Japan, which has the longest lived population in the world is taking public health seriously as a key objective of central and local governments. Relative to most OECD countries levels of risky health behaviour are low, but like Japan’s OECD peers a growing burden of non-communicable diseases, and a growing elderly population, are significant health challenges. This chapter, which appraises the overall architecture Japan’s public health system, points to areas of strength and weakness. In particular, this chapter stresses that in a highly decentralised system, where local government has significant responsibility for delivery of public health actions, Japan must establish a careful combination of strong central strategic leadership, local autonomy and responsiveness to local needs, and sharing of best practice across regions, and across sectors.
OECD Reviews of Public Health: Japan

Chapter 1. The Public Health System in Japan
Abstract
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
1.1. Introduction
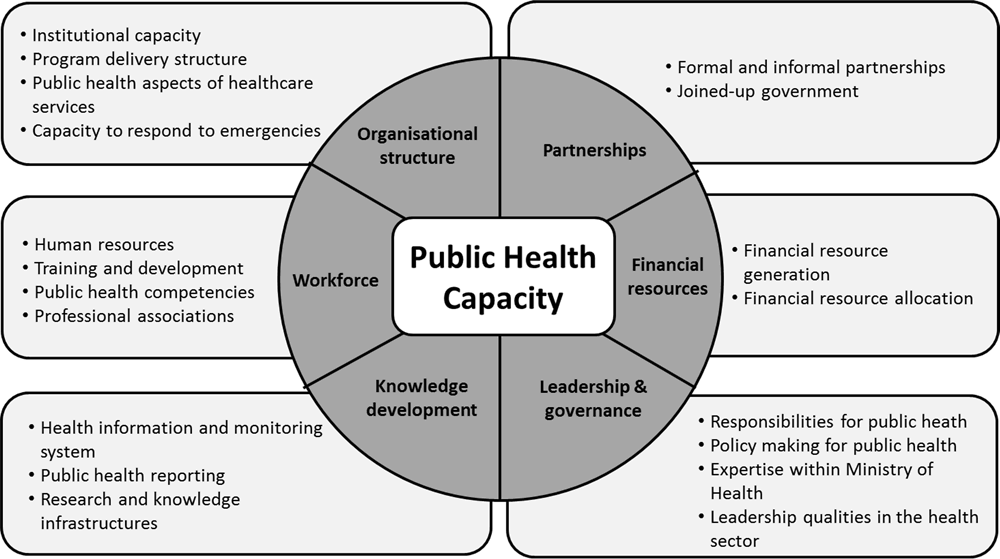
Public health issues have gained importance across OECD countries in recent years, as governments grapple with the best way to prevent disease and ill-health, and help their populations live longer, healthier lives. This chapter gives an overview of the epidemiological context and national public health needs in Japan, sets out a summary of the strengths and weaknesses of Japan’s public health system, and where weaknesses are identified makes recommendations for policy strengthening. The description of public health policies in this chapter is structured according to a framework for analysing the public health system detailed in Figure 1.1 below.
Figure 1.1. Appraising Japan’s public health capacity – analytical framework
1.2. The public health picture in Japan
1.2.1. The health status of the Japanese population
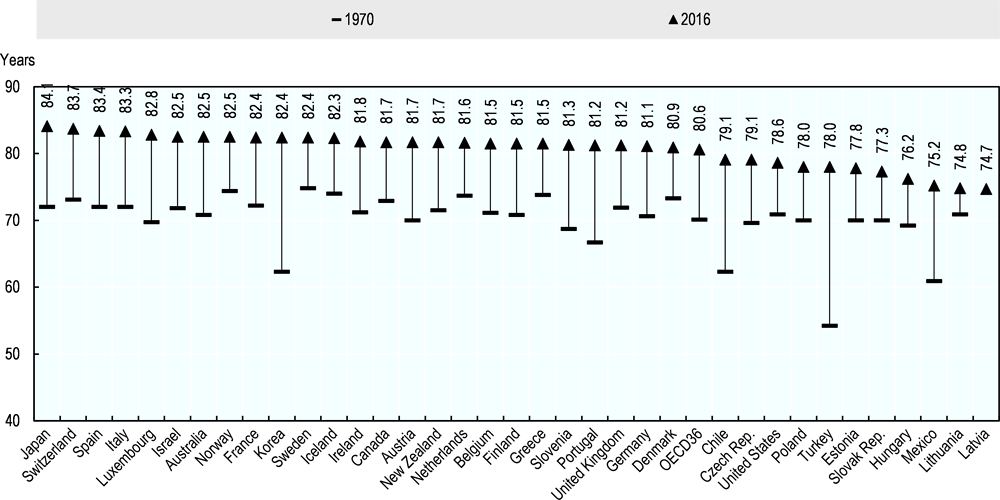
While Japan has the longest life expectancy at birth in the OECD (Figure 1.2), it is nonetheless an increasingly elderly society, with a low birth rate. The average life expectancy in Japan was 83.9 in 2015; 80.98 for men and 87.14 for women, compared to the OECD average of 80.6 years (OECD, 2017[1]).
Figure 1.2. Life expectancy at birth, 1970 and 2016 (or nearest year)
The proportion of people over 65 years old in Japan rose to 27.3% in 2016, the highest among the OECD countries. Although Japan’s total fertility rate has grown slightly over the past ten years, the number of birth has been declining overall. Changes to the structure of Japan’s population have had an impact on the stability of Japan’s social security systems; rapid aging of the Japanese population has significantly increased the old-age dependency rate. Twenty years ago there were 4.8 working-age people for each dependent elderly person; by 2015, the number had dropped to 2.3. The dependency rate is projected to fall even further in Japan, to 1.3, by 2065 (National Institute of Population and and Social Security Research, 2017[2]).
Despite being the longest-lived population in the OECD, perceived health status among adults in Japan is relatively poor; in 2015 only one third of the Japanese population reported that their health status is ‘good or very good’, almost half of the OECD average (Figure 1.3), while other OECD countries with similar longevity like Spain, Switzerland and Australia show better perceived health status than the OECD average. There are at least two possible explanations: first, the perceived health status is made by the self-assessment and can be affected by cultural factors; secondly, elderly people and women often report themselves in poor health, and in Japan the proportion of elderly people, and elderly women in particular, is high (Fujii, Oshio and Shimizutani, 2014[3]; OECD, 2017[1]).
Figure 1.3. Perceived health status among adults, 2016 (or nearest year)
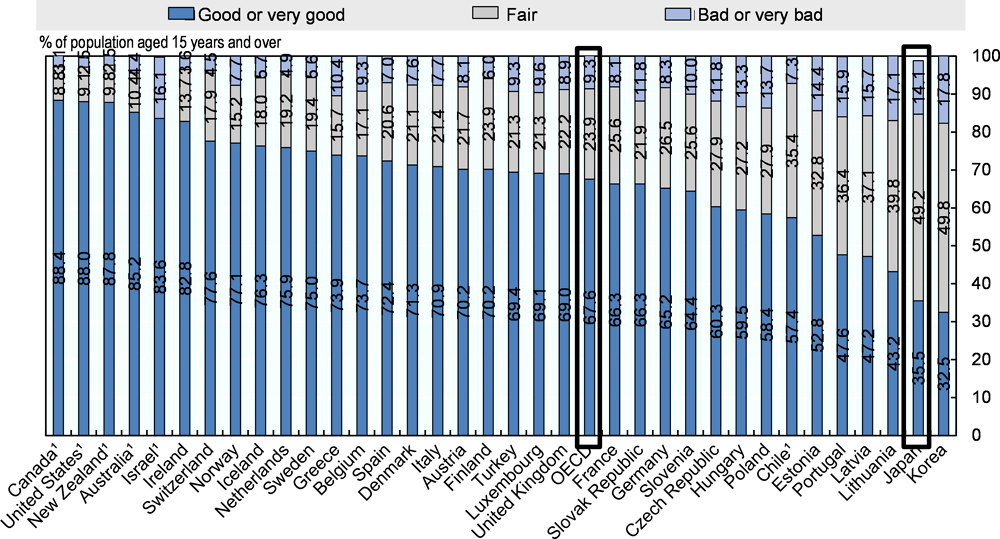
Source: OECD Health Statistics (EU-SILC for European countries), https://doi.org/10.1787/health-data-en.
1.2.2. Burden of disease
As in other OECD countries, the main burden of disease in Japan comes from non-communicable diseases. Hypertensive diseases, diabetes, cardiovascular diseases, cancers, and cerebrovascular disease account for 50% of all mortality; cancer has been the main cause of mortality since 1981, with the rate of 28.7% of all mortality in 2015 followed by cardiovascular disease (15.2%), pneumonia (9.4%) and cerebrovascular diseases (8.7%) (MHLW, 2015[4]). Looking at the mortality rate by major cancers, lung cancer is the highest among men and colon cancer for women. OECD data shows that overall cancer incidence is lower in Japan (217.1 aged-standardised rates per 100 000 persons) than other OECD countries (270.5 per 100 000). Although cardiovascular diseases are the second leading cause of mortality in Japan, the mortality rate with age-standardised rates per 100 000 population is the lowest among the OECD countries and shows a 40% decrease in the mortality rate between 1990 and 2015 (OECD, 2017[1]).
Although non-communicable disease represents the most significant part of Japan’s disease burden, some communicable diseases are still present in Japan, notably tuberculosis, which has higher incidence in Japan than in other OECD countries. The incidence rate of tuberculosis in Japan was 18 (per 100 000 person) in 2014, which is lower than the other Asian countries, yet higher amongst OECD countries (WHO, 2015) (see Figure 1.4). Mortality rate from tuberculosis was 2.4 (per 100 000 people) in Japan in 2016, while the OECD average is 1.6 (WHO, 2016[5]).
Amongst newly registered tuberculosis patients, 14.2% were diagnosed as diabetic and 9.1% as HIV positive. Of the 9 878 newly enrolled pulmonary tuberculosis culture positive tuberculosis patients, 0.5% showed drug resistance in 2016. Newly registered cases are found mostly among elderly people over 80 years old; 29.2% between 80-89 years old and 10.5% among over 90 years old (MHLW, 2016[6]). Since tuberculosis is an air-borne infectious disease (which is nonetheless recommended as a routine vaccination in Japan) it can cause a huge impact once it spread in a community such as at school or a hospital. There was a tuberculosis outbreak in 2012 at a hospital in Japan, which had 78 tuberculosis patients among the inpatients and the staffs (Nikkei Economic News, 2012[7]).
Figure 1.4. Incidence rate and prevalence and mortality rate of tuberculosis in 2014
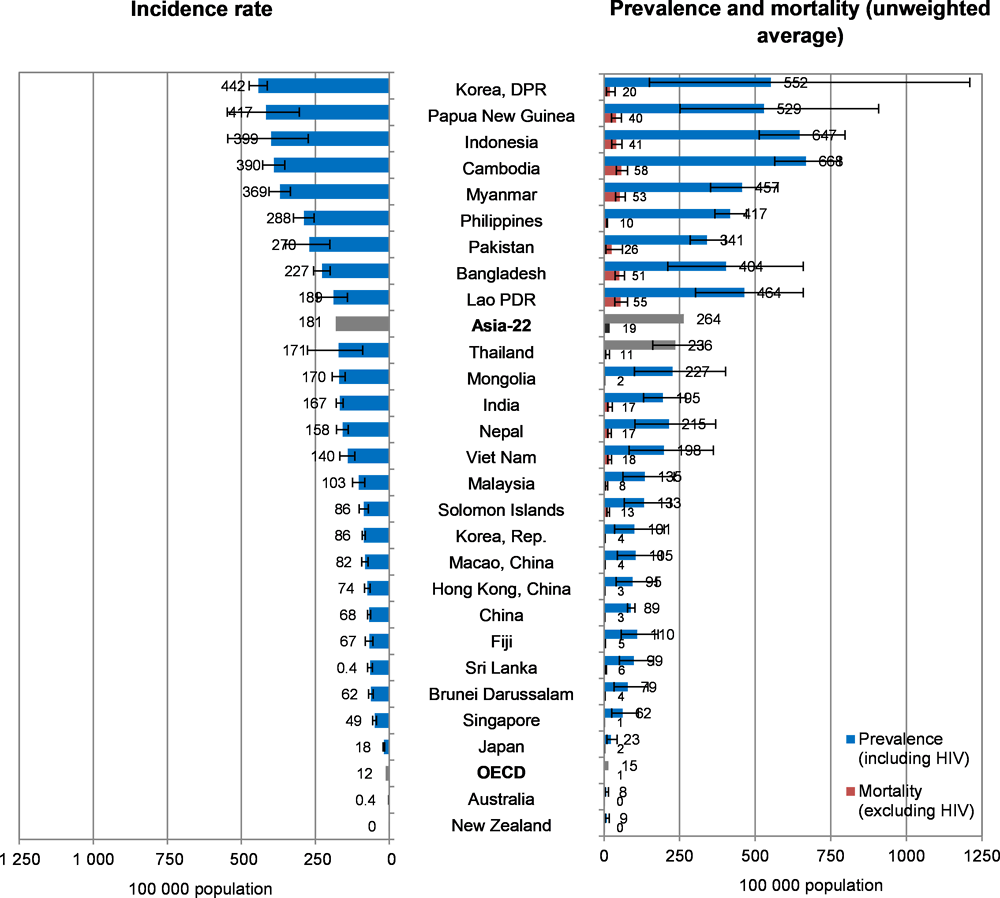
Source: World Health Organization (2015[8]), Global tuberculosis report 2015, http://www.who.int/iris/handle/10665/191102.
The incidence of HIV/AIDS in Japan increased up to 2008, but has been relatively stable since then; 1 448 of new cases were reported in 2016, the majority of which occurred among men, and amongst young people under 30 (MHLW, 2016[9]). HIV incidence and AIDS prevalence are nonetheless much lower than the OECD average. The major transmission route is sexual contact; there were a few cases of HIV/AIDS reported among intravenous drug users of 0.1%, while no cases of mother-to-child transmission were reported (MHLW, 2016[9]).
Acquired immunodeficiency syndrome (AIDS), including HIV infection, and syphilis, are classified as the term “Class V Infectious Disease” as used in the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases. Under the Act, the MHLW prepares and makes public guidelines on the prevention of specified infectious diseases, such as sexually transmitted diseases and HIV/AIDs, to facilitate comprehensive prevention measures. These measures consist of three goals: (1) the promotion of public awareness and dissemination of information on infectious diseases; (2) the establishment of screening and counselling service systems via public health centres; and (3) the delivery of quality and proper medical services.
In particular since 2007, when HIV/AIDS incidence was increasing, Japan renewed the prevention measures and HIV tests at the local health centres. Specific measures include producing and distributing posters and leaflets, holding various educational events including those for World AIDS Day, producing and distributing supplemental materials distributed at school for health education, and establishing a community centre for counselling and providing information about sexual practices. Japan should ensure that information campaigns target all populations, especially statistically at-risk population groups, for example young men who have sex with men. Public health centres nationwide offer individuals HIV screening tests free of charge in an attempt to establish screening and counselling systems. Screening tests for sexually transmitted diseases are also available at local public health centres, but the fees and the subjects for screening differ according to municipalities. Sexually transmitted disease education for students has been implemented in classes for physical education, and health and physical education. HIV/AIDs treatment services are well integrated into the public health system in Japan though the network of various types of hospitals specialised in HIV/AIDS treatments. HIV/AIDS patients have access to 380 core hospitals specialised in the comprehensive treatment of HIV/AIDS at the national level, to 59 core hospitals at the prefectural level, to 14 regional core hospitals in eight regions nationwide, as well as to the AIDS Clinical Centre at the National Centre for Global Health and Medicine which offer the state-of-the-art technologies to treat HIV/AIDS treatment.
1.2.3. Risk factors
The majority of non-communicable diseases, such as cancer, cardiovascular diseases, cerebrovascular diseases and diabetes are driven by some risk factors such as obesity, tobacco and alcohol consumption, which make up the primary disease burden in Japan.
Compared to other OECD countries, rates of risky health behaviour such as drinking and smoking are relatively low. In Japan annual alcohol consumption is 7.2g, below the OECD average of 9.0g (OECD, 2017[1]). Although the average consumption of alcohol per person in Japan has decreased, the number of women consume ‘excess’ amongst of alcohol (more than 20g) on a daily basis has been increasing since 2010 (MHLW, 2016[10]). Cigarettes per smoker per day are 15.5 in Japan, lower than the OECD average of 18.4 per day. The population of smokers in Japan was 18.3% in 2015; with 30.2% of men and 8.2% of women smoking. Smoking rates are relatively low and have been declining of average, driven by declining rates of male smoking, while rates of smoking amongst women especially young women has not changed (Chao, Hashimoto and Kondo, 2015[11]; Honjo and Kawachi, 2000[12])Exposure to passive smoke is up to 42.2% at restaurants and 30.9 at the workplace (MHLW, 2017[13]).
The rate of obesity (BMI >30) in Japan was 3.7% in 2015, which is again considerably lower than the OECD average of 19.5% in 2015 (OECD, 2017[1]). Japan, however, defines obesity as having a BMI of more than 25 (studies have shown that East Asians can exhibit metabolic risk factors, such as insulin resistance, with a lower BMI than Africans and Caucasians (Kodama et al., 2013[14]). Following this definition the prevalence of obesity was 30.5% for men and 20.0 for women, and the average BMI was 23.6 for men and 22.3 for women in 2016 (MHLW, 2017[13]).
Salt consumption among adults in Japan was 10.8g per day for men and 9.2g per day for women in 2016 (MHLW, 2017[13]) which is much higher than the WHO-recommended salt intake of less than 5g per day (WHO, 2016[15]). “Dietary Reference Intakes for Japanese (2015)” sets the tentative dietary goal for salt consumption by 2020; the index recommends that men consume less than 8.0g per day of salt and 7.0g for women as the median between the WHO intake recommendation (5 g/day) and the intake (10.8g per day for men and 9.2g per day for women) in 2010-2011, while Health Japan 21 (the second term) recommends decreasing salt intake to 8g by 2022. The WHO recommends that adults consume no more than 2 g sodium/day, which is equivalent to 5 g salt/day, and that children consume less (WHO, 2012[16]). Japanese salt consumption decreased significantly in the 1970s, and has remained steady since the 1980s, and is higher compared than in other OECD countries (Anderson et al., 2010[17]; Asakura et al., 2014[18]). Traditionally Japanese food contains significant quantities salt, for instance in foods such as pickles or miso soup, with people in the northern area of Japan tending to take more salt rather than the Japanese overall average, but more recently processed food is becoming another major source of salt (MHLW, 2015[19]; Asakura et al., 2016[20]).
Outdoor and indoor air pollution is a major environmental cause of NCDs such as ischemic heart disease, stroke and respiratory disease including acute respiratory infection and chronic obstructive pulmonary disease (WHO, 2014[21]). It can also lead low-birth weight, dementia and immune system disorder (WHO, 2017[22]). It is estimated that 7 million people died due to the air pollution on the earth and this is a global burden of disease. The main outdoor pollutions are carbon monoxide, nitrogen oxide, ozone, and particulate matter (PM). PM2.5 with a smaller diameter rather than PM10 goes to deeper inside lung and cause more serious lung and circulation problems. Most of the OECD countries show higher grade of exposure to PM2.5 compared to the WHO guidelines. While the average exposure population to PM2.5 amongst OECD has decreased between 1990 and 2015, Japan shows an increased rate of exposure, from 5% to 24% (OECD, 2017[1]). The Air Pollution Control law in Japan stipulates responsibilities of each entity in implementing countermeasures for hazardous air pollutants. The Ministry of Environment monitors the level of the different types of air pollutants and gives a warning in case of detecting harmful level of air pollution (The Ministry of Environment, 2012[23]). Local municipalities also monitor pollution level, and Tokyo prefecture supports those diagnosed air pollution-related lung disease under 18 years old by the air pollution medical expenses subsidy system (Tokyo Metropolitan Welfare and Health Administration, 2018[24]). Business operators are checked by local municipalities under the air pollution health measures, and required or encouraged to reduce the emission of hazardous pollutant and to report emission exceeding set thresholds (The Ministry of Environment, 2012[23]).
1.2.4. Mental wellbeing and suicide in Japan
Suicide is a significant cause of death among OECD countries, and is a global concern. The rate of suicide in Japan in 2014 was 17.6 per 100 000 population, above the OECD average of 12.1 (OECD, 2017[1]). Although the suicide rate in Japan has shown a gradual decrease since 1998, it remains higher than the OECD average indeed, the suicide rate is steadily decreasing across OECD countries, falling by approximately 30% between 1990 and 2015. Most recently, despite an overall falling trend, suicide has increased amongst young Japanese populations.
In 2006 the MHLW established the ‘Basic Law on Suicide Prevention’, followed by a stronger measure in 2015, when the goal of reducing the suicide rate by 30% by 2026 was set. Japan’s suicide strategy is focused on improving the social issues, detecting mental disorders earlier, changing the norms and stigma around suicide and mental illness, and delivering accurate information about suicide and mental illness through the media (MHLW, 2007[25]). The MHLW has also established policies in the “Suicide Measure Outline” for preventing suicide and supporting people at risk. First, to reduce the risk of excessively long working weeks, the working hours have been regulated since 2016, a measure against harassment at work was introduced and employers are obliged to regularly perform Stress-Checks (MHLW, 2017[26]) (see Chapter 3). Second, the strategy sets out that stronger cooperation system is needed by local doctors and psychiatrists for improving early detecting of mental health disorders. Given the stigma around mental illness in Japan, the MHLW considers it important to disseminate accurate information about mental illness, including among ‘gatekeepers’ such as primary care physicians, school teachers, local health staffs and industrial health workers, who can guide the high-risk people to proper intervention by psychologists and other specialists (MHLW, 2007[25]). The Ministry of Health has also set up suicide prevention telephone ‘hotlines’ for people who needs mental support. (MHLW, 2017[27]).
Some more localised plans have also been put in place. Suicide was the biggest cause of death between people aged 20 and 39 years old in Japan in 2016 (MHLW, 2018[28]). Kyoto, where a lot of universities are located, with large population of 1.47 million in 2017, implemented a treat for suicide in 2015. Under this initiative, the universities in Kyoto created a community where students can support each other and watch out for signs of mental distress (Kyoto prefecture, 2015[29]).
1.3. Organisational Structure
Governance of the Japanese public health system is relatively fragmented: responsibilities for planning, designing and delivering services are split between central and local levels of government, between different Ministries, and between providers within the health system (for instance Public Health Centres) and private actors (notably work places and occupational physicians).
1.3.1. The Japanese Health System
Medical provision in Japan is managed by the Japanese Medical Law (Iryo Hou), which controls the establishment of hospitals and their function, Medical Plan (Iryo Keikaku), and Basic Policy for Securing Medical Delivery System (MHLW, 1948[30]). Medical Facilities are largely divided into hospitals with more than 20 beds, and clinics with less than 20 beds. There were 179 000 medical facilities in total in Japan in 2016 including dental facilities; 5% of facilities are hospitals and more than 55% is clinics. National or public hospitals count for less than 20%, and 3% for clinics, which are increasing (MHLW, 2016[31]).
The Iryo Keikaku medical plan defines the medical area (geographically) and the numbers of beds at the secondary medical area to the tertiary medical area; the secondary medical area is made up by some municipal areas, where the number of general and nursing care beds are controlled. The tertiary medical area includes a defined number of high-functioned medical institutions in prefectural units such as for mental care, tuberculosis and infectious care (MHLW, 2010[32]). Although the medical functions in each medical area are clearly defined, patients have free choice over which hospital to consult, based on their preference.
Box 1.1. Long-Term Care Insurance in Japan
As Japan’s population is aging, the number of elderly people who require support and care are increasing; Japan’s lower birth rate has also meant that there are fewer family members to assist elderly people in their care. The Long-term Care Insurance (Kaigo Hoken) Act was enacted in 1997 and came into effect from 2000 in order to support elderly people to be more independent in daily activities, offering user-oriented programmes based on the social insurance. This is not only for those over 65 years old with demands of nursing care or assistance, but also applies to those over-40 years olds who need medical care or assistance with specific chronic diseases and diseases such as terminal stage of cancer or rheumatoid arthritis (MHLW, 2018[33]).
Long-term care users are able to receive medical and welfare services at a lower cost, and they have more options from both public and private services including a home-visit service, out-patients services and admission services depending on the degree of assistance demands. There are seven categories for demands and they are certified by municipalities according to the needed support in a daily life such as eating meal, taking a bath or going to the toilet (MHLW, 2018[33]).
Source: MHLW (2018[33]). “Current Public Long Term Care System”, https://www.mhlw.go.jp/content/0000213177.pdf.
Primary care system
Most of the OECD countries have significant and well-developed primary care system to manage non-emergency care, chronic conditions, and in some countries act as a gatekeeper for secondary care, typically led by general practicioners or family doctors. In Japan, though much of the health care activity that takes place outside of inpatient settings could be classed as primary care, the vast majority of physicians are specialist or semi-specialists (OECD, 2015[34]). Primary care specialists, generalists, or specialised family doctors are not common. Instead, primary care is delivered at community clinics, and at some municipal and prefectural health centres (see (Ikegami, 2016[35]), by missed teams including physicians and nurses (OECD, 2015[34]).
This health system structure means that primary care-led management of chronic conditions such as diabetes or chronic heart disease is more challenging in the Japanese context. According to the Japan Medical Association, only 53.7% of Japanese had a personal doctor in 2014, although almost 70% of people agree to have a specific primary doctor expecting wide range of treatment and care such as health check, providing proper information about a specialist, visiting homecare and mental health care (The Japan Medical Association General Policy Research Organization, 2014[36]). Patients are not required to register with a single practice or physician, and instead can visit multiple physicians, in many cases without a referral; Japan had the second-highest rate of doctor consultations per person in the OECD in 2015 (12.7 annually per person, compared to the OECD average of 6.9) (OECD, 2017[1]).The Japan Medical Association (JMA) established a training system in 2016 to become a personal doctor who can be the first consultant for a patient as a gatekeeper and familiar with the local medicine and social welfare (Japan Medical Association, 2016[37]), but these professionals are not widespread in Japan. Since 2010 the Japan Primary Care Association has also lobbied for the establishment of a ‘primary care board’.
However, while Japan does not have a traditional primary care/General Practitioner system, in Japan employers with more than 50 employees are required to have more than one occupational doctor to take care of employee’s health and safety based on the labour safety and health law (Rohdoh annzenn eisei); employers with more than 3000 employees must have more than two full-time occupational doctors. Occupational doctors at workplace are mainly in charge of managing health condition of workers, giving advices on overworking workers, and preventing mental disorders in cooperating with a public health nurse and a sanitation supervisor at workplace (MHLW, 2017[26]). Considering the increasing demand for attention to mental health at workplace, the MHLW reset the labour safety specifications in 2015 for the occupational doctors roles; occupational physicians are now also expected to collect the specific working conditions such as over working and stress about a workers who has a problem on his/her health (MHLW, 2017[26]).
Local health centres also play an important role in delivering public health care. Local public health centres – prefectural health centres and municipal health centres – conduct medical surveillance, improve public health projects, prevent epidemic disease, investigate and analyse population statistics for communities, which are located at each prefecture, cabinet designated city, core city and other city specified by cabinet (MHLW, 2010[38]). Prefectural public health centres are responsible for conducting broad-based operations such as food hygiene and infectious diseases, while municipal health centres deal with direct businesses closer to the communities such as infant health checks, cancer screening, and health promotion. Prefectural and municipal governments set the budget for public health centres and health plan as a whole under the discussion with relevant organisations (Japanese Association of Public Health Center Directors, 2016[39]) (Figure 1.5).
Figure 1.5. Hoken-jo and Hoken-center
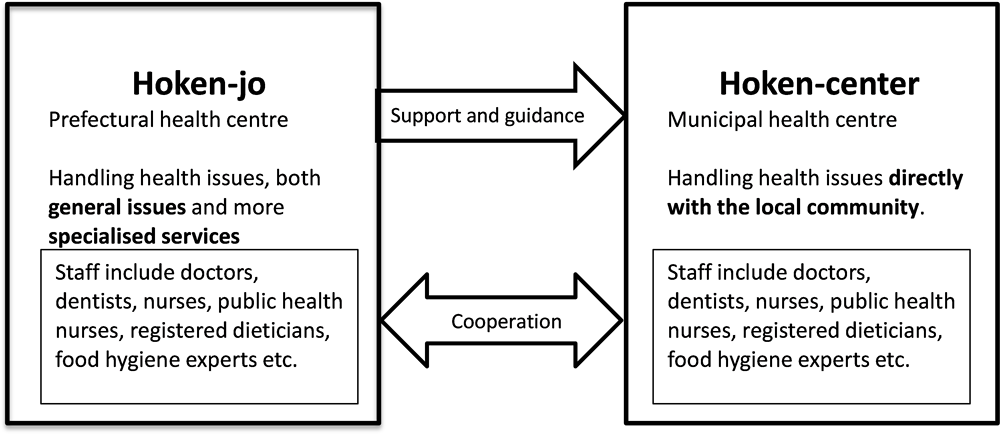
Source: Adapted from: the Role and System of Health Government in Japan, http://slidesplayer.net/slide/11365156/.
As an independent administrative corporation, some medical research centres and national hospitals specialised in cancer, cardiac disease, mental illness and paediatrics contribute to the improvement and promotion of public health by conducting surveys, research and development of technology (MHLW, 2012[40]).
1.3.2. Delivery of essential public health operations in Japan
Vaccination programmes in Japan
Vaccine administration and promotion is the responsibility of the local government, based on recommendations by the Ministry of Health, Labour and Welfare. Vaccination programmes in Japan were started by the Immunization Act, established in 1948. Some vaccinations are highly recommended for the 13 selected diseases as a routine vaccination programme based on the WHO recommendation (WHO, 2018[41]), including hepatitis B virus added in 2016. In addition, 5 vaccinations are recommended depending on health status and age as part of a non-routine vaccination programme (National Institute of Infectious Diseases, 2016[42]). Since 1994 no vaccinations are mandated by law. The vaccination guidelines are reviewed every five years and as necessary.
The central government prepares stockpiles of vaccinations, while Public Health Centres allocate vaccinations and establish vaccination prioritisation along with the Municipality and local branch of the medical association. Municipalities are mainly in charge of implementing the vaccination programmes and providing information about effectiveness and safety to citizens. Vaccination based on the immunisation law is covered by municipal voucher, yet actual expenses may be collected depending on local municipality. On the other hand, non-routine vaccination is paid by out-of-pocket (MHLW, 2018[43]).
The vaccination rate in Japan slightly exceeds the OECD average with 96% for diphtheria, tetanus and pertussis (DTP) and measles in 2015, which is scheduled at the age of one (Figure 1.6) (OECD, 2017[1]). The vaccination rate is overseen by the MHLW every year.
Figure 1.6. Percent of children aged 1 vaccinated for diphtheria, tetanus, and pertussis (DTP) and measles, 2016 (or nearest year)
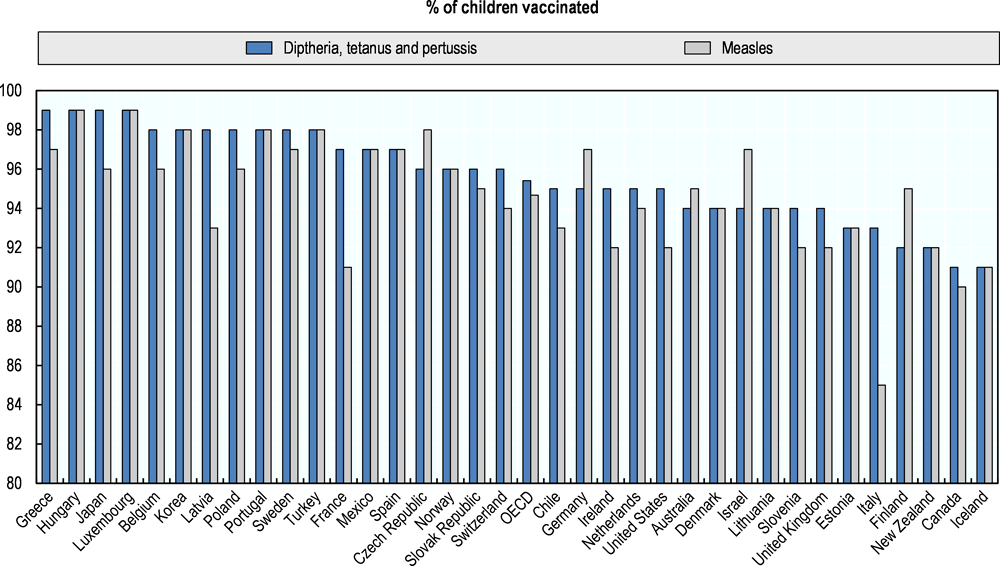
1. All data estimated. 2. Measles data estimated.
Source: OECD Health Statistics, https://doi.org/10.1787/health-data-en.
In Japan there is some anxiety around vaccinations and adverse events. The HPV (Human Papillomavirus) vaccination programme was initiated in 2009 in Japan as a part of routine vaccination programme with the expectation of reducing risk of cervical cancer, in line with a WHO review of the impact of HPV vaccinations (WHO, 2007[44]), and the initial rate of vaccination in 2012 was almost 70%. In the United States, 60% of adolescents aged between 13-17 years old received one or more doses of HPV vaccine (Walker et al., 2017[45]). National data in Australia shows that HPV 3 dose vaccination coverage for adolescents turning 15 in 2016 is approximately 77% for females and 71.6% for males (National HPV Vaccination Program Register, 2016[46]) Although HPV vaccination is recommended for females, the rate of HPV vaccination in Japan declined to 0.5% in 2015 after the Ministry of Health, Labour and Welfare withdrew the HPV vaccine recommendation in 2014. This withdrawal was followed suspicions being raised by patient organisations and some experts that the vaccination had induced adverse events such as extensive pain and movement disorders. Although the Japan Society of Obstetrics and Gynaecology declared in 2017 that there is no evidence of a link between HPV vaccination and the neurological disorders based on available research, the MHLW has not retracted its statement on the HPV vaccination, and further research is ongoing.
Food Safety Commission for food safety assurance
Food assessment and control in Japan is led by the Food Safety Commission, MHLW and the Ministry of Agriculture. The Food Safety Commission takes charge of evaluating the amount of hazardous substances such as pesticide or feed additives in food. The MHLW establishes the standards for food contents, and monitors whether the rules are complied with for domestic food, and implements quarantine tests for imported food. The Ministry of Agriculture is responsible for pesticides and drugs used on animals. Operations for evaluating quality, safety and effectiveness of chemical substances in food are entrusted to external research institutions as necessary, such as National Institute of Health Sciences.
Public Health Centres at the municipality level oversee the food safety of food suppliers such as shops, restaurants, and manufacturers. Certain types of food stores, restaurants and food industries must obtain a licence from a Public Health Centres to be able to handle food, and they must have a full-time food administrator, who conduct food hygiene and sanitary environment control under the Food Sanitation (Syokuhinn Eisei) Act (MHLW, 2018[47]). Public Health Centres conduct regular or ad-hoc on-site inspections to check building structure, water supply, food storage, and handling of food. A restaurant mainly serving alcohol needs additionally to obtain a licence from the police. In the process of food manufacturing, there are national standards for processing and cooking food. Some food has a strict manufacturing condition; raw milk and raw goat milk must be heat sterilised with 63℃ for 30 minutes or with an equivalent method (Distribution System Research Center, 2007[48]). When food poisoning is suspected, the diagnosing doctor must report within 24 hours to a Public Health Centres, after which the MHLW monitors incidence. Bacterial contamination is strictly monitored with a national standard (MHLW, 2014[49]).
Tackling Antimicrobial resistance (AMR) in Japan
AMR is now spreading worldwide as a result of misuse or overuse of antibiotics. This is a global public health concern, threatening human and animal health, and above all efficacy of antibiotics. The measure should be taken for protecting human from treatable infectious disease. The average antibiotic consumption amongst OECD in 2014 was approximately 20.5 daily dose per day (DDD) per 1 000 persons and the prevalence of antibiotics resistance was about 15%, which had increased during the previous 10 years (OECD, 2016[50]) http://www.oecd.org/health/health-systems/AMR-Policy-Insights-November2016.pdf). Japanese survey report reported that Japan used approximately 15.8 DDD in 2013 and the data reports that antimicrobial resistance for gram negative bacillus was relatively lower in the world; 17% of Pseudomonas aeruginosa and 18% of Escherichia coli (WHO, 2014[51]).
Japan Nosocomial Infections Surveillance (JANIS) was established in 2000 for early detection of in-hospital infection and had monitored the rate of antimicrobial resistance in Japan. In 2006, an amendment to the Medical Care Act was endorsed: all the medical institutes were obliged to have an infectious control committee and all staff had to participate in an educational lecture on in-hospital infectious control. According to JANIS’ 2014 report, the prevalence of Methicillin-resistant Staphylococcus aureus (MRSA) had decreased between 2009 and 2014 from 58.7% to 49.1% (The Government of Japan, 2016[52]).
Due to the growing global concern around AMR, an international action plan on AMR was adopted at the World Health Organization General Assembly in 2015. Accordingly, Japan took the measure of tackling AMR following the ‘One Health’ approach across affiliated ministries and related agencies between 2016 and 2020, including local municipality governments, medical institutes, medical and pharmaceutical association. ‘One Health’ sets out that AMR policy must take an inter-sectoral approach, considering the impact of antimicrobial use in animals, agriculture and the environment and the impact on human health. The Government of Japan set goals in the 6 fields to reduce the usage of antibiotics to 33% for humans and animals, and to reduce the prevalence of AMR in Japan for sustainability of infection control in the future: The fields are education, monitoring, infection control, usage of antimicrobial drugs, medical research, and international cooperation (The Government of Japan, 2016[52]). Education programmes are necessary not only for medical workers but also for the general population ; 2014 survey in Japan showed that more than two thirds of parents had given a medicine to their children not following the instructions, which is thought to also contribute to increased microbial resistance (The Government of Japan, 2016[52]). Amongst the member countries of WHO, only Japan is setting the numerical targets by 2020; Penicillin resistance Streptococcus Pneumoniae (PRSP) should be less than 15%, MRSA 20%.
1.3.3. Primary, secondary and tertiary prevention in Japan
Primary prevention programme with Health Japan 21
The MHLW established “Health Japan 21” as the primary strategy for health promotion and risk prevention in 2013, aiming at preventing lifestyle diseases at the national level based (Knko Zoshin) Law. This strategy includes extending the healthy life expectancy, reducing health inequality, preventing non-communicable diseases, managing supportive society, and improving healthy lifestyle, etc. Under Health Japan 21 the government set out a role for prefectural and municipal governments and local health centres. Although the government set broad targets to be achieved by 2022, the specific targets are entrusted to each prefecture based on each situation (MHLW, 2012[53]). Health Japan 21 is further discussed in Chapter 2.
Secondary prevention
Secondary prevention consists of identifying diseases at an earlier stage to enable more effective treatment and better outcomes. Screening and health checks are major pillars of secondary preventions in many OECD countries, and can be applied selectively (e.g. to a target population, based on risk and vulnerability), or to the whole population. In Japan a wide number of health checks are in place, which are detailed in Chapter 3. For example, for detecting ‘lifestyle diseases’ the Tokutei-Kenshin ‘Specific Health Check-up’ is offered to persons between 40 and 74 years old. If any irregularities are identified individuals are advised on appropriate follow-up steps (MHLW, 2018[54]).
Tertiary prevention
In many cases, if chronic diseases are well-managed, the complications of these diseases can be avoided or delayed, contributing to a better quality-of-life for the affected person and lower costs for the health system.
The approach to tertiary prevention depends on the disease. To take an example, mismanagement of diabetes can lead to various complications, such as diabetic kidney disease. There were approximately 330 000 haemodialysis patients in Japan in 2016 and it was estimated that 43.2% of new haemodialysis patients were caused by diabetes (Japanese Society for Dialysis Therapy, 2017[55]). Haemodialysis costs 400 000 Japanese yen per person per month, and the total medical cost for haemodialysis in Japan comes up to 1.57 trillion Japanese yen per year. Many municipalities have taken measures to prevent diabetic kidney disease, as it can impair patients’ health status and has a profound impact on medical expenses. In Matumoto City, Nagano prefecture, for instance, after offering preventive education to type 2 diabetes patients with the 2nd and the 3rd stage of diabetic nephropathy under the cooperation with local doctors, pharmacists and nutritionists, medication compliance. The MHLW also promotes a wide use of measures to prevent people from developing diabetic nephropathy by collecting advanced efforts made by Matumoto City and other municipalities and reporting them nationwide (Japanese Society for Dialysis Therapy, 2017[55]). In Hiroshima a particularly effective disease management effort prevent diabetic nephrology was undertaken, in which patients received self-management education from disease management nurses and were supported by the nurses in cooperation with their primary physicians (Kazawa et al., 2015[56])Efforts such as the one in Matumoto City do exist in Japan, but it does not appear that there is a national approach to chronic disease management. The government, therefore, has developed the standard disease management programme for diabetic nephropathy as a guideline for municipalities and other relevant institutions. Furthermore, while many countries rely on large primary care sectors and/or general practitioners to manage chronic diseases and prevent complications, Japan does not have a traditional primary care or GP sector (see (OECD, 2015[34]). Therefore, alternative approaches to tertiary prevention are all the more critical in the Japanese context.
1.4. Leadership and governance
While the Ministry of Health, Labour and Welfare can set the strategic direction for the Japanese health system, and has some influence over key actors in the system through a range of legislative requirements delivery of public health actions and more detailed planning are to other system stakeholders. The MHLW may need to seek ways to establish the extent to which public health actors are effectively delivering on the nationally set strategies and public health competencies, and to look for more effective ways of sharing and promoting best practices.
1.4.1. Key actors in the public health system
Japan’s health service structure has four administrative boundaries: the Ministry of Health, Labour and Welfare; prefectural governments (at public health departments); public health centres (Hoken-jo); and municipal governments of cities, towns or villages (at public health sections). The Ministry of Health, Labour Welfare (MHLW) consists of the ministry proper (honsho) which includes Minister’s Secretariat and 11 bureaus, the external organisations including the Central Labour Relations Commission, various councils, National Hansen’s Disease (leprosy) Sanatoriums, testing laboratories, and quarantine offices. The MHLW has also local branches that are made up of the Regional Bureaus of Health and Welfare and Prefectural Labour Bureaus (MHLW, 2018[57]).
1.4.2. Engagement across government
Health-related policies are diverse and coordination with other ministries and agencies is very important. The Ministry of Health, Labour and Welfare (MHLW) collaborates with other ministries such as Ministry of Agriculture, Forestry and Fisheries (MAFF), the Ministry of Education, Culture, Sports, Science and Technology (MEXT), the Ministry of Environment, with coordination by the Cabinet Secretariat. For instance, the AMR countermeasure plan was created in 2016 in the Ministerial Meeting on Infectious Disease Control Measures, which needed cooperation mainly with the MEXT, the MAFF, Ministry of Foreign Affairs. In this countermeasure, the MHLW takes the central role and the responsibilities of each ministry and agency are decided according to the purpose. They established each part of plans working with other partners including Ministries and independent administrative agency such as National Institute of Infectious Disease, National Centre for International Medical Research, and local health centre (The Government of Japan, 2016[52]).
For tobacco control, there is a tobacco control ministries liaison conference with more than 10 ministries involved including the Metropolitan Police Department and Ministry of Finance and the Ministry of Environment, the Ministry of Economy, Trade and Industry (MITI), etc. (MHLW, 2004[58]). However, this liaison conference has not been held since 2014.
Other examples of cross-government coordination include:
With the MEXT, the MHLW created a council and three subcommittees: the Education and Labour Policy Subcommittee, the Childcare Support Measures Meeting Subcommittee, Education, Child Welfare and the Social Security Measures Subcommittee, and conduct practical consultations. The MAFF has established the Shokuiku Promotion Meeting, comprised of experts and related Ministers. This meeting promotes the Basic Program for Shokuiku Promotion (Syoku-iku Kihon Keikaku) to improve population knowledge of diet and understanding of how to make more appropriate food choices
Regarding food safety management, the Food Safety Committee performs the general risk assessment, with the MHLW and the MAFF cooperating to decide regulation for each risk related to food hygiene, and agriculture, livestock and fisheries respectively based on the assessment (Food Safety Commission of Japan, 2016[59]).
The MHLW works with the Environment Agency for reduction of CO2 from industries with other Ministries such as the National Land Ministry of Transportation and the MITI (The Ministry of Environment, 2017[60]).
However, when it comes to public health policy, and health policy in general, cross-government coordination does not appear to be systematic or a priority in Japan. Some initiatives are undertaken between Ministries, but the different roles of Ministries in developing high-level strategies such as Health Japan 21, for instance, are unclear. When confronting public health challenges, or improving population health in the broadest sense, consistent cross-sectoral engagement is critical, as Finland (see Box 1.2) has found. Challenges around good cross-governmental working seem to be found in other areas of health policy, for instance planning for emergencies, as well (see Chapter 4). There is also a risk that weak cross-government collaboration is reproduced at the local level, which would not be uncommon compared to other countries. For instance, some prefectural administrations in Japan have suggested that lowering silos within the government took a concerted push, and strong leadership from the prefectural leadership. It does not appear that the MHLW offers any guidance to at present to local government to collaboratively deliver on public health expectations.
Box 1.2. Joined-up government in Finland
In Finland, a ‘Health in All Policies’ approach has been put at the centre of health policy making for close to half a century. Such an approach emphasises that decisions and policies made in areas outside of traditional health policy making – around transport, agriculture, education, employment, etc. – have a significant impact on citizens’ health, and on the delivery of services by the health system. In Finland the Health in All Policies approach therefore demands that all sectors of government keep health concerns at the forefront, are kept accountable for policies impacting health and health care, that pro-health inter-sectoral action is prioritised, and that policy makers, politicians and the public across all sectors are informed about how decisions they make will affect health and health systems.
This cross-sectoral focus in Finland in fact began with a desire to improve public health, starting with a focus on improving nutrition, reducing smoking, and reducing accidents. This approach has been promoted both at the WHO and in EU-level work, for example during Finland’s EU Presidency in 2006 they adopted ‘Health in All Policies’ as the theme for work on health. At the Finnish level, work has evolved from addressing single health problems such as accidents, to larger scale programmes, to the introduction of legislation, broad objectives, and Governmental inter-sectoral programmes. A cross-governmental approach is seen, for example, as having been key to the halving of overweight and obesity rates amongst five-year olds. To improve the nutrition of Finnish children, and reduce overweight, municipal health departments, urban planning departments, schools and day care worked together. Each actor played a part: the urban planning department improved school playgrounds, more physical activity was introduced in schools, sugary snacks were replaced by healthier school lunches, and the health department focused on parent education on healthy eating.
In addition, cross-governmental cooperation is pursued around specific health risks, for example diabetes. In a preventive strategy coordinated by the Finnish Diabetes Association, the Ministry of Education and the Ministry of Social Affairs and Health came together to prevent diabetes, support high-risk populations, and deliver early diagnosis and management for newly diagnosed diabetics. The Ministry of Education took responsibility for managing the health-care system and non-governmental organisations such as Finnish Centre for Health Promotion and schools for children. The Ministry of Social Affairs and Health was in charge of setting up support from the national network of nutritional-education and weight-management services (Finish Diabetes Association, 2003[61]).
Source: Melkas, T. (2013[62]), “Health in all policies as a priority in Finnish health policy: A case study on national health policy development”, Scandinavian Journal of Public Health, Vol. 41/11_suppl, pp. 3-28, http://dx.doi.org/10.1177/1403494812472296; Leppo, K. et al. (2013[63]), Health in All Policies, http://www.euro.who.int/__data/assets/pdf_file/0007/188809/Health-in-All-Policies-final.pdf; Finnish National Institute for Health and Welfare (2016[64]), Health in All Policies – Health promotion – THL, https://thl.fi/fi/web/health-promotion/health-in-all-policies; WHO (2015[65]), Finland curbs childhood obesity by integrating health in all policies, World Health Organization, http://www.who.int/features/2015/finland-health-in-all-policies/en/.
1.4.3. Regional and local public health leadership
Japan has a decentralised administration, and municipalities and local governments are responsible for playing the central role of implementing policies on education and health and welfare services, including for public health. Basic protocols and legislation are set by the central government, and local government (prefecture or municipality) must follow the mandated legal frame set by the upper legislative hierarchy (for instance, a municipality must follow directives set by MHLW and relevant prefecture office). The central regulation and local implementation should ensure minimum requirements across municipalities.
The public budget is often a mix of municipality’s own budget with a subsidy from prefecture level, and central government level. For example, long-term care insurance is operated by the municipality (or alliance of municipalities) and is half financed by premiums from municipality beneficiaries, and the rest is covered by the central government (25%), prefecture level (12.5%), and municipality (12.5%).
Local governments develop public health programs that attach importance to their local characteristics and meet the needs of local residents. This process provides local residents with opportunities to be involved in their own communities and become responsible for the maintenance and improvement of their own health.
Figure 1.7. Structure of health service delivery and planning in Japan
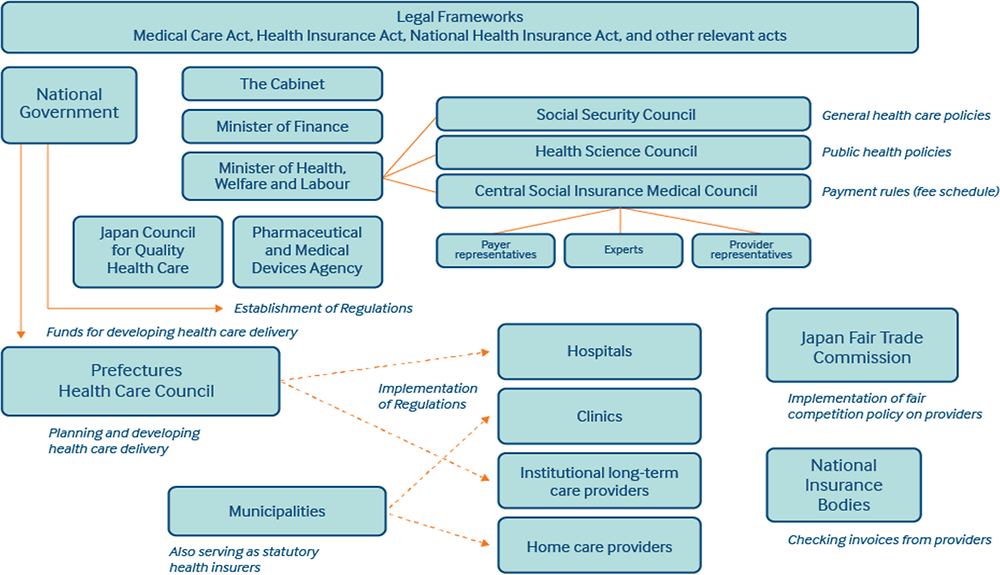
Note: This figure gives a simplified representation of the structure of the Japanese health system.
Source: Ryozo Matsuda (2017[66]), “Japan: International Health Care System Profiles”, in The Commonwealth Fund: International Health Care System Profiles, The Commonwealth Fund, https://international.commonwealthfund.org/countries/japan/.
Based on the guidelines of the Ministry of Health and Welfare, each prefecture establishes a Medical Plan in consultation with relevant professional associations (e.g. the Japanese Medical Association), and with some community and patient representative organisations at the local level to reflect local medical condition and need. Under the Medical Law enacted in 2007, the medical collaboration system was introduced for each of four diseases (cancer, cerebro vascular disease, acute cardiac ischemic disease, diabetes) and 5 projects (emergency medical care, disaster medicine, remote medicine, perinatal care, paediatric medicine including paediatric emergency medicine). In 2013, mental illness and home health care were added: “5 diseases, 5 projects and home care medicine” is promoted with this system, as is cooperation with neighbouring prefectures to secure medical care in the area around the boundary of the prefecture (MHLW, 2017[67]).
In this structure, where considerable independence is given to municipalities, there is clear potential for excellent examples of practices to develop. For example, Kanagawa–prefecture has developed a comprehensive healthy aging strategy (see Box 1.3); Adachi City has introduced a Health Japan 21 strategy which can be considered close to international best practice (see Chapter 2).
Box 1.3. Me-Byo Project in Hakone, Kanagawa-prefecture
There is a local municipality which performs active implementations in the east of Japan. Kanagawa–prefecture shows its positive action by joining the WHO’s global programme, ‘Age-friendly Cities’, which aims to create comfortable communities for elderly people to live in (Kanagawa Prefecture, 2018[68]).
While Hakone-city, one of the cities in Kanagawa-prefecture, plans the clear vision for the aging society, which influences widely on the government’s measure. This project is now implemented at the prefecture level.
Me-Byo is an invented word meaning preventing diseases and managing healthier status even with a health issue. In an aging society, living without any health issue might be difficult, however, people can obtain healthier status even with a health problem.
Kanagawa-prefecture takes a measure for tackling an aging society called ‘Healthcare New Frontier aiming at an active society where all the generation could live healthy lives even at the age of 100. They insist on the importance of the four main achievements, being aware of each role in a society as an individual, a professional, researcher, a municipality, and a nation;
1. Visualising the risk and current situation in order to prevent a disease,
2. Developing human resource for leading the local health activities and innovations,
3. Promoting the data management for the better products and services,
4. Changing the behaviour for better lifestyle and health literacy.
The plan is based on the two main concepts; 1. Improving the health status by preventive intervention such as keeping motivation and changing behaviour for healthier lifestyle. 2. Doing practical research and development of the latest medical technology . For example, Kanagawa-prefecture plans to promote working circumstance at a company to improve health satisfaction among the workers, and building an educational institute which takes part in improving a human recourse in the future (Kanagawa Prefecture, 2018[68]).
In 2017, Kanagawa-prefecture held a conference to establish concrete solutions to these achievements (Kanagawa Prefecture, 2018[68]). Although evaluation method is necessary, it is expected that they would proceed a countermeasure against the aging society ahead the other prefectural administrations.
Source: Kanagawa Prefecture (2018[68]), Collaboration with WHO, http://www.pref.kanagawa.jp/docs/mv4/cnt/f537393/p1104811.html.
In Japan’s decentralised administration local responsibility for public health delivery is clearly key. It is possible, however, that some municipalities have robust public health programmes and others may have weaker ones. In addition, it is possible that some centrally set expectations actually hinders competition and efficient use of local resources across and within municipalities.
The challenge in Japan is that it is difficult to understand which municipalities are delivering high quality and comprehensive public health policy, and which municipalities are struggling; some information, for example copies of municipal strategies and some indicators, is held by the MHLW but this is not publically available. Nor does the central government appear to have a particularly strong role in supporting or strengthening the approach of ‘under-performing’ municipalities. At present, the main mechanism that the Ministry uses to promote best-practice examples is through ‘awards’ which are published on the Ministry website. In terms of introducing greater national coherence to the public health sector, and strengthening central leadership, it may be that strategies set are too broad which leaves local levels of government to choose from a selection of different areas on which to focus activities. While this can be a good way to allow local government to be responsive to local context and local needs, it may also contribute to an uneven package of public health activities across the country. While minimum expectations for local authorities and private actors are set in different areas of public health are set (through the various legislation for instance), it is not clear that there is a strong mechanism for checking that these minimum standards are set.
In addition, despite the strongly decentralised system, Japan does not have a good system for sharing best practices and promoting exchanges, especially between local-level authorities. Occasionally the MHLW has taken best practice examples from local settings and applied them to legislation, for example the co-payment reduction for elderly medical care which was begun by a rural municipality, and then adopted to national legislation in 1973. The MHLW has held meetings about 8 times a year since 1999 to exchange information and opinion among municipal staff and the staff of the MHLW for improving health and welfare services according to local characteristics and planning methods (MHLW, 2018[69]), but neither the municipalities nor the MHLW report examples of cross-learning across municipal or local governments. This seems like a major missed opportunity to spread best practices nationally, and for weaker municipalities to learn from stronger ones. Best practice examples are also usually showcased in narrative reports, rather than through empirical evaluation of processes and/or outcomes, which precludes municipalities from extracting lessons from the best practice case to be applied to their own local conditions.
It may be, firstly, desirable for the MHLW to look for more robust ways to support less highly performing prefectures/municipalities to take up best practices; it is not clear that there is a strong mechanism for checking that centrally defined minimum standards are met by each municipality. While the strict decentralised organisation of the Japanese system and the autonomy of municipalities must be respected, a more active supporting role by the MHLW for under-performing municipalities could be envisioned. Secondly, encouraging local governments to exchange ideas and discuss common issues and challenges around public health (and health in general) seems desirable – other decentralised OECD countries have Association of Local Authorities and Regions, for instance in the Nordic countries, or in Italy – which can serve this function (see Box 1.4). The way in which Finland uses a nationwide benchmarking tool is particularly compelling. In Japan an annual conference for local government focused on public health – for instance focused on Health Japan 21, or the Smart Life Project – might be the place to start. Such a conference could promote informal dialogue between regions, and could also highlight best practice examples from municipalities, or perhaps include an award ceremony for examples of excellence.
Third, the MHLW should better use existing monitoring systems and statistics for empirical evaluation of policy successes and shortcomings. The MHLW could support local government to adopt data-driven monitoring, policy-evaluation and policy-making through central legislation and/or targeted subsidies. In Finland the public data portal that benchmarks local public health performance shows top performers, and those with room to improve (Box 1.4).
Box 1.4. Cross-region learning in decentralised health systems: Finland, Italy and Sweden
Decentralised health systems are not uncommon in OECD countries. In order to facilitate the sharing of best practice between regions, and to benchmark performance, some countries have established associations of regional and local authorities, and/or annual events to gather together representatives of local government.
Finland launched a nationwide benchmarking tool called TEAviisari in 2010 to evaluate the health promotion activities delivered by its 297 municipalities (Saaristo, 2017[70]). The National Institute for Health and Welfare collects data on 810 individual indicators every two years. These indicators are presented in an online tool, where they can be analysed and compared at the municipal, regional or administrative level.
The tool assesses Health Promotion Capacity Building, focusing on seven dimensions: commitment, management, monitoring and needs assessment, resources, common practices, participation and other core functions (Saaristo et al., 2018[71]). For each dimension, municipalities receive a score between 0 and 100, with 100 indicating a desirable quality.
While the tool was primarily designed to increase the accountability and transparency for municipalities, the data also serves other purposes. It is used to monitor the implementation of the Health Care Act and the Act on the Promotion of Sports and Physical Activity (Saaristo, 2017[70]). The data is also used to determine whether or not municipalities qualify for a “health promotion incentive” – accounting for 2.5% of the national municipality budget.
In Italy, the National Agency for Regional Health Services (AGENAS – Agenzia Nazionale per i Servizi Sanitari Regionali) acts as a scientific and technical body of the Italian National Health service, and acts to support health care planning at the national and regional levels (OECD, 2015[72]). For example, AGENAS compares costs and efficiency of health services, promotes quality, seeks to spread health innovation and experimentation with new models of care. AGENAS is jointly accountable to the Italian health care regions, and the Ministry. Maintaining high standards across the regions, including through benchmarking of regional performance through comparable indicators, accreditation, and surveillance of medical education are other roles.
In Sweden, the Swedish Association of Local Authorities and Regions (SALAR) represents Sweden’s 290 municipalities and 20 county councils/regions (SALAR, 2018[73]; OECD, 2013[74]). Membership to the Association is voluntary, but SALAR can act as a powerful advocacy voice representing the local governments at the central and European level. SALAR strives to promote and strengthen local self-governance, and also provides local governments with practical support and advice. When it comes to health, SALAR takes a leading role in benchmarking activities amongst the regions, publishing quality registers, and more than 150 indicators of health care quality and efficiency. SALAR has also collaborated with national bodies, for example the National Board of Health and Welfare, to produce thematic reports and studies.
Source: Saaristo, V. (2017[70]), TEAviisari, a tool for benchmarking health promotion capacity building in Finland, http://www.eurohealthnet-magazine.eu/ehn-magazine-8/teaviisari-a-tool-for-benchmarking-health-promotion-capacity-building-in-finland/; Saaristo, V. et al. (2018[71]), “The comparative and objective measurement of health promotion capacity-building: from conceptual framework to operationalization”, http://dx.doi.org/10.1177/1757975918769608; SALAR (2018[73]), About SALAR – SKL, https://skl.se/tjanster/englishpages/aboutsalar.995.html; OECD (2015[72]), OECD Reviews of Health Care Quality: Italy 2014: Raising Standards, https://dx.doi.org/10.1787/9789264225428-en; OECD (2013[74]), OECD Reviews of Health Care Quality: Sweden, https://doi.org/10.1787/9789264204799-en.
1.4.4. Leadership from Japanese civil society
The Japan Medical Association, and its regional branches, have an influential role in the governance of the Japanese health system. The JMA contributes to local Medical Plans, setting concrete numerical targets, and then local municipalities are responsible for the promotion and implementation of medical plan for citizens based on prefectural medical policy. The medical plans, and progress made, are reported to the MHLW every year especially for “5 diseases, 5 projects and home care medicine” (MHLW, 2017[67]).
However, aside from the involvement of the JMA – representing physicians – Japanese civil society is notably absent from the public health sphere. For example, civil society do not appear to be systematically consulted when municipalities develop public health strategies (although this could happen on an ad-hoc basis). Nor is the MHLW obviously engaging civil society groups in the Health Japan 21 strategy.
It may be that the civil society voice in the health space – including around public health – is relatively under-developed in Japan. There are a small number of actors, for example the HGPI. The Health and Global Policy Institute (HGPI) is a Japanese non-profit think-tank established in 2004 conducting medical policy survey and research, information exchange, human resource development with the aim of presenting policy options for citizen-based health policy. They work with various stakeholders, such as clinical doctors, medical journalist, public health professionals, and politicians, to seek feasible policies, while keeping a politically neutral position. Their activities include providing policy lectures to those with high interest in policy, performing surveys on Japanese public opinions and suggesting a recommendation on specific issues in Japan, for instance about dementia and cancer (Health and Global Policy Institue, 2018[75]).
The MHLW should seek out dialogue with civil society groups systematically, and especially when designing and assessing major strategies such as Health Japan 21; in time regular engagement by the MHLW could improve the confidence of nascent patient and citizen groups. Some other OECD countries have a diverse range of groups with different focuses in the public health space, even if in general engagement of civil society is not a main pillar of efforts to improve public health. In general, reflecting and collecting patients’ views is understood to be a priority part of a people-centred health care system (OECD, 2017[76]). Japan should seek to systematically include patient’s voices in policy making and any performance assessment or evaluations that are undertaken, either through inclusion of civil society or patient groups, through collection of patient-reported indicators of care experiences or outcomes, or both.
1.5. Partnerships and collaborations
1.5.1. Engagement with patient groups
Many patient associations in Japan mainly support patients to with learning and knowledge-acquisition related to diseases they suffer from, and peer-support in a group settings. Such groups are mostly made up of members with same diseases such as breast cancer or lung cancer, or similar health conditions such as chronic status with a respirator. “Baku-baku no kai” is one of the patient associations in Japan for patients with ventilator and their parents founded in 1990. Currently, there are 500 members nationwide, and this association is supporting families for the patients to live with their goals in the society, and appealing the necessity of enriching regional support (Baku-baku no kai, 2018[77]). Another organisation in Japan, called the National Federation of Mental Health and Welfare Party “Minna (mi-n-na) Net” was established in 2006 to contribute to independence of mentally disabled people and promotion of social participation. They provide consultation support for people with mental disorders and their families, and research on social participation of people with mental disabilities, to promote the welfare of mentally disabled people and their families. They organise all the 47 prefectural-based association and support their regional events. There are limited exemption supports of transportation expenses for patients with mental disorders in Japan and this organisation created a petition and signed campaign to reduce the economic burden of patients and their families in 2015 (The National Federation of Mental Health and Welfare Party, 2018[78]).
Japanese patient groups formally engage with the central government in various policymaking processes. A number of regulations mandate that representatives of patient groups take part in of councils and committees sponsored by the MHLW to discuss relevant policies. Under the Cancer Control Act, for example, the following is stipulated, "Article 10 (2) The Minister of Health, Labour and Welfare requires to hear the opinions from the Heads of relevant administrative agencies and Cancer Control Promotion Council the in designing the Basic Plan to Promote Cancer Control Program. Article 25 The Cancer Control Promotion Council shall be organized within 20 members. The members of the council shall be appointed by the Minister of Health, Labour and Welfare from among cancer patients, their families, their bereaved families, those engaged in cancer medical and experts with academic experience." Some patient associations do try to send a patient’s representative as a stakeholder to a conference for the development of treatment guidelines or medical projects, but this does not appear to be systematic (MHLW, 2015[79]). However, there are a large number of small non-governmental organisations in Japan, about half of which are working in the health and welfare space, including around public health issues (see Box 1.5) (Cabinet Office, 2018[80]) (MHLW, 2010[81]). The MHLW has formally recognised the importance of working with such groups, but it does not appear that the groups engage with local governments on any systematic basis.
The engagement of patient groups in the public health sphere can be more challenging, as many patient groups are as in Japan focused on advanced or established diseases, rather than preventive activities. However, patient involvement is increasingly seen as a fundamental necessity for policy making in OECD countries, especially at the national level. In OECD countries such as Australia, Norway, Sweden and the United Kingdom there is national legislation that gives a formal definition of patient rights and patients and service users are also systematically involved at the service level or the decision-making level. Some organisations in OECD countries have well-established two-way cooperation between medical providers and patient groups in making decision on health care system. In the United Kingdom, for instance, requirements for the development of clinical guidelines by the National Institute for Health and Care Excellence (NICE) include at least 2 lay members who have personal experience of using health care or care services as participants to the drafting process (NICE, 2014[82]).
Box 1.5. A Japanese NGO tackling alcohol addiction
Alcohol addiction can be a major challenge for affected individuals, and can lead to further serious short and long-term health issues. Additionally alcohol-related problems are highly likely to affect not only the addicted person also the people around them such as family and friends (MHLW, 2006[83]). Alcohol-addiction and harmful alcohol can also contribute to third party harm such as traffic accidents.
ASK, a Japanese non-governmental organisation, was established in 1983 to increase the awareness of the risks of alcohol addiction, and to aim for a society which can support those who recover from addiction. ASK’s activities are raining awareness of risks caused by alcohol, organising group activities for preventing binge drinks and promoting alcohol related disorders basic law, etc., suggesting the health policies about alcohol, developing human resource, doing research about the drinking habit among teenagers to raise a social issue and supporting the patients with alcohol related disorders and their surroundings.
ASK supports, for instance, families who have addicted members, and also give some lectures and offer programmes for training supporters such as medical staffs, educators and leaders in a community. ASK also has worked with the government to address some problems around drinking, for example in 1986, ASK asked the Ministry of Education to have preventive education programmes on alcohol at school for teenagers. There are lectures for preventing alcohol, smoking and substance use since 1989 at elementary school to high school (for students aged between 6 and 18 on average). Another request was made to the government and alcohol companies to attach warning signs on alcohol beverage to prevent pregnant women from drinking alcohol in 2003. The MHLW has created a guideline for this, and alcohol consumption amongst pregnant women has fallen in 2013 compared to 2010 although the rate of drinking population amongst women increased (National Institute of Health and Nutrition, 2016[84]).
ASK’s activity has since broadened to preventive actions for multiple addictions including substance addiction, gambling addiction and internet addition (ASK, 2018[85]).
Source: MHLW (2006[83]), Prevention of Drinking Behavior and Related Problems, http://www.mhlw.go.jp/topics/tobacco/houkoku/061122b.html; National Institute of Health and Nutrition (2016[84]), Health Japan 21 Assessment, National Institute of Health and Nutrition, http://www.nibiohn.go.jp/eiken/kenkounippon21/kenkounippon21/dete_detail_05.html#04_03; ASK (2018[85]), Welcome to ASK's website!, https://www.ask.or.jp/english.
1.5.2. Partnerships with the private sector
The private sector in Japan plays a particularly important role in promoting public health, for several possible reasons. First, because of the structure of the health insurance system a large number of companies have direct responsibility for the health of their employees. Second, given the strongly decentralised nature of health policy implementation in Japan the MHLW relies heavily on companies to deliver public health interventions in the workplace. And third, it appears that Japanese companies are particularly engaged with notion of workplace wellbeing and many are organising interventions in this sphere. Healthy workplace practices in companies are reputed to be a key recruitment tool, and a way for competing companies to attract top graduates.
The Ministry of Health and Welfare has significant programmes which encourage health promotion in workplaces. Health Japan 21 and the Smart Life Project encourage workplaces to prevent health lifestyles – increased movement and exercise, eating more healthfully, smoking cessation for example – and the Smart Life Project has an awards programme that recognises workplaces who have introduced commendable initiatives. Additionally, under occupational health and safety laws set by the central government, employers are mandated to provide health check-ups (see Chapter 3), and preventive measures for safety, including the provision of an occupational physician for all companies with over 50 employees.
However, since the provision of an occupational physician applies only to large companies, around half the workers in Japan are not covered under the law. For the small business sector, the Japan Organization of Occupational Health and Safety (under MHLW labour bureau) provides regional occupational health centres to support occupational health prevention for small business.
The Ministry of Economy, Trade and Industry (METI) has also been focused on improving health as a means of boosting workplace productivity, and working with the Tokyo Stock Exchange has developed an awards programme for large companies (listed on the JPX) which have done the most to promote a healthy workplace and healthy employees. The approach was expanded in 2017 to a broader programme which surveys and recognising excellent ‘Health and Productivity Management (HPM)’ organisations, including in smaller companies (‘major enterprises’ and ‘SMEs’). Companies volunteer themselves for the programme which, while showing that a large number of companies see HPM practices as important, risks drawing out only the top performers.
Building off of the other efforts by the MHLW and METI, the Japan Health Conference (Nihon Kenko Kaigi) is an organisation fully supported by the government to promote healthy life expectancy and appropriate health care in Japan. The conference encourages private organisations such as economic organisations, health care organisations, insurers and local governments to take measures to improve health status among their workers. In 2018, the Japan Health Conference, with the support of MITI , honoured companies which practice excellent health management. The Conference also develops guideline to promote healthier working practices, and educational materials about prevention, primary care, health insurance and medical information. The ambition is that by 2020 small-scale organisations, such as companies and local communities , to function on health promotion independently. (MITI, 2018[86]).
The engagement of companies in Japan with promoting health behaviour and the strong emphasis that the MHLW and METI put on workplace responsibility can be seen as an example of broad stakeholder engagement with public health concerns in Japan. However, existing programmes – the METI and TSE awards, the Smart Life Programme – reward top-performers, while companies that are less engaged with workplace health are far less visible. In a differently structured health system this might be less of a challenge, but given the strong reliance on employers and workplaces as key actors in delivering public health interventions in Japan, the risk is that only a small part of the population are benefitting.
1.6. Financial resources
1.6.1. Spending on health and public health
Estimated national health expenditure in Japan per capita was USD 4 519 in 2016, situating Japan as one of the highest spenders on health in OECD (OECD, 2016[87]). The ratio to gross domestic product (GDP) (Figure 1.8) was an estimated 10.9% in 2016, higher than the OECD average of 9.0% (OECD, 2017[1]). Looking at the medical expenses by age group, elderly people aged 65 years or over accounted for almost 60% of expenditure in 2015 (MHLW, 2015[88]).
Figure 1.8. Health expenditure as a share of GDP, 2017 (or nearest year)
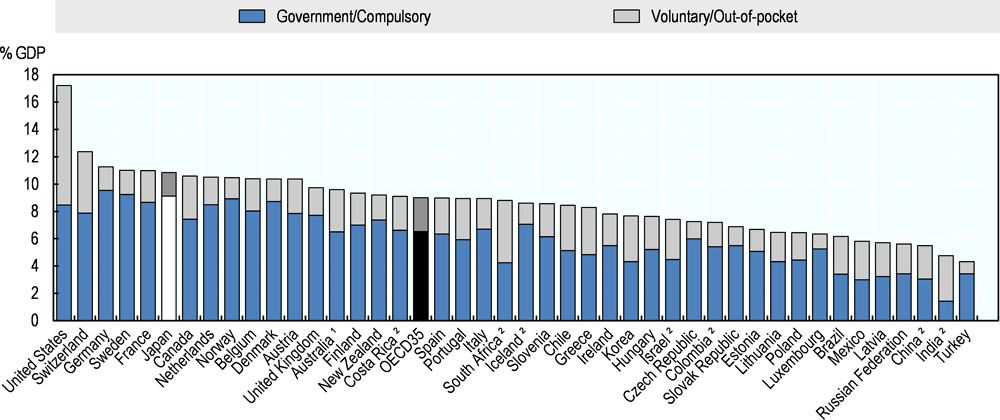
Source: OECD Health Statistics 2018, https://doi.org/10.1787/health-data-en; WHO Global Health Expenditure Database.
National health expenditure in Japan is covered by central government, municipal governments, health insurance and out-of-pocket payments; in 2015 38.9% was covered by the public funds (25.7% by the central government and 13.2% by the local government), 48.8% by health insurance (20.6% employers and 28.2% the insured), and 11.6% by patient’s out-of-pocket Overview of the National Health Care Fee in 2015 (MHLW, 2015[88]).
Public spending on public health is used for activities including health check-ups, vaccination programmes, infectious disease such as treatment of tuberculosis and sexual transmitted diseases, maternal health and some care for those with mental disorder, and for those who harmed by public pollution (MHLW, 2015[89]) Responsibility for funding particular areas of public health services vary: for example, the expenses for specific health check-up, excluding a co-payment, are covered by the central government, prefectural government and municipal governments (cities, towns, and villages), each paying one third, as set out under Article 72-(5) of the National Health Insurance Act. Article 20 of the Act on Assurance of Medical Care for Elderly People provides that the insurers carry out specific health check-ups (tokutei-kenshin) for the insured aged 40 and older.
Under the Employee’s Health Insurance (EHI) programs, the contributions, which are collected by the insurers (providers) from the insured, cover the expenses for benefits, part of the contribution is allocated to the expenses for specified health check-ups. Insurers are obliged to provide specific health check-ups and specific health guidance to the insured and the non-working dependents who are aged between 40 and 74. Prior to 2008 employers or municipalities were responsible for the provision of such check-ups.
No tax resources are earmarked for public health programs, but some major programmes are financed by the central government budget, or by municipalities, or both. These include:
Vaccination programs: the central government has the office for vaccination programs at Health Service Department, Health Service Bureau of the MHLW. A total of 1741 municipal governments nationwide are responsible for the implementation of routine vaccination programs. Routine vaccines for babies and children are offered at no cost by most municipalities. For immunisations that can prevent individuals from developing a disease or from worsening disease conditions, part of the cost may be covered by some municipalities;
Health promotion programs implemented by municipalities under the Health Promotion Act: The central government finances part of the expenses paid by prefectural governments earmarked for the health promotion programs that are implemented by municipalities, and finance part of the expenses required for Designated Cities to implement these programs;
Cancer screenings implemented by municipalities: most cancer screenings are financed by grants to local government
The central government also helps finance only the public health programs that are particularly designed to improve health, but local public health programs are mainly financed by municipalities.
1.6.2. Some payment mechanisms exist to incentivise public health functions amongst key providers
An amendment was made in 2015 to the National Health Insurance Act to establish a sustainable health insurance system. The Amended Act obliges insurers to make efforts to perform health promotion activities necessary to enhance the health of the insured, besides specific health check-up and specific health guidance. The MHLW created the concrete guideline in 2016 for insures to incentivise the insured at workplaces (MHLW, 2017[90]) On the other hand the government decided a mechanism to evaluate insurers' achievement, which incentives insurers who are tackling specific health examination, specific health guidance, health prevention and promotion. Insurers receive a penalty (by being charged with additional amounts in subsidies that are paid by insurers and taken into the programs for those 75 and over organized at prefectural level) when they show a low rate of receiving health check-up among the employees, and are incentivised (by earning reduced amounts in subsidies for the programs for those 75 and over) when they increase the rate of health check-up receivers and encourage employees for health prevention and better healthy behaviours in order to optimise health care spending (MHLW, 2017[91]).
Japan has experimented with a small number of programmes that offer financial or in-kind incentives to citizens undertaking healthy behaviours. There was a pilot study in one of the cities in Shizuoka prefecture, through an initiative started by the municipal governments, where the citizens can get benefits from shops supporting the health promotion programme by practicing health exercise and health check-up. People can receive some coupon for shopping at local shops when they follow a ‘healthy life’ for two weeks, for example exercising, eating healthy meals, undertaking a health check etc. The coupons are offered through the cooperation of companies and stores in the city, while no public expenditure was used for this incentive system. (MHLW, 2017[92]).
1.7. Knowledge development
1.7.1. Key data sources for understanding public health
Japan has some rich sources of public health data, including data from health checks, from public municipal data, health insurance data, data drawn from institutions, and surveys. The National Survey of Health and Nutrition for example has existed for 70 years and is a best practice model that other OECD countries could follow (Box 1.6).
However, linking data from different data sources is challenging. Problems with linkages mean, firstly, that data does not follow the individual if they change employment or insurance provider, and secondly that there are limits to how data can be exploited within the system. For example, health check data could be used more fully (see Chapter 3), and data on screening is collected but not centralised.
There are some signs of planned efforts to link data to improve understanding health care use, for example the MHLW is planning to initiate the Data Health Plan in 2020 based on the Act on Assurance of Medical Care for Elderly People to decide and assess the proper medical expense by collecting the medical receipt data and information of specific health check-up and specific health guidance, which counts more than 14 billion cases and 220 million cases. These data have been provided to a third party since 2013 for improving the quality of medicine and promoting evidenced based medicine (MHLW, 2018[93]).
In addition, discussion of having a unique patient identifier are ongoing (social security number is used for taxes) – in Japan’s relatively fragmented system (especially in this case the many insurers) having a UPI would be an advantage when it comes to disease management.
Box 1.6. The National Survey of Health and Nutrition
The National Institute of Health and Nutrition has existed almost for 100 years and been in charge of analysis of the national health and nutrition survey conducted by the MHLW and technical support for the research by not only the central government and municipalities to make the better health policies including Health Japan 21 (National Institute of Health and Nutrition, 2018[94]). The survey samples about 15 000 citizens annually to document their health and nutrition characteristics and behaviours. The survey is also used to monitor the Health Japan 21 strategy; to correspond with the baseline, interim and final assessments of the second term of HJ21, expanded surveys were or will be conducted in 2012, 2016, and 2020, covering a larger number of districts and triple the sample.
The survey gives very detailed information on the health and habits of the population, and can also be used to compare regions within Japan. The survey includes a physical examination (height, weight, abdominal circumference, blood pressure, blood test), a medical interview, and questions about exercise. The dietary survey includes meal classification for each family member, information about total food intake, and a lifestyle habits questionnaire (eating habits, exercise, rest, alcohol intake, smoking, dental health). The protocol for following the survey, which is undertaken by teams including physicians, registered dieticians, public health nurses and clinical laboratory technicians and clerks, are clearly set out in significant detail.
The regular undertaking of this survey means that detailed trends, broken down by region, can be tracked over time. For example, over the past 70 years meat intake has increased significantly while fish intake declined from the late 1990s; daily steps taken appear to have done down over the past two decades, salt intake has declined slightly, while the prevalence of underweight has increased amongst Japanese women (20-69 years) since the 1980s. This survey is a particularly powerful tool in understanding the health status of the Japanese population, and can help track the impact of policies targeting behavioural change.
Source: National Institute of Health and Nutrition (2018[94]), National Institution of Health and Nutrition, http://www.nibiohn.go.jp/eiken/.
1.7.2. Promoting health literacy around public health
Based on the Health Promotion Law (Kenko Zoshin Hou), stakeholders such as the government, prefectures, municipalities, and medical institutions are expected to cooperate to provide health education for promoting health literacy in Japan. The MHLW has created a website for patients and health workers, called ‘“Information site for evidence-based Japanese integrative Medicine’ which focuses on promoting the importance of medical providers understanding the patient’s level of health literacy as they approach building a relationship with the patient. Communication training for medical students was only systematically introduced from 2003.
For local governance, each municipality is responsible for promoting health education amongst citizens. For example in Chiba prefecture, besides civil lectures on preventive medicine, Chiba University Preventive Medicine Center and the municipalities have collaborated on a health project and research project based on health check data to build more effective health policies and healthier lives.
The Ministry of Education, Culture, Sports, Science and Technology (MEXT) provides education on health knowledge for children from elementary school to high school (mostly 6-18 years old) for the purpose of promoting school health, including prevention of drug abuse and drinking, and smoking prevention education, prevention of infectious disease, and mental health awareness. For instance, preventive education for drug abuse is suggested to be performed in physical and health education class annually, supported by an intervention from an expert. This approach is understood to be widely followed, for example in Ibaraki prefecture, the implementation rate in the prefectural high school was 99% in 2010 (MEXT, 2012[95]).
However, a survey of health literacy in Japan suggested that 85% of the Japanese population has low health literacy (Moreira, 2018[96]). According to the EU-Q47 survey performed in European countries and in Japan, which is comprehensive measure of health literacy across countries, there is a possibility that health literacy in Japan is lower compared to the European countries, especially when it comes to finding a reliable information for making a decision (Nakayama et al., 2015[97]).
1.8. Workforce
1.8.1. Human resource in public health care
Public Health Centres are indispensable for carrying out health services under the municipal government. Under the Community Health Act, Public Health Centres (hokenjo) serve as a hub for academic activities for regional public health, for promoting evidence-based effective and efficient local public health measures that reflect local characteristics, and effective coordination with other related measures in the fields of health care, long-term care and welfare. Public Health Centres are staffed by doctors, dentists, pharmacists, health nurses, and midwives based on Local Health Law (Chiiki Hoken Hou). Depending on demands, Public Health Centres also have medical technicians such as nutritionists, statistical engineers, and clinical laboratory technicians. Public Health Centres usually employ a public health physician working in the community health field as a Director, although most of the health centres do not require any specific certificates (Japanese Association of Public Health Center Directors, 2016[39]). Indeed under the law (Article 5-(1) of the Community Health Act), in principle, the heads of public health centres must be medical doctors because the centres serve as a hub for regional public health and community medicine. In addition, they must be: (1) a person who have spent more than three years engaging in public health work; (2) a person who have completed the designated training programme at the National Institute of Public Health; or (3) a person who have approved by the heads of local municipalities who consider them having the same level of knowledge and skills as the persons described in the two items above. The National Institute of Public Health provides candidates with necessary trainings to become heads of Public Health Centres and offers training programs for employees (or those who have achieved the same level) in health-care business, environmental health, and other public health fields.
A wide range of skills is necessary to become public health specialists, including an understanding of infectious diseases, maternal and child health, lifestyle diseases/cancer/intractable diseases, mental health, environmental health (foods and the environmental issues), and medical and pharmaceutical affairs. In recent years, they also tasked with the implementation of various local measures to address health emergencies that require the knowledge of multiple disciplines to solve. In this process, public health specialists need to work closely with related organisations and stakeholders such as long-term care and welfare professionals and local residents. Public health is a compulsory subject for the national doctor’s exams, and graduates can study public health in a handful of post graduate schools in Japan (MEXT, 2017[98]). Public Health Centres should have a doctor as a director who has training in public health, yet there is a shortage of certificated doctors. In Tokyo, although there are 130 public health doctors are working in 2015, Tokyo needed 50 more public health doctors. They make effort to have more doctors who want to work for public health sector such as local health centre or prefectural government by offering lectures and promotions (MHLW, 2016[99]). Updated general information about public health is found on websites maintained by medical associations such as the Japanese Society of Public Health, Japan Public Health Association and the Japanese Association of Public Health Center Directors. These Associations also hold regular conference and educational lectures for public health doctors and those who work for public health.
There are 30 000 occupational health doctors practically working as a clinician in Japan, although there are 90 000 occupational health doctors certificated in Japan. Trainings are offered at specific universities or through courses by the by Japan Medical Association (The Occupational Health Promotion Foundation, 2018[100]). There are two licensures for occupational physician. One is issued by JMA, and a second licensure is issued by The Japan Society of Occupational Health.
The number of full-time public health nurses in local government was 34 522 in 2016; 14.6% of which work in prefectural Public Health Centres, and the rest in municipal Public Health Centres (MHLW, 2017[101]). Public health nurses’ licence in Japan is certified to those who pass both of the national examination of nursing and the public health nurse qualification. Public health nurses support public health implementation at government offices or public centres, industrial health offices, and school health offices with the wide range of tasks from health consults to health policies. Public health nurses must complete at least one year of necessary training at public health nurse training schools and need to pass the national exam for registered public health nurses. But the licenses for registered public health nurses are granted to persons who have passed the national examination for registered nurses.
Although. Additionally, although the number of nurses in Japan is increasing, the turnover rate is over 10% (Japanese Nursing Association, 2016[102]) it is seen as necessary to take measures to reduce the turnover rate. The MHLW has tried to grasp the exact number of practicing nurses in Japan by using a system by which nurses report their contact details when they leave jobs, and has sought to support retired nurses to go back to work by providing reinstatement training and employment information to them (MHLW, 2015[103]).
The MHLW plans to increase nurses with advanced skills for specific medical interventions (tokutei-koi-kennsyuu-syuuryou-sya), but they do not perform similar practices as expected in nurse practitioners in some OECD countries. The MHLW has developed a new system for nurses to be trained to perform specific medical interventions to respond to the long-term care needs in various clinical settings, including homecare. While in some OECD countries “nurse practitioners” are independent to perform specific medical procedures and may not be required to work under the supervision of a physician, in Japan nurses who have completed the appropriate training course are still required to perform their practice according to instructions from physicians.
Responses to public health emergencies, and disaster preparedness measures, are also important roles for the government and the Ministry of Health, Labour and Welfare. Specific human resource assessments and registration have been carried out and the detailed tasks for disaster scenarios are still under consideration (MHLW, 2016[104]) (see also Chapter 4).
Figure 1.9. Practising nurses per 1 000 population, 2000 and 2015 (or nearest year)
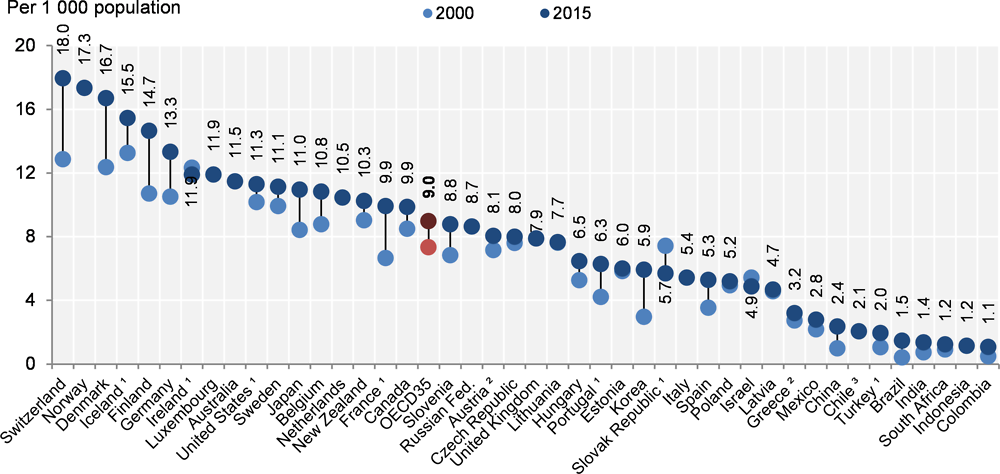
Source: OECD (2017[1]), Health at a Glance 2017: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/health_glance-2017-en.
1.8.2. Opportunities and challenges given Japan’s a-typical public health workforce
Unlike many in many OECD countries where primary care practitioners bear the bulk of responsibility for delivering public health education and services, Japan does not have a dedicated workforce with specific training in areas typically understood as ‘primary care’, nor do they have a strong gate-keeping function, or general practitioners. Instead, public health care and primary care-type functions, including health checks and screenings, disease management, and vaccinations, are delivered by a mix of semi-generalist/semi-specialists in the community, by Public Health specialists, by Occupational Physicians, by nurses and by public health nurses. From April 2018 a new system for the certification of new medical specialities, including general practitioners, was launched. At present, it is too early to assess the impact of this new certification on the Japanese medical workforce. However, for the moment Japan’s somewhat a-typical health workforce presents both challenges and opportunities for public health. The contribution of unique workforce roles such as public health nurses in is a strength. The fact that employed persons should have regular (or semi-regular) contact with a dedicated occupational health physician could also be an advantage in terms of education, disease management, and helping to reduce health risk factors such as smoking or overweight.
The MHLW also appears to have ambitious plans around the use of physicians’ assistants. Given that Japan has a relatively high number of nurses and a relatively low number of doctors this approach seems an effective approach.
However, the design of the Japanese health workforce could present some challenges in terms of delivering effective public health interventions. Notably, in theory the quality of service delivered by occupational physicians (Ops) could vary significantly. It is not clear that all OPs are delivering the most effective interventions for instance to reduce risk factors, nor that their focus is consistently on health improvement so much as the delivery of occupational health checks.
The central government and the National Institute of Public Health offer various training programs. Local municipalities also provide training programs to nurture experts who advance their knowledge about public health. There are training programmes for public health nurses and office staff who work for local Public Health Institutions. There are 129 public health doctors in total working in Bureau of Social Welfare and Public in Tokyo prefecture including the prefectural government office and municipal Public Health Centres. (Bureau of Social Welfare and Public, 2017[105]). These workers receive training on public health organised by the MHLW, National Health Sciences Institute, National Centre of Mental and Nervous Centre, Tuberculosis Prevention Tuberculosis Research Institute, etc.
For public health nurses, the training programmes are organised by the MHLW and planned at public health centres, collaborating with educational or research institutions. Depending on the institution to which they belong, the content of the training might be different, yet it should cover all the area of the government, industry and medicine (MHLW, 2011[106]).
The certificate system for a social medicine specialist started in 2017 in Japan, organised by the Japan Board of Public Health and Social Medicine, but implementation has been postponed. The training consists of the basic programme for the learning knowledge, and practical learning in the field of the central and local government, industrial and environmental health, and medicine (Social Medicine Council, 2016[107]).
1.9. Conclusion
While Japan has the longest life expectancy at birth in the OECD, it is nonetheless an increasingly elderly society, with a low birth rate, and a burden of disease dominated by chronic conditions. Governance of the Japanese public health system is relatively fragmented, and in this landscape of multiple actors and stakeholders, the central government and the Ministry of Health, Labour and Welfare (MHLW) appears to have relatively weak levers through which to pursue public health goals. While the MHLW can set the strategic direction for the system, and has some influence over key actors in the system through a range of legislative requirements, delivery of public health actions and more detailed planning are to other system stakeholders. Across the different areas of public health care – including the delivery of Health Japan 21, and public health emergency planning and response –an global picture of how well the whole Japanese system is delivering on the objectives set by the MHLW is missing. At present it does not appear that the MHLW has a strong mechanism for establishing the extent to which public health actors are delivering on nationally set strategies, for example, on Health Japan 21 (Chapter 2), or on nationally expected public health functions, for example health checks delivered by employers or municipalities (Chapter 3). If Japan is to meet the ambitious national goals set in HJ21 then it is critical that all local level governments are putting in place effective strategies and actions.
In Japan it is recognised that while local governments are responsible for implementation, the national government plays a role of keeping public health service policies consistent and reducing gaps in the service provision across the country. However in some cases, it may also be that strategies set are too broad which leaves local levels of government to choose from a selection of different areas on which to focus activities. While this can be a good way to allow local government to be responsive to local context and local needs, it may also contribute to an uneven package of public health activities across the country. While minimum expectations for local authorities and private actors are set in different areas of public health are set (through the various legislation for instance), it is not clear that there is a strong mechanism for checking that these minimum standards are set.
In addition, Japan may wish to look for ways to include a greater diversity of stakeholder voices in public health policy making and debate. In particular, voices from civil society and health service users did not appear to be influential in the Japanese system. Active inclusion of patients and service users’ views in the both setting strategic policy goals for the health system and day-to-day decisions should be prioritised, and effective public-facing communication strategies would be a priority if Japan were to make changes to core prevention services, for instance health checks.
References
[17] Anderson, C. et al. (2010), “Dietary Sources of Sodium in China, Japan, the United Kingdom, and the United States, Women and Men Aged 40 to 59 Years: The INTERMAP Study”, Journal of the American Dietetic Association, Vol. 110/5, pp. 736-745, http://dx.doi.org/10.1016/j.jada.2010.02.007.
[20] Asakura, K. et al. (2016), “Sodium sources in the Japanese diet: difference between generations and sexes”, Public Health Nutrition, Vol. 19/11, pp. 2011-2023, http://dx.doi.org/10.1017/S1368980015003249.
[18] Asakura, K. et al. (2014), “Estimation of sodium and potassium intakes assessed by two 24 h urine collections in healthy Japanese adults: a nationwide study”, British Journal of Nutrition, Vol. 112/07, pp. 1195-1205, http://dx.doi.org/10.1017/S0007114514001779.
[85] ASK (2018), Welcome to ASK's website!, https://www.ask.or.jp/english (accessed on 22 May 2018).
[77] Baku-baku no kai (2018), Live with a Ventilator, https://www.bakubaku.org/ (accessed on 22 May 2018).
[105] Bureau of Social Welfare and Public (2017), Tokyo Metropolitan Government Public Health Doctor Wanted Guide, http://www.fukushihoken.metro.tokyo.jp/joho/soshiki/hoken/hoken/oshirase/faq.html (accessed on 22 May 2018).
[80] Cabinet Office, 2. (2018), Japanese NPO, https://www.npo-homepage.go.jp/about/toukei-info/ninshou-zyuri (accessed on 22 May 2018).
[11] Chao, D., H. Hashimoto and N. Kondo (2015), “Dynamic impact of social stratification and social influence on smoking prevalence by gender: An agent-based model”, Social Science & Medicine, Vol. 147, pp. 280-287, http://dx.doi.org/10.1016/J.SOCSCIMED.2015.08.041.
[48] Distribution System Research Center (2007), “Manual for formulation of norms for sophistication of quality control in the wholesale market”, http://www.maff.go.jp/j/shokusan/sijyo/info/pdf/manual.pdf.
[61] Finish Diabetes Association (2003), “Programme for the Prevention of Type 2 Diabetes in Finland”, https://www.diabetes.fi/files/1108/Programme_for_the_Prevention_of_Type_2_Diabetes_in_Finland_2003-2010.pdf (accessed on 08 June 2018).
[64] Finnish National Institute for Health and Welfare (2016), Health in All Policies - Health promotion - THL, https://thl.fi/fi/web/health-promotion/health-in-all-policies (accessed on 14 June 2018).
[59] Food Safety Commission of Japan (2016), What is the Food Safety Commission?, https://www.fsc.go.jp/iinkai/ (accessed on 22 May 2018).
[3] Fujii, M., T. Oshio and S. Shimizutani (2014), “Self-rated Health Status of Japanese and Europeans in Later Life: Evidence from JSTAR and SHARE”, Japanese Economic Review, Vol. 65/4, pp. 483-498, http://dx.doi.org/10.1111/jere.12029.
[75] Health and Global Policy Institue (2018), About Health and Global Policy Institue(HGPI), https://hgpi.org/en/ (accessed on 22 May 2018).
[12] Honjo, K. and I. Kawachi (2000), “Effects of market liberalisation on smoking in Japan”, Tobacco Control, Vol. 9, pp. 193-200, http://dx.doi.org/10.1136/tc.9.2.193.
[35] Ikegami, N. (2016), “Achieving Universal Health Coverage by Focusing on Primary Care in Japan: Lessons for Low- and Middle-Income Countries”, International Journal of Health Policy and Management, Vol. 5/5, pp. 291-293, http://dx.doi.org/10.15171/ijhpm.2016.22.
[37] Japan Medical Association (2016), Family Medical Training Program, http://www.med.or.jp/doctor/kakari/ (accessed on 22 May 2018).
[39] Japanese Association of Public Health Center Directors (2016), Number of Public Health Centers Installed, http://www.phcd.jp/03/about/#donna (accessed on 22 May 2018).
[102] Japanese Nursing Association (2016), Survey on 2016 Hospital Nursing Actual Condition, http://dx.doi.org/10.9%、新卒看護職員離職率.
[55] Japanese Society for Dialysis Therapy (2017), “Current Status of Chronic Dialysis Therapy in Japan”, https://docs.jsdt.or.jp/overview/index.html.
[68] Kanagawa Prefecture (2018), Collaboration with WHO, http://www.pref.kanagawa.jp/docs/mv4/cnt/f537393/p1104811.html (accessed on 22 May 2018).
[56] Kazawa, K. et al. (2015), “Efficacy of a disease management program focused on acquisition of self-management skills in pre-dialysis patients with diabetic nephropathy: 24 months follow-up”, Journal of Nephrology, Vol. 28/3, pp. 329-338, http://dx.doi.org/10.1007/s40620-014-0144-2.
[14] Kodama, K. et al. (2013), “Ethnic differences in the relationship between insulin sensitivity and insulin response: A systematic review and meta-analysis”, Diabetes Care, http://dx.doi.org/10.2337/dc12-1235.
[29] Kyoto prefecture (2015), “On the efforts of suicide strengthening month”, http://www.pref.kyoto.jp/koho/kaiken/documents/27022702.pdf.
[63] Leppo, K. et al. (2013), “Health in All Policies”, http://www.euro.who.int/__data/assets/pdf_file/0007/188809/Health-in-All-Policies-final.pdf (accessed on 14 June 2018).
[66] Matsuda, R. (2017), “Japan : International Health Care System Profiles”, in The Commonwealth Fund: International Health Care System Profiles, The Commonwealth Fund, https://international.commonwealthfund.org/countries/japan/ (accessed on 23 January 2019).
[62] Melkas, T. (2013), “Health in all policies as a priority in Finnish health policy: A case study on national health policy development”, Scandinavian Journal of Public Health, Vol. 41/11_suppl, pp. 3-28, http://dx.doi.org/10.1177/1403494812472296.
[98] MEXT (2017), Professional Graduate School, http://www.mext.go.jp/a_menu/koutou/senmonshoku/08060508.htm (accessed on 22 May 2018).
[95] MEXT (2012), “Drug Abuse Prevention Classroom Promotion Manual”, http://www.mext.go.jp/component/a_menu/education/detail/__icsFiles/afieldfile/2018/03/08/1401907_3.pdf.
[33] MHLW (2018), “Current Public Long Term Care System”, https://www.mhlw.go.jp/content/0000213177.pdf.
[47] MHLW (2018), Food Hygiene Manager, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000049348.html (accessed on 22 May 2018).
[43] MHLW (2018), “How to Pay for Immunization”, http://www.mhlw.go.jp/stf/shingi/2r9852000000ts0v-att/2r9852000000tsiq.pdf.
[28] MHLW (2018), “Population dynamics in our country”, http://www.mhlw.go.jp/toukei/list/dl/81-1a2.pdf.
[93] MHLW (2018), Providing Medical Information, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryouhoken/reseputo/index.html (accessed on 22 May 2018).
[69] MHLW (2018), Seminars for Municipal Staffs, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hokabunya/shakaihoshou/seminar/index.html (accessed on 22 May 2018).
[54] MHLW (2018), Specific Health Check-up, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000161103.html (accessed on 22 May 2018).
[57] MHLW (2018), The System of the MHLW, http://www.mhlw.go.jp/kouseiroudoushou/shigoto/ (accessed on 22 May 2018).
[90] MHLW (2017), “Guidelines concerning efforts to provide incentives for personal prevention and health promotion”, http://www.mhlw.go.jp/file/04-Houdouhappyou-12401000-Hokenkyoku-Soumuka/0000124570.pdf.
[27] MHLW (2017), Measure for Suicide, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/shougaishahukushi/jisatsu/ (accessed on 22 May 2018).
[91] MHLW (2017), “Medical / nursing care - Enriching the lives of consumers”, https://www.kantei.go.jp/jp/singi/keizaisaisei/miraitoshikaigi/suishinkaigo_iryokaigo_dai5/siryou3.pdf.
[67] MHLW (2017), “Medical Plan”, http://www.mhlw.go.jp/file/06-Seisakujouhou-10800000-Iseikyoku/0000159901.pdf (accessed on 01 June 2018).
[26] MHLW (2017), “Outline of current industrial physician system”, http://www.mhlw.go.jp/file/05-Shingikai-12602000-Seisakutoukatsukan-Sanjikanshitsu_Roudouseisakutantou/0000166494.pdf.
[101] MHLW (2017), “Results of public health nurse activity area survey (area survey) Summary”, http://www.mhlw.go.jp/toukei/saikin/hw/hoken/katsudou/09/dl/ryouikichousa_h29_houdou.pdf.
[13] MHLW (2017), The National Health and Nutrition Survey in Japan, 2016., http://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h28-houkoku.pdf.
[92] MHLW (2017), “個人の予防・健康づくりに向けたインセンティブを提供する取り組み事例”, http://www.mhlw.go.jp/file/04-Houdouhappyou-12401000-Hokenkyoku-Soumuka/0000124573.pdf.
[104] MHLW (2016), “About DHEAT (Disaster Health Emergency Assistance Team)”, MHLW, http://www.mhlw.go.jp/file/05-Shingikai-10901000-Kenkoukyoku-Soumuka/0000131931.pdf (accessed on 02 June 2018).
[9] MHLW (2016), “AIDS Surveillance Committee, AIDS Occurrence Trend, 2016”, http://api-net.jfap.or.jp/status/2016/16nenpo/h28gaiyo.pdf.
[99] MHLW (2016), “Efforts to secure public health physicians to secure public health physicians to secure public health physicians”, http://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000119115.pdf.
[10] MHLW (2016), “Outline of the results of the National Health and Nutrition Survey”, http://www.nibiohn.go.jp/en/files/Section_of_the_National_Health_and_Nutrition_Survey/nhns2007.pdf.
[6] MHLW (2016), “The annual report of Tuberculosis Register Information Survey”, http://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000175603.pdf.
[31] MHLW (2016), “The survey of medical facilities”, http://www.mhlw.go.jp/toukei/saikin/hw/iryosd/16/dl/02_01.pdf.
[4] MHLW (2015), “Demographic Atatistics, 2015”.
[79] MHLW (2015), “Japan Vision Health care 2035 Proposal”, http://www.mhlw.go.jp/seisakunitsuite/bunya/hokabunya/shakaihoshou/hokeniryou2035/.
[19] MHLW (2015), “Japanese Dietary Reference Intake 2015”.
[103] MHLW (2015), Notification System of Nursing License Holder, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000095486.html (accessed on 22 May 2018).
[88] MHLW (2015), “Overview of National Health Care Costs in 2005”, http://www.mhlw.go.jp/toukei/saikin/hw/k-iryohi/15/dl/data.pdf.
[89] MHLW (2015), The Ministry of Health, Labor and Welfare Related Public Expenses Medical Institution List, https://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/dl/info03l-k_h260509-08.pdf.
[49] MHLW (2014), Food Poisoning, http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/shokuhin/syokuchu/index.html (accessed on 01 June 2018).
[53] MHLW (2012), “Basic policy for promoting comprehensive promotion of public health promotion”, http://www.mhlw.go.jp/bunya/kenkou/dl/kenkounippon21_01.pdf.
[40] MHLW (2012), Independent Administrative Agency, http://www.mhlw.go.jp/kouseiroudoushou/shokanhoujin/dokuritsu/ (accessed on 22 May 2018).
[106] MHLW (2011), “New Nursing Staff Training Guideline”, http://www.mhlw.go.jp/bunya/iryou/oshirase/dl/130308-3.pdf.
[38] MHLW (2010), “Recent Trends in Community Health”.
[81] MHLW (2010), “Recommendations on measures to cooperate with volunteers and NPOs in the administrative field of the Ministry of Health, Labor and Welfare”, http://www.mhlw.go.jp/stf2/shingi2/2r9852000000izeg-att/2r9852000000izip.pdf.
[32] MHLW (2010), “The summary of Medal Plan”, http://www.mhlw.go.jp/stf/shingi/2r9852000000zc42-att/2r9852000000zc72.pdf.
[25] MHLW (2007), “Suicide Measure Outline”, http://www.mhlw.go.jp/file/06-Seisakujouhou-12200000-Shakaiengokyokushougaihokenfukushibu/0000172329.pdf.
[83] MHLW (2006), Prevention of Drinking Behavior and Related Problems, http://www.mhlw.go.jp/topics/tobacco/houkoku/061122b.html (accessed on 22 May 2018).
[58] MHLW (2004), Tobacco Control Concerned Ministries Meeting, http://www.mhlw.go.jp/topics/tobacco/kaigi/secchi.html (accessed on 22 May 2018).
[30] MHLW (1948), Medical Law, http://www.mhlw.go.jp/topics/bukyoku/isei/shikarinsyo/gaiyou/kanren/iryo.html (accessed on 22 May 2018).
[86] MITI (2018), Health Management Superior Corporate Accreditation System, http://www.meti.go.jp/policy/mono_info_service/healthcare/kenkoukeiei_yuryouhouzin.html (accessed on 22 May 2018).
[96] Moreira, L. (2018), “Health literacy for people-centred care: Where do OECD countries stand?”, OECD Health Working Papers, Vol. No. 107 /OECD Publishing, Paris, https://doi.org/10.1787/d8494d3a-en..
[97] Nakayama, K. et al. (2015), “Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy”, BMC Public Health, http://dx.doi.org/10.1186/s12889-015-1835-x.
[46] National HPV Vaccination Program Register (2016), Coverage Data - National HPV Vaccination Program Register, http://www.hpvregister.org.au/research/coverage-data (accessed on 22 May 2018).
[94] National Institute of Health and Nutrition (2018), National Institution of Health and Nutrition, http://www.nibiohn.go.jp/eiken/ (accessed on 22 May 2018).
[84] National Institute of Health and Nutrition (2016), Health Japan 21 Assessment, National Institute of Health and Nutrition, http://www.nibiohn.go.jp/eiken/kenkounippon21/kenkounippon21/dete_detail_05.html#04_03 (accessed on 28 May 2018).
[42] National Institute of Infectious Diseases (2016), Japanese Vaccination Schedule, https://www.niid.go.jp/niid/ja/component/content/article/320-infectious-diseases/vaccine/2525-v-schedule.html (accessed on 22 May 2018).
[2] National Institute of Population and and Social Security Research (2017), “Japan's Future Population”, http://www.ipss.go.jp/pp-zenkoku/j/zenkoku2017/pp29_ReportALL.pdf.
[82] NICE (2014), “Developing NICE guidelines: a guide for stakeholders and the public”, https://www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/developing-NICE-guidelines-information-for-stakeholders.pdf.
[7] Nikkei Economic News (2012), Tuberculosis, 78 people are outbreaks Infection in Tokyo Hospital 10 people onset, https://www.nikkei.com/article/DGXNASDG0903Z_Z00C12A7CC1000/ (accessed on 22 May 2018).
[1] OECD (2017), Health at a Glance 2017: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/health_glance-2017-en.
[76] OECD (2017), PaRIS: Patient-Reported Indicator Survey. The next generation of OECD health statistics., http://www.oecd.org/health/PaRIS.htm (accessed on 22 May 2018).
[50] OECD (2016), “Antimicrobial Resistance”, http://www.oecd.org/health/antimicrobial-resistance.htm.
[87] OECD (2016), Health expenditure and financing, http://stats.oecd.org/index.aspx?r=598147 (accessed on 08 June 2018).
[72] OECD (2015), OECD Reviews of Health Care Quality: Italy 2014: Raising Standards, OECD Reviews of Health Care Quality, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264225428-en.
[34] OECD (2015), OECD Reviews of Health Care Quality: Japan 2015: Raising Standards, OECD Reviews of Health Care Quality, OECD Publishing, Paris, http://dx.doi.org/10.1787/9789264225817-en.
[74] OECD (2013), OECD Reviews of Health Care Quality: Sweden 2013, OECD Reviews of Health Care Quality, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264204799-en.
[70] Saaristo, V. (2017), TEAviisari, a tool for benchmarking health promotion capacity building in Finland, EuroHealthNet Magazine, http://www.eurohealthnet-magazine.eu/ehn-magazine-8/teaviisari-a-tool-for-benchmarking-health-promotion-capacity-building-in-finland/ (accessed on 17 October 2018).
[71] Saaristo, V. et al. (2018), “The comparative and objective measurement of health promotion capacity-building: from conceptual framework to operationalization”, Global Health Promotion, p. 175797591876960, http://dx.doi.org/10.1177/1757975918769608.
[73] SALAR (2018), About SALAR - SKL, https://skl.se/tjanster/englishpages/aboutsalar.995.html.
[107] Social Medicine Council, 2. (2016), Social Medicine Program, http://shakai-senmon-i.umin.jp/standards.html#seibi (accessed on 22 May 2018).
[52] The Government of Japan (2016), National Action Plan on Antimicrobial Resistance (AMR) 2016-2020.
[36] The Japan Medical Association General Policy Research Organization (2014), “Survey on Japanese medical attitudes, The Japan Medical Association General Policy Research Organization”, http://www.jmari.med.or.jp/download/WP331.pdf.
[60] The Ministry of Environment (2017), “Energy Countermeasure Special Account”, http://www.env.go.jp/guide/budget/h29/h29-ann/b2_energy.pdf.
[23] The Ministry of Environment (2012), Outline of the Air Pollution Control Law, http://www.env.go.jp/air/osen/law/ (accessed on 22 May 2018).
[78] The National Federation of Mental Health and Welfare Party (2018), Minna Net, https://seishinhoken.jp/ (accessed on 22 May 2018).
[100] The Occupational Health Promotion Foundation (2018), To Become an Industrial Physician, http://www.zsisz.or.jp/insurance/naruniwa/ (accessed on 22 May 2018).
[24] Tokyo Metropolitan Welfare and Health Administration (2018), Outline of Children's Chronic Specific Disease Medical Expenditure Subsidy Program, http://www.fukushihoken.metro.tokyo.jp/kodomo/kosodate/josei/syoman/top.html (accessed on 22 May 2018).
[45] Walker, T. et al. (2017), “National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2016”, MMWR. Morbidity and Mortality Weekly Report, Vol. 66/33, pp. 874-882, http://dx.doi.org/10.15585/mmwr.mm6633a2.
[41] WHO (2018), “WHO Recommendations for Routine Immunization - summary tables”, WHO, http://www.who.int/immunization/policy/immunization_tables/en/ (accessed on 22 May 2018).
[22] WHO (2017), “Healthier Fairer Safer The Global Health Journey”.
[15] WHO (2016), Salt Reduction, http://www.who.int/en/news-room/fact-sheets/detail/salt-reduction (accessed on 22 May 2018).
[5] WHO (2016), “Tuberculosis country profile of Japan”, https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=JP&LAN=EN&outtype=pdf.
[65] WHO (2015), Finland curbs childhood obesity by integrating health in all policies, World Health Organization, http://www.who.int/features/2015/finland-health-in-all-policies/en/ (accessed on 14 June 2018).
[21] WHO (2014), “7 million premature deaths annually linked to air pollution”, WHO, http://www.who.int/mediacentre/news/releases/2014/air-pollution/en/ (accessed on 22 May 2018).
[51] WHO (2014), “ANTIMICROBIAL RESISTANCE Global Report on Surveillance”, http://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748_eng.pdf?sequence=1.
[16] WHO (2012), Guideline: Sodium intake for adults and children, World Health Organization, Geneva, http://www.who.int/nutrition/publications/guidelines/sodium_intake_printversion.pdf.
[44] WHO (2007), “Human Papillomavirus and HPV Vaccines”, WHO, http://www.who.int/bulletin/volumes/85/9/06-038414/en/ (accessed on 22 May 2018).
[8] World Health Organization (2015), Global tuberculosis report 2015, 20th ed., World Health Organization, http://www.who.int/iris/handle/10665/191102.