Olusoji Adeyi
Resilient Health Systems

Olusoji Adeyi
Resilient Health Systems
Development assistance for health has contributed to impressive health gains over the years but has also perpetuated fragile health systems and dysfunctional institutions in developing countries. The architecture and incentives of development assistance for health have led many countries to underfund basic health services in their own budgets and become overly aid‑dependent. Aid dependency can diminish country ownership over health policy priorities and service delivery. The COVID-19 pandemic has shown the perils of overdependence on external sources of finance and distant suppliers for critical health needs. Shifting aid to financing regional and global public goods rather than basic health budgets would generate greater added value, increase the accountability and ownership of health expenditures, and rebalance the power relationship between the Global South and Global North for the benefit of all.
Since 2000, development assistance for health has accounted for a growing share of overall expenditure on health in low-income and lower middle-income countries. In the same period, government’s share of expenditure on health in low-income countries fell.
To achieve global health goals, development assistance for health should be transformed so that developing countries pay for basic health services from their own resources and development co‑operation partners focus on boosting investment in regional and global public goods.
The ambitions of the global health agenda supported by development assistance for health (DAH) are lofty, including universal health coverage by 2030, achieving global health security and building human capital. At first glance, these seem rational considering recent progress. For example, several dimensions of aggregate health outcomes have improved since 1990, albeit with variations across and within regions and countries. There has been striking progress in reducing child mortality, with rapid declines and narrower gaps between high-income countries (HICs), low-income countries (LICs) and lower middle-income countries (LMICs) (Figure 6.1). To the extent that DAH partly financed technologies that contributed to this progress, it must be seen as a net positive, with results that should make both financiers and recipients proud.
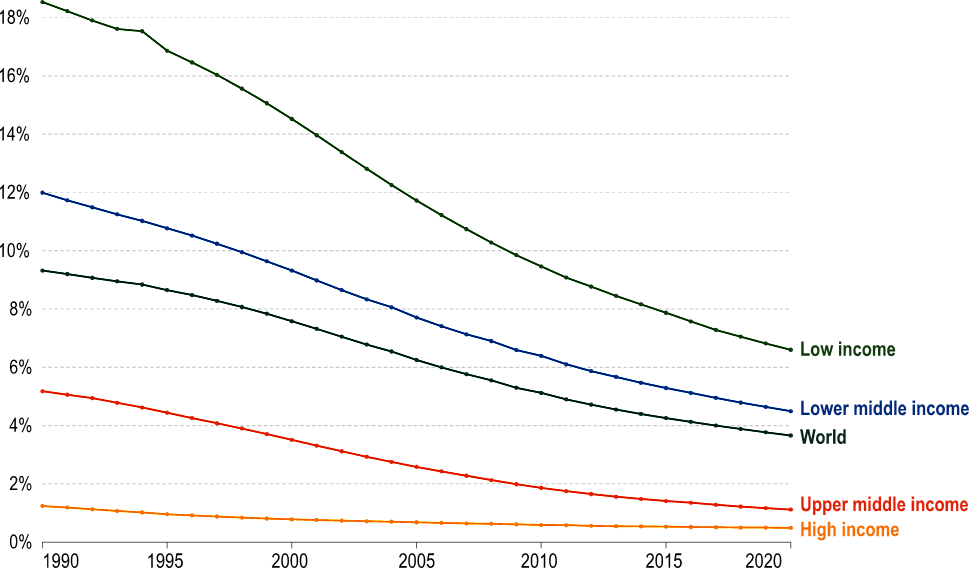
Note: The child mortality rate measures the share of children who die before reaching the age of five.
Source: Ortiz-Ospina (2022[1]). Global Health, https://ourworldindata.org/health-meta.
The broader global health landscape, however, gives cause for concern: severe weaknesses in health systems; dysfunctions in multilateral and bilateral forums (Krishnan, 2022[2]); and inequities in access to life‑saving diagnostics, vaccines and therapeutics. These overlapping challenges converged during the COVID-19 pandemic (Adeyi, 2022[3]; Nature, 2021[4]; Independent Panel for Pandemic Preparedness and Response, 2021[5]), which also highlighted how dependent many LICs remain on development co-operation to fund basic health services and commodities. The current approach to development finance for health in developing countries is in part responsible. The persistent dependency on development assistance for health, and countries’ tendency to use it as a substitute for health commitments in their own budgets, point to the need for donors and recipient countries to adopt new relationships around health financing.
This is not a call to reduce or end this assistance but to repurpose it in ways that build developing countries’ self‑sufficiency and local accountability while boosting investment in global and regional public goods. This approach would mean that developing countries pay for basic health services from their own resources and according to their own priorities; that strategic decisions for the Global South are made by the Global South at regional or country level; that recipient countries are not bound to using aid dollars to purchase goods and services from donor country suppliers; and that the Global South develops its own network of institutions and expertise for health security, resilient health systems and locally sustainable financing. This transformation would also help achieve the global health goals of the 2030 Agenda for Sustainable Development.
There is evidence that development assistance for health partially substitutes for domestic budgets that would have been allocated to health (Dieleman and Hanlon, 2013[6]; Farag et al., 2009[7]). Aid exceeds government health spending in many LICs. In 2019, external aid to developing countries for health rose to USD 17 billion (WHO, 2021[8]) and nearly three‑quarters of health spending in LICs was financed by a combination of external aid and inherently regressive out-of-pocket spending. From 2000 to 2019, the share of external aid in total health spending rose from 16% to 29% while the share accounted for by government transfers declined from 28% to 21% (Figure 6.2) (WHO, 2021[8]).
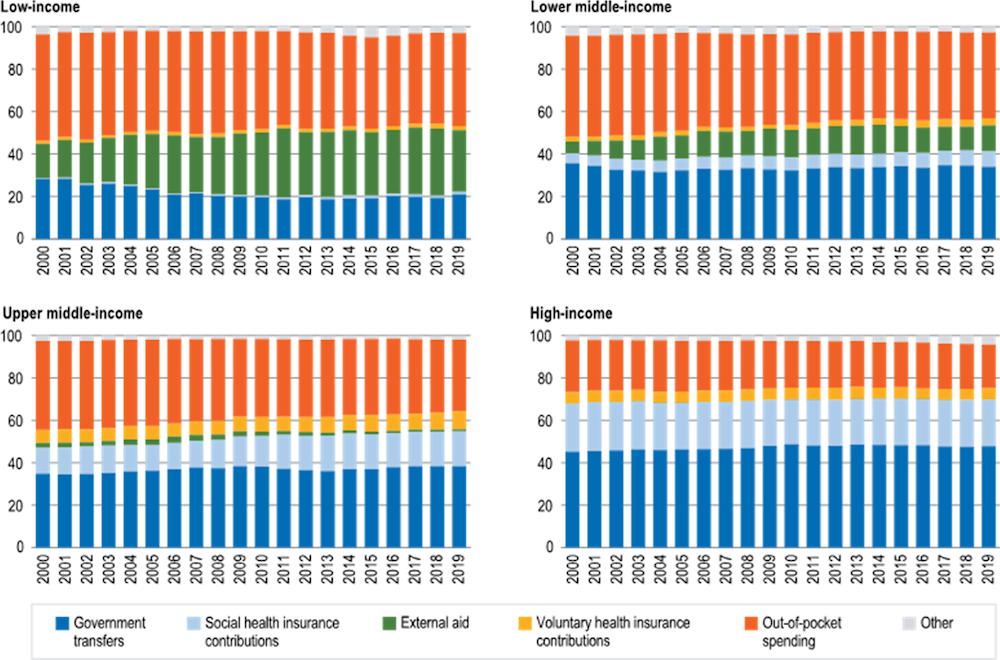
Notes: Other sources are compulsory prepayments to private insurance, domestic non-governmental organisation contributions and health services operated by enterprises for their employees. The Netherlands and Switzerland organise health financing mainly through compulsory insurance but with funding based on mandatory fixed premiums or a combination of payroll tax and fixed premiums. For these countries, all mandatory contributions are included in estimates of social health insurance contributions.
Source: WHO (2021[8]). Global Expenditure on Health: Public Spending on the Rise?, https://apps.who.int/iris/handle/10665/350560.
Sub-Saharan Africa is especially dependent on development assistance for health compared to other regions. For 2019, external health expenditure1 was 22.3% of current health expenditures in the World Health Organization (WHO) Africa region, far surpassing the external health expenditure of 0.5% in Europe, 1.9% in the Americas, 3.2% in the eastern Mediterranean, 6.9% in Southeast Asia and 14.4% in the Western Pacific region (WHO, 2021[9]). Assistance for malaria control and elimination is an instructive example. Of the USD 3.3 billion invested globally in 2020, international financiers provided more than USD 2.2 billion, of which more than three-quarters (79%) went to the WHO Africa region. That this is the situation two decades after the Abuja Declaration, in which African leaders pledged to allocate more of their own budgets to health (Organisation of African Unity, 2001[10]), illustrates the dysfunctions and perverse incentives of development assistance for health; it undermines domestic government accountability for health.
Debt servicing constrains the fiscal space for government health expenditures, but a range of other factors impacts on governments’ ability or willingness to spend more. Uncritical advocacy for debt relief, especially by non‑governmental organisations from the Global North (Oxfam, 2022[11]), perpetuates a charity-based narrative that ignores the intricacies of the international financial system and wrongly casts Global South governments as passive victims that lack agency to allocate more of their own resources to health (Adeyi, 2021[12]). Many countries that benefited from debt relief under the Heavily Indebted Poor Countries, or HIPC, Initiative (IMF, 2021[13]) or agreements with the Paris Club (2022[14]) have since accumulated high levels of debt and continued to be dependent on development assistance for health. While HICs have greater fiscal capacity and spend more on health per capita in general, there are large variations in health spending within each income group and prioritising health is largely a choice at each income level (WHO, 2021[8]).
The combination of DAH dependency and expectations of debt relief constitutes a moral hazard in that it encourages fiscal profligacy in LICs and LMICs and thus reinforces the power imbalances between the Global North and Global South. Multiple factors beyond debt burdens constrain government health spending in the Global South, among them the low tax-to-gross domestic product ratio in many countries that do a poor job of collecting domestic revenues; corruption, which diverts tax revenues from public investments and safety nets; allocative inefficiencies in the health sector; and weak public financial management.
Realign incentives in favour of more domestic resource mobilisation relative to gross national income, more government expenditure on health, efficient purchasing of health services within domestic resources and probity in public financial management.
More attention needs to be paid to factors such as these, and debt relief should be explicitly conditioned on a government stipulation to assume financing of basic health services and commodities by 2030. This would realign incentives in favour of more domestic resource mobilisation relative to gross national income, more government expenditure on health, efficient purchasing of health services within domestic resources and probity in public financial management.
Donors and recipient countries can do much better in terms of meeting their commitments to local ownership and enabling LICs and LMICs to rely more on their own resources to fund basic health services and commodities. Despite the pledges in the 2005 Paris Declaration on Aid Effectiveness and the related 2008 Accra Agenda for Action (OECD, 2008[15]), certain bilateral financiers perform poorly on the Quality of Official Development Assistance, a tool that measures and compares financiers on indicators most relevant to development effectiveness and quality (Mitchell, Calleja and Hughes, 2021[16]). In the specific matter of DAH, little has changed in the key asymmetries that have long undermined country ownership (Noor, 2022[17]). The development community continues to emphasise globally determined, aspirational ideals whose achievement requires large amounts of assistance for indefinite periods and to rely on global financing entities that purport to solve local problems. An example is the recent call by the Lancet Commission on lessons for the future from the COVID-19 pandemic for a new and bigger “Global Health Fund” to be headquartered in Geneva (Sachs et al., 2022[18]). The call is a distraction from the real issues. Not only would the envisioned new fund duplicate the functions of existing regional and global development banks, it would also risk perpetuating the damaging worldview that the destiny of health in LICs and LMICs must depend on decisions taken in Geneva by financiers from the Global North that are not accountable to those countries’ citizens.
Achieving global health ambitions requires forthright recognition and correction of the dependencies that development assistance for health creates and the ways in which it disincentivises country ownership and domestic accountability. This will not be easy due to the escalation of commitment bias, the legacy of power and institutional dynamics in global health, and the “reductive tendency”, as defined by Gras et al. (2020[19]), in DAH. The colonial origins of these dynamics (Packard, 2016[20]; Adeyi, 2022[3]) have contributed to today’s power imbalance in global health and DAH, whereby the terms of engagement are mediated through global institutions and financiers and decisions reflect their preferences rather than input from developing countries.
For politicians in donor countries, it is relatively easy to make the case for aid budgets to their taxpayers by focusing on the virtues of saving the lives of children and mothers in poorer countries, especially when such DAH is tied to goods and services sold by firms in donor countries. It is more difficult for them to make the case for financing the development of sustainable, accountable institutions in the Global South. The result is that donors continue financing what they rationally should not. There is a better approach to make development assistance for health work for donors and recipients.
While the challenges are daunting, there is a compelling case for transformative changes in development assistance for health. The solution lies in a deliberate transition from the current system to one that is fit for the 21st century. The purpose, architecture, incentives and power dynamics of DAH should evolve along four dimensions.
Assistance should shift to addressing global and regional threats to health and where it has the greatest potential added value. Based on recent estimates for country-specific functions, this shift would mean repurposing up to 76% of current development assistance for health (Schäferhoff et al., 2019[21]). Ending DAH for basic health and inputs – including items such as those on the WHO List of Essential Medicines and Diagnostics as well as maternal health services, childhood vaccines, insecticide-treated bed nets for malaria and routine supply chain management – is an essential part of the transition. These inputs and services are elemental, necessary, cost-effective and routine, and the need for them is generally predictable. Financing these should thus be the primary responsibility of each individual country and not dependent on charity from outside.
The central focus of health-related development assistance should instead be on areas such as pandemic preparedness and disease outbreak detection and control systems; publicly funded research and development whose results are not constrained by the current regime of intellectual property rights at the World Trade Organization (Nature, 2021[4]); and institutions such as centres for disease control, institutes of public health, pharmaceutical regulation agencies, centres for health technology assessment, and referral laboratories. Financing of the Africa Centres for Disease Control and Prevention (by various parties including the World Bank, the Bill & Melinda Gates Foundation, and the Mastercard Foundation) is one example of such a high value-adding investment. Another is the investment by the International Finance Corporation (2022[22]) in Avacare Global to enable the company to expand its manufacturing and distribution of pharmaceutical and healthcare consumable products, including generic drugs, in Africa. A third example is the programme to improve preparedness capacities for public health emergencies in the Organisation of Eastern Caribbean States region.
This transition should be phased rather than abrupt and exclude extreme situations such as war and humanitarian disasters. The target deadline could be 2030 to align with the 2030 Agenda, which calls for universal health coverage by 2030 “including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all” (United Nations, 2015[23]).
This transition should be phased rather than abrupt and exclude extreme situations such as war and humanitarian disasters.
During the transition, bilateral financiers from HICs that currently procure and distribute medicines and equipment in LICs and LMICs should repurpose those funds to factory-gate subsidies, whereby the donor pays most of the commodity price to the manufacturer. The donor then steps back while the LICs and LMICs take responsibility for procuring those heavily subsidised products via their own public and private sector enterprises. The price reductions arising from the subsidy would increase the purchasing power of country budgets and shift the locus of accountability and control from foreign capitals of the Global North to governments in the Global South. This approach has been shown to work on a large scale (Tougher et al., 2012[24]).
Leaders of LICs and LMICs should lead and take ownership as the principal decision makers about their countries’ health policies and programmes. National medium-term expenditure frameworks – not the preferences of international financiers, foundations and bilateral aid agencies – would then drive country budgets. This would help make leaders of LICs and LMICs accountable and responsible for the consequences of their actions and inactions. The premise of this shift is that economic development, including health, cannot happen without some variety of compact between the government and the governed and the recognition that it is impossible to develop someone else’s country from the outside (Deaton, 2013, pp. 267-325[25]).
Shifting the locus of accountability to LIC and LMIC capitals means abandoning the cycles of lofty global declarations based on implicit but unrealistic promises and expectations of unlimited DAH for indefinite durations. Rather than utopian goals, countries would adopt challenging but more sensible goals and do the hard work to improve and finance basic health services using domestic resources. Crucially, it also means transitioning to a future in which politicians and policy makers in LICs and LMICs bear the electoral and social consequences if they do not make demonstrably serious efforts to improve health and health systems in their own countries.
Under this approach, global and regional entities such as WHO, the World Bank, regional development banks and regional centres for disease control could publish league tables of effort and achievement. There would be no need for any new entity at the global level, but existing multilateral institutions would reorient themselves to better serve countries and regions and enable the proposed transition. Country-level compacts would thrive without the distraction and fanfare of unrealistic goals set at the global level, putting an end to expectations that DAH must underpin the solution to every major problem in health, as illustrated by the Health4Life Fund, which remains unfunded (Ravelo, 2022[26]).
Development assistance for health should no longer be tied to services and products from the donor country, and bilateral donors should no longer dictate which contractors from their countries should provide technical assistance to recipient countries. Tied DAH, which features asymmetry of information between financiers and beneficiaries, is subject to capture by entrenched contractors in the donor countries – what Norris (2012[27]) has termed a “development-industrial complex” – and fosters situations in which financiers repeatedly foist upon recipient countries forms of technical assistance that are irrelevant or harmful. A different approach is to put funds for technical assistance in time-bound drawdown facilities. Recipient countries would then take charge of the selection criteria and procurement of technical assistance, with the processes and results based on explicit criteria that are published in the public domain for transparency. This novel proposition is likely to generate opposition from long‑entrenched providers of aid-financed technical assistance that would lose power and future contracts, including some contractors, universities and think tanks in the Global North. However, summoning the courage to manage these and related headwinds is necessary for the transition to succeed.
The countries and subregions of the Global South should invest in developing their own knowledge-based networks and combine these with increased self-financing. These networks would include institutions; industries (in partnerships with the private sector); deep expertise in science, technology and biomedicine; and supply chains for increased self-sufficiency in essential medical supplies. The COVID-19 pandemic has shown all countries, particularly LICs and LMICs, the perils of being overly dependent on external financiers and distant suppliers for mission-critical technologies.
The proposed transition offers a clear and specific path from the present to a much better future. It would position the LICs and LMICs, rather than the HICs and financing institutions, as the principals in planning, financing and addressing their own health challenges. The transition will not be easy: It requires letting go of the status quo, which is familiar and comfortable but dysfunctional. The new approach would set the world on a path to more durable progress in global health and eliminate dependency in the relationship between the Global North and the Global South. A brighter future is possible if all rise to the challenge.
[3] Adeyi, O. (2022), Global Health in Practice: Investing Amidst Pandemics, Denial of Evidence, and Neo-dependency, World Scientific Publishing, Singapore, https://doi.org/10.1142/12520.
[12] Adeyi, O. (2021), “Opinion: Global health, narcissistic charity, and neo-dependency”, Development Today, https://www.development-today.com/archive/dt-2021/dt-9--2021/global-health-narcissistic-charity-and-neo-dependency (accessed on 28 October 2022).
[25] Deaton, A. (2013), The Great Escape: Health, Wealth, and the Origins of Inequality, Princeton University Press, Princeton, NJ.
[6] Dieleman, J. and M. Hanlon (2013), “Measuring the displacement and replacement of government health expenditure”, Health Economics, Vol. 23/2, pp. 129-140, https://doi.org/10.1002/hec.3016.
[7] Farag, M. et al. (2009), “Does funding from donors displace government spending for health in developing countries?”, Health Affairs, Vol. 28/4, pp. 1045-1055, https://doi.org/10.1377/hlthaff.28.4.1045.
[19] Gras, D. et al. (2020), “Wicked problems, reductive tendency, and the formation of (non-)opportunity beliefs”, Journal of Business Venturing, Vol. 35/3, p. 105966, https://doi.org/10.1016/j.jbusvent.2019.105966.
[13] IMF (2021), “Factsheet – Debt relief under the Heavily Indebted Poor Countries (HIPC) Initiative”, International Monetary Fund, Washington, DC, https://www.imf.org/en/About/Factsheets/Sheets/2016/08/01/16/11/Debt-Relief-Under-the-Heavily-Indebted-Poor-Countries-Initiative (accessed on 28 October 2022).
[5] Independent Panel for Pandemic Preparedness and Response (2021), COVID-19: Make it the Last Pandemic, Independent Panel for Pandemic Preparedness and Response, https://theindependentpanel.org/wp-content/uploads/2021/05/COVID-19-Make-it-the-Last-Pandemic_final.pdf.
[22] International Finance Corporation (2022), “IFC and Avacare Partner to increase access to medicines and healthcare goods in Africa”, press release, https://pressroom.ifc.org/all/pages/PressDetail.aspx?ID=27029 (accessed on 28 October 2022).
[2] Krishnan, V. (2022), “The power imbalance undermining global health”, Atlantic, https://www.theatlantic.com/international/archive/2022/07/covid-trips-agreement-vaccines-global-health/670551.
[16] Mitchell, I., R. Calleja and S. Hughes (2021), The Quality of Official Development Assistance, Center for Global Development, Washington, DC, https://www.cgdev.org/publication/quality-official-development-assistance (accessed on 28 October 2022).
[4] Nature (2021), “Editorial: A patent waiver on COVID vaccines is right and fair”, Nature, Vol. 593/7860, p. 478, https://doi.org/10.1038/d41586-021-01242-1.
[17] Noor, A. (2022), “Country ownership in global health”, PLOS Global Public Health, Vol. 2/2, p. e0000113, https://doi.org/10.1371/journal.pgph.0000113.
[27] Norris, J. (2012), “Hired gun fight”, Foreign Policy, https://foreignpolicy.com/2012/07/18/hired-gun-fight (accessed on 28 October 2022).
[15] OECD (2008), Paris Declaration and Accra Agenda for Action, OECD, Paris, https://www.oecd.org/dac/effectiveness/parisdeclarationandaccraagendaforaction.htm (accessed on 17 August 2022).
[10] Organisation of African Unity (2001), Abuja Declaration on HIV/AIDS, Tuberculosis and Other Related Infectious Diseases, Organisation of African Unity, Abuja, https://au.int/sites/default/files/pages/32894-file-2001-abuja-declaration.pdf.
[1] Ortiz-Ospina, E. (2022), “Global health”, Our World in Data, https://ourworldindata.org/health-meta (accessed on 28 October 2022).
[11] Oxfam (2022), “New index shows governments worldwide stoked an inequality explosion during COVID-19 pandemic”, press release, Oxfam International, https://www.oxfam.org/en/press-releases/new-index-shows-governments-worldwide-stoked-inequality-explosion-during-covid-19 (accessed on 20 October 2022).
[20] Packard, R. (2016), A History of Global Health: Interventions into the Lives of Other Peoples, Johns Hopkins University Press, Baltimore, MD.
[14] Paris Club (2022), “Agreements concluded with Paris Club”, web page, https://clubdeparis.org/en/traitements (accessed on 28 October 2022).
[26] Ravelo, J. (2022), “NCDs are top global killer but trust fund coffers are empty”, Devex, https://www.devex.com/news/ncds-are-top-global-killer-but-trust-fund-coffers-are-empty-104021 (accessed on 28 October 2022).
[18] Sachs, J. et al. (2022), “The Lancet Commission on lessons for the future from the COVID-19 pandemic”, The Lancet, Vol. 400/10359, pp. 1224-1280, https://doi.org/10.1016/S0140-6736(22)01585-9.
[21] Schäferhoff, M. et al. (2019), “International funding for global common goods for health: An analysis using the Creditor Reporting System and G-FINDER databases”, Health Systems & Reform, Vol. 5/4, pp. 350-365, https://doi.org/10.1080/23288604.2019.1663646.
[24] Tougher, S. et al. (2012), “Effect of the Affordable Medicines Facility-malaria (AMFm) on the availability, price, and market share of quality-assured artemisinin-based combination therapies in seven countries: A before-and-after analysis of outlet survey data”, The Lancet, Vol. 380/9857, pp. 1916-1926, https://doi.org/10.1016/s0140-6736(12)61732-2.
[23] United Nations (2015), “Background – Universal Health Coverage Day”, web page, https://www.un.org/en/observances/universal-health-coverage-day/background (accessed on 28 October 2022).
[9] WHO (2021), “External health expenditure (EXT) as percentage of current health expenditure (CHE) (%)”, The Global Health Observatory, World Health Organization, Geneva, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/external-health-expenditure-(ext)-as-percentage-of-current-health-expenditure-(che)-(-) (accessed on 28 October 2022).
[8] WHO (2021), Global Expenditure on Health: Public Spending on the Rise?, World Health Organization, Geneva, https://apps.who.int/iris/handle/10665/350560 (accessed on 28 October 2022).
← 1. WHO defines external health expenditure as the external sources spent on health as a percentage of total current health expenditures.