This section reviews the indicator selection process and criteria applied to populate the HSPA framework (Section 4.1). The list of indicators selected and suggested for the first the Czech HSPA implementation is provided in Section 4.2. More details on indicators within each domain and subdomain, including information on possible data disaggregation, indicator methodologies, data sources, data custodians, and indicator custodians is provided in Annex D.
Health System Performance Assessment Framework for the Czech Republic

4. Populating the HSPA framework with indicators
4.1. Indicator selection process and criteria
The selection of indicators for populating domains relies on two main concepts 1) the meaningfulness of the indicator for performance assessment and 2) quality of underlying data and feasibility of measurement. A balance must be reached between the conceptual relevance of indicators and the practical possibilities for measuring and reporting on the selected indicators (Figure 4.1). Not all selected indicators must be fully feasible and usable at the moment of the design of the HSPA – some may be aspirational – but conisation should be given to the commitment and capacity to develop and operationalise these indicators as part of the HSPA implementation plan.
For the purposes of the Czech HSPA, selection criteria for indicators also included an assessment of health system strategic priorities and goals dimensions (e.g. efficiency, resilience, access, person-centredness, and quality of care) and desired performance sub-dimensions. Other considerations included the feasibility of reporting on the indicators, the validity and reliability of selected indicators, and applicability for international benchmarking. In the final selection process, a third aspect was also considered – indicators selected for a specific domain or subdomain were assessed as a group. The criteria applied focused on whether the selected indicators as a group describe the (sub)domain in its entirety. In other words, a group of excellent, relevant indicators calculated from reliable data may not be enough if those indicators describe the given domain, or subdomain, only in part and not entirely. In such case, discussions were held in the principal working group on enlarging the indicator group by another existent or placeholder indicator to capture the full scope of a (sub)domain.
Figure 4.1. Trade‑off considered in HSPA indicator selection
Source: The Netherlands HSPA Development.
Box 4.1. International experience with selecting HSPA indicators
Countries have taken different approaches in the selection of indicators to populate their HSPAs during the development process. Malta scored indicators on three criteria: 1) importance 2) feasibility and 3) scientific soundness. The importance criteria accounted for 40% of the score, and the other two criteria accounted for 30% each. Indicators scoring above 60% were considered for inclusion. In Latvia, indicators were scored on value (usability to assess a benchmark/goal) and ability to assess trends. Ireland also assessed indicators on two main dimensions: fit for purpose (alignment to HSPA functions) and if they are fit for use (measurable and methodologically robust).
In Slovenia, indicator selection was achieved via a consensus development process. Indicator performance is then combined with 0‑3 “Importance score” in reporting. The Netherlands also used a consensus development process, looking at both the healthcare system’s objectives to determine the indicator domains and relevant indicators to be used, while at the bottom the data sources and scientific state of the art determine the data availability and reliability to populate indicators.
The discussion on potential indicators for the Czech HSPA was launched in the working group during its 5th workshop in April 2022, after the first draft of HSPA framework was developed. The discussion has benefitted from an overview of health data availability and data and information flow landscape in the Czech Republic, prepared as a meeting background document by the OECD team; an overview of the Czech health data custodians is provided in Annex E. First ideas on possible indicators were collected from the break-out group brainstorming on possible indicators during this workshop.
Following the first draft of HSPA report, multiple technical focus groups were held to discuss data availability and possible indicators in particular domains in detail, with the OECD team providing international expertise and knowledge inputs into the national experts’ discussion; for an overview of technical focus groups see Annex C.
As an initial step for the indicator selection process, a long list of more than 1 400 indicators was composed at the Ministry of Health. The list included indicators reported and published by the main health data custodians in the Czech Republic; indicators reported by the Czech Republic to international databases such as Eurostat and OECD; indicators published by international organisations and projects based on nationally submitted data (such as the OECD’s Potential years of life lost, and SHARE survey results); indicators featuring in the Czech health sector strategic documents; and indicators developed as placeholders from the various technical discussions held during this project.
Due to the nature and process of collecting indicators for the long list, some indicators were featuring more than once on the list (drawn from multiple sources) or provided different granularity and/or measuring units for the same data. Hence, the long list was shortlisted by the project management team to approx. 400 indicators. The shortlist was created mainly by removing duplications and by grouping similar and overlapping indicators together under one indicator name. Furthermore, priority was given to indicators reflecting national health system strategic priorities and goals, the availability and feasibility of indicator reporting, the validity and reliability of primary data, and the applicability of international benchmarking.
Majority of those indicators were already in use, regularly reported to Eurostat, OECD, or other international organisations.
The shortlist of approx. 400 indicators was sent to members of principal working group. The members were given several votes in each subdomain that they could use to select indicators that would – in their view – serve the best the purpose of HSPA (Table 4.1). They were asked to assess both the fit-for-use of each individual indicator and the fit-for-purpose of individual indicators as well as the group of indicators that they choose to vote for in each subdomain.
Table 4.1. Number of votes by subdomains assigned in the indicator scoring exercise
|
Domain |
Subdomain |
No of votes assigned for the scoring exercise |
|---|---|---|
|
Health Status |
Avoidable mortality |
2 |
|
Health Status |
Burden of disease |
6 |
|
Health Status |
Experienced health |
2 |
|
Health Status |
Life expectancy |
7 |
|
Health Risks |
Diet, nutrition |
2 |
|
Health Risks |
Environmental Risks |
2 |
|
Health Risks |
Physical exercise |
2 |
|
Health Risks |
Habits |
4 |
|
Access |
Financial access |
2 |
|
Access |
Geographical access |
2 |
|
Access |
Waiting times |
2 |
|
Quality |
Care appropriateness |
6 |
|
Quality |
Clinical effectiveness |
4 |
|
Quality |
People‑centredness |
2 |
|
Quality |
Safety |
3 |
|
Financial Stability |
4 |
|
|
Integrated care delivery |
Continuity of care |
2 |
|
Integrated care delivery |
Coordination of care |
2 |
|
Integrated care delivery |
Long term care |
2 |
|
Integrated care delivery |
Prevention |
6 |
|
Cost-effective care delivery |
6 |
|
|
Equitable care delivery |
2 |
|
|
Workforce |
Capacity |
6 |
|
Workforce |
Future needs |
2 |
|
Workforce |
Shortage |
2 |
|
eHealth and Technologies |
Health information infrastructure |
3 |
|
eHealth and Technologies |
R&D and health technologies |
1 |
|
Financing |
7 |
|
|
Resilience |
7 |
Note: The votes were assigned to domains and subdomains according to the draft the Czech HSPA framework as of February 2023. Small adjustments were yet made to the HSPA framework following the results of the indicator scoring exercise and the subsequent expert consultations.
Source: The Czech HSPA project, February 2023.
The total of 24 experts from 16 institutions participated in the indicator scoring exercise, representing healthcare providers (26%), patients (10%), the system view (42%), and health insurance funds (21%). The votes assigned by individual experts were weighted to account for the fact that various stakeholder groups (e.g. patients vs providers) were not equally represented. The choice of indicators across domains was surprisingly unanimous among stakeholder groups, which made the pre‑final selection of indicators largely consensual.
The results of stakeholder voting were presented back to the principal working group for feedback and further discussion during workshops 7 and 8 (held in March 2023), providing detailed discussion on each individual selected indicator as well as on the (sub)domain’s indicator entirety. A few ideas and suggestions came up during those workshops, which led to further refinement of the HSPA framework and to withholding some indicators and adding few others. The list of 119 indicators was sent for review to the main the Czech data custodians and individual consultations of HSPA project management team were then held with representatives of institutions that shall be the indicator custodians of most of the HSPA indicators. In-depth discussions were held with CZSO, National Institute for Public Health, and UZIS. Various data sources were considered for indicators with data source options, sometimes an indicator was replaced by a similar yet more relevant one; in some cases, an indicator was excluded for known problems with primary data validity. The final list of 122 indicators was sent to the principal working group for a final review and presented during the last principal working group meeting in April 2023.
Figure 4.2. Indicator selection process to populate the Czech HSPA framework
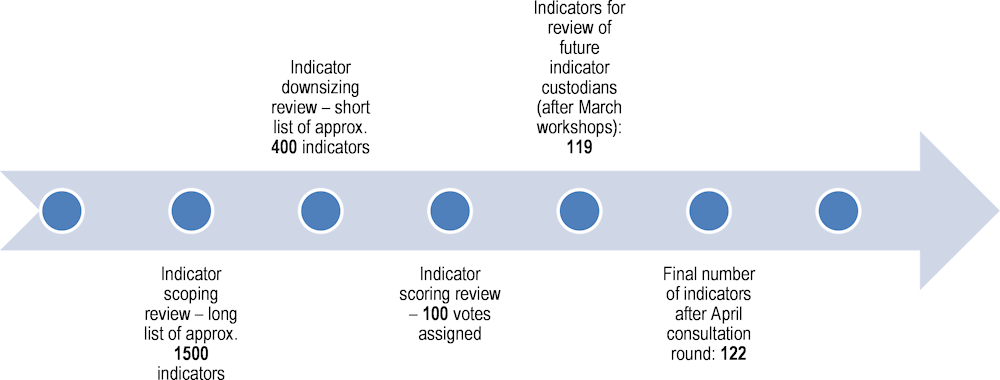
Source: The Czech HSPA project.
4.2. Indicators selected for the Czech HSPA
In total, 122 indicators were chosen to populate the Czech HSPA framework. The choice was made through the iterative process of consultations with the working group’s members. This process benefited from the scoping and the scoring exercise as described in Section 4.1 above. As the emphasis was put on data availability, most of the indicators come from existing sources and are ready to be implemented for the first round of the HSPA in the Czech Republic. However, some 32 other indicators are placeholders, where further development is needed. These are of two types. Primary data may be already existent (are collected), but there is not yet a clear consensus on the indicator methodology. Or, alternatively, an indicator has been inspired by an existing indicator methodology in another country or international organisation and its methodology needs to be localised to the Czech content and data availability requires checking and/or further development. Figure 4.3 presents the numbers of indicator in each framework domain and subdomain.
Figure 4.3. The final number of indicators per (sub)domain in the Czech HSPA framework
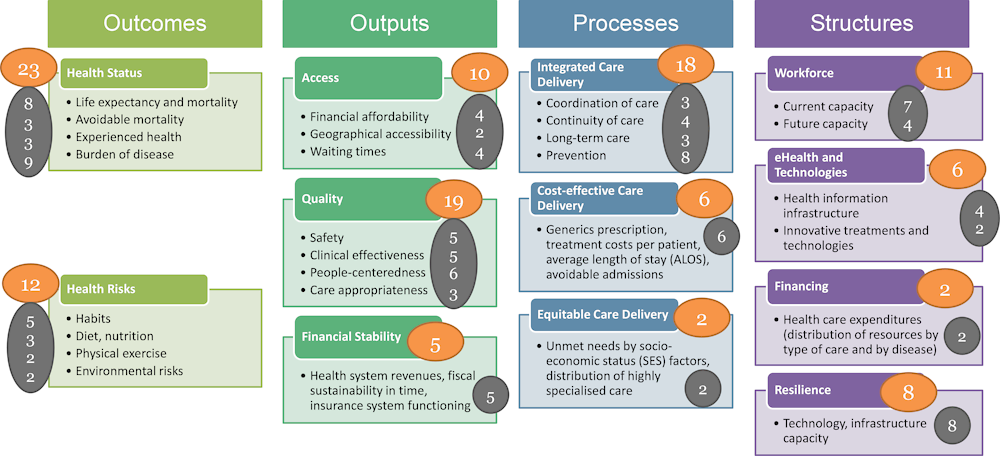
Note: Number of indicators for domains are in yellow circles, number of indicators for subdomains are in grey circle.
Source: The Czech HSPA project.
The Table 4.2 presents the list of selected indicators by the 12 HSPA framework domains and the 28 subdomains. For each indicator, information is provided on the domain, subdomain and indicator title. Detailed information on indicators is provided in Annex D. Indicators were selected to reflect the scope and depth of individual domains but also to reflect ongoing health-reforms or to shed light on existing problems – such as the state of mental health, financial affordability of dental care, progress in e‑health and others. The list of indicators selected during this project shall serve as an input for the next HSPA implementation phase. Further discussions among HSPA stakeholders, mainly the data custodians and suggested indicator custodians, are foreseen and deemed appropriate to develop detailed technical sheets for each individual indicator (see Section 6.2).
Annex D provides detailed information on indicators per framework domains. For each domain, a summary of selected indicators is provided together with a dedicated table. This table includes information on each indicator’s possible data disaggregation, possible benchmarking (international, regional, and time series, if available), indicator methodology, primary data source, data custodian, and indicator custodian. Primary data source can be health insurance administrative data (claim data from providers, custodied by the UZIS in the National Registry of Reimbursed Health Care, NRHZS), clinical or population registry data, and various reporting and survey data. In the last case, name of the survey is also provided. Data custodian indicates the institution, which is responsible for collecting the data and its custody, whereas indicator custodian is the institution responsible for contextualising and interpretation of the indicator within the Czech HSPA. In many cases, data custodian and indicator custodian is the same institution, while in other the data and indicator custodians differ.
In certain cases when alternatives exist, decision has yet to be taken on the choice of the data source, which will have a direct impact on the possible indicator disaggregation. Discussions during the HSPA implementation phase are foreseen for instance on the selection of survey data versus administrative (claim) data for particular indicators. While the former allows for socio‑economic status disaggregation, the latter are more accurate and allow for regional comparison. Similarly, in case of some other indicators further discussions are to be held on the use of international versus national survey results.
Table 4.2. List of proposed indicators for the Czech HSPA
The list of proposed indicators is the result of iterative consultation process held with the Principal Working Group members and other experts and the indicator scoping and the scoring exercise and shall serve as an input to the HSPA implementation phase.
|
Domain |
Subdomain |
Indicator name |
Indicator status |
|---|---|---|---|
|
Health Status |
Life expectancy |
Life expectancy at birth, by gender (Years) |
Existent |
|
Health Status |
Life expectancy |
Healthy life years at birth, by gender (Years) |
Existent |
|
Health Status |
Life expectancy |
Life expectancy, by gender (Years) |
Existent |
|
Health Status |
Life expectancy |
Healthy life years at 65, by gender (Years) |
Existent |
|
Health Status |
Life expectancy |
Main causes of mortality (%) |
Existent |
|
Health Status |
Life expectancy |
Peri-neonatal mortality by age of mother, by residence and occurrence (hlth_cd_aperro) |
Existent |
|
Health Status |
Life expectancy |
Mortality from circulatory diseases (specific disease rate per 100 000 population (age‑standardised)) |
Existent |
|
Health Status |
Life expectancy |
Cancer mortality by cancer site (%) |
Existent |
|
Health Status |
Avoidable mortality |
Preventable causes of mortality (number of deaths) |
Existent |
|
Health Status |
Avoidable mortality |
Treatable causes of mortality (number of deaths) |
Existent |
|
Health Status |
Avoidable mortality |
Potential Years of Life Lost (PYLL) |
Existent |
|
Health Status |
Experienced health |
Limitations due to health reasons (EU-SILC) |
Existent |
|
Health Status |
Experienced health |
Self-perceived health by sex, age and degree of urbanisation (hlth_silc_18) |
Existent |
|
Health Status |
Experienced health |
Patient reported outcome measures based on the PaRIS project |
Placeholder |
|
Health Status |
Burden of disease |
Multiple chronic diseases among people aged 65 and over, by gender (% people aged 65 and over with at least two chronic diseases) (SHARE) |
Existent |
|
Health Status |
Burden of disease |
Standardised trend of causes of hospitalisation per 100 000 inhabitants |
Existent |
|
Health Status |
Burden of disease |
Prevalence of (selected) chronic diseases and disabilities (EHIS) |
Existent |
|
Health Status |
Burden of disease |
Prevalence of diabetes (% of population aged 15 and over) |
Existent |
|
Health Status |
Burden of disease |
People with health disabilities by gender and age and by the help of another person |
Existent |
|
Health Status |
Burden of disease |
Share of adults at risk of depression (% of population aged 18+ at risk of depression) |
Existent |
|
Health Status |
Burden of disease |
Limitations in daily activities among people aged 65 and over (% people aged 65 and over) (SHARE) |
Existent |
|
Health Status |
Burden of disease |
Comorbidity index by UZIS (the share of population with high comorbidity index based on administrative data) |
Existent |
|
Health Status |
Burden of disease |
Incapacity to work (number per sick-insured population and/or average sick leave length) (sick leaves due to illness, CZSO data) |
Existent |
|
Health Risks |
Habits |
Number of deaths by risk factors |
Existent |
|
Health Risks |
Habits |
Smoking |
Existent |
|
Health Risks |
Habits |
Alcohol consumption |
Existent |
|
Health Risks |
Habits |
Estimate of cardio-vascular risks |
Existent |
|
Health Risks |
Habits |
Health literacy |
Placeholder |
|
Health Risks |
Diet, nutrition |
Metabolic syndrome |
Existent |
|
Health Risks |
Diet, nutrition |
Body mass index (BMI) by sex, age and country of birth (hlth_ehis_bm1b) |
Existent |
|
Health Risks |
Diet, nutrition |
Frequency of drinking sugar-sweetened soft drinks by sex, age and body mass index (hlth_ehis_fv7m) |
Existent |
|
Health Risks |
Physical exercise |
Effort involved in performing work-related physical activity by sex, age and degree of urbanisation (hlth_ehis_pe1u) |
Existent |
|
Health Risks |
Physical exercise |
Performing (non-work-related) physical activities by sex, age and degree of urbanisation (hlth_ehis_pe3u) |
Existent |
|
Health Risks |
Environmental risks |
Premature deaths due to air pollution PM2.5 (rate per 100 000 population) |
Existent |
|
Health Risks |
Environmental risks |
Monitoring: air pollution, drinking and bathing water pollution, community noise, contaminants in food chains and dietary exposures, human biomonitoring, occupational health hazards |
Existent |
|
Access |
Financial affordability |
% reporting unmet medical needs by income |
Existent |
|
Access |
Financial affordability |
Out-of-pocket spending on health as share of final household consumption (%) |
Existent |
|
Access |
Financial affordability |
Share of households with catastrophic health spending by consumption quintile (% of all households) |
Placeholder – methodology exists |
|
Access |
Financial affordability |
Household out-of-pocket spending by type of expenditures (e.g. pharmaceuticals, hospitalisations, outpatient care, dental) |
Existent |
|
Access |
Geographical accessibility |
Average number of patients registered with a GP, by region |
Placeholder – data exists |
|
Access |
Geographical accessibility |
Share of patients for whom primary care is accessible within a geographical limit |
Placeholder – data exists |
|
Access |
Waiting times |
Waiting time of more than two weeks to get an appointment with a specialist (% of population asking an appointment) |
Placeholder |
|
Access |
Waiting times |
Unmet needs for dental examination due to financial, geographic, or waiting time reasons (% of unmet needs) |
Existent |
|
Access |
Waiting times |
Waiting time for a first face‑to-face contact in an outpatient mental health care centre |
Placeholder |
|
Access |
Waiting times |
Share of patients for whom primary care is accessible within a geographical limit |
Placeholder – data exists |
|
Quality |
Safety |
Prevalence of healthcare‑associated infections (% of patients hospitalised) |
Existent |
|
Quality |
Safety |
Number of hospitals monitoring prevalence of bloodstream infections based on ECDC |
Existent |
|
Quality |
Safety |
Share of selected microorganism resistance based on the EARS-NET methodology |
Existent |
|
Quality |
Safety |
Prevalence of hospital-acquired cat II-IV pressure ulcers (% of patients hospitalised) |
Existent |
|
Quality |
Safety |
Falls in hospitals |
Existent |
|
Quality |
Clinical effectiveness |
Case fatality within 30 days after admission for AMI (pop aged 45+, linked data, percentage) |
Existent |
|
Quality |
Clinical effectiveness |
Case fatality within 30 days after admission for ischaemic stroke (pop aged 45+, linked data, percentage) |
Existent |
|
Quality |
Clinical effectiveness |
Cancer survivals – percentage share by age, sex, and type |
Existent |
|
Quality |
Clinical effectiveness |
Set of indicators on quality of care for patients with stroke |
Existent |
|
Quality |
Clinical effectiveness |
Patients with cancer reviewed by multidisciplinary diagnostic team (% of newly diagnosed cancer patients) |
Existent |
|
Quality |
Care appropriateness |
Datasets on antibiotics use |
Placeholder – under development |
|
Quality |
Care appropriateness |
Caesarean section rate (per 1 000 live births) |
Existent |
|
Quality |
Care appropriateness |
Use of antidepressants (total DDD/1 000 pop/day) |
Placeholder |
|
Quality |
Care appropriateness |
Proportion of adult diabetics with appropriate follow-up (% of diabetic patients under insulin) |
Placeholder |
|
Quality |
Care appropriateness |
Patients who received palliative care (% of terminal cancer patients who died in the year) |
Placeholder – methodology exists |
|
Quality |
Care appropriateness |
Self-reported use of non-prescribed medicines by sex, age and educational attainment level (hlth_ehis_md2e) |
Existent |
|
Quality |
People‑centredness |
Doctor providing easy-to understand explanations (%) |
Placeholder |
|
Quality |
People‑centredness |
Average rating of healthcare providers in the patient satisfaction survey |
Placeholder – data exists |
|
Quality |
People‑centredness |
Patient reported experience measure based on the PaRIS project |
Placeholder |
|
Financial Stability |
Total revenues of statutory health insurance |
Existent |
|
|
Financial Stability |
Total expenditures of statutory health insurance system |
Existent |
|
|
Financial Stability |
Health expenditure from public sources as share of total health spending (%) |
Existent |
|
|
Financial Stability |
Health expenditure as a share of GDP (% GDP) |
Existent |
|
|
Financial Stability |
Ratio of health insurance funds’ reserves to current expenditure |
Existent |
|
|
Integrated care delivery |
Coordination of care |
Avoidable hospital admissions (diabetes, COPD, CHF, hypertension) |
Existent |
|
Integrated care delivery |
Coordination of care |
Use of emergency care within 5 days after the last visit (after discharge or after outpatient visit) |
Placeholder – data exists |
|
Integrated care delivery |
Coordination of care |
Ratio of GP-registered and GP-nonregistered patients using emergency and out-of-hours care |
Placeholder – data exists |
|
Integrated care delivery |
Continuity of care |
Patient outcomes one year after discharge from stroke and heart failure (crude rate per 100 people) |
Existent |
|
Integrated care delivery |
Continuity of care |
Time from a positive screening for a certain cancer type to treatment |
Placeholder |
|
Integrated care delivery |
Continuity of care |
Timespan between two episodes of care that should follow one another (according to clinical guidelines) |
Placeholder – data exists |
|
Integrated care delivery |
Continuity of care |
General practitioner encounter within 7 days after hospital discharge (% patients 65+) |
Placeholder – data exists |
|
Integrated care delivery |
Long term care |
Long-term care in residential facility (% pop aged 65+) |
Placeholder |
|
Integrated care delivery |
Long term care |
Long-term home nursing care (% pop aged 65+) |
Placeholder |
|
Integrated care delivery |
Long term care |
Polypharmacy among the elderly (5 or more drugs of >80 DDD per year) (% of insured population 65+) |
Placeholder – data exists |
|
Integrated care delivery |
Prevention |
Number of patients attending regular GP check-up |
Existent |
|
Integrated care delivery |
Prevention |
Number of patients attending regular dental check-up |
Existent |
|
Integrated care delivery |
Prevention |
Colorectal cancer screening (% of people screened) |
Existent |
|
Integrated care delivery |
Prevention |
Breast cancer and cervical cancer screenings (hlth_ps_scre) |
Existent |
|
Integrated care delivery |
Prevention |
Vaccination against influenza, people aged 65 (% of people) |
Existent |
|
Integrated care delivery |
Prevention |
Childhood mandatory vaccination |
Existent |
|
Integrated care delivery |
Prevention |
HPV vaccination |
Existent |
|
Integrated care delivery |
Prevention |
% of cancer diagnosed at early stage |
Existent |
|
Cost-effective care delivery |
Healthcare expenditures from SHI by ICD‑10 chapters, by sex by 1 inhabitant |
Existent |
|
|
Cost-effective care delivery |
One‑day surgical admissions (% of surgical admissions) |
Existent |
|
|
Cost-effective care delivery |
ER visits for social, mental or psychic reason (% of admission in ER in general hospitals) |
Placeholder |
|
|
Cost-effective care delivery |
Distribution of the number of hospitalisations according to duration and ICD‑10 chapters |
Existent |
|
|
Cost-effective care delivery |
Hospitalisation and average length of treatment by age group |
Existent |
|
|
Cost-effective care delivery |
Use of low-cost medication (% of total ambulatory DDDs) |
Placeholder |
|
|
Equitable care delivery |
Self-reported unmet needs for medical examination by sex, age, main reason declared and income quintile (hlth_silc_08) |
Existent |
|
|
Equitable care delivery |
Self-reported unmet needs for dental examination by sex, age, main reason declared and degree of urbanisation (hlth_silc_22) |
Existent |
|
|
Workforce |
Current capacity |
Physicians by sex and age (hlth_rs_phys) |
Existent |
|
Workforce |
Current capacity |
Health workforce migration (hlth_rs_wkmg) |
Existent |
|
Workforce |
Current capacity |
Practising doctors per 1 000 population |
Existent |
|
Workforce |
Current capacity |
Practising dentists per 1 000 population |
Existent |
|
Workforce |
Current capacity |
Practising nurses per 1 000 population |
Existent |
|
Workforce |
Current capacity |
Share of labour costs due to overtime / contracted working hours / total HR costs |
Placeholder |
|
Workforce |
Current capacity |
Patient-to-nurse ratio |
Placeholder |
|
Workforce |
future capacity |
Medical graduates (per 100 000 population) |
Existent |
|
Workforce |
future capacity |
Nursing graduates (per 100 000 population) |
Existent |
|
Workforce |
future capacity |
Nurses aged 50+ (% of those professionally active) |
Existent |
|
Workforce |
future capacity |
% of physicians aged over 60, or 65, based on [physicians by sex and age (hlth_rs_phys)] |
Existent |
|
eHealth and Technologies |
Health information infrastructure |
People searching health information online |
Existent |
|
eHealth and Technologies |
Health information infrastructure |
Share of providers who keep medical records solely in electronical form |
Existent |
|
eHealth and Technologies |
Health information infrastructure |
Percentage of physician practices that can share information with hospitals about patients’ current medications |
Placeholder |
|
eHealth and Technologies |
Health information infrastructure |
Share of providers who use e‑prescription for medical devices |
Placeholder |
|
eHealth and Technologies |
R&D and health technologies |
CT, MRI, and PET exams per 1 000 population |
Existent |
|
eHealth and Technologies |
R&D and health technologies |
State budget expenditures on R&D in healthcare |
Existent |
|
Financing |
Healthcare expenditure in the Czech Republic by type of care |
Existent |
|
|
Financing |
Healthcare expenditure in the Czech Republic by type of care per 1 inhabitant |
Existent |
|
|
Resilience |
Long-term care beds in nursing and residential care facilities by NUTS 2 regions (hlth_rs_bdsns) |
Existent |
|
|
Resilience |
Supply of ambulatory child- and adolescent mental health care |
Placeholder |
|
|
Resilience |
Existence of an early detection drug shortage mechanism |
Placeholder |
|
|
Resilience |
Primary care capacity |
Placeholder |
|
|
Resilience |
Hospital beds per 1 000 population |
Existent |
|
|
Resilience |
Occupancy rate of curative (acute) care beds (%) |
Existent |
|
|
Resilience |
Adult ICU occupancy rate (%) |
Existent |
|
|
Resilience |
Adult intensive care beds (per 100 000 population) |
Existent |
Source: The Czech HSPA project, April 2023.
For additional information:
Annex D: List of indicators populating the Czech HSPA framework.
Overview tables of individual indicators by subdomains, with details on data disaggregation availabilities, methodology, data sources, data custodians, and indicator custodians.
Infographics showing selected existing indicator and their possible disaggregation, benchmarking, and visualisation.
Annex E: Overview of the Czech health data custodians and data sources