Cervical cancer is one of the few cancers that may be largely preventable for the new generations of women through HPV vaccination programmes of young girls and boys, that have been by now integrated in most countries. Over the past 15 years, all EU countries except Poland launched HPV vaccination programmes, starting first with young girls and gradually expanding the programmes to young boys also (ECDC, 2020[1]). In addition, over three‑fourths of EU countries have implemented population-based cervical cancer screening programmes (European Commission, 2017[2]).
WHO recommends countries strive to reach an incidence rate of less than 4 new cases of cervical cancer per 100 000 women each year, but European countries have yet to achieve this target. To reach this goal, WHO recommends 90% HPV vaccination coverage among girls by age 15, 70% coverage of cervical cancer screening at ages 35 and 45, and improvement of the coverage of treatment (i.e. treating 90% of women with pre‑cancer and managing 90% of women with invasive cancer) (WHO, 2020[3]).
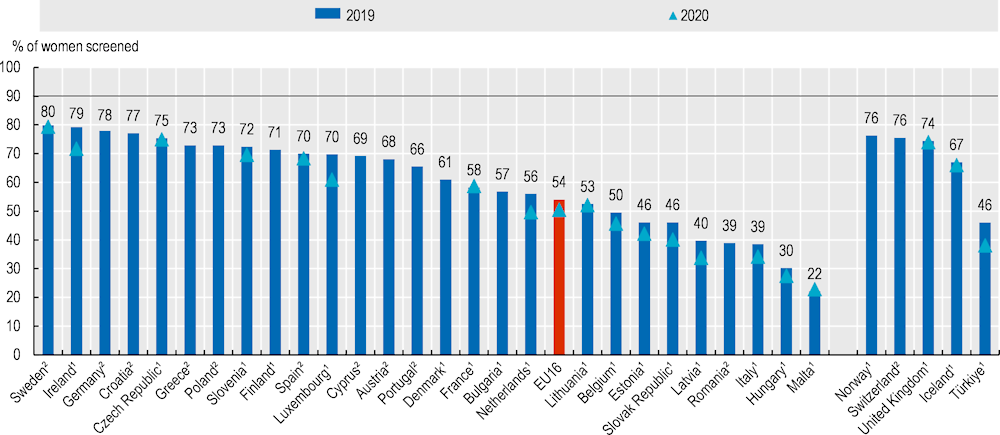
In the year before the pandemic (2019), the proportion of women aged 20‑69 who had been screened for cervical cancer within the past three years remained low in many European countries (Figure 6.24). The proportion was particularly low in Malta (22%) and Hungary (30%).
Cervical cancer screening uptake was adversely impacted by the COVID‑19 pandemic, as was breast cancer screening (see indicator “Breast cancer screening and outcomes”). All countries that reported 2020 data had a lower screening rates than the year before, except Malta and France. The decline was largest in Luxembourg, where screening rates decreased by almost 9 percentage points.
Colorectal cancer was the second most common cause of cancer death in men (after lung cancer) and the third most common cause (after breast and lung cancers) among women in Europe in 2019 (see indicator “Mortality from cancer” in Chapter 3). The main risk factors for colorectal cancer are age, ulcerative colitis, a personal or family history of colorectal cancer or polyps, and lifestyle factors (such as a diet high in fat and low in fibre, physical inactivity, obesity, tobacco and alcohol consumption). The European Commission Initiative on Colorectal Cancer develops evidence‑based guidelines for colorectal cancer prevention, screening and diagnosis and quality assurance scheme throughout the entire care pathway from prevention, screening and diagnosis to treatment, follow-up and palliative care.
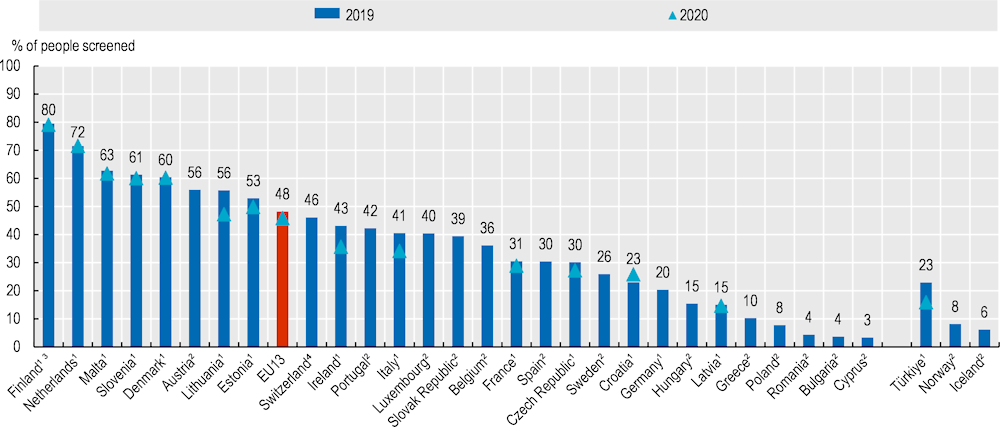
Following the EU Council recommendations on cancer screening in 2003, a growing number of European countries have introduced nationwide screening programmes for colorectal cancer. Country policies typically support routine faecal occult blood tests for people in their 50s and 60s (European Commission, 2017[2]).
Participation rates in colorectal cancer screening programmes varies from a high of 80% in Finland to a low of less than 5% in Cyprus, Bulgaria and Romania (Figure 6.25). Similar to cervical cancer screening, almost all countries reporting 2020 data had lower participation rates in 2020 than in 2019. The largest decline was 8 percentage points in Lithuania and 7 percentage points in Ireland.