Optimal feeding practices of infants can increase their chances of survival. They play an important role for healthy growth and development, decrease rates of stunting and obesity and stimulate intellectual development (UNICEF, 2019[1]).
Breastfeeding is an unequalled way of providing nutrition for infants. Breast milk gives infants the nutrients they need for healthy development, including the antibodies that help protect them from common childhood illnesses such as diarrhoea and pneumonia, the two primary causes of under-five child mortality worldwide. Breastfeeding is also linked with better health outcomes later in life. Adults who were breastfed as babies often have lower blood pressure and lower cholesterol, as well as lower rates of overweight, obesity and type 2 diabetes (Horta, Cesar and WHO, 2013[2]; Horta, Loret de Mola and Victora, 2015[3]; Victora et al., 2016[4]). Breastfeeding also improves school attendance and is associated with higher income in adult life. More than 800 000 deaths amongst children under five could be saved every year globally if all children 0‑23 months were optimally breastfed. Breastfeeding also benefits mothers through assisting in fertility control, reducing the risk of breast and ovarian cancer later in life and lowering rates of obesity (UNICEF, 2019[1])
The WHO Baby-Friendly Hospital Initiative outlines detailed recommendations on protecting, promoting, and supporting breastfeeding in facilities providing maternal and newborn services (WHO, 2017[5]). WHO and UNICEF recommend early initiation of breastfeeding within 1 hour of birth, exclusive breastfeeding for the first 6 months of life, and introduction of nutritionally-adequate and safe complementary (solid) foods at 6 months together with continued breastfeeding up to 2 years of age or beyond.
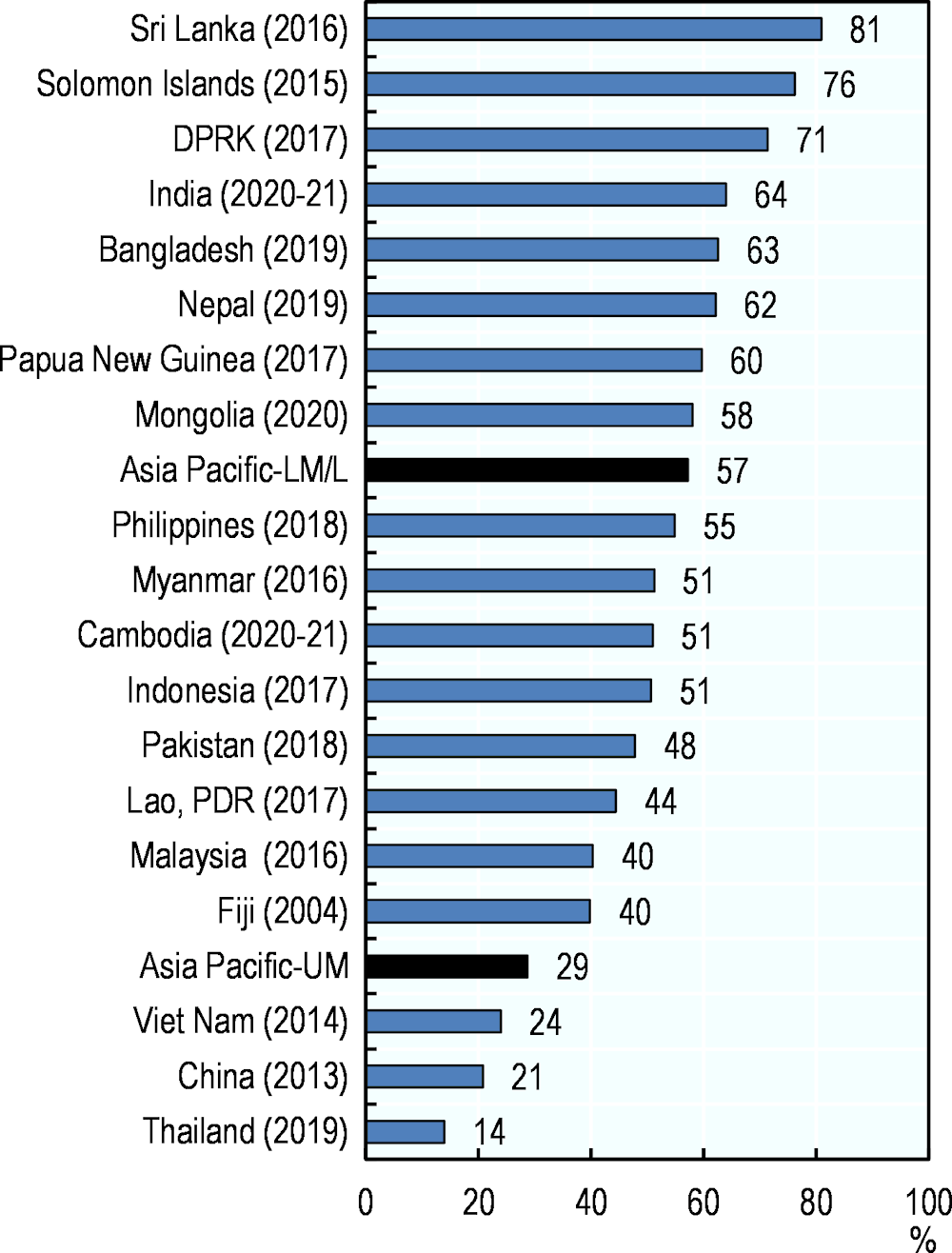
In 2012, the World Health Assembly endorsed a comprehensive implementation plan on maternal, infant, and young child nutrition, which specified a set of six global nutrition targets and one of the targets aims to increase the rate of exclusive breastfeeding in the first six months up to at least 50% by 2025. Globally, this target has not been achieved as 44% of children under six months being exclusively breastfed in 2021 (UNICEF, 2021[6]). However, in the Asia-Pacific region, Sri Lanka, the Solomon Islands, DPRK, Cambodia, India, Bangladesh, Nepal, Papua New Guinea, Mongolia, the Philippines, Myanmar and Indonesia have already achieved this target (Figure 4.3). The proportion of infants exclusively breastfed for the first six months of life in lower-middle- and low-income Asia-Pacific countries was two times the proportion reported in upper-middle-income countries. Policies and regulations on marketing of breast-milk substitutes and workplace support to breastfeeding as well as breastfeeding counselling in health facilities and societal beliefs favouring mixed feeding contribute to variations in exclusive breastfeeding rates across countries (Local Burden of Disease Exclusive Breastfeeding Collaborators, 2021[7]).
However, several Asia-Pacific countries and territories are lagging as less than one in four infants was exclusively breastfed in Thailand, China, and Viet Nam (Figure 4.3). Key factors contributing to inadequate breastfeeding rates include unsupportive hospital and health care practices and policies; lack of adequate skilled support for breastfeeding, specifically in health facilities and the community; aggressive marketing of breast milk substitutes and inadequate maternity and paternity leave legislation and unsupportive workplace policies (UNICEF, 2019[1]). Several countries and territories which increased exclusive breastfeeding practice have implemented these policies. For example, the Bangladesh Breastmilk Substitutes (BMS) Act was developed in 2013 to ensure that mothers and families get accurate and unbiased information, free of commercial pressure, to feed infants and young children, and it also regulates the inappropriate marketing and distribution of BMS (Toolkits, 2019[8]). Since, the rate of exclusive breastfeeding in Bangladesh increased from 55.3% in 2014 to 62.6% in 2019 (OECD/WHO, 2018[9]). Another example is Cambodia, where the government implemented several diverse activities starting in 2004, including the establishment of breastfeeding practices in hospitals and community-based volunteers advocating the benefit of breastfeeding to expecting and new mothers. Consequently, the exclusive breastfeeding rates for babies under six months in Cambodia rose from 7% in 2000 to 65% in 2014. However, after considerable progress, there was a subsequent decline to 51% in 2020/21. This latter example demonstrates that it remains difficult to achieve sustained improvements in exclusive breastfeeding practice even if countries see initial improvements – therefore sustained and broad-based support is essential.
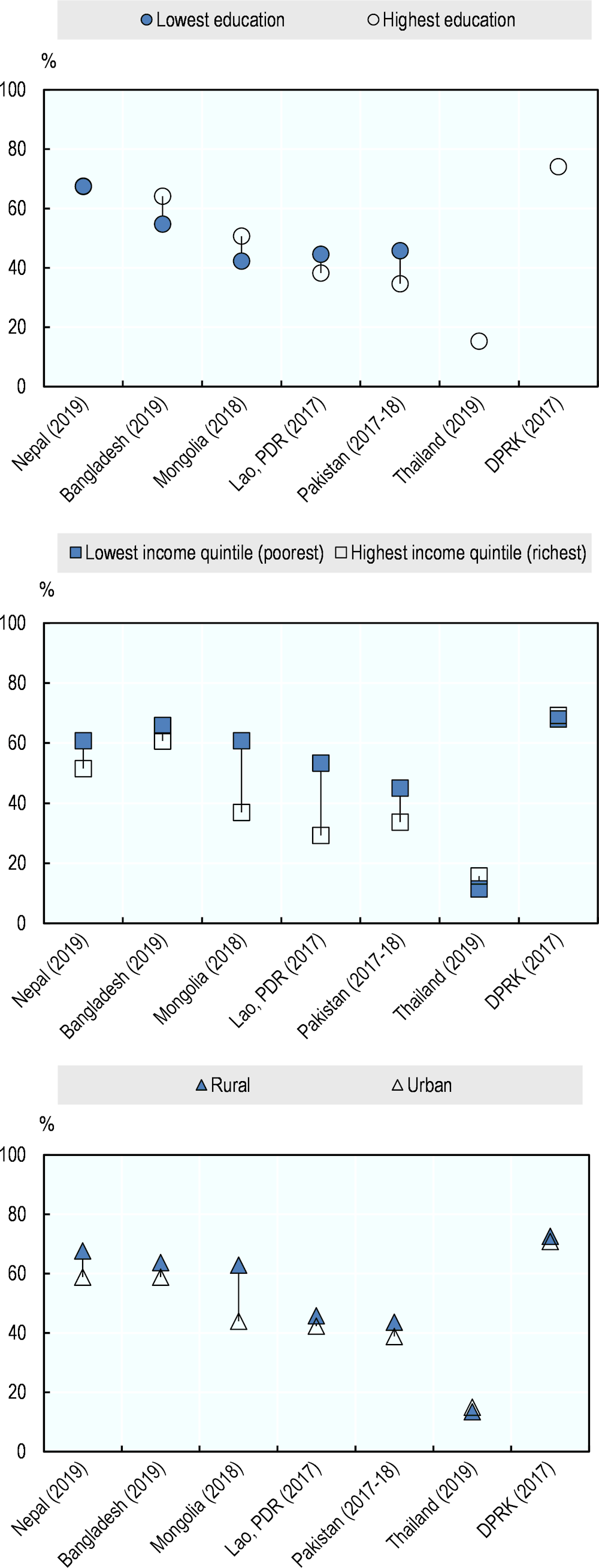
In Nepal, Bangladesh, Mongolia, Lao PDR and Pakistan, the rate of exclusive breastfeeding was higher amongst women living in households in the poorest income quintile as compared to women living in the richest households (Figure 4.5). Across countries and territories in Asia-Pacific, a higher level of education was not always associated with a higher rate of exclusive breastfeeding. While in Bangladesh and Mongolia women with the highest education level were much more likely to follow exclusive breastfeeding recommendations than those with the lowest education, the opposite trend was observed in countries and territories such as Lao PDR and Pakistan. In Mongolia, women living in rural areas are almost 50% more likely to breastfeed as compared to women living in urban areas.
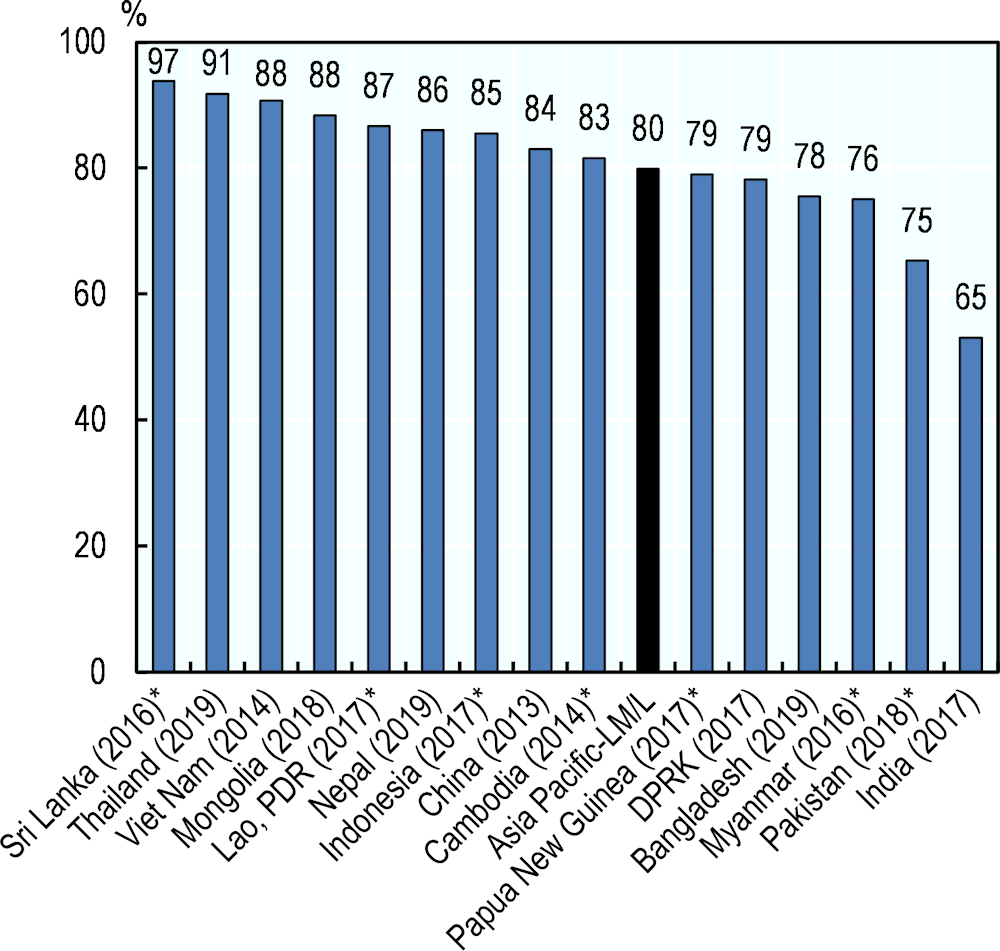
After the first six months of life, an infant needs additional nutritionally adequate and safe complementary foods, while continuing breastfeeding. Appropriate complementary foods were introduced to around half of the children between 6‑8 months in India, whereas complementary foods were introduced to more than nine out of ten infants in Sri Lanka, Thailand and Viet Nam (Figure 4.4).
Considering persisting high levels of childhood malnutrition (see indicator “Child malnutrition and overweight” in Chapter 4), infant feeding practices must be further improved (UNICEF, 2019[1]).