Marion Devaux
Alena Piatrova
Pedro Isaac Vazquez-Venegas
Marion Devaux
Alena Piatrova
Pedro Isaac Vazquez-Venegas
This chapter provides insight on why health and well-being programmes at the workplace are needed, lays out the motivations for employers to invest in programmes to promote healthy lifestyles among employees, and assesses the potential reach out of these programmes. Finally, based on 2020 survey data, it describes the type of health and well-being programmes implemented by employers.
Workplace‑actions are essential for ensuring employee health and safety and they are an ideal means to promote health and well-being given that adults spend a large portion of their lives at work.
Population ageing, spread of chronic conditions in the working-age population and the rise in health consciousness among employers and employees – in particular, after the COVID‑19 pandemic – are key drivers for the demand for workplace health and well-being programmes.
Workplaces can expand the outreach of health promotion interventions, beyond primary care services, communities and schools, in particular towards workers with health risks and low access to health care.
Motivations for employers to invest in health and well-being programmes for their employees are driven by several factors, including economic rationale, reputation motives, employee satisfaction, and external incentives.
Workplace health and well-being programmes can lower health care cost and productivity losses. Such programmes reduce medical treatment costs, showing positive cost benefit ratios. Studies with a follow-up period of one to seven years indicate that for each dollar invested in workplace health and well-being programmes, employers can save between USD 1.5 and USD 5.6 in health care spending.
Moreover, workplace programmes improving lifestyles, health and well-being, can reduce sick leave absenteeism by 25% and thus, increase work productivity. Scaling up interventions addressing sedentary behaviour and promoting physical activity at the workplace would increase work productivity by the equivalent of 37 000 full-time equivalent workers to the workforce per year in 30 OECD countries and would return USD 4 in the form of economic benefit for each dollar invested.
Companies that offer health and well-being programmes can improve their corporate image, improving attraction and retention of talent.
Employers that offer health and well-being programmes can increase employee satisfaction and motivation to perform work. Higher employees’ satisfaction and performance can improve services to customers, and in turn increase customer loyalty and revenues for the company.
Support programmes led by governments or health insurance companies can motivate employers to buy in health and well-being programmes.
Workplace‑based programmes that promote health and well-being among employees have a great potential coverage.
Across OECD, 610 million people are employed in the formal sector, representing a sizeable potential population target for workplace‑based interventions. About two‑thirds are employed in small and medium-sized enterprises (SMEs), while one‑third are in large size companies.
SMEs are less likely than large companies to offer health and well-being programmes, partly because of the programme‑related cost, insufficient human resources and lack of programme knowledge. However, a number of facilitators, especially directed at SMEs, can help the adoption of workplace health and well-being programmes, including strengthening occupational health services, developing national accreditation for health and well-being providers, integrating occupational health rules in the supply chains, creating certified recognition programmes for employers, and offering subsidies for SMEs.
Employee participation is key for maximising the effectiveness of workplace health and well-being programmes. The drivers for higher participation of employees are strong organisational programme support, low fees paid by the employee, and closer connections among employees.
Various types of workplace health and well-being programmes have been implemented, mostly by large companies, while their implementation raises some considerations.
Data from the 2020 Workforce Disclosure Initiative survey illustrates the variety of health and well-being programmes implemented by 114 worldwide large size companies.
More than two‑thirds of the companies (68%) reported they provided their employees with programmes addressing stress and mental health disorders. More than half (53%) offered an Employee Assistance Programme or a well-being programme, while less than one‑third offered programmes related to physical inactivity, addiction to tobacco and alcohol, obesity and nutrition, or ergonomics. The data does not report on the actual uptake by the employees, which makes it hard to assess the actual reach out of the programmes.
The success of workplace health-promoting programmes relies in part on organisational factors such as an integrated approach to occupational safety and health prevention and a healthy workplace culture.
The implementation of such programmes raises questions on actual uptake by the employees and on the effect of the programmes, which can be blurred by the heterogeneity in programmes and studies. A great number of studies support that workplace programmes can improve lifestyles and health outcomes in the short and medium-term, while evidence is less conclusive on their long-term effects.
80% of the WDI surveyed companies reported to adopt actions that widen an individual’s health related choices, for instance, by offering healthier food options in cafeteria, providing sit-stand desks, or offering addiction management programmes. Smaller proportions reported to provide health information, training, and financial incentives. As many programmes use new technology and digital tools, some concerns may be raised about data protection and privacy, and quality of health information.
During the COVID‑19 crisis, companies had to adapt to protect their employees from the spread of the virus, ensuring health and safety at work. COVID‑19 responses included enabling teleworking, enhancing hygiene measures to limit the propagation of the coronavirus, providing financial protection – such as salary guarantees – and by offering mental health support. In particular, 53% (19 out of 66) of the WDI surveyed companies reported to offer mental health programmes as a COVID‑19 response.
Workplace health and well-being programmes primarily aim to improve employee’s lifestyle behaviours at work, in order to avoid or postpone the occurrence of chronic diseases (e.g. such as mental health disorders, musculoskeletal disorders, obesity). These programmes need to be founded on a solid occupational safety and health management system, based on risk assessment. In particular, the European Agency for Safety and Health at Work (EU-OSHA) underlines that these programmes are only effective when occupational hazards are managed successfully (EU-OSHA, 2010[1]). The role of occupational health professionals is paramount to diagnose risks and health problems in companies, help better define the needs and respond by targeting adequate workplace health and well-being programmes. The involvement of employees and managers, in a participatory process, is also key for successful workplace programmes, and efforts to build a healthy workplace culture are essential to advance employee health and well-being (Box 3.1).
The WHO Healthy Workplace model combines health protection and health promotion approaches. The WHO Healthy Workplace model defines that workers and managers can together influence the health, safety and well-being of the workers and the sustainability of the workplace, by considering four dimensions: physical work environment, psychosocial work environment, personal resources, and enterprise community involvement (Joan Burton, 2010[2]). An important feature of this model is the participatory process that involves employees at all levels to determine needs and solutions. Within this framework, the culture of health and well-being in an organisation is a key element for building physical and psychosocial work environment. Recent evidence showed that health and well-being outcomes across a wide range of workplace interventions are mediated by workplace culture change, such as job control, organisation support, work climate, management style, flexibility, work time expectation, supervisor support, line manager’s attitude and actions (Quigley et al., 2022[3]). Such organisational changes are essential as they are the enabling conditions for a change.
This chapter offers an analysis of workplace health and well-being programmes (WHWP) that aim to promote employee health, healthy lifestyles and well-being, on top of an effective occupational health and safety management system (not discussed in this chapter). Section 3.2 examines the reasons why these programmes are needed. Section 3.3 lays out the motivations for employers to invest in programmes to promote healthy lifestyles among employees. Section 3.4 evaluates the potential reach out of these programmes. Finally, Section 3.5 describes the type of health and well-being programmes implemented by employers, using 2020 survey data.
With an ageing workforce, employers have a role to play to maintain good health and well-being of their employees. By 2050, more than four in ten individuals in the world’s most advanced economies are likely to be older than 50 (OECD, 2020[4]). Older workers are more likely to live with one or multiple chronic diseases (Chapter 2). Employers who prevent occupational risks and implement workplace health and well-being programmes can create healthy working environment, by offering employees the support they need to maintain good levels of physical health, mental health and well-being – for instance, by ensuring employees feel seen, heard, appreciated and that their work has meaning (OECD, 2020[4]). As adults spend a large portion of their lives in employment, workplace‑based actions are essential for ensuring health and safety at work and are increasingly considered as a potentially effective tool to influence choices favouring healthier lifestyles across the work-life continuum from the first job to retirement. For example, well-being-centred policies can achieve dietary improvements – through changes in the selection of daily menus and snacks provided in workplace cafeterias -, promote physical activity, reduce sedentary behaviour and sitting time through dedicated education, behavioural programmes and provision of sit-stand workstations, or tackle harmful alcohol consumption through services offered by schemes like Employee Assistance Programmes (EAP) (Box 3.2). Additionally, employers have started implementing workplace wellness programmes, which may provide various educational materials, classes, seminars, group activities, individual counselling sessions and incentives of different kinds to encourage participation (such as rewards and reimbursements).
EAPs have their origin in the United States at the beginning of the 20th century, with the first programmes to address alcoholism at work. From the 1970s, when the US Government created the National Institute on Alcoholism and Alcohol Abuse (NIAAA), there was an acceleration of the spread of the EAP concept throughout diverse workplace settings.
EAP is a voluntary, work-based programme that offers free and confidential assessments, short-term counselling, referrals, and follow-up services to employees who have personal and/or work-related problems. EAPs address a broad and complex body of issues affecting mental and emotional well-being, such as alcohol and other substance abuse, stress, psychological disorders, health care concerns, work relationship issues, financial or non-work related legal issues, and family problems.
EAPs are employee benefit programmes commonly proposed by companies in the United States and the United Kingdom, but are also available in over 150 countries.
Workplaces are complementary to primary care services, communities and schools for the purpose of health promotion reach out. People with lower income have lower access to health care specialists and lower uptake of preventive services compared to those with higher income (OECD, 2019[5]). Not only specific health policies can help address these inequalities, but also workplace‑based interventions can play a role to target people at risk. Workplaces provide a unique setting to reach out to individuals at potential health risk, including workers who do not often access health care services and those with low health literacy who often need the most support but receive the least (Saint-Martin, Inanc and Prinz, 2018[6]). A study based in an immigrant-dense community in Sweden found that screening diabetes at the workplace is more efficient than in the community and primary care settings (Shahim et al., 2018[7]). The cost of identifying one person with diabetes was 14 times lower in the workplace than in the primary health care centre (EUR 8 (USD 9.5) versus EUR 112 (USD 132) per case diagnosed, respectively). Workplace interventions, because they can reach out to individuals with lower access to health care and more health risks, can help to some extent break the link between health and socio-economic inequalities, at least for people who are in work. Evidence from a systematic review also supports that workplace health promotion programmes may contribute to reducing socio-economic inequalities in health behaviours. Precisely, the study identified six studies with 18 comparisons that provided quantitative information on workplace programme effects, of which 13 comparisons showed equal effectiveness across socio-economic groups, and 5 comparisons showed significantly higher effect sizes among workers in a low socio-economic position (Van De Ven, Robroek and Burdorf, 2020[8]). These findings only apply to people who are in work. Other types of intervention are necessary to address broader health inequalities, in particular targeted to unemployed people, who are more likely to be in worse health and die prematurely than those in more favourable socio-economic circumstances.
Interest in workplace health and well-being programmes (WHWP) is clearly growing. The history of the demand for WHWP varies by country, in particular due to national context and health system characteristics. For instance, in the United States, health coverage is largely employment-based. Employers substantially contribute to the cost of health insurance for their employees, and may use WHWP as a means for reducing medical costs. It is common that US companies offer programmes to promote health and well-being at work to their employees. In a nationally representative study of US worksites, almost half of worksites offered some type of health promotion or wellness programmes to employees (Linnan et al., 2019[9]). In the Nordic countries, well-established occupational health services and the importance of work-life balance contributed to make health promotion a natural component of workplace setting. In Japan, as the country does not have a traditional primary care and/or general practitioners as many other countries do, occupational doctors are the primary contact for employees – including employees with chronic disease‑ to access health care services. Despite these differences in national settings, countries face common challenges regarding ageing population and the spread of chronic conditions in the working-age population (Chapter 2). These challenges combined with the rise in health consciousness among employers and employees – possibly reinforced after the COVID‑19 pandemic – are key drivers for the growing demand for WHWP. In 2020, the global corporate wellness market1 was valued at USD 40.2 billion, and it is estimated to expand at a compound annual growth rate of 8.2% from 2021 to 2028 (Transparency Market Research, 2022[10]).
Employers who intend to implement health and well-being programmes can be motivated by a number of reasons. When interviewing US employers who did implement programmes, cost control over health care spending is the most cited objective, followed closely by other motives. A 2020 survey from the Integrated Benefits Institute questioned more than 300 Chief Finance Officers (CFOs) in the United States about the metrics they used to track whether their company’s health benefits strategy meets its goals. The most cited metric was health care spending (55% of the respondents). Besides costs, the focus was on employee participation (54%), employee satisfaction with benefits (49%), performance indicators -such as sickness absence, attraction and retention- (45%) and health status of employees (36%), while only 29% of respondents reported they tracked financial return on investment (IBI, 2020[11]). In countries where corporate health insurance plays a smaller role than in the United States, motivations for employers may be different. In Japan, the companies that signed up to the Health and Productivity Management (H&PM) governmental programme aim for strengthening management strategy, with the top-two objectives being to improve employee health and improve employee satisfaction and motivation, as indicated in a survey of 2 523 employers (Figure 3.1).
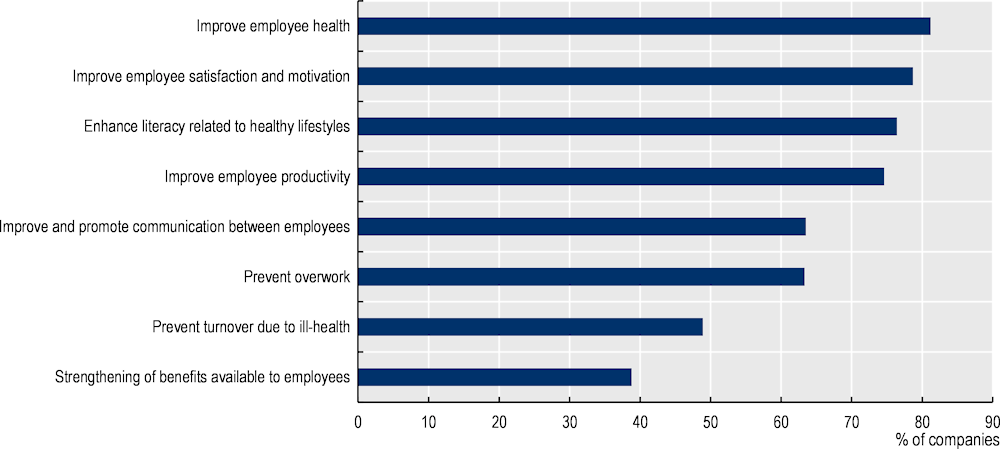
Note: Survey of 2 523 companies in Japan in 2020.
The remainder of this section presents the four main motivations for employers to implement and invest in WHWP, namely: i) employers can lower health care costs and productivity losses; ii) employers can improve their corporate image and their ability to attract and retain talent; iii) employers can increase employee satisfaction and motivation to perform work, and iv) external incentives from governments and health insurance companies can boost employer’s motivation.
WHWP reduce medical treatment costs, showing positive cost benefit ratios. Evidence, mostly from the United States, shows that the cost of wellness programmes paid by the employer is generally paid off by savings in medical spending. The amount of the returns varies across studies. For instance, a 2010 meta‑analysis found that for every dollar spent on workplace wellness programmes, medical costs fall by about USD 3.3 (Baicker, Cutler and Song, 2010[13]). Research by RAND Corporation found that workplace wellness programmes followed for seven years reduce the employer’s average health care costs by about USD 30 per member per month, equivalent to an economic return2 of USD 1.5 for every dollar invested (Mattke et al., 2014[14]). In a systematic review and meta‑analysis, the economic benefits3 are up to USD 5.6 for each dollar invested (Chapman, 2012[15]). The RAND study also showed that disease management programmes have a higher return on investment (USD 3.8 for 1) than lifestyle management programmes (USD 0.5 to 1) – the former are designed for employees who have a chronic disease, whereas the latter are designed for employees with health risks, such as smoking and obesity, to help them reduce those risks and prevent the occurrence of chronic diseases.
WHWP that manage to improve lifestyles, health and well-being, have the potential to reduce absenteeism and increase work productivity. Evidence suggests that workplace health promotion programmes can improve work ability and reduce sickness absences (Murphy et al., 2018[16]; Kuoppala, Lamminpää and Husman, 2008[17]; Rongen et al., 2013[18]). In particular, workplace‑based lifestyle management programme significantly reduces sickness absence by slightly more than one hour per employee‑year (Mattke et al., 2014[14]). A 2012 meta‑analysis based on 62 studies concluded that WHWP is associated with an average 25% reduction in sick leave absenteeism (Chapman, 2012[15]). Translated into monetary terms, for every dollar spent on workplace wellness programmes, the employer can save USD 2.7 in absenteeism costs (Baicker, Cutler and Song, 2010[13]). An OECD analysis showed that programmes addressing workplace sedentary behaviour by encouraging movement and reducing sitting time – such as making sit-stand workstations and treadmill desks available to employees – would improve employment and reduce absenteeism and presenteeism, by adding to the workforce the equivalent of 37 000 full-time equivalent (FTE) workers per year in 30 OECD countries (Figure 3.2). The cost of implementing workplace sedentary behaviour programmes is estimated between USD PPP 43 and USD PPP 144 per target person across the countries studies (equivalent to USD PPP 1 to 2 per capita). Taking into account the impacts on health and life expectancy, savings in health expenditure and labour market cost, this programme would return USD 4 in the form of economic benefit (i.e. Growth Domestic Product) for each dollar invested (OECD, 2019[19]).
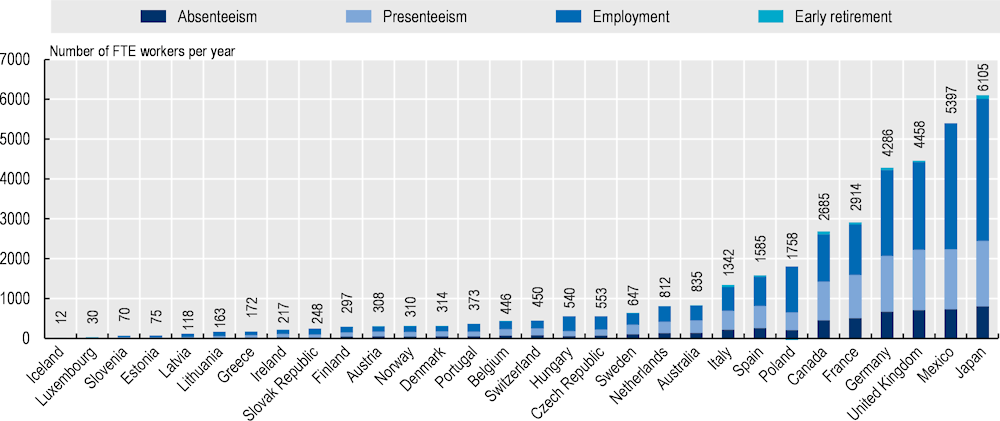
Note: Labour market inputs include employment and productivity when employed. They are expressed in the number of full-time equivalent workers and are calculated for the working-age population. OECD analyses based on the OECD SPHeP-NCDs model, which forecast the evolution of non-communicable diseases (NCDs) and risk factors and their related costs over the next 30 years.
Source: OECD (2019[19]), The Heavy Burden of Obesity, https://doi.org/10.1787/67450d67-en.
Companies implementing health and well-being programmes are generally favourably seen by potential and current employees, which helps improve their corporate image and their ability to attract and retain talent (EU-OSHA, 2012[20]; OECD, 2019[21]). Higher turnover rates are associated with high cost of replacement, including recruiting and training costs, but also with loss of productivity and loss of engagement from other employees. The cost of replacing an employee can range from 1.5 to 2 times the employee’s annual salary. In the United States, the cost of voluntary turnover is estimated at USD 1 trillion every year (Gallup, 2019[22]). Companies that are attractive enough to retain talent can avoid these increased costs.
Companies that provide upgraded health benefits to their employees can increase employee’s satisfaction and motivation to perform work. Improved employee job satisfaction and commitment to the organisation may improve employee service to customers and in turn, increase customer’s loyalty (EU-OSHA, 2012[20]). A meta‑analysis of more than 300 studies found a significant positive correlation between employee job satisfaction and employee productivity (correlation r = 0.2) and customer loyalty (r = 0.31), and a negative correlation with staff turnover (r = ‑0.25) (Krekel, Ward and De Neve, 2019[23]).
Support programmes led by governments or health insurance companies can also motivate employers to implement health and well-being programmes. A report from the European Agency for Health and Safety at Work (EU-OSHA) suggests that support programmes by national and local government (e.g. such as guidelines) encourage employers to implement workplace health programmes, especially for small and medium-sized enterprises (SMEs) which may have only limited resources and expertise to design and implement such types of programmes (EU-OSHA, 2012[20]). For instance, the United Kingdom and Canada have implemented a framework to assist employers to better assess musculoskeletal disorders (MSDs) risks at work, and provide guidelines for best practice interventions tailored for the assessed risks. Another example is Japan where the government provides incentives for employers to promote health and well-being at the workplace within the H&PM programme (Chapter 4). Government-led initiatives to support WHWP are further discussed in Chapter 4. In some countries, support from health insurance companies can be a practical lever for organisations and business to implement and invest in workplace health promotion activities. An example is the Vitality programme that originated from a private health insurer in South Africa, and then was rolled out across a range of enterprises worldwide, including Japan, the United Kingdom, the United States and China, and covers now more than 20 million people. Companies that subscribe to Vitality provide their employees with access to a health programme based on targets and rewards for healthy living (Box 3.3).
Discovery Health, a private health insurer, has developed and has been running one of the most well-known examples of a privately-managed health prevention programme. The Vitality programme was first rolled out in South Africa to be subsequently extended to other markets, including the United Kingdom, the United States and China (Lambert and Kolbe-Alexander, 2013[24]). Participation in the programme is voluntary and membership is offered for a nominal fee equivalent to about USD 20 per month. However, in some cases, the fee paid by the participant is significantly smaller. For example, in the United States, almost 90% of the membership fee for the Vitality programme is covered by the employers (Lambert and Kolbe-Alexander, 2013[24])
This incentive‑based programme rests on four pillars: assessment and screening, healthy choices, health knowledge and physical activity. Beneficiaries are encouraged to participate in different health-related activities such as health checks, exercising and healthy eating. Those who are sufficiently active are given bonus points, which can be exchanged for various rewards, such as upgrades in Vitality health status, free beverages or movie tickets, or discounts at various participating businesses. In addition, gym memberships are subsidised, and fruit and vegetable purchases are eligible for a cash rebate. It was found that the cash rebate has been effective in increasing expenditure on healthy foods by 9.3%, and decreasing spending on less healthy food by 7.2% (Sturm et al., 2013[25]). The Vitality programme combined with the Apple Watch leads to a 34% increase in physical activity level, corresponding to 4.8 extra days of physical activity per month (Vitality Group, n.d.[26]). The Vitality programme was also found to reduce medical care costs, which created an additional incentive for private insurers to invest in prevention. For example, compared to Vitality members not participating in the programme, participants have about 15% lower hospital-related costs for cancer, 21% lower hospital costs for endocrinal and metabolic syndrome, and 7% lower for cardiovascular diseases (Patel et al., 2010[27]).
Source: (OECD, 2019[19]), The Heavy Burden of Obesity, https://doi.org/10.1787/67450d67-en.
External support to employers can be paid off as promoting health and well-being at the workplace have wider economic benefits. Governments that take actions to incentivise employers to implement WHWP (as discussed in Chapter 4) can get economic returns. Beyond the profits for the employer, workers and the society-as-a-whole can also benefit from WHWP. These benefits are difficult to measure as they occur most likely in the long term (e.g. delayed chronic diseases and additional years lived in good health). The OECD SPHeP-NCDs framework aims to take into account the future benefits of public health interventions, at the population level. More precisely, a voluntary workplace wellness programme4 (that includes health risk assessment, classes, materials, group activities, counselling and environmental changes in the workplace) would save each year USD 260 million in health expenditure – broadly corresponding to the annual spending on preventive care in Lithuania or Slovenia – and would increase labour productivity by adding up to 38 000 workers to the workforce each year in 36 OECD, G20 and EU countries (due to increased employment and reduced absenteeism and presenteeism). Combining the effects on life expectancy, health expenditure, employment and productivity, workplace wellness programmes pay-off. The total return in GDP across the 36 countries is roughly equal to the total cost of implementing the policy in all countries (OECD, 2019[19]). Another example is alcohol brief intervention at the workplace, which aims to detect and advice employees with harmful alcohol use. Alcohol brief intervention would save each year USD 205 million in health expenditure – corresponding to the annual spending on preventive care in Lithuania or Slovenia-, and would add up to 49 000 workers to the workforce annually in 48 OECD, G20 and EU countries (OECD, 2021[28]).
In OECD countries, 610 million people are employed in the formal sector, making a sizeable potential target for workplace‑based interventions. In 2020, 66% of the working-age people were employed in OECD countries, with variations from 46% in Türkiye to 80% in Iceland (OECD, 2021[29]). At the OECD level, this represents 610 million employed persons in total. Employed persons could potentially benefit from a workplace‑based health and well-being programme, if the company offers such programmes.
Large companies5 are more likely than SMEs to offer health and well-being programmes. Business size was the most important predictor of whether a programme was offered according to evidence from Australia, Germany and the United States (Taylor et al., 2016[30]; Beck et al., 2015[31]; Mattke et al., 2014[32]). In particular, in the United States, 33% of the smallest firms (50‑100 employees) have a wellness programme, compared to 80% of the larger ones (over 1 000 employees); of those, 60% of the smallest employers and 90% of the larger employers used incentives, mostly monetary, to promote programme uptake. Several reasons explain why SMEs are less likely to take up health and well-being programmes than large companies; these include programme cost, insufficient knowledge about cost-effectiveness, immaturity of management organisation, insufficient human resources, delayed adoption of new technologies and equipment, lack of employee’s interest, and employee’s concerns about privacy. Nevertheless, when compared to larger firms, SMEs may be in a good position to successfully adopt WHWP. Their potential advantages include less bureaucracy, easier implementation, greater personal accountability of employees, and potential for team bonding (McCoy et al., 2014[33]). Across OECD, one‑third of workers – 201 million people – are employed in large companies, while two‑thirds – 409 million people – are employed in SMEs. This data varies by country, with 58% of the workers employed in large companies in the United States to less than 20% in Greece and Korea (Figure 3.3). As employees in large companies are more likely to be offered a WHWP, they represent a more reachable target for WHWP.
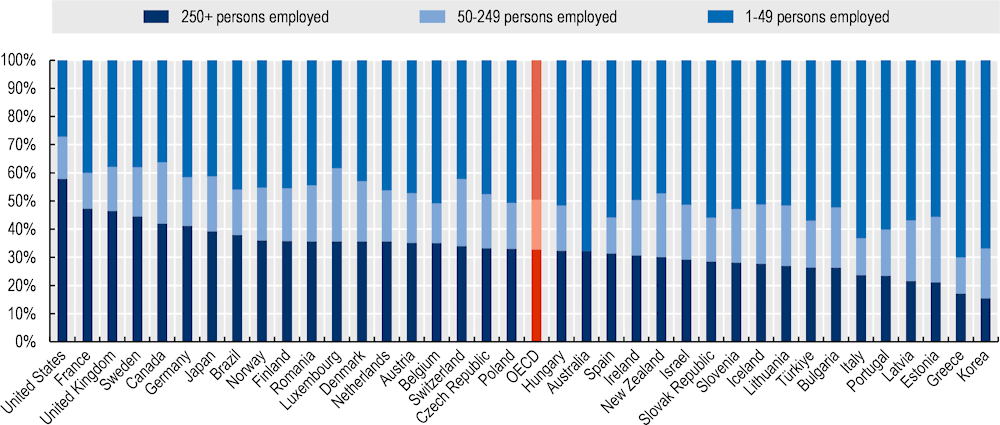
Note: The number of employees in Canada, Japan, and the United Kingdom includes all persons, workers and employees, covered by a contractual arrangement and working in the unit who receive compensation for their work, whether full-time or part-time.
Source: OECD Business Statistics by Employment Size Class, (2022[34]).
The potential of WHWP for SMEs is significant too. About 409 million workers are employed in SMEs in OECD countries. This potential target is, however, less accessible because SMEs face more barriers when implementing WHWP than large companies, due to programme‑related cost, insufficient human resources, and lack of programme knowledge. Government leadership can support SMEs in the process of implementing WHWP by strengthening occupational health services, developing national accreditation for health and well-being providers, involving the supply chains, and by creating certified recognition programmes for employers and offering subsidies to SMEs (further discussed in Chapter 4).
First, the accessibility and quality of occupational health services are strong determinants of employers’ motivation and ability to promote health at the workplace. This is especially important for SMEs that often lack financial and human resources to engage health specialists or advisors. Investing in the training and employment of occupational health specialists help protect and promote health, prevent work-related illness and promote return to work after illness.
Second, developing a nationally recognised system of quality standards and formal accreditation for providers of health and well-being services may facilitate user buy-in and foster the implementation of workplace programmes (Saint-Martin, Inanc and Prinz, 2018[6]).
Third, the supply chain can play an important role on occupational safety and health provision in micro and small businesses. If large businesses engage with their supply chain, both upstream and downstream, then occupational health and safety improvements can be fostered in SMEs. For instance, examples in the construction sector show that occupational safety and health rules can be integrated in the general planning of construction processes, involving small businesses in the supply chain (EU-OSHA, 2018[35]). Strengthened inspection and enforcement can help to step up the implication of the supply chains. European survey data show that compliance with legal obligations and fear of fines from the inspectorate are the most important drivers of action (EU-OSHA, 2019[36]).
Last, to overcome the affordability issue, governments can incentivise SMEs to implement WHWP through subsidies targeted at SMEs and by creating certified recognition programmes for employers, as discussed in Chapter 4. For instance, in Japan, where SMEs play a substantial role in the national economy and employ a large share of the workforce, the government has launched the H&PM certified recognition programme (Chapter 4). The number of SMEs applying for recognition programme has been significantly progressing. More precisely, the number of companies applying for the H&PM certificate has grown from 397 to 12 255 SMEs over the period 2016‑21 (Ministry of Economy Trade and Industry, 2022[37]).
Not only the size of the target population but also the participation rate of employees matter to make the full potential of WHWP. To maximise effectiveness, WHWP need a meaningful participation rate of employees. A German study of 61 companies found that employee participation in corporate wellness programmes varied between 0.07% to 100% across companies, with a mean participation at 15% (Lier, Breuer and Dallmeyer, 2019[38]). Several factors can explain such variations in participation rate, including company characteristics, type of programmes, and country setting. For instance, the German study identified strong programme support by the organisation,6 low employee co-payment and closer connections among employees (proxied by the size of the company) as drivers of employee participation. In SMEs, closer connections among employees build personal accountability and encourage participation in WHWP (McCoy et al., 2014[33]). The national legal and policy context is also a determining factor (Chapter 4). For instance, in Japan, employers are required to provide a core health check-up annually to full-time employees, and virtually all employees participate (OECD, 2019[21]).
WHWP vary by worksites (sector of industry, work environment and culture), by design (type of intervention, follow up) and by target (health behaviour). This section presents a range of WHWP, highlighting good practices and challenges, including programmes that address occupational risk factors (e.g. psychosocial risks) (3.5.1) and programmes that aim to adopt healthier behaviours (3.5.2). Finally, it highlights the variety of levers used in workplace programmes to drive employee behavioural change (3.5.3).
Work environments can expose employees to potential risks for health. As highlighted in Chapter 2, work-related diseases and injuries accounted for 1.9 million deaths worldwide in 2016, of which occupational injuries represent 360 000 deaths (WHO and ILO, 2021[39]). A strong occupational safety and health management system is paramount to prevent and manage occupational diseases and injuries. On top of this, dedicated health promotion actions can address occupational risk factors, such as for mental health disorders and MSDs. Early intervention to prevent occupational psychosocial risks (e.g. work‑related stress, long working hours), de‑stigmatisation around mental health issues, integrated delivery of health and employment services, return to work programmes to rehabilitate workers who were out of work because of a disease, are different avenues to prevent and treat mental health disorders. The Bell Let’s Talk programme in Canada is a good example of how employers can help raise awareness and tackle stigma about mental health issues (Box 3.4). Programmes for MSDs prevention can take the form of ergonomics, work breaks and/or physical exercises, and they mostly vary by sector of industry, work environment and by work culture. Such variety in MSDs interventions makes it difficult to draw solid conclusions on their effectiveness from systematic assessments (Hoe et al., 2018[40]).
Bell Canada or Bell is a Canadian telecommunications company, with more than 52 000 team members. In 2010, Bell Canada launched the ‘Bell Let’s Talk’ mental health programme to encourage discussion and increase awareness and acceptance of mental health issues. It is today the largest-ever corporate initiative supporting Canadian mental health. The programme was created around four strategies to promote mental health awareness: fighting mental health stigma, improving access to care, supporting research, and leading example of mental health in the workplace. The initiative includes a mandatory leader training, an employee and family assistance programme, psychological care benefits, employee awareness and educational initiatives, and a return-to-work programme. Bell monitors the effectiveness of the programme, tracking over 90 key performance indicator, such as short-term disability, long-term disability, usage of benefits and programmes supporting mental health, and employee engagement.
Since the start of the ‘Bell Let’s Talk’ programme in 2010, Bell has seen a positive return on investment. In 2018, for every dollar (USD 1) invested in workplace mental health programmes, USD 4.10 were returned in benefits. Bell measured a 190% increase in the usage of benefits and programme compared to the level of 2010. Data also show a 50% reduction in mental health-related short-term disability relapse and reoccurrence, and a 20% reduction in short-term disability claims in 2018 compared to the 2010 baseline (Deloitte Insights, 2019[41]).
Most employers take actions to reduce psychosocial risks at work, while MSDs risk prevention is less often cited. The 2020 Workforce Disclosure Initiative (WDI) data shows that all the 114 companies reported providing at least one health and well-being programme to their employees (ShareAction, 2022[42]) (Box 3.5). Nearly seven out of ten companies (68%) offer a mental health or stress programme to their employees (Figure 3.5). More than half (53%) offer EAP or well-being programme.7 Other programmes proposed to employees focussed on physical inactivity (31%), addiction to tobacco and alcohol (30%), access to onsite medical services (26%), obesity and nutrition (23%), health insurance coverage (15%) and ergonomics and MSDs (11%).
The WDI aims to improve corporate transparency and accountability on workforce issues, provide companies and investors with comprehensive and comparable data and help increase the provision of good jobs worldwide. ShareAction, a not-for-profit organisation, carries out the WDI survey annually since 2017.
In 2020, 141 global (worldwide) companies took part in the WDI survey – a 20 percent increase on 2019. These companies represent 11 sectors of the industry (communication services, customer discretionary, consumer staples, energy, financials, industrials, information, technology, materials, real estate, utilities) (Figure 3.4). The survey covers 19 countries (Australia, Belgium, Canada, China, Denmark, Finland, France, Germany, Italy, Japan, Mexico, Netherlands, Norway, South Africa, Spain, Sweden, Switzerland, the United Kingdom, and the United States), with a large number of companies (55 out of 141) being established in the United Kingdom. The analysis presented in this report is based on the data of 114 companies for which data was complete.
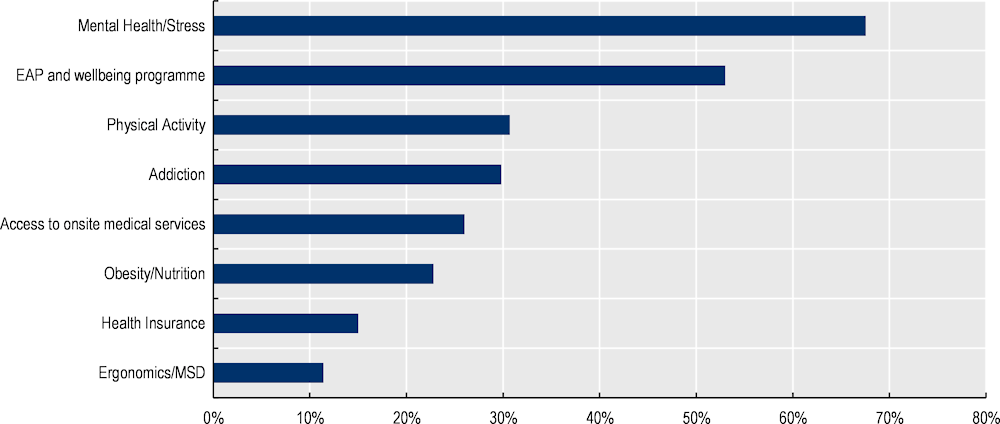
Note: MSD musculo-skeletal disorders. EAP Employee Assistance Programme. Well-being programmes include financial counselling, various leave options, additional services to accommodate particular needs. As companies may offer several answers, the sum is higher than 100%.
Source: OECD analysis based on 2020 WDI data.
A limitation with data reported by employers is that it cannot capture employee perspectives on health and safety at work, including on uptake and the appropriateness and adequacy of measures taken. Evidence shows that there can be significant disconnects and misalignment between employer and employee perspectives, which suggest that provision of health support by employers is not matching the expectations of employees in many cases. A survey of human resources (HR) leaders and employees in Australia, Canada, the United Kingdom and the United States found that, while almost half (47%) of HR leaders said they strongly agreed that their company supported employee well-being, less than a quarter (24%) of employees said that they strongly agreed that their company supported employee well-being (Achievers Workforce Institute, 2022[43]). This employee‑employer gap also exists in mental health, despite this being an area where employers report implementing many measures to support employees as shown in Figure 3.5. Comparing surveys of employers and employees in the United States by McKinsey & Company, whereas 65% of employers reported that employee mental health was supported either “well” or “very well”, only 51% of employees held the same view (McKinsey & Company, 2021[44]). A similar trend can be seen from the Achievers Workforce Institute survey, which found that 40% of HR leaders said that their company offered employees with resources to support mental well-being, whereas only 18% of employees reported that they felt supported at work in managing mental well-being (Achievers Workforce Institute, 2022[43]).
Further to ensuring health and safety at work, employer responsiveness to employee’s needs was challenged during the COVID‑19 crisis. Companies had to adapt to protect their employees from the spread of the virus. From the very beginning of the COVID‑19 pandemic, many employers showed to effectively respond to employee needs offering both health-related measures and financial support (Box 3.6). Long COVID‑19 represents an additional challenge for employers, as employees previously infected by the virus may suffer for long-standing illnesses. A survey of 804 organisations in the United Kingdom, representing more than 4.3 million employees, found that 46% of organisations have employees who have experienced long COVID in the last 12 months, and that 26% of employers include long COVID among their main cause of long-term sickness absence (CIPD, 2022[45]).
During the COVID‑19 crisis, companies had to adapt to protect their employees from the spread of the virus, ensuring health and safety at work. The WDI data contains an ad-hoc questionnaire related to COVID‑19 measures implemented in the early phase of the pandemic in 2020. Sixty-six out of the 141 surveyed companies provided answer to the COVID‑19 related questions.
Mental health programmes were the most often cited measures across all sectors (35 out of 66 companies, 53%), with four specific sectors being largely represented: financials (23%), consumer discretionary (20%), industrials and utilities (both at 11%). Enabling teleworking conditions in order to reduce the presence of workers onsite and limit propagation of the virus was cited by 36% of companies, especially from four sectors: communication services, consumer discretionary (non-essential and luxury goods and services), information technologies and finally utilities. Enhanced hygiene measures and social distancing were explicitly mentioned by 29%, mostly cited by the utilities sector (basic amenities such as water, electricity and sewage). About 21% of companies cited COVID‑19 medical upkeep such as company-paid tests and vaccination. Finally, temporary closures of facilities due to government imposed sanitary measures for non-essential businesses were reported by 6% of the companies, mostly by consumer discretionary company (representing 50% of those who responded).
In addition to health-related measures, company’s responses to COVID‑19 largely rely on financial protection of employees, which indirectly had protective effects on their mental health and well-being. Wealth, income and work are key dimensions of people’s well-being (OECD, 2020[46]). For instance, in the 2020 WDI data, 56% of companies introduced an extended paid sick leave as a response to COVID‑19, in order to assure that employees feel allowed to not going to work either because they are ill themselves or because they need to take care of others. Furthermore, 54% of companies provided some form of financial safety net to protect employees from financial hardship. These measures consist of emergency employee funds, salary guarantees, burial funds, and cash transfers to employees that were in positions of precarity due to the COVID‑19 pandemic and qualified for the allocation of relief funds.
Workplace‑based programmes can focus on various behavioural risk factors, such as smoking, harmful alcohol use, physical inactivity, poor diet, or a combination of these. As highlighted in the 2020 WDI data, 31% of the 114 large company employers reported having implemented programmes to increase physical activity, 30% to combat addiction, and 23% to address obesity and nutrition. Across Europe, health promotion actions at the workplace have increased over time, according to the EU-OSHA’s European Survey of Enterprises on New and Emerging Risks (ESENER). For instance, 32% of the respondent companies reported they implemented measures raising awareness of nutrition among employees in 2019, compared to 28% in 2014 (ESENER, 2019[47]). A number of programmes led by public or private employers illustrate good practices of WHWP, such as the Healthy Lifestyle Incentive Programme in the Salt Lake County (Box 3.7) and the smoking cessation programme at General Electrics (Box 3.8). Additional examples of good practices on promoting healthy lifestyles are collected by the European network of workplace health promotion (ENWHP), a not-for-profit association, which aims to facilitate dissemination of good workplace health practices in Europe (ENWHP, 2022[48]).
The Healthy Lifestyle Incentive Programme (HLIP) is an occupational health intervention for all employees of the Salt Lake County in the state of Utah in the US. Its aim is to curb the increasing trends in rates of obesity, diabetes, heart disease and cancer, and their contingent costs. The programme includes free annual screenings, tailored feedback on screening results and incentives awarded within a token economy system that grants points to employees who engage in a set of health promoting activities (Neville, Merrill and Kumpfer, 2011[49]).
At the end of each programme year, points are exchanged by cash at the rate of USD 1 per 5 points with a typical cash award of between USD 75 and USD 250 per employee. If at the initial screening employees had cholesterol, blood pressure, proportion of body fat, and tobacco use under pre‑set thresholds, they were awarded points. If, during the year, participants attended a 10‑week weight loss or tobacco cessation class, had a mammogram or prostate exam, had follow-up for elevated cholesterol or blood pressure, and reported 20 days of exercise, they were awarded points as well.
For the period that goes from 2004 to 2008, the HLIP had a total cost of about USD 1.3 million. By assuming that participants would have generated the same average costs as non-participants if they had not taken part in the programme, the costs averted in medical and drug prescription claims were estimated to be about USD 4.8 million. Net savings generated by the programme were about USD 3.5 million, or USD 3.85 dollars saved per USD 1 spent in the implementation of the programme (Merrill et al., 2011[50]).
In 2008, a trial for a smoking cessation programme took place at General Electric Corporation. The trial intended to financially reward employees to help them quit. The trial was successful, and GE generalised the programme to its 152 000 US employees (Schilling, 2009[51]).
The financial incentives were structured as follows: USD 100 for completion of a smoking-cessation programme, USD 250 for cessation of smoking within 6 months after study enrolment, as confirmed by a biochemical test, and USD 400 for abstinence for an additional 6 months after the initial cessation, as confirmed by a biochemical test. Both the incentivised group and the control group enjoyed the same generous GE health benefits package, which covers tobacco cessation pharmaceuticals but does not pay for smoking cessation programs.
Results showed that after 12 months, the incentivised group had a smoking cessation rate three times higher than the control group (14.7% vs. 5.0%) (Volpp et al., 2009[52]). Evidence from the Netherlands also supports that financial incentives, in addition to training programmes (consisting of a 90‑min session of smoking cessation group training at the workplace per week for 7 weeks), are effective to help employees quit smoking (van den Brand et al., 2018[53]).
Organisational factors contribute to the success of workplace lifestyle‑promoting programmes, such as the development of a healthy workplace culture (discussed above in Box 3.1) and the integration of surrounding work-related exposure and hazards into the programme. The starting point for workplace programmes aiming to promote employee health, healthy lifestyles and well-being, relies on good prevention and management of occupational risks. Growing evidence shows that an integrated approach of health promotion to occupational safety and health has greater outcomes such as improved health behaviours, employee participation, reductions in injury illness and disability, reducing costs, and enhancing productivity (Tamers et al., 2019[54]). In the United States, the National Institute of Occupational Safety and Health (NIOSH) supports the Total Worker Health®8 approach that integrates protection from work-related safety and health hazards with promotion of injury and illness-prevention efforts to advance employee well-being. For instance, the Total Worker Health® smoking cessation programme recommends an integrated approach to addressing not only personal factors (e.g. access to tobacco cessation pharmaceuticals) but also work-related hazards, such as chemical exposure that may exacerbate respiratory conditions, lack of control over work and work schedules. Addressing occupational risk factors and ensuring the workplace is safe increase employee buy-in for health promotion efforts (NIOSH, 2015[55]).
Evidence from the literature suggests that employees who benefit from a workplace programme modify health behaviours, although the heterogeneity across studies makes it difficult to draw solid conclusions. The literature research identified a large number of studies looking at the effects of workplace health programmes on health behavioural changes. For instance, smoking cessation programmes, in particular those entailing financial incentives, are effective to help employees quit smoking and remain abstinent after 12 months (van den Brand et al., 2018[53]; Volpp et al., 2009[52]; Cahill, Hartmann-Boyce and Perera, 2015[56]). A systematic review and meta‑analysis, based on seven RCTs, showed that workplace interventions were effective in reducing alcohol consumption compared to usual care, although the quality of the studies was relatively low. Workplace interventions were effective in particular among the heavier drinkers with a reduction of 2.6 standards units of alcohol per week (Yuvaraj et al., 2019[57]). A two‑year multicomponent workplace programme which included actions to promote a healthy diet, including through information events and education awareness campaigns, was found to increase consumption of fruit and vegetables by 0.3 servings a day (Afshin et al., 2015[58]). A systematic review and meta‑analysis found that educational and behavioural strategies addressing sedentary behaviour significantly reduced sitting time by 16 min per eight-hour workday, environmental strategies by 73 min (which include the provision of sit-stand workstations and treadmill desks), and multi-component intervention by 89 min (Chu et al., 2016[59]). Similarly, evidence from a randomised controlled trial (RCT) found that workplace sedentary programmes based on organisational, educational and behavioural changes significantly reduced sitting time by 22 min per day, and up to 64 min when associated with a sit-stand desk (Edwardson et al., 2022[60]). While interventions to address sedentary behaviour are important for office‑based workers, those working in more physically demanding jobs need different strategies to ensure health-enhancing physical activity and sufficient recovery time between tasks. A workplace wellness programme, entailing health risk assessment for employees, group activities, individual counselling about healthy lifestyles, and provision of performance‑related bonuses or reimbursements to encourage participation, reduced Body Mass Index (BMI) after 12 months (Penalvo et al., 2017[61]). These findings are further supported in an umbrella review of the effectiveness and cost-effectiveness of workplace health promotion programmes (including single or combined lifestyle programmes), summarizing the conclusions of 60 meta‑analysis and systematic reviews. This review found strong evidence of a favourable effect of workplace well-being programmes on health behaviours (physical activity, smoking cessation), on health outcomes of weight and BMI, stress/distress, anxiety/depression, and mental well-being (Murphy et al., 2018[16]). But, studies that assess WHWP, differ by design (type of intervention, follow up), worksites, populations examined, target (health behaviour), and by outcome measures. While some studies assess the effect on employee participation, some other look at health behaviour changes (or intention to change), and others at absenteeism. Overall, the variety in the programmes and their assessment makes difficult to summarise the evidence in a systematic way (Wolfenden et al., 2018[62]).
While some evidence supports changes in health behaviours on the short- and medium-term (up to 12 months), evidence for the long-term is scarcer. There are a few studies that could follow WHWP for a long period of time, and further research is needed on longer follow-up periods (Sidossis et al., 2021[63]). For instance, the long-term participation in the Healthy Lifestyle Incentive Programme implemented in the Salt Lake County improved BMI, blood pressure and cholesterol 8 years after enrolment (Neville, Merrill and Kumpfer, 2011[49]). In general, questions remain on the long-term effectiveness and sustainability of such programmes. It is likely that participants may get used to the programme or even lose interest in it. The initial effect of the intervention then tends to level off after a certain period of time. Renewing the programme, boosting personal accountability and monitoring outcomes over time can help to avoid lassitude of participants, and foster participation on the long-term. Also, to maintain interest in the programme, the interventions can be further tailored to specific individuals based on their risk factors or attitudes, or by increasing health literacy among employees (OECD, 2019[21]).
WHWP can take various forms. A variety of levers can help to drive behavioural change towards healthy lifestyles. These were categorised into four main groups (Sassi and Hurst, 2008[64]). First, public health actions that widen an individual’s choices, for instance, by offering healthier food options in cafeteria, providing sit-stand desks, or offering addiction management programmes such as EAP. Second, actions that influence individual’s choices through persuasion, provision of information, or other suitable means (other than prices), like programmes that offer points and rewards to employees, such as the Healthy Lifestyle Incentive Programme in the Salt Lake County (Box 3.7). Third, actions that change the price of selected choice options, such as for instance financial incentives for smoking cessation (Box 3.8). Fourth, actions that restrict the choices by banning selected choice options, such as smoking bans (which is the responsibility of governments rather than the employer in many countries, as discussed in Chapter 4).
Widening individual’s choices is the type of intervention most frequently reported by the employers of the WDI survey, followed by information campaigns and education. As shown in Figure 3.6, in the 2020 WDI data, 80% of the companies reported to offer health and well-being programmes that widen individual’s choices, such as healthier food options at the workplace, addiction management, or EAP. Nearly two in five companies (38%) provide health information to their employees in the forms of pamphlets, awareness campaigns, and informative website and newsletters. About 18% provide education programmes through workshops, training, and seminars. Fourteen percent reported to provide health insurance coverage to its employees to support their access to medical care. About 8% offer financial incentives or rewards such as discount for gym membership or rewards for healthy behaviours (Figure 3.6).
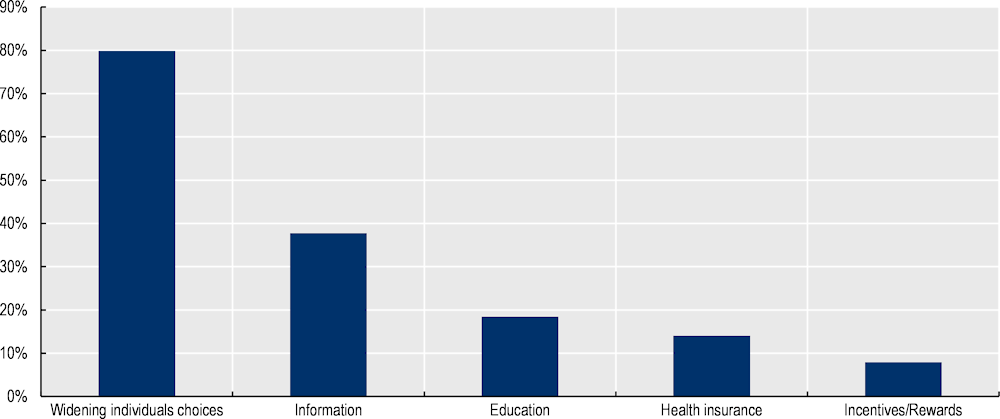
Note: As companies may offer several answers, the sum is higher than 100%.
Source: OECD analysis based on 2020 WDI data.
New technology and digital tools can simplify the delivery and management of WHWP. As of 2021, there are 6.4 billion smartphone users around the world (Statista, 2022[65]), corresponding to 80% of the global population owning a smartphone. Stakeholders involved in the design, implementation and evaluation of health programmes can benefit from this trend by adopting new digital tools to simplify and optimise the adoption of WHWP. For example, paper-based screening surveys can be easily moved to digital web-based supports, personalised information on health habits can be delivered by means of automatically generated messages, and incentive systems to reward healthy behaviours can be more readily and precisely managed by integrating them into digital environments. There are great opportunities for digital tools for health risk prevention and diseases management when promoted at the workplace, as illustrated in the Choose Well 365 programme implemented in a hospital workplace in the United States (Box 3.9). But a number of concerns have to be taken into consideration, for instance about data protection and privacy, and health regulation to avoid misleading health claims.
The Choose Well 365 randomised clinical trial was implemented at a hospital workplace in Massachusetts in the United States (Thorndike et al., 2021[66]). Its goal was to promote healthier dietary choices at the canteen by means of modifications of the choice environment, tailored feedback, and monetary incentives. The programme was run for a period of 12 months. The programme consisted in a food tag system in which items were labelled green if they were deemed “healthy”, yellow if considered “less healthy” and red if “least healthy”. Workers underwent an initial electronically-delivered screening that included indicators such as body-weight, fasting glucose and lipid-profile, and that asked the participants on their wish to maintain or lose weight.
Employees in the intervention group received automatically generated e‑mails twice a week. The first e‑mail contained information on the food purchase at the canteen during the prior week- proportion of food items purchased by tag colour, calories purchased and performance with reference to the calorie budget. The second e‑mail contained two personalised health tips on healthy eating, physical activity, or disease prevention, and a simple and healthy recipe.
A USD 20 incentive was awarded to employees the first time they passed the 40%, 60%, or 80% thresholds of monthly green purchase. If a participant maintained green purchases above a new threshold without passing the next threshold, or if they stay above 80% of green tag food purchases, they earned USD 5 for the month. Employees below the 40% threshold at baseline could earn the most money – USD 115 – during the intervention.
Results showed that, at 12 months, the intervention group, compared with baseline, had significantly decreased purchase of red- labelled items, decreased calories purchase per day by 49.5 kcal and significantly improved the proportion of green items purchased.
Population ageing, the spread of chronic conditions and the rise in health consciousness among employers and employees – in particular, after the COVID‑19 pandemic- are key drivers for the demand for workplace health and well-being programmes. There are multiple motivations for employers to invest in health and well-being programmes for their employees, including economic rationale, reputation motives, employee satisfaction, and external incentives. Workplace health and well-being programmes have a great potential in terms of population outreach and benefits for employers and employees. Regulation and incentives led by governments (discussed in the next chapter) are key levers for making the full potential of workplace health and well-being programmes.
[43] Achievers Workforce Institute (2022), Empowering Employee Wellbeing in the New World of Work, https://www.achievers.com/resources/white-papers/workforce-institute-employee-wellbeing/ (accessed on 17 May 2022).
[58] Afshin, A. et al. (2015), “CVD Prevention Through Policy: a Review of Mass Media, Food/Menu Labeling, Taxation/Subsidies, Built Environment, School Procurement, Worksite Wellness, and Marketing Standards to Improve Diet”, Current cardiology reports, Vol. 17/11, https://doi.org/10.1007/S11886-015-0658-9.
[13] Baicker, K., D. Cutler and Z. Song (2010), “Workplace Wellness Programs Can Generate Savings”, Health Affairs, Vol. 29/2, pp. 304-311, https://doi.org/10.1377/hlthaff.2009.0626.
[31] Beck, D. et al. (2015), “Patterns and predictors of workplace health promotion: cross-sectional findings from a company survey in Germany”, BMC Public Health 15, https://doi.org/10.1186/s12889-015-1647-z.
[56] Cahill, K., J. Hartmann-Boyce and R. Perera (2015), “Incentives for smoking cessation”, Cochrane Database of Systematic Reviews, Vol. 2015/5, https://doi.org/10.1002/14651858.CD004307.PUB5/MEDIA/CDSR/CD004307/REL0005/CD004307/IMAGE_N/NCD004307-CMP-003-05.PNG.
[15] Chapman, L. (2012), “Meta-evaluation of worksite health promotion economic return studies: 2012 update”, American Journal of Health Promotion, Vol. 26/4, https://doi.org/10.4278/ajhp.26.4.tahp.
[59] Chu, A. et al. (2016), “A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers”, Obesity Reviews, Vol. 17/5, pp. 467-481, https://doi.org/10.1111/obr.12388.
[45] CIPD (2022), Nearly half of employers have staff who have experienced long COVID in the last year, new research finds, https://www.cipd.co.uk/about/media/press/08022long-covid#gref (accessed on 19 April 2022).
[41] Deloitte Insights (2019), The ROI in workplace mental health programs: Good for people, good for business - A blueprint for workplace mental health programs, https://www2.deloitte.com/us/en/insights/topics/talent/workplace-mental-health-programs-worker-productivity.html (accessed on 8 April 2022).
[60] Edwardson, C. et al. (2022), “Effectiveness of an intervention for reducing sitting time and improving health in office workers: three arm cluster randomised controlled trial”, BMJ, Vol. 378, p. e069288, https://doi.org/10.1136/BMJ-2021-069288.
[48] ENWHP (2022), Models of good practice | ENWHP, https://www.enwhp.org/?i=portal.en.moveeu-models-of-good-practice (accessed on 6 September 2022).
[47] ESENER (2019), OSH Management / Measures for health promotion among employees, https://visualisation.osha.europa.eu/esener/en/survey/comparisons/2019/osh-management/en_1/company-size/E3Q157_1/EU27_2020/1 (accessed on 31 August 2022).
[36] EU-OSHA (2019), Third European Survey of Enterprises on New and Emerging Risks (ESENER 3), EU-OSHA, https://www.enshpo.eu/pdfs/news01.pdf (accessed on 5 September 2022).
[35] EU-OSHA (2018), Safety and health in micro and small enterprises in the EU: Final report from the 3-year SESAME project, EU-OSHA, https://osha.europa.eu/en/publications/safety-and-health-micro-and-small-enterprises-eu-final-report-3-year-sesame-project (accessed on 5 September 2022).
[20] EU-OSHA (2012), Motivation for employers to carry out workplace health promotion, EU-OSHA, https://osha.europa.eu/en/publications/motivation-employers-carry-out-workplace-health-promotion (accessed on 23 March 2022).
[1] EU-OSHA (2010), Workplace Health Promotion for Employers - Factsheet 93, Safety and health at work EU-OSHA, https://osha.europa.eu/en/publications/factsheet-93-workplace-health-promotion-employers (accessed on 30 August 2022).
[22] Gallup (2019), This Fixable Problem Costs U.S. Businesses $1 Trillion, https://www.gallup.com/workplace/247391/fixable-problem-costs-businesses-trillion.aspx (accessed on 23 March 2022).
[40] Hoe, V. et al. (2018), Ergonomic interventions for preventing work-related musculoskeletal disorders of the upper limb and neck among office workers, John Wiley and Sons Ltd, https://doi.org/10.1002/14651858.CD008570.pub3.
[11] IBI (2020), The Business Value of Health Benefits: Findings from IBI’s 2020 CFO survey, Integrated Benefits Institute, https://www.ibiweb.org/resource/2020-cfo-survey/ (accessed on 23 March 2022).
[2] Joan Burton (2010), WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices, WHO, Geneva, https://www.who.int/occupational_health/healthy_workplace_framework.pdf (accessed on 7 March 2022).
[23] Krekel, C., G. Ward and J. De Neve (2019), Employee Wellbeing, Productivity and Firm Performance, Centre for Economic Performance, London, https://cep.lse.ac.uk/pubs/download/dp1605.pdf (accessed on 24 March 2022).
[17] Kuoppala, J., A. Lamminpää and P. Husman (2008), “Work health promotion, job well-being, and sickness absences - A systematic review and meta-analysis”, Journal of Occupational and Environmental Medicine, Vol. 50/11, https://doi.org/10.1097/JOM.0b013e31818dbf92.
[24] Lambert, E. and T. Kolbe-Alexander (2013), “Innovative strategies targeting obesity and non-communicable diseases in South Africa: What can we learn from the private healthcare sector?”, Obesity Reviews, https://doi.org/10.1111/obr.12094.
[38] Lier, L., C. Breuer and S. Dallmeyer (2019), “Organizational-level determinants of participation in workplace health promotion programs: A cross-company study”, BMC Public Health, Vol. 19/1, https://doi.org/10.1186/s12889-019-6578-7.
[9] Linnan, L. et al. (2019), “Results of the Workplace Health in America Survey”, American journal of health promotion : AJHP, Vol. 33/5, p. 652, https://doi.org/10.1177/0890117119842047.
[32] Mattke, S. et al. (2014), Workplace Wellness Programs: Services Offered, Participation, and Incentives, https://www.rand.org/pubs/research_reports/RR724.html (accessed on 16 November 2021).
[14] Mattke, S. et al. (2014), “Do Workplace Wellness Programs Save Employers Money?”, RAND Research Brief, https://doi.org/10.7249/RB9744.
[33] McCoy, K. et al. (2014), “Health Promotion in Small Business: A Systematic Review of Factors Influencing Adoption and Effectiveness of Worksite Wellness Programs”, J Occup Environ Med, Vol. 56/6, pp. 579-587, https://doi.org/10.1097/JOM.0000000000000171.
[44] McKinsey & Company (2021), National surveys reveal disconnect between employees and employers around mental health need, https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/national-surveys-reveal-disconnect-between-employees-and-employers-around-mental-health-need (accessed on 17 May 2022).
[50] Merrill, R. et al. (2011), “Lowering employee health care costs through the Healthy Lifestyle Incentive Program”, Journal of public health management and practice : JPHMP, Vol. 17/3, pp. 225-232, https://doi.org/10.1097/PHH.0B013E3181F54128.
[37] Ministry of Economy Trade and Industry (2022), Announcement of Organizations Selected under the 2022 Certified Health & Productivity Management Outstanding Organizations Recognition Program, https://www.meti.go.jp/english/press/2022/0309_002.html (accessed on 15 June 2022).
[12] Ministry of Economy Trade and Industry (2021), Survey of 2523 companies that implement the Health and Productivity Management strategy, 2020, https://www.meti.go.jp/policy/mono_info_service/healthcare/kenko_keiei.html (accessed on 15 November 2022).
[16] Murphy, R. et al. (2018), An Umbrella Review of The Effectiveness and Cost-Effectiveness of Workplace Wellbeing Programmes, Department of Health, Ireland, https://assets.gov.ie/7975/3958857ca9a9403bb8ea90ef471a62d0.pdf (accessed on 24 March 2022).
[49] Neville, B., R. Merrill and K. Kumpfer (2011), “Longitudinal outcomes of a comprehensive, incentivized worksite wellness program”, Evaluation and the Health Professions, Vol. 34/1, https://doi.org/10.1177/0163278710379222.
[55] NIOSH (2015), Using Total Worker Health™ Concepts to Enhance Workplace Tobacco Prevention and Control, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, https://www.cdc.gov/niosh/docs/wp-solutions/2015-202/pdfs/2015-202.pdf?id=10.26616/NIOSHPUB2015202 (accessed on 26 September 2022).
[34] OECD (2022), OECD Statistics, https://stats.oecd.org/ (accessed on 23 May 2022).
[29] OECD (2021), OECD Employment Outlook, OECD Publishing, Paris, https://doi.org/10.1787/19991266.
[28] OECD (2021), Preventing Harmful Alcohol Use, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/6e4b4ffb-en.
[46] OECD (2020), How’s Life? 2020: Measuring Well-being, OECD Publishing, Paris, https://doi.org/10.1787/9870c393-en.
[4] OECD (2020), Promoting an Age-Inclusive Workforce: Living, Learning and Earning Longer, OECD Publishing, Paris, https://doi.org/10.1787/59752153-en.
[5] OECD (2019), Health for Everyone?: Social Inequalities in Health and Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/3c8385d0-en.
[21] OECD (2019), OECD Reviews of Public Health: Japan: A Healthier Tomorrow, OECD Reviews of Public Health, OECD Publishing, Paris, https://doi.org/10.1787/9789264311602-en.
[19] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/67450d67-en.
[27] Patel, D. et al. (2010), “The association between medical costs and participation in the vitality health promotion program among 948,974 members of a South African health insurance company”, American Journal of Health Promotion, https://doi.org/10.4278/090217-QUAN-68R2.1.
[61] Penalvo, J. et al. (2017), “Do Worksite Wellness Programs Improve Dietary Behaviors and Adiposity? A Systematic Review and Meta-analysis”, Circulation, https://www.ahajournals.org/doi/abs/10.1161/circ.135.suppl_1.mp005 (accessed on 26 September 2019).
[3] Quigley, J. et al. (2022), Promoting workplace health and well-being through culture change. An evidence review, Health Research Board, Dublin, http://www.hrb.ie (accessed on 9 June 2022).
[18] Rongen, A. et al. (2013), Workplace health promotion: A meta-analysis of effectiveness, https://doi.org/10.1016/j.amepre.2012.12.007.
[6] Saint-Martin, A., H. Inanc and C. Prinz (2018), “Job Quality, Health and Productivity: An evidence-based framework for analysis”, OECD Social, Employment and Migration Working Papers, No. 221, OECD Publishing, Paris, https://doi.org/10.1787/a8c84d91-en.
[64] Sassi, F. and J. Hurst (2008), “The prevention of lifestyle-related chronic diseases: an economic framework”, OECD Health Working Papers, Vol. 32, http://www.oecd.org/health/health-systems/40324263.pdf.
[51] Schilling, B. (2009), What Happened When GE Paid Employees to Quit Smoking? | Commonwealth Fund, The Commonwealth Fund Newsletter article, https://www.commonwealthfund.org/publications/newsletter-article/what-happened-when-ge-paid-employees-quit-smoking (accessed on 28 March 2022).
[7] Shahim, B. et al. (2018), “Effectiveness of different outreach strategies to identify individuals at high risk of diabetes in a heterogeneous population: a study in the Swedish municipality of Södertälje”, European journal of preventive cardiology, Vol. 25/18, pp. 1990-1999, https://doi.org/10.1177/2047487318805582.
[42] ShareAction (2022), Workforce Disclosure Initiative, https://shareaction.org/investor-initiatives/workforce-disclosure-initiative (accessed on 23 May 2022).
[63] Sidossis, A. et al. (2021), “Healthy lifestyle interventions across diverse workplaces: a summary of the current evidence”, Current opinion in clinical nutrition and metabolic care, Vol. 24/6, pp. 490-503, https://doi.org/10.1097/MCO.0000000000000794.
[65] Statista (2022), Number of smartphone subscriptions worldwide from 2016 to 2027, https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/ (accessed on 7 April 2022).
[25] Sturm, R. et al. (2013), “A cash-back rebate program for healthy food purchases in South Africa: Results from scanner data”, American Journal of Preventive Medicine, https://doi.org/10.1016/j.amepre.2013.02.011.
[54] Tamers, S. et al. (2019), “Total Worker Health ® 2014-2018: The Novel Approach to Worker Safety, Health, and Well-Being Evolves”, Int J Environ Res Public Health, https://doi.org/10.3390/ijerph16030321.
[30] Taylor, A. et al. (2016), “The role of business size in assessing the uptake of health promoting workplace initiatives in Australia”, BMC Public Health, Vol. 16/1, https://doi.org/10.1186/S12889-016-3011-3/TABLES/6.
[66] Thorndike, A. et al. (2021), “Automated Behavioral Workplace Intervention to Prevent Weight Gain and Improve Diet: The ChooseWell 365 Randomized Clinical Trial”, JAMA network open, Vol. 4/6, https://doi.org/10.1001/JAMANETWORKOPEN.2021.12528.
[10] Transparency Market Research (2022), Corporate Wellness Market Outlook 2028, https://www.transparencymarketresearch.com/corporate-wellness-market.html (accessed on 24 March 2022).
[8] Van De Ven, D., S. Robroek and A. Burdorf (2020), “Are workplace health promotion programmes effective for all socioeconomic groups? A systematic review”, Occupational and Environmental Medicine, Vol. 77/9, pp. 589-596, https://doi.org/10.1136/OEMED-2019-106311.
[53] van den Brand, F. et al. (2018), “Effect of a workplace-based group training programme combined with financial incentives on smoking cessation: a cluster-randomised controlled trial”, The Lancet. Public health, Vol. 3/11, pp. e536-e544, https://doi.org/10.1016/S2468-2667(18)30185-3.
[26] Vitality Group (n.d.), VitalityAppleStudy - Vitality, https://www.vitalitygroup.com/vitalityapplestudy/ (accessed on 31 March 2022).
[52] Volpp, K. et al. (2009), “A Randomized, Controlled Trial of Financial Incentives for Smoking Cessation”, NEJM, Vol. 360/7, pp. 699-709, https://doi.org/10.1056/NEJMSA0806819.
[39] WHO and ILO (2021), WHO/ILO joint estimates of the work-related burden of disease and injury, 2000-2016: global monitoring report, https://www.who.int/publications/i/item/9789240034945 (accessed on 21 December 2021).
[62] Wolfenden, L. et al. (2018), “Strategies to improve the implementation of workplace-based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity”, The Cochrane database of systematic reviews, Vol. 11/11, https://doi.org/10.1002/14651858.CD012439.PUB2.
[57] Yuvaraj, K. et al. (2019), “Effectiveness of Workplace Intervention for Reducing Alcohol Consumption: a Systematic Review and Meta-Analysis”, Alcohol and Alcoholism, Vol. 54/3, pp. 264-271, https://doi.org/10.1093/ALCALC/AGZ024.
← 1. Service types include health risk assessment, fitness, smoking cessation, health screening, weight management, nutrition, stress management, disease management, vaccination, etc.
← 2. Only for medical cost savings.
← 3. This calculation is based on 44 studies, with an observation period of a minimum of 12 months in duration. The savings were limited to a single economic variable (mostly medical cost savings), and were divided by the entire programme cost.
← 4. It is assumed that this intervention would reach its maximum effectiveness 12 months after implementation (body mass index reduction by up to 0.64kg/m2), and then completely disappear after 36 months.
← 5. As per the OECD definition, small-sized companies (1‑49 employees), medium size (50‑249 employees) and large sized companies (250+ employees).
← 6. Measured as the degree to which the company leadership team supports the corporate fitness programme and promotes its success.
← 7. Financial counselling, various leave options, additional services to accommodate particular needs.
← 8. Total Worker Health® is a registered trademark of the U.S. Department of Health and Human Services.