This section presents the Czech HSPA framework and describes its domains and subdomains. While taking account of the development process that led to establishing and recognising common HSPA framework across health sector stakeholders, the stock of this project’s activities is described in Annex C.
Health System Performance Assessment Framework for the Czech Republic

3. The Czech HSPA framework
3.1. The process
The Czech HSPA framework was developed in several iterations. The first draft was the output of interactive sessions of workshops 4 and 5, held in April 2022 (see Annex C). The working group members generated themes and ideas that were then grouped into common domains.
The framework was further elaborated on and refined throughout the next project phases, following the discussions and suggestions raised during the focus group meetings, the project management team meetings, the indicator selection process consultations, and the inputs from the High-Level Advisory Board members. The later took regular note of the framework development and approved the final version of the Czech HSPA framework on its meeting in April 2023.
3.2. The Czech HSPA framework domains, and subdomains
The Czech HSPA framework is composed of 12 domains grouped into 4 areas: Outcomes, Outputs, Processes, and Structures (Figure 3.1). The domains are further detailed out by 28 subdomains, covering different aspects of the Czech health system to align with the defined HSPA purpose and scope (see Sections 2.2 and 2.3).
Figure 3.1. The Czech HSPA framework
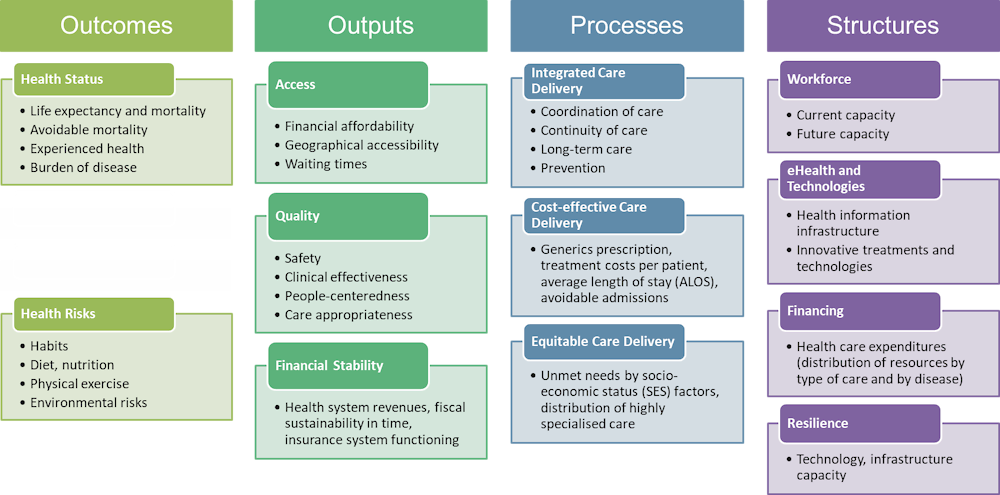
Source: The Czech HSPA project.
The ultimate Outcomes of the health system are covered within the Health Status domain, looking at life expectancy and mortality, avoidable mortality, people’s experienced health, and burden of disease. The domain of the Health Risks is placed a little aside because it focuses on people’s lifestyle and environment, which is not a direct outcome of a health system, but can be influenced, to some degree, for instance by prevention campaigns and improved health literacy. This domain thus covers topics grouped into lifestyle habits such as smoking and alcohol consumption, healthy diet, physical exercise, and risks imposed by the living environment.
The three domains in the Output area include measurements of the direct outputs of the health system, focusing on healthcare accessibility and quality and health system financial stability. The Access domain involves the three dimensions of accessibility of health services, along the definitions of healthcare financial affordability, geographical accessibility, and waiting times. Complementarily, the Quality domain features topics of healthcare safety, clinical effectiveness, people‑centredness, and care appropriateness. Finally, the Financial Stability domain looks at health system revenues, fiscal sustainability, and the public health insurance system functioning.
The area of Processes describes what is happening in the health system to reveal strengths and weaknesses related to healthcare organisation and delivery. Under the Integrated Care Delivery domain, the co‑ordination of health services is described as processes involving interactions of various healthcare providers, which are usually required to care for chronically ill people. Simultaneously, the Continuity of Care subdomain describes patient pathways and the smoothness of care delivery for a single diagnose or health event, and the Long-Term Care and Prevention subdomains complement the Care Integration domain. The second domain of Processes involves Cost-effective Care Delivery, focusing on areas where cost-effectiveness measurement is feasible: prescriptions, treatment costs, length of hospitalisations, and avoidable admissions. The Equitable Care Delivery aims to describe the inequalities in healthcare consumptions based on socio‑economic status, looking in particular at unmet healthcare needs due to specific reasons and for specific groups of population.
The last area of the Czech HSPA framework covers structures of the healthcare system, ranging from domains focusing on health workforce, to those focusing on eHealth and technologies, financing, and health system resilience.
The detailed description of subdomains of the Czech HSPA framework is provided in Table 3.1.
Table 3.1. Description of the Czech HSPA domains and subdomains
|
Area |
Domain |
Subdomain |
Description |
|---|---|---|---|
|
Outcomes |
Health status |
Life expectancy |
The “life expectancy” area analyses life expectancy, healthy life expectancy and the main causes of death. |
|
Outcomes |
Health status |
Avoidable mortality |
The area of “avoidable mortality” aims at monitoring deaths from preventable or treatable causes. |
|
Outcomes |
Health status |
Experienced health |
The patients subjective experience of their own health |
|
Outcomes |
Health status |
Burden of disease |
The “burden of disease” area analyses the incidence and prevalence of the most common diseases and the occurrence of comorbidities. |
|
Outcomes |
Health Risks |
Habits |
Monitoring of behaviour related to risky lifestyle (i.e. substance abuse) |
|
Outcomes |
Health risks |
Diet, nutrition |
Monitoring of behaviour related to eating habits and diet |
|
Outcomes |
Health risks |
Physical exercise |
Monitoring of behaviour related to active lifestyle (i.e. physical exercise) |
|
Outcomes |
Health risks |
Environmental risks |
Monitoring of environmental risks for health. |
|
Outputs |
Access |
Financial affordability |
Financial affordability of healthcare services for the patients |
|
Outputs |
Access |
Geographical accessibility |
Geographical accessibility of healthcare services |
|
Outputs |
Access |
Waiting times |
Accessibility of health services in time |
|
Outputs |
Quality |
Safety |
Safety of care may be defined as “the degree to which the system does not harm the patient” |
|
Outputs |
Quality |
Clinical effectiveness |
Effectiveness of care is ’the degree of achieving desirable outcomes and the degree to which care is provided according to evidence (EBM). |
|
Outputs |
Quality |
People‑centredness |
The patients’ subjective experience with the health system |
|
Outputs |
Quality |
Care appropriateness |
Appropriate care is healthcare that is relevant with regard to the patient’s health status, clinical needs and current knowledge (i.e. care provided by a provider with the right expertise or level of specialisation, in the right time) |
|
Outputs |
Financial stability |
Analysis of the income side of the system, analysis of the financial resources of the system and their stability (and sufficiency) over time. |
|
|
Processes |
Integrated care delivery |
Coordination of care |
Ongoing co‑ordination of multiple providers in the care of a chronically ill patient, including measurement of the consequences of insufficient co‑ordination (e.g. avoidable hospitalisations). (E.g., care of an ophthalmologist, diabetologist and GP for a patient with diabetes) |
|
Processes |
Integrated care delivery |
Continuity of care |
It measures the patient’s journey through the system (patient pathway), the continuity of patient care between individual providers within a single diagnosis (e.g. early rehabilitation after a heart attack) |
|
Processes |
Integrated care delivery |
Long-term care |
Indicators describing the functioning of long-term care and home care. |
|
Processes |
Integrated care delivery |
Prevention |
Ability of the system to avoid the occurrence of a disease (primary prevention, e.g. using vaccination), or to identify a disease as early as possible in order to initiate treatment without delay (secondary prevention, e.g. screening programmes). |
|
Processes |
Cost-effective care delivery |
The indicators measure ways of providing healthcare that are considered cost-effective. It also measures the consequences of care failure, such as avoidable admissions. |
|
|
Processes |
Equitable care delivery |
Availability of healthcare services to patients regardless of their sex, age, education or income |
|
|
Structures |
Workforce |
Current Capacity |
Current availability and capacity of medical personnel |
|
Structures |
Workforce |
Future Capacity |
Future availability and capacity of medical personnel |
|
Structures |
eHealth and technologies |
Health information infrastructure |
How fast and how easily are health-information accessible for the patient and for relevant providers |
|
Structures |
eHealth and technologies |
Innovative treatments and technologies |
Availability of hi-tech equipment and innovation in the healthcare sector |
|
Structures |
Financing |
Analysis of the expenditure side of the healthcare system (e.g. by types of care, diagnoses) |
|
|
Structures |
Resilience |
Ability of the healthcare system to absorb, respond to and adapt to unexpected events. |
Source: The Czech HSPA project.
For additional information:
Annex C: Process of determining the Czech HSPA framework domains.
HSPA framework development workshops
Technical focus groups
Study visit to Belgium