Cardiovascular disease is the major cause of death in Asia-Pacific, accounting for 35% of the total deaths in the region in 2019 (Zhao, 2021[1]). Ischaemic heart diseases and stroke were the two major causes of death in Asia-Pacific in 2019, accounting for 25.4% of total deaths in South-East Asia and 34.5% of all deaths in the Western Pacific region (Institute for Health Metrics and Evaluation, 2022[9]; indicator “Mortality from cardiovascular diseases” in Chapter 3). Additionally, both are associated with significant health, social and other non-financial costs, because of the persistent disabilities suffered by many survivors.
Quality, notably effectiveness of treatment following acute myocardial infarction (AMI) and stroke has improved significantly over the past decades. Until the 1990s, treatment focused on prevention of complications and rehabilitation but since then great improvements in AMI survival rates were achieved with thrombolysis (Gil et al., 1999[2]). Effectiveness of treatment for ischaemic stroke has also improved dramatically over the last decade, through early identification of suspected ischaemic stroke patients and timely acute reperfusion therapy. Countries can further improve quality of stroke care through timely transportation of patients, evidence‑based medical interventions and access to high-quality specialised facilities such as stroke units (OECD, 2015[3]). Due to COVID‑19, however, access to high-quality care was hampered in some cases. In Hong Kong (China), for instance, there was an increase in the delayed access to high-quality care among patients suffering from AMIs during the early period of the pandemic because of hospitals following additional precautionary measures to prevent infection and/or patients fearing infection (Tam et al., 2020[4]).
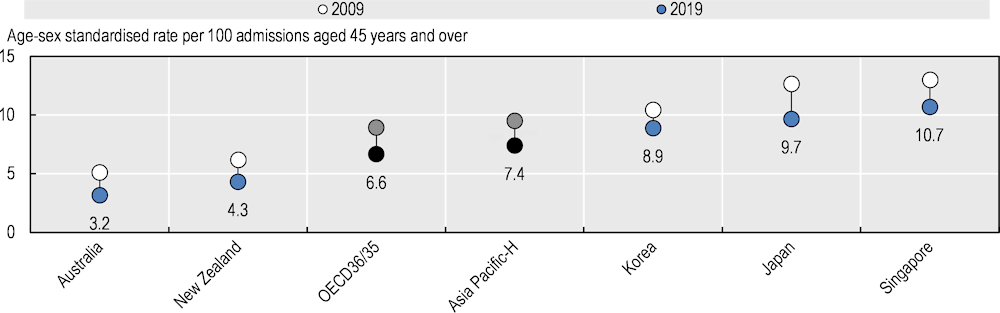
For both AMI and stroke, the case‑fatality rate is a useful measure of acute care quality, reflecting notably the effectiveness of medical interventions, including early thrombolysis or treatment with aspirin when appropriate, and catheterisation, as well as co‑ordinated and timely transport of patients. For AMI, age‑standardised in-hospital case‑fatality rates within 30 days of admission were low in Australia (3.2%) and New Zealand (4.3%) and high in Singapore (10.7%) in 2019 (Figure 7.4). The case‑fatality rate generally decreased over the past decade and the cross-country difference decreased over time. Beyond the quality of care provided in hospitals, differences in hospital transfers, average length of stay, emergency retrieval times and average severity of AMI and stroke may influence 30‑day case‑fatality.
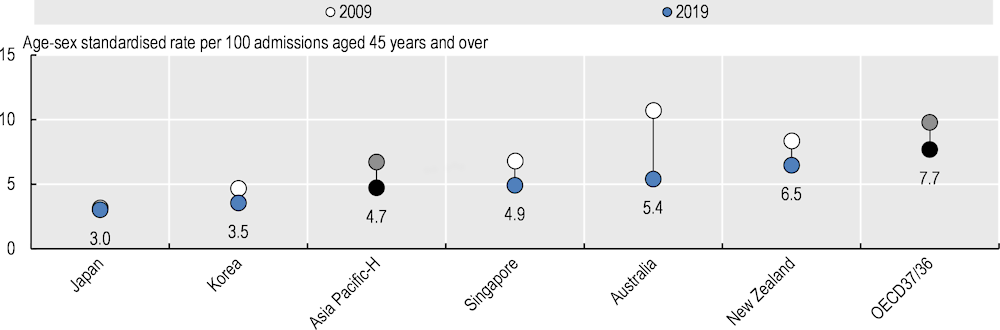
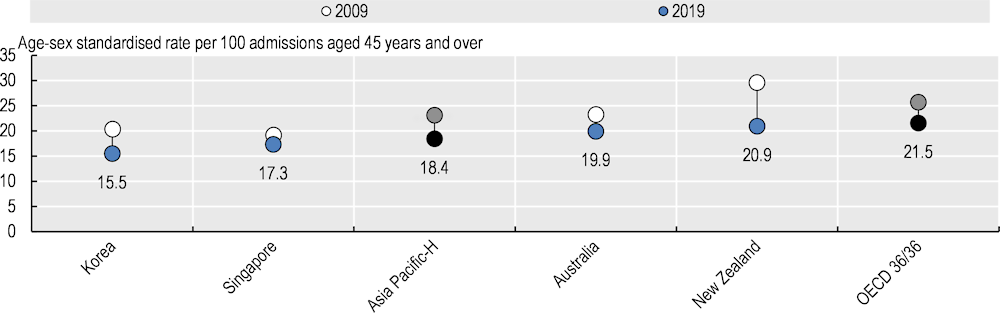
For ischemic stroke, the lowest case‑fatality rates were reported in Japan (3.0%) and Korea (3.5%), while New Zealand reported the highest rate of 6.5% (Figure 7.5). Fatality rates for haemorrhagic stroke are significantly higher than for ischemic stroke for all countries, and countries that achieve better survival for one type of stroke also tend to do well for the other. The lowest case‑fatality rates for haemorrhagic stroke were reported in Korea (15.5%), with New Zealand reporting the highest rate of 20.9% (Figure 7.6). Given the initial steps of care for stroke patients are similar, this suggests that system-based factors play a role in explaining the differences across countries. Low rates in Japan are due in part to recent efforts dedicated to improving the treatment of stroke patients through systematic blood pressure monitoring, major material investment in hospitals and establishment of stroke units (OECD, 2015[5]).
National measures for AMIs and stroke are affected by within-country variations in performance at the hospital level. Reducing this variation is key to providing equitable care and reducing overall mortality rates. Although monitoring and reporting of hospital-level performance is becoming increasingly important in Asia-Pacific, only Korea is regularly reporting hospital-level performance (OECD, 2019[6]). Multiple factors contribute to variations in outcomes of acute care, including hospital structure, processes of care and organisational culture. Recent research points to higher total numbers of hospital patients as being significantly related to higher performance; this may support national movements towards concentration of care services (Lalloué et al., 2019[7]).