operating independently (six Hospital Groups, nine Community Health Organisations plus Children’s Health Ireland) with no overlap in management and clinical oversight. Furthermore, Hospital Groups and Community Health Organisations serve different populations and are not geographically aligned, while there is no management structure that oversees the budget process at a specific territorial area. In addition, the funding system is siloed across particular care settings, which reduces the system’s transparency and limits the traceability of spending.
The current system of service delivery has addressed governance and funding in acute and community care separately. This led to multiple management layers, differentiated corporate, accounting and IT systems and, thereby, diluted accountability settings and fragmented care for patients when they move between primary, community and acute care venues (HSE, 2022a). Moreover, rather than being linked to key outcomes for defined populations, the type and level of health and social care services, as well as the relative budgetary allocations, were decided by the HSE based on service providers’ proposals. Such institutional settings were unfit to deliver on the key Sláintecare objective of putting in place a patient-centric, community-first model of integrated health and social care service delivery.
The creation of six new Regional Health Areas (RHAs) is a key step to deliver decentralised integrated care. Having approved RHAs’ geography in 2019, the Government recently agreed on a preferred geographically-based model to regionalise service delivery (DOH, 2022). Set to be operational by early 2024, each RHA will be endowed with an annual budget via a Population-Based Resource Allocation (PBRA) funding model, with an executive manager directly accountable to the HSE board. These new regional units will take on responsibility for delivering integrated (physical and mental) health and social care services, gradually replacing the current network (HSE, 2022a). Tasked with planning, funding, managing and delivering integrated and patient-centred care based on local population needs, RHAs will empower community-level decision making and local ownership. They should also facilitate more cost-effective access to health and social care services closer to patients’ home (DOH, 2022).
Linking the creation of Regional Health Areas to the adoption of a PBRA funding model could significantly enhance the efficiency of public healthcare spending. By distributing healthcare resources in ways that reflect the specific needs of varying population profiles, rather than based on the requests from different categories of providers as is currently the case, PBRA will enable better service planning, while promoting equity in health outcomes and more effective resource allocation (McCarthy et al., 2022). Moreover, on the back of RHAs’ clearly defined responsibility for delivering integrated care services to their citizens, PBRA will support enhanced accountability. This will pave the way for stronger incentives to improve corporate governance and the system’s transparency, allowing for better spending traceability and more meaningful assessments of its effectiveness.
The adoption of a PBRA funding model in Ireland is currently hampered by the limited coverage of the unique health identifier and by the technical difficulty – due to data unavailability – to match the utilisation of health services, as well as their costs, to specific characteristics of the population, i.e. individual socioeconomic status (McCarthy et al., 2022). Hence, the adoption of a unique health identifier should be prioritised, while greater linkages between national healthcare datasets are pursued. However, custodians of Irish personal health datasets make limited use of treatments for variables that pose a risk of re-identification, nor is systematic de-identification of datasets before analysis reported (Oderkirk, 2021). This poses risks to data confidentiality and may erode patients’ trust in digital solutions, which is needed for them to agree with the processing of their personal data. This should be complemented by a legislated national data governance framework, as is currently under discussion in the Health Information Bill.
Centralising the governance and appropriate national health information functions in a single, independent body could ensure greater data protection and support confidence. The new institution could be responsible for linkage and de-identification services across available health data collections and act as their single custodian (HIQA, 2022). The new entity should take a lead role in the implementation of a national data governance framework, outlining the conditions for data collection, secondary use and secured sharing in an anonymised form. Extending the possibility of sharing health information with eligible private and not-for-profit research services, currently precluded, would be welcome, as it may enhance the potential to utilise data for evidence-based policy-making.
Devolved responsibilities to the newly established regional bodies will take place within a highly centralised national governance framework. HSE’s annual National Service Plans (NSP), which set service priorities, will continue to drive healthcare planning and resource allocation across the system. Though the ways in which new NSP drafts will take account of the reformed governance framework is currently under discussion, it is expected that each RHA will assume responsibility for their implementation at the regional level. Based on information currently available, to ensure economies of scale and effective resource utilisation, the national HSE is expected to centralise the main corporate functions, such as finance control, human resources and IT support. HSE will also remain the contracting body for the procurement of all goods, services and capital inputs required by the national delivery of health services, as RHAs’ legal status will not allow them to enter into contracts in their own right. Clinical models of care and clinical pathways, to be applied across the country, will continue to be set at the national level. The government pledged to test a shadow budget cycle in 2023 (Houses of the Oireachtas, 2022b).
Through the Enhanced Community Care programme, the Government has provided a framework involving all service providers delivering care within communities. The programme, funded with more than €200 million over 2020-22, aims to foster the provision of decentralised primary care. This will help to reduce the risks of hospital admission and relieve the pressure on acute hospitals (DOH, 2021c). The build-up of local care capacity, in particular, was pursued by breaking down the newly established RHAs into 96 Community Healthcare Networks (CHN), in line with the approach previously adopted with Community Health Organisations (Committee on the Future of Healthcare, 2017). Defined, as much as possible, according to county boundaries, each network is set to deliver primary care services to an average population of about 50 000. These usually include professional services by occupational, speech and language therapists, physiotherapists, podiatrists, and dieticians, as well as social workers. In addition, since service delivery must occur in strict cooperation with GPs, a leading general practitioner is designated in each Community Healthcare Network, with the task of coordinating and representing GPs at the network level. This approach, based on multi-disciplinary teams, helps bring decision-making closer to the point of care. Moreover, it makes the networks key institutional structures enabling more integrated end-to-end care pathways (HSE, 2022a). Out of the total 96, as of end-2021, among pandemic-related disruptions, only 39 CHNs have been properly established and possess an appointed manager, with about 25% of staff already recruited, as full roll-out is set to be completed by end 2022.
Other initiatives, such as the Community Interventions Teams and Community Specialist Hubs, tailor appropriate care for patients with acute or chronic conditions with the aim of reducing visits to emergency departments and hospital admissions, as well as facilitating easier discharge from hospitals. In acute cases, interventions would occur mainly at home, while for chronic conditions, emphasis would be given to preventative measures. These initiatives are being supported by the planned creation of 3 500 new job positions over the 2021-22 biennium (HSE, 2022a).
Reforms have put GPs at the centre of community-based primary care. A 2019 joint agreement assigned to GPs who opted in an active role in chronic disease management for eligible patients aged 75 and over, which was later extended to patients older than 70 in response to the COVID-19 pandemic (HSE, 2022e). Since January 2022, these GPs may also develop a care plan for adult patients diagnosed with a chronic condition and who hold a Medical or a GP Visit Card. In addition, GPs can refer eligible patients, aged at least 65, to chronic disease management treatment or prevention programmes, based on specific risk criteria. This referral is based on a suite of tests offered to ‘at risk’ patients to identify those with an undiagnosed chronic disease or at high risk of developing it (HSE, 2022e).
GPs can also refer patients to community-level mental health counselling services and specialists. Although about one fifth of GP consultations pertain to mental ill-health symptoms (ICGP, 2021), they mostly consist of mild-to-moderate anxiety and depression. These can usually be alleviated through lifestyle advice and follow-up at practice level, based on the GPs’ stronger knowledge of the patients’ background, reducing overreliance on mental health medication services. However, continued provision of training is key to ensure that GPs possess the mental health competencies required to accurately evaluate and diagnose patients (OECD, 2021c).
GPs’ role in Ireland’s health system, as both gatekeepers and central actors in preventive care, has been further strengthened by new measures enhancing their direct and timely access to diagnostics. At the height of the pandemic, GP direct referral to diagnostics was extended to the whole population, but is currently limited to adult patients with a medical or GP card. Direct access to diagnostics allows GPs to treat patients who would otherwise have been referred to outpatient hospital departments and, at the same time, reduces waiting times from testing to treatment (Roland et al., 2006; Sibbald, 2009). While this potentially risks increased incidence of inappropriate referrals, international evidence suggests the risk is relatively low and no significant differences in the use of diagnostics between GPs and hospital specialists are observed (O’Riordan et al., 2013). Moreover, a significant proportion of GP investigations were found on the whole to reduce outpatient referrals (Winpenny et al., 2016). Nonetheless, easier access to diagnostics may boost demand. Evidence suggests that protocols to regulate the use of tests and onward referral procedures strongly influences the effectiveness of care pathways (Williams et al., 2007). Systematic use of locally agreed protocols, to be followed by GPs and other actors in order to decide whether specific tests are required and how to access them, would help rationalise the use of existing diagnostic facilities, limit the risk of excessive take up and support effective planning.
Effectively integrated care services at the point of delivery will require successful coordination across different care providers. The new governance should ensure RHAs have an adequate degree of autonomy to fine tune service delivery, as well as its operational organisation, based on their specific population needs. The new Health System Performance Assessment will improve measurement, monitoring and reporting processes. It will thus enable a better understanding of health policy performance. Shifting towards a measurable and quantifiable outcome-based model, and away from the current activity-based indicators, the new tool will significantly support better evidence-based health policy decisions, particularly if increasingly underpinned by more coherently linked datasets. At the same time, policy-makers should avoid ‘locking’ RHAs strictly into common performance patterns. Namely, the outcome-based indicators should not be turned into specific, quantitative policy objectives to be met by all regional bodies, as this would stifle local policy innovation.
Cancer is a leading cause of deaths in Ireland, accounting for around 32% of the total in 2019. This was three percentage points higher than mortality due to circulatory diseases and 6 percentage points above the corresponding EU average in 2017 (Figure 2.25). Due to greater prevalence of risk factors, e.g., smoking and alcohol consumption, men were slightly overrepresented in cancer-related casualties (53%), while individuals older than 65 accounted for close to 80% of the total. Gastrointestinal, as well as respiratory and thoracic, represented the types of cancer associated with the highest number of deaths, accounting for 9% and 6% of total deaths, respectively (Matthews et al., 2021). While the number of deaths caused by cancer has increased by 6% since 2013, the standardised mortality rate, which adjusts for population increase and ageing, decreased over the same period. This occurred on the backdrop of significant improvements, over the past 20 years, in age-standardised five-year net survival rates across almost all types of cancer (Figure 2.26). This reflected more effective treatment for specific cancers but, to some extent, also increased predominance of those with more favourable prognoses (NCRI, 2021).
Main causes of mortality as a percentage of all deaths
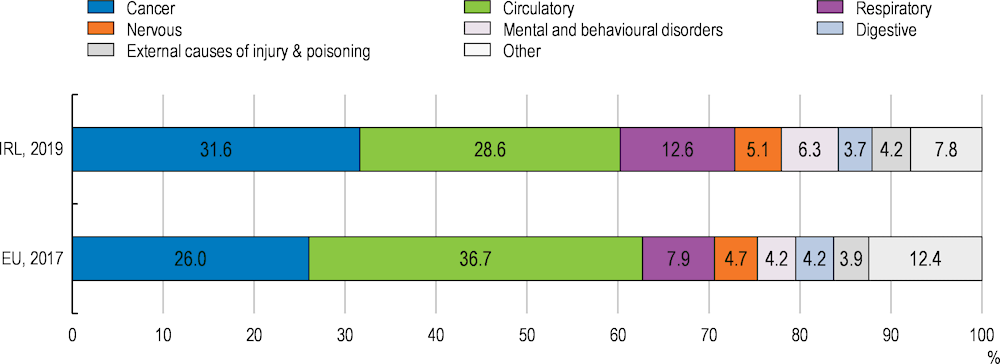
Source: Eurostat (2022), "Causes of death - Deaths by country of residence and occurrence - Table HLTH_CD_ARO", Eurostat database.
Age-standardised 5-year net survival, 2014-2018 diagnosis period
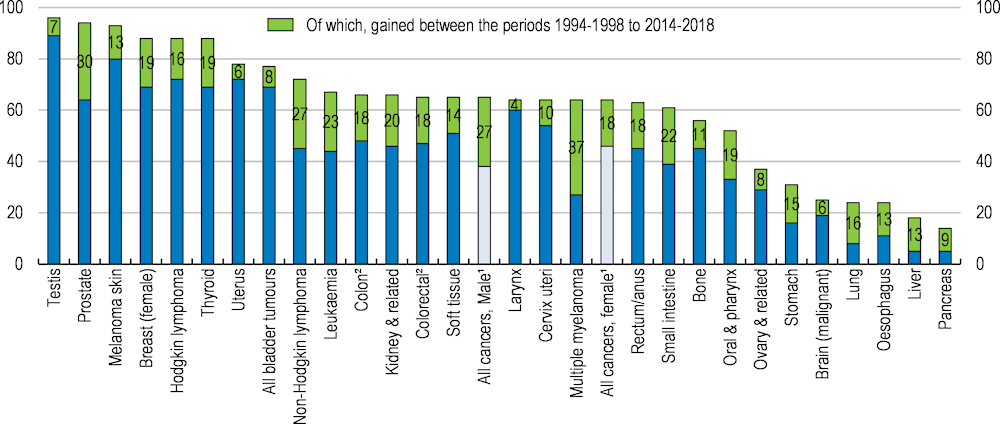
1. Excluding non-melanoma skin cancer.
2. Excluding carcinoid tumours of appendix.
Source: National Cancer Registry Ireland, Annual Report 2021.
Cancer prevention and care will be important priority areas. Projections produced shortly before the COVID-19 pandemic implied the country’s age-standardised cancer incidence rate would become one of the highest in the European Union by 2020 (OECD, 2021a; OECD/EU, 2021). Calculations made in 2019 by the National Cancer Registry and applying the average rates of cancer by age cohort during the 2011-15 period to official national population projections, suggested that, based on demographics alone (population growth and ageing), the annual number of diagnosed invasive cancers would double between 2015 and 2045. Gains in treatment efficiency in line with historical trends, however, could limit the projected demographic-driven surge to 50% by reducing the individual relative risk of morbidity (NCRI, 2019).
The indirect effects of COVID-19 on cancer diagnosis and treatment could worsen the trend. Cancer services struggled to meet demand already prior to the pandemic, due to underfunding. The Government, though, reacted promptly to the outbreak of COVID-19 by allocating €92 million to cancer services in 2020-21, partly to support the continued implementation of the National Cancer Strategy 2017-2026, as well as by prioritising continued delivery of cancer care throughout the pandemic. Moreover, it temporarily relocated some cancer services to private facilities. Even so, the number of patients referred by GPs to Cancer Rapid Access Clinics decreased markedly following the first introduction of sanitary restrictions, while national cancer screening programmes were all paused in March 2020 and only resumed in the second half of the year, on a phased basis (DoH/HSE/NCCP, 2020). At the same time, physical distancing requirements and infection prevention and control measures limited diagnostic and treatment capacity, even though organisational changes and adaptive behaviour helped smooth these effects over successive waves of COVID-19.
Population growth, together with more effective diagnostics and treatments, also resulted in a growing number of cancer survivors. The latter, including all individuals living through or after cancer treatment, accounted for about 4% of the Irish population as of end 2019 (NCRI, 2021; NCRI, 2019). While early diagnostics and better treatments have increasingly enabled a part of cancer survivors to resume work (Kennedy et al., 2007), longer cancer survivorships may nonetheless pose serious challenges to the sustainability of health systems. Needs for cancer treatment, financial support and ongoing diagnostics will consequently expand over time and further add to ageing-related fiscal pressures. In this context, calculations made in Mariotto et al. (2020), with reference to the United States, might help illustrate the possible magnitude of the fiscal costs related to improved and prolonged cancer survivorship, with the overall outlays for medical services and prescription drugs, delivered to cancer survivors, accounting for over 5% of national health spending in 2015 (slightly above 1% of GDP).
Adequate planning should ensure rising demand for long-term support and follow-up solutions to the specific needs of cancer survivors is met in a cost-effective way. The complex and multidimensional nature of survivors’ needs, which may involve physical, psychological, social and financial issues, makes establishing effective cancer survivorship programmes particularly cumbersome (O’Connor et al., 2019). Flexible but comprehensive policy approaches are thus required to enable rapid tailored support based on cancer and treatment type, while enhanced integration between health and social services would ensure significant efficiency gains. Developing and promoting effective survivorship care patterns has become an official government objective in 2017, with the launch of the ten-year National Cancer Strategy. In line with the Sláintecare health strategy, the plan outlined a greater role for primary care in the delivery of survivorship care, which heretofore was mainly concentrated in public hospitals (DOH, 2017a). In addition, in 2020, the National Cancer Control Programme developed a set of guidelines to support hospital and community-based care centres in the delivery of psychosocial care to patients with cancer and their families (NCCP, 2020).
While many cancer survivors gradually renew with normal living conditions after successful treatment, a good number of them are faced with physical and psychological impairments limiting their quality of life and ability to engage in working or other activities. The latter are estimated to account for about one quarter of cancer survivors in Ireland, with poorer and older individuals, especially those living alone, among the most heavily affected (DOH, 2017a). Side effects of cancer may emerge several months or even years after treatment. They vary in prevalence and severity, depending on the type of cancer, stage of the disease, treatment received and other factors related to patient profiles (ACS, 2021). In a similar context, further complicated by the risk of recurrence, adequate survivorship programmes should provide tailored and integrated assistance along both the short- and long-term effects of cancer and its treatments (O’Connor et al., 2019). In order to ensure the best possible quality of life for cancer survivors and their families, these programmes should effectively combine health care with psychosocial and financial support, especially when cancer is treated as a chronic disease. Enhanced efforts to link population-based cancer registry data with health relevant information on patients’ quality of life, or patient-reported outcomes (Smith et al., 2016), would help improve monitoring and surveillance of the long-term and late effects of cancer while strengthening the effectiveness of survivorship programmes.
When working-age cancer survivors resume employment, they are likely to work fewer hours than at the time of diagnosis, face higher risks of unemployment and weaker career prospects (Hanley et al., 2013; Rottenberg et al., 2016; de Boer et al., 2020). Recent survey evidence suggested that, over a sample of Irish cancer survivors having returned to formal employment in the past ten years following a cancer diagnosis (with a median 26 weeks of related leave), about 40% judged their leave period too short. Among these, half indicated financial need as the main driver of their return to work (Connolly et al., 2021), consistent with evidence of sizeable out-of-pocket payments and financial stress among cancer survivors in Ireland (O’Ceilleachair et al., 2017; Hanley et al., 2018). Premature reinsertion in the working environment, though, could result in undue stress to perform for cancer survivors. Possible difficulties encountered in accomplishing working tasks could affect their psychological balance and strengthen incentives to leave the labour market, heightening the risk of higher social costs.
Measures facilitating a more gradual and flexible return to full-time employment could help limit the risk of cancer survivors’ permanent detachment from the labour market. In line with Irish Cancer Society’s proposals, the establishment of occupational health support programmes for SMEs and the self-employed could complement these measures. While the introduction of a new statutory sick pay scheme by January 2023 will be an important improvement, coverage of sick pay leave will likely remain relatively weak among employees of SMEs and self-employed workers, for whom pressures to (re)take up work are stronger. In such a context, cancer patients could face undue financial hardship upon diagnosis and until the end of their treatment, which could be eased by extending eligibility to Medical Cards/GP Visit Cards on a discretionary basis. To increase uptake, transparency should be increased and complexity in the awarding of cards should be reduced. This would help those belonging to the population groups and cancer types covered by public free care programmes to avoid foregoing screening and diagnostics that may enable early treatment in the case of cancer recurrence, due to prohibitive costs, and thereby ensure higher survival.
Behavioural risk factors, such as smoking and alcohol consumption, were linked to more than 35% of all deaths in Ireland in 2019. Limiting the incidence of these risk factors would help improve societal welfare, by enabling larger savings on public spending and stronger productivity outturns, thanks to reduced chronic diseases. Though smoking continued to represent a major contributor to mortality (OECD/EU, 2021), Ireland halved adult smoking rates to levels well below the OECD average by 2019 (Figure 2.27), on the back of a comprehensive policy strategy supported by strong tobacco taxation and pricing policies, aimed at reducing smoking rates to less than 5% by 2025 (HSE, 2018). Moreover, the incidence of smoking among people aged 15 became relatively limited in recent years, though it increased somewhat in 2019, following the diffusion of e-cigarettes (OECD, 2021a).
High levels of alcohol consumption in the population pose serious policy challenges. In 2019, Ireland’s adults aged 15 and over, on average, consumed 10.8 litres of pure alcohol per capita, an amount matching the series’ long-term average since 1970 and 2.1 litres above the average OECD country. Besides, over one fifth of Irish adults reported regular heavy alcohol consumption (one half among men), while episodes of drunkenness appeared more limited among 15-year-olds relative to their European peers (OECD/EU, 2021; OECD, 2021b). Harmful alcohol consumption contributes to chronic diseases like cirrhosis, diabetes, cardiovascular disease (CVD) and cancer, and causes injuries and premature deaths. Such alcohol-related diseases have wider detrimental societal consequences that emerge through four main channels: higher health spending, shortened life expectancy, reduced labour market participation and lower productivity.
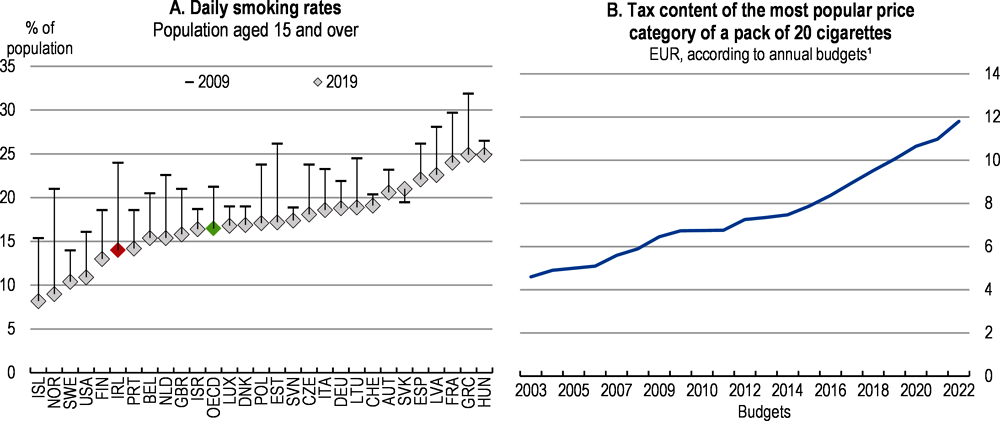
1. Including the April 2009 emergency budget.
Source: OECD, Health Statistics database; HSE (2018), "The State of Tobacco Control in Ireland: HSE Tobacco Free Ireland Programme 2018", Health Service Executive, Dublin.
Recent OECD research based on the OECD Strategic Planning for Public Health for NCDs model and the OECD long-term economic model tried to shed light on the combined long-term impact of diseases caused by alcohol consumption. Based on simulations for the period 2020-50 across a sample of 52 countries, OECD (2021d) estimated that daily alcohol per capita consumption of 12 grammes for women and 18 grammes for men, respectively equivalent to 1 and 1.5 standard drinks, accounted for 88% of all cases of dependence and 37% of all cases of cirrhosis over the period considered. The results also highlighted that daily alcohol consumption above the identified caps could result in a significant deterioration of population health at the end of the period, amounting to a 1.1 year loss of Healthy Life Expectancy (HALE) for an average individual in OECD countries, versus a 1.2 year loss for an Irish individual on average. The ensuing higher morbidity would result in lower labour market participation and increased public spending on health care. At the same time, the financing requirements to cover the higher spending on medical treatments for alcohol related diseases, over the reference period, were projected to raise the overall annual tax rate, measured as the increase in government primary revenue (as a percentage of GDP) needed to stabilise the public debt ratio, by 0.6 percentage points in Ireland at the end of the projection horizon, against 0.4 percentage points for the OECD. Although affected by considerable limitations and uncertainties, these estimates suggest significant scope for scaling up efforts aimed at curbing the damaging consequences of alcohol consumption.
Earlier OECD work concluded that the most effective and cost-efficient response to harmful alcohol consumption consisted into a multi-pronged strategy combining measures around four main dimensions: regulating alcohol advertising – in a bid to prevent underage drinking; tackling alcohol related violence and traffic injuries; providing primary care counselling and treatment for alcohol dependence; and taxing and pricing to reduce the affordability of alcohol (OECD, 2015b). Simulations in OECD (2021d) suggested how a similar package, augmented with more innovative measures like minimum unit pricing and tighter statutory bans on alcohol advertising targeting children, could ensure large gains in life years in Ireland (and most other OECD countries), as well as significant savings in health expenditure and labour market costs, owing to reduced incidence of chronic diseases. While involving sizeable costs, such measures were projected to yield the highest returns on investment, relative to alternative packages focused mainly on restricting alcohol availability.
Ireland enacted its national alcohol prevention strategy, the Public Health Alcohol Act, in October 2018, with the aim of drastically reducing the damage deriving from society’s excessive exposure to harmful alcohol consumption, especially among children and younger people. The Act included a set of policy measures broadly in line with OECD recommendations, as they provided for the introduction of a minimum unit price and labelling requirements on alcohol products, as well as for tightened structural separation of alcohol sale in mixed retail outlets and restrictive regulations of alcohol marketing. New rules, gradually phased in in recent years, prohibited advertising of alcohol products near schools or, among others, in public parks, transport and stations, as well as in sports events involving a large participation of children (DOH/HES, 2019). Promotions involving the sale or supply of alcohol at a reduced price or free of charge were banned, as was the possibility, for retailers, to award loyalty card points on purchases of alcohol. At the same time, alcohol companies’ opportunities to sponsorship events were significantly restricted (DOH/HES, 2021b).
Tightening of the laws against alcohol-impaired driving complemented the set of prevention policies outlined in the Alcohol Act. This included mandatory disqualification and a significant increase in the fine for a first drink-driving offence, were the motorist to have blood alcohol concentration above 50 mg/100 ml (O’Dwyer et al., 2021). The move should help reduce the negative externalities of drunk-driving, in a context in which driving under the influence of alcohol is a relatively common practice, especially among younger male individuals (RSA, 2021). Intoxicated driving is a major factor in serious road injury and fatal collisions. Evidence based on data from closed coronial cases revealed that between 2013 and 2017, about 37% of road user fatalities were related to alcohol use, with over half of the fatalities in the 15-34 year group (RSA, 2020).
Increased alcohol affordability gave price regulation a key role in the authorities’ toolkit to reduce the burden of alcohol-related harm. Over recent decades, Ireland saw alcohol consumption moving away from the on-trade sector, with the number of pub licenses declining by more than one fifth between 1998 and 2018, while off-premise wine and spirit licenses increased fourfold (O’Dwyer et al., 2021). This contributed, since 2000, to a marked surge in alcohol affordability in the off-premise sector, relative to the OECD average, driven by rising real incomes as well as cheaper alcohol prices (OECD, 2021d). In addition, alcohol became particularly affordable for Irish young people after 2013, once the economic recovery led to renewed gains in household income. Under such circumstances, the government prioritised increases in the price of cheaper alcohol products, the ones more likely to be consumed by heavy and younger drinkers and, thereby, associated with larger negative externalities. With limited room for further tax increases, because of excise and VAT rates on alcohol beverages already among the highest in the EU (OECD, 2020d), the 2018 Alcohol Act opted for setting a €0.1 minimum price per gramme of alcohol, in order to make the cheapest alcoholic beverages significantly less affordable. The measure, however, became effective only at the beginning of 2022.
Empirical evidence on minimum unit pricing adoption in OECD countries seems to confirm rapid reductions in the consumption of targeted alcohol beverages after the measure’s introduction (Table 2.3). As for Ireland, simulations commissioned by the Department of Health, early in the process, to model the impact on alcohol consumption of a €1 minimum price per standard drink, estimated an 8.8% reduction for the total population, against a 15.1% drop in alcohol consumption in the case of high-risk drinkers (Angus et al., 2014). International evidence also found the adoption to be accompanied by reductions in emergency department admissions (Sherk et al., 2018), alcohol-related assault offences, protective custody episodes and road traffic crashes resulting in fatalities or injuries (Coomber et al., 2020). Moreover, policy-induced increases in the price of alcoholic beverages have been associated with lower rates of alcohol dependence (Henderson et al., 2004) and reduced alcohol-related morbidity and mortality (Wagenaar et al., 2010; Zhao et al., 2013; Anderson et al., 2009), though health gains from the policy are unequally distributed among socioeconomic groups (Holmes et al., 2014).
Selected studies
|
Studies |
Country of introduction |
Date of introduction |
Minimum unit price |
Variation in off-trade alcohol consumption since date of introduction |
|---|---|---|---|---|
|
Anderson et al. (2021) |
Scotland |
May 2018 |
0.5 GBP per standard unit of pure alcohol (8g) |
-7.6%¹ (after seven months) |
|
Anderson et al. (2021) |
Wales |
March 2020 |
0.5 GBP per standard unit of pure alcohol (8g) |
-8.6% (after ten months) |
|
Taylor et al. (2021) |
Northern Territory, Australia |
October 2018 |
AUD 1.30 per standard unit of pure alcohol (10g) |
-51% for cheap cask wine -21% for total wine (after 12 months) |
|
Stockwell et al. (2012) |
Saskatchewan Province, Canada² |
April 2010³ |
Ranging from CAD 1.16 to 1.89 by beverage type and alcohol strength Per standard unit of alcohol (17.05 ml ethanol) |
-9.2% (for a 10% increase in the minimum price of all beverages, after 24 months) |
1. Estimates from Anderson et al. (2021) revealed that similar reductions were maintained in 2020, relative to 2018.
2. MUPs on alcohol are set by the Saskatchewan Liquor and Gaming Authority (SLGA), which has a monopoly on alcohol distribution and a partial monopoly on the sale of alcohol in liquor stores. Minimum prices apply directly to liquor store retail prices and also to the prices at which SLGA sells alcohol to bar and restaurants, hence, they indirectly on-trade retail prices, although to a smaller degree.
3. Date at which SLGA introduced a comprehensive set of new and increased minimum prices. The latter were originally introduced for spirits other than brandy and cognac in 2003, beer in 2005, wine in 2008 and higher strength cooler, brandy and cocktails in April 2010.
Source: Anderson, A. et al. (2021), “Impact of minimum unit pricing on alcohol purchases in Scotland and Wales: controlled interrupted time series analyses”, Public Health, Vol. 6, Lancet; Taylor, N. et al. (2021), “The impact of a minimum unit price on wholesale alcohol supply trends in the Northern Territory, Australia”, Substance Use, Australian and New Zealand Journal of Public Health, Vol. 45, No. 1; Stockwell, T. et al. (2012), “The Raising of Minimum Alcohol Prices in Saskatchewan, Canada: Impacts on Consumption and Implications for Public Health”, American Journal of Public Health, Vol. 102, No.12.
The number of overweight and obese adults is a growing concern. Measured overweight, including obesity, affected 61% of the Irish population as of 2019, slightly above the average of OECD countries with available data, with about one quarter of the population being obese. Both overweight and obesity rates were broadly stable over recent decades (OECD, 2021a). Overweight and obesity are major risk factors for various chronic diseases and individuals with an unhealthy weight are at higher risk of severe consequences from COVID-19 (Katz, 2021). Moreover, by putting people at a higher risk of sickness and disability, higher body mass is found to be associated with lower employment opportunities, earnings and productivity (Campbell et al., 2021; OECD, 2019b). These effects considered, overweight-related diseases are expected to reduce healthy life expectancy in Ireland by 2.9 years, on average, over the next 30 years, because of higher premature mortality (-3.2 years for the OECD average). Over the same period, average annual overweight-driven health expenditure would increase by 9.0% (+8.4% for the OECD), which, in turn, would add fiscal pressure and, therefore, increase the average annual government primary revenue needed to stabilise the debt-to-GDP ratio by 0.8 percentage points (+0.6 for the OECD).
Ireland is among the OECD countries taxing sugar-sweetened drinks. The excise duty, introduced in 2018, effectively reduced demand for popular soft drinks and, at the same time, incentivised manufacturers to reduce their sugar content, especially in those preferred by children. Exposure to economic vulnerability in early childhood, in particular, is significantly associated with being overweight and obese (Maître et al, 2021).
Supporting healthier diets, particularly among lower-income households, would complement measures to reduce sugar intake. Reliable labels on the front of pre-packaged foods are key to ensure consumers make informed food purchases in line with disease prevention policies. To facilitate this, the European Commission, as committed in its 2020 Farm to Fork strategy, is set to propose harmonised mandatory front-of-pack labelling for food products by end-2022 (European Commission, 2020), Ireland is among the OECD countries allowing front-of-pack labels on a voluntary basis, but only to the extent they repeat the – mandatory or complementary – nutrition contents displayed in back-of-pack labels. Overall, increased use of food labelling has resulted in higher purchases of healthier food in many countries (Cecchini and Warin, 2016; Barreiro-Hurlé et al., 2010). Food labels’ effectiveness in supporting healthy dietary choices, however, depends on certain consumer characteristics: higher levels of income and education are positively associated with greater use and understanding of nutritional information, which are less easily interpretable by more disadvantaged categories (Storcksdieck Bonsmann et al., 2020). As a result, simpler front-of-pack labels combining colour-coded information with, for instance, a graded indicator conveying immediate graphic information about the product’s amount of key nutrients, as in the “Nutri-Score” recently launched in France, would help enable healthier food choices (OECD, 2022b).
Tackling the economic and social burden of obesity is a policy priority in Ireland. Under the framework of the Healthy Ireland Agenda, a ten-year Obesity Policy and Action Plan was launched in 2016 (Government of Ireland, 2016), followed by the establishment of a cross-departmental implementation advisory group in 2017. By identifying regulation as a priority policy tool towards enabling healthier dietary choices, the Plan gave way to the development of behavioural science-based research, particularly on the positive impact of portion size markings in reducing the excessive consumption of food high in fat, salt and sugars (Robertson et al., 2020). Moreover, the Department of Health launched a public consultation on front-of-pack nutrition labelling and scores in 2021. Recent OECD work suggests that the implementation of front-of-pack labelling, such as Nutri-Score, would have beneficial effects for Ireland’s population and its economy, namely via long-term health expenditure savings and improved labour market participation (OECD, 2022b).
Supporting more balanced and healthier school meal programmes could strengthen children’s food literacy and have long-term beneficial effects on their health. Dietary practices formed early in life tend to leave a lasting imprint (Murimi et al., 2018). The school free-meal programme, managed and funded by the Department of Social Protection (with the involvement of local authorities, in the case of primary schools), is currently benefitting 230 000 children belonging to over 1 500 schools featuring significant concentration of disadvantage, with students participating on a voluntary basis (Darmody, 2021). The scheme, in particular, had a key role in supporting struggling families during the COVID-19 crisis, following the decision to extend the provision of school meals beyond academic years, in order to cover for the summer breaks. Over the years, schools participating in the state meal programme have mainly used its cold lunch option. Only recently did the Department of Social Protection extend its pilot Hot School Meal Programme, initially tested in 37 schools, to over 55 000 primary school pupils in disadvantaged schools. Under current rules, funding for school meals is provided for food items only, excluding any expenditure on staff or equipment (Darmody, 2021). This, together with relatively low maximum rates of payment per meal, tilts the system towards purchases of pre-packed food resulting from larger-scale production. While such meals may meet basic nutritional standards, a large part of their components are often ultra-processed (Darmody, 2021).
By enabling increased consumption of freshly prepared food, particularly among more disadvantaged pupils who are less likely to have access to it, the establishment of in-school or community-level kitchens could enhance pupils’ dietary resilience and food literacy, potentially resulting in long-lasting changes to daily dietary habits. This would be in line with considerable internal demand for higher quality food in Irish schools (Browne et al., 2019; EDC, 2020), as well as with international experiences in countries like Japan, Australia (the Kitchen Garden Programme) and England (The Food for Thought project, Box 2.5), where lunches are an integral part of the education curricula. Positive indirect economic effects would also spread to local communities through additional employment opportunities and increased sustainability of supply chains, by means of greater involvement with networks of local producers.
Relatively tight regulations apply to the advertising of energy-dense foods, including a ban on targeting children in radio and television ads (OECD, 2019b). Additionally, a voluntary code of conduct, agreed between the government, advertising and broadcasting authorities, as well as various industry associations, tightened the rules on non-broadcast media advertising and marketing of High Fat, Salt and Sugar (HFSS) food and (non-alcoholic) drink products in 2018 (DOH, 2017b). While detailed, these provisions failed to outline a regulatory body tasked to oversee compliance and able to investigate potential complaints. As a result, the Advertising Standards Authority for Ireland (ASAI) recently issued new rules restricting marketing communications for HFSS products targeting children younger than 15, broadly in line with the stance adopted in anti-alcohol regulations (ASAI, 2021). However, the new rules are not legally binding. Making compliance with rules on non-broadcast media advertising and marketing of these products mandatory, as in alcohol advertising, would limit the risks involved with children’s exposure to aggressive promotion of unhealthy products. Moreover, the development of digital media and technology, together with increasingly sophisticated profiling techniques, make the detection and enforcement of harmful food advertising particularly complex, notwithstanding 2018 data regulations prohibiting online targeting of children by advertisers (DOJ, 2018). Implementing a system of fines, while outlining clear monitoring and enforcement responsibilities, as well as easily accessible complaint mechanisms, could enhance regulatory efficiency and foster reformulation incentives in food manufacturing.
The Food for Thought (FFT) school meal project was established in 2003 by six local head teachers in the Liverpool City region. They had grown unhappy with the quality and healthiness of meals that local authorities, either directly or through large private contractors, provided to children in their schools. As such, they established a not-for-profit company with the purpose of providing partner schools with daily meals freshly prepared on site and of greater variety. To ensure a broader positive return to local communities, schools employ their specific catering teams, while FFT’s 30-persons staff support manage the system on their behalf and support them in the case of absentees. However, administratively, schools continue to deal with payments by families and pay FFT for its services thereafter. Costs, as well as all profits, are shared among participant schools pro-rata to the number of meals served. Decisions are taken by a Board whose members are the head teachers of the schools using the service. FFT’s network has gradually expanded to include 86 schools in the Liverpool City region. In 2021, it served about two million meals.
Strong reliance on food products sourced from local providers helps FFT preserve its cost-competitiveness, relative to large private catering companies, while supporting community-level businesses. Moreover, the company’s modus operandi allows it to flexibly adapt food provision to the tastes of children from different communities, which also helps them to become accustomed to dietary variety. Emphasis is laid on the educational value of food processes. This includes reviewing menus every six weeks to follow fruit and vegetable seasonality or the adoption of learning modules aimed at empowering children’s knowledge on food’s origins and on how to prepare it, as well as on related environmental issues.
Source: www.foodforthoughtschools.co.uk
|
MAIN FINDINGS |
RECOMMENDATIONS (key in bold) |
|---|---|
|
Moving towards a system centred on care needs |
|
|
The capped tax relief on private health insurance premiums accentuates the two-tiered nature of the health system. |
Remove the tax relief or consider making it conditional on means-testing. |
|
Entitlement to publicly-financed care services depends on several criteria that have been adjusted over time, increasing uncertainty. |
Streamline and harmonise eligibility criteria across publicly-funded health schemes and limit their adjustments over time. |
|
A new Sláintecare consultant contract has been proposed to effectively reduce understaffing by improving working conditions in public hospitals. Full separation of public and private specialist practice may permanently weaken incentives for inter-sectoral professional mobility. |
Further increase the number of consultant and medical training posts to effectively reduce understaffing. To attract talent, ensure the new contract enables flexible combinations of clinical hours with research and management tasks, according to specialists’ skills, interests and propensities. |
|
The challenge of long waiting lists needs to be addressed by policy action in a number of areas. There is room to move some diagnosis and care from hospitals to primary and community care. Not all patients use the most appropriate health pathways, either being referred to specialists that are not the correct ones or presenting themselves to emergency rooms to get diagnostic tests. |
Keep the path of increases in public hospital capacity in line with planned objectives and improve waiting time management. Build a proper information base to monitor progress of the Waiting List Action Plan. Provide assistance to medical professionals outside the acute hospital sector to direct patients to primary or community care rather than hospitals when appropriate. |
|
Pre-pandemic demand for home care support exceeded the corresponding supply of services, resulting in long waiting lists, which could further be exacerbated in the near future. |
Support effective integration of home care with other community-based health, long-term care and social services. Set cost thresholds – linked to comprehensive assessments of patients’ need – above which a user is shifted from home to institutional care settings. |
|
Home care for the elderly involves lower societal costs, but when the patient becomes sicker, the costs rise and the quality of care diminishes. |
Establish integrated funding and service delivery to offer home care and admission to long-term residential care when needed. |
|
The Single Assessment Tool (SAT) is a key IT tool to support enhanced operational integration across all health and social long-term care providers, enabling large efficiency gains and the provision of more effective person-centred care services. |
Accelerate the implementation of the Single Assessment Tool across the country in order to move towards more effective person-centred care services. Extend access to SAT data, at the individual and/or aggregate level, to acute and other community care providers. |
|
Ensuring equitable and cost-effective healthcare |
|
|
Within the most expensive High-Tech Drug pharmaceutical spending arrangement, the price of patented originator medicines may be reduced based on the average price paid in 14 European countries. |
Consider linking downward price adjustments to an average of the lowest prices among the chosen benchmark countries. |
|
The use of generics and biosimilars remains modest. The European Medicines Agency has recently confirmed that biosimilar medicines approved in the European Union are interchangeable with their reference drug. |
Enhance competition in the off-patent and biosimilar drug market, ensuring that market penetration of medications is not artificially suppressed by the existing system of mandatory price reductions. Regularly update the Health Products Regulatory Authority list of interchangeable medicines in order to increase utilisation of lower cost non-originator products. Encourage the increased use of biosimilars, including by considering making them as interchangeable as generics. |
|
The Sláintecare reforms are overhauling the Irish healthcare system. The system is currently overly centralized and biased towards expensive hospital-based treatments. |
Implement the reforms to create Regional Health Areas and rebalance healthcare delivery across primary, community and long-term care and hospitals. Improve value for money in health spending through a repeated use of spending reviews. |
|
The success of Regional Health Areas will depend on a suitable funding system and data availability. The funding system is currently fragmented across care settings and lacks transparency, limiting the traceability of healthcare spending. Monitoring the health system is hindered by its complexity, lack of adequate information, fragmented data governance and underdeveloped digital infrastructure. |
Introduce a Population-Based Resource Allocation funding model, as planned, to improve financial reporting and management and strengthen equity in health outcomes. Prioritise reforms to enhance the take-up of a unique health identifier across health services and centralise governance and appropriate national health information functions within a single independent body. |
|
Effectively integrated care services at the point of delivery by Regional Health Areas (RHAs) will require successful coordination across different care providers and improved measurement, monitoring and reporting processes. |
Ensure RHAs have the autonomy to effectively arrange the coordination of care providers and service delivery based on the needs of their population. Use the new Health System Performance Assessment to support better evidence-based decisions, but avoid locking RHAs into strict, common performance patterns. |
|
Ensuring healthier lives |
|
|
Growing needs for cancer treatment, financial support and ongoing diagnostics over longer spells of time could add to ageing costs. |
Establish effective and cost-efficient cancer survivorship programmes aimed at meeting survivors’ needs along the physical, psychological, social and financial dimensions. In line with the 2017-2026 National Cancer Strategy, continue to expand the delivery of cancer survivorship care at the community and primary care level. |
|
Many cancer survivors’ return to formal work occurs prematurely and mainly based on financial need considerations, which could strengthen incentives to leave the labour market and result in higher social costs. |
Introduce measures enabling a more gradual and flexible return to full-time employment for cancer survivors. Consider establishing occupational support programmes for SME employees and the self-employed, who may face pressures to resume work because of weaker coverage of sick pay leave. |
|
A cancer diagnosis could represent a significant source of financial stress to the patient and her/his family, even at income levels well above the thresholds traditionally set for eligibility to the Medical Card. |
Continue to expand means-tested eligibility to primary care to ensure financial protection of patients. Increase transparency and reduce complexity in the awarding of cards to increase uptake. |
|
The move towards off-premise alcohol sales at cheaper prices increases consumption among younger people. |
Continue to use minimum unit pricing of alcohol as a lever to reduce its affordability in the off-premise sector. |
|
There is room to improve the use of food labelling, which is associated with higher purchases of healthier food, to make it more interpretable to more disadvantaged consumers. |
Adopt a scheme conveying simpler graphic information on the amount of key nutrients in pre-packaged food products, in line with EU-level efforts towards harmonised mandatory front-of-pack labelling. |
|
A voluntary and non-binding code of conduct restricts marketing and non-broadcast media advertising of High Fat, Salt and Sugar food and non-alcoholic drink products targeting children younger than 15. Technological development and sophisticated profiling technics make detection and enforcement of harmful food advertising more complex. |
Make compliance with rules on non-broadcast media advertising and marketing of High Fat Salt and Sugar food and drink products mandatory, as in alcohol advertising. Introduce a regulatory body overseeing compliance and investigating potential complaints. |
|
Supporting balanced and healthier school meal programmes could have long-term beneficial effects on children’s health. |
Consider extending the eligibility for funding from the state’s school meal programmes to expenditures on equipment and staff. |
ACS (2021), Cancer Treatment and Survivorship – Facts & Figures 2019-2021, American Cancer Society, Atlanta.
Anderson, P., D. Chisholm and D.C. Fuhr (2009), “Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol”, The Lancet, Vol. 373, No. 9682, pp. 2234-2246.
Angus, C. et al. (2014), “Model-based appraisal of minimum unit pricing for alcohol in the Republic of Ireland”, ScHARR, University of Sheffield.
Araujo, E.C., T. Grant Evans and A. Maeda (2016), “Using economic analysis in health workforce policy-making”, Oxford Review of Economic Policy, Vol. 32, No. 1, pp. 41-63.
ASAI (2021), Code of Standards for Advertising and Marketing Communications in Ireland: Section 8 – Food and Non-Alcoholic Beverages, Advertising Standard Authority for Ireland, Dublin.
Bakx, P., B. Wouterse, E. van Doorslaer and A. Wong (2020), “Better off at home? Effects of nursing home eligibility on costs, hospitalizations and survival”, Journal of Health Economics, Vol. 73.
Barreiro-Hurlé, J. et al. (2010), “Does nutrition information on food products lead to healthier food choices?”, Food Policy, Vol. 35, No.3, pp. 221-229.
Beazley, I. et al. (2019), “Decentralisation and performance measurement systems in health care”, OECD Working Papers on Fiscal Federalism, No. 28, OECD Publishing, Paris.
Brick, A. and S. Connolly (2021), “Waiting Times for Publicly Funded Hospital Treatment: How does Ireland Measure Up?”, The Economic and Social Review, Vol. 52/1.
Browne, S. et al. (2019), “We Know What we Should Eat But we Don’t…: A Qualitative Study in Irish Secondary Schools”, Health Promotion International, Vol. 35, No. 35, pp. 984-993.
Burke, S., S. Parker, P. Fleming, S. Barry and S. Thomas (2021), “Building health system resilience through policy development in response to COVID-19 in Ireland: From shock to reform”, The Lancet Regional Health - Europe, Vol. 9.
Burke, S., S. Barry, R. Siersbaek, B. Johnston and M. Ní Fhallúin (2018), “Sláintecare – A ten-year plan to achieve universal healthcare in Ireland”, Health Policy, Vol. 122, pp. 1278-82.
Campbell, D.D. et al. (2021), “Effects of increased body mass index on employment status: a Mendelian randomisation study”, International Journal of Obesity, Vol. 45, pp. 1790-1801.
Casey, E and K. Carroll (2021), "The Path for Ireland's Health Budget", Analytical Note, No. 14, Irish Fiscal Advisory Council.
Cecchini, M. and L. Warin (2015), “Impact of food labelling systems on food choices and eating behaviours: a systematic review and meta-analysis of randomised studies”, Obesity Reviews, Vol. 17, No. 3, pp. 201-210.
Charnes, A., W.W. Cooper and E. Rhodes (1978), “Measuring the efficiency of decision making units”, European Journal of Operational Research, Vol. 2, pp. 429-444.
Citizens Information (2021), Health Services in Ireland.
Colombo, F., A. Llena-Nozal, J. Mercier and F. Tjadens (2011), “Help Wanted? Providing and Paying for Long-Term Care”, OECD Health Policy Studies, OECD Publishing, Paris.
Colombo, F. and N. Tapay (2004), “Private Health Insurance in OECD Countries: The Benefits and Costs for Individuals and Health Systems”, OECD Health Working Papers, No. 15, OECD Publishing, Paris.
Comas-Herrera, A. et al. (2021), “Mortality associated with COVID-19 in care homes: international evidence”, International Long Term Care Policy Network.
Committee of Public Accounts (2021), HSE Financial Statement 2020, Houses of the Oireachtas, Dublin.
Committee on the Future of Healthcare (2017), Sláintecare Report, Houses of the Oireachtas, Dublin.
Connolly, S., H. Russell and E. Henry (2021), “Returning to Employment Following a Diagnosis of Cancer: An Irish Survey”, ESRI Survey and Statistical Report Series, No. 103, Dublin.
Connolly, S. and R. White (2019), “Uptake of cancer screening services among middle and older ages in Ireland: The role of healthcare eligibility”, Public Health, Vol. 173, pp. 42-47.
Connolly, S. and M.A. Wren (2019), “Universal care in Ireland: what are the prospects for reform?”, Health Systems & Reform, Vol. 5(2), pp. 94-99.
Coomber, K. et al. (2020), “Investigating the introduction of the alcohol minimum unit price in the Northern Territory”, Final Report, prepared for the Northern Territory Department of Health, Deakin University, Geelong Australia.
Croghan, S.M. et al. (2021), “Perceptions of higher specialist trainees and fellows of the proposed Sláintecare consultant contract and implications for workforce planning in Ireland”, Journal of Medical and Health Studies, Vol. 2, No. 2.
Darmody, M. (2021), “A kitchen at the heart of a school: an investigation into school meals in the Republic of Ireland”, Irish Educational Studies, Vol. 40, No. 4.
De Biase, P., S. Dougherty and L. Lorenzoni (2022), “Ageing and the long-run fiscal sustainability of health care across levels of government”, OECD Working Papers on Fiscal Federalism, No. 38, OECD Publishing.
de Boer, A. et al. (2020), “Long-term work retention after treatment for cancer: a systematic review and meta-analysis”, Journal of Cancer Survivorship, Vol. 14, No. 2, pp. 135-150.
Delamaire, M. L. and G. Lafortune (2010), “Nurses in advanced roles: A description and evaluation of experiences in 12 developed countries”, OECD Health Working Papers, No. 54, OECD Publishing, Paris.
DOH (2022), Business Case for the Implementation of Regional Health Areas (RHAs), Department of Health, Dublin.
DOH (2021a), Health in Ireland: Key Trends 2021, Department of Health, Dublin.
DOH (2021b), COVID-19 Nursing Homes Expert Panel Recommendations - Third Progress Report, Department of Health, September, Dublin.
DOH (2021c), Sláintecare Implementation Strategy and Action Plan 2021-2023, Department of Health, Dublin.
DOH (2017a), National Cancer Strategy 2017-2026, Department of Health, Dublin.
DOH (2017b), Non-Broadcast Media Advertising and Marketing of Food and Non-Alcoholic Beverages, including Sponsorship and Retail Product Placement: Voluntary Code of Practice, Department of Health, Dublin.
DOH/HSE (2021a), Home Support Services: Preparedness and impact of COVID-19 on services, Department of Health and Health Service Executive Joint Paper, Dublin.
DOH/HSE (2021b), Public Health (Alcohol) Act 2018 – Guidance for Industry, Sections 15 and 16, Department of Health and Health Service Executive, October.
DOH/HSE/NCCP (2020), Cancer Services in Ireland in the Context of COVID-19, Department of Health, Health Service Executive and National Cancer Control Programme, Dublin.
DOH/HSE (2019), Public Health (Alcohol) Act 2018 – Guidance for Industry, Department of Health and Health Service Executive, July.
DOJ (2018), Data Protection Act 2018: Explanatory Memorandum, Department of Justice, Dublin.
Dougherty, S., P. de Biase and L. Lorenzoni (2022), “Funding the future: The impact of population ageing on revenues across levels of government”, OECD Working Papers on Fiscal Federalism, No. 39, OECD Publishing, Paris.
Dougherty, S. et al. (2019), “The impact of decentralisation on the performance of health care systems: A non-linear relationship”, OECD Working Papers on Fiscal Federalism, No. 27, March, OECD Publishing, Paris.
Dutu, R. and P. Sicari (2020), “Public spending efficiency in the OECD: benchmarking health care, education and general administration”, Review of Economic Perspectives, Vol. 20, No. 3, pp. 253-280.
ECDC (2022), Surveillance Data from Public Online National Reports on COVID-19 in Long-term Care Facilities, European Centre for Disease Prevention and Control, Stockholm.
EDC (2020), National Strategy Group for Hunger Prevention in Schools, Educational Disadvantage Centre, Dublin City University.
European Commission (2021), The 2021 Ageing Report. Economic and Budgetary Projections for the EU Member States (2019-2070), Brussels.
European Commission (2020), Farm to Fork Strategy: For a fair, healthy and environmentally friendly food system, Brussels.
European Commission (2019), Country Report Ireland, 2019 European Semester Country Report.
Färe, R., S. Grosskopf and C.A.K. Lovell (1993), Production Frontiers, Cambridge University Press.
Fennelly, O. et al. (2018), “Advanced practice physiotherapy-led triage in Irish orthopaedic and rheumatology services: national data audit”, BMC Musculoskeletal Disorders, Vol. 19, No. 181.
Ferrinho, P. et al. (2004), “Dual practice in the health sector: review of the evidence”, Human Resources for Health, Vol. 2, No. 14.
Fleming, P. et al. (2022), “Implications for health system reform, workforce recovery and rebuilding in the context of the Great Recession and COVID-19: a case study of workforce trends in Ireland 2008-2021”, Human Resources for Health, Vol. 20, No. 48.
Garattini, L. and A. Padula (2018), “Dual practice of hospital staff doctors: Hippocratic or hypocritic?”, Journal of the Royal Society of Medicine.
Government of Ireland (2023), Budget 2023 Expenditure Report, Dublin.
Government of Ireland (2021), About the Department of Health, Dublin.
Government of Ireland (2016), A Healthy Weight for Ireland: Obesity Policy and Action Plan 2016-2025, Dublin.
Hanley, P., R. Maguire, A. O’Ceilleachair and L. Sharp (2018), “Financial hardship associated with colorectal cancer survivorship: The role of asset depletion and debt accumulation”, Psycho-Oncology, Vol. 27, No. 9, pp. 2165-2177.
Hanley, P. et al. (2013), “Work-related productivity losses in an era of ageing populations: the case of colorectal cancer”, Journal of Occupational and Environmental Medicine, Vol. 55, No. 2, pp. 128-134.
Heffron, M. and K. Socha-Dietrich (2019), “The Irish paradox: Doctor shortages despite high numbers of domestic and foreign medical graduates”, in Recent Trends in International Migration of Doctors, Nurses and Medical Students, OECD Publishing, Paris.
Henderson, C., X. Liu, A.V. Diez Roux, B.G. Link and D. Hasin (2004), “The effects of US state income inequality and alcohol policies on symptoms of depression and alcohol dependence”, Social Science and Medicine, Vol. 58, No. 3, pp. 565-75.
Hennessy, M., C. Shine and E. Walker (2021), “Healthcare Capital Investment in Ireland”, Spending Review 2021, Department of Health, Dublin.
HIA (2022), Quarterly Report on Health Insurance - 2nd Quarter, The Health Insurance Authority, Dublin.
HIA (2021), Annual Report and Accounts 2020, The Health Insurance Authority, Dublin.
HIQA (2021), Acute and Community Healthcare Services, Health Information and Quality Authority, Dublin.
HIQA (2020), Guidelines for Economic Evaluation of Health Technologies in Ireland, Health Information and Quality Authority, Dublin.
Holmes, J. et al. (2014), “Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study”, The Lancet, Vol. 383, No. 9929, pp. 1655-1664.
Holtorf, A.P. et al., (2019), “External reference pricing for pharmaceuticals – A survey and literature review to describe best practices for countries with expanding healthcare coverage”, Value in Regional Health Issues, Vol. 19, pp. 122-131.
Houses of the Oireachtas (2022a), Debate of the Joint Committee on Health, 9 February.
Houses of the Oireachtas (2022b), Debate of the Joint Committee on Health, 6 April.
Houses of the Oireachtas (2020), Debate of the Special Committee on COVID-19 Response, 2 June.
HSE (2022a), National Service Plan 2022, Health Service Executive, Dublin.
HSE (2022b), Annual Report and Financial Statements 2021, Health Service Executive, Dublin.
HSE (2022c), 2022 Waiting List Action Plan, Government of Ireland.
HSE (2022d), Single Assessment Tool (InterRAI), Health Service Executive, Dublin.
HSE (2022e), Structured Chronic Disease Management Programme Phase 2, Health Service Executive, Dublin.
HSE (2021a), Health Services Performance Profile October-December 2020, Health Service Executive, Dublin.
HSE (2021b), Medical Workforce Report 2020-21, Health Service Executive, Dublin.
HSE (2020), Performance and Accountability Framework, Health Service Executive, Dublin.
HSE (2018), The State of Tobacco Control in Ireland, Health Service Executive, Dublin.
HSE (2016), Towards Successful Consultant Recruitment, Appointment and Retention, Health Service Executive, Dublin.
Humphries, N., J. Creese, J.P. Byrne and J. Connell (2021), “COVID-19 and doctor emigration: the case of Ireland”, Human Resources for Health, Vol. 19, No. 29.
Humphries, N., J. Connell, J. Negin and J. Buchanan (2019), “Tracking the leavers: towards a better understanding of doctor migration from Ireland to Australia 2008-2018”, Human Resources for Health, Vol. 17, No. 36.
ICGP (2021), ICGP Response to Consultation on Review of the Mental Health Act, Irish College of General Practitioners, Dublin.
IFAC (2015), “Controlling the health budget: Annual budget implementation in the public health area”, Analytical Note, No. 8, Irish Fiscal Advisory Council, Dublin.
IGEES (2019), “Health Workforce Consultant Pay and Skills Mix, 2012-2017”, Spending Review 2019, Irish Government Economic and Evaluation Service, Department of Public Expenditure and Reform, Dublin.
IMO (2017), Irish Medical Organisation Submission to the Public Service Pay Commission, Ireland Medical Organisation, Dublin.
Independent Review Group (2019), Report of the Independent Review Group established to examine Private Activity in Public Hospitals, February.
INMO (2022), Submission to the Joint Committee on Health Emergency Department Overcrowding, Irish Nurses and Midwives Organisation.
INMO (2021), Pre-Budget Submission 2022, Irish Nurses and Midwives Organisation.
IPHA (2021), Framework Agreement on the Supply and Pricing of Medicines – Final Version, Irish Pharmaceutical Healthcare Association, Dublin.
IRG (2019), Report of the Independent Review Group Established to Examine Private Activity in Public Hospitals, Independent Review Group.
Katz, M. (2021), “Regardless of Age, Obesity and Hypertension increase risks with COVID-19”, JAMA Internal Medicine, Editor’s Note.
Keane, C., M. Regan and B. Walsh (2021), “Failure to take-up public healthcare entitlements: evidence from the Medical Card system in Ireland”, Social Science & Medicine, Vol. 281, 114069.
Kennedy, F. et al. (2007), “Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer”, European Journal of Cancer Care, Vol. 16, No. 1, pp. 17-25.
Kennelly, B. et al. (2020), “The COVID-19 pandemic in Ireland: an overview of the health service and economic policy response”, Health Policy and Technology, Vol. 9, No. 4, pp. 419-429.
Kok, L., C. Berden and K. Sadiraj (2014), “Costs and benefits of home care for the elderly versus residential care: a comparison using propensity scores”, The European Journal of Health Economics, Vol. 6, pp. 119-131.
Lorenzoni, L. and S. Dougherty (2022), “Understanding differences in health care spending: A comparative study of prices and volumes across OECD countries”, Health Services Insights, Vol. 15.
Lorenzoni, L. et al. (2019), “Health Spending Projections to 2030: New results based on a revised OECD methodology”, OECD Health Working Papers, No. 110, OECD Publishing, Paris.
Lorenzoni, L. et al. (2017), “Cyclical vs structural effects on health care expenditure trends in OECD countries”, OECD Health Working Papers, No. 92, OECD Publishing, Paris.
Maître, B., H. Russell and E. Smyth (2021), “The Dynamics of Child Poverty in Ireland: Evidence from the Growing Up in Ireland Survey”, Research Series, No. 121, Economic and Social Research Institute, Dublin.
Mariotto, A., L. Enewold, J. Zhao, C. Zeruto and K. Yabrof (2020), “Medical Care Costs Associated with Cancer Survivorship in the United States”, Cancer, Epidemiology, Biomarkers and Prevention, Vol. 29/7, Philadelphia.
Matthews, S., M. Pierce, S. O’Brien Green, E. Hurley, B.M. Johnston, C. Normand and P. May (2021), “Dying and Death in Ireland: What do we routinely measure, how can we improve?”, Irish Hospital Foundation, Dublin.
McCarthy, T., C. Lindberg and C. O’Malley (2022), “Towards Population-Based Funding for Health: Evidence Review and Regional Profiles”, Spending Review 2022, Department of Health, Dublin.
Mercille, J., B. Turner and D.S. Lucey (2021), “Ireland’s takeover of private hospitals during the COVID-19 pandemic”, Health Economics, Policy and Law, Vol. 17, No. 2, pp. 232-237.
Mesabbah, M. and Arisha, A. (2016), “Performance management of public healthcare services in Ireland: a review”, International Journal of Health Care Quality Insurance, 29(2).
Moran, P. a/nd E. Halpin (2021), Spending Review 2021: Expanded Provision of Home Support and Total Costs of Long-Term Care for Older Persons – A Scoping Review and Explanatory Analysis, Irish Government Economic and Evaluation Service, Government of Ireland, Dublin.
Müller, M. and K. Socha-Dietrich (2020), “Reassessing private practice in public hospitals in Ireland: an overview of OECD experiences”, OECD Health Working Papers, No. 118, OECD Publishing, Paris.
Murimi, M.W., A.F. Moyeda-Carabaza, B. Nguyen, S. Saha, R. Amin and V. Njike (2018), “Factors that contribute to effective nutrition education interventions in children: a systematic review”, Nutrition Reviews, Vol. 76, No. 8, pp. 553-580.
Murphy, R. et al. (2020), “The Better Letter Initiative: An Impact Evaluation of a Redesigned Inpatient and Day Case Appointment Letter”, Department of Health Research Paper, Dublin.
Murphy, R. and C. Taaffe (2019), “Using SMS Reminders to Reduce Non-attendance at Hospitals Appointments: an Umbrella Review of Key Issues”, Department of Health Research Paper, Dublin.
NCPP (2020), Hospital and Community-based Psychosocial Care for Patients with Cancer and their Families: A Model of Care for Psycho-Oncology, National Cancer Control Programme, Dublin.
NCRI (2021), Cancer in Ireland 1994-2019 – Annual Report, National Cancer Registry Ireland, Cork.
NCRI (2019), Cancer Incidence Projections for Ireland 2020-2045, National Cancer Registry Ireland, Cork.
Nolan, A. (2017), “Health: Funding, Access and Efficiency”, in The Economy of Ireland: Policy-Making in a Global Context, edited by J. O’Hagan and F. Toole, Palgrave Editions, London.
Nolan, A. et al. (2014), The Impact of the Financial Crisis on the Health System and Health in Ireland, WHO.
O’Ceilleachair, O. et al. (2017), “Counting the cost of cancer: out-of-pocket payments made by colorectal cancer survivors”, Supportive Care in Cancer, Vol. 25, No. 9, pp. 2733-2741.
O’Connor, M. et al. (2019), “The unmet needs of cancer survivors in Ireland: A scoping review 2019”, National Cancer Survivorship Needs Assessment, Irish Cancer Society and National Cancer Registry Ireland.
Oderkirk, J. (2021), “Survey results: National health data infrastructure and governance”, OECD Health Working Papers, No. 127, OECD Publishing, Paris.
O’Dwyer, C., D. Mongan, A. Doyle and B. Galvin (2021), “Alcohol Consumption, alcohol-related harm and alcohol Policy in Ireland”, HRB Overview, Series 11, Health Review Board, Dublin.
OECD (2022a), Social Protection for Long-Term Care in Old Age: Latest Estimates, forthcoming.
OECD (2022b), Healthy Eating and Active Lifestyles: Best Practices in Public Health, OECD Publishing, Paris.
OECD (2021a), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris.
OECD (2021b), A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill-Health, OECD Health Policy Studies, OECD Publishing, Paris.
OECD (2021c), Fitter Minds, Fitter Jobs: From Awareness to Change in Integrated Mental Health, Skills and Work Policies, Mental Health and Work, OECD Publishing, Paris.
OECD (2021d), Preventing Harmful Alcohol Use, OECD Health Policy Studies, OECD Publishing, Paris.
OECD (2020a), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris.
OECD (2020b), Waiting Times for Health Services: Next in Line, OECD Health Policy Studies, OECD Publishing, Paris.
OECD (2020c), OECD Economic Surveys: Ireland 2020, OECD Publishing, Paris.
OECD (2020d), Consumption Tax Trends 2020: VAT/GST and Excise Rates, Trends and Policy Issues, OECD Publishing, Paris.
OECD (2019a), OECD at a Glance 2019, OECD Publishing, Paris.
OECD (2019b), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris.
OECD (2018), Accounting and Mapping of Long-Term Care Expenditure under SHA 2011, OECD Publishing, Paris.
OECD (2017a), OECD Economic Surveys: Slovak Republic 2017, OECD Publishing, Paris.
OECD (2017b), Budget Transparency Toolkit: Practical Steps for Supporting Openness, Integrity and Accountability in Public Financial Management, OECD Publishing, Paris.
OECD (2015a), OECD Economic Surveys: Switzerland 2015, OECD Publishing, Paris.
OECD (2015b), Fiscal Sustainability of Health Systems: Bridging Health and Finance Perspectives, OECD Publishing, Paris.
OECD/EU (2021), Ireland Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
O’Riordan, M., C. Collins and G. Doran (2013), Access to Diagnostics – A Key Enabler for a Primary Care led Health Service, Irish College of General Practitioners, Dublin.
Prior, S. et al. (2021), Review of High-Tech Drug Expenditure – Spending Review 2021, Irish Government Economic and Evaluation Service, Dublin.
Public Service Pay Commission (2012), Recruitment and Retention Module 1 Report, Dublin.
Rocard, E., P. Sillitti and A. Llena-Nozal (2021), “COVID-19 in long-term care: Impact, policy responses and challenges”, OECD Health Working Papers, No. 31, OECD Publishing, Paris.
Roland, M. et al. (2006), “Outpatient services and primary care: A scoping review of research into strategies for improving outpatient effectiveness and efficiency”, NCCSDO Department of Health, University of Manchester.
Rottenberg, Y., N.Z. Ratzon, M. Cohen, A. Hubert, B. Uziely and A.G.E.M. de Boer (2016), “Unemployment risk at 2 and 4 years following colorectal cancer diagnosis: a population-based study”, European Journal of Cancer, Vol. 69, pp. 70-76.
RSA (2021), Driver Attitudes and Behaviour Survey 2020, Road Safety Authority, Ballina, Co. Mayo.
RSA (2020), Road Deaths and Alcohol, 2013-2017, Road Safety Authority, Ballina, Co. Mayo.
Schneider, S. and C. Devitt (2018), “Accessing health care in times of economic growth and economic downturn: Evidence from Ireland”, Journal of European Social Policy, Vol. 28(4), pp. 357-369.
Sibbald B. (2009), “Direct Access to Diagnostic Services”, British Journal of General Practice, Vol. 59, No. 562.
Siciliani, L., V. Moran and M. Borowitz (2014), “Measuring and comparing health care waiting times in OECD countries”, Health Policy, Vol. 118/3, pp. 292-303.
Sherk, A., T. Stockwell and R.C. Callaghan (2018), “The effect on emergency department visits of raised alcohol minimum prices in Saskatchewan, Canada”, Drug and Alcohol Review, Vol. 37, No. 51.
Shine, C. and M. Hennessy (2022), “Health Capital Investment in Ireland: An Analysis of Healthcare Infrastructure Capacity”, Spending Review 2022, Irish Government Economic and Evaluation Service and Department of Health, Dublin.
Simar, L. and P.W. Wilson (2007), “Estimation and inference in two-stage, semi-parametric models of production processes”, Journal of Econometrics, Vol. 136, No. 1.
Smith, S. et al. (2019), “Geographic profile of healthcare needs and non-acute healthcare supply in Ireland”, Research Series, No. 90, Economic and Social Research Institute, Dublin.
Smith, T.G. et al. (2016), “The rationale for patient-reported outcomes surveillance in cancer and a reproducible method for achieving it”, Cancer, Vol. 122-3, pp. 344-351.
Storcksdieck Bonsmann, S. et al. (2020), “Front-of-pack nutrition labelling schemes: a comprehensive review”, EUR 29811 EN – Publication Office of the European Union, Luxembourg.
The Irish Examiner (2022), “Carer shortage leaves almost 1,000 people in Cork and Kerry without homecare”, 29 September.
The Irish Times (2021), “Medical card holders’ waiting three years for hearing tests”, 3 March.
Thejournal.ie (2022), “44% increase in the number of Irish doctors emigrating to Australia since 2018”, 22 April.
Thomas, S. et al. (2021), “Sláintecare implementation status in 2020: Limited progress with entitlement expansion”, Health Policy, Vol. 125, No. 3, pp. 277-283.
Thomas, S., S. Burke and S. Barry (2014), “The Irish health-care system and austerity: sharing the pain”, The Lancet, Vol. 383, No. 9928, pp. 1545-1546.
Travers, J. et al. (2019), “Delaying and reversing frailty: a systematic review of primary care interventions”, British Journal of General Practice.
Turner, B. and S. Smith (2020), “Uncovering the complex role of private health insurance in Ireland”, in Private Health Insurance, History, Politics and Performance, edited by Thomson et al., European Observatory on Health Systems and Policies, World Health Organisation - Europe.
Valero-Bover, D. et al. (2022), “Reducing non-attendance in outpatient appointments: predictive model development, validation, and clinical assessment”, BMC Health Services Research 2022 22:1, Vol. 22/1, pp. 1-8.
VanderBent, S. and B. Kuchta (2010), Valuing Home and Community Care, Community Providers Association Committee, Ontario, Canada.
Wagenaar, A., A. Tobler and K. Komro (2010), “Effects of alcohol tax and price policies on morbidity and mortality: a systematic review”, American Journal of Public Health, Vol. 100, No. 11, pp. 2270-2278.
Walsh, B. and S. Lyons (2021), “Demand for the statutory home support scheme”, Research Series, No. 122, Economic and Social Research Institute, Dublin.
Walsh, B. et al. (2021), “Projections of expenditure for primary, community and long-term care in Ireland, 2019-2035, based on the Hippocrates model”, Research Series, No. 126, Economic and Social Research Institute, Dublin.
Walsh, B., C. Mac Domhnaill and G. Mohan (2021), “Developments in healthcare information systems in Ireland and internationally”, ESRI Survey and Statistical Report Series, No. 105, Economic and Social Research Institute, Dublin.
Walsh, B., S. Lyons, S. Smith, M.A. Wren and J. Eighan (2020), “Does formal home care reduce inpatient length of stay?”, ESRI Research Bulletin, November Bulletin, Economic and Social Research Institute, Dublin.
Wells, J and M. White (2014), “The impact of the economic crisis and austerity on the nursing and midwifery professions in the Republic of Ireland: Boom, bust and retrenchment”, Journal of Research in Nursing.
Williams, D. and S. Thomas (2017), “The impact of austerity on the health workforce and the achievement of human resources for health policies in Ireland (2008-2014)”, Human Resources for Health, Vol. 15, No. 62.
Williams, S.C. et al. (2007), “Developing a robust and efficient pathway for the referral and investigation of women with post-menopausal bleeding using a cut-off of < or = 4 mm for normal thickness”, The British Journal of Radiology, Vol. 80, No. 957.
Williamson, A. et al. (2021), “‘Missingness’ in health care: Associations between hospital utilization and missed appointments in general practice. A retrospective cohort study”, PLoS ONE, Vol. 16/6.
Winpenny, E. et al. (2016), “Outpatient services and primary care: Scoping review, studies and international comparisons”, Health Services and Delivery Research, National Institute for Health Research, London.
Wilson, P.W. (2008), “FEAR 1.0: A software package for frontier efficiency analysis with R”, Socio-Economic Planning Sciences, Vol. 42, No. 4, pp. 247-254.
Wren, M.A. and A. Fitzpatrick (2020), “How does Irish healthcare expenditure compare internationally?”, Research Series, Number 114, October, Economic and Social Research Institute, Dublin.
Zhao, J. et al. (2013), “The relationship between minimum alcohol prices, outlet densities and alcohol-attributable deaths in British Columbia, 2002-09”, Addiction, Vol. 108, No. 6, pp. 1059-69.