Yevgeniy Goryakin
Sabine Vuik
Michele Cecchini

Yevgeniy Goryakin
Sabine Vuik
Michele Cecchini
Overweight is a serious public health problem requiring a co-ordinated, multi-sectoral response. This chapter provides a broad overview of existing policy approaches, both national and international, aimed at improving diet and encouraging physical activity in OECD, EU28 and Group of 20 (G20) countries. Particular attention is paid to policies that are either innovative, or have a solid evidence base for their effectiveness, including policies that aim to influence lifestyle choices through information and education; policies that expand healthy choice options; policies designed to modify the costs of health-related choices, and policies aimed at regulating or restricting unhealthy options. Both the opportunities presented by the introduction of the selected policies, as well as the challenges associated with their implementation, are discussed.
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
All the countries considered in this analysis, except one, currently have a national action plan to address adult overweight; seven countries do not yet have a national childhood obesity plan.
A large majority of countries already implement mandatory back-of-pack nutrition labelling, but only four countries have implemented front-of-pack labelling, which is recognised as the most effective option. There is still a lack of action in such areas as mandatory labelling of restaurant menus.
Many countries strictly regulate content of certain harmful foods (e.g., trans fats and partially hydrogenated oils). Four countries have implemented taxation of foods high in calories, in particular sugar-sweetened beverages.
Only a few countries have implemented compulsory restrictions for advertising that target children, with the majority of countries having voluntary regulations in place.
More needs to be done to promote physical activity and a healthy diet in primary care, especially among those at risk for developing overweight-related non-communicable diseases (NCDs). About one in three OECD countries have such a policy in place, but a number of challenges may hinder its effectiveness.
A number of innovative policies have emerged recently. Several countries have taken advantage of both traditional and new media to implement mass media campaigns to promote healthy lifestyles.
Recognising the importance of a healthy workforce, a limited number of public and private sector employers have started to implement various workplace wellness programmes on their premises. However, such interventions can be expensive, and a cost-effectiveness analysis for them (preferably taking into account productivity benefits) should be undertaken.
A number of improvements in urban infrastructure with the potential of benefiting both human health and the environment have been implemented. These include introducing cycle lanes and bike-sharing schemes; increasing public transport options and expanding the amount of green space However, more cross-sectoral co-operation is needed, as policies originating from other sectors may have a significant impact on population health.
In an attempt to tackle some of the key social and environmental determinants of overweight1 and its underlying unhealthy lifestyles, countries around the world have significantly up-scaled their policy actions. At an international level, greater impetus for action was initiated in 2011 with the first United Nations (UN) High-level Meeting on non-communicative diseases (NCDs), and continued with the adoption of an internationally agreed set of commitments and targets (Box 5.1). At a national level, the fight against overweight has advanced mainly around national action plans, sometimes developed based on the World Health Organization’s (WHO) Global Strategy on Diet, Physical Activity and Health and other relevant global action plans.
Since the early 2000s, there has been increasing recognition of the importance of overweight-related NCDs as a determinant of sustainable human development, as well as of the need for international co-operation to tackle the burden of NCDs. Action in this field has significantly intensified since 2011, with the first UN High-level Meeting on NCDs. Following the UN High-level Meeting, countries have committed to achieving a number of targets and goals indicated below. Previous OECD analysis concluded that reaching these targets would produce significant economic benefits (Devaux et al., 2019[1]).
2011: the United Nations General Assembly adopts a declaration calling to go beyond health system strengthening and to address the social determinants of health, including preventing exposure to risk factors for NCDs.
2013: the NCD Global Action plan is adopted by WHO, aiming to increase priority for actions to prevent and control NCDs locally and internationally. Six objectives were established, including initiatives to strengthen national capacity, governance, multi-sectoral action, health-promoting environments, people-centred primary health care and universal health coverage.
2013: countries agree a set of voluntary targets for risk factor reduction by 2025 compared to baseline levels in 2010, in the framework of the "Global monitoring framework on NCDs" which tracks the implementation of the WHO NCD Global Action Plan, including:
a 25% relative reduction in the overall mortality from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases
halting the rise in diabetes and obesity
a 10% relative reduction in prevalence of insufficient physical activity
a 25% relative reduction in the prevalence of raised blood pressure.
2015: Sustainable Development Goals (SDGs) are adopted, including a target to reduce premature mortality by one-third by 2030.
2018: A Global Action Plan on Physical Activity is agreed by WHO, including a target of a 15% relative reduction by 2030, using the baseline of 2016, in the global prevalence of physical inactivity in adults and adolescents.
Virtually all the OECD, EU28 and G20 countries have comprehensive policy frameworks to tackle major determinants of overweight. As of 2019, all countries included in this analysis, but one, have adopted a national action plan to address adult obesity. Seven countries so far have not implemented national obesity strategies specifically aimed at children. In many cases, countries have also developed national guidelines to promote physical activity and multi-sectoral nutritional plans, with the latter present in all the reviewed countries (Figure 5.1)2.
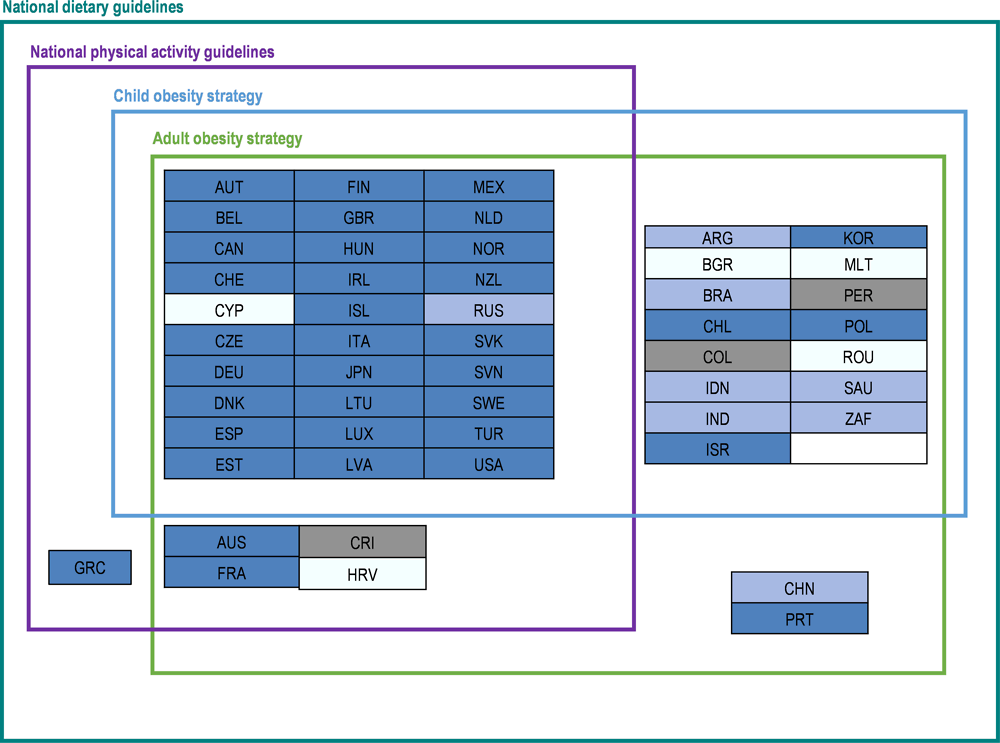
Note: OECD countries in dark blue; other G20 non-OECD countries in light blue; other EU non-OECD countries in white; other countries partnering with the OECD in grey.
Source: WCRFI (2016[2]), “NOURISHING-framework” http://www.wcrf.org/int/policy/nourishing-framework; Development Initiatives (2018[3]), 2018 Global Nutrition Report: Shining a light to spur action on nutrition, https://globalnutritionreport.org/d7447a; WHO (2012[4]), Global database on the Implementation of Nutrition Action (GINA), https://www.who.int/nutrition/gina/en/; WHO (2018[5]), “Physical activity country factsheets”, http://www.euro.who.int/en/health-topics/disease-prevention/physical-activity/data-and-statistics/physical-activity-fact-sheets/physical-activity-country-fact-sheets.
While the vast majority of countries do have national plans, their portfolios of actual policy responses, as well as the level of implementation vary a lot, giving scope to further upscale action at a country level. This chapter reviews the existing national policy landscape, placing a particular focus on a limited set of policies that are either recognised as particularly innovative, or for which there is a well-developed body of evidence on their effectiveness.
In line with the OECD framework (Sassi and Hurst, 2008[6]), public health policies, including policies to tackle overweight and to promote healthier lifestyles can be categorised into the following four broad groups (also see Figure 5.2):
policies influencing lifestyles through information and education
policies widening the set of healthy choice options
policies modifying the cost of health-related choices, and
policies regulating or restricting actions promoting unhealthy choice options.
While some policies may be very effective, none of them is sufficient in isolation. For example, policy actions aiming to influence lifestyle choices through information or education are important, but not sufficient for someone living in a community where it is difficult to purchase healthy foods, or where exercise options are limited. In such cases, action plans to widen the set of healthy options are essential, such as the provision of certain infrastructure or food retail improvements. Lifestyles can also be influenced by the marketing of calorie-dense and/or ultra-processed foods, regardless of where one lives. Therefore, a certain amount of regulation may be needed, for example in the form of limiting marketing practices (especially advertising targeting children), taxation or even banning certain foods or nutrients (e.g. trans fats).
However, even these policies may not be sufficient unless other causes of the recent increase in overweight rates are addressed, such as rising income inequality or poverty (Pickett et al., 2005[7]; Drewnowski and Specter, 2004[8]). At the very least, such policies should pay particular attention to the needs of the lower socio-economic status (SES) groups, who are often the least resilient to the influence of the obesogenic environments in which they live.
Source: Broadly based on Sassi and Hurst (2008[6]), “The Prevention of Lifestyle-Related Chronic Diseases: an Economic Framework”, https://dx.doi.org/10.1787/243180781313.
Note: The policy actions shown in this figure are only examples, and do not aim to represent all the options that could be implemented by countries.
Both population-level and targeted polices are needed to address the underlying causes of overweight. The former group includes interventions affecting different population groups without distinction, such as food labelling or environmental changes including, for example, those following the implementation of a regulation. On the other hand, targeted policies aim to affect a distinct population group, particularly those at higher risk for developing chronic diseases, such as high-risk individuals in working-age populations, or those needing primary care, or with a particularly high risk of developing overweight. Of great interest are policies designed to protect children, who are particularly vulnerable to outside influences such as advertising, which may affect their preferences well into adulthood (Connell, Brucks and Nielsen, 2014[9]).
In general, prevention policies with the most attractive cost-effectiveness profile are those reaching the largest number of individuals (Chokshi and Farley, 2012[10]), although even they should take into account various population characteristics (Hawkes et al., 2015[11]). At the same time, more targeted policies can also make a strong impact, although their cost-effectiveness is typically improved when higher-risk groups are targeted (Rose, 2001[12]). For instance, well-designed primary care-based interventions to identify adults with overweight or other risk factors, followed by lifestyle counselling have been shown to be cost-effective and affordable for health care systems in OECD countries (OECD, 2010[13]).
A distinction potentially more important than the population or target group dichotomy is between policies that target behaviours, and those that aim to make changes to the overall environment including, for example, widening a set of choices to buy healthy food or to do more physical activity (Lean, Astrup and Roberts, 2018[14]). This distinction can be particularly important as policies in these two categories often produce unequal effects on different SES population groups. For example, mass media campaigns can target behavioural change by providing information on ways to improve diet quality, while reformulation policies aim to affect overall food supply. While both policies are population-level, and both aim to achieve similar goals, mass media campaigns may benefit educated people more, as the effectiveness of campaigns may depend on general literacy and the ability to process information quickly. Indeed, some evidence indicates the potential for mass media campaigns to generate such inequalities (Lorenc et al., 2013[15]). On the other hand, reformulation policies may have a stronger effect on the overall food system, and thus lead to a more equitable effect on health. Therefore, policies should be designed carefully to ensure that they do not lead to the exacerbation of health inequalities.
Better coordination of actions across multiple sectors, including public-private sector collaboration, may help tackle not only overweight, but also other key public health priorities. For example, policies that reduce overweight can also help deal with such issues as climate change (OECD, 2017[16]), poverty and income inequality (Nugent et al., 2018[17]), economic productivity, absenteeism and presenteeism (Feigl et al., 2019[18]). At the same time, policies in other areas, not necessarily aiming to tackle overweight, can contribute to improved diet and physical activity. For example, actions to improve the quality of the urban built environment and air quality, such as through increasing the number of accessible parks and recreational areas, may lead to a greater amount of physical activity and better overall health, therefore lowering overweight levels (Swinburn et al., 2019[19]). Another example of synergetic policies are the actions which may simultaneously reduce congestion and pollution on the roads, as well as increase population-level physical activity, such as sustainable public transport options (Xiao, Goryakin and Cecchini, 2019[20]), or bike-sharing schemes and cycle lanes.
While potential synergies in cross-sectoral collaboration may appear obvious at first, in practice the amount of such collaboration will depend on the degree of mutual understanding of the benefits by all stakeholders. For example, urban planners, or environmental agencies, may be receptive to the health-promoting potential of public transport systems, active travel options or of green space areas, as they may already support such policy actions for other reasons. In other cases, establishing multi-sectoral collaboration can be more challenging, and may require going beyond demonstrating the health benefits of a given policy. For example, achieving necessary changes to agricultural policies or food systems is not easy, but the policy process may benefit from the evidence that such changes will also be good for the environment (Willett et al., 2019[21]), or that they can result in greater economic productivity and additional tax revenues. Likewise, there may be resistance to introducing advertising regulation, or pricing policies, but showing that they can lead not only to better health outcomes, but also to greater educational achievement, better productivity and a positive impact on public finances, may help generate the will for political action.
Finally, carefully designed collaboration between the public and private sector can be an additional lever to influence the determinants of overweight (Box 5.2). Often, the industry may be concerned that some public health actions may impose costs of doing business. There are however, ways for the industry to minimise such costs (see Chapter 7), while enjoying the benefits of more socially responsible corporate image.
Carefully designed public-private partnerships (PPPs) in public health can be advantageous to all stakeholders, including industry, government and consumers. For industry, working with governments in this area can create new opportunities and market niches for healthier products. For example, in the last few years, soft drinks producers have started diversifying their portfolios to introduce products that consumers see as being a healthier choice, with the main aim being to offset the declines in the soft drinks market (Daniel B. Kline, 2018[22]). Another rationale, from the industry’s point of view, is to forestall stronger legislative action by the government. For example, the United Kingdom’s sugar reduction programme specifically states that if the voluntary reformulation programme with food producers does not result in sufficient progress, alternative levers will need to be used (Department of Health & Social Care, 2016[23]). Finally, this collaboration can help industry support their corporate social responsibility efforts and improve public image, while contributing to population health. For example, in Japan, the government runs a contest for company wellness schemes, rewarding the most successful ones with “excellence awards” and public recognition (OECD, 2019[24]). In Spain, the government recognises the food and beverage industry players with the NAOS Strategy Awards (Strategy for Nutrition, Physical Activity and Obesity Prevention) for their initiatives whose objectives contribute to obesity prevention through the promotion of healthy diet and/or regular physical exercise (Aecosan, 2019[25]).
From the governmental point of view, working together with the industry can mobilise more resources. In addition, by engaging with the industry and understanding their concerns and limitations, governmental institutions can develop programmes that are attractive to all participants. For instance, in Chile, the Ministry of Agriculture works with the National Federation of Independent Street Markets (covering 60% of all street traders) to provide access to healthy foods in underserved areas and to disseminate information on healthy diets (OECD, 2019[26]). In Australia, the Healthy Food Partnership Reformulation Working Group is developing reformulation targets in consultation with the industry to gauge technical feasibility (Healthy Food Partnership, 2018[27]). In Spain, a new reformulation action was initiated in 2016, involving 20 agreements with food sector associations representing more than 398 companies.
However, establishing successful PPPs to achieve public health goals is not easy, as was shown, for example, in a study on the effectiveness of self-regulation of food marketing to children (Galbraith‐Emami and Lobstein, 2013[28]). Therefore, when designing such programmes, any potential for the conflict of interest should be considered and minimised, with clear objectives and accountability processes set out from the beginning. The governments should also be resistant to the use of such partnerships as purely a marketing opportunity for the industry, without actually implementing effective actions.
As mentioned above, the set of available policies targeting the burden of overweight can be categorised into those influencing lifestyles through information and education; those widening the set of healthy choice options; those modifying the cost of health-related choices, and, finally, those regulating or restricting actions promoting unhealthy choice options. This section provides a more detailed overview of the existing policy environment.
Communication-based approaches through the provision of information and education represent a significant share of disease prevention policies put in place by OECD countries, and may take a number of forms. For example, they can help consumers make informed food purchases by providing relevant information on food and menu labels. They can be employed as part of health promotion and social marketing campaigns aimed at changing behaviours adversely affecting health, including through the use of mobile apps. They can also be used to support other disease prevention policies, such as aiding health education campaigns targeting schoolchildren, workers or primary care users. Although these interventions do not generally target a particular group, their effectiveness in some cases may depend on factors like the SES of the population. For example, it was found that restaurant menu labelling leads to greater calorie reduction in areas where residents are more educated and have higher incomes (Borgmeier and Westenhoefer, 2009[29]; Sinclair, Cooper and Mansfield, 2014[30]).
Food labels on pre-packaged foods aim to inform consumers about the nutritional value of foods. They can include “informative” labels containing a list of nutrients, usually put on the back, or clearly visible “interpretive” labels providing nutritional information in a more easy-to-understand format, usually put on the front. In addition, front-of-pack (FoP) labels may aim to warn about nutrients that should be consumed in limitation or avoided altogether, e.g. salt, sugar, saturated fats content, or highlight positive aspects such as dietary fibre content.
Food labels can be an effective and credible source of information for shoppers (Campos, Doxey and Hammond, 2011[31]; Sacks et al., 2011[32]). For example, a review of 58 studies conducted from 2003‑2006 in the EU15 countries concluded that there was widespread consumer interest in use of nutritional information on food packages. Up to 50‑60% of consumers checked nutritional labels at least occasionally in countries such as Ireland, the United Kingdom, France and Sweden (Grunert and Wills, 2007[33]). Previous OECD work has also concluded that food labelling was associated with an 18% increase in the number of people selecting healthier food products (Cecchini and Warin, 2016[34]). In Spain, high correlation was found between nutritional label use and healthier food purchases (Barreiro-Hurlé, Gracia and De-Magistris, 2010[35]). Regarding specific labelling types, it appears that FoP labels are more effective than back-of-pack (BoP) labels (Grunert and Wills, 2007[33]; Campos, Doxey and Hammond, 2011[31]). Likewise, there is evidence that multiple traffic light systems providing color-coded information about the amount of key nutrients, usually put at the front, may be more effective compared to other alternatives including, for example, guideline daily amount (GDA) labels (Hawley et al., 2013[36]).
Almost all reviewed countries require some sort of nutrition labelling on packaged foods. Mandatory BoP label is the most common form of labelling, as it is mandatory in 34 OECD countries (Figure 5.3). Conversely, mandatory FoP informative labels are still rare, as only four OECD countries implement them (Figure 5.3). Finally, in two OECD countries, BoP labelling is mandatory only in specific cases. In Turkey, BoP labelling is mandatory only when a health claim is made, while Switzerland also only has voluntary BoP labelling, unless exporting to the European Union. In the European Union, Regulation 1169/2011 on the "Provision of Food Information to Consumers” has required that the following nutrients be listed at the back-of-pack of most pre-packaged foods from 2016 onward: energy value; the amounts of fat, saturates, carbohydrates, sugars, protein and salt.
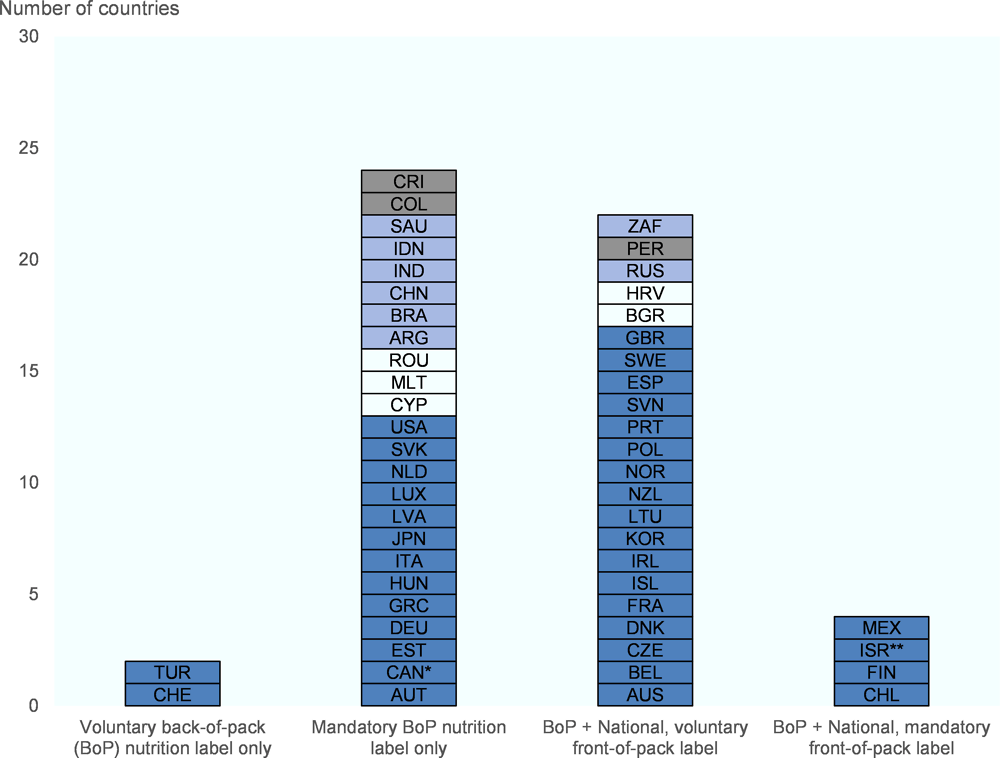
Note: OECD countries in dark blue; other G20 non-OECD countries in light blue; other EU non-OECD countries in white; other countries partnering with the OECD in grey.
* Canadian legislation on mandatory FoP labelling is the subject of a proposal; ** Mandatory FoP label to come into force in 2020;
Source: WCRFI (2016[2]), “NOURISHING-framework” http://www.wcrf.org/int/policy/nourishing-framework; WHO (2012[4]), Global database on the Implementation of Nutrition Action (GINA), https://www.who.int/nutrition/gina/en/; Kelly and Jewell (2018[37]), “What is the evidence on the policy specifications, development processes and effectiveness of existing front-of-pack food labelling policies in the WHO European Region?”, EUFIC (2018[38]), Global Update on Nutrition Labelling.
In 2016, Chile introduced a mandatory labelling system for pre-packaged foods, to signal to consumers products that do not meet certain criteria in terms of nutritional content. It is hoped that this system will stimulate reformulation by the industry.
Specifically, four black and white labels are used to indicate whether a certain foodstuff is high in calories, salt, sugar or fat (OECD, 2019[26]). If the food exceeds the mandated thresholds set by the government, which are among the strictest in the world, warning signs have to be placed on the package, which read “high in” followed by calories, saturated fat, sugar or sodium, as well as “Ministry of Health”. If a product exceeds more than one limit, more than two signs have to be placed on the package. The thresholds have been gradually tightened over time, and are currently set at the following levels:
Sodium (mg/100 g or ml): 400 for solid foods; 100 for liquids
Sugar (g/100g or ml): 10 for solid foods; 5 for liquids
Saturated fats (g/100g or ml): 4 for solid foods; 3 for liquids
Energy (kcal/100g or ml): 275 for solid foods; 70 for liquids.

In addition to mandatory schemes, some voluntary initiatives have also been adopted. One prominent example is the Keyhole logo, a voluntary scheme implemented in several, mostly Nordic, countries. Participating businesses can put a keyhole logo on the front of the packages of the food they sell, when it has less fat, sugar or salt, dietary fibre and whole grains, compared to other foods in the same category. One study found that about 95% of consumers were aware of the Keyhole Logo in Sweden, and that its purpose was broadly understood (Grunert and Wills, 2008[39]). Another example is the voluntary FoP summary label recently adopted in France, based on an intuitive colour scheme (Box 5.4).
In October 2018, France introduced a FoP label called Nutri-Score. It is used on a voluntary basis by about 90 companies including several major retailers and food processors in France and Belgium, with Spain also recently approving the use of the label (van der Bend and Lissner, 2019[40]). It is based on a five-colour scale that summarises the healthiness of a product, and provides a single, compound score, which may aid interpretation by the consumers. On the other hand, consumers who prefer to have more information about a specific ingredient (e.g. the amount of sugar), may prefer a system like the traffic light labelling in the United Kingdom, which provides separate assessments for four ingredients.
To select the most appropriate FoP label design, a randomised experiment was undertaken in France in 2016, with particular attention paid to purchasing decisions made by low-income households (Ministère des Solidarités et de la Santé, 2017[41]). The experiment took place in 60 retail stores and concerned 1 300 food products from four food categories: freshly prepared foods, pastries, breads, and canned prepared meals. Four types of FoP nutritional information systems were tested: Nutri-Score; multiple traffic lights; simplified nutritional labelling system and modified reference intakes. The Nutri-Score was found to have the strongest effect on the overall quality of the shopping cart, compared to the other labels (Ministère des Solidarités et de la Santé, 2017[41]). In addition, several experimental studies conducted in the virtual supermarket settings showed similar results (Chantal and Hercberg, 2017[42]).

Restaurant menu labelling involves listing information on the calorie content, as well as on the content of other nutrients, such as salt and sugar, of items on the menu at points-of-purchase of restaurants and cafeterias. This can be done with or without contextual information like recommended daily calorie intake, or interpretive information such as a traffic light system design. It can also be done with the help of PACE (physical activity calorie equivalent) labels that indicate the number of minutes of exercise needed to burn off the calories consumed.
Emerging evidence indicates that menu labelling can positively affect consumer behaviour, and that there is strong public support for it (Mah et al., 2013[43]; Pulos and Leng, 2010[44]; Morley et al., 2013[45]). A recent systematic review and meta-analysis (Sinclair, Cooper and Mansfield, 2014[30]) of mostly mandatory initiatives found that participants who received menus with labels consumed 41 fewer calories per purchase, compared to the control group. The same study also found that contextual or interpretive labels were more effective, by reducing calorie consumption by 81 kcal. Emerging evidence also suggests that menu labelling with the exercise component (i.e. so-called PACE labelling) can be as effective as calorie labelling at reducing the number of calories ordered at fast food outlets (Antonelli and Viera, 2015[46]; Seyedhamzeh et al., 2018[47]). Similar to what has been shown for food labelling, there is tentative evidence that mandatory menu labelling, besides influencing consumer behaviour, might also encourage restaurants to reformulate their menus by offering lower calorie content (Block and Roberto, 2014[48]; Bleich et al., 2015[49]).
The introduction of menu labelling can produce unequal behavioural changes across population groups. Available evidence suggests that menu labelling may be more effective in women (Afshin et al., 2015[50]; Nikolaou, Lean and Hankey, 2014[51]); those with a higher level of education (Fernandes et al., 2016[52]); and in people who already prefer to eat healthily (Vyth et al., 2011[53]). In addition, certain barriers may hinder their impact (Thomas, 2016[54]). For example, businesses, and especially smaller establishments, may lack expertise, time or other resources to correctly estimate the amount of the nutrients to put on the menu. As a result, some businesses are concerned about potential libel risk arising from incorrect estimation of nutritional information (Thomas, 2016[54]). Nutritional information also has to be carefully presented to be both readable and aesthetically pleasing to consumers.
Mandatory menu labelling initiatives are relatively recent and therefore implemented in a limited number of settings. In the United States, all chain restaurants with at least 20 outlets have been required to show calorie information on their menus since 2018 (Cleveland, Simon and Block, 2018[55]), although several municipalities and states had implemented related legislation even earlier. In one evaluation conducted in Washington State, such legislation resulted in a per purchase decrease of calories by 38 kcal after 18 months of implementation (Krieger et al., 2013[56]). In addition, from mid-2018, these regulations have also covered operators of at least 20 types of vending machines in the United States (Dell, 2018[57]). In Australia, several states introduced legislation between 2011‑18 requiring restaurant chains with more than 20 outlets in the state (or more than seven in the Australian Capital Territory), or 50 or more in the whole of Australia, to display the energy content of their menu items (Niven et al., 2019[58]). In Ontario, Canada, all food service chains, with at least 20 locations, have been required to list calorie counts on their menus since January 2017 (Ontario.ca, 2018[59]).
Health-promoting mass media campaigns have the potential to reach many people, while affecting multiple overweight risk factors at the same time. Such campaigns can be implemented through both traditional (television, radio, newspaper) or new media (online marketing, social networks [e.g. social media]) and are often implemented at the national level, although, in some cases, they can be launched by local authorities.
Mass media campaigns are often implemented as part of a policy package, which makes evaluation of their effectiveness complicated (Afshin et al., 2017[60]). Still, a limited number of studies assessing their effectiveness do exist. For example, the “2&5” mass marketing campaign in Western Australia resulted in a population-wide increase in the mean intake of fruit and vegetable servings by about 0.2 servings per day over three years (Pollard et al., 2008[61]). In the United Kingdom, following the introduction of the Change4Life social marketing campaign (see Box 5.5) 58% people switched to lower-fat dairy products compared to 26% in the comparison group (Wrieden and Levy, 2016[62]). An OECD review of studies assessing mass media campaigns to promote an active lifestyle estimated that within one month of the intervention starting, mass media campaigns can result in a 60% increase in the number of people who are considered at least moderately active, with the effect disappearing after about 3 years (Goryakin et al., 2017[63]).
Most, if not all OECD countries, already have, or have had in the past, at least one nationally run mass media campaign to encourage healthier lifestyles. For example, there is almost universal governmental promotion of fruit and vegetable consumption, not only of the well-known “5-a-day” target (e.g. in Chile, Germany, Italy, Mexico, New Zealand, Spain) but also of other types, e.g. "6-a-day" in Denmark (Haraldsdóttir, 1999[64]), or the “2&5” campaign in Western Australia which promotes eating two servings of fruit and five servings of vegetables a day (Pollard et al., 2008[61]). There are also examples of governmental programmes encouraging physical activity, such as the “Eat Move” campaign in France or Change4Life campaign in England and Wales (see Box 5.5).
Increasingly, such campaigns are provided through innovative channels, such as the “Choose to Live Healthily” campaign in Chile (Elige vivir sano) which is distributed with the help of an online component, e.g. using a web-based tool to calculate calorie intake and to create an agenda for health events. In the Netherlands, the Nutrition Centre has been in charge of several online public health campaigns encouraging healthier food choices, for example by providing recipes and tips for healthier eating through a dedicated website, mobile apps and an online tool (Wammes, Oenema and Brug, 2007[65]).
When designing mass media campaigns, it is important to take into account a number of challenges. For example, they are usually time-limited and not necessarily repeated on a regular basis. In addition, while innovative approaches to disseminating information may offer promising avenues to reach out to certain population groups, especially to the younger population, it is important to make sure that such policies do not create digitally-driven inequalities in health (Neter and Brainin, 2012[66]). Therefore, the use of more traditional channels, such as television and printed media, should also be maintained. More generally, mass media campaigns should be designed while keeping the needs of all people, and especially those living in the economically and socially underprivileged communities, in mind. Thus, promotion of healthy lifestyles should go hand in hand with ensuring that sufficient healthy options are available for those wishing to take advantage of them.
Change4Life (C4L) is an ongoing social marketing campaign established in 2009 to tackle the overweight problem in England, through the promotion of healthy food choices and physical activity (Levy, 2013[67]). C4L is a preventative policy designed to provide healthy lifestyle advice, also with tips for reducing alcohol intake and helping families to find local sports activities. Both children and adults are targeted through press, radio advertisement campaigning and a website.
Change4Life promotes healthy weight through a programme of eight behavioural changes:
1. reducing intake of fat, particularly saturated fat (Cut Back Fat)
2. reducing intake of added sugar (Sugar Swaps)
3. controlling portion size (Me Size Meals)
4. eating at least five portions of fruit and vegetables per day (5 a Day)
5. establishing three regular mealtimes each day (Meal Time)
6. reducing the number of snacks (Snack Check)
7. doing at least 60 minutes of moderate-intensity activity per day (60 Active Minutes)
8. reducing time spent in sedentary activity (Up and About).
The Government decided to avoid a visible involvement in the campaign, to guarantee the idea of a bottom-up movement where the main actors are children and their families. According to one evaluation (Wrieden and Levy, 2016[62]), three weeks after the start of the campaign, 32% of the intervention group had purchased a lower-sugar drink compared with 19% of the comparison group; and 24% had made a change to a lower-sugar cereal compared with 12% of the comparison group.
More recently, a number of countries have shown increasing interest in testing new electronic tools designed to promote various health-related behavioural changes (Leahey et al., 2016[68]; Schippers et al., 2017[69]; Semper, Povey and Clark-Carter, 2016[70]). Among them are applications, which can help individuals count the numbers of steps they walk in a day, or estimate calories consumed. Individuals can also take advantage of various technological options, which can, for example, link calorie information to product barcodes that can be scanned by phones; generate charts on trends in calorie consumption and physical activity levels; provide information on nearby health and wellness events/facilities; and promote health behaviours through various rewards programmes. In the simplest form, such tools can deliver health information as text messages (Hall, Cole-Lewis and Bernhardt, 2015[71]), or they can operate as more complex E-health behavioural interventions, including, for example, mobile health apps, computer-assisted personalised feedback, web-based courses and interactions over social media (Hutchesson et al., 2015[72]; Oosterveen et al., 2017[73]).
Emerging evidence indicates the potential of such technologies to positively affect health outcomes. For example, a recent systematic review and meta-analysis concluded that the use of mobile phone applications is related to a significant decrease in body mass index (BMI) of about 0.43 kg/m2 (Mateo, Granado-Font et al. 2015). Nevertheless, the uptake and usage of most apps can also be quite low (Yoganathan and Kajanan, 2013[74]; Neubeck et al., 2015[75]). For example, a US study estimated that over half of all health apps on the iTunes store were downloaded no more than 550 times (Neubeck et al., 2015[75]). The uptake of mobile apps may depend on various factors, such as the spread and intensity of the marketing campaigns promoting their use, as well as privacy-related concerns (Neubeck et al., 2015[75]).
There are already some examples of such technologies in practice. In Austria, an online tool enables the comparison of sugar, salt, fat and energy content of foods across different product categories (lebensmittellupe.at, 2019[76]). Likewise, in Estonia, the National Institute for Health Development implemented a web-based tool to help households calculate the amount of salt and sugar in their diet, and software to check the nutritional value of products by name or brand (Toitumine.ee, 2019[77]). In England, the family-oriented Change4Life campaign ran the targeted “Smart Swaps” campaign in 2014 to help reduce sugar, saturated fat and salt consumption by providing healthy tips and recipes through a dedicated website and mobile apps. They also promoted the “Be Food Smart” app that provides sugar, saturated fat and salt content in packaged products by scanning the barcode. Some other examples of such technologies are shown in boxes Box 5.6 and Box 5.7.
The Health Promotion Board (HPB) is a governmental organisation that implements health promotion campaigns and disease prevention programmes in Singapore. HPB launched a mobile app called Diet and Activity Tracker (iDAT) in 2011, which helps individuals count their calorie intake by recognising components of over 1 000 dishes and beverages, and also helps them track their physical activity levels (Goryakin et al., 2017[63]). In 2016, iDAT was replaced by Healthy 365, a platform complementing the extension to the National Steps Challenge (NSC) programme, encouraging individuals to attain more steps every day. NSC leverages the use of technologies such as a steps tracker and HPB’s Healthy 365 mobile app, to nudge participants towards a more active lifestyle. For example, anyone who downloads Healthy 365 and chooses to participate in the National Steps Challenge (NSC) can be ranked on their physical activity performance through a mobile tracking mode system. Participants can also earn various rewards, thanks to commercial agreements with sport centres, wellness companies, or food and beverage industries. In March 2016, 156 000 sign-ups for the National Steps Challenge were recorded through Healthy 365 (Goryakin et al., 2017[63]). It was also found that 58% of participants were still active over a four-month period.
The “Be He@lthy, Be Mobile” (BHBM) is a joint initiative between the International Telecommunication Union (ITU) and the WHO established in 2013. BHBM is the first UN initiative to use population-wide mobile health (mHealth) prevention services at scale, and claims to be the largest-scaled mHealth initiative for NCDs in the world.
The main goal of BHBM is to encourage and facilitate partnerships between Ministries of Health, Ministries of Information and Communication Technology, academia and local civil society, with the goal of scaling up national mHealth programmes for NCD prevention and management. Specifically, the initiative aims to leverage the power of mobile technology to deliver a number of public health messages. In addition, other mediums for information dissemination are being considered for the future, including interactive voice response systems, web-based messaging platforms, audio systems, and tablet devices. BHBM programme is also exploring opportunities afforded by artificial intelligence and big data for health promotion and disease prevention, for example by improving diagnosis and treatment decision-making processes.
BHBM now works mostly in low and middle-income countries: India, Philippines, Senegal, Zambia, Tunisia, Egypt and Costa Rica, and is in a preparatory phase in Sudan and Burkina Faso. It is also active in two OECD countries, Norway and the United Kingdom. So far, more than 3.5 million people have received messages through BHBM programmes. Independent impact evaluations have confirmed, for example, that there was a 19% quit rate amongst participants in the mTobaccoCessation programme. In Zambia, mCervicalCancer programme resulted in a 6% increase in cervical cancer screenings.
Currently, the focus of the programme is on helping people to stop smoking, exercise and eat healthy. It also aims to increase awareness about diabetes, breast and cervical cancer. BHBM and WHO have started collaborating with a leading internet company to facilitate sharing health advice through new and innovative platforms. For example, WHO considers reaching out to more people through an app for fitness to share its physical activity recommendations (WHO, 2019[78]).
Physicians may be in a good position to provide advice on proper nutrition (Ockene et al., 1999[79]), including diet, or better yet, to combine the prescription of physical activity with a nutrition education component (Elliot and Hamlin, 2018[80]). Primary care settings also present an obvious opportunity to provide information and advice on healthy lifestyles and to encourage physical activity, especially among the at-risk population groups. In developed countries, up to 80% of the population visit their general practitioner (GP) at least once a year (Sanchez et al., 2015[81]), implying that GPs may be ideally suited to provide advice on adequate physical activity levels. Such advice can take the form of general behavioural counselling (Grossman et al., 2017[82]), or more formal prescribing (Goryakin, Suhlrie and Cecchini, 2018[83]).
There is already good evidence that prescribing physical activity in primary care settings may increase the physical activity levels of sedentary patients, at least in the short-term (Orrow et al., 2012[84]; Campbell et al., 2015[85]; Sanchez et al., 2015[81]; Lin et al., 2010[86]). According to a recent systematic review and meta-analysis, prescribing physical activity for people at risk of developing chronic diseases may increase physical activity by about 56 extra minutes of moderate-level exercise per week, which can account for about a third of the 150 minutes per week of moderate exercise recommended by WHO (Goryakin, Suhlrie and Cecchini, 2018[83]). There is also evidence that counselling by dieticians can contribute to improving the quality of diet (Hebert et al., 1999[87]).
Physical activity on prescriptions programmes exist in at least one-third of OECD countries. For example in the United Kingdom, they were introduced as early as 1990s, and in Scandinavian countries- in the 2000s (for a Swedish example, see Box 5.8). They have also been introduced in Germany, the Netherlands (Box 5.9), Austria, Belgium, Spain, Portugal, the United States, Canada, New Zealand and Australia (Arsenijevic and Groot, 2017[88]). The programme design varies. For example, in some countries, prescriptions are given by GPs, while in others by nurses or other health professionals. Prescribed physical activity can be facility, home-based, or both, and may be limited to aerobics, or include other activity types, such as walking, swimming or gardening. Programme duration can also vary (Arsenijevic and Groot, 2017[88]).
Such policies should be designed carefully to take into account a number of challenges. For example, although they are generally more effective when the meetings between physicians and patients are frequent (Goryakin, Suhlrie and Cecchini, 2018[83]), this also implies greater programme cost. In addition, community support, including, for example, access to local walking clubs and aerobic classes, may be needed for better programme effectiveness (Estabrooks, Glasgow and Dzewaltowski, 2003[89]), which again may imply the need for additional resources. Recruitment of physicians may be challenging, with some studies citing their lack of interest, time constraints and concerns about understaffing levels, among the causes hindering the implementation of this intervention (Aittasalo et al., 2006[90]). Programme implementation may also be hindered by lack of health literacy among patients and by various barriers to sustaining behavioural change over time (WHO, 2016[91]). At the same time, medical professionals mention such constraints as lack of dedicated clinical guidelines, especially in relation to risk assessment, inadequate referral schemes and lack of coordinated patient pathways, as well as insufficient financial mechanisms incentivising prevention (WHO, 2016[91]). In some countries, medical curricula may also inadequately emphasise the benefits of prevention (Allan et al., 2004[92]). Therefore, in practice, many of the target individuals, potentially benefitting from this intervention, may not actually receive the counselling in the countries in which prescription of physical activity is currently implemented.
The Swedish physical activity on prescription programme was selected as a best practice example by the European Commission (European Commission, 2019[93]). This is a patient-centred counselling programme, in which patients at risk of developing NCDs receive written individualised prescriptions from a medical worker (who may be any qualified licensed health care practitioner, and not necessarily a medical doctor), for both everyday physical activities, as well as for aerobic fitness, strength and flexibility training. The prescription also specifies duration, frequency and intensity of the exercise. There is also a formal follow-up procedure, the results of which go into the patient’s medical record. The ultimate aim of this scheme is to help patients integrate physical activity into their daily lives (Kallings, 2016[94]). An evaluation concluded that the programme significantly contributed not only to increases in self‐reported moderate physical activity level at least once a week, from 19% to 36%, but also to better quality of life (Kallings et al., 2008[95]).
Since 2002, physically inactive patients at higher risk of cardiovascular diseases (CVDs), hypertension or type two diabetes who live in the Netherlands can be enrolled into the exercise on prescription programmes. Before issuing a prescription, GPs talk to patients to evaluate their commitment to participating in the programme as well as to pay a one-time fee of up to 100 euros. If this commitment is obtained, GPs issue a formal written prescription, which the patients then take to the exercise clinics, where they undergo a health assessment, and attend a counselling session (Sørensen et al., 2011[96]). An evaluation of the programme established that after four months of participation, up to 30% of patients increased their physical activity levels, and up to 25% experienced improvements in their quality of life (Sørensen et al., 2011[96]).
Although policies influencing lifestyles through information and education are important, they may not be sufficient if the local environment presents limited opportunities to engage in healthy lifestyles. For example, prescribing physical activity may be ineffective if there is a lack of safe, walkable and green spaces. Likewise, encouraging people to eat more fruits and vegetables through mass media campaigns may be of limited value if the opportunities to buy healthy food are limited, or if food preparation skills are lacking. Although a systematic, multifaceted response is needed to achieve favourable long-term outcomes, with one promising example being the Milan Urban Food Policy Pact (see Box 5.10), initially the changes to the community environment do not necessarily have to be drastic. For example, there is evidence from four cities in South and North America that the policies of closing streets to traffic even temporarily to encourage physical activity can be highly cost-beneficial (Montes et al., 2012[97]).
As more than 50% of the world’s population currently lives in urban areas (with the proportion expected to increase significantly in the coming years), ensuring an equitable and environmentally sustainable supply of healthy food in urban areas is critically important. The Milan Urban Food Policy Pact is a voluntary international protocol committing the parties to the agreement to develop resilient, inclusive, diverse and sustainable food systems designed to provide healthy, accessible and affordable food to all people, while protecting biodiversity and reducing food waste (Milanurbanfoodpolicypact, 2019[98]). The protocol was announced in 2014 in Johannesburg during a C40 meeting (see Box 5.15), and signed in 2015 in Milan, by mayors of more than 100 cities at the time of EXPO 2015. Currently, almost 200 cities are signatories to the Pact, benefiting from information and standards sharing, as well as from various relevant joint actions. Although the Pact is voluntary, a number of cities are interested in monitoring their progress in meeting various relevant indicators reflecting six main focus areas of the pact: food governance; sustainable diets and nutrition; social and economic equity; food production; food supply and distribution; food waste. The Food and Agricultural Organization supports this initiative by developing performance indicators to measure progress, as well as by helping disseminate relevant best practices (Milanurbanfoodpolicypact, 2019[98]).
As children are in early stages of their lives, they are only just beginning to develop critical thinking skills and learning to exercise self-control, which makes them particularly vulnerable to outside influences. For example, they share their parents’ diet and acquire exercise-related habits from them. Children’s food learning can also be affected in other ways, and as early as when they go to nursery school. In school, they may be affected both by the food options that surround them, and by their peers. Their choices are also influenced by the broader environment in which they live. For example, some communities may provide accessible options to exercise or buy healthy food, while others may be described as “food deserts” or “food swamps” (Saunders, Saunders and Middleton, 2015[99]). Therefore, the health-related behaviours of children can be affected not only through policies that specifically target them, but in many other ways, too (see Box 5.13).
There are various interventions designed to encourage healthy lifestyles among children (Wang et al., 2015[100]; Nooijen et al., 2017[101]). A meta-analysis of studies combining intensive classroom physical activity lessons led by trained teachers, moderate-to-vigorous physical activity sessions, distribution of nutritional education materials and provision of healthful foods, found that such interventions can reduce BMI by an average of 0.3 kg/m2 (Wang et al., 2015[100]). However, although creating right conditions in schools is important, it is alone unlikely to achieve a long-term impact without the involvement of other family members, or improving community environment as a whole. For example, one review found stronger evidence for school-based programmes including the involvement of other family members or a community, compared to the purely school-based ones (Van Sluijs, McMinn and Griffin, 2008[102]). In addition, family-based programmes, where education is provided to parents on the value of physical activity in their children, as well as on the practical steps of achieving it, can increase physical activity by a standardised mean difference of 0.41 (Brown et al., 2014[103]).
Some concrete examples of such policies include the EU School Fruit Scheme, launched in 2009 (Box 5.11). Another example is the Coordinated Approach to Child Health in the United States (CATCH), a comprehensive intervention to promote healthy eating in school cafeterias, and encourage physical activity by providing, for example, necessary physical equipment in elementary schools (Coleman et al., 2005[104]). In Australia, a programme called Crunch&Sip® promotes consumption of fruit, vegetables and water during class time (Nathan et al., 2012[105]), by providing a daily classroom break that allows students to eat fruits and vegetables, as well as by distributing various educational resources. In Slovenia, the “Kids to kids” programme teaches primary school pupils to prepare healthy meals (Kuhnapato.si, 2019[106]). In Chile, schoolchildren benefit from a comprehensive “Contrapeso” (“Against Overweight”) programme provided by the Ministries of Health, Education, Sports and Agriculture, which includes improvements in the quality of food provided to students in school, as well behavioural interventions (e.g. based on gamification) to promote physical activity (OECD, 2019[26]).
The EU school fruit and vegetable scheme was launched in 2009, with the view to encouraging healthy eating habits among children at school. It distributed fruit and vegetables to schools throughout the European Union, using funding from the EU Common Agricultural Policy. In 2017, the programme was replaced with the broader scheme, which also added the separate milk component. More recently, the EU High Level Group on Nutrition and Physical Activity has recommended that the Member States only fund the distribution of products with no added sugar under this scheme (European Commission, 2018[107]). Following on this recommendation, an additional two Member States have decided to only subsidise milk without added sugar in their primary schools (European Commission, 2019[108]).
The programme has several guiding principles, including the provision of fresh, seasonable fruit and vegetables and exclusion of products with added sugar, salt, fat and artificial sweeteners. The EU budget for the scheme is EUR 250 million annually, including EUR 150 million for fruit and vegetables, and EUR 100 million for milk (EC, 2019[109]).
School-based programmes may also include certain regulations. Thus, in 35 reviewed countries, there are already mandatory nutritional standards for schools, while in another 15 such standards are voluntary (Figure 5.6). For example, in the United States, a nation-wide US Healthy, Hunger-Free Kids Act (HHFKA) was introduced in 2010. One of its aims is to limit the amount of saturated fat, salt and added sugars that is permitted in food sold on school premises (Schneider et al., 2012[110]). Other examples include local area bans on vending machines in elementary schools in Arkansas, the District of Columbia, Florida, Indiana and Texas (bridgingthegapresearch.org, 2013[111]); advertising restrictions in schools (Palakshappa et al., 2016[112]); or healthier food procurement requirements for school nutrition programmes, as in Slovenia, where governmental dietary guidelines for food provided in schools are complemented by food procurement standards (Gregorič et al., 2015[113]). For more information about public procurement in schools, see Box 5.12.
Procurement mechanisms can be a useful tool to encourage healthier food consumption among schoolchildren, especially given a large share of the total social food service market accounted for by the educational sector (estimated to be around 30% in Europe) (Caldeira et al., 2017[114]). As lunch meals can account for about 35% of the total daily energy (Caldeira et al., 2017[114]), such policies can bring about not only health benefits, but also contribute to better school performance and therefore to long-term human capital accumulation. Property executed food procurement schemes may also reward businesses that are driven not just by the profit motives, but are also cognisant of the broader societal consequences of their practices.
Public procurement of school meals may apply both to the purchases of raw food materials to be prepared subsequently in the school cafeterias, and to the partial or full contracting out of food catering services to the third parties (Caldeira et al., 2017[114]). Despite the potential benefits of well-designed procurement programmes, there are substantial challenges to implementing them in practice. For example, it may be difficult to translate the nutritional guidelines into actionable procurement requirements, especially given a number of other criteria that need to be taken when contracts are awarded (e.g. price; quality; non-discrimination; environmental sustainability). Evaluation of bids and monitoring the compliance with the procurement requirements may also be expensive and time-consuming. Recognizing this, the European Commission has recently prepared a tool aimed at helping schools draft better food catering contracts (European Commission, 2019[108]). There may also be difficulties in bringing the chefs and the kitchen staff on board, as they may have alternative views on the food they would like to prepare. In some cases, specific mandatory school food standards may be unclear or even absent (Caldeira et al., 2017[114]).
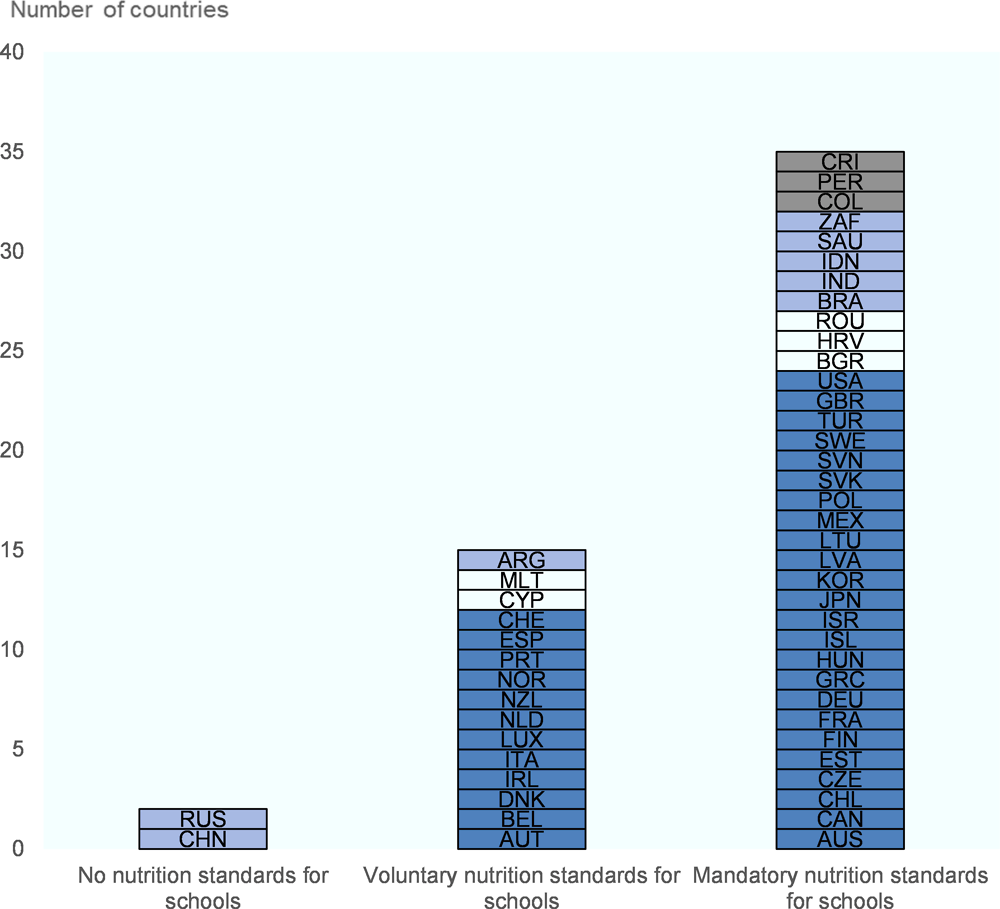
Note: OECD countries in dark blue; other G20 non-OECD countries in light blue; other EU non-OECD countries in white; other countries partnering with the OECD in grey.
Source: WCRFI (2016[2]), “NOURISHING-framework” http://www.wcrf.org/int/policy/nourishing-framework; WHO (2012[4]), Global database on the Implementation of Nutrition Action (GINA), https://www.who.int/nutrition/gina/en/; EU-JRC (2015[115]), School food policy country factsheets; WHO (2019[116]), WHO European Database on Nutrition, Obesity and Physical Activity (NOPA); FAO (2019[117]), Nutrition guidelines and standards for school meals: a report from 33 low and middle-income countries.
In addition to policies that are designed to target children, such as family and school-based programmes and advertising restrictions, there are other polices that have the potential to reach this population group. For example, food and menu labelling, improving the urban environment and regulatory changes such as taxations, reformulations, or even bans on certain unhealthy ingredients can all affect children directly or indirectly through their parents.
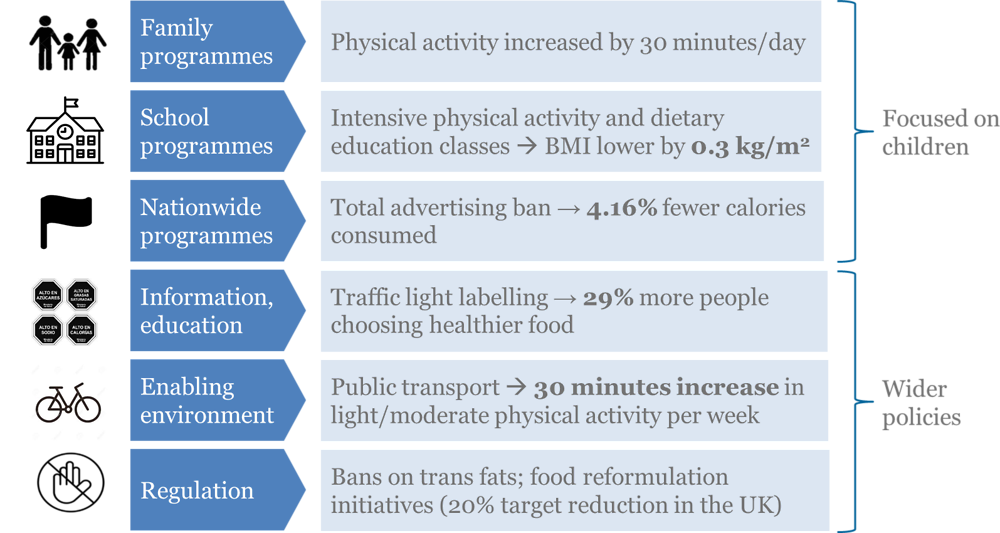
Source: Brown et al. (2014[103]), “Family-based interventions to increase physical activity in children: A meta-analysis and realist synthesis protocol”, http://dx.doi.org/10.1136/bmjopen-2014-005439; Wang et al. (2015[100]), “What childhood obesity prevention programmes work? A systematic review and meta-analysis”, http://dx.doi.org/10.1111/obr.12277; Goryakin et al. (2017[63]), “The Role of Communication in Public Health Policies: the Case of Obesity Prevention in Italy”, http://www.salute.gov.it/imgs/C_17_pubblicazioni_2647_allegato.pdf; Cecchini and Warin, (2016[34]), “Impact of food labelling systems on food choices and eating behaviours: a systematic review and meta‐analysis of randomized studies”, http://dx.doi.org/10.1111/obr.12364; Xiao, Goryakin and Cecchini (2019[20]), “Physical Activity Levels and New Public Transit: A Systematic Review and Meta-analysis”, http://dx.doi.org/10.1016/j.amepre.2018.10.022; Tedstone et al. (2018[118]), Calorie reduction: The scope and ambition for action.
As adults spend a large portion of their lives in employment, workplace-based actions are increasingly considered as a potentially effective tool to influence choices favouring healthier lifestyles. For example, such policies can achieve dietary improvements through changes in the selection of daily menus and snacks provided in workplace cafeterias (Geaney et al., 2016[119]; Allan et al., 2017[120]), or can promote physical activity and reduce sitting time through the provision of sit-stand workstations (Chu et al., 2016[121]). As a complementary action to changes in the working environment, employers have started implementing workplace wellness programmes, which may provide various educational materials, classes, seminars, group activities and individual counselling sessions encouraging healthy lifestyles, as well as give incentives such as bonuses and reimbursements to encourage participation (Baicker, Cutler and Song, 2010[122]).
From the employers’ point of view, such programmes may be attractive for at least two reasons. First, the implementation of such programmes can generate reductions in absenteeism-related costs while increasing productivity among employees (Baicker, Cutler and Song, 2010[122]). Second, companies implementing such programmes are generally favourably seen by potential and current employees, which helps improve their corporate image and their ability to attract and retain talent (OECD, 2019[24]).
The evidence on the effectiveness of such programmes is still limited, but results from selected studies, including some meta-analyses, appear to be promising, at least in relation to short-term outcomes. For example, a two-year multicomponent workplace programme which included actions to promote a healthy diet, including through information events and education awareness campaigns, was found to increase consumption of fruit and vegetables by 0.3 servings a day (Afshin et al., 2015[50]). Similarly, workplace interventions involving changes in the surrounding environment to encourage less sitting time, for example through the provision of sit-stand workstations and treadmill desks, were found to reduce sitting time by 72.78 min per eight hour workday (Chu et al., 2016[121]). A workplace wellness programme, entailing such components as health risk assessment for employees, group activities and individual counselling about healthy lifestyles, as well as provision of various incentives such as performance-related bonuses or reimbursements to encourage participation, was found to reduce BMI by up to 0.64 kg/m2 at the 12 month mark (Penalvo et al., 2017[123]). On the other hand, questions remain about long-term effectiveness and sustainability of such programmes, especially in smaller companies (McCoy et al., 2014[124]).
Although interest in such programmes is growing, they are still relatively infrequently implemented in OECD countries, and when they are, there are usually no evaluations of their effectiveness. One notable exception is Japan, where such programmes are very popular (Box 5.14). Another example of an incentive-based multicomponent workplace programme is the one managed by the Vitality Group in South Africa, with the emerging evidence suggesting its effectiveness not only in terms of encouraging such behaviour as healthy eating, but also in relation to reducing health expenditure (see Box 5.15). In Ireland, a National Workplace Wellbeing day was launched in 2015 with the stated aim to promote physical activity and better nutrition in the workplace, with more than 700 companies participating in 2019 (Civil Service Employee Assistance Service, 2018[125]).
Central and local governments in Japan provide various incentives, usually in the form of awards, for employers, both public and private, to implement workplace health promotion programmes. These programmes often focus on affecting such risk factors as unhealthy diet, physical inactivity, harmful alcohol consumption, smoking and mental well-being (OECD, 2019[24]). The activities are often carried out in small teams so that people can better motivate each other.
In general, the scope and comprehensiveness of such programmes is directly proportional to the size of the company, although as a rule, they comprise both targeted (e.g. health check-ups to identify people at higher risk of NCDs), and population-level approaches (e.g., menu labelling and healthier foods offers in canteens, provision of pedometers and installation of standing desks to encourage physical activity).
The participation rates in such programmes are usually very high, which may be due to both cultural reasons, as well as owing to the provision of various incentives. For example, rewards such as money, additional leave or other benefits may be given to participating employees based on meeting various targets, such as walking a minimum number of steps, or reaching a certain BMI threshold.
While promising, there is still a lack of data on the long-term effectiveness of such programmes, with some companies reporting improvements in health outcomes, reduction in absenteeism as well as savings in health expenditure. Conversely, some other companies failed to identify any positive changes, which may partly be due to the methodological limitations in the analyses.
Discovery Health, a private health insurer, has developed and has been running one of the most well-known examples of a privately-managed health prevention programme. The Vitality programme was first rolled out in South Africa to be subsequently extended to other markets, including the United Kingdom, the United States and China (Lambert and Kolbe-Alexander, 2013[126]). Participation in the programme is voluntary and membership is offered for a nominal fee equivalent to about USD 20 per month. However, in some cases, the fee paid by the participant is significantly smaller. For example, in the United States, almost 90% of the membership fee for the Vitality programme is covered by the employers (Lambert and Kolbe-Alexander, 2013[126])
This incentive-based programme rests on four pillars: assessment and screening, healthy choices, health knowledge and physical activity. Beneficiaries are encouraged to participate in different health-related activities such as health checks, exercising and eating healthy. Those who are sufficiently active are given bonus points, which can be exchanged for various rewards, such as upgrade in Vitality health status, free beverages or movie tickets, or discounts at various participating businesses. In addition, gym memberships are subsidised, and fruit and vegetable purchases are eligible for a cash rebate. It was found that the cash rebate has been effective in increasing expenditure on healthy foods by 9.3%, and decreasing spending on less healthy food by 7.2% (Sturm et al., 2013[127]). The Vitality programme was also found to reduce medical care costs, which created an additional incentive for private insurers to invest in prevention. For example, compared to Vitality members not participating in the programme, participants have about 15% lower hospital-related costs for cancer, 21% lower hospital costs for endocrinal and metabolic syndrome, and 7% lower for cardiovascular diseases (Patel et al., 2010[128]).
There are numerous examples of policies designed to make it easier for people to integrate physical activity into their daily lives through active travel and walking. They can include, for example, access to dedicated cycle lanes and bike-sharing schemes. Other actions can also include urban planning to increase the number of parks, recreational areas and green spaces, as well as expanding access to convenient public transport options to encourage people to switch from car use and to walk more to reach their destinations.
Active travel options, such as travelling by bicycle, can increase physical activity and decrease the need for passenger vehicles, and ultimately improve physical (Martin et al., 2015[129]; Otero, Nieuwenhuijsen and Rojas-Rueda, 2018[130]) and mental health (Martin, Goryakin and Suhrcke, 2014[131]). The evidence on the effectiveness of interventions to encourage greater bicycle use is still emerging, although some early results are promising. For example, three years after a walking and cycling route was built in a city in Brazil, those living less than 500 meters away from it increased their walking and moderate-to-vigorous physical activity by about 50 minutes per week, compared to almost no change in those who lived 1 000‑1 500 meters away (Pazin et al., 2016[132]). Physical activity can also be encouraged by better access to public transport. For example, for each person living in a community exposed to a newly available public transport system, walking increases by about 30 minutes per week (Xiao, Goryakin and Cecchini, 2019[20]). Active travel, walking and physical activity in general can be encouraged by better access to parks, green space areas and recreational facilities. For example, in the United States, living near parks and playgrounds is associated with a statistically significant reduction in childhood obesity, by 0.47 kg/m2 and 0.27 kg/m2 among boys and girls, respectively (Fan and Jin, 2014[133]).
There are numerous best practices in this area, including dedicated cycle lanes and bike-sharing schemes in cities such as Copenhagen, London, Amsterdam, Paris, Vienna and New York. As an added benefit, riding bicycles can also contribute to reduced air pollution, as in Barcelona, where the scheme was linked to the reduction of yearly CO2 emissions by about 9 000 tonnes (Rojas-Rueda et al., 2011[134]). On a global level, C40 is the network of the world’s largest cities that collaborate to take action on climate change while improving the quality of urban life (Box 5.16). Other policies of note include: closing central parts of the cities to traffic on certain days of the week in Latin America (Sarmiento et al., 2016[135]); the introduction of electric (or zero emission) buses in the cities, with China being the leading producer and user of such buses in the world (Bloomberg New Energy Finance, 2018[136]); or community programmes to encourage leisure-time physical activity, such as the Bewegt Im Park programme in Austria providing free yoga, pilates and fitness classes to people of all ages and fitness levels in public parks or other open spaces (bewegt-im-park.at, 2019[137]).
While these policies have the potential to positively affect the health of many people, their implementation often relies on local administrations, which may have limited incentives or support at a national level. This creates a risk that poorer communities are less likely to have sufficient resources to implement such actions. Without appropriate intergovernmental fiscal transfers, there is a threat of increasing health inequalities driven by such disparities in financing (OECD, 2019[24]).
Urban areas are one of the most important contributors of greenhouse gas emissions, with a large share accounted for by transport. Recognising this, the C40 Cities Climate Leadership Group was established in 2005 to promote sustainable urban development (C40, 2019[138]). The group serves as a network for knowledge and best practice sharing, as well as for technical assistance. Originally, the network was supposed to be open only to megacities based on such criteria as having a population size of at least three million people. However, it gradually opened up to the other city categories, for example “innovator cities”, as exemplified by implementing internationally recognised environmental work, and “observer cities”, which currently cannot join the network formally, but nevertheless can significantly benefit from participation. Currently, the network includes around 90 of the world’s largest cities located on all continents, except Antarctica.
The network shares various good practices to help tackle climate change and encourage sustainable urban development. Many of these practices also promote active travelling and, more in general an active lifestyle. For example, there are case studies of Istanbul’s Metrobüs system in Turkey, which provides about 600 000 passenger trips a day, while simultaneously reducing CO2 emissions by 167 tons/day (C40Cities, 2016[139]), or Mexico City’s cycle lanes, which were estimated to result in USD 65 million in monetary benefits since 2007, with almost 70% of this benefit coming from improved physical fitness (C40Cities, 2016[140]). Another example are urban actions to adapt to future climate change events, including more severe rainfalls, as in the Space to Grow programme launched in Chicago in 2013 to redesign school playgrounds into green storm water areas, with the view to reducing the flood risk, promote environmental education and physical activity (C40Cities, 2016[141]).
The traditional economic rationale for fiscal policies targeting foods and beverages depends on whether their prices fully reflect social and economic consequences of their consumption (OECD, 2010[142]). For example, it has been argued that soft drink prices may not take into account the costs associated with the medical conditions caused by overweight, including, among the others, higher cost of medical care, and losses in productivity among people who develop such conditions (Brownell et al., 2009[143]). Thus, from the social point of view, the amount of consumption of such foods may be too high. Conversely, consumption of healthy foods such as fruits and vegetables may be socially suboptimal if their prices do not reflect the positive economic effects associated with their consumption and its positive effects on the health of the population. Economic incentives, including price interventions, may be used as a useful tool to promote changes in dietary behaviours to encourage a more balanced diet.
Governments can affect food-related consumer behaviour by implementing targeted price policies. Most policy action in this field has focused on increasing the price of products high in sugar, saturated fats or salt. Such policies may also include targeted price reduction for healthier foods sold in shops (Horgen and Brownell, 2002[144]).
Among the various price policies, taxation of sugar-sweetened beverages (SSBs) is gaining particular attention. In general, evaluations of such policies have found that they do have an intended effect on consumption, with one recent systematic review and meta-analysis concluding that a 10% SSB tax was related to a 10% decline in SSB purchases and dietary intake (Teng A, Jones A, Mizdrak A, Signal L, Genç M, 2019[145]). It is also clear that the magnitude of the tax effect varies depending on the programme design, on the size of the tax and the extent of its pass-through to consumers (i.e. extent to which producers pass the tax to consumers through an increase in the price of the taxed product). For example, in Mexico, an SSB tax in the amount of 1 peso/L (about 0.05 USD/L) was almost entirely passed to the consumers, resulting in a 10% increase in the price of SSBs (Caro et al., 2018[146]) and a 6‑12% drop in per capita purchases (Colchero et al., 2016[147]). In Chile, an 8% tax difference between two SSB categories, containing high and low amounts of sugar, resulted in a price difference of 3.3%, equivalent to an additional 15 pesos (about 0.04 USD/L) for a typical 500 ml beverage (Nakamura et al., 2018[148]). As a result, monthly purchased volume was reduced as well, although the estimated effect varied between 4‑21%, depending on the methodology used (see Box 5.17). In the United States, the city of Berkeley levies tax at a rate of USD 0.01 per ounce (0.34 USD/L), equivalent to a price increase of about 8% after a pass-through of about 47% of tax, which resulted in a 21% decline in sales of SSBs in low-income neighbourhoods (Falbe et al., 2016[149]). Evidence on the long-term effect of these taxes, especially on health-related outcomes, is still based on modelling studies. For example, OECD (2010[142]) and Cecchini and Sassi (2015[150]) have both estimated that the savings from such policies are greater when a long-term perspective is taken.
Among reviewed countries, a large majority (35) do not have any health-related food taxes in place (Figure 5.8). Seventeen countries, including 13 OECD countries, tax SSBs or other foods. Some examples of taxation policies include “soda taxes” in France (Berardi et al., 2016[151]), Chile (Nakamura et al., 2018[148]; Caro et al., 2018[146]), Mexico (Colchero et al., 2016[147]), the United Kingdom (Pell et al., 2019[152]), the city of Berkeley, (Falbe et al., 2016[149]) and the State of Pennsylvania in the United States (Zhong et al., 2018[153]) (for further details on soft drink tax policy in the UK, see Box 5.18). Other examples include a tax on food high in saturated fats in Denmark (abolished in 2013) (Bødker et al., 2015[154]), or on ready-to-eat meals in Hungary (Bíró, 2015[155]).
The design of price policies should take into account potential multiple challenges. First, there should be a sufficient pass-through of the tax in the form of a price increase, as minimal changes in price are unlikely to significantly modify purchasing patterns. Second, any potential substitution effect should be taken into account as well. For example, if SSBs are taxed, people may switch to other high-calorie drinks (e.g. high-fat milks, or juices) (Jou and Techakehakij, 2012[156]; Sassi, Belloni and Capobianco, 2013[157]), increase their consumption of non-beverage foods high in sugar, or even increase purchases of alcoholic beverages (Quirmbach et al., 2018[158]). Third, if the demand curve is inelastic, then there may be little change in consumption, although, on a positive side, low elasticity may also imply little substitution with other calorie-dense foods or beverages (Sassi, Belloni and Capobianco, 2013[157]). There is also concern about the adverse economic effect of such taxes, especially on low-income groups. However, previous OECD analyses suggest that health improvements resulting from such actions may disproportionately benefit the poor (Sassi et al., 2009[159]; Sassi, Belloni and Capobianco, 2013[157]). In addition, revenues generated from the application of such taxes may be designed to benefit primarily low-income households (Sassi et al., 2018[160]).
In 2014, an SSB tax was introduced in Chile for beverages with a sugar concentration of 6.25 grams per 100 ml or more. Specifically, the tax was increased from 13% to 18% for SSBs above this threshold, while for drinks below the threshold, the tax was decreased from 13% to 10%, effectively producing an eight percentage point tax difference (OECD, 2019[26]). Unlike Mexico, where there was almost complete pass-through of the tax, in Chile the resulting price difference between the two SSB groups was considerably smaller, of about 2‑3%. In addition, in Mexico, where taxation is by volume, in Chile the tax only applies to a baseline price, and therefore there is a weaker link between the amount of sugar in a purchased drink and the amount of tax applied.
Two evaluations found a statistically significant positive effect on monthly purchased volume, with population-level effectiveness of the tax varying between 3.4% and 21%, depending on the methodology used (Caro et al., 2018[146]; Nakamura et al., 2018[148]). At the lower end of this estimate, this equates to a reduction of about 108 ml/capita per month (Caro et al., 2018[146]), and at the higher end to 766 ml per person per month (Nakamura et al., 2018[148]). Assuming that a litre of SSB contains about 400 calories, this equates to a monthly reduction of 43‑306 calories per person.
In 2018, the United Kingdom implemented a Soft Drinks Industry levy targeting all pre-packaged soft drinks containing at least 5 grams of added sugar per 100 ml of drink.
The UK tax combines features of several tax designs. For example, as with Chile, different tax rates apply depending on the amount of sugar in a given beverage: in drinks where sugar content ranges between 5‑8 g per 100 ml, a tax rate is equal to 18 pence (USD 0.23) per litre, while in drinks containing more than 8 g per 100 ml, a tax rate of 24 pence (USD 0.30) per litre applies. Similar to Mexico, it charges a set amount per litre of a beverage so that there is direct link with volume. The UK tax does not target any potential substitute of SSBs including, for example, milk-based drinks, artificially-sweetened beverages, pure fruit juices, or any other foods potentially high in calories/sugar.
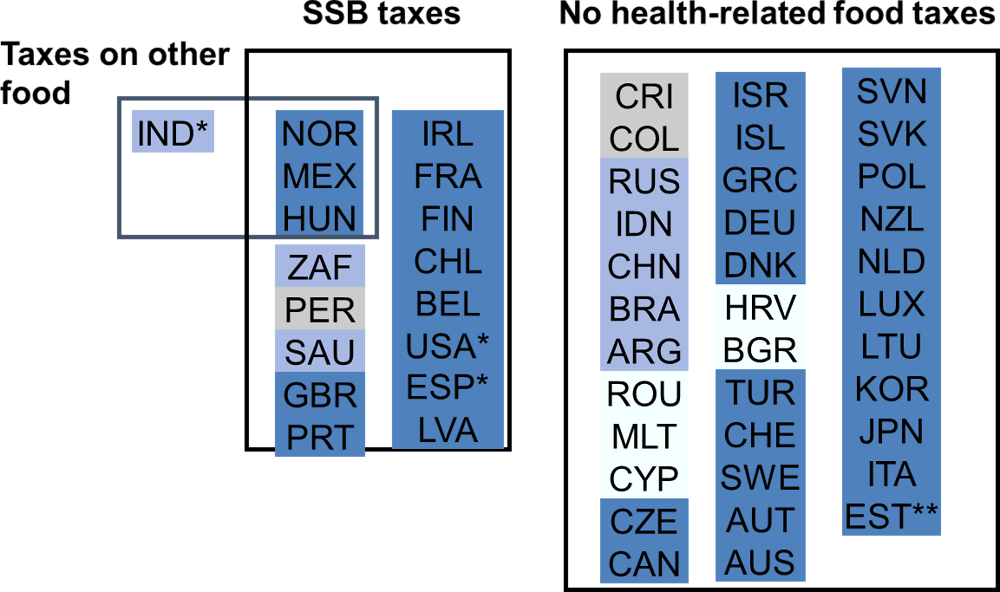
Note: OECD countries in dark blue; other G20 non-OECD countries in light blue; other EU non-OECD countries in white; other countries partnering with the OECD in grey.
* Sub-national laws; ** The Estonian Parliament has approved legislation taxing soft drinks, but this was not implemented by the government.
Source: WCRFI (2016[2]), “NOURISHING-framework” http://www.wcrf.org/int/policy/nourishing-framework; Development Initiatives (2018[3]), 2018 Global Nutrition Report: Shining a light to spur action on nutrition, https://globalnutritionreport.org/d7447a.
While much less common than other price policies, some countries also provide targeted subsidies for foods considered healthy by their nutritional profile. Some of the most widespread forms of food subsidies include vouchers for healthy meals (McFadden et al., 2014[161]) or discounts for healthier foods purchases through governmental assistance programmes (Lu et al., 2016[162]).
There is tentative evidence that price discounts and vouchers can encourage healthier food purchases, including consumption of fruits and vegetables, and low-fat and low-calorie foods, in such settings as supermarkets, university and school cafeterias, farmers’ markets and restaurants (An, 2013[163]), However, the evidence on the long-term effectiveness of such policies is still lacking.
Most of these programmes are designed to benefit specific, generally low-income population groups. For example, in New York City, the Health Bucks programme provides Supplemental Nutrition Assistance Program (SNAP) recipients with a USD 2 coupon for every USD 5 spent on fresh fruits and vegetables at participating farmers’ markets. It was found that daily sales were higher at the markets that offered this incentive to the SNAP benefit recipients, compared to markets that did not (Baronberg et al., 2013[164]). In Philadelphia, the SNAP users of a similar healthy foods subsidy programme were about 2.4 times more likely than non-users to report increased consumption of fruit and vegetables (Young et al., 2013[165]). In Canada, the Nutrition North Canada governmental programme provides subsidies to improve access for people living in isolated communities to nutritious perishable foods, including fruits and vegetables (Fieldhouse and Thompson, 2012[166]), although the programme was criticised for not ensuring that the food is affordably and equitably priced because of the lack of price caps (Galloway, 2017[167]). Another example is the US federally funded Special Supplemental Nutrition Program for Women, Infants, and Children (Box 5.19).
Similar to price policies, certain conditions have to be met for such subsidies to be effective. Most importantly, they should lead to sufficient price and consumption responses, so that such incentives do not simply translate into greater company profits. In addition, it is important to ensure that such programmes do not actually increase health inequalities (Darmon et al., 2014[168]).
Special Supplemental Nutrition Program for Women, Infants, and Children is funded by the United States federal government and is administered by all 50 states. The programme provides vouchers to buy nutritious foods, for example baby foods, fruits and vegetables, eggs, cheese, whole wheat bread and other whole wheat foods, dried and canned beans/peas at participating stores, to eligible women and their children. The eligibility criteria include being a low-income pregnant, breastfeeding or non-breastfeeding postpartum woman. In addition, the programme provides access to health screenings, nutrition and breastfeeding counselling.
The programme has existed since 1972, but was amended in 2009 by the US Department of Agriculture, to take into account the nutritional recommendations for the American Academy of Paediatrics, the American Academy of Family Physicians, and the Institute of Medicine (Lu et al., 2016[162]). The package was revised to include more nutrient-dense foods and beverages, and to limit the provision of foods high in added sugar and saturated fats. One study concluded that the 2009 changes have resulted in significant improvements in the availability and variety of healthy foods in participating stores (Andreyeva et al., 2012[169]).
There has been growing interest in the impact of economic incentives, mainly positive incentives, on the quality of the local community nutritional environment (Bowen, Barrington and Beresford, 2015[170]). Policies of this kind typically go beyond taxation of specific food items or subsidies to the individual consumers, and target food retailers. For example, there can be incentives for retailers to improve availability, accessibility and affordability of food options in their stores, or to increase the density of healthier food outlets/farmers’ markets, especially in underserved neighbourhoods.
There are important methodological challenges in consistently measuring the quality of the community food environment across different studies (Glanz et al., 2016[171]; Caspi et al., 2012[172]). However, emerging evidence indicates that the community nutritional environment is an important determinant of diet and health. For example, in a US study, the prevalence of obesity was lower for people who live in areas with easier access to food outlets that may have a greater number of healthy food options, such as supermarkets and fruit and vegetable markets (Rundle et al., 2009[173]). Likewise, in Italy, a greater density of the farmers’ markets was associated with lower BMI (Bimbo et al., 2015[174]).
A number of local initiatives designed to improve the quality of the local nutrition environment have been implemented recently. For example, the Healthy Food Financing initiative was established in 2014 in the United States, which provides financial incentives for healthier food outlets to be located in underserved neighbourhoods (Block and Subramanian, 2015[175]). In Singapore, food and beverage companies receive various incentives to provide healthier food options inside stores through the Healthier Dining Programme established in 2014 (HPB, 2019[176]).
Food marketing represents a key factor incentivising the consumption of high-calorie and nutrient-poor foods through persuasive messages (Adams et al., 2012[177]). Advertising restrictions typically take the form of a ban on commercial advertising for certain products during peak viewing time for children, although the target age of the affected children can vary (e.g., under 12 years of age in Sweden, or 14 years of age in Chile).
Studies suggest that statutory restrictions on commercial food advertising and promotion can have a significant effect on dietary intake. For example, in Quebec, the implementation of this policy was followed by a reduction in calorie consumption at fast-food restaurants of between 5.6 billion and 7.8 billion per year (Dhar and Baylis, 2011[178]). Another study in Australia concluded that banning television advertising for energy-dense food during children’s peak viewing times was highly cost-effective (Magnus et al., 2009[179]). On the other hand, a systematic review concluded that voluntary pledges to restrict high-calorie advertising may not be as effective in reducing exposure of children to advertisements, which may be due to the lack of enforceability or penalties for non-compliance (Galbraith‐Emami and Lobstein, 2013[28]).
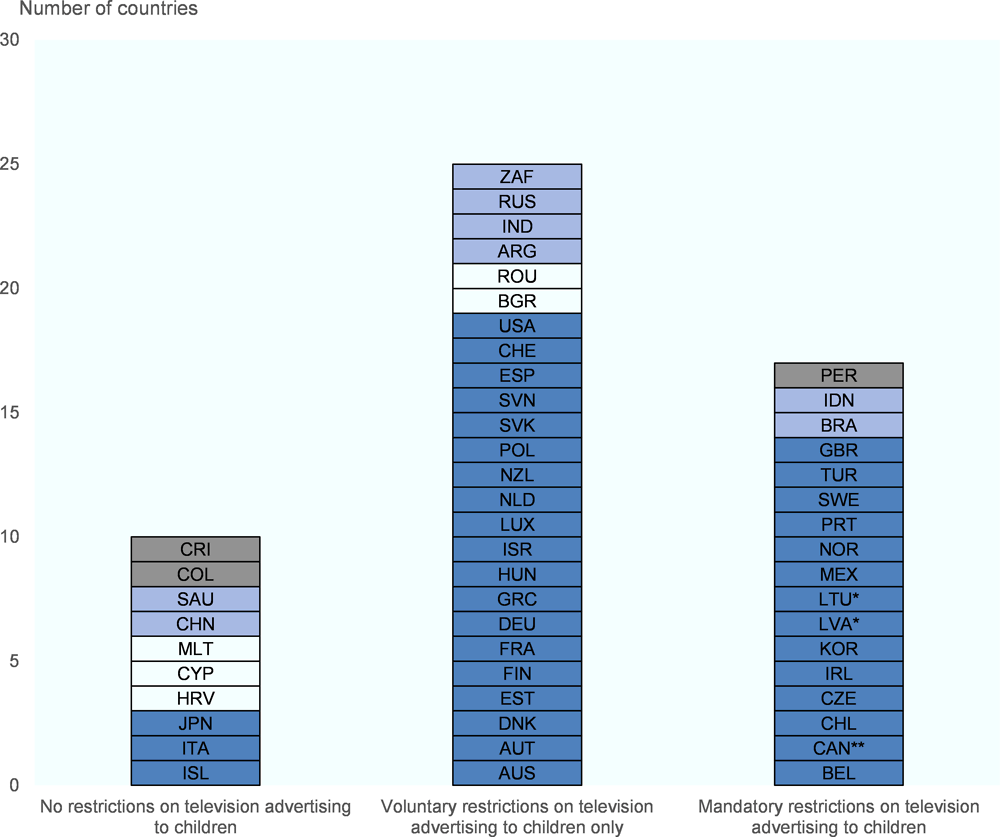
Note: OECD countries in dark blue; other G20 non-OECD countries in light blue; other EU non-OECD countries in white; other countries partnering with the OECD in grey.
* Mandatory regulation only applies to energy drinks; ** Province-level regulation (Quebec). In addition, voluntary industry framework applies across the whole country.
Source: WCRFI (2016[2]), “NOURISHING-framework” http://www.wcrf.org/int/policy/nourishing-framework; WHO (2012[4]), Global database on the Implementation of Nutrition Action (GINA), https://www.who.int/nutrition/gina/en/; Boyland et al. (2018[180]), “Evaluating implementation of the WHO Set of Recommendations on the marketing of foods and non-alcoholic beverages to children”.
Despite the public health guidance put in place by WHO (2010), relatively few countries (17) have implemented statutory advertising restrictions concerning diet targeting children, while in ten countries there are no restrictions whatsoever (Figure 5.9). In some countries, for example Chile, Korea, and Brazil, advertising restrictions extend to non-broadcast media as well, e.g. social media and the internet in general. France has established that any potentially unhealthy food and beverage advertising must be accompanied by a message emphasising principles of dietary education (Hawkes, 2007[181]).
The largest group of countries (25) has instead preferred to let food manufacturers adopt self-regulation, although it has been argued that this approach usually does not go far enough (Galbraith‐Emami and Lobstein, 2013[28]). For example, in Denmark, a self-regulation code has been in place since 2008 through “The Forum of Responsible Food Marketing Communication” (see also Box 5.20). In Norway, the government restricts advertising targeting children on broadcast channels, but restriction of advertising on other channels, such as cinemas, internet and the press is only on a voluntary basis (Hawkes, 2007[181]). In the European Union, a voluntary pledge was launched in 2007 to commit the food industry to not advertise calorie-dense food on media channels where children under the age of 12 make up at least 35% of the audience (Galbraith‐Emami and Lobstein, 2013[28]). In addition, the Audiovisual Media Services Directive is expected to come into force soon in the European Union, setting out the framework for the EU-wide cooperation on national legislation in a number of areas covering all audiovisual media, including protecting children from inappropriate advertising of foods high in salt, sugar and fat (European Commission, 2019[182]).
In 2008, the Forum of Responsible Food Marketing Communication implemented the Danish Code of Responsible Food Marketing Communication, a co-operation between Danish food and beverage industries, and the retail and media sectors. The code targets the marketing of products with a high content of sugar, fats and salt to children via television, printed media and the internet (Kelly et al., 2015[183]).
The Code is a self-regulatory initiative, targeting food and beverage marketing for children aged 13 and under. According to the Code, products which exceed guideline limits for salt, sugar and fat content in ten food categories should not be marketed, with the responsibility to observe the code resting on food manufacturers themselves, and the compliance checked by the secretariat of the Forum. Members of the Forum of Responsible Food Marketing Communication meet two to three times a year to discuss progress, coordinate activities and evaluate potential violations.
There has been some criticism in relation to the voluntary nature of the code, and in particular on the relatively low age limit applicable to such advertisements, 13 years old. To compare, in the United Kingdom the limit is 16 years old and in Ireland it is 18 years old (WHO, 2010[184]). Another criticism is that certain forms of advertising are excluded, such as sponsorships and outdoor advertising (Cathaoir, 2017[185]). Nevertheless, it was reported that the number of advertisements in the media covered by the agreement and for relevant products has fallen markedly since the establishment of the code (Chafea, 2016[186]).
In some cases, there may be a need for more stringent regulatory restrictions. Typically, such restrictions will apply to specific foods with potentially harmful properties, such as foods containing trans fats, especially industrially-produced ones (see Box 5.21). In general, trans fats are not present in foods in their natural form, but are added for other reasons, such as to enhance food taste, texture and shelf life. Trans fats also have attractive properties from the food-manufacturing point of view, as they can be solid at room temperature and melt when cooking. The main issue with trans fats is not that they promote overweight, although some tentative evidence indicates that it may be a risk factor (Astrup et al., 2008[187]), but rather that there is a direct link between trans fat consumption and such outcomes as heart disease (Stender and Dyerberg, 2004[188]). Therefore, there is a strong need for policies requiring industrial reformulation of foods that currently contain trans fats.
Starting from 2018, US and Canadian food manufacturers and restaurants can no longer produce foods containing partially hydrogenated oils (PHOs), which are primary sources of trans fats. In the case of the United States, the ban came into force after a decade of working with the food industry to voluntarily reduce, and eliminate, the use of artificial trans fats. Several other countries, for example, Chile, also have strict limits on the amount of trans fats, such as no more than 2% of the total fat content. In the European Union, recently adopted Regulation 2019/649 stipulates that industrially produced trans fats in foods intended for final consumption shall not exceed 2g per 100g of fat (European Commission, 2019[189]). There are also examples of voluntary initiatives such as in the United Kingdom, where several supermarkets pledged in 2012 to work towards voluntary removal of products containing artificial trans fats from their shelves. One evaluation found that the effect of such voluntary policy was negligible (Knai et al., 2017[190]). On the other hand, a study attributed a reduction in CVD mortality rates observed in Denmark in recent years to the mandatory policy implemented in 2004 which restricted the content of artificial trans fats in certain food products (Restrepo and Rieger, 2016[191]).
There are also examples of community regulations restricting the availability of calorie-dense foods. In a number of cities in California, restaurants are required to offer plain, sparkling or flavoured water, with no added natural or artificial sweeteners, milk or non-dairy milk alternatives as the default beverage in children’s meals (Natlawreview.com, 2019[192]). In France, unlimited offers of sweetened beverages have been banned in schools and restaurants since 2017 (BBC, 2017[193]). In the United Kingdom, a number of local authorities have developed planning restrictions to exclude hot food takeaways less than 400 meters away from target locations such as schools (London.gov.uk, 2017[194]).
Recently, the International Food and Beverage Alliance (IFBA) has committed to phasing out industrially-processed trans fats from the global food supply by 2023. IFBA was founded in 2008, with one of its stated aims being to support WHO’s efforts to improve global public health. IFBA has made a series of other core commitments over the years, including to support WHO’s 2004 Global Strategy on Diet, Physical Activity and Health and the 2011 UN Declaration on the Prevention and Control of NCDs.
Specifically, IFBA has declared that its member companies will commit not to exceed 2 g of industrial trans fats per 100 g fat/oil in their products worldwide by 2023. Eliminating artificial trans fats from the global food supply is one of the WHO’s current priority targets (WHO, 2019[195]).
Countries have made substantial progress in setting up and implementing a variety of policy measures to address overweight, largely by tackling poor diet and nutrition and lack of physical activity. As of 2019, virtually all OECD countries have a national action plan on obesity in place, and a vast majority of countries has a specific action plan to tackle obesity in children as well as national guidelines to promote healthy diets and active lifestyles. Most OECD countries have also implemented a wide range of policy options to promote healthier lifestyles. Despite this undeniable progress, the still rising overweight rates point to the fact that the response has not yet been up to the challenge. The implementation of policies “on the ground” and their effectiveness at the population level is hindered by a number of factors. In a number of cases, policies are implemented in non-effective ways or actions are not uniformly implemented throughout the country. In other cases, limited resources or practical problems end up restricting the number of individuals who could potentially benefit from the policy.
Public health interventions often represent good value for money, but resource allocation tends to favour treatment-related approaches. The reasons for these are often political (e.g., it may be more popular to promise spending on hospitals or on doctors, than to increase taxes on calorie-dense and/or ultra-processed foods). However, there should be an honest discussion on the long-term sustainability of this approach. In addition, there should be better understanding of the economic benefits of prevention (which will include not only saved costs from treatment, but also economic benefits from better productivity). Moreover, the implementation of effective prevention interventions can help relieve the long-term pressure facing the health care sector, allowing it to focus on more complex medical issues. Health care interventions can still be appropriate for people with severe obesity, but the right balance between prevention and treatment must be found for the other groups.
Moving forward, there is a need to prioritise resources going into prevention, which, as discussed in Chapter 6, is often a highly cost-effective investment. In addition, better understanding of which specific design feature of policies works best is needed. To ensure policy inception and implementation, it is important to work extensively with multiple stakeholders, both in other governmental and non-governmental agencies, and in the private sector, as appropriate. Broadly speaking, even though win-win solutions will not always be attainable, cross-sectorial co-operation addressing co-benefits and return on investments into obesity prevention policies are crucial for successful policy implementation.
[177] Adams, J. et al. (2012), “Effect of restrictions on television food advertising to children on exposure to advertisements for ‘less healthy’foods: repeat cross-sectional study”, PloS one, Vol. 7/2, p. e31578.
[25] Aecosan (2019), NAOS Strategy Awards, http://www.aecosan.msssi.gob.es/en/AECOSAN/web/nutricion/seccion/Premios_NAOS.htm.
[50] Afshin, A. et al. (2015), “CVD prevention through policy: a review of mass media, food/menu labeling, taxation/subsidies, built environment, school procurement, worksite wellness, and marketing standards to improve diet”, Current cardiology reports, Vol. 17/11, p. 98.
[60] Afshin, A. et al. (2017), The prospective impact of food pricing on improving dietary consumption: A systematic review and meta-analysis, http://dx.doi.org/10.1371/journal.pone.0172277.
[90] Aittasalo, M. et al. (2006), “A randomized intervention of physical activity promotion and patient self-monitoring in primary health care”, Preventive medicine, Vol. 42/1, pp. 40-46.
[92] Allan, J. et al. (2004), Clinical prevention and population health: Curriculum framework for health professions, http://dx.doi.org/10.1016/j.amepre.2004.08.010.
[120] Allan, J. et al. (2017), Environmental interventions for altering eating behaviours of employees in the workplace: a systematic review, http://dx.doi.org/10.1111/obr.12470.
[169] Andreyeva, T. et al. (2012), “Positive Influence of the Revised Special Supplemental Nutrition Program for Women, Infants, and Children Food Packages on Access to Healthy Foods”, Journal of the Academy of Nutrition and Dietetics, http://dx.doi.org/10.1016/j.jand.2012.02.019.
[163] An, R. (2013), Effectiveness of subsidies in promoting healthy food purchases and consumption: A review of field experiments, http://dx.doi.org/10.1017/S1368980012004715.
[46] Antonelli, R. and A. Viera (2015), “Potential effect of physical activity calorie equivalent (PACE) labeling on adult fast food ordering and exercise”, PloS one, Vol. 10/7, p. e0134289.
[88] Arsenijevic, J. and W. Groot (2017), Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses, http://dx.doi.org/10.1136/bmjopen-2016-012156.
[187] Astrup, A. et al. (2008), Nutrition transition and its relationship to the development of obesity and related chronic diseases, http://dx.doi.org/10.1111/j.1467-789X.2007.00438.x.
[122] Baicker, K., D. Cutler and Z. Song (2010), “Workplace wellness programs can generate savings”, Health Affairs, http://dx.doi.org/10.1377/hlthaff.2009.0626.
[164] Baronberg, S. et al. (2013), “The Impact of New York City’s Health Bucks Program on Electronic Benefit Transfer Spending at Farmers Markets, 2006–2009”, Preventing Chronic Disease, http://dx.doi.org/10.5888/pcd10.130113.
[35] Barreiro-Hurlé, J., A. Gracia and T. De-Magistris (2010), “Does nutrition information on food products lead to healthier food choices?”, Food Policy, Vol. 35/3, pp. 221-229.
[193] BBC (2017), “Free soda: France bans unlimited sugary drink refills”, https://www.bbc.com/news/world-europe-38767941.
[151] Berardi, N. et al. (2016), “The impact of a ‘soda tax’ on prices: evidence from French micro data”, Applied Economics, http://dx.doi.org/10.1080/00036846.2016.1150946.
[137] bewegt-im-park.at (2019), Wie funktioniert BEWEGT IM PARK?, https://www.bewegt-im-park.at/wie-funktioniert-bewegt-im-park/.
[174] Bimbo, F. et al. (2015), “The hidden benefits of short food supply chains: Farmers’ markets density and body mass index in Italy”, International Food and Agribusiness Management Review.
[155] Bíró, A. (2015), “Did the junk food tax make the Hungarians eat healthier?”, Food Policy, http://dx.doi.org/10.1016/j.foodpol.2015.05.003.
[49] Bleich, S. et al. (2015), “Restaurants with calories displayed on menus had lower calorie counts compared to restaurants without such labels”, Health affairs, Vol. 34/11, pp. 1877-1884.
[48] Block, J. and C. Roberto (2014), “Potential benefits of calorie labeling in restaurants”, Jama, Vol. 312/9, pp. 887-888.
[175] Block, J. and S. Subramanian (2015), “Moving Beyond “Food Deserts”: Reorienting United States Policies to Reduce Disparities in Diet Quality”, PLoS Medicine, http://dx.doi.org/10.1371/journal.pmed.1001914.
[136] Bloomberg New Energy Finance (2018), Electric Buses in Cities. Driving Towards Cleaner Air and Lower CO2, https://c40-production-images.s3.amazonaws.com/other_uploads/images/1726_BNEF_C40_Electric_buses_in_cities_FINAL_APPROVED_%282%29.original.pdf?1523363881.
[154] Bødker, M. et al. (2015), “The Danish fat tax-Effects on consumption patterns and risk of ischaemic heart disease”, Preventive Medicine, http://dx.doi.org/10.1016/j.ypmed.2015.03.031.
[29] Borgmeier, I. and J. Westenhoefer (2009), “Impact of different food label formats on healthiness evaluation and food choice of consumers: A randomized-controlled study”, BMC Public Health, http://dx.doi.org/10.1186/1471-2458-9-184.
[170] Bowen, D., W. Barrington and S. Beresford (2015), “Identifying the Effects of Environmental and Policy Change Interventions on Healthy Eating”, SSRN, http://dx.doi.org/10.1146/annurev-publhealth-032013-182516.
[180] Boyland, E. et al. (2018), Evaluating implementation of the WHO Set of Recommendations on the marketing of foods and non-alcoholic beverages to children, The World Health Organization, Regional Office for Europe.
[111] bridgingthegapresearch.org (2013), State Laws for School Snack Foods and Beverages, http://foods.bridgingthegapresearch.org/#ng10s/2012/AR.
[143] Brownell, K. et al. (2009), “The Public Health and Economic Benefits of Taxing Sugar-Sweetened Beverages”, New England Journal of Medicine, http://dx.doi.org/10.1056/NEJMhpr0905723.
[103] Brown, H. et al. (2014), “Family-based interventions to increase physical activity in children: A meta-analysis and realist synthesis protocol”, BMJ Open, http://dx.doi.org/10.1136/bmjopen-2014-005439.
[138] C40 (2019), C40 Cities, https://www.c40.org/about.
[140] C40Cities (2016), Benefits of Climate Action: Piloting A Global Approach To Measurement. Appendix., https://www.c40.org/researches/measuring-benefits-appendix.
[141] C40Cities (2016), Cities100: Chicago - Adsorptive Playgrounds Foster Social Cohesion, https://www.c40.org/case_studies/cities100-chicago-adsorptive-playgrounds-foster-social-cohesion.
[139] C40Cities (2016), Good Practice Guide. Bus Rapid Transit, C40 Cities Climate Leadership Group, https://www.c40.org/case_studies/c40-good-practice-guides-istanbul-metrobus-system.
[114] Caldeira, S. et al. (2017), Public Procurement of Food for Health., Luxembourg: Publications Office of the European Union.
[85] Campbell, F. et al. (2015), “A systematic review and economic evaluation of exercise referral schemes in primary care: A short report”, Health technology assessment, Vol. 19/60.
[31] Campos, S., J. Doxey and D. Hammond (2011), “Nutrition labels on pre-packaged foods: a systematic review”, Public health nutrition, Vol. 14/08, pp. 1496-1506.
[146] Caro, J. et al. (2018), “Chile’s 2014 sugar-sweetened beverage tax and changes in prices and purchases of sugar-sweetened beverages: An observational study in an urban environment”, PLoS Medicine, http://dx.doi.org/10.1371/journal.pmed.1002597.
[172] Caspi, C. et al. (2012), “The local food environment and diet: A systematic review”, Health and Place, http://dx.doi.org/10.1016/j.healthplace.2012.05.006.
[185] Cathaoir, K. (2017), Food Marketing to Children in Sweden and Denmark: A Missed Opportunity for Nordic Leadership, http://dx.doi.org/10.1017/err.2017.24.
[150] Cecchini, M. and F. Sassi (2015), “Preventing Obesity in the USA: Impact on Health Service Utilization and Costs”, PharmacoEconomics, http://dx.doi.org/10.1007/s40273-015-0301-z.
[34] Cecchini, M. and L. Warin (2016), “Impact of food labelling systems on food choices and eating behaviours: a systematic review and meta‐analysis of randomized studies”, obesity reviews, Vol. 17/3, pp. 201-210, http://dx.doi.org/10.1111/obr.12364.
[186] Chafea (2016), Study on the impact of marketing through social media, online games and mobile applications on children’s behaviour, http://file:///C:/Users/Goryakin_Y/Downloads/Study_on_the_impact_of_marketing_through.pdf.
[42] Chantal, J. and S. Hercberg (2017), “Development of a new front-of-pack nutrition label in France: the five-colour Nutri-Score”, Public Health Panorama.
[10] Chokshi, D. and T. Farley (2012), “The Cost-Effectiveness of Environmental Approaches to Disease Prevention”, New England Journal of Medicine, http://dx.doi.org/10.1056/nejmp1206268.
[121] Chu, A. et al. (2016), “A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers”, Obesity Reviews, http://dx.doi.org/10.1111/obr.12388.
[125] Civil Service Employee Assistance Service (2018), National Workplace Wellbeing Day, https://www.cseas.per.gov.ie/national-workplace-wellbeing-day-april-13th-2018/.
[55] Cleveland, L., D. Simon and J. Block (2018), “Compliance in 2017 with federal calorie labeling in 90 chain restaurants and 10 retail food outlets prior to required implementation”, American Journal of Public Health, http://dx.doi.org/10.2105/AJPH.2018.304513.
[147] Colchero, M. et al. (2016), “Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: Observational study”, BMJ (Online), http://dx.doi.org/10.1136/bmj.h6704.
[104] Coleman, K. et al. (2005), “Prevention of the epidemic increase in child risk of overweight in low-income schools: The El Paso coordinated approach to child health”, Archives of Pediatrics and Adolescent Medicine, http://dx.doi.org/10.1001/archpedi.159.3.217.
[9] Connell, P., M. Brucks and J. Nielsen (2014), “How Childhood Advertising Exposure Can Create Biased Product Evaluations That Persist into Adulthood”, Journal of Consumer Research, http://dx.doi.org/10.1086/675218.
[22] Daniel B. Kline (2018), PepsiCo Continues Its Push Into Healthy Snacks, https://www.fool.com/investing/2018/06/01/pepsico-continues-its-push-into-healthy-snacks.aspx.
[168] Darmon, N. et al. (2014), “Food price policies improve diet quality while increasing socioeconomic inequalities in nutrition”, International Journal of Behavioral Nutrition and Physical Activity, http://dx.doi.org/10.1186/1479-5868-11-66.
[57] Dell, E. (2018), Calorie Disclosure, https://www.vendingmarketwatch.com/home/article/12414882/calorie-disclosure (accessed on 22 July 2019).
[23] Department of Health & Social Care (2016), “Childhood Obesity: A Plan For Action”, HM Government, http://dx.doi.org/10.7748/ns.31.1.15.s17.
[1] Devaux, M. et al. (2019), “Assessing the potential outcomes of achieving the World Health Organization global non-communicable diseases targets for risk factors by 2025: is there also an economic dividend?”, Public Health, http://dx.doi.org/10.1016/j.puhe.2019.02.009.
[3] Development Initiatives (2018), 2018 Global Nutrition Report: Shining a light to spur action on nutrition, Development Initiatives, Bristol, UK, https://globalnutritionreport.org/d7447a.
[178] Dhar, T. and K. Baylis (2011), “Fast-food consumption and the ban on advertising targeting children: the Quebec experience”, Journal of Marketing Research, Vol. 48/5, pp. 799-813.
[8] Drewnowski, A. and S. Specter (2004), Poverty and obesity: The role of energy density and energy costs.
[109] EC (2019), School fruit, vegetables and milk scheme, https://ec.europa.eu/agriculture/school-scheme_en.
[80] Elliot, C. and M. Hamlin (2018), “Combined diet and physical activity is better than diet or physical activity alone at improving health outcomes for patients in New Zealand’s primary care intervention”, BMC Public Health, http://dx.doi.org/10.1186/s12889-018-5152-z.
[89] Estabrooks, P., R. Glasgow and D. Dzewaltowski (2003), “Physical activity promotion through primary care”, Jama, Vol. 289/22, pp. 2913-2916.
[38] EUFIC (2018), Global Update on Nutrition Labelling.
[115] EU-JRC (2015), School food policy country factsheets, European Commission - JRC Science Hub.
[189] European Commission (2019), COMMISSION REGULATION (EU) 2019/649 of 24 April 2019 amending Annex III to Regulation (EC) No 1925/2006 of the European Parliament and of the Council as regards trans fat, other than trans fat naturally occurring in fat of animal origin, https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32019R0649&from=EN.
[93] European Commission (2019), EUPAP - An European Physical Activity on Prescription model, https://webgate.ec.europa.eu/chafea_pdb/health/projects/847174/summary.
[108] European Commission (2019), Initiatives on Nutrition and Physical Activity, https://ec.europa.eu/health/sites/health/files/nutrition_physical_activity/docs/2019_initiatives_npa_en.pdf.
[182] European Commission (2019), Revision of the Audiovisual Media Services Directive (AVMSD), https://ec.europa.eu/digital-single-market/en/revision-audiovisual-media-services-directive-avmsd.
[107] European Commission (2018), Opinion of the High Level Group on Nutrition and Physical Activity, https://ec.europa.eu/health/sites/health/files/nutrition_physical_activity/docs/hlg_opinion_addedsugars_school_fruitvegetablesmmilkscheme_en.pdf.
[149] Falbe, J. et al. (2016), “Impact of the Berkeley excise tax on sugar-sweetened beverage consumption”, American Journal of Public Health, http://dx.doi.org/10.2105/AJPH.2016.303362.
[133] Fan, M. and Y. Jin (2014), “Do neighborhood parks and playgrounds reduce childhood obesity?”, American Journal of Agricultural Economics, http://dx.doi.org/10.1093/ajae/aat047.
[117] FAO (2019), Nutrition guidelines and standards for school meals: a report from 33 low and middle-income countries., CC BY-NC-SA 3.0 IGO., Rome.
[18] Feigl, A. et al. (2019), “The short-term effect of BMI, alcohol use, and related chronic conditions on labour market outcomes: A time-lag panel analysis utilizing European SHARE dataset”, PLoS ONE, http://dx.doi.org/10.1371/journal.pone.0211940.
[52] Fernandes, A. et al. (2016), “Influence of menu labeling on food choices in real-life settings: a systematic review”, Nutrition reviews, Vol. 74/8, pp. 534-548.
[166] Fieldhouse, P. and S. Thompson (2012), “Tackling food security issues in indigenous communities in Canada: The Manitoba experience”, Nutrition and Dietetics, http://dx.doi.org/10.1111/j.1747-0080.2012.01619.x.
[28] Galbraith‐Emami, S. and T. Lobstein (2013), “The impact of initiatives to limit the advertising of food and beverage products to children: a systematic review”, obesity reviews, Vol. 14/12, pp. 960-974.
[167] Galloway, T. (2017), “Canada’s northern food subsidy nutrition north Canada: A comprehensive program evaluation”, International Journal of Circumpolar Health, http://dx.doi.org/10.1080/22423982.2017.1279451.
[119] Geaney, F. et al. (2016), “The effect of complex workplace dietary interventions on employees’ dietary intakes, nutrition knowledge and health status: A cluster controlled trial”, Preventive Medicine, http://dx.doi.org/10.1016/j.ypmed.2016.05.005.
[171] Glanz, K. et al. (2016), “Measures of Retail Food Store Environments and Sales: Review and Implications for Healthy Eating Initiatives”, Journal of Nutrition Education and Behavior, http://dx.doi.org/10.1016/j.jneb.2016.02.003.
[63] Goryakin, Y. et al. (2017), The Role of Communication in Public Health Policies: the Case of Obesity Prevention in Italy, http://www.salute.gov.it/imgs/C_17_pubblicazioni_2647_allegato.pdf.
[83] Goryakin, Y., L. Suhlrie and M. Cecchini (2018), “Impact of primary care-initiated interventions promoting physical activity on body mass index: Systematic review and meta-analysis”, Obesity Reviews, http://dx.doi.org/10.1111/obr.12654.
[113] Gregorič, M. et al. (2015), “School nutrition guidelines: Overview of the implementation and evaluation”, Public Health Nutrition, http://dx.doi.org/10.1017/S1368980014003310.
[82] Grossman, D. et al. (2017), Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adultswithout cardiovascular risk factors: US preventive services task force recommendation statement, http://dx.doi.org/10.1001/jama.2017.7171.
[39] Grunert, K. and J. Wills (2008), “Pan-European Consumer Research on In-store Observation, Understanding & Use of Nutrition Information on Food Labels, Combined with Assessing Nutrition Knowledge”, Brussels: European Food Information Council.
[33] Grunert, K. and J. Wills (2007), “A review of European research on consumer response to nutrition information on food labels”, Journal of Public Health, Vol. 15/5, pp. 385-399.
[71] Hall, A., H. Cole-Lewis and J. Bernhardt (2015), “Mobile Text Messaging for Health: A Systematic Review of Reviews”, SSRN, http://dx.doi.org/10.1146/annurev-publhealth-031914-122855.
[64] Haraldsdóttir, J. (1999), “Dietary guidelines and patterns of intake in Denmark”, British Journal of Nutrition, http://dx.doi.org/10.1017/s0007114599000884.
[181] Hawkes, C. (2007), Marketing Food to Children: Changes in the Global Regulatory Environment 2004-2006, https://www.who.int/dietphysicalactivity/regulatory_environment_CHawkes07.pdf.
[11] Hawkes, C. et al. (2015), Smart food policies for obesity prevention, http://dx.doi.org/10.1016/S0140-6736(14)61745-1.
[36] Hawley, K. et al. (2013), The science on front-of-package food labels, http://dx.doi.org/10.1017/S1368980012000754.
[27] Healthy Food Partnership (2018), “Healthy Food Partnership Reformulation Program: Evidence Informing the Approach, Draft Targets and Modelling Outcomes”.
[87] Hebert, J. et al. (1999), “A dietitian-delivered group nutrition program leads to reductions in dietary fat, serum cholesterol, and body weight: The Worcester Area Trial for Counseling in Hyperlipidemia (WATCH)”, Journal of the American Dietetic Association, http://dx.doi.org/10.1016/S0002-8223(99)00136-4.
[144] Horgen, K. and K. Brownell (2002), “Comparison of price change and health message interventions in promoting healthy food choices”, Health Psychology, http://dx.doi.org/10.1037/0278-6133.21.5.505.
[176] HPB (2019), Healthier Dining Grant Schemes, https://www.hpb.gov.sg/healthy-living/food-beverage/healthier-dining-grant-schemes.
[72] Hutchesson, M. et al. (2015), “eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis”, Obesity Reviews, http://dx.doi.org/10.1111/obr.12268.
[156] Jou, J. and W. Techakehakij (2012), “International application of sugar-sweetened beverage (SSB) taxation in obesity reduction: Factors that may influence policy effectiveness in country-specific contexts”, Health Policy, http://dx.doi.org/10.1016/j.healthpol.2012.05.011.
[94] Kallings, L. (2016), “The Swedish approach on physical activity on prescription”, HEPA, Vol. 6, https://www.clinhp.org/ifile/Vol6_Supplement2_HEPA_p31_p33.pdf.
[95] Kallings, L. et al. (2008), “Physical activity on prescription in primary health care: A follow-up of physical activity level and quality of life”, Scandinavian Journal of Medicine and Science in Sports, http://dx.doi.org/10.1111/j.1600-0838.2007.00678.x.
[37] Kelly, B. and J. Jewell (2018), What is the evidence on the policy specifications, development processes and effectiveness of existing front-of-pack food labelling policies in the WHO European Region?, WHO Regional Office for Europe 8 (Health Evidence Network (HEN) synthesis report 61), Copenhagen.
[183] Kelly, B. et al. (2015), New Media but Same Old Tricks: Food Marketing to Children in the Digital Age, http://dx.doi.org/10.1007/s13679-014-0128-5.
[190] Knai, C. et al. (2017), “An evaluation of a public-private partnership to reduce artificial trans fatty acids in England, 2011-16”, European Journal of Public Health, http://dx.doi.org/10.1093/eurpub/ckx002.
[56] Krieger, J. et al. (2013), “Menu labeling regulations and calories purchased at chain restaurants”, American journal of preventive medicine, Vol. 44/6, pp. 595-604.
[106] Kuhnapato.si (2019), Kids to kids – Let’s prepare an healthy traditional meal, https://www.kuhnapato.si/files/TEKMOVANJE8/evaluation-report.pdf.
[126] Lambert, E. and T. Kolbe-Alexander (2013), “Innovative strategies targeting obesity and non-communicable diseases in South Africa: What can we learn from the private healthcare sector?”, Obesity Reviews, http://dx.doi.org/10.1111/obr.12094.
[68] Leahey, T. et al. (2016), “A randomized controlled trial testing an Internet delivered cost–benefit approach to weight loss maintenance”, Preventive Medicine, http://dx.doi.org/10.1016/j.ypmed.2016.04.013.
[14] Lean, M., A. Astrup and S. Roberts (2018), “Making progress on the global crisis of obesity and weight management”, BMJ (Online), http://dx.doi.org/10.1136/bmj.k2538.
[76] lebensmittellupe.at (2019), Lebensmittel uter der Lupe, https://lebensmittellupe.at/index.php?id=1577.
[67] Levy, L. (2013), “Dietary strategies, policy and cardiovascular disease risk reduction in England”, Proc Nutr Soc, Vol. 72/4, pp. 386-389.
[86] Lin, J. et al. (2010), “Behavioral counseling to promote physical activity and a healthful diet to prevent cardiovascular disease in adults: a systematic review for the US Preventive Services Task Force”, Annals of internal medicine, Vol. 153/11, pp. 736-750.
[194] London.gov.uk (2017), Mayor cracks down on opening of new hot-food takeaways around schools, https://www.london.gov.uk/press-releases/mayoral/mayor-cracks-down-on-new-takeaways-near-schools.
[15] Lorenc, T. et al. (2013), “What types of interventions generate inequalities? Evidence from systematic reviews”, Journal of Epidemiology and Community Health, http://dx.doi.org/10.1136/jech-2012-201257.
[162] Lu, W. et al. (2016), “Evaluating the Influence of the Revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Food Allocation Package on Healthy Food Availability, Accessibility, and Affordability in Texas”, Journal of the Academy of Nutrition and Dietetics, http://dx.doi.org/10.1016/j.jand.2015.10.021.
[179] Magnus, A. et al. (2009), “The cost-effectiveness of removing television advertising of high-fat and/or high-sugar food and beverages to Australian children”, International Journal of Obesity, Vol. 33/10, pp. 1094-1102.
[43] Mah, C. et al. (2013), “Ready for policy? Stakeholder attitudes toward menu labelling in Toronto, Canada”, Can J Public Health, Vol. 104/3, pp. e229-34.
[131] Martin, A., Y. Goryakin and M. Suhrcke (2014), “Does active commuting improve psychological wellbeing? Longitudinal evidence from eighteen waves of the British Household Panel Survey”, Preventive Medicine, Vol. 69, http://dx.doi.org/10.1016/j.ypmed.2014.08.023.
[129] Martin, A. et al. (2015), “Impact of changes in mode of travel to work on changes in body mass index: Evidence from the British Household Panel Survey”, Journal of Epidemiology and Community Health, http://dx.doi.org/10.1136/jech-2014-205211.
[124] McCoy, K. et al. (2014), “Health Promotion in Small Business”, Journal of Occupational and Environmental Medicine, http://dx.doi.org/10.1097/jom.0000000000000171.
[161] McFadden, A. et al. (2014), “Can food vouchers improve nutrition and reduce health inequalities in low-income mothers and young children: A multi-method evaluation of the experiences of beneficiaries and practitioners of the Healthy Start programme in England”, BMC Public Health, http://dx.doi.org/10.1186/1471-2458-14-148.
[98] Milanurbanfoodpolicypact (2019), Milan Urban Food Policy Pact, http://www.milanurbanfoodpolicypact.org/.
[41] Ministère des Solidarités et de la Santé (2017), EVALUATION EX ANTE DE SYSTEMES D’ETIQUETAGE NUTRITIONNEL GRAPHIQUE SIMPLIFIE, https://solidarites-sante.gouv.fr/IMG/pdf/rapport_comite_scientifique_etiquetage_nutritionnel_150317.pdf.
[97] Montes, F. et al. (2012), “Do health benefits outweigh the costs of mass recreational programs? an economic analysis of four ciclovía programs”, Journal of Urban Health, http://dx.doi.org/10.1007/s11524-011-9628-8.
[45] Morley, B. et al. (2013), “What types of nutrition menu labelling lead consumers to select less energy-dense fast food? An experimental study”, Appetite, Vol. 67, pp. 8-15.
[148] Nakamura, R. et al. (2018), “Evaluating the 2014 sugar-sweetened beverage tax in Chile: An observational study in urban areas”, PLoS Medicine, http://dx.doi.org/10.1371/journal.pmed.1002596.
[105] Nathan, N. et al. (2012), “Effectiveness of a multi-strategy intervention in increasing the implementation of vegetable and fruit breaks by Australian primary schools: A non-randomized controlled trial”, BMC Public Health, http://dx.doi.org/10.1186/1471-2458-12-651.
[192] Natlawreview.com (2019), State of California Passes Law Limiting Sugary Drinks Offered in Children’s Meals, https://www.natlawreview.com/article/state-california-passes-law-limiting-sugary-drinks-offered-children-s-meals.
[66] Neter, E. and E. Brainin (2012), “eHealth literacy: extending the digital divide to the realm of health information.”, Journal of medical Internet research, http://dx.doi.org/10.2196/jmir.1619.
[75] Neubeck, L. et al. (2015), The mobile revolution-using smartphone apps to prevent cardiovascular disease, http://dx.doi.org/10.1038/nrcardio.2015.34.
[51] Nikolaou, C., M. Lean and C. Hankey (2014), “Calorie-labelling in catering outlets: acceptability and impacts on food sales”, Preventive medicine, Vol. 67, pp. 160-165.
[58] Niven, P. et al. (2019), “Effects of health star labelling on the healthiness of adults’ fast food meal selections: An experimental study”, Appetite, http://dx.doi.org/10.1016/j.appet.2019.01.018.
[101] Nooijen, C. et al. (2017), Effectiveness of interventions on physical activity in overweight or obese children: a systematic review and meta-analysis including studies with objectively measured outcomes, http://dx.doi.org/10.1111/obr.12487.
[17] Nugent, R. et al. (2018), Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals, http://dx.doi.org/10.1016/S0140-6736(18)30667-6.
[79] Ockene, I. et al. (1999), “Effect of physician-delivered nutrition counseling training and an office-support program on saturated fat intake, weight, and serum lipid measurements in a hyperlipidemic population: Worcester area trial for counseling in hyperlipidemia (WATCH)”, Archives of Internal Medicine, http://dx.doi.org/10.1001/archinte.159.7.725.
[26] OECD (2019), OECD Reviews of Public Health: Chile: A Healthier Tomorrow, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264309593-en.
[24] OECD (2019), OECD Reviews of Public Health: Japan: A Healthier Tomorrow, OECD Publishing, Paris, https://doi.org/10.1787/9789264311602-en.
[16] OECD (2017), Healthy people, healthy planet. The role of health systems in promoting healthier lifestyles and a greener future, OECD, https://www.oecd.org/health/health-systems/Healthy-people-healthy-planet.pdf.
[13] OECD (2010), Obesity and the Economics of Prevention: Fit not Fat, OECD Publishing, Paris, http://dx.doi.org/10.1787/9789264084865-en.
[142] OECD (2010), Obesity and the Economics of Prevention: Fit not Fat, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264084865-en.
[59] Ontario.ca (2018), Calories on menus, https://www.ontario.ca/page/calories-menus.
[73] Oosterveen, E. et al. (2017), A systematic review of eHealth behavioral interventions targeting smoking, nutrition, alcohol, physical activity and/or obesity for young adults, http://dx.doi.org/10.1016/j.ypmed.2017.01.009.
[84] Orrow, G. et al. (2012), “Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials”, Bmj, Vol. 344, p. e1389.
[130] Otero, I., M. Nieuwenhuijsen and D. Rojas-Rueda (2018), “Health impacts of bike sharing systems in Europe”, Environment International, http://dx.doi.org/10.1016/j.envint.2018.04.014.
[112] Palakshappa, D. et al. (2016), “Association between state school nutrition laws and subsequent child obesity”, Preventive Medicine, http://dx.doi.org/10.1016/j.ypmed.2016.06.039.
[128] Patel, D. et al. (2010), “The association between medical costs and participation in the vitality health promotion program among 948,974 members of a South African health insurance company”, American Journal of Health Promotion, http://dx.doi.org/10.4278/090217-QUAN-68R2.1.
[132] Pazin, J. et al. (2016), “Effects of a new walking and cycling route on leisure-time physical activity of Brazilian adults: A longitudinal quasi-experiment”, Health and Place, http://dx.doi.org/10.1016/j.healthplace.2016.02.005.
[152] Pell, D. et al. (2019), “Support for, and perceived effectiveness of, the UK soft drinks industry levy among UK adults: Cross-sectional analysis of the International Food Policy Study”, BMJ Open, http://dx.doi.org/10.1136/bmjopen-2018-026698.
[123] Penalvo, J. et al. (2017), “Abstract MP005: Do Worksite Wellness Programs Improve Dietary Behaviors and Adiposity? A Systematic Review and Meta-analysis”, Circulation, Vol. 135/suppl_1, pp. AMP005-AMP005.
[7] Pickett, K. et al. (2005), “Wider income gaps, wider waistbands? An ecological study of obesity and income inequality”, Journal of Epidemiology and Community Health, http://dx.doi.org/10.1136/jech.2004.028795.
[61] Pollard, C. et al. (2008), “Increasing fruit and vegetable consumption: success of the Western Australian Go for 2&5® campaign”, Public health nutrition, Vol. 11/03, pp. 314-320.
[44] Pulos, E. and K. Leng (2010), “Evaluation of a voluntary menu-labeling program in full-service restaurants”, American Journal of Public Health, Vol. 100/6, pp. 1035-1039.
[158] Quirmbach, D. et al. (2018), “Effect of increasing the price of sugar-sweetened beverages on alcoholic beverage purchases: an economic analysis of sales data”, Journal of epidemiology and community health, http://dx.doi.org/10.1136/jech-2017-209791.
[191] Restrepo, B. and M. Rieger (2016), “Denmark’s Policy on Artificial Trans Fat and Cardiovascular Disease”, American Journal of Preventive Medicine, http://dx.doi.org/10.1016/j.amepre.2015.06.018.
[134] Rojas-Rueda, D. et al. (2011), “The health risks and benefits of cycling in urban environments compared with car use: Health impact assessment study”, BMJ (Online), http://dx.doi.org/10.1136/bmj.d4521.
[12] Rose, G. (2001), “Sick individuals and sick populations”, International Journal of Epidemiology, http://dx.doi.org/10.1093/ije/30.3.427.
[173] Rundle, A. et al. (2009), “Neighborhood food environment and walkability predict obesity in New York City”, Environmental Health Perspectives, http://dx.doi.org/10.1289/ehp.11590.
[32] Sacks, G. et al. (2011), “‘Traffic-light’nutrition labelling and ‘junk-food’tax: a modelled comparison of cost-effectiveness for obesity prevention”, International Journal of Obesity, Vol. 35/7, pp. 1001-1009.
[81] Sanchez, A. et al. (2015), “Effectiveness of physical activity promotion interventions in primary care: A review of reviews”, Preventive medicine, Vol. 76, pp. S56-S67.
[135] Sarmiento, O. et al. (2016), “The Ciclovía-Recreativa: A Mass-Recreational Program With Public Health Potential”, Journal of Physical Activity and Health, http://dx.doi.org/10.1123/jpah.7.s2.s163.
[157] Sassi, F., A. Belloni and C. Capobianco (2013), “The Role of Fiscal Policies in Health Promotion”, OECD Health Working Papers, No. 66, OECD Publishing, Paris, https://dx.doi.org/10.1787/5k3twr94kvzx-en.
[160] Sassi, F. et al. (2018), Equity impacts of price policies to promote healthy behaviours, http://dx.doi.org/10.1016/S0140-6736(18)30531-2.
[159] Sassi, F. et al. (2009), “Improving Lifestyles, Tackling Obesity: The Health and Economic Impact of Prevention Strategies”, OECD Health Working Papers, No. 48, OECD Publishing, Paris, https://dx.doi.org/10.1787/220087432153.
[6] Sassi, F. and J. Hurst (2008), “The Prevention of Lifestyle-Related Chronic Diseases: an Economic Framework”, OECD Health Working Papers, No. 32, OECD Publishing, Paris, https://dx.doi.org/10.1787/243180781313.
[99] Saunders, P., A. Saunders and J. Middleton (2015), “Living in a ‘fat swamp’: exposure to multiple sources of accessible, cheap, energy-dense fast foods in a deprived community”, British Journal of Nutrition, http://dx.doi.org/10.1017/s0007114515001063.
[69] Schippers, M. et al. (2017), A meta-analysis of overall effects of weight loss interventions delivered via mobile phones and effect size differences according to delivery mode, personal contact, and intervention intensity and duration, http://dx.doi.org/10.1111/obr.12492.
[110] Schneider, L. et al. (2012), “The Extent to Which School District Competitive Food and Beverage Policies Align with the 2010 Dietary Guidelines for Americans: Implications for Federal Regulations”, Journal of the Academy of Nutrition and Dietetics, http://dx.doi.org/10.1016/j.jand.2012.01.025.
[70] Semper, H., R. Povey and D. Clark-Carter (2016), A systematic review of the effectiveness of smartphone applications that encourage dietary self-regulatory strategies for weight loss in overweight and obese adults, http://dx.doi.org/10.1111/obr.12428.
[47] Seyedhamzeh, S. et al. (2018), “Physical activity equivalent labeling vs. calorie labeling: a systematic review and meta-analysis”, International Journal of Behavioral Nutrition and Physical Activity, http://dx.doi.org/10.1186/s12966-018-0720-2.
[30] Sinclair, S., M. Cooper and E. Mansfield (2014), “The influence of menu labeling on calories selected or consumed: a systematic review and meta-analysis”, Journal of the Academy of Nutrition and Dietetics, Vol. 114/9, pp. 1375-1388. e15.
[96] Sørensen, J. et al. (2011), “Exercise on prescription: Changes in physical activity and health-related quality of life in five Danish programmes”, European Journal of Public Health, http://dx.doi.org/10.1093/eurpub/ckq003.
[188] Stender, S. and J. Dyerberg (2004), Influence of trans fatty acids on health, http://dx.doi.org/10.1159/000075591.
[127] Sturm, R. et al. (2013), “A cash-back rebate program for healthy food purchases in South Africa: Results from scanner data”, American Journal of Preventive Medicine, http://dx.doi.org/10.1016/j.amepre.2013.02.011.
[19] Swinburn, B. et al. (2019), “The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report”, The Lancet, http://dx.doi.org/10.1016/s0140-6736(18)32822-8.
[118] Tedstone, A. et al. (2018), “Calorie reduction: The scope and ambition for action”, London: Public Health England.
[145] Teng A, Jones A, Mizdrak A, Signal L, Genç M, W. (2019), “Impact of sugar‐sweetened beverage taxes on purchases and dietary intake: Systematic review and meta‐analysis”, Obesity Reviews.
[54] Thomas, E. (2016), “Food for thought: obstacles to menu labelling in restaurants and cafeterias”, Public Health Nutrition, http://dx.doi.org/10.1017/s1368980015002256.
[77] Toitumine.ee (2019), Magusad ja soolased näksid, https://toitumine.ee/kuidas-tervislikult-toituda/toidusoovitused/magusad-ja-soolased-naksid.
[40] van der Bend, D. and L. Lissner (2019), “Differences and similarities between front-of-pack nutrition labels in Europe: A comparison of functional and visual aspects”, Nutrients, http://dx.doi.org/10.3390/nu11030626.
[102] Van Sluijs, E., A. McMinn and S. Griffin (2008), “Effectiveness of interventions to promote physical activity in children and adolescents: Systematic review of controlled trials”, British Journal of Sports Medicine, http://dx.doi.org/10.1136/bmj.39320.843947.BE.
[53] Vyth, E. et al. (2011), “Influence of placement of a nutrition logo on cafeteria menu items on lunchtime food choices at Dutch work sites”, Journal of the American Dietetic Association, Vol. 111/1, pp. 131-136.
[65] Wammes, B., A. Oenema and J. Brug (2007), “The evaluation of a mass media campaign aimed at weight gain prevention among young Dutch adults”, Obesity, http://dx.doi.org/10.1038/oby.2007.330.
[100] Wang, Y. et al. (2015), “What childhood obesity prevention programmes work? A systematic review and meta-analysis”, Obesity Reviews, http://dx.doi.org/10.1111/obr.12277.
[2] WCRFI (2016), NOURISHING Framework, http://www.wcrf.org/int/policy/nourishing-framework.
[78] WHO (2019), Be He@lthy, Be Mobile - Innovations, https://www.who.int/ncds/prevention/be-healthy-be-mobile/innovations/en/ (accessed on 29 May 2019).
[116] WHO (2019), WHO European Database on Nutrition, Obesity and Physical Activity (NOPA).
[195] WHO (2019), WHO welcomes industry action to align with global trans fat elimination targets, https://www.who.int/news-room/detail/07-05-2019-who-welcomes-industry-action-to-align-with-global-trans-fat-elimination-targets.
[5] WHO (2018), Physical activity country factsheets, http://www.euro.who.int/en/health-topics/disease-prevention/physical-activity/data-and-statistics/physical-activity-fact-sheets/physical-activity-country-fact-sheets.
[91] WHO (2016), Integrating diet, physical activity and weight management services into primary care.
[4] WHO (2012), “Global database on the Implementation of Nutrition Action (GINA)”, World Health Organization, https://www.who.int/nutrition/gina/en/.
[184] WHO (2010), A framework for implementing the set of recommendations on the marketing of foods and non-alcoholic beverages to children, https://www.who.int/dietphysicalactivity/framework_marketing_food_to_children/en/.
[21] Willett, W. et al. (2019), “Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems.”, Lancet (London, England), http://dx.doi.org/10.1016/S0140-6736(18)31788-4.
[62] Wrieden, W. and L. Levy (2016), “’Change4Life Smart Swaps’: quasi-experimental evaluation of a natural experiment”, Public health nutrition, pp. 1-5.
[20] Xiao, C., Y. Goryakin and M. Cecchini (2019), Physical Activity Levels and New Public Transit: A Systematic Review and Meta-analysis, http://dx.doi.org/10.1016/j.amepre.2018.10.022.
[74] Yoganathan, D. and S. Kajanan (2013), Persuasive Technology for Smartphone Fitness Apps.
[165] Young, C. et al. (2013), “Improving Fruit and Vegetable Consumption Among Low-Income Customers at Farmers Markets: Philly Food Bucks, Philadelphia, Pennsylvania, 2011”, Preventing Chronic Disease, http://dx.doi.org/10.5888/pcd10.120356.
[153] Zhong, Y. et al. (2018), “The Short-Term Impacts of the Philadelphia Beverage Tax on Beverage Consumption”, American Journal of Preventive Medicine, http://dx.doi.org/10.1016/j.amepre.2018.02.017.
← 1. Throughout this chapter, the nutritional status of individuals is defined according to WHO guidelines and thresholds and uses body-mass index (BMI). Overweight is defined as a BMI higher than 25 kg/m2; pre-obesity is defined as a BMI of 25-30 kg/m2; and obesity is defined as a BMI higher than 30 kg/m2. Obesity can be further divided into class I, class II and class III obesity. Class I obesity is the milder form of obesity and is defined as a BMI of 30-35 kg/m2; class II obesity is defined as a BMI of 35-40 kg/m2; while class III obesity is defined as a BMI over 40 kg/m2. Morbid obesity includes class II and class III obesity and is defined as a BMI higher than 35 kg/m2. Further information can be found in Chapter 2 - Box 2.1. Using body mass index (BMI) to define levels of adiposity.
← 2. OECD accession and selected partner countries include: Brazil (also a G20 country), China (also a G20 country), Colombia, Costa Rica, India (also a G20 country), Indonesia (also a G20 country), Peru and South Africa (also a G20 country).