The burden of breast cancer among women is significant in the Asia-Pacific region, where it is the cancer with the highest incidence and mortality rates in South-East Asia and the highest incidence and second highest mortality rates in Western Pacific region. In 2020, according to estimates based on pre‑pandemic trend, approximately 948 000 women were expected to be newly diagnosed with breast cancer and over 316 000 died of the disease in the region (International Agency for Research on Cancer (IARC), 2022[17]; see indicator “Mortality from cancer” in Chapter 3). Several factors are known to increase the risk of breast cancer, such as increasing age, genetic predisposition, oestrogen replacement therapy and lifestyle factors including obesity, physical inactivity, nutrition habits and alcohol consumption (World Cancer Research Fund/American Institute for Cancer Research, 2018[1]; González-Jiménez et al., 2014[2]).
In many Asia-Pacific countries, the incidence of breast cancer has increased over recent decades. Over recent decades, age‑standardised annual incidence rates per 100 000 women have risen quickly in China, India, Japan and Korea (IARC, 2022[3]) and the rates reached over 75 per 100 000 women in Japan and Singapore and about 65 per 100 000 women in Fiji and Korea in 2020. Incidence rates were already high (over 90 per 100 000 women) in Australia and New Zealand, where they have increased more slowly in recent years (IARC, 2022[4]).
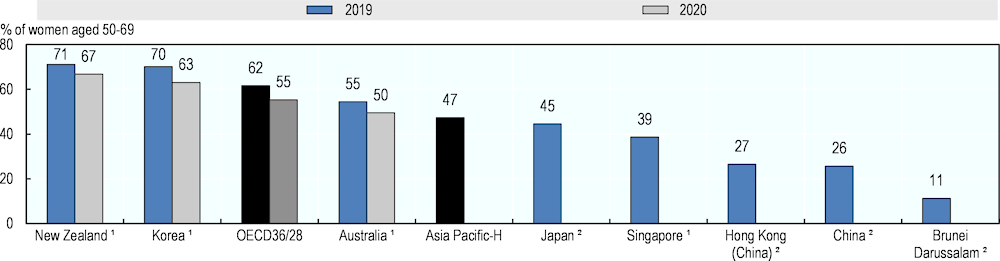
In the 1990s, Australia, Japan and New Zealand introduced national breast cancer screening programmes to effectively detect the disease early and reduce mortality (OECD, 2013[5]; IARC, 2016[6]). This has contributed to higher proportions of women being diagnosed at an early stage, and in those countries, over 50% of women with breast cancer were diagnosed at an early stage of disease during 2010‑14 (OECD, 2021[7]). Korea and Singapore also introduced a national screening programme around 2000, while China introduced screening programmes at the community level in the late 2000s (IARC, 2016[6]). In 2015, Indonesia rolled out its screening programme nationally and the roll-out of breast cancer programmes is ongoing in Brunei Darussalam and Viet Nam (Wahidin, 2018[8]; Pham et al., 2019[9]; Ministry of Health Brunei Darussalam, 2020[10]). Most of these countries monitor effective implementation of breast cancer screening programme. Prior to the pandemic, mammography rate was high at above 70% in New Zealand and Korea while low at just over 10% in Brunei Darussalam. However, in 2020, the COVID‑19 pandemic disrupted breast cancer screening programmes in countries in Asia-Pacific (Figure 7.7; see Chapter 2 “The health impact of COVID‑19”).
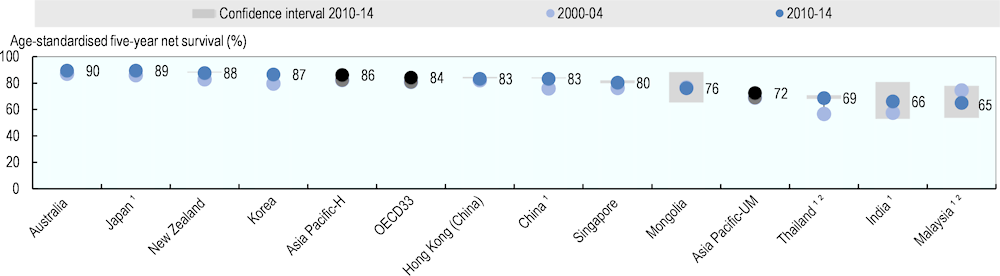
Cancer survival is one of the key measures of the effectiveness of health care systems in managing cancer, reflecting both early detection and the effectiveness of treatment. The wide range in age‑standardised five‑year net survival in Asia-Pacific countries and territories (Figure 7.8; Allemani et al., 2018[31]) suggests that the quality of breast cancer care varies widely in the region. For women diagnosed during 2010‑14, age‑standardised five‑year net survival was highest in high-income countries such as Australia and Japan (89.5% and 89.4%, respectively), whereas in Malaysia, India and Thailand, the probability that breast cancer patients survive their cancer for at least five years was less than 70%. In most Asia-Pacific countries and territories, five‑year net survival for women with breast cancer has improved in recent years, reflecting overall improvement in the quality of cancer care. China, India, Korea and Thailand in particular have seen a large improvement in five‑year net survival since 2000‑04.
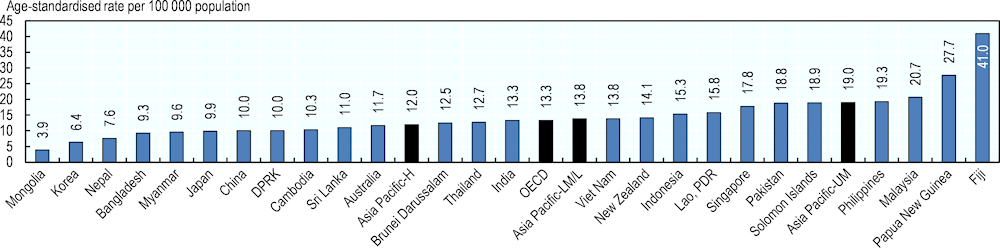
In 2020, mortality rates from breast cancer, reflecting effectiveness in early detection and treatment, and underlying trends in incidence, prevalence and survival, varied over ten‑fold between countries and territories in the Asia-Pacific region. The rate was lowest in Mongolia at 3.9 per 100 000 women and the highest in Fiji at 41.0 per 100 000 women. The average age‑standardised mortality rate was higher in upper-middle, lower-middle- and low-income countries than in high-income countries (Figure 7.9), although the pattern of incidence rates in the region was opposite.