The COVID-19 pandemic has had a major impact on the health of Luxembourg's population. The mobilisation of resources and actors around the interministerial crisis unit was remarkable, and enabled new systems to be developed rapidly and health services to expand to absorb the shock of the health crisis. However, the pandemic also revealed structural weaknesses in the healthcare system, suggesting a lack of preparedness. This chapter assesses the resilience of Luxembourg's health system, taking into consideration the direct and indirect effects of the health crisis. The strengths and weaknesses of the crisis management in Luxembourg are also analysed in terms of the level of pandemic preparedness, the mechanisms implemented to absorb the shock and contain the pandemic, and the policies put in place to help certain health system functions recover.
Evaluation of Luxembourg's COVID-19 Response

4. The resilience of the Luxembourg health system to COVID-19
Abstract
Key findings
The Luxembourg health system responded and adapted remarkably well to the COVID-19 pandemic, as shown by numerous measures such as intensive testing for cases, contact tracing, the increase in hospital capacity, and the health reserve. However, Luxembourg needs to strengthen key aspects of preparedness to ensure that its health system is more resilient to future threats (for example, by strengthening information systems, increasing health personnel and setting up a central purchasing and logistics unit for critical products). Following the crisis, the health system must also be adapted to address long-term needs and mitigate the indirect effects of the pandemic (by strengthening primary care and continuing to address vaccine hesitancy, for example).
The direct health impact, measured in terms of excess mortality, has been lower in Luxembourg than the average for other OECD member countries. Up to and including the first half of 2022, the excess mortality rate was 1 226 per million population in Luxembourg, more than 60% lower than the OECD average. However, the pandemic has disproportionately affected older and disadvantaged populations. The mortality rate among the population aged 80 and over residing in long-term care facilities (a population that is on average more vulnerable than in other OECD member countries) is almost double the OECD average.
The effectiveness of Luxembourg's vaccination campaign in reducing hospitalisations and deaths is undeniable. The campaign was carried out successfully thanks to the efforts made upstream by thematic groups starting in March 2020, allowing work to be done on key issues such as the storage and delivery process, and the development of information systems. Although the vaccination campaign was highly personalised (with invitations sent out and personal accompaniment to appointments), vaccine hesitancy still appears to be relatively high. Despite overestimation biases, in May 2022 almost 30% of people residing in Luxembourg were still not fully vaccinated. It would have been beneficial to deploy vaccination in doctors' surgeries and retail pharmacies earlier in Luxembourg. Targeted awareness-raising based on community approaches should be strengthened.
The indirect consequences of the pandemic in Luxembourg are worrying, both in terms of delays in diagnoses and routine care, and in terms of deteriorating mental health (mainly among young people and people in employment).
Luxembourg has suffered from several shortcomings in terms of pandemic preparedness. Outside of the critical infrastructure sector, Luxembourg was not aware of the status of stocks of PPE at the beginning of the pandemic, and there was no information system in place to manage the crisis. The country's reliance on cross-border health workers also made the health system extremely vulnerable to border closures during the first lockdown to contain the spread of the disease. Finally, the lack of infection prevention and control expertise and medical support in long-term care facilities limited their ability to respond quickly to the health crisis. The interministerial crisis unit put in place innovative measures to compensate for the lack of preparedness, such as the development of the Qlik information system, the provision of temporary accommodation for cross-border health workers and the implementation of training in long-term care facilities.
The responsiveness of the interministerial crisis unit and the mobilisation of stakeholders was remarkable, putting in place several pragmatic solutions from mid-March 2020 onwards to absorb the shock and contain the pandemic:
Intensive testing of cases was implemented at the start of the pandemic through a range of actions such as mass screening and the formation of mobile teams. This large-scale screening strategy is among the best practices established by OECD member countries to reduce virus transmission and detect clusters in specific areas early.
The contact-tracing system proved to be effective and thorough in identifying contact cases thanks to three key factors: strengthening of the teams, specific support for certain categories of vulnerable populations following retrospective surveys, and the development of the Care+ application.
The sharp increase in hospital capacity enabled the number of intensive care beds to double during the first wave of the epidemic, allowing the health system to withstand the large influx of patients from Luxembourg itself and from neighbouring countries. This increase was made possible by cancelling non-urgent and non-essential surgical and medical activities during this first wave.
Health workers were mobilised during the first two waves of the pandemic by means of the health reserve and redeploying staff to areas of critical activity, thereby preventing any shortages of health personnel for COVID-19 care.
New care-delivery models were able to redress some of the weaknesses in Luxembourg's healthcare system. The goal is to sustain these efforts and evaluate practices to improve health system resilience:
Luxembourg restructured primary care to respond more efficiently to all of the population’s needs during the first waves of the pandemic. The implementation of advanced care centres and COVID-19 consultation centres in the primary care sector in Luxembourg is among the best practices of OECD member countries. Luxembourg must continue to strengthen primary care based on multidisciplinary teams that put greater emphasis on health risk prevention and co-ordinated care.
Remote consultations, remote monitoring of COVID-19 patients and electronic prescription services were rapidly deployed to maintain access to care in Luxembourg. However, remote consultations accounted for just 9% of all medical consultations in Luxembourg in 2020, compared to an average of 21% in all OECD member countries. Luxembourg should implement indicators to assess the quality of telemedicine services, including factors such as safety, care outcomes and user satisfaction (as ten other OECD member countries have already done).
New mental health support mechanisms were created for the public and healthcare workers, but multisectoral approaches that link mental health to education, youth and employment policies are lacking, so the needs of at-risk populations are not being met. The policies implemented in Australia, Canada and France are good examples of this being done.
4.1. Introduction
According to the OECD's “New approaches to economic challenges” analysis framework, the evaluation of health systems resilience is based on a cycle composed of four phases: 1. Anticipate; 2. Absorb; 3. Recover; and 4. Adapt. These four phases are essential to reduce the scale and severity of crises, and to minimise the direct and indirect consequences they have on health. This chapter assesses the resilience of Luxembourg's health system, taking into consideration the direct and indirect effects of the health crisis. The strengths and weaknesses of the management of the crisis in Luxembourg are also analysed in terms of the level of pandemic preparedness, the mechanisms implemented to absorb the shock and contain the pandemic, and the policies put in place to help certain health system functions recover.
The COVID-19 pandemic reached Luxembourg on 1 March 2020. The country mobilised significant financial resources during the first two years of the pandemic to respond to the health crisis. In 2020 and 2021, the Health Directorate spent more than EUR 166 million to address the needs of the crisis specifically. Additional financial resources and the remarkable mobilisation of stakeholders around the interministerial crisis unit enabled innovative measures to be developed rapidly and health services to expand. However, the pandemic also revealed structural weaknesses in the healthcare system suggesting a lack of pandemic preparedness. Like other OECD member countries, Luxembourg must now adapt by drawing lessons from the pandemic to improve the performance of the health system and its resilience to potential future pandemics.
4.2. The direct health impact of COVID-19 in Luxembourg
4.2.1. Although the prevalence of COVID-19 infections has been high in Luxembourg, the death toll has been much lower than in other OECD member countries
The COVID-19 pandemic has had a major impact on the health of Luxembourg's population. From January 2020 to December 2021, Luxembourg had one of the highest infection rates among OECD member countries. Despite lower rates of COVID-19-related deaths than in all other OECD member countries, life expectancy fell in Luxembourg in 2020, as was the case for most of these countries.
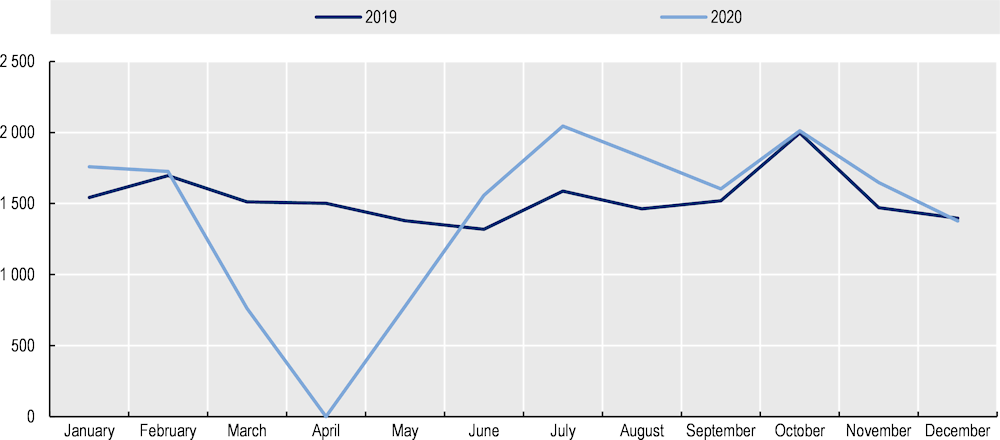
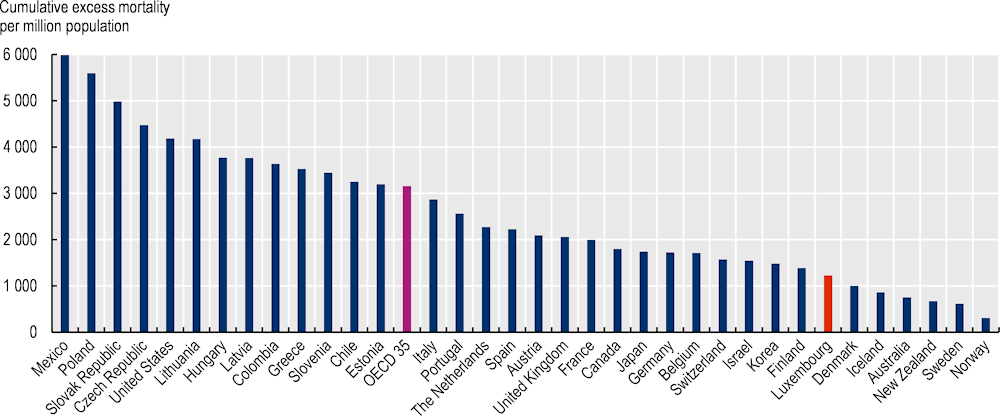
At the end of December 2021, the cumulative number of reported cases of COVID-19 in Luxembourg was 17 213 per 100 000 inhabitants, well above the OECD average of 12 401 per 100 000 inhabitants. Luxembourg had the ninth-highest prevalence of COVID-19 among OECD member countries (Figure 4.1). This elevated infection rate reflects the country's high capacity to detect infections and the wide variety of testing strategies implemented in the country (see section on Luxembourg’s mass testing policy has proven to be effective in curbing the spread of the virus).
Figure 4.1. The prevalence of COVID-19 in the population of Luxembourg was among the highest in OECD member countries
Note: The data depend on the ability of countries to detect COVID-19 infections – which was particularly limited in many countries at the beginning of the crisis – and the testing strategies they have implemented. Data are considered up to and including week 52 of the 2021 calendar year.
Source: European Centre for Disease Prevention and Control (2021[1]), “COVID-19 datasets”, European Centre for Disease Prevention and Control (database), https://opendata.ecdc.europa.eu/covid19/nationalcasedeath/; and Our World in Data (database) for non-European countries.
From January 2020 to the first half of 2022, COVID-19 caused 1 306 deaths per million population in Luxembourg, slightly below the OECD member country average of 1 462 deaths per million population. Up to and including the first half of 2022, the excess mortality rate1 was 1 226 per million population in Luxembourg, more than 60% lower than the OECD average (3 156 per million population). The number of excess deaths per million population in Luxembourg is also much lower than those recorded in certain neighbouring countries, such as France (1 996 additional deaths per million population), Germany (1 724 additional deaths per million population) and Belgium (1 709 additional deaths per million population) (Figure 4.2).
As in other OECD member countries, the high number of deaths in 2020 had an impact on life expectancy. Life expectancy in Luxembourg fell by 11 months in 2020, compared to an average decrease of 8.5 months across the European Union (EU) (OECD/European Observatory on Health Systems and Policies, 2022[2]). According to provisional Eurostat estimates, in 2021 life expectancy increased by seven months to 82.8 years (close to its 2019 pre-pandemic level) (Eurostat, 2021[3]).
Figure 4.2. The cumulative excess mortality rate per million population is well below the OECD average
Note: Excess mortality data are not available for Costa Rica, Ireland and Türkiye. The OECD average is a weighted average. Excess mortality is calculated by comparing figures with those from 2015 to 2019. Data are considered up to and including week 13 of the 2022 calendar year. Data are limited for Colombia (up to and including week 35 of 2021), Mexico (all 52 weeks of 2021), Canada (up to and including week 6 of 2022) and Australia (up to and including week 12 of 2022).
Source: OECD (2022) based on Eurostat and national data.
4.2.2. The pandemic disproportionately affected older and vulnerable populations
As in all OECD member countries, the vast majority of deaths attributable to COVID-19 occurred in older people living in residential facilities. Between March and the end of May 2020, almost half (46%) of the deaths attributed to COVID-19 in Luxembourg were among residents of long-term care facilities (Rocard, Sillitti and Llena-Nozal, 2021[4]). If we look at the same indicator among those aged 80 or above, Luxembourg comes third, with only Slovenia and Belgium faring worse. The mortality rate among the population aged over 80 years residing in residential facilities in Luxembourg is almost double the average for OECD member countries (Figure 4.3). However, it should be emphasised that the organisation of the long-term care system in Luxembourg favours home care, so only older and highly dependant people with multiple comorbidities live in institutions. Thus, those living in long-term care facilities in Luxembourg are on average more vulnerable than in other OECD member countries.
Moreover, at the beginning of the pandemic, Luxembourg decided to ensure that older people residing in residential facilities could remain there throughout their illness and that, unless required for medical reasons or desired by the resident or their family, they would not be hospitalised. As such, all residential facilities were provided with COVID kits supplied by the Ministry of Health's pharmacy service and containing the medication needed for end-of-life care and to provide palliative care at the person's bedside (see Section 3). This measure, taken in order to prevent older people in the terminal stage of their illness being taken out of their usual environment, has resulted in a high mortality rate in these residential facilities.
Figure 4.3. Mortality rates in Luxembourg's residential facilities are among the highest in all OECD member countries
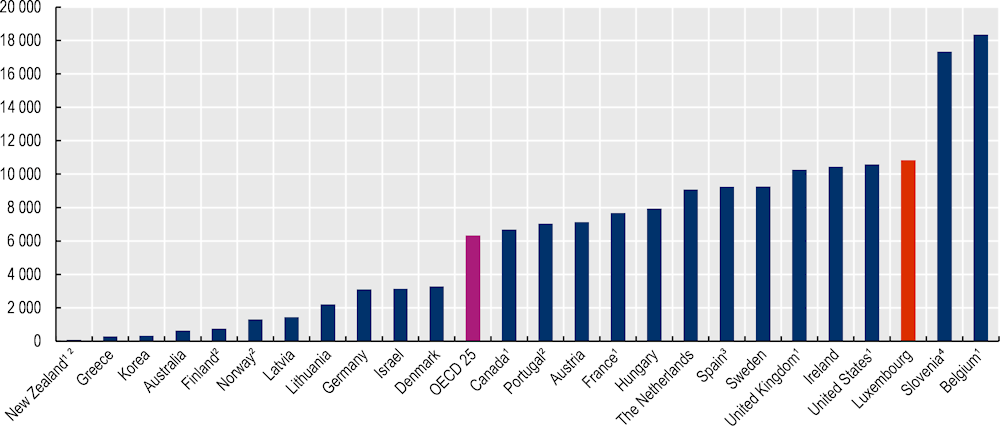
Note: Cumulative death data up to and including early February 2021.
1. Includes confirmed and suspected deaths.
2. Includes only deaths that occurred in long-term care facilities.
3. The data come from regional governments using different methodologies, some including suspected deaths.
4. Slovenia includes deaths that occurred in retirement homes and long-term social care facilities.
Source: Rocard, E., P. Sillitti and A. Llena-Nozal (2021[4]), "COVID-19 in long-term care: Impact, policy responses and challenges", OECD Health Working Papers, No. 131, OECD Publishing, Paris, https://doi.org/10.1787/b966f837-en.
The pandemic has also disproportionately affected disadvantaged members of the population and people born in another country. Hospitalisation and death rates differ significantly depending on income level (Van Kerm, Salagean and Amétépé, 2022[5]). Between 1 March 2020 and 27 October 2021, the risk of being hospitalised in intensive care for COVID-19 and the death rate were 1.6 times and 1.4 times greater, respectively, among people with a low standard of living than those with the highest standard of living. Some individuals born in another country were also more heavily affected by the pandemic in terms of rates of infection, hospitalisation and death (Van Kerm, Salagean and Amétépé, 2022[5]). The risk of developing severe forms of COVID-19 was, for example, two and three times higher for residents born in Italy and in any former Yugoslav country, respectively, than for people born in Luxembourg.
The unequal social distribution of COVID-19 morbidity and mortality (whereby rates are higher among the most disadvantaged populations) in Luxembourg is a reality that must be taken into account when developing health policies in the country. The aim is to strengthen the supply of health services to people who are less likely to receive care in the health system and to implement appropriate information and awareness-raising strategies.
4.2.3. While the effectiveness of the vaccination campaign in Luxembourg is undeniable, vaccination coverage is slightly lower than the average in OECD member countries
Several empirical studies have confirmed the effectiveness of the vaccination campaign in reducing hospitalisations and deaths in Luxembourg, especially among people over 70 years of age and those living in residential facilities (Alkerwi et al., 2021[6]; Government of Luxembourg, 2021[7]). As of 16 November 2021, vaccination was over 90% effective in protecting against hospitalisation and death for three age groups considered (70+, 50–69, and 25–49 years) (Government of Luxembourg, 2021[7]).
The vaccination campaign conducted by the interministerial crisis unit was a success for several reasons. Firstly, high priority was given to organising the vaccine campaign from March 2020 onwards, with the establishment of five thematic groups2 that began work very early on key topics such as defining prioritisation criteria, communication, vaccine supply and developing information systems. Thanks to the work carried out upstream by the thematic groups, Luxembourg was able to meet pharmaceutical requirements, with the High Commission for National Protection entering into contracts with Comptoir Pharmaceutique Luxembourgeois (a private wholesaler-distributor). This public-private partnership ensured that storage, set-up and delivery all ran smoothly, and that agent training could be organised. The work carried out upstream by the thematic groups also made it possible to develop information systems for sending vaccination invitations, making appointments online and recording information about those vaccinated. As an example, the Ministry of Health sent vaccination invitations to every person defined as a priority in the vaccination schedule, giving them the option of using the online vaccination application (Box 4.1). Luxembourg's vaccination campaign was therefore highly personalised, which was not the case in other OECD member countries.
Box 4.1. Luxembourg's vaccination campaign was more personalised than in some other OECD member countries
In Luxembourg, the Ministry of Health invited every person defined as a priority in the vaccination schedule to receive their vaccine. Each invitation included a personal access code that allowed the recipient to log into the vaccination application launched by the Government IT Centre. People could also use a hotline operated by the Health Directorate to receive help with making an appointment.
Other OECD member countries also used online appointment booking platforms to facilitate the implementation of the vaccination campaign, but users did not have personalised support mechanisms like those in place in Luxembourg. In France, for example, the Ministry for Solidarity and Health entrusted online management of vaccination appointments to various service providers, including the companies Doctolib, KelDoc and meSoigner. While these platforms made it easy to find an appointment, people in France did not receive letters or access codes, which can slow down the speed of a vaccination campaign, especially in the event of changes in the vaccination schedule.
Source: OECD (2022), Information-gathering questionnaire for the Luxembourg Crisis Management Evaluation.
In Luxembourg, the vaccination campaign started at the end of December 2020, almost a month earlier than in some neighbouring countries (such as France) in four vaccination centres. The country started to vaccinate health professionals, those working at health facilities (including residential facilities for older people) and residents of these facilities on 28 December 2020. The country's vaccination strategy had six phases based on individuals' risk of exposure, with the degree of vulnerability varying by age and health status (Government of Luxembourg, 2021[8]).
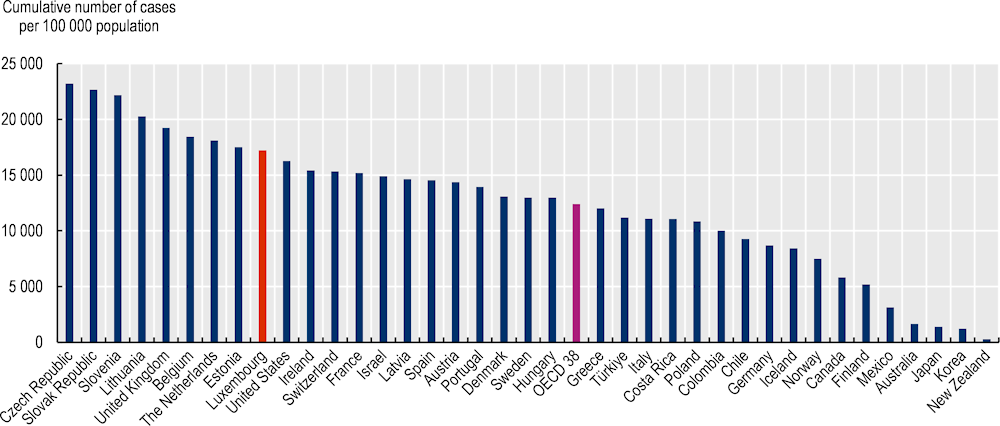
Between 28 December 2020 and 15 June 2021, the vaccination invitation response rate was 73%, demonstrating strong adherence to the vaccination campaign among the public (Government of Luxembourg, 2021[9]; Alkerwi et al., 2021[6]). In contrast, in May and June 2021, 12.7% of the population was still not ready to be vaccinated against COVID-19 (STATEC, 2021[10]), and at the end of May 2022, 73% of people living in Luxembourg had completed the full vaccination schedule (Figure 4.4), lower than the average in other European countries. It should be noted that about 5% of the resident population were probably vaccinated abroad and thus not identified by Luxembourg's system (which may mean that the official figures are an underestimate) (Bertemes and Hentschel, 2021[11]).
According to the Luxembourg Institute of Socio-Economic Research, vaccination rates are positively correlated with standard of living, and vary significantly by country of birth. For example, high-income populations are almost 80% more likely to be vaccinated, compared to only 58% among low-income populations, with these differences remain after adjusting for other socio-demographic characteristics (Van Kerm, Salagean and Amétépé, 2022[5]).
In order to improve vaccination coverage, the government of Luxembourg has proposed various actions to reach people with lower vaccination rates, such as young people aged 20 to 35, secondary school students and isolated or vulnerable populations. These initiatives, which are all equally important, include setting up lists where people can opt in to be vaccinated and using mobile teams to vaccinate older people in their homes, residents in care homes, students in secondary schools and people in certain communes. These efforts are remarkable and were also implemented in the majority of OECD member countries: by 2022, at least 18 other countries had implemented home-based vaccination with the use of mobile teams (OECD, forthcoming[12]).
Figure 4.4. The proportion of the population who completed the vaccination schedule is lower in Luxembourg than the OECD average
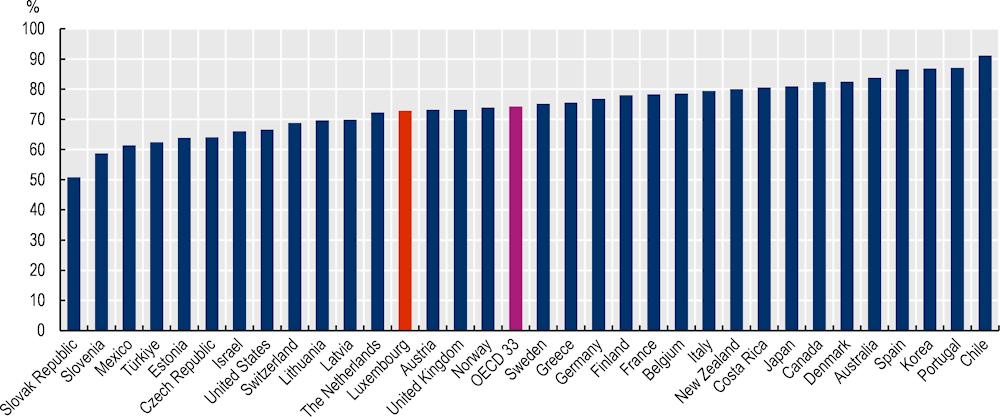
Note: The percentage represents the total number of people who received all doses prescribed by the initial vaccination protocol, divided by the total population of the country.
Source: Our World in Data (accessed 1 June 2022).
The government of Luxembourg conducted several communication campaigns in response to vaccine hesitancy, including the Ech si geimpft, an Du ? [I am vaccinated, are you?] campaign, which encouraged people to discuss COVID-19 vaccination with their general practitioner (GP) to allay any fears or concerns they may have had. A telephone line was set up to allow vaccine-hesitant people to discuss their fears and concerns with doctors from the Centre Hospitalier de Luxembourg (CHL). In order to educate the country's health professionals and best prepare them to answer patients' questions, the Health Directorate held "Lunch Talks", during which experts shared information about COVID-19 vaccines with them and answered their questions. "Expert Videos" were also created, in which experts from Luxembourg's scientific community (mainly professors from the University of Luxembourg and the Luxembourg Institute of Health) explained the vaccines to the general public.
The vast majority of the government's communication campaigns on the subject were written in the country's five main languages: Luxembourgish, French, German, English and Portuguese, and many were also translated into Tigrinya, Spanish, Russian, Albanian, Serbian and Turkish.
With its Loss dech impfen! Och an denger Gemeng [Get vaccinated! Even in your commune] initiative, the government made vaccination even more accessible to citizens. This was accompanied by leaflets sent out in advance to all households in each commune. This targeted communication campaign also identified the sociocultural profile of the communes. Based on this profile, the leaflets were translated into further languages to include those particularly present in these communities. In addition, as part of the vaccination communication efforts, the government reached out to the country's religious communities and provided them with information. In collaboration with the Catholic community, a video address was recorded with a religious representative to respond to the community's hesitations.
Finally, the Impfbotschafter (vaccination ambassador) and Froen un d'Santé (Facebook Live health Q&A) formats were also used to counter vaccine hesitancy. Vaccination ambassadors are representatives of the healthcare roles who volunteer to raise awareness in their personal and professional environments. Thanks to regular training sessions organised by the Health Directorate, they were prepared for their mission, received support in their activity and were able to answer citizens' questions through direct personal contact. The Froen un d'Santé format was an event that took place on social media almost weekly in which experts answered questions from the public live. The format won the Patient Experience Award at the Luxembourg Healthcare Gala in July 2022.
These awareness-raising activities, which are targeted at the populations least likely to be vaccinated and are based on multisectoral partnerships, must be strengthened in order to further increase vaccination coverage in Luxembourg, particularly among disadvantaged populations and those born in another country. It should also be noted that although many GPs participated in the vaccination campaign in vaccination centres, private practices were only involved in the vaccination campaign in Luxembourg later on. However, private GPs promote vaccination, especially with their patients. It is difficult to determine whether earlier deployment of COVID-19 vaccination in private practices would have been a key factor in reducing vaccine hesitancy or reluctance among patients, but national surveys conducted in the United States have revealed that the majority of disadvantaged people prefer to be vaccinated in their doctor's office rather than elsewhere (The Commonwealth Fund, 2021[13]; Frost, 2021[14]). Retail pharmacies were only authorised to administer vaccines against COVID-19 late in the process: starting from March 2022 in Luxembourg, compared with March 2021 in England, France and Switzerland and June 2021 in Italy.
4.2.4. Approximately 60% of patients with COVID-19 report at least one symptom more than one year after the acute phase of infection
In Luxembourg, a significant proportion of patients with COVID-19 continue to feel the effects of the disease several months later. According to estimates by the Luxembourg Institute of Health (Luxembourg Institute of Health, 2022[15]), one in six COVID-19 patients report at least one symptom one year after the acute phase of infection, with fatigue, shortness of breath, and irritability the most common ones. One-third of COVID-19 patients continued to experience fatigue one year later, 13% reported that respiratory symptoms were affecting their quality of life, and more than half (54%) had ongoing sleep problems.
The Luxembourg Ministry of Health has prioritised multidisciplinary care for long COVID, in partnership with CHL, GPs and certain rehabilitation facilities, in order to develop a person-centred care network (Government of Luxembourg, 2021[16]). A pilot project began on 1 August 2021, with a budget of EUR 1.01 million (Centre Hospitalier du Luxembourg, 2021[17]). The implementation in Luxembourg of multidisciplinary management of patients with long COVID, co-ordinated between GPs, specialists and hospitals, is one of the best practices in OECD member countries to respond effectively to this new public health challenge (OECD, forthcoming[18]).
4.3. The indirect consequences of the pandemic in Luxembourg
The indirect consequences of the pandemic in Luxembourg are worrying, both in terms of healthcare utilisation, and in terms of deteriorating mental health (mainly among young people and people in employment).
4.3.1. Luxembourg recorded a decline in consultations with health professionals
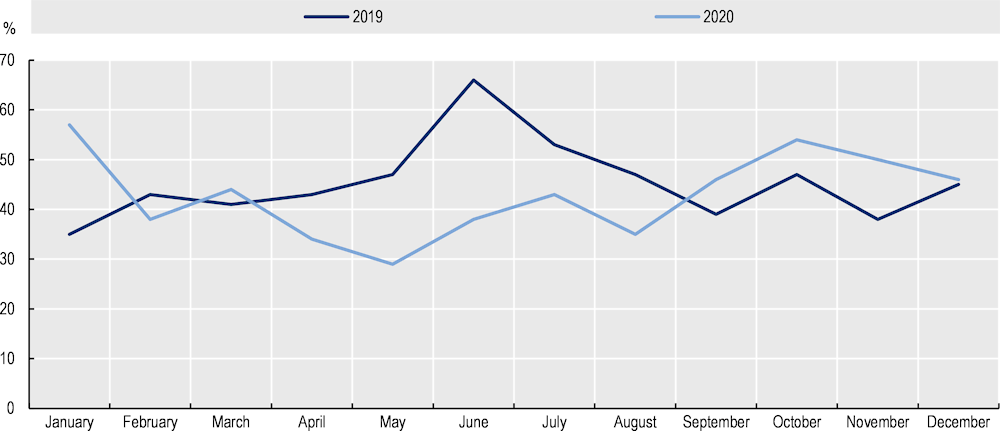
Data on the number of consultations with different health professionals, and analysis of how this has changed over time, show that the number of consultations fell in 2020 compared with 2019. GPs, dentists, dermatologists, ophthalmologists, paediatricians and psychiatrists saw their consultations decrease by more than 10% throughout the year (Figure 4.5). Similar findings were also observed in other OECD member countries, such as Australia, Austria, Belgium, France, Norway and Portugal (OECD, 2021[19]).
Figure 4.5. Changes in the number of consultations with selected health professionals in cities, 2019 compared with 2020
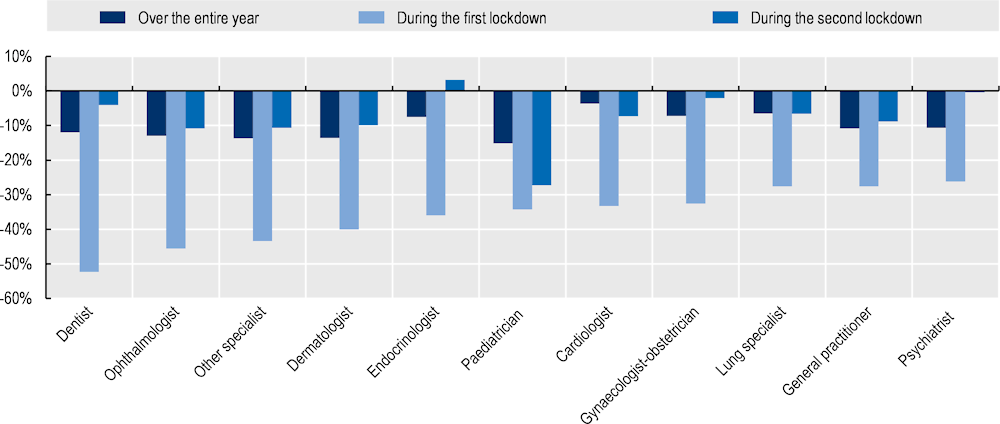
Note: The data include outpatient visits and remote consultations. The data compare the number of consultations in 2020 with 2019 (over the entire year), then March through May 2020 (the first lockdown) is compared with the same period in 2019, and November and December 2020 (the second lockdown) are compared with the same period in 2019.
Source: General Inspectorate of Social Security of Luxembourg (2022).
For all health professionals, the drop-in activity was particularly sharp during the first lockdown. The number of consultations with health professionals fell by more than 26% in the March to May 2020 period compared with the same period in 2019 (Figure 4.5). Dentists, ophthalmologists and endocrinologists saw their activity drop significantly, with a reduction of over 40% in the number of consultations. The decrease in the number of consultations during the second lockdown was much less pronounced, with the exception of paediatricians, who saw their activity fall by 27%. However, it is still difficult to assess the consequences of the decline in consultations on the health of the population in Luxembourg.
4.3.2. Hospital activity decreased and the number of non-urgent operations reduced in most hospitals
To increase the capacity of the health system and to respond to the outbreak of COVID-19 cases, Luxembourg quickly cancelled certain hospital treatments. Non-urgent and non-essential operations were postponed in Luxembourg's hospitals, which may have led to increased waiting times for certain types of surgery. The hospitals for which data are available (CHL, Centre Hospitalier Emile Mayrisch and Hôpitaux Robert Schuman) show a clear decrease in operations over the whole year of 2020 compared with 2019, ranging from -6% at CHL to -20% at Centre Hospitalier Emile Mayrisch (Figure 4.6). Similarly, the number of visits to the emergency department decreased by between 11% and 40% in 2020 compared with 2019, and the number of medical imaging exams also decreased by between 17% and 29% in 2020 compared with 2019. The reduction in hospital activity was particularly significant during the first lockdown. At CHL, for example, March to June 2020 saw a sharp decline in activity compared to 2019, with a drop of almost 30% in operations and the number of visits to the emergency department (Antares Consulting, 2020[20]). The impact of this decrease in activity on the health of the population and the possible resulting loss of opportunity cannot yet be assessed.
Figure 4.6. Hospital activity fell in 2020 compared with 2019
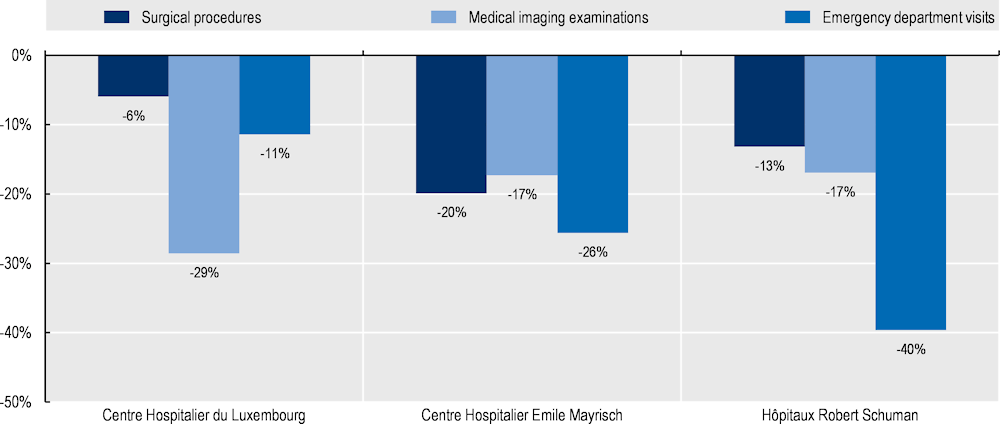
Note: At CHL, the decrease in medical imaging examinations corresponds only to radiology procedures.
Source: 2020 annual reports of the three hospitals available online: CHL, Centre Hospitalier Emile Mayrisch and Hôpitaux Robert Schuman.
4.3.3. Cancer screening and treatment were delayed in 2020
Organised screenings for certain cancers were disrupted by the lockdown in Luxembourg. For the year as a whole, the number of breast cancer screenings fell by 7% in 2020 compared to 2019. The drop in the number of screenings was greatest during the first lockdown (Figure 4.7). As the first lockdown came to an end, activity returned with an increase in the number of breast cancer screenings in June 2020. Similarly, the number of cervical cancer screenings carried out decreased by 6% in 2020 compared with 2019.
In total, and based on data from the National Health Laboratory, regarding the number of pathological diagnoses of malignant tumours each month in 2019 and 2020, Fondation Cancer estimates that approximately 10% of expected cases of cancer were not detected and surgeries were not performed in 2020 (Mittelbrownn, 2021[21]).
Figure 4.7. Breast cancer screening dropped significantly in 2020 compared with 2019
Cancer treatment has also suffered from delays, with a sharp decline in the number of oncology procedures. The number of hysterectomy operations, for example, dropped by 27% in 2020 compared with 2019. Similarly, the number of mastectomies fell sharply during the first lockdown, then gradually returned to levels close to those seen in 2019. From September 2020, the level of activity exceeded that recorded over the same period in 2019 (Figure 4.8).
A survey of a panel of oncologists shows that lockdown reduced the total number of radiotherapy sessions by almost a quarter in May 2020 compared with the same period in 2017 and 2019 (Backes et al., 2020[22]). Even after lockdown, the number of radiotherapy sessions remained lower between July and October 2020 than during the same period in 2017 and 2019. Data provided by the Centre National de Radiothérapie du Luxembourg, or National Centre for Radiotherapy in Luxembourg, show that over the whole year of 2020, the total number of radiotherapy sessions decreased by 5.3% compared to the previous year (i.e. 1 390 fewer sessions).
Delays in the diagnosis and treatment of cancer are likely to have a serious impact on the patient's prognosis. Available estimates show that a four-week delay in surgical treatment for cancer increases the risk of death by about 7%, while four-week delays in non-surgical treatment may increase the risk of death by 13% (Hanna et al., 2020[23]).
Activity data for 2021, supplemented by data from Luxembourg's National Cancer Registry, will make it possible to conduct a more precise assessment of the indirect consequences of the pandemic on the diagnosis and treatment of cancers in the country.
Figure 4.8. Cancer surgery activity decreased during the first lockdown
4.3.4. The health crisis has had a significant impact on the mental health of the population, particularly among younger people and those in employment
In Luxembourg, as in many OECD member countries, the pandemic and the measures implemented to curb the spread of the disease during the first two waves have had significant negative consequences on people’s mental health.
A survey conducted by the National Institute for Statistics and Economic Studies in collaboration with ILRES shows signs of a clear deterioration in the mental health of Luxembourgers. One in three residents say their mental health deteriorated during the COVID-19 pandemic, a proportion that reduces with age (STATEC, 2020[24]). Around 37% of 18–44-year-olds reported that their mental health had deteriorated, compared to 22% of those aged 65 and older. The main factors associated with the deterioration of mental health were a decline in physical health, a loss of job security, increasing expenses (STATEC, 2020[24]) and a deterioration in social relationships during periods of lockdown (STATEC, 2020[25]).
The results of the COVID-KIDS study also show a deterioration in satisfaction among children. One-third of children aged 6 to 11 and 43% of children aged 12 to 16 reported that their satisfaction with life had decreased. Children also reported experiencing negative emotions and worries frequently or very frequently during the pandemic. One in six of younger children (6–11 years) and one-third of older children (12–16 years) reported experiencing negative emotions (Kirsch et al., 2022[26]).
In addition, the eighth Quality of Work Index survey conducted in 2020 showed that risk of falling into depression had increased as a result of the COVID-19 pandemic (CSL, 2021[27]). The share of survey participants at high risk of depression had increased from 8% in 2019 to 11% in 2020. Today, one in three workers are at risk of depression as a result of the pandemic, and more than one in ten show very strong signs of depression.
4.4. How resilient was pandemic management in Luxembourg?
4.4.1. Luxembourg anticipated the pandemic risk very early on
Luxembourg has an influenza pandemic ERP that has only partially met the needs of managing the crisis
In the context of the adoption of the International Health Regulations, Luxembourg has had an influenza pandemic ERP since 2006, following the spread of avian influenza in 2004 and the H1N1 pandemic in 2009. The influenza pandemic ERP defines the planning and preparedness, surveillance, prevention and consequence management to address the risk of an influenza pandemic (Government of Luxembourg, 2021[28]).
While the 2009 H1N1 pandemic required that the influenza pandemic ERP be put into action, it must be noted that it has not been updated since 2006. Nevertheless, the lessons learned from that pandemic and the Ebola epidemic contributed useful additions to the range of measures used to tackle this pandemic. It should also be noted that no pandemic preparedness exercises were actually conducted prior to the first case of COVID-19, indicating the low operationality of the influenza pandemic ERP (see Chapter 2). Similarly, some practical aspects have been neglected in the influenza pandemic ERP, such as the plan for continuity of medical care for conditions other than the pandemic disease; training and education on infection prevention and control measures for health professionals; logistics and research and development of vaccines and other drugs; psychological support for the public; and civil society participation. All of these components are essential for assessing needs and managing a pandemic crisis well (see Chapter 2).
Interministerial meetings were held at the end of January 2020, with the crisis unit set to work on 1 March 2020
Since the end of January – and at the request of the Prime Minister – the Governmental Council, the High Commission for National Protection and the various stakeholders met on numerous occasions (until 28 February), in the form of either a crisis unit or interministerial meetings to analyse the level of preparedness of the measures included in the influenza pandemic and Ebola ERPs and to assess crisis management needs.
On 1 March 2020 (the date the first positive case was detected in the country), the crisis unit was set to work. Its membership was modified regularly from 15 March 2020 onwards to better reflect concerns relating to the health crisis. The crisis unit, chaired by the High Commission for National Protection and the Ministry of Health, is composed of several working groups, which oversee and work on separate areas, such as hospitals, diagnosis and contact tracing, testing, primary care, care homes and care networks, logistics, the health reserve and communication (see Chapter 3). The unit co-ordinates all the work carried out by hospitals, laboratories, primary care providers, pharmacies, nursing homes and care networks, while managing logistics, medical supplies, health staffing, communication and psychosocial support around the crisis.
The flexibility of the crisis unit and the multidisciplinary composition of the working groups allowed Luxembourg to be reactive and innovative in managing the crisis. Many public actors at all levels of governance (including communes and fire departments) quickly joined the national effort to tackle the crisis. However, it is regrettable that civil society and user representatives were not more involved in the various crisis unit working groups during the pandemic (see Chapter 3).
4.4.2. Structural difficulties weakened the level of operational preparedness for the pandemic
National stocks of PPE were initially insufficient, but the logistics unit quickly placed several orders
The lack of knowledge about the good status of PPE stocks in health and care institutions reflects a lack of preparedness to face such a large pandemic in Luxembourg. The logistics unit,3 as the sole government buyer, manager and distributor of PPE and medical devices, quickly overcame this lack of preparedness.
The High Commission for National Protection acquired 200 000 FFP2 masks in 2017 as part of the influenza pandemic ERP, and national stocks of PPE totalled 1 048 000 units of surgical masks, 235 135 units of FFP2 masks, 20 340 units of Tyvek gowns, and 780 100 units of gloves prior to the declaration of a state of emergency. In accordance with crisis plans, these national stocks were used primarily to cover the needs of critical infrastructure and were not designed to ensure the wide distribution of masks and other equipment to the general population or to businesses in general.
Health and care facilities were not required to monitor their stocks, so when the state of emergency was declared, the government was not aware of the amount they held of these supplies. For this reason, the logistics unit conducted a national PPE census on 19 March. Estimates based on daily consumption over the previous seven days as at 19 March indicated that there were not enough surgical masks in stock to cover the needs of healthcare workers in the event of an outbreak.
Daily stock management monitoring was set up to provide daily updates on the delivery and use of equipment for all hospitals and care facilities. This monitoring has been essential for assessing needs in real time and preventing equipment shortages. Alongside this, supply networks were expanded, enabling essential PPE and medicines to be acquired from different suppliers (based in Asia in particular) and using all mechanisms, including the European Union. This equipment included masks, gloves, disinfectants and protective clothing, as well as the respirators and medication needed to treat COVID-19 patients. According to High Commission for National Protection figures, more than 84 million units of surgical masks and 3.3 million units of FFP2 masks were ordered directly from China in March 2020. These orders were placed before the European and global PPE market was saturated. The logistics unit also purchased four scanners that were made available to the four hospitals.
PPE and medical devices purchased by the logistics unit quickly made up for Luxembourg's shortcomings in terms of preparedness. To strengthen the level of preparedness for similar crises in the future, the government of Luxembourg is planning to set up a central purchasing unit for critical products that will manage procurement, logistics and storage at the national level, demonstrating Luxembourg's ability to adapt.
No information system existed at the beginning of the pandemic to manage the crisis
At the beginning of the crisis, Luxembourg did not have an information system in place capable of monitoring the evolution of the pandemic, in terms of either epidemiological surveillance or the use of health resources, particularly for the hospital system. Nevertheless, the implementation of the Qlik information system on 17 March 2020 enabled the spread of the virus to be monitored and pressure on hospitals to be assessed.
While reporting of certain communicable diseases has been mandatory in Luxembourg since the law of 1 August 2018 was implemented as part of public health protection (Official Journal of the Grand Duchy of Luxembourg, 2018[29]), the computer application used to manage and monitor infectious diseases was not designed to perform ad hoc data analysis and did not allow for the collection of negative polymerase chain reaction (PCR) test results under mandatory reporting. It was therefore not possible to monitor the positivity rate and to obtain a complete overview of epidemiological developments in the country (Government of Luxembourg, 2021[30]). The other information systems used also proved inadequate to meet the information and indicator requirements for managing the crisis. In March 2020, there were not enough data available on hospitalisations to conduct daily surveillance and analyse the impact of the pandemic on hospital operations. There was, for example, no monitoring of intensive care beds, COVID-19 and non-COVID-19 occupancy rates, emergency services’ activity levels, and COVID-19 hospital admissions. For the long-term care sector, there were no harmonised indicators, either quantitative or qualitative, to document the activities and resources of the various facilities (see Chapter 3).
The crisis unit's monitoring working group has made major efforts to develop new information systems to monitor the spread of the virus and assess pressure on hospitals. A collection and compilation system and an automatic analysis and reporting system were progressively set up in collaboration with the various crisis unit working groups, health system actors and policy makers. Since 17 March 2020, the new centralised Qlik information system has enabled the number of COVID-19 cases and deaths in hospitals to be recorded and hospital capacity to be identified in real time. For long-term care facilities, this measure arrived later; it was not until April 2020 that the Qlik information system was used to identify cases in such facilities. Over the months, the integration of the various data sources into the new information system (Box 4.2) enabled numerous statistics and dashboards to be introduced that were used on a daily basis to help manage the crisis.
While the implementation of the Qlik information system has been critical to Luxembourg's response, the government must continue its efforts to develop a single information system, where databases are interoperable, with a unique identifier for patients and where health services are automatically linked. Despite improvements linked to the pandemic and to the implementation of shared medical records, Luxembourg's information systems are still incompatible. As some OECD member countries have shown, an integrated health information system allows for better management of health crises. Canada, Denmark, Estonia, Finland, South Korea, Latvia, the Netherlands and Sweden all stand out for their integrated information systems that linked data from multiple health sectors and provided real-time data from the onset of the pandemic crisis (Oderkirk, 2021[31]).
Box 4.2. The Qlik database
The Qlik application brings together COVID-19 data from various actors (such as laboratories, hospitals, care homes, the General Inspectorate of Social Security, and advanced care centres) in different thematic dashboards that allow users to follow the evolution of the pandemic and conduct relevant analyses.
It has been progressively improved by integrating other data (such as those from the mass screening programme and contact tracing, those relating to vaccination administration and coverage, those concerning the status of wastewater, and individual data from the General Inspectorate of Social Security) to perform sectoral analyses and identify possible sources of outbreaks. Automated daily reports were developed for several bodies (such as the Ministry of Education, the Ministry of Family Affairs and the Fédération des Hôpitaux Luxembourgeois, or Luxembourg Hospitals Federation). Aggregate data are also publicly available.
Source: OECD (2022), Information-gathering questionnaire for the Luxembourg Crisis Management Evaluation.
Luxembourg is highly dependent on cross-border healthcare workers
The Luxembourg health system is critically dependant on people from other countries in terms of healthcare and medical staff, making it extremely vulnerable to border closures during initial efforts to contain the COVID-19‑ pandemic.
Luxembourg's government has been concerned about the shortage of health professionals for several years. The number of new graduates each year does not make up for natural retirements in some disciplines. As a result, the percentage of doctors from other countries continues to increase every year. The share of doctors living abroad but practising in Luxembourg almost doubled between 2008 and 2017, from 15.6% to 26.4% (IGSS Luxembourg, 2021[32]). In 2019, 62% of healthcare professionals, 21% of GPs and 34% of specialist doctors practising in Luxembourg were living abroad (Lair-Hillion, 2019[33]). Moreover, despite the presence of cross-border workers, Luxembourg has very few doctors compared to other OECD member countries. With approximately 3 doctors per 1 000 inhabitants in 2019, Luxembourg is well below the OECD average (3.6 per 1 000 inhabitants), despite an increase of 39% since 2000 (OECD, 2021[19]). This low density of doctors was, until now, mainly due to the lack of medical training available in the country, which created a dependence on doctors trained elsewhere. Luxembourg's first Bachelor of Medicine degree was created in 2021.
On the other hand, Luxembourg has one of the highest densities of nurses in the OECD (11.7 nurses per 1 000 inhabitants compared with the OECD average of 8.8 per 1 000 inhabitants). However, more than two-thirds of practising nurses live in neighbouring countries (29% in France, 24% in Germany and 12% in Belgium) but are attracted by the better salaries and good working conditions on offer in Luxembourg (OECD/European Observatory on Health Systems and Policies, 2022[2]).
As border closures were not one of the measures included in the influenza pandemic ERP, Luxembourg had to react quickly and work in close co-operation with Germany, Belgium and France. Passes were distributed to healthcare professionals to facilitate border crossings, and the government of Luxembourg offered free temporary accommodation to cross-border employees of the healthcare and long-term care sector starting in April 2020. These measures demonstrate a commitment to solidarity and co-operation between countries that should be commended.
In order to meet the needs of its population and to be less dependent on workers from other countries during future health crises, Luxembourg must invest more in its healthcare workforce. Increasing medical staff, introducing multidisciplinary approaches and adapting the training and role of healthcare professionals are all extremely relevant policies given Luxembourg's situation (Box 4.3).
Box 4.3. Overview of policies for investing in the health workforce in selected OECD member countries
Increasing medical staff
In France, the Contrat d'aide à l'installation des médecins is a one-off grant paid to doctors in two instalments. Its objective is to help doctors meet the investment costs associated with starting work, such as premises, equipment and other miscellaneous expenses. There are also contrats d'engagement de service public, whereby medical students and interns are given a monthly allowance. In return, the students undertake to practise in an area determined by the regional health agencies after completing their training for a period equal to that during which they received the allowance.
Adapting the responsibilities of health professionals
In Australia, Canada, Estonia, France, Ireland, Latvia, Sweden and the United Kingdom, nurses' skills grew through the development of their initial and continuing training. In these countries, the tasks of advanced practice nurses tend to include prevention and screening. Retail pharmacists also play a greater role in health promotion and prevention in Belgium, England, Finland, France, Italy and Switzerland. During the COVID-19 pandemic, pharmacists saw their responsibilities expanded to include maintaining essential therapeutic monitoring and protecting the most vulnerable from exposure to the virus. In addition, the expansion of pharmacists' competencies allowed them to exceptionally renew expired prescriptions for patients with chronic conditions (France), administer COVID-19 vaccines (in France, the United Kingdom and Italy) and perform diagnostic tests (the United States, Australia and England).
Pursuing multidisciplinary approaches
In Canada, the United Kingdom, France, Australia and the United States, multi-professional health centres (as opposed to isolated practices) offer co-ordinated care, with greater emphasis on health promotion, prevention, therapeutic education and social support. Multidisciplinary approaches are not only essential for managing chronic conditions but also help to better monitor and reduce lifestyle-related risk factors, especially among the most disadvantaged. The use of multi-professional health centres also aims to ensure an adequate supply of care in areas with low medical density and to address financial concerns about access to care for disadvantaged populations.
Source: OECD (2020[34]), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en; OECD (forthcoming[35]), Improving the Resilience of Health System.
Care homes and networks suffered from a lack of infection prevention and control knowledge and medical support at the beginning of the health crisis
As demonstrated in Section 2 of this chapter, the health situation in long-term care facilities was severe in Luxembourg. This was due to two structural factors: a lack of expertise in infection prevention and control, and a lack of medical support in long-term care facilities. While long-term care facility managers received numerous memos from the Health Directorate, the Ministry of Health and the Ministry of Family Affairs at the start of March 2020, it was not until the end of March that orders and recommendations on infection prevention were issued. As a result, the long-term care sector began responding too late.
The Health Directorate did not issue an order for the care of vulnerable people until 30 March 2020 (Government of Luxembourg, 2021[36]), followed by recommendations on the strategy for using PPE on 6 April 2020 (Abdelrahman et al., 2021[37]) and on preventing infection in long-term care facilities on 23 April 2020 (Government of Luxembourg, 2020[38]). Training in good hygiene practices and infection prevention for long-term care facilities was implemented from 28 March onwards,4 alongside the use of medical support devices from early April:
the provision of COVID kits (kits supplied by the Health Directorate containing the medication needed for the regular or on-call doctor to provide end-of-life care or palliative care at the person's bedside)
the establishment of a dedicated on-call line of GPs for residential facilities for older people
the hospitalisation of anyone with COVID-19 on the advice of the doctor for the person’s well-being
the implementation of hygiene training for healthcare workers, accompanied by site visits from the Health Directorate and the Ministry of Family Affairs to assess whether the training meets the needs of the field
the establishment of a hygiene officer and a hygienist within the Confederation of Care and Assistance Providers.
While these measures are essential to provide medical support to long-term care facilities, improve care co-ordination and increase capacity for hygiene and infection control, they would have benefited from being implemented earlier given the severity of the disease for older people. This would have reduced the excess mortality rate of these residential facilities, which was 60% in April 2020 (Abdelrahman et al., 2021[37]). These measures should be made permanent to help alleviate the structural difficulties faced by long-term care facilities5 and enable a faster response to future health emergencies.
Moreover, according to the various stakeholders interviewed during the information-gathering mission, the response was often different between the health sector and the long term-care sector. Luxembourg, for example, chose not to prioritise vaccination for people in contact with residents of long‑term care facilities, who are the most vulnerable to severe forms of the disease. As such, external service providers working in long-term care facilities (e.g. cleaners and catering staff) were not defined as a priority population when the vaccination campaign was launched on 28 December 2020, whereas this was the case in the hospital sector.
In this regard, it is important to remember that it is the Ministry of Family Affairs – not the Ministry of Health – that is responsible for overseeing long-term care facilities. As discussed in the Waringo evaluation report (Abdelrahman et al., 2021[37]), long-term care facilities received recommendations from both ministries, which meant that messages were less clear and hindered the day-to-day management of the pandemic in these facilities. Luxembourg should therefore give careful consideration to the issue of supervision of long-term care facilities, including integrated centres for older people and care homes, which provide other services in addition to accommodation. In France, supervision of long-term care facilities falls under the responsibility of the Ministry for Solidarity and Health, while in Belgium it is the responsibility of the federal public service Santé Publique or Public Health (formerly the Ministry of Social Affairs and Public Health).
4.4.3. The responsiveness of the Luxembourg health system allowed it to absorb the shock
Luxembourg’s mass testing policy has proven to be effective in curbing the spread of the virus
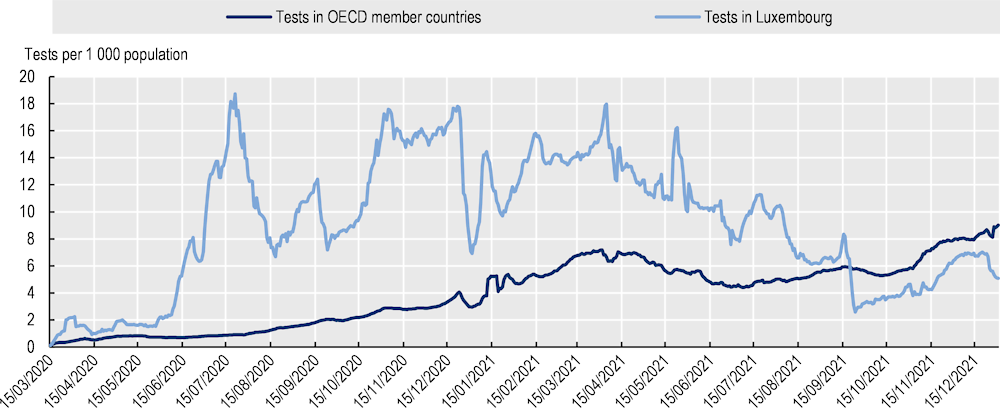
Intensive case testing was implemented at the start of the pandemic, beginning on 25 February 2020. Initially, people with symptoms of COVID-19 returning from areas defined as at risk for SARS‑CoV‑2 by the European Centre for Disease Prevention and Control were tested at home by health inspectors. The first tests were all performed by the National Health Laboratory, before testing capabilities were developed in private medical testing laboratories (Laboratoires Réunis, Ketterthill laboratories and BioneXt laboratories). Available data show that Luxembourg is among the countries with the highest testing capacity in the OECD, reaching up to 18 tests per week per 1 000 inhabitants in July 2020 (much higher than the average in other OECD member countries) (Figure 4.9).
Figure 4.9. Luxembourg has conducted far more tests than the average in other OECD member countries
The crisis unit’s testing working group carried out a wide range of actions in the field of testing (Government of Luxembourg, 2021[39]), demonstrating the government of Luxembourg’s commitment to containing the COVID-19 pandemic:
Numerous test sites were opened, such as advanced care centres, COVID-19 consultation centres and drive-through COVID-19 test centres.
Systematic screening of certain sectors of activity (such as construction, commerce, care and hospitality) was implemented in order to minimise the risk of infection at the end of lockdown.
Large-scale testing was implemented from 18 May to 15 September 2020 under the responsibility of the Luxembourg Institute of Health. Participation in this testing programme was voluntary and by personal invitation only. The first phase of large-scale testing guided the lifting of lockdown by identifying asymptomatic individuals in order to intervene early in virus transmission chains (Box 4.4).
At Luxembourg Airport, all passengers were able to get a free test upon entering the country from the end of May 2020.
Mobile teams were deployed, initially as part of large-scale, targeted testing, but also to respond to clusters of infections, for example, in schools, businesses and long-term care facilities.
Exceptional actions were carried out to encourage citizens to get tested by distributing free rapid antigen tests to businesses or directly to households.
School-based testing was also conducted by National Health Laboratory from November 2020 to July 2021 (over 32 800 tests conducted) and from September 2021 to December 2021 (over 9 600 tests conducted) (see Chapter 5).
The early and rapid detection of cases has been essential to limit and stop the spread of COVID‑19 in Luxembourg. The results of the evaluation of the first and second phases of large-scale testing demonstrate the effectiveness of the system in controlling transmission of the virus (Wilmes et al., 2021[40]). Based on modelling, the total number of possible cases would have been 42.9% higher without the large-scale testing programme.
Although Luxembourg’s testing policy stands out from other OECD member countries in terms of both its scope and the wide range of strategies it employed, it should be noted that this system was introduced much later in long-term care facilities. According to the Waringo report, PCR testing of all residents and staff in the facilities was not performed by the National Health Laboratory mobile teams until 21 April, more than one and a half months after the first positive case was detected in Luxembourg (Abdelrahman et al., 2021[37]). As part of the second phase of large-scale testing, mobile teams were deployed to all long-term care facilities on a planned and repeated basis, as well as whenever an outbreak of infection was detected (starting on 16 September 2020).6
Box 4.4. Large-scale testing is among the best practices of OECD member countries
Beginning on 18 May 2020 and continuing through 15 September 2020, the first phase of the large‑scale testing programme was implemented. The population was divided into three categories based on their risk of exposure to the virus, with each category being invited at different intervals. With a theoretical maximum capacity of 20 000 tests per day, 1 520 445 invitations for reverse transcription PCR testing were sent out during the first phase of the programme and 560 082 tests were performed. Under the second and third phases of the programme (beginning on 16 September 2020 and 15 September 2021, respectively), a PCR testing capacity of 53 000 tests per week was implemented across eight drive-through sites, one airport site, five mobile teams for certain facilities, and the option to get tested before or upon return from a trip abroad.
The large-scale testing strategy is among the best practices established by OECD member countries to reduce virus transmission, assess transmission dynamics and detect clusters in specific areas early. Among OECD member countries, only Korea, Australia and Latvia implemented large-scale testing policies (OECD, forthcoming[12]).
Source: OECD, based on documents sent by the High Commission for National Protection and the Health Directorate, and the information‑gathering mission.
The contact-tracing system was effective and allowed for personalised support
The large-scale testing programme was accompanied by a contact-tracing system that allowed for early detection of cases and outbreaks. This strategy, which aims to break chains of transmission, was implemented as early as March 2020 by the Health Directorate’s central contact-tracing unit. This system proved to be effective in identifying contact cases in an exhaustive manner and providing responses and support specifically for vulnerable population.
According to data from the contact-tracing unit, the system was effective in comprehensively identifying contact cases. In 2021, the average number of contacts per case in Luxembourg was 5.2. In total, as at 24 March 2022, 266 862 positive case investigations had been completed and 812 644 contacts had been processed. In addition, in periods of moderately high incidence, 90% of cases were called within 24 hours of receiving a positive result. Delays were nevertheless noted during the second wave of the pandemic (in October and November 2020) when it took 3.3 and 6.9 days for cases to receive a call from the contact-tracing unit, respectively (Government of Luxembourg, 2021[41]).
The success of the contact-tracing system in Luxembourg can be explained by three factors: i) major strengthening of the contact-tracing unit’s teams; ii) a support system for vulnerable populations; and iii) the implementation of the remote Care+ service, allowing case investigations to be conducted and online services to be provided to those testing positive:
The contact-tracing service employed health professionals from the Health Directorate and then recruited – through the health reserve mechanism – volunteers, staff from other agencies and staff who had been redeployed or made redundant due to the pandemic. According to data from the Ministry of Health, up to 400 people (300 full-time equivalents) were working on Luxembourg’s contact-tracing system at the same time. A training programme was developed for all new employees assigned to contact tracing.
It should also be noted that the contact-tracing system sought to investigate the origin of infection in some contact cases, as was also done in some other OECD member countries (such as Korea). This retrospective follow-up was implemented in some hospitals, residential and healthcare facilities, companies, schools and disadvantaged populations to document the circumstances and causes of infections. Advice and specific support were also offered to implement pandemic prevention and control measures. This support system was essential for providing responses to vulnerable populations, enabling better adherence to isolation measures and hygiene protocols.
Finally, the development of the Care+ service allowed all positive cases to be identified and investigated, clusters to be recorded, sources of infection to be determined, and quarantine and testing orders to be issued. By enabling the epidemiological analysis of transmission chains, this tool promoted the co-ordination of the different contact-tracing sectors of activity and allowed calls and complex investigations to be prioritised.
Intensive care bed capacity doubled during the first wave of the pandemic, but no additional beds had to be mobilised
Luxembourg provided sufficient hospital care during the COVID-19 pandemic thanks to a large plan which increased hospital capacity. While the measures put in place largely met the needs of the huge influx of COVID-19 patients, they resulted in the excessive suspension of operations and other non-emergency procedures, with potential losses of opportunity for patients.
The interministerial crisis unit’s hospital working group, in charge of co-ordinating hospital services, conducted an inventory of hospital capacity and intensive care beds on 16 and 17 March 2020 so that this capacity could be redeployed to treat COVID-19 patients. Four phases of operation were set out in the national COVID-19 surge capacity plan, with the objective of spreading patients across different hospitals and co-ordinating efforts according to the magnitude of the pandemic. The reorganisation of hospital services also resulted in temporary facilities being set up for the admission and treatment of patients requiring hospitalisation, with, for example, a field hospital being opened in the CHL car park, additional intensive care beds being installed, and recovery rooms being redeployed to intensive care units. In addition, in hospital emergency departments, the development of patient triage protocols led to the implementation of specific pathways for COVID and non-COVID patients.
As a result of these different measures (and based on the modelling performed by the COVID-19 Task Force (see Chapter 3), the number of level 3 intensive care beds (resuscitation beds) more than doubled during the first wave of the pandemic, from 102 before the pandemic to 244 on 19 March 2020 (Figure 4.10). The reorganisation of hospital services therefore helped Luxembourg to respond to the large influx of patients both from Luxembourg itself and from neighbouring countries (notably France, Belgium and Germany).
Figure 4.10. Intensive care bed capacity more than doubled during the first wave of the pandemic
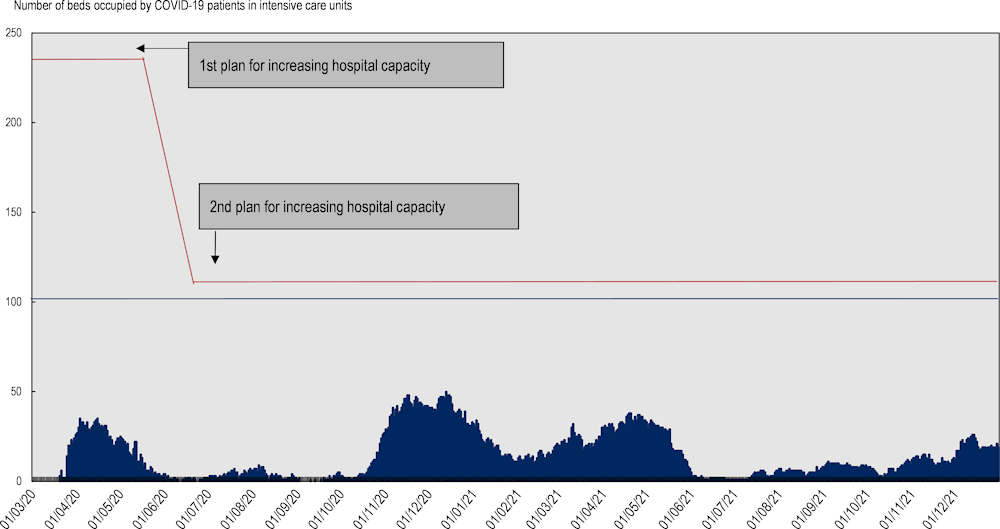
Note: The blue area represents the daily number of COVID-19 patients in level 3 intensive care. The blue line represents initial hospital capacity in level 3 intensive care beds before the pandemic. The red line represents the additional hospital capacity mobilised during the pandemic.
Source: OECD (2022), mission to gather information from the Ministry of Health.
A list of non-COVID hospital procedures to be suspended was defined in parallel with the plan to increase hospital capacity. According to the Ministry of Health, the phasing out of hospital activity during the first phase of the pandemic was inadequate and resulted in an excessive reduction in surgical and other non-emergency procedures (as reported in Section 2 of this chapter). The government of Luxembourg drew lessons from the first wave when defining a second plan to increase hospital capacity in July 2020 onwards. This more detailed plan made it possible to better pace the response and maintain as much non‑COVID hospital activity as possible after July 2020.
A wide range of policies helped to prevent a shortage of healthcare workers for COVID-19 care
In response to the increased demand for healthcare during the COVID-19 pandemic, the government of Luxembourg implemented a wide range of policies to mobilise additional staff members and prevent a shortage of healthcare workers for COVID-19 care. However, this mobilisation for COVID-19 care came at the expense of other areas of care, such as outpatient and non-emergency hospital treatment.
The government launched a mandatory census of all regulated health professionals, including medical interns, students, retirees and staff on unpaid leave in March 2020.A platform for the registration of medical and non-medical volunteers was also set up, allowing a health reserve7 to be established in Luxembourg in March 2020. Enrolment in the health reserve was open to all practitioners (including those working in private practices) and the contracts included an attractive hourly remuneration – a key factor in the success of the scheme. According to data provided by the Ministry of Health, 2 378 doctors, 6 120 other healthcare workers and 3 635 other volunteers had registered for the health reserve by 23 March 2020. During the first wave of the pandemic in 2020, 716 workers were deployed to different entities in the health system by the health reserve (Table 4.1). During the second wave, which started in November 2020, the number of care workers assigned to COVID pathways in hospitals almost doubled thanks to the health reserve. Between December 2020 and February 2022, 925 healthcare workers (nurses, doctors, physiotherapists and pharmacists) were mobilised by the health reserve for the COVID-19 vaccination campaign. These data attest to the usefulness of the health reserve in Luxembourg for the rapid mobilisation of workers in various fields of expertise. Among OECD member countries, only 13 other countries used a health reserve during the COVID-19 pandemic (Canada, Costa Rica, Finland, France, Greece, Israel, Italy, Latvia, Lithuania, Slovenia, Spain, the United Kingdom and the United States). In the short and medium term, the health reserve should be maintained, with volunteers receiving continuous and adapted training so they can be mobilised quickly during future pandemics.
Table 4.1. The health reserve mobilised more than 700 workers during the first wave of the pandemic
|
Number of professionals mobilised, by service |
|
|---|---|
|
Administration |
22 |
|
Telephone helplines |
29 |
|
Test centres |
30 |
|
Advanced care centres |
240 |
|
Hospitals |
163 |
|
Supported housing |
5 |
|
Care homes |
188 |
|
Home care services |
35 |
|
Care and socio-pedagogical support services |
4 |
|
Total |
716 |
Source: OECD (2022), Information-gathering questionnaire sent to the Ministry of Health.
In addition, with regard to hospitals and residential facilities for older people, a number of other policies were implemented during the different waves of the pandemic (such as adjusting legal working hours (Official Journal of the Grand Duchy of Luxembourg, 2020[42]), reorganising clinical teams, providing training for students and healthcare workers, and not closing borders to allow the movement of cross‑border health workers). All of these measures made it possible to avoid a shortage of health workers to respond to the COVID-‑19 pandemic in Luxembourg, as well as Germany, Finland and Switzerland (Figure 4.11).
Figure 4.11. Unlike the majority of OECD member countries, Luxembourg did not suffer from a shortage of health workers to respond to the COVID-19 pandemic
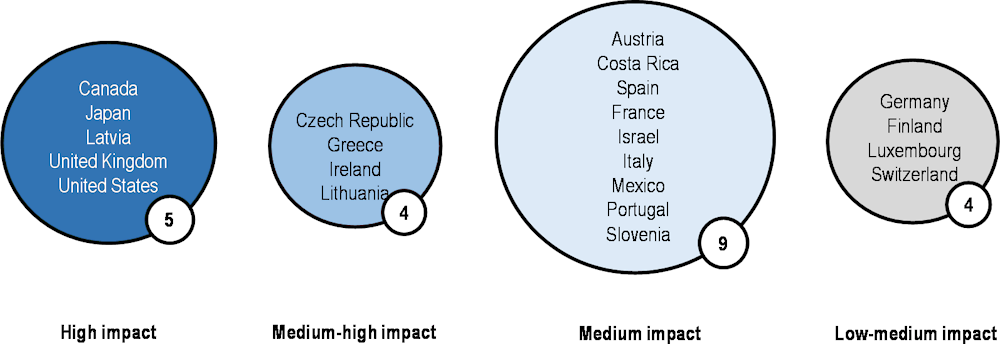
Note: This Figure shows countries’ responses to the question: “On a scale of 1 to 5, please indicate the impact of the lack of healthcare workers to respond to the COVID-19 pandemic: 1 (low), 2 (low-medium), 3 (medium), 4 (medium-high) and 5 (high).”
Source: OECD health systems resilience questionnaire.
4.4.4. New ways of organising the healthcare system allowed some of its functions to recover
Advanced care centres, composed of multi-professional teams, strengthened primary care in Luxembourg
At the start of the COVID-19 pandemic (23 March 2020), the government and health professional organisations set up four advanced care centres in the primary care sector. The objective of these centres, which are composed of multidisciplinary care teams, was to provide care specific to COVID-19 patients to relieve hospitals (COVID pathway), but also to ensure the continuity of primary care for other patients (non‑COVID pathway) (Government of Luxembourg, 2020[43]). Drive-through testing was also set up outside these centres. Advanced care centres saw a peak in visits the week of 30 March 2020 and recorded a total of 21 313 visits from March through May 2020. Following the resumption of activity in private practices, these centres were gradually closed. COVID-19 consultation centres were reopened in autumn 2020 and during the first half of 2021.
The establishment of advanced care centres and COVID-19 consultation centres as primary care facilities that support the delivery of community medicine services and help relieve the hospital system during pandemics is among the best practices of OECD member countries. Not only do advanced care centres reduce the risk of infection between COVID and non-COVID patients, but they also harness the potential of primary care to meet the full spectrum of health care needs. Among OECD member countries, Austria, Slovenia, Australia and the United Kingdom are among those that have reorganised primary care to respond more efficiently to the needs of the population as a whole (OECD, 2021[44]).
Reorganising and strengthening primary care with multidisciplinary teams is essential for health systems to function properly, both to increase resilience to future pandemics and to meet the changing needs of the population (OECD, 2021[44]). Luxembourg must therefore continue to strengthen primary care in order to improve quality and efficiency by promoting the creation of multi-professional medical practices. The creation of more advanced medical centres is a first step in strengthening primary care, but they should be geared more towards a multidisciplinary and co-ordinated practice that promotes better risk prevention. At least 18 OECD member countries have developed multidisciplinary primary care facilities (OECD, 2020[34]).
The development of telehealth in Luxembourg has improved but the benefits of the new services need to be evaluated
As in other OECD member countries, remote consultations, remote monitoring of COVID-19 patients and online prescription services were rapidly deployed in Luxembourg to maintain access to care for populations while limiting transmission of the virus (OECD, 2021[19]).
The remote consultation system, with electronic transmission of documents, was made available to the entire population in March 2020. In compliance with security and data protection requirements, this new service also offers functionalities that allow the digitalisation of the general patient journey, such as booking appointments, issuing prescriptions and sending medical data to other facilities (eHealth Agency, 2021[45]). Both the public and healthcare professionals in Luxembourg showed strong resilience during the pandemic by embracing these new technologies: the number of remote consultations peaked at almost 18 000 during the week of 23‑29 March 2020. The public authorities also encouraged the use of telemedicine by introducing a new act into the nomenclature of the National Health Fund (CNS, Luxembourg, 2021[46]). However, remote consultations accounted for just 9% of all medical consultations in Luxembourg in 2020, compared with an average of 21% in all OECD member countries (Figure 4.12.
Figure 4.12. The use of remote consultations in Luxembourg is lower than in other OECD member countries
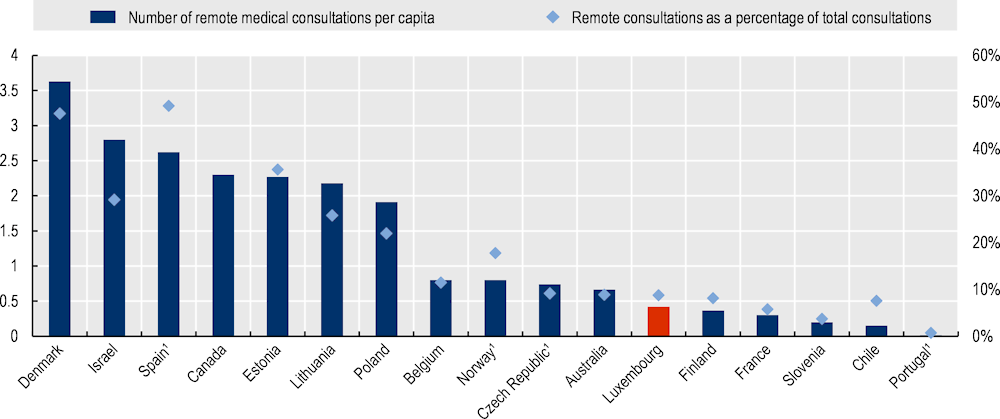
1. The Figure for Norway excludes remote specialist consultations, the Figure for Spain includes GP and paediatrician consultations at primary care centres in the national health system, and the Figure for Portugal includes only remote medical consultations with hospitals. Figures for the Czech Republic are estimates.
Source: OECD health statistics; OECD one-time collection of data on remote consultations (2022).
International studies demonstrate the benefit of remote care services in improving access to care in the general population, but concerns remain about access to these services for disadvantaged populations and those in rural areas (OECD, forthcoming[47]). Similarly, the satisfaction of users and healthcare professionals varies considerably from one country to another. Luxembourg has so far not evaluated the benefits and risks of deploying remote care services. In this respect, Luxembourg should implement indicators to assess the quality of telemedicine services, including factors such as safety, care outcomes and user satisfaction, as ten other OECD member countries have already done (Belgium, Canada, England, Estonia, France, Israel, Mexico, the Netherlands, Norway and the United States) (OECD, forthcoming[47]). These assessments will allow for analysis of the practices and the reasons for the reduced use of remote consultations compared with other OECD member countries.
New counselling services were developed during the pandemic but multisectoral approaches are lacking
As reported in Section 2, the mental health of the population deteriorated significantly during the pandemic, particularly among young people and employed people. New mental health support mechanisms were created for the public and healthcare workers, but multisectoral approaches that link mental health to education, youth and employment policies are needed to meet the needs of the most at‑risk populations.
To support the mental health of care workers and the general population, Luxembourg implemented new forms of support, including online information documents, new mental health helplines and increased access to mental health services (such as psychotherapy). This new online information includes tips on how to maintain good mental health during the pandemic and how to self-manage anxiety, depression and substance use.
These new measures, while necessary for the general population and for health workers, should be accompanied by multisectoral approaches, given the disruption that the pandemic has caused in terms of work organisation and in schools (see Chapter 5). Multisectoral mental health policies for young people and those in employment would allow to pay more attention to the mental health of these groups. In this respect, Luxembourg could take inspiration from the approaches developed in certain OECD member countries, such as Australia, Canada and France (Box 4.5).
It should be noted, however, that the Plan de Relance Sport (or Sport Recovery Plan) drawn up by the Ministry of Sport has indirectly supported mental health in Luxembourg in the context of the pandemic, in particular among young people. Numerous grants and subsidies have been allocated to various sports clubs and to families (Government of Luxembourg, 2021[48]). To encourage families to enrol their children in a sports club, the Ministry of Sport has, for example, contributed to the enrolment fee by paying EUR 50 for each new membership. Scientific research has shown that these targeted investments in sport are beneficial to the mental health of the population and promote social cohesion (Guthold et al., 2019[49]; OECD, 2021[19]).
Box 4.5. Multisectoral approaches to supporting the mental health of young people and employed people in selected OECD member countries
In Australia, Headspace centres provide comprehensive support to 100 000 people aged 12 to 25 each year, with a focus on mental health interventions. Headspace centres also collaborate with schools to offer specific support to students.
In Canada, the Mental Health Commission has a set of guidelines to help companies create work environments that support employees’ mental health. One of the key components of promoting mental health in the workplace is training for managers and supervisors.
In France, to address concerns about the mental health of students during the COVID-19 crisis and university closures, the Chèque Psy Étudiant scheme, which was launched in February 2021, allows students to have three appointments with a psychologist or psychiatrist free of charge. This was expanded in April 2021 with the introduction of a programme offering up to ten free sessions with a mental health specialist for children aged 3 to 17 years.
Source: OECD (2021[50]), “Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/0ccafa0b-en.
4.5. Summary of recommendations
4.5.1. Prepare for future crises
Develop a single information system, where databases are interoperable, with a unique identifier for patients and where health services are automatically linked (as in Canada, Denmark and Korea).
Invest more in the health workforce by increasing medical staff (as in France with support for GPs when they set up practice), introducing multidisciplinary approaches (as in Australia, Austria, Slovenia and the United States), and adapting the training and responsibilities of healthcare professionals (as in Canada, France and Latvia with the development of advanced practice nurses).
Strengthen hygiene skills and the medicalisation of long-term care facilities, and improve quality governance. Luxembourg could also give further consideration to the supervision of longterm care facilities.
Invest in multi-professional teams for primary care that promotes better access to risk prevention and meets all care needs in health crises (as has been done in 18 other OECD member countries).
Set up a central procurement and logistics unit for all health institutions for critical products, drugs and medical devices, in order to organise the national supply, logistics and storage of these products.
Maintain the health reserve, providing required training in key public health areas, such as epidemiological surveillance and contact tracing.
4.5.2. Absorb the shock and help health system functions to recover
Involve civil society and user representatives more in the management of the crisis, particularly in the various working groups of the interministerial crisis unit and the COVID-19 Task Force.
Involve the primary care sector to meet all the public’s needs, in particular primary care doctors’ office and retail pharmacies to accelerate vaccination coverage.
Strengthen the provision of health services to disadvantaged populations, who are at higher risk of developing severe forms of the disease, through activities aimed at preventing risk factors, and by continuing to develop community-based actions to reduce vaccine hesitancy.
Strengthen screening and monitoring of depressive disorders, and develop multisectoral mental health policies for young people and those in employment (as in Australia, Canada and France).
Evaluate the benefits and risks of deploying remote care services, particularly with regard to access, care quality, patient safety and user experience (as in Belgium, England and the United States).
Reconsider the increase in hospital capacity more closely to ensure the continuity of non‑emergency procedures. Establish co-operation between hospitals both to organise the pandemic care pathway and to ensure that non-emergency hospital procedures continue to run.
References
[37] Abdelrahman, T. et al. (2021), Étude indépendante au sujet des clusters observées dans certaines structures d’hebergement pour personnes âgées, https://www.chd.lu/wps/wcm/connect/public/6ef41195-c7eb-4054-8cec-ecf7519ed7f5/groupe+de+travail+clusters+rapport+def1.pdf?MOD=AJPERES&ContentCache=NONE&CACHE=NONE&CVID=nGpR.OB (accessed on 13 June 2022).
[6] Alkerwi, A. et al. (2021), Premiers résultats de l’évaluation de l’effectivité vaccinale contre la COVID-19, au Luxembourg, https://covid19.public.lu/dam-assets/covid-19/vaccinations/Rapport-2-effectivite-vaccinale-au-Luxembourg-VFinale-18102021-AN.pdf.
[20] Antares Consulting (2020), Réalisation d’un bilan du potentiel de la performance institutionnelle à la suite de l’expérience du COVID 19 : Présentation générale, Document envoyé suite à la mission de collecte d’information de l’OCDE en mai 2022.
[22] Backes, C. et al. (2020), Lessons learned from COVID-19 lockdown for cancer care: a nationwide survey of oncologists in Luxembourg, https://ssm.lu/wp-content/uploads/2021/01/20202.pdf.
[11] Bertemes, J. and U. Hentschel (2021), Enquête sur la vaccination contre la COVID-19, https://www.science.lu/fr/enquete-vaccination-contre-covid-19/combien-personnes-vaccinees-souhaitent-recevoir-une-dose-rappel-combien-parents-veulent-faire-vacciner-leurs-enfants (accessed on 13 June 2022).
[17] Centre Hospitalier du Luxembourg (2021), Présentation du projet-pilote de réseau de prise en charge pluridisciplinaire du long-COVID, https://www.chl.lu/fr/actualites/presentation-du-projet-pilote-de-reseau-de-prise-en-charge-pluridisciplinaire-du-long (accessed on 13 June 2022).
[46] CNS, Luxembourg (2021), Nomenclatures - Résulat, La Caisse Nationale de Santé, https://cns.public.lu/fr/outils-simulateurs/nomenclatures.html?q=C45 (accessed on 13 June 2022).
[27] CSL (2021), Présentation des résultats de la 8e enquête du Quality of work Index (2020), Chambre des Salariés Luxembourg, https://www.csl.lu/wp-content/uploads/2021/01/csl-resume-de-la-presentation-de-la-8e-enquete-francais.pdf.
[51] CSL (2021), Qualité des services pour personnes âgées - Amendements - Projet de loi 63/2021, Chambre des Salariés Luxembourg, Ministère de la Famille, de l’Intégration et à la Grande Région, https://www.csl.lu/wp-content/uploads/2021/10/63-2021-qualite-des-services-pour-personnes-agees-amdts.pdf.
[1] ECDC (2021), COVID-19 datasets, European Centre for Disease Prevention and Control, https://opendata.ecdc.europa.eu/covid19/nationalcasedeath/ (accessed on 12 October 2021).
[45] eHealth Agency (2021), Le service de téléconsultation, https://www.esante.lu/portal/fr/infos-e-sante/services-pour-professionnels-de-sante-188-252.html (accessed on 13 June 2022).
[3] Eurostat (2021), Life expectancy continued to decrease in 2021 in the EU, https://ec.europa.eu/eurostat/en/web/products-eurostat-news/-/ddn-20220506-2 (accessed on 13 June 2022).
[14] Frost, M. (2021), Primary care’s role in COVID-19 vaccination, ACP Internist and American College of Physicians, https://acpinternist.org/archives/2021/04/primary-cares-role-in-covid-19-vaccination.htm (accessed on 13 June 2022).
[30] Government of Luxembourg (2021), Evaluation sur la gestion COVID au Luxembourg : Monitoring et suivi de la pandémie, Ministère de la Santé, Luxembourg.
[16] Government of Luxembourg (2021), L O N G- C O V I D, PRÉSENTATION DU PROJET -PILOTE DE RÉSEAU DE PRISE EN CHARGE PLURIDISCIPLINAIRE DU LONG-COVID, Conférence de Presse - Ministère de la Santé, Luxembourg, https://covid19.public.lu/fr/actualite-covid-19/communiques/2021/07/08-long-covid.html (accessed on 13 June 2022).
[8] Government of Luxembourg (2021), Note à l’attention du Conseil de Gouvernement : Catégorisation des personnes à vacciner contre la COVID-19 pour les phases restantes du déploiement de la stratégie de vaccination, Document envoyé suite à la mission de collecte d’information de l’OCDE - Ministère de la Santé, Luxembourg.
[41] Government of Luxembourg (2021), Organisation et fonctionnement du Contact Tracing, Rapport preparé par l’inpection sanitaire le 15 décembre 2021, Document envoyé suite à la mission de collecte d’information de l’OCDE - Ministère de la Santé, Luxembourg.
[48] Government of Luxembourg (2021), Plan de relance SPORT 2.0 : Nouvelles mesures de soutien pour le sport luxembourgeois, Ministère des Sports, https://sports.public.lu/fr/actualites/articles/2021/06-juin/plan-de-relance-sport-2-0.html#:~:text=Le%20minimum%20attribu%C3%A9%20par%20club,formulaire%20aff%C3%A9rent%20est%20disponible%20ici (accessed on 13 June 2022).
[28] Government of Luxembourg (2021), Plan gouvernemental “Pandémie grippale”, https://infocrise.public.lu/fr/grippe-pandemie/plans-gouvernementaux/plan-gouvernemental-pandemie-grippale.html (accessed on 13 June 2022).
[39] Government of Luxembourg (2021), Population Testing, Document envoyé suite à la mission de collecte d’information de l’OCDE - Ministère de la Santé, Luxembourg.
[9] Government of Luxembourg (2021), Prochaines étapes de la campagne de vaccination, Ministère d’Etat / Ministère de la Santé.
[36] Government of Luxembourg (2021), Rapport du Plan d’action prévention et contrôle de l’infection « rappel des bonnes pratiques en matière d’hygiène » destiné au secteur extrahospitalier dans le contexte de la crise sanitaire liée au COVID-19, Document envoyé suite à la mission de collecte d’information de l’OCDE - Ministère de la Santé, Luxembourg.
[7] Government of Luxembourg (2021), Rapport national d’évaluation de l’effectivité vaccinale contre la COVID-19, Ministère de la santé - Service épidémiologique et Statistique, https://covid19.public.lu/dam-assets/covid-19/vaccinations/Rapport-mis-a-jour-du-16122021-effectivite-vaccinale-au-Luxembourg.pdf.
[43] Government of Luxembourg (2020), Flash-COVID N°1 : Centres de soins avancés (CSA), Ministère de la Santé, Luxembourg, https://gouvernement.lu/dam-assets/documents/actualites/2020/07-juillet/10-nvlle-infections-covid/Flash-covid.pdf.
[38] Government of Luxembourg (2020), Visites dans les CIPAs - Recommandations : prevention de l’infection, Document envoyé suite à la mission de collecte d’information de l’OCDE - Ministère de la Santé, Luxembourg.
[49] Guthold, R. et al. (2019), “Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants”, The Lancet child and Adolescent Health, Vol. 4, pp. 23-35, https://doi.org/10.1016/S2352-4642(19)30323-2.
[23] Hanna, T. et al. (2020), “Mortality due to cancer treatment delay: systematic review and meta-analysis”, BMJ, Vol. 371/m4087, https://doi.org/10.1136/bmj.m4087.
[32] IGSS Luxembourg (2021), Rapport général sur la sécurité sociale au Grand-Duché de Luxembourg, Inspection générale sur la sécurité sociale, https://igss.gouvernement.lu/fr/publications/rg/2020.html (accessed on 13 June 2022).
[26] Kirsch, C. et al. (2022), L’impact de la pandémie de la Covid-19 au Luxembourg en 2021 : Les enfants de 6 à 16 ans partagent leur bien-être subjectif et leurs expériences., https://www.unicef.lu/site-root/wp-content/uploads/2022/02/UNI_CEF_Report2022_FR-1.pdf.
[33] Lair-Hillion, M. (2019), État des lieux des professions médicales et des professions de santé au Luxembourg : Rapport final et recommandations, Sante et Prospectives, Luxembourg.
[15] Luxembourg Institute of Health (2022), Six personnes sur dix atteintes de COVID-19 présentent encore au moins un symptôme un an plus tard, selon une longue étude sur Covid, https://www.lih.lu/en/six-in-ten-people-with-covid-19-still-have-a-least-one-symptom-a-year-later-long-covid-study-reveals/ (accessed on 13 June 2022).
[21] Mittelbrownn, M. (2021), L’impact aux échelons mondial et national de la COVID-19 sur les diagnostics de cancer, Infocancer n°103, Fondation Cancer.
[31] Oderkirk, J. (2021), “Survey results: National health data infrastructure and governance”, OECD Health Working Papers, No. 127, Éditions OCDE, Paris, https://doi.org/10.1787/55d24b5d-en.
[19] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[44] OECD (2021), “Strengthening the frontline: How primary health care helps health systems adapt during the COVID 19 pandemic”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/9a5ae6da-en.
[50] OECD (2021), “Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/0ccafa0b-en.
[34] OECD (2020), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en.
[12] OECD (forthcoming), Building resilient health system in face of COVID-19.
[35] OECD (forthcoming), Improving the Resilience of Health System.
[47] OECD (forthcoming), La télémédecine dans les pays de l’OCDE : Conséquences du COVID-19 – Résumé et principales conclusions.
[18] OECD (forthcoming), Long-COVID across OECD countries.
[2] OECD/European Observatory on Health Systems and Policies (2022), Luxembourg: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris, https://doi.org/10.1787/3c147ce7-en.
[42] Official Journal of the Grand Duchy of Luxembourg (2020), Loi du 29 octobre 2020 portant dérogation temporaire à l’article L. 211-12 du Code du travail, https://data.legilux.public.lu/file/eli-etat-leg-loi-2020-10-29-a868-jo-fr-pdf.pdf.
[29] Official Journal of the Grand Duchy of Luxembourg (2018), Loi du 1er août 2018 sur la déclaration obligatoire de certaines maladies dans le cadre de la protection, https://data.legilux.public.lu/file/eli-etat-leg-loi-2018-08-01-a705-jo-fr-pdf.pdf.
[4] Rocard, E., P. Sillitti and A. Llena-Nozal (2021), “COVID-19 in long-term care : Impact, policy responses and challenges”, OECD Health Working Papers, No. 131, Éditions OCDE, Paris, https://doi.org/10.1787/b966f837-en.
[10] STATEC (2021), “La confiance dans la science : un facteur essentiel de la vaccination contre le Covid-19”, STATNEWS, Vol. 40, https://statistiques.public.lu/dam-assets/fr/actualites/conditions-sociales/sante-secu/2021/07/20210727/STN40_Trust_Covid_v06_FR.pdf.
[25] STATEC (2020), “Le confinement a dégradé le bien-être des résidents”, Vol. 36, https://statistiques.public.lu/dam-assets/fr/actualites/conditions-sociales/conditions-vie/2020/11/20201113/20201113.pdf.
[24] STATEC (2020), “One in three Luxembourg residents report their mental health declined during the COVID-19 crisis”, Regards, Vol. 8, https://statistiques.public.lu/dam-assets/catalogue-publications/regards/2020/regards-08-20.pdf.
[13] The Commonwealth Fund (2021), The Room Where It Happens: The Role of Primary Care in the Next Phase of the COVID-19 Vaccination Campaign, https://doi.org/10.26099/jt9h-ge63.
[5] Van Kerm, P., I. Salagean and F. Amétépé (2022), La COVID-19 au Luxembourg: Le gradient social de l’épidémie, https://liser.elsevierpure.com/fr/publications/la-covid-19-au-luxembourg-le-gradient-social-de-l%C3%A9pid%C3%A9mie (accessed on 13 June 2022).
[40] Wilmes, P. et al. (2021), “SARS-CoV-2 transmission risk from asymptomatic carriers: Results from a mass screening programme in kuxembourg”, The Lancet Regional Health - Europe, Vol. 4, https://doi.org/10.1016/j.lanepe.2021.100056.
Notes
← 1. The analysis of excess mortality data, corresponding to deaths recorded in excess of the number that would normally have been expected at a given time of the year, makes it possible to avoid, in part, problems with data comparability due to differences in national practices of accounting for, recording and codifying these deaths.
← 2. In charge respectively of: i) the vaccination strategy (target populations to be vaccinated, prioritisation of groups); ii) communication and organising a hotline; iii) the supply of vaccines (negotiations with the European Commission, arrangements for delivery of vaccines to Luxembourg, training of vaccinators according to the manufacturers' instructions); iv) developing information systems (sending out invitations, making appointments, recording information on those vaccinated, providing computer equipment); v) and logistics and vaccination centres (identifying vaccination sites, transporting and storing vaccines within the country, designing and operating vaccination centres and mobile vaccination teams).
← 3. The logistics unit was set up under the responsibility of the Ministry of Defence within the crisis unit of the Ministry of Health and the High Commission for National Protection on 17 March 2020. The logistics unit was initially composed of representatives from the Health Directorate, the Army, the High Commission for National Protection, and the Grand Ducal Fire and Rescue Corps.
← 4. A total of nine training sessions were organised between 28 March and 6 April 2020 with 189 participants representing integrated centres for older people, care homes, home care networks and private practice nurses. According to data provided by the High Commission for National Protection, training on good hygiene practices saw an attendance rate of 94%, indicating that the programme was a success.
← 5. Some of these measures have already been made permanent through amendments to Bill No. 7524 on the quality of services for older people made by the government on 29 September 2021 (CSL, 2021[51]). These amendments provide for the introduction of a reference person for infection prevention and control and compliance with hygiene and sanitary regulations, the obligation to include in the facility’s general regulations the hygiene and sanitary rules to be respected and a system for infection prevention and control, and the introduction of governance for quality management.
← 6. A total of 109 facilities benefited from these testing operations, following 186 interventions during which 16 501 tests were performed and 628 positive cases were detected.
← 7. The Act of 17 July 2020 introducing a series of measures to combat the COVID-19 pandemic made it possible for the Ministry of Health to hire health professionals or doctors about to receive their licence to practice.