Twenty-first century health systems will be built around data and information. Data and their efficient exchange are fundamental to generating the information needed to improve and optimise health system performance. This chapter brings together the key findings of this review of how health data are managed and used in Korea and makes recommendations for creating an integrated national health information system. The chapter outlines what is meant by health data and an integrated health information system, and its role in advancing health care and it outlines the strengths and challenges of the Korean health information landscape. The review finds that Korea is well placed to build an integrated health information system that will support a high-performing health system and recommends central leadership and a national health information strategy including greater harmonisation of clinical and health data, an enabling legal and policy framework, building trust and fostering collaboration among key stakeholders, and developing a hub as a single entry point for secure data access.
Towards an Integrated Health Information System in Korea

1. Key findings and recommendations
Abstract
In June 2021, the Korean Ministry of Health and Welfare commissioned the OECD to gather evidence and review the management and use of health data in Korea, and to recommend changes that would enable creating a health data and information system to support achieving national health policy objectives, with a special focus on using health data to improve health system performance.
To understand the strengths and weaknesses of the current arrangements in Korea and to develop recommendations, the OECD, through a series of focus groups and interviews, consulted national experts from a range of stakeholder groups (See Annex A). The discussions focused on:
Health data interoperability (exchange and sharing): What are the challenges and what are the policy tools that can address them? i.e. regulations, incentives, standards, certification?
Organisation and governance: What national institutions and governance mechanisms support a strong and trustworthy national health information system?
The information gathered through these consultations was complemented with information on Korea and other OECD countries collected through the OECD’s regular monitoring of countries’ health information systems including:
1. Survey of National Health Data Development, Use and Governance (2019‑20)
2. Survey of Electronic Health Record System Development, Data Use and Governance (2021)
3. Survey of Changes to Health Data and Governance due to the COVID‑19 Pandemic (2021).
This final report and recommendations from the OECD review comprises four chapters. Chapter 1 summarises the key findings and recommendations stemming from the review, beginning with a short explanation of why an integrated health information system is so critically important. The review finds that Korea is well placed to build a high-performing health system that will not only improve outcomes but create a world-leading data environment that produces cutting-edge research and innovation to advance the health and well-being of people in Korea and beyond. To create a truly 21st Century health system, Korea should focus on greater harmonisation of clinical data, an enabling legal and policy framework, and building trust and fostering collaboration among key stakeholders.
Chapter 2 describes the requirements and the benefits of a health information system where data can be accessed efficiently and securely by actors who need them and by those who can generate valuable information and knowledge by using them. It also outlines the current situation in Korea regarding health data infrastructure progress across OECD countries.
Chapter 3 describes the Korean health system in terms of how its structure, organisation and governance influence the way health data are generated, managed and used to advance health system objectives. It also examines the main strengths and shortcomings of current arrangements in Korea to manage health and social care data including legislation and policies, health information infrastructure and health data interoperability. Chapter 3 outlines the changes needed to establish an integrated health information system in Korea that supports a learning health system, setting out the requirements to take advantage of strengths and to address the problems uncovered in this study.
A 21st century health system relies on first-rate data infrastructure
Twenty-first century health systems will be built around data and information. In simple terms, an integrated health information system enables the secure exchange and movement of data to where they can be used to create information and knowledge that advances policy and health system objectives. Integrated health information systems require a strong data infrastructure made up of the relevant data assets, technology, agencies and institutions needed for the collection, storage, maintenance, distribution and (re)use of data by the different end users.
It is necessary to distinguish between data and information. Data are raw figures and facts and, in and of themselves, may not be very valuable. Information, on the other hand, is meaning and insights that are obtained from the analysis of data. While data infrastructure is a key element, an information system also includes the capacity to convert data into usable information and knowledge. A useful analogy is an integrated transportation network, which allows passengers to move safely and securely across regional boundaries around the entire country using various transport types. While the physical and technical infrastructure is an essential component, such a system also requires people and institutions to ensure it operates effectively, efficiently, safely, and predictably. Thus, this report focusses on obtaining value from health data within Korea by developing a system that yields information.
All data have several potential uses
An integrated health information system would help Korea improve its capacity to get the best performance and value out of its health system in three ways. Firstly, it would directly improve care quality (including safety, effectiveness and efficiency). Secondly, it would improve patient empowerment by enabling people to access their own health information and for this information to “follow the patient” wherever they seek care in the health system. Thirdly, it would also raise the country’s capacity to use health and other data for other important secondary purposes, such as informing continuous assessment of health system performance, and enable learning and improvement cycles from the national level to the clinician’s office. It would enable more effective and efficient:
Public health monitoring and surveillance,
Resource allocation and reimbursement to reward value,
Biomedical research and development, and
Innovation such as big data analytics and artificial intelligence that will enhance knowledge‑based decisions for patient care and health system governance.
A range of data assets are relevant to an integrated health information system. For Korea this includes data generated during acute‑ and long-term health care, data on public health and social care as well as other relevant data sources such as social, economic and environmental data where necessary (Figure 1.1).
Using data to improve performance
Data and their efficient exchange to generate useful information (such as metrics and indicators) are fundamental in generating the information needed to improve and optimise health system performance. Performance can only be defined around the goals and objectives of a health system. While these may vary, the metrics and indicators needed to assess how well the system achieves its goals, and where improvement is needed, require data. Because system objectives typically cover various domains ranging from technical efficiency to equity and sustainability, a range of data from various sources will be needed to generate the necessary metrics and indices (Figure 1.1).
A ‘learning health system’ leverages its data in this manner to improve performance through continuous cycles of reflection, adjustment and evaluation. Learning health systems aim to deliver health services that are of high quality and value, that improve health and well-being and, at the same time, provide innovative and rewarding workplace environments for health professionals (AHRQ, 2019[1]). Moreover, performance domains will include areas that benefit from the sharing of information (prevention and care co‑ordination, for example). The importance of an infrastructure that enables the smooth exchange and sharing of high-quality data can therefore not be understated.
Figure 1.1. The main data types in a nation-wide health information system

Image credits: © Shutterstock.com/Moab Republic, Shutterstock.com/Cube 29, Shutterstock.com/Millering, Shutterstock.com/Qualit Design.
Interoperability and governance enable efficient and secure exchange of data
Countries making progress in this regard appreciate that data are a non-rivalrous asset (one of the hallmarks of a public good), and that each data point can and should have many uses. Data should therefore be harnessed to generate maximum social benefit. To do this, all data must be coded according to agreed technical and semantic formats. Only this way can data be meaningfully exchanged, sent to where they are needed, or analysed. Standardisation is especially important the Korean system where care provision is highly fragmented and competitive.
It is important to stress that an integrated health information system does not require all data of a certain type to be kept in a single location. It is quite possible to achieve the key objectives outlined above without central storage or even aggregation. A unified and co‑ordinated approach to national data governance can enable smooth information exchange and use for a range of purposes without compromising privacy, security, and ownership of data. In fact, a federated approach to data (which is more compatible with the Korean system’s supply side structure) can be more optimal.
Ensuring that data can be exchanged across national borders and beyond can amplify the benefits of data analytics and research in, for example, the context of public health, rare diseases, pharmacovigilance, and precision medicine. An information system that follows international data standards facilitates within-country and cross-border health care delivery and business opportunities for Korean research and technology sectors.
An integrated health information system requires a data governance framework that avoids the over-use of consent to authorise data exchange, in favour of legal authorisation and an approach that protects privacy and ensures data security while enabling data to be exchanged and used for legitimate purposes. The OECD Council Recommendation on Health Data Governance sets out the elements for a national health data governance framework and fosters a “privacy-by-design”1 approach that is consistent with emerging transnational requirements such as those set out in the EU General Data Protection Regulation (GDPR) (See Annex B).
Clinical data play a key role
Clinical data are a key component of any health information system looking to improve care quality, optimise performance and enable research and innovation. All OECD countries that are making progress with their integrated health information systems have:
Established a national organisation that is responsible for setting national clinical terminology and electronic messaging (exchange) standards
Created a multidisciplinary governing body for the national organisation that represents key stakeholders
Use unique identification of patients and health care providers
Adopted international terminology standards for diagnoses, medications, laboratory tests and medical images
Adopted the HL7 FHIR standard for data exchange (electronic messaging); and participate in global collaborative projects to improve international data standards.
Most countries have one country-wide electronic health record system and are exchanging these data at the national level including data sharing among physician offices and hospitals about patients’ treatment, medication use, laboratory tests and images. Most countries also have a Patient Internet Portal where patients can access their own medical records from all of their current health care providers. Many countries are also utilising EHRs for other secondary purposes including public health monitoring, health system performance monitoring, patient safety surveillance and health and medical research. Some are also developing big data analytics including machine learning, artificial intelligence algorithms with EHRs.
OECD countries have reported in a recent OECD survey several levers to improve the spread and interoperability of their electronic clinical data.
A legal requirement for health care providers to meet national standards for EHR interoperability. Thirteen countries reported to have a legal requirement for health care providers to adopt an electronic health record system (software) that conformed with national standards for both clinical terminology and electronic messaging (exchange).
A certification of EHR system (software) vendors that required them to adopt national standards for both clinical terminology and electronic messaging. Again, thirteen have a certification that requires software vendors to meet requirements for national EHR interoperability.
Financial incentives (or penalties) for health care providers to install an EHR system that meets national standards and requirements for national EHR interoperability. Nine countries report incentives for health care providers to keep their EHR system up to date as clinical terminology and electronic messaging standards change over time; and eight report incentives for health care providers to install and EHR system from a certified software vendor.
The Korean health system performs very well, with some room for improvement
Korea’s health system is unique. On the demand side, a single payer ensures universal coverage as well as one of the richest administrative datasets in the world. Governance is shared among several agencies, including the Health Insurance Review and Assessment Agency (HIRA) and the National Health Insurance Service (NHIS), which also hold very large data assets. On the supply side, Korea is one of the most fragmented systems in the OECD. Health care providers are almost exclusively private, and acute care hospitals feature prominently in care provision. Patients have abundant freedom to choose providers, and gatekeeping to secondary and tertiary care is comparatively weak with a high degree of competition between providers and commensurately less collaboration and integration of care. From a data infrastructure perspective, the result is poorly harmonised and exchanged clinical data. There is a strong track record of key reforms, most notably the creation of the single‑payer model 21 years ago. Providers and the medical professions can be very influential in policy development.
Optimising health system performance relies on good data and information
The special focus of this review was using data to optimise health system performance. Defining performance must consider the objectives of a health system. In Korea these encompass:
1. safety, efficiency and effectiveness (i.e. quality) of care
2. equity (fairness) in access to care and health outcomes
3. sustainability, which comprises a. ensuring the system copes with rising chronic diseases and demographic change (e.g. disease prevention and managing NCDs in non-acute settings), and b. supporting innovation and the development of cutting-edge medical technologies.
A good health data infrastructure and information system are critical to achieving these objectives in three ways. First by providing the necessary data and information on whether these objectives have been achieved or not. Metrics and indicators are needed to inform policy makers as well as providers and practitioners about performance in the domains relevant to them. Only through regular monitoring and feedback can improvement occur, and performance be optimised. Such a learning health system is only possible with a strong data infrastructure and health information system that covers all key performance domains. Such a system needs to go beyond answering the questions of “What went wrong (or right)?” to the more important questions of “Why did this happen?” and “What changes are needed to minimise risks and maximise value fairly across a domain or the system as a whole?”
Second, achieving all the above objectives relies on health data exchange among relevant actors ranging from patients and their providers to regulators and policy makers, to researchers and industry. These actors can then use the available data to generate information and knowledge that is relevant to them, enabling them to monitor, learn and improve on a continuous basis.
Third, it paves the way for regulatory and policy mechanisms that incentivise better performance and enable more optimal resource allocation. For example, moving from a fee‑for-service remuneration model to one that rewards value for money is only possible with granular data on outputs (activity) as well as outcomes (including patient-reported outcomes) and costs across entire care cycles that span the acute, non-acute and long-term care settings. This is only possible with a fully integrated health data infrastructure.
The Korean health system can improve in areas that require better information exchange
The Korean health system compares well to other OECD countries on some metrics including avoidable mortality and treatable mortality. This is unsurprising given the strength and ubiquity of acute care in Korea. Most Koreans (71%) report being satisfied with the availability of quality health care (the figure is close to the OECD average). More recently, the health system’s management of the COVID‑19 pandemic achieved case numbers and deaths that were among the lowest in the world. Notably, this was achieved through unprecedented collaboration across agencies and sectors that enabled the standardisation, integration (linkage) of data among them and the development of a secure mechanism to make these rich data accessible to a range of actors for the purpose of pandemic management and research.
There are important areas where the Korean health system compares less favourably to OECD countries. These point to where tools that enable improvement may need to be implemented. For example, Korea has a relatively high morbidity from NCDs and avoidable hospital admissions for diabetes and asthma. Rates of depression, anxiety and suicide are among the highest in the OECD, as is the proportion of people who rate their health as poor (OECD, 2021[2]).
While policy makers may point to Korea’s life expectancy, which is among the highest in the OECD, longevity is a blunt indicator of health system performance (and even less useful for health care) due to the many non-medical factors that contribute to people’s health and longevity. Insofar as life expectancy is a proxy for health, little is known in Korea about differences across social strata – and therefore about health equity (one of the main objectives of the health system).
Performance in several domains is unknown through lack of information
Although the Korean health system has abundant claims, administrative and activity data, consolidated data on outcomes (e.g. unplanned readmission) beyond where this results in a claim (e.g. admission to hospital) or an end point (e.g. death) are lacking. Clinical outcomes (e.g. test results) as well as patient-reported metrics are not reported consistently nor integrated nationally. Problems with coding and reporting present-on admission (POA) flags have been described. These and other issues mean that Korea does not provide several health statistics collected by the OECD (see Table 1.1).
This situation is problematic because it reduces the capacity of Korea to monitor, evaluate and learn and thus improve performance across the health system. It also points to key areas where Korea’s health data infrastructure must be improved. This is not to say that the data do not exist – they do, typically in EMR systems of providers. It is the lack of infrastructure to harness these data for the purpose of monitoring and improvement that is missing and needs to be addressed.
Table 1.1. Selected indicators and statistics not reported to OECD by Korea
|
Patient safety |
|
|
Care quality |
|
|
Other |
|
Building on the Korean system’s many strengths
Korea has taken great strides towards creating a health data infrastructure conducive to a high-performing, modern health system. Its insurance claims data, in terms of coverage, volume and detail, are among the best in the world. The National Health Insurance System (NHIS) holds health care data (e.g. admission, outpatient service, emergency treatment, prescribed drugs), long-term care data (e.g. nursing, home care, prescribed drugs), public health data (e.g. birth and death, demographics, lifestyle, health checkup), social care data (e.g. Medical Aid, assisting device for the disabled, etc.), and contextual data (e.g. occupation, income level, environmental information. NHIS uses these data assets to support coverage expansion for the less-advantaged population, and to improve efficiency and sustainability through policies such as the benefit/health check-up system, finance analysis system, cost information analysis system and fraud detection system. The My Health Bank system is shared with the public based on this data-driven system.
HIRA programmes such as the Drug Utilisation Review (DUR), the Benefits Information Analysis System and the broader transition towards value‑based claims review, for example, provide a strong foundation to establish a learning health system by improving the interoperability of clinical data for direct patient care, developing personal health environments, and the creation of research infrastructures for the life and the social sciences. In addition, Korea has a strong and committed academic research community that has produced some outstanding work over the years.
Excellent foundations for data availability and governance
Korea reports excellent data availability, maturity and coverage of key health datasets compared to other OECD countries. For much of its data, Korea also stands out for having a very short time lapse between when a data record is first created and when it is included in the national dataset used for analysis. Korea was one of only 7 countries that reported having a unique patient/person identifying number that could be used for record linkage that is included within 90% or more of their national health datasets. Korea is also among the countries with the strongest data governance across key national datasets considered (Figure 1.2).
For secondary uses of data (statistics and research etc.), Korea is already quite advanced in creating an intermediary solution to improve health data interoperability through a Common Data Model (CDM). A CDM maps data from multiple organisations that use different standards to a standardised structure that makes it possible for data to be used for analytical applications, allowing for efficient data pooling and data integration for health statistics and research. Much of the data held by HIRA, as well as the EMR data of over 40 Korean hospitals have already been mapped to the Observational Medical Outcomes Partnership (OMOP) CDM as part of the global Observational Health Data Sciences and Informatics (OHDSI) Project. However, a CDM is not a practical solution for most primary uses of data such as enabling the smooth exchange of data between health care providers for direct patient care or the development of a “real time” and interactive patient Internet portal – often called a Personal Health Record.
Recent reforms demonstrate that Korea has the capability to plan and implement major structural reform of the health system, overcoming internal and external resistance. This experience will stand it in good stead to implement the necessary reforms to create a health information system for the 21st century.
Figure 1.2. Dataset availability, maturity and use, and dataset governance
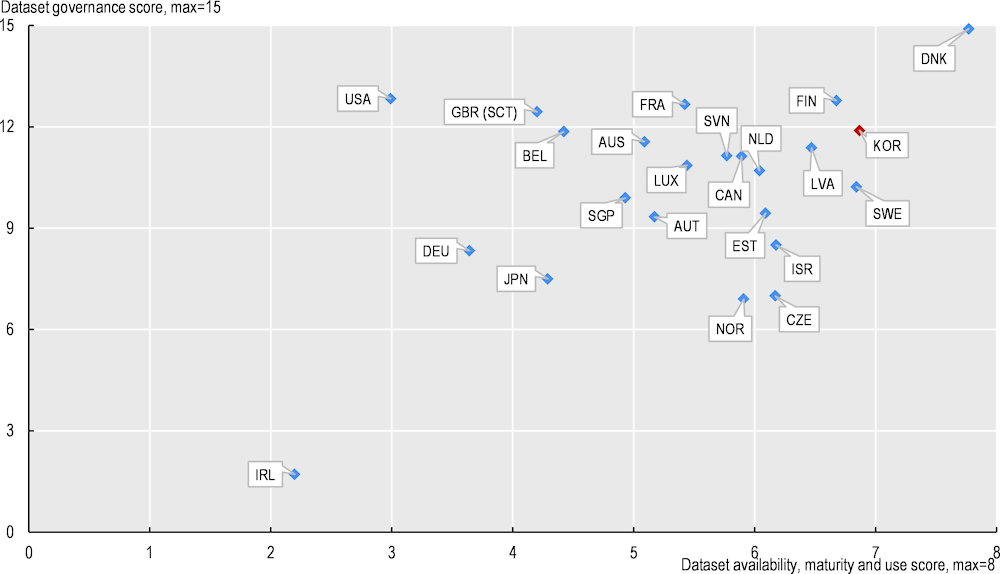
Note: Dataset governance score is the sum or the proportion of health care datasets meeting 15 dataset governance elements and the dataset availability, maturity and use score is the sum of the proportion of health datasets meeting 7 elements of dataset availability maturity and use.
Source: Oderkirk (2021[3]), “Survey results: National health data infrastructure and governance”, https://doi.org/10.1787/55d24b5d-en.
NHIS is ushering in integrated services for chronic disease patients by gathering scattered information
Korea is attempting to build a comprehensive chronic disease management system by integrating patient data scattered across organisations. KDCA has built health behaviour and chronic disease management status data based on the annual national nutrition survey. NHIS has benefit claim data, lifestyle data such as drinking, smoking, and exercise, and actual measurement data from health checkups. NHIS analysed its own data to produce condition management indicators including indicators about risk factors, metabolic syndrome, chronic diseases, and complications by small scale regions and workplaces. The Chronic Diseases Management Registration Program is a public data platform that collaborates with primary care providers to collect and accumulate chronic disease patient data (medical measurement and health management behaviour).
My Health Bank (a personal health record) supports individuals to manage their health risk factors, and helps policy makers set up tailored measures for their region. To build a national chronic disease management system, KDCA and NHIS are attempting to integrate the National Health Nutrition Survey and the health check-up and medical treatment system, which is expected to revolutionise the chronic disease monitoring system.
An expanded Drug Utilisation Review (DUR) as an example of what is possible
The DUR system was established in 2010 to provide a prospective, real-time review of drug prescriptions to minimise the risk of safety harms such as contraindications, drug/drug interactions or ingredient duplication. It uses data held by HIRA to provide real time advice and alerts to clinicians and pharmacists.
The DUR illustrates the current strengths of Korean data and foreshadows the possibility of an integrated data infrastructure in Korea. If expanded to include a broader range of data, it could serve as both a decision support tool as well as a world-class pharmacovigilance system. The DUR would be more useful for clinical decision making if it included information about patient-level diagnostics, pathology and test results, and if DUR advice were directly accessible within hospital and clinic EMRs – that is within the “clinical workflow”. Such an expansion requires integration of EMR and claims data as well as integration of DUR data and EMR systems. This expansion could transform DUR into a full drug safety information system, able to support regulatory decision making and post-market surveillance of drugs. Such a transformation is a clear application of the learning health system paradigm (Figure 1.3).
Figure 1.3. A learning health system illustrated through medication surveillance
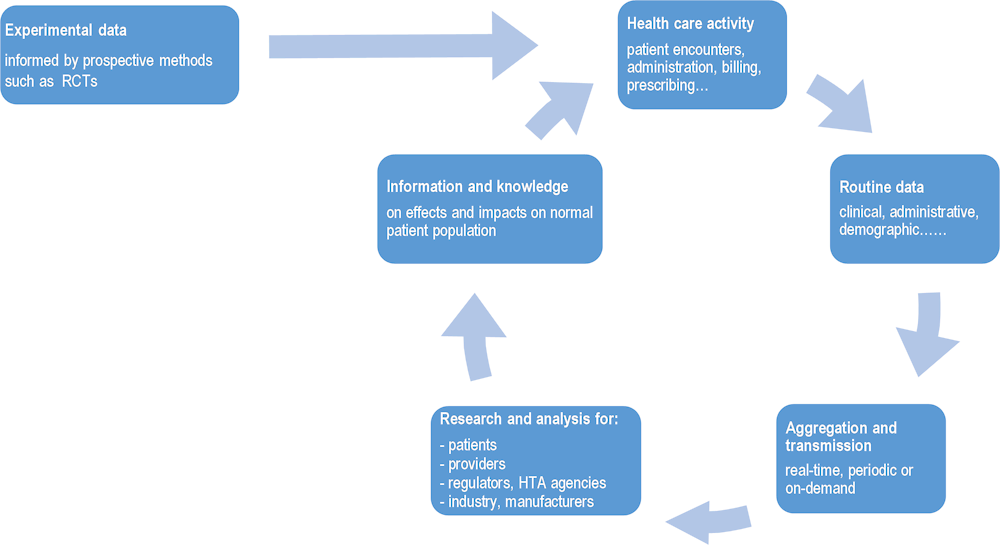
Source: OECD (2019[4]), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, https://doi.org/10.1787/e3b23f8e-en.
Value‑based claims review and assessment and reimbursement analysis exemplify steps in the right direction
HIRA is moving towards a more nuanced review and assessment process that aims to maximise value for patients and NHI enrolees as opposed to minimising costs. While the previous process accepted or adjusted the benefit paid based on standardised amounts on an item-by-item basis, the new approach is a more comprehensive judgement that considers the local context, quality of service and treatment outcome. It also includes expert participation by providers, academics, and policy makers, creating a “virtuous cycle” of learning development of indicators, fine‑tuning standards and developing indicators that inform continuous learning.
HIRAs Benefits Information Analysis System also demonstrates many of the principles and requirements using data to promote continuous learning and improvement. The Benefits Information Analysis System draws on claims and other data held by HIRA as well as data held by Statistics Korea and the Korean weather service to analyse trends in the frequency and costs of medical interventions both within and outside the NHI coverage with the aim of preventing unnecessary medical services, preparing policy measures through medical service use analysis conducted from user and provider perspectives, and creating a more effective yet sustainable medical environment. The initiative has driven several successful outcomes in several clinical areas including magnetic resonance imaging for stroke patients and the treatment of thyroid cancer.
Obstacles to building trust and harmonising data limit development of a learning health system
While Korea has many advantages supporting a learning health system, such a system will not develop in Korea with addressing key obstacles to building trust and, consequently, to harmonising and sharing data while protecting privacy and data security. These obstacles are a lack of trust, social licence and incentives toward data sharing and collaboration, the lack of a framework for research access to data, incoherent EMR systems and a lack of patient-reported data, and laws or their interpretation in practice that block progress toward a learning health system.
Lack of trust, social license and incentives toward data sharing and collaboration
Trust is essential to the development of an integrated health information system that will meet the needs of Korean society. Many experts consulted identified the need to rebuild public trust in the exchange of data among health care providers and between providers and national health data organisations and the government. There is a lack of trust between health care providers and the government and even a lack of trust among national health data organisations that limit the possibility of progress toward secure and privacy-protective data exchange and integration to serve the public interest.
There are several areas where a lack of trust between health care providers and the government is limiting progress in health data sharing and use for the benefit of the public. Providers voiced concerns that if they did routinely exchange data with one another that they would be responsible for data breaches/leaks and face a public backlash that would hurt their reputation and business. Providers also resist exchanging data for fear of losing patients to other health care providers, particularly large hospitals.
Health care organisations and individual providers are reluctant to share financial data with public agencies such as HIRA and NHIS. In part, this is because they view their data as a business asset, that is a private good to use to generate profit from their use and sale. Also, there are concerns that standardising and integrating EMR data with NHIS/HIRA create opportunities for unfair comparisons, and that the introduction of standards for data exchange will diminish the diversification of medical care and treatment methods that could be provided to patients (particularly privately insured services) and will harm physicians economically.
In the absence of financial incentives for data interoperability, the benefits of data interoperability and integration are perceived to mainly accrue to government, researchers and health insurers, while the costs of improving the interoperability of health information systems are mainly borne by health care providers. Government leadership and legislative and policy tools are needed to create the right environment for information exchange and collaboration that creates a “win-win” for all stakeholders in a learning health system.
Neither NHIS, nor HIRA, have a specific mandate or resources to support the improvement of health care quality and safety that permits development of a learning health system. Further, there are legal and administrative barriers to collaboration between HIRA and NHIS and between these two agencies and other key national stakeholders in the health information system, such as the Korean Health Information Service (KHIS), the Korean Disease Control Agency (KDCA) and Statistics Korea (KOSTAT) that make it very unlikely that further development of a learning system will occur over time within the existing system.
Further, the MoHW and other parts of the Korean Government, launch IT and data projects which overlap one another and lack a unifying strategy or purpose among them so that if would be possible for them to work together efficiently to achieve common objectives that improve Korea’s health system and people’s health.
Lack of a framework for research access to data
There is no unifying framework for research access to health data in Korea. As a result, there are different separate initiatives underway that are each trying to fulfil a similar need resulting in unnecessary duplication of effort and expense. For example, HIRA accepts and reviews applications for access to its data holdings and provides a secure research room on its premises as well as real-time remote data access services for approved applications. The NHIS also accepts and reviews applications for access to NHIS data via dedicated terminals (remote access) within data analysis centres in multiple regions.
Researchers interviewed indicate that both HIRA and NHIS have long waiting lists for approval to access data with waiting times of several months to up to one year. Further there is no mechanism to appeal an approval decision.
Incoherent EMR systems and a lack of patient-reported data
While Korea has most of the key national health datasets that the OECD considers essential to a national health information system, there are important gaps. Although all Korean health- and long-term care providers record clinical data within EMRs, most of these data are not interoperable owing to the lack of consistent standards for terminology or exchange. Voluntary participation of health care providers in contributing to national datasets is a reason for incomplete coverage. This means that there isn’t a national clinical data set, but instead there are small silos of data that are difficult to access and use.
Patient-reported data on outcomes and experiences of care can shed light on how health services perform. Collection and use of these data in Korea are still nascent. For example, paper questionnaires are used although some hospitals reportedly collect PROM data electronically. PROMS data collection could be integrated in to the clinical “work flow” as part of national EMR requirements.
KHIS provides certification for vendors and providers and carries out standardisation of data formats for the entire nation. It is anticipated that standardisation for data exchange and semantic interoperability will spread using EMR certification as a tool. MoHW is leading a pilot project of an EMR-certified fee schedule with providers and will evaluate the use of standardised EMRs. In particular, the standards will be applied to assessment items in stages, such as patient safety, treatment continuity, patient health management, and public policy support.
Regarding secondary use, KHIS plans to build a standardisation strategy for public policy support. Currently, its focus is on primary uses of data, and not on other critical uses of data for statistics, health system performance monitoring and medical research. The development of standards within KHIS excludes the development of secondary “use cases” to ensure that the data will meet the requirements of a learning health system. No role exists for the large national health data holders in the development of standards by KHIS, nor is there any mechanism for KHIS to evaluate or integrate data standards being developed by these other national organisations.
Laws and their interpretation in practice that block progress toward a learning health system
Korean laws governing the primary and secondary uses of data protect individuals’ privacy but to do so in a manner that creates barriers to the privacy-protective uses of data to serve the public interest. “Privacy-by-design” mechanisms that support data sharing, linkage and accessibility should be permitted.
In Korea, it is legally possible to extract EMR data for secondary uses, but the interpretation of the laws is so strict that doing so is difficult in practice. Further, integrating health data in the custody of the main organisations responsible for national health data (HIRA, NHIS, KDCA and KOSTAT) would seem to be legally possible to generate “official statistics” but current legislation (or its interpretation) make collaboration limited, highly bureaucratic, expensive and slow.
Best practices in “privacy-by-design”, such as where organisations share a common pseudonymisation algorithm that is applied to their data so that they may be linked by pseudonymised ID, are not supported by law or policy. Further, large national organisations that are trusted to process personal health data are distrusted to undertake data linkages to serve the public interest when the linkages involve integrating their data together.
Experts representing civil society organisations in Korea advocated for reforming the Korean data protection law to require pseudonymisation of identifiers and the secure storage of pseudonymisation linkage keys to strengthen data protection and build trust. Further, these organisations are concerned the legal penalties for data misuse are not high enough to be a deterrent to misuse.
Creating a learning health system in Korea
Korea has many of the building blocks in place to develop a modern health data governance and information system that supports a learning health system. Policy actions are recommended to create the foundation for a world-class 21st Century health information system that serves the needs of the Korean people. These policy recommendations are summarised below (see Chapter 4).
Building trust among stakeholders and the public
Creating a learning health system will steer Korea away from the current situation of data silos toward an integrated system where secure data exchange, linkage and secondary uses are the norm. Building a learning health system will require a mindset that sees data as a public good and a resource that can be harnessed to advance the health and welfare of the Korean people. This will require a change management approach that builds trust among all stakeholders and the public.
This approach should include consulting with governmental agencies about their needs, and with non-government stakeholders especially patient groups, regions and municipalities, provider organisations, health professional groups, insurers, academia, biomedical industry and software vendors. It will require a sustained public information campaign, public consultations and other avenues for public input into the strategy, including public consultations at all stages of development, and a dialogue with the public about the benefits of data sharing and exchange, with the goal of valuing health data in Korea as a public good. This public dialogue must assuage public and stakeholder concerns about privacy risks and reassure them by clearly communicating about how privacy will be protected when data are used. Further, it must deliver on these protections in practice.
Adequate resourcing of these activities will be critically important. This means allocating sufficient time and resources to consultation with stakeholder bodies and the public at all points in the development of the strategy, so that progress from a draft strategy to a final strategy to roadmaps and implementation will feel natural, expected and safe.
Central leadership
Central leadership means that the MoHW – or any new authority or agency designated by the ministry – would oversee the development and implementation of the national strategy and its components outlined above. It would develop the campaigns and tools to build trust among stakeholders and the public, and develop and maintain analytics products and dashboards for ministerial policy making and reporting, and evaluate and publicly report on progress in the implementation of the national strategy.
It would need to facilitate progress in policy and legal reforms to support the on-going development of an integrated health information system, co‑ordinate planning and funding of health information projects within the ministry to align them with the strategy. The MoHW would also need to ensure that the transition to, and maintenance of, the new arrangements across all levels of the system are adequately resourced.
Developing a national health information strategy
A central authority such as the Ministry of Health and Welfare (MoHW) or an appointed agency should lead the development of a national health information strategy for using all available data efficiently, intelligently, and securely for a range of purposes. An important part of the strategy would be to change the current institutional arrangements which are characterised by overlap, duplication, and inconsistent approaches to managing and using health data.
Internal support will be needed to build a team to take the lead. The ministry could consider creating a new unit or separate authority/agency that engages experts in health information systems, health data science and informatics and health data governance. This expertise will be essential to ensuring an effective national strategy is developed and implemented.
The national strategy should align with broader policy frameworks to build a digital society (such as the Digital New Deal or a subsequent strategy). In fact, most countries that are successfully digitalising their health systems have a national digital strategy – and data governance – that encompasses all areas of public policy including health. The advantages of a cross-sector approach are particularly strong in the health arena given the value placed on privacy and security, the key role of non-health data (which can greatly enhance knowledge‑generation), and the fact that makes a country more attractive for investment of biotech capital.
A legislative framework and supportive policies
Legal authority will be needed to authorise and finance the national strategy and its implementation. Legal reforms are also needed to bring the health data governance law within Korea closer to the OECD Recommendation on Health Data Governance (OECD, 2019[5]).
The OECD Recommendation calls on countries to implement a national health data governance framework and sets out the principles for the development, content and evaluation of the framework. Implementation of this framework may require legal reforms or the publication of guidelines to ensure that all stakeholders in the health information system have a common understanding of their roles and responsibilities with respect to health data development and use and privacy and security protections. The national data governance framework should emphasise privacy-by-design and adherence to FAIR principles, that is that data are findable, accessible, interoperable and reusable.
Areas for potential legal reforms noted in this study include a revision to the Data Protection Law to enable national agencies who are already trusted to collect and process health data to be legally permitted to link data between them for legitimate purposes within the health-related public interest. Further revisions to privacy law should strengthen safeguards to protect data privacy and security, such as requiring data pseudonymisation and having penalties for data misuse that discourage illegal data uses that have damaged public trust.
A unifying policy framework is also necessary that will support a learning health system. Different bureaus within the MoHW are developing policies and funding projects that will affect the health information system and this needs to be co‑ordinated within the MoHW as well as greater co‑ordination among national agencies who have their own health information projects. Further co‑ordination is needed at the whole of government level as other ministries are also funding health information projects for purposes of scientific or economic development.
Revisions may be needed to legislations authorising existing national agencies responsible for health information if their existing mandates create obstacles to collaboration or their resource allocations are insufficient to support collaboration. Revisions may also be needed to legacy legislations that pose unnecessary obstacles to a learning health system.
Enabling the National Health Insurance Institutions (NHIS&HIRA) to collaborate with each other and other agencies
HIRA was launched to be an intermediary between the National Health Insurance Service and health care providers, to protect health care providers from any potential unfairness that might have arisen from the consolidation of numerous insurers toward a single public insurance system. This role as a fair and objective intermediary (honest broker) could be strengthened by ensuring both legally and in its funding that HIRA is fully independent of NHIS and the government and focussed upon health care improvement for the benefit of all stakeholders.
To fulfil this role, and to operate at arm’s length from the government, the governance of the National Health Information System would require representation of all key stakeholder groups: patients, consumers, health care providers, governmental agencies and businesses that contribute to and depend upon the health information system.
The range of data that could be linked and integrated to realise a learning health system would need to be expanded to include:
EMR data, particularly lab results, and imaging results
Data related to patient outcomes such as present on admission (POA) flags, Patient-reported outcomes (PROMS) and experiences (PREMS), and clinical outcomes
Environmental, behavioural and socio‑economic characteristics of patients
Private insurance claims and uninsured health care services.
Patient Registry
Organisational changes at HIRA would also help to both minimise the burden of reporting born by health care providers and maximise the clinical value of the quality registries HIRA would be supporting. The real-time microdata HIRA collects currently from health care providers for the purpose of adjudication of health care insurance claims must be integrated with real-time clinical data to provide real-time clinical care quality and safety monitoring that is useful for health care providers continual improvement of patient outcomes and health care workplaces.
The current process of duplicative data collection, with a separate and non-real time data collection system for the assessment side of HIRA, should be phased out because it is unnecessary and slow, with quality indicators on the assessment side lagging health care events by several years.
Instead, the collection of real-time data from health care providers should be based on the collection of clinically relevant and timely data for a full monitoring, reflection and evaluation cycle of improvement of the health system. Priority should be given to designing a data collection and reporting system that provides high quality and timely information supporting decision making of different stakeholders.
Further, data integration and exchange among HIRA, NHIS, KDCA and KOSTAT will be essential to creating a learning health system that includes the surveillance, evaluation and improvement of health outcomes of patients with infectious and chronic diseases. Such surveillance is part of the mandate of the new KDCA, but its mandate cannot be fulfilled without data exchange and integration with the data collected by the other agencies.
However, at the present time, negotiating data sharing agreements among national agencies where data linkage is necessary has been very complicated and resource consuming for all national agencies. Further, where national agencies do not see the exchange and data linkage as a specific win-win for them, they may not engage in negotiations or may drag out work over a long period of time.
Moving forward, it will be essential to incentivise co‑operation among national agencies toward a common shared goal of developing a learning health system that improves the outcomes of patients and the effectiveness and efficiency of health care services. (See also Recommendation 7 on creating a single entry point for shared data.)
Integrating the KHIS in the new Korean data infrastructure
A first-rate health data infrastructure and information system in Korea will require an expansion of the KHIS remit to cover secondary uses and, as described in the previous section, greater collaboration with other key actors. The global standards for data exchange and semantic interoperability, administered and governed by KHIS, must include “privacy-by-design” protections, particularly federated learning (distributed analytics) building forward from the recent experience of HIRA with OHDSI. Standards should include interoperability in analytics, information and knowledge and foster the broad adoption of the OMOP common data model (CDM), building from recent investments of the MoHW as well as the Ministry of Industry.
Clinical (EMR) data are an integral part of a learning health system. The KHIS has no mandate for considering secondary use of EMR data, or the contribution of the OMOP Common Data Model to realising intermediate goals for clinical data interoperability. While there is a role envisaged for KHIS in providing health information governance, it would not be possible for KHIS to fulfil such a role without working closely with the national agencies responsible for health data. KHIS should be intimately involved in developing and implementing a learning health system, as all key stakeholders should be. Revisions may be needed to the authorising legislation for KHIS.
Supporting and incentivising data quality and exchange
To complement laws and policies, funding and financial incentives will be needed to encourage compliance with national data standards, for demonstrating (verifiable) data interoperability, and to ensure national agencies responsible for health data have the resources needed to support greater inter-agency collaboration to realise the strategy.
This will require a review of government funding and financial incentives related to the exchange and use of health data, including research projects funded by government ministries. It may also require explicit financial incentives to encourage health care providers, national agencies responsible for health data and other actors to move to certified IT solutions and succeed in achieving verifiable interoperability.
Demonstrating verifiable interoperability would include incentive payments, funding or accreditation that is conditional upon passing data quality checks and passing thorough (random) data quality audits, as well as meeting national requirements for data privacy and security protection (see Chapter 4).
Korean government plans call for financial incentives to EMR software vendors to adopt national standards for data terminology and exchange and to health care providers/organisations who demonstrate they are using an EMR that conforms with national standards. These planned incentives do not include funding for the transition costs that may be faced by health care institutions as they convert from their existing system to the new standards. Concerns were raised in this study regarding the costs for infrastructure, such as upgrades to software, hardware and networking, and softer costs related to staff training and lower productivity during the transition. These up-front costs may be too high for small clinics and hospitals to self-fund and therefore they may not be able to convert, despite the attractiveness of the incentive payment.
The MoHW should also evaluate how plans for broader reforms to health care funding and remuneration that reward care co‑ordination and value‑based care would affect the design and functioning of the learning health system. In short, this will include: 1. needs-based funding to hospitals and provider organisations for transitioning their local data systems and infrastructure to an agreed national format and standard; 2. incentives for verifiable interoperability and meaningful use of health data including auditing data quality, interoperability and privacy and security protections AND successful and consistent provision of data to authorised agencies (in addition to KHIS certification process); and 3. a fair and balanced method to sanction and penalise lack of compliance, comprising financial and other levers.
A single entry point for secure data access
OECD countries are increasingly providing a unique entry point for access to all public sector health data, either through an expanded mandate of an existing national organisation or through the creation of a new organisation. This unique entry point has a primary aim of improving access to health data for secondary uses that are within the public interest while protecting data privacy and security (see Chapter 2 for examples).
Given the current arrangements for access to data in Korea are fragmented, the government may consider consolidating these activities into a one‑stop-shop for secure access to various health data from a variety of sources outlined in Figure 2.1. Such consolidation into a single data hub would simplify the process for researchers and other secondary users of Korean health data, and enable secure, record-level linkage of all relevant datasets to create valuable knowledge. It would make access to data for research and other secondary purposes in Korea more secure, efficient and easier. Further, it would make public sector health data collection, data use and data protection more fully transparent to the public and to the research community.
This would not require all data to be copied, transferred or held in one repository as it is now possible to perform complex analyses across a distributed or federated network. Under this approach, data always remain with their custodians. Only queries (research questions), and the aggregate results, are sent back and forth between the requestor (or hub) and the data holder. The precondition of a distributed network is that all sources of data to be accessed have already been coded to the same Common Data Model, such as the OMOP CDM which Korea has already invested in.
Moreover, the hub could support Korea in providing data linkage and access services at ‘arm’s length’ from organisations with direct involvement in the provision or assessment of health insurance, or in the provision of health care or public health services. This independence from the policy and business of health care could build greater trust among the stakeholders that the purpose of health data linkages and uses are to serve the public interest in better health, high quality health care and in privacy protection and data security.
The involvement of all key health information system stakeholders in the governance of this hub would create the opportunity to engage these stakeholders in a collaborative effort to develop and improve the quality and efficiency of standards for health data terminology, exchange and interoperability for both primary and secondary data uses.
However, a hub alone will not be sufficient to improve collaboration and data sharing among the large national organisations who are processing personal health data. The national strategy must emphasise the importance of secure access to, linkage of and sharing of health data to serve the public interest and include the necessary changes to organisational mandates, legislations and resources to ensure that exchanging data becomes the default position, where the exchange is secure and the purpose of the exchange is to serve the health-related public interest.
References
[1] AHRQ (2019), About Learning Health Systems, https://www.ahrq.gov/learning-health-systems/about.html.
[3] Oderkirk, J. (2021), “Survey results: National health data infrastructure and governance”, OECD Social, Employment and Migration Working Papers, OECD Publishing, Paris, https://doi.org/10.1787/55d24b5d-en.
[2] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[4] OECD (2019), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/e3b23f8e-en.
[5] OECD (2019), “Recommendation of the Council on Health Data Governance”, OECD, Paris, http://www.oecd.org/health/health-systems/Recommendation-of-OECD-Council-on-Health-Data-Governance-Booklet.pdf.
Note
← 1. Privacy-by-design involves designing IT systems in a way that pro‑actively anticipates and addresses risks to data privacy and security so they may be mitigated. In such approaches, the privacy of all individuals whose data is within the system is protected by default. The protection of individuals’ privacy and data security is embedded within the architecture and functionality of the IT system. At the same time, the IT system supports all uses and re‑uses of data that are in the public interest.