Obesity is one the main causes of morbidity and mortality in Chile, and the growing prevalence is creating a major threat to the health of the country. Chile has put in place a comprehensive portfolio of interventions, from population-level fiscal policies, to school- and workplace-focused programmes, to individual interventions in primary care. There are a number of ways in which Chile could further strengthen its portfolio of interventions, including through expanding some polices so that they cover a greater share of the population, and a greater number of food products. In addition Chile’s private health insurers – the ISAPRES – have a bigger role to play, and could do more to positively influence the health of their insurees.
OECD Reviews of Public Health: Chile
Chapter 2. Tackling obesity, unhealthy diet and physical inactivity
Abstract
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
2.1. Introduction
Obesity is one the main causes of morbidity and mortality in Chile, and the growing prevalence is creating a major threat to the health of the country. In this chapter, we explore the causes and impacts of this risk factor, as well as Chile’s policy response. Chile has put in place a comprehensive portfolio of interventions, from population-level fiscal policies, to school- and workplace-focused programmes, to individual interventions in primary care. This chapter examines these interventions, and makes a number of recommendations for ways to further improve the effectiveness – and cost-effectiveness – of Chile’s ambitious obesity strategy.
2.2. Obesity and associated unhealthy behaviours are a top public health priority in Chile
2.2.1. Nearly two-thirds of the Chilean population, and a third of children, is overweight or obese
In 2016, 39.8% of the Chilean population was overweight, and another 34.4% was obese (Ministerio de Salud, 2017[1]). This is one of the highest rates observed among OECD countries, though many others also have a high prevalence of overweight and obesity (see Figure 2.1). While data is too scarce to analyse the trend of obesity in Chile, data from the National Health Survey shows that the obesity rate has increased considerably in recent years, despite improved awareness and action. While between 2003 and 2009 obesity rates went from 24.5% to 25.1%, in 2016 this number rose to 34.4% (Ministerio de Salud, 2017[1]).
Figure 2.1. Measured obesity prevalence in 2016 (or nearest year)
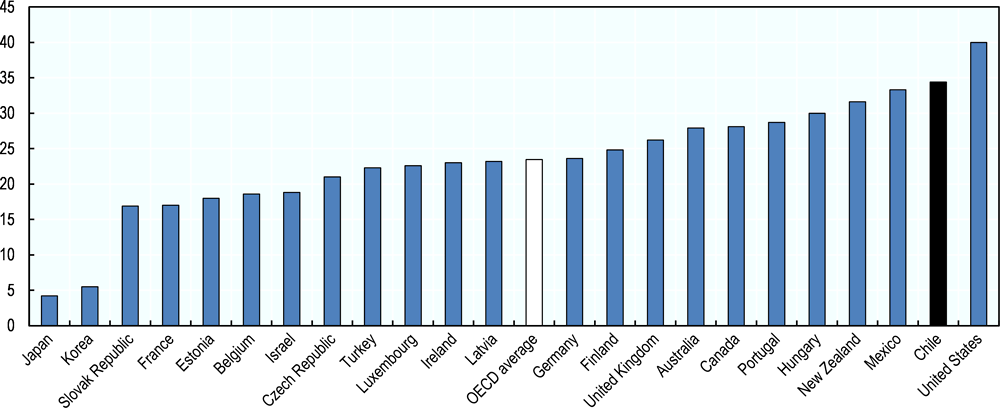
Source: OECD Health Statistics, https://doi.org/10.1787/health-data-en.
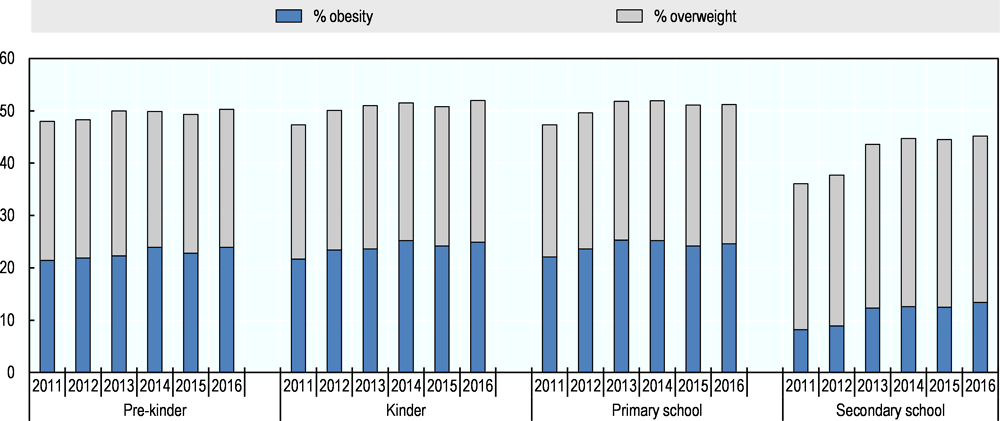
As in other countries, Chile has seen an increase in the number of children who are overweight or obese (see Figure 2.2). The rate of overweight and obesity for children aged 13 years old in Chile was nearly 45%, which is the highest rate in any OECD country for which data is available. A recent survey of Chilean students paints a similar picture, with just over 50% of pre-school children already overweight (see Figure 2.3). Children who are overweight are more likely to be overweight as adults, and are at greater risk of poor health in the future (OECD, 2015[2]; OECD, 2010[3]) . As such, Chile’s high prevalence of childhood overweight and obesity can be considered a ‘health time-bomb’ (OECD, 2010[3]).
Figure 2.2. Childhood overweight prevalence in 2010 (or nearest year)
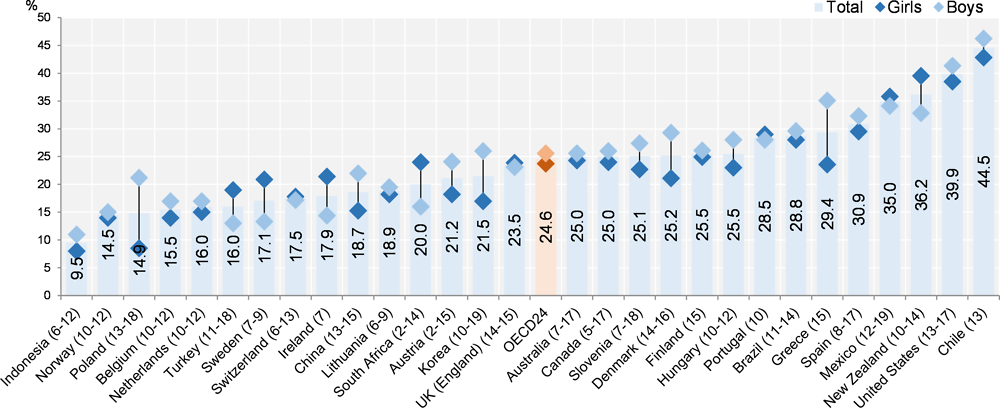
Note: The numbers in parentheses refer to the age of the children surveyed in each country.
Source: OECD Health at a Glance 2017 (OECD, 2017[4]).
Figure 2.3. Measured overweight and obesity among Chilean children, 2011 to 2016
2.2.2. Obesity and associated factors contribute significantly to the overall burden of disease in Chile
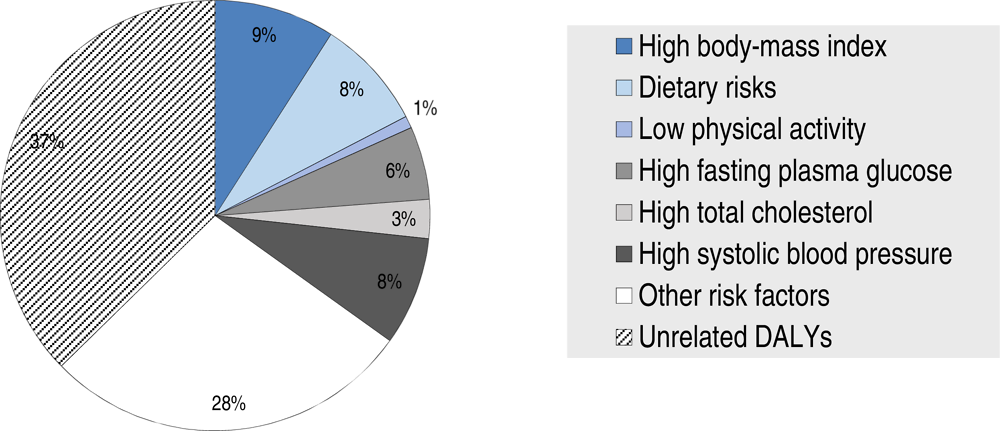
Burden of disease is the impact of a health problem as measured by mortality, morbidity, or other indicators. It can be quantified in terms of Disability-Adjusted Life Years (DALYs), which is equivalent to one year of healthy life lost. In 2016, high body mass index (BMI) was the cause of 9.1% of total DALYs in Chile, while closely associated risk factors – dietary risks and low physical activity – contributed another 9.2% (see Figure 2.4). The potential consequences of obesity – high levels of blood glucose, cholesterol and blood pressure – together account for an additional 16.6% of total DALYs. Overall, obesity and its causes and consequences contribute significantly to the burden of disease in Chile.
Figure 2.4. Chile’s burden of disease (DALYs) by risk factor, 2016
2.2.3. A number of factors are driving the high rate of obesity
The rise of obesity in Chile in the past decades is associated with a decrease in levels of physical activity and an increase in consumption of calorie-dense food. These processes can be linked to several factors, such as changes in lifestyle and in the economy.
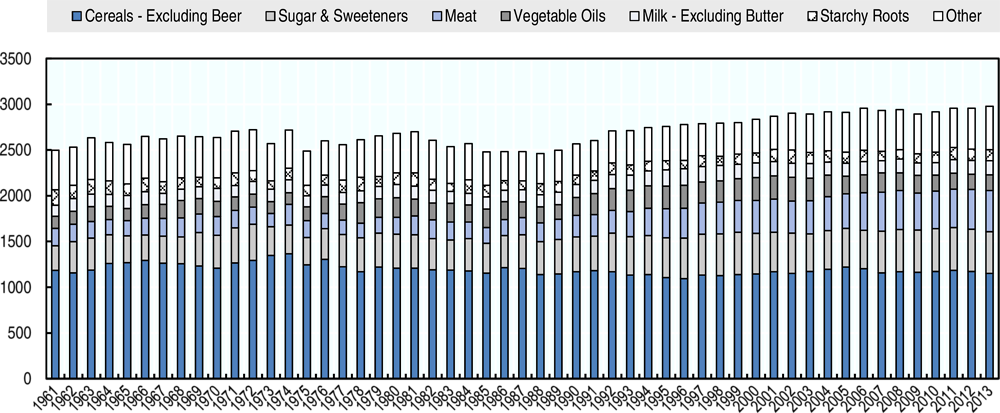
Since 1961, total food availability has increased by nearly 20%, from just under 2 500 kcal/capita/day to nearly 3 000 kcal/capita/day in 2013 (see Figure 2.5). This increase is almost entirely attributable to an increase in calories from animal products (733 kcal/capita/day in 2013 versus 402 in 1961) and sugar and sweeteners (458 kcal/capita/day in 2013 versus 269 in 1961). A higher food energy supply leads to an increase in average population body weight (Vandevijvere et al., 2015[7]).
Figure 2.5. Food supply in Chile (kcal/capita/day)
Other factors have also contributed to this phenomenon. For example, the increased female labour force participation has often been accompanied by an increase in overweight and obesity, as family eating habits change (Philipson, 2001[9]; OECD, 2010[3]). In Chile, the participation of women in the labour force has increased by almost 60% in recent decades. In 1990, 32% of women were active in the labour force, while in 2015, the rate had risen to 51% (ILO, 2015[10]).
While the diet in Chile has been evolving, Chileans have also been shifting towards a more sedentary lifestyle. Total physical activity is usually divided into four main domains: work, transport, domestic and discretionary-time physical activity (Bull et al., 2004[11]). Available evidence suggests that Chileans have been performing less physical activity in at least two of these four domains.
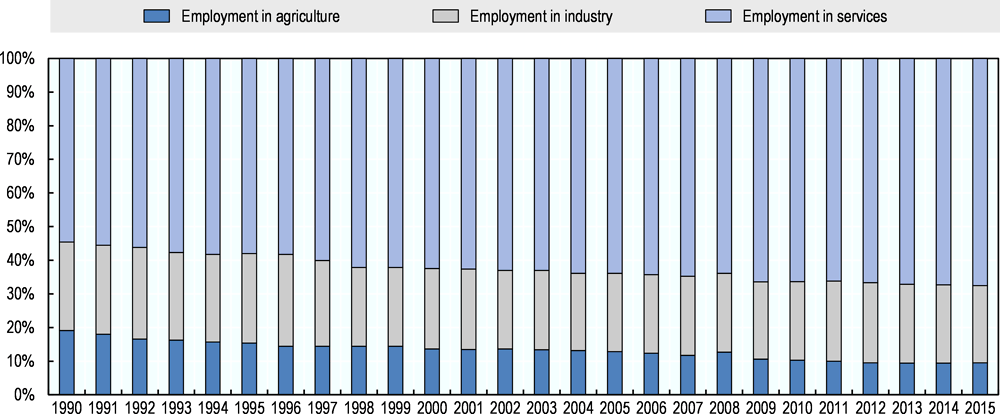
During the last few decades, the Chilean economy has further developed into a service economy. This evolution translates into fewer physically demanding jobs and an increasing amount of sedentary work, such as office jobs (Gendler, 2014[12]; OECD, 2010[3]). Since 1990, the share of jobs in the tertiary sector (e.g. provision of services and utilities) has increased from 55% to 68% (Figure 2.6). The share of jobs in the primary (e.g. agriculture, mining) and secondary (e.g. industry such as processing and manufacturing) sectors, which tend to require a higher level of physical activity, has dropped from 19% to 9% and 26% to 23%, respectively.
Modes of transportation have evolved as well. The number of circulating passenger cars per 1 000 inhabitants in Chile has risen from 71 in 1998 to 171 in 2016 (INE, 2001[13]; 2005[14]; 2007[15]; 2011[16]; 2016[17]; World Bank, 2017[18]). Car ownership is associated with lower levels of walking and cycling transport (Mackett and Brown, 2011[19]), and spending more time in cars has been shown to increase the probability of obesity (Frank, Andresen and Schmid, 2004[20]).
Figure 2.6. Employment by sector
In addition to these macro-economic factors, there also are individual determinants that influence lifestyle and obesity, including housing, education, gender, the environment, income and age. The prevalence of obesity in Chile increases with age. While 24.6% of 20 to 29 year olds is obese, this rises to 41.7% in 50 to 64 years old (Ministerio de Salud, 2017[1]). Women are more likely to be obese than men: in 2016, 38.4% of women in Chile was obese, compared to 30.2% of men (OECD, 2018[22]).
In children on the other hand, a higher prevalence of obesity was found for boys compared to girls (Herrera, Lira and Kain, 2017[23]). Interestingly, the same study found that children from a more vulnerable socio-economic background were less likely to be obese, but this same group also saw the largest increase in obesity between 2009 and 2013.
A study of diet and physical activity identified males under the age of 20, or over the age of 65, who had either a low education or a high socio-economic status, as having the least healthy behaviours in Chile when both diet quality and level of physical activity were considered at the same time (Graf and Cecchini, 2018[24]). When looking at diet specifically, people aged 20 to 64 with a low or medium socio-economic status and medium or high education had the lowest quality diet.
2.3. Chile has put in place a comprehensive policy package to tackle obesity
There is a wide range of policies and interventions that governments can use to tackle obesity, from population-level fiscal policies to individual-level counselling interventions. Combining different approaches in a multi-intervention strategy, targeting different population groups and settings, significantly enhances the impact on health (OECD, 2010[3]).
Chile has sought to address high obesity levels by implementing a wide-ranging portfolio of actions to address the main causes of obesity: physical inactivity and in particular unhealthy diets, taking a social determinant approach (see Figure 2.7). At the national level, mass media campaigns are being used to educate the public on healthy choices. National laws on marketing, labelling and sugar taxes have been implemented in an effort to improve diets. At the regional level, city-wide programmes are bringing together different stakeholders to deliver multifaceted interventions, and to transform local spaces. Schools and work places are also involved to create healthy environments for their students and employees. Finally, primary care plays a key role in delivering individual interventions to high risk people.
Figure 2.7. Chile’s policy package to tackle obesity
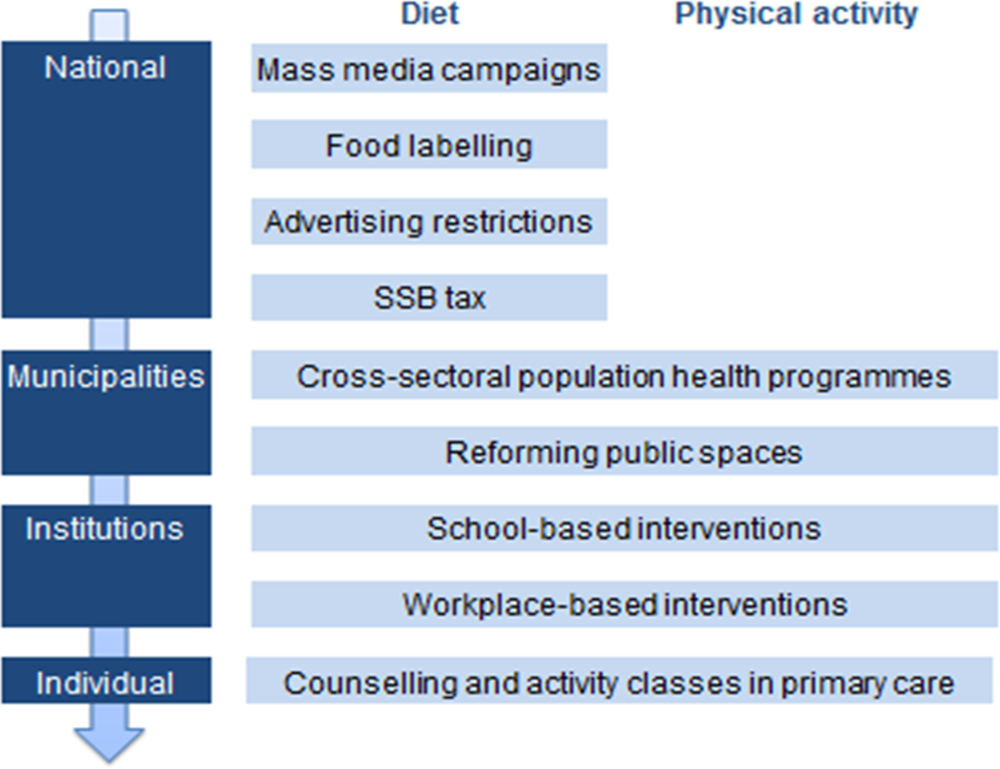
Source: Author’s elaboration
2.3.1. Mass media campaigns have played a part in Chile’s prevention strategy
Mass media campaigns are an important part of a public health strategy. To improve diets, many countries have run campaigns focused on increasing the consumption of fruit and vegetables. Rather than telling the public what they should not do, these campaigns present a positive message.
In 2004, Chile launched a major campaign to promote the consumption of 5 portions of fruit and vegetables a day (Hawkes, 2013[25]). The campaign is run by the 5-a-Day Corporation, a not-for-profit organisation set up by the Institute of Nutrition and Food Technology, other academic institutions, and private sector organisations such as the Association of Supermarkets.
The campaign includes a website, twitter messages and advertisements on radio and television. The 5-a-Day Corporation also creates a range of educational materials, including posters and leaflets, and coordinates education at supermarkets, workplaces and in schools (Zacarías et al., 2006[26]). The campaign has produced several popular recipe books, in cooperation with the Ministry of Agriculture.
Another mass media campaign was launched to promote the newly introduced warning labels on food. This campaign lasted for one month, and saw spots aired 3 to 4 times a day on television and 10 to 12 times a day on the radio. The high cost of this campaign (ca. 500m pesos or 650k Euros) has led the Ministry to review other options for future campaigns, including online video website YouTube.
2.3.2. Chile’s threshold values for food warning labels are among the strictest in the world
Many countries have introduced front-of-package food labelling schemes, to help the public make healthier choices when buying food. The majority of these programmes are voluntary schemes, where producers are incentivised to produce healthy products which are rewarded with a ‘healthy choice’ or ‘low in …’ label. A few countries have introduced mandatory warning labels, such as Finland the ‘high in salt’ label, and Chile’s new labelling scheme.
In 2016, a mandatory food labelling system took effect in Chile that uses four black labels to indicate whether a certain foodstuff is high in calories, salt, sugar or fat (see Figure 2.8) (Ramirez, Sternsdorff and Pastor, 2016[27]). The labels only apply to packaged food, and are not required for bulk goods or unpackaged food, including bread and fast food.
Figure 2.8. Chile’s food labels

Source: Chile Ministry of Health.
The thresholds for the labels are being introduced in a phased design, with increasingly strict targets set at 24 and 36 months after implementation. The final thresholds, which will come into force in 2019, are ambitious compared to other international labelling standards (see Figure 2.9). Finland also introduced mandatory warning labels for products high in salt in 1993, tightening the threshold for various products in 2009 (Sarlio-Lahteenkorva, 2015[28]). In 2016 the limits were re-evaluated in light of new EU regulation on food labelling. However, both Finland’s historic and current limits are higher than the thresholds that Chile will use after 36 months.
Figure 2.9. Comparison of food warning label thresholds
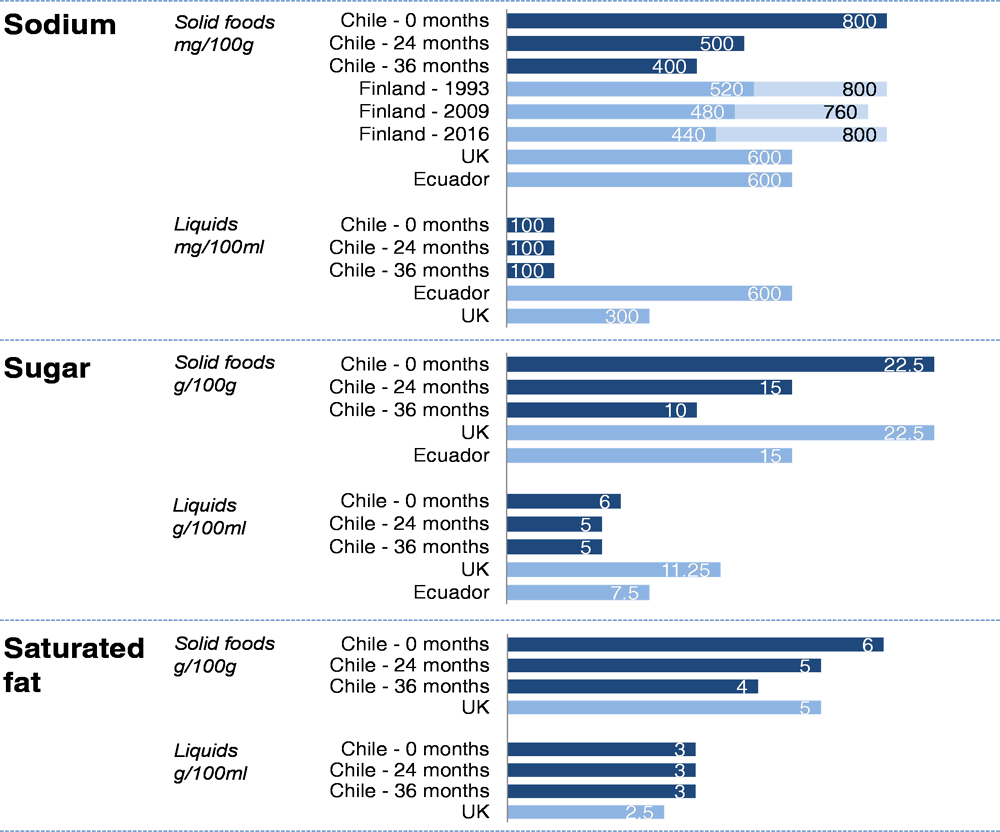
Note: Values for UK and Ecuador are for the ‘red’ or ‘high’ label; Finland has set different sodium thresholds for different products, ranging from 440mg/100g for bread to 800 mg/100g for crisp bread, cheese and breakfast cereals.
The labels do not only function to encourage consumers to make healthier choices, but also determine where and how a product can be marketed and sold. Products that carry a warning label cannot be sold or advertised in schools, nor can they be advertised to children under 14. They cannot be given away for free, or accompanied by presents such as toys or games (Ramirez, Sternsdorff and Pastor, 2016[27]).
Enforcement of the policy is done regionally. The Regional Ministerial Secretariats (SEREMI) of Health are tasked with monitoring food products through random testing, sampling a higher number of food products aimed at children. In the first year, 3000 inspections took place, 28% of which identified issues with either the ‘high in’ label, or its advertisement to children or sale within schools (Ministerio de Salud, 2017[34]). The majority of the resulting 524 judgements were warnings and admonitions (91%), but they also included fines (7%) and sales prohibitions (0.6%). 1.5% was dismissed.
Testing is not limited to a review of the nutritional label but includes chemical analysis of the food. The Ministry of Health conducts annual reviews of nutrient labels for a selection of food products that are widely consumed, or that have previously been shown to misrepresent their nutritional composition. The 2017 report shows that, of the 41 products tested, 78% had an accurate label (Ministerio de Salud, 2017[35]). In 23.3% of the samples analysed for sugar the actual content was higher than the reported content by 20% or more. The same was found for 20% of samples analysed for salt content, and 33% of energy content samples. It is important to note though that the products sampled had a higher risk of misreporting, and the overall prevalence may therefore be lower. In addition to these checks, citizens can also report complaints or misuse of the labels (Box 2.1).
Box 2.1. The role of civil society in monitoring food labels
In response to the new food labelling laws introduced in 2016, Chile’s national consumer organisation, Conadecus, announced the launch of the Observatory for Food and Advertising. This observatory will regularly review food labels, ingredients and nutritional composition of food products, and advertising practices, to assess whether or not they comply with national regulations. Their aim is to improve transparency for the customers, and increase compliance by providing recommendations to the Ministry of Health.
The involvement of public interest watchdogs in enforcing labelling standards has been instrumental in other countries. In Denmark, independent consumer rights organisation Taenk has taken on a similar role. After discussions with producers did not result in any changes, Taenk brought complaints on 26 products and their labels to the Danish Veterinary and Food Administration. Foodwatch in the Netherlands, an organisation independent of the government and food companies, organises an annual competition where 24 000 consumers vote for the most misleading health claim on a food product. Presented in an entertaining and amusing way, the aim of this campaign is to make consumers more critical of health claims and food labels.
In addition to consumers, other civil society groups can also be involved. For example, a greater involvement could be envisaged for patients associations, medical societies and other relevant groups of stakeholders depending on the matter under discussion. However, civil society in Chile tends to be arranged in small organisations, which limits their ability to influence and support public health objectives.
The policy has already had an impact. An evaluation by the Ministry of Health found that 44% of consumers used the labels to compare products, and 92% of them were encouraged to buy less or to buy different products (Ministerio de Salud, 2017[34]). In addition, the industry has responded to the policy by reformulating products and introducing alternatives that are below the label threshold. Nestle, for example, has changed the recipe of popular breakfast cereal Chocapic to include artificial sweetener Stevia, in addition to reducing the sugar content by 25% over the last five years (Nestle, 2017[39]).
However, there are some limitations of the policy. For bottles and other non-square packaging the label can be printed towards the side of the front label, potentially obscuring it if the product is slight rotated when displayed in store (Castro Villarroel and Medel Valdivia, 2017[40]). Including the label on the front and the back of the product could help address this issue. The law is also currently limited to pre-packaged, non-alcoholic food and beverages. Expanding it to include more products such as bread, fast food and alcoholic beverages would level the playing field between products and could inform the public about the nutrient profile and calorie impact of these products.
2.3.3. Chile has implemented comprehensive regulations to restrict the marketing of unhealthy foods to children
Advertisement of unhealthy products can have a strong influence on diets, and the WHO has developed guidelines on the marketing of food and drinks to children (World Health Organization, 2010[41]). Countries are encouraged to reduce the exposure of children to marketing of foods high in saturated fats, trans-fatty acids, free sugars, or salt.
Chile has implemented regulation to curb the advertisement of unhealthy foods. Marketing regulations currently fall under two laws. The first forbids all marketing of unhealthy food with “high in” labels directed at children under 14, in all places (including the internet), through all means, and at all times. The second law, which complements the first one, prohibits marketing to all audiences of food with labels between 6am and 10pm on TV and in cinemas. The definition of marketing directed at children includes advertisement with children, with the voices of children, with music for children, or depicting a place for children (e.g. schools); or when a television audience consists of more than 20% children.
To ensure compliance, the Ministry of Health works with the National Television Council, the National Consumer Service and the Ministry of Education (Ministerio de Salud, 2017[34]). In November of 2016, the National Consumer Service sued three multinational food companies for their breakfast cereal mascots which they claimed breached the ban on advertising foods with labels to children, requesting fines of USD 90 million for each (Servicio Nacional del Consumidor, 2016[42]). In March 2017, fines of more than USD 10 million were requested for another four companies (Servicio Nacional del Consumidor, 2017[43]). However, the Court of Appeals and, later, the Supreme court have dismissed the cases and ruled that the enforcement of the labelling law is up to the SEREMI and not the courts (La Tercera, 2017[44]) (La Tercera, 2018[45]).
The ban is difficult to monitor and enforce for the Ministries. The central government checks audience composition of television, radio, press, magazines, and internet content by working with tracking systems such as Megatime and Admetricks. However, the use of internet among children is less easy to monitor. This is a major issue as studies in other countries have shown that children’s websites are a prime target for food advertisements (Ustjanauskas, Harris and Schwartz, 2014[46]).
In addition to regulating screen and print marketing, Chile has also restricted outdoor advertising and the law includes a ban on advertising unhealthy foods inside schools. Legislation banning outdoor marketing of unhealthy products one block around schools has been adopted by 10 municipalities, and is being considered by another 200 of the 350 municipalities in Chile.
2.3.4. The implementation of a sugar-sweetened beverage tax shifted consumption towards low-sugar products
In October 2014, Chile also introduced a SSB tax as part of the tax reform (Reforma Tributaria), which came into force in September 2016. Prior to the reform, all SSBs were taxed at 13%. After the reform, the tax became dependent on the amount of sugar in the beverage: SSBs with more than 6.25gr of sugar/100ml (or 15gr/240ml as stated in the law) are taxed at 18%, while SSBs below this threshold are taxed at 10%.
An official evaluation of the policy was conducted by the University of Chile, the Catholic University of Chile, the University of Santiago and the University of York. They found that the change in tax resulted in a 3.4% decrease in household purchases of high-sugar SSBs, while the volume of low-sugar SSBs purchased increased by 10.7% (Caro et al., 2018[47]).The Treasury has said that the current level of taxation of SSBs has had no negative impact on employment, which is consistent with evidence from Mexico (Guerrero-López, Molina and Colchero, 2017[48]).
This evaluation did not however look at the behaviour of the producers of SSBs. The introduction of a tax can incentivise the reformulation of SSB products to decrease sugar content. In the United Kingdom for example, the expected revenue from the Soft Drink Industry Levy was reduced by more than half as manufacturers reformulated their drinks to avoid a higher tax rate (Government of the United Kingdom, 2018[49]).
2.3.5. Municipalities play an important role in delivering cross-sectoral population health programmes
Non-communicable diseases, including obesity, are the result of a large number of determinants. Some of these can be addressed through healthcare, but many lie beyond the remit of the Ministry of Health. Housing, income, education and the environment all influence diet and exercise, but are governed by policies from the ministries dealing with education, agriculture, finance, housing, urban development and social services. Greater collaboration across ministries holds the potential for better incorporation of health objectives in policy making across government departments.
Chile has a decentralised administration, and the responsibility for delivering education, social services, primary health care, parks and recreation all lie with the municipalities. As a result, the municipalities are uniquely positioned to develop cross-sectoral programmes. They achieve this by developing Community Health Promotion Plans which focus on the wider determinants of health (Ministerio de Salud, 2014[50]).
An example of a population health initiative at the regional level is the Santiago Sano programme, in Chile’s capital city Santiago (see Chapter 1). This programme delivers interventions on alcohol, sexual health, physical activity for the elderly, and childhood obesity (Box 2.2), by bringing together stakeholders from every municipal department into 40 dedicated committees. Through cross-sectoral collaboration, the programme was able to create community gardens, launch healthy food stalls, run workshops, and change physical education in schools, amongst other things.
Non-health initiatives at the local level can have an important impact on population health. The Ministry of Housing and Urban Development-led “I Love my Neighbourhood” programme was introduced in 2006 to counter the deterioration of neighbourhoods, recover social spaces and strengthen the social fabric (Ministerio de Vivienda y Urbanismo, 2016[51]). Their work reviving neighbourhoods also created new outdoor space and communal gardens, which contribute to physical activity and healthier diets.
Box 2.2. Tackling childhood obesity in Santiago
In Chile’s capital city of Santiago the city Mayor and her administration have made reducing childhood obesity a policy priority. In 2016 the Mayor’s office developed a plan to galvanise school communities to play a bigger role in reducing childhood obesity. This plan was developed in the context of Bloomberg Philanthropies’ ‘Mayor’s Challenge’ and Santiago was one of five Latin American prize winners.
Out of this approach grew the ‘Juntos Santiago’ (Together Santiago) which is part of the Santiago Sano programme. Juntos Santiago aims to reduce obesity rates in Santiago schools and neighbourhoods through gamification, involving children, parents, teachers and communities who compete to win prizes for completing healthy challenges.
Participating schools and neighbourhoods compete in three types of challenges: choosing healthier food options, a step challenge, and a healthy activity challenge where children compete in local sporting and exercise events. By completing the health challenges schools or neighbourhoods win points, which can be used for prizes such as family activities or cooking courses.
A second wave of implementation aims to broaden the programme scope, for example rewarding expanded sport and health transport options or the creation of school gardens. An online platform was also developed to allow groups to track their progress and communicate with other participants, and where schools can communicate with parents.
2.3.6. Chile is taking steps to transform public spaces to encourage physical activity and healthy diets
Another example of a cross-sectoral programme is the Elige Vivir Sano en Comunidad (Choose Healthy Living in the Community) initiative. This programme is run by the Ministry of Social Development, but supported by the Ministries of Health, Education, Labour and Social Welfare, Housing, Sport and Finance (Ministerio de Desarrollo Social, 2017[54]). Under this programme, a number of initiatives have been implemented that aim to create a healthier environment, which promotes and enables an active lifestyle.
The Health Squares initiative aims to provide the public with places to exercise. The programme runs an interactive map of outdoor exercise locations. These Health Squares have a range of exercise equipment and can be used free of charge by the public. For the Open Streets initiative, designated roads and streets are temporarily closed for motor traffic, and opened up to the public for jogging, cycling and walking. Games and workshops are also organised in the streets to get people active.
The CicloRecreoVia programme is developing routes which are exclusive to cyclists, to stimulate the active transport in the population (CicloRecreoVia, 2017[55]). While currently there are a number of separate cycling routes, the goal is to create a single Metropolitan Cycle Road, to connect all the neighbourhoods of Santiago and allow people to cross the entire city. The cycling routes are available on Sundays, and every weekend 40 000 people make use of them (CicloRecreoVia, 2017[55]).
To encourage healthier diets, food markets have been established to promote the consumption fresh local products. Where previously there were so-called ‘food deserts’ – places where no healthy foods could be purchased – this initiative creates an environment that support a healthy lifestyle. This programme is run in close collaboration with the Ministry of Agriculture (Box 2.3).
Box 2.3. The role of the Ministry of Agriculture – Ensuring access to healthy food
The Ministry of Agriculture in Chile reports three main objectives: 1. To ensure food production; 2. To ensure the quality of food produced; 3. To ensure access to food. They provide technical and financial support to producers, in particular small- and medium-sized producers, with the objective of increasing the production and increase export. The Ministry is also involved in a number of programmes with strong links to public health:
The Ministry supports ‘rural markets’, to facilitate the sale of fresh local products produced by small producers. In particular, they try to reduce the food chain from producers to consumers; to work with municipalities to identify places for the markets; and to support producers with the preparation of documents. Fruits and vegetables sold at these markets are cheaper than in supermarkets, and they are located to decrease food deserts.
About 10 years ago, the Ministry launched a programme bringing together public institutions and private industry, working together to promote reformulation toward healthier products, focusing on sausages, jam, and cheese.
The Ministry of Agriculture works together with the Ministry of Health and of Education to improve diets in schools. For the Contrapeso programme, the Ministry of Agriculture supports schools in finding local providers of healthy produce.
2.3.7. A comprehensive portfolio of school-based interventions has been developed to improve diet and exercise in students
As shown in Figure 2.2, Chile has the highest rates of childhood obesity among OECD countries, and this rate is growing (OECD, 2017[56]). The impact of childhood obesity on later health is significant, and interventions to curb this rising tide are therefore crucial. Schools play an important role in fighting childhood obesity, by providing children with a healthy environment and by educating them on healthy lifestyles.
Chile has implemented a comprehensive school-based intervention on obesity. The Contrapeso programme aims to promote healthy eating and physical activity among school children (JUNAEB, 2016[57]). It is managed by the governmental organisation JUNAEB (the National Board of School Aid and Scholarships), which is responsible for the welfare of students from primary school to university. JUNAEB is part of the Ministry of Education, but the Ministries of Health, of Sport and of Agriculture also contribute to the design and running of the programme.
The Contrapeso programme consists of 50 measures, including:
A restriction on the sale of unhealthy products in schools. School cafeterias and vending machines are prohibited from selling products that carry the “high in” black label (see section on food labelling). In addition, the school food programme managed by JUNAEB was reformulated to contain less sugar, sweeteners and salt, and more fruit, vegetables and whole grains.
Increasing the healthy food choices available for the BAES card. Approximately 500 thousand students attending high school are entitled to a special card which they can use to buy food. The Contrapeso programme is working to restrict the use of this BAES card to healthy options only, and to increase the number of outlets where the card can be used.
Bracelets to monitor physical activity. Students receive a bracelet which counts steps and analyses sleeping time, to encourage them to reach physical activity targets. The programme also promotes gamification, by providing resources for teachers to develop games and competitions using the bracelets (Box 2.4).
Involving the family. Rather than focusing only on the school environment, the Contrapeso programme engages parents to improve students’ lifestyle outside of school and to develop role models. Families can participate together in educational workshops, and school menus and nutritional information are available online for parents.
JUNAEB has a budget of about USD 1 billion, 70% of which is spent on providing food in schools or to top-up BAES cards. JUNAEB also provides computers for students, and the physical activity bracelets. According to JUNAEB, the implementation of the Contrapeso programme, including changes in the food canteens and the provision of the physical activity bracelets, did not produce any substantial change in the annual budget as all the improvements have been implemented following contract negotiations with manufacturers and suppliers.
The Contrapeso programme was launched in 2016, and is currently being implemented in phases. Participation is compulsory for public schools and for publicly subsidized schools. By the end of 2019, 11 000 schools and 1.8M students in Chile will be covered by the programme. However, in its current form private schools are not included in the programme, which account for about 20% of students.
Box 2.4. Increasing physical activity through gamification
What is gamification?
Gamification in its broadest sense refers to the use of game design elements in non-game contexts. In healthcare specifically, it has become a popular method to promote behaviour change. By creating a game around healthy behaviour, these interventions aim to increase motivation and sustain habits. Generally, gamification refers to interventions that involve some form of technology.
What types of gamification exist?
Different technology platforms are being used for gamification in healthcare, including traditional gaming consoles (e.g. motion-controlled ‘exergames’, where players have to exercise, jump and dance to control their avatar onscreen), smartphones (e.g. apps which can be used to track a run and compare the distance and route to other users) or dedicated physical activity monitors (e.g. activity bracelets, which awards badges when the individual reaches a goal number of steps for the day).
Games encourage healthy behaviours in various ways. They can provide the capacity to monitor and improve lifestyle, for example by counting steps or by educating. They can also increase motivation, by creating goals, giving out incentives such as badges, or by providing social support. Finally, games can provide the opportunity or trigger needed to make changes in lifestyle, through competition and peer pressure, or reminders and alerts.
Does gamification work?
Gamification in healthcare is a relatively new concept and there is no definite answer yet on its effectiveness in changing behaviours. Nevertheless, a number studies have reported encouraging results that show gamification interventions can increase physical activity, improve diets, contribute to weight loss and increase adherence to online programmes. For example, one study, looking at the gamification of dietary decision-making in school cafeterias through a competition, showed an increase in fruit and vegetable consumption of 66% and 44% respectively. Another intervention delivered through a social network app increased weekly moderate-to-vigorous physical activity in adults by 135 minutes versus a control group. However, the long-term impact of these interventions requires further research.
2.3.8. Voluntary workplace interventions are incentivised through accreditation
Obesity influences the performance of employees, and can lead to absenteeism and presenteeism (OECD, 2010[3]). It is therefore in the employers’ best interest to invest in the health of their workforce. Considering the large amount of time spent in the office, workplace-based interventions can have a considerable impact on overweight and obesity. Employers can create incentives for healthy behaviours; design a healthy workplace with healthy food options and opportunities for exercise; or generally encourage a culture of health (Heinen and Darling, 2009[65]).
While Chile does not have a centrally mandated workplace-based programme, the Chilean government has supported the implementation of voluntary actions in workplaces. So far, about 200 to 250 workplaces have implemented interventions including dedicated walking breaks, physical activity courses, and bicycle parking spaces.
There is no economic incentive associated with the interventions, but organisations can apply for an official certification (SEREMI de Salud O'Higgins, 2013[66]). Companies that conduct an internal review to identify improvement opportunities and develop an improvement plan can become an accredited Workplace Health Promotor (Lugares de Trabajo Promotores de Salud). This certification, and the positive publicity associated with it, functions as an additional incentive for companies to invest in the health of their employees.
The government could develop policies to encourage the implementation of workplace-based health and lifestyle interventions. In the USA, the Affordable Care Act permits employers to provide discounts of up to 30% on healthcare coverage charges to employees who participate in wellness programmes (US Department of Labor, 2014[67]). In addition, the government could provide subsidies, support research and improve dissemination into effective wellness schemes (Goetzel, 2016[68]).
2.3.9. Primary care plays a key role in delivering counselling and physical activity classes
In many OECD countries, the primary care physician functions as a first point of contact in case of illness, and a trusted source of information (OECD, 2010[3]). They are in a unique position to advise patients on healthy diet and exercise. Structured counselling programmes, delivered by primary care physicians and dieticians, have been proven to significantly reduce fat intake and BMI. Chile has a strong primary care system, which plays a key part in the obesity strategy through the Vida Sana programme.
The Vida Sana counselling and physical activity programme was started 10 years ago as a pilot, and has been part of the national prevention package in Chile since 2014. To date, there are about 300 teams delivering this intervention throughout Chile. This one-year programme aims to improve physical activity and diet in patients with obesity, or overweight patients with other risk factors. Participants receive individual and group counselling sessions with nutritionists and psychologists. To contain the delivery cost, medical doctors are only involved if the patient specifically requires medical attention (e.g. in case of diseases). In addition, patients complete 144 hours of physical activity in classes guided by a physical education teacher, physical activity therapist, or kinesiologist (Ministerio de Salud, 2015[69]).
While the sessions take place in primary care centres, the programme is completely independent and run by dedicated councillors. The costs of the intervention, around USD 119 per participant per year, are covered by the national health fund (FONASA). In 2015, 54 529 people participated in the programme, accounting for 6% of the potential target population of 870k people (DIPRES, 2016[70]). To these participants the programme delivered nearly 500k activities, including 164k consultations with dieticians, and 127k physical activity classes.
Despite the high cost associated with the programme, there is reason to believe that it is cost-effective. Intensive counselling interventions combining primary care physicians and dietician are known to be high-cost, but they also have the largest impact in terms of DALYs saved (OECD, 2010[3]). As such, they may also be of interest to the private health insurers (Box 2.5).
Box 2.5. The role of private health insurance schemes
Private insurers (ISAPREs) currently play only a marginal role in prevention, despite covering about 15%-18% of the population. According to the Association of ISAPREs, 10% of individuals change their insurance scheme each year – reducing the incentive as well as the opportunity for individual providers to invest in prevention and public health initiatives. In addition, as the ISAPREs can unilaterally charge a risk-rated premium, the large majority of elderly patients are covered by the public FONASA. This further reduces the incentive for the ISAPREs to invest in prevention and healthy aging.
Some ISAPREs have nevertheless experimented with interventions in this area. One organisation tested a diabetes programme that provides individuals at risk with a funded savings account, which tops up as patients comply with certain pre-determined activities. This funding could be used later in life to cover medical treatment. Conversely, ISAPREs report that all the previous attempts to implement tertiary prevention programmes, empowering patients to limit further disease development, did not bring the expected results and were discontinued. The Association of ISAPREs has, however, indicated that it would support reforms and governmental action that would increase their involvement in public health.
In other countries, private insurers have invested in prevention to reduce cost. For example, in Germany, private insurers or sickness funds are required by law to develop and offer Disease Management Programmes (DMP), which aim to improve coordination and enhance quality of care for the chronically ill. Sickness funds receive incentives for establishing DMPs and enrolling patients. While insurers are free to design their own DMPs, they need to be validated by the Federal Insurance Agency. In 2012, it was estimated that 70% of all diabetic patients were enrolled in a DMP. Diabetic patients enrolled in a DMP were shown to have a lower hospitalisation and mortality rates, and to have lower cost: €122 per patient, including DMP administration and service costs, versus €169 for controls.
Private health insurers in Chile would benefit from primary prevention interventions to tackle unhealthy behaviours and to promote an active lifestyle. Available evidence suggests that private health insurers can expect reduced hospital and drug expenditure. Part of these savings could then be used to kick-start DMPs, which would sustain further reductions in expenditure.
Sources: (Cecchini and Sassi, 2015[71]; OECD/WHO, 2014[72]).
2.4. Further policies can be implemented or expanded to enhance Chile’s current obesity strategy
Chile has put in place a large range of interventions and programmes to curb the rise of obesity. Taxation of sugar-sweetened beverages has been implemented to reduce the consumption of these drinks, strict labelling regulation has driven the reformulation of unhealthy food products, and the primary care service in Chile is playing a vital role in delivering prevention programmes.
The Ministry of Health is already working with other Ministries and stakeholders on several initiatives, but there remains scope to do more. The Ministry has indicated an aspiration to further strengthen the collaboration with the Ministry of Education to increase physical activity levels in schools. It is also important to engage the private health insurers, who are a key stakeholder in both delivery of and benefiting from prevention.
However, a number of further steps could still be taken to improve, complement or expand the current strategy on obesity.
2.4.1. Nutritional labelling policies could be strengthened and expanded to include other products and settings
Chile is ahead of the trend with its strict labelling laws. The use of simple front-of-package warning labels, as has been implemented in Chile, prompts a higher response rate from consumers than a list of nutrients (OECD, 2017[56]). In addition, the scheme has already proven effective in incentivising the reformulation of unhealthy products.
The current labelling programme can be strengthened in a number of ways to increase its impact. The warning labels could be included on both the front and back of packages, to ensure they are clearly displayed at all times. The labelling law can also be extended to cover alcohol products, to create a level playing field for all food and drink products and increase public awareness about the caloric content of alcoholic beverages and. For example, one study found that 16% of consumers said they would reduce their alcohol consumption if calorie information was provided (TNS European Behaviour Studies Consortium, 2014[73]).
In a number of OECD countries, including Canada, Mexico and the United States, it is mandatory to provide nutritional information in certain cases, for example for alcoholic beverages with additives such as sweeteners, for non-standard or prepared beverages, or for beverages which carry a nutritional claim (International Alliance for Responsible Drinking, 2017[74]).
Chile could consider implementing additional labelling regulation that applies to other settings. For example, the labelling laws could be expanded to include menus in chain restaurants, as has been done in states and cities in the USA, Canada and Australia, or to prepared, take-away food (OECD, 2017[56]).
2.4.2. The ISAPREs could play a more active role in the prevention and management of obesity
While private insurers play an important role in Chile’s healthcare system, they are less involved in obesity prevention. Private insurers should play a more active role in promoting healthy behaviours and preventing the complications of chronic diseases. An example of a prevention programme managed by a private health insurer is the Vitality programme, which is run by South Africa's largest private health insurer, Discovery Health (Lambert and Kolbe-Alexander, 2013[75]). This incentive-based programme is based on four pillars: assessment and screening, healthy choices, health knowledge, and physical activity. Beneficiaries are encouraged to participate in different activities such as health checks and visits to dieticians through a points system. In addition, gym memberships are subsidised, and fruit and vegetable purchases are eligible for a 25% cash rebate. The cash rebate has been effective in increasing expenditure on healthy foods by 9.3%, and decreasing spend on less healthy food by 7.2% (Sturm et al., 2013[76]). The Vitality programme has resulted in a reduction in medical claims for Discovery Health, thus providing a direct incentive for private insurers to invest in prevention.
The ISAPREs should be encouraged to play a more active role in promoting healthy behaviours and preventing the complications of chronic diseases. For the ISAPREs, offering an attractive prevention and promotion package to enrolees – for instance following the Vitality programme model – could give a competitive advantage. If this is insufficient, the Ministry might look for ways to incentivise greater engagement by the ISAPREs.
In addition, the Ministry could consider including basic prevention services with proven effectiveness and a high return on investment in the minimum package of services that ISAPREs are required to deliver. For example, marketplace healthcare plans offered under the US Affordable Care Act are required to offer cholesterol and diabetes screening, as well as diet and obesity counselling (U.S. Centers for Medicare & Medicaid Services, 2017[77]). As coverage providers for close to 20% of the Chilean population, the ISAPREs should expect to become a more active partner in the effort to reduce obesity.
2.4.3. The successful school-based programme could be expanded to include more measures, cover more schools, and extend to other sectors
Addressing the growing rate of childhood obesity is vital for Chile. The Contrapeso programme in Chilean schools delivers a wide range of interventions to improve diets, physical activity and health education in students. This successful programme could be further expanded to increase its impact across society.
In addition to banning the marketing and sale of unhealthy foods in school, these activities also might be restricted around schools. Some municipalities have already banned outdoor advertising around schools, and these initiatives should be evaluated to determine the effectiveness. If they are proven to have an impact, the Ministry could work with the other municipalities to extend this programme to all regions.
The existing programme should also be extended to private schools, either through a voluntary agreement or as part of their accreditation. Currently about 80% of students (i.e. all students attending a public school or a school receiving funding from the government) is covered. Extending the programme to private schools would result in virtually universal coverage of children.
The healthy food programme implemented at schools could be further extended to other places, such as the army and all the canteens in public institutions. In a second stage, the programme could be also cover food vouchers provided by employers. Lunch or meal vouchers are given to employees to buy food at lunchtime in restaurants and other outlets near work. While these were originally a means to fight malnutrition, they can also be used to fight overweight (Wanjek, 2005[78]). Restricting the use of these vouchers to healthy food options, similar to the credit cards given to students, would improve the diets of employees.
2.4.4. Physical activity interventions could be expanded and better coordinated to complement the policies on diet
The current obesity strategy in Chile encompasses a wide range of interventions to improve the diet of Chileans. However, the policies on physical activity show some room for improvement. While there exist physical activity initiatives at the local level, there seems to be a weaker central coordination and strategy. Especially since physical activity promotion is dependent on a large number of sectors (including housing, urban planning, education and transport), developing a cross-governmental strategy is crucial to ensure effectiveness and sustainability (OECD/WHO, 2015[79]).
To provide a coordinated approach to physical activity, the government of Slovenia has developed the National Programme for Nutrition and HEPA (Health-enhancing physical activity) 2015—2025 (WHO, 2015[80]). Led by the Ministry of Health, the programme also involves around 16 other Ministries and administrative agencies and institutes, as well as NGOs and professional associations. The programme invests in green open spaces for recreation and organised sports activities; promotes walking, cycling, and hiking in nature; promotes active transport; and ensures the availability of high-quality sports and HEPA programmes.
The use of active transport is an area where Chile could also increase its efforts. The central government could incentivise and support the local implementation of schemes that provide bicycles, improve road safety or encourage active transport. For example, the Smarter Choices, Smarter Places programme was set up by the Scottish government, and provides funding for local initiatives that aim to increase the uptake of walking, cycling and the use of public transport (Norwood et al., 2014[81]). The programme funds the implementation of infrastructure and transport facilities, but also campaigns and training events.
2.4.5. Monitoring and evaluation are key to ensure Chile’s strategy is effective
Chile’s obesity strategy is multifaceted and includes many different stakeholders, interventions, target populations and outcomes. To assess the effectiveness of the implemented policies and to measure achievements, Chile should put in place rigorous monitoring systems. Well-designed monitoring systems are also a fundamental tool to support the design of further innovative policies or to address potentially unwanted consequences of policies already in place.
As discussed in Chapter 1, Chile needs to improve the availability of key health data, including data on obesity and overweight. Chile has fairly robust data on child obesity rates, collected by JUNAEB as the Mapa Nutricional, and through regular child health checks especially in infancy. The Ministry of Social Affairs also collects self-reported obesity rates for children in the CASEN survey every 2 to 3 years. In addition, the data from the activity bracelets could provide novel insights into physical activity patterns among school children.
However, data availability for adult health risk factors, including obesity, depends primarily on a periodic National Health Survey. There was no health survey undertaken between 2009 and 2016, which meant that for much of the period in which Chile has introduced its ambitious obesity strategy the impact on population health has been obscured. Regularly updated, robust data on obesity levels in the population will be critical for better tailoring the prevention approach in the years to come. The importance of improving the information availability for public health is further explored in Chapter 1, along with examples of different approaches taken by other OECD countries to collect more regular data.
In addition to information on obesity prevalence, Chile may benefit from having more data and insight into the food environment (e.g. what people buy, where they shop, and what they eat). This data would also allow the government to analyse if people change their habits as a result of the policies that have been implemented.
Chile should take action to rigorously monitor the impact of individual obesity policies. The official evaluation of Chile’s SSB policy by the University of Chile, the Catholic University of Chile, the University of Santiago and the University of York is a good example of an academically rigorous approach to policy review. Other interventions should receive similar reviews to ensure their cost-effectiveness.
Monitoring of the implementation of policies is also vital. The enforcement of the food labelling law, and sales of food in schools, is the responsibility of the SEREMI, who monitor food products according to the guidelines provided by the central government. At a national level the Ministry of Health conducts chemical analysis to verify food labels.
The collection and use of any type of individual-level data needs to be carefully governed to ensure privacy is protected. Putting in place a clear framework for data protection, legislation, an accreditation process, and best practices in data security can help create a high-value, privacy-protective health information system (OECD, 2015[82]).
2.5. Conclusion
Obesity is one of the main risk factors threatening the Chilean population and economy. The rates of adult and childhood obesity are higher than the OECD average and would continue to rise without intervention. Chile has put in place an ambitious set of policy measures to combat the rise of obesity. At the national level, mass media campaigns are used to promote healthy lifestyles. National laws on marketing and labelling provide a strong legislative basis to promote healthier choices. A sugar-sweetened beverage tax has been introduced. In many respects, Chile is at the forefront of international public health policy. As a result, international evidence is not always available on the effectiveness of these policies, making it all the more important that initiatives are properly monitored and evaluated.
Local governments are contributing to the fight against obesity with city-wide and community programmes, which aim to provide more healthy food options and stimulate physical activity. Contrapeso, a programme of school-based interventions, encompasses a wide range of interventions aimed at school-aged children, including education on healthy eating, restrictions on the sale of unhealthy products in schools and increasing the healthy food choices available for school meals. Similarly, workplace-based programmes have also been implemented to promote physical activity at work. Finally, at the individual level the primary care system is playing an important role in providing one-on-one counselling and treatment through the Vida Sana programme.
There are a number of ways in which Chile could further strengthen its portfolio of interventions. Chile could expand some of the national policies to include more products and people. For example, the warning logos could be used on menus and alcoholic beverages. Chile should carefully assess the impact of its SSB tax. The success of the Contrapeso programme could be rolled out in other public settings, such as the army or government organisations. There is also a larger role to play for the private insurers, the ISAPREs. Since 17-18% of the Chilean population is covered by the ISAPREs, they have the potential to make a significant impact on population health. To achieve this, it is important to put in place a mechanism by which the ISAPREs can influence their population’s lifestyle, as well as benefit from the savings.
Underpinning all these efforts should be a rigorous monitoring system. There currently is a lack of understanding of the effectiveness of the different policies, and the overall impact they are having on obesity, related disease and the economy in Chile. Cost-effectiveness studies are needed for the different interventions, as well as more regular data on obesity prevalence in the population and the food environment.
References
[53] Bloomberg Philanthropies (2016), Mayors Challenge, http://mayorschallenge.bloomberg.org/ (accessed on 17 July 2017).
[11] Bull, F. et al. (2004), “Physical Inactivity”, in Comparative Quantification of Health Risks, WHO, Geneva.
[47] Caro, J. et al. (2018), “Chile’s 2014 sugar-sweetened beverage tax and changes in prices and purchases of sugar-sweetened beverages: An observational study in an urban environment”, PLOS Medicine, Vol. 15/7, p. e1002597, http://dx.doi.org/10.1371/journal.pmed.1002597.
[40] Castro Villarroel, P. and L. Medel Valdivia (2017), Informe de vigilancia nutricional en alimentos y su publicidad, Corporacion Nacional de Consumidores y Usuarios, http://www.conadecus.cl/conadecus/wp-content/uploads/2011/09/Informe-FINAL-2.pdf (accessed on 05 July 2017).
[71] Cecchini, M. and F. Sassi (2015), “Preventing Obesity in the USA: Impact on Health Service Utilization and Costs”, PharmacoEconomics, Vol. 33/7, pp. 765-776, http://dx.doi.org/10.1007/s40273-015-0301-z.
[55] CicloRecreoVia (2017), CicloRecreoVía, http://www.ciclorecreovia.cl/que-es/ (accessed on 06 July 2017).
[37] Conadecus (2017), Nutricionista y gestor del Observatorio del Etiquetado Nutricional cuenta los detalles de la iniciativa, http://www.conadecus.cl/conadecus/?p=15196 (accessed on 06 July 2017).
[29] Department of Health (2016), Guide to creating a front of pack (FoP) nutrition label for pre-packed products sold through retail outlets, https://www.food.gov.uk/sites/default/files/multimedia/pdfs/pdf-ni/fop-guidance.pdf (accessed on 05 July 2017).
[58] Deterding, S. et al. (2011), From game design elements to gamefulness, ACM Press, New York, New York, USA, http://dx.doi.org/10.1145/2181037.2181040.
[70] DIPRES (2016), Informe Final de Evaluacion Programa Vida Sana, http://www.dipres.gob.cl/595/articles-149542_informe_final.pdf (accessed on 10 August 2017).
[8] FAO (2017), FAOSTAT Statistics Database, Food and Agriculture Organization of the United Nations, Rome.
[36] Foodwatch (2016), Over misleidende marketing, https://www.foodwatch.org/nl/onze-campagnes/onderwerpen/misleidende-marketing/2-minuten-informatie/ (accessed on 06 July 2017).
[20] Frank, L., M. Andresen and T. Schmid (2004), “Obesity relationships with community design, physical activity, and time spent in cars”, American Journal of Preventive Medicine, Vol. 27/2, pp. 87-96, http://dx.doi.org/10.1016/j.amepre.2004.04.011.
[12] Gendler, A. (2014), The Consequences of an Industrial Food System: A Cross-National Examination of the Role of Mechanization in the Rising Obesity Epidemic, Lehigh University, http://jsaw.lib.lehigh.edu/campbell/gendler_abigail.pdf (accessed on 07 August 2017).
[68] Goetzel, R. (2016), “How Can The Government Improve Prevention Programs In The Workplace?”, Health Affairs Blog, http://healthaffairs.org/blog/2016/09/02/how-can-the-government-improve-prevention-programs-in-the-workplace/ (accessed on 08 August 2017).
[49] Government of the United Kingdom (2018), Soft Drinks Industry Levy comes into effect, https://www.gov.uk/government/news/soft-drinks-industry-levy-comes-into-effect (accessed on 21 September 2018).
[24] Graf, S. and M. Cecchini (2018), “Identifying patterns of unhealthy diet and physical activity in four countries of the Americas: a latent class analysis”, Rev Panam Salud Publica, Vol. 42/e56, https://doi.org/10.26633/ RPSP.2018.56.
[48] Guerrero-López, C., M. Molina and M. Colchero (2017), “Employment changes associated with the introduction of taxes on sugarsweetened beverages and nonessential energy-dense food in Mexico”, Preventive Medicine, Vol. 105, pp. S43-S49, https://ac.els-cdn.com/S0091743517303249/1-s2.0-S0091743517303249-main.pdf?_tid=7df27306-e4b6-11e7-bd3d-00000aab0f01&acdnat=1513685990_d122bc2fa31cea96def7ba26a4b83049 (accessed on 19 December 2017).
[25] Hawkes, C. (2013), Promoting healthy diets through nutrition education and changes in the food environment: an international review of actions and their effectiveness, FAO, http://www.fao.org/docrep/017/i3235e/i3235e.pdf (accessed on 10 July 2017).
[65] Heinen, L. and H. Darling (2009), “Addressing obesity in the workplace: the role of employers.”, The Milbank quarterly, Vol. 87/1, pp. 101-22, http://dx.doi.org/10.1111/j.1468-0009.2009.00549.x.
[23] Herrera, J., M. Lira and J. Kain (2017), “Socioeconomic vulnerability and obesity in Chilean schoolchildren attending first grade: comparison between 2009 and 2013”, Rev Chil Pediatr, Vol. 88/6, pp. 736-743, http://dx.doi.org/10.4067/S0370-41062017000600736.
[6] IHME (2018), GBD Results Tool, http://ghdx.healthdata.org/gbd-results-tool (accessed on 25 October 2018).
[10] ILO (2015), Labor force participation rate, modelled ILO estimates.
[17] INE (2016), Parque de Vehículos, http://www.ine.cl/estadisticas/economicas/transporte-y-comunicaciones?categoria=Anuarios.
[16] INE (2011), Parque de Vehículos, http://www.ine.cl/estadisticas/economicas/transporte-y-comunicaciones?categoria=Anuarios.
[15] INE (2007), Parque de Vehículos, http://www.ine.cl/estadisticas/economicas/transporte-y-comunicaciones?categoria=Anuarios.
[14] INE (2005), Parque de Vehículos, http://www.ine.cl/estadisticas/economicas/transporte-y-comunicaciones?categoria=Anuarios.
[13] INE (2001), Parque de Vehículos, http://www.ine.cl/estadisticas/economicas/transporte-y-comunicaciones?categoria=Anuarios.
[74] International Alliance for Responsible Drinking (2017), Beverage Alcohol Labeling Requirements - Data by Country, http://www.iard.org/policy-tables/beverage-alcohol-labeling-requirements/ (accessed on 14 August 2017).
[59] Johnson, D. et al. (2016), “Gamification for health and wellbeing: A systematic review of the literature”, Internet Interventions, Vol. 6, pp. 89-106, http://dx.doi.org/10.1016/j.invent.2016.10.002.
[63] Jones, B. et al. (2014), “Gamification of Dietary Decision-Making in an Elementary-School Cafeteria”, PLoS ONE, Vol. 9/4, p. e93872, http://dx.doi.org/10.1371/journal.pone.0093872.
[57] JUNAEB (2016), ContraPeso, http://contrapeso.junaeb.cl/ (accessed on 05 July 2017).
[5] JUNAEB (2016), Mapa Nutricional 2016, https://www.junaeb.cl/wp-content/uploads/2017/07/mapa_nutricional_2016_final_Comunicaciones.pdf (accessed on 19 July 2017).
[30] La Ministra de Salud Publica (2013), REGLAMENTO SANITARIO DE ETIQUETADO DE ALIMENTOS PROCESADOS PARA EL CONSUMO HUMANO, http://www.controlsanitario.gob.ec/wp-content/uploads/downloads/2014/08/REGLAMENTO-SANITARIO-DE-ETIQUETADO-DE-ALIMENTOS-PROCESADOS-PARA-EL-CONSUMO-HUMANO-junio-2014.pdf (accessed on 05 July 2017).
[45] La Tercera (2018), Firmas de alimentos ganan en la Suprema por etiquetado, http://www2.latercera.com/noticia/firmas-alimentos-ganan-la-suprema-etiquetado/ (accessed on 20 August 2018).
[44] La Tercera (2017), Dos en Uno y Kellogg’s ganan nueva disputa legal por etiquetado, http://www2.latercera.com/noticia/dos-uno-kelloggs-ganan-nueva-disputa-legal-etiquetado/ (accessed on 20 August 2018).
[75] Lambert, E. and T. Kolbe-Alexander (2013), “Innovative strategies targeting obesity and non-communicable diseases in South Africa: what can we learn from the private healthcare sector?”, Obesity Reviews, Vol. 14/S2, pp. 141-149, http://dx.doi.org/10.1111/obr.12094.
[60] Lister, C. et al. (2014), “Just a fad? Gamification in health and fitness apps.”, JMIR serious games, Vol. 2/2, p. e9, http://dx.doi.org/10.2196/games.3413.
[61] Looyestyn, J. et al. (2017), “Does gamification increase engagement with online programs? A systematic review”, PLOS ONE, Vol. 12/3, p. e0173403, http://dx.doi.org/10.1371/journal.pone.0173403.
[19] Mackett, R. and B. Brown (2011), “Transport, Physical Activity and Health: Present knowledge and the way ahead”, https://www.ucl.ac.uk/news/pdf/transportactivityhealth.pdf (accessed on 08 August 2017).
[64] Maher, C. et al. (2015), “A Web-Based, Social Networking Physical Activity Intervention for Insufficiently Active Adults Delivered via Facebook App: Randomized Controlled Trial”, Journal of Medical Internet Research, Vol. 17/7, p. e174, http://dx.doi.org/10.2196/jmir.4086.
[54] Ministerio de Desarrollo Social (2017), Elige Vivir Sano en Comunidad, http://eligevivirsano.gob.cl/ (accessed on 06 July 2017).
[1] Ministerio de Salud (2017), Encuesta Nacional de Salud 2016-2017 Primeros resultados, http://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf (accessed on 07 June 2018).
[34] Ministerio de Salud (2017), Informe de evaluacion de la implementacion de la ley sobre composicion nutricional de los alimentos y su publicidad, http://web.minsal.cl/wp-content/uploads/2017/05/Informe-Implementaci%C3%B3n-Ley-20606-junio-2017-PDF.pdf (accessed on 24 August 2017).
[35] Ministerio de Salud (2017), Informe de Vigilancia Nutricional Contenido de Nutrientes Críticos en Alimentos Envasados, https://dipol.minsal.cl/wrdprss_minsal/wp-content/uploads/2018/02/Informe-programa-nutrientes-2017.pdf (accessed on 07 June 2018).
[69] Ministerio de Salud (2015), Orientacion programa vida sana 2015, https://www.slideshare.net/drjoseluiscontreras/orientacion-programa-vida-sana-2015-final (accessed on 05 July 2017).
[50] Ministerio de Salud (2014), Orientaciones para planes comunales de promocion de la salud 2014, http://web.minsal.cl/sites/default/files/orienplancom2014.pdf (accessed on 14 August 2017).
[51] Ministerio de Vivienda y Urbanismo (2016), Compilation of Neighbourhood best practices.
[52] Municipalidad de Santiago (2016), Municipalidad de Santiago gana en el Mayors Challenge 2016, http://www.municipalidaddesantiago.cl/municipalidad-de-santiago-gana-el-mayors-challenge-2016/ (accessed on 17 July 2017).
[39] Nestle (2017), Mejora continua de productos, http://www.nestle.cl/nhw/mejora-continua-de-productos (accessed on 10 July 2017).
[81] Norwood, P. et al. (2014), “Active travel intervention and physical activity behaviour: An evaluation”, Social Science & Medicine, Vol. 113, pp. 50-58, http://dx.doi.org/10.1016/j.socscimed.2014.05.003.
[22] OECD (2018), OECD Health Statistics 2018, OECD Publishing, Paris, https://doi.org/10.1787/health-data-en.
[4] OECD (2017), Health at a Glance 2017: OECD Indicators, OECD Publishing, Paris, http://dx.doi.org/10.1787/health_glance-2017-en.
[56] OECD (2017), Obesity Update 2017, http://www.oecd.org/health/obesity-update.htm (accessed on 13 July 2017).
[2] OECD (2015), Health at a Glance 2015: OECD Indicators, OECD Publishing, Paris, https://dx.doi.org/10.1787/health_glance-2015-en.
[82] OECD (2015), Health Data Governance: Privacy, Monitoring and Research, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264244566-en.
[3] OECD (2010), Obesity and the Economics of Prevention: Fit not Fat, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264084865-en.
[79] OECD/WHO (2015), Promoting Health, Preventing Disease: The Economic Case, Open University Press - McGraw-Hill, Buckingham, https://dx.doi.org/10.1787/9780335262274-en.
[72] OECD/WHO (2014), Paying for Performance in Health Care: Implications for Health System Performance and Accountability, Open University Press - McGraw-Hill, Buckingham, https://dx.doi.org/10.1787/9789264224568-en.
[9] Philipson, T. (2001), “The World-Wide Growth in Obesity: An Economic Research Agenda”, Health Econ, Vol. 10, pp. 1-7.
[33] Pietinen, P. (2009), Finland´s experiences in salt reduction, https://ec.europa.eu/health/sites/health/files/nutrition_physical_activity/docs/ev20091021_pietinen_en.pdf (accessed on 16 August 2017).
[27] Ramirez, R., N. Sternsdorff and C. Pastor (2016), Chile's Law on Food Labelling and Advertising: A Replicable Model for Latin America?, LLorente & Cuenca, http://www.desarrollando-ideas.com/wp-content/uploads/sites/5/2016/05/160504_DI_report_food_chile_ENG.pdf (accessed on 05 July 2017).
[28] Sarlio-Lahteenkorva, S. (2015), Reducing salt intake requires national and international efforts, https://eupha.org/repository/sections/fn/Sirpa__Reducing_salt_intake_in_Finland_Milan_2015.pdf (accessed on 04 August 2017).
[62] Schoeppe, S. et al. (2016), “Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review.”, The international journal of behavioral nutrition and physical activity, Vol. 13/1, p. 127, http://dx.doi.org/10.1186/s12966-016-0454-y.
[66] SEREMI de Salud O'Higgins (2013), Lugares de Trabajo Promotores de la Salud, https://promocionsexta.wordpress.com/lugares-de-trabajo-promotores-de-la-salud-ltps/ (accessed on 05 July 2017).
[43] Servicio Nacional del Consumidor (2017), Ley de Etiquetado de Alimentos: SERNAC denuncia a Dos en Uno, Carozzi, Evercrisp y Walmart por incumplimiento a la normativa publicitaria para menores de 14 años, http://www.sernac.cl/ley-de-etiquetado-de-alimentos-sernac-denuncia-a-dos-en-uno-carozzi-evercrisp-y-walmart-por-incumpli/ (accessed on 05 July 2017).
[42] Servicio Nacional del Consumidor (2016), Ley de Etiquetado de Alimentos: SERNAC denuncia a Nestlé, Kelloggs y Masterfoods por incumplir normativa publicitaria para menores de 14 años, http://www.sernac.cl/ley-de-etiquetado-de-alimentos-sernac-denuncia-a-nestle-kelloggs-y-masterfoods-por-incumplir-normati/ (accessed on 05 July 2017).
[76] Sturm, R. et al. (2013), “A Cash-Back Rebate Program for Healthy Food Purchases in South Africa”, American Journal of Preventive Medicine, Vol. 44/6, pp. 567-572, http://dx.doi.org/10.1016/j.amepre.2013.02.011.
[32] Sydan.fi (2017), Suolaa vahemman, http://www.sydan.fi/ruoka-ja-liikunta/suolaa-vahemman (accessed on 16 August 2017).
[38] Taenk (2017), Forbrugerrådet Tænk har anmeldt 26 madvarer for vildledning | Forbrugerrådet Tænk, https://taenk.dk/aktiviteter-og-kampagner/aerlig-snak-eller-ren-salgsgas/forbrugerraadet-taenk-anmelder-14-produkter (accessed on 06 July 2017).
[73] TNS European Behaviour Studies Consortium (2014), Study on the Impact of Food Information on Consumers' Decision Making, https://ec.europa.eu/food/sites/food/files/safety/docs/labelling_legislation_study_food-info-vs-cons-decision_2014.pdf (accessed on 10 August 2017).
[77] U.S. Centers for Medicare & Medicaid Services (2017), Preventive care benefits for adults, https://www.healthcare.gov/preventive-care-adults/ (accessed on 08 August 2017).
[67] US Department of Labor (2014), The Affordable Care Act and Wellness Programs - Fact Sheet, https://www.dol.gov/sites/default/files/ebsa/about-ebsa/our-activities/resource-center/fact-sheets/fswellnessprogram.pdf (accessed on 08 August 2017).
[46] Ustjanauskas, A., J. Harris and M. Schwartz (2014), “Food and beverage advertising on children's web sites”, Pediatric Obesity, Vol. 9/5, pp. 362-372, http://dx.doi.org/10.1111/j.2047-6310.2013.00185.x.
[7] Vandevijvere, S. et al. (2015), “Increased food energy supply as a major driver of the obesity epidemic: a global analysis”, Bull World Health Organ, Vol. 93, pp. 446-456, http://dx.doi.org/10.2471/BLT.14.150565.
[78] International Labour Organization (ed.) (2005), Food at Work: Workplace Solutions for Malnutrition, Obesity and Chronic Diseases, http://www.ilo.org/wcmsp5/groups/public/@dgreports/@dcomm/@publ/documents/publication/wcms_publ_9221170152_en.pdf (accessed on 14 August 2017).
[80] WHO (2015), Slovenia - Physical Activity Fact sheet, http://www.euro.who.int/__data/assets/pdf_file/0007/288124/SLOVENIA-Physical-Activity-Factsheet.pdf (accessed on 09 August 2017).
[21] World Bank (2018), Jobs Data for Chile, http://datatopics.worldbank.org/jobs/country/chile (accessed on 25 October 2018).
[18] World Bank((n.d.)), Population database (indicator), http://data.worldbank.org/indicator/SP.POP.TOTL?locations=CL&name_desc=false.
[31] World Cancer Research Fund International (2017), NOURISHING framework - nutrition label standards and regulation on the use of claims and implied claims on food, http://www.wcrf.org/sites/default/files/1_Nutrition%20labels_Feb_2017_v2.pdf (accessed on 05 July 2017).
[41] World Health Organization (2010), Set of recommendations on the marketing of foods and non-alcoholic beverages to children, http://apps.who.int/iris/bitstream/10665/44416/1/9789241500210_eng.pdf (accessed on 13 July 2017).
[26] Zacarías, I. et al. (2006), “Programa «5 al Dia » para promover el consumo de verduras y frutas en Chile”, Revista chilena de nutrición, Vol. 33, pp. 276-280, http://dx.doi.org/10.4067/S0717-75182006000300010.