This annex contains information presented at the 3rd working group workshop in January 2022 and included in the background meeting document for the 4th and 5th workshops held in April 2022. It provides a summary health data infrastructure, data availability, and information and data flows between the Czech health data stakeholders, which are relevant for the HSPA development.
Health System Performance Assessment Framework for the Czech Republic

Annex E. Overview of the Czech health data custodians and data sources
Policy and health data governance
There are various institutions that feel a level of ownership of some health data and databases. Often, institutions use the very same primary data to feed various datasets (i.e. data are clustered or presented from different perspectives, but composed of the same primary data). Generally, there are four main sources of data used within the Czech healthcare system: the healthcare providers’ claim data, the healthcare providers’ periodical reports (including performance, workforce, and clinical reporting), the health insurers’ performance data, and population surveys. These are (but not always) linked to the basic population registry information, such as the deaths and the births; often, the linkage is performed on an ad hoc basis for a specific purpose, including on demand for a specific indicator for an international data reporting. The fifth source of data is the dataset of the State Institute for Drug Control (SUKL); though most (but not all) of their information is included also in the claim data of the health insurance funds; the structured dataset of the SUKL has not been used for policy setting or policy decision making so far.
The main responsible body for health data processing for policy-making purposes is the Institute of Health Information and Statistics (UZIS). While there is a rich information in the data it is in its custody, most of it is not publicly available, and it is available to the Ministry of Health only upon a request. Apart from the COVID‑19 related statistics, the Czech Republic is not sharing de‑identified health datasets for monitoring and research and has not research data centre or remote data access service (OECD, 2022[21]).
Using information from processed datasets in policy- and decision-making is limited. Often, health data stream does not reach institutions responsible for policy making and/or institutions mandated with decision-making. This is partly due to no back-looping of processed data and/or resulting information-rich indicators has been incorporated in the Czech health data landscape. Ministry of Health does not make any use of, or does not have access to, resulting processed claim data, clinical registry data, and prescription data.
The Health 2030 National Strategy has been the first strategic document supported by an extensive analytical study, produced by the UZIS (see UZIS (2020[12])). Previously, data sharing between the UZIS and MoH has been reported as slow and cumbersome. A change in this approach is signalled by the legislation passed in August 2021 amending the Act on Health Services. This legislation introduced the so-called Resort Reference Statistics (RRS) and mandated the Ministry of Health to define these statistics, or indicators, in an accompanying legislation act. This by-law has not yet been produced and it has been discussed throughout the HSPA project how to link their definition and development to the HSPA framework development. As part of the HSPA project discussions, an agreement has been reached between the MoH and UZIS that HSPA indicators in the custody of UZIS would be listed among the Resort Reference Statistics, while the list of these statistics would be broader, covering areas and data details also out of the scope of the HSPA (see Section 5).
Health data infrastructure
The currently collected health data in the Czech Republic contains an extensive amount of information and data is routinely being collected through various sources. While claim data show robust data collecting infrastructure, collected clinical information is not always reliable due to missing incentives to report it properly. Outcome data are generally missing, but exceptions exist. However, not all collected information is further processed.
Generally, different datasets within the Czech health data landscape are not being linked automatically, but linkages on an ad hoc basis is usually possible. Such linkages are performed by the Institute of Health Information and Statistics usually for a specific reason or based on a request – for instance for the purposes of international reporting, or, a recent case, to support development of the Strategic Framework for Health Care Development in the Czech Republic to 2030, the “Health 2030” National Strategy, by an analytical study.
The Box A E.1 provides an overview of the Czech health data custodians and the type and content of databases in their custody. The next sections then detail out information on individual institutions’ available data and datasets, available as of December 2021/January 2022.
Box A E.1. Overview of the Czech health data custodians
Health Insurance Funds (HIFs)
administrative (claim) data from healthcare providers for reimbursement purposes, connected to population registry;
health insurance contributions data (including employment status).
Ministry of Health (MoH)
reporting data on HIFs‘ overall, mainly financial, performance (number of members, financial situation, selected healthcare consumption indicators);
survey data from care providers (highly specialised inpatient care data; inpatient quality self-assessment data; costly medical technology aggregate data; some workforce data).
Institute of Health Information and Statistics (ÚZIS)
survey data provided by healthcare providers on their structure and workforce (registry of healthcare professionals and registry of health service providers, economic performance data of hospitals etc.);
clinical registry data reported by healthcare providers on selected diagnoses and hospitalisation (12 national health registries, including 11 clinical, or diagnostically specific, registries + 1 hospitalisation registry);
survey data provided by healthcare providers within the reference providers’ network for the CZ-DRG purposes;
population survey data (EHIS, collected by CZSO);
administrative (claim) data provided by the health insurance funds
data taken from other institutions and survey data (basic population registry, death certificate registry).
Czech Statistical Office (CZSO)
population data (population registry, death registry, other demographics; census data not used in heath policy making so far, but newly small legislative exemption exists);
population survey data (survey management for EHIS);
other survey data (disability, population incapacity to work, student and graduate registry);
System of Health Accounts database (aggregate data submitted by the HIFs, or HIFs via UZIS, and other central and regional government bodies);
Health care workforce remuneration using MoSA survey on wage remuneration and MoF information system on tariffs.
State Institute for Drug Control (SUKL)
datasets from the electronic prescription system;
datasets from the electronic system of reimbursed medical devices and aids (since 2022).
National Public Health Institute (SZÚ)
data from the EHES survey (linked to the EHIS dataset provided by the UZIS);
smoking and tobacco use (NAUTA) survey data;
datasets on antibiotics use (from KZP);
various monitoring (air pollution, water, noise).
Ministry of Finance
the same data as the MoH on HIFs overall (mainly financial) performance.
Health Insurance Bureau (KZP)
data on healthcare consumed abroad and healthcare consumed domestically by other EU nationals (a clearance centre for the Czech SHI system towards other EU countries);
healthcare quality indicators using selected claim data from the HIFs.
Source: OECD background document to the Czech HSPA framework development workshops held in April 2022.
Health insurance funds’ data
The HIFs dispose of a set of claim data from healthcare providers submitted for reimbursement purposes. Generally, all HIFs have the claim data in the same structure, based on the VZP data interface, which is publicly available (www.vzp.cz/poskytovatele/vyuctovani-zdravotni-pece). None of the HIFs has, however, a complete set of the claim data – each health insurance fund has data on health services to be reimbursed only for its members (insurees). This creates some limitations, because the market is fragmented. Currently, there are seven public self-governed health insurance funds, with the VZP having the highest market share of more than 50% of all insured people.
The HIFs have the basic demographic information on each of their members, linked to the State population registry: the permanent address, death information, birth information. On voluntary basis, the members generally provide their HIFs also with the information on their contact address and other contact details. The contact address may better serve the indicative purpose of where a given person is actually living and consuming the health services.
In addition, the HIFs have also information on each member’s socio‑economic status – people are obliged to report to their HIF if they qualify for a defined group of economically inactive population, such as pensioners, students, unemployed, and parents on parental leaves. The health insurance funds have also a complete overview of earnings of the self-employed people and a structured overview of economic situation of employees according to their employers (prior to abolishment of annual contribution ceiling, the HIFs had also an information on high-income individual employees). However, the HIFs generally do not link the economic status information to the claim data, because entitlement to benefits is not conditioned upon paid contributions. It would require further consultations with HIFs’ representatives on the possibility to link healthcare consumption data to individual economic status.
Each insured person has a unique personal identifier, the same ID number is used in population registry and is used in healthcare reimbursement claims as well.
Pharmaceuticals – HIFs have information, linked to their individual members, only on prescribed drugs that have been collected and have a non-zero reimbursement. They obtain the data from pharmacies (generally on a monthly basis), but can also download data from the ePrescription system of the SUKL (an instant online system). HIFs do not have access to all ePrescription data; they can view and download only data fulfilling the above‑stated conditions. This possesses a slightly smaller information than is included in the full dataset of the electronic prescription (ePrescription) system at the SUKL, which contains information on all prescribed drugs, also those with zero reimbursement and those that have not been collected (with clear indication of those that have not been collected). Pharmaceuticals consumed during inpatient stays are not reported in any of the systems (see below).
Medical devices and aids (MDA) – information on prescribed MDA is received by a HIF only when a patient collects it and the provider claims the reimbursement, generally a month later. Data are often nonreliable until spring of the next year, till when providers are free to report and claim any additions to the preceding year – the late reporting of some of the reimbursed care and services is especially common with hospitals. Better overview of prescribed MDA might be later available from the electronic MDA prescription record of the SUKL, which is in practice since 3/2022, but on voluntary basis only.
Only information that is valued in reimbursement, is reliable in the claim data.1 Generally, for any health service, a HIF has an information on patient identification, date of provision, provider identification, and place of provision. Reported diagnosis is highly unreliable, unless it is valued in the reimbursement itself (for instance, the services provided to patients diagnosed with COVID‑19 have higher reimbursement rate than for patients without this diagnosis, thus information on COVID‑19 diagnosis is reliable; otherwise, the primary and secondary diagnosis information is meaningless, because reporting methodology is missing, and physicians may also choose not to report any).
For general practitioners for children and adolescents, not all visits (physician contacts) are reported, because most services are paid by capitation. Only provision of FFS-reimbursed services can be obtained from the claim data. These include prevention, vaccination, blood collection.
For general practitioners for adults, same FFS-reimbursed services as for GPs for children are captured in the claim data. In addition, starting 2020, data on GPs for adults visits/physician contacts are reliable from the HIFs’ claim data. FFS per physician contact has been somehow captured in the reimbursement following the abolishment of user fees, but with an annual cap, leading the GPs to stop claiming (i.e. reporting) visits above the reimbursement limit each year (for instance, a GP did not report any patient visit code after September in a given year). Time series on GP visits from the claim data prior to 2020 are thus inapplicable. Still, following the 2020, obtaining the number of GP visits from claim data will be more reliable than the current time series developed by the UZIS from the healthcare providers’ regular reporting.2 Besides, the claim data allows for deeper analysis of patients’ behaviour also on regional level and taking into account other socio-demographic factors. Still, HIFs have no further information on reported GP visits other than when it occurred – the reported diagnosis is unreliable (see above).
For outpatient specialists, HIFs have information on “almost everything”: apart from patient identification and date of care provision, services are reported using the List of Services (Seznam zdravotních výkonů), an MoH directive with some 4 000 detailed services; rarely, there may be 2 different services under one code, such as the magnetic resonance of an arm and of a leg. Provider information is detailed down to the specific physician office (this information is treated differently by each HIF, because it has no reimbursement consequences, so providers are not motivated to update the information on provision place and their physicians regularly; thus, it depends on each HIF how prudent it is in enforcing a regular update, see also below).
The FFS reimbursement applies also to gynaecologic care and care during the pregnancy; since 2020 the later has changed to capitation payments per trimesters, but some services still must be reported in detail to obtain the capitation payment.
Dental care is reimbursed differently, still preventive care can be explored from the claim data for those stomatologists that have contracts with the HIFs (not all stomatologist do – some are relying only on direct payments from their patients or have contracts only with selected HIFs. In such cases, patients do not get reimbursed from their HIF for prevention and dental treatments). Capitation payment for preventive dental services is under discussion – such change would prevent obtaining the dental prevention information from the claim data.
Acute care hospitals report all services according to the List of Services, though their reimbursement is structured differently (see below). Since the List of Services has been through minimal major changes over past decade, data on individual inpatient health services provision from this dataset may be a valuable source of information, with sufficiently long time series. Pharmaceuticals consumed during hospitalisation are not reported (and are not captured in the ePrescription system either); the exemption are the so-called separately charged drugs (zvlášť účtované léky), which are reported (and reimbursed) separately – generally, these are costly innovative drugs, including oncology care drugs, and HIFs have detailed overview of their consumption based on the claim data. It is assumed that cost of all other drugs is reimbursed within the service reimbursement. For the long-term healthcare facilities, reimbursement is based on per diem payment, with a specific pharmaceutical per diem capitation payment. Hospitalisation days are known for all types of inpatient facilities (though not reimbursed explicitly for the acute care hospitals, but length of inpatient stay is relevant for the DRG grouper, hence hospitals are motivated to report it correctly). Since 2021, CZ-DRG grouper is used to measure volume of provided care of acute care hospitals and to reimburse some 44% of their services. Prior to that, the IR-DRG grouper was used, resulting in a non-comparability of the old and new DRG data. Still, the grouping for reimbursement purposes is done by the HIFs, thus the HIFs dispose of complete set of relevant primary data – reported based on the List of Services, the length of inpatient stay, and comorbidities. DRG reimbursements are subject to continuous change, including the merging of the base rates for different hospital types. For this reason, the DRG overall payment is currently not a suitable input for any indicator calculation.
Regarding reporting of diagnosis in acute inpatient care, caution is needed to interpret claim data in this domain. Often, physicians tend to report suspected diagnosis that is used for further diagnostics, instead of the final diagnosis after examination is completed. There is no information on the health status of a patient at the time of patient reception, the same applies to health status at the time of discharge. Only information on death or transfer to another ward or facility can be tracked. Some chronic conditions can be assessed using the information of consumed pharmaceuticals prior to the inpatient stay – the algorithm used for risk adjustment and redistribution can be used (see information in the section on MoH data regarding the pooling of funds data); alternatively, the “separately charged drugs” during an inpatient stay could be used to assess some chronic conditions of a patient.
There is no automatic linkage in the datasets that would allow for instant obtaining of information on, for instance, the number of patients transferred from acute care to rehabilitation facilities following big orthopaedic surgeries or AMI or stroke acute treatment. Still, such information can be obtained from the claim data upon demand (may be excessively time‑ and staff-demanding for some HIFs, however). Similarly, HIFs do not explore on a regular basis whether for instance diabetic patients follow the regular check-ups at the ophthalmologists. On an ad hoc basis and upon demand, HIFs are able to provide information on a patient consuming the referred care. However, the data do not allow for assessing whether a patient was referred to other specialists and has not followed the referral. This could change once the project of electronic referral is implemented (as of early 2022, no implementation phase yet).
Apart from the claim data, HIFs also dispose of an information on healthcare providers. As part of their contract with a HIF, a care provider is obliged to report medical specialty of its staff, number of its personnel, FTEs, health technology equipment, and operating times. Though providers are obliged to report immediately any change to this information, generally they do not do it.3 Moreover, each HIF keeps record of its contracted providers on its own; it happens often that information on the same provider differs among HIFs‘ records. The providers have to report similar information to the UZIS as part of their regular annual reports; following the COVID‑19 health workforce bonuses, paid based on these records, the UZIS has been undertaking checks between the datasets followed by datasets cleaning.
Data provided by the health insurance funds to the UZIS: Apart from code lists (číselníky a seznamy), the HIFs provide UZIS with the following datasets from their databases:
Data on the provider reported (claimed) and HIF-reimbursed care – list of claimed services (based on the List of Services directive) and pharmaceutical codes, on a quarterly basis with a monthly delay (with accounting clearance taking place after the end of the calendar year), including data on the length of hospitalisation
Total reimbursement per provider – on a biannual basis.
The list of their contracted healthcare providers, including information on staffing and health technology equipment of each contracted provider4 – on a quarterly basis, with a monthly delay.
Data processed by the Health Insurance Bureau:
The Health Insurance Bureau (Kancelář zdravotního pojištění, KZP) processes data on healthcare consumed abroad by the Czech SHI members and healthcare consumed domestically by other EU nationals and acts as the clearance centre for the Czech SHI system towards other EU countries.
The KZP acts also as a supporting organisation to the HIFs in different aspects. Recently, the KZP was mandated by the HIFs to carry on the project of healthcare quality indicators. These indicators are constructed from the claim data of the HIFs, in collaboration with the respective medical societies and professional medical associations. Claim data are provided to the KZP by the individual HIFs following a new indicator approval by the KZP’s board and detail data request. Hence, the KZP performs its analysis only on defined part of the claim data information, which has been approved by all the HIFs for a specific quality indicator development, validation, and feedback to the HIFs and to the healthcare providers.
The KZP indicators are age, sex, and morbidity standardised, allowing to compare providers to other providers of similar size. Health care outcomes measured by the KZP indicators can be viewed by health insurance funds as well as by individual providers upon secured access to the KZP‘s portal at https://puk.kzp.cz/.
The KZP continuous working on developing more care quality indicator. In early 2022, the care quality indicators included indicators on surgery treatments, gynaecology and obstetrics, neurology, and antibiotics prescription.
Ministry of Health data
Pooling of funds data.
The risk adjustment and redistribution has long history in the Czech SHI, with several major changes. The most recent one, in force since 2018, introduced the pharmacy-based cost groups (PCGs) as a proxy for selected chronic conditions. Originally, the PCGs were copied from the 2012 Dutch system of risk adjustment; in 2020 minor changes occurred (one PCG was dropped for not meeting the statistical requirements) and in 2022 four new groups will be created and 2 existing groups will be split. This has some consequences for general usability of timeseries but shall not effect greatly the PCG groups that has not changed. Starting 2022, there will be 30 PCG groups. The mechanism of rating the risk of selected chronic conditions has been well established, but till today it is used solely for pooling of funds and redistribution purposes. It has not been used for other purposes, such as reimbursement purposes or health policy decision making.
The relevant data are at the Ministry of Health – all HIFs report on annual basis the cost structure of their members, including their age and sex and a complete list of reimbursed pharmaceuticals per each member. The cost structure of each patient is calculated based on a valuation methodology described in the MoH directive for comparability purposes; the reported costs thus differ from the actual reimbursement costs. The MoH creates one dataset from information provided by all HIFs (merging information on people who switched the HIFs) and calculates the age‑sex and the PCG risk indexes for the next year. An anonymised complete dataset is then provided back to the HIFs for their analytical purposes.
This dataset may serve various purposes – besides providing the average costs per age groups, it may well serve for analysing the development of chronic conditions and prevalence or treatment of diseases captured in the PCG risk groups.
The dataset has also some limitations – for instance, if a patient is hospitalised, consumption of pharmaceuticals is not captured in the HIFs claim data (see above in the paragraph on Health insurance funds’ data), leading to a potential of that patient being ultimately missed from the given PCG risk group. Control analysis of the HIFs show that bias created by this issue is generally negligible (also due to a common practice, especially in LTC facilities, when a patient is discharged to collect his/her pharmaceuticals from a pharmacy and then readmitted into the hospital again).
Data usage above the defined use for risk adjustment and redistribution would either require the approval of the risk-adjustment supervisory body or would require a change in legislation; the first option shall not pose a problem for the MoH being member of this supervisory body.
Data on HIFs’ overall performance
Overall performance (mainly financial) of the health insurance funds is monitored by the Ministry of Health and the Ministry of Finance. For this purpose, the HIFs report their Health Insurance Plans (zdravotně pojistné plány) for next calendar year with expected data on the current calendar year to both the MoF and MoH. Annual Reports are submitted after a year is closed. Also, representatives of both Ministries serve as members of the Supervisory boards of each HIF and are provided the financial and performance results on a regular basis throughout the year.
The set of information to be publicly available through the Health Insurance Plans and the Annual Reports is defined in the MoH directive. Information includes:
information on statutory health revenues, information on insured population, HIF’s number of employees and the administrative costs, data on SHI expenditures, and expenditure data divided by type of care. Financial performance indicators include the current expenses and revenues, costs and gains, overdue payables, financial reserves in days of expenditures, etc.
The non-public part of the annual reports also includes few selected indicators, mainly preventive care consumption indicators, provided for information purposes to the MoH only, broken down to the level of districts (75, including the capital city of Prague as one single district): the number of general preventive examinations, dental preventive examinations, gynaecological preventive examinations, share of insurees aged 65+ vaccinated against flu, and statistics of complaints about ensuring local and time accessibility of care.
Institute for Health Information and Statistics (UZIS) data
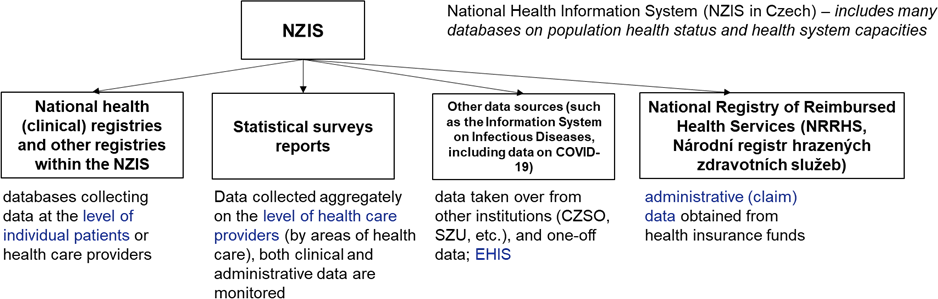
National Health Information System (NZIS in the Czech) includes many databases on population health status and health system capacities. Those datasets that are based on patient level data use the same unique personal identifier. The legislation allows for linkages of all datasets in the custody of the UZIS.
The UZIS also custodies data provided by the healthcare providers on their structure and workforce (registry of healthcare professionals and registry of health service providers, economic performance data of hospitals etc.); data provided by healthcare providers on selected diagnoses and hospitalisation (12 national health registries, including 11 clinical, or diagnostically specific, registries + 1 hospitalisation registry); data provided by healthcare providers within a reference providers’ network for the CZ-DRG purposes; and data taken from other institutions and survey data (basic population registry, EHIS, death certificate registry).
UZIS also reports health and healthcare indicators to international databases.
National Registry of Reimbursed Health Services (NRHZS, Národní registr hrazených zdravotních služeb) contains administrative (claim) data provided by (populated by) the HIFs on reimbursed health services.
National health (clinical) registries and other registries within the NZIS are databases collecting data at the level of individual patients or healthcare providers, usually (but not always) populated by the healthcare providers (see below). The reporting to these registries is done via reports that can but need not to be automatic of the hospital’s IT system. The reports have prescribed structure by the UZIS and in certain cases, a hospital’s IT system has been adjusted to generate a report directly from the hospital’s internal data (which are not necessarily equal to the patient’s medical record).
National Health Registries:
National Registry of Hospitalization (NRHOSP, Národní registr hospitalizací) – contains patient-level data, populated by healthcare providers, validated (cross-checked) using the NRRHS dataset.
Diagnostically specific clinical registries – currently 11 registries, includes patient-level data.
oncological registry, cardiovascular surgeries and interventions registry – populated by healthcare providers
diabetology registry – populated using the NRRHS claim data
National Registry of Healthcare Professionals (NRZP, Národní registr zdravotnických pracovníků) includes statistical survey (reporting) data, populated by schools, healthcare providers, professional chambers.
National Registry of Health Services Providers (NRPZS, Národní registr poskytovatelů zdravotních služeb) includes statistical survey (reporting) data, populated by healthcare providers.
Surveys:
UZIS is processing data collected through CZSO household survey on health for the EHIS survey. For details on the EHIS survey, see below under the CZSO section and the SZU section.
UZIS also analyses data from the reference providers’ network (also for the CZ-DRG purposes).
Figure A E.1. Structure of the National Health Information System
Czech Statistical Office (CZSO) data
System of Health Accounts (SHA)5 contains an internationally comparable comprehensive statistics on healthcare expenditures in the Czech Republic according to the ICHA international classification, according to the type of care provided (HC), type of healthcare provider (HP) and source of financing (HF), and in their combination. It also includes part of social care expenditures (social care allowance, senior homes subsidies). Contains aggregate data submitted by the HIFs and other central and regional government bodies (recently, HIFs aggregate data replaced by the UZIS calculations performed on the pooled original claim data). Ministry of Health submits part of the information on type of care distribution of reimbursements that is not clearly indicated in the claim data; the MoH obtains this aggregate information from individual HIFs and reports total numbers to the CZSO.
Population data (population registry, demographics – age and gender structure, mortality). Census data has not been used in the health policy making; only aggregate data can be used as individual data are required by the law to be deleted when census data processed.
European Health Interview Survey (EHIS) – household sample survey, every 6 years (last in 2019, 8 000 respondents aged 15+), shared European methodology. CZSO collects the data since 2014, data processing is done by the UZIS (see above). Sample surveys on health status since 1993, since 2008 based on the uniform European methodology (prior to 2014, survey implemented by UZIS on a different household sample). The survey focuses not only on health status, but also on the use of healthcare (doctor’s visits, hospitalisations) and selected aspects of lifestyle closely related to health (consumption of fruits and vegetables, physical activity, and smoking). Some results of the survey are included in the Statistical Yearbook of the Czech Republic 2020.6
Sample survey on people with disability (Výběrové šetření osob se zdravotním postižením VŠPO) – household sample survey. Information on disabled people, not only on those captured in the statistics of state social care allowance and invalidity pension. Includes information on health disabled people’s age, gender, economic activity, education, activities of daily living self-sufficiency and caring support usage, quality of life and health status. Results are publicly available.7
Incapacity to work statistics8 – jointly with Česká správa sociálního zabezpečení (ČSSZ), biannually, since 1989. Includes incidence, prevalence, average length of work incapacity. By cause, type of economic sector, by regions and districts, and also by age and gender and by diagnosis. Statistics on fatal injuries are also publicly available.
Statistics on research and development expenditures in the health sector9 – annual survey (reporting) of all companies, schools and research institutions. Expenditures on research and development are available explicitly for healthcare providers. Number of researchers is available for medical sciences.
Public budget expenditures on health and medical research by socio‑economic objectives10 (international classification Government Budget Appropriations for R&D, GBARD) is based on administrative data. Distribution also according to support founders and support receivers. The dataset includes more areas, one of them is the Protection and Improvement of Human Health.
Health care workforce remuneration is different dataset from the UZIS statistics on the same topic, as the two have different primary data sources. The CZSO dataset builds on two sources: a sample survey on wage remuneration (done by the Ministry of Social Affairs) and on the information system on tariffs‘ pays (by the Ministry of Finance). Information is publicly available for instance in the newly published CZSO publication Focus on Women and Men 2022,11 in Chapter 2. Health (tables 2‑24 to 2‑27), (CZSO, 2022[13]).
Information on medical and health service students and graduates, the data is taken from the student registry (systém Sdružených informací matrik studentů, SIMS). Data for university students always refer to 31 December of the relevant year, data for graduates to the entire calendar year. The healthcare field of study is defined on the basis of the Classification of Fields of Education CZ-ISCED-F 2013, using the narrowly defined field 091 Health care, which includes the following detailed fields of education: Dentistry (0911); Human Medicine (0912); Nursing and midwifery (0913); Medical diagnostics and treatment techniques (0914); Therapy and Rehabilitation (0915); Pharmacy (0916); Traditional and alternative medicine and therapy (0917). Publicly available indicators can be found in Chapter 2. Health of the publication Focus on Women and Men 2022 (tables 2‑19 to 2.23) (CZSO, 2022[13]).
Statistics on eHealth use – derived from the UZIS’s providers‘ annual reporting and processed by the CZSO, focuses on providers‘ IT equipment and offered eHealth services. The second source of information on this topic is the household sample surveys on ICT use of individuals and households. Publicly available indicators can be found on CZSO webpage12 and in the annual CZSO publication Information Society in Numbers, chapter G: ICT in healthcare providers.13
State Institute for Drug Control (SUKL) data
SUKL is in charge of the datasets on information retrieved from the electronic prescription system; and newly also datasets from the electronic system of reimbursed medical devices and aids and vaccination administration database.
Medical products database
Pharmacies database
Registry of medical devices (registr zdravotnických prostředků)
Electronic prescription system (ePreskripce) – patient-level database
individual drug records
Includes all prescribed medical products, also the non-collected ones
includes prescription drugs with zero reimbursement
Vaccination administration database – new, obligatory evidence since 1/2022
Prescribed medical device database – new since 3/2022, voluntary
National Public Health Institute (SZÚ) data
Data from the EHES survey on population health status
EHES (European Health Examination Survey) was piloted in 2010‑11 (400 people). The first standard survey round was in 2014. The second regular survey round was carried out in July 2019 – February 2020 (4 000 people), connected to the European Health Interview Survey (realised by the CZSO as part of its household sample survey). The EHES survey was co‑ordinated by the SZU and realised by the SZU with the help of Regional Public Health Authorities, the Public Health Institutes (there are 2 such Institutes in the Czech Republic), and selected healthcare providers.
EHES is linked to the EHIS survey: EHIS survey co‑ordinated by the UZIS and carried out by the CZSO using its household survey interview network using the CAPI method, but PAPI and CATI14 are also allowed. In EHES survey, EHIS respondents aged 25‑64 were offered a medical examination – including measurement of height, weight and waist circumference, measurement of blood pressure, determination of blood fat level (total and HDL and LDL cholesterol and triglycerides), determination of blood sugar level (HbA1c – glycated haemoglobin) and examination of thyroid hormone (TSH).
Data on EHIS is administered by the UZIS. Data on EHES is administered by the SZU. Respondents’ EHES ID is matched to their EHIS IDs, so EHES and EHIS data are linked and pooled together by the SZU. Manual for EHES survey in the Czech Republic is available in the Czech language at the SZU webpages15 (the same as for the 2014 survey round). Selected 2019 study results are also publicly available.16
NAUTA (Národní výzkum užívání tabáku a alkoholu v České republice), the National survey on tobacco and alcohol use in the Czech Republic. Regular surveys have been on since 1997, the last one in 2020 (1 769 respondents, representative for the Czech population aged 15+ by age, sex, and regions; results of these surveys enter the WHO Health for All database. Survey results are publicly available.17 Surveys are based on structured face‑to-face interviews; for tobacco use the survey uses the set of key questions of the Tobacco Questions for Surveys (TQS) of the GATS; for alcohol use the survey uses the common method for frequency and quantity use of the Beverage Specific Frequency‐Quantity Method of the EU SMART project, adding a question on binge drinking. Details can be found in Csémy et al. (2021).18
HAPIEE (Health, Alcohol and Psychosocial factors in Eastern Europe)19 survey is a population health cohort study focusing on lifestyle and psycho-socio factors. Started in 2002‑05 (8 800 respondents) when all respondents filled the survey questionnaire and underwent a medical examination including blood tests. Since 2010, roughly each 2 years a questionnaire is sent to respondents by post. Last survey round finished in 2018.
Regular SZÚ monitoring: air pollution, drinking and bathing water pollution, community noise, contaminants in food chains and dietary exposures, human biomonitoring, occupational health hazards.20
Surveys on allergies in children – since 1996, every 5 years, with the last one in 2016.21 Details on historical and abandoned surveys can be found at SZU webpage,22 including for the HELEN survey (abandoned in 2014).
Datasets on antibiotics use. Recently, the SZU was provided data on antibiotics prescription (collected antibiotics only) by the KZP, with the primary data source being the HIFs’ claim data. Analysis performed by the KZP allows to track prescription behaviour of individual physicians (only collected prescriptions with non-zero reimbursement are included).
Notes
← 1. Note, all data in the National Registry of Reimbursed Services comes from the claim data and is not tied to the patients‘ medical records. Diagnosis information included in this dataset is not very reliable, except for few (minor) cases which can be strictly traced to non-zero reimbursement purposes.
← 2. Which is the current practice of reporting this indicator to international organisations.
← 3. The level of inaccuracies in providers’ reporting to the HIFs was revealed when extra bonuses were compensated by the HIFs to the healthcare providers based on the evidence of their employees during the COVID‑19 pandemic.
← 4. Basically this means the UZIS ends up with 8 different lists of healthcare providers – 7 provided by the HIFs and the 8th from the regular providers‘ reporting to the UZIS.
← 5. CZSO (2021), Výsledky zdravotnických účtů ČR 2010‑19. https://www.czso.cz/csu/czso/vysledky-zdravotnickych-uctu-cr-m6hwrlzbbw.
← 8. https://www.czso.cz/csu/czso/pracovni-neschopnost-pro-nemoc-a-uraz-v-ceske-republice-1-pololeti-2021.
← 14. CAPI – Computer Assisted Personal Interview; PAPI – Paper Assisted Personal Interview; CATI – Computer Assisted Telephone Interview.
← 17. http://www.szu.cz/tema/podpora-zdravi/prevence‑zavislosti. For the period 1997‑2011, results available at http://www.szu.cz/tema/podpora-zdravi/studie-kuractvi-dospele-populace-cr-2011.
← 18. Csémy, Dvořáková, Fialová, Kodl, Malý, Skývová (2021). Národní výzkum užívání tabáku a alkoholu v České republice 2020 (NAUTA). Státní zdravotní ústa, vhttp://www.szu.cz/uploads/documents/szu/aktual/nauta_2020.pdf.
← 19. The Czech survey details are available at http://www.szu.cz/hapiee.
← 20. Details at http://www.szu.cz/ehes/vybrane-vysledky-studie-ehes-2019, and especially at http://www.szu.cz/uploads/documents/chzp/souhrnna_zprava/SZU_Report_2019.pdf.