In Asia-Pacific countries and territories, according to estimates based on pre‑pandemic trends, almost 462 000 people were expected newly diagnosed with oesophageal cancer and over 415 000 people died of it in 2020. Among all cancers, oesophageal cancer has the sixth highest incidence rates and fifth highest mortality rates in the region (IARC, 2022[1]). The risk is higher among men, and among people who smoke and drink alcohol.
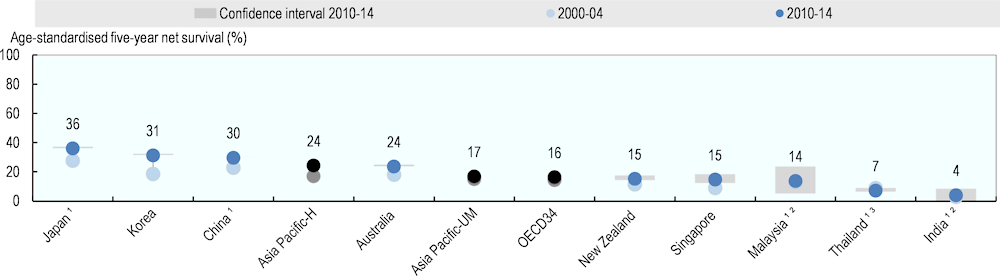
Age‑standardised five‑year net survival for oesophageal cancer, reflecting effectiveness in early detection and treatment, has improved in most countries in the region since the early 2000s. For adults diagnosed during 2010‑14, the highest five‑year net survival was in Japan (36.0%) and Korea (31.3%) and the lowest was in India (4.1%) and Thailand (7.1%) (Figure 7.13). Countries with population-based gastric screening programmes, such as Korea and Japan, have experienced substantial improvements over the past few decades, and now have the highest levels of oesophageal cancer survival worldwide. Prior to the COVID‑19 pandemic, mortality rates due to oesophageal cancer had also decreased in Australia, Japan, Korea, New Zealand and Singapore (IARC, 2022[2]). However, the pandemic may reverse these trends in some cases because emerging evidence points to an increased severity of oesophageal cancer among patients diagnosed during the early period of the pandemic (Okuyama et al., 2022[3]; Miyawaki et al., 2022[4]).
In 2020, over 37 000 people were expected newly diagnosed with melanoma of the skin and almost 12 000 people died of it in Asia-Pacific (IARC, 2022[1]). In 2020, incidence rates vary widely, from below 0.2 per 100 000 population in Viet Nam and Nepal and to over 30 per 100 000 population in Australia and New Zealand (IARC, 2022[1]). Melanoma of the skin is mainly caused by exposure to ultraviolet radiation, and people with a low level of skin pigmentation, a family history of the disease or poor immune function are at higher risk.
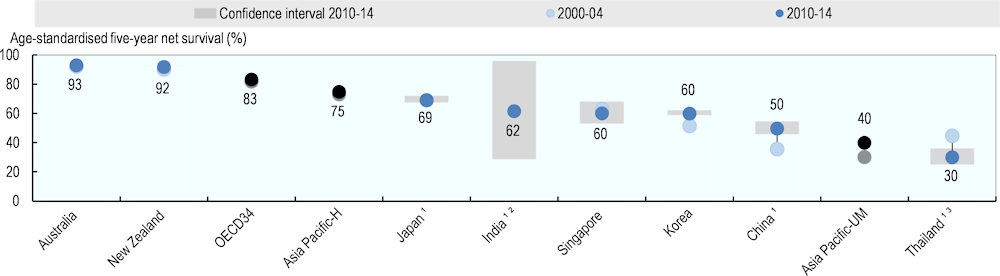
Age‑standardised five‑year net survival for melanoma of the skin ranges from 30% in Thailand to over 90% in Australia and New Zealand (Figure 7.14). In countries with high incidence rates, such as Australia and New Zealand, public health efforts have focused on raising awareness of the importance of recognition of the early symptoms of melanoma, helping to achieve the highest levels of survival. In some countries such as Singapore and Korea, a less favourable distribution of histologic sub-types – such as a higher proportion of nodular and acral lentiginous melanomas, which have a poorer prognosis – may also help to explain relatively low survival estimates (CONCORD Working Group, 2022[5]). Health policies targeting specific populations could help improve awareness, early diagnosis and access to treatment.
In recent years, net survival from melanoma of the skin has increased in most countries. Together with public health efforts, the introduction of immunotherapies and targeted treatments for metastatic melanoma has led to unprecedented clinical benefit and may have contributed to improving short-term survival (Di Carlo et al., 2020[6]). During the pandemic, dermatology units around the world rapidly adopted telemedicine and this may improve access to and outcomes of care if the quality of telemedicine is assured.
Leukaemia is the most common cancer among children aged 0‑14 and up to 86 000 children in Asia-Pacific region were expected newly diagnosed in 2020 (IARC, 2022[1]). The causes of leukaemia are not well known, but some known risk factors include inherited factors, such as Down syndrome and a family history of leukaemia, and non-inherited factors, such as exposure to ionising radiation. There are different types of leukaemia but about three‑quarters of cases among children are acute lymphoblastic leukaemia (ALL). The prognosis for leukaemia depends on various factors including age, initial white blood cell count, gender, initial reaction to induction treatment and type of leukaemia. Children with acute leukaemia who are free of the disease for five years are considered to have been cured, as remission after five years is rare.
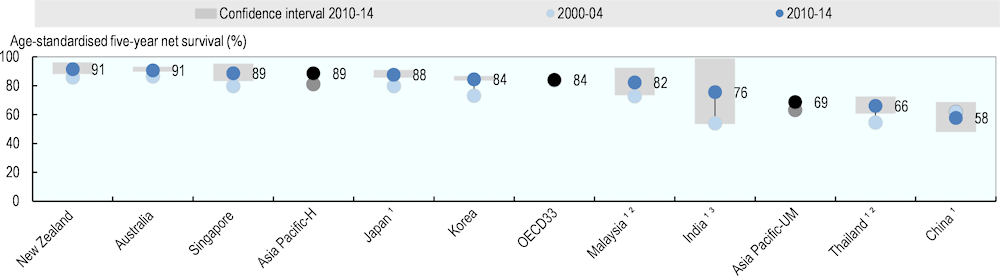
Age‑standardised five‑year net survival for ALL among children was on average 88.5% during 2010‑14 in high-income countries in Asia-Pacific and 68.6% in upper-middle‑income countries in the region (Figure 7.15) and net survival improved over the period across countries, mainly due to progress in chemotherapy and stem cell transplantation technology. Mortality due to leukaemia among children decreased across countries where data are available (IARC, 2022[2]). However, countries have not benefited equally from progress in medical technologies; while survival estimate is high at 91% in New Zealand and Australia, it is low at 58% in China.