This chapter focuses on health literacy, a key skill individuals need to acquire in order to deal with the increasing complexity of the health-related information landscape. Health literacy is an important determinant of how much health-related knowledge and information individuals can acquire and how they use such knowledge and information to promote and maintain their health. The chapter maps individuals’ health literacy levels in 15 OECD countries and the relevance of health literacy for health outcomes. It also presents initiatives developed by countries to promote health literacy and improve the quality of communication and information in the healthcare sector to ensure the sector adequately serves the needs of individuals with diverse levels of health literacy.
OECD Skills Outlook 2023

6. Empowering through health literacy: Skills to navigate health information and make informed decisions
Abstract
Key messages
Health literacy encompasses the knowledge, motivation and skills required to access, comprehend, assess and apply information to make informed decisions regarding healthcare, disease prevention and the enhancement of overall well-being over the life course. It has far-reaching consequences for individuals’ ability to manage their health, use preventive services and take part in decision making regarding their health and well-being. At the societal level, health literacy impacts healthcare use, prevention and health promotion programmes, equity and social justice, as well as productivity. This chapter maps levels of self-reported health literacy in 15 OECD countries that took part in the European Health Literacy Population Survey 2019‑2021 (HLS19), evaluates disparities in health literacy and identifies associations between health literacy and health outcomes.
The chapter also explores the policies and initiatives that Austria, Germany, Ireland and Portugal have implemented in recent years to promote health literacy among their populations and improve the capacity of healthcare systems to deliver information and services in ways that are better aligned with the capacity of communities to access, understand, appraise and apply such information.
Key empirical findings include:
On average, across the 15 participating countries, 44% of respondents indicated that they would find it difficult or very difficult to judge the advantages and disadvantages of different treatment options. In addition, 42% indicated that they would find it difficult or very difficult to decide how to protect themselves from illness using information from the mass media, and 38% indicated that they would find it difficult or very difficult to find information on how to handle mental health problems. By contrast, only 8% indicated that they would find it difficult or very difficult to act on advice from their doctor or pharmacist.
Differences in health literacy across socio-economic characteristics such as gender, age and level of education are minor. In contrast, more socio-economically deprived individuals tend to report lower levels of health literacy than those without financial deprivation.
Individuals with higher levels of health literacy tend to engage in and adopt healthier lifestyles, such as consuming more fruits and vegetables and exercising more. They are also more likely to report being in good or very good health and are less likely to report suffering from at least one long-term illness or health problem; to have used emergency healthcare services in the two years preceding the survey; and to have used medical or surgical specialists. For example, a difference of 10 percentage points in the number of health-related tasks individuals perceive as very easy or easy is associated with a difference of around 1.4 percentage points in the likelihood of consuming fruit and vegetables, a 1.9 percentage-point difference in the likelihood of engaging in physical exercise, 2.4 percentage points in the likelihood of reporting being in good or very good health and 1.3 percentage points in the likelihood of suffering from a long‑term illness or condition.
6.1. Introduction
Technology, such as health apps, wearable devices, and online health platforms, provides individuals with unprecedented access to health information and tools that allow them to monitor and manage their health and well-being. However, the effectiveness of these resources hinges on users’ ability to comprehend, evaluate and apply the information they encounter. If individuals misinterpret health data or rely on inaccurate information, they can make wrong self-diagnoses, inadequate treatment adherence or misguided health decisions. While technological developments in generative artificial intelligence might improve early disease detection and treatment options, they also run the risk of amplifying online misinformation, amplifying the importance for individuals to have the ability to critically evaluate and discern health information. In an era of rampant digital misinformation, individuals lacking strong health literacy skills are more susceptible to becoming the victims of false and misleading claims, potentially compromising their health and undermining the effectiveness of evidence-based medical practices.
Enhanced health literacy empowers individuals to make informed decisions about their health, enabling them to harness technology effectively. By comprehending medical terms, understanding treatment options and critically evaluating digital health information, individuals can optimise their engagement with technology-driven healthcare, leading to better health outcomes and improved overall well-being. In an era where technology increasingly intertwines with healthcare, cultivating strong health literacy has become an essential tool for navigating the intricate intersection of medicine and innovation.
Health literacy is an important determinant of how much health-related knowledge individuals can acquire, the behaviours they engage in, how healthy they are and how costly it is to promote and maintain one’s health (Mancuso, 2009[1]). Individuals with low health literacy generally experience poorer health outcomes than those with higher health literacy (Berkman et al., 2011[2]). This has significant implications not only for individuals but also for societies directly due to healthcare expenditures and indirectly due to lower productivity and lower fiscal contributions (Mårtensson and Hensing, 2011[3]). Health literacy and its promotion have, therefore, become a public policy priority at both the national and international levels.
Until recently, many countries did not have formal policies related to the development of population-wide health literacy or were in the early stages of developing programmes (Heijmans et al., 2015[4]). However, the importance of health literacy as a key factor that can support public health is increasingly recognised. For example, the United States released the National Action to Improve Health Literacy in 2010, which “seeks to engage organizations, professionals, policymakers, communities, individuals, and families in a linked, multi-sector effort to improve health literacy” (Centers for Disease Control and Prevention, 2010[5]), and in 2021, Australia introduced the National Preventive Health Strategy 2021‑2030 (Australian Government - Department of Health, 2021[6]).
At the international level, health literacy has gradually been included in international frameworks and global declarations. For instance, the need to improve health literacy was included in the World Health Organization’s (WHO) Health 2020 European framework (WHO, 2013[7]), in the Shanghai Declaration (WHO, 2016[8]) and in the WHO’s “Roadmap for Implementing Health Literacy Initiatives across Europe” (Schaeffer and Gille, 2021[9]; WHO, 2019[10]). In addition, at the 2017 OECD Health Ministerial meeting, ministers agreed that in order to make health systems more people-centred, “efforts are needed to address barriers to health literacy of the population” (OECD, 2017[11]). Furthermore, the WHO recognised the role played by health literacy in reducing the burden of non-communicable diseases and in accelerating progress towards the targets on non-communicable diseases in the Sustainable Development Goals and disseminated a large number of case studies and interventions aimed at promoting health literacy development for the prevention and control of non-communicable diseases (WHO, 2022[12]).
Policy makers’ growing interest in how health literacy can be promoted and nurtured follows the publication of multiple studies revealing insufficient levels of health literacy in many countries (Schaeffer et al., 2021[13]). For example, studies found that in the United States, about half of adults have inadequate health‑related literacy (Morrow et al., 2006[14]). In addition, a more recent health literacy survey conducted in the United States documented that “more than one-third of adults cannot determine the proper way to take prescription medicines based on typical instructions found on container labels” (Parker and Ratzan, 2010[15]). Data from the European Health Literacy Survey (HLS-EU), conducted in 2011, revealed that one in ten respondents had insufficient health literacy and almost one in two had limited health literacy in the eight EU member states surveyed (Sørensen et al., 2015[16]). Meanwhile, almost 60% of adults in Australia had low health literacy (Nakayama et al., 2015[17]). More broadly, an OECD study found that in 18 OECD countries, at least one-third of the population has poor health literacy levels, and in 12 of those countries, that share is higher than half (Moreira, 2018[18]). The European Health Literacy Population Survey 2019‑2021 (HLS19) report also notes that there are considerable variations in levels of general health literacy1 across countries, indicating that health literacy is a contextual concept that must be measured individually at the country level (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]).
Yet, to date, no single survey exists that provides large-scale cross-country comparable measures of health literacy across all OECD countries. HLS19 (Pelikan et al., 2022[20]) is the first multinational standardised study that uses standardised instruments across countries and establishes a framework to conduct comparisons over time (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]). At the same time, the variety of sampling and data collection procedures used in HLS19 means that country comparisons should be interpreted with caution. Cross-country comparisons remain limited, and there is not yet a “gold standard” to measure health literacy (Moreira, 2018[18]). For example, in Australia, Canada and the United States, health literacy is calculated using proxies from general skills surveys, while many European countries rely on the HLS-EU (Moreira, 2018[18]).
6.2. What is health literacy?
Having high levels of health literacy means that an individual knows when and where to seek help and has the ability to understand healthcare providers’ instructions and explanations regarding their health conditions and treatment options (Mancuso, 2009[1]; Mårtensson and Hensing, 2011[3]). It also means that an individual has the skill set necessary to navigate and adequately use complex healthcare systems (Griese et al., 2020[21]; 2022[22]; Parker and Ratzan, 2010[15]; Sørensen et al., 2015[16]). In addition, being health literate enables people to make decisions concerning their healthcare options, disease prevention and ways in which they would like to maintain or improve their health throughout their lives (Heijmans et al., 2015[4]).
Several formal definitions of health literacy exist. In this report, the definition put forth by Sørensen and colleagues in 2012 was adopted. Sørensen and colleagues (2012[23]) conducted a systematic review of the literature and existing definitions to identify the central health literacy dimensions. This definition is, therefore, inclusive and comprehensive. Furthermore, this definition was the basis of the framework that guided data collection on health literacy in OECD countries as part of the HLS19, a project of the WHO Action Network on Measuring Population and Organizational Health Literacy (M-POHL) (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]).
Thus, health literacy, for the purposes of this report, is “the knowledge, motivation and competences to access, understand, appraise and apply health information in order to make judgements and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life throughout the course of life” (Sørensen et al., 2012[23]).
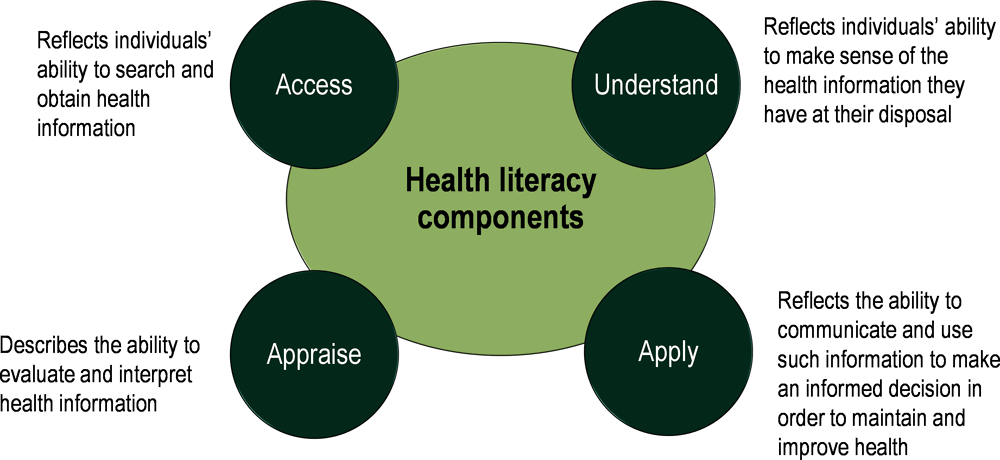
According to this definition, health literacy is characterised by four dimensions relevant for healthcare, disease prevention and health promotion. The first is access, which reflects individuals’ ability to search for and obtain health information. The second is understand, which reflects individuals’ ability to make sense of the health information they have at their disposal. The third is appraise, which describes the ability to evaluate and interpret health information. The fourth is apply, which reflects the ability to communicate and use such information to make an informed decision in order to maintain and improve health (Sørensen et al., 2012[23]) (Figure 6.1).
Understood as a relational concept (Parker, 2009[24]; Parker and Ratzan, 2010[15]), health literacy does not only emerge from personal skills and abilities but in conjunction with the availability, comprehensibility, accessibility and practicability of health-related information, communications and offers.
Figure 6.1. Health literacy components
6.3. Health literacy matters
Health literacy has several consequences for individuals and societies. At the individual level, health literacy has far-reaching consequences for individuals’ ability to participate in the self-management of their health problems, preventive care, health promotion and healthcare decision making. At the societal level, health literacy impacts healthcare use, prevention and health promotion programmes, equity and social justice, as well as productivity.
6.3.1. Health literacy supports individuals’ self-management, use of preventive care and decision making
Limited levels of health literacy are related to poorer adherence to medication regimens (Baker, 2007[25]), a lower ability to take medications appropriately, poorer ability to interpret labels and health messages (Berkman et al., 2011[2]), and missed doctor visits (Mancuso, 2009[1]; Mårtensson and Hensing, 2011[3]). This is particularly problematic in the management of chronic conditions such as hypertension, diabetes and acute respiratory conditions, which require self-management on a day-to-day basis or during acute episodes (Baker, 2007[25]; Paasche-Orlow and Wolf, 2007[26]; Schaeffer, 2017[27]).
Individuals with low levels of health literacy also use fewer preventive services than individuals with higher health literacy (Kim and Xie, 2017[28]). For example, studies find that individuals with low levels of health literacy are less likely to take part in recommended screenings (Herndon, Chaney and Carden, 2011[29]) and vaccinations (Baker, 2007[25]; Berkman et al., 2011[2]; The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]) and to delay seeking medical care because they do not understand preventive care and/or are unaware of the symptoms that require action (Paasche-Orlow and Wolf, 2007[26]). Individuals with limited health literacy experience greater difficulty taking part in shared decision making when interacting with healthcare professionals than individuals with higher levels of health literacy (Seo et al., 2016[30]). The lack of shared decision making may be especially consequential in situations where medical professionals’ biases may lead them to provide varying levels of care to different patients. In fact, different levels of care by gender and ethnic status have been documented.
Higher levels of general health literacy are also important for health promotion, which refers to the “ability to regularly update oneself on determinants of health in the social and physical environment, to understand health-related information and derive meaning, to interpret and evaluate information on determinants of health in the social and physical environment, and to make informed decisions on health determinants in the social and physical environment, and also engage in joint action” (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]).
6.3.2. Health literacy benefits society
The literature indicates that individuals with high health literacy make greater use of preventive services and engage more often in the self-management of chronic conditions, leading them to seek care only when the symptoms of diseases make such contact unavoidable (Weiss and Palmer, 2004[31]). This makes treatment regimens more expensive and prolonged and could potentially result in the development of longstanding and limiting conditions, which could lead to excessive human and financial resources being allocated to healthcare (Rondia et al., 2019[32]). In fact, evidence from the United States suggests that low levels of health literacy lead to unnecessary resource utilisation and expenditure (Rasu et al., 2015[33]), costing the healthcare system between USD 106 billion to USD 236 billion annually (Vernon et al., 2007[34]).
Lower participation in preventive screenings among individuals with lower levels of health literacy can mean that individuals may involuntarily put the broader community as well as themselves at risk (Van den Broucke, 2014[35]). Similarly, individuals with low levels of health literacy could transmit infectious diseases, such as COVID‑19, by failing to wash their hands or wearing a face mask, failing to remain at home when they have symptoms or failing to respect other protective behaviours. A recent study in Ireland found that young people who had sufficient levels of health literacy about COVID‑19 and the way the disease was transmitted adhered to most precautionary measures (Griebler, Dietscher and Flaschberger, 2022[36]; Nearchou et al., 2022[37]). Similarly, a study from Portugal shows that higher levels of health literacy were associated with better attitudes towards COVID‑19 preventive strategies (Silva and Santos, 2021[38]).
Health literacy also impacts productivity and, thus, economic growth. By promoting health, health literacy enhances productivity (Sørensen et al., 2012[23]), and estimates suggest that at the population level, health problems and limitations reduce productive capacities by about 5‑8% of gross domestic product (GDP) depending on the country (Llena-Nozal, Martin and Murtin, 2019[39]).
6.4. Factors that shape the development of health literacy and how well health literacy translates into health
A number of factors shape the likelihood that individuals will accumulate health literacy and how effectively health literacy will promote individuals’ health and well-being. These include information-processing skills, individual background characteristics and contextual factors.
6.4.1. Information-processing skills
Information-processing skills are crucial precursors of health literacy. For example, skills such as reading literacy and numeracy skills are necessary if individuals are to be able to read medicine labels, information pamphlets, appointment slips, and insurance and consent forms. In fact, studies have found that improving individuals’ health literacy and subsequent health status is dependent on individuals reaching minimum standards of general literacy (Quaglio et al., 2016[40]). At the same time, health literacy is a key bridge between an individual’s general literacy skills and their health context (Nielsen-Bohlman, Panzer and Kindig, 2004[41]). In addition to reading literacy and numeracy skills, individuals need oral communication skills (speaking and listening abilities) (Cavanaugh, 2011[42]; Jain and Green, 2016[43]; Oxley, 2009[44]) as well as comprehension skills so that they can describe their symptoms, ask appropriate follow-up questions and accurately interpret the information and instructions shared with them (Mancuso, 2008[45]). Critical thinking, analysis, decision making, problem solving, and the ability to seek guidance are also skills that underpin health literacy (Mancuso, 2008[45]; Speros, 2005[46]; Wilson, 2001[47]).
6.4.2. Individual factors
Disparities in health literacy exist between individuals from different socio-economic and demographic backgrounds.
Older individuals tend to have lower levels of health literacy (Baker et al., 2002[48]; Berens et al., 2016[49]; Kutner et al., 2006[50]; Vogt, Schaeffer and Berens, 2019[51]; Zamora and Clingerman, 2011[52]) and suffer more negative consequences when they lack health literacy because they are more likely to take medications and interact with health services (Quaglio et al., 2016[40]); are more likely to live with chronic diseases and health-related demands; and may experience other difficulties when dealing with healthcare systems. Therefore, older individuals, i.e. individuals who in general have the greatest healthcare needs, are also the ones that are the least prepared to navigate the healthcare system. In fact, there is evidence that health literacy may be lowest among individuals aged 65 or older and that a rapid decline in health literacy skills starts after the age of 55 (Manafo and Wong, 2012[53]).
This could be because being health literate involves certain cognitive skills that become increasingly challenged as one ages, especially as age-related conditions such as dementia increase (Manafo and Wong, 2012[53]; Oxley, 2009[44]). Furthermore, older people tend to process and learn information more slowly (Speros, 2009[54]). They also have less working memory, experience greater difficulty handling multiple bits of information at one time, and have a harder time completing tasks that require inference or reasoning (Speros, 2009[54]). With age, individuals also experience declines in their vision, hearing and mobility, which can directly affect how they gather and process information and prevent them from carrying out the necessary measures needed to manage their health (Speros, 2009[54]). At the same time, difficulties in dealing with a healthcare system may become more visible when demands in this regard increase.
Studies also reveal that women have, on average, higher levels of health literacy than men (Bazrafkan et al., 2018[55]; Kutner et al., 2006[50]; Van der Heide et al., 2013[56]). The health literacy gap between men and women could be a result of women’s increased familiarity with navigating the healthcare system, given that women tend to report more health issues and use healthcare services more often than men (Bertakis et al., 2000[57]; Kalseth and Halvorsen, 2020[58]; Lee, Lee and Kim, 2014[59]) and/or because women have traditionally had caregiver roles (whether of children or elderly relatives) and thus have had more contact with the healthcare system (Lee, Lee and Kim, 2014[59]; Sudore et al., 2006[60]). Finally, women may develop higher levels of health literacy as a response to the fact that healthcare professionals treat men and women differently, are less likely to involve women in decision making, and are more likely to discount their reports of ailments (Criado Perez, 2019[61]; Samulowitz et al., 2018[62]).
Health literacy is also higher among individuals with higher levels of educational attainment because of the greater cognitive, economic and social resources individuals with higher levels of educational attainment possess (Morrow et al., 2006[14]; Quenzel, 2017[63]; Kutner et al., 2006[50]; WHO, 2013[64]; Van der Heide et al., 2013[56]). In addition, studies have identified differences in health literacy across ethnic and income groups, differences that can, in part, explain disparities in health outcomes across such groups (Chaudhry et al., 2011[65]; Kutner et al., 2006[50]; Schillinger, 2020[66]; Sentell and Halpin, 2006[67]; Sørensen et al., 2015[16]; Van der Heide et al., 2013[56]).
6.4.3. Contextual factors
Socio-economic and demographic characteristics influence a person’s health literacy and can help a person navigate their healthcare context, but the ability to use a healthcare system and understand healthcare information also depends on context, including the way in which information is communicated (Griese, Schaeffer and Berens, 2022[68]; Moreira, 2018[18]; Rondia et al., 2019[32]). Health literacy is a shared responsibility that emerges from the interaction of individuals’ skills and the demands of healthcare systems (Sørensen et al., 2012[23]).
Understanding and addressing health literacy is important as people are faced with more health information than ever before (Nielsen-Bohlman, Panzer and Kindig, 2004[41]). People can now obtain information from national media, the Internet, social media, healthcare providers or health education. In addition, people are able to access diverse health information and, more worryingly, health misinformation in a variety of ways (Nakayama et al., 2015[17]). Recent research on COVID‑19 and health literacy in Japan found that low levels of health literacy are associated with high susceptibility to misinformation (Cheng and Nishikawa, 2022[69]).
Furthermore, chronic diseases require complicated self-management regimens, thus shaping the importance for societies to invest in health literacy and the specific demands that individuals and healthcare systems face (WHO, 2022[12]). Changes in the information landscape and in the incidence of chronic diseases have occurred at a time in which there has been an increased push for more consumer-driven care, and as a result, individuals must play a more active role in managing their health (Rondia et al., 2019[32]; Weishaar et al., 2019[70]), such as seeking out information, understanding rights and responsibilities and making health decisions (Nielsen-Bohlman, Panzer and Kindig, 2004[41]). The underlying assumption behind these demands and responsibilities is that people have the knowledge and skills to be active agents and decision makers in their health context. However, studies reveal that there is a “mismatch” between people’s health literacy skills and the demands of health systems: many health-related materials, such as consent forms and medication instructions, often exceed the reading skills of the average high-school graduate (Nielsen-Bohlman, Panzer and Kindig, 2004[41]).
6.5. Disparities in health literacy within and across countries
This section aims to compare self-reported health literacy levels across countries and sheds light on disparities. While large-scale assessments or surveys allow for cross-country comparison of various skills, cross-country comparison of health literacy remains limited. To allow comparison across a broad range of countries, this section draws on information obtained from the HLS19, a cross-sectional multi-centre survey that was conducted in 17 countries between November 2019 and June 2021 (15 of them OECD countries) (information on sampling and the target population can be found in The HLS19 Consortium of the WHO Action Network M-POHL (2021[19])).
Health literacy was measured in the HLS19 by asking participants to indicate how easy or difficult they found performing a series of 12 general health literacy tasks. Answers were based on a four-point Likert scale with the following options: “very easy”, “easy”, “difficult” and “very difficult”. This information was also combined into a health literacy score of items with valid responses that were answered to be “very easy” or “easy”. The health literacy score ranges from 0 to 100, with higher numbers denoting a higher level of health literacy (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]). Thus, the scores measure health literacy as the percentage of health-related tasks experienced as “very easy” or “easy” by a respondent. A detailed description of survey instruments and technical details on administration, implementation and scaling is available in the technical chapters of the HLS19 report (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]).
Two caveats need to be considered when evaluating results. First, although data collection was originally planned for 2019‑20, this had to be extended and adjusted due to the COVID‑19 pandemic. Only data collection for Germany was completed before the pandemic began. All other participating countries started or completed data collection during the pandemic, which reached different intensity levels at different times in different countries. Tables 2.15, 2.16, 2.17 and 2.18 in the HLS19 International Report (The HLS19 Consortium of the WHO Action Network M-POHL, 2021[19]) detail data collection instruments and dates for participating countries. As a result, country comparisons of HLS19 data should be interpreted with caution. Figure 6.2 shows the percentage of respondents across the 15 countries who reported that it would be “very difficult” or “difficult” to perform 12 health literacy tasks, as well as the country with the highest and lowest shares. Second, results reflect self-reports of participants rather than whether participants in the study were able to complete health literacy tasks or not.
Figure 6.2. Percentage of respondents who responded “very difficult” or “difficult” when asked to rate performing 12 health literacy tasks, selected OECD countries, 2019‑20
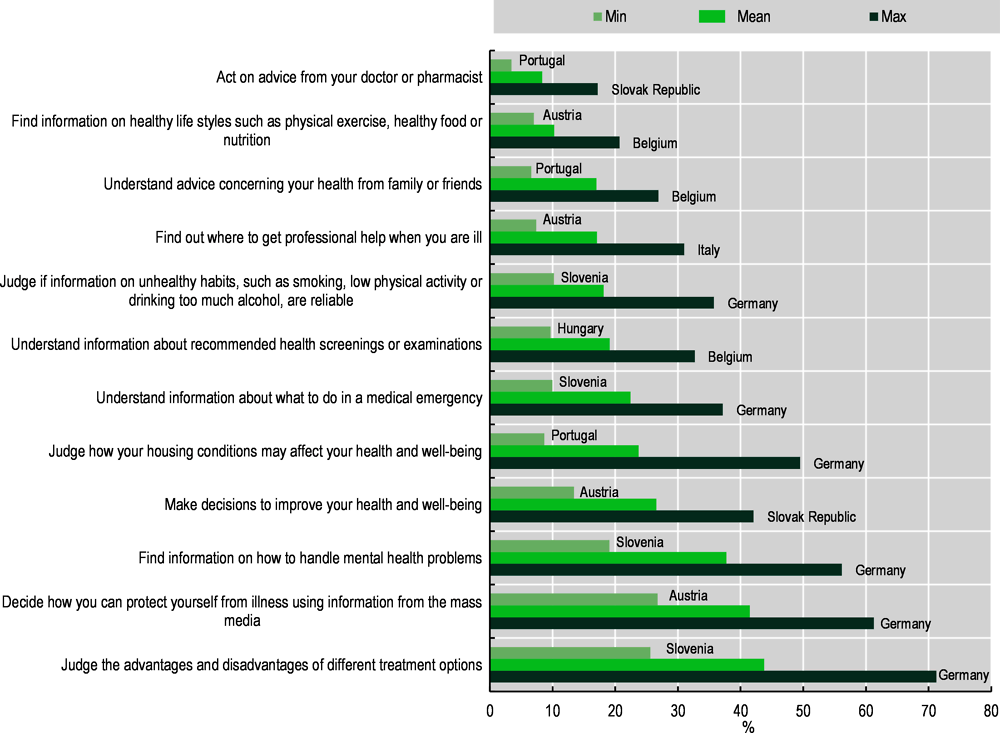
Note: The figure illustrates the percentage of respondents who responded that they would find it “very difficult” or “difficult” to perform each of the 12 tasks that were part of the core health literacy assessment instrument. The middle bar indicates the HLS19 OECD average, while the long (short) bars indicate for each task, the percentage of respondents who indicated that they would find “very difficult” or “difficult” to perform each of the 12 tasks in the country where this percentage was highest (and lowest). Due to the wide variety of sampling and data collection procedures across countries, country differences should be interpreted with caution.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
On average, individuals found it most difficult to “judge the advantages and disadvantages of different treatment options” (44%); “decide how you can protect yourself from illness using information from the mass media” (42%); and “find information on how to handle mental health problems” (38%). In Germany, as many as 71% of respondents indicated that they would find it “very difficult” or “difficult” to judge the advantages and disadvantages of different treatments compared to 26% of respondents in Slovenia. Similarly, 61% of respondents in Germany found deciding how one can protect oneself from illness using information from the mass media” to be “very difficult” or “difficult”, compared to 27% of respondents in Austria. Of the 15 countries, Germany also had the highest share of respondents who indicated that they would find “very difficult” or “difficult” (56%) to find information on how to handle mental health problems, while Slovenia had the lowest share of respondents (19%). In contrast, individuals generally found it least difficult to “act on advice from your doctor or pharmacist” (8%); “find information on healthy lifestyles such as physical exercise, healthy food or nutrition” (10%); and “understand advice concerning your health from family or friends” (17%).
Individual responses were used to derive a composite health literacy score. Table 6.1 reveals that, on average, respondents in the countries with available data experienced 76.3% of the health literacy tasks they were presented with to be “very easy” or “easy”. Levels of health literacy vary. In Slovenia, Portugal and Austria, on average, participants experienced 86%, 85% and 85% of the health literacy tasks as “very easy” or “easy”. By contrast, in Italy, Belgium and Germany, on average, participants experienced 69%, 66% and 65% of the tasks as “very easy” or “easy”. However, country comparisons of HLS19 data should be interpreted with caution due to the above-mentioned limitations.
Table 6.1. Mean score values of health literacy proficiency, selected OECD countries, 2019-20
Percentage of HLS19-Q12 items that respondents found to be easy or very easy
|
Country |
Mean (%) |
|---|---|
|
Austria |
85 |
|
Belgium |
66 |
|
Switzerland |
77 |
|
Czech Republic |
76 |
|
Germany |
65 |
|
Denmark |
77 |
|
France |
78 |
|
Hungary |
80 |
|
Ireland |
79 |
|
Israel |
73 |
|
Italy |
69 |
|
Norway |
79 |
|
Portugal |
85 |
|
Slovenia |
86 |
|
Slovak Republic |
70 |
|
HLS19 OECD average |
76 |
Note: Due to the wide variety of sampling and data collection procedures across countries, country comparisons and comparisons with the HLS19 OECD average should be interpreted with caution.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
6.5.1. Disparities in levels of health literacy
Figure 6.3 suggests that men and women have broadly similar levels of health literacy across the 15 HLS19 OECD countries with data available. For example, 84% of male respondents in Austria perceived health literacy tasks as “very easy” or “easy” compared to 85% of female respondents. Similarly, 77% of male and female respondents in France and Switzerland perceived health literacy tasks as “very easy” or “easy”.
Figure 6.3. Mean score values of health literacy proficiency by gender, selected OECD countries, 2019‑20
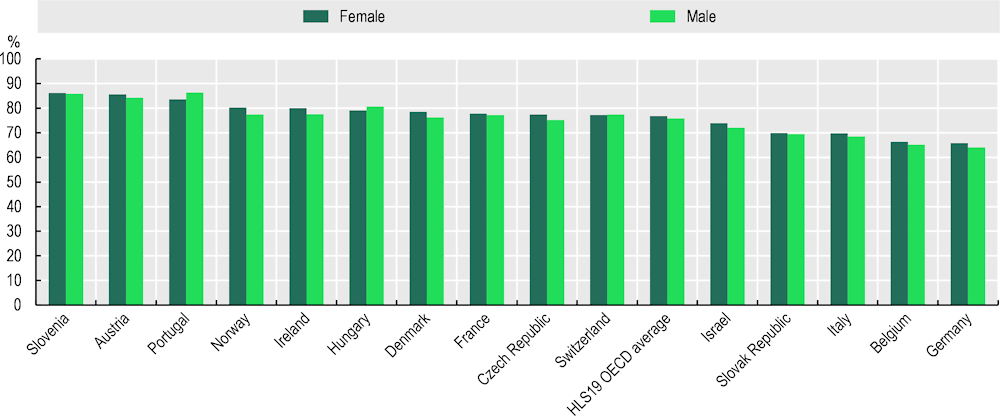
Note: The figure illustrates the health literacy index by gender in each of the HLS19 OECD countries. Specifically, the figure illustrates the percentage of male and female respondents who perceived health literacy tasks as “very easy” or “easy”.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
By contrast, Figure 6.4 suggests that health literacy differs across individuals with varying levels of financial deprivation. Financial deprivation was calculated by summarising the scores of respondents on the following three questions: “How easy or difficult is it usually for you to afford medication if needed?”, “How easy or difficult is it usually for you to afford medical examinations and treatments if needed?” and “How easy or difficult is it for you to pay all bills at the end of the month?” The response categories were “very easy”, “easy”, “difficult”, and “very difficult”.
On average, individuals with no or some financial deprivation perceived 79% of the health literacy tasks as “very easy” or “easy”, whereas individuals with considerable or severe financial deprivation considered 68% of the health literacy tasks as “very easy” or “easy”. In Slovenia, respondents with no or some financial deprivation perceived 90% of the health literacy tasks as “very easy” or “easy”, while in Austria, Hungary, Ireland, and Portugal, individuals with no or some financial deprivation perceived slightly more than 80% of the health literacy tasks as “very easy” or “easy”. In Slovenia, respondents with considerable or severe financial deprivation perceived 80% of the health literacy tasks as “very easy” or “easy”. Individuals with considerable or severe financial deprivation in Austria, the Czech Republic, Denmark, France, Hungary, Ireland, Portugal and Switzerland perceived two-thirds of the health literacy tasks as “very easy” or “easy”. Again, country comparisons of HLS19 data should be interpreted with caution due to the above-mentioned limitations.
Figure 6.4. Mean score values of health literacy, by levels of financial deprivation, selected OECD countries, 2019-20
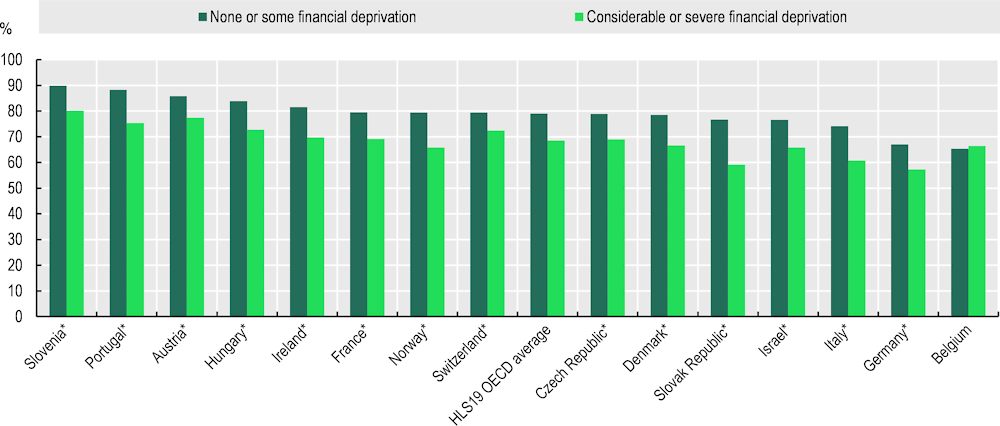
Note: The figure shows the percentage of respondents who perceived health literacy tasks as “very easy” or “easy”, depending on their financial deprivation. Financial deprivation was calculated by summarising the scores of respondents who answered “very difficult” or “difficult” to the following three questions: “How easy or difficult is it usually for you to afford medication if needed?”, “How easy or difficult is it usually for you to afford medical examinations and treatments if needed?” and “How easy or difficult is it for you to pay all bills at the end of the month?” The dark green bars represent the percentage of respondents who experience none or some financial deprivation, whereas the light green bars represent the percentage of respondents who experience considerable or severe financial deprivation. The asterisk (*) means that the differences in mean levels of health literacy between those who have none or some financial deprivation and those who have considerable or severe financial deprivation are statistically significant at the 5% level. Due to the wide variety of sampling and data collection procedures across countries, country comparisons should be interpreted with caution.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
Differences in health literacy across individuals with different levels of educational attainment are generally small. Figure 6.5 indicates that, on average, 73% of the health literacy tasks were perceived as “very easy” or “easy” among individuals with at most a lower secondary education degree; 76% among individuals with an upper secondary degree; and 78% among individuals with a post-secondary or a short-cycle tertiary programme degree as well as individuals with a tertiary degree. In HLS19, educational attainment was measured using the International Standard Classification of Education (ISCED) scale, which also incorporates professional experiences. It could be that other measures like, e.g. years in education, would have yielded slightly different results. The finding that health literacy differs depending on whether individuals face financial deprivation or not but not depending on their educational qualifications could reflect the fact that although health literacy is correlated with academic skills, it is a different construct which has not been prioritised in formal education. Individuals who experience financial deprivation may have fewer opportunities than those who have not had the opportunity to invest in the acquisition of health literacy over the life course.
Figure 6.5. Mean score values of health literacy, by educational attainment, selected OECD countries, 2019-20
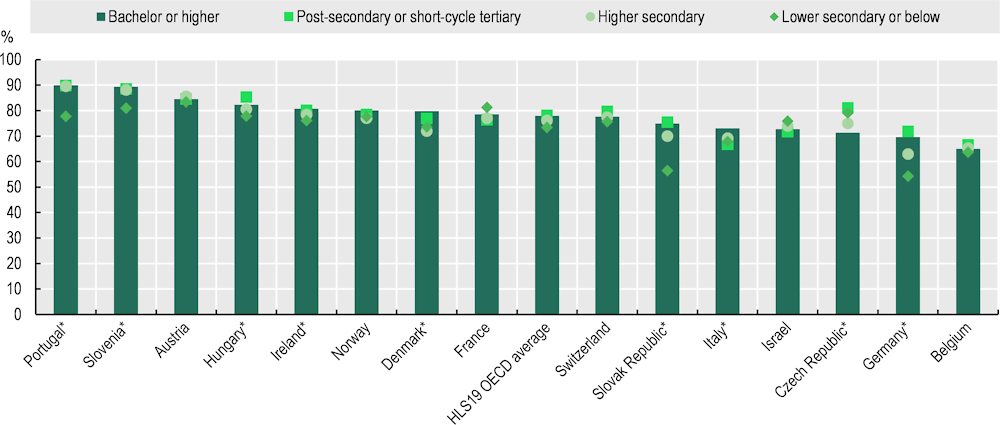
Note: The figure shows the percentage of respondents who perceived health literacy tasks as “very easy” or “easy”, depending on their educational attainment. Education attainment was measured using the ISCED. The green diamond represents the percentage of respondents that completed lower secondary or below. The light green circles represent the percentage of respondents who completed higher secondary. The green squares represent the percentage of respondents who completed post-secondary or short-cycle tertiary. The dark green bars represent the percentage of respondents who completed either lower secondary or below. The asterisk (*) means that the differences in the mean level of health literacy based on educational attainment are statistically significant at the 5% level. Due to the wide variety of sampling and data collection procedures across countries, country comparisons should be interpreted with caution.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
Figure 6.6 indicates that the mean score values of health literacy do not differ greatly across age groups. On average across HLS19 OECD countries, 76% of the health literacy tasks were perceived as “very easy” or “easy” among 18‑35 year-olds; 77% among 36‑75 year-olds; and 74% among more mature individuals.
Figure 6.6. Mean score values of health literacy by age in selected OECD countries, 2019‑20
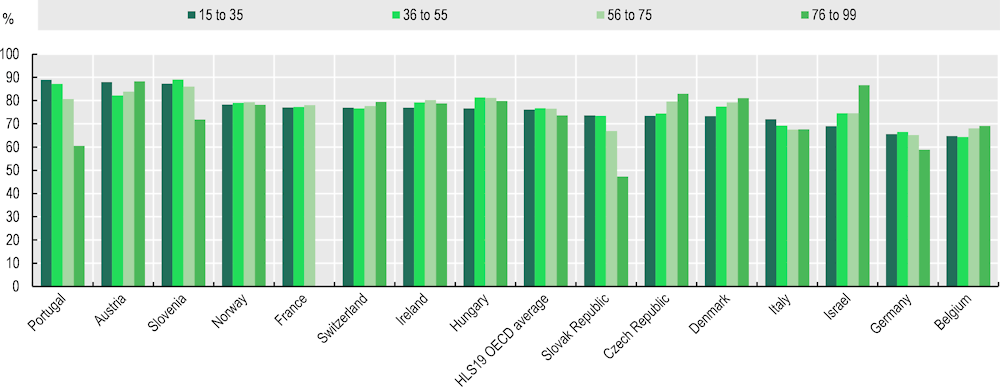
Note: The figure illustrates the percentage of respondents in an age bracket who perceived health literacy tasks as “very easy” or “easy”. Age was measured in years but grouped into four categories. Each bar represents an age bracket, starting with 15‑35, followed by 36‑55, then 56‑75, and finally 76 and older. Due to the wide variety of sampling and data collection procedures across countries, country comparisons should be interpreted with caution.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
Box 6.1. Health Literacy in selected Asian and Latin American countries
Instruments used in the HLS19 produced by HLS-EU have been used in Japan to compare health literacy levels in the country to those observed in the European context (Nakayama et al., 2015[17]). In line with Europe, levels of general health literacy in Japan predicted health status even after controlling for gender, age group, education, income, occupation, self-assessed living conditions and municipality size (Nakayama et al., 2015[17]). However, analyses revealed that although Japan is one of the countries with the longest life expectancy in the world, health literacy in the Japanese population is lower than in Europe, with Japanese respondents rating all test items as more difficult than European respondents: Japanese respondents found 22% more tasks to be difficult or very difficult than their European counterparts (Nakayama et al., 2015[17]). The difference in health literacy levels between Japan and European countries was attributed to the greater difficulty in accessing reliable and understandable health information in Japan because of the lack of a comprehensive national platform to aid individuals in locating information about treatments and illnesses (Nakayama et al., 2015[17]).
In Latin America, few studies have been conducted on health literacy. When such studies are conducted, they use different surveys and differ in terms of target population, sampling and instruments to assess health literacy levels, all of which reduce cross-country comparability. Therefore, there is considerable variation in estimates of levels of health literacy in the population, ranging between 5.0% and 73.3% (Arrighi et al., 2021[71]). In Mexico, for example, Mávita-Corral and colleagues conducted a cross-sectional study using the European Health Literacy Survey Questionnaire produced by the HLS‑EU. The questionnaire was administered to a sample of 477 individuals that included students, academics and administrative staff. The study found that 9% of individuals had excellent health literacy; 40% had sufficient levels of health literacy; 43% had problematic levels of health literacy; and 8% had inadequate health literacy levels (Mávita-Corral, 2017[72]; Nakayama et al., 2015[17]). In Argentina, by contrast, a random sample of patients in a University Hospital was assessed and interviewed using the Short Assessment of Health Literacy for Spanish-speaking Adults. The Short Assessment of Health Literacy is a validated health literacy assessment tool containing 50 items designed to assess a Spanish-speaking adult’s ability to read and understand common medical terms (Agency for Healthcare Research and Quality, 2022[73]), which is based on the Rapid Estimate of Adult Literacy in Medicine (REALM) tool (Lee et al., 2006[74]). The study found that about 30% of patients had inadequate health literacy levels (Konfino et al., 2009[75]). In Brazil, Coelho and colleagues assessed functional health literacy, which they define as the “degree to which individuals can obtain, process, and understand basic information and services necessary for making appropriate health-related decisions” (Coelho et al., 2014[76]). They measure functional health literacy using the Brief Test of Functional Health Literacy in Adults, which is a shortened version of the Test of Functional Health Literacy (TOFHLA) – another tool that was developed to screen levels of health literacy and that divides people into categories with low or high levels of health literacy (Sørensen et al., 2013[77]). The Brief Test of Functional Health Literacy in Adults was administered to patients in two Brazilian public hospitals in 2009. The study found that 58% of patients had inadequate functional health literacy (Coelho et al., 2014[76]). In addition to the test, the researchers conducted two dialogue rounds with the patients with adequate functional health literacy (Group 1) and inadequate functional health literacy (Group 2) in order to evaluate each group’s understanding of food serving sizes. Overall, those with inadequate functional health literacy had greater difficulty understanding the food guide. Such findings demonstrate that low levels of health literacy can impact self-management and awareness of how to lead a healthy life more broadly.
In the United States, a literacy assessment conducted by the US Department of Education found that nearly 90% of US adults are not proficient in reading, understanding and acting on medical information. More specifically, according to the survey, “one in three patients has ‘basic’ or ‘below basic’ health literacy”. Similarly, in 2006, the Australian Bureau of Statistics found that almost 60% of adult Australians had low health literacy and that “a total of 59% of 17‑74 year-olds did not have adequate health literacy skills to effectively and efficiently understand and apply health-related information in their daily lives” (Choudhry et al., 2019[78]). Canada is no different – results from the International Adult Literacy and Skills published by the Canadian Council on Learning indicate that “six in ten Canadian adults do not have the skills needed to adequately manage their health and health-care needs” (Canadian Council on Learning, 2008[79]).
The surveys conducted in Japan and Mexico translated the instruments used in the HLS19 produced by HLS-EU and, as such, can be used to similarly compare results. However, the other surveys conducted in Argentina, Brazil, the United States, Australia and Canada do not use translated versions of the EU-HLS, nor do they use indicators that are comparable to the EU‑HLS, which limits the ability to compare health literacy levels across OECD countries that are not part of Europe and that are thus not part of the EU-HLS.
6.5.2. Disparities in health behaviours, health status and healthcare utilisation across individuals with different levels of health literacy
The data suggest that individuals with higher levels of health literacy tend to engage in healthier lifestyles: they consume fruits and vegetables more frequently and exercise more than individuals with lower levels of health literacy (Table 6.2). They are also more likely to report being in good general health and are less likely to report suffering from long-term illnesses or health problems (Table 6.3). Finally, they are less likely to use emergency healthcare services and surgical specialists (Table 6.4).
For example, on average, across the 15 HLS19 OECD countries with available data, a difference of 10 percentage points in the number of health literacy tasks individuals perceive as “very easy” or “easy” is associated with a difference of 2 percentage points in the likelihood that respondents reported consuming fruits and vegetables at least four days a week. This difference corresponds to 1.4 percentage points when comparing individuals with different levels of health literacy and the same age, gender, level of educational attainment and financial deprivation. Similarly, on average, across the HLS19 OECD countries, a difference of 10 percentage points in the number of health literacy tasks individuals perceive as “very easy” or “easy” is associated with a difference of 2.1 percentage points increase in the likelihood that respondents reported exercising at least four days a week. This difference corresponds to 1.9 percentage points when individuals with different levels of health literacy and the same age, gender, level of educational attainment and financial deprivation are compared.
Table 6.2. The association between health literacy and health lifestyles, in selected OECD countries, 2019‑20
Differences in the percentage of adults who consumed fruits and vegetables at least four days a week and the percentage of adults who are engaged in physical activity at least four days a week as a function of 1 percentage point difference in the number of health literacy tasks that an individual perceives as “very easy” or “easy”
|
Fruit and vegetable consumption |
Engagement in physical activity |
|||
|---|---|---|---|---|
|
No controls |
With socio-economic controls |
No controls |
With socio-economic controls |
|
|
Austria |
0.32* |
0.27* |
0.29* |
0.25* |
|
Belgium |
0.18* |
0.12* |
0.17* |
0.15* |
|
Czech Republic |
0.15* |
0.04 |
0.22* |
0.20* |
|
Denmark |
0.26* |
0.18* |
0.25* |
0.22* |
|
France |
0.16* |
0.11* |
0.09 |
0.07 |
|
Germany |
0.26* |
0.19* |
0.19* |
0.17* |
|
HLS19 OECD average |
0.20* |
0.14* |
0.21* |
0.19* |
|
Hungary |
0.21* |
0.11 |
0.17* |
0.24* |
|
Ireland |
0.11* |
0.05 |
0.15* |
0.13* |
|
Israel |
0.28* |
0.17* |
0.20* |
0.09 |
|
Italy |
0.21* |
0.20* |
0.25* |
0.23* |
|
Norway |
0.15* |
0.09* |
0.24* |
0.22* |
|
Portugal |
0.02 |
0.05 |
0.19* |
0.11 |
|
Slovak Republic |
0.34* |
0.28* |
0.33* |
0.26* |
|
Slovenia |
0.19* |
0.19* |
0.34* |
0.36* |
|
Switzerland |
0.15* |
0.09 |
0.14* |
0.10 |
Note: Socio-economic controls include age, gender, level of educational attainment and financial deprivation.
Results are based on linear probability models. The choice to use linear probability models instead of logistic models or probit models, given the dichotomous nature of the dependent variable was driven by interpretability and the fact that estimates from different sets of linear probability models are more comparable across models than estimates from logistic or probit regression estimates (Mood, 2009[80]). However, estimates might not be valid for values close to the edges. The asterisk (*) indicates statistical significance at the 5% level.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
Health literacy is also positively associated with health status: for example, across the 15 HLS19 OECD countries, a difference of 10 percentage points in the number of health literacy tasks individuals perceive as “very easy” or “easy” is associated with on average, a 3.9 percentage points increase in the likelihood that respondents reported being in very good or good health. This difference corresponds to a 2.4 percentage-point increase when individuals with different levels of health literacy and the same age, gender, level of educational attainment and financial deprivation are compared.
Table 6.3. The association between health literacy and health, selected OECD countries, 2019‑20
Differences in the percentage of adults who report being in very good or good health and who report suffering from at least one long-term illness or health problem as a function of 1 percentage point difference in the number of health literacy tasks that an individual perceives as “very easy” or “easy”
|
Adults reporting being in very good or good health |
Adults reporting suffering from at least one long-term illness or health problem |
|||
|---|---|---|---|---|
|
|
No controls |
With socio-economic controls |
No controls |
With socio-economic controls |
|
Austria |
0.43* |
0.31* |
‑0.32* |
‑0.19* |
|
Belgium |
0.32* |
0.25* |
‑0.03 |
‑0.03 |
|
Czech Republic |
0.15* |
0.15* |
‑0.04 |
‑0.05 |
|
Denmark |
0.59* |
0.45* |
‑0.24* |
‑0.19* |
|
France |
0.41* |
0.31* |
‑0.15* |
‑0.11* |
|
Germany |
0.52* |
0.31* |
‑0.19* |
‑0.04 |
|
HLS19 OECD average |
0.39* |
0.24* |
‑0.22* |
‑0.13* |
|
Hungary |
0.36* |
0.24* |
‑0.23* |
‑0.18* |
|
Ireland |
0.32* |
0.2* |
‑0.15* |
‑0.1* |
|
Israel |
0.2* |
0.15* |
‑0.15* |
‑0.17* |
|
Italy |
0.31* |
0.2* |
‑0.15* |
‑0.08* |
|
Norway |
0.31* |
0.23* |
‑0.15* |
‑0.09 |
|
Portugal |
0.63* |
0.2* |
‑0.63* |
‑0.32* |
|
Slovak Republic |
0.42* |
0.1* |
‑0.27* |
‑0.04 |
|
Slovenia |
0.62* |
0.31* |
‑0.42* |
‑0.18* |
|
Switzerland |
0.33* |
0.24* |
‑0.14* |
‑0.11 |
Note: Socio-economic controls include age, gender, level of educational attainment and financial deprivation.
Results are based on linear probability models. The choice to use linear probability models instead of logistic models or probit models, given the dichotomous nature of the dependent variable was driven by interpretability and the fact that estimates from different sets of linear probability models are more comparable across models than estimates from logistic or probit regression estimates (Mood, 2009[80]). However, estimates might not be valid for values close to the edges. The asterisk (*) indicates statistical significance at the 5% level.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
Because individuals with higher levels of health literacy adopt healthier lifestyles, are in better overall health and are better at managing their conditions, other things being similar, individuals with higher levels of health literacy are less likely to use emergency services or surgical specialists (Table 6.4). At a time of tight public health budgets, reducing the need for individuals to use emergency services and specialist care can contribute to lower healthcare costs.
Table 6.4. The association between health literacy and the use of emergency healthcare services and surgical specialists, selected OECD countries, 2019‑20
Differences in the percentage of adults who report having used emergency healthcare services in the past 24 months and who report having used medical or surgical specialists at least once in the past 12 months as a function of 1 percentage point difference in the number of health literacy tasks that an individual perceives as “very easy” or “easy”
|
Adults using emergency healthcare services |
Adults using medical or surgical specialists |
|||
|---|---|---|---|---|
|
No controls |
With socio-economic controls |
No controls |
With socio-economic controls |
|
|
Austria |
‑0.27* |
‑0.23* |
‑0.04 |
‑0.04 |
|
Belgium |
‑0.19* |
‑0.15* |
0.09 |
0.08 |
|
Czech Republic |
‑0.05 |
0.02 |
0 |
‑0.01 |
|
Denmark |
‑0.09* |
‑0.04 |
‑0.12* |
‑0.15* |
|
France |
‑0.13* |
‑0.09* |
‑0.08 |
‑0.09 |
|
Germany |
‑0.11* |
‑0.02 |
‑0.16* |
‑0.11* |
|
HLS19 OECD average |
‑0.17* |
‑0.12* |
‑0.07 |
‑0.04 |
|
Hungary |
‑0.23* |
‑0.2* |
‑0.08 |
‑0.07 |
|
Ireland |
‑0.18* |
‑0.09 |
‑0.18* |
‑0.21* |
|
Israel |
‑0.19* |
‑0.13 |
‑0.04 |
‑0.03 |
|
Italy |
‑0.07* |
‑0.03 |
0.01 |
0.01 |
|
Norway |
‑0.13* |
‑0.1* |
‑0.08 |
‑0.064 |
|
Portugal |
‑0.34* |
‑0.3* |
‑0.12 |
‑0.12 |
|
Slovak Republic |
‑0.23* |
‑0.18* |
‑0.14* |
‑0.05 |
|
Slovenia |
‑0.14* |
‑0.1* |
‑0.13* |
‑0.04 |
|
Switzerland |
‑0.13* |
‑0.09 |
‑0.12* |
‑0.09 |
Note: Socio-economic controls include age, gender, level of educational attainment and financial deprivation.
Results are based on linear probability models. The choice to use linear probability models instead of logistic models or probit models, given the dichotomous nature of the dependent variable, was driven by interpretability and the fact that estimates from different sets of linear probability models are more comparable across models than estimates from logistic or probit regression estimates (Mood, 2009[80]). However, estimates might not be valid for values close to the edges. The asterisk (*) indicates statistical significance at the 5% level.
Source: The HLS19 Consortium of the WHO Action Network M-POHL (2021[19]), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
6.6. Policy efforts to promote health literacy and improve access to healthcare information and services
Austria, Germany, Ireland and Portugal have taken measures to promote health literacy among their populations and/or adapt how they disseminate information to ensure individuals with varying levels of health literacy can access services and make the most of healthcare. The following section focuses on these four countries and the policies and initiatives they have implemented in recent years.
6.6.1. Austria
Health literacy in Austria received nationwide attention after the preliminary results of the HLS-EU released in 2011/12 revealed that health literacy in the country was significantly lower than the government had expected (Dietscher, Nowak and Pelikan, 2020[81]). Some 56% of all Austrians only had limited health literacy – a share that was higher than the international average of 48% (HLS-EU-Consortium, 2012[82]; Sørensen et al., 2015[16]). The same year, two fundamental health reform processes were launched in Austria with the aim of increasing in the following 20 years the number of “healthy years” lived by individuals in Austria. The health reforms included ten public-health-oriented national health targets developed in consultation with stakeholders from different sectors, relevant institutions and civil society (Dietscher, Nowak and Pelikan, 2020[81]). Improving health literacy in the population was one of the ten national health targets2 (Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz, 2022[83]).
In order to achieve higher health literacy among Austrians, a working group composed of representatives from different policy fields, expert organisations, non-governmental organisations and social security institutions was established. The group was tasked with developing three sub-targets and adopting matching interventions in different sectors, including healthcare, education, community settings and extracurricular youth work (Dietscher, Nowak and Pelikan, 2020[81]). Applying the “management by targets” approach, the Austrian Ministry of Health, the Austrian provinces and social security institutions representatives defined intervention areas that were further developed during the second period of the national reform strategy (2017‑21) (Dietscher, Nowak and Pelikan, 2020[81]).
The group aimed to improve the quality of communication and information in the healthcare sector by using a national health information website3 and setting national priorities. Moreover, the Austrian Health Literacy Alliance (Österreichische Plattform Gesundheitskompetenz) was implemented as a national health literacy co‑ordination structure. Funded through mechanisms of the ongoing Austrian healthcare reform, the partners started some new interventions and contributed to interventions already initiated by the national health targets (Dietscher, Nowak and Pelikan, 2020[81]). In addition, the group envisaged that Austria would continue to participate in the HLS-EU. In the second period of Austria’s reform strategy, the goal of enhancing the organisational structure of health literacy was added as an intervention area (Bundesministerium für Gesundheit und Frauen, 2017[84]; Dietscher, Nowak and Pelikan, 2020[81]).
The above-mentioned Austrian Health Literacy Alliance was implemented in 2015 and has since become essential to the development of health literacy. A core team chaired by a representative from the Austrian Federal Ministry of Social Affairs, Health, Care and Consumer Protection and composed of representatives from the federal government, federal states, social security institutions and Health in All Policies partners acts as the Alliance’s decision-making body. Organisations and individuals whose activities and projects contribute to improving the population’s health literacy are encouraged to become members of the Alliance (Österreichische Plattform Gesundheitskompetenz, 2022[85]).
In addition to an annual national health literacy conference that the Alliance organises, it established intersectoral working groups to create activities, guidelines and tools in five focus areas. The focus areas include: 1) high-quality health information (such as developing materials that a wide range of people can understand); 2) high-quality communication in healthcare (such as improving healthcare professionals’ conversation skills and enabling patients to ask more clarifying questions; 3) health-literate organisations; 4) empowerment of citizens and patients; and 5) measuring health literacy through the continuing participation in HLS-EU, and follow-up surveys such as HLS19, and development of other health literacy surveys (e.g. with a focus on SARS-CoV-2 or children’s health literacy) (Österreichische Plattform Gesundheitskompetenz, 2022[85]; 2022[86]).
The HLS-EU study found that many Austrians struggle to understand the extent to which the health-related information they are exposed to is trustworthy (Pelikan, Röthlin and Ganahl, 2013[87]). Considering that a study from 2015 suggested that only 11% of articles about health and diseases in online and print media in Austria reported scientific knowledge correctly, whereas 60% either exaggerated or understated the scientific facts, the Austrians’ insecurity about their ability to assess the quality of written health information is not surprising (Kerschner et al., 2015[88]). In order to ensure high-quality health information, the Alliance defined 15 quality criteria for good health information that organisations are encouraged to use when producing health information in brochures, videos, websites or other formats (Box 6.2.). Moreover, the Alliance created a factsheet with practical guidelines on comprehensible language for written health information. In addition, two checklists that the Alliance developed help individuals and healthcare providers assess whether the written health information they receive or want to pass on to their patients is trustworthy and of high quality. Furthermore, to increase health literacy among refugees who do not speak German, the Alliance prepared short videos about the Austrian health system in Arabic, Dari and Somali (Österreichische Plattform Gesundheitskompetenz, 2022[89]).
Box 6.2. The Austrian Health Literacy Alliance’s criteria for publishing high-quality health information
The Austrian Health Literacy Alliance developed a brochure to guide organisations that want to produce high-quality health information. Moreover, the Austrian Health Literacy Alliance encourages organisations to write and publish method papers in which they describe how the quality criteria defined by the Alliance have been taken into consideration in their health information publications. This, in turn, can be expected to increase the organisations’ credibility and allow them to act as role models (Österreichische Plattform Gesundheitskompetenz, 2020[90]).
The 15 criteria are grouped into basic criteria (Criteria 1‑3), selection and presentation of facts criteria (Criteria 4‑11) and credibility criteria (Criteria 12‑15) (Österreichische Plattform Gesundheitskompetenz, 2020[90]):
Basic criteria
1. Identification of special information needs. The health information should be tailored, comprehensible and useful for its respective target group.
2. Systematic research. The used sources should be appropriately chosen for the respective question and easily verifiable.
3. Selection of the evidence. The target group should receive the most up-to-date information from the best available studies while being informed about potential research gaps and biases.
Selection and presentation of facts criteria
4. Choice and presentation of results (endpoints). The target group should receive information through the selected endpoints to assess impacts on their daily lives.
5. Choice and presentation of comparisons. Individuals should be able to use the facts to make informed choices for or against an examination or treatment.
6. Dealing with numbers and risk information. Benefits and harms should be presented in a balanced, gender-appropriate and comprehensible manner that includes absolute risk information, such as meaningful and uniform reference values like 1 in 1 000).
7. Consideration of age and gender differences. The target group should be informed about the natural course of the disease and about the intervention’s effects, benefits, harms and risks, considering their age and gender.
8. Adaptation to the target group. Content, cultural aspects, language, design and medium should be adapted to the target group.
9. Objectively appropriate presentation. An appropriate and realistic presentation in language and image should offer the target group a basis for decision making, while any uncertainties should be named.
10. Ratings and recommendations. Through the clear separation of information and recommendations, the target group should be able to make health decisions in line with their needs and values.
11. Procedure for the preparation of decision aids. The target group should be able to make informed choices for or against different examination and treatment options.
Credibility criteria
12. Transparency about responsible persons. Users should be able to assess the source and reliability of health information.
13. Disclosure of conflicts of interest. Users should be able to identify conflicts of interest behind the information.
14. Description of formats and contents. Individuals should be able to quickly decide whether they want to use the health information.
15. Updating the contents. Users should be able to assess the topicality and updating process of the information.
Source: Österreichische Plattform Gesundheitskompetenz (2020[90]), Gute Gesundheitsinformation Österreich: Die 15 Qualitätskriterien (Good Health Information Austria: The 15 Quality Criteria), https://oepgk.at/wp-content/uploads/2020/12/2020_11_18_die-gute-gesundheitsinformation.pdf.
However, clear communication does not only concern written or recorded health information. According to the HLS-EU survey from 2011/12, 22% of the respondents indicated that they found it challenging to understand what their doctor was telling them, while 32% of the respondents said that, based on the information their doctor gave them, they considered it difficult to decide about medical procedures (HLS-EU-Consortium, 2012[82]). The HLS-EU study from 2019 identified challenges in active patient participation, which include sufficient conversation time, easy-to-understand language, encouraging the patients to share their personal views and ideas, actively listening to them and involving them in decision-making processes (Griebler et al., 2021[91]). In order to enhance conversation quality in healthcare and create a more patient-centred healthcare culture, the Alliance developed a comprehensive national strategy, focusing on four fields of action: staff empowerment, patient empowerment, organisational and process development, and health system and culture development (Österreichische Plattform Gesundheitskompetenz, 2022[92]).
More concretely, health professionals should be able to improve their conversation competences during all stages of their career – be it in education, training, further education or at the workplace. Communication skills courses and “train-the-trainer” programmes were developed for this purpose, as well as a nationwide trainer network. The participants evaluated the trainings very positively and indicated a significant increase in their self-assessed competences following the completion of the training (Ammentorp et al., 2021[93]; Österreichische Plattform Gesundheitskompetenz, 2022[92]; Sator, Holler and Rosenbaum, 2021[94]).
As communication should not be one-sided, patients are equally encouraged to actively participate in their healthcare. In order to support the empowerment of patients, the Alliance introduced an Austrian adaptation of the international “Ask me 3” initiative, which encourages patients to ask at least three questions during their medical appointment: 1) “What is my health problem?”; 2) “What can I do?”; 3) “Why should I do this?” At the same time, health professionals should ensure that patients feel comfortable enough to ask questions and understand the answers to them (Österreichische Plattform Gesundheitskompetenz, 2022[95]). Some social security institutions also offer patient training and coaching to prepare patients for medical appointments (Dietscher, Nowak and Pelikan, 2020[81]; Österreichische Plattform Gesundheitskompetenz, 2022[92]). Another important aspect of patients’ empowerment is well‑designed and well-implemented patient rights. Following the first research results from 2020 that uncovered a need to improve the design and implementation of patients’ rights, more concrete implementation proposals are currently being developed (Österreichische Plattform Gesundheitskompetenz, 2022[95]; Schmotzer and Nowak, 2021[96]).
The Alliance also aims to enhance the organisational aspect of health literacy. By creating a starter kit, which includes a flexible practice guide describing nine different sub-processes and four self-assessment tools that can be used by healthcare institutions, primary care units, companies, as well as institutions offering extracurricular youth work, the Alliance wants to support organisations in achieving this goal. Moreover, the Alliance is developing and testing recognition processes that organisations can apply for to be awarded a “health-competent organisation” recognition (Österreichische Plattform Gesundheitskompetenz, 2022[97]).
All in all, the fortunate publication timing of the first HLS-EU in 2011/12 enabled health literacy to be incorporated into the health targets and “management by targets” approach within the Austrian health reform processes, which resulted in the identification of several focus areas and the development of matching activities to improve the Austrian population’s health literacy. However, despite being recognised that health literacy interventions should be carried out in different sectors influencing health literacy outcomes, such as education or community settings, most discussions focused on the healthcare sector. Moreover, while the pioneering pilot projects were considered successful, health literacy interventions have yet to prove to be efficient in the long term, as well as to maintain public funding and interest.
The results of the HLS19 study in which Austria participated together with 16 other countries show that Austria’s position in European health literacy saw some clear improvement. These results are promising and show that the efforts taken are worthwhile. Currently, priorities for the next healthcare reform period (2024‑28/9) are being negotiated, and it is hoped that health literacy will remain high on the agenda.
6.6.2. Germany
Following the results of the HLS-EU in 2012 (HLS-EU-Consortium, 2012[82]) as well as studies on health literacy in Germany (Jordan and Hoebel, 2015[98]; Schaeffer et al., 2016[99]), an independent civil society initiative was established to set up an action plan to promote population-level health literacy (Schaeffer et al., 2021[13]).
The initiative convened a group of independent experts and a series of working group workshops with representatives from different sectors and established a monitoring office. The expert group helped develop the framework of the National Action Plan by reviewing the literature on definitions of health literacy and its determinants, reviewing existing action plans established to promote health literacy and analysing the effectiveness of different interventions. The scoping phase led to the identification of four thematic priorities – referred to as action areas – and the establishment of working groups to develop a set of recommendations and guiding principles for the implementation of initiatives undertaken to advance the thematic priorities (Box 6.3 describes the recommendations within the four thematic priorities and the guiding principles for the implementation of such recommendations) (Schaeffer et al., 2021[13]).
The core elements of the National Action Plan were then discussed and further developed in two workshops and individual consultations with potential partners, stakeholders, interest groups and patient representatives. The first workshop involved stakeholders from the health and education systems and the Alliance for Health Literacy, whereas the second workshop involved patient and self-help organisations. In the workshops, the experts and workshop participants discussed the core elements of the National Action Plan, using three guiding questions: 1) “Has the importance of the field of action for Germany been adequately defined?”; 2) “Which fields of action should be at the centre of the action plan?”; and 3) “Which actors and partners can promote these lines of action?” The main goals of the workshops and individual consultations were to include different perspectives in finalising the Action Plan, establish collaborations with important stakeholders from different sectors and create motivation to implement the Action Plan (Schaeffer et al., 2021[13]).
The final version of the National Action Plan, published in 2018, consists of a section explaining health literacy’s political and social relevance, the concepts and definitions of health literacy, crucial empirical findings and 15 recommendations within 4 action areas. The action areas focus on: 1) promoting health literacy in all areas of everyday life; 2) creating a user-friendly and user-centred, health-literate healthcare system; 3) living a health-literate life coping with chronic illness; and 4) systematically expanding health literacy research. In addition to explaining why each recommendation is relevant, the report suggested concrete actions that could be undertaken and which actors should implement each recommendation (Schaeffer et al., 2018[100]). Box 6.3 lists the 15 recommendations and the 5 guiding principles to apply when implementing the National Action Plan.
Box 6.3. Germany’s National Action Plan: 15 recommendations to improve the population’s health literacy
Action field 1: Promote health literacy in all areas of everyday life
1. Enable the education system to promote health literacy early on in life. This can be achieved by placing health literacy in the curricula of elementary schools, secondary schools, universities, as well as in vocational training institutions and adult education.
2. Promote health literacy in professional life and at the workplace. This could be done by organising health literacy learning and training opportunities in the workplace.
3. Strengthen health literacy regarding food consumption and nutrition. One of the recommendations to strengthen health literacy with regard to nutrition in Germany was to label consumer products, especially food, beverages, and dietary supplements, more clearly and comprehensibly and to introduce a traffic light system that is mandatory for food manufacturers in order to indicate how nutritious different foods are.
4. Facilitate the handling of health information in the media. The suggestion by Germany’s National Action Plan was to empower health professionals to recommend quality-assured print and digital health information.
5. Empower communities to strengthen the health literacy of citizens in their living environment. A proposed approach, put forward by the National Action Plan, to strengthen the health literacy of citizens is to collaborate with educational institutions, sports clubs, fitness studios, citizens’ initiatives and self-help groups in order to develop attractive events to discuss health problems in the residential neighbourhood/at the community level.
Action field 2: Create a user-friendly and health-literate healthcare system
6. Integrate health literacy as a standard at all levels of the healthcare system. This can be done by including the promotion of health literacy structurally in the healthcare system and removing obstacles to its implementation by organisations and healthcare professions, for example, through adequate further development of the remuneration system.
7. Facilitate navigation within the healthcare system, increase transparency and reduce administrative barriers. A proposed approach in Germany is to make navigation within and between healthcare organisations easier and simplify administrative procedures such as forms and contracts.
8. Create comprehensible, effective communication between health professionals and users. An example of what can be done in Germany to create more user-friendly health information is to establish interpreting services and translation aids so that language is not a barrier for migrants, immigrants or refugees.
9. Create user-friendly health information. In Germany, the suggestion is to consider simplifying health-related information, for instance, by writing in plain or easy language or providing it in a visual format so that people who have difficulties reading and understanding language can also access and understand it.
10. Facilitate and strengthen patient participation. This can be done by developing standardised practices on how to take into account patients’ voices and opinions throughout the treatment and care process and by more clearly stipulating patients’ rights in relation to care providers.
Action field 3: Living a health-literate life with chronic illness
11. Integrate health literacy into caring for the chronically ill. An approach is to design care programmes and facilities for those with chronic illnesses in such a way that it addresses not only the physical aspects of the illness but also the psychological, social and economic challenges of living with a chronic disease.
12. Facilitate and support a health-literate handling of disease progression and its consequences. A suggested approach is to promote initiatives that make a prescribed course of medical treatment, such as the intake of required medication, more comprehensible and co‑designable so that pharmaceuticals can be packed in the same package in case individuals are required to take several of them. In doing so, the goal would be to promote health literacy of people with chronic illnesses in dealing with their medication(s).
13. Strengthen the self-management ability of people with chronic illness and their families. It is proposed in Germany to consider adapting self-management programmes so that they focus on not only the expert’s view but also the perspective and problems of those with the disease and their relatives.
14. Promote health literacy for coping with everyday life and chronic illness. A proposal is to use mass media communication to increase public awareness about the importance and impact of chronic illness and make people with chronic illness and their families visible so that people are aware of the (sometimes invisible) struggles individuals with chronic diseases have.
Action field 4: Systematically research health literacy
15. Develop health literacy research. As part of the action plan, the proposal is to measure the population’s health literacy regularly and examine individual, societal and organisational determinants of health literacy, all in an effort to develop evidence-based interventions.
Basic principles to consider when implementing the National Action Plan
1. Reduce social and health inequality.
2. Change individual as well as structural conditions.
3. Enable user participation and shared decision making.
4. Use the possibilities digitalisation offers.
5. Establish the co‑operation of actors from all sectors of society.
Source: Schaeffer et al. (2018[100]), National Action Plan Health Literacy: Promoting Health Literacy in Germany, www.hlca-consortium.de/wp-content/uploads/2018/06/National-Action-Plan-Health-Literacy.pdf; Nationaler Aktionsplan Gesundheitskompetenz Geschäftsstelle (2020[101]), 15 konkrete Empfehlungen, um die Gesundheitskompetenz zu stärken (15 concrete recommendations to strengthen health literacy), www.nap-gesundheitskompetenz.de/aktionsplan/.
In order to increase the National Action Plan’s impact on health literacy, a three-part collaborative and co‑productive diffusion, dissemination, and implementation strategy was developed. Following a successful event aimed at representatives from media, politics, science and the administration, the National Action Plan was circulated by mail and electronically. Moreover, the National Action Plan was disseminated through publications in relevant journals and presentations at conferences to reach key implementation actors, including politicians and decision makers at the federal and federal state levels, executives of healthcare sector associations and organisations, as well as representatives from the education and training sectors. A dedicated website4 was created to further inform the general public about the National Action Plan and to provide extensive and up-to-date information on its development, fields of action, recommendations, future and past events, and the topic of health literacy in general (Schaeffer, Gille and Hurrelmann, 2020[102]).
Implementing the National Action Plan involved translating the 15 recommendations into concrete measures and relying on stakeholder support. To this end, consecutive strategy and policy papers have further developed specific recommendations and examined certain aspects of health literacy and specific population groups. Therefore, several workshops were conducted, which gathered experts from science and practice to specify selected recommendations of the National Action Plan. A total of eight strategy papers and four policy papers have been published so far, one of the latest additions being a call for putting greater efforts into the promotion of health literacy against the backdrop of the COVID‑19 pandemic and considering the recommendations of the National Action Plan on Health Literacy and its strategy papers (Schaeffer et al., 2022[103]).
Since the publication of the National Action Plan, several health literacy projects have been developed and implemented to promote health literacy. In addition to the National Action Plan, there are other networks and interest groups in Germany working on health literacy (Schaeffer and Gille, 2021[9]). For example, the Federal Ministry of Health (MoH), together with the stakeholders of the German healthcare system, launched the “Alliance for Health Literacy” (Bundesministerium für Gesundheit, n.d.[104]) in 2017. The members have committed themselves to developing new projects to improve health literacy. The German Network for Health Literacy, founded in 2019 (Schaefer and Ollenschläger, 2019[105]), the working group on health literacy in the German Network for Health Services Research (Ernstmann et al., 2020[106]) and the division of patient information and participation within the German Network for Evidence-Based Medicine (Lühnen et al., 2017[107]) are also worth mentioning in this context. In addition, the “Alliance Health Literacy and School” since recently advocates for developing a co-ordinated strategy for the holistic promotion of health literacy in schools and the systematic implementation of it (Okan et al., 2021[108]). Most of the initiatives are relatively young.
Although the discussion on health literacy started in Germany somewhat more than only ten years ago – later than in many other countries – a wide body of research on health literacy has developed. Meanwhile, several studies on population health literacy in Germany are available, as well as results on specific population groups (e.g. children and adolescents, people with migration backgrounds, etc.) and many other aspects of health literacy. Intervention research has also been slowly developing. For a considerable while, particular attention has been paid to the area of organisational health literacy and, most recently, to the health literacy of health professionals (Schaeffer, Haarmann and Griese, 2023[109]). Despite this progress, the expansion of research funding in the area of health literacy would be desirable.
6.6.3. Ireland
In Ireland, health literacy is an important element of the Healthy Ireland Framework. Part of this framework was created by a host of partners (the Department of Health, the Department of Children and Youth Affairs, the Department of Education and Skills, the Health Service Executive Directorates, statutory agencies, community and voluntary bodies, and the private sector), focusing on the goal of addressing and prioritising health literacy in developing future policy, such as education and information interventions (Department of Health Ireland, 2013[110]). Within this framework, several action plans were proposed, most notably, the Healthy Ireland Action Plan 2021‑2025 (Healthy Ireland, 2021[111]), the Sláintecare Action Plan 2019 (Department of Health Ireland, 2019[112]) and the Sláintecare Implementation Strategy and Action Plan 2021‑2023 (Department of Health Ireland, 2021[113]). These action plans aimed to strengthen the ease with which individuals could access the health sector and benefit from it and create a modern, responsive and integrated public health system. As part of the action plans, a series of initiatives were developed to promote health literacy among children and adults.
The Irish Heart Foundation’s (IHF) Health Literacy in Schools Project focused on promoting health literacy among young people aged 12 to 16 in post-primary schools that were part of the Delivering Equality of Opportunity in Schools programme,5 their families and teachers. Adolescents from disadvantaged communities in Ireland often experience poorer health and worse educational outcomes than their peers from more advantaged communities. For this reason, the WHO, University College Dublin, Dublin City University, National University of Ireland, Galway, and Swinburne Technological University created a tailored literacy measurement tool to track health literacy levels among adolescent populations; measure the effectiveness of interventions aimed at promoting health literacy in schools in Ireland; and create instruments to develop a national study to measure health literacy, its determinants and consequences for post-primary school-aged children. On top of measurement efforts, the project aimed to create a framework to build capacity within the schooling system to promote health literacy and an out-of-school lab experience (LifeLab) for adolescents to explore health and health literacy.6 The IHF recruited over 60 schools to participate in the project and rolled out the measurement instrument to over 1 500 adolescents in late 2021 and early 2022 (Irish Heart Foundation, 2021[114]; WHO, 2019[115]).
The Department of Health, the National Treatment Purchase Fund, the Health Service Executive, and the National Adult Literacy Agency (NALA), as well as experts in behavioural science, collaborated to create the Better Letter Initiative (BLI) to improve communication and decrease the burden faced by individuals accessing health services. It did so by implementing the use of plain English and behavioural science in healthcare. Therefore, the BLI did not directly seek to improve health literacy in the population but, rather, redesign services to make them more accessible, including to individuals with low levels of health literacy, and facilitate engagement despite cognitive heuristics and biases. Findings of the projects in the BLI indicated that by redesigning the content of Waiting List Validation Letters,7 the number of patients who did not respond dropped from 24% to 19%. Furthermore, due to the redesign and redrafting of inpatient and day case appointment letters, the number of patients who confirmed their appointment rose from 67% to 76%, and the rate of patients who did not attend their appointment declined from 11% to 5.3%. Ongoing work is considering how outpatient appointment offer letters and text reminders could be redesigned to further strengthen patient engagement (Department of Health Ireland, 2021[116]).
NALA aims to improve health literacy. NALA created and introduced ten literacy-friendly standards (Box 6.4), a literacy audit tool to assess healthcare settings and identify areas for improvement, short one‑hour webinars for healthcare professionals to make them more literacy-friendly, and the “Crystal Clear” mark to highlight pharmacies that have shown commitment to providing a literacy-friendly service to their customers. Furthermore, NALA offers a range of services to build health literacy among adult populations. These include free over-the-phone tuition for adults on literacy and numeracy and health literacy awareness videos tailored to cancer patients and their relatives (NALA, 2021[117]). Finally, NALA published a guide on improving communication in the health sector together with the Irish Health Information and Quality Authority (HIQA). The report includes detailed guidance documents for healthcare professionals and social care services to improve their communication with adults and children (HIQA, 2015[118]).
Box 6.4. Ireland’s National Adult Literacy Agency’s quality standards to become a literacy-friendly pharmacy
For a pharmacy to become “Crystal Clear,” it has to follow ten quality standards which focus on four areas: 1) communication; 2) staff awareness and responding sensitively; 3) policies and procedures; and 4) evaluating and improving. NALA provides tips on how to achieve each of these standards and checklists for pharmacies to see whether they already fulfil these standards.
Communication
1. Use plain English when speaking with people.
2. Write a medication label in plain English.
3. Check that people understand what you have told them.
4. Improve the layout of your pharmacy.
Staff awareness and responding sensitively
5. Improve staff awareness of health literacy and literacy-friendly work practices.
6. Respond sensitively to people with literacy and numeracy needs.
Policies and procedures
7. Develop a literacy-friendly policy.
8. Help people find and use important information and instructions.
9. Support staff to improve their own literacy, numeracy and digital skills, if needed.
Evaluating and improving
10. Evaluate and continually improve your literacy-friendly service.
Source: NALA (2021[117]), A Guide to Becoming a Crystal Clear Pharmacy, www.nala.ie/publications/the-crystal-clear-pharmacy-programme-and-its-crystal-clear-mark/.
6.6.4. Portugal
Following the successful implementation of the HLS-EU, whose results were published in 2012, Portugal developed and administered a national Health Literacy Survey in 2014. To improve health literacy, the Portuguese Directorate-General of Health developed an action plan based on international best practices. The Health Literacy Action Plan (Plano de Ação para a Literacia em Saúde) aims to promote improvements in health literacy in Portugal as well as organisational reforms and the better communication capacity of the National Health Service (SNS) and the health system in general, so as to promote easier and higher‑quality interactions, including among individuals with low levels of health literacy (Ministério da Saúde, 2018[119]).
The action plan is person-centred and uses a lifecycle approach, meaning that it considers how health literacy can be best promoted in childhood, adolescence, adulthood and elderly years. Furthermore, the action plan considers individuals in their social and relational context and how family relationships, peer groups and the broader community have the potential to shape an individual’s health literacy but also, in turn, can benefit from the individual’s health literacy. Finally, the action plan takes into account specific settings and contexts to define the following targeted strategic objectives: 1) promote the adoption of healthy lifestyles in everyday life; 2) train the population to make proper use of the health system; 3) promote the well-being of those affected by chronic disease; and 4) promote knowledge and research. For each objective, the action plan lists priority areas (e.g. nutrition or mental health); specific objectives according to the lifecycle (e.g. training parents and caretakers); transversal means (e.g. healthcare professionals or media); specific means (e.g. education professionals or social platforms); and products to use (e.g. websites or guidelines). The action plan also emphasises the importance of building close co‑ordination between different strategic partners, including ministries, academia, professional bodies, scientific societies, media and civil society (Ministério da Saúde, 2018[119]).
The action plan aims to equip health professionals with tools to effectively promote health literacy, develop campaigns and thematic interventions that speak to the population, and strengthen the network of stakeholders promoting health literacy. It does so by implementing a variety of measures and programmes. For example, the Literacy, Health and Well-Being Division in the General Directorate of Health and the Care Integration Programme focus on improving people’s autonomy and critical thinking regarding health. Furthermore, the Good Practices Handbook for Health Literacy – Empowering Health Professionals was introduced to support health professionals in better understanding what health literacy entails, how they can promote the acquisition of health literacy in the population, and how they can help break barriers faced by and promote positive outcomes of people with low levels of health literacy. The overall strategy of the action plan, in conjunction with the SNS+Proximity programme, which aims to put patients at the centre of the health system, and the Health Literacy Library, a tool that simplifies and provides information for citizens, their friends, family, and health professionals, is not just to make the health system easier to use for patients and health professionals but also to improve trust in the system as a whole (Ministério da Saúde, 2019[120]).
During the COVID‑19 pandemic, Portugal designed a Health Literacy Intervention Plan to empower individuals and communities facing the crisis. The plan had four axes:
The first axis revolved around developing information material, in particular, good practices in health literacy. This information material was developed by looking at good practices in health literacy, using scientific evidence, and eventually establishing context-specific support tools to guide the implementation of these good practices.
The second axis, called Health Literacy Intelligence, collected information on the population’s perceptions of the pandemic, risks associated with exposure and infection, as well as on the communication channels used in order to eventually personalise communication formats and content to avoid the spread of misinformation.
The third axis aimed to provide the population with the targeted information before, during, and after the emergency to influence behaviour to promote public health and control the crisis.
The fourth axis, referred to as Social Mobilisation, focused on creating micro-influencers in local communities in order to tackle and avoid misinformation, clarify all preventive measures that could be taken to protect oneself and others during the crisis, promote adherence to public health guidance measures and create a bridge between the scientific community and civil society.
All in all, the strategy’s multi-dimensional aspect intended to minimise social disruption and allow for different interventions based on the evolution of the crisis and local needs while maintaining a “the person at the centre of the system” approach (Ministério da Saúde, 2020[121]). Additionally, the government provided a guide for health professionals and scientists, specifically focused on communication strategies to promote adherence to vaccination against COVID‑19. The guide argued that professionals should emphasise the benefits at an individual and collective level to their own patients and social circle. Furthermore, the document highlighted how best to promote vaccination take-up, including prioritising the users' perspective and clarifying and addressing potential doubts and concerns of patients without discounting individual worries and experiences (Ministério da Saúde, 2021[122]).
6.7. Conclusions
The pandemic highlighted that whether innovations in the prevention and treatment of disease are successful or not hinges on the ability of individuals to comprehend, evaluate and apply the information they have about disease prevention and treatment. Without health literacy, individuals are prone to misinterpret health data, fall prey to unfounded health claims and mistrust innovative treatment options and regimens, thus leading to misguided health decisions.
The chapter reveals that many individuals find it difficult to judge the advantages and disadvantages of different treatment options, decide how to protect themselves from illness using information from the mass media and find information on how to handle mental health problems. These results, alongside results on the positive association between health literacy and general health, between health literacy and the likelihood that individuals will engage in healthy lifestyle choices, and the negative association between health literacy and the utilisation of emergency services, point to the need to strengthen population-level health literacy.
Identifying individuals with low levels of health literacy is therefore critical to reducing health inequalities and as a public health measure since lack of health literacy can lead some individuals to engage in behaviours that place entire communities at risk. Moreover, strengthening population-level health literacy is likely to reduce health expenditures since it has been shown to reduce emergency care and help individuals reduce the likelihood of developing chronic conditions, which pose a heavy burden on healthcare systems and to more effectively manage these when developing such conditions. As people are exposed to more health information than ever before – including inaccurate and misleading information – health literacy can reduce susceptibility to misinformation, disinformation and malinformation.
Increases in complexity in the information individuals are exposed to and in the incidence of chronic diseases have occurred at a time in which there has been an increase in the expectation that individuals will play an active role in managing their health. Increased choices can only result in improved outcomes if individuals have the knowledge and skills to be active agents and decision makers and if relevant information is communicated in ways that are aligned with their knowledge and skills. Reducing the mismatch between people’s health literacy skills and the demands of health systems can be pursued by, for example, strengthening the health literacy of individuals who currently have low levels of health literacy and improving the ability of healthcare providers to effectively communicate information in ways that best empower people’s ability to make decisions about their health.
References
[73] Agency for Healthcare Research and Quality (2022), Personal Health Literacy Measurement Tools, https://www.ahrq.gov/health-literacy/research/tools/index.html#short (accessed on 9 July 2023).
[93] Ammentorp, J. et al. (2021), “Upscaling communication skills training – lessons learned from international initiatives”, Patient Education and Counseling, Vol. 104/2, pp. 352-359, https://doi.org/10.1016/j.pec.2020.08.028.
[71] Arrighi, E. et al. (2021), “Scoping health literacy in Latin America”, Global Health Promotion, Vol. 29/2, pp. 78-87, https://doi.org/10.1177/17579759211016802.
[6] Australian Government - Department of Health (2021), National Preventive Health Strategy, https://www.health.gov.au/sites/default/files/documents/2021/12/national-preventive-health-strategy-2021-2030_1.pdf (accessed on 13 July 2023).
[25] Baker, D. (2007), “Health literacy and mortality among elderly persons”, Archives of Internal Medicine, Vol. 167/14, p. 1503, https://doi.org/10.1001/archinte.167.14.1503.
[48] Baker, D. et al. (2002), “Functional health literacy and the risk of hospital admission among Medicare managed care enrollees”, American Journal of Public Health, Vol. 92/8, pp. 1278-1283, https://doi.org/10.2105/ajph.92.8.1278.
[55] Bazrafkan, L. et al. (2018), “Investigating the effect of education on health literacy and its relation to health-promoting behaviors in health center”, Journal of Education and Health Promotion, Vol. 7/1, p. 127, https://doi.org/10.4103/jehp.jehp_65_18.
[49] Berens, E. et al. (2016), “Health literacy among different age groups in Germany: results of a cross-sectional survey”, BMC Public Health, Vol. 16/1, https://doi.org/10.1186/s12889-016-3810-6.
[2] Berkman, N. et al. (2011), “Low health literacy and health outcomes: An updated systematic review”, Annals of Internal Medicine, Vol. 155/2, p. 97, https://doi.org/10.7326/0003-4819-155-2-201107190-00005.
[57] Bertakis, K. et al. (2000), “Gender differences in the utilization of health care services”, Journal of Family Practice, Vol. 49/2, pp. 147-152, https://pubmed.ncbi.nlm.nih.gov/10718692/.
[104] Bundesministerium für Gesundheit (n.d.), Allianz für Gesundheitskompetenz (Alliance for Health Literacy), https://www.bundesgesundheitsministerium.de/gesundheitskompetenz/allianz-fuer-gesundheitskompetenz.html (accessed on 28 June 2023).
[84] Bundesministerium für Gesundheit und Frauen (2017), Gesundheitsziele Österreich: Richtungsweisende Vorschläge für ein gesünderes Österreich – Langfassung (Health Targets Austria: Trend-setting Proposals for a Healthier Austria - Long version), https://gesundheitsziele-oesterreich.at/website2017/wp-content/uploads/2018/08/gz_langfassung_2018.pdf.
[83] Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz (2022), Austrian Health Targets, https://gesundheitsziele-oesterreich.at/english-summary/.
[79] Canadian Council on Learning (2008), Health Literacy in Canada: A Healthy Understanding, https://escholarship.org/uc/item/890661nm (accessed on 5 July 2023).
[42] Cavanaugh, K. (2011), “Health literacy in diabetes care: Explanation, evidence and equipment”, Diabetes Management, Vol. 1/2, pp. 191-199, https://doi.org/10.2217/dmt.11.5.
[5] Centers for Disease Control and Prevention (2010), National Action Plan to Improve Health Literacy, https://www.cdc.gov/healthliteracy/planact/national.html (accessed on 13 July 2023).
[65] Chaudhry, S. et al. (2011), “Racial disparities in health literacy and access to care among patients with heart failure”, Journal of Cardiac Failure, Vol. 17/2, pp. 122-127, https://doi.org/10.1016/j.cardfail.2010.09.016.
[69] Cheng, J. and M. Nishikawa (2022), “Effects of health literacy in the fight against the COVID-19 infodemic: The case of Japan”, Health Communication, Vol. 37/12, pp. 1520-1533, https://doi.org/10.1080/10410236.2022.2065745.
[78] Choudhry, F. et al. (2019), “Health Literacy Studies Conducted in Australia: A Scoping Review”, International Journal of Environmental Research and Public Health, Vol. 16/7, p. 1112, https://doi.org/10.3390/ijerph16071112.
[76] Coelho, M. et al. (2014), “Functional health literacy and healthy eating: Understanding the brazilian food guide recommendations”, Revista de Nutrição, Vol. 27/6, pp. 715-723, https://doi.org/10.1590/1415-52732014000600006.
[61] Criado Perez, C. (2019), Invisible Women: Data Bias in a World Designed for Men, Abrams Press.
[116] Department of Health Ireland (2021), Health Research and Statistics, https://www.gov.ie/en/collection/3c5bc8-health-research-and-statistics/#behavioural-insights-and-patient-public-engagement.
[113] Department of Health Ireland (2021), Sláintecare Implementation Strategy and Action Plan 2021-2023, https://www.gov.ie/en/publication/6996b-slaintecare-implementation-strategy-and-action-plan-2021-2023/.
[112] Department of Health Ireland (2019), Sláintecare Action Plan 2019, https://assets.gov.ie/22606/4e13c790cf31463491c2e878212e3c29.pdf.
[110] Department of Health Ireland (2013), Healthy Ireland: A Framework for Improved Health and Wellbeing 2013-2025, https://www.hse.ie/eng/services/publications/corporate/hienglish.pdf.
[81] Dietscher, C., P. Nowak and J. Pelikan (2020), “Health Literacy in Austria: Interventions and Research”, in Studies in Health Technology and Informatics, https://doi.org/10.3233/SHTI200032.
[124] Dublin City University (2020), What are DEIS Schools?, https://www.dcu.ie/access/what-are-deis-schools.
[106] Ernstmann, N. et al. (2020), “DNVF Memorandum Gesundheitskompetenz (Teil 1) – Hintergrund (DNVF Memorandum Health Literacy (Part 1) – Background, Relevance, Research Topics and Questions in Health Services Research)”, Das Gesundheitswesen, Vol. 82/07, pp. e77-e93, https://doi.org/10.1055/a-1191-3689.
[36] Griebler, R., C. Dietscher and E. Flaschberger (2022), “Gesundheitskompetenz in Zeiten von Corona und COVID-19: Ergebnisse aus Österreich [Health literacy in times of Corona and COVID-19: Results from Austria]”, in Gesundheitskompetenz, Springer Reference Pflege – Therapie – Gesundheit, Springer Berlin Heidelberg, Berlin, Heidelberg, https://doi.org/10.1007/978-3-662-62800-3_85-1.
[91] Griebler, R. et al. (2021), Gesundheitskompetenz in Österreich: Ergebnisse der österreichischen Gesundheitskompetenzerhebung HLS19-AT (Health literacy in Austria: Results of the Austrian Health Literacy Survey HLS19-AT), https://oepgk.at/wp-content/uploads/2021/08/hls19-at-bericht-bf.pdf.
[21] Griese, L. et al. (2020), “Challenges in Navigating the Health Care System: Development of an Instrument Measuring Navigation Health Literacy”, International Journal of Environmental Research and Public Health, Vol. 17/16, p. 5731, https://doi.org/10.3390/ijerph17165731.
[22] Griese, L. et al. (2022), “HLS19-NAV—Validation of a new instrument measuring navigational health literacy in eight European countries”, International Journal of Environmental Research and Public Health, Vol. 19/21, p. 13863, https://doi.org/10.3390/ijerph192113863.
[68] Griese, L., D. Schaeffer and E. Berens (2022), “Navigational health literacy among people with chronic illness”, Chronic Illness, Vol. 19/1, pp. 172-183, https://doi.org/10.1177/17423953211073368.
[111] Healthy Ireland (2021), Healthy Ireland Strategic Action Plan 2021-2025, https://www.gov.ie/en/publication/441c8-healthy-ireland-strategic-action-plan-2021-2025/.
[4] Heijmans, M. et al. (2015), Study on Sound Evidence for a Better Understanding of Health Literacy in the European Union: Final Report, European Commission, Publications Office, https://doi.org/10.2818/150402.
[29] Herndon, J., M. Chaney and D. Carden (2011), “Health literacy and emergency department outcomes: A systematic review”, Annals of Emergency Medicine, Vol. 57/4, pp. 334-345, https://doi.org/10.1016/j.annemergmed.2010.08.035.
[118] HIQA (2015), Communicating in Plain English, https://www.hiqa.ie/hiqa-news-updates/hiqa-publishes-guidance-aimed-improving-communication-health-and-social-care.
[82] HLS-EU-Consortium (2012), Comparative Report on Health Literacy in Eight EU Member States, http://cpme.dyndns.org/adopted/2015/Comparative_report_on_health_literacy_in_eight_EU_member_states.pdf.
[114] Irish Heart Foundation (2021), Irish Heart Foundation brings health literacy to global stage, https://irishheart.ie/news/irish-heart-foundation-brings-health-literacy-to-global-stage/.
[43] Jain, D. and J. Green (2016), “Health literacy in kidney disease: Review of the literature and implications for clinical practice”, World Journal of Nephrology, Vol. 5/2, p. 147, https://doi.org/10.5527/wjn.v5.i2.147.
[98] Jordan, S. and J. Hoebel (2015), “Gesundheitskompetenz von Erwachsenen in Deutschland (Health literacy of adults in Germany)”, Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, Vol. 58/9, pp. 942-950, https://doi.org/10.1007/s00103-015-2200-z.
[58] Kalseth, J. and T. Halvorsen (2020), “Health and care service utilisation and cost over the life-span: A descriptive analysis of population data”, BMC Health Services Research, Vol. 20/1, https://doi.org/10.1186/s12913-020-05295-2.
[88] Kerschner, B. et al. (2015), “Wie evidenzbasiert berichten Print- und Online-Medien in Österreich? Eine quantitative Analyse (How evidence-based are print- and online mass media in Austria? A quantitative analysis)”, Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen, Vol. 109/4-5, pp. 341-349, https://doi.org/10.1016/j.zefq.2015.05.014.
[28] Kim, H. and B. Xie (2017), “Health literacy in the eHealth era: A systematic review of the literature”, Patient Education and Counseling, Vol. 100/6, pp. 1073-1082, https://doi.org/10.1016/j.pec.2017.01.015.
[75] Konfino, J. et al. (2009), “Alfabetización en salud en pacientes que asisten a un hospital universitario [Health literacy in patients attending a university hospital]”, Medicina (B Aires), http://www.scielo.org.ar/scielo.php?pid=S0025-76802009000700007&script=sci_arttext&tlng=pt (accessed on 7 July 2023).
[50] Kutner, M. et al. (2006), The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy, National Center for Educational Statistics (ED), Washington, DC and American Institutes for Research (CRESS), Kensington, MD, https://eric.ed.gov/?id=ED493284.
[59] Lee, H., J. Lee and N. Kim (2014), “Gender differences in health literacy among Korean adults”, American Journal of Men’s Health, Vol. 9/5, pp. 370-379, https://doi.org/10.1177/1557988314545485.
[74] Lee, S. et al. (2006), “Development of an Easy-to-Use Spanish Health Literacy Test”, Health Services Research, Vol. 0/0, pp. 060720074824046-???, https://doi.org/10.1111/j.1475-6773.2006.00532.x.
[39] Llena-Nozal, A., N. Martin and F. Murtin (2019), “The economy of well-being: Creating opportunities for people’s well-being and economic growth”, OECD Statistics Working Papers, No. 2019/02, OECD Publishing, Paris, https://doi.org/10.1787/498e9bc7-en.
[107] Lühnen, J. et al. (2017), Leitlinie evidenzbasierte Gesundheitsinformation [Guideline evidence-based health information], https://www.leitlinie-gesundheitsinformation.de/wp-content/uploads/2017/07/Leitlinie-evidenzbasierte-Gesundheitsinformation.pdf (accessed on 28 June 2023).
[53] Manafo, E. and S. Wong (2012), “Health literacy programs for older adults: A systematic literature review”, Health Education Research, Vol. 27/6, pp. 947-960, https://doi.org/10.1093/her/cys067.
[1] Mancuso, J. (2009), “Assessment and measurement of health literacy: An integrative review of the literature”, Nursing & Health Sciences, Vol. 11/1, pp. 77-89, https://doi.org/10.1111/j.1442-2018.2008.00408.x.
[45] Mancuso, J. (2008), “Health literacy: A concept/dimensional analysis”, Nursing & Health Sciences, Vol. 10/3, pp. 248-255, https://doi.org/10.1111/j.1442-2018.2008.00394.x.
[3] Mårtensson, L. and G. Hensing (2011), “Health literacy - a heterogeneous phenomenon: A literature review”, Scandinavian Journal of Caring Sciences, Vol. 26/1, pp. 151-160, https://doi.org/10.1111/j.1471-6712.2011.00900.x.
[72] Mávita-Corral, C. (2017), “Alfabetización en salud de una comunidad universitaria del noroeste de México en el año 2016”, Investigación en Educación Médica, https://doi.org/10.1016/j.riem.2017.03.002.
[122] Ministério da Saúde (2021), Literacia em saúde e comunicação na promoção da adesão à vacinação contra a COVID-19 (Health and communication literacy in promoting adherence to vaccination against COVID-19), https://www.dgs.pt/documentos-e-publicacoes/dgs-publicanbspmanual-sobre-literacia-para-promover-a-adesao-a-vacinacao.aspx.
[121] Ministério da Saúde (2020), Health Literacy and COVID-19 in Portugal: Plan, Practice and Challenges, https://www.dgs.pt/documentos-e-publicacoes/literacia-em-saude-e-a-covid-19-plano-pratica-e-desafios-pdf.aspx.
[120] Ministério da Saúde (2019), Manual de Boas Práticas Literacia em Saúde: Capacitação dos Profissionais de Saúde (Good Practice Guide Health Literacy: Building Capacity among Health Professionals), https://doi.org/10.13140/RG.2.2.17763.30243.
[119] Ministério da Saúde (2018), Health Literacy Action Plan Portugal 2019-2021, https://www.dgs.pt/documentos-e-publicacoes/plano-de-acao-para-a-literacia-em-saude-2019-2021-pdf.aspx.
[80] Mood, C. (2009), “Logistic regression: Why we cannot do what we think we can do, and what we can do about it”, European Sociological Review, Vol. 26/1, pp. 67-82, https://doi.org/10.1093/esr/jcp006.
[18] Moreira, L. (2018), “Health literacy for people-centred care: Where do OECD countries stand?”, OECD Health Working Papers, No. 107, OECD Publishing, Paris, https://doi.org/10.1787/d8494d3a-en.
[14] Morrow, D. et al. (2006), “Correlates of health literacy in patients with chronic heart failure”, The Gerontologist, Vol. 46/5, pp. 669-676, https://doi.org/10.1093/geront/46.5.669.
[17] Nakayama, K. et al. (2015), “Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy”, BMC Public Health, Vol. 15/1, https://doi.org/10.1186/s12889-015-1835-x.
[117] NALA (2021), A Guide to Becoming a Crystal Clear Pharmacy, https://www.nala.ie/publications/the-crystal-clear-pharmacy-programme-and-its-crystal-clear-mark/.
[101] Nationaler Aktionsplan Gesundheitskompetenz Geschäftsstelle (2020), 15 konkrete Empfehlungen, um die Gesundheitskompetenz zu stärken (15 concrete recommendations to strengthen health literacy), https://www.nap-gesundheitskompetenz.de/aktionsplan/ (accessed on 9 February 2023).
[37] Nearchou, F. et al. (2022), “Health literacy of COVID-19 and compliance with precautionary measures: A cross-sectional study in adolescents and young adults in Ireland”, Youth, Vol. 2/2, pp. 165-180, https://doi.org/10.3390/youth2020013.
[41] Nielsen-Bohlman, L., A. Panzer and D. Kindig (eds.) (2004), Health Literacy: A Prescription to End Confusion, National Academies Press, Washington, DC, https://doi.org/10.17226/10883.
[11] OECD (2017), “Ministerial Statement”, The Next Generation of Health Reforms, OECD Health Ministerial Meeting, https://www.oecd.org/health/ministerial-statement-2017.pdf (accessed on 23 March 2022).
[108] Okan, O. et al. (2021), Gesundheitskompetenz und Schule. Entwicklung von 100 Leuchtturmschulenbis zum Jahr 2025. Ein Visionspapier [Health literacy and school. Development of 100 lighthouse schools by 2025. A vision paper], https://fuldok.hs-fulda.de/opus4/frontdoor/deliver/index/docId/892/file/Allianz_GK_und_Schule-Vision2025_Stand210223.pdf (accessed on 28 June 2023).
[85] Österreichische Plattform Gesundheitskompetenz (2022), About the Alliance, https://oepgk.at/english-summary-about-the-alliance/.
[95] Österreichische Plattform Gesundheitskompetenz (2022), Bürger- und Patientenempowerment [Citizen and patient empowerment], https://oepgk.at/buerger-und-patientenempowerment/.
[92] Österreichische Plattform Gesundheitskompetenz (2022), Gute Gesprächsqualität im Gesundheitssystem (High-quality talks in the health system), https://oepgk.at/gute-gespraechsqualitaet-im-gesundheitssystem/#quellen.
[89] Österreichische Plattform Gesundheitskompetenz (2022), Gute Gesundheitsinformation Österreich (Good Health Information Austria), https://oepgk.at/gute-gesundheitsinformation-oesterreich/.
[86] Österreichische Plattform Gesundheitskompetenz (2022), Messung der Gesundheitskompetenz (Health literacy measurement), https://oepgk.at/messung-der-gesundheitskompetenz/.
[97] Österreichische Plattform Gesundheitskompetenz (2022), Rahmenbedingungen in Organisationen und Settings (Framework conditions in organisations and settings), https://oepgk.at/rahmenbedingungen-in-organisationen-und-settings/.
[90] Österreichische Plattform Gesundheitskompetenz (2020), Gute Gesundheitsinformation Österreich: Die 15 Qualitätskriterien (Good Health Information Austria: The 15 Quality Criteria), https://oepgk.at/wp-content/uploads/2020/12/2020_11_18_die-gute-gesundheitsinformation.pdf.
[44] Oxley, H. (2009), “Policies for healthy ageing: An overview”, OECD Health Working Papers, No. 42, OECD Publishing, Paris, https://doi.org/10.1787/226757488706.
[26] Paasche-Orlow, M. and M. Wolf (2007), “The causal pathways linking health literacy to health outcomes”, American Journal of Health Behavior, Vol. 31/Suppl 1, pp. S19-S26, https://doi.org/10.5555/ajhb.2007.31.supp.S19.
[24] Parker, R. (2009), “Measuring Health Literacy: What? So What? Now What?”, in Measures of Health Literacy: Workshop Summary, Institute of Medicine Roundtable on Health Literacy, National Academies Press, Washington, DC, https://www.ncbi.nlm.nih.gov/books/NBK45386/.
[15] Parker, R. and S. Ratzan (2010), “Health literacy: A second decade of distinction for Americans”, Journal of Health Communication, Vol. 15/sup2, pp. 20-33, https://doi.org/10.1080/10810730.2010.501094.
[20] Pelikan, J. et al. (2022), “Measuring Comprehensive, General Health Literacy in the General Adult Population: The Development and Validation of the HLS19-Q12 Instrument in Seventeen Countries”, International Journal of Environmental Research and Public Health, Vol. 19/21, p. 14129, https://doi.org/10.3390/ijerph192114129.
[87] Pelikan, J., F. Röthlin and K. Ganahl (2013), Die Gesundheitskompetenz der österreichischen Bevölkerung nach Bundesländern und im internationalen Vergleich (Health literacy of the Austrian population by province and in international comparison), https://fgoe.org/sites/fgoe.org/files/project-attachments/Gesundheitskompetenz_Bundesl%C3%A4nder_%C3%96ffentlich.pdf.
[40] Quaglio, G. et al. (2016), “Accelerating the health literacy agenda in Europe”, Health Promotion International, p. daw028, https://doi.org/10.1093/heapro/daw028.
[63] Quenzel, G. (2017), “Health Literacy und Gesundheitsverhalten vulnerabler Bevölkerungsgruppen [Health literacy and health behavior of vulnerable population groups]”, in Doris Schaeffer, J. (ed.), Health Literacy: Forschungsstand und Perspektiven, Hogrefe.
[33] Rasu, R. et al. (2015), “Health Literacy Impact on National Healthcare Utilization and Expenditure”, International Journal of Health Policy and Management, Vol. 4/11, pp. 747-755, https://doi.org/10.15171/ijhpm.2015.151.
[32] Rondia, K. et al. (2019), Health Literacy: What Lessons Can Be Learned from the Experiences of Other Countries?, Belgian Health Care Knowledge Centre, https://kce.fgov.be/sites/default/files/2021-11/KCE_322_Health_Literacy_Report_0.pdf.
[62] Samulowitz, A. et al. (2018), “’Brave men’ and ’emotional women’: A theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain”, Pain Research and Management, Vol. 2018, pp. 1-14, https://doi.org/10.1155/2018/6358624.
[94] Sator, M., P. Holler and M. Rosenbaum (2021), “National train-the-trainer certificate programme for improving healthcare communication in Austria”, Patient Education and Counseling, Vol. 104/12, pp. 2857-2866, https://doi.org/10.1016/j.pec.2021.07.046.
[105] Schaefer, C. and G. Ollenschläger (2019), Deutsches Netzwerk Gesundheitskompetenz DNGK - Ein Forum für Forscher und die Öffentlichkeit [German Health Competence Network DNGK - A forum for researchers and the public], QUALITAS, https://dngk.de/wp-content/uploads/2022/03/dngk-qualitas-2019-01.pdf (accessed on 28 June 2023).
[9] Schaeffer, D. and S. Gille (2021), “Gesundheitskompetenz im Zeitalter der Digitalisierung (Health literacy in the digital age: Where do we stand?)”, Prävention und Gesundheitsförderung, Vol. 17/2, pp. 147-155, https://doi.org/10.1007/s11553-021-00872-7.
[102] Schaeffer, D., S. Gille and K. Hurrelmann (2020), “Implementation of the National Action Plan Health Literacy in Germany - Lessons learned”, International Journal of Environmental Research and Public Health, Vol. 17/12, p. 4403, https://doi.org/10.3390/ijerph17124403.
[13] Schaeffer, D. et al. (2021), “National Action Plan Health Literacy in Germany origin, development and structure”, Journal of Public Health, https://doi.org/10.1007/s10389-021-01616-9.
[109] Schaeffer, D., A. Haarmann and L. Griese (2023), Professionelle Gesundheitskompetenz ausgewählter Gesundheitsprofessionen in Deutschland [Professional health competence of selected health professionals in Germany], https://www.stiftung-gesundheitswissen.de/sites/default/files/2023-06/2023_06_20_Ergebnisbericht_Studie_professionelle_Gesundheitskompetenz.pdf (accessed on 28 June 2023).
[103] Schaeffer, D. et al. (2022), Deutschland braucht mehr Gesundheitskompetenz. Ein Plädoyer von Autorinnen und Autoren des „Nationalen Aktionsplan Gesundheitskompetenz“ [Germany needs more health literacy. A plea from the authors of the “National Health Literacy Action Plan”], https://oepgk.at/wp-content/uploads/2022/02/pladoyer-fur-mehr-gesundheitskompetenz.pdf (accessed on 28 June 2023).
[100] Schaeffer, D. et al. (2018), National Action Plan Health Literacy: Promoting Health Literacy in Germany, http://www.hlca-consortium.de/wp-content/uploads/2018/06/National-Action-Plan-Health-Literacy.pdf.
[27] Schaeffer, D. and J. Pelikan (eds.) (2017), Chronische Krankheit und Health Literacy [Chronic Illness and Health Literacy], Hogrefe.
[99] Schaeffer, D. et al. (2016), Gesundheitskompetenz der Bevölkerung in Deutschland - Ergebnisbericht (Health literacy of the population in Germany - Results report), Universität Bielefeld, https://doi.org/10.2390/0070-pub-29081112.
[66] Schillinger, D. (2020), “The intersections between social determinants of health, health literacy, and health disparities”, in Health Literacy in Clinical Practice and Public Health, https://doi.org/10.3233/SHTI200020.
[96] Schmotzer, C. and P. Nowak (2021), Aufwertung von Patientenrechten zur Unterstützung von Gesundheitskompetenz (Upgrading patients’ rights to support health literacy), https://oepgk.at/wp-content/uploads/2021/07/bericht-der-osterreichischen-plattform-gesundheitskompetenz.pdf.
[67] Sentell, T. and H. Halpin (2006), “Importance of adult literacy in understanding health disparities”, Journal of General Internal Medicine, Vol. 21/8, pp. 862-866, https://doi.org/10.1111/j.1525-1497.2006.00538.x.
[30] Seo, J. et al. (2016), “Effect of health literacy on decision-making preferences among medically underserved patients”, Medical Decision Making, Vol. 36/4, pp. 550-556, https://doi.org/10.1177/0272989x16632197.
[38] Silva, M. and P. Santos (2021), “The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: A cross-sectional study”, International Journal of Environmental Research and Public Health, Vol. 18/10, p. 5421, https://doi.org/10.3390/ijerph18105421.
[16] Sørensen, K. et al. (2015), “Health literacy in Europe: Comparative results of the European Health Literacy Survey (HLS-EU)”, The European Journal of Public Health, Vol. 25/6, pp. 1053-1058, https://doi.org/10.1093/eurpub/ckv043.
[23] Sørensen, K. et al. (2012), “Health literacy and public health: A systematic review and integration of definitions and models”, BMC Public Health, Vol. 12/1, https://doi.org/10.1186/1471-2458-12-80.
[77] Sørensen, K. et al. (2013), “Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q)”, BMC Public Health, Vol. 13/1, https://doi.org/10.1186/1471-2458-13-948.
[54] Speros, C. (2009), “More than words: Promoting health literacy in older adults”, The Online Journal of Issues in Nursing, Vol. 14/3, https://doi.org/10.3912/ojin.vol14no03man05.
[46] Speros, C. (2005), “Health literacy: Concept analysis”, Journal of Advanced Nursing, Vol. 50/6, pp. 633-640, https://doi.org/10.1111/j.1365-2648.2005.03448.x.
[60] Sudore, L. et al. (2006), “Limited literacy in older people and disparities in health and healthcare access”, Journal of the American Geriatrics Society, Vol. 54/5, pp. 770-776, https://doi.org/10.1111/j.1532-5415.2006.00691.x.
[19] The HLS19 Consortium of the WHO Action Network M-POHL (2021), International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL, https://m-pohl.net/sites/m-pohl.net/files/inline-files/HLS19%20International%20Report.pdf.
[123] The National Treatment Purchase Fund (2023), Waiting List Validation, https://www.ntpf.ie/home/Waiting_List_Validation.htm (accessed on 2023).
[35] Van den Broucke, S. (2014), “Health literacy: A critical concept for public health”, Archives of Public Health, Vol. 72/1, https://doi.org/10.1186/2049-3258-72-10.
[56] Van der Heide, I. et al. (2013), “Health literacy of Dutch adults: A cross-sectional survey”, BMC Public Health, Vol. 13/1, https://doi.org/10.1186/1471-2458-13-179.
[34] Vernon, J. et al. (2007), Low Health Literacy: Implications for National Health Policy, Department of Health Policy, School of Public Health and Health Services, George Washington University, https://publichealth.gwu.edu/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_4_07.pdf.
[51] Vogt, D., D. Schaeffer and E. Berens (2019), “Health literacy in later phases of life. Findings from Germany and other countries”, in Orkan O, B. (ed.), International Handbook of Health Literacy. Research, practice and policy across the life span, https://doi.org/10.51952/9781447344520.013.
[70] Weishaar, H. et al. (2019), “Framing health literacy: A comparative analysis of national action plans”, Health Policy, Vol. 123/1, pp. 11-20, https://doi.org/10.1016/j.healthpol.2018.11.012.
[31] Weiss, B. and R. Palmer (2004), “Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population”, The Journal of the American Board of Family Medicine, Vol. 17/1, pp. 44-47, https://doi.org/10.3122/jabfm.17.1.44.
[12] WHO (2022), Health Literacy Development for the Prevention and Control of Noncommunicable Diseases, Volume I: Overview, World Health Organization, https://www.who.int/publications/i/item/9789240055339.
[115] WHO (2019), Acting Together – WHO National Health Literacy Demonstration Projects (NHLDPs) Address Health Literacy Needs in the European Region, World Health Organization, https://apps.who.int/iris/bitstream/handle/10665/327059/php-5-2-3-233-243-eng.pdf?sequence=1&isAllowed=y.
[10] WHO (2019), Draft WHO European Roadmap for Implementation of Health, World Health Organization, https://www.euro.who.int/__data/assets/pdf_file/0003/409125/69wd14e_Rev1_RoadmapOnHealthLiteracy_190323.pdf.
[8] WHO (2016), Promoting Health in the SDGs: Report on the 9th Global Conference for Health Promotion, World Health Organization, https://www.who.int/publications/i/item/WHO-NMH-PND-17.5.
[7] WHO (2013), Health 2020: A European Policy Framework and Strategy for the 21st Century, World Health Organization, https://www.euro.who.int/__data/assets/pdf_file/0011/199532/Health2020-Long.pdf.
[64] WHO (2013), Health Literacy: The Solid Facts, World Health Organization, https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf?sequence=1&isAllowed=y.
[47] Wilson, K. (2001), Promoting Health Literacy, Clemson Univ., SC. Inst. on Family and Neighborhood Life, https://eric.ed.gov/?id=ED466621.
[52] Zamora, H. and E. Clingerman (2011), “Health literacy among older adults: A systematic literature review”, Journal of Gerontological Nursing, Vol. 37/10, pp. 41-51, https://doi.org/10.3928/00989134-20110503-02.
Notes
← 1. “General health literacy” refers to health literacy more broadly, as opposed to specific types of healthy literacies, such as digital health literacy or vaccination health literacy.
← 2. The ten Austrian health targets are: 1) to provide health-promoting living and working conditions for all population groups through co‑operation of all societal and political areas; 2) to promote fair and equal opportunities in health, irrespective of gender, socio-economic group, ethnic origin and age; 3) to enhance health literacy in the population; 4) to secure sustainable natural resources such as air, water and soil and healthy environments for future generations; 5) to strengthen social cohesion as a health enhancer; 6) to ensure conditions under which children and young people can grow up as healthy as possible; 7) to provide access to a healthy diet for all; 8) to promote healthy, safe exercise and activity in everyday life through appropriate environments; 9) to promote psychosocial health in all population groups; and 10) to secure sustainable and efficient healthcare services of high quality for all.
← 5. “Delivering Equality of Opportunity in Schools (DEIS), the Action Plan for Educational Inclusion, was launched by the Department of Education and Skills in May 2005. The plan focuses on addressing the educational needs of children and young people from disadvantaged communities, from pre-school through second-level education (3 to 18 years). Some 852 primary level and second level schools in Ireland are included in the DEIS initiative. Of these, 658 are primary schools while 194 are secondary schools.” (Dublin City University, 2020[124]).
← 6. LifeLab is a purpose-built educational laboratory showing young teenagers how their lifestyles may affect their future heart health; see www.bhf.org.uk/informationsupport/heart-matters-magazine/research/lifelab.
← 7. “The validation of waiting lists is a process whereby the accuracy of waiting lists is checked by asking patients whether they still require their procedure.” (The National Treatment Purchase Fund, 2023[123]).