Marion Devaux
Shunta Takino
Michele Cecchini

Marion Devaux
Shunta Takino
Michele Cecchini
This chapter summarises the key findings of this report. It first explores the links between work and employee health and well-being. It then discusses the potential of interventions in the workplace to promote health and well‑being. It also describes policy levers implemented in G7 and three other OECD countries in the Asia and Pacific region to support and incentivise employers to promote health and well-being in the workplace. Finally, it examines how companies that promote employee health and well‑being can attract investors that prioritise environmental, social and governance (ESG) considerations, and what initiatives exist to facilitate such investments.
The relationship between health and work goes in both directions. Employment and work conditions affect people’s health, and health conditions affect employment and workers’ productivity. The rise in unhealthy lifestyles and related chronic diseases poses a threat to the health of the workforce and damages labour market outcomes.
Characteristics of work, including a safe work environment, job quality, job strain, work organisation, occupation and sector of employment, and employment type all shape and influence workers’ health. For instance, according to data from the European Working Conditions Survey, in 2015, workers with a poor working environment (40%) were more than twice more likely to report that work had a negative impact on their health than workers in a good working environment (15%). Differences in the nature of work by socio-economic status also contribute to the social gradient in health, as individuals of lower socio-economic status are more likely to have less secure jobs and lower quality jobs that, in turn, have an adverse impact on health.
Major risk factors for non-communicable diseases (NCDs), such as overweight, smoking, harmful alcohol use, and high levels of stress, are widespread in the adult population. For instance, two in five full-time employees (42%) reported being stressed in OECD countries in 2017‑19, a leading risk factor for mental health conditions, cardiovascular diseases and musculoskeletal disorders. Long COVID‑19 has added to the burden of long-standing illnesses and is estimated to affect around 10% of people infected by the coronavirus.
Having unhealthy lifestyles and NCDs is associated with a lower probability of being employed and lower work productivity when employed. For instance, smokers are estimated to take 28% more days off work than ex-smokers in the United States, and this difference is 18% in France, Germany, Italy, Spain and the United Kingdom, based on 2013 data. The productivity losses due to NCD-related presenteeism – that is reduced productivity while at work – tend to be two to three times higher than that of absenteeism, in 12 OECD and G20 countries.
Combined with the prevention of occupational risks, workplace health promotion programmes benefit employees, improving their lifestyles, health and well-being, while also producing benefits for the employers.
Workplace‑based programmes can reach out up to 610 million people employed in the formal sector in OECD countries. About two‑thirds of these people are employed in small and medium sized enterprises (SMEs) that are less likely than large companies to implement such programmes due to limited resources and lack of scale in absence of specific incentives.
Workplace health promotion programmes are worth the investment. They can reduce health care spending, decrease sickness absenteeism and increase work productivity. For instance, based on OECD modelling-based analyses, scaling up interventions addressing sedentary behaviour and promoting physical activity at work could improve employment and productivity equivalent to having an increase of 37 000 workers per year in 30 OECD countries, with a positive economic return of USD 4 for each dollar invested. Promoting employees’ health also strengthens corporate image – which helps recruit and retain talent – and increases employees’ satisfaction and work engagement.
Employees generally benefit from workplace programmes, with evidence for improved lifestyles and health (e.g. smoking cessation, healthier weight) in the short and medium-term. High participation is crucial for maximising the potential effectiveness of such programmes. Organisational factors – such as an integrated approach to occupational safety and health prevention, and a healthy workplace culture – also contribute to the success of workplace health-promoting programmes.
A growing number of companies are implementing health promotion programmes across European countries. For instance, according to the European Survey of Enterprises on New and Emerging Risks, 32% of the respondent companies reported they implemented measures raising awareness of nutrition among employees in 2019, compared to 28% in 2014.
An OECD analysis of data from 114 companies worldwide participating in the 2020 Workforce Disclosure Initiative shows that health and well-being programmes usually offer support for various risk factors for NCDs. Mental health and stress programmes were the most often reported programmes, with more than two‑thirds (68%) of participating companies, although the data do not report the uptake by or experiences of employees. The data also show how companies adapted their responses to ensure health and safety at work during the COVID‑19 crisis, including in particular, mental health support, measures to limit the propagation of the virus, such as enabling teleworking and enhancing hygiene and financial support, such as salary guarantees.
Governments use a range of policy levers to support employers in promoting health and well-being in the workplace, as identified in an analysis of ten countries, including G7 countries and OECD countries in the Asia and Pacific region:
Workplace regulations set minimum standards in terms of preventing risks and managing health, safety and well-being at work, and feature prominently in efforts to prevent long working hours, limit smoking, and promote timely return-to-work following sickness absence. Regulations on maximum working hours exist in six of the ten countries. All ten countries limit smoking at work, with Australia, New Zealand and the United Kingdom enforcing a comprehensive workplace smoking ban. Employer-paid sick leave systems exist in six of the ten countries reviewed, while gradual return-to-work mechanisms exist in only two countries. In some countries such as federal governments, sub-national authorities may play an important role in occupational safety and health regulation and enforcement.
Financial incentives include lower insurance premiums, tax credits and subsidies for employers of SMEs. In all ten countries reviewed, employers with a better record of ensuring worker health and safety can benefit from lowered accident insurance premiums. Corporate tax credits for expenditure related to workplace health and well-being were identified at the national level in France, Germany, Italy and the United Kingdom. Subsidies for employers to promote health and well-being at work were identified in at least four countries (either national or sub-national level).
Disseminating information and guidance developed together with other stakeholders, such as charities, trade unions and employer associations, can facilitate the promotion of health and well-being at the workplace. This can increase awareness – especially for stigmatised health issues – and increase understanding among employers and managers of effective measures. Government-developed tools for employers to diagnose gaps in their workplace health programmes were identified in France, Germany, the United Kingdom and the United States. Guidance related to COVID‑19 has also been widely disseminated to employers, typically related to sanitary measures, ventilation, teleworking, facilitation of sick leave and self-isolation.
Certification and award schemes provide reputational benefits for employers, by certifying that employers meet certain standards relating to health and well-being promotion at work. For example, the Health and Productivity Management Programme in Japan is a particularly large‑scale certification and award scheme covering more than 80% of the largest publicly owned companies in the Nikkei 225. These schemes often go hand-in-hand with the disclosure of information on company-led programmes and health and well-being in the workplace, which can be used to inform both policy and employer interventions, although collection of such data can raise concerns about data protection and privacy in some countries.
The special focus looks at how to attract investors and private funds to steer their investment towards companies promoting health and well-being among their employees, as this can amplify and reinforce government efforts to promote health and well-being at work. It draws on the growing interest in using environmental, social and governance (ESG) and human capital considerations to guide investments.
Institutional investors and private funds, looking for sustainable and socially responsible investments, seek to invest in companies that prioritise the health and well-being of their employees. In the United States, between 2001 and 2014, companies that were awarded for their workplace health programmes saw their combined stock value appreciated up to three times more than companies comprising the Standard & Poor’s 500 Index. Evidence in Japan also suggests that companies certified by the Health and Productivity Management Programme also perform better on the Tokyo Stock Exchange.
Supporting ESG investments can create a virtuous cycle, where the incentive for companies to promote employee health is amplified. This is because a company that promotes the health and well-being of employee is rewarded not only with a healthier workforce, but also with an increased likelihood of receiving investment.
A key limitation to unlocking this virtuous cycle is the lack of comparable information on health and well-being at work that would allow investors to differentiate between companies that effectively promote the health and well-being of their employees and those that do not. Governments and other stakeholders are closing this gap through regulatory changes that require companies to report information on health and well-being programmes, as well as voluntary initiatives promoting information disclosure. Standard-setting initiatives, such as the Global Reporting Initiative, play an important role in harmonising and standardising the disclosure mechanisms through work across countries and companies.
Health and well-being are fundamental for enjoying a good and productive life. While health and well-being impact employment prospect and productivity at work, they are conversely affected by the nature of work. For instance, people living with a chronic disease are less likely to be employed than those with no disease, and have more work absence and are less productive (OECD, 2019[1]; OECD, 2021[2]). Conversely, the nature of work, such as for example high job strain, influences employees’ health and well-being, the latter being related to the physical, psychological, emotional and psychosocial experiences lived at work, encompassing physical and mental health, and job satisfaction.
As adults spend a large portion of their lives in employment, workplace‑based actions are crucial for ensuring employee health and safety and are increasingly considered as key for promoting health, healthy lifestyles and well-being, in particular to influence choices favouring healthier lifestyles across the work-life continuum from the first job to retirement. Employers have long had statutory requirements to protect workers against occupational risks for health and safety (such as chemicals, carrying heavy loads, etc.). Yet employers do not necessarily take the next step of actively promoting healthy lifestyles, health and well-being in the workplace. There are further opportunities for workplaces to expand the outreach of health promotion interventions, in particular towards workers with increased health risks, and to adapt to enable workers with disabilities, including chronic diseases, to continue working. To achieve this goal, efforts to improve health in the workplaces have to adapt to the changing world of work, recognising the rising number of employees in non-standard forms of employment (i.e. part‑time, temporary or self‑employed workers), often undertaking new forms of work (such as gig workers, platform workers).
Megatrends such as population ageing, the spread of chronic health conditions, and the challenges these pose for the financial sustainability of the health system place even greater importance on promoting health and preventing non-communicable diseases (NCDs) through work. The workforce is ageing: by 2050, more than four in ten individuals in the world’s most advanced economies will be older than 50 (OECD, 2020[3]). Older workers are more likely to live with one or multiple chronic diseases that limit their participation in work and social activities. In response to these trends, there is rising consciousness among employees, employers and investors of the importance of a healthy workforce, which was amplified in the wake of the COVID‑19 pandemic.
Governments can steer employers to promote the health and well-being of their employees in the workplace. The benefits of early action to promote safety, health and well-being of employees are large for society-at-large, given that the economic costs of poor health include reduced workforce productivity, pressures on the social security system and increased health care expenditure. Governments therefore have an important role of supporting employers to scale up actions to promote the health and well-being of their employees, to promote effective return-to-work following sickness absences and to accommodate workplaces for those with chronic conditions.
This report supports the inclusion of active health promotion at work in the existing framework for occupational health and safety. This action enlarges the scope of actions from occupational hazards protection to health promotion, such as workplace interventions to prevent behavioural lifestyle risk factors for NCDs (Figure 1.1). The objectives of this report are to examine the potential of promoting health and well-being at the workplace, and highlight the policy levers available to governments to support employers to promote the health and well-being of their employees. Section 1.2 outlines the bi-directional relationship between health and work, and explains how the rise in unhealthy lifestyles and their related chronic diseases has negative impacts on the health of the workforce and productivity. Section 1.3 highlights that workplace programmes can reach a wide range of individuals across OECD countries, and thus improve employees’ lifestyles, health and well-being, while also producing benefits for the employers. Section 1.4 describes how health promotion at work fits in the national contexts of ten countries studied, including the Group of 7 (G7) and three other OECD countries in the Asia and Pacific region (Australia, Korea, and New Zealand). Sections 1.5 to 1.8 examine four types of policy levers, including regulation, financial incentives, dissemination of information, and certification and award schemes. Section 1.9 explains how companies that promote employee health and well-being are likely to attract growing interest from investors and discusses how governments – working together with other stakeholders – can trigger socially responsible investment towards health-promoting companies. Section 1.10 presents concluding remarks.
The relationship between health and work is bidirectional. Employment and working conditions affect people’s health (both physically and mentally), and conversely, health conditions impact employment and productivity at work (James, Devaux and Sassi, 2017[4]). This section recognises the former (Section 1.2.1), and then focusses on the latter, in order to highlight the importance of promoting health and well-being of working-age people (Section 1.2.2), but also for better labour market outcomes (Section 1.2.3).
Characteristics of work, including safe work environment, job quality, job strain, work organisation, occupation and sector, and employment type all shape and influence employee health (Saint-Martin, Inanc and Prinz, 2018[5]). A safe workplace, free from recognised hazards, is essential for protecting from work-related diseases and injuries, ensuring employee safety and health. While being in good quality work in general protects against ill-health, not all jobs are equally health-promoting. High job strain – which is characterised by low autonomy, repetitive work, long working hours and high frequency of workplace conflicts – is a major risk factor for ill-health (OECD, 2018[6]). For instance, based on analysis of data from the 2015 European Working Conditions Survey, in Europe, around 40% of workers reporting a poor working environment said that their work had a negative impact on their health, compared to 15% among workers with a good working environment (OECD, 2018[6]). Differences in the nature of work by socio-economic status also contribute to the social gradient of health, as individuals of lower socio-economic status are more likely to have less secure jobs and lower quality jobs that have an adverse impact on health (Institute of Heath Equity and Public Health England, 2015[7]).
Trends in the world of work – including the rise of new forms of employment and teleworking – are also having an impact on employee health. For instance, although the rise of teleworking and hybrid work only affects a small proportion of the total workforce (OECD, 2021[8]), it presents new challenges for employee health in workplaces that are affected. In particular, gig and platform workers who may be difficult to reach by workplace actions, are at risk of work-related stress, income insecurity and poor work-life balance. While well-managed telework can bring valuable flexibility, it can also present challenges such as increasing the risk of irregular hours and the blurring of work-life boundaries, which can be a risk factor for mental distress and anxiety (OECD, 2021[9]).
Unhealthy lifestyles, such as overweight, smoking, harmful alcohol use, and high levels of stress -which are major risk factors for NCDs – are widespread in the adult population. In OECD countries, more than 16% of the adult population smoked daily in 2019, and nearly 30% reported heavy episodic drinking at least once a month in 2016 (Figure 1.2). Overweight, which also includes obesity, affected more than half of the adult population (56%) in 2019 (OECD, 2021[10]), increasing the risk of diabetes, cardiovascular diseases (CVDs) and cancers. In 2017‑19, two in five full-time employees (42%) reported being stressed (Gallup Analytics, 2021[11]), a leading risk factor for mental health conditions as well as CVDs and musculoskeletal disorders (MSDs).
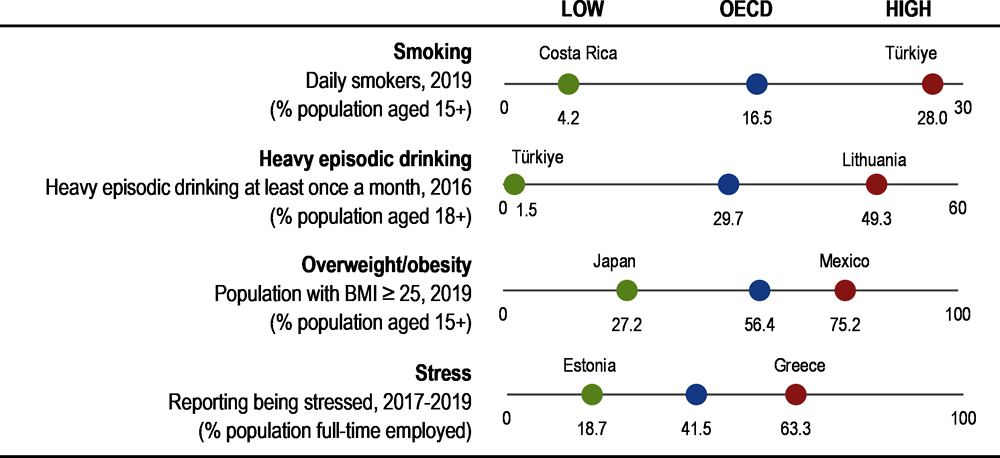
Note: Heavy episodic drinking is drinking more than 60 grammes of pure alcohol per drinking session.
Source: OECD Health Statistics 2021 for obesity/overweight and smoking; (OECD, 2021[2]) for heavy episodic drinking; (Gallup Analytics, 2021[11]) for level of stress.
Long COVID‑19 is adding to the burden of diseases in the working age population. Long COVID‑19 symptoms – such as fatigue, breathlessness, chest pain or anxiety that last weeks or months – are adding to the burden of long-standing illnesses, as it is estimated to affect about 10% of people infected by the coronavirus (Rajan et al., 2021[12]). Long COVID‑19 symptoms are more often associated with age, being female, overweight, prior hospitalisation for COVID‑19, and a number of symptoms in the acute phase (OECD, 2021[10]).
NCDs, including mental health conditions and substance use disorders, greatly affect the population in working age (20 to 64 years), with disparities across population groups. The chronic conditions that are the most often reported by working-age people are mental health disorders and MSDs. For instance in EU countries, about 43% of adults in working age reported suffering from MSDs (Eurostat, 2022[13]), while 45% faced risk factors for their mental well-being at work (e.g. time pressure, work overload, job security, etc.) (Eurostat, 2021[14]). When looking at the burden of disability – that accounts for premature death and the years lived with limitations – cancers rank first. Data from the Global Burden of Diseases shows that nearly three‑quarter of the burden of NCD-related disability in the age group 20‑64 is caused by five conditions: cancers (17%), MSDs (17%), mental health disorders (12%), CVDs (11%), substance use disorders (7%) and diabetes (7%) (IHME, 2020[15]). There are also important social inequalities in health. Individuals with lower education tend to report more NCDs than individuals with higher education. For instance, in EU member states, among people aged 16 to 64, those with lower education were 39% more likely to report a long-standing illness or health problem than those with higher education in 2020 (Eurostat, 2022[13]). In the United States, in a sample of 30‑64 year-olds, people with less than a bachelor’s degree had greater multi-morbidity than those with a bachelor’s degree or higher (Johnson-Lawrence, Zajacova and Sneed, 2017[16]). In Canada, nearly 18% of adults with less than high school education reported being diagnosed with at least two chronic diseases, compared to 7% of those with post-secondary graduate education, in 2019 (Public Health Agency of Canada, 2021[17]).
Evidence shows that having unhealthy lifestyles and NCDs is associated with a lower likelihood of being employed and less productivity when at work. People affected by one or multiple chronic diseases are often limited in their participation in social activities and work, potentially affecting employment prospect and productivity at work. An extensive review of the literature was carried out to examine the association between lifestyle risk factors, NCDs and labour market outcomes. Findings show that people with unhealthy lifestyles and NCDs have a lower probability of being employed and are less productive when at work (Table 1.1). For instance, smokers are estimated to take 28% more days off work than ex-smokers in the United States, and this difference is 18% in France, Germany, Italy, Spain and the United Kingdom, based on the 2013 National Health and Wellness Survey. Women with obesity are 68% more likely to miss work than women with a healthy weight, while this is not observed in men. The productivity losses associated with obesity-related diseases are equivalent to 54 million fewer full-time workers across 52 OECD, EU and G20 countries, which is similar to the number of employed persons in Mexico (OECD, 2019[1]). In addition to absenteeism, health issues can result in reduced productivity while at work, also known as presenteeism. When assessing the economic impact of NCDs in 12 OECD and G20 countries, the productivity losses due to presenteeism are two to three times higher than that due to absenteeism (Rasmussen, Sweeny and Sheehan, 2016[18]).
|
|
Employment |
Absenteeism |
Presenteeism |
|---|---|---|---|
|
Obesity |
People with obesity are less likely to be employed as compared to individuals with healthy weight. |
Higher BMI increases risk of sickness and disability by 8% per 1 kg/m2 BMI increase (Campbell et al., 2021[19]). (causal) Women with obesity are 68% more likely to miss work than women with healthy weight, this effect is non significant among men (Destri et al., 2021[20]) |
Presenteeism was found to be more prevalent among workers with obesity and overweight as compared to those with healthy weight (Keramat et al., 2020[21])). |
|
Smoking |
Smokers who are seeking reemployment, 27% were re‑employed a year after job loss, compared to 56% of non-smokers (Prochaska et al., 2016[22]). |
Current smokers in the US have 28% more absenteeism than former smokers; in five European countries, the difference is 18% while it is 61% in China (Baker et al., 2017[23]). |
Current smokers have 28%, 18% and 16% more presenteeism than former smokers, respectively in the US, five European countries and China (Baker et al., 2017[23]). |
|
Alcohol |
Problem drinking reduces employment (MacDonald and Shields, 2004[24]), and is linked to job loss (Airagnes et al., 2019[25]). |
Former drinkers and heavy drinkers work annually 1‑1.5 month less over the 20‑year observation period, compared with moderate drinkers (Böckerman, Hyytinen and Maczulskij, 2017[26]). |
A large body of evidence exists in support of alcohol-related presenteeism, but that this is weakened by low research quality and a lack of longitudinal designs (Magnus Thørrisen et al., 2019[27]) |
|
Diabetes |
Lower probability of employment (Devaux and Sassi, 2015[28]); and longer period of unemployment (Rodríguez-Sánchez and Cantarero-Prieto, 2017[29]). |
2‑10 more days of sickness absences (causal) (Breton et al., 2013[30]). |
Less workhour productivity when diabetic with symptoms: Individuals with diabetes and neuropathic symptoms are found to be 18% more likely to lose more than 2 hours of work per week due to illness when compared to their non-diabetic counterparts (causal) (Breton et al., 2013[30]) (Mori et al., 2020[31]). |
|
Cancer |
Lung cancer survivors are 61% more likely to be unemployed (Vayr et al., 2019[32]). |
Cancer survivors take 12 times more sick leave in the first year post-diagnosis than healthy workers, with sick leaving remaining still higher than the healthy average worker in the subsequent years (Sjövall et al., 2012[33]) |
Cancer patients and cancer survivors are more likely to experience presenteeism than controls, due to chronic symptoms associated cancer with treatment (Soejima and Kamibeppu, 2016[34]). |
|
Cardiovascular diseases (CVD) |
Workers with CVD were 2.5 times more likely to leave employment due to disability, 1.3 times more likely to take early retirement (Kouwenhoven-Pasmooij et al., 2016[35]). |
CVD workers missed 92 days compared to 11 days missed by non-CVD workers (Calvo-Bonacho et al., 2014[36]). |
The productivity loss among workers with CVD is twice higher from presenteeism than from absenteeism (Gordois et al., 2016[37]). |
|
Mental health conditions |
60% of people with moderate mental health conditions are employed compared to 70% of those with no mental distress (OECD, 2021[9]). |
Employees living with mental health conditions are more likely to be absent compared to those without mental health conditions; 12 additional days of sickness absence per year (OECD, 2021[9])). |
The productivity loss among workers with a mental health conditions is partially attributable to presenteeism. It is not clear if the impact of mental health conditions on presenteeism outweighs the impacts on absenteeism, and this may differ across countries (OECD, 2012[38]). |
|
MSDs |
Workers with MSD are less likely to be in fulltime employment (Summers, Jinnett and Bevan, 2015[39]); Working-age men/women with arthritis are 20%/25% less likely than their counterparts without arthritis to be economically active (Lubeck, 2003[40]). |
The number of days missed peaked at 147 days per year in the group diagnosed with rheumatoid arthritis, compared to 59 days in the general population (Neovius, Simard and Askling, 2011[41]). |
For the workers who experience clinically meaningful back pain, almost 80% of them also report productivity loss due to presenteeism, with 4.4 hours missed per worker over a two‑week period (Dall et al., 2013[42]). |
Source: Authors.
The observed negative labour market outcomes of unhealthy lifestyles and NCDs may reflect a true effect of unhealthy lifestyles and related health conditions on disabilities and work, or discrimination towards people with unhealthy lifestyles and NCDs. For instance, people with obesity are less likely to be employed, and when employed, they earn less than those with healthy weight. Evidence found that this reflects both a causal effect of obesity and its related health conditions on labour market outcomes, as well as discrimination and stigmatisation towards obese people. In this case, discriminatory hiring against obese persons and sorting into jobs with less customer contact – and thus lower wages- can explain poorer labour market outcomes for obese people (Averett, 2019[43]). That said, obesity appears to exert a causal effect on employment status, largely by affecting an individual’s health (diseases) rather than through increased unemployment arising from social discrimination (Campbell et al., 2021[19]).
As the evidence on health and well-being of the working-age population points to a significant impact of health on productivity, employers have a role to play not only to maintain good health and well-being of their employees, but also to increase labour participation and productivity. The following section examines the potential of workplace‑based interventions to enhance the health and well-being of employees.
Workplace‑based health and well-being programmes show great potential in terms of population outreach. In OECD countries, 610 million people are employed in the formal sector, making a sizeable population target for workplace health programmes. About one‑third (201 million) are employed in large companies, while about two‑thirds (409 million) are employed in small and medium sized enterprises (SMEs) (Figure 1.3). SMEs face greater challenges in implementing such programmes because of the cost of the programmes, insufficient human resources and lack of programme knowledge.
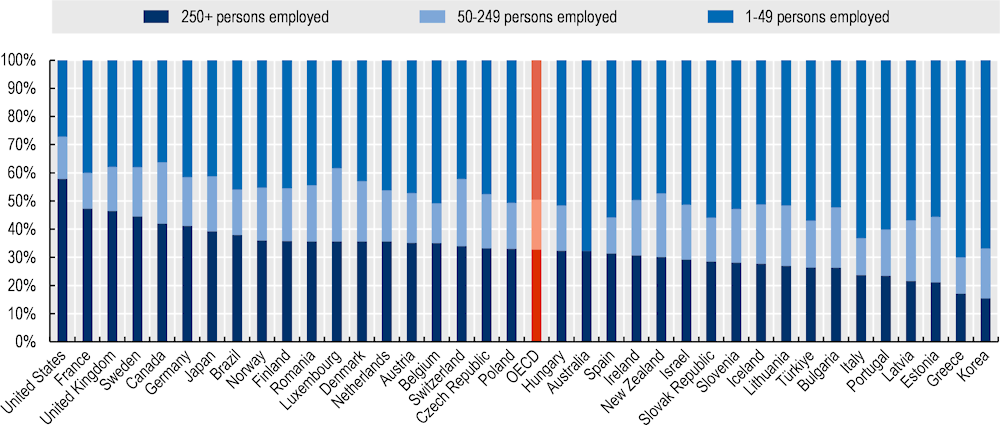
Note: The number of employees in Canada, Japan, and the United Kingdom includes all persons, workers and employees, covered by a contractual arrangement and working in the unit who receive compensation for their work, whether full-time or part-time.
Source: OECD Business Statistics by Employment Size Class, (2022[44]).
Although workplace health programmes are designed principally to benefit employees, they bring benefits to both employees and employers. For employees, workplace programmes can improve lifestyles (e.g. smoking cessation, healthier weight) and health in the short and medium-term, although robust evidence is lacking on their long-term effects (Sidossis et al., 2021[45]). Employee participation is crucial for maximising the potential impact of such programmes. For employers, workplace health and well-being programmes can reduce health care spending, decrease sickness absenteeism and increase work productivity. For instance, studies with a follow-up period of one to seven years indicate that for each dollar invested in workplace health and well-being programmes, employers can save between USD 1.5 and USD 5.6 in health care spending (Mattke et al., 2014[46]; Chapman, 2012[47]; Baicker, Cutler and Song, 2010[48]). Moreover, workplace programmes improving lifestyles, health and well-being, help reduce sick leave absenteeism by 25% (Chapman, 2012[47]) and thus, increase productivity. For instance, modelling work indicates that scaling up interventions reducing sedentary behaviour and promoting physical activity at the workplace could improve employment and productivity resulting in the equivalent of an additional 37 000 full-time equivalent workers per year in 30 OECD countries, for a cost between USD PPP 1 and 2 per capita (OECD, 2019[1]). Taking into account the impacts on health and life expectancy, savings in health expenditure and labour market cost, this programme would return USD 4 in the form of economic benefit for each dollar invested. Workplace programmes can also strengthen corporate image, which helps to recruit and retain talent, as individuals increasingly expect their employers to take into consideration their health and well-being.
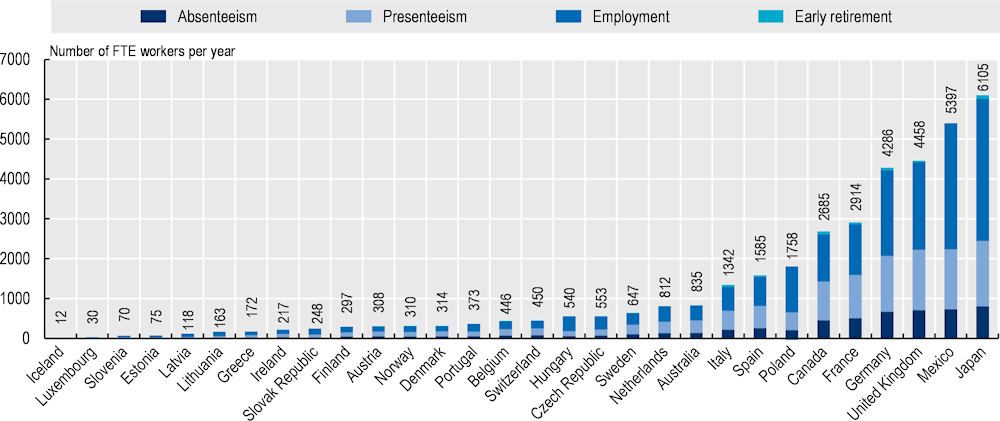
Note: FTE means full-time equivalent. Labour market inputs include employment and productivity when employed. They are expressed in the number of full-time equivalent workers and are calculated for the working-age population. OECD analyses based on the OECD SPHeP-NCDs model, which forecast the evolution of NCDs and risk factors and their related costs over the next 30 years.
Source: OECD, The Heavy Burden of Obesity, (OECD, 2019[1]).
The success of workplace health-promoting programmes relies in part on organisational factors such as an integrated approach into occupational safety and health prevention, and a healthy workplace culture. The starting point for workplace programmes that aim to promote employee health, healthy lifestyles and well-being, relies on good prevention and management of occupational risks. Growing evidence shows that an integrated approach of health promotion to occupational safety and health has greater outcomes, such as improved health behaviours, employee participation, reductions in injury illness and disability, reducing costs, and enhancing productivity (Tamers et al., 2019[49]). Another important condition for the success of workplace health programmes is a healthy workplace culture to create the enabling factors for employee uptake. Recent evidence showed that health and well-being outcomes across a wide range of workplace interventions are mediated by workplace culture change, such as job control, organisation support, work climate, management style, flexibility, work time expectation, supervisor support, line manager’s attitude and actions (Quigley et al., 2022[50]).
Workplace health programmes usually offer support for various risk factors for NCDs. Data from the 2020 Workforce Disclosure Initiative survey illustrates the variety of health and well-being programmes implemented by 114 worldwide large‑size companies. These companies represent 11 sectors of the industry (communication services, customer discretionary, consumer staples, energy, financials, industrials, information, technology, materials, real estate, utilities), and cover 19 countries (Australia, Belgium, Canada, China, Denmark, Finland, France, Germany, Italy, Japan, Mexico, Netherlands, Norway, South Africa, Spain, Sweden, Switzerland, the United Kingdom, and the United States), with a large number of companies (55 out of 141) being established in the United Kingdom. More than two‑thirds (68%) of participating companies reported offering stress and mental health programmes, although the data does not report on the actual uptake by employees (Figure 1.5). About 80% of the surveyed companies reported adopting actions that widen health-related choices of individuals, for instance by offering healthier food options in the cafeteria, providing sit-stand desks, or offering addiction management programmes. Such workplace programmes have increased over time, across European countries. For instance, according to the European Survey of Enterprises on New and Emerging Risks, 32% of the respondent companies reported they implemented measures raising awareness of nutrition among employees in 2019, compared to 28% in 2014 (ESENER, 2019[51]). During the COVID‑19 crisis, employer ability to respond to employee needs was challenged (Box 1.1).
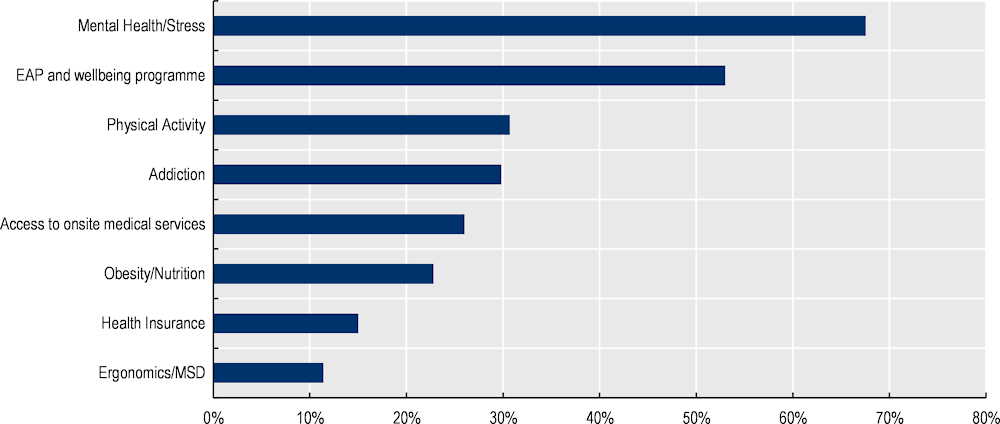
Note: MSD musculo-skeletal disorders. EAP Employee Assistance Programme are employee benefit programmes aiming to address a wide range of issues (e.g. mental and emotional well-being, financial). Well-being programmes include financial counselling, various leave options, additional services to accommodate particular needs. As companies may offer several answers, the sum is higher than 100%.
Source: OECD analysis based on 2020 WDI data.
During the COVID‑19 pandemics, companies had to adapt policies to protect their employees from the spread of the virus. According to the 2020 Workforce Disclosure Initiative data, from the very beginning of the COVID‑19 pandemic, many employers showed to effectively respond to employee needs offering health-related measures such as enabling teleworking, enhancing hygiene measures to limit the propagation of the coronavirus, and mental health support.
Long COVID‑19 represents an additional challenge for employers, as employees previously infected by the virus may suffer for long-standing illnesses -such as fatigue, breathlessness, chest pain or anxiety. A survey of 804 organisations in the United Kingdom, representing more than 4.3 million employees, found that 46% of organisations have employees who have experienced long COVID in the last 12 months, and that 26% of employers include long COVID among their main cause of long-term sickness absence (CIPD, 2022[52]).
In many circumstances, employers will see the promotion of health and well-being of their employees as a priority, but this is not always the case. Barriers, such as the cost of the programmes, insufficient human resources and lack of programme knowledge often hinder employers, in particular in SMEs, to implement health and well-being programmes for their employees. Governments can support employers to promote the health and well-being of their employees in the workplace through a mix of regulations, financial and non-financial incentives, as discussed in the next section.
The responsibility for promoting health and well-being at work lies in the domain of both health policy and labour market policy. As shown in Figure 1.6, labour and workplace legislation and health system characteristics set the foundation for the range of policy levers available to governments to promote health at work. The policy levers identified across the ten countries studied in detail (Australia, Canada, France, Germany, Italy, Japan, Korea, New Zealand, the United Kingdom, and the United States) include (i) regulation, (ii) financial incentives, (iii) dissemination of information, and (iv) certification and award schemes. Government efforts to promote health and well-being at work can be amplified by attracting investors and private funds that seek to align their investments with sustainability and societal values, to invest in companies that prioritise the health and well-being of their employees. Figure 1.6 also shows the range of stakeholders involved in health promotion at work, which in addition to governments and policy makers, includes occupational health professionals – who play a key role to diagnose risks and health problems in companies, identify needs and solutions – insurance institutions, employers, employees, trade unions and social partners. Collective bargaining, for instance, plays an important role in wage‑setting, job security and working time arrangement, all of which are issues that are closely related to health and well-being (OECD, 2019[53]).
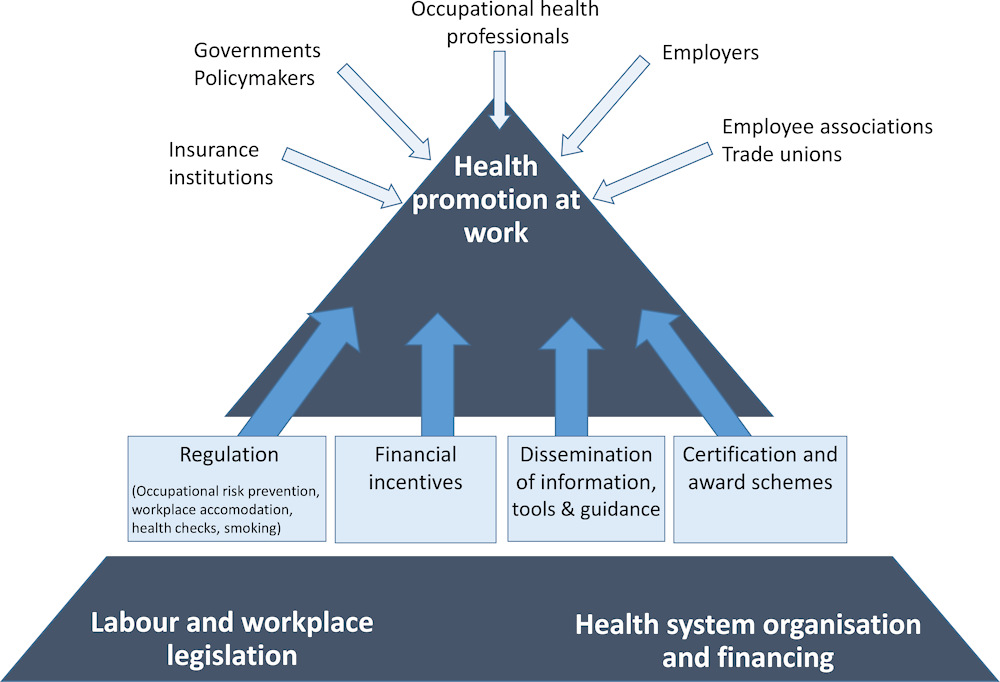
Source: Authors.
Standards and legislation relating to health and safety at work have existed for decades at the international, national and sub-national level (Department for Work and Pensions, 2021[54]). An example is the 1989 European Union Framework Directive on safety and health at work. In more recent years, new considerations for health promotion – adding to accident prevention and safety – have been included in national occupational health and safety strategies (such as in Germany) or within broader health promotion strategies (such as in Japan). One challenge that remains is in ensuring clarity on the responsibility of health promotion at work, as a lack of clarity can result in weak co‑ordination and a lack of attention placed on this issue (OECD, 2021[9]).
The institutional and financial arrangements of health promotion at the workplaces also result in significant heterogeneity across countries. For example, whereas in some countries such as Japan, occupational physicians are a hub through which workers access support including specialised treatment (OECD, 2019[55]), in others such as the United Kingdom, general practitioners play a more prominent role in referring individuals with health issues to access appropriate treatment (OECD, 2020[56]). In countries with a national health system (e.g. Australia, Canada, Italy, New Zealand and the United Kingdom), individuals are also entitled to health care based on residency and health care services is mostly financed by government schemes and thus employers tend to play a smaller role. By comparison, in countries where employers contribute to the cost of health insurance for employees (e.g. the United States), employers have a stronger incentive to promote the health and well-being of their employees.
Beyond legislation on the prevention of occupational risks and the promotion of health at work, regulations also exist on specific issues such as working hours, workplace health checks, smoking and alcohol consumption at the workplace, all of which are important areas to set a foundation for health promotion through work. The review based on ten countries identifies a range of regulations related to health at work, which management and enforcement may be under the responsibility of sub-national authorities in countries with decentralised governments. As shown in Figure 1.7, while most of the ten countries studied set maximum working hours and mandate employer-paid sick leave, other regulatory measures such as health check requirements and measures to control workplace alcohol consumption control are less common. While almost all countries restrict smoking in the workplace in some capacity, only three have a comprehensive ban that applies across the country.
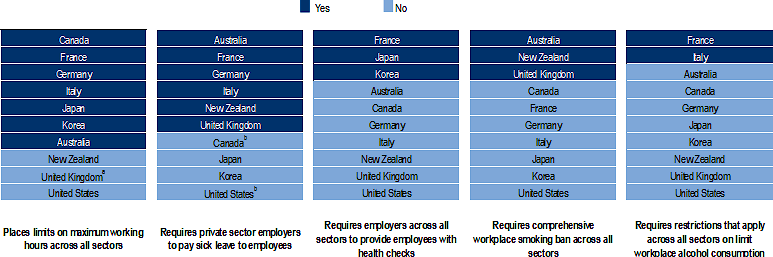
Note: a The United Kingdom has maximum hours but there is an option allowing employees to opt-out, which is typically included in contracts.
b Canada and the United States require private sector employers to pay sick leave to employees in a number of sub-national regions.
Source: Information presented on maximum working hour regulation is from the OECD Policy Questionnaire on Working Time Regulation, 2020, the findings of which are published in Employment Outlook, OECD (2021[8]). Information presented on sick leave is from Towards equitable and adequate paid sick leave, OECD (Forthcoming[57]). Information presented on smoking bans is from the Global Health Observatory, World Health Organization (2021[58]) complemented and updated with information from national sources. Information presented on health checks and alcohol consumption is based on a review of national sources by authors.
The review of regulation policies identified the following more detailed findings:
Regulating hours: six of the ten countries studied (Canada, France, Germany, Italy, Japan, and Korea) specify maximum weekly working hours (OECD, 2021[8]). When enforced and complemented with supporting measures, such regulation can protect employees from working excessively long hours.
Monitoring employee health: three of the ten countries (France, Japan and Korea) place requirements for employers to ensure their employees receive health checks or screenings across all sectors. This may reflect differences in the role of primary care and concerns over privacy and discrimination based on health or disability status (Box 1.2).
Prohibiting smoking: three countries have comprehensive smoking bans in enclosed workplaces (Australia, New Zealand, and the United Kingdom) (World Health Organization, 2021[58]), and four prohibit smoking in enclosed workplaces except in designated rooms (France, Italy, Japan and Korea). Comprehensive smoking bans are significantly more effective than partial bans at reducing exposure to second-hand smoke (Ward et al., 2013[59]).
Limiting alcohol consumption: no country prohibits alcohol consumption in the workplace across all sectors. Regulations prohibiting alcohol consumption exist primarily for jobs where influence of alcohol can increase injury risk (e.g. construction work) or where impairment due to alcohol can threaten public safety (e.g. bus driver).
Practices and rules about collection and disclosure of employee health data differ across jurisdictions due to varying approaches to data protection and privacy. For instance, in Japan, employers are authorised to collect data on employee health and well-being outcomes as this is a key aspect of the implementation of annual health checks. In the United States, employers are only permitted to ask employees to take health examinations and collect information on the findings if this need is directly related to the employee’s responsibilities or the duties of the employer. In the European Union, the General Data Protection Regulation (GDRP) recognises data concerning health as a special category of data. This places strict limitations on collection of information on employee health by employers, with specific limitations such as cases where collection of health data is necessary for carrying out contractual obligations (e.g. the provision of sick leave) or for public health and safety purposes (European Union, 2016[60]).
The issue of how to protect employee data privacy while also meeting public health objectives has received renewed attention during the COVID‑19 crisis. Information not collected previously such as previous and current coronavirus infection status, vaccination status for COVID‑19 and temperature checks, all became valuable for employers seeking to minimise infection risk among their on-site employees. For instance, employers in the United Kingdom have been able to ask employees about their COVID‑19 vaccination status on the condition that this is to protect the health and safety of other employees (Information Commissioner’s Office, 2022[61]). In Germany, meanwhile, employers were generally forbidden to ask employees about their vaccination status except in certain industries, but this was overruled by a later decision in March 2022, which allows for employers to request their employees to provide information on their 3G status (vaccinated (“geimpft”), recovered (“genesen”) or negative test result (“getested”)) as a public health measure (Federal Ministry of Health, 2022[62])
Regulation around sick leave, return-to-work and workplace accommodations play a particularly important role in health at the workplace, by supporting people experiencing ill-health or health conditions to remain in employment. While these measures are primarily changes in regulation, they can also create and be supported by financial incentives.
Paid sick leave: six countries provide employer-paid sick leave at the national level (varying from 3 days to 196 days) (OECD, Forthcoming[57]). Paid sick leave usually consists of a period of employer-paid sick leave combined with a period of government- or tax-funded paid sickness benefit. Employer-paid sick leave must be of sufficient duration to create sizeable incentives for employers to prevent sickness, absence from work, and promote timely return-to-work of employees (OECD, Forthcoming[57]).
Workplace accommodations: all ten countries require employers to make adjustments or accommodations for workers with disabilities (Department for Work and Pensions, 2021[54]). Eligibility should also be extended to also include workers with health conditions (OECD, Forthcoming[57]). Accommodation typically involves an increase in flexibility provided to employees rather than significant increases in expenditure (OECD, 2021[63]).
Gradual return-to-work mechanisms: only Germany and the United Kingdom provide mechanisms to facilitate employees who have been absent from work to initially return to work with reduced hours or lighter working duties, with a view to phased return to regular duties. Such mechanisms can help facilitate return-to-work while also promoting recovery from ill-health (OECD, 2021[9]). Most countries also require employers to take measures to facilitate return-to-work.
Financial incentives are important levers for governments to encourage and facilitate employers to go beyond basic accident prevention and safety, and to promote health and well-being through the workplace. Whereas regulation is usually suitable to set a minimum standard for employers to comply with, financial incentives can support employers looking to go beyond their legal responsibilities, by proactively promoting the health and well-being of their employees. Financial incentives and support are particularly important for micro, small and medium-sized enterprises. Three main types of financial incentives were identified, namely, insurance premium variation, tax credits, and subsidies and grants. As shown in Figure 1.8, accident insurance‑based incentives were identified in all the ten countries studied, while tax credits and subsidies and grants were identified in half or less of the ten countries.
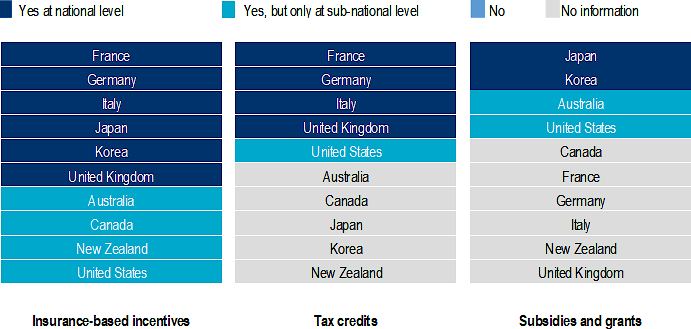
Note: No information indicates that no such measure could be identified in the review by the authors. Where financial incentives are implemented at the sub-national level, this figure does not differentiate between those cases where coverage is national (i.e. the entire country) and those where coverage only includes certain regions, territories and states.
Source: Information presented is based primarily on authors’ review of national sources. For European countries, authors drew first on Economic incentives to improve occupational safety and health: a review from the European perspective, European Agency for Safety and Health at Work (2010[64]), and updated information based on a review of national sources.
The review of financial incentives identified the following more detailed findings:
Insurance‑based incentives: all ten countries have accident insurance systems or workers’ compensation insurance boards, which reward companies that promote better health among their employees with lower insurance premiums. While such assessments are often limited to the past record of employers in preventing accidents and injuries, the responsibility of insurance institutions can extend further. In Italy, the National Institute for Insurance against Accidents at Work (INAIL) provides a reduction in the insurance premium for employers participating in a programme to promote health in the workplace through measures such as healthy diets, and subsidies for projects to promote health and safety in the workplace (2022[65]). Health insurance companies also play a notable role in France, Germany and Japan, where employers and employees together contribute to health insurance, and in the United States, where employers are required to provide health insurance coverage for employees.
Tax credits: four of the ten countries (France, Germany, Italy and the United Kingdom) provide tax credits at the national level related to health and well-being, and such credits are also available at the sub-national level in several states in the United States (Lankford, Kruger and Bauer, 2009[66]). Compared to subsidies, tax credits are often easier to implement administratively, as they can be included within existing mechanisms relating to tax reporting mechanisms. Tax credits specific to promoting active commuting to work also exist in France and the United Kingdom. In Germany, employers can receive a tax exemption for expenditures up to EUR 600 (USD 710) per employee per year to promote health at the workplace, with measures eligible including programmes to promote healthy diets, physical activity, stress management and addiction treatment (Federal Ministry of Health, 2022[67]).
Subsidies and grants: subsidies and grants were identified in two countries at the national level (Japan and Korea) and two other countries at the sub-national level (Australia and the United States). Subsidies are usually targeted at SMEs (Box 1.3), but also often only available to a very limited number of employers, especially if they are provided as competitive grants. In Japan, subsidies are available for SMEs implementing a Mental Health Promotion Plan and for those ensuring employees with health conditions can balance their work with accessing medical treatments and supports (Japan Organisation of Occupational Health and Safety, 2021[68]).
While about 409 million of workers are employed in SMEs in OECD countries, this potential target is less accessible because SMEs face more barriers when implementing health and well-being programmes for their employees than large companies. These barriers include, for instance, programme‑related cost, insufficient human resources, and lack of programme knowledge.
Government leadership can support SMEs in the process of implementing health programmes by investing in the training and employment of occupational health professionals to strengthen occupational health services, and developing national accreditation for providers of health and well-being services to frame the supply side (Saint-Martin, Inanc and Prinz, 2018[5]). Another avenue of actions is through better supply chain arrangements. If large businesses engage with their supply chain – both upstream and downstream – then occupational health and safety improvements can be fostered in SMEs (EU-OSHA, 2018[69]). Finally, governments can trigger SMEs to implement health and well-being programmes by offering subsidies to SMEs and by creating certified recognition programmes for employers who invest in health and well-being promotion for their employees (Section 1.8).
Governments can also facilitate employers in implementing workplace health and well-being programmes through dissemination of information on the benefits for employers to invest in health of their employees and through providing guidelines and other tools that can support the implementation of good practices by employers. This can increase awareness – especially for stigmatised health issues such as mental health (OECD, 2021[9]) – and increase the understanding among employers and managers of effective measures. While such initiatives are a low cost way for governments to increase awareness and facilitate employer action, the involvement of non-governmental stakeholders – including charities, trade unions and employer associations – helps ensure widespread outreach to employers and when developing health and well-being promotion tools and guidelines for them.
All ten countries studied provide information at the national level on health, safety and well-being in the workplace, typically through their agencies dedicated to occupational safety and health. Some countries also have dedicated agencies for researching and disseminating information on health in the workplace with an increasing focus on health promotion and early intervention. At the international level, the European Agency for Safety and Health at Work (EU-OSHA) plays a large role in both researching on the effectiveness of interventions to promote health at work and in disseminating this information to relevant stakeholders including employers.
Self-assessment tools, which allow employers to diagnose the extent to which they are effectively promoting health and well-being among employees, are available in at least four of the ten countries (France, Germany, the United Kingdom and the United States). In the United States, the Centre for Disease Control and Prevention (CDC) developed a Worksite Health ScoreCard, which allows employers to assess the extent to which they have implemented evidence‑based measures to promote the health and well-being of employees by filling out a questionnaire. The ScoreCard includes questions related to many areas, including weight management, physical activity, high blood pressure, tobacco use, musculoskeletal disorders, stress, sleep and maternal health (Centers for Disease Control and Prevention, 2022[70]).
Information and guidance on the COVID‑19 crisis has been widely disseminated to employers. Guidance covers issues relating to slowing the spread of the coronavirus such as ventilation, teleworking and sanitary measures, but also other impacts of the pandemic such as ensuring employee well-being, managing stress and supporting workers experiencing long COVID. In particular, in order to support workers experiencing long-lasting health impacts of COVID‑19 infections, guidance has been issued to employers in at least three countries (Japan, the United Kingdom, and the United States) as well as by EU-OSHA.
Governments can recognise employers that put in place best practices by providing them with certifications and awards, thus incentivising employers to promote health and well-being in the workplace. Some schemes are government-led, ranging from large‑scale national schemes such as the Health and Productivity Management (H&PM) programme in Japan to smaller schemes such as the Corporate Health Standard in Wales (United Kingdom). Non-governmental stakeholders, including private sector actors and non-profit organisations, have also developed such schemes.
The purpose of award and certification schemes is to create reputational benefits for employers promoting health and well-being in the workplace. There are at least three important criteria to ensure the credibility and usefulness of such schemes. Schemes must be: (1) sustainable and sufficiently long-lasting to develop a good reputation; (2) visible and disseminated to relevant stakeholders; and (3) be based on sound evidence that can effectively differentiate higher-performing employers implementing good practices compared to employers simply meeting legal obligations.
It is important to make a distinction between certification and award schemes. Whereas certification shows that an employer meets a certain standard of health and well-being promotion at work, award schemes are typically competition-style schemes, where recognition is only available to a limited number of employers. A limitation of certification and award schemes (and especially award schemes) is that they are exclusive, and usually only accessible to higher-performing employers, and may thus offer little incentive for health promotion in workplaces where it is not considered a priority. Some schemes such as the H&PM programme in Japan, combine aspects of both certification and award schemes. Launched in 2014 by the Ministry of Economy, Trade and Industry (METI), H&PM provides certification for employers meeting a minimum standard in promoting health and well-being at work, and the top 500 SMEs and top 500 large enterprises receive an additional award (2021[71]). Japan also has similar recognition schemes to promote physical activity and bicycle commuting.
Certification and award schemes go hand-in-hand with collection of more granular information on health and well-being in the workplace, which can be used to widen the evidence base to inform both policy and employer interventions. This is because certification and award schemes are typically based on information shared by employers on the health and well-being outcomes of employees and the specific measures and programmes they implement. The H&PM programme, for instance, provides a wealth of information relating to employer motivations and the relationship between health interventions at the workplace and health outcomes, given the scale of the programme. Even with smaller programmes such as the Workplace Well-being Awards, organised by Mind in the United Kingdom, there are opportunities to identify innovative practices that could be disseminated to employers seeking inspiration. The collection of employee health data nonetheless raise concerns about data protection and privacy in some countries (Box 1.2).
Institutional investors and private funds are seeking to direct investment towards companies that promote the health and well-being of their employees, in particular, investment that is aligned with ESG and human capital considerations (Box 1.4). According to an estimate by the Global Intangible Finance Tracker,1 intangible assets such as human capital, employee health and culture hold more than half (54%) of a company’s market value (Brand Finance, 2021[72]). Investors are also increasingly seeking to invest in companies that prioritise the health and well-being of their employees (BlackRock, 2022[73]), especially in the wake of the COVID‑19 pandemic, which has placed a spotlight on the importance of the health and well-being of employees.
ESG criteria are used by institutional investors and private funds as they seek to align their investments with sustainability and societal values. The environmental ‘E’ pillar encompasses the effect that companies’ activities have on the environment (directly or indirectly). The ‘E’ pillar is being increasingly used by investors who seek long-term value and alignment with the green transition (OECD, 2021[74]). The social ‘S’ pillar encompasses how a company manages relationships with employees, suppliers, customers, and the communities where it operates. It includes workforce‑related issues (such as health, diversity, training), as well as broader societal issues such as human rights. The governance ‘G’ pillar encompasses a company’s leadership, executive pay, audits, internal controls, transparency policies for public information, codes of conduct or shareholder rights.
Investors are increasingly considering ESG factors when evaluating companies. ESG investing is expected to represent one‑third of the global assets under management by 2025 (Bloomberg, 2021[75]), and as of 2020, over USD 30 trillion in assets incorporate ESG assessments (OECD, 2020[76]).
There are many ESG ratings providers, each using different data sources, methodologies and frameworks to establish ratings (Boffo and Patalano, 2020[77]). The growing demand for ESG investing is hampered by a lack of transparency, international inconsistencies and comparability challenges, and this is a risk that also exists for health and well-being indicators.
At least two motivations steer investors towards health-promoting companies. First, investors may consider companies that promote the health and well-being of its employees to be more valuable. While no causal relationship can be asserted, evidence from US studies shows that the stock values of companies awarded for their workplace health programmes outperformed the companies comprising the Standard and Poor’s 500 (S&P500) index, and the result holds across award schemes calculated through different approaches (Figure 1.9). Between 2001 and 2014, companies that were awarded for their workplace health programmes saw their combined stock value appreciate up to three times more than companies comprising the S&P500 index (Goetzel et al., 2016[78]; Grossmeier et al., 2016[79]; Fabius et al., 2016[80]). There is also promising evidence that suggests that in Japan, companies that have been certified in the H&PM programme also perform better on the Tokyo Stock Exchange (Ministry of Economy Trade and Industry of Japan, 2021[71]). While further examination and greater evidence is required to claim that workplace health promotion results in higher financial performance, this finding is consistent with the discussion in Section 1.2, which showed that poor health in the labour market results in a significant decrease in productivity among workers.
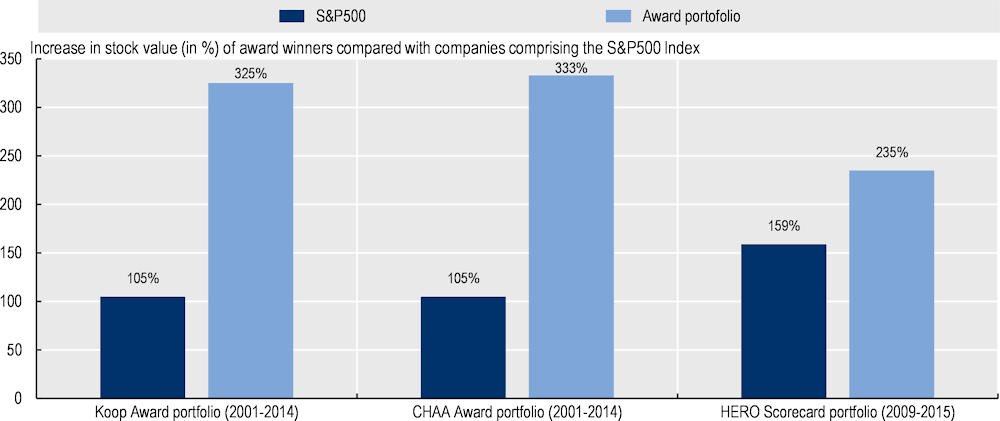
Note: S&P500 refer to companies comprising the Standard and Poor’s 500 Index, which includes the 500 largest companies listed on stock exchanges in the United States. CHAA Corporate Health Achievement Award. HERO Health Enhancement Research Organization. The period over which stock value increases are compared, is 2001‑14 for both the Koop Award and the CHAA Award, but is less than half the length (2009‑15) for the comparison of stock values for the HERO Scorecard. This may explain the smaller differential between the stock values of companies comprising the S&P 500 and HERO award-winners.
Source: Goetzel, R. et al. (2016[78]), “The Stock Performance of C. Everett Koop Award Winners Compared With the Standard & Poor’s 500 Index”, https://doi.org/10.1097/JOM.0000000000000632; Grossmeier, J. et al. (2016[79]), “Linking workplace health promotion best practices and organizational financial performance: Tracking market performance of companies with highest scores on the HERO Scorecard”, https://doi.org/10.1097/JOM.0000000000000631; Fabius, R. et al. (2016[80]), “Tracking the Market performance of companies that integrate a culture of health and safety: An assessment of corporate health achievement award applicants”, https://doi.org/10.1097/JOM.0000000000000638.
Second, information on company-led initiatives to promote health and well-being of the workforce is likely to be of interest for investors that look for sustainable, socially responsible investment. The health and well-being of employees, often incorporated within considerations around human capital, is increasingly seen as an important pillar of the non-financial performance of companies (Siegerink, Shinwell and Žarnic, 2022[81]). The importance of the health and well-being of employees beyond the immediate health impacts was put into further spotlight by the COVID‑19 pandemic, which began as a health crisis, but soon became a broader social, labour market and economic crisis.
As shown in Figure 1.10, as both investors and companies value the health and well-being of employees, this can create a virtuous cycle, where the incentive for employers to promote employee health is amplified. This is because an employer that promotes the health and well-being of employees is rewarded not only with a healthier workforce, but also with an increased likelihood of receiving investment. The key obstacle to this is that investors are unable to differentiate effectively between employers/companies that actively promote the health and well-being of its employees and those that do not. This is due to a general lack of information on the health and well-being of the workforce, and the absence of standardised disclosure and reporting mechanisms that either require or incentivise employers to provide information on their health and well-being programmes. Given the global nature of investment, it is important to standardise and harmonise practices across countries on disclosure mechanisms to allow for international comparison of company performance on health promotion.
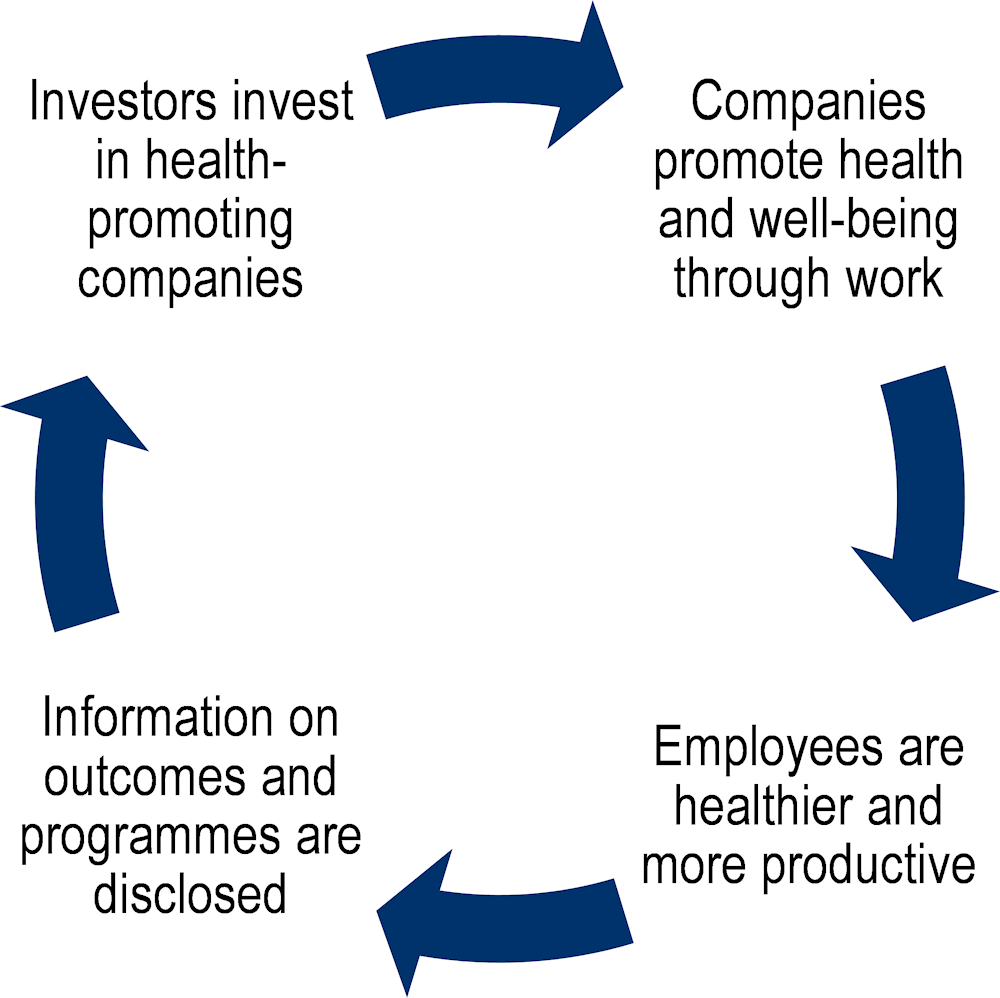
Source: Authors.
Governments can thus play an important role – working together with relevant stakeholders – to promote the disclosure and reporting of employers/companies efforts towards the health and well-being of employees. Besides providing impetus for other companies to learn and emulate good practices, this has the potential in turn, to steer investment towards employers/companies that promote the health and well-being of their employees.
While efforts to disclose data on health and well-being of the workforce remain scarce, there are initiatives emerging in some jurisdictions, which are classified into three categories. These are (1) government-led reforms for mandatory disclosure, (2) voluntary initiatives to promote disclosure often led by investors, and (3) efforts to standardise and harmonise disclosure mechanisms across countries and companies. Examples of initiatives from each category are described below.
Government-led reforms for mandatory disclosure: these are only just emerging such as in the United States or limited in scope such as in the European Union. In the United States, the Workforce Investment Disclosure Act – which was introduced in the Senate in 2021 – would require, if it were passed, publicly traded companies to disclose a range of human capital metrics, including workforce turnover rates, skills and development training, workforce engagement, pay and benefits, and workforce health and safety (United States Congress, 2021[82]). In the European Union, the Directive for Non-Financial Reporting requires large companies to disclose their measures to address social and environmental challenges, which includes issues related to employee health and well-being (European Union, 2013[83]).
Voluntary initiatives to promote disclosure: non-governmental stakeholders such as investors and charities often lead these initiatives, which exist across many of the ten countries studied. The Workforce Disclosure Initiative, which is led by a charity group and financially supported by the UK Government, has developed a reporting mechanism for companies to disclosure their approaches to human capital and workforce issues (ShareAction, 2022[84]). The Japanese Government also discloses information on measures implemented and health outcomes reported by companies that participate in the Health & Productivity Management Programme for companies that are listed in the Nikkei 225, which includes 80% of the largest publicly-owned companies in Japan (Ministry of Economy Trade and Industry of Japan, 2021[71]).
Initiatives to standardise and harmonise disclosure mechanisms: such initiatives, which are typically led by organisations with a standard-setting influence, can standardise the indicators that companies report on to allow for comparability across countries and companies. For instance, the Global Reporting Initiative, which sets standards used by 75% of the world’s largest companies in their ESG reporting (KPMG, 2020[85]), includes the implementation of health promotion programmes in its reporting guidelines on occupational health and safety, which was released in 2018 (Global Reporting Initiative Standards, 2018[86]).
Safety, health and well-being of employees are valuable to all stakeholders, including employees, employers, governments, investors and society-at-large. Integrating health and well-being promotion to the prevention of occupational safety and health risks contributes to greater results for the benefits of employee and employers. Workplaces are an ideal location to spread and implement health promotion and well-being activities in the working-age population, not least as populations across the OECD countries age and face an increasing burden of unhealthy lifestyles and chronic diseases. A range of policy levers is available to governments to incentivise employers to promote health and well-being among workers. These include regulation (such as regulation of working hours and smoking bans), financial incentives (such as insurance premium deductions, tax credits and subsidies to SMEs), dissemination of good practices to employers, and certification and award schemes to recognise employers that excel in health promotion. Regulation and dissemination of good practices are more widely used as policy levers across the ten countries than financial incentives and certification and award schemes among the ten countries studied. While the assessment presented in this report focussed on G7 and three OECD countries in the Asia and Pacific region, there are initiatives aimed at promoting health and well-being at the workplace in other OECD countries not reviewed here.
The rise of ESG criteria, which are increasingly used by investors to determine whether companies are sustainable and socially responsible, presents an opportunity to amplify government efforts to promote health and well-being in the workplace. Employee health and well-being should be of interest to both investors and employers as it is a key element of the ‘S’ social pillar of ESG and as a healthy workforce is the foundation for a successful company. The special focus chapter of this report therefore looks at how to steer investment in companies that promote employee health and well-being. A key issue that emerges from this is the need for mechanisms for disclosure of information on health and well-being that are of interest to investors. It also raises questions about what indicators should be disclosed and how to ensure investors are able to make comparisons between the performance of different companies.
[25] Airagnes, G. et al. (2019), “Alcohol, tobacco and cannabis use are associated with job loss at follow-up: Findings from the CONSTANCES cohort”, PloS one, Vol. 14/9, https://doi.org/10.1371/JOURNAL.PONE.0222361.
[43] Averett, S. (2019), “Obesity and labor market outcomes - The hidden private costs of obesity: lower earnings and a lower probability of employment”, IZA World of Labor, https://doi.org/10.15185/izawol.32.v2.
[48] Baicker, K., D. Cutler and Z. Song (2010), “Workplace Wellness Programs Can Generate Savings”, Health Affairs, Vol. 29/2, pp. 304-311, https://doi.org/10.1377/hlthaff.2009.0626.
[23] Baker, C. et al. (2017), “Benefits of quitting smoking on work productivity and activity impairment in the United States, the European Union and China”, International journal of clinical practice, Vol. 71/1, https://doi.org/10.1111/IJCP.12900.
[73] BlackRock (2022), Our approach to engagement on human capital management, BlackRock, https://www.blackrock.com/corporate/literature/publication/blk-commentary-engagement-on-human-capital.pdf (accessed on 4 April 2022).
[75] Bloomberg (2021), ESG assets may hit $53 trillion by 2025, a third of global AUM, https://www.bloomberg.com/professional/blog/esg-assets-may-hit-53-trillion-by-2025-a-third-of-global-aum/ (accessed on 14 April 2022).
[26] Böckerman, P., A. Hyytinen and T. Maczulskij (2017), “Alcohol Consumption and Long-Term Labor Market Outcomes”, Health Economics (United Kingdom), Vol. 26/3, pp. 275-291, https://doi.org/10.1002/HEC.3290.
[77] Boffo, R. and R. Patalano (2020), ESG Investing: Practices, Progress and Challenges, OECD, Paris.
[72] Brand Finance (2021), Global Intangible Finance Tracker 2021, https://brandirectory.com/download-report/brand-finance-gift-2021.pdf (accessed on 27 May 2022).
[30] Breton, M. et al. (2013), “Burden of Diabetes on the Ability to Work: A systematic review”, Diabetes Care, Vol. 36/3, p. 740, https://doi.org/10.2337/DC12-0354.
[36] Calvo-Bonacho, E. et al. (2014), “Influence of high cardiovascular risk in asymptomatic people on the duration and cost of sick leave: results of the ICARIA study”, European Heart Journal, Vol. 35/5, pp. 299-306, https://doi.org/10.1093/EURHEARTJ/EHT156.
[19] Campbell, D. et al. (2021), “Effects of increased body mass index on employment status: a Mendelian randomisation study”, International Journal of Obesity 2021 45:8, Vol. 45/8, pp. 1790-1801, https://doi.org/10.1038/s41366-021-00846-x.
[70] Centers for Disease Control and Prevention (2022), CDC Worksite Health ScoreCard, CDC Worksite Health ScoreCard, https://www.cdc.gov/workplacehealthpromotion/initiatives/healthscorecard/introduction.html (accessed on 1 April 2022).
[47] Chapman, L. (2012), “Meta-evaluation of worksite health promotion economic return studies: 2012 update”, American Journal of Health Promotion, Vol. 26/4, https://doi.org/10.4278/ajhp.26.4.tahp.
[52] CIPD (2022), Nearly half of employers have staff who have experienced long COVID in the last year, new research finds, https://www.cipd.co.uk/about/media/press/08022long-covid#gref (accessed on 19 April 2022).
[42] Dall, T. et al. (2013), “Modeling the indirect economic implications of musculoskeletal disorders and treatment”, Cost Effectiveness and Resource Allocation, Vol. 11/1, pp. 1-14, https://doi.org/10.1186/1478-7547-11-5/TABLES/5.
[54] Department for Work and Pensions (2021), “International Comparison of Occupational Health Systems and Provisions”, https://www.gov.uk/government/publications/international-comparison-of-occupational-health-systems-and-provisions (accessed on 11 January 2022).
[20] Destri, K. et al. (2021), “Impacts of Obesity On Absenteeism and Indirect Costs Among Working Adults: A Longitudinal Analysis From The EpiDoc Study”, https://doi.org/10.21203/RS.3.RS-882530/V1.
[28] Devaux, M. and F. Sassi (2015), “The Labour Market Impacts of Obesity, Smoking, Alcohol Use and Related Chronic Diseases”, OECD Health Working Papers, No. 86, OECD Publishing, Paris, https://doi.org/10.1787/5jrqcn5fpv0v-en.
[64] Elsler, D. (ed.) (2010), Economic incentives to improve occupational safety and health : a review from the European perspective, Publications Office of the European Union, https://data.europa.eu/doi/10.2802/21517.
[51] ESENER (2019), OSH Management / Measures for health promotion among employees, https://visualisation.osha.europa.eu/esener/en/survey/comparisons/2019/osh-management/en_1/company-size/E3Q157_1/EU27_2020/1 (accessed on 31 August 2022).
[69] EU-OSHA (2018), Safety and health in micro and small enterprises in the EU: Final report from the 3-year SESAME project, EU-OSHA, https://osha.europa.eu/en/publications/safety-and-health-micro-and-small-enterprises-eu-final-report-3-year-sesame-project (accessed on 5 September 2022).
[60] European Union (2016), “Regulation 2016/679 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC”, Official Journal of the European Union, Vol. 59, https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=OJ:L:2016:119:TOC (accessed on 6 April 2022).
[83] European Union (2013), “Directive 2013/34/EU of the European Parliament on the annual financial statements”, Official Journal of the European Union, Vol. 56, https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=uriserv%3AOJ.L_.2013.182.01.0019.01.ENG&toc=OJ%3AL%3A2013%3A182%3ATOC (accessed on 6 June 2022).
[13] Eurostat (2022), Database - Eurostat, https://ec.europa.eu/eurostat/data/database (accessed on 15 March 2022).
[14] Eurostat (2021), Self-reported work-related health problems and risk factors - key statistics - Statistics Explained, https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Self-reported_work-related_health_problems_and_risk_factors_-_key_statistics (accessed on 21 December 2021).
[80] Fabius, R. et al. (2016), “Tracking the Market performance of companies that integrate a culture of health and safety: An assessment of corporate health achievement award applicants”, Journal of Occupational and Environmental Medicine, Vol. 58/1, https://doi.org/10.1097/JOM.0000000000000638.
[62] Federal Ministry of Health (2022), FAQ: vaccination status query for employees, https://www.bundesgesundheitsministerium.de/coronavirus/faq-arbeitnehmerselbstaendige/faq-impfstatusabfrage.html (accessed on 7 June 2022).
[67] Federal Ministry of Health (2022), Workplace health promotion: tax benefits [Betriebliche Gesundheitsförderung: Steuerliche Vorteile], https://www.bundesgesundheitsministerium.de/themen/praevention/betriebliche-gesundheitsfoerderung/steuerliche-vorteile.html (accessed on 28 March 2022).
[11] Gallup Analytics (2021), World Poll Gallup data.
[86] Global Reporting Initiative Standards (2018), GRI 403: Occupational Health and Safety, https://www.globalreporting.org/standards/media/1910/gri-403-occupational-health-and-safety-2018.pdf (accessed on 8 June 2022).
[78] Goetzel, R. et al. (2016), “The Stock Performance of C. Everett Koop Award Winners Compared With the Standard & Poor’s 500 Index”, Journal of occupational and environmental medicine, Vol. 58/1, pp. 9-15, https://doi.org/10.1097/JOM.0000000000000632.
[37] Gordois, A. et al. (2016), “Productivity losses associated with cardiovascular disease: a systematic review”, Expert Review of Pharmacoeconomics and Outcomes Research, Vol. 16/6, pp. 759-769, https://doi.org/10.1080/14737167.2016.1259571.
[79] Grossmeier, J. et al. (2016), “Linking workplace health promotion best practices and organizational financial performance: Tracking market performance of companies with highest scores on the HERO Scorecard”, Journal of Occupational and Environmental Medicine, Vol. 58/1, https://doi.org/10.1097/JOM.0000000000000631.
[15] IHME (2020), GBD Compare | IHME Viz Hub, https://vizhub.healthdata.org/gbd-compare/ (accessed on 22 December 2021).
[61] Information Commissioner’s Office (2022), Data protection and Coronavirus-19 – relaxation of government measures, https://ico.org.uk/global/data-protection-and-coronavirus-19/ (accessed on 3 June 2022).
[7] Institute of Heath Equity and Public Health England (2015), Promoting good quality jobs to reduce health inequalities, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/460700/2a_Promoting_good_quality_jobs-Full.pdf (accessed on 18 May 2022).
[4] James, C., M. Devaux and F. Sassi (2017), “Inclusive growth and health”, OECD Health Working Papers, No. 103, OECD Publishing, Paris, https://doi.org/10.1787/93d52bcd-en.
[68] Japan Organisation of Occupational Health and Safety (2021), 2021 occupational safety and health grants [Reiwa 3-nendo-ban sangyō hoken kankei josei-kin], https://www.johas.go.jp/sangyouhoken/tabid/1944/Default.aspx (accessed on 28 March 2022).
[16] Johnson-Lawrence, V., A. Zajacova and R. Sneed (2017), “Education, race/ethnicity, and multimorbidity among adults aged 30–64 in the National Health Interview Survey”, SSM - Population Health, Vol. 3, p. 366, https://doi.org/10.1016/J.SSMPH.2017.03.007.
[21] Keramat, S. et al. (2020), “A longitudinal exploration of the relationship between obesity, and long term health condition with presenteeism in Australian workplaces, 2006-2018”, PLOS ONE, Vol. 15/8, p. e0238260, https://doi.org/10.1371/JOURNAL.PONE.0238260.
[35] Kouwenhoven-Pasmooij, T. et al. (2016), “Cardiovascular disease, diabetes and early exit from paid employment in Europe; the impact of work-related factors”, International Journal of Cardiology, Vol. 215, pp. 332-337, https://doi.org/10.1016/J.IJCARD.2016.04.090.
[85] KPMG (2020), The time has come - the KMPG Survey of Sustainability Reporting 2020, https://assets.kpmg/content/dam/kpmg/xx/pdf/2020/11/the-time-has-come.pdf (accessed on 8 June 2022).
[66] Lankford, T., J. Kruger and D. Bauer (2009), “State Legislation to Improve Employee Wellness”, The Science of Health Promotion, Vol. 23/4, pp. 283-289.
[40] Lubeck, D. (2003), “The costs of musculoskeletal disease: health needs assessment and health economics”, Best practice & research. Clinical rheumatology, Vol. 17/3, pp. 529-539, https://doi.org/10.1016/S1521-6942(03)00023-8.
[24] MacDonald, Z. and M. Shields (2004), “Does problem drinking affect employment? Evidence from England”, Health Economics, Vol. 13/2, pp. 139-155, https://doi.org/10.1002/hec.816.
[27] Magnus Thørrisen, M. et al. (2019), “Association between alcohol consumption and impaired work performance (presenteeism): a systematic review”, BMJ Open, Vol. 9, https://doi.org/10.1136/bmjopen-2019-029184.
[46] Mattke, S. et al. (2014), “Do Workplace Wellness Programs Save Employers Money?”, RAND Research Brief, https://doi.org/10.7249/RB9744.
[71] Ministry of Economy Trade and Industry of Japan (2021), Enhancing Health and Productivity Management Programme [Kenkō keiei no suishin ni tsuite].
[31] Mori, T. et al. (2020), “The Impact of Diabetes Status on Presenteeism in Japan”, Journal of occupational and environmental medicine, Vol. 62/8, pp. 654-661, https://doi.org/10.1097/JOM.0000000000001922.
[65] National Institute for Insurance against Accidents at Work - INAIL (2022), National Institute for Insurance against Accidents at Work [Oscillazione del tasso per prevenzione], https://www.inail.it/cs/internet/attivita/assicurazione/premio-assicurativo/oscillazione-del-tasso/oscillazione-del-tasso-per-prevenzione.html (accessed on 10 February 2022).
[41] Neovius, M., J. Simard and J. Askling (2011), “How large are the productivity losses in contemporary patients with RA, and how soon in relation to diagnosis do they develop?”, Annals of the Rheumatic Diseases, Vol. 70/6, pp. 1010-1015, https://doi.org/10.1136/ARD.2010.136812.
[44] OECD (2022), OECD Statistics, https://stats.oecd.org/ (accessed on 23 May 2022).
[63] OECD (2021), Disability, Work and Inclusion in Ireland: Engaging and Supporting Employers, OECD Publishing, Paris, https://doi.org/10.1787/74b45baa-en.
[74] OECD (ed.) (2021), ESG Investing and Climate Transition: Market Practices, Issues and Policy Considerations, https://www.oecd.org/finance/ESG-investing-and-climate-transition-market-practices-issues-and-policy-considerations.pdf (accessed on 4 April 2022).
[9] OECD (2021), Fitter Minds, Fitter Jobs: From Awareness to Change in Integrated Mental Health, Skills and Work Policies, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/a0815d0f-en.
[10] OECD (2021), Health at a Glance, OECD Publishing, Paris, https://doi.org/10.1787/19991312.
[8] OECD (2021), OECD Employment Outlook 2021: Navigating the COVID-19 Crisis and Recovery, OECD Publishing, Paris, https://doi.org/10.1787/5a700c4b-en.
[2] OECD (2021), Preventing Harmful Alcohol Use, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/6e4b4ffb-en.
[76] OECD (2020), OECD Business and Finance Outlook 2020: Sustainable and Resilient Finance, OECD Publishing, Paris, https://doi.org/10.1787/eb61fd29-en.
[3] OECD (2020), Promoting an Age-Inclusive Workforce: Living, Learning and Earning Longer, OECD Publishing, Paris, https://doi.org/10.1787/59752153-en.
[56] OECD (2020), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en.
[53] OECD (2019), Negotiating Our Way Up: Collective Bargaining in a Changing World of Work, OECD Publishing, Paris, https://doi.org/10.1787/1fd2da34-en.
[55] OECD (2019), OECD Reviews of Public Health: Japan: A Healthier Tomorrow, OECD Reviews of Public Health, OECD Publishing, Paris, https://doi.org/10.1787/9789264311602-en.
[1] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/67450d67-en.
[6] OECD (2018), Good Jobs for All in a Changing World of Work: The OECD Jobs Strategy, OECD Publishing, Paris, https://doi.org/10.1787/9789264308817-en.
[38] OECD (2012), Sick on the Job?: Myths and Realities about Mental Health and Work, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/9789264124523-en.
[57] OECD (Forthcoming), Towards equitable and adequate paid sick leave in Korea, OECD Publishing.
[22] Prochaska, J. et al. (2016), “Likelihood of Unemployed Smokers vs Nonsmokers Attaining Reemployment in a One-Year Observational Study”, JAMA internal medicine, Vol. 176/5, pp. 662-670, https://doi.org/10.1001/JAMAINTERNMED.2016.0772.
[17] Public Health Agency of Canada (2021), Canadian Chronic Disease Indicators (CCDI), https://health-infobase.canada.ca/ccdi/data-tool/?Dom=1 (accessed on 23 September 2022).
[50] Quigley, J. et al. (2022), Promoting workplace health and well-being through culture change. An evidence review, Health Research Board, Dublin, http://www.hrb.ie (accessed on 9 June 2022).
[12] Rajan, S. et al. (2021), In the wake of the pandemic Preparing for Long COVID, WHO, Copenhagen, https://apps.who.int/iris/bitstream/handle/10665/339629/Policy-brief-39-1997-8073-eng.pdf (accessed on 19 April 2022).
[18] Rasmussen, B., K. Sweeny and P. Sheehan (2016), HEALTH AND THE ECONOMY The Impact of Wellness on Workforce Productivity in Global Markets, U.S. Chamber of commerce, https://www.uschamber.com/assets/archived/images/documents/files/global_initiative_on_health_and_the_economy_-_report.pdf (accessed on 17 March 2022).
[29] Rodríguez-Sánchez, B. and D. Cantarero-Prieto (2017), “Performance of people with diabetes in the labor market: An empirical approach controlling for complications”, Economics & Human Biology, Vol. 27, pp. 102-113, https://doi.org/10.1016/j.ehb.2017.05.005.
[5] Saint-Martin, A., H. Inanc and C. Prinz (2018), “Job Quality, Health and Productivity : An evidence-based framework for analysis”, OECD Social, Employment and Migration Working Papers, OECD, Paris, https://www.oecd-ilibrary.org/social-issues-migration-health/job-quality-health-and-productivity_a8c84d91-en (accessed on 7 January 2022).
[84] ShareAction (2022), Workforce Disclosure Initiative, https://shareaction.org/investor-initiatives/workforce-disclosure-initiative (accessed on 23 May 2022).
[45] Sidossis, A. et al. (2021), “Healthy lifestyle interventions across diverse workplaces: a summary of the current evidence”, Current opinion in clinical nutrition and metabolic care, Vol. 24/6, pp. 490-503, https://doi.org/10.1097/MCO.0000000000000794.
[81] Siegerink, V., M. Shinwell and Ž. Žarnic (2022), “Measuring the non-financial performance of firms through the lens of the OECD Well-being Framework: A common measurement framework for “Scope 1” Social performance”, OECD Papers on Well-being and Inequalities, No. 03, OECD Publishing, Paris, https://doi.org/10.1787/28850c7f-en.
[33] Sjövall, K. et al. (2012), “Sickness absence among cancer patients in the pre-diagnostic and the post-diagnostic phases of five common forms of cancer”, Supportive Care in Cancer, Vol. 20/4, pp. 741-747, https://doi.org/10.1007/s00520-011-1142-8.
[34] Soejima, T. and K. Kamibeppu (2016), “Are cancer survivors well-performing workers? A systematic review”, Asia-Pacific Journal of Clinical Oncology, Vol. 12/4, pp. e383-e397, https://doi.org/10.1111/AJCO.12515.
[39] Summers, K., K. Jinnett and S. Bevan (2015), “Musculoskeletal Disorders, Workforce Health and Productivity in the United States”, http://www.theworkfoundation.com. (accessed on 17 December 2021).
[49] Tamers, S. et al. (2019), “Total Worker Health ® 2014-2018: The Novel Approach to Worker Safety, Health, and Well-Being Evolves”, Int J Environ Res Public Health, https://doi.org/10.3390/ijerph16030321.
[82] United States Congress (2021), S. 1815 - Workforce Investment 5 Disclosure Act of 2021, https://www.congress.gov/117/bills/s1815/BILLS-117s1815is.pdf (accessed on 6 June 2022).
[32] Vayr, F. et al. (2019), “Lung cancer survivors and employment: A systematic review”, Lung Cancer, Vol. 131, pp. 31-39, https://doi.org/10.1016/J.LUNGCAN.2019.03.010.
[59] Ward, M. et al. (2013), “The efficacy of different models of smoke-free laws in reducing exposure to second-hand smoke: A multi-country comparison”, Health Policy, Vol. 110/2-3, pp. 207-213, https://doi.org/10.1016/J.HEALTHPOL.2013.02.007.
[58] World Health Organization (2021), The Global Health Observatory: Smoke-free indoor offices, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/gho-tobacco-control-protect-smoke-free-public-places-indoor-offices (accessed on 11 January 2022).
← 1. The Global Intangible Finance Tracker report, produced by Brand Finance, ranks the world’s largest companies by intangible asset value. Intangible assets fall into three categories – rights (including leases, agreements, contracts), relationships (including a trained workforce), and intellectual property (including brands, patents, copyrights).