Christina Xiao
Sahara Graf

Christina Xiao
Sahara Graf
This chapter presents patterns and trends for overweight and obesity in OECD countries, OECD accession and selected partner countries, EU28 countries, and Group of 20 (G20) countries. Overall, obesity prevalence is increasing in all countries analysed and severe or morbid obesity is also on the rise. These patterns are examined in both adults and children, and separate analyses are performed to determine whether rates of overweight and obesity vary among different population groups, such as by sex and socio-economic status, including income and education. Lastly, this chapter covers various determinants of obesity, such as diet, physical activity, and sedentary behaviour, in order to elucidate targeted health policy strategies.
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
Obesity continues to be a pressing public health issue. In 2016, more than one in three (35.1%) adults in OECD countries were considered pre-obese, with more than one in five (23.2%) adults considered obese.
Prevalence of obesity is lower in children than in adults. About one in five children (18.7%) in OECD countries are considered pre-obese and one in ten children (9.9%) obese.
Obesity rates have continuously grown over the few decades, with average increases between 46.7% and 59.0% in adult obesity observed in OECD, OECD accession and selected partner countries1, EU28 and G20 countries between 1996 and 2016.
Rates of adult obesity growth have been gradual, although in countries with high increases in obesity, morbid obesity accounts for more than half of the growth. The proportion of morbid obesity has been observed to represent as much as 70-80% of obesity growth, as is the case in the United States, Saudi Arabia, and New Zealand.
Obesity rates are not uniform across all social groups; certain groups display higher rates of obesity depending on sex and socio-economic status. In general, there is a higher prevalence of women with obesity compared to men. For the majority of countries, individuals with the lowest incomes or least education are two to three times more likely to be overweight or obese than individuals in the highest income group or with high levels of education.
A well-balanced healthy diet and physical activity are key in preventing overweight and non-communicable diseases (NCDs). However, trends in diet and physical activity have shifted towards unhealthy diets and more sedentary behaviour over the past few decades, due to urbanisation and changes in food and the environment.
Only half of the population of certain countries (Chile, Italy, Mexico, and Spain) are observed to consume a healthy diet. In general, women are more likely to have a healthier diet and consume at least five servings of fruits and vegetables per day compared to men. The wealthier and more educated were also more likely to exhibit healthier dietary behaviour.
Only one in three individuals are sufficiently active. Women are less likely to perform sufficient amounts of physical activity compared to men, as are persons with a lower education. However, women are less likely to demonstrate excessive sedentary behaviour.
1. OECD accession and selected partner countries include: Brazil (also a G20 country), China (also a G20 country), Colombia, Costa Rica, India (also a G20 country), Indonesia (also a G20 country), Peru and South Africa (also a G20 country).
Obesity, defined as a body mass index (BMI) greater or equal to 30 kg/m2 (see Box 2.1 for additional information), continues to be a pressing public health concern, as worldwide, obesity has nearly tripled since 1975. In 2016, more than 1.9 billion adults aged 18 years or older – representing 39% of the world’s adult population – were considered overweight (i.e. a BMI greater or equal to 25 kg/m2); of these individuals, more than 650 million – representing 13% of the world’s adult population – were considered obese (WHO, 2018[1]). Of the original 31 countries included for analysis in the 2010 OECD report on obesity, Obesity and the Economics of Prevention: Fit not Fat (OECD, 2010[2]), average rates of adult obesity in OECD countries have increased from 21.3% in 2010 to 24.0% in 2016, which corresponds to about an additional 50 million people with obesity. Overweight is also widespread among children; worldwide, 41 million children under the age of five classified as overweight or obese, and a further 340 million children and adolescents aged 5-19 are considered overweight or obese in 2016 (WHO, 2018[1]).
Overweight is a well-recognised risk factor for the development of various chronic diseases, including type 2 diabetes, cardiovascular diseases, respiratory diseases, musculoskeletal disorders, several types of cancer, and depression (Abdelaal, le Roux and Docherty, 2017[3]; Guh et al., 2009[4]). These risks also increase with corresponding increases in BMI. Increases in BMI can also have an indirect impact on mortality (Prospective Studies Collaboration et al., 2009[5]), as an estimated 2.8 million people die each year due to being overweight or obese (WHO, 2017[6]).
Adverse health effects due to overweight have also been observed during earlier life stages. Children and adolescents with obesity are at increased risk of developing breathing difficulties, insulin resistance, psychological effects, fractures, hypertension, and can display early markers of cardiovascular disease (WHO, 2019[7]; WHO, 2018[1]; Reilly, 2003[8]). The effects of childhood obesity can persist into adulthood, since children with obesity are more likely to stay obese as adults, are at higher risk of developing cardiovascular diseases such as diabetes, coronary heart disease, and hypertension later in life, and have premature mortality rates more than twice as high as individuals of normal weight (Reilly and Kelly, 2010[9]; WHO, 2019[7]; Maffeis and Tatò, 2001[10]).
In addition to being a public health concern, overweight poses a serious threat to the economy of countries around the world. As described in Chapter 3 and Chapter 4 of this publication, overweight has significant negative effects on the health budgets of countries, since it adversely affects educational outcomes and human capital formation as well as labour force productivity and the broader economy. Thus, health effects associated with overweight, combined with these other social and economic consequences, have contributed to a global economic and health burden.
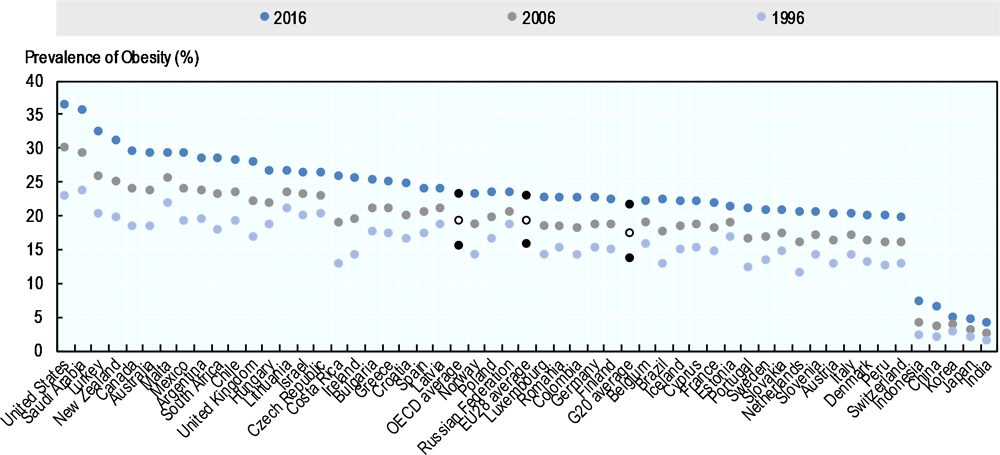
More than one in three persons are considered pre-obese (i.e. with a BMI of 25-29.9 Kg/m2) and one in five persons are considered obese in OECD, OECD accession and selected partner countries, and EU28 and G20 countries (Annex Table 2.A.1). However, large differences exist when individual countries are considered, particularly for obesity rates (Figure 2.1). While prevalence of pre-obesity is broadly comparable across countries, with 46 out of 52 countries having rates of pre-obesity ranging between 31.3% and 38.6%, the analyses did find a nearly ten-fold variation in obesity rates in adults, with rates ranging from 3.9% in India to 36.2% in the United States. Similarly, in OECD countries, obesity rates range from 4.3% in Japan to 36.2% in the United States. In 19 countries, mainly located in North America and Europe, at least a quarter of the adult population is considered obese. A few countries, including Saudi Arabia and the United States, have a higher prevalence of obesity (36.2% and 35.4%, respectively) than that of pre-obesity (34.3% and 31.7%, respectively). On the other hand, rates are comparably lower in Asian countries such as India, Indonesia, China, Japan and Korea, where only 3.9% to 6.9% of the population are considered obese. Focusing on OECD countries outside Asia, the prevalence of adult obesity is also comparatively lower in some European countries such as Austria, Denmark, Italy, Slovakia, Slovenia, Sweden, and Switzerland, which have obesity rates around 20%.
BMI is the most widely used proxy for body adiposity to assess population-level rates of overweight, as it is easily derived from a person’s weight and height. For adults 20 years of age and older, BMI is interpreted using standard weight categories, regardless of sex, body type, age and ethnicity (CDC, 2017[11]). Weight categories and the associated BMI thresholds are presented in the table below.
|
Weight Status |
BMI thresholds |
|---|---|
|
Underweight |
< 18.5 Kg/m2 |
|
Normal or Healthy Weight |
18.5‑24.9 Kg/m2 |
|
Overweight |
≥ 25.0 Kg/m2 |
|
Pre-obesity |
25.0‑29.9 Kg/m2 |
|
Obesity |
≥ 30.0 Kg/m2 |
|
Class I Obesity |
30‑34.9 Kg/m2 |
|
Severe/morbid obesity |
≥ 35.0 Kg/m2 |
|
Class II Obesity |
35-39.9 Kg/m2 |
|
Class III Obesity |
≥ 40 Kg/m2 |
Note: In some Asian countries such as China, Japan, and Korea, categories of pre-obesity and obesity are lower than those of other countries. For instance, Japan defines obesity as a BMI of more than 25 kg/m2 (Kanazawa et al., 2002[12]). This is based on studies finding that East Asians are at higher risk for developing diseases such as diabetes and heart disease at a lower BMI than Africans and Caucasians (WHO Expert Consultation, 2004[13]).
Source: WHO (2019[14]), Body mass index – BMI, http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
BMI thresholds used in children differ from those used in adults to take into account growth and development. For instance, in children under five years of age, overweight is determined as weight-for-height greater than two standard deviations above the WHO Child Growth Standards median, whereas obesity is considered as weight-for-height greater than three standard deviations above the WHO Child Growth Standards median. For children aged 5-19, overweight is defined as BMI-for-age greater than one standard deviation above the WHO Growth Reference median, and obesity is greater than two standard deviations above the WHO Growth Reference median (WHO, 2018[1]). In addition, in clinical practice, the International Obesity Task Force (IOTF) criteria are also widely used to determine BMI levels in children (Cole and Lobstein, 2012[15]).
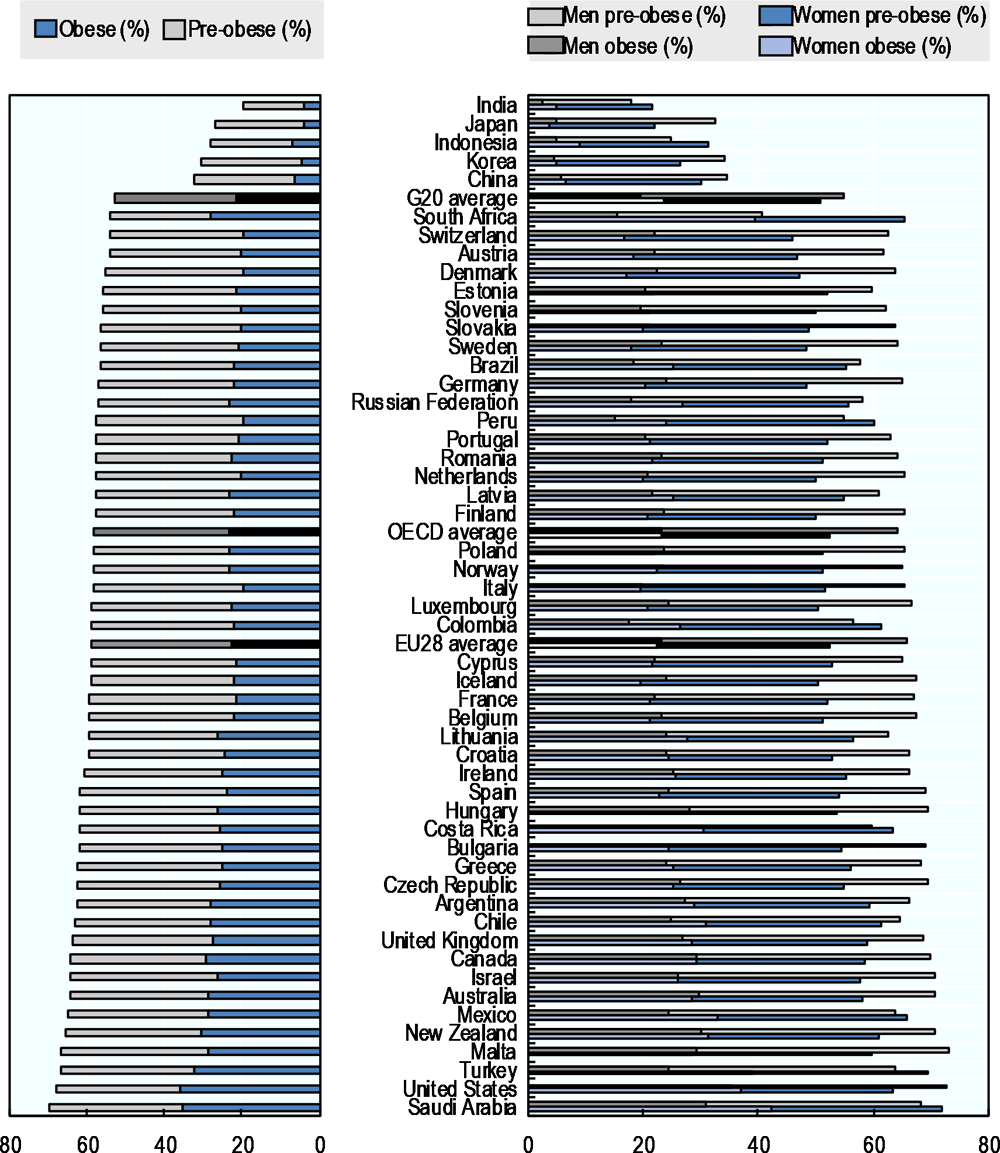
Notes: Data is age-standardised. Additional information on the comparability of this data with data in OECD.Stat can be found in Box 2.2.
Source: OECD analyses on the WHO Global Health Observatory (2018[16]) data, “Mean body mass index (BMI) trends among adults”, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/bmi_trends_adults/en/.
Individuals with morbid levels of obesity now comprise a significant share of the population in OECD, G20, and EU28 countries. In 2016, almost one-tenth (7.5%) of individuals in OECD countries were considered morbidly obese (Figure 2.3), which is defined as individuals with BMI levels above 35 kg/m2 (or class II/III obesity). Similar rates were found for EU28 (6.9%) and G20 countries (7.8%). Among all OECD, G20, and EU28 countries, morbid obesity accounted for between 9.7% (Japan) and 48.1% (United States) of total obesity prevalence. Countries with the highest obesity rates tend to also have the highest levels of morbid obesity; these countries included Saudi Arabia (37.7% obesity prevalence, including 15.2% morbid obesity prevalence), the United States (37.3% obesity prevalence including 18.0% morbid obesity prevalence), and Turkey (33% obesity prevalence including 11.5% morbid obesity prevalence).
This report primarily reports prevalence data from the WHO Global Health Observatory (2018[16]). This dataset covers all the 52 countries analysed in this report, and provides age-standardised estimates using a range of data sources. Age standardization is a technique used to increase the cross-country comparability of data when the age profiles of the populations included in the analysis are different and when there are significant differences in the age group-specific prevalence rates of the dimension under consideration – as it is the case for overweight and obesity rates.
For its Health Statistics, the OECD also collects data on overweight and obesity prevalence (Figure 2.2). This data comes from national surveys, and is presented without any adjustment by age group, and split by measured and self-reported estimates. Due to the difference in data sources, and adjustments such as age-standardisation, the prevalence values of the two datasets can be different.
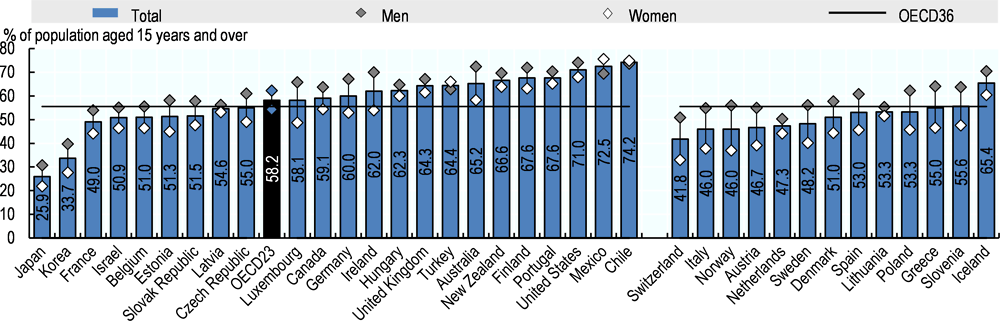
Note: Left- and right-hand side estimates utilised measured and self-reported data, respectively. OECD36 average includes both data types.
Source: OECD Health Statistics 2019.
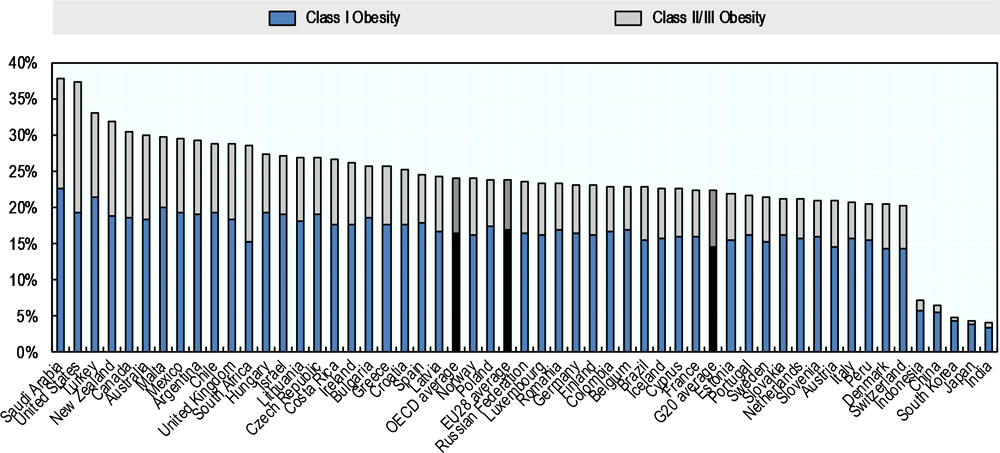
Note: Class I obesity is represented by BMI values between 30 and 35, whereas class II/III or morbid obesity is represented by BMI values greater than 35. Data is age-standardised. Additional information on the comparability of this data with data in OECD.Stat can be found in Box 2.2.
Source: NCD-RisC (2017[17]), “Adult body mass index: Evolution of BMI over time”, http://ncdrisc.org/data-downloads-adiposity.html.
Average rates of pre-obesity and obesity tend to be considerably lower in children compared to rates in adults (Figure 2.4). For instance, in 2016, the average rate of pre-obesity and obesity in children aged 5‑19 years of age in OECD countries was 18.7% and 9.9%, respectively. Rates of pre-obesity and obesity are similar in EU28 (18.6% versus 9.3%) and G20 countries (17.3% versus 10.9%). Children in the United States have among the highest prevalence of pre-obesity and obesity, with rates of 20.4% and 21.4%, respectively. Conversely, children in India have lowest levels of pre-obesity and obesity, where the share is 4.8% and 2.0%, respectively. Overall, prevalence of pre-obesity is generally higher than the prevalence of obesity, except in the United States (20.4% versus 21.4%) and Saudi Arabia (18.2% versus 17.4%), where rates of pre-obesity and obesity are approximately equal. In nearly all countries (51 out of 52), boys have slightly higher rates of obesity than girls, with an OECD average of 11.9% for boys compared to 8% for girls, EU28 average of 11.4% for boys compared to 7.1% for girls, and G20 average of 12.6% for boys compared to 9.0% for girls (Annex Figure 2.A.1). Pre-obesity levels in boys and girls, on the other hand, are nearly equal in OECD (19.0% in boys versus 18.4% in girls), EU28 (19.2% in boys versus 17.9% in girls), and G20 countries (17.4% in boys versus 17.1% in girls).
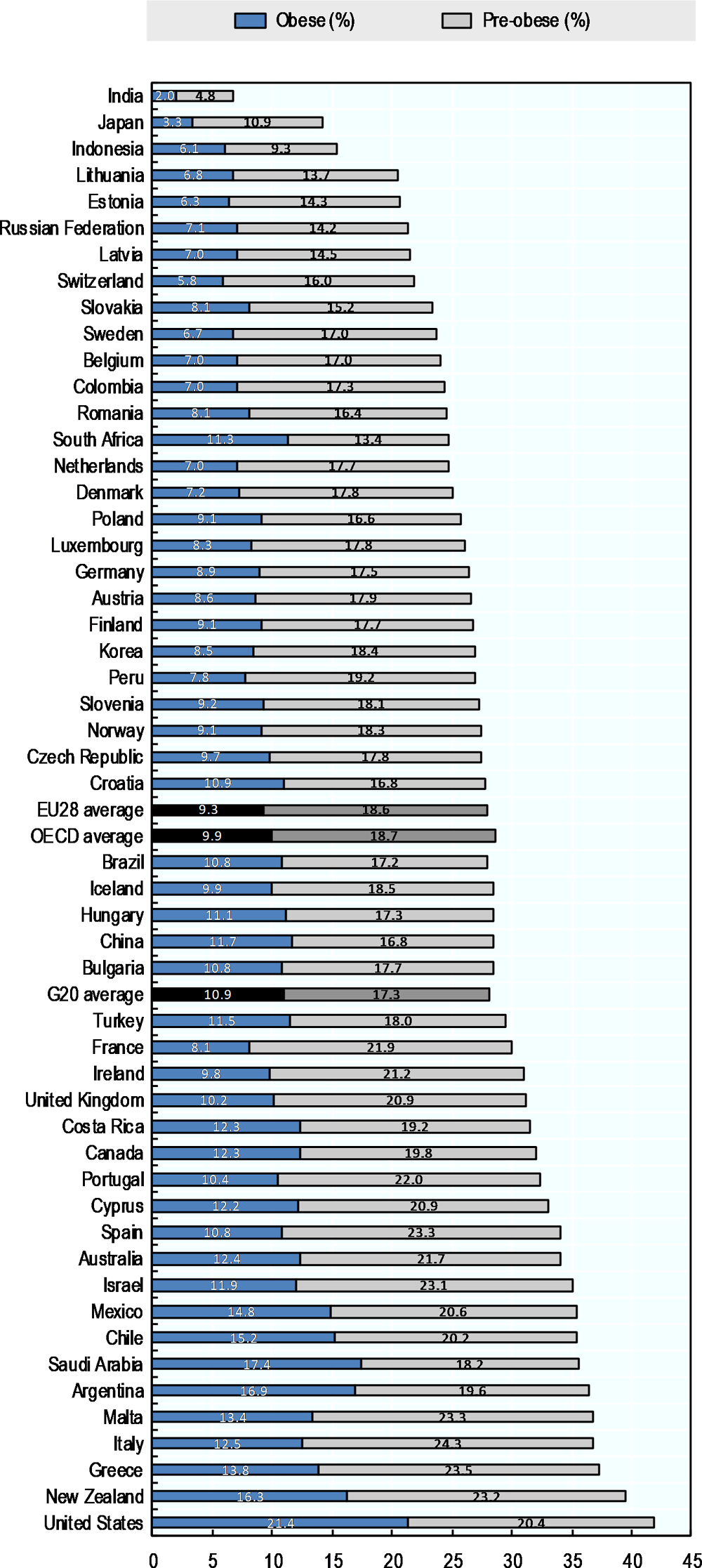
Note: Children between 5‑19 years of age. Data is age-standardised.
Source: OECD analyses on WHO Global Health Observatory (2018[18]) data, “Prevalence of obesity among children and adolescents”, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adolescents/en/.
Trend analyses (Figure 2.5 and Annex Figure 2.A.2) demonstrate a persistent increase in overweight and obesity in adults in all OECD, OECD accession and selected partner countries, EU28 and G20 countries over the past 40 years (WHO Global Health Observatory, 2018[16]). Between 1996 and 2016, pre-obesity prevalence grew by 18.6% in OECD countries, 17.5% in EU28 countries, and 25.5% in G20 countries. During this same period, there was a much greater percentage increase in obesity prevalence, as obesity prevalence grew by 50.4% in OECD countries, 46.7% in EU28 countries, and 59.0% in G20 countries. These trends are expected to continue, as across many OECD countries, obesity rates are projected to rise unless effective policy actions are promptly put in place (Devaux et al., 2017[19]).
Notes: Data is age-standardised. Additional information on the comparability of this data with data in OECD.Stat can be found in Box 2.2.
Source: OECD analyses on the WHO Global Health Observatory (2018[16]) data, “Mean body mass index (BMI) trends among adults”, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/bmi_trends_adults/en/.
The rate of increase in obesity prevalence reveals another important dimension of the obesity epidemic: growth in morbid obesity (class II and class III obesity) is now similar to the growth in class I obesity. Between 2005 and 2016, average morbid obesity growth rates gradually rose in OECD, EU28 and G20 countries, while class I obesity growth rates slowly declined (Figure 2.6). In OECD countries, class I obesity rates have grown by an average of 0.20 percentage points per three-year period between 2005 and 2016, whereas class II and III obesity rates have grown by an average of 0.23 percentage points per three-year period. Increases in class I and class II-III obesity rates between 2005 and 2016 are similar for both EU28 (0.20 and 0.20 percentage points per three-year period, respectively) and G20 countries (0.21 and 0.22 percentage points per three-year period, respectively). Morbid obesity growth accounts for around 50% of the increase in obesity rates in OECD, G20, and EU28 countries between 2014 and 2016. Broadly speaking, countries with the highest increases in total obesity rates, such as the United States (0.67 percentage points) and Saudi Arabia (0.66 percentage points) between the years 2014-2016, also have some of the highest average shares of morbid obesity growth. For example, in the United States and Saudi Arabia, respectively 79% and 74% of the growth in total obesity can be attributable to growth in morbid obesity (Annex Figure 2.A.3). Conversely, countries with some of the lowest absolute increases in total obesity rates, including China, India, Japan, and Korea, have the lowest share of morbid obesity growth (between 13% and 27%). Moreover, there are some significant differences by sex, with growth rates for morbid obesity in men observed to be greater than those of women in 33 out of 52 countries.
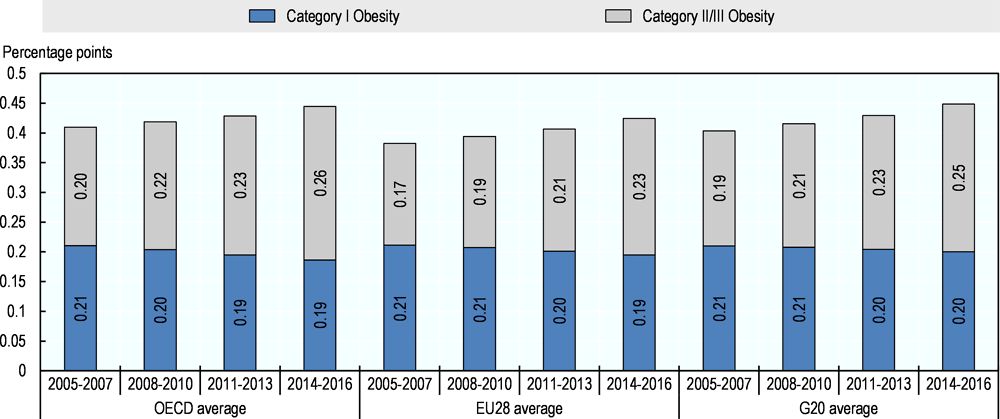
Notes: Data is age-standardised. Additional information on the comparability of this data with data in OECD.Stat can be found in Box 2.2.
Source: NCD-RisC (2017[17]), “Adult body mass index: Evolution of BMI over time”, http://ncdrisc.org/data-downloads-adiposity.html.
In children aged 5-19, obesity prevalence also steadily increased between 1975 and 2016, with similar patterns and rates of growth (an average 0.3 percentage points per year) found for OECD, EU28 and G20 countries (Figure 2.7). Among individual countries, however, there are different trends in rates of obesity over time. While most countries tend to display a steady rate of growth over time – such as in Mexico, New Zealand, and Saudi Arabia – others have accelerated, particularly in more recent years. For instance, China and South Africa have historically had a very low prevalence of obesity, but rates have been rising dramatically and are now comparable to those found in OECD countries. Conversely, in other countries, the rate of growth in obesity prevalence has been slowing over the past 20 years, such as in Denmark and Japan. For instance, the average change in obesity rate decreased by 70% in Denmark and 60% in Japan between 1996‑2005 and 2006‑16. In the United States, the country with the highest prevalence of child obesity, the rate of growth has more than halved, decreasing from a growth rate of 0.6 percentage points per year in 1995-2000 to 0.2 percentage points per year in 2011-2016.
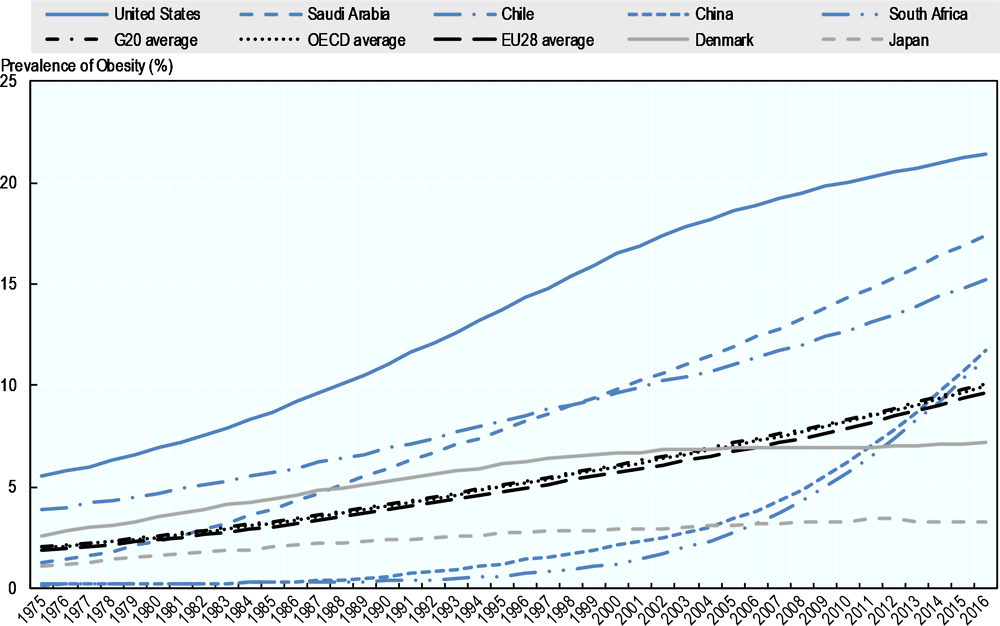
Note: Children 5‑19 years of age. Data is age-standardised.
Source: OECD analyses on WHO Global Health Observatory (2018[18]) data, “Prevalence of obesity among children and adolescents”, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adolescents/en/.
Rates of obesity are not uniformly distributed across countries, as a number of individual and sociocultural factors can influence the development of obesity. Disparities in rates of overweight have been observed among individuals of different sexes and socio-economic status (SES), indicators of which can include income, education, and social class.
For the majority of OECD, EU28, and G20 countries, rates of obesity are relatively equal between men and women (Figure 2.1). For instance, within OECD countries, an average of 23.1% of women and 23.2% of men are considered obese. A similar pattern is found in EU28 countries, as 22.4% of women are obese compared to 23.4% of men. In G20 countries, however, there is a higher prevalence of obesity among women (23.6% of women versus 19.4% of men).
Conversely, rates of pre-obesity tend to be higher in men compared to women. The average rate of pre-obesity is about ten percentage points higher in men compared to women in both OECD (29.3% in women versus 41.0% in men) and EU28 countries (29.9% in women versus 42.2% in men). Among G20 countries, the gap is narrower (27.2% in women versus 35.4% in men). Countries with higher levels of obesity, including South Africa, Saudi Arabia, Turkey and the United States also have higher inequality levels between men and women. In these countries, there is about a 10-25% difference in obesity levels between men and women.
Inequalities in income can be evaluated using the relative index of inequality (RII). RII is a statistical measure used to approximate the level of inequality in a health outcome (such as overweight and obesity) due to a socio-economic characteristic. According to OECD analysis, the majority of EU28 countries have higher rates of overweight and obesity among the bottom 20% or quintile of income-earners (hereafter referred to as the lowest income groups) compared to the top 20% or quintile of income-earners (hereafter referred to as the highest income groups) (Figure 2.8). For example, an RII or 1.5 suggests that individuals at the lowest quintile of income are 50% more likely to develop overweight or obesity than individuals at the highest quintile of income.
In general, women tend to have higher levels of income-related inequality in obesity compared to men, with the least-wealthy women being up to two to three times more likely to be obese than those with the highest level of income in ten countries. For instance, in ten countries, the least wealthy women are more than twice as likely to be obese compared to the wealthiest women. In men, there are only two countries where those at the lowest income group have double the risk of obesity, Belgium (RII=2.2) and the Netherlands (RII=2.0). Furthermore, in nine countries, men with higher levels of income are 10-20% more likely to be obese than men with lower levels of income.
In both sexes, relative inequalities in overweight are smaller than those in obesity. For 29 out of 31 countries, rates of overweight in women are higher in the lowest income group compared to the highest income group, as RII values ranged from 1.04 to 1.71. Income-related inequality in overweight rates is the highest among women living in Luxembourg, Spain, Belgium, and France (RII=1.63-1.71). On the other hand, men exhibit the opposite trend; half the countries analysed have rates of overweight that are higher in the wealthiest 20% of the male population, compared to the least wealthy group. Interestingly, countries with the lowest levels of overweight in men tend to have the highest RII values. This is seen in a similar, though lesser extent, in women. Moreover, inequalities in overweight are generally larger in western European countries compared to countries in central-eastern Europe.
Smaller gaps in both overweight and obesity prevalence between income groups are observed in men compared with women. For instance, on average, women and men in the lowest income group are, respectively, 90% and 50% more likely to be obese compared to individuals in the highest income group. Similar findings have been reported in other studies (Bilger, Kruger and Finkelstein, 2016[20]), and may be explained by theories and evidence positing that men in lower income groups are more likely to work at jobs that require manual labour and are thus more physically active (Lakdawalla and Philipson, 2009[21]). Another explanation that has been put forward is that women may be more likely to invest more energy and resources into looking thinner (Judge and Cable, 2011[22]), since they have been shown to be more affected by negative societal attitudes towards obesity (Puhl and Brownell, 2001[23]; Sattler et al., 2018[24]).
Social disparities in overweight and obesity are here assessed in relation to income levels. Another social marker, namely the education level, could be used to examine inequalities. An OECD report found that education-related inequalities in overweight are pronounced, especially among women, while inequalities are less clear-cut among men in OECD countries (OECD, 2019[25]). Overall, this pattern of inequality is consistent with the results presented in Figure 2.8, with only minor discrepancies for a small number of countries. Such differences can be explained by the fact that the distribution of the population across education levels varies from the distribution across income groups, and the marginal effects of education and income on overweight are unlikely to be identical.
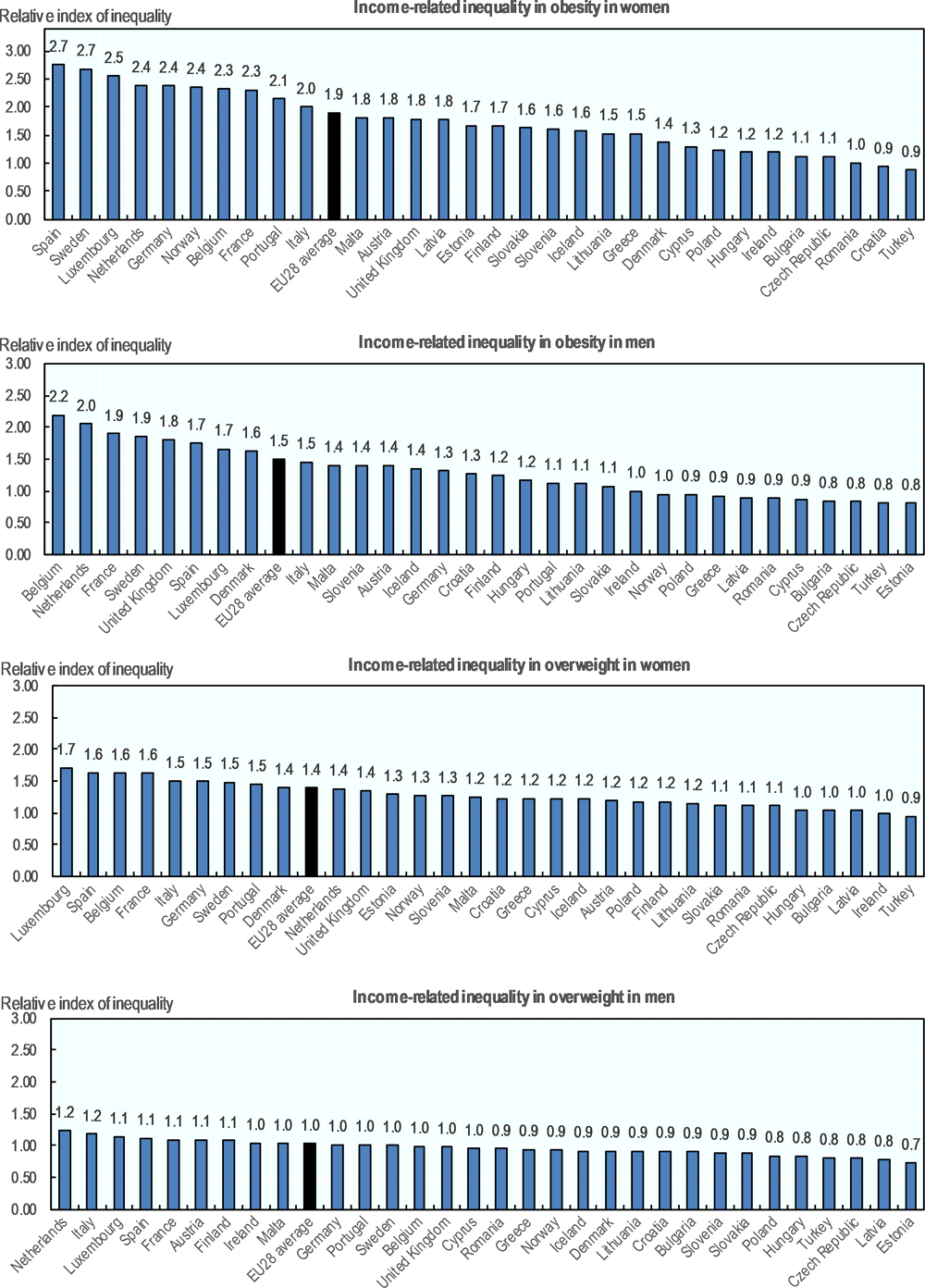
Note: Analysis includes EU28 countries and Turkey only.
Source: OECD analysis on Eurostat (2018[26]) data, “Body mass index (BMI) by sex, age and income quintile (%)”, http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_ehis_de2&lang=en.
While multiple factors contribute to weight, including genetic predisposition and environmental influences, increase in the BMI level primarily occurs due to the imbalance between energy intake from diet and energy output through physical activity (Hill, Wyatt and Peters, 2012[27]). Greater exposure to obesogenic environments, whether they are built, social, or political, has been implicated along with unhealthy dietary habits and lack of physical activity as major drivers behind the rise of overweight and obesity levels along with their associated chronic diseases. As globalisation and urbanisation have grown in the past few decades, there has been a corresponding increase in the amount of energy-dense foods consumed and a reduction of physical activity levels due to sedentary behaviour associated with the shift towards office jobs and more inactive modes of transport (Costa-Font and Mas, 2016[28]; Popkin, 2006[29]). However, overweight and its associated chronic diseases are largely preventable (Hruby and Hu, 2014[30]), and as described in Chapter 5 of this publication, effective public health actions exist to promote healthier lifestyles.
The remainder of this section looks at some of the key determinants underpinning the global epidemic of overweight and its associated chronic diseases, placing a special focus on diet and lack of physical activity.
Addressing calorie intake is widely considered as key to managing the obesity epidemic, since energy imbalance resulting from increased food intake and lower energy expenditure is associated with an increase in average population bodyweight. Over the past fifty years, total food supply has increased by nearly 20% in OECD, OECD accession and selected partner countries, EU28 and G20 countries, from 2 700 kcal/capita/day in 1961 to a little more than 3 200 kcal/capita/day in 2013 (Figure 2.10). Between 1961 and 2013 in OECD countries, total food supply grew by around 10%, or from 3 000 kcal/capita/day to 3 300 kcal/capita/day. Similarly, food supply in EU28 countries grew by approximately 8% (from 2 800 kcal/capita/day in 1961 to 3 000 kcal/capita/day). Growth in food supply was much greater in G20 and OECD accession and selected partner countries, where supply grew by around 22% (from 2 750 kcal/capita/day in 1961 to 3 350 kcal/capita/day in 2013) and 44% (from 2 000 kcal/capita/day in 1961 to 2 900 kcal/capita/day in 2013), respectively.
While it has been determined that the number of calories consumed contributes strongly to weight gain, food quality is also considered an important part of preventing weight gain. Weight gain has been associated with the consumption of processed foods that are higher in starches, refined grains, fats, and sugars, whereas weight loss was associated with consuming fruits and vegetables, whole grains, nuts, and yogurts (Mozaffarian et al., 2011[31]), even regardless of genetics or insulin-response to carbohydrates (tolerance for carbs or fat) (Gardner et al., 2018[32]). This lends support to the idea that diet quality, in addition to quantity, may play a role in determining individual’s weight.
The quality of diet may be measured in different ways and according to a number of indicators. A first parameter is a sufficient consumption of healthy dietary elements including, for example, a sufficient consumption of fibre. A second factor is the intake of nutrients that, if consumed above certain quantities, would contribute to the development of health issues (e.g. free sugar). Finally, a number of indexes have been developed to gauge the quality of diet, taking into account all foods and nutrients consumed over a period of time.
Consumption of at least 400 grams, or five portions, of fruit and vegetables per day is one of the key elements of a healthy diet (WHO, 2018[33]). However, according to recent OECD analysis, daily fruit and vegetable consumption remains low for the majority of the 11 OECD countries analysed (Graf and Cecchini, 2017[34]). The prevalence of fruit and vegetable intake, measured as meeting either the recommended daily consumption of five fruits and vegetables or fibre intake, was measured to be below 40% for 10 out of the 11 countries included for analysis, namely, Australia, Canada, Chile, England, France, Italy, Mexico, Spain, Hungary, and the United States. The only exception was Korea, where the recommended daily consumption of fibre was just under 60%.
Consumption of free sugar is already high in OECD countries and is expected to grow further in the future. Consuming excessive amounts of free sugar is considered a risk factor for overweight (Bray and Popkin, 2014[35]; Te Morenga, Mallard and Mann, 2012[36]). This is because foods or drinks with free sugars, including sugar-sweetened beverages (Malik et al., 2013[37]), may facilitate excessive calorie consumption without adding specific nutrients (Popkin et al., 2006[38]; WHO, 2019[39]). Moreover, the consumption of sugar-sweetened beverages are a marker of an unhealthy diet, as drinkers tend to consume more calories, have a poor quality of diet, and exercise less (Ranjit et al., 2010[40]; Miller et al., 2019[41]; Khan and Sievenpiper, 2016[42]). Consumption of sugar through sugary foods, such as grain-based desserts (cakes, cookies, pies) and sodas is already high in OECD countries (Figure 2.9). In addition, according to an OECD-FAO joint report (OECD/FAO, 2018[43]), calorie intake derived from sugar consumption is expected to increase by up to approximately 10 000 kcal per capita in several countries by 2027 (compared to levels in 2015-2017). This corresponds to a respective 12% and 22% increase in China and India, two countries that have among the lowest rates of obesity. Furthermore, in the United States, the country with the highest levels of obesity, calorie intake from sugar is projected to increase by 6 000 kilocalories by 2027, or by more than 5%.
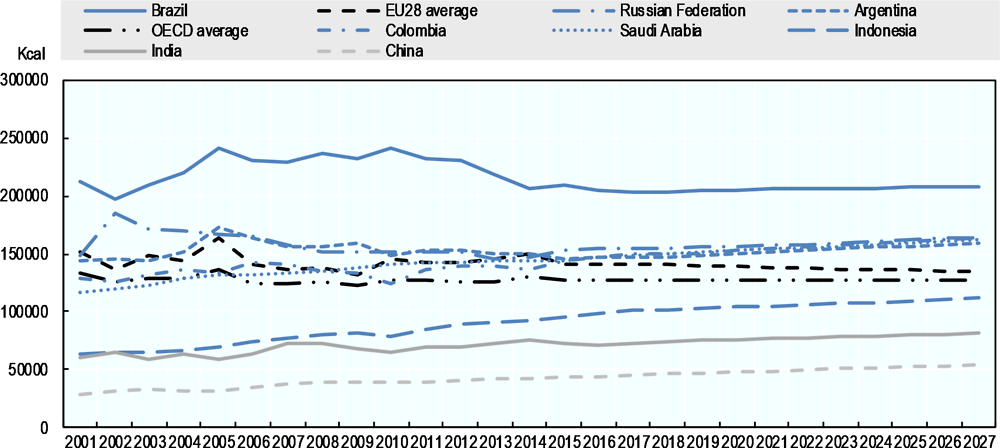
Source: OECD/FAO (2018[43]), OECD-FAO Agricultural Outlook 2018-2027, https://dx.doi.org/10.1787/agr_outlook-2018-en.
Other nutrients with the potential to support growth in overweight and its associated chronic diseases are also consumed in higher quantities. A large portion of the increase in calorie supply in OECD, EU28 and G20 countries is driven by an increase in production of animal products (from 672 kcal/capita/day in 1961 to 853 kcal/capita/day in 2013) (Figure 2.10). There was a great increase in animal product supply in OECD accession and selected partner countries (166%) and EU28 member states (74%), while G20 countries and OECD countries had smaller growth rates: 19% and 9% respectively, between 1961 and 2013.
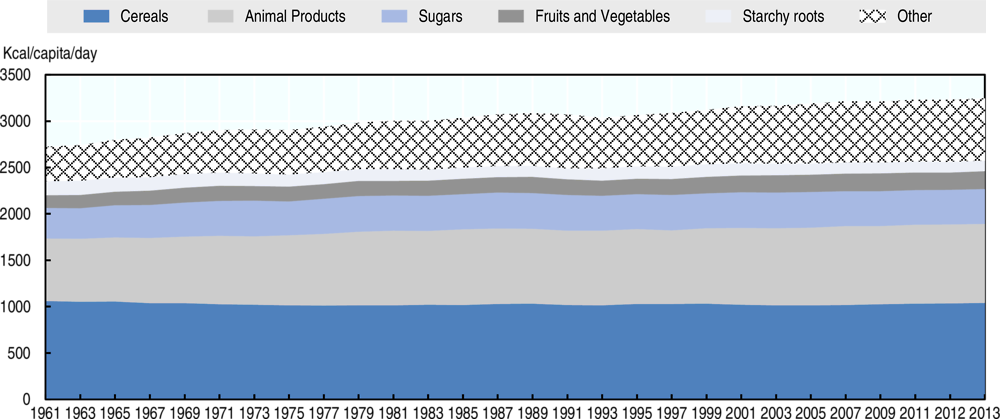
Note: Animal products include animal meat, animal fat, offal, eggs, fish and seafood, and dairy.
Source: OECD/FAO (2018[43]), OECD-FAO Agricultural Outlook 2018-2027, https://dx.doi.org/10.1787/agr_outlook-2018-en.
Finally, beyond fruit and vegetable consumption or consumption of specific nutrients, quality of diet can be measured in multiple other ways. The Mediterranean Diet Score, Healthy Food Index, and scores based on nutritional intake have all been used to assess diet quality (Burggraf et al., 2018[44]). By applying these composite indexes of food quality, an OECD analysis of 11 countries found that, in a number of countries (Chile, Italy, Mexico and Spain), a little more than half of the population consumes a healthy diet, as according to the national guidelines and international standards. In the United Kingdom, less than one in three persons were found to consume a healthy diet (Graf and Cecchini, 2017[34])
Some population groups are more likely to have an unhealthy diet. According to the OECD analyses on national data of 11 countries, women are more likely than men to have a healthy diet and consume at least five fruits and vegetables per day in countries such as Australia, Canada, Chile, England, France, Italy, and Spain, whereas they are less likely to achieve the five portions a day threshold in Hungary, Korea, and the United States (Graf and Cecchini, 2017[34]). For instance, in Canada, the odds of consuming the recommended amount of fruits and vegetables are up to 2.3 times higher in women compared to men.
Individuals with different education and SES levels have different dietary patterns. Continuing with the OECD study based on 11 countries, those who are highly educated are more likely to consume recommended amounts of fruits and vegetables (odds ratio [OR] up to 2.1) and have a healthier diet (OR up to 1.4) compared to those with medium or low levels of education (Graf and Cecchini, 2017[45]). Nonetheless, there are some exceptions. For example, in Chile, Italy, and Korea, fruit and vegetable consumption are almost equal between education groups, whereas in Chile, Mexico, and Spain, the odds of consuming a healthy diet are also not significantly different. In general, individuals with a lower SES are less likely to consume a sufficient amount of fruit and vegetables or have a healthy diet, though fewer results are significant. This is consistent with studies reporting that the effect of education on quality of diet is at least as great or stronger than other socio-economic indicators, such as income (Monsivais and Drewnowski, 2009[46]; Si Hassen et al., 2016[47]). One study found that more highly educated individuals reported higher quality and therefore more costly diets, regardless of income level (Monsivais and Drewnowski, 2009[48]).
Overweight is often conceptualised using the energy balance equation, which states that weight gain occurs when energy intake exceeds energy expenditure, representing a positive energy imbalance. The opposite also holds true; weight loss is thought to occur when energy expenditure exceeds energy intake, representing a negative energy imbalance. Energy expenditure is comprised of several components, including resting metabolic rate, thermic effect of food (energy associated with the digestion and processing of food), and physical activity (Hall et al., 2012[49]). Physical activity, in particular, is the second largest component of daily energy expenditure (FAO, 2003[50]) following resting metabolic rate – i.e. the energy burnt by the body in a state of complete rest – and accounts for approximately 10-30% of calories burned every day (Westerterp et al., 1996[51]; Westerterp, 2013[52]). However, compared to resting metabolic rate, physical activity is more variable (Caudwell et al., 2013[53]; Westerterp, 2018[54]). Thus, interventions can be used to target and influence physical activity levels to increase energy expenditure, thereby promoting weight loss. In addition, more time spent on physical activity, which involves higher energy expenditure, means less time for sedentary behaviour (Box 2.3) and more opportunities to contribute to a negative energy imbalance. This is important because on average, adults spend more than half of their waking time in sedentary behaviour, at work, in leisure, or in transport (Clark and Sugiyama, 2015[55]).
Alongside physical activity, another important dimension to consider is excessive sedentary behaviour, which should not be confused with lack of physical activity. Sedentary behaviour is characterised as any waking behaviour involving low-energy expenditure, such as when an individual is lying, reclining, sitting, or standing (Sedentary Behavior Research Network, 2017[56]). Physical inactivity, on the other hand, is defined as performing insufficient amounts of recommended moderate to vigorous physical activity (Bull, 2003[57]). Individuals can be sedentary yet physically active, and vice-versa (van der Ploeg and Hillsdon, 2017[58]). As an example of the former state, individuals can sit for the majority of the week but still achieve 150 minutes or more of moderate-vigorous physical activity per week. As an example of the latter, individuals with standing occupations can spend little of their time in a sedentary state and not complete any physical activity.
Sedentary behaviour is also distinct from physical activity as a risk factor for mortality, cardiovascular disease, certain cancers, hypertension, and diabetes (Rezende et al., 2014[59]; Thorp et al., 2011[60]). Independent of changes to physical activity, more time spent on sedentary behaviours, such as television viewing, has been associated with significant increases in waist circumference in both men and women (Wijndaele et al., 2010[61]; Wijndaele et al., 2010[62]). Significant detrimental effects of television viewing have also been observed with waist circumference, systolic blood pressure, and markers of metabolic risk, even among physically active men and women (Healy et al., 2008[63]).
In recognition of the detrimental effects of sedentary behaviours, the World Health Organization (WHO) has put forth recommendations on screen time for children under the age of five, such as not exposing children under the age of one to any screen time and that screen time should be limited to less than one hour per day for children between one and four years of age (WHO, 2019[64]).
An OECD analysis on use of time and domains of physical activity (Box 2.4) in Canada, France, Germany, and the United States (Figure 2.11) found that men and women spend between 80 minutes and 105 minutes per day on physical activity, which consists of sport, domestic physical activity, active travel, and occupational physical activity (Graf and Cecchini, 2019[65]). Moreover, men spend an average of 720 minutes per day on sedentary behaviour, which also includes work, and motorised travel, whereas women spend about 620 minutes per day on these same activities.
Four areas of daily living have been identified in which physical activity occurs (Bull et al., 2004[66]; Pratt et al., 2004[67]). These include the home, transport, workplace, and leisure time (Sallis et al., 2006[68]). Collectively, these areas are known as the domains of physical activity.
|
Physical activity domain |
Definition or examples |
|---|---|
|
Domestic |
Can include household chores, gardening, child care, shopping, moving heavy objects, and incidental physical activity |
|
Transport |
Walking or cycling for transport, walking or climbing stairs to access public transport |
|
Occupational |
Work-related physical activity, may involve manual labour, walking, lifting or carrying objects |
|
Leisure time |
Includes various types of recreational activities, including hobbies, sports, and exercise |
Differences involving time spent on physical activity and sedentary behaviour differs by sex and country (Graf and Cecchini, 2019[65]). Overall, women spend more time on total physical activity than men do, but some differences exist. Women report 15 additional minutes of domestic physical activity per day, compared to men (i.e. 57 minutes versus 41 minutes). Conversely, on average, men spend slightly more time on leisure sports (i.e. 17 minutes versus 13 minutes) than women do. Moreover, both men and women spend between 2 and 15 minutes in daily active travel. Time spent on domain-specific physical activity differs by country as well. Men and women in France spend the most time on active transport (12 and 15.7 minutes, respectively), followed by men and women in Germany (10 and 11 minutes, respectively), Canada (5.1 and 5.6 minutes, respectively), and the United States (3.3 and 2.5 minutes, respectively). Men in Canada and Germany spend the most time on leisure sports (20.4 and 18.8 minutes per day, respectively), which accounts for about 20% of their daily physical activity.
On average, men and women spend more than six hours a day on sedentary activities – approximately 40% of waking time. In general, women tend to spend less time on sedentary behaviours (375 minutes versus 382 minutes). Men in Germany and France have the highest levels of sedentary behaviour (423 and 414 minutes, respectively). In addition to this, men also spend more time working, as they spend about 270 minutes compared to women, who spend about 180 minutes. Both men and women also spend an average of around one hour on motorised travel, with men spending on average seven more minutes on motorised travel (i.e. 67 minutes versus 60 minutes) than women. Among these individuals, men in the United States and France spend the most time using motorised travel (73 and 70 minutes, respectively).
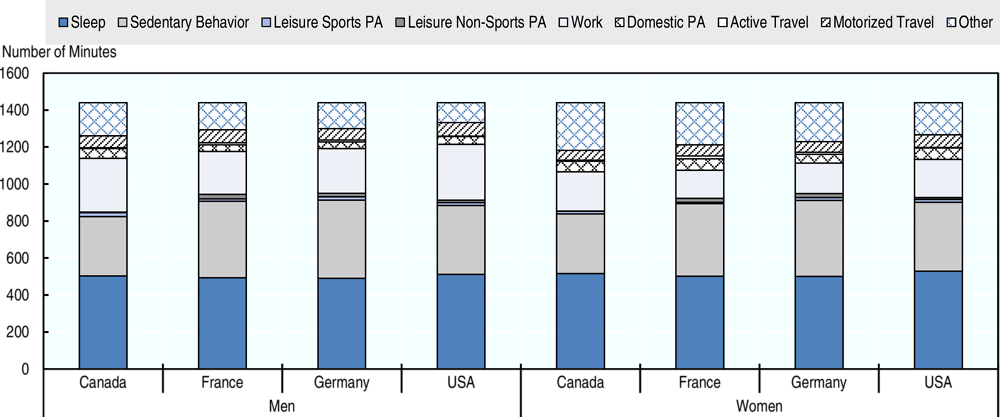
Source: Graf and Cecchini (2019[65]), “Current and past trends in physical activity in four OECD countries: Empirical results from time use surveys in Canada, France, Germany and the United States”, https://doi.org/10.1787/22cad404-en.
Regular physical activity (Box 2.5), and even light-intensity physical activity (Füzéki, Engeroff and Banzer, 2017[69]), has a number of health benefits, including the prevention of NCDs (such as cardiovascular disease, diabetes, and cancer), hypertension, obesity, depression, and premature mortality (Warburton and Bredin, 2017[70]; Warburton, Nicol and Bredin, 2006[71]; Reiner et al., 2013[72]). Despite these health benefits, in 2016, the prevalence of insufficient physical activity among adults was greater than 40% in 13 countries (Figure 2.12). In OECD countries, about one-third (32.1%) of individuals perform insufficient amounts of physical activity, whereas this value is slightly higher in EU28 (33.1%) and G20 (34.0%) countries. The highest levels of insufficient physical activity are found in Saudi Arabia, which had a prevalence of 53.1%, whereas the lowest levels are found in China, with a prevalence of 14.1%. Across all countries, except for China, Finland and Indonesia, rates of insufficient physical activity are higher among women compared to men. The disparity between the sexes is greatest in Costa Rica, India, Saudi Arabia, South Africa, Turkey, and the United States, with differences as high as 20 percentage points.
If current trends continue, then prevalence of insufficient physical activity is expected to rise. An analysis of trends in physical activity levels between 2001 and 2016 of 169 countries found that insufficient physical activity, defined as not meeting the physical activity recommendations as set out by WHO, increased by more than 5 percentage points in high-income Western countries but remained substantially stable in high-income countries in the Asia-Pacific region (Guthold et al., 2018[73]).
The WHO global recommendations on physical activity for health were developed in order to promote physical activity as a primary prevention of NCDs at the population level (WHO, 2010[74]; WHO, 2019[64]). These guidelines are presented below.
at least 30 minutes of physical activity.
at least 180 minutes of physical activity in any intensity spread throughout the day.
at least 60 minutes of moderate to vigorous intensity physical activity per day
more than 60 minutes of daily physical activity may bring about additional health benefits
most daily physical activity should be aerobic, and vigorous intensity physical activity should be performed at least 3 times per week.
at least 150 minutes of moderate to vigorous intensity physical activity per week, or at least 75 minutes of vigorous intensity physical activity per week
aerobic activity should be performed in bouts of at least 10 minutes
to attain additional health benefits, moderate-intensity aerobic physical activity should be performed for 300 minutes per week. Adults can also engage in 150 minutes of moderate-to-vigorous or vigorous-intensity aerobic physical activity per week for more health benefits.
at least 150 minutes of moderate aerobic exercise per week, or at least 75 minutes of vigorous aerobic physical activity per week.
it is also recommended to perform aerobic activity in bouts of at least 10 minutes.
for additional health benefits, adults aged 65 and above should perform moderate intensity aerobic physical activity for 300 minutes per week, or engage in 150 minutes of moderate-to-vigorous or vigorous intensity activity.
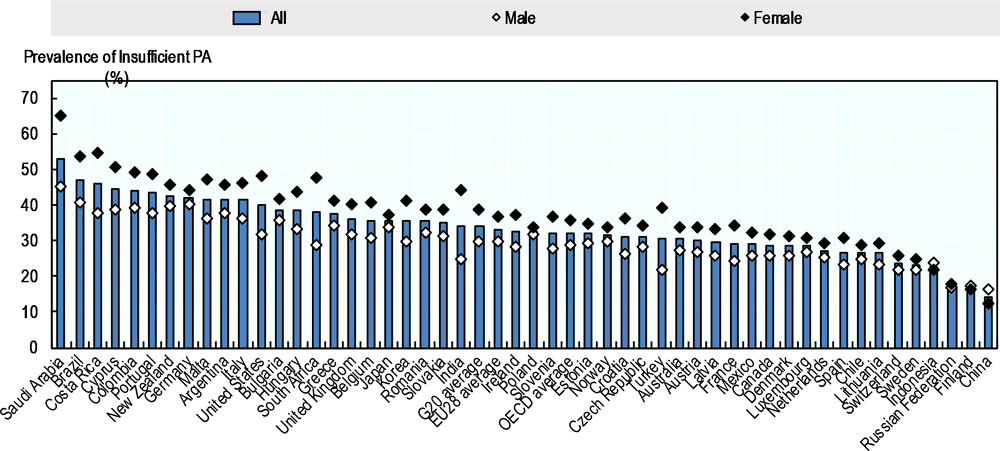
Note: Data unavailable for Iceland, Israel, and Peru. Data is age-standardised.
Source: WHO (2018[75]), “Prevalence of insufficient physical activity among adults”, http://apps.who.int/gho/data/node.main.A893?lang=en.
Just as there are gender and SES gaps in prevalence of overweight, there are also disparities between different groups in meeting recommended physical activity levels. According to an OECD analysis of 11 countries, women are less likely to achieve the amount of physical activity recommended by WHO (see Box 2.5 for further information on WHO thresholds) compared to men (Graf and Cecchini, 2017[34]). In general, men and those with higher levels of education are about 20-50% more likely to have sufficient levels of physical activity than those with low levels of education. Exceptions to this association include Chile, where level of education was found to minimally impact the amount of physical activity achieved (OR = 1.04), as well as Mexico, in which highly-educated individuals are less likely (OR = 0.73) to achieve the recommended physical activity levels compared to those with a low or medium level of education. The relationship between SES and sufficient physical activity is less clear. SES was not found to be significant in England, Korea, or Spain, while physical activity was positively associated with SES in Australia and the United States. For instance, in Australia, the odds of achieving sufficient amounts of physical activity are 60% higher in high-SES individuals compared to their lower SES counterparts.
In general, men are more likely to demonstrate excessive sedentary behaviour (see Box 2.3 for further information on the definition of sedentary behaviours) (Graf and Cecchini, 2017[34]). In Australia, Korea, Mexico, Spain, and the United States, those with higher levels of education are more likely to be sedentary than those with lower levels of education. Overall, high-SES individuals are about two to three times more likely to display sedentary behaviour compared to lower income groups in Australia, Chile, England, and Spain. The same relationship can be seen in Korea, Mexico, and the United States, though the difference is not as large (OR = 1.36, 1.62, and 1.82, respectively).
Unhealthy lifestyles, including poor diet, physical inactivity and sedentary behaviours, tend to occur simultaneously in specific population groups that can be identified through their demographic and socio-economic characteristics. These population groups should be considered a top priority for policy action to tackle unhealthy lifestyles, as they are at highest risk of developing chronic diseases.
Based on the results of an OECD analysis on the most recent waves of national health surveys from Brazil Chile, England, Korea, Mexico, Spain, and the United States, the following conclusions can be drawn (Graf and Cecchini, 2017[34]; Graf and Cecchini, 2018[76]):
Men tend to have more unhealthy lifestyles than women. In all the included countries, except for the United States, men consistently report more unhealthy diets and more excessive sedentary behaviour than women. However, men are more likely to achieve the recommended amount of physical activity compared to women.
The effect of education varies across different dimensions, such as diet and physical activity. Individuals with a lower level of education are more likely to consume an unhealthy diet. Furthermore, less-educated individuals are also less likely to be physically active, but they are also less likely to demonstrate sedentary behaviours.
Individuals with low SES are also more likely to report an unhealthy diet. However, in the majority of countries, individuals with high SES are more likely to report higher sedentary behaviours. Moreover, individuals with higher SES (defined by taking into account occupation or income) are less likely to achieve the recommended level of physical activity. Overall, when all the dimensions (i.e. both diet and physical activity) are taken into account, individuals with high SES tend to have more unhealthy lifestyles, mainly due to the lower level of physical activity and higher level of excessive sedentary behaviour;
Unhealthy lifestyles go beyond overweight. With the exception of the United States, overweight and obesity are not strong predictors for unhealthy diets, insufficient physical activity, or excessive sedentary behaviour. Thus, policies to tackle unhealthy lifestyles should not exclusively focus on individuals with overweight but should be based on a broader perspective.
Obesity continues to be a pressing global issue, as rates have grown over the past few decades in all OECD, OECD accession and selected partner countries, EU28 and G20 countries. Western countries that have historically had the highest rates of obesity continue to have the greatest prevalence of obesity, though non-western countries have also seen large increases in obesity prevalence over the past forty years. Particularly of note are trends in morbid obesity, where countries with some of the highest rates and largest increases in obesity also have a corresponding higher proportion of morbid obesity growth. Rates of childhood obesity growth are also worrisome – in countries such as China, Saudi Arabia, and South Africa, child obesity has grown significantly in the past few decades. As discussed in the next chapter, this has significant implications for the burden of disease and health costs for the years to come. Certain population groups including women, the less-educated, and lower-income groups are of particular concern as they are more likely to be obese.
Several factors have been identified as key drivers of the obesity epidemic, including diet, physical activity, and sedentary behaviour. These behaviours differ by geographical context, but several patterns have emerged. Firstly, calorie availability has been growing over the past half century and is expected to grow, particularly for certain nutrients, such as sugar. Secondly, rates of insufficient physical activity remain high particularly in women. Additionally, in general, more disadvantaged groups, including the less-educated and low-income individuals, were less likely to have a healthy diet or achieve sufficient levels of physical activity. All these unhealthy lifestyles can be tackled by effective and efficient policy options, as discussed in Chapter 5 and Chapter 6.
[3] Abdelaal, M., C. le Roux and N. Docherty (2017), “Morbidity and mortality associated with obesity”, Annals of Translational Medicine, Vol. 5/7, pp. 161-161, http://dx.doi.org/10.21037/atm.2017.03.107.
[20] Bilger, M., E. Kruger and E. Finkelstein (2016), “Measuring Socioeconomic Inequality in Obesity: Looking Beyond the Obesity Threshold”, Health Economics, Vol. 26/8, pp. 1052-1066, http://dx.doi.org/10.1002/hec.3383.
[35] Bray, G. and B. Popkin (2014), “Dietary Sugar and Body Weight: Have We Reached a Crisis in the Epidemic of Obesity and Diabetes?”, Diabetes Care, Vol. 37/4, pp. 950-956, http://dx.doi.org/10.2337/dc13-2085.
[57] Bull, F. (2003), “Defining physical inactivity”, The Lancet, Vol. 361/9353, pp. 258-259, http://dx.doi.org/10.1016/s0140-6736(03)12290-8.
[66] Bull, F. et al. (2004), “Physical inactivity”, in Comparative Quantification of Health Risks, WHO, Geneva.
[44] Burggraf, C. et al. (2018), “Review of a priori dietary quality indices in relation to their construction criteria”, Nutrition Reviews, Vol. 76/10, pp. 747-764, http://dx.doi.org/10.1093/nutrit/nuy027.
[53] Caudwell, P. et al. (2013), “Physical Activity, Energy Intake, and Obesity: The Links Between Exercise and Appetite”, Current Obesity Reports, Vol. 2/2, pp. 185-190, http://dx.doi.org/10.1007/s13679-013-0051-1.
[11] CDC (2017), About Adult BMI, https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html.
[55] Clark, B. and T. Sugiyama (2015), “Prevalence, Trends, and Correlates of Sedentary Behavior”, in Physical Activity, Exercise, Sedentary Behavior and Health, Springer Japan, Tokyo, http://dx.doi.org/10.1007/978-4-431-55333-5_8.
[15] Cole, T. and T. Lobstein (2012), “Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity”, Pediatric Obesity, Vol. 7/4, pp. 284-294, http://dx.doi.org/10.1111/j.2047-6310.2012.00064.x.
[28] Costa-Font, J. and N. Mas (2016), “‘Globesity’? The effects of globalization on obesity and caloric intake”, Food Policy, Vol. 64, pp. 121-132, http://dx.doi.org/10.1016/j.foodpol.2016.10.001.
[19] Devaux, M. et al. (2017), OECD Obesity Update 2017, OECD, http://www.oecd.org/health/obesity-update.htm (accessed on 4 February 2019).
[26] Eurostat (2018), Body mass index (BMI) by sex, age and income quintile (%), http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_ehis_de2&lang=en (accessed on 16 April 2019).
[50] FAO (2003), Human energy requirements: Principles and definitions, http://www.fao.org/3/y5686e/y5686e04.htm (accessed on 8 April 2019).
[69] Füzéki, E., T. Engeroff and W. Banzer (2017), “Health Benefits of Light-Intensity Physical Activity: A Systematic Review of Accelerometer Data of the National Health and Nutrition Examination Survey (NHANES)”, Sports Medicine, Vol. 47/9, pp. 1769-1793, http://dx.doi.org/10.1007/s40279-017-0724-0.
[32] Gardner, C. et al. (2018), “Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association With Genotype Pattern or Insulin Secretion”, JAMA, Vol. 319/7, p. 667, http://dx.doi.org/10.1001/jama.2018.0245.
[65] Graf, S. and M. Cecchini (2019), “Current and past trends in physical activity in four OECD countries: Empirical results from time use surveys in Canada, France, Germany and the United States”, No. 112, OECD, Paris, https://doi.org/10.1787/22cad404-en (accessed on 26 June 2019).
[76] Graf, S. and M. Cecchini (2018), “Identifying patterns of unhealthy diet and physical activity in four countries of the Americas: a latent class analysis”, Revista Panamericana de Salud Pública, Vol. 42, http://dx.doi.org/10.26633/rpsp.2018.56.
[34] Graf, S. and M. Cecchini (2017), Diet, physical activity and sedentary behaviours: Analysis of trends, inequalities and clustering in selected OECD countries, https://www.oecd-ilibrary.org/social-issues-migration-health/diet-physical-activity-and-sedentary-behaviours_54464f80-en (accessed on 4 February 2019).
[45] Graf, S. and M. Cecchini (2017), Diet, physical activity and sedentary behaviours: Analysis of trends, inequalities and clustering in selected OECD countries, https://www.oecd-ilibrary.org/social-issues-migration-health/diet-physical-activity-and-sedentary-behaviours_54464f80-en (accessed on 4 February 2019).
[4] Guh, D. et al. (2009), “The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis”, BMC Public Health, Vol. 9/1, http://dx.doi.org/10.1186/1471-2458-9-88.
[73] Guthold, R. et al. (2018), “Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants”, The Lancet Global Health, Vol. 6/10, pp. e1077-e1086, http://dx.doi.org/10.1016/s2214-109x(18)30357-7.
[49] Hall, K. et al. (2012), “Energy balance and its components: implications for body weight regulation”, The American Journal of Clinical Nutrition, Vol. 95/4, pp. 989-994, http://dx.doi.org/10.3945/ajcn.112.036350.
[63] Healy, G. et al. (2008), “Television Time and Continuous Metabolic Risk in Physically Active Adults”, Medicine & Science in Sports & Exercise, Vol. 40/4, pp. 639-645, http://dx.doi.org/10.1249/mss.0b013e3181607421.
[27] Hill, J., H. Wyatt and J. Peters (2012), “Energy Balance and Obesity”, Circulation, Vol. 126/1, pp. 126-132, http://dx.doi.org/10.1161/circulationaha.111.087213.
[30] Hruby, A. and F. Hu (2014), “The Epidemiology of Obesity: A Big Picture”, PharmacoEconomics, Vol. 33/7, pp. 673-689, http://dx.doi.org/10.1007/s40273-014-0243-x.
[22] Judge, T. and D. Cable (2011), “When it comes to pay, do the thin win? The effect of weight on pay for men and women.”, Journal of Applied Psychology, Vol. 96/1, pp. 95-112, http://dx.doi.org/10.1037/a0020860.
[12] Kanazawa, M. et al. (2002), “Criteria and classification of obesity in Japan and Asia-Oceania”, Asia Pacific Journal of Clinical Nutrition, Vol. 11/s8, pp. S732-S737, http://dx.doi.org/10.1046/j.1440-6047.11.s8.19.x.
[42] Khan, T. and J. Sievenpiper (2016), “Controversies about sugars: results from systematic reviews and meta-analyses on obesity, cardiometabolic disease and diabetes”, European Journal of Nutrition, Vol. 55/S2, pp. 25-43, http://dx.doi.org/10.1007/s00394-016-1345-3.
[21] Lakdawalla, D. and T. Philipson (2009), “The growth of obesity and technological change”, Economics & Human Biology, Vol. 7/3, pp. 283-293, http://dx.doi.org/10.1016/j.ehb.2009.08.001.
[59] Lucia, A. (ed.) (2014), “Sedentary Behavior and Health Outcomes: An Overview of Systematic Reviews”, PLoS ONE, Vol. 9/8, p. e105620, http://dx.doi.org/10.1371/journal.pone.0105620.
[10] Maffeis, C. and L. Tatò (2001), “Long-Term Effects of Childhood Obesity on Morbidity and Mortality”, Hormone Research in Paediatrics, Vol. 55/1, pp. 42-45, http://dx.doi.org/10.1159/000063462.
[37] Malik, V. et al. (2013), “Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis”, The American Journal of Clinical Nutrition, Vol. 98/4, pp. 1084-1102, http://dx.doi.org/10.3945/ajcn.113.058362.
[41] Miller, C. et al. (2019), “Who drinks sugar sweetened beverages and juice? An Australian population study of behaviour, awareness and attitudes”, BMC Obesity, Vol. 6/1, p. 1, http://dx.doi.org/10.1186/s40608-018-0224-2.
[48] Monsivais, P. and A. Drewnowski (2009), “Lower-Energy-Density Diets Are Associated with Higher Monetary Costs per Kilocalorie and Are Consumed by Women of Higher Socioeconomic Status”, Journal of the American Dietetic Association, Vol. 109/5, pp. 814-822, http://dx.doi.org/10.1016/j.jada.2009.02.002.
[46] Monsivais, P. and A. Drewnowski (2009), “Lower-Energy-Density Diets Are Associated with Higher Monetary Costs per Kilocalorie and Are Consumed by Women of Higher Socioeconomic Status”, Journal of the American Dietetic Association, Vol. 109/5, pp. 814-822, http://dx.doi.org/10.1016/j.jada.2009.02.002.
[31] Mozaffarian, D. et al. (2011), “Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men”, New England Journal of Medicine, Vol. 364/25, pp. 2392-2404, http://dx.doi.org/10.1056/nejmoa1014296.
[17] NCD-RisC (2017), Adult body mass index: Evolution of BMI over time, http://ncdrisc.org/data-downloads-adiposity.html (accessed on 16 April 2019).
[25] OECD (2019), Health for Everyone?: Social Inequalities in Health and Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/3c8385d0-en.
[2] OECD (2010), Obesity and the Economics of Prevention: Fit not Fat, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264084865-en.
[43] OECD/FAO (2018), OECD-FAO Agricultural Outlook 2018-2027, OECD Publishing, Paris/Food and Agriculture Organization of the United Nations, Rome, https://dx.doi.org/10.1787/agr_outlook-2018-en.
[29] Popkin, B. (2006), “Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases1–3”, The American Journal of Clinical Nutrition, Vol. 84/2, pp. 289-298, http://dx.doi.org/10.1093/ajcn/84.1.289.
[38] Popkin, B. et al. (2006), A new proposed guidance system for beverage consumption in the United States, http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.879.7714&rep=rep1&type=pdf.
[67] Pratt, M. et al. (2004), “Economic interventions to promote physical activity”, American Journal of Preventive Medicine, Vol. 27/3, pp. 136-145, http://dx.doi.org/10.1016/j.amepre.2004.06.015.
[5] Prospective Studies Collaboration, P. et al. (2009), “Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies.”, Lancet (London, England), Vol. 373/9669, pp. 1083-96, http://dx.doi.org/10.1016/S0140-6736(09)60318-4.
[23] Puhl, R. and K. Brownell (2001), “Bias, Discrimination, and Obesity”, Obesity Research, Vol. 9/12, pp. 788-805, http://dx.doi.org/10.1038/oby.2001.108.
[40] Ranjit, N. et al. (2010), “Dietary and activity correlates of sugar-sweetened beverage consumption among adolescents.”, Pediatrics, Vol. 126/4, pp. e754-61, http://dx.doi.org/10.1542/peds.2010-1229.
[8] Reilly, J. (2003), “Health consequences of obesity”, Archives of Disease in Childhood, Vol. 88/9, pp. 748-752, http://dx.doi.org/10.1136/adc.88.9.748.
[9] Reilly, J. and J. Kelly (2010), “Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review”, International Journal of Obesity, Vol. 35/7, pp. 891-898, http://dx.doi.org/10.1038/ijo.2010.222.
[72] Reiner, M. et al. (2013), “Long-term health benefits of physical activity – a systematic review of longitudinal studies”, BMC Public Health, Vol. 13/1, p. 813, http://dx.doi.org/10.1186/1471-2458-13-813.
[68] Sallis, J. et al. (2006), “An ecological approach to creating active living communities”, Annual Review of Public Health, Vol. 27/1, pp. 297-322, http://dx.doi.org/10.1146/annurev.publhealth.27.021405.102100.
[24] Sattler, K. et al. (2018), “Gender differences in the relationship of weight-based stigmatisation with motivation to exercise and physical activity in overweight individuals”, Health Psychology Open, Vol. 5/1, p. 205510291875969, http://dx.doi.org/10.1177/2055102918759691.
[56] Sedentary Behavior Research Network (2017), “Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome”, International Journal of Behavioral Nutrition and Physical Activity, Vol. 14/1, http://dx.doi.org/10.1186/s12966-017-0525-8.
[47] Si Hassen, W. et al. (2016), “Socioeconomic Indicators Are Independently Associated with Nutrient Intake in French Adults: A DEDIPAC Study.”, Nutrients, Vol. 8/3, p. 158, http://dx.doi.org/10.3390/nu8030158.
[36] Te Morenga, L., S. Mallard and J. Mann (2012), “Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies”, BMJ, Vol. 346/jan15 3, pp. e7492-e7492, http://dx.doi.org/10.1136/bmj.e7492.
[60] Thorp, A. et al. (2011), “Sedentary Behaviors and Subsequent Health Outcomes in Adults”, American Journal of Preventive Medicine, Vol. 41/2, pp. 207-215, http://dx.doi.org/10.1016/j.amepre.2011.05.004.
[58] van der Ploeg, H. and M. Hillsdon (2017), “Is sedentary behaviour just physical inactivity by another name?”, The international journal of behavioral nutrition and physical activity, Vol. 14/1, p. 142, http://dx.doi.org/10.1186/s12966-017-0601-0.
[70] Warburton, D. and S. Bredin (2017), “Health benefits of physical activity: a systematic review of current systematic reviews”, Current Opinion in Cardiology, Vol. 32/5, pp. 541-556, http://dx.doi.org/10.1097/HCO.0000000000000437.
[71] Warburton, D., C. Nicol and S. Bredin (2006), “Health benefits of physical activity: the evidence.”, CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, Vol. 174/6, pp. 801-809, http://dx.doi.org/10.1503/cmaj.051351.
[54] Westerterp, K. (2018), “Exercise, energy balance and body composition”, European Journal of Clinical Nutrition, Vol. 72/9, pp. 1246-1250, http://dx.doi.org/10.1038/s41430-018-0180-4.
[52] Westerterp, K. (2013), “Physical activity and physical activity induced energy expenditure in humans: measurement, determinants, and effects”, Frontiers in Physiology, Vol. 4, http://dx.doi.org/10.3389/fphys.2013.00090.
[51] Westerterp, K. et al. (1996), “Energy expenditure and physical activity in subjects consuming full-or reduced-fat products as part of their normal diet.”, The British journal of nutrition, Vol. 76/6, pp. 785-95, http://www.ncbi.nlm.nih.gov/pubmed/9014648 (accessed on 17 April 2019).
[14] WHO (2019), Body mass index - BMI, http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 10 April 2019).
[64] WHO (2019), Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age, https://apps.who.int/iris/bitstream/handle/10665/311664/9789241550536-eng.pdf?sequence=1&isAllowed=y (accessed on 14 May 2019).
[39] WHO (2019), Reducing free sugars intake in adults to reduce the risk of noncommunicable diseases, WHO, https://www.who.int/elena/titles/free-sugars-adults-ncds/en/ (accessed on 19 April 2019).
[7] WHO (2019), Why does childhood overweight and obesity matter?, https://www.who.int/dietphysicalactivity/childhood_consequences/en/ (accessed on 8 February 2019).
[33] WHO (2018), Healthy diet, https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 16 April 2019).
[1] WHO (2018), Obesity and overweight, https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 January 2019).
[75] WHO (2018), Prevalence of insufficient physical activity among adults, WHO, http://apps.who.int/gho/data/node.main.A893?lang=en (accessed on 16 April 2019).
[6] WHO (2017), 10 facts on obesity, WHO, http://dx.doi.org/111111.
[74] WHO (2010), Global recommendations on physical activity for health, https://apps.who.int/iris/bitstream/handle/10665/44399/9789241599979_eng.pdf;jsessionid=99CCB9D95277EB40CA55E9A49483B493?sequence=1 (accessed on 16 April 2019).
[13] WHO Expert Consultation (2004), “Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies”, The Lancet, Vol. 363/9403, pp. 157-163, http://dx.doi.org/10.1016/s0140-6736(03)15268-3.
[16] WHO Global Health Observatory (2018), Mean body mass index (BMI) trends among adults, WHO, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/bmi_trends_adults/en/ (accessed on 5 April 2019).
[18] WHO Global Health Observatory (2018), Prevalence of obesity among children and adolescents, WHO, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adolescents/en/ (accessed on 16 April 2019).
[61] Wijndaele, K. et al. (2010), “Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk Study”, International Journal of Epidemiology, Vol. 40/1, pp. 150-159, http://dx.doi.org/10.1093/ije/dyq105.
[62] Wijndaele, K. et al. (2010), “Increased Cardiometabolic Risk Is Associated with Increased TV Viewing Time”, Medicine & Science in Sports & Exercise, Vol. 42/8, pp. 1511-1518, http://dx.doi.org/10.1249/mss.0b013e3181d322ac.
Annex Table 2.A.1 presents the list of countries included in the analysis and its affiliation to the various groups, including OECD countries, OECD accession and selected partner countries, EU28 member states and G20 countries. Countries can be part of multiple groups at the same time and contribute to the calculation of averages for all the group they are part of.
Annex Figure 2.A.1 details the prevalence of childhood pre-obesity and obesity by sex in OECD countries, OECD accession and selected partner countries, EU28 member states and G20 countries. This includes children between 5 and 19 years of age.
Annex Figure 2.A.2 shows adult overweight trends between the years 1996, 2006, and 2016 among OECD countries, OECD accession and selected partner countries, EU28 member states and G20 countries.
Annex Figure 2.A.3 represents country-specific trends of class I and class II/III (morbid) obesity between the years 2005 and 2016 via three-year averages. Percentages reflect the proportion of total obesity change that is change in morbid obesity.
|
Country |
OECD |
OECD accession and selected partner countries |
EU28 |
G20 |
|---|---|---|---|---|
|
Argentina |
X |
|||
|
Australia |
X |
X |
||
|
Austria |
X |
X |
||
|
Belgium |
X |
X |
||
|
Brazil |
X |
X |
||
|
Bulgaria |
X |
|||
|
Canada |
X |
X |
||
|
Chile |
X |
|||
|
China |
X |
X |
||
|
Colombia |
X |
|||
|
Costa Rica |
X |
|||
|
Croatia |
X |
|||
|
Cyprus |
X |
|||
|
Czech Republic |
X |
X |
||
|
Denmark |
X |
X |
||
|
Estonia |
X |
X |
||
|
Finland |
X |
X |
||
|
France |
X |
X |
X |
|
|
Germany |
X |
X |
X |
|
|
Greece |
X |
X |
||
|
Hungary |
X |
X |
||
|
Iceland |
X |
|||
|
India |
X |
X |
||
|
Indonesia |
X |
X |
||
|
Ireland |
X |
X |
||
|
Israel |
X |
|||
|
Italy |
X |
X |
X |
|
|
Japan |
X |
X |
||
|
Korea |
X |
X |
||
|
Latvia |
X |
X |
||
|
Lithuania |
X |
X |
||
|
Luxembourg |
X |
X |
||
|
Malta |
X |
|||
|
Mexico |
X |
X |
||
|
Netherlands |
X |
X |
||
|
New Zealand |
X |
|||
|
Norway |
X |
|||
|
Peru |
X |
|||
|
Poland |
X |
X |
||
|
Portugal |
X |
X |
||
|
Romania |
X |
|||
|
Russian Federation |
X |
|||
|
Saudi Arabia |
X |
|||
|
Slovakia |
X |
X |
||
|
Slovenia |
X |
X |
||
|
South Africa |
X |
X |
||
|
Spain |
X |
X |
||
|
Sweden |
X |
X |
||
|
Switzerland |
X |
|||
|
Turkey |
X |
X |
||
|
United Kingdom |
X |
X |
X |
|
|
United States |
X |
X |
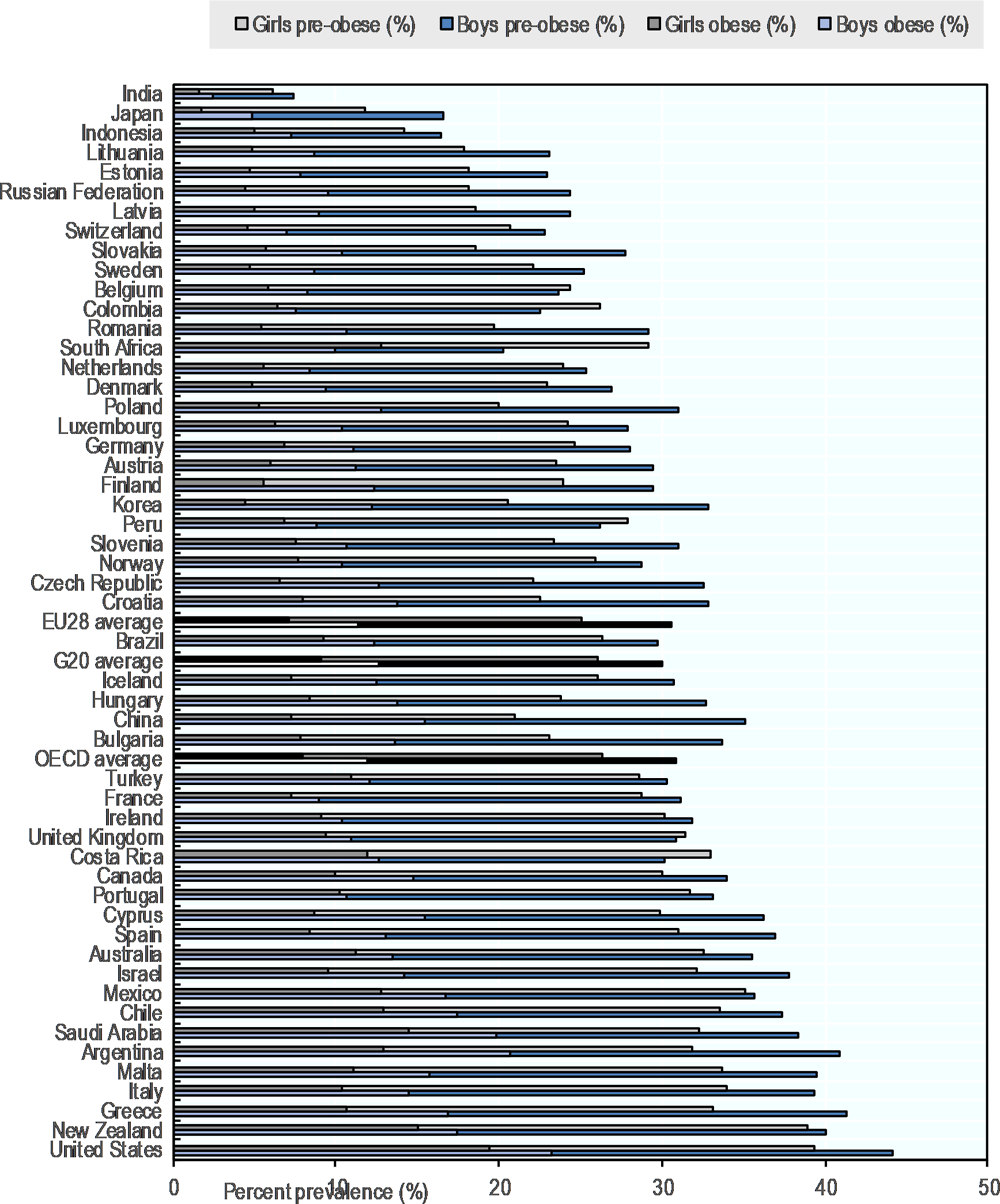
Note: Children between 5‑19 years of age. Data is age-standardised.
Source OECD analyses on WHO Global Health Observatory (2018[18]) data, “Prevalence of obesity among children and adolescents”, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adolescents/en/.
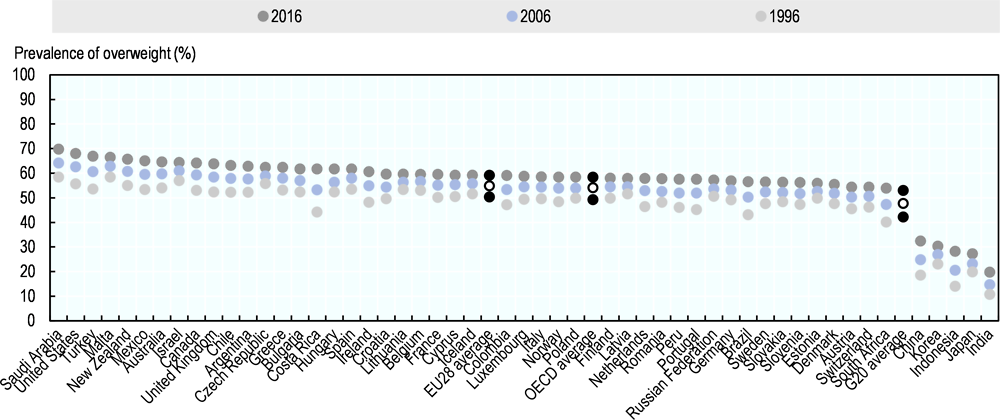
Note: Data is age-standardised. Additional information on the comparability of this data with data in OECD.Stat can be found in Box 2.2.
Source: OECD analyses on WHO Global Health Observatory (2018[16]) data, “Mean body mass index (BMI) trends among adults”, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/bmi_trends_adults/en/.
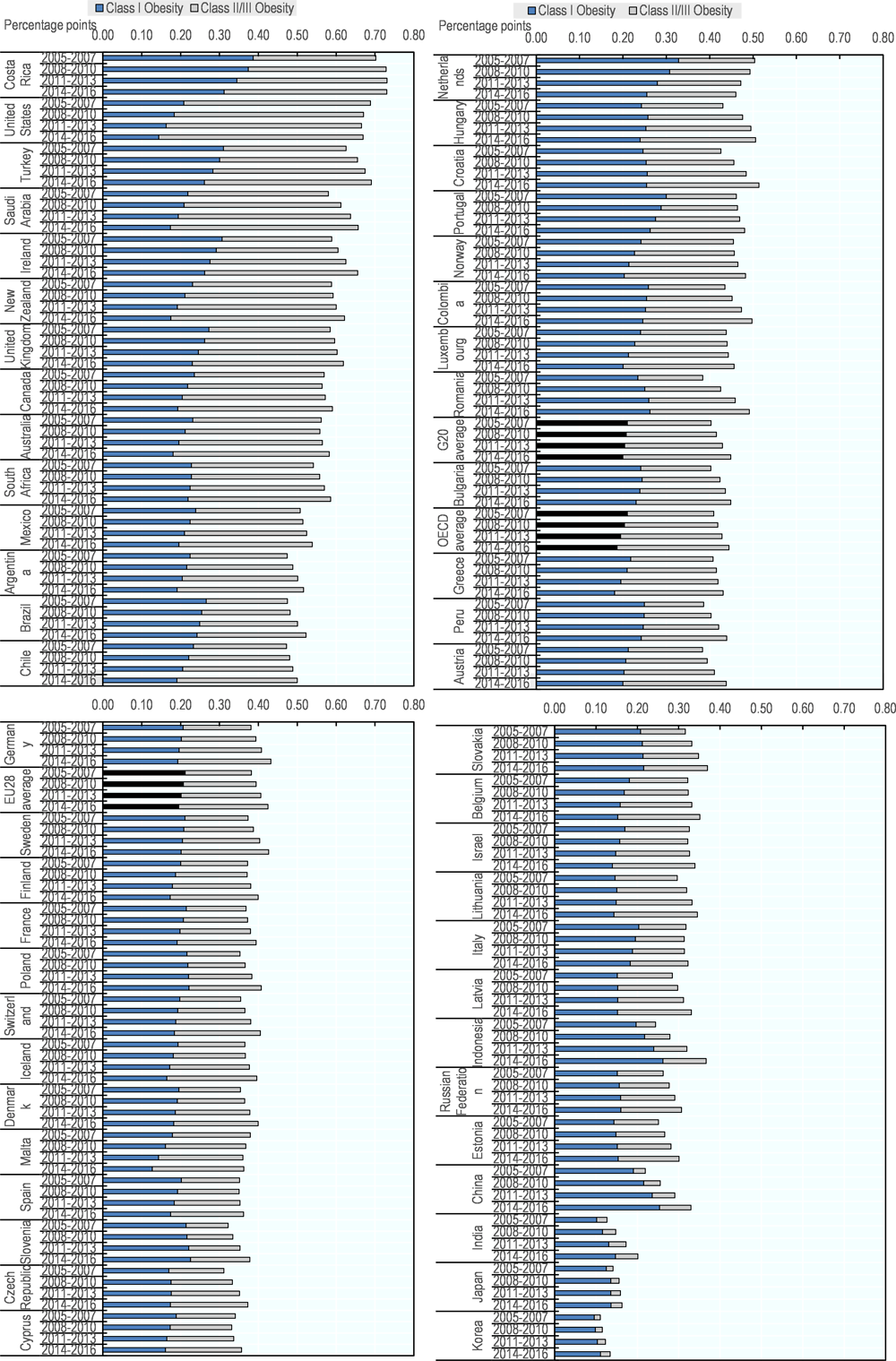
Note: Data is age-standardised. Additional information on the comparability of this data with data in OECD.Stat can be found in Box 2.2.
Source: OECD analyses on the NCD-RisC (2017[17]) data, “Adult body mass index: Evolution of BMI over time”, http://ncdrisc.org/data-downloads-adiposity.html.