Michele Cecchini
Marion Devaux
Michele Cecchini
Marion Devaux
Harmful alcohol use is a pressing public health issue and a key driver of non-communicable diseases, injuries and premature deaths. This chapter brings together the main messages of this publication and describes the policy implications identified by new OECD analyses of the health, social and economic burden of alcohol-related diseases. It presents trends and projections for up to 52 OECD, Group of 20 (G20) and European Union (EU27) countries, and makes a strong economic case for upscaling investment in policies to tackle harmful alcohol consumption. The chapter presents the expected effectiveness, impact on health expenditure and return on investment for ten policy interventions and four policy packages aimed at addressing harmful alcohol use. It concludes by analysing the potential impact public health policies may have on the industry and approaches to mitigate costs.
While alcohol is highly valued by many consumers as a source of individual pleasure and social enjoyment, and its production and trade represent an important part of the economy in many countries, harmful alcohol consumption is among the leading risks to population health, causing many non-communicable diseases which, in turn, have wider detrimental societal consequences. Measures that governments can implement to address harmful alcohol consumption can target either all consumers or those that drink more heavily. Interventions targeting all consumers – such as alcohol taxation or regulation of advertising – are highly effective at the population level but, by affecting all people who drink independently of their level of alcohol consumption, they also involve interpersonal trade‑offs in welfare. To the extent that policies to tackle harmful alcohol use require such complex trade‑offs to be made, it is ultimately up to each country to consider the most appropriate mix of policies to implement. The work undertaken by the OECD seeks to provide evidence on the health and economic impacts of alternative policies to tackle this risk factor to help countries make these complex decisions.
Once both recorded and unrecorded alcohol consumption are taken into account, World Health Organization (WHO) data suggest that people aged 15 years and over in OECD countries drank on average 10 litres of pure alcohol per person per year in 2018 – equivalent to about 20 cl of wine or half a litre of beer per day. While average alcohol consumption in OECD countries changed little between 2010 and 2018, significantly different trends can be observed across countries. During this period, alcohol consumption increased most in Spain and Iceland, while it decreased significantly in Estonia and Lithuania.
Harmful patterns of alcohol consumption remain highly prevalent in the OECD population. According to WHO data, 30% of adults engaged in binge drinking at least once in the previous month, while OECD analyses show that more than 60% of teenagers aged 15 years drink alcohol and one in five has experienced drunkenness at least twice in life. In addition, analyses of six OECD countries suggest that between a third and a half of all alcohol is consumed by people who drink heavily.
The OECD Strategic Public Health Planning for non-communicable diseases (SPHeP-NCDs) model shows that diseases caused by drinking more than 1 drink per day for women and 1.5 drinks per day for men will reduce life expectancy at birth by 0.9 years over the period 2020‑50. By 2050, around 1.1 million premature deaths from alcohol-related diseases will occur in OECD, Group of 20 (G20) and European Union (EU27) countries.
Drinking above the 1/1.5 drinks per day cap is responsible, on average, for 87% of all treatment costs for dependence, 35% of treatment costs for cirrhosis and 4% of treatment costs for injuries and cancers.
According to the simulations, on average, OECD countries will spend about 2.4% of their total health expenditure on treating diseases caused by drinking more than 1 drink per day for women and 1.5 drinks per day for men, each year over the next 30 years. This is equivalent to USD PPP 61 per capita per year. In total, USD PPP 138 billion per year will be spent on treating these diseases across all the countries included in the analysis. This is equivalent to, for instance, the current health spending in Australia, or more than twice the current health spending in Belgium.
Among teenagers, never experiencing drunkenness is associated with a 30% higher likelihood of performing well at school. Analysis of longitudinal datasets from New Zealand, the United Kingdom, the United States and the Russian Federation suggests that, in the long term, students who weekly drink alcohol may have lower educational performances and lower educational attainment, at least in some countries, and particularly in the case of girls.
Individuals with medical conditions caused by drinking more than 1 drink per day for women and 1.5 drinks per day for men are less likely to be employed and, if employed, are likely to have reduced productivity. When reduced labour force participation and productivity due to alcohol-related diseases are converted into an economic value, OECD countries lose about USD PPP 595 billion per year. This is roughly equivalent to the annual gross domestic product (GDP) of Belgium or Sweden.
Medical conditions caused by drinking more than the 1/1.5 drinks per day cap and their consequences on life expectancy, health expenditure, employment and productivity cause GDP to be 1.6% lower in OECD countries. They also exact a heavy toll on personal budgets, corresponding to about a 0.43 percentage point increase in total fiscal pressure, or USD PPP 232 per capita per year.
OECD countries can further upscale policy initiatives to tackle harmful alcohol consumption. Six categories of policy are usually implemented by countries, including modifying the cost of alcohol; modifying the availability of alcohol; countering drink-driving; regulating alcohol marketing; enhancing screening and brief interventions; and modifying consumption through consumer information. Once implemented, however, the level of implementation of policies “on the ground” and their effectiveness at the population level vary.
Upscaling countries’ efforts to tackle harmful alcohol consumption – both by implementing new policy options and by strengthening policies currently in place – would bring health benefits to the whole population and save money. The choice of which types of intervention to implement remains with countries, based on a careful assessment of various trade‑offs.
Overall, the assessed policies may significantly reduce the burden of disease caused by harmful alcohol consumption and increase population health. The OECD microsimulation model shows that interventions targeting the whole population tend to have the largest impact, but these affect all people who drink – including those drinking at low/moderate levels – creating the need for trade‑offs from policy-makers. Targeted interventions, such as alcohol counselling in primary care and personalised pharmacological treatment, have a significant short- to medium-term impact on people who engage in harmful drinking only. This can avoid some of the difficult trade‑offs, but such interventions are less effective at the population level.
Savings in health expenditure can be significant, ranging from USD PPP 207 billion (minimum unit pricing) to USD PPP 6 billion (workplace programmes) between 2020 and 2050 across all the countries included in the analysis.
Combining interventions in “prevention packages” would return higher benefits. For example, investing in a mixed package to upscale policies already in place in many OECD countries – including regulation of advertising, sobriety checkpoints, alcohol taxation and alcohol counselling in primary care – results in a gain of 3.5 million life years per year across all 48 countries included in the analysis and saves about USD PPP 16 billion annually in health expenditure.
Prevention packages to tackle the consequences of harmful alcohol consumption are a good investment for countries. By considering changes in population health, health and other government expenditure and labour force productivity, the OECD long-term economic model evaluates that for every USD 1 invested in any of the packages, economic benefits for countries vary between USD 1.4 and USD 16.4, depending on the policy package studied. Such public health policies may affect industry revenue, but countermeasures exist to minimise costs.
During the last decade, per capita alcohol consumption in OECD countries largely remained stable, although some countries experienced significant shifts in consumption. Beyond average trends, the analyses identified some worrying statistics related to harmful alcohol consumption.1 First, binge drinking is highly prevalent in OECD countries,2 with 30% of adults engaging in heavy episodic drinking at least once in the past 30 days. Second, despite it being illegal in many countries, more than 60% of teenagers aged 15 drink alcohol, and one in five reported having ever been drunkenness at least twice. Third, large inequalities exist: alcohol consumption is heavily concentrated in specific population groups, such as women with a high level of education and individuals in the lowest and highest income groups.
Alcohol-related diseases such as cancers, cardiovascular diseases, injuries and alcohol dependence pose a serious threat to the economy of countries and to the budgets of their citizens. In total, USD PPP 138 billion per year is spent across the 52 assessed countries,3 including OECD, Group of 20 (G20) and European Union (EU27) countries, on medical conditions caused by drinking above 1 drink per day for women and 1.5 drinks per day for men. In addition, the same chronic diseases negatively affect labour force productivity: individuals with at least one chronic disease are less likely to be employed in the following year and, if employed, are more likely to be absent or less productive. Similarly, children who have experienced drunkenness and initiate drinking at an early age show a lower likelihood of performing well at school. This can lower educational attainment later on, which in turn lowers the level of human capital in the future. All these factors combine to depress the social welfare and economy of countries, resulting in a total economic burden that may be vary between 0.2% (in Turkey) to 3.8% (in Lithuania) of gross domestic product (GDP).
More can be done to tackle harmful alcohol consumption and its associated conditions. Of the 52 countries included in the analysis, 41 have adopted a national written alcohol policy; among these, 19 countries have an aligning action plan to implement the national policy on alcohol. The vast majority of countries have also implemented comprehensive sets of policies consistent with the ten key areas of policy actions and interventions identified in the World Health Organization (WHO) Global Strategy to Reduce the Harmful Use of Alcohol (WHO, 2010[1]). However, the high health and economic burden caused by harmful alcohol consumption shows that there is scope to scale up efforts further. Too often, policy actions are not implemented in their most effective form, or are not uniformly implemented throughout the country. In other cases – such as interventions delivered by the health system – limited resources or practical problems limit their coverage.
Governments should consider upscaling efforts in a number of areas, chosen according to whether they want to implement population-wide policies or individual-level policies that specifically target high-risk individuals. These groups of policies have different characteristics, implementation costs and impacts on population health. Further, the decision to upscale action on any of these interventions also requires consideration of other trade‑offs that often go beyond their public health impact. For example, the impact on the economy and the labour market, as well as which type of consumer the policy aims to target, should all be considered. The decision on where to strike a balance between population and individual approaches to alcohol policy must be left to individual governments. The work undertaken by the OECD provides detailed estimates of policy impacts both at the population level and in specific subgroups, thereby supporting an evidence‑based approach to such decisions.
By using its microsimulation model – the OECD Strategic Public Health Planning for non-communicable diseases (SPHeP-NCDs) model – the OECD has calculated that scaling up action by increasing investments in highly effective “best practices” would have a significant impact on the health of the population and the economy. Greater results would be achieved by implementing packages of policies. For example, between 2020 and 2050, the most effective package – the mixed package plus- would prevent a total of 265 million cases of major chronic diseases across the 48 countries analysed,4 including liver cirrhosis, cancers, cardiovascular diseases, injuries and cases of alcohol dependence, leading to a gain of up to 4.6 million life years (LYs) annually. Savings in health expenditure would equal around USD PPP 28 billion annually in the 48 countries studied. A healthier population and reductions in government spending on health would also improve labour market participation and productivity, with positive effects for the broader economy. While some of these public health interventions carry direct implications and costs for the alcohol industry, available evidence and new OECD analyses suggest that consumers may reallocate expenditure to other discretionary goods, possibly offsetting some of the broader economic implications of these policies.
On average, across OECD countries, a person aged 15 years and over consumes 10 litres of pure alcohol per year, which is roughly equivalent to two bottles of wine or nearly 4 litres of beer per week. Men consume more alcohol than women in all countries, with about a three‑fold gender gap. Beer is the most consumed type of alcoholic beverage in OECD countries, corresponding to about 42% of all alcohol consumed; wine accounts for 29% and spirits, including all distilled beverages, for 23%. Among G20 countries the average alcohol consumption is lower, at 7.9 litres per capita. This is driven by a number of countries with very low levels of consumption, including Saudi Arabia, Indonesia, India and Turkey. On the other hand, the EU27 average is higher, at 11.3 litres per capita.
Per person alcohol consumption increases significantly when figures are related to the number of people who drink rather than the total population. On average in OECD countries, 32% of the population abstained from alcohol consumption in the past year, with women more likely to be abstainers than men (42% of women vs. 21% of men). In OECD countries, people who drink consume on average 15.4 litres of pure alcohol per year, ranging from 7.0 litres in Israel to 28.5 litres in Turkey per capita in 2018.5 While the average consumption in G20 countries is lower, the per-drinker consumption is equal to the OECD at 15.4 litres per year per consumer. This is due to a number of countries (such as South Africa, Turkey, the Russian Federation and Brazil) where the number of people who drink is lower, but where those who do drink consume larger quantities than in other countries.
According to WHO data, per capita total alcohol consumption – including both recorded and unrecorded alcohol consumption – has remained stable since 2010, but large cross-country differences exist. Between 2010 and 2018, total per capita consumption decreased by 0.17 litres in OECD countries (from 10.18 litres to 10.01 litres), by 0.20 litres in EU27 countries (from 11.48 litres to 11.28 litres) and by 0.37 litres in G20 countries (from 8.24 litres to 7.88 litres). However, some countries that had high levels of consumption in 2010 have seen large decreases, including Estonia (‑3.2 litres) and Lithuania (‑2.0 litres). Conversely, about half of the countries analysed saw alcohol consumption increase; this increase was highest in Spain (+2.7 litres) and Iceland (+1.6 litres). Usually, across countries, men experienced a greater increase in alcohol consumption than women between 2010 and 2018.
It is still too early to understand any long-term effect that the COVID‑19 pandemic may have produced on patterns of alcohol consumption. Nonetheless, early evidence would suggest that people modified their drinking habits during the first wave of the pandemic, with different population groups reporting either a decrease or an increase in alcohol consumption (Box 1.1).
At the beginning of 2020, the COVID‑19 pandemic spread across the globe, leading countries to enforce national lockdowns. Emerging evidence shows that these lockdowns had an impact on people’s lifestyles, including their drinking habits. While it is too early to say whether this impact will be temporary or long-lasting, some population groups reported either an increase or a decrease in alcohol use. Researchers have explored the impact of policies to contain COVID‑19 on patterns of alcohol consumption through two types of data: market sales data and self-reported and survey-based data.
Analyses of alcohol market data show a collapse in on-premise markets (e.g. bars, pubs and restaurants) and an increase in off-premise markets (e.g. retail outlets, online) during the COVID‑19 pandemic. For instance, off-premise markets for Belgium, Spain and the United States show a significant increase in sales, up to +234% in online sales in the case of the United States (Eurocare, 2020[2]; Nielsen, 2020[3]). Especially, alcohol e‑commerce has increased in 19 countries (Australia, Brazil, Canada, China, Colombia, France, Germany, India, Italy, Japan, Mexico, Poland, the Russian Federation, South Africa, Spain, Thailand, Turkey, the United Kingdom, and the United States) (IWSR, 2020[4]).
Globally, considering both on- and off-premise markets, the overall alcohol market shows resilience, especially in a few countries (IWSR, 2020[4]), although an overall decline is pronounced in others, for instance in Switzerland (Movendi International, 2020[5]). Governmental sources monitoring sales – mainly for taxation purpose‑ show an overall increase in alcohol consumption, in a few countries for which data is available. For example, in the United States, data from 15 States suggest a 4.0% increase in the quantity of alcohol sold in the period January to August 2020, compared to the same period in the previous year (National Institute on Alcohol Abuse and Alcoholism, 2020[6]). German data suggest an increase in alcohol tax revenues of 3.3% in 2020, compared to 2019 (Bundesministerium der Finanzen, 2021[7]). Finally, in the United Kingdom, the provisional 2020‑21 financial year to date totals for alcohol duty receipts show an increase by 4.5% compared to the same period in the previous year. More specifically, the beer and cider duty receipts decreased by 9.7% and 11.3%, while the wine and spirits duty receipts increased by 13.1% and 10.7% (HM Revenue and Customs, 2020[8]). Another study based on household purchases data in the United Kingdom found a 41% excess of alcohol purchases during the confinement relative to the preceding year, but no excess purchase once adjusted for expected normal purchases from on-licenced premises. Excess purchases, without these adjustments, were higher the lower the age of the main shopper and the higher the income (Anderson et al., 2020[9]).
Self-reported data tend to be less accurate, but they usually facilitate better segmentation of the analysis by population groups. Data from national public health agencies in France and Belgium show that the closure of bars and restaurants during the lockdown was associated with an overall reduction in alcohol consumption, especially among young adults. In the same period, some other population groups (such as people aged 35‑50 and parents of young children) reported higher than usual consumption (Gisle et al., 2020[10]; Santé Publique France, 2020[11]). Similarly, a study from the United States showed a significant increase in the frequency, but not the quantity, of consumption during the lockdown compared to the year before, especially among people aged 30‑59, women and non-Hispanic White individuals (Pollard, Tucker and Green, 2020[12]).
A notable example of self-reported data is the Global Drug Survey special edition on COVID‑19 (Winstock et al., 2020[13]), which was run for seven weeks between May and June 2020 and gathered responses from about 60 000 individuals across 11 countries (Figure 1.1). Findings from the survey show that:
Overall, 31% of respondents did not report any change in their drinking frequency during the first lockdown, 26% had decreased frequency and 43% had increased frequency, with little difference across sexes. Half of women and 44% of men reported no change in the frequency of binge drinking.
Among the individuals surveyed, 43% reported no change in the quantity drunk, while 21% had decreased consumption and 36% had increased consumption.
The context of drinking alcohol has changed since before COVID‑19: 75% of respondents declared drinking alone at home, with or without other people connected by calls or chats. Among these, 42% reported that they drank alone more often during the lockdown, while 39% reported no change and 19% reported drinking alone less often. Data also show large reductions in the proportion of people consuming alcohol at house parties, smaller gatherings, nightclubs and events.
Change in alcohol consumption since before COVID‑19, average across 11 countries
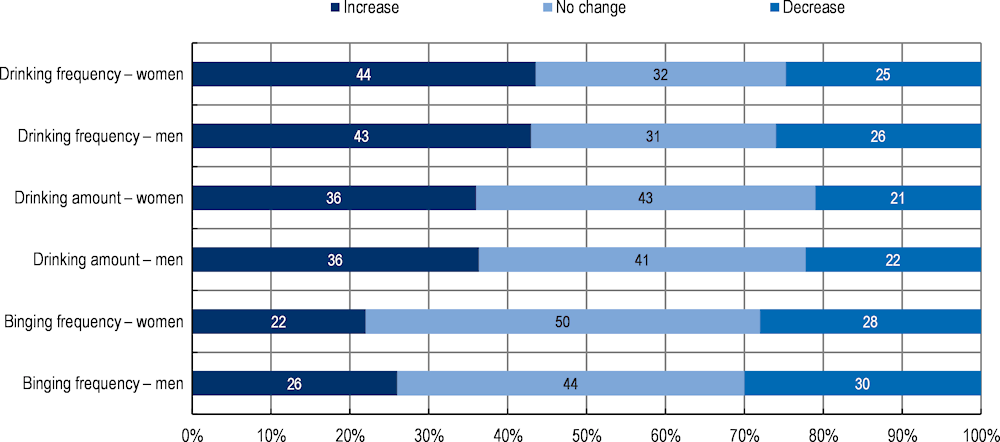
Note: Data collected in May and June 2020 in Australia, Austria, Brazil, France, Germany, Ireland, the Netherlands, New Zealand, Switzerland, the United Kingdom and the United States
Source: Winstock et al. (2020[13]), GDS COVID‑19 Special Edition: Key findings report, https://www.globaldrugsurvey.com/gds-COVID-19-special-edition-key-findings-report.
The averages presented mask significant inequalities both across countries and within the same country, across different population groups. The OECD has analysed the available data and identified trends and patterns suggesting that specific population groups are more likely to bear the bulk of the health, social and economic burden of harmful alcohol consumption. Specifically, the analysis focused on high-risk patterns of alcohol consumption, on alcohol consumption in underage individuals and on socio‑economic inequalities by income and education levels. The analysis also used a sex lens to highlight inequalities.
Heavy drinking – drinking volumes of alcohol above guideline amounts – and binge drinking (or heavy episodic drinking) – drinking at least 60 grammes or more of pure alcohol in one single occasion – are considered particularly dangerous patterns of alcohol consumption as they carry additional risks. For example, people who drink heavily are at increased risk of developing alcohol dependence (CDC, 2020[14]), which affects 3.7% of the population in OECD countries or about 50 million people. Binge drinking increases the risk of injuries and has been shown to be a risk factor for heart disease, even when overall alcohol consumption is low to moderate (Rehm et al., 2003[15]).
New OECD analyses on micro-level data for Canada, England (United Kingdom), France, Korea, Mexico and the United States concluded that people who drink heavily make up only 4% to 14% of the population, but they consume between a third and a half of all alcohol. As these calculations are based on self-reported alcohol consumption – which is known to be considerably underestimated, especially in people who drink heavily (Boniface, Kneale and Shelton, 2014[16]) – the actual proportion of alcohol consumed by people who drink heavily is probably even higher. An additional set of analyses looking at the 20% of people who drink the most shows that this group accounts for 65% to 87% of all alcohol consumed. Results from the OECD analyses are broadly aligned with previous evidence showing that people who drink heavily generally consume the majority of all alcohol (see, for example, Livingston and Callinan (2019[17]); Richard et al. (2019[18])).
Binge drinking is highly prevalent in OECD countries, with 30% of adults having engaged in heavy episodic drinking at least once in the past 30 days. Prevalence of binge drinking is particularly high in Central and Eastern European countries. For example, 49% of the population in Lithuania engages in heavy episodic drinking at least once in 30 days (see additional analyses on regional differences in Box 1.2). Within countries, binge drinking is not uniform across the population: some groups are at higher risk. Specifically, as discussed in Section 1.1.4, women with higher levels of education and individuals in the lowest and highest income groups show the highest likelihood for binge drinking, while the middle socio‑economic classes have the lowest rates of monthly binge drinking.
OECD analysis shows that a significant share of teenagers aged 15 years have both drunk alcohol and experienced episodes of drunkenness. In addition to being illegal, drinking in childhood is predictive of future drinking – even after adjusting for family income and minority status, which are two well-known confounders. OECD analyses of longitudinal data from the United States found that among teenagers who drank weekly when aged 15‑18, boys were 56% more likely and girls 121% more likely to drink weekly when aged 21‑25 than peers who rarely drank during childhood. Even monthly drinking during childhood increased the risk of weekly drinking six years later by 49% in men and 79% in women. Findings from the OECD analyses on the US dataset are broadly confirmed by other analyses in the literature, which conclude that children who begin drinking are more likely to continue drinking at an older age.
Analyses of the 31 countries included in the 2017‑18 wave of the Health Behaviour in School-aged Children (HBSC) survey6 identified the following patterns:
About one in five teenagers, both boys and girls, aged 15 years and attending school have experienced drunkenness at least twice in their life. Within the OECD, Iceland shows the lowest prevalence: 7% of both boys and girls reported experiencing drunkenness. Conversely, Denmark reported the highest percentages for both boys (37%) and girls (47%).
Younger generations are less likely to experience drunkenness at age 15 than a decade ago; if they had been drunk, this had occurred at an older age, although differences are small. Over the period 2001‑14, the average age of first drunkenness increased slightly from 13.7 to 14.0 years old in boys and from 13.9 to 14.2 years old in girls across 21 OECD countries.7
Despite a small decline in the period 2014‑18, lifetime alcohol use among adolescents remained high, varying from 64% in 2014 to 62% in 2018 among boys and from 64% to 63% among girls, on average across OECD countries.
Harmful patterns of alcohol consumption continue in young adulthood. On average across OECD countries,8 monthly binge drinking is most common in the two youngest age groups (those aged 15 to 44), after which it becomes less prevalent with increasing age.
Patterns of drinking across different socio‑economic groups are not straightforward. The OECD analysis took into consideration both income and education levels, as well as the sex effect on these relationships, given that the literature generally finds different patterns.
Analyses focusing on the level of income found a U- or J-shaped curve relationship between income and the likelihood of binge drinking in many countries, and many see the lowest rates of monthly binge drinking in the middle socio‑economic classes. On average in OECD countries, women and men are more likely to binge drink monthly if they are in the lowest or two highest income groups. Exceptions are Belgium, Canada and Slovenia, where a positive relationship between income and binge drinking is observed, with those in the highest income group most likely to binge drink monthly. France, Greece and the United States see a negative relationship, where people on a lower income are more likely to binge drink monthly.
Analyses focusing on binge drinking by level of education show inequalities that differ by sex. On average across 26 OECD countries, women with higher educational attainment are 13% more likely to engage in monthly binge drinking (14% of women with higher education binge drink monthly versus 12% of women without higher education). For men, however, roughly half of countries show an inverse relationship – those with lower educational attainment are more likely to binge drink monthly. Findings from both analyses should be interpreted in the light of the fact that data are based on self-reported alcohol consumption from national surveys, and may be subject to misreporting by the heaviest drinkers or some socio‑economic groups.
Much attention has been paid to potential differences in drinking behaviours between countries in Northern and Southern Europe. While in the past, drinking patterns were considered very different between countries in Northern Europe – where alcohol was traditionally consumed less frequently but at higher levels – and those in Southern Europe – where heavy episodic drinking was less common – patterns of alcohol consumption have increasingly converged over the past 40 years.
An OECD analysis explored regional differences in patterns and outcomes of alcohol drinking across Europe and investigated the potential reasons behind these differences. The analysis covered five European regions: the Nordic, Eastern, Baltic, West-Central and Southern regions.1The main findings show that there is no clear geographical north – south divide in drinking patterns and outcomes. Rather, the picture is more complex:
The Southern region countries show lower drinking levels, low prevalence of risky drinking patterns and smaller burden on health.
The Nordic countries generally have relatively lower drinking levels and a lower burden on health, but they have relatively higher prevalence of alcohol dependence.
The Baltic countries have the highest drinking levels, having experienced the sharpest increase in alcohol consumption over recent decades. They have relatively higher prevalence of alcohol dependence, and a higher burden on health.
Countries in the Eastern and West-Central regions are globally in an intermediate position on these dimensions.
European countries have implemented a battery of policy actions to prevent harmful alcohol use, although the level of implementation varies. Notably, alcohol control policies are more stringent in Nordic countries and in Lithuania.
Beyond policy actions, other factors such as genetics, individual characteristics, socio‑economic status and environmental factors – such as societal drinking norms – also influence drinking patterns and outcomes over the life course.
1. The Nordic region includes: Finland, Iceland, Norway and Sweden; the Baltic region: Estonia, Latvia and Lithuania; the Eastern region: Bulgaria, Croatia, Hungary, the Czech Republic, Poland, Romania, the Slovak Republic and Slovenia; the West-Central region: Austria, Belgium, Denmark, Germany, Ireland, Luxembourg, the Netherlands, Switzerland and the United Kingdom; and the Southern region: Cyprus, France, Greece, Italy, Malta, Portugal and Spain.
While alcohol is highly valued by many consumers as a source of individual pleasure and social enjoyment, and its production and trade represent an important part of the economy in many countries, harmful alcohol consumption is among the leading risks to population health, causing many NCDs which, in turn, produce a detrimental effect on the global economy. Alcohol is a causal factor for more than 200 disease and injury conditions, including alcohol dependence, liver cirrhosis, some cancers and cardiovascular diseases, with differences by gender (WHO, 2018[19]). Globally, men drink more than women and bear the bulk of the burden of alcohol-related diseases and injuries, but alcohol affects women differently. Owing to biological differences, women have a higher risk of alcohol-related diseases such as liver diseases and breast cancer. Moreover, alcohol use can cause harm to others, as it can contribute to injuries resulting from violence, road traffic crashes and foetal alcohol spectrum disorders. However, the impact of alcohol consumption is not limited to the health of the general population. Harmful alcohol consumption also has important personal, social and economic consequences. First, treatment of patients with alcohol dependence and alcohol use disorders and other alcohol-related chronic conditions increases health expenditure. Second, students – young students in particular – with harmful patterns of alcohol consumption show a higher probability of lower academic performance which, in the long run, may lead to lower educational attainment; this negatively affects an individual’s socio‑economic status in adulthood and the human capital of countries. Third, alcohol-related chronic conditions affect individuals’ productivity and workforce participation, with a negative impact on labour market outputs. At a macroeconomic level, all these dimensions negatively affect the GDP of a country and create the conditions for increased fiscal pressure.
The OECD carried out a comprehensive assessment of the health and economic burden of alcohol-related diseases in 52 countries, using the OECD SPHeP-NCDs model and the OECD long-term economic model (Box 1.3) to evaluate the impact of two different scenarios:
A first scenario uses a ceiling of alcohol consumption at 1 drink per day for women and 1.5 drinks per day for men – that is equivalent to 12 grammes of pure alcohol per day for women and 18 grammes per day for men. In addition, this scenario assumes no binge drinking, as this has been shown to be a risk factor for disease even when overall alcohol consumption is light to moderate (Roerecke and Rehm, 2010[20]).9 Throughout the rest of this chapter, this is referred to as the 1/1.5 drinks per day cap. To account for uncertainty on the possible protective effect of alcohol consumption on ischaemic cardiovascular diseases and diabetes, a sensitivity analysis on this scenario is also presented in Box 1.4.
The second scenario calculates the total burden of alcohol-related medical conditions. For practical purposes, and following a standard approach, this is done by simulating a scenario that evaluates how assessed outcomes change resulting from a fictitious elimination of the risk factor and, consequently, of all alcohol-related diseases. Results for this scenario are discussed in Box 1.5.
The OECD SPHeP-NCDs model is an advanced systems modelling tool for public health policy and strategic planning. It is used to predict the health and economic outcomes of the population of a country, or a region, up to 2050. The model simulates synthetic populations of 52 countries, including OECD member countries, G20 countries, EU27 countries and OECD accession and selected partner countries.
The model covers 12 categories of disease, including seven directly related to alcohol (alcohol dependence, cirrhosis, injuries, cancer, depression, diabetes and cardiovascular diseases). Incidence and prevalence of diseases in a specific country’s population are calibrated to match estimates from international datasets. The links between alcohol consumption and diseases are modelled through age‑ and sex-specific relative risks retrieved from the literature and depend on both the volume and the patterns of alcohol consumption, as relevant (see Box 4.1 in Chapter 4).
The impact of harmful alcohol consumption on labour market outcomes is simulated through the effects mediated by chronic diseases, given that the evidence on the links between alcohol consumption and diseases, and between diseases and reduced labour force productivity is much stronger. While this approach is likely to be conservative (by disregarding, for example, the negative effect that heavy drinking can have on employment or productivity independently of any medical condition), the resulting findings rely on stronger evidence.
The model was used to simulate various scenarios, including the burden related to different levels of alcohol consumption (two scenarios described in Section 1.2) and policy scenarios (described in Section 1.4). Policy scenarios were modelled on evidence of the highest quality, which includes effectiveness of interventions at the individual level; time to the maximum effectiveness achieved and effectiveness over time; eligible population and exposure; and cost of running the intervention.
To assess the population-level impact of a scenario, model outputs were evaluated against a “business-as-usual” scenario, in which age‑ and sex-specific exposures to risk factors remain unchanged over 2020‑50, and the provision of preventive and health services is implemented at the current levels, specific to a country. Comparison of the business-as-usual scenario and the analysis scenario returned the impact on health, health care expenditure and labour market outcomes. The impact on labour market outcomes was evaluated using the human capital approach, which is based on assumptions including, for example, those on reserve labour force, friction costs and the impact on reserve wages. To assess the uncertainty of the effectiveness of an intervention, a sensitivity analysis was undertaken to look at the variability of the estimates of the impact of the policy interventions.
Assessment of the long-term effects of a scenario (either policy scenario or the burden of different levels of consumption) on the whole economy was carried out by linking the OECD SPHeP-NCDs model and the OECD long-term economic model, which is a macroeconomic model. The two models are linked through changes in population structure and life expectancy, employment and productivity and health care expenditure to measure their impact on GDP and fiscal pressure. The calculation of the costs presented in this report does not take into account some dimensions. For example, the analysis does not include the following costs:
the cost of justice (e.g. alcohol-related violence and injuries)
expenditure on lobbying and litigation to avoid the implementation of policies incurred by the industry
the cost to counter industry-led actions incurred by the government and civil society organisations
the social burden of alcohol use related to, for example, unwanted teenage pregnancies and the long-term consequences of foetal alcohol syndrome
broader factors related to social bonding and pleasure of drinking in moderation, maintenance of the landscape and vineyards, tourism and potential population resistance to stringent policy-making.
The analysis makes no assumptions about substitution effects from alcohol to other goods and services that could result from an intervention, which could mitigate the effects on the wider economy (e.g. tax revenues or employment).
For more information on the OECD SPHeP-NCDs model, see Box 4.1 in Chapter 4 and Box 7.1 in Chapter 7, and the SPHeP-NCDs Technical Documentation, available at: http://oecdpublichealthexplorer.org/ncd-doc.
Alcohol-related medical conditions, including chronic diseases and injuries, produce detrimental long-term consequences and reduce the quality of life of the affected individuals. In addition, many of these conditions cannot be cured, and increase the probability of premature mortality. The burden of disease caused by drinking more than the 1/1.5 drinks per day cap is significant:
Over the period 2020‑50, diseases caused by this level of alcohol consumption will reduce life expectancy by about 0.9 years across OECD countries. In individual countries, life expectancy will be reduced by between 0.01 years in Saudi Arabia and 1.90 years in Lithuania (Figure 1.2).
As many as 1.1 million people will die prematurely in OECD, EU27 and G20 countries by 2050. On average in OECD countries, 24 people per 100 000 population will die prematurely each year due to alcohol consumption above the 1/1.5 drinks per day cap. In the EU27, this average is higher, at 28 per 100 000, mostly driven by relatively high premature mortality rates in Central and Eastern European countries.
Related diseases greatly affect a person’s quality of life. Drinking above the 1/1.5 drinks per day cap causes 1.1 billion cases of dependence, corresponding to 88% of all cases. Similarly, this level of drinking is responsible for 38% of all cases of liver cirrhosis and 4% of all injuries.
Annual impact of alcohol consumption above 1 and 1.5 drinks per day for women and men, on life expectancy in years, average over 2020‑50
Not surprisingly, at the population level, the health burden (measured in terms of healthy life expectancy, an indicator capturing both the length of life and the quality of life) tends to be greatest in countries with higher volume and more detrimental patterns of alcohol consumption, such as Latvia and Lithuania, and lowest in countries with lower average consumption, such as Turkey and Israel.
The effectiveness of national health care services in treating the medical consequences of alcohol consumption can also influence the overall health burden. Effective health care systems can reduce complications and reduce fatalities, as in the case of certain cancers or cardiovascular diseases. For example, Canada and Iceland show a lower burden than other countries with similar levels of alcohol consumption, such as Estonia and Chile.
A further element to take into account is the contribution of other diseases not caused by alcohol (such as certain infectious diseases) in driving the total burden of disease in a country. For example, the burden of any alcohol consumption on liver cirrhosis is significant, but it can only explain a share of the total burden of cirrhosis across assessed countries. Other factors, such as viral hepatitis, would remain a significant driver of liver cirrhosis (particularly in countries where this group of infections is highly prevalent) even if all the cases linked to alcohol consumption were eliminated.
Previous analyses, using different methods, concluded that the impact of alcohol consumption on health expenditure would range between 1% and 7% of a country’s total health expenditure. New OECD calculations, based on the most recent evidence and cross-country comparable data applied to the OECD microsimulation model, broadly confirm this range of estimates and extend analyses to a comprehensive set of countries. The OECD analyses show that drinking more than the 1/1.5 drinks per day cap will significantly increase health expenditure in 2020‑50:
In OECD countries, 2.4% of total health spending will be devoted to treating diseases caused by drinking above the 1/1.5 drinks per day cap. Lithuania will devote nearly 4.2% of health expenditure to this, while Turkey will devote 0.12% (Figure 1.3). In total, USD PPP 138 billion per year will be spent across all the countries included in the analysis (OECD and partner countries, EU27 and G20 countries).
OECD countries will spend on average USD PPP 61 annually per capita. The United States (USD PPP 168 per capita), Luxembourg (USD PPP 143) and Germany (USD PPP 135) will spend the most (Figure 1.3).
Drinking above the 1/1.5 drinks per day cap is responsible, on average, for 87% of all treatment costs for dependence, 35% of treatment costs for cirrhosis and 4% of treatment costs for injuries and cancers.
Annual health expenditure due to diseases caused by alcohol consumption above the 1/1.5 drinks per day cap, in USD PPP per capita and as a percentage of total health expenditure, average 2020‑50
Not all cross-country variability in alcohol-related health expenditure can be attributed to differences in patterns of alcohol consumption. The price of delivering health care services, the mix of health care services used and the share of the population with access to effective health care services are some examples of factors that play a role in modulating total health expenditure. For example, Ireland, Luxembourg and the United States show an alcohol-related health burden just below the OECD average but, at the same time, they rank among the top countries in terms of alcohol-related disease impact on health expenditure. Conversely, Romania and Mexico show an impact of alcohol-related diseases on population health that is significantly higher than the corresponding impact on their health expenditure.
Analyses carried out with the OECD model used data from the Global Burden of Disease Study (GBD 2016 Alcohol Collaborators, 2018[21]) and accounted for a protective effect of alcohol consumption on ischaemic cardiovascular diseases and diabetes for some age groups. However, these effects are debated: some studies conclude that there is no protective cardiovascular effect once lifetime abstainers are separated from those who quit and do not drink for health reasons (Naimi et al., 2017[22]; Stockwell et al., 2016[23]). To account for this uncertainty around relative risks, a sensitivity analysis was carried out (only for OECD countries) to take out any protective effect. Results from the modified version of the model found that under the assumption of no protective effect of alcohol consumption:
Any alcohol consumption continues causing greater population health harms compared to drinking above the 1/1.5 drinks per day cap. For instance, any alcohol consumption contributes to lowering life expectancy by 1.1 years, compared to 0.8 years for the burden of drinking above the 1/1.5 drinks per day cap.
Medical conditions caused by any alcohol drinking lead to higher medical spending (USD PPP 58 per capita per year) compared to only drinking above the 1/1.5 drinks per day cap (USD PPP 52 per capita per year).
Medical conditions caused by any alcohol drinking contribute to a higher loss of employment and productivity (USD PPP 506 per capita per year) compared to drinking above the 1/1.5 drinks per day cap (USD PPP 334 per capita per year).
Estimates of the burden of any alcohol drinking obtained in the sensitivity analysis are higher than those in the analysis assuming some protective effects.
The OECD analysed micro-level data for adolescents aged 11‑15 in 32 countries and studied the association between performance at school and alcohol consumption. In many countries, adolescents who had never experienced drunkenness in their lifetime were more likely to report better performances at school. This was demonstrated, for example, by self-reporting of higher marks and lower probability of antisocial behaviours. Relationships are significant after controlling for mediating and confounding factors such as age, gender, family affluence, overweight categories and smoking status. Specific findings suggest that:
Girls had a higher probability of good performance at school compared to boys when they had never experienced drunkenness in all countries but Portugal. However, if they had ever experienced drunkenness, girls performed less well than boys in a third of the countries (10 countries).
An analysis of 29 OECD countries showed that from 2002 to 2014 the difference in school performance by drunkenness slightly widened among girls and remained constant among boys. Specifically, the data suggest a small but significant reduction in school performance among girls who had ever drunk and a stable trend among those who had never experienced drunkenness. Among boys, the trends in school performance were similar in both groups, maintaining a constant level of inequality.
On average across countries, boys and girls who had never experienced drunkenness were 30% more likely to perform well at school. The largest inequalities were seen in Iceland, Spain and Italy for boys, and in Iceland, Hungary and Belgium for girls. The lowest degree of inequality was observed in Denmark and Portugal for boys, and in the Czech Republic and Denmark for girls.
Children who reported frequent drunkenness were twice as likely as those who never drank alcohol to exhibit antisocial behaviour with their classmates. In particular, 50% of boys who had experienced drunkenness 11 times or more in their lifetime reported bullying their classmates, compared to 24% among abstainers.
Initiation of alcohol drinking was significantly associated with poorer school performance in 12 (out of 32) countries for boys and 15 countries for girls, with the strength of the relationship varying across countries. For instance, in Austria 69% of abstainer boys were likely to perform well at school compared to 66% of boys who had ever consumed alcohol. The gradient was steeper and significant in Belgium, where 69% of abstainer boys were likely to perform well compared to 61% of boys who had ever consumed alcohol.
Alcohol use is also negatively associated with life satisfaction, particularly in the case of girls. Specifically, girls who had never drunk alcohol self-reported a score of life satisfaction 27% higher than those who had been drunk more than ten times (score 7.74 vs. 6.10; i.e. 1.64 points higher on a scale of 0 to 10). For boys, the difference in life satisfaction score was 0.86 points (score 7.99 vs. 7.13), corresponding to a 12% higher score in those who had never drunk alcohol. The association between life satisfaction and alcohol consumption is complex, and other unmeasured factors such as mental health problems and trauma may underlie both outcomes.
Alcohol consumption in adolescents may also produce long-term consequences for educational outcomes. Analysis of longitudinal datasets from New Zealand, the United Kingdom, the United States and the Russian Federation suggests that, in the long term, students with harmful patterns of alcohol consumption may have lower educational performance and attainment, at least in some countries and particularly in the case of girls. Specifically, the OECD analyses found the following relationships to be statistically significant:
In the United States, monthly drinking was associated with a decrease in the grade point average (GPA)10 one year later of 0.11 points for boys and 0.11 points for girls, and weekly drinking with a decrease of 0.19 points for boys and 0.20 points for girls compared to those who rarely or never drank. Binge drinking has an even greater association with GPA, as weekly binge drinking is linked to a reduction in the GPA of boys (0.25 points) and girls (0.21 points). A reduction of 0.25 points would bring a student with the median GPA of 2.75 down to the fortieth percentile.
In the United States, girls who drank weekly were 21% less likely to complete higher education than those who rarely or never drank, and girls who binge drank weekly were 32% less likely to complete higher education.
In the United Kingdom, girls reporting weekly drinking during high school were more likely to leave full-time education 0.35 years earlier than girls who never or rarely drank. In addition, both sexes reporting binge drinking more than once in two weeks saw a decrease in the number of years spent in full-time education, by 0.60 years for boys and 0.56 years for girls, compared to those who never binge drank.
In New Zealand, weekly drinking was associated with a 0.56 year decrease in the age at which boys left full-time education.
Educational outcomes are key determinants for the formation of human capital and for the individual’s future socio‑economic status. Improving the cognitive skills of the population can lead to significant economic gains, and relatively small improvements to labour force skills can have a large impact on the future well-being of a nation.11 In addition, differences in health and health behaviours, resulting from alcohol use at young ages, can also reinforce existing social inequalities; this has an impact on social welfare. Differences in health at a young age are perpetuated in adulthood, and can lead to social inequalities, such as differences in job prospects and income gaps (Marmot, 2010[24]).
Alcohol use can influence educational outcomes through various pathways. First, alcohol use and related diseases (such as mental health issues) may have a direct biological effect on cognitive function and concentration at school – for example, by creating learning problems. Second, alcohol use can lead to behaviours that affect educational performance, such as lower attendance or commitment. Third, emotional or mental health factors related to alcohol use can affect educational performance. However, the relationship between alcohol use and educational outcomes is complex and multidirectional, and inverse relationships may also exist. In addition, a wide range of confounding factors may influence both the risk factors and the educational outcomes, such as family income, parental education, self-esteem and motivation.
Individuals with chronic diseases, including those caused by alcohol consumption, are more likely to be unemployed and to miss days of work. Further, when they are at work, they are less likely to be productive than healthy individuals. The new OECD analyses looked at the relationship between alcohol consumption and chronic diseases and how chronic diseases affect labour force productivity (Box 1.3). The analyses showed that chronic diseases caused by drinking more than the 1/1.5 drinks per day cap affect the productivity of the labour force by reducing the workforce by the equivalent of about 33 million people per year: about 26 million due to reduced employment, 5 million due to presenteeism and 2 million due to absenteeism in all the countries studied. When all these effects are converted into an economic value using the human capital approach, OECD countries lose about USD PPP 595 billion per year. This is roughly equivalent to the annual GDP of Belgium or Sweden.
At the macroeconomic level, medical conditions caused by drinking above the 1/1.5 drinks per day cap and their broader societal consequences causes GDP to be 1.6% lower on average in OECD countries over the next 30 years (Figure 1.4). The impact on G20 countries is slightly smaller, with GDP 1.4% lower, but larger in 24 EU countries, at 1.9%. In absolute terms, and across all the 48 countries included in the analysis, this impact on GDP translates into a loss of about USD PPP 1.6 trillion per year from 2020 to 2050 – similar to the average annual GDP of Canada or Spain.
Percentage difference in GDP due to diseases caused by alcohol consumption above the 1/1.5 drinks per day cap, average 2020‑50
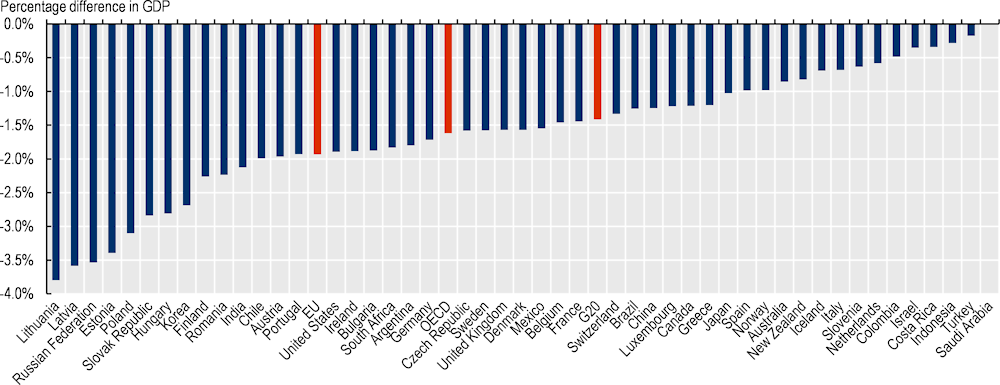
Source: OECD analyses based on the OECD SPHeP-NCDs model and OECD long-term economic model, 2020.
Medical conditions caused by drinking above the 1/1.5 drinks per day cap and their broader societal consequences also exact a heavy toll on personal budgets. All these factors are responsible for a 0.43 percentage point increase in total fiscal pressure, measured as government primary revenue as a share of GDP. This is equivalent to an increase in tax rate of USD PPP 232 per capita per year in OECD countries. In Ireland, the OECD country experiencing the highest impact, the disease‑mediated consequences of drinking above the 1/1.5 drinks per day cap cost more than USD PPP 573 per capita per year. Other countries that show a significant impact on fiscal pressure include the United States, Austria and Sweden.
Alongside the evaluation of the impact of alcohol consumption above the 1/1.5 drinks per day cap, the OECD models were used to calculate the impact of all alcohol-related diseases. This is not considered a policy option in itself; rather, an interesting thought experiment. The risk of some diseases such as alcohol dependence, cancers, cirrhosis and injuries is increased even at low levels of alcohol consumption, and this has an impact on other related dimensions, such as health care expenditure, labour force productivity and the economy. The OECD model calculated that cumulatively over the next 30 years in 52 countries:
An extra 4.2 people per 100 000 population will die prematurely, causing a loss of an additional two months on the population’s life expectancy. This is a 17% greater reduction in life expectancy compared to drinking above the 1/1.5 drinks per day cap.
Compared to drinking above the 1/1.5 drinks per day cap, it is estimated that individuals will develop approximately 14% more cases of dependence (1 263 million cases) as well as 128% more cases of injuries (48 million cases) and 97% more cases of cancers (10 million cases).1
The burden of all alcohol-related diseases on health expenditure will be USD PPP 40 per capita per year. The small protective effect of alcohol on ischaemic cardiovascular diseases (Box 1.4) and longer life expectancy are the main drivers explaining the difference between the two estimates.
On average, all alcohol-related diseases will contribute to a loss in productivity equal to USD PPP 404 per capita annually. This is about 45% larger in magnitude than the USD PPP 278 economic loss resulting from the diseases attributable to alcohol consumption above the 1/1.5 drinks per day cap.
All alcohol-related diseases will cause GDP to be 2.1% lower on average. This is greater than the 1.6% difference resulting from the diseases attributable to alcohol consumption above the 1/1.5 drinks per day cap.
In the OECD, the tax rate will be 0.51 percentage points of GDP higher due to all the alcohol-related diseases. This is greater than the 0.40 percentage points of GDP found in the scenario looking at alcohol consumption above the 1/1.5 drinks per day cap.
1. The OECD analyses do not take into account the impact of alcohol consumption on foetal alcohol spectrum disorder (FASD) and foetal alcohol syndrome, which are two highly crippling and prevalent conditions. For example, FASD is estimated at 19.8 per 1 000 population of children and young people in European countries (Lange et al., 2017[25]).
The rationale for government intervention to tackle harmful alcohol consumption is strong and has a global mandate. In 2010, WHO Member States agreed to the Global Strategy to Reduce the Harmful Use of Alcohol (WHO, 2010[1]), thereby recognising the issue as a key public health priority. As part of the Global Strategy, ten target areas were identified to assist national policy-makers with developing an effective, holistic policy response. More recently, given that harmful alcohol use is a key risk factor for NCDs, the Global Strategy played an important role in shaping the WHO Global NCD Action Plan 2013‑20 (WHO, 2013[26]), which includes a specific global target to reduce harmful use of alcohol by 10%. Finally, the United Nations Sustainable Development Goals, as part of its target to ensure healthy lives and promote well-being (Goal 3), includes a target to reduce harmful alcohol use in line with the Global Strategy. Specifically, target 3.5 relates to strengthening the prevention and treatment of substance abuse, including alcohol.
At the national level, the fight against harmful alcohol consumption has advanced primarily around national action plans, sometimes developed on the basis of the WHO Global Strategy and relevant global action plans. The ability of governments to design, implement and monitor the effectiveness of prevention strategies, which combine different best practice policy approaches, is critical to success.
OECD countries can further upscale their policy action to tackle harmful consumption of alcohol. Of the 37 OECD member countries, 32 have a written alcohol policy in place, and almost half (17 countries) also have a specific action plan for their national policy (Figure 1.5). Similarly, the vast majority of G20 countries have a written alcohol policy, and South Africa is the only non-OECD G20 country that also has a national action plan.
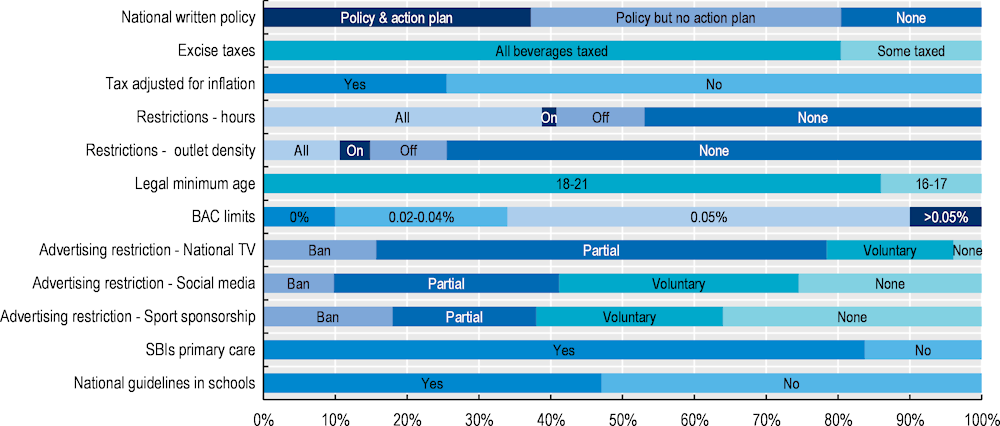
Note: The figure includes information for OECD countries, non-OECD European countries, non-OECD G20 countries and OECD accession countries. BAC = blood alcohol concentration. SBIs = screening and brief interventions. A similar figure, focusing only on OECD countries can be found in Annex Figure 1.A.1.Results do not include missing data.
Source: WHO (2020[27]) Global Information System on Alcohol and Health (GISAH), https://www.who.int/data/gho/data/themes/global-information-system-on-alcohol-and-health.
Most OECD countries have implemented a wide range of policies to tackle harmful alcohol consumption. Despite this, the implementation of policies “on the ground” and their effectiveness at the population level are hindered by a number of factors. In some cases, policies are implemented in forms that are not the most effective or may not be uniformly implemented throughout the country. In other cases, the policy may not be implemented as intended. Finally, limited resources or practical problems may end up limiting the number of individuals that may benefit from the policy.
By reviewing available evidence and international datasets, OECD work has identified six categories of policy broadly implemented by countries. These domains include those within WHO’s SAFER framework in addition to consumer information (WHO, 2018[28]):
policies to modify the cost of alcohol
policies to modify the availability of alcohol
policies to counter drink-driving
policies to regulate alcohol marketing
policies to enhance screening, brief interventions and treatment
policies to modify consumption through consumer information.
Given the complexity of tackling harmful consumption of alcohol, the review also identified that countries generally implement a set of complementary policies to create an environment that hinders harmful drinking. For example, since the mid‑1990s, the Russian Federation has implemented significant policy reforms including policies targeting pricing, production, drink-driving, availability and advertising. WHO evaluated that, because of these reforms, between 2003 and 2016 alcohol consumption fell by 43%, with significant decreases in heavy episodic drinking (WHO Regional Office for Europe, 2019[29]). Alcohol dependence and mortality also fell markedly over this period; regarding the latter, rates of death attributable to suicide dropped by approximately 60%, homicides by approximately 80% and transport crashes by over 50%.
In the OECD, Ireland is among the countries currently in the process of reforming their alcohol strategy. In 2018, Ireland approved the Public Health (Alcohol) Act to reduce annual alcohol consumption by 2 litres per person by 2020. Example policies in the Act include minimum unit pricing (MUP); restrictions/bans on alcohol sponsorship during certain events; restrictions on alcohol advertising across different media and locations, as well on advertisement content; restrictions on promotions such as “buy one get one free”; and health labelling on alcohol products including energy value, alcohol content and health risks.
Policies to modify the price of alcohol are among the most widely implemented interventions by OECD, EU27 and G20 countries, and may take a number of forms. Various forms of taxation, such as unitary tax (based on the size of the beverage), volumetric tax (based on the ethanol content) and ad valorem tax (based on the value of the beverage) have been used for many years, either in isolation or in combination with one another. MUP is a more recent policy intervention that aims to set a mandatory floor price per unit of alcohol or standard drink.12 Finally, policies to increase the price of alcohol may take different forms such as bans on below-cost selling; bans on volume discounts; and minimum mark-ups and profit margins, which cap minimum profit margins for wholesalers and retailers.
An OECD review of policies to modify the cost of alcohol concluded that 80% of reviewed countries mandate taxation for all beverage types, with the remaining countries taxing only beer and spirits. Countries may also choose to combine taxes, as in Australia, where beer and spirits are subject to a volumetric tax and wine is subject to an ad valorem tax. In addition to excise taxes, alcohol products in all OECD countries are subject to a value‑added tax (VAT), ranging between 7.7% (Switzerland) and 27% (Hungary). Only 27% of OECD countries periodically adjust alcohol taxes for inflation, while the remainder do not have an automatic system in place. Implementing such a mechanism is particularly important for unitary and volumetric taxes, as opposed to ad valorem taxes, as otherwise the impact of the excise tax decreases over time, contributing to making alcoholic beverages more affordable (Box 1.6). A common approach to ensure a periodic adjustment of the excise tax is to link it to consumer price indexes; this is done in Australia, Italy and Israel, among others.
In addition to such taxes, some governments have become increasingly interested in MUP. The main characteristic of MUP is that it specifically targets cheap alcoholic beverages. In addition, unlike taxes, it prevents retailers from absorbing the additional cost of production. Finally, MUP is particularly effective in targeting people with problematic drinking and young people, as these population groups are more likely to consume cheap forms of alcohol. Several countries have implemented MUP, including Canada (British Columbia, Manitoba, Newfoundland and Labrador, Nova Scotia and Quebec), one territory in Australia, the United Kingdom (Scotland and Wales) and the Russian Federation. An OECD analysis of the implementation of MUP in OECD countries found great variability across jurisdictions. Specifically, MUP was found to be USD 1.09‑1.10 per standard drink in Scotland and Wales (United Kingdom) and between USD 2.26‑3.42 plus taxes per standard drink in British Columbia (Canada), depending on the type of alcohol product.
Alcohol affordability is a determinant of alcohol consumption and is affected by three key factors: income, the price of alcohol (which is influenced by taxation) and the price of other goods.
OECD analysed alcohol affordability in the off-premise market (e.g. supermarkets) across several European countries and Australia, Canada and the United States for the period 2000‑18 (Figure 1.6). Findings from this analysis show that:
Across the 28 OECD countries analysed, alcohol affordability in off-premise market increased by nearly 50% over the period. This means that in 2018, purchasing the same quantity of alcohol was on average 50% more affordable when compared to 2000, once changes in real income and the relative price of alcohol are taken into account.
Alcohol became more affordable in the majority of countries, particularly among those located in Eastern Europe. Only three countries experienced a decline in affordability, by 33% (Iceland), 30% (Greece) and 4% (Italy).
Alcohol affordability index (index year 2000 = 100)
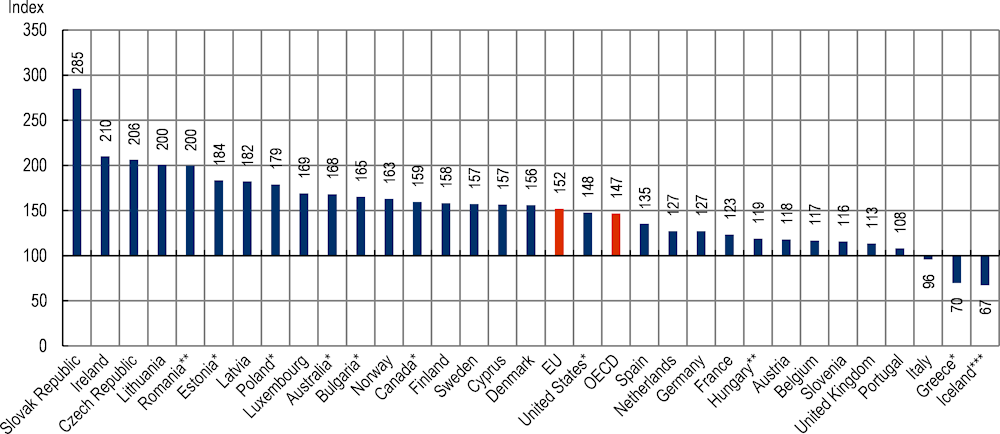
Note: An alcohol affordability value below 100 indicates that alcohol is less affordable owing to either (or both) a decline in real income or a rise in the relative price of alcohol, and vice versa. *Latest data from 2017, **starting year 2001, ***latest data from 2014. Missing data in Europe for Turkey, Switzerland, Croatia and Malta.
Source: Eurostat (2019[30]), Harmonised Index Of Consumer Prices: All items, https://ec.europa.eu/eurostat/databrowser/view/prc_hicp_aind/default/table?lang=en; Eurostat (2019[31]), Harmonised Index Of Consumer Prices: Alcoholic beverages, https://ec.europa.eu/eurostat/databrowser/view/PRC_HICP_AIND__custom_287314/default/table?lang=en; Eurostat (2019[32]), Adjusted Disposable Income, Gross, https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do; Australian Bureau of Statistics (2019[33]), 6401.0 Consumer Price Index: Alcoholic beverages, https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/dec-2019; Australian Bureau of Statistics (2019[34]), 6401.0 Consumer Price Index, All groups CPI, https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/dec-2019; Statistics Canada (2019[35]), Table 18‑10‑0005‑01 Consumer Price Index: Annual average, not seasonally adjusted, https://doi.org/10.25318/1810000501-eng; U.S. Bureau of Labor Statistics (2019[36]), Alcoholic Beverages in U.S. City Average: All urban consumers, not seasonally adjusted (series ID: CUUR0000SAF116), https://www.bls.gov/cpi/#data.
The main driver of alcohol affordability was examined for the period 2013‑18. This period was chosen to limit the influence of the global financial crisis and the subsequent marked fall in real income. Nevertheless, the analysis found that rising real incomes were behind the increase in affordability in the majority of countries studied (i.e. growth in real income exceeded growth in the relative price of alcohol) (Figure 1.7). Exceptions, however, included Belgium, Estonia, Greece, Sweden and the United Kingdom. For example, in Belgium, real income rose by 5%, which was lower than the 9% increase in the relative price of alcohol, causing alcohol affordability to decline.
Of the eight countries that saw a decline in the relative price of alcohol between 2013 and 2018, seven do not adjust their alcohol excise tax rate for inflation (including the United Kingdom, Ireland and Norway). Conversely, countries that do adjust for inflation – Australia, Belgium, Canada, France, Italy and Spain – experienced either no change or an increase in the relative price of alcohol.
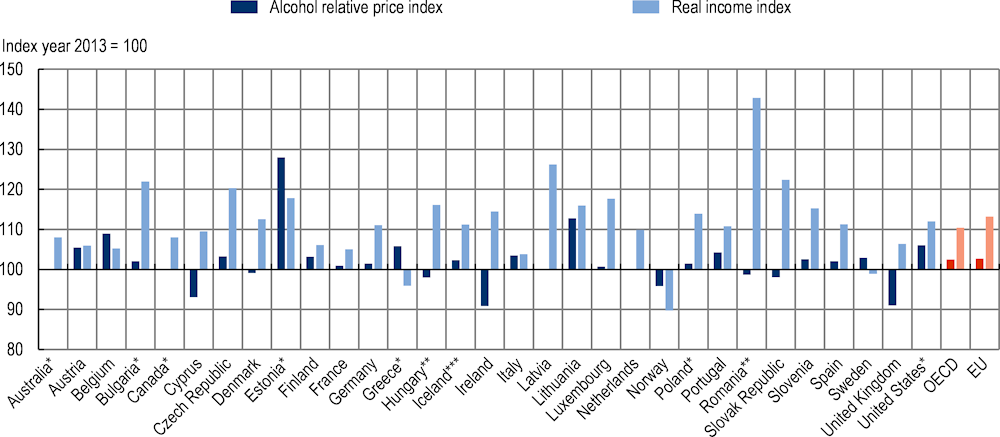
Note: For the alcohol relative price index, a figure above 100 indicates that alcohol is more expensive, while for the real income index, a figure above 100 indicates that real income has risen. *Latest data from 2017; **starting year 2001; ***latest data from 2014. Data are missing for Croatia and Switzerland in Europe.
Source: Eurostat (2019[30]), Harmonised Index of Consumer Prices: All items, https://ec.europa.eu/eurostat/databrowser/view/prc_hicp_aind/default/table?lang=en; Eurostat (2019[31]), Harmonised Index of Consumer Prices: Alcoholic beverages, https://ec.europa.eu/eurostat/databrowser/view/PRC_HICP_AIND__custom_287314/default/table?lang=en; Eurostat (2019[32]), Adjusted Disposable Income, Gross, https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do; Australian Bureau of Statistics (2019[33]), 6401.0 Consumer Price Index: Alcoholic beverages, https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/dec-2019; Australian Bureau of Statistics (2019[34]), 6401.0 Consumer Price Index: All groups CPI, https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/dec-2019; Statistics Canada (2019[35]), Table 18‑10‑0005‑01 Consumer Price Index: Annual average, not seasonally adjusted, https://doi.org/10.25318/1810000501-eng; U.S. Bureau of Labor Statistics (2019[36]), Alcoholic Beverages in U.S. City Average: All urban consumers, not seasonally adjusted (series ID: CUUR0000SAF116), https://www.bls.gov/cpi/#data.
Traditional policies under this heading include, for example, restrictions on hours and days of alcohol sales, restrictions on the density of alcohol outlets and minimum legal purchasing age. While different in their implementation, the objective of all these actions is to limit the opportunity for people to purchase and consume alcohol to specific hours of the day (or days of the week), to specific population groups or, finally, to a limited number of outlets in a given area. Restrictions may apply to on-premise (e.g. restaurants and bars) and/or off-premise establishments (e.g. liquor stores). In the case of restrictions on hours and days of alcohol sales, the intervention typically targets late‑night drinking in order to reduce alcohol-related violence and injury or, in the case of sales restrictions during days, drinking during the weekend.
About half (53%) of countries included in the analysis restrict alcohol sales to specific hours; a similar proportion of countries apply no restrictions at all. Among countries implementing such a policy, the majority (73%) restrict sales in both on- and off-premise outlets, with another 23% of countries only restricting sales in off-premise outlets. The remaining 4% of countries instead restrict on-premise sales. Restrictions according to the day (such as on a public holiday) tend to be significantly less common. For example, in the OECD, just 11% of countries apply this restriction to both premise types, while 73% of countries apply no restrictions (the remainder of countries either have no data or apply restrictions to off-premise establishments only).
In addition to restricting hours and days of sale, policy-makers may also limit the number and concentration (e.g. by population size) of outlets in a given area with a permit to sell alcohol (for consumption on site or elsewhere). The sale of alcohol can also be restricted by the location and type of outlet, such as petrol stations. For example, as of January 2020, Lithuania has banned alcohol sales on beaches and pavilions, as well as during public events for drinks with an alcohol content above 7.5%. While recommended by WHO, restricting the number of outlets is only applied by a minority of countries. Only about one in four countries reviewed have some form of restriction on outlet density – either for on- and off-premise outlets (11%), or for on-premise (4%) or off-premise (11%) outlets only. Among OECD countries, Chile and Ireland restrict outlet density for on- and off-premise outlets, while in Canada responsibility for regulating outlet density lies with municipalities (with the exception of New Brunswick and Prince Edward Island for off-premise outlets). Jurisdictions with the greatest restrictions on outlet density are Quebec, Alberta, British Columbia, Manitoba and Yukon.
In all the countries reviewed, the legally mandated minimum age for purchasing alcohol ranges from 16 to 21 years, with 86% of countries setting the minimum threshold at 18 years or above. Among OECD countries, 84% apply the same threshold across all alcohol types. Country exceptions typically increase the minimum age by two years for spirits. For example, in Norway and Finland (off-premise), the minimum age is 18 for beer and wine and 20 for spirits.
Policies to counter drink-driving are among the most common implemented by countries. A frequently applied policy is to set blood alcohol concentration (BAC) limits, given that for every 0.02% increase in the proportion of alcohol in a person’s bloodstream, the probability of being in a fatal motor vehicle crash increases by approximately 70% (Taylor and Rehm, 2012[37]). However, BAC limits alone are not sufficient to alter behaviours and, therefore, to reduce alcohol-related crashes. Drivers must also believe that they are at risk of being identified and prevented from driving under the influence of alcohol. Therefore, other policies within this category aim to enforce BAC limits and to limit the possibility that people with a BAC above the threshold will drive a vehicle. Policy tools commonly employed by countries include sobriety checkpoints, penalties for drink-driving and, to a lesser extent, ignition interlock systems.
All countries included in the review enforce a BAC limit, but significant variation exists on the maximum limit. The majority of countries (56%) set the BAC limit at 0.05% for the general population; another 34% set BAC limits at lower than 0.05%. The highest BAC limit is 0.08% and is enforced in five countries: Canada, Mexico, Malta, the United Kingdom (with the exception of Scotland, which is set at 0.05%) and the United States (with the exception of Utah). Conversely, Brazil, the Czech Republic, Hungary, Romania and the Slovak Republic enforce a zero tolerance policy (i.e. the maximum BAC level is 0.00%). In addition, it is common for countries to employ lower BAC limits for novice or young drivers and professional drivers than for those in the general population. In the OECD, over half of member countries (21 countries) enforce lower BAC limits for professional and novice/young drivers. In these countries, BAC limits range between zero tolerance and 0.03% for professional and novice/young drivers.
Enforcement of sobriety checkpoints is also commonly employed. Sobriety checkpoints can be implemented in two forms. The first type – selective breath tests – consists of pre‑determined checkpoints where police officers must have reason to believe the driver is under the influence of alcohol to test blood alcohol levels. Under the second type – random breath tests – drivers are selected at a random to have their blood alcohol level tested. With the exception of Mexico, all OECD member countries implement one or both sobriety checkpoints. To maximise their potential, it is important that sobriety checkpoints are widely publicised, highly visible and conducted frequently.
If drink-drivers are identified, they are subject to penalties or, in some countries, to compulsory participation in an ignition interlock programme. The majority of OECD member countries (33 countries) penalise drink-drivers by suspending or revoking their licence and/or imposing a fine. Long- or short-term detention is another common tool to punish drink-drivers (in 27 countries), and to a lesser extent vehicle impoundment, mandatory treatment and community service. Penalties typically become stricter for repeat offenders. Some countries also implement ignition interlock programmes, which require drivers to take a breath test to assess their blood alcohol level in order to start their vehicle. The review found that five OECD countries (Belgium, Canada, Denmark, France and certain states in the United States) currently penalise first-time drink-drivers with ignition interlocks; in some places (New Zealand and certain states in the United States) this penalty is used for repeat offenders.
This category of policies includes all actions to regulate the promotion and marketing of alcohol products. The OECD review focused on some of the most common forms of regulation, particularly related to regulation of advertising on traditional media platforms (e.g. television, radio and print media) and new digital media platforms (e.g. social media), as well as on sport sponsorship. However, other forms of policy exist that target advertising through, for example, direct mail and product placement, which entails placing a specific product in another work – such as a film – with promotional intent. The policy-making process in this category is changing more rapidly than in other sectors, particularly in the case of new digital media, to follow the evolution of the technology.
Restrictions on marketing efforts – how, when and where they can be used and who they can target – are widely applied, although very few countries have comprehensive bans in place. Across analysed countries, 96% employ some form of restriction on alcohol advertising on national TV, and only two countries – Chile and Croatia (only for beer) – do not implement any restrictions. However, in the majority of cases, restrictions are implemented as either partial restrictions (i.e. the restriction applies during a certain time of day or for a certain place, or to the content of events) or voluntary restrictions (i.e. the alcoholic beverage industry follows its internal voluntary rules). Evidence regarding the effectiveness of voluntary restrictions indicates that young people are frequently exposed to alcohol advertisements under this arrangement (Noel, Babor and Robaina, 2017[38]). Specifically, 63% of the countries reviewed enforce partial restrictions, while 18% employ voluntary restrictions. Only seven OECD countries and one non-OECD G20 country (16% of the countries reviewed) enforce statutory bans. Active surveillance to monitor adherence to regulations also exists and is implemented by 35 of the 37 OECD member countries. In Australia, alcohol marketing is characterised as a “quasi-regulatory” system, with guidelines set by industry, advertising and government representatives. Similar arrangements exist in the United Kingdom, New Zealand and Japan.
During the last few years, the advertising landscape has altered significantly, with brands shifting their focus from traditional forms of media to digital media platforms, including social media. This is reflected by advertising expenditure – for example, in the United Kingdom, online advertising expenditure grew by 189% between 2007 and 2016; conversely, television experienced a 2% decline (Ofcom, 2017[39]). Despite this, fewer OECD countries have regulatory arrangements in place to limit alcohol advertising via social media compared to via traditional media. Further, where regulatory arrangements do exist, they are partial restrictions. The review of policies in place to limit advertising on digital media platforms found that 25% of countries do not have any regulation in place and that another 33% employ voluntary regulation. A further 31% of countries enforce partial bans, while only five countries (10% of the countries reviewed) have a statutory ban in place, including Lithuania, Norway and Turkey in the OECD.
The alcohol industry is a key sponsor of sporting events, sporting teams and individual athletes across the world, as this is a vast sector, providing high levels of exposure. In addition, available evidence shows that alcohol sponsorship in sport is associated with initiation of drinking for previous abstainers and higher levels of consumption among people who currently drink (Smith and Foxcroft, 2009[40]; Houghton et al., 2014[41]). In response to these concerns, 64% of countries reviewed have implemented some form of ban to restrict the alcohol industry’s influence in sport. In the OECD, Spain, France, Norway and Turkey have implemented legally binding bans on sport sponsorship across all beverages. A further 17 countries apply partial or voluntary restrictions (e.g. restrictions on sponsoring sporting teams and/or sporting events), while 14 countries apply no restrictions.
The health system response to tackling harmful alcohol use mainly includes two types of policy, which aim to identify individuals with a real or potential problem with alcohol and to help them address the issue through motivation and/or pharmaceutical support. Screening and brief interventions (SBIs) is an example of this group of interventions. SBIs target people who consume hazardous amounts of alcohol that are identified through standard questionnaires (e.g. AUDIT, CAGE or FAST). Those identified as at risk receive further assistance via a brief intervention. Specialised treatment for people who are dependent on alcohol is another intervention in this category that specifically targets patients with alcohol use disorders, particularly in the most severe forms. The intervention entails more intensive treatment and pharmacotherapy.
Among the countries reviewed, 84% have developed and implemented national guidelines and standards of care for SBIs in primary care related to hazardous and harmful alcohol use. In the OECD, only three countries – Greece, Korea and the Slovak Republic – do not report SBI guidelines for alcohol use in primary care. Conversely, in some countries such as England (United Kingdom), SBIs are undertaken as part of a normal health check. In other countries such as Finland, Hungary, Latvia, the Netherlands, Portugal, Spain, Sweden and the rest of the United Kingdom, SBIs are also used in emergency departments and during obstetric visits. Outside the sector, SBIs are used by workplaces, particularly in fields where harmful alcohol use is dangerous to others (e.g. driving, public safety and national security roles), but these initiatives are often rolled out by the private sector and comprehensive mapping of their implementation is not possible. Finally, advances in technology are increasingly allowing replacement of traditional face‑to-face interventions with digital interventions. For example, this is an approach being implemented in Australia.
One of the characteristics of this category of interventions is that they target populations at high risk and those that have already developed dependency without affecting individuals with low and moderate levels of alcohol consumption. Despite the high share of countries reporting the existence of guidelines for this type of intervention, their implementation on the ground has significant room for improvement. Finding recent data on the actual coverage is difficult but, for example, a WHO publication in 2009 concluded that less than 10% of the population at risk for harmful alcohol consumption are routinely identified, and less than half of those diagnosed are offered advice (WHO Regional Office for Europe, 2009[42]).
Communication-based approaches are among the most widely implemented public health interventions by OECD countries, and may take a number of forms. For example, in the field of tackling harmful alcohol consumption, they can help consumers make informed purchases by providing relevant information on alcohol container labels. They can be employed as part of health promotion and social marketing campaigns, including through the use of mobile apps, aimed at increasing awareness and at changing patterns of alcohol consumption. They can also be used to support other disease prevention policies, such as aiding health education campaigns targeting schoolchildren and other population groups.
Information provided by alcohol container labels differs across OECD member countries, with no uniform approach applied. Generally, the review identified two main types of labels.
Nutritional information aims to educate consumers on relevant nutritional aspects – mainly calorie content – of the specific alcoholic product. Across the OECD, only five countries have a national legal requirement to provide consumers with calorie information on all alcohol containers: Greece, Ireland, Israel, Mexico and Turkey. Several other countries have engaged, or plan to engage, in voluntary agreements with industry to provide this information. For example, at the EU level, signed memorandums of understanding committed representatives of the spirits industry to provide energy labels on 66% of all spirit containers and Brewers of Europe to provide energy labels on all beer bottles and cans by the end of 2022.
Health warnings aim to inform consumers of the potential health risks associated with consuming alcohol. Health warning labels on alcohol containers are currently mandatory in 12 OECD countries (Colombia, France, Greece, Israel, Japan, Lithuania, Mexico, Norway, Korea, Portugal, Turkey and the United States), and are in the process of implementation in another three (Australia, Ireland and New Zealand). However, several other countries have voluntary arrangements in place.
While there is little evidence to suggest that mass media campaigns reduce alcohol consumption (Young et al., 2018[43]), they are a commonly implemented policy tool among OECD countries. Different forms of mass media campaigns exist and include those focusing on tackling drink-driving; those aiming to improve awareness and knowledge of the long-term risks associated with alcohol consumption; and those “challenging” people to abstain from alcohol for one month. Several other campaigns are also in use, including those targeted at short-term consequences (e.g. financial consequences or “hangovers”) and parental behaviour (e.g. educating parents on how their actions influence a child’s attitude towards alcohol).
Despite being illegal, it is common for underage schoolchildren to consume alcohol. This is cause of concern for many reasons, including – as discussed in Section 1.2.3 – poorer performance at school and lower life satisfaction. For reasons such as those outlined above, school-based drug prevention programmes are common across the countries reviewed: 47% have in place national guidelines regarding prevention and reduction of alcohol-related harm in schools. This figure increases to 51% when considering only OECD countries. If a country has no national school guidelines, however, it does not necessarily mean that students are not accessing alcohol prevention programmes.
To tackle harmful alcohol consumption, countries should upscale their efforts, both by implementing new policy options and by strengthening policies currently in place. Drawing on available evidence, the OECD used its microsimulation model to assess the impact on population health, health expenditure and the broader economy of a comprehensive set of highly effective policy actions (Table 1.1 and Annex Table 1.A.1). The choice of policies modelled was based on a number of criteria, including the availability of quantitative evidence to feed the OECD model. In addition, these policies needed to be aligned with the WHO Global Strategy to Reduce the Harmful Use of Alcohol (WHO, 2010[1]) and, ideally, to be part of countries’ policy priorities. Finally, as far as possible, policies were selected with the objective of covering a multitude of targets and providing a comprehensive set of options, depending on countries’ policy priorities. For example, individuals with patterns of high-risk drinking are specifically targeted by health care policies and workplace‑based programmes, and are highly responsive to MUP – given that they are more likely to consume cheap alcohol, which is specifically targeted by MUP. Children are instead most responsive to regulation of advertising, and are specifically targeted by school-based interventions. Injuries and violence are prevented particularly effectively by restrictions on outlet opening hours and sobriety checkpoints. Actions were also combined into four “policy packages”, including both existing and innovative policies, to show the advantages of comprehensive strategies, in line with the discussion in Section 1.3. The analysis assumes that interventions are implemented at the beginning of 2020, and the impact of interventions is assessed for 30 years, up to 2050.13 It covers up to 48 countries, including OECD countries together with other non-OECD EU27 Member States, Brazil, the People’s Republic of China, Costa Rica, India, the Russian Federation and South Africa.
Simulation models like the one used in the OECD analysis have many strengths. They can provide evidence in areas in which direct empirical investigation may be difficult or impossible. However, they also require assumptions, and have to rely on a variety of input data, which may vary in terms of quality. Further, they simplify certain aspects by including in the calculation only particular dimensions, depending on the availability of high-quality data (see Box 1.3 above). Finally, outputs from models cannot replace the need for policy-makers to decide where to strike a balance between different policy options but, as in the case of this analysis, they can provide detailed estimates of policy impacts, thereby supporting an evidence‑based approach to such decisions.
|
Regulation and/or restriction of alcohol |
Pricing policies |
Health care policies to advise and treat people |
Health education and promotion |
|---|---|---|---|
|
Restrictions on outlet opening hours |
Alcohol taxation |
Alcohol counselling in primary care |
School-based programmes |
|
Statutory ban on alcohol advertising to children |
MUP |
Personalised pharmacological treatment |
Workplace‑based programmes |
|
Regulation of alcohol advertising |
|||
|
Sobriety checkpoints |
Findings from the OECD microsimulation model show that all the assessed interventions have the potential to promote population health, produce savings in health expenditure and increase labour force participation and productivity. The return on investment is extremely high for many of the assessed policies. In some cases, however, the average return on investment across countries is below 1, meaning that each USD 1 invested in these policies produces an impact on GDP lower than the investment.
Pricing policies and some interventions to regulate and/or restrict alcohol (restrictions on outlet opening hours and sobriety checkpoints) consistently show the highest impact on the assessed outcomes. Three reasons may explain why these interventions are particularly effective. First, these are all population-wide actions, affecting a large share of the population: virtually all people who drink – not just those who drink heavily – in the case of price policies and regulation of opening hours. Second, some of these interventions have a specific focus on people who engage in high-risk drinking, as is the case for sobriety checkpoints and for MUP, which has a larger impact on people who engage in hazardous and harmful drinking. Third, interventions such as restrictions on outlet opening hours and sobriety checkpoints have a direct effect on injuries and assaults, which can produce long-term benefits – for example, in the case of young adults killed in car crashes.
Actions targeting either specific individuals (alcohol counselling in primary care and personalised pharmacological treatment) or specific population groups (e.g. individuals employed in medium-sized and large‑sized enterprises through workplace‑based programmes) target high-risk individuals and patients with either alcohol dependence or alcohol use disorders, and can produce a significant short- to medium-term benefit in those exposed to the intervention. An additional advantage of these interventions is that they do not affect other individuals, such as those that do not have dependence. As described in Section 1.3.5, these interventions currently cover only a very limited share of the potential beneficiaries, and there is great potential for improvement, even beyond the level investigated by this analysis. Among this group of interventions, upscaling coverage of alcohol counselling in primary care to cover 20% of people who drink heavily and who are not alcohol dependent shows the most positive impact on the assessed outcomes and, particularly, on containing health expenditure.
Finally, actions targeting children and regulation of advertising generally show the smallest impact over a 30‑year period. While some of the actions targeting children are particularly effective (for example, statutory bans on alcohol advertising to children decrease underage drinking by 35%), they generally require longer periods to produce significant health effects at the population level, so the potential of these policies is not fully captured by an analysis over 30 years. In addition, for some of these interventions, such as school-based interventions, the evidence suggests no long-term effects after the end of the period of exposure (MacArthur et al., 2018[44]). In the case of regulation of advertising, this is an intervention entailing only partial restrictions – rather than a comprehensive statutory ban – limiting, but not avoiding, exposure to alcohol advertising.
Overall, the assessed policies may significantly reduce the burden of disease caused by harmful alcohol consumption, and may increase population health. The impact of actions on morbidity (measured in disability-adjusted life years – DALYs), taking into account how chronic diseases affect quality of life, is generally greater than their impact on mortality (measured in LYs), indicating that public health actions delay the development of chronic diseases to later in life, rather than preventing their development completely. Specifically, findings from the OECD microsimulation model show that:
Interventions can have a very large impact on alcohol dependence and injuries. Between 2020 and 2050, up to 74 million cases of dependence can be prevented by MUP and up to 48 million cases of injuries by sobriety checkpoints. To put this in context, 74 million cases of dependence roughly correspond to 7% of all cases of alcohol dependency.
Interventions such as increased taxation, MUP and sobriety checkpoints produce the largest health gains, resulting in between 1.1 million and 1.5 million LYs gained annually in the 48 countries included in the analysis.
The effect of the interventions on DALYs does not decline over time, even after discounting, suggesting that these interventions have long-lasting effects, with future cohorts of people who will be also affected.
An improvement in population health goes hand in hand with a positive impact on health expenditure. Although it might seem intuitive to expect that reducing the burden caused by harmful alcohol consumption will lead to a reduction in health expenditure, this is by no means guaranteed, since people avoiding alcohol-related disease conditions may still suffer from other competing diseases and/or accumulate additional health expenditure as a result of living longer. Nevertheless, the OECD model suggests that this is not the case for public health actions tackling harmful alcohol consumption, and all the interventions modelled contribute to a reduction in health expenditure. More specifically, the OECD model suggests that:
All interventions have a significant impact on health expenditure, cumulatively saving between USD PPP 6 billion (workplace programmes) and USD PPP 207 billion (MUP) between 2020 and 2050 in the 48 countries studied.
In terms of impact on health expenditure per capita, MUP and taxation can save about USD PPP 4 per capita per year, and counselling in primary care is the third most effective intervention on this dimension, producing savings equal to about USD PPP 1.4 per capita per year. All the other interventions produce average savings between USD PPP 0.1 and USD PPP 1.0 per capita per year.
MUP, taxation and restrictions on opening hours are cost-saving, meaning that health expenditure savings significantly outweigh the intervention costs. For all the other interventions, the implementation cost is higher than the health expenditure savings in all countries, or – for advertising regulation and bans, counselling in primary care and sobriety checkpoints – in selected, mainly non-OECD, countries.
A sensitivity analysis was carried out to test the uncertainty around these results. It confirms that MUP, taxation and restrictions on opening hours produce significant gains in DALYs while being cost-saving. Six of the other interventions are cost-effective, since they save DALYs at a cost below USD 50 000/DALY, a threshold often used to define cost-effective interventions in health. School-based and workplace programmes produce health gains at a cost above or close to the USD 50 000/DALY threshold (see Annex Figure 7.A.3 in Chapter 7).
In addition to reduced health costs, implementation of the assessed policies also leads to a reduction of costs caused by suboptimal productivity of the labour force. By reducing the incidence of alcohol-related chronic diseases and injuries, all the interventions show potential to increase labour force participation and productivity, mainly through an increase in employment and reductions in presenteeism and absenteeism. It is calculated that taxation – the most effective policy action – would help bring an additional 809 000 people to the labour market through increased employment, while another 371 000 individuals would be “virtually” gained through decreased absenteeism and presenteeism. Overall, each year, this would correspond to up to USD PPP 31 billion in lost productivity that can be saved in all the 48 countries combined for this intervention. More than half of this sum would be produced by higher labour force participation, with another 37% due to labour force productivity. Reductions in early retirement can generally be considered a less important driver. In general, savings from avoiding reduced labour force productivity considerably exceed the savings from reduced health expenditure.
Implementation costs vary substantially across interventions and countries. The cost of implementing the policy actions varies according to a number of factors, including whether the intervention aims to cover the whole population (e.g. price policies and regulation and/or restriction of alcohol availability) or aims to target individuals (e.g. health care policies to advise and treat people). The latter are generally more costly on a per capita basis. Other factors such as the involvement of specialised workforce (medical personnel or police) or of the private sector to deliver the intervention (as in workplace‑based programmes) may also have an impact on total costs. Low-resource interventions cost from as little as USD PPP 0.05 to USD PPP 0.1 per capita per year, depending on the country and the characteristics of the interventions. More resource‑intensive interventions can cost up to about USD PPP 5 per capita per year.
Implementation of the policies analysed in this report may also entail other costs, some of which may have to be directly disbursed by governments; in other cases, these costs may be borne by private entities, including individuals and the alcohol industry. Many of these costs are difficult to estimate because of poor evidence or the absence of publicly available data. Box 1.3 above reports a list of cost items that are not included in this analysis, while Section 1.5 discusses the potential impact that specific public health policies to tackle harmful alcohol consumption may have on industry revenues.
When all the costs and savings considered in the analysis are taken into account, the OECD model concludes that, consistently across geographical settings, the majority of the policy actions considered are a good investment for countries. Results from the analysis show that most investments in these measures completely pay for themselves and, in many cases, produce an effect on the economy of the countries and on the budget of their citizens that is significantly greater than their implementation cost. Policies are generally expected to contribute to an increase in GDP above trend for the 45 countries14 analysed in the range of 0.001‑0.055% annually, corresponding to an additional output of up to USD PPP 10‑11 per capita per year for the interventions with the highest impact.
Further, the OECD microsimulation model found that for each USD 1 invested in the prevention of harmful alcohol consumption, there is a return of up to USD 183 in the form of total economic benefits (in terms of GDP) on average each year over the next 30 years. Figure 1.8 summarises the health and economic impact of the ten policy interventions studied and the four policy packages that are presented in the next section. When the calculation is carried out only by considering OECD countries, the return on investment is even higher, at up to USD 371 for each USD 1 invested (Annex Figure 1.A.2). More importantly, all the assessed policies prolong life, not just during a person’s later years but also by keeping people healthy during the central part of their life and allowing them to do the things that they enjoy and that society needs.
Average per year for the period 2020‑50
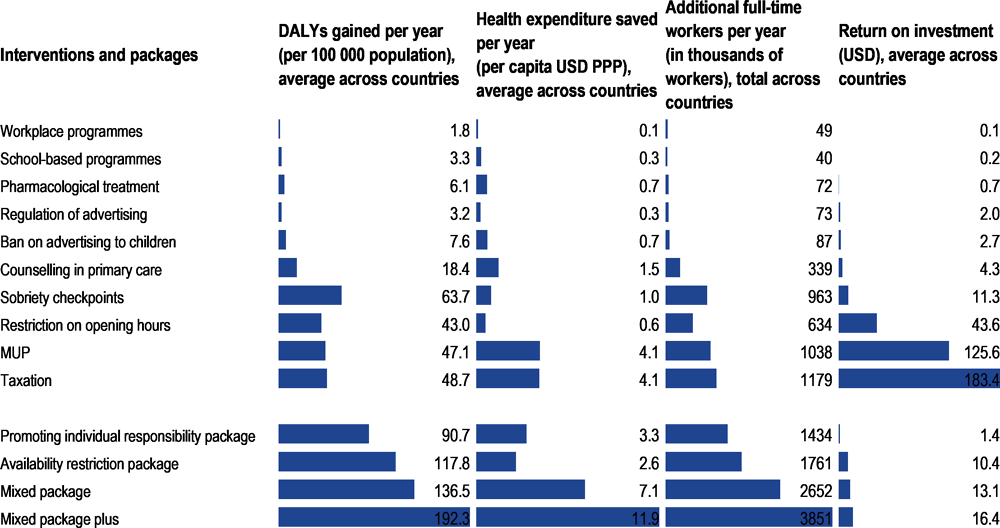
Note: Estimates for the return on investment are the result of the total increase in GDP in the 45 countries produced by the policy, divided by the total cost of implementing the policy in these countries.
Source: OECD analyses based on the OECD SPHeP-NCDs model and OECD long-term economic model, 2020.
Combining public health actions into prevention packages provides multiple advantages. Harmful alcohol consumption affects population health and the economy through different pathways, and a number of factors underpin the development of unhealthy patterns of harmful alcohol consumption. A first substantial advantage of combining single actions into prevention strategies is that packages of interventions can address multiple determinants at the same time. In addition, packages can target different population groups simultaneously, producing better results for the whole population. Finally, policies within a package can interact with one another, sustaining positive behavioural changes in a more than additive fashion. As discussed in Section 1.3, countries are increasingly interested in implementing policy packages; the case of the Russian Federation provides interesting evidence of their impact. Analyses carried out with the OECD model take into account these first two components, but adopt a conservative assumption on the potential super-additivity of combining policies into packages, given the lack of robust data to model interactions.
Previous OECD work on tackling harmful alcohol consumption concluded that a multi-pronged strategy would provide a comprehensive, effective and cost-effective response to harmful alcohol consumption by addressing some of its key determinants. The strategy was nicknamed “the PPPP approach”, based on the four key dimensions it aimed to address: promotion of alcohol to children; police to limit the negative consequences of harmful alcohol consumption on others (e.g. violence and traffic injuries); primary care to help patients with harmful alcohol consumption; and price to limit the affordability of cheap alcohol (Sassi, 2015[45]).
In this round of analyses, the OECD gauged the effect of four promising policy packages (Table 1.2):
The mixed package broadly overlaps with the PPPP approach and focuses primarily on the most cost-effective interventions by upscaling their implementation. Actions included in this package are already implemented in many (but not all) countries included in the study, but with a lot of variability in terms of implementation and design.
The mixed package plus considers the same policies included in the mixed package but boosts these with promising and innovative policies such as MUP and statutory bans on alcohol advertising targeting children.
The availability restriction package focuses primarily on interventions to limit the accessibility of alcoholic beverages. This entails implementation of the most effective version of these interventions, scaling up interventions already in place.
The promoting individual responsibility package focuses on interventions that are less intrusive for individuals and less politically sensitive to implement.
|
Mixed package |
Mixed package plus |
Availability restriction package |
Promoting individual responsibility package |
|---|---|---|---|
|
Alcohol taxation |
Alcohol taxation |
Regulation of alcohol advertising |
Sobriety checkpoints |
|
Regulation of alcohol advertising |
Regulation of alcohol advertising |
Sobriety checkpoints |
School-based programmes |
|
Sobriety checkpoints |
Sobriety checkpoints |
Statutory ban on alcohol advertising to children |
Workplace‑based programmes |
|
Alcohol counselling in primary care |
Alcohol counselling in primary care |
Restrictions on outlet opening hours |
Alcohol counselling in primary care |
|
MUP |
Personalised pharmacological treatment |
||
|
Statutory ban on alcohol advertising to children |
The mixed package and, in particular, the mixed package plus produce the highest impact during the timeframe considered for the analysis (between 2020 and 2050) (Figure 1.8). Conversely, the package promoting individual responsibility would be about 50‑90% less effective than the mixed package plus, depending on the explored outcomes. More specifically, the OECD model calculates that:
Overall, for each USD PPP 1 invested in one of the policy packages, a return of USD PPP 1.4 to USD PPP 16.4 can be expected in the form of economic benefits. The return on investment is highest for the mixed package plus. The return on investment for OECD countries would be even greater, ranging from USD PPP 2.4 to USD PPP 30.9 for each USD PPP 1 invested.
The return on investment for policy packages is lower than for some specific interventions. The implementation cost of policy packages is greater than the implementation cost for single interventions – in particular, for interventions entailing price increase and regulation (Annex Table 1.A.1). It should be remembered, however, that the return on investment is not the only dimension to consider when selecting interventions, and policy packages have much greater effectiveness (e.g. on population health) than single interventions; this is another dimension to take into account in the policy-making process.
Up to USD PPP 28 billion in health expenditure can be saved annually across the 48 countries included in the study, following implementation of the mixed package plus. The mixed package produce savings of USD PPP 16 billion and the availability restriction package savings of USD PPP 4 billion.
There is also a substantial impact on GDP, with the mixed package plus expected to increase GDP between 0.05% and 0.34% across the countries included in the study. The mixed package and the availability restriction package produce a lower effect, ranging from 0.03% to 0.21%. The promoting individual responsibility package would have the lowest impact, ranging from 0.01% to 0.11%.
Each year, the total labour force of the 48 countries included in the analysis would increase by an equivalent of about 3.9 million employees from the mixed package plus, 2.7 million from the mixed package, 1.8 million from the availability restriction package and 1.4 million from the package promoting individual responsibility, owing to increased labour force participation and productivity. Overall, the output of the labour force increases by between USD PPP 22 billion (promoting individual responsibility package) and USD PPP 90 billion (mixed package plus) per year.
All the packages would lead to a gain in LYs every year: 4.6 million LYs from the mixed package plus, 3.5 million LYs from the mixed package, 2.6 million LYs from the availability restriction package and 2.2 million LYs from the promoting individual responsibility package. The four packages would also save between 4.3 million and 8.4 million DALYs per year in all modelled countries.
Public health policies to reduce harmful alcohol consumption carry direct implications for industry and business, particularly in the case of the alcohol industry. Consisting of alcohol producers and both off- and on-trade vendors, the alcohol industry can be required to change a marketing strategy, invest in research and development (R&D) or change production methods, which can result in implementation costs. Policies can also affect the income of companies directly, as they may change sales revenues, profit margins or ancillary sales. In some cases – as, for example, with MUP – policies may actually may have a positive impact on industry by providing additional revenues. At the industry level, policies may have an impact in terms of illicit and cross-border trade and on employment. Finally, alcohol policies may have a broader impact on other industries, as individuals’ income not spent on alcohol products may be used for other purposes.
The OECD reviewed factors that may affect industry revenues following the implementation of public health actions to tackle harmful alcohol consumption (Figure 1.9). Overall, costs to industry are difficult to calculate, given the lack of publicly available data. Moreover, this analysis was not able to identify sound evidence on certain dimensions, such as expenditure on lobbying and litigation to avoid the implementation of policies incurred by the industry and others. Based on information available in the academic literature or government publications, the review did not find evidence indicating that costs to industry outweigh costs caused by harmful alcohol consumption.
Any policy that affects alcohol products based on the amount of alcohol they contain may lead alcohol producers to reformulate their products. Changes in advertising regulations or pricing policies may require companies to modify their packaging and marketing strategies. The most important cost items that result from these policies are changes in marketing and advertising spend; redesign and printing costs; investment in development of techniques to lower the alcohol content of beverages; and changes in production costs. Additional compliance costs may also be associated with employing staff or consultants to work on regulatory compliance, administration and reporting. The OECD review looked at all these dimensions.
Policies that change the regulations around alcohol marketing – such as advertising restrictions and policies that restrict competition on price – may cause alcohol companies to develop a new advertising strategy, change their product portfolio or divert marketing funding to other channels. Accordingly, industry may have to spend money on advertising agency fees (or commit time internally) to review and redesign marketing strategies. Changes in advertising regulations may also force companies to switch to other marketing channels. However, in specific cases, it has been shown that current advertising practices may be adapted to meet new standards (for example, targeting an older audience or airing at a different time), without affecting the cost (Ross, Sparks and Jernigan, 2016[46]).
Price policies such as taxes or minimum prices may result in costs for vendors for changing menus and price displays – in terms of both printing and labour costs. However, where prices are displayed on shelves, digitally or on single‑use paper menus, these costs may be minimal. Similarly, the introduction of warning labels on alcohol containers can incur redesign and printing costs. In 2020, Food Standards Australia New Zealand (FSANZ, 2020[47]) estimated the average cost per stock-keeping unit for including a pregnancy warning label at AUD 4 924 (USD 3 420). This cost could be lowered for companies that voluntarily change labels once a year or more, as mandatory label changes can be combined with voluntary changes.
If producers decide to respond to new policies by reducing the alcohol content of their products, they have to invest in R&D, and may incur higher production costs. While many techniques for producing lower-alcohol products exist, producers need to experiment to find the right approach for their product. This includes costs for consumer testing of new products, as taste remains one of the main issues for the acceptability of lower-alcohol products. In the production phase, the reformulated product may also entail higher production costs, depending on the type of process used to produce the lower-alcohol beverage. For example, the cost of buying a reverse osmosis machine to lower the alcohol content may vary between USD 30 000 and more than USD 2 million. In Australia, the cost to rent an alcohol removal machine was estimated at AUD 0.10 (USD 0.07) per litre to reduce the alcohol content by 1%.
Many alcohol policies are designed to reduce the consumption of alcohol; they therefore affect the earnings of the industry. However, the impact of policies on the industry can differ widely. For example, taxes can affect either sales or profits; price policies have different impacts on off-trade and on-trade vendors; minimum prices and reformulation may actually increase income for the industry; and a reduction in sales of alcohol products can lead to a reduction in sales of other products.
The impact of taxation on alcohol producers and vendors is strongly dependent on the amount of tax they decide to pass on to consumers through higher prices – the pass-through rate. If the tax is not passed on to the consumer, industry covers the cost by reducing its profit margin. Conversely, if the industry passes on the tax, sales are likely to be lower. Factors that affect industry’s choice between these two options include the expected response of consumers, the competitiveness of the market and negotiations between producers and vendors, based on their relative bargaining power.
Within the industry of alcohol vendors, policies such as sales restrictions and price policies may affect off-trade and on-trade vendors differently depending on their design. For example, taxation is likely to have a greater impact on off-trade than on-trade sales, as price elasticity is generally greater in off-trade. Similarly, MUP has a greater impact on off-trade vendors as on-licence prices are between two and four times higher than for the off-trade (Rabinovich et al., 2012[48]).
Among alcohol producers, minimum prices can be expected to benefit both premium brands and low-priced products, although through different mechanisms. One the one hand, the increase in price for products at the low end reduces the price gap with higher-priced, premium products, making them more attractive. On the other hand, increased income from minimum prices remains with the industry, and the higher price charged in low-priced products may partly or completely offset the losses in sales. For example, a study for the Welsh Government looking at a GBP 0.50 (USD 0.60) MUP showed a decrease in consumption of 3.6% across the population (with, importantly, the greatest effect among people who engage in harmful drinking), but a 1.4% increase in spending (Angus et al., 2017[49]).
In addition to the company-level impacts discussed above, alcohol policies can also affect the industry as a whole. Stricter regulation of price or availability may lead to an increase in unrecorded alcohol sales, such as illicit sales or cross-border trade. Policies that affect the alcohol industry can have consequences for employment in this sector. In addition, other alcohol policies such as advertising restrictions may also have an industry-level impact on competition between companies – in particular, in the case of smaller companies and new entrants. While any impact greatly depends on the competitive landscape and alcohol market in each country, as well as the specifics of the policy, previous OECD work recommends that policy-makers should consider how any new regulation may affect the competitive process (OECD, 2020[50]).
Policies such as taxation and those modifying the availability of alcohol may make illicit products seem more convenient or more available. Ineffective enforcement of policies, including inadequate penalties for activities related to illicit alcohol and corruption, also play a role in enabling illicit trade of alcohol products. The amount of unrecorded alcohol consumption in OECD countries is estimated at 1.4 litres per person per year, corresponding to 14% of total annual consumption. Illicit sales reduce income for the industry and, through avoided taxation, negatively affect government revenues (OECD, 2016[51]). For example, in the EU27, the sale of counterfeit wine and spirits was estimated to result in an annual loss of EUR 2.7 billion in sales for the industry, and EUR 2.2 billion in tax revenue and reduced social security contributions for governments (EUIPO, 2018[52]). In addition, where taxes or regulations are introduced in one country only, or where they are significantly higher or stricter than in other countries, this may contribute to an increase in cross-border trade.
Reductions in employment levels in the alcohol industry are likely to be offset by growth in employment in other industries. Changes in alcohol sales as a result of price policies or any other policy aimed at reducing alcohol consumption could lead to a loss of employment in the alcohol industry. However, the displacement of demand and jobs could cause employment in other industries to grow. For example, evidence from previous – mostly modelling-based – studies suggests that:
A potential small decrease in jobs in the Australian wine industry as a result of volumetric wine taxes (between 0.5% and 6.8% of total employment depending on the tax scenario) could be met with an increase in employment in the industries taking over the irrigated regions formerly used for vines (Fogarty and Jakeman, 2011[53]).
The additional revenue generated by an excise tax increase of USD 0.05 per drink would lead to a net increase of 8 183 jobs in the five US states15 included in the analysis, with this figure declining to 7 792 when introducing a 5% sales tax on beer, wine, and distilled spirits (Wada et al., 2017[54]).
If the United Kingdom used a theoretical 10% increase in alcohol tax to increase spending on public services, then there would be over 17 000 more full-time equivalent jobs. In addition, gross value added would increase by GBP 847 million (USD 1 039 million) (Connolly et al., 2019[55]).
It is important to note that these studies primarily look at the impact of taxes on trade in various industries – they do not take into account the health impacts of reduced alcohol consumption, which also affect employment. Finally, some studies suggest that there may be friction costs in the short term, which can include time off work in between jobs and the costs of hiring and (re)training (Kigozi et al., 2016[56]).
An OECD analysis of household expenditure data complemented the Fogarty and Jakeman (2011[53])., Wada et al. (2017[54]) and Connolly et al. (2019[55]) studies by examining the potential impact of alcohol policies on other industries. It found that a policy-induced decrease in alcohol purchases could potentially encourage alcohol-purchasing households to switch consumption to other goods and services. Specifically, the study analysed the share of household budget that is devoted to purchasing alcohol, and compared spending habits between households that do and do not purchase alcohol to better understand how they may reallocate expenditure in response to a reduction in alcohol purchases. The analysis, which incorporated 19 European countries and the United States,16 found that:
Households spent between USD PPP 294 and USD PPP 1 349 on alcohol in 2015, or between 1.0% and 3.4% of their total budget. Consequently, a policy inducing a 10% decrease in alcohol purchases would make available an additional USD PPP 29 per household in Hungary and up to USD PPP 135 per household in Ireland, which may be reallocated to other industries.
Alcohol-spending households spend a higher proportion of total expenditure on discretionary (non-essential) items, including restaurants and hotels (5.9% vs. 4.9%), and recreation and culture (6.4% vs. 5.6%).
Given that discretionary items are more responsive to changes in income due to higher elasticity (Jääskelä and Windsor, 2011[57]), the findings suggest that a decrease in alcohol expenditure could be offset by additional expenditure on other discretionary goods.
Harmful consumption of alcohol has been widely acknowledged as one of the key risk factors to population health, and alcohol-related chronic diseases have a significant impact on the global economy. Despite policy efforts by countries across the world, gaps remain in the policy response to this top public health threat. The current and projected health burdens caused by alcohol-related chronic diseases are enormous, as are their costs to health systems and society, and the personal costs borne by the general population through increased taxation, lower probability of being employed and lower educational attainment.
Positive results achieved by countries that have implemented far-reaching policy packages show that more can be done to address this public health threat. Policy-makers have a comprehensive menu of “traditional” public health interventions from which to choose. Emerging policies, such as MUP – which targets cheap alcohol that is more likely to be consumed by people with harmful patterns of alcohol consumption – and policies to modify the environment in which we live offer further opportunities to prevent harmful alcohol consumption. Health systems also need to do more to support those suffering from hazardous and harmful drinking, as well as individuals with alcohol dependence. Preventing the exposure of children to alcohol promotion and avoiding harm to others – for example, by tightening policies to counter drink-driving – also fit well in a comprehensive package to tackle harmful alcohol consumption. Investing in policy packages saves millions of lives and generates savings that are greater than the implementation costs. The OECD simulations show that for every USD 1 invested in a policy packages that include all the policies set out above, up to USD 16 is returned in economic benefits. While industry revenues may be affected by policy measures, either in profitable or unprofitable ways, countermeasures exist to minimise additional costs.
[9] Anderson, P. et al. (2020), “Impact of COVID-19 Confinement on Alcohol Purchases in Great Britain: Controlled Interrupted Time-Series Analysis During the First Half of 2020 Compared With 2015–2018”, Alcohol and Alcoholism, Vol. 2020, pp. 1-11, http://dx.doi.org/10.1093/alcalc/agaa128.
[49] Angus, C. et al. (2017), Model-based Appraisal of the Comparative Impact of Minimum Unit Pricing and Taxation Policies in Wales: Interim report, Welsh Government, Cardiff, http://gov.wales/statistics-and-research/research-likely-impact-public-attitudes-towards-minimum-unit-price-alcohol/?lang=en (accessed on 22 February 2018).
[33] Australian Bureau of Statistics (2019), 6401.0 Consumer Price Index: Alcoholic beverages, Australian Bureau of Statistics, Canberra, https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/dec-2019.
[34] Australian Bureau of Statistics (2019), 6401.0 Consumer Price Index: All groups CPI, Australian Bureau of Statistics, Canberra, https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/dec-2019.
[16] Boniface, S., J. Kneale and N. Shelton (2014), “Drinking pattern is more strongly associated with under-reporting of alcohol consumption than socio-demographic factors: Evidence from a mixed-methods study”, BMC Public Health, Vol. 14/1, p. 1297, http://dx.doi.org/10.1186/1471-2458-14-1297.
[7] Bundesministerium der Finanzen (2021), Steuereinnahmen 2020.
[14] CDC (2020), Alcohol Use and Your Health, Centers for Disease Prevention and Control, Atlanta, GA, https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm (accessed on 12 November 2020).
[55] Connolly, K. et al. (2019), “Can a policy-induced reduction in alcohol consumption improve health outcomes and stimulate the UK economy? A potential ‘double dividend’”, Drug and Alcohol Review, Vol. 38/5, pp. 554-560, http://dx.doi.org/10.1111/dar.12962.
[52] EUIPO (2018), Synthesis Report on IPR Infringement, European Union Intellectual Property Office, Alicante, http://dx.doi.org/10.2814/833376.
[2] Eurocare (2020), Alcohol Consumption in Times of COVID-19, Eurocare, Brussels, https://www.eurocare.org/cares.php?sp=alcohol-and-health&ssp=alcohol-consumption-in-times-of-covid-19 (accessed on 10 November 2020).
[32] Eurostat (2019), Adjusted Disposable Income, Gross, European Commission, Luxembourg, https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do.
[31] Eurostat (2019), Harmonised Index Of Consumer Prices: Alcoholic beverages, European Commission, Luxembourg, https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do.
[30] Eurostat (2019), Harmonised Index Of Consumer Prices: All items, European Commission, Luxembourg, https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do.
[53] Fogarty, J. and G. Jakeman (2011), “Wine tax reform: The impact of introducing a volumetric excise tax for wine”, Australian Economic Review, Vol. 44/4, pp. 387-403, http://dx.doi.org/10.1111/j.1467-8462.2011.00653.x.
[47] FSANZ (2020), Proposal P1050: Pregnancy warning labels on alcoholic beverages, Food Standards Australia New Zealand, Canberra, https://www.foodstandards.gov.au/code/proposals/Pages/P1050Pregnancywarninglabelsonalcoholicbeverages.aspx.
[21] GBD 2016 Alcohol Collaborators (2018), “Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016”, Lancet, Vol. 392/10152, pp. 1015-1035, http://dx.doi.org/10.1016/S0140-6736(18)31310-2.
[10] Gisle, L. et al. (2020), Deuxième Enquête de Santé COVID-19: Résultats préliminaires, Sciensano, Brussels, https://www.sciensano.be/en/biblio/deuxieme-enquete-de-sante-covid-19-resultats-preliminaires (accessed on 10 November 2020).
[8] HM Revenue and Customs (2020), National Statistics: Alcohol Bulletin Commentary (August to October 2020), HM Revenue and Customs, London, https://www.gov.uk/government/publications/alcohol-bulletin/alcohol-bulletin-commentary (accessed on 8 February 2021).
[41] Houghton, F. et al. (2014), “Children’s awareness of alcohol sponsorship of sport in Ireland: Munster Rugby and the 2008 European Rugby Cup”, International Journal of Public Health, Vol. 59/5, pp. 829-832, http://dx.doi.org/10.1007/s00038-014-0568-4.
[4] IWSR (2020), Beverage alcohol in 2020 performs better than expected - IWSR, https://www.theiwsr.com/beverage-alcohol-in-2020-performs-better-than-expected/ (accessed on 5 March 2021).
[57] Jääskelä, J. and C. Windsor (2011), “Insights from the household expenditure survey”, Reserve Bank of Australia Bulletin, pp. 1-12, https://www.rba.gov.au/publications/bulletin/2011/dec/pdf/bu-1211-1.pdf.
[56] Kigozi, J. et al. (2016), “Estimating productivity costs using the friction cost approach in practice: A systematic review”, European Journal of Health Economics, Vol. 17/1, pp. 31-44, http://dx.doi.org/10.1007/s10198-014-0652-y.
[25] Lange, S. et al. (2017), “Global prevalence of fetal alcohol spectrum disorder among children and youth: A systematic review and meta-analysis”, JAMA Pediatrics, Vol. 171/10, pp. 948-56, http://dx.doi.org/10.1001/jamapediatrics.2017.1919.
[17] Livingston, M. and S. Callinan (2019), “Examining Australia’s heaviest drinkers”, Australian and New Zealand Journal of Public Health, Vol. 43/5, pp. 451-456, http://dx.doi.org/10.1111/1753-6405.12901.
[44] MacArthur, G. et al. (2018), “Individual-, family-, and school-level interventions targeting multiple risk behaviours in young people”, Cochrane Database of Systematic Reviews, Vol. 2018/10, p. CD009927, http://dx.doi.org/10.1002/14651858.CD009927.pub2.
[24] Marmot, M. (2010), Fair Society, Healthy Lives: The Marmot Review, University College London, http://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-full-report-pdf.pdf (accessed on 3 September 2018).
[5] Movendi International (2020), Switzerland: Alcohol sales collapse during COVID-19 lockdown, Movendi International, Stockholm, https://movendi.ngo/news/2020/06/05/switzerland-alcohol-sales-collapse-during-covid-19-lockdown/ (accessed on 10 November 2020).
[22] Naimi, T. et al. (2017), “Selection biases in observational studies affect associations between “moderate” alcohol consumption and mortality”, Addiction, Vol. 112/2, pp. 207-214, http://dx.doi.org/10.1111/add.13451.
[6] National Institute on Alcohol Abuse and Alcoholism (2020), Alcohol Sales During the COVID-19 Pandemic, Surveillance Report #115, https://pubs.niaaa.nih.gov/publications/surveillance-covid-19/COVSALES.htm (accessed on 15 March 2021).
[3] Nielsen (2020), Rebalancing the “COVID-19 Effect” on Alcohol Sales, Nielsen, Chicago, Il, https://nielseniq.com/global/en/insights/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/ (accessed on 10 November 2020).
[38] Noel, J., T. Babor and K. Robaina (2017), “Industry self-regulation of alcohol marketing: a systematic review of content and exposure research”, Addiction, Vol. 112, pp. 28-50, http://dx.doi.org/10.1111/add.13410.
[50] OECD (2020), Regulatory Impact Assessment, OECD Best Practice Principles for Regulatory Policy, OECD Publishing, Paris, https://dx.doi.org/10.1787/7a9638cb-en.
[51] OECD (2016), Illicit Trade: Converging Criminal Networks, OECD Reviews of Risk Management Policies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264251847-en.
[39] Ofcom (2017), Communications Market Report, Ofcom, London, https://www.ofcom.org.uk/__data/assets/pdf_file/0017/105074/cmr-2017-uk.pdf.
[12] Pollard, M., J. Tucker and H. Green (2020), “Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US”, JAMA Network Open, Vol. 3/9, p. e2022942, http://dx.doi.org/10.1001/jamanetworkopen.2020.22942.
[48] Rabinovich, L. et al. (2012), Further Study on the Affordability of Alcoholic Beverages in the EU, RAND Corporation, Santa Monica, CA, https://ec.europa.eu/health//sites/health/files/alcohol/docs/alcohol_rand_2012.pdf (accessed on 2 August 2017).
[15] Rehm, J. et al. (2003), “The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview”, Addiction, Vol. 98/9, pp. 1209-1228, http://dx.doi.org/10.1046/j.1360-0443.2003.00467.x.
[18] Richard, J. et al. (2019), “La consommation d’alcool chez les adultes en France en 2017”, Bulletin Epidémiologique Hebdomadaire, Vol. 5-6, pp. 89-97, https://www.santepubliquefrance.fr/docs/bulletin-epidemiologique-hebdomadaire-19-fevrier-2019-n-5-6 (accessed on 3 March 2020).
[20] Roerecke, M. and J. Rehm (2010), “Irregular heavy drinking occasions and risk of ischemic heart disease: A systematic review and meta-analysis”, American Journal of Epidemiology, Vol. 171/6, pp. 633-644, http://dx.doi.org/10.1093/aje/kwp451.
[46] Ross, C., A. Sparks and D. Jernigan (2016), “Assessing the impact of stricter alcohol advertising standards: The case of Beam Global Spirits”, Journal of Public Affairs, Vol. 16/3, pp. 245-254, http://dx.doi.org/10.1002/pa.1584.
[11] Santé Publique France (2020), Tabac, Alcool: Quel impact du confinement sur la consommation des Français?, Santé Publique France, Paris, https://www.santepubliquefrance.fr/presse/2020/tabac-alcool-quel-impact-du-confinement-sur-la-consommation-des-francais (accessed on 10 November 2020).
[45] Sassi, F. (ed.) (2015), Tackling Harmful Alcohol Use: Economics and Public Health Policy, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264181069-en.
[40] Smith, L. and D. Foxcroft (2009), “The effect of alcohol advertising, marketing and portrayal on drinking behaviour in young people: Systematic review of prospective cohort studies”, BMC Public Health, Vol. 9, p. 51, http://dx.doi.org/10.1186/1471-2458-9-51.
[35] Statistics Canada (2019), Table 18-10-0005-01 Consumer Price Index: Annual average, not seasonally adjusted, Statistics Canada, Ottawa, https://doi.org/10.25318/1810000501-eng.
[23] Stockwell, T. et al. (2016), “Do ’moderate’ drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality”, Journal of Studies on Alcohol and Drugs, Vol. 77/2, pp. 185-198, http://dx.doi.org/10.15288/jsad.2016.77.185.
[37] Taylor, B. and J. Rehm (2012), “The relationship between alcohol consumption and fatal motor vehicle injury: High risk at low alcohol levels”, Alcoholism: Clinical and Experimental Research, Vol. 36/10, pp. 1827-1834, http://dx.doi.org/10.1111/j.1530-0277.2012.01785.x.
[36] U.S. Bureau of Labor Statistics (2019), Alcoholic Beverages in U.S. City Average: All urban consumers, not seasonally adjusted, U.S. Bureau of Labor Statistics, Washington DC, https://www.bls.gov/cpi/#data.
[54] Wada, R. et al. (2017), “Employment impacts of alcohol taxes”, Preventive Medicine, Vol. 105, pp. S50-S55, http://dx.doi.org/10.1016/J.YPMED.2017.08.013.
[27] WHO (2020), Global Information System on Alcohol and Health (GISAH), World Health Organization, Geneva, http://www.who.int/substance_abuse/activities/gisah/en/ (accessed on 4 August 2020).
[19] WHO (2018), Global Status Report on Alcohol and Health 2018, World Health Organization, Geneva, https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1 (accessed on 10 September 2019).
[28] WHO (2018), SAFER: A World Free from Alcohol Related Harms, World Health Organization, Geneva, https://www.who.int/substance_abuse/safer/msb_safer_brochure.pdf.
[26] WHO (2013), Global Action Plan for the Prevention and Control of NCDs 2013-2020, World Health Organization, Geneva, https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1&isAllowed=y.
[1] WHO (2010), Global Strategy to Reduce the Harmful Use of Alcohol, World Health Organization, Geneva, https://www.who.int/publications/i/item/9789241599931.
[29] WHO Regional Office for Europe (2019), Alcohol Policy Impact Study: The effects of alcohol control measures on mortality and life expectancy in the Russian Federation, WHO Regional Office for Europe, Copenhagen, https://apps.who.int/iris/bitstream/handle/10665/328167/9789289054379-eng.pdf?sequence=1&isAllowed=y.
[42] WHO Regional Office for Europe (2009), Evidence for the Effectiveness and Cost-effectiveness of Interventions to Reduce Alcohol-related Harm, WHO Regional Office for Europe, Copenhagen, https://www.euro.who.int/__data/assets/pdf_file/0020/43319/E92823.pdf (accessed on 23 November 2020).
[13] Winstock, A. et al. (2020), GDS COVID-19 Special Edition: Key findings report, Global Drug Survey, London, https://www.globaldrugsurvey.com/gds-covid-19-special-edition-key-findings-report/ (accessed on 10 November 2020).
[43] Young, B. et al. (2018), “Effectiveness of mass media campaigns to reduce alcohol consumption and harm: A systematic review”, Alcohol and Alcoholism, Vol. 53/3, pp. 302-316, http://dx.doi.org/10.1093/alcalc/agx094.
Annex Figure 1.A.1 provides a breakdown of key policies to tackle harmful alcohol consumption among OECD countries. For example, 84% of all OECD countries tax all alcohol beverages; 86% have a legal minimum age of 18 or over; and 46% have a national written policy for alcohol and an aligning action plan.
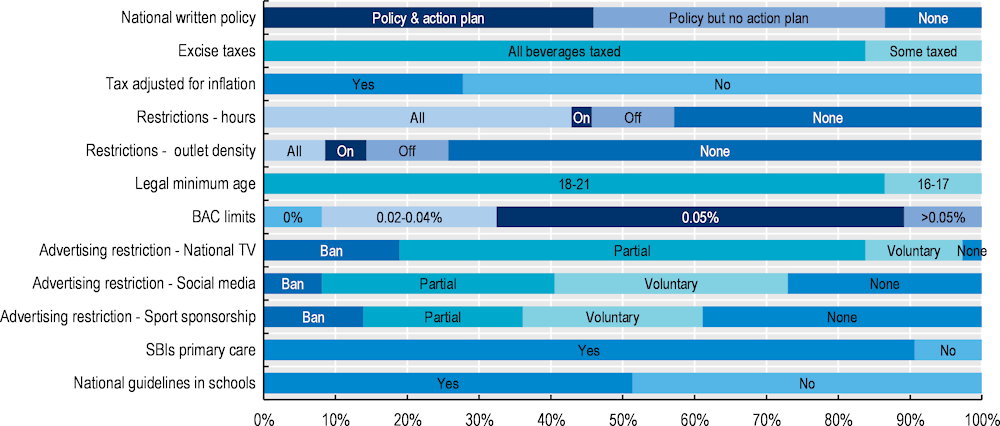
Note: Results do not include missing data.
Annex Figure 1.A.2 presents the health and economic impacts of interventions and policy packages, as well as the return on investment, for OECD countries only.
Average per year over the period 2020‑50
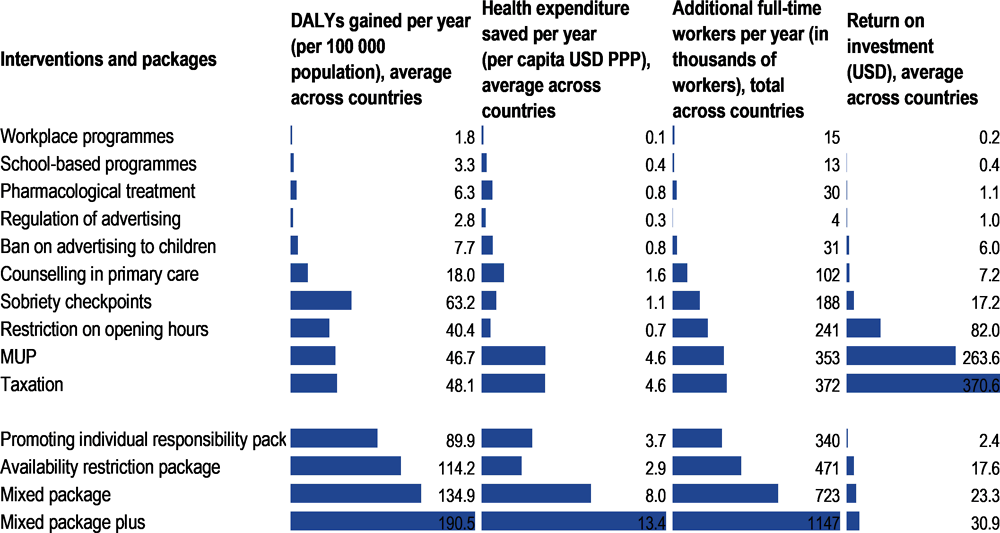
Note: Estimates for the return on investment are the result of the total increase in GDP in the 45 countries produced by the policy divided by the total cost of implementing the policy in these countries.
Source: OECD analyses based on the OECD SPHeP-NCDs model and OECD long-term economic model, 2020.
Annex Table 1.A.1 provides a brief summary of the key inputs to replicate the effects of the ten policy interventions (described in Section 1.4) within the OECD SPHeP-NCDs model.
These key inputs include:
age of the target population
proportion of people exposed to the intervention – these two first inputs help to define the coverage of the intervention
effectiveness of the intervention at the individual level – this parameter captures how individual behaviour changes, following exposure to the interventions, and as far as possible, this evidence is taken from peer-reviewed meta‑analyses, preferably from randomised control trials
cost of implementing the intervention (e.g. costs related to its planning, administration, monitoring and evaluation and so on, as well as costs of providing material).
|
|
Workplace |
School-based |
Taxation |
MUP |
Sobriety checkpoints |
Sales hours restriction |
Regulation of advertising |
Ban on advertising to children |
Counselling |
Treatment of dependence |
|---|---|---|---|---|---|---|---|---|---|---|
|
Target age |
18‑65 years |
10‑15 years |
all |
all |
>18 years |
all |
all |
<18 years |
all |
all |
|
Exposure |
0.9‑2.5% |
90% |
100% |
100% |
80% |
40‑99% |
100% |
90% |
20% |
20% |
|
Effectiveness |
Alc cons: ‑41 g/week |
Drinking initiation: ‑20%; dependence: ‑30% |
10% price increase reduces alc cons by: ‑4% to ‑7% |
Alc cons: ‑0.6% to ‑3.3% |
Traffic injuries: ‑25% (year 1); 15% (year 2); ‑16% thereafter |
Assault injuries: ‑34%; traffic injuries: ‑1.5% |
Alc cons in young people: ‑0.84%; number of people who binge drink: ‑1.6% |
Underage drinking: ‑35%; prob of dependence: ‑30% |
Alc cons: ‑42 g/week (men), ‑30 g/week (women) |
Alc cons: Acamprosate: ‑31%; Naltrexone: ‑122 g/week |
|
Per capita cost, USD PPP |
3.7‑5.4 |
0.5‑0.7; per child: 10‑15 |
0.05‑0.08 |
0.07‑0.11 |
0.6‑0.8 |
0.1‑0.2 |
0.3‑0.4 |
0.3‑0.4 |
0.2‑0.3; per person treated: 24‑35 |
0.2‑0.3; per person treated: 171‑521 |
Note: Alc cons: alcohol consumption; prob: probability.
← 1. This report acknowledges the concept of harmful alcohol use reported in the WHO Global Strategy to Reduce the Harmful Use of Alcohol.
← 2. Unless otherwise specified (e.g. due to lack of data) Costa Rica is normally included in the OECD averages, as it is expected that Costa Rica will become an OECD member country before the release of the report.
← 3. The 52 countries are Argentina, Australia, Austria, Belgium, Brazil, Bulgaria, Canada, Chile, the People’s Republic of China, Colombia, Costa Rica, Croatia, Cyprus, the Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, India, Indonesia, Ireland, Israel, Italy, Japan, Korea, Latvia, Lithuania, Luxembourg, Malta, Mexico, the Netherlands, New Zealand, Norway, Peru, Poland, Portugal, Romania, the Russian Federation, Saudi Arabia, the Slovak Republic, Slovenia, South Africa, Spain, Sweden, Switzerland, Turkey, the United Kingdom and the United States.
← 4. The 48 countries considered for this analysis are Australia, Austria, Belgium, Brazil, Bulgaria, Canada, Chile, China, Colombia, Costa Rica, Croatia, Cyprus, the Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, India, Ireland, Israel, Italy, Japan, Korea, Latvia, Lithuania, Luxembourg, Mexico, Malta, the Netherlands, Norway, New Zealand, Poland, Portugal, Romania, the Russian Federation, the Slovak Republic, Slovenia, South Africa, Spain, Sweden, Switzerland, Turkey, the United Kingdom and the United States.
← 5. Alcohol consumption per person who drinks is equal to the quantity of alcohol consumed divided by the number of people who drink. In Turkey, the number of people who drink is small, but the volume of alcohol consumption per person who drinks is high.
← 6. The HBSC survey includes the following countries: Austria, Belgium, Bulgaria, Canada, Croatia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, the Netherlands, Norway, Poland, Portugal, Romania, the Russian Federation, the Slovak Republic, Slovenia, Spain, Sweden, Switzerland and the United Kingdom.
← 7. Individual-level data for HBSC 2017‑18 were not available at the time of this report, and the analysis could not include data from the most recent wave.
← 8. The countries included in this analysis are: Austria, Belgium, Bulgaria, Canada, Croatia, Cyprus, the Czech Republic, Denmark, Estonia, Finland, France, Greece, Hungary, Iceland, Ireland, Korea, Latvia, Lithuania, Luxembourg, Malta, Mexico, Norway, Poland, Portugal, Romania, the Slovak Republic, Slovenia, Spain, Sweden, the United Kingdom and the United States. The analyses were carried out on data from NHANES 2015 (United States); Baromètre santé 2017 (France); ENCODAT 2016‑17 (Mexico); Canadian Community Health Survey 2015‑16 (Canada); KNHANES 2018 (Korea); and EHIS 2014 (remaining 26 countries). Further information can be found in Chapter 2.
← 9. The 1/1.5 drinks per day cap was chosen because at these levels alcohol may have some protective effect on specific diseases such as ischaemic cardiovascular diseases and diabetes for some age groups (GBD 2016 Alcohol Collaborators, 2018[21]).
← 10. The GPA is the standard grading system used in the United States ranging from 0 to 4.0, where 4.0 is the best.
← 11. For example, it has been evaluated that a modest goal of all OECD countries boosting their average Programme for International Student Assessment scores by 5% (corresponding to 25 points) over the next 20 years would increase the GDP of OECD countries by USD 115 trillion over the lifetime of the generation born in 2010.
← 12. A standard drink is a measure of alcohol consumption in a drink and differs across beverage types and countries. In Australia, for example, one standard drink includes 10 grammes of alcohol, so a 750 ml bottle of wine (13.5% alcohol by volume) contains eight standard drinks.
← 13. Unless otherwise specified, all the results presented in this section are undiscounted, meaning they are not calculated by accounting for the present value of future outcomes.
← 14. Out of the 48 countries included in this analysis, three countries were not included in the OECD long-term economic model and could not be included in the analysis of the impact on GDP (Croatia, Cyprus and Malta). For the same reason, Costa Rica could not be included in the analysis of the impact on fiscal pressure.
← 15. The five US states included in the analysis are Arkansas, Florida, Massachusetts, New Mexico and Wisconsin.
← 16. In addition to the United States, the following European countries were analysed: Belgium, Denmark, Estonia, Finland, France, Greece, Hungary, Ireland, Italy, Lithuania, Latvia, Luxembourg, Poland, Portugal, the Slovak Republic, Slovenia, Spain, Sweden and the United Kingdom.