Yevgeniy Goryakin
Alexandra Aldea
Aliénor Lerouge
Yvan Guillemette

Yevgeniy Goryakin
Alexandra Aldea
Aliénor Lerouge
Yvan Guillemette
Properly implemented, a reformulation policy can help achieve a win-win-win outcome for public health, the food industry and for consumers. This section briefly discusses the opportunities and challenges presented by the implementation of the set of actions needed to achieve food and beverage reformulation, while also presenting the health and economic outcomes based on a scenario of a 20% calorie reduction in foods high in sugar, salt, calories and saturated fats.
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
Achieving a 20% calorie reduction for foods high in sugar, salt, calories and saturated fats can result in significant health gains, with up to 1.1 million cases per year of cardiovascular diseases, diabetes and cancer avoided annually in the 42 countries included in the analysis.
About USD PPP 13.2 billion can be saved each year across the countries considered in this study, which corresponds to about 0.21% reduction in total health expenditure.
Reformulation can increase the gross domestic product (GDP) of 42 countries by 0.51% on average each year relative to the trend, generating additional economic growth similar to the whole economy of Chile (i.e. about USD PPP 456 billion).
Food reformations, if properly implemented, can be a win-win-win for public health, for the food industry and for consumers. It is important to ensure that such initiatives are implemented to achieve the original purpose, and do not serve to defer other, more rigorous, policy actions or to make unjustified health claims.
Food reformulation delivers a different end product through a deliberate change in the production process or in the content of ingredients. Most producers reformulate their products every few years as part of their normal business process, for example to improve quality, save costs, respond to changes in consumer preferences or as an adjustment to food-related governmental policies (Webster and Hawkes, 2009[1]).
Product reformulation can be challenging to implement, especially if it results in a large change in taste over the short term. On the other hand, gradually implemented product reformulations may be one of the least intrusive ways to help the public improve their diet, as it reduces the need for counting calories and checking for other potentially unhealthy ingredients without affecting their dietary habits. Gradual reformulations may also help businesses preserve their sales, as the public are more likely to adjust to a new taste over time, as has been the case, for example, with salt reduction targets (Tedstone et al., 2018[2]). Reformulations may also help businesses open new market niches, for example by attracting people from the health-conscious segment of the market.
In recent years, many OECD countries have been showing a growing interest for policies promoting food reformulation. Much of this interest was fostered by successful attempts to promote reductions in the content of salt in pre-packaged food and the pressing need for countries to implement ambitious programmes to halt the raise in obesity1 and childhood obesity. Since the early 2000s, a number of OECD countries have been in discussions with industry on suitable actions to promote reductions in calorie content or in specific nutrients such as sugar or fat, mainly saturated fat.
In some countries, reformulation initiatives are mandatory. For example, following a United States Department of Agriculture ruling in 2015, the United States food manufacturers and restaurants can no longer produce foods containing partially hydrogenated oils, a primary source of trans fats. Some countries have strict controls, sometimes even bans, on the amount of trans fat in foods (or their major sources, such as partially hydrogenated oils), including Austria, Canada, Chile, Denmark, Hungary and Latvia. Mandatory limits on the amount of salt have also been set, for example, in Argentina, Belgium, Bulgaria, Greece, Hungary, Netherlands, Portugal and South Africa (WCRFI, 2016[3]). There are also examples of voluntary reformulation initiatives, which are most often undertaken in collaboration between private companies and governmental entities as highlighted in Box 7.1. They often focus on the reduction and replacement of trans fats and saturated fat content, salt, and sometimes on reducing the amount of sugar. In addition, they can aim to increase the content of certain healthy foods such as whole grains or nutrients, such as dietary fibre.
In 2010, the Ministry of Health in Austria, the Agency for Health and Food Safety and the Industrial Bakers of Austria agreed on a voluntary target to reduce the salt content in bakery products by 15% by 2015. This initiative is part of an overall nutrition action plan which also includes the promotion of healthy eating (WHO, 2013[4]).
In 2015, the Government of Australia launched the Healthy Food Partnership. Its stated aim is to improve the dietary habits of Australians by making healthier food choices easier and more accessible and by raising awareness of better food choices and portion sizes. The Partnership is a collaboration between the government, food industry bodies and public health groups. Its focus is on making progress in the following areas:
o continuing to support industry with food reformulation
o supporting consumers with eating appropriate levels of core foods such as fruit, vegetables, whole grains, meat, fish and dairy, and appropriate levels of energy intake
o educating consumers on appropriate portion and serve sizes
o improving consumer knowledge and awareness of healthier food choices, including through developing and publicising tools and resources for consumers and health professionals.
The Healthy Food Partnership follows a previous initiative, the Food and Health Dialogue, which was launched in 2009 to provide a collaborative forum where the government could work together with the health sector and food industry to improve the availability of healthy food options and increase consumer awareness and understanding of the link between food choices and health outcomes. During the time the Food and Health Dialogue was active, a number of priority food categories were targeted for reformulation to reduce sodium content. A subsequent evaluation of the Dialogue found a significant reduction in the average sodium content of products in most of the targeted categories (Heart Foundation, 2016[5]).
Although there is already a mandatory 2% limit on the amount of salt allowed in bread in Belgium, the Belgian food and drink industry also agreed to reduce voluntarily the salt content of foods over the period 2009-2012 by 10%, using a self-reporting framework (WCRFI, 2016[3]). This reduction was implemented gradually so that consumers would not notice any significant taste differences. The plan also included a public awareness campaign supported by the authorities to educate consumers. The actual reduction varied by product. For example, according to estimates provided by the Belgian Food Industry Federation (Fédération de l'industrie alimentaire Belge), by 2013, there was a reduction in salt content from 16% to 36% in meat products, 22% in bread, 17% in powdered soup, 15% to 29% in ready meals and 7.5% to 20% in cheese (FoodDrink Europe, 2015[6]).
The “Whole Grain Partnership” was established in 2008 with the aim of increasing the intake of whole grains. The partnership sets standards that companies need to meet on the minimum amount of whole grains contained in products before they can put a certification logo on their package. In addition, such products should not contain amounts of added sugar and salt above a certain threshold. The programme places greater emphasis on foods consumed at breakfast and dinner (Fagt et al., 2018[7]). This partnership includes the Danish government, non-governmental organisations focusing on health (such as the Danish Cancer Society and the Danish Diabetes Association), the food and drink industry, and retailers. One evaluation attributed the change in the intake of whole grains in the Danish population from 36 g/day in 2007 to 63 g/day in 2014 to the effect of the partnership (Greve, Carsten, 2014[8]).
The Programme National Nutrition Santé (PNNS) has been in force since 2001. It is a government-led, multi-stakeholder programme that promotes health across the population with nine objectives including reductions in saturated fats, salt and sugar intake (Haut Conseil de la santé publique, 2017[9]). The food and non-alcoholic beverage industry committed to voluntarily reformulating their products through charters, which resulted, for example, in a 3‑14% reduction in the amount of salt in 2012 (Haut Conseil de la santé publique, 2017[9]).
The French Syndicat National des Boissons Rafraîchissantes (SNBR) representing 80% of the French beverage market signed an agreement in 2014 with the French government within the framework of the Programme National pour l’Alimentation and pledged to reduce by 5% the calorie and sugar content per litre in soft drinks by 2015 compared to 2010 (Challenges.fr, 2014[10]).
A voluntary agreement was reached in 2009 between four main baker associations, and the Italian government, to reduce the amount of salt in some products by 10-15% within two years (WCRFI, 2016[3]).
In 2017, seven beverage manufacturers representing 70% of the sugar-sweetened beverage (SSB) market in Singapore voluntarily agreed to reduce the content of sugar in their drinks to a maximum level of 12% by the year 2020. This pledge was made in the context of collaboration between the industry and The Diabetes Prevention and Care Taskforce at the Singapore Ministry of Health (WCRFI, 2016[3]).
In Spain, a reformulation initiative called “The collaboration plan for the improvement of food and beverage composition and other measures, 2020” was recently agreed between the Spanish Food Safety and Nutrition Agency and a number of food sector associations involving almost 400 companies. This initiative aims to reduce the amount of added sugar, salt and saturated fat reduction in the manufacturing and retail sectors, and to increase healthier options in a number of different settings. The initiative is expected to give the companies sufficient time (until the end of 2020) to implement the reformulation of their foods, and has already resulted in the signing of 20 relevant agreements (Aecosan, 2018[11]).
The US Healthy Weight Commitment Foundation is a multi-stakeholder, industry-led initiative, aiming to significantly reduce the amount of calories in the participating businesses’ products between 2010 and 2015. Lower-calorie products drove more than 80% of the sales growth among the participating companies, four times more than higher-calorie products (Samuel Mary, 2017[12]). The foundation claims that its member companies (including major actors in the soft drink business) sold 6.4 trillion fewer calories in the United States in 2012 than in 2007, which was 400% above their original goal (Samuel Mary, 2017[12]).
In the European Union, a number of reformulation initiatives have been launched. For example, in 2008, a framework was agreed to reduce salt in food by 16% within 4 years. Furthermore, a target benchmark was agreed to reduce saturated fat by 5% until 2016 and by an additional 5% by 2020. In 2015, the Added Sugars Annex was agreed promoting a voluntary 10% reduction by 2020 of added sugars in processed food (European Commission, 2019[13])
The Union of European Beverages Associations (UNESDA), representing the European soft drink industry, has committed to voluntarily reducing added sugar in beverages by 10% by 2020, compared to 2015 baseline. A mid-term evaluation carried out by auditors concluded that there was a 11.9% reduction in added sugar achieved by the end of 2017 (UNESDA, 2019[14]).
Another voluntary reformulation example is the UK initiative challenging UK food manufacturers to reduce the amount of calories in relevant foods by 20% by 2024; especially those consumed by children (see Box 7.2). In 2018, the OECD put forward a proposal to the G20 for a global deal between national governments and industry to scale up the UK efforts worldwide.
The obesity burden facing the younger generation is a problem with serious long-term consequences. Recognising this, the United Kingdom unveiled a policy action plan in 2016 to deal with childhood obesity (Department of Health & Social Care, 2016[15]). The government also announced a sugar reduction programme the same year, challenging the food and beverage industry to reduce the amount of sugar by 20% by 2020.
However, it soon became clear that a more ambitious programme was needed in order to make a significant impact on childhood obesity in the United Kingdom. In 2018, the government set out details for the reformulation programme challenging the industry to reduce calories from relevant foods (i.e. those high in sugar, salt, calories and saturated fat, such as ready meals, pizzas, snacks sauces and dressings) by 20% by 2024 (Tedstone et al., 2018[2]). Together with the sugar reduction programme and the soft drink levy introduced in 2018, it is hoped that about 50% of all calories consumed by children in the United Kingdom will be covered. Such a target requires commitment not only from the food and beverage manufacturers, but also from retailers, restaurants and other food outlets, takeaway and delivery services. Since this programme is not mandatory, achieving the targets may be challenging. One approach is for the government to monitor and publish the progress, highlighting the participants that are doing well, or those lagging behind.
Although the focus of the programme is explicitly on food and drink sold to children under the age of 18, it is likely that other age groups will benefit as well, since adults eat similar food. Indeed, it was estimated that on a per capita basis, such an initiative can result in an average reduction of 68 calories per day for the whole population (Tedstone et al., 2018[2]).
Food reformulation can also occur as a reaction to some other governmental measures, which at first sight may appear unrelated. For example, food manufacturers can respond to the labelling requirements by voluntary reformulation to make the product more attractive to consumers (for example, by reducing calorie, salt or sugar content) (Hawley et al., 2013[16]). Likewise, restaurants may have an incentive to voluntarily reduce portion sizes when they face the menu labelling requirements (Littlewood et al., 2016[17]). Taxation of sugary beverages and other calorie-dense products can also induce product reformulation and other supply-side responses that can increase their positive impact on health (Chaloupka, Powell and Warner, 2019[18]). Such reformulations are more likely to happen when the tax targets specific ingredient(s) within the products, rather than total weight or volume of a product (Ecorys, 2014[19]).
Whatever the motivation for reformulation, it is important to ensure that such initiatives are implemented effectively to achieve the original purpose, and that they do not prevent governments from implementing other evidence-based policies. It is also important to ensure reformulations are not used to make unjustified health claims.
The reduction in calories consistent with the voluntary reformulation policy proposed in the United Kingdom is modelled from 2020 until 2050. Specifically, Public Health England proposes a 20% calorie reduction for the foods in the relevant categories, i.e. high in sugar, salt, calories and saturated fats. Furthermore, they calculated that this would translate into 68 fewer calories per day for the whole population (Tedstone et al., 2018[2]).
This target reduction is implemented as a scenario rather than an actual policy. In practice, achieving such a large reduction will require the implementation of many different policies and actions, including the establishment of partnerships among all the various stakeholders to effectively address the technical, social and policy issues arising throughout this effort. Some of the policies that countries have put in place to promote food reformulation include food labelling and menu labelling, mass media campaigns, changes in portion sizes, price policies targeting nutrient content above a certain threshold (e.g. sugar content), incentives for research and development.
The major assumption behind modelling this scenario is that consumers will not compensate for this reduction in calories per item by buying a larger number of items, or switching to higher calorie alternatives not covered by reformulation. The population coverage is assumed to be 100%. The analysis covered 42 countries2.
While a global deal to reduce calorie content in relevant foods by 20% would not address all the causes underpinning the obesity epidemic, including for example low levels of physical activity, the OECD model calculates that, if such plan was to be implemented in 42 countries worldwide, it would have a significant impact on the health and economy of countries.
Achieving a reduction of 20% in calories from relevant food groups across 42 countries will prevent the development of up to 1.1 million cases per year of non-communicable diseases in the 42 countries included in the analysis. Most of the gains in health will be achieved through a reduction in cardiovascular diseases (CVDs) (about 771 000 cases per year would be prevented) with additional reductions in diabetes, dementia and cancers.
On a population-standardised basis, reformulations will contribute the most to avoiding CVDs in China and Eastern Europe; while its effect on avoiding cancers and dementia will be higher in Western Europe (Figure 7.1). The reduction in the diabetes rate appears similar across regions. As a side effect of extended life expectancy in the population, due to the implementation of the intervention, people will also slightly increase their lifetime risk of developing other chronic conditions, mainly mental illnesses. Nonetheless, as testified by the significant gains in life years (LYs) and disability-adjusted life years (DALYs) discussed below, the effect of food reformulation on population health will be overwhelmingly positive.
Impact on new disease cases, number per 100 000 population annually, 2020-2050
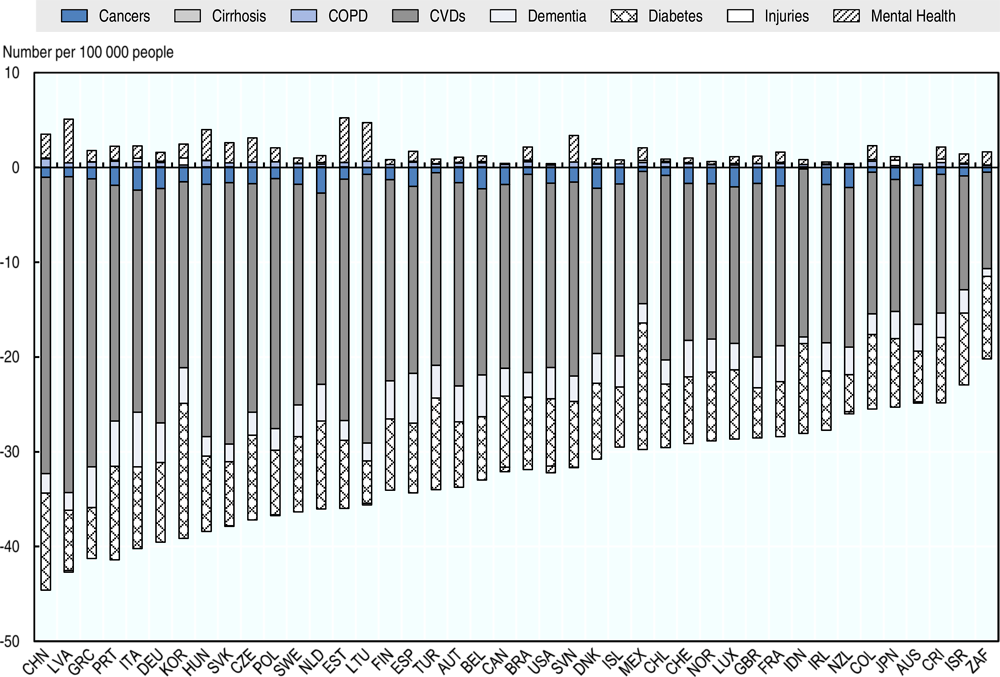
Note: COPD: Chronic obstructive pulmonary disease; CVDs: cardiovascular diseases.
Source: OECD SPHEP-NCDS MODEL, 2019.
Overall, 4 million DALYs and 3.1 million LYs are predicted to be gained each year from 2020 to 2050 as a result of implementing the reformulation scenario in all 42 countries. This will translate into an increase in life expectancy of about 2.9 months above trend, similar to the average gain in life expectancy experience in OECD countries in the last 2.5 years.
The largest per capita effect is expected to occur in Central and Eastern European countries, due to the larger burden of obesity-related diseases, with up to 180 DALYs that can potentially be gained annually per 100 000 population in Latvia (Figure 7.2). The smallest change is expected in South Africa with 59 DALYs expected to be gained per 100 000 population. In almost all cases, the gain in DALYs is predicted to be significantly larger than in LYs.
Number of DALYs and LYs gained per 100 000 population annually, 2020-2050
Overall, about USD PPP 13.2 billion can be saved each year across the countries considered in this study, which corresponds to about 0.21% reduction in total health spending. The strongest reduction in annual health expenditure3 per capita will be in the United States, up to almost USD PPP 16 saved each year (Figure 7.3). The largest reductions in health expenditure in relation to the total health budget are expected to occur in Turkey, Korea and the Netherlands (about 0.31% to 0.33% of the total health budget).
Finding that food reformulation contributes to lower medical spending in all countries suggests that it is an economically prudent strategy. Indeed, although reformulation can lead to people living longer and therefore needing more access to health care, in all cases cumulative health expenditure gains will remain positive, including in countries where life expectancy gains are potentially the largest. This is mostly due to the fact that reformulation not only helps increase life expectancy, but also leads to people living longer in a healthy state.
Impact on health expenditure, in USD PPP per capita and as a percentage of total health budget, annual average over 2020-2050
The reformulation policy is also predicted to make a significant impact on labour market outputs, as shown in Figure 7.4. The biggest impact is predicted in Western and Northern European countries, Korea and the United States, with up to USD PPP 50 that can be saved annually in Switzerland. Most of these savings will come from reductions in work-related presenteeism and increases in the employment rate, while the effect on early retirement is predicted to be negligible. In addition, savings from changes in labour market outputs are expected to be two to three times larger than savings in health expenditure (compare Figure 7.4 and Figure 7.3).
Impact on labour market costs, in USD PPP per capita and by component, annual average over 2020-2050
Finally, it was estimated that the GDP of countries is expected to be above trend by 0.51% on average each year, generating an additional economic growth similar to the whole economy of Chile (i.e. about USD 456 billion).
In recent years, many OECD countries have been showing a growing interest in policies promoting food reformulation. Much of this interest was fostered by successful attempts to promote reductions in the content of salt in pre-packaged foods and the pressing need for countries to implement ambitious programmes to halt the rise in obesity and childhood obesity.
More recently, in 2018, the OECD put forward to the G20 a proposal for a global deal between national governments and industry to scale up the UK initiative globally. While a global deal to reduce calorie content in relevant food by 20% will not address all the causes underpinning the obesity epidemic, including for example low levels of physical activity, the OECD model calculates that, if such plan was to be implemented in 42 countries worldwide, it would have a significant impact on the health and the economy of countries.
[11] Aecosan (2018), Collaboration PLAN for the improvement of the composition of food and beverages and other measures 2020, http://www.aecosan.msssi.gob.es/AECOSAN/docs/documentos/nutricion/Plan_Colaboracion_INGLES.pdf.
[10] Challenges.fr (2014), Les fabricants de sodas s’attaquent au sucre dans leurs boissons, https://www.challenges.fr/entreprise/les-fabricants-de-sodas-s-attaquent-au-sucre-dans-leurs-boissons_132595.
[18] Chaloupka, F., L. Powell and K. Warner (2019), “The Use of Excise Taxes to Reduce Tobacco, Alcohol, and Sugary Beverage Consumption”, Annual Review of Public Health, http://dx.doi.org/10.1146/annurev-publhealth-040218-043816.
[15] Department of Health & Social Care (2016), Childhood Obesity: A Plan For Action, https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action/childhood-obesity-a-plan-for-action.
[19] Ecorys (2014), Food taxes and their impact on competitiveness in the agri-food sector, http://file:///C:/Users/Goryakin_Y/Downloads/Impact%20of%20Food%20Taxes%20-%20Final%20%20Report.pdf.
[13] European Commission (2019), Initiatives on Nutrition and Physical Activity, https://ec.europa.eu/health/sites/health/files/nutrition_physical_activity/docs/2019_initiatives_npa_en.pdf.
[7] Fagt, S. et al. (2018), “Breakfast in Denmark. Prevalence of Consumption, Intake of Foods, Nutrients and Dietary Quality. A Study from the International Breakfast Research Initiative”, Nutrients, http://dx.doi.org/10.3390/nu10081085.
[6] FoodDrink Europe (2015), Balanced Diets & Healthy Lifestyles: Food and drink industry initiatives..
[8] Greve, Carsten, A. (2014), The Evolution of the Whole Grain Partnership in Denmark., Copenhagen Business School and the Danish Whole Grain Partnership, Copenhagen.
[9] Haut Conseil de la santé publique (2017), “Pour une Politique nationale nutrition santé en France”, https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=632.
[16] Hawley, K. et al. (2013), The science on front-of-package food labels, http://dx.doi.org/10.1017/S1368980012000754.
[5] Heart Foundation (2016), Report on the Evaluation of the nine Food Categories for which reformulation targets were set under the Food and Health Dialogue, https://www1.health.gov.au/internet/main/publishing.nsf/Content/7BD47FA4705160A6CA25800C008088B9/$File/Healthy%20Food%20Partnership%20Evaluation%20Report_Heart%20Foundation.pdf.
[17] Littlewood, J. et al. (2016), Menu labelling is effective in reducing energy ordered and consumed: A systematic review and meta-analysis of recent studies, http://dx.doi.org/10.1017/S1368980015003468.
[12] Samuel Mary (2017), Food and Nutrition Security Thematic and Impact Investing, Kepler Cheuvreux, https://www.longfinance.net/media/documents/ESG_Cookbook.pdf.
[2] Tedstone, A. et al. (2018), Calorie reduction: The scope and ambition for action, Public Health England, London.
[14] UNESDA (2019), European soft drinks industry on track to meet commitment to reduce added sugars by 10% by 2020, https://www.unesda.eu/wp-content/uploads/2019/06/UNESDA-10-FINAL-180619.pdf.
[3] WCRFI (2016), NOURISHING Framework, https://www.wcrf.org/sites/default/files/Improve-food-supply.pdf.
[1] Webster, J. and C. Hawkes (2009), Reformulating food products for health: context and key issues for moving forward in Europe, http://ec.europa.eu/health//sites/health/files/nutrition_physical_activity/docs/ev20090714_wp_en.pdf (accessed on 7 July 2017).
[4] WHO (2013), “Mapping salt reduction initiatives in the WHO European Region”, WHO Regional Office for Europe.
← 1. Throughout this chapter, the nutritional status of individuals is defined according to WHO guidelines and thresholds and uses body-mass index (BMI). Overweight is defined as a BMI higher than 25 kg/m2; pre-obesity is defined as a BMI of 25-30 kg/m2; and obesity is defined as a BMI higher than 30 kg/m2. Obesity can be further divided into class I, class II and class III obesity. Class I obesity is the milder form of obesity and is defined as a BMI of 30-35 kg/m2; class II obesity is defined as a BMI of 35-40 kg/m2; while class III obesity is defined as a BMI over 40 kg/m2. Morbid obesity includes class II and class III obesity and is defined as a BMI higher than 35 kg/m2. Further information can be found in Chapter 2 - Box 2.1. Using body mass index (BMI) to define levels of adiposity.
← 2. The countries covered by the analysis include: Australia, Austria, Belgium, Brazil, Canada, Chile, China, Colombia, Costa Rica, Czech Republic, Germany, Denmark, Estonia, Finland, France, Greece, Hungary, Ireland, Iceland, Indonesia, Israel, Italy, Japan, Latvia, Lithuania, Korea, Luxembourg, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Slovakia, Slovenia, Spain, Sweden, Switzerland, South Africa, Turkey, United Kingdom, United States.
← 3. Health expenditure measures the final consumption of health care goods and services for personal health care including curative care, rehabilitative care, preventative care, ancillary services and medical goods but not long-term care.