In Chile, cancer is the second leading cause of death and could become the first cause in the near future. In order to reduce the disease burden, Chile could do more to prevent many deaths due to cancer through cancer screening and prevention. This chapter describes the epidemiological burden of cancer in Chile, assesses the governance of Chilean cancer care system and public health policies in terms of prevention and early detection of cancer based on cross-national comparisons, and concludes with a number of policy recommendations which could help Chile strengthen cancer screening and prevention. Together with policies to promote healthy lifestyles, public health policies specific to cancer are key to reducing the burden of cancer in Chile.
OECD Reviews of Public Health: Chile
Chapter 3. Cancer screening and prevention in Chile
Abstract
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
3.1. Introduction
In Chile, as in other OECD countries, cancer is a leading cause of death, for which effective screening and prevention strategies are a high policy priority. Chile has already built mechanisms to screen for some cancers, but weaknesses remain, including in areas of system capacity, stakeholder involvement, population awareness, and data systems to monitor and implement public health policies to fight against cancer.
This chapter begins by setting out the current cancer burden in Chile, as well as recent trends in cancer incidence and mortality. Secondly, the strengths and weaknesses of Chile’s cancer care system are explored, followed by a close examination of the Chile’s public health policies in the area of cancer, including vaccination and screening and diagnosis for different cancers such as cervical, breast, prostate, colorectal, stomach and liver cancer. Finally, the chapter makes a series of recommendations on the policy priorities for Chile when it comes to increasing cancer screening coverage and promoting early detection of cancer.
3.2. Burden of cancer is high in Chile
Across OECD countries, cancer is the second highest cause of death, but the burden of cancer is increasing faster relative to the first cause of death, diseases of circulatory system. The mortality rate of cardiovascular diseases has declined substantially over recent decades, while cancer mortality has also decreased but at a slower pace. This section summarises cancer incidence and mortality rates and their changes over time in Chile compared to OECD averages to illustrate the relative importance of cancer for public health policies in Chile.
3.2.1. In Chile, cancer incidence is low but cancer could become the first cause of mortality in the near future
Cancer incidence in Chile is significantly lower than that in most OECD countries. There were 196 new cases of cancer per 100 000 population in 2018 which is 35% lower than the OECD average at 301. Across OECD countries, cancer incidence has generally been increasing in recent years, and Chile follows this trend (OECD, 2018[1]; IARC GLOBOCAN, 2018[2]). Since the prevalence of risk factors such as smoking and obesity is high and sometimes increasing in Chile (see Chapters 1 and 2), cancer incidence is likely to continue increasing.
Despite a low rate of cancer incidence in Chile, the burden of cancer is high in Chile. In 2015, based on the mortality rates adjusted to the OECD population structure, cancer accounted for 202 deaths per 100 000 population, only slightly lower than the OECD average of 208. Potential years of life years lost, a summary measure of premature mortality and an indicator of disease burden among people aged between 0 and 69 years old, shows that 20% of all potential years of life years lost is due to cancer. This is a significant share, albeit lower than the OECD average of 27% (OECD, 2018[1]).
In terms of leading causes of death, in Chile, cancer surpassed diseases of the respiratory system in 1970, and since then as observed in many other OECD countries, it is the second highest cause of death after diseases of circulatory system (with the mortality rate of 226 deaths per 100 000 population in Chile and 290 deaths per 100 000 population on average across OECD countries in 2015). Across OECD countries including Chile, the mortality rate for diseases of circulatory system has decreased rapidly over the past decades while cancer mortality has also decreased but at a slower pace, so the relative burden of cancer mortality is increasing in the OECD.
Following this trend, in Chile it is expected that the burden of cancer will continue to be significant and cancer could become the first cause of deaths in the near future. Already in some regions such as Arica and Parinacota, Tarapaca and Antofagasta in the north of Chile, and Araucania, the poorest region in terms of GDP per capita, and Los Rios in the south, cancer has become the first cause of deaths (Ministry of Health, 2014[3]).
3.2.2. Many people in Chile develop and die from preventable cancers
In Chile, prostate cancer has the highest incidence at 51 new cases per 100 000 men in 2018, followed by breast cancer with 41 new cases per 100 000 women. Colorectal cancer has the third highest incidence with 21 new cases per 100 000 population for both genders and it is higher among men (24 new cases per 100 000 men compared to 18 new cases per 100 000 women). Stomach cancer follows (18 new cases per 100 000 population) and it is much higher among men (27 new cases per 100 000 men compared to 10 new cases per 100 000 women). Lung cancer has the fifth highest incidence at 13 new cases per 100 000 population for both genders and more new cases are found among men (17 per 100 000 men compared to 12 per 100 000 women). To summarise by gender, among men, prostate, stomach, colorectal, lung and kidney cancer have the highest incidence rate while among women, incidence is high for breast, colorectal, cervical, gallbladder and lung cancer in Chile (IARC GLOBOCAN, 2018[2]).
Many of these cancers share common risk factors including poor lifestyles such as obesity, lack of physical activity, smoking, diet and alcohol consumption (Box 3.1). For instance, one study found that 20% of cancer in Chile may be related to obesity (Garmendia, Ruiz and Uauy, 2013[4]), so recommendations to tackle risk factors such as smoking, obesity, alcohol consumption, and physical inactivity that are laid out in previous chapters are very relevant for cancer and important in reducing risks of developing different cancers.
Box 3.1. Risk factors for cancers with highest mortality rates in Chile
Different risk factors are known to contribute to developing cancer. Although not exhaustive, this box lists major risk factors for cancers with highest mortality in Chile in an alphabetical order.
Bladder cancer: smoking, exposure to chemicals such as arsenic, aniline dyes, 2-Naphthylamine, 4-Aminobiphenyl, xenylamine, benzidine, and o-toluidine, age, gender, personal history of bladder or other urothelial cancer, genetic predisposition such as a mutation of retinoblastoma (RB1) and family history.
Breast cancer: age, family history of breast cancer or ovarian cancer, genetic predisposition such as BRCA1 and BRCA2 gene mutation, previous diagnosis of breast cancer, breast density, lifestyles including obesity, physical inactivity, unhealthy and unbalanced diet, alcohol consumption, hormone replacement therapy and contraceptive pill.
Cervical cancer: human papilloma virus (HPV) infection, smoking, weakened immune system, diet low in fruits and vegetables, overweight, and long-term use of oral contraceptive pill.
Colorectal cancer: age, family history of colorectal cancer or polyps, Crohn's disease, ulcerative colitis, genetic predisposition including familial adenomatous polyposis (FAP) and Lynch syndrome (hereditary non-polyposis colorectal cancer (HNPCC)), and lifestyle factors such as a diet high in fat and low in fibre, lack of physical activity, obesity, tobacco and alcohol consumption.
Gallbladder cancer: age, obesity, smoking, unhealthy diet, gallstones, cholecystitis, diabetes, and family history of gallstones, cholecystitis or gallbladder cancer.
Kidney cancer: obesity, smoking, high blood pressure (hypertension), family history of kidney cancer, genetic conditions such as Von Hippel-Lindau syndrome, and long-term dialysis.
Liver cancer: cirrhosis, cirrhosis caused by excessive alcohol consumption, long-term hepatitis B or C viral infection, haemochromatosis, and lifestyles such as obesity, unhealthy diet and inactivity.
Lung cancer: smoking and passive smoking, exposure to radon and/or certain chemicals and substances such as arsenic, asbestos, beryllium, cadmium, coal and coke fumes, silica and nickel, air pollution, and family history of lung cancer.
Pancreas cancer: age, smoking, diabetes, chronic pancreatitis, stomach ulcer, Helicobacter pylori infection, family history and genetic predisposition such as hereditary breast and ovarian cancer syndrome, caused by BRCA1 or BRCA2 gene mutations and familial atypical multiple mole melanoma (FAMMM) syndrome caused by p16/CDKN2A gene mutations.
Prostate cancer: age, family history, obesity, lack of exercise, smoking, diet and genetic predisposition including BRCA1 or BRCA2 gene mutations, Lynch syndrome.
Stomach cancer: age, gender, smoking, H. pylori infection, diet, a family history, genetic predisposition including HNPCC, FAP and BRCA1 and BRCA2, having another type of cancer, pernicious anaemia, peptic stomach ulcer, and stomach surgery.
As of 2018, the incidence of cancers which are common in Chile is generally lower than those in most OECD countries with some exceptions. On average across OECD countries, the incidence rate is 71 per 100 000 men for prostate cancer, 78 per 100 000 women for breast cancer, 31 per 100 000 population for colorectal cancer and 29 for lung cancer and they are all higher than the rates in Chile in 2018. For some cancers such as cervical, stomach and gallbladder cancer, however, the rate in Chile is higher than the OECD average. For instance, for cervical cancer, incidence rate in Chile is almost 30% higher than the OECD average of 9 new cases per 100 000 women (IARC GLOBOCAN, 2018[2]).
Turning to mortality, the most recent data available show that in Chile cancer accounts for 252 deaths per 100 000 men, which is lower than the average rate in the OECD (274) but not significantly lower despite much lower cancer incidence (222 new cases per 100 000 men in Chile compared to 342 on average in the OECD). Among men, in 2015 cancer with highest mortality in Chile is prostate cancer (44 per 100 000 men), stomach cancer (40), lung cancer (32), colorectal cancer (22) and liver cancer (12). The mortality rate in Chile is lower than the OECD average for lung and colorectal cancer, about the same for liver cancer, and higher than the average for prostate and stomach cancer (OECD, 2018[1]; IARC GLOBOCAN, 2018[2]).
According to the latest data, cancer mortality amongst women in Chile is 168 deaths per 100 000 women, slightly higher than the OECD average (163 per 100 000) while the incidence rate is much lower than the average (178 new cases per 100 000 women in Chile compared to 271 on average in the OECD). Among women, the leading cause of cancer mortality in Chile is breast cancer (19 per 100 000 women), colorectal cancer (18) and lung cancer (17), stomach cancer (15) and pancreas cancer (10) in 2015. The mortality rate is also high for cervical cancer (8) and liver cancer (8). Compared to most OECD countries, the rate is low for breast, lung and pancreas cancer and about the same for colorectal cancer but high for stomach, cervical and liver cancer (OECD, 2018[1]; IARC GLOBOCAN, 2018[2]).
Following the trends across OECD countries, mortality rates due to all cancers are higher among men than among women in Chile. The gender difference in cancer mortality can be explained at least partly by higher prevalence of some risk factors among men (see Chapter 1 and Chapter 2).
3.2.3. Lung, prostate and colorectal cancer mortality rates in Chile have not declined as they have in many OECD countries
Although overall cancer mortality rates have been declining in Chile, as in most OECD countries, the pace was different by gender and Chile made slower progress among men than among women. Among men, the decline was slightly slower in Chile than in most OECD countries. Since the peak of cancer mortality rate in the OECD and in Chile in 1993, mortality has declined by 17% in Chile while the OECD average decline was 22. Amongst women cancer mortality was highest in 1984 in many OECD countries, and highest in Chile in 1985. Since the 1984 peak, the female OECD cancer mortality average dropped by 19% while the rate for Chile fell by 21% (Figure 3.1). For both men and women, overall cancer mortality decline in Chile was mainly due to the reduction for stomach cancer (Figure 3.2 and Figure 3.4).
Figure 3.1. Cancer mortality rates among men and women, Chile and OECD, 1980-2015
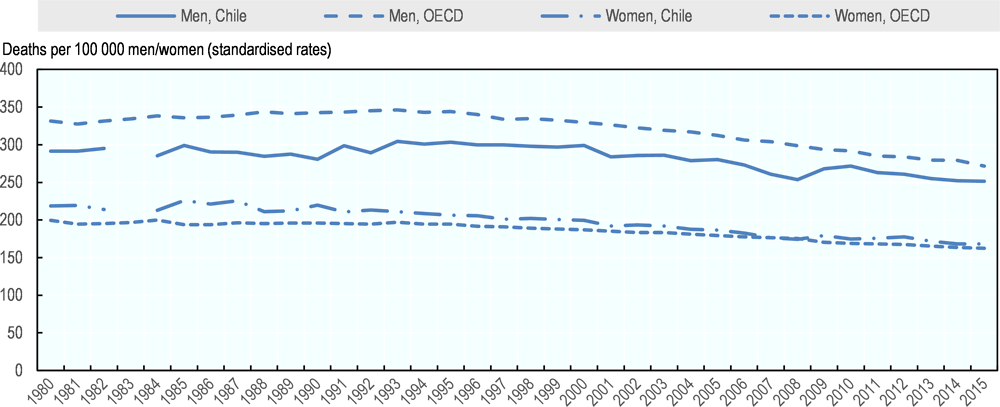
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
For some cancer such as lung, prostate and colorectal cancer, the trend in mortality rates among men in Chile deviated from the OECD averages. For lung cancer, in the 1980s most OECD countries had a much higher mortality rate than Chile, but since 1980 the OECD average lung cancer mortality rate has declined faster (by 26% compared to by 15% in Chile), probably reflecting at least partly the smoking rate which continues to be high in Chile compared to many OECD countries (see Chapter 1). On the other hand, for prostate and colorectal cancer, mortality rate in Chile increased while most OECD countries managed to have a decreasing trend over recent decades (Figure 3.2 and Figure 3.3).
Figure 3.2. Mortality rates of major cancers among men in Chile, 1980-2015
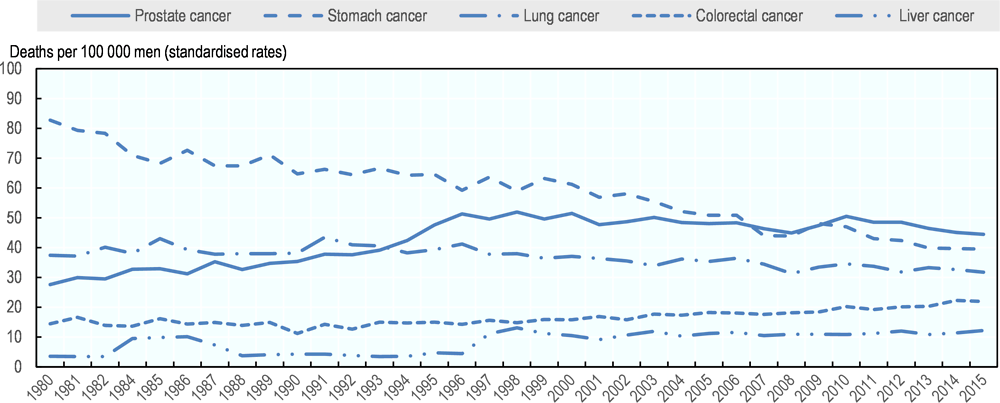
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
Figure 3.3. Average mortality rates of major cancers among men in the OECD, 1980-2015
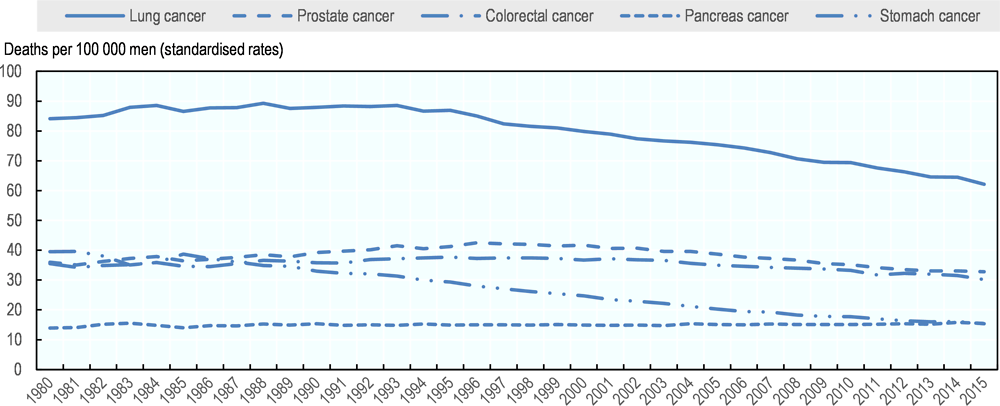
Source: OECD Health Statistics 2018 https://doi.org/10.1787/health-data-en.
Similarly, among women, for breast and colorectal cancer, the mortality trend in Chile was different from the trend in most OECD countries. With regards to breast cancer, the mortality rate in Chile was 35% lower than OECD averages in 1980, but it did not decline as fast as in many other OECD countries (since 1980 a decline of 9% in Chile compared to 25% on average in the OECD). As for colorectal cancer, similar to the trend observed for men, the mortality rate has declined steadily in most OECD countries since 1980 but Chile experienced an increase, narrowing the gap with the OECD average (Figure 3.4 and Figure 3.5).
Figure 3.4. Mortality rates of major cancers among women in Chile, 1980-2015
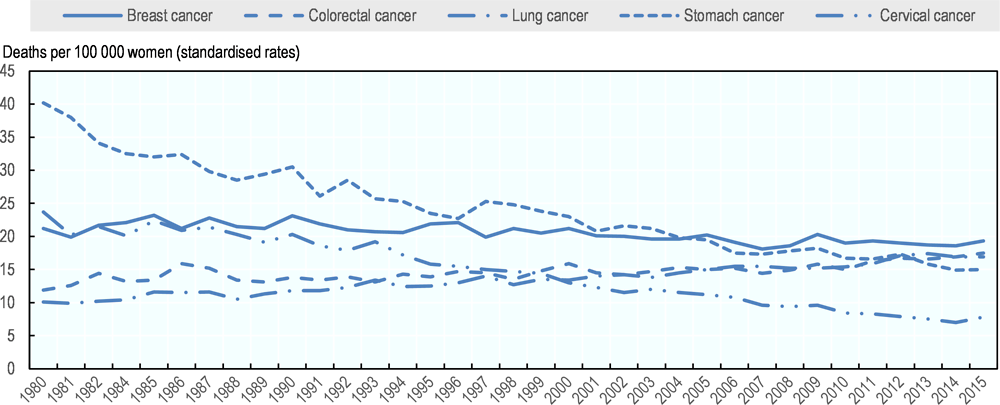
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
With regards to lung cancer, contrary to the overall trend among men, the mortality rate for women has increased across OECD countries including Chile over the past decades, and the rate grew slightly faster in Chile (by 67% between 1980 and 2015) than the OECD average (by 62%). Smoking is considered to increase the risk of developing lung cancer later in life and an increasing mortality trend is likely to reflect an increase in smoking rates among women decades ago (OECD, 2015[7]).
Figure 3.5. Average mortality rates of major cancers among women in the OECD, 1980-2015
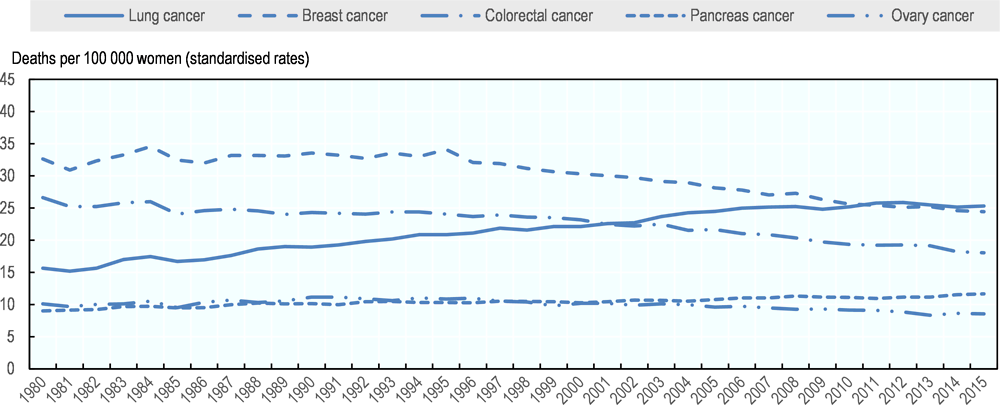
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
3.2.4. In Chile, the burden of cancer varies by regions, ethnicity and socio-economic group
Cancer incidence in Chile varies by region, socio-economic and ethnic background. The incidence of stomach cancer is relatively high among indigenous populations, and gallbladder cancer incidence is higher among people with certain ethnic origins, lower educational attainment, women and urban residents (Jimenez de la Jara et al., 2015[8]). These within-country variations in incidence may be partly related to differences in modifiable lifestyle factors for which public health measures can play some role, while they are also likely to be related to differences in genetic predisposition to some extent.
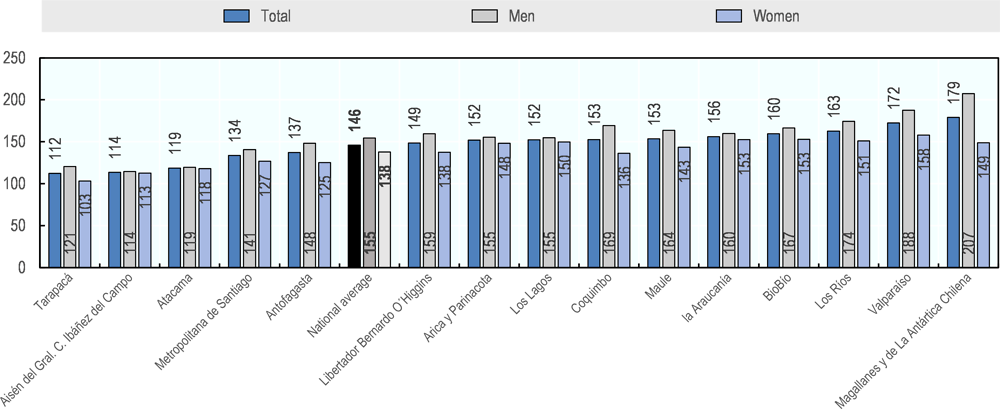
The cancer mortality rate also varies across Chile’s regions. The overall cancer mortality is high in some regions including Los Rios, Valparaiso and Arica y Parinacota, while it is low in Tarapaca region (Figure 3.6). The mortality rate of specific cancers is also different across regions. For example, the mortality of rectal cancer is high in southern regions (The Government of Chile, 2010[9]). The mortality rate of colon cancer is particularly high in Magallanes and Arica at over 10 per 100 000 population and it grew rapidly over the past decade, particularly in Arica. In Valparaiso, Maule and Magallanes the mortality rate of stomach cancer is higher than the national average while in Valparaiso, Maule and Los Ríos the mortality rate of prostate cancer is higher than the national average. As to lung cancer the regions of Arica and Parinacota, Antofagasta, Atacama, Valparaiso, Metropolitan Santiago and Aisén have mortality rates higher than the national average (Roco et al., 2013[10]). The incidence rate of colon cancer is highest in southern regions of Chile, while skin cancer incidence is high in the northern region of Antofagasta at 60 per 100 000 women and 75 for men while it is as low as 8 and 10 respectively, in Bio Bio, and 21 and 19 in Los Ríos (The Government of Chile, 2010[9]).
Figure 3.6. Cancer mortality rates by region in Chile, 2014
Cancer mortality rate is also different by individual’s ethnic and socio-economic background. Cancer mortality is higher among those with lower education, and mortality differences by socio-economic background are particularly prominent for gallbladder, gastric, cervical and prostate cancer (The Government of Chile, 2010[9]). Mortality rates are also sometimes different by ethnic group. For example, mortality from gallbladder cancer is high in rural areas particularly among indigenous people with Mapuche descent who also have a higher incidence rate of gallbladder cancer than other population groups (Moore et al., 2014[11]). Within-country variations in mortality may be related to differences in modifiable lifestyle factors and genetic predispositions but they are associated at least partly with variations in other factors such as screening coverage and access to and quality of cancer diagnosis and treatment.
Cancer screening structures are in place but could be strengthened Across OECD countries, strong cancer care systems share some common characteristics. They have solid governance structures and policy tools such as having a responsible person or institution for cancer care, implementing comprehensive cancer care policies, setting cancer-specific goals with defined timeframe, allocating adequate level of resources for achieving policy goals, embedding effective incentives for improving quality of cancer care, periodically monitoring and reporting progress on cancer control and giving feedback to different stakeholders for continuous improvement (OECD, 2013[12]). Across countries, these governance structures and policy tools are associated with better cancer outcomes. This section evaluates the current state of Chile’s cancer care system based on its governance structures, policy tools and cancer care outcomes, relative to other OECD countries.
3.2.5. Chile has developed its cancer care system incrementally to tackle the increasing burden of cancer
Chile has been strengthening its cancer care system incrementally over the past several decades. Since the late 1980s, Chile has developed several programmes to reduce the burden of cancer; Chile’s National Cancer Programme is now composed of five discrete programmes. The first programme is the National Cervical Cancer Programme introduced in 1987, relatively early compared to most OECD countries. Then, in 1988, two programmes, the National Programme of Cancer Drugs for Adult and the National Programme of Cancer Drugs for Children were implemented, and in 1995, another two programmes, National Breast Cancer Programme, and National Pain Relief and Palliative Care Programme were introduced (Ministry of Health, 2015[13]). The National Cancer Programme has an emphasis on health promotion, prevention and early diagnosis, and it developed guidelines for delivering cancer care. This programme also aims to assure equitable access to cancer care among patients and to improve continuity and quality of care throughout patient pathway while responding to the need of patients and their families.
Since the 2000s, Chile has been tackling cancer as one of the major diseases in the country. In 2000, the national health strategy called Health Priorities 2000-2010 was introduced with an aim of tackling risk factors for non-communicable diseases, in particular diseases with high burden which included cancer, cardiovascular disease, respiratory diseases, diabetes, mental health and dental health. The subsequent Health Priorities 2011-2020 also aims to reduce the burden of major diseases and focuses on cancer as the second priority disease. In addition, in 2005, in view of achieving universal health care, Universal Access with Explicit Guarantees (AUGE) was introduced to improve access, quality, financial protection and timeliness of health care for priority diseases including cancer (see Chapter 1). Initially, AUGE included 10 cancers including paediatric, breast, cervical, prostate, gastric, prostate cancer, acute and chronic leukaemia, lymphoma and primary tumours of the central nervous system. Since then, the type of cancer and cancer care interventions covered by AUGE have increased and as of 2018, 17 interventions related with cancer are included.
Box 3.2. Universal Access with Explicit Guarantees (AUGE) for cancer
In 2005, Chile introduced the Universal Access with Explicit Guarantees (AUGE) and access to care, quality of care, financial protection and timeliness of care for 80 priority health conditions including different types of cancer, diabetes, hypertension are assured legally for all population insured either by FONASA or ISAPRES (see also Chapter 1). Quality of care is assured through registration and accreditation of providers delivering AUGE-covered services, and medical protocols need to be followed for AUGE-covered interventions. Patients are guaranteed to receive care within defined waiting time which is set for each health condition, and if the public sector is not able to provide care within the waiting time guarantee, patients can seek care in the private system and the cost of private health services is covered by FONASA. Studies show that AUGE has contributed to improving health outcomes and equity (Bitrán, Escobar and Gassibe, 2010[14]; Frenz et al., 2014[15]).
Over years AUGE-covered cancers have been progressively expanded. For example, AUGE initially covered breast and cervical cancers in 2005, coverage was expanded to gastric and prostate cancers from 2006 and bladder and colorectal cancers were included in 2013. Childhood cancer is also covered. However, as of 2018, among cancer with high disease burden, lung cancer is not included in AUGE. while care for lung cancer is still available in public hospitals within the limit of their yearly budget and in private hospitals. Table 3.1 shows the waiting time guarantee set in relation to diagnosis, treatment and follow-up care for AUGE-covered cancers.
Table 3.1. AUGE coverage and waiting time guarantees for cancer care
|
|
Starting year |
Screening |
Diagnostic confirmation |
Suspected case to specialist consultation |
Biopsy and other tests |
Treatment |
Follow-up care |
|---|---|---|---|---|---|---|---|
|
Cervical cancer |
2005 |
30 days of suspected case |
40 days |
20 days |
30 days if pre-invasive, 20 days if invasive, complementary treatment within 20 days |
First control within 90 days |
|
|
Breast cancer |
2005 |
45 days |
45 days |
30 days since diagnostic confirmation, complementary treatment within 20 days of medical indication |
First control within 90 days |
||
|
Gastric cancer |
2006 |
30 days since specialist referral |
30 days |
Surgery within 30 days of diagnostic confirmation, eradication treatment within 7 days, and specialist care within 60 days if peptic ulcers and confirmation of H. Pylori bacteria |
|||
|
Prostate cancer |
2006 |
60 days since diagnostic confirmation |
60 days since biopsy and other tests |
First control within 45 days |
|||
|
Gallbladder cancer |
2013 |
30 days for patients age 35-49 with gallstones in gallbladder or bile ducts |
Surgical removal of gallbladder within 90 days of diagnostic confirmation |
||||
|
Colorectal cancer |
2013 |
45 days since diagnostic confirmation |
30 days of medical indication |
First control within 90 days |
Source: (Ministry of Health, 2015[13]).
Like Chile, many OECD countries initially implemented specific cancer programmes. However, OECD countries such as the Czech Republic, France and the United Kingdom then introduced overarching and comprehensive cancer control policies through National Cancer Strategies or National Cancer Plans, starting in the 2000s. These strategies or policies initially focused on prevention and screening but have since been expanded to cover treatment, follow-up, care co-ordination, palliative care, patient-centred care and monitoring. Although an introduction of the national strategy or plan is not a prerequisite for building strong cancer care systems, a number of OECD countries have leveraged the introduction of National Cancer Control Strategies or Plans by undertaking a number of reforms needed to tackle cancer control simultaneously. For example, countries have simultaneously put in place policies or strategies such as improving access to cancer care and resource allocation, promoting quality of cancer care throughout patient pathway and driving efficiency gains in cancer care delivery, and have also focused on involving different stakeholders in the cancer care system (see Box 3.3).
Box 3.3. National Cancer Plans in several OECD countries
In recent years, a growing number of OECD countries have introduced National Cancer Control Plans to strengthen the governance of cancer care, and over time, policy focus for cancer control has changed across countries.
Several OECD countries such as Belgium, the Czech Republic, Italy, the Netherlands and Sweden implemented various discrete cancer policies before introducing a comprehensive national plan. In the Czech Republic, for example, cancer policy in the early 2000s focused on screening programmes for breast and cervical cancers; later in the decade, in 2005, a more comprehensive effort, the National Cancer Control Programme, was introduced to improve the quality of care and cancer survival more broadly.
Several OECD countries changed the focus of National Cancer Control Strategies to continue tackling emerging policy challenges in recent decades. In England, for example, the NHS Cancer Plan was introduced in 2000, and outlined the government’s comprehensive national programme for investment in and reform of cancer services. Building on the progress made since the NHS Cancer Plan, in 2007 the Cancer Reform Strategy was introduced to set a direction for cancer services over the next five years. It focused on preventing cancer, diagnosing cancer earlier, ensuring better treatment, living better with and beyond cancer, reducing cancer inequalities and delivering cancer care in the appropriate settings through better use of information and stronger commissioning and funding.
To give another example, in France, the first Cancer Plan with a comprehensive approach was implemented between 2003 and 2006, and was followed by the second Cancer Plan 2009-2013 that dealt with emerging challenges such as research, monitoring, prevention, screening, patient care and life during and after cancer. The third Cancer Plan was introduced in 2014 and is effective until 2019. This Plan focuses on prevention, early diagnosis, access to high quality care and innovations and more patient-centred care. It also aims to tackle inequalities in cancer incidence and cancer outcomes. The governance of cancer care has been also strengthened by establishing an independent body (Institut National du Cancer) to oversee the overall implementation of cancer control, allocating additional resources to achieve specific objectives, and monitoring and evaluating the progress made (OECD, 2013[12]; OECD/European Observatory on Health Systems and Policies, 2017[16]).
In some OECD countries, involvement of different stakeholders including regional authorities was key for the success of nationwide cancer control. For instance, the cancer care strategy in the Spanish National Health System, first introduced in 2006 and updated in 2009 with new policies and strategic goals, was designed through close collaboration with all key stakeholders including civil society. It was a co-ordinated effort between the Minister of Health and the regional governments and such stakeholder involvement facilitated the implementation of cancer care strategy across health authorities in regions. In Italy, regional governments participated extensively in the development of the first National Cancer Control Plan in 2006, which was adopted and implemented much more consistently at the local level than earlier initiatives were. Regional authorities have been key players in cancer control in a few other countries such as Canada and Sweden, which developed regional plans first and then National Cancer Plans, and countries such as Australia and Korea developed regional plans outlining the implementation strategies for local stakeholders, based on the National Cancer Plans (OECD, 2013[12]).
3.2.6. Key governance structure and policy tools already exist in Chile for cancer control
Although Chile has not introduced overarching National Cancer Strategies or Plans, it has a cancer care system supported by a clearly defined governance structure and policy tools for cancer control.
Responsibility for cancer care is clearly set out in Chile, and the Ministry of Health has the overall responsibility for the governance of cancer care system. In particular, within the Ministry, the National Cancer Plan Unit is in charge of defining cancer care policies and supervising its compliance. There are also departments which take charge of specific issues; the Department in charge of the National Immunization Program (PNI) is responsible for all immunisation schemes which include HPV and hepatitis B vaccinations; the Department of Primary Health Care within the Ministry is in charge of the implementation of PNI and screening for cervical, breast, colon and stomach cancer provided at primary health centres. In other OECD countries too, the responsibility of cancer control often falls to the Ministry of Health and it is held accountable for meeting the targets it set. In addition, in Chile, regional health authorities and health care professionals are responsible for implementing cancer screening programmes in particular for cervical cancer, based on the primary care system goals set at the regional level.
As in other OECD countries with strong governance of cancer care systems, Chile has established some cancer-specific targets or objectives at the national level, and timeframes were specified for achieving them. For example, targets of Health Priorities 2000-2010 included targets such as decreasing age-standardised mortality rate by 40% for cervical cancer, by 25% for breast cancer and by 25% for gallbladder cancer during the implementation period. Although targets were not necessarily met, some progress was made for these cancers particularly for cervical and gallbladder cancer. Other time-bound targets included areas of early detection, screening, reduced waiting time and improved treatment. Health Priorities 2011-2020, which is currently in place, also sets a goal of decreasing cancer mortality by 5% by 2020, and between 2011 and 2015, Chile has already decreased mortality rate by 4.1% (OECD, 2018[1]).
Additional resources were also made available to improve access to cancer care in Chile recently. Chile spends about 1% of GDP on cancer care (Jimenez de la Jara et al., 2015[8]) which is higher than the spending level in most OECD countries. Part of this investment was made to improve the availability of specialised care for different types of cancer. The number of public cancer care centres were increased from 19 in 2002 to 21 in 2010 (OECD, 2013a), and as of 2017, there were also 7 radiotherapy units, 29 chemotherapy units, 12 oncohematology units, 1 centre providing bone-marrow transplant for adults, and 1 centre providing bone-marrow transplant for children. Additional public funding was also made available to pay for procedures and treatment covered by AUGE, as its coverage has expanded in recent years (Box 3.2).
Chile has taken multiple approaches to assure financial access to cancer care among patients and their family. Primary care provides services for different health conditions including cancer, such as screening and diagnosis tests, palliative care and many routine blood tests, and all these services are provided free of charge. For AUGE-covered services a co-payment of 20% of the total cost is required by patient but a maximum payment limit is set for health care, including pharmaceuticals. To assure access to health care among the poor no co-payment is required for AUGE-covered services by low income patients if they are insured by FONASA or ISAPRES (OECD, 2013[12]). In addition, according to the Ricardo Soto law, certain cancer patients can also seek additional financial support for exceptionally high cost treatment, in which the Central Commission, composed of oncologists in the capital Santiago, evaluates the eligibility of each cancer case. For example, inclusion criteria are examined for the use of Herceptin, and approximately 120 to 140 breast cancer patients are allowed to receive the treatment for free every year (OECD, 2013[12]).
The Chilean cancer care system has also sought efficiency gain and quality improvement through improved resource allocation and reorganised cancer care delivery in recent years. For instance, Chile has centralised cancer care delivery by concentrating resources and expertise at specialised institutions as seen in other OECD countries. Cancer networks have been also established in order to facilitate co-ordination among professionals engaged in oncology care (OECD, 2013[12]).
Chile also implemented several additional policies focusing on improving the quality of cancer care. First, the Central Commission of Experts, established in 1988 and now called the Programa Adulto Nacional de Drogas Antineoplásicas – PANDA, develops clinical guidelines to standardise and assure quality of cancer care. Second, reimbursement is linked with evidence-based care delivery and only those treatments and procedures that comply with the guidelines are reimbursed. As a result, the compliance level and quality of cancer care are considered to be improving. Third, similar to other OECD countries, Chile developed unified licensing and certification systems to train medical professionals with specialised expertise and skills in cancer care and started cancer service accreditation system in 2005, although there is a report that professional licensing has not been implemented systematically within the country (OECD, 2013[12]). Finally, for types of cancer covered by AUGE, the patient pathway is organised based on an optimal treatment plan which also includes follow-up and palliative care in a timely manner based on waiting time guarantee (Box 3.2). Palliative care, for instance, is provided systematically in a co-ordinated manner to all cancer patients, either in hospitals or at home, by multidisciplinary team composed of physicians, nurses, psychologist, kinesiologists and other health professionals working together with patients and their caregivers.
3.2.7. Cancer care in Chile is better organised for some cancers than for others
Cancer care is organised relatively well for certain cancer such as cervical, breast and childhood cancer, which are all covered by AUGE. Given a long history of prioritising women’s health, the network of gynaecologists and midwives is well established and distributed all over the country in Chile. As for childhood cancer, since its inclusion in the AUGE, infrastructure and medical equipment have been improved in most centres providing care. Consequently, cancer care is provided to all children in need of care in a relatively timely manner and the quality is considered similar across providers despite a shortage of qualified health professionals at medium and high complexity establishments such as hemato-oncological and paediatric oncologist nurses, paramedical technicians, psychologists and social workers.
For other cancers, however, access to care is patchy. The availability of cancer care institutions such as facilities providing radiotherapy and chemotherapy still varies across regions, and travel to specialised care facilities is often difficult. According to the most recent data available the number of certified oncologists per capita was also low in Chile, at below three per million population in 2009 while the density was higher in other OECD countries. For instance, Sweden has as high as over 60 certified oncologists per million population. In addition to oncologists, there is also a need for radiologists, pathologists and surgeons including thoracic surgeons in Chile, and the availability of health care professionals is particularly low in smaller cities and rural areas. For example, surgeons who can treat lung cancer patients appropriately are concentrated only in a few big cities, leading to geographic inequality in access to care among patients (OECD, 2013a). Some reports also suggest that access to care is not assured sufficiently for cancer such as stomach and gallbladder cancer (Jimenez de la Jara et al., 2015[8]).
3.2.8. Chile still faces many challenges in cancer control
Despite the progress made in strengthening governance of the cancer care system and delivery of cancer care particularly for priority cancers, data suggests that Chile still lags behind many OECD countries in terms of cancer control. As shown before in the Section 3.1, despite its very low cancer incidence, cancer mortality in Chile is only slightly lower than the OECD average. Over recent decades, among men, cancer mortality rates declined more slowly in Chile compared to most OECD countries. Among women, although the decline in the mortality rates was faster than in most OECD countries, the mortality rate in Chile continues to be higher than the OECD average.
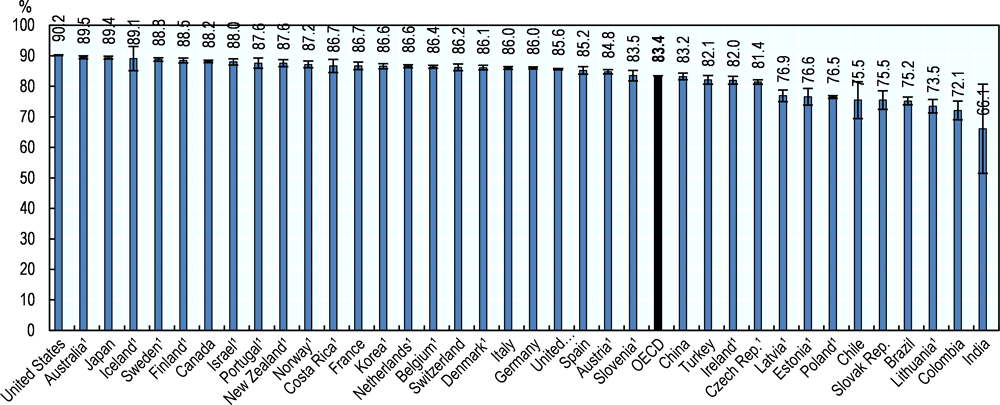
These data reflect a number of following challenges that the Chilean health system faces. First, as described in Chapters 1 and 2, among its population, risk factors are increasing, leading to an increasing burden of non-communicable diseases including cancer. Second, while most OECD countries have achieved universal health coverage already in the 1970s and 1980s and hence have a more established health system to tackle different policy areas including cancer control, Chile still continues aiming at achieving universal health coverage (Figure 3.7) and assuring access to health care through AUGE. Although slowly decreasing, the share of those with unmet health care needs is still high at around 8% in 2015 (Ministry of Health, 2015[13]), so it is more challenging to focus on its fight against cancer in Chile, compared to many other OECD countries.
Figure 3.7. Population coverage for a core set of services, 2016 (or nearest year)
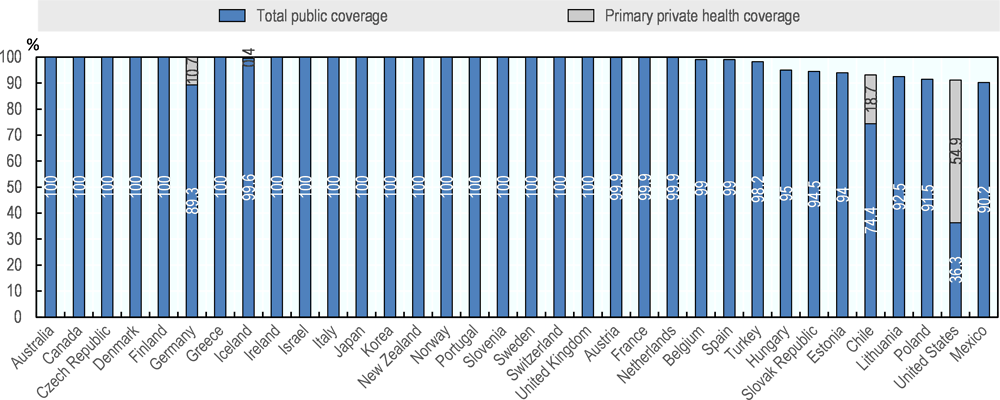
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
Third, as discussed in Cancer Care: Assuring Quality to Improve Survival (OECD, 2013[12]) a full suite of policies need to be implemented to improve cancer-related outcomes, but challenges still remain in Chile’s health system despite the efforts made to improve cancer care delivery and to strengthen the governance of cancer care in recent years. For example, monitoring of cancer control is essential for identifying issues in cancer care, and improving quality of cancer care, but despite some important progress made, monitoring mechanisms for cancer care are still weak in Chile. For childhood cancer, an integrated information system has been developed, allowing an assessment of clinical management and outcomes in the country. In addition, hospital cancer registries, implemented in 2011, monitor the quality of cancer care at an increasing number of providers. Chile also participates in the international surveillance and monitoring of cancer care through its participation to the OECD, WHO including Pan American Health Organization and the CONCORD Programme. However, despite these developments the current health information system in Chile still does not enable regular monitoring and reporting of some key data in cancer care, such as cancer survival estimates across all regions and over time at the national level beyond childhood leukaemia and cervical cancer (see Box 3.4), or more modern forms of data such as patient experiences (PREMs) with cancer care and cancer outcomes including patient-reported outcomes (PROMs) which cover quality of life and functional ability (OECD, 2017[17]).
Box 3.4. Cancer survival estimates for Chile
Chile participates in the CONCORD programme, the global programme for the surveillance of cancer, led by the London School of Hygiene and Tropical Medicine (Allemani et al., 2018[18]). While Most OECD countries participate in the CONCORD programme at the national level, allowing nationally-representative survival data to be reported for international comparisons. However, Chile participates based on four regional registries developed which cover less than 20% of the population (Jimenez de la Jara et al., 2015[8]).
Despite the data coverage, the CONCORD data are considered the best available Chilean cancer survival data for international comparisons, and according to this programme, survival prospect of cancer patients, which is often used as a proxy for assessing effectiveness of cancer care, is still one of the lowest in the OECD. Five-year net survival was 75.5% for breast cancer patients who were diagnosed between 2010 and 2014, and this is much lower than the OECD average of 83.4% (Figure 3.8). For the same period, five-year net survival for cervical cancer was 56.7%, about 10 percentage points lower than the OECD average of 65.6%. Similarly for acute lymphoblastic leukaemia for children, this data source reports five-year net survival at 63.9%, much lower than the OECD average of 86.3% and for colon cancer, the survival estimate remains one of the lowest in the OECD (OECD, 2018[1]; OECD, 2017[17]).
Figure 3.8. Breast cancer five-year net survival, 2010-14
Note: 95% confidence intervals represented by H. 1. Data with 100% coverage of the national population.
Source: CONCORD programme, London School of Hygiene and Tropical Medicine.
These data available for international comparisons depict a rather worrying picture of the current state of cancer care in Chile but a caution is needed to interpret Chilean data from the CONCORD programme. For childhood leukaemia, one of the priority cancers in the country, Chile has a nationwide established health information system and this allows reporting of national survival estimates. According to this national source, survival of childhood leukaemia has improved substantially between the periods 2000-2004 and 2005-2009 (PINDA, 2009[19]) On the other hand, the data from the CONCORD programme based on four registries show that the change between these periods was not statistically significant (OECD, 2018[1]). Hence, it is possible that the data generated from four regional registries, reported by the CONCORD, does not reflect the national situation. Given this issue of data coverage, this chapter mainly uses cancer mortality to assess cancer care performance in Chile relative to other countries, even though cancer survival estimates are considered as important statistics to evaluate the effectiveness of cancer care including early diagnosis and treatment across countries.
3.3. Prevention and cancer screening have been introduced in Chile but cancer outcomes remain relatively poor
In terms of prevention and early detection of cancer, Chile made some progress. Yet, it is not generally as effective as in best performing countries in the OECD. This section summarises the progress made as well as challenges that Chile faces to advance prevention and early detection of cancer, including vaccination and screening and diagnosis for different cancer such as cervical, breast, prostate, colorectal, stomach, and liver cancer.
3.3.1. Cervical cancer screening has improved early detection but its coverage could still be increased
Chile has a well-established cervical cancer screening programme. In 1987, Chile reorganised its cervical cancer screening and introduced a nationwide screening programme, a move which was relatively early compared to other OECD countries. Previously, a cervical screening service started in 1965 took Pap smears annually from women attending the maternal and childcare units of the primary health centre. Since the service indirectly targeted women at low risk of cervical cancer but not those with potentially high risk who do not seek health care, it was considered not effective (Sepúlveda and Prado, 2005[20]). Based on the analysis of age-specific mortality rates, a nationwide screening programme was developed and rolled out. Currently a Pap smear is available to women aged between 25 and 64 every three years and annual screening is provided to women with presence of risk factors. The target age of the screening programme is slightly different from many other OECD countries, which target women aged between 20 and 69 (OECD, 2018[1]). In Chile, women in the target group can have a Pap smear taken as part of Preventive Examination (EMP) (see Chapter 1) free of charge. Cervical cancer screening is also part of AUGE, and Pap smears taken outside of the Preventive Examination are also provided free of charge.
In order to increase screening coverage, several efforts have been made, and were essential in rolling out the cervical cancer screening programme nationwide. First, Chile involved stakeholders such as regional health authorities and health care providers at the preparation stage before introducing cervical cancer screening programme, and this early stakeholder involvement has formed a critical mass of highly motivated individuals at different levels for implementing the programme. Secondly, in order to reach out effectively to target women, primary health care registries have been used to identify target population for cervical cancer screening and target women are reached by invitation letter or volunteers visiting them at home (Sepúlveda and Prado, 2005[20]). Third, to provide incentives for high quality care among primary care providers, pay for performance is in place for various goals set in Primary Health Care Indicators, and this monitoring framework includes a goal related to the coverage of Pap smear. Each of these goals is decided every year for each region based on negotiations between regional administrations (Communas), municipality and health care professionals to align with the availability of resources and health care plan. The full bonus payment is made only if all goals are attained, so there is a pressure to achieve these goals together among professionals at the municipality level.
In terms of quality of diagnosis, standards for cervical cancer screening and quality assurance procedures in Chile are similar to those in other OECD countries. For example, peer review is performed to verify Pap smear results and the Cancer Prevention Centre of the Clinical Hospital of the University of Chile provides quality assessment of these results, contributing to the effective early diagnosis of cervical cancer in the country.
These efforts contributed to increased cervical cancer screening coverage and better outcomes for cervical cancer initially. Cervical cancer screening coverage in Chile increased, and women diagnosed with early stage of cervical cancer increased while those diagnosed with more advanced cervical cancer decreased. Together with policies aiming at improved health care access though AUGE and higher quality of care, systematic approaches taken for cervical cancer screening may have contributed to a mortality decline (Figure 3.4), although this decrease may be also related to changes in the patterns of reproductive health such as reduced parity and postponed child-bearing) (Sepúlveda and Prado, 2005[20]).
However, in the past decade screening coverage has decreased, and the incidence and mortality rates of cervical cancer remain higher in Chile than in many other OECD countries. The average national screening rate peaked at 68.0% in 2008 and since then it has declined, reaching at 55.9% in 2015 which is lower than the OECD average of 61.1% and well below Chile’s national goal of 80%, a level which a few countries such as Austria, the United States, Sweden and Germany have achieved in the OECD (OECD, 2018[1])(Figure 3.9). Although mortality rates declined by 63% since the start of screening programme in 1987 while the OECD average has declined by only 41%, mortality rate in Chile (7.8 deaths per 100 000 women) continued to be higher than that of the OECD average (4.1 per 100 000) in 2015 (Figure 3.4 and Figure 3.5). It should be also noted that the mortality rate in Chile has increased since 2014 (7.0 per 100 000 women).
Figure 3.9. Cervical cancer screening in women aged 20-69 within the past 3 years, around 2006 and around 2016
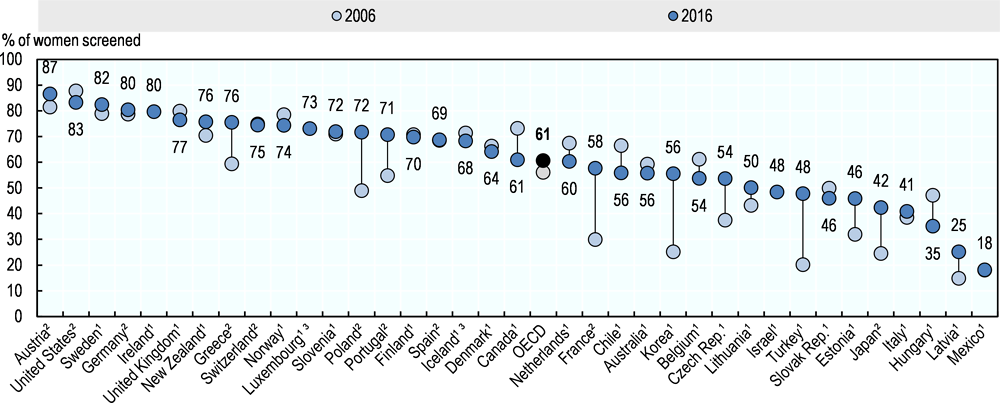
Note: The OECD average is unweighted and only includes countries with data covering the whole time period. 1. Programme. 2. Survey. 3. Three-year average.
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
A recent decline in screening rates could be explained by lowering public awareness on the benefit of regular Pap smear. Among women aged between 25 and 65 who not undergo Pap smear, over a quarter reported that it did not apply to them, another quarter thought it was not needed, while about 10% forgot about the test and another 10% did not have time. In addition, approximately 7% reported that tests scared or distressed them and about 3% of them did not know that they had to do it (Sakellariou and Rotarou, 2017[21]).
Within Chile, screening coverage continues to vary by regions and by population group with different socio-economic background. In 2015, the lowest screening rate was found in the region of Aysen at 55% and the highest rate was observed in Los Rios at 64% (Ministry of Health, 2015[13]). Contrary to a trend on overall access to health care, cervical cancer screening coverage is higher among those in rural areas than those in urban areas. The coverage is also higher among women with higher education, private health insurance, good self-reported health status and contact with health professionals for treatment for other diseases (Sakellariou and Rotarou, 2017[21]).
3.3.2. The introduction of HPV vaccination could help reduce the burden of cervical cancer in the near future
Like a number of other OECD countries, Chile introduced a school-based HPV vaccination as part of the National Immunisation Programme in 2014 to reduce an infection of most common types of HPV and the incidence of cervical cancer, which is still substantially higher than the OECD average. The immunisation programme, which is free of charge, provides the first dose of quadrivalent HPV vaccine to girls in 4th grade (between 9 and 10 years old) and the second dose to girls in 5th grade. In 2015 and 2016, a catch-up programme targeting girls in 6th, 7th and 8th grades was also conducted. This is in line with the WHO recommendations to include HPV vaccinations as part of national immunisation programmes primarily for girls aged between 9 and 13 years old in countries where the prevention of cervical cancer is a public health priority, the introduction is feasible and financially sustainable and cost-effective (WHO, 2014[22]).
Chile has taken a comprehensive multi-stakeholder approach to assure high coverage of HPV vaccination. The vaccine introduction was planned not only with health professionals but also with the education sector, and a manual was prepared for school teachers (WHO, 2014[22]). Parents or guardians of girls at the target age are also informed about the benefits, safety and risks of HPV vaccination to their girls, and before administering vaccination, they are asked to sign an informed consent. Furthermore, for any queries, a call centre called “Salud Responde” is made available at the Ministry of Health.
These efforts have enhanced knowledge of HPV vaccination among the population and led to high vaccination rates since its start. In 2015, the vaccination rate was about 85% (Schilling, Gonzalez and Muñoz, 2016[23]) and vaccination coverage is equally high across regions and socio-economic groups. This consistently high vaccination coverage across population groups suggests that the incidence of cervical cancer is likely to decrease in the country in the years to come.
Nonetheless, screening programme continues to be important for early detection of cervical cancer in Chile, and this is particularly so given a relatively high incidence and mortality rates in Chile compared to most OECD countries. HPV vaccination is not sufficient to prevent cervical cancer because some parents or guardians have not given consent to administer vaccination and their girls have not received vaccination, and existing vaccines do not protect against all high-risk HPV types.
3.3.3. An increase in mammography coverage would likely reduce the burden of breast cancer
The breast cancer screening programme is relatively new in Chile, and since the introduction of the National Breast Cancer Screening Programme in 1998, screening protocols have been changed several times. The programme initially used clinical breast examination but the share of breast cancer cases diagnosed at the early stage remained very low. In 2001, mammography was introduced as part of services provided at primary health centres. Then, in 2005 mammography screening was included in the EMP every three years for women aged between 50 and 59 years old for free. Since 2014, for women covered by the public health system, mammography has been provided free of charge as part of the imaging programme at primary health centres, and the age limit for these women was extended to 69 years of age. In many OECD countries population-based mammography is provided every two years to women aged between 50 and 69, so in Chile, the target women is limited as women who are under the private health system are covered only up to age 59 and screening is provided less frequently. Quality of breast cancer screening is considered good and Chile follows international standards such as double-reading of mammographs.
In addition to mammography, as in other OECD countries, genetic testing for breast cancer has become available to assess propensity of developing breast cancer among certain women in Chile. Fuorescen In Situ Hybridation (FISH) is available for people with HER2+ in both public and private health networks. In the public network, FISH Tests are carried out at Hospital Luis Tisné in the Metropolital Region and in Regional Hospital in the region of Valdivia. Breast cancer risk evaluation tests (BRCA) is additionally available at private health providers. But they are not provided for free to women with high risks in Chile unlike several OECD countries; for example, in Canada, BRCA is provided free to patients with specific indications including family history of breast or ovarian cancer and after genetic counselling (OECD, 2013[12]). In some OECD countries, people with genetic predispositions to breast cancer are monitored systematically but separately, outside of the screening programme.
The coverage of mammography screening continues to be much lower than the OECD average. Chile has a relatively well-distributed network of gynaecologists based on its historical focus on women’s health, aiming to assure access to care among women, but the coverage of mammography is 37%, much lower than the OECD average of 60% and the national screening coverage for cervical cancer (Figure 3.10). Mammography coverage is particularly low among those with low socio-economic background including educational attainment (Puschel and Thompson, 2011[24]).
Figure 3.10. Mammography screening in women aged 50-69 within the past 2 years, around 2006 and around 2016
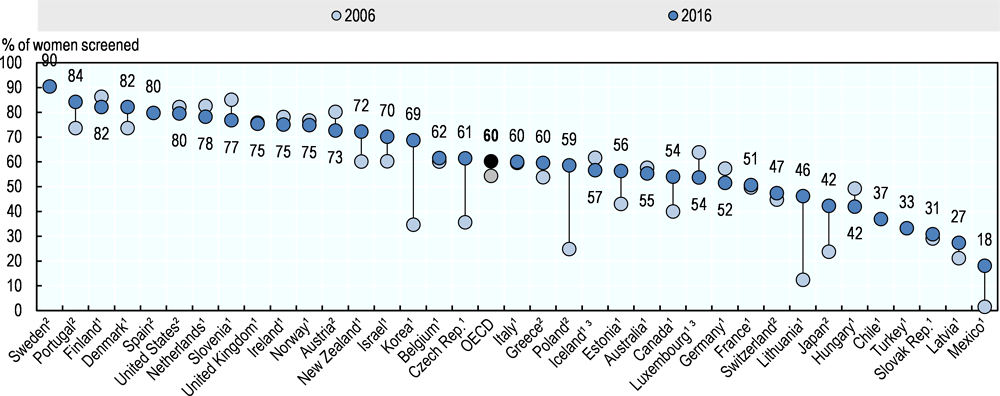
Note: The EU average is unweighted and only includes countries with data covering the whole time period. 1. Programme. 2. Survey. 3. Three-year average.
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en.
Since the introduction of the screening programme in 1998 in Chile, breast cancer mortality rate has declined but not as fast as in most OECD countries. The mortality rate for breast cancer decreased by 9% between 1998 and 2015 but across OECD countries the decline was 22% during the same period, and while the incidence rate in Chile is about half of the OECD average, the mortality rate in Chile is only 21% lower than the OECD average in 2015 (OECD, 2018[1]; IARC GLOBOCAN, 2018[2]). This may be due to factors such as lifestyle changes and relative progress in the quality of breast cancer care compared to other OECD countries, but the low screening coverage also poses a question of the screening programme’s effectiveness in reducing the burden of breast cancer in the country.
Low screening coverage for breast cancer can be explained by different factors and as seen for Pap smear, it is partly due to low public awareness on the benefits of mammography. One study suggests that among women aged between 50 and 75 who did not undergo mammography, more than half of them believed that they did not need it or it did not apply to them, or did not know that they needed to do it, and about 30% of women forgot to do it, did not have time or reported that the test scared or distressed them (Sakellariou and Rotarou, 2017[21]). Another study also found that secrecy, shame, fear and fatalism were associated to mammography and people continued to have greater confidence in breast self-examination (BSE) which was previously promoted as the appropriate screening method (Puschel and Thompson, 2011[24]). Related to this, the public may not be well informed about current screening protocols following a number of changes made in the National Breast Cancer Screening Program, which also includes target age.
Limited physical access to mammographs is also associated with a low coverage of breast cancer screening. In 2016, the number of mammographs in Chile was 15 mammographs per million population in Chile, which was lower than the OECD average of 23, although this may reflect a relatively low incidence rate in Chile compared to most OECD countries (Figure 3.11) (OECD, 2018[1]). Among women between 50 and 75 years of age who did not undergo mammography, more than 6% could not schedule an appointment, but for aPap smear, the share of target women who did not undertake the test due to not being able to schedule an appointment was lower at less than 3% (Sakellariou and Rotarou, 2017[21]). This suggests that compared to Pap smear, access is an issue for mammography in Chile. To overcome geographic challenges, a mobile mammograph, a truck carrying mammographs, is available in Chile, but access remains challenging in isolated regions.
Figure 3.11. Mammographs, 2016 (or nearest year available) and breast cancer incidence, 2018
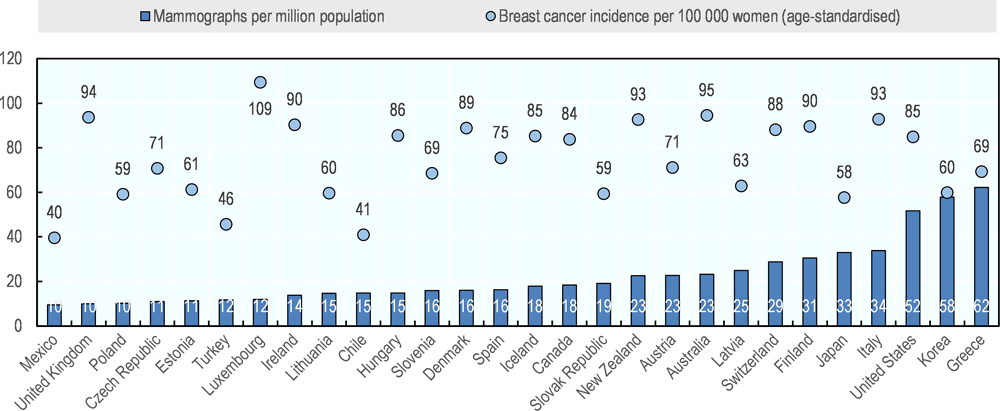
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en and IARC GLOBOCAN 2018.
Furthermore, low mammography coverage could be explained by the lack of incentives for providers such as peer pressure and financial remuneration. For instance, unlike cervical cancer screening, specific goals are not set in relation to mammography coverage for local health systems as part of Primary Health Care Indicators, and pay for performance is not available for health care professionals providing mammography screening. Hence, low policy focus on mammography at the health system level, compared to cervical cancer screening, is also likely to be related to low awareness not only among the public but also among health care professionals and subsequently leads to low mammography coverage.
3.3.4. For other cancers, preventive vaccinations and screening tests are also available but access to screening and diagnostic tests vary
Prostate cancer has the highest cancer incidence and mortality in Chile, but as in other OECD countries a screening programme does not exist. Population-based prostate cancer screening programme is not recommended internationally because even if detected, the majority of prostate tumours are not harmful and although some benefits of prostate cancer screening in reducing mortality risk have been observed across countries, harms such as unnecessary anxiety and treatment often lead to distressing side effects including impairment in sexual, bladder and/or bowel functions, and they are considered to outweigh benefits (IARC, 2016[25]). In Chile clinical examination and imaging is provided for symptomatic benign prostate hypertrophy as an AUGE condition.
For colorectal cancer, which has the third highest cancer incidence and mortality rates in Chile, opportunistic screening is available. It is either faecal occult blood Test (FOBT) every two years to people aged 50 and over, or colonoscopy every 10 years to people older than 50. However, an increasing number of OECD countries have introduced a population-based colorectal cancer screening programme for free to target population in recent years, and in many of these countries target population is those in their 50s and 60s often with an upper age limit ranging between 64 and 74 (OECD, 2013[12]). In view of identifying ways to reduce the increasing burden of colorectal cancer, Chile has undertaken analyses recently to assess cost-effectiveness of implementing a population-based colorectal cancer screening programme, and a pilot screening programme was conducted in three cities and found effective in detecting colorectal cancer at the early stage (López-Kostner et al., 2018[26]). These findings support the advantages of introducing population-based colorectal cancer screening programme in Chile.
As for stomach cancer, while screening programmes are not common in the OECD, given high incidence and mortality rates (fourth highest for both incidence and mortality among all cancers and both rates above OECD average), people who are 40 years of age and over with related symptoms can undergo selective upper endoscopy and H. pylori detection test at primary health centres for free in Chile. This is in line with the recommendations given by the IARC, the specialised cancer agency of the WHO to countries with high burden of stomach cancer. In particular, IARC recommends that these countries explore the introduction of population-based H. pylori screening and treatment while considering local contexts such as health priorities and cost-effectiveness (IARC Helicobacter pylori Working Group, 2014) because H. Pylori infection is one of the important risk factors for stomach cancer among others including dietary and behavioural, and genetic factors (Forman and Burley, 2006[27]) (Box 3.1). A few OECD countries with high burden of stomach cancer also have screening; while a nationwide screening programme is available in Korea, similarly to Chile Japan does not have an organised screening programme (OECD, forthcoming[28]).
In terms of lung cancer, anti-smoking policies can contribute to its prevention and Chile has a range of anti-smoking policies as described in Chapter1. But unlike many OECD countries, smoking cessation treatment is not publicly-funded health service in Chile.
Liver cancer also has one of the highest cancer incidence and mortality in Chile, and several public health policies have been implemented to reduce its disease burden. As in the majority of OECD countries, Chile provides vaccinations against Hepatitis B as part of the National Immunisation Programme since 2005 for free at primary health centres to reduce a risk of acute and chronic liver diseases including liver cancer. The vaccination rate has been high, covering over 90% of children with four doses at 2, 4, 6 and 18 months of age (OECD, 2018[1]). Hepatitis B vaccination is also provided to all health professionals and other population at risk based on epidemiological situation. The quality of vaccination has been monitored and assured by the Public Health Institute, a designated agency responsible for its quality assurance. In relation to liver cancer, Hepatitis C virus infection is also one of the main causes together with cirrhosis and steatosis of liver and infection of Hepatitis B in Chile, so at blood bank, all liver donors can also undertake a detection test for Hepatitis C virus infection.
Chile makes efforts to assure quality of screening for these cancers. Quality assurance of screening is done at the centres performing tests and supervised by national and international centres. In addition, when it was found that the quality of cancer screening could be further improved, Chile has followed necessarily steps to assure high quality cancer diagnosis. For instance, after some questions on the quality of colorectal cancer diagnosis were raised based on the comparisons between practice in Chile and international standards (Okada et al., 2016[29]), Chile has taken steps to standardise and improve the quality of colorectal cancer diagnosis through international collaboration.
3.3.5. Some efforts to build public awareness of cancer screening and prevention have been made
In order to build public awareness of the prevention and early detection of cancer, Chile has carried out several initiatives. Awareness-building campaigns are undertaken periodically such as International Day for specific cancer throughout a year. Over the past decade, together with all stakeholders involved, the Department of Cancer within the Ministry of Health has also organised The Week of Cancer Prevention annually, to build awareness on cancer through more education and enhanced communication. It also provides an opportunity for cancer screening. In addition, health care providers usually inform patients and their families in the target age to undergo vaccinations and cancer screening during their medical consultation.
However, access to these cancer screening tests is considered low. Since the information system is not established for opportunistic screening tests, screening coverage is not well understood. Challenges raised in the previous section for mammography coverage are relevant also for these cancers, and low public awareness of the importance of early detection of cancer and the lack of provider incentives for increasing the coverage of screening tests also point to low coverage of these screening services. In addition, long waiting time in primary care also lead to challenges in accessing these tests as they are provided in primary care settings.
Partly reflecting such challenges, outcomes of prostate, colorectal, stomach, lung and liver cancers are relatively poor in Chile compared to other OECD countries. These relatively poor outcomes suggest that further efforts concerning prevention and early detection of these cancers can be made.
3.4. Chile needs to further strengthen its effort in cancer prevention and screening
In order to reduce the burden of cancer, Chile could to do more in the areas of cancer prevention, cancer screening and early detection of cancer. This section focuses on advances that Chile could make in view of improving cancer screening coverage and promoting early detection of cancer, particularly in areas such as stakeholder engagement, communication strategies, resource allocations, quality assurance and monitoring. These recommendations could be incorporated either in an overarching National Cancer Strategy or Plan with consolidated efforts or with specific policy focus, or they could be incorporated as part of specific policies, for instance, for cancer screening programmes and/or the development of a national cancer registry. Recommendations related to risk factors which are relevant for reducing risks of developing cancers among people in Chile, for instance smoking, harmful alcohol consumption, or obesity, and approaches that Chile can take with regards to expanding the role of genetic tests to complement existing cancer screening and other diagnostic services, are discussed in the other chapters of this review.
3.4.1. Systematic involvement of key stakeholders needs to be encouraged to further develop strategies for cancer prevention and screening
With a view to further enhance cancer strategies such as cancer prevention and screening nationwide, Chile could involve key local stakeholders during the policy development and decision-making processes as done in other OECD countries. As mentioned in Section 3.2, in countries with decentralised health systems including Australia and Spain, an involvement of different key local stakeholders including regional authorities and civil society has led to a successful nationwide implementation of cancer strategies.
In fact, Chile already has a good example of stakeholder involvement for cervical cancer and such efforts should be extended when developing prevention and screening strategies for other cancers. Key local stakeholders need to be involved in developing and strengthening screening strategies for other cancer such as breast, colorectal and stomach cancer because barriers to accessing cancer screening may be specific to regions and different among people with different cultural and socio-economic background within the country. Voices of local stakeholders such as regional administrations, health care providers and representatives of the civil society need to be sought in order to identify specific barriers to accessing cancer screening and to address specific needs particularly among the disadvantaged. The goal should also be ensuring that all stakeholder are be better informed, and therefore more engaged in providing diagnostic services effectively to the target population. This could indirectly help to build the public awareness on the importance of early detection of cancer.
3.4.2. More systematic personalised invitations could improve cancer screening coverage
In order to improve coverage of cancer screening, Chile could adopt a more systematic and personalised approach in inviting target populations, as has been implemented in many OECD countries. An increasing number of OECD countries identify each individual in the target group and send a personal invitation letter for cancer screening, issued through a registry in a systematic manner. In Chile, however, an invitation letter is sent only for cervical cancer screening and information provided in the letter may not be sufficient. In the majority of OECD countries, the invitation letter includes information on the benefits and potential harms of cancer screening such as false-positive screening results, over-diagnosis and over-treatment, and asks for either signed or verbal informed consent for screening (European Commission, 2017[30]). This practice is in accordance with international recommendations as the WHO recommends organised population-based mammography screening programmes to provide information on both benefits and risks of mammography screening so that target women are able to make an informed decision before undergoing mammography (WHO, 2014[31]). In many OECD countries, additional efforts are also made to invite people with positive screening results in the past for follow-up assessment, and in some countries such as Denmark, Finland, Germany, Ireland, Italy, the Netherlands, Spain, Sweden and the United Kingdom, appointment date is fixed for mammography in the letter to further facilitate access to cancer screening (European Commission, 2017[30]; IARC, 2015[32]).
As additional cost is associated with these invitation strategies, cost-effectiveness approaches would need to be applied in Chile. Several studies have been undertaken and assessed the effectiveness of invitation strategies in increasing cancer screening. For example, a systematic review of different studies conducted in various countries found that effective screening invitations include a postal invitation and telephone reminders, primary care physician’s signature on invitation letter, and scheduled appointment instead of open appointment (Camilloni et al., 2013[33]). In addition, a Chilean study undertaken in one of the underserved municipalities in the region of Santiago found that cancer screening invitation by postal mail already increased screening coverage, but a postal invitation, complemented by telephone call and face-to-face intervention, substantially increased the coverage (Puschel and Thompson, 2011[24]). Future studies would also need to examine the cost associated with each of the invitation options and its impact in order to identify the most appropriate cost-effective strategies which may be different across regions.
3.4.3. Better communication and information-sharing strategies could improve public awareness and health literacy
Alongside more personalised invitation to cancer screening, Chile could develop further communication and information-sharing strategies to improve public awareness on cancer prevention and screening and health literacy of the population. In this context, the Ministry of Health in Chile has developed manuals for informing the public in the community and at work about healthy lifestyles to prevent cancer and the importance of early detection for cancer. However, these manuals are extensive and include information for various different audiences all together, for instance, to be used by health professionals for diagnosis and referral and to guide patients through pathway. It may be more effective in increasing public awareness if separate materials are developed specifically for the public.
As systematic sharing of information related to cancer is limited, particularly for cancer without organised screening programmes, Chile could also better develop information-sharing strategies to help patients to seek care, including cancer diagnostic services, at the right place at the right time. In this context, an increasing number of OECD countries have developed information-sharing platforms to better involve and enable patients in taking care of their own health and navigating through health care systems for their conditions. For example, some OECD countries including Denmark (see Box 3.5), England and Estonia have developed a platform such as a website or e-Health account to share evidence-based information on health care for different diseases including cancer throughout patient pathway with a view to promoting health literacy of the population and to support them to seek health care including cancer screening, diagnosis and treatment appropriately in a timely manner.
Box 3.5. Sundhed.dk, the Danish e-health portal
Sundhed.dk, the Danish e-health portal, is the official portal for the public Danish health care services and enables patients and health care professionals to find information and communicate. It is a public, internet-based portal that collects and distributes health care information among citizens and health care professionals. In a secure part of the portal the patient has access to:
Personal health data on treatments and notes from hospital records, information about medication and visits to the GP;
Various e-services including making appointments with GP’s, prescription renewals and electronic communication with the GP;
Information on waiting times at all public hospitals and ratings of hospitals in terms of patient experienced quality;
Patient networks and the sundhed.dk handbook for patients.
This portal brings the entire Danish health care sector together and provides an accessible setting for citizens and health care professionals to meet and efficiently exchange information. By servicing both the citizens and the health professionals, the portals aim is to enable the two to achieve cooperation based on the same data. This empowers the citizen and gives the health professionals better tools to improve quality in care (OECD, 2013[12]).
3.4.4. Chile should explore ways to improve access to cancer screening and diagnostic tests across regions and population groups
There are some signs that low access to cancer screening and diagnostic tests are related to unequal availability of resources across regions. To improve geographic access to diagnostic services including cancer screening, Chile could consider taking following approaches, likely in tandem.
First, Chile could seek to ensure that necessary medical technologies are in place across all regions. For instance, the number of colonoscopes is not adequate in some regions and waiting time is long, so Chile needs to assure access to medical technologies across regions and population groups.
Second, innovative technological solutions could be explored as they can help overcome geographic challenges in assuring access, and can also be cost-effective. Although still limited, Chile already uses mobile mammography, and could seek other more mobile solutions to increase cancer screening. For instance, Turkey also faces geographic challenges and it increased the use of mobile screening units and tele-radiology (OECD, 2014[34]). Chile could also consider utilising high-quality self-sampling tools for cancer screening. Some countries such as the Czech Republic, Denmark, Finland and Norway have undertaken trials to send self-sampling device for cervical cancer screening such as lavage and brush devices to target age women who had previously declined screening participation and these targeted trials using new device were found effectiveness at reaching out to non-participants. In addition, women’s experiences were generally positive and sample devices were well received (Burger et al., 2017[35]; Enerly et al., 2016[36]; Ondryášová et al., 2015[37]). A systematic review of studies conducted in various countries found that for colorectal cancer, mailing a self-sampling kit to target population was an effective way to improve screening coverage (Camilloni et al., 2013[33]).
Third, given the geographic characteristics of Chile, financial support to cover travel cost may be needed, particularly among low-income groups with high risks to assure access to different diagnostic tests if geographic access is still considered problematic even after expanding the use of technological solutions. Unmet health care needs are high among those with low income group living in isolated areas (Ministry of Social Development, 2015[38]), but so far, financial support for travel cost is available only for child patients and one adult guardian for distances longer than 500km. Other patients and their guardians still need to bear the travel cost completely and the existing infrastructure does not sometimes allow easy access to health care including diagnostic services for cancer. Some OECD countries also face such geographic challenge and to assure access to cancer care, Finland, for example, provides a subsidy to cover travel cost to all cancer patients. It may be too costly to cover the entire cost, so an adequate level of cost-sharing and target population group would need to be identified in the Chilean context.
3.4.5. Comprehensive information systems can help manage screening programmes more effectively
Chile has developed a monitoring system for cancer screening and cancer care system based on population surveys and some cancer registries, but its coverage is limited in terms of type of cancer and regions. For breast and cervical cancer, population-based surveys regularly collect screening coverage and barriers to screening in view of seeking ways to increase screening coverage. However, such data collection efforts are not being made for other cancer such as colorectal cancer. In relation to cancer registries, the first regional registry was developed in the region of Los Ríos in 1989, followed by Antofagasta in 1998 and Biobío in 2006. However, cancer registry has not been established at the national level, so even after all these regional registries become fully operational, they will cover only about 18.5% of the population in Chile (Jimenez de la Jara et al., 2015[8]). For cervical cancer and childhood cancer, however, an integrated information system has been developed at the national level. The information system for cervical cancer has been expanded and data are linked across providers in the private and public sectors and registries. For childhood cancer, data from private and public sectors have been integrated in the national cancer registry since 2011.
A comprehensive information system based on registries is essential for efficient management of screening programmes and cancer care delivery. It can identify target population who have and have not participated in the screening programmes, those who are monitored outside of the programme due to their previous diagnosis of cancer and/or genetic predisposition to specific cancer and those who do not consent to do screening. Using such a system, personalised invitations and reminders for cancer screening, which are important for increasing screening coverage, can be sent systematically to target population. In the majority of OECD countries, national cancer registries have been established and their information systems allow monitoring cancer incidence and survival at the national as well as regional levels for a number of cancers. For example in New Zealand, the Cancer Registry Act, introduced in 1993, aims to improve information base for cancer prevention and research. Its cancer registry collects data including date of diagnosis, site of primary care, type of cancer test, morphology, grade, staging information and site-specific information, and monitors incidence, mortality and survival regularly by cancer and also by region (Ministry of Health, 2014[3]).
To develop population-based screening programme further, Chile would also need to integrate individual-level data collected within and outside of cancer screening programmes around screening, diagnosis and treatment in a more systematic manner across regions and providers for different cancer. Such information can increase efficiency and effectiveness of cancer screening. If Chile decides to include genetic information in the integrated information system, regulations specific to genetic data would need to be developed also. As a development of integrated information system can be costly, Chile could prioritise the information needs as has been done in other OECD countries. For example, in New Zealand, due to concerns over cost, data on certain cancer such as benign neoplasms are not collected (Ministry of Health, 2014[3]).
Rich data generated from integrated information system need to be analysed periodically to assess the effectiveness of existing cancer screening protocols such as target group, screening frequency and/or methods and across population with different background. Chile has started assessing the effectiveness of screening programmes for breast and cervical cancer based on information collected at registries including stage information, and such efforts need to be extended to other cancer.
Several OECD countries also use information around cancer screening to improve quality of screening programmes (OECD, 2012[39]) (Box 3.6). They provide feedback to individual providers and benchmarking is also possible. A systematic literature review supports these additional efforts as it found that provider assessment and feedback contribute to increased coverage for cervical, breast and colorectal cancer screening (Sabatino et al., 2012[40]). Based on these initiatives elsewhere, Chile could explore ways to effectively utilise data to drive improvement in cancer screening quality across providers.
Box 3.6. Quality Assurance system for cancer screening in Israel
A comprehensive quality assurance mechanism has been developed in Israel for breast cancer. Every entry to the cancer detection centre is registered in a centralised electronic database, which was established in the mid-1990s. The database contains screening information from all public and private providers, and over 90% of diagnosis test results for individuals who had a mammography. Data including detection rates, recall rates, further examination rates, and staging information, and negative/positive test result rates are provided to all providers every year so that they can compare their performance relative to the national average and to other providers in the country. Using the database, every care pathway is monitored, and providers receive a report in case of an irregular pathway. A similar system exists for colorectal cancer, but there is a need to improve the collection of colonoscopy data (OECD, 2012[39]).
Furthermore, Chile may wish to explore effective ways of reporting key health information such as screening coverage to improve public awareness on cancer screening. Many OECD countries make these data available in the public domain in a user friendly manner. In the similar vein, Chile also reports screening coverage for breast and cervical cancer in the public domain. However reporting of these data can be improved. For example, even though the breast cancer screening programme in Chile targets women aged between 50 and 69 years, survey reports published by the Ministry of Social Development include screening coverage referring to women aged 35 and over (Ministry of Social Development, 2015[38]). Similarly, for cervical cancer, even though the screening programme targets women between 25 and 64 years of age, screening coverage of women aged 15 and over is reported. Chile may want to consider reporting data consistently for their analyses and reports.
3.4.6. Effective detection of cancer at an early stage requires strong primary care and standardised and high quality diagnosis
In Chile, cancer screening is provided at primary health centres or provided based on referrals from these centres, so access to primary care and its quality are essential for successful cancer screening. However, resources are stretched, resulting in long waiting time in primary care, short consultation time and poor care coordination. While strategies to improve prevention and cancer screening are critical, improvement in cancer survival will also depend on having an effective and high quality primary care sector.
For effective detection of cancer at early stage, Chile also needs to continue assuring the quality of diagnosis. Chile already follows international standards in assuring quality of screening for breast and cervical cancer, and has also taken steps to standardise and improve the quality of diagnosis through clinical guideline developments based on international collaboration for colorectal cancer, genetic testing for breast cancer and leukaemia. Such efforts ought to be continued for different types of cancer in order to provide high quality diagnostic services.
3.5. Conclusion
In Chile, cancer could become the first cause of mortality in the near future because while overall mortality rates from cancer are declining, they are not falling as fast as mortality due to other diseases, and risk factors for cancer are also increasing among the population. In order to tackle the burden of cancer, Chile has strengthened cancer care governance and delivery, and introduced cervical and breast cancer screening programmes. However, more still needs be done in order to strengthen Chile’s cancer screening programme. There is scope to expand the coverage of screening – notably by improving stakeholder engagement in developing cancer screening strategies, introducing more systematic personalised invitation for cancer screening, developing better communication strategies to increase public awareness. As primary care is a key for providing cancer screening in Chile, primary care strengthening should not be overlooked as a part of cancer prevention and detection strategies. Chile should also look to improve geographic access to screening and diagnostic tests for instance through innovative solutions and financial support for the disadvantaged. Meanwhile, developing a more comprehensive monitoring system for cancer screening would help Chile in both the administration of the cancer screening programme – assuring effective target population coverage – and be a rich source of data with which Chile could periodically assess the effectiveness of existing cancer screening protocols.
References
[18] Allemani, C. et al. (2018), “Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries”, The Lancet, Vol. 391/10125, pp. 1023-1075, http://dx.doi.org/10.1016/S0140-6736(17)33326-3.
[5] American Cancer Society (2017), Cancer A-Z, https://www.cancer.org/cancer.html (accessed on 14 December 2018).
[14] Bitrán, R., L. Escobar and P. Gassibe (2010), “After Chile’s Health Reform: Increase In Coverage And Access, Decline In Hospitalization And Death Rates”, Health Affairs, Vol. 29/12, pp. 2161-2170, http://dx.doi.org/10.1377/hlthaff.2010.0972.
[35] Burger, E. et al. (2017), “The Cost-Effectiveness of Cervical Self-Sampling to Improve Routine Cervical Cancer Screening: The Importance of Respondent Screening History and Compliance”, Cancer Epidemiology Biomarkers & Prevention, Vol. 26/1, pp. 95-103, http://dx.doi.org/10.1158/1055-9965.EPI-16-0350.
[33] Camilloni, L. et al. (2013), “Methods to increase participation in organised screening programs: a systematic review”, BMC Public Health, Vol. 13/1, p. 464, http://dx.doi.org/10.1186/1471-2458-13-464.
[36] Enerly, E. et al. (2016), “Self-Sampling for Human Papillomavirus Testing among Non-Attenders Increases Attendance to the Norwegian Cervical Cancer Screening Programme”, PLOS ONE, Vol. 11/4, p. e0151978, http://dx.doi.org/10.1371/journal.pone.0151978.
[30] European Commission (2017), Cancer Screening in Report on the implementation of the Council Recommendation on cancer screening, https://ec.europa.eu/health/sites/health/files/major_chronic_diseases/docs/2017_cancerscreening_2ndreportimplementation_en.pdf (accessed on 19 September 2018).
[27] Forman, D. and V. Burley (2006), “Gastric cancer: global pattern of the disease and an overview of environmental risk factors”, Best Practice & Research Clinical Gastroenterology, Vol. 20/4, pp. 633-649, http://dx.doi.org/10.1016/j.bpg.2006.04.008.
[15] Frenz, P. et al. (2014), “Achieving effective universal health coverage with equity: evidence from Chile”, Health Policy and Planning, Vol. 29/6, pp. 717-731, http://dx.doi.org/10.1093/heapol/czt054.
[4] Garmendia, M., P. Ruiz and R. Uauy (2013), “Obesity and cancer in Chile: estimation of population attributable fractions (Obesidad y cáncer en Chile: estimación de las fracciones atribuibles poblacionales)”, Revista médica de Chile, Vol. 141/8, pp. 987-994, http://dx.doi.org/10.4067/S0034-98872013000800004.
[25] IARC (2016), European Code Against Cancer - Why is prostate cancer screening not recommended?, https://cancer-code-europe.iarc.fr/index.php/en/ecac-12-ways/screening-recommandation/key-points-about-cancer-screening/216-prostate-cancer-screening-not-recommended (accessed on 14 December 2017).
[32] IARC (2015), IARC Handbooks of Cancer Prevention: Benefits of mammography screening outweigh adverse effects for women aged 50–69 years, http://ci5.iarc.fr/cI5I-x/default.aspx. (accessed on 19 September 2018).
[2] IARC GLOBOCAN (2018), Cancer Today, http://gco.iarc.fr/today/home (accessed on 20 November 2018).
[8] Jimenez de la Jara, J. et al. (2015), “A snapshot of cancer in Chile: analytical frameworks for developing a cancer policy”, Biological Research, Vol. 48/1, p. 10, http://dx.doi.org/10.1186/0717-6287-48-10.
[26] López-Kostner, F. et al. (2018), “Programa multicéntrico de cribado de cáncer colorrectal en Chile [Results of a multicentric colorectal cancer screening program in Chile]”, Revista médica de Chile, Vol. 146/6, pp. 685-692, http://dx.doi.org/10.4067/s0034-98872018000600685.
[13] Ministry of Health (2015), AUGE 10 years, Ministry of Health, Santiago.
[3] Ministry of Health (2014), Basic Health Indicators Chile 2014, Ministry of Health, Santiago.
[38] Ministry of Social Development (2015), CASEN 2015: Health Synthesis results, http://observatorio.ministeriodesarrollosocial.gob.cl/casen-multidimensional/casen/docs/CASEN_2015_Resultados_salud.pdf (accessed on 14 December 2018).
[11] Moore, S. et al. (2014), “Cancer in indigenous people in Latin America and the Caribbean: a review.”, Cancer medicine, Vol. 3/1, pp. 70-80, http://dx.doi.org/10.1002/cam4.134.
[6] NHS Choices (2017), Health A-Z - NHS, https://www.nhs.uk/conditions/ (accessed on 14 December 2018).
[1] OECD (2018), OECD Health Statistics 2018, OECD Publishing, Paris, https://doi.org/10.1787/health-data-en.
[17] OECD (2017), Strengthening the international comparison of health system performance through patient-reported indicators, OECD, Paris, https://www.oecd.org/els/health-systems/Recommendations-from-high-level-reflection-group-on-the-future-of-health-statistics.pdf (accessed on 14 December 2018).
[7] OECD (2015), Health at a Glance 2015: OECD Indicators, OECD Publishing, Paris, https://dx.doi.org/10.1787/health_glance-2015-en.
[34] OECD (2014), OECD Reviews of Health Care Quality: Turkey 2014: Raising Standards, OECD Reviews of Health Care Quality, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264202054-en.
[12] OECD (2013), Cancer Care: Assuring Quality to Improve Survival, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264181052-en.
[39] OECD (2012), OECD Reviews of Health Care Quality: Israel 2012: Raising Standards, OECD Reviews of Health Care Quality, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264029941-en.
[28] OECD (forthcoming), OECD Reviews of Public Health: Japan, OECD Publishing, Paris.
[16] OECD/European Observatory on Health Systems and Policies (2017), France: Country Health Profile 2017, State of Health in the EU, OECD/European Observatory on Health Systems and Policies, Paris/Brussels, http://dx.doi.org/10.1787/888933593532.
[29] Okada, T. et al. (2016), “International collaboration between Japan and Chile to improve detection rates in colorectal cancer screening”, Cancer, Vol. 122/1, pp. 71-77, http://dx.doi.org/10.1002/cncr.29715.
[37] Ondryášová, H. et al. (2015), “[Utilization of self-sampling kits for HPV testing in cervical cancer screening - pilot study].”, Ceska gynekologie, Vol. 80/6, pp. 436-43, http://www.ncbi.nlm.nih.gov/pubmed/26741158 (accessed on 19 September 2018).
[19] PINDA (2009), Cáncer del Niño : Programa del Cáncer en Niños, Unidad de Cáncer, MINSAL.
[24] Puschel, K. and B. Thompson (2011), “Mammogram screening in Chile: Using mixed methods to implement health policy planning at the primary care level”, The Breast, Vol. 20, pp. S40-S45, http://dx.doi.org/10.1016/j.breast.2011.02.002.
[10] Roco, Á. et al. (2013), “Situación del cáncer en Chile 2000 – 2010 [Cancer Status in Chile 2000 – 2010]”, Cuad. méd.-soc, Vol. 53/2, pp. 83-94, http://www.colegiomedico.cl83ARTÍCULOSORIGINALES (accessed on 14 December 2018).
[40] Sabatino, S. et al. (2012), “Effectiveness of Interventions to Increase Screening for Breast, Cervical, and Colorectal Cancers”, American Journal of Preventive Medicine, Vol. 43/1, pp. 97-118, http://dx.doi.org/10.1016/j.amepre.2012.04.009.
[21] Sakellariou, D. and E. Rotarou (2017), “Utilisation of cancer screening services by disabled women in Chile”, PLOS ONE, Vol. 12/5, p. e0176270, http://dx.doi.org/10.1371/journal.pone.0176270.
[23] Schilling, A., C. Gonzalez and F. Muñoz (2016), HPV Vaccination Coverage at 2 years of Initiating the National Vaccination Programe for Chilean Girls, http://secure.key4events.com/key4register/AbstractList.aspx?e=477&preview=1&aig=-1&ai=10766 (accessed on 14 December 2018).
[20] Sepúlveda, C. and R. Prado (2005), “Effective cervical cytology screening programmes in middle-income countries: The Chilean experience”, Cancer Detection and Prevention, Vol. 29/5, pp. 405-411, http://dx.doi.org/10.1016/J.CDP.2005.07.001.
[9] The Government of Chile (2010), The National Strategies of Health 2011-2020, Government of Chile, Santiago.
[22] WHO (2014), “Human papillomavirus vaccines: WHO position paper, October 2014.”, Weekly Epidemiological Record, Vol. 89/43, pp. 465-91, http://www.ncbi.nlm.nih.gov/pubmed/25346960 (accessed on 14 December 2018).
[31] WHO (2014), “WHO | WHO position paper on mammography screening”, WHO.