Tuberculosis (TB) is one of the leading causes of death from an infectious disease in Asia-Pacific. In 2020, there were 5.8 million incident (new and relapsed) TB cases worldwide – a reduction from 7.1 million reported cases in 2019 due to the COVID‑19 pandemic indirect impact-, an estimated 1.3 million deaths amongst HIV-negative people globally (WHO, 2021[1]). TB cases and deaths occur disproportionately amongst men, but the burden of disease amongst women is also high as it remains amongst the top three killers for them in the world. Most cases of TB are curable if diagnosed early and the appropriate treatment is provided, therefore curtailing onward transmission of infection.
TB was declared a global health emergency by the WHO in 1993, and the WHO-co‑ordinated Stop TB Partnership set targets of halving TB prevalence and deaths by 2015 compared with a baseline of 1990. The WHO’s End TB Strategy (post‑2015) which followed the Stop TB Strategy aims at ending the global TB epidemic by 2035, in line with the Sustainable Development Goals (Sharma, 2017[2]). In 2018, the UN General Assembly High-Level Meeting on the fight against TB endorsed a political declaration to emphasise an importance of accelerating progress towards End TB targets (UNGA, 2018[3]).
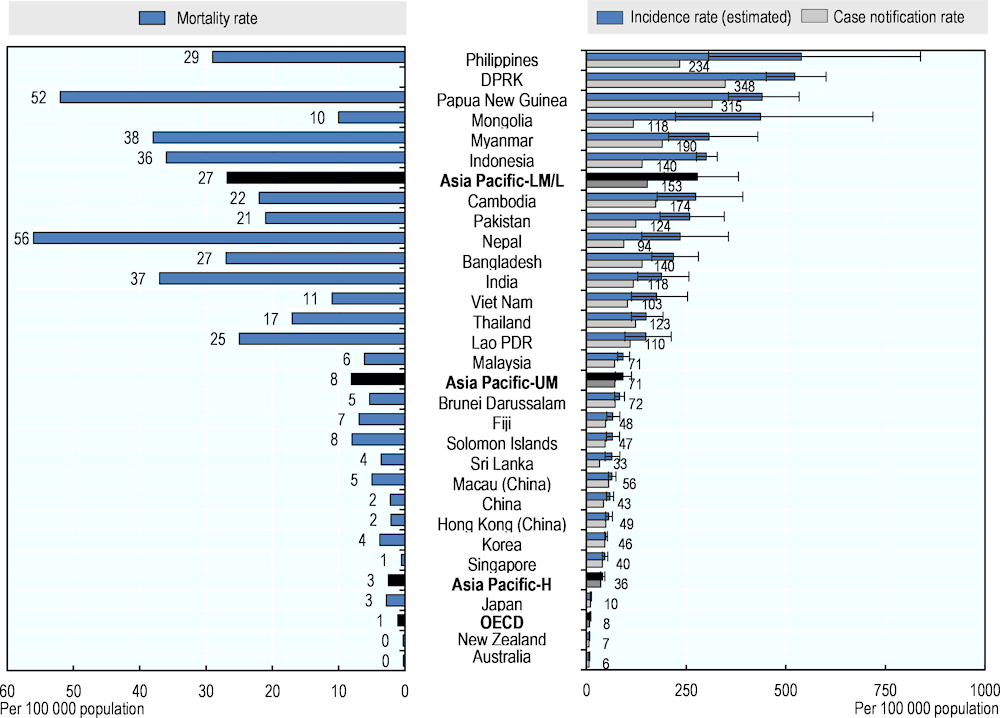
In Asia-Pacific, TB mortality rates were high in Nepal and Papua New Guinea with over 50 deaths of people without HIV per 100 000 population (Figure 3.23, left panel).
South-East Asia accounted for 43% of the estimated TB cases globally in 2020, more than any other WHO region. India (26.0% of TB cases globally), China (8.5%), Indonesia (8.4%), the Philippines (6.0%), Pakistan (5.8%), and Bangladesh (3.6%) were amongst the most affected countries and territories in 2020 – keeping in mind that these countries and territories also had important reductions in the reporting of cases due to the COVID‑19 pandemic – (WHO, 2021[1]). The case notification rate is particularly high in DPRK and Papua New Guinea, at more than 300 cases per 100 000 population. An incidence rate higher than 500 cases per 100 000 population was estimated for the Philippines and DPRK, while for Australia and New Zealand less than 10 incident cases per 100 000 population were estimated (Figure 3.23, right panel).
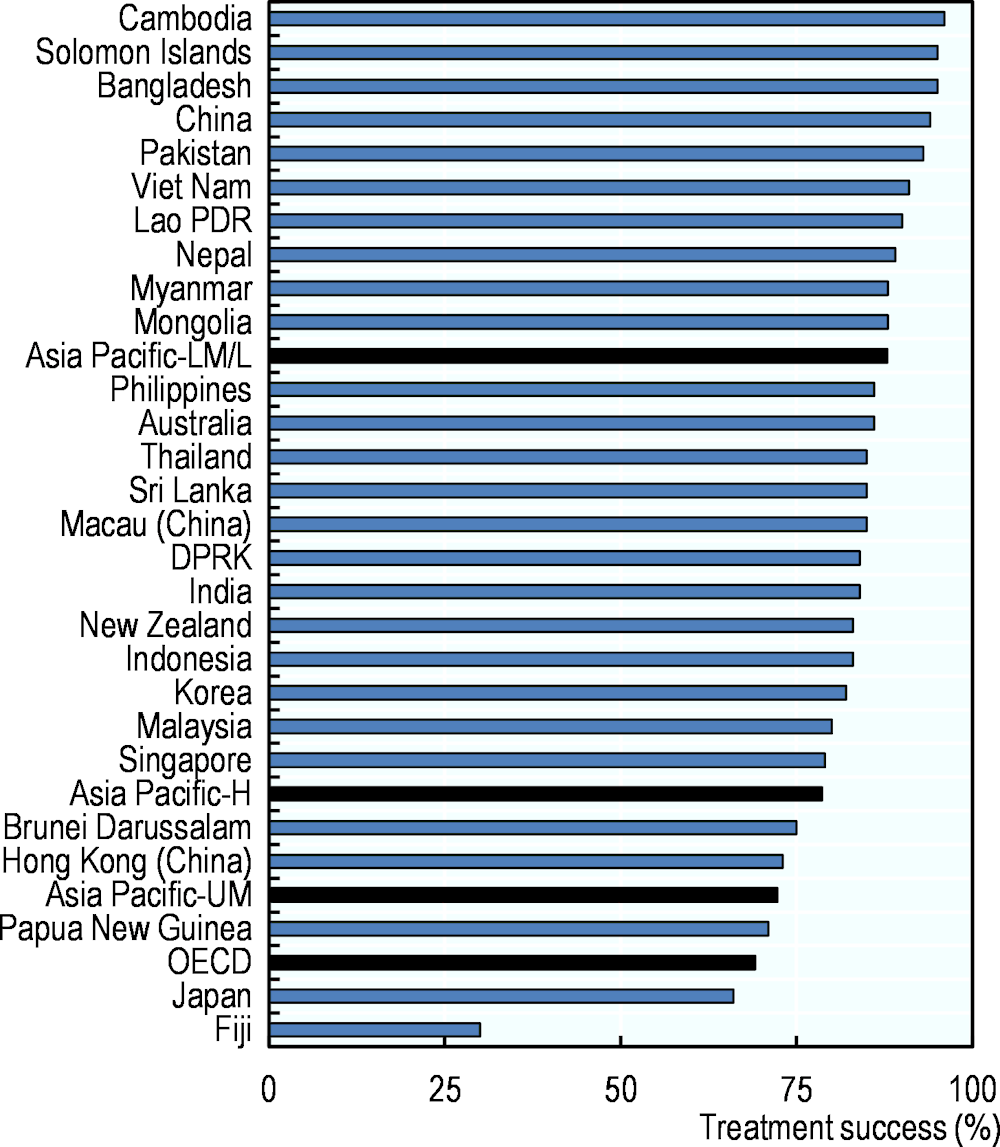
High-quality TB services have expanded, and many cases are treated, reaching the treatment success rate for new TB cases of more than 85% in many Asia-Pacific countries and territories in 2019 (Figure 3.24). Nevertheless, Fiji reports a low treatment success rate at 30%. In countries and territories where TB predominantly affects older people -such as Japan and Hong Kong (China)-, treatment success rate was lower than 75%.
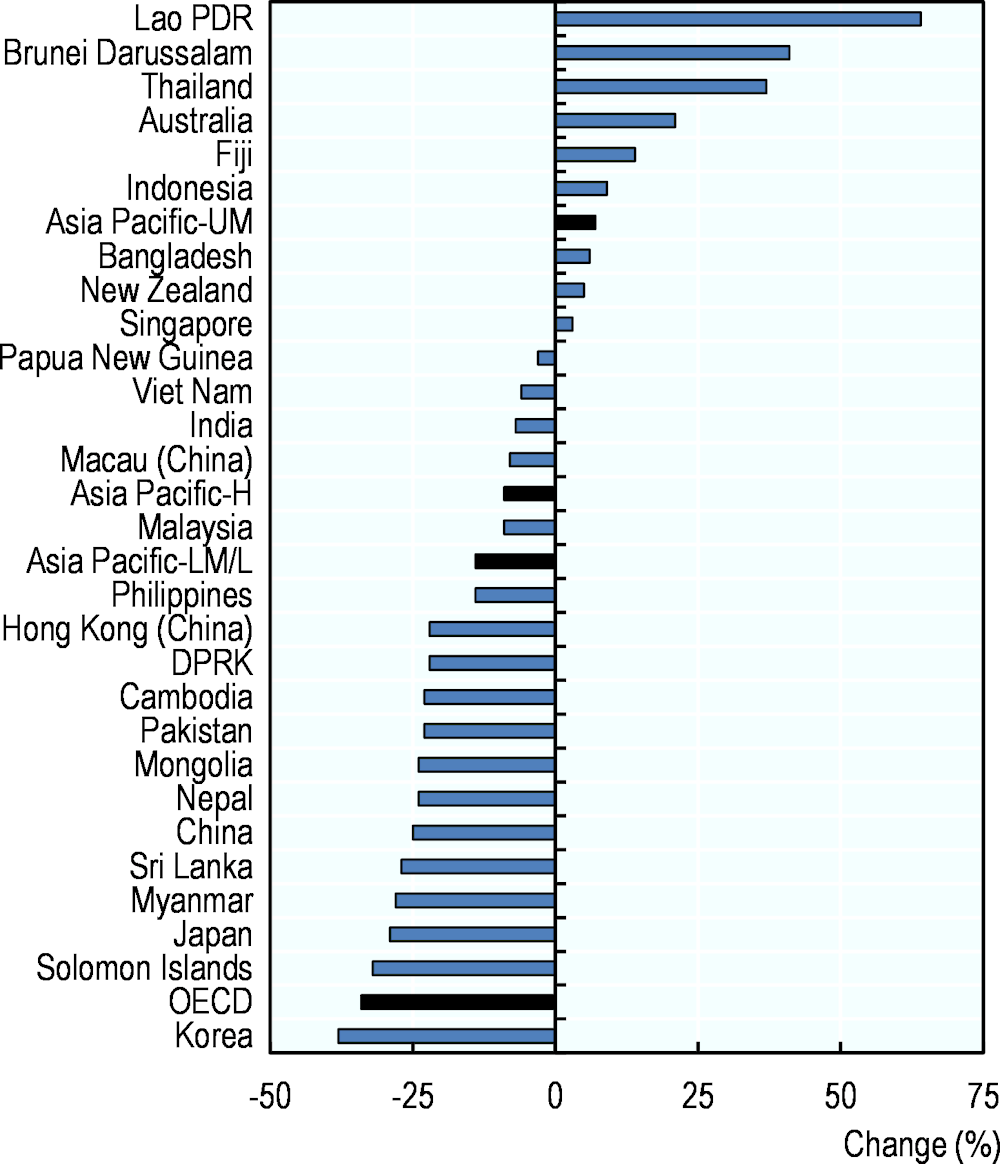
The Asia-Pacific region is rising to the challenges presented by TB. In a large part of the countries and territories, case notification rates have declined from 2015 to 2020 (Figure 3.25). However, countries and territories like Lao PDR, Thailand, Fiji, Indonesia, Bangladesh, Singapore, New Zealand, Australia and Brunei Darussalam are showing upward trends, with the latter four belonging to the high-income economies group and experiencing low base case notification rates. The region still faces important challenges in TB control, including providing services to those in greatest need, especially the poor and vulnerable. HIV-TB co‑infection, the emergence of drug-resistant strains, a sizeable proportion of TB-affected population facing catastrophic costs due to TB, funding gaps and the need for greater technical expertise all remain threats to progress (WHO, 2016[4]; WHO, 2019[5]). Concerning drug-resistant TB (MDR/RR-TB), the burden is high in China with 7.1% of new cases are estimated to have MDR/RR-TB. This proportion is also high at 5.1% in Myanmar and Viet Nam, at above 4%. Treatment of MDR/RR-TB can take up to two years and is far more costly than drug susceptible strains.