The overuse, underuse or misuse of prescription medicines causes significant hazards to health and leads to wasteful care. These risks apply notably to the misuse of antibiotics, opioids and benzodiazepines in primary care.
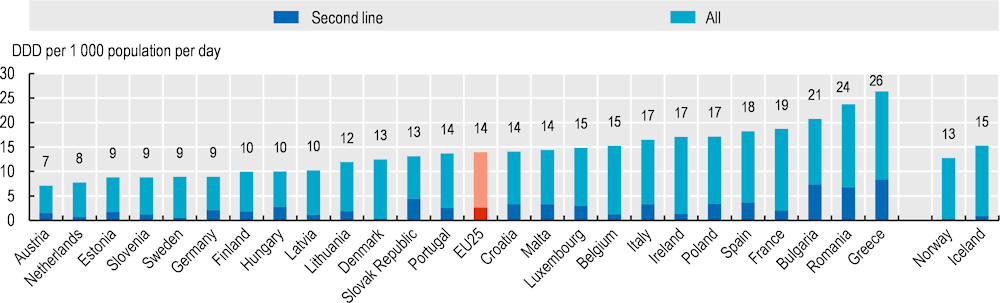
Antibiotics should be prescribed only where there is a need that is clearly supported by evidence, to reduce the risk of resistant strains of bacteria. For example, quinolones and cephalosporins are considered second-line antibiotics in most prescribing guidelines, and should be used only when first-line antibiotics are ineffective. Total volume of antibiotics and second-line antibiotics (as a proportion of total volume) have been validated as markers of quality, given the rising public health concern caused by antimicrobial resistance (AMR) across OECD countries (OECD, 2018[1]).
Total volume of antibiotics prescribed in primary care varied almost four‑fold across EU countries in 2020, with Austria and the Netherlands reporting the lowest volumes, and Greece, Romania and Bulgaria reporting the highest. Volumes of second-line antibiotics vary almost 25‑fold across countries: the Nordic countries except Finland reported the lowest volumes, whereas Greece and Bulgaria reported the highest (Figure 6.26). Cross-country variation in the use of antibiotics is likely to be explained by differences in prevalence of AMR, guidelines and incentives that govern primary care prescribers, and attitudes towards optimal treatment of infectious illness.
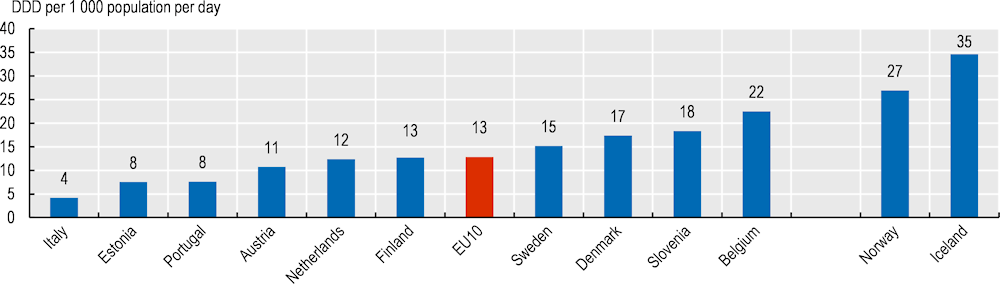
Opioids are often used to treat strong acute pain like pain associated with cancer. Over the last decade, they have been increasingly used to treat chronic pain, despite the risk of dependence, dose increase, shortness of breath and death (OECD, 2019[2]).
Across EU countries, the average volume of opioids prescribed in primary care in 2019 was 13 defined daily doses (DDDs) per 1 000 population per day. Iceland and Norway reported more than twice the EU average; Italy reported the lowest volumes (Figure 6.27). The wide variation can be partly explained by varying clinical practice and prescribing in pain management, regulation, and trends in substance abuse.
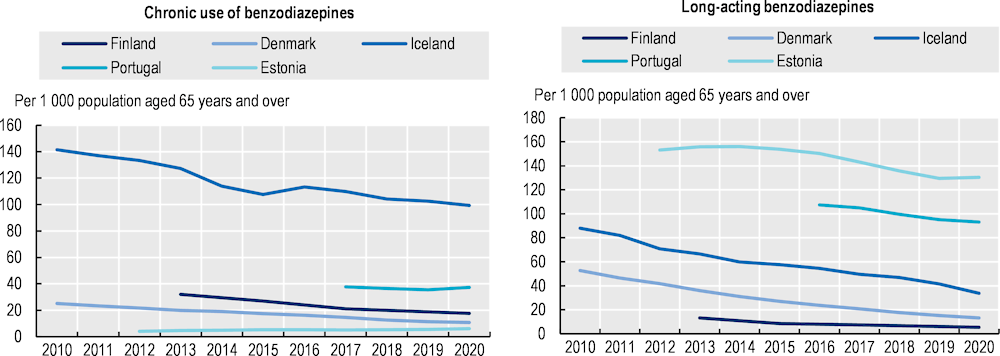
Most guidelines advise complete avoidance of benzodiazepines for older adults given the risk of dizziness, confusion and falls. Long-term use of benzodiazepines can lead to adverse events (overdoses), tolerance, dependence and dose escalation. Long-acting (as opposed to short-acting) benzodiazepines are also discouraged given a longer effect for the body to eliminate (OECD, 2017[3]).
Over the past decade, the use of benzodiazepines, both long-term and long-acting, decreased across EU countries (Figure 6.28). Large declines in long-term use have occurred in Iceland while Denmark and Iceland experienced a large decline in the use of long-acting benzodiazepines. Still, striking variations persist across countries. Long-term use of benzodiazepines in Iceland is 16‑fold higher than that in Estonia. Conversely, the use of long-acting benzodiazepines in Estonia is highest in the EU and 23‑fold higher than that in Finland. The wide variation is partly explained by reimbursement and prescribing policies for benzodiazepines, as well as differences in disease prevalence.