For decades, health policy makers have strived to achieve high-performing health systems that deliver good health outcomes to populations, prevent ill-health and provide high-quality care available to all at affordable cost for payers and patients.
These issues have become even more pressing today. Health systems are under enhanced pressure to perform well under new circumstances. The COVID‑19 crisis has rocked societies and economies. It highlighted the necessity for health systems to be adequately equipped to handle and promptly recover from high-impact shocks. In this context, it has become essential for health systems to develop ways of assessing their resilience to disruption. This notion of resilient health systems is critical no matter whether the shock is caused by an external cause, such as a pathogen with pandemic potential, other biological threats, war, or by more enduring challenges such as population ageing and environmental threats.
Too often, health systems have been focused on what the system can deliver, rather than on people’s needs and preferences. People demand care that is better centred around what matters most to them, and health systems must be able to measure and assess their ability to meet patients’ needs and expectations. Health systems also need to improve the outcomes and experience of care, including as measured and reported by patients themselves. Furthermore, with the ageing of populations, evolving health needs also call for more continuity of care, integration of services and data, and health literate populations. These are all key components of high-performing and people‑centred health systems.
Climate change is an enduring challenge putting further pressure on health systems. It calls for immediate action to respond adequately to the new and incremental health needs caused by heat waves and other climate‑related threats. It also requires reducing the environmental impact and carbon footprint of health systems themselves. Yet today we still do not adequately assess the ability of health systems to respond to the stress posed by global warming on the health and well-being of people, nor their ability to contribute to environmental sustainability and reduce their carbon footprint.
Digitalisation and artificial intelligence provide new opportunities to rethink how health systems can deliver high-quality care that is accessible to all. Telemedicine offers opportunities to bring services closer to people. Artificial Intelligence has great potential to improve clinical care, research, and system governance. These could improve health system performance, but ethical and governance challenges need to be tackled – and health systems must be able to assess their impact more effectively.
Finally, the need for health systems to provide high-quality and safe care in a context of growing pressure on budgets means that they are increasingly being asked to deliver, reward and measure value rather than sheer volume of care. Efforts to improve value for money needs to be accompanied by improved ability to assess the implications for different population groups, irrespective of age, income, or gender, with special attention given to the most vulnerable.
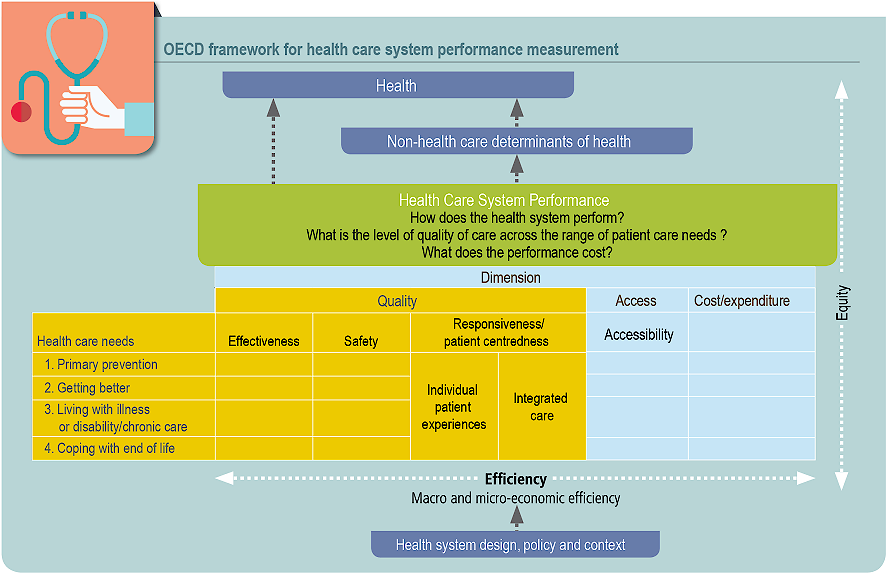
This evolving policy context call for a new vision of health system performance assessment that integrates new dimensions of performance such as resilience, people‑centredness, and environmental sustainability.
Health system performance assessment (HSPA) has become a crucial element in ensuring that health systems provide quality healthcare and meet people’s needs. By consistently and systematically evaluating health systems, HSPA serves as a valuable instrument for policy makers to identify areas that require improvement, support a more efficient allocation of resources, and assess the achievement of key policy objectives.
Over the past three decades, assessing the performance of health systems has formed a key part of the OECD’s efforts to support a high quality of care amid rising expenditures and changing demographic trends. Measures of health system performance have evolved as new evidence from health sector policy and experiences emerged since the OECD first published comparative reviews of health system reforms in 1992 (see Annex A for a more detailed description of the history of health system performance assessment). The renewed Framework developed by the Secretariat reflects the changing landscape of health systems today and combines several components of other frameworks currently in use.