The COVID-19 pandemic put enormous stress on health systems, forcing them to cope with an unknown pathogen while also continuing to deliver routine care and respond to acute care needs unrelated to the pandemic. This chapter assesses the impact of the COVID-19 crisis on health and on the health system in Belgium. It looks at the direct and indirect health impacts of the pandemic and the effectiveness of the health system’s response, with a particular focus on the impact of the pandemic on vulnerable groups.
Evaluation of Belgium’s COVID-19 Responses

4. The health systems response to COVID-19 in Belgium
Abstract
Key findings
A number of weaknesses in pandemic preparedness complicated Belgium’s response to the COVID-19 pandemic and led it to fare poorly during 2020, the first year of the pandemic. The adjusted increase in deaths in 2020 was more than twice the OECD average, indicating how hard the initial waves of the pandemic hit Belgium. The decision to dispose of and not replenish the strategic stockpiles of personal protective equipment prior to the pandemic, and differing rules around allocation to different parts of the health system, meant that some operators of critical infrastructure and essential health and social care services faced major shortages. Nursing homes were ill-equipped in terms of infection control expertise and often faced major problems sourcing key protective equipment. Moreover, the political situation at the outset of the pandemic, the multitude of often overlapping crisis structures set up to address the pandemic, and the lack of clearly assigned responsibilities meant that in practice crisis response channels were sometimes side-lined in favour of decisions made directly by a fairly small group of actors.
Older populations, especially those in nursing homes, and other vulnerable groups were particularly hard hit, particularly in the first year of the COVID-19 pandemic. Nearly half (45%) of all COVID-19 deaths in Belgium were among residents of nursing homes between early 2020 and September 2022. Nursing home residents, of which Belgium has a higher share than nearly all other OECD countries, comprised nearly three in five deaths (57%) in 2020. Belgium made several attempts to integrate the unique circumstances of vulnerable groups, such as homeless people and undocumented migrants, in its decision making, for example through representation of advocates in key crisis management bodies. However, their needs were not always prioritised particularly in the initial months of the crisis response. The severe impacts on these population groups and the major challenges encountered around certain basic pandemic preparedness measures, such as the procurement of personal protective equipment, underscore that Belgium could do much more to prepare proactively for future health crises, particularly for vulnerable populations.
Despite these shortcomings, the Belgian health system was able to respond fairly robustly to the challenges it faced from the COVID-19 pandemic and to adapt over the course of it, leading to an improved response in 2021 and 2022. Through March 2022, the direct health impact of COVID-19 in Belgium was lower than the OECD average and comparable to that of many neighbouring countries, with the average adjusted increase in deaths between 2020 and 2022 some 2.5% higher than the 2015-2019 period, compared with 5.3% higher across the OECD on average for the same period. Many of the measures taken by Belgium in responding to the crisis, such as the management of hospital capacity and the roll-out of the vaccination campaign, were broadly successful when compared with other OECD countries. Belgium incorporated lessons learned from the first two waves into its pandemic response, which resulted in a much better performance in 2021 and 2022 compared to 2020.
The pandemic holds several lessons learned to ensure that Belgium continues this path to prepare proactively for future health crises, particularly for vulnerable populations:
The indirect health impacts of the pandemic were serious, with delays in routine care and significant impacts on mental health, particularly for young and vulnerable populations, as well as certain professions.
Long COVID remains a concern for an important subset of people who contract COVID-19, with concerning implications not only for health but also employability and broader well-being.
The impact of the pandemic on the mental health of healthcare workers who were on the front lines of the crisis has been significant.
Despite the complexity of Belgium’s crisis response management, several of the health initiatives adopted to fight the virus were largely successful:
Belgium’s vaccination campaign was rolled out quickly and strategically, with identification and prioritisation of key vulnerable groups and good co-ordination between the federal government and federated entities. As of March 2022, nearly four-fifths (78%) of the total population had completed their vaccination protocol, a share higher than the OECD average and above the neighbouring countries of France, Germany, Luxembourg and the Netherlands.
A relatively high number of hospital beds, as well as a tightly organised hospital response, and the development of a multi-stage hospital contingency plan, helped prevent hospitals from becoming overwhelmed during the crisis.
Data was quickly collected to monitor the spread of COVID-19 and facilitate informed decision making, with a new data infrastructure for information from hospitals and nursing homes scaled up at the start of the crisis.
Belgium was able to address some workforce shortages exacerbated by the pandemic through a range of strategies, including support from medical and non-medical volunteers, the deployment of military personnel to some nursing homes and hospitals, and task shifting.
Care delivery approaches were adapted during and following the pandemic to help ensure access to, and continuity of, care:
Reimbursement for teleconsultations was quickly approved. While widely used, the take-up of teleconsultation services remains lower than many neighbouring countries.
New models of primary care delivery were harnessed to improve the co-ordination of care for both COVID-19 and non-COVID-19 patients and to identify patients particularly vulnerable to the impacts of COVID-19 and its mitigation measures.
Support for mental health services was expanded, with a scale-up in funding for mental health services and strengthening of primary-level mental health support.
Clinical pathways supporting care for long COVID have been introduced to improve the co-ordination of care around specific patient needs.
4.1. How hard hit was Belgium by COVID-19? The direct health impact of COVID-19
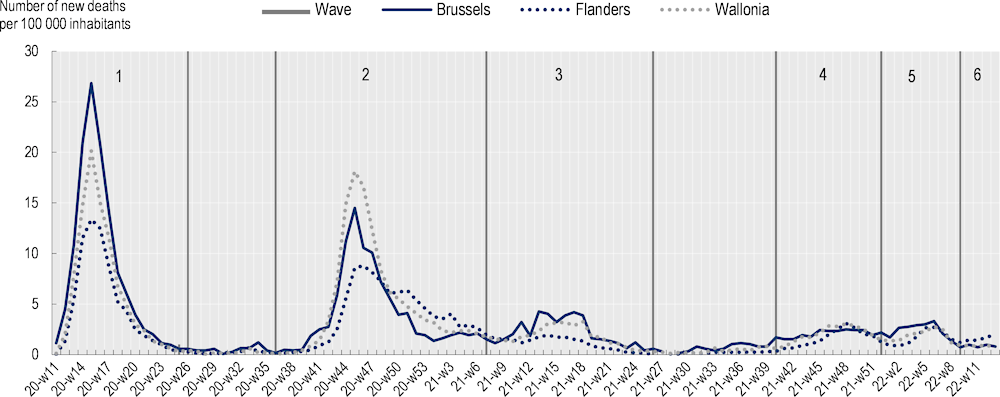
4.1.1. Belgium recorded its highest number of deaths in waves one and two
While Belgium’s first COVID-19 patient was detected on 4 February 2020 in an asymptomatic person returning from Wuhan (Renard et al., 2021[1]), a second case detected on 1 March 2020 marked the start of the pandemic in the country (Renard et al., 2021[1]). Over the period covered in this report, Belgium experienced six COVID-19 waves (Figure 4.1) and incurred a total of 30 811 COVID-19-related deaths between its first COVID-19-related death on 7 March 2020 and the end of March 2022: 4 073 deaths in Brussels, 11 122 deaths in Wallonia and 15 616 deaths in Flanders.
Waves one and two were by far the most severe in terms of mortality, accounting for 70% of total COVID-related deaths over the period from March 2020 to March 2022. The country recorded the highest number of daily deaths in wave one, with a total of 322 deaths on 8 April 2020, and the highest number of deaths per wave in the second wave, with a total of 11 949 COVID-19-related deaths (Peeters et al., 2021[2]; Bustos Sierra et al., 2021[3]).
Figure 4.1. Weekly new deaths per region per 100 000 inhabitants
From March 2020 to March 2022
In terms of absolute mortality, Belgium appeared as an outlier, with absolute cumulative mortality ranging far above that of many other countries in the initial months of the pandemic (Luyten and Schokkaert, 2021[6]). This can in part be attributed to a broader inclusion of deaths. In contrast to many other countries that initially only counted confirmed, in-hospital COVID-19 deaths, Belgium included both suspected COVID-19 deaths and deaths that occurred outside of hospitals in its mortality data from the start of the pandemic, as a way to limit underreporting of cases (Bustos Sierra et al., 2020[7]; Renard et al., 2021[1]).
4.1.2. The increase in mortality in Belgium was higher than in neighbouring countries in 2020 but lower than in most OECD countries in 2021 and 2022
During the pandemic – and particularly early in 2020 – many countries measured the relative and absolute impact of the pandemic in terms of the number of positive cases, hospitalisations due to COVID-19, and COVID-19-related deaths. While these measures were relatively straightforward to include in health information systems and are helpful for within-country analyses, international comparisons based on these measures are difficult to interpret, due to differences in identifying all COVID-19 related cases and deaths, different approaches and capacities to testing for COVID-19, and different practices in recording probable but not test-confirmed cases. A comparison of the overall number of deaths recorded in a period against a ‘baseline’ – the average number of deaths during the same period in recent years – can help to address many of these comparability challenges. This simple measure of ‘excess mortality’ provides a proxy for the overall impact of COVID-19. In looking at overall deaths, the impacts of the pandemic are captured not only through deaths directly linked to COVID-19, but those who may have been missed (for example, due to place of death or lack of testing) as well as deaths that could be linked to missed or delayed treatment due to the pandemic. This measure is particularly appropriate when undertaking international comparisons, where the measurement challenges highlighted above complicate direct comparisons of official COVID-19 cases and deaths.
There are a variety of approaches on how to measure excess mortality, using different underlying data, and calculating ‘expected’ deaths using different baseline periods, standardisations, and trends (Schöley et al., 2023[8]). Such methodological differences mean that there are differences in the magnitudes reported across different studies, as well as some challenges in interpreting their results. In common with other international studies, OECD estimates use an age-standardised mortality rate (ASMR) approach to take into account variations in population structure and size – that themselves impact mortality in a given country and over time – while still comparing against a historical baseline average. As such, they capture changes in overall mortality over time and between countries, rather than focusing explicitly on COVID-19-related mortality as some other models (such as that of WHO) have attempted to do. While there are differences in the estimates of excess mortality, other approaches to calculate the impact on mortality tend to arrive at similar results in term of relative levels and trends over time and between countries (Office for National Statistics, 2022[9]; Eurostat, 2023[10]). Using a more sophisticated modelled (extrapolated) mortality baseline would have led to a higher estimated excess mortality for countries where life expectancy was improving and all-cause mortality was declining prior to the pandemic, and can lead to slightly different relative country rankings.
Based on OECD estimates, the overall increase in mortality in Belgium for the period from 2020 to 2022 was below the OECD average, and lower than in its neighbouring countries of France, Germany, Netherlands, but higher than in Luxembourg (Figure 4.2) (OECD, 2022[11]; Morgan et al., 2023[12]). However, a closer examination throughout the different stages of the pandemic reveals great variation across the years, with a particularly high increase in mortality in Belgium in 2020, but lower than historical rates in both 2021 and 2022. The intensity of the first two COVID-19 waves in 2020 in Belgium led to a sharp increase in the number of deaths in 2020, with the mortality rate in 2020 (adjusted for population change1) being 11.8% higher compared to the pre-pandemic years (2015-2019), and more than twice that of the OECD average of 5.8%. In 2020, Belgium had the 9th highest excess mortality in the OECD, performing more poorly than all of its neighboring countries. However, following the sharp increase in 2020, mortality was 3.2% lower in 2021 and 1.2% lower in 2022 compared to the pre-pandemic years.
In Belgium’s neighbouring countries, the pattern over the pandemic years was mixed. Luxembourg experienced a pattern that was similar to that of Belgium, with higher mortality in 2020 but a lower mortality rate in both 2021 and 2022, compared to its 2015-2019 average. France and the Netherlands experienced their highest increases in mortality in 2020, but the rate remained higher than pre-pandemic years throughout the three years, and remained higher than pre-pandemic levels in 2021 and 2022. In Germany, the mortality rate was also above pre-pandemic levels throughout the three-year period, increasing in each year of the pandemic. Similar findings can be found for the impact of COVID-19 on life expectancy. Belgium and France recorded a reduction in life expectancy in the first year of the pandemic, and fully recovered in the following year, whereas Germany continued to see deteriorating life expectancy in 2021 compared to 2020 (Schöley et al., 2022[13]).
Within Belgium, all three regions experienced their highest increases in mortality in 2020. The mortality rate was 9.9% higher in Flanders, 13.8% higher in Wallonia, and 20.8% higher in Brussels in 2020, compared to their 2015-2019 averages. In contrast, mortality was lower across all three regions in 2021 (‑4.5% in Brussels, -3.4% in Wallonia, -2.8% in Flanders) and negative or effectively unchanged in 2022 (‑3.5% in Brussels, -2.2% in Wallonia, 0.3% in Flanders) compared to the 2015-2019 average.
It is important to reiterate that these estimates measure mortality patterns over annual and three-year periods. The continual tracking and dissemination of weekly data on deaths throughout the pandemic has shown that the variance is naturally of a much higher magnitude and that countries or regions may have experienced significant peaks in mortality that resulted in acute pressures on health systems and emergency services. The examination of average annual mortality rates does not reveal the variation in mortality on a weekly basis and the impact on health systems and society at specific times.
Figure 4.2. Change in the mortality rate for 2020-22 (compared to the period 2015-19), %
Age-standardised mortality rates (ASMR)
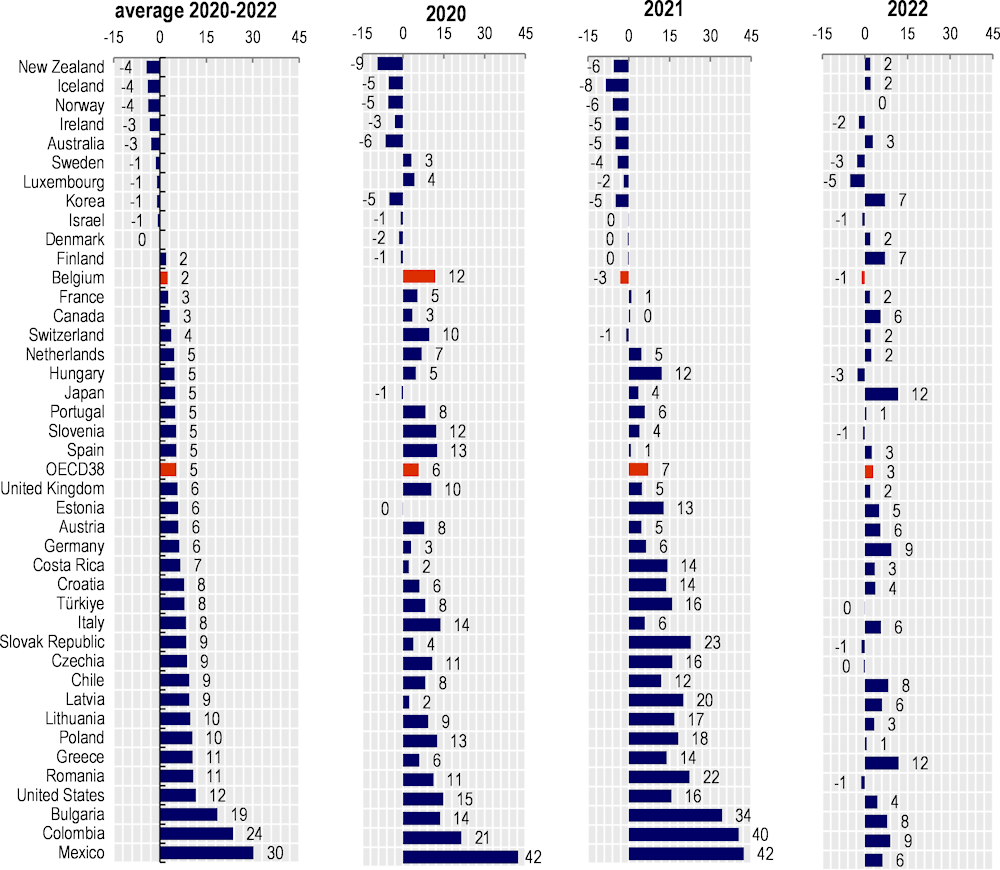
Note: Data refer to the age-standardised mortality rate (ASMR) method using 2015 OECD population structure. The bars represent the annual excess mortality for the average of 2020-2022 and for each of the years indicated compared to 2015-2019. Data are sorted based on increasing excess mortality for the average 2020-2022.
Source: Morgan, D., et al. (2023[12]), “Examining recent mortality trends: The impact of demographic change”, OECD Health Working Papers, No. 163, OECD Publishing, Paris, https://doi.org/10.1787/78f69783-en.
4.1.3. Like in other countries, older populations in Belgium made up the vast majority of COVID-19-related mortality
COVID-19 incidence rates and mortality were unevenly distributed. Older populations and people in nursing homes were disproportionally affected. Of the nearly 31 000 COVID-19-related deaths recorded in Belgium between the start of the pandemic and March 2022, 92% occurred among people aged 65 and above, with nearly half of all deaths affecting the population aged 85 and older (Sciensano, 2023[5]). While the uptake of COVID-19 vaccines dramatically reduced the death rate from the virus, including among older populations (who have recorded some of the highest levels of COVID-19 vaccination), the proportion of all COVID-19-related deaths impacting older populations has not changed substantially over the course of the pandemic. Indeed, 90% of deaths that occurred in the first quarter of 2022 took place among people 65 and older, including 46% among those 85 and above, compared to 92% and 48%, respectively, over the course of 2020 and 2021 (Sciensano, 2023[5]).
The proportion of deaths occurring in nursing homes and among nursing home residents was particularly severe during the first two waves of the pandemic. Between March 2020 and September 2022, nearly one-third (32%) of all COVID-19-related deaths in Belgium occurred in nursing homes, with nearly one in two (45%) deaths occurring among residents of nursing homes, irrespective of their place of death (Jurcevic et al., 2023[4]). In 2020, more than two in five (43%) deaths from COVID-19 occurred in nursing homes, and nursing home residents made up nearly three-fifths (57%) of all COVID-19 deaths. While nursing home residents continue to make up a significant proportion of COVID-19 deaths, the proportion of all COVID-19 deaths occurring among nursing home residents fell to 24% and 31% in 2021 and 2022, respectively (Jurcevic et al., 2023[4]). This distribution of COVID-19-related deaths, particularly during the first two waves of the pandemic, indicates a challenging and in some cases suboptimal response in long-term care facilities.
Mortality rates among residents of nursing homes in Belgium have previously been reported to be the highest among OECD countries (Rocard, Sillitti and Llena-Nozal, 2021[14]). The difference in recording COVID-19 mortality between Belgium and other OECD countries makes it difficult to evaluate the extent to which long-term care facilities in Belgium were disproportionately hit compared to other OECD countries.
At more than 67 beds per 1 000 people aged 65 and above, Belgium has one of the highest numbers of long-term care beds in facilities and hospitals across the OECD. The number of long-term care beds per capita is well above the OECD average of 45.6 beds per 1 000 people aged 65 and above, and higher than all but Luxembourg and the Netherlands (OECD, 2023[15]). The fact that a comparatively higher proportion of Belgium’s older residents live in nursing homes compared to many other OECD countries has meant that the impact of poor infection control and preparedness in nursing homes – a very serious situation in Belgium during the pandemic, but not unique to the country – has had a disproportionate impact compared to many other countries.
4.1.4. Other vulnerable groups, including people of low socio-economic status and certain ethnic and professional groups, were particularly hard-hit
Across OECD countries, the COVID-19 pandemic has affected certain socio-economic, ethnic, and professional groups particularly hard (McGowan and Bambra, 2022[16]; Aburto et al., 2022[17]; Berchet, Bijlholt and Ando, 2023[18]). These findings were no different in Belgium. A study using linked data from the Belgian National Register found that during the first months of the pandemic, excess mortality was particularly high among immigrant men of Sub-Saharan African descent, with higher mortality among older men of migrant backgrounds, compared with native-born Belgians (Vanthomme et al., 2021[19]).
Higher incidence and mortality rates were also recorded among people from a lower socio-economic background. Between March 2020 and June 2021, the incidence rate of confirmed cases of COVID-19 in Belgium between March 2020 and June 2021 was 24% higher in the most deprived areas than in the least deprived ones (Meurisse et al., 2022[20]). In line with that, a study using linked Belgian administrative data demonstrated that in the first wave of the pandemic, excess mortality among people in the lowest income decile was more than twice that of people in the highest income decile (Decoster, Minten and Spinnewijn, 2021[21]).
Similar patterns of high incidence and mortality rates among people with lower incomes, those living in more deprived areas, and ethnic minorities have been found in other OECD countries. An OECD review of evidence related to COVID-19 outcomes among disadvantaged and vulnerable groups found that the risk of dying from COVID-19 was 40-60% higher among those in the lowest income groups in Canada, Luxembourg, the Netherlands and Sweden compared to those in the highest income groups (Berchet, Bijlholt and Ando, 2023[18]). However, differences in study methodologies, designs, and the time periods covered across analyses complicate direct comparisons of the differential impacts of COVID-19 by different categories of vulnerability (Berchet, Bijlholt and Ando, 2023[18]).
Certain professions have also been found to have experienced higher incidence of COVID-19 compared with other professions (Verbeeck et al., 2021[22]). This reflects the reduced abilities of certain professional groups to comply with certain non-pharmacological interventions that can help to reduce infection rates, particularly of those requiring close personal interaction, such as health professionals and employees in the transportation and hospitality sectors (Verbeeck et al., 2021[22]).
4.1.5. Long COVID continues to impact an important number of Belgians
More than three years into the pandemic, long COVID continues to impact the daily lives of a non-negligible proportion of people who are infected with COVID-19. In Belgium, health authorities have launched many initiatives intended to better understand the prevalence and impact of long COVID. Overall, these studies find that long COVID has serious impacts on well-being and quality of life for a significant proportion of people experiencing long COVID symptoms.
Sciensano, the national public health institute of Belgium, launched the COVIMPACT project in April 2021. The project ran for two years and followed a cohort of patients in Belgium who had been infected with COVID-19 to evaluate the long-term impacts – in terms of mental health, social well-being, and physical health – of COVID-19 and explore what determinants may impact better or worse long-term outcomes (Sciensano, 2023[23]). Results from the study found that nearly half (47%) of all participants continued to have at least one symptom related to their initial COVID-19 infection after three months, with close to one-third (32%) of participants reporting they had at least one symptom six months after their initial infection (Smith et al., 2022[24]). About one-fifth of respondents reported having received a formal diagnosis of long COVID from a healthcare professional (21% after 3 months, 22% after 6 months) (Smith et al., 2022[24]).
While a high proportion of respondents reported having at least one symptom at least three months following their initial COVID-19 infection, many also reported that they felt they had broadly recovered from COVID-19. At both three and six months post infection, fewer than 10% of respondents reported that they had either not at all recovered from COVID-19 or had not recovered very much, with just 3% of respondents reported that they felt they had not recovered at all (Smith et al., 2022[24]).
Surveys of patients in Belgium have further underscored the potential financial and employment impact of long COVID. In a Federal Health Care Knowledge Centre (Federaal Kenniscentrum voor de Gezondheidszorg / Centre Fédéral d’Expertise des Soins de Santé (KCE)) survey of long COVID patients, three-fifths of patients reported that they had an incapacity to work following their COVID-19 infection, with just one-third of respondents reporting that they had returned to work as usual at the time of the survey (Castanares-Zapatero et al., 2021[25]). More than one quarter (26%) of respondents had returned to work, but at fewer hours than they had worked prior to their infection, while nearly two-fifths (38%) reported not having returned to work at all due to their health problems (Castanares-Zapatero et al., 2021[25]). Some 37% of respondents experienced negative financial consequences due to their condition, with the impact due to reductions in employment, medical expenses, or a combination of these factors representing the major drivers of financial loss associated with long COVID (Castanares-Zapatero et al., 2021[25]).
Patients with long COVID experience a wide range of symptoms, meaning the care they need to help treat the condition is not always straightforward and can require services from a range of healthcare settings and professionals. In the KCE survey, co-ordination of care around long COVID was found to be poor, with an insufficiently integrated and multidisciplinary approach hampering patient-centred care (Castanares-Zapatero et al., 2021[25]). Moreover, reimbursement limits set by the national social security system – such as a maximum of 18 physiotherapy services reimbursed per year – were found to be insufficient to address the ongoing long COVID care needs of some patients (Institut national d'assurance maladie-invalidité, 2022[26]).
Through March 2022, patients with long COVID had access to care services through established reimbursement schemes, but no specialised services or care pathways were reimbursed for long COVID (Castanares-Zapatero et al., 2021[25]). While these previous agreements likely covered a certain proportion of the care needed for long COVID and the majority of long COVID patients surveyed in the KCE survey responded being satisfied in their interactions with the health system, a comprehensive, holistic diagnostic work-up for long COVID was found to be lacking, with patients sometimes experiencing delays in proper referrals as a result (Castanares-Zapatero et al., 2021[25]).
To improve the health system’s response to caring for people with long COVID, notably around the co-ordination of care, the National Institute for Health and Disability Insurance (Institut national d’assurance maladie-invalidité / Rijksinstituut voor ziekte- en invaliditeitsverzekering (INAMI-RIZIV)) began reimbursing services for personalised long COVID care pathways in July 2022. Reimbursements cover services that would not have been covered by existing reimbursement agreements. To be eligible, patients must have a formal diagnosis of long COVID from a general practitioner, a minimum of 12 weeks after an initial COVID-19 infection (Institut national d'assurance maladie-invalidité, 2022[26]). Policy changes to support the continuity of long COVID care were introduced earlier in some countries. In the United Kingdom, for example, NHS England launched an enhanced service specification to improve long COVID assessment and care in primary care beginning in June 2021 (NHS England, 2021[27]).
Going forward, it will be important to monitor the potential impacts of long COVID and other long-term health impacts of the pandemic to better understand their impact on the daily and working lives of people as well as the response needed from the health system. Few countries have monitored the potential prevalence of long COVID systematically on a population level. Regular household surveys in the United States (the Census Bureau’s Household Pulse Survey) and the United Kingdom (through the Office of National Statistics UK Coronavirus Infection Survey) stand out as examples of regular measurement of self-reported long COVID and its impacts on daily life. Belgium should consider how it can make use of its extensive data infrastructure, including data from the Crossroads Bank for Social Security, to monitor any changes to the health status of its population and to the impacts it may have on socioeconomic outcomes and the labour market.
4.2. What indirect impacts did COVID-19 have on health in Belgium?
4.2.1. The pandemic took a significant toll on mental health in Belgium
Across the 14 OECD countries with available data, the COVID-19 pandemic led to substantial increases in the prevalence of self-reported poor mental health, with the proportion of the population reporting symptoms of anxiety and depression doubling in a number of countries (Figure 4.3) (OECD, 2023[15]). In Belgium, the prevalence of both self-reported depression and anxiety almost doubled between 2019 and 2020, with 18% of survey respondents reporting symptoms of depression and 20% reporting symptoms of anxiety, in 2020, up from about 1 in 10 in 2019. While self-reported anxiety and depression fell in 2022 compared to 2020, they remain above pre-pandemic levels, with 15% of respondents reporting symptoms of depression and 17% symptoms of anxiety in 2022 (OECD, 2023[15]). Prevalence estimates may be affected by data reporting factors such as more and more sympathetic discussion of mental health in the media contributing to a greater willingness to disclose mental health concerns, or a higher likelihood of disclosing mental health concerns in online self-reporting compared to in-person (Moron, Irimata and Parker, 2023[28]). Nonetheless, a worsening of mental health status especially during the most acute phases of the pandemic, particularly for already-vulnerable groups such as those with low incomes, unemployed persons, or young people, was a pattern seen across OECD countries (Daly, Sutin and Robinson, 2020[29]; Bruggeman et al., 2022[30]; Moulin et al., 2023[31]; OECD, 2021[32]).
Figure 4.3. National estimates of prevalence of depression or symptoms of depression, 2019-22 (or nearest year)
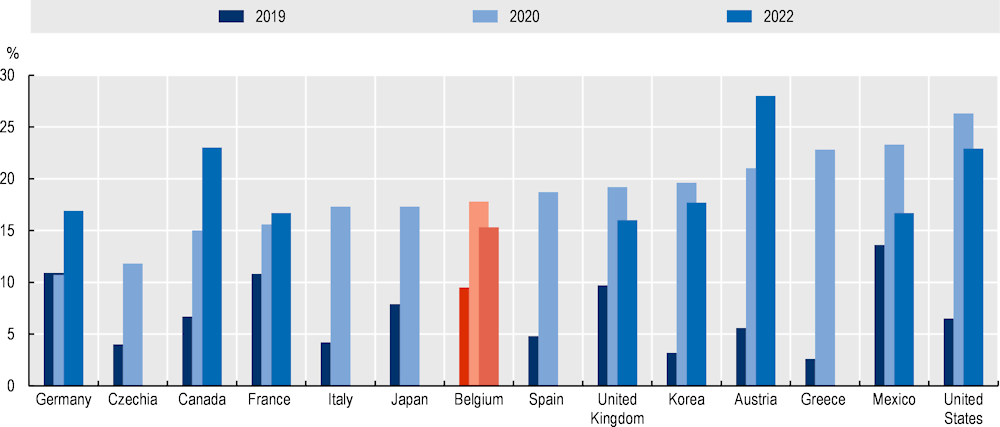
Notes: Survey instruments and population samples differ between countries and in some cases across years within countries, which limits direct comparability. Pre-pandemic data for Czechia is from 2017; Canada from 2015-19; Japan from 2013; Belgium from 2018; United Kingdom from 2019-March 2020; and Korea from 2016-19.
Source: OECD (2023[33]), OECD Health Statistics 2023.
The utilisation of medicines related to mental health treatment appears to have fallen during the pandemic. Compared to the previous year, antidepressant prescriptions fell at the start of 2020 and remained lower than prior to the pandemic into 2021 (Figure 4.4).
Figure 4.4. Average monthly percentage of adults who purchased a prescribed antidepressant over the last 3 months
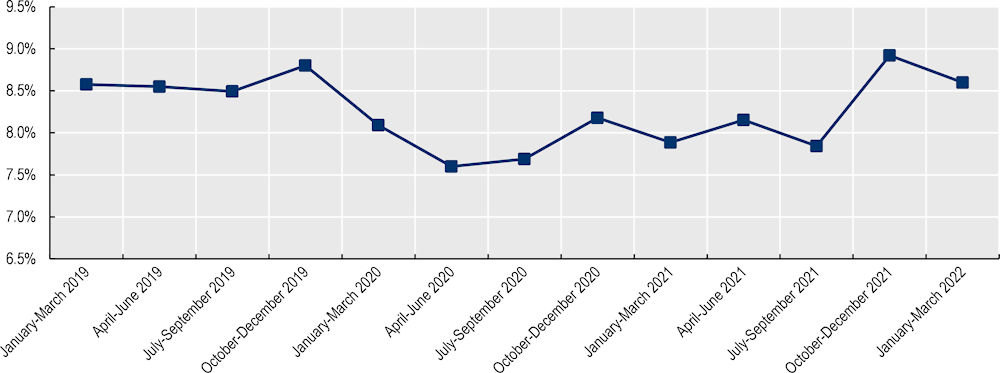
Note: Unweighted three-month averages calculated based on monthly data.
Source: L’Agence InterMutualiste (2023[34]), ATLAS IMA website.
Data from primary care in Flanders suggests that the distribution of care for mental health conditions also changed over the pandemic period. Overall, general practitioners provided more mental healthcare over the course of 2000 and 2021 than prior to the pandemic, with the volume of registrations for mental healthcare rising by nearly 9% in 2020 and 40% in 2021, compared with the 2018-2019 period (Vandamme et al., 2023[35]). While care increased for depression and anxiety, care for other important mental health conditions – such as eating disorders and care for substance abuse problems – fell in primary care over the course of the pandemic and had not recovered by the end of 2021 (Vandamme et al., 2023[35]).
Relatively early on in the pandemic, regional authorities adopted measures to strengthen the provision and continuity of mental healthcare. Walloon health authorities increased the mental health workforce during the pandemic by funding an additional 189 full-time positions to strengthen outpatient mental health services, as well as services related to suicide prevention, palliative care and mental health support for care workers and those living in long-term care facilities (OECD, 2023[36]). Brussels scaled up mental health services targeted at specific populations, creating a temporary telephone hotline to provide psychological support to caregivers, increasing the number of child and youth front-line mental health teams, and increasing outreach in outpatient mental healthcare, including outreach for vulnerable groups (OECD, 2023[36]). The region also scaled up the number of lieux de liens – places of connection – community centres that are accessible to people with psychiatric and psychological conditions, but which operate outside of the formal mental health system (Lasserre and Misson, 2021[37]; OECD, 2023[36]).
Ongoing health reforms undertaken by authorities, including at the federal level through the Interministerial Conference on Public Health, aim to ensure the continuity of mental healthcare and expand access to psychosocial services for those who newly needed them. These reforms built on efforts already underway prior to the pandemic to strengthen the access and affordability of primary mental healthcare services, and include EUR 112.5 million in additional funding earmarked to strengthen primary mental healthcare (Healthy Belgium, 2023[38]). Reforms to the mental health system intended to strengthen first-line mental health services were based on the existing 32 mental healthcare networks, each covering specific regions and targeting both adult and child and adolescent mental health services. In particular, the reforms were aimed at helping to improve prevention and early detection, as well as to identify vulnerable groups and consider broader socioeconomic factors that could contribute to poor mental health (Office of Frank Vandenbroucke, 2022[39]). Beginning in September 2021, access to mental health services were expanded to include up to 20 visits with a psychologist for the out-of-pocket cost of EUR 11 per session (EUR 4 per session for those entitled to supplemented refunds), or EUR 2.50 per session for group therapy.
Funding was also earmarked to support specific populations and mental health outreach efforts related to the pandemic, including EUR 1.5 million to support mental health support for students, EUR 4.7 million to strengthen mobile crisis teams targeting children and adolescents, and EUR 55.5 million to support self-employed adults, including free psychological care (Healthy Belgium, 2023[38]).
4.2.2. Certain vulnerable and professional groups were at higher risk of poor mental health and reduced access to mental health services during the pandemic
In addition to youth and young adults, people with disabilities, residents of nursing homes, people with low social support, and those with a lower prevalence of meaningful activities, including employment, were found to be at higher risk of poor mental health such as anxiety and depression during the pandemic (Bruggeman et al., 2022[30]; Godderis, 2021[40]). The disproportionate impact of the pandemic on poor mental health among young people has been identified as a major health outcome of the pandemic across countries, and Belgium is no exception. Across all waves of the BELHEALTH Cohort Surveys conducted during the pandemic, the youngest adults (age 18-29) reported the highest prevalence of depressive symptoms, with the oldest adults (age 65+) consistently reporting the lowest prevalence of symptoms of depression (Figure 4.5).
Figure 4.5. Percentage of adults with a depressive disorder (according to PHQ-9), by age group
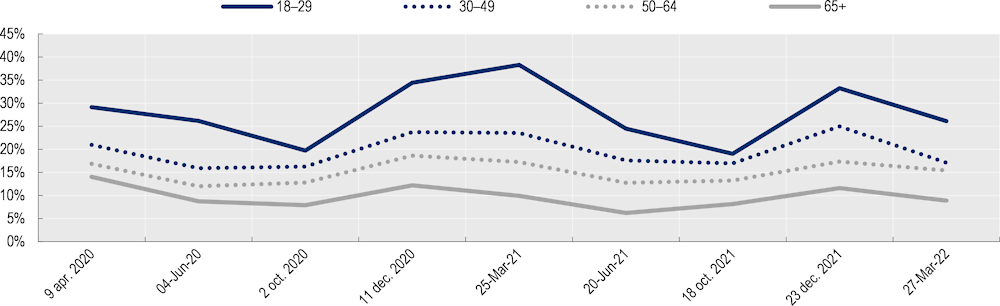
Note: The PHQ-9 is a self‐administered questionnaire which scores each of the 9 DSM‐IV criteria for depression as “0” (not at all) to “3” (nearly every day). This scale includes a Major depressive syndrome (total sum of all items > 4 and the item “Little interest or pleasure in doing things” or “Feeling down, depressed, or hopeless” >1) and Other depressive syndrome as well (total sum of all items between 1 and 5 and the item “Little interest or pleasure in doing things” or “Feeling down, depressed, or hopeless” >1). https://www.sciencedirect.com/science/article/pii/S0163834313001278
Source: Sciensano (2023[41]), Sciensano Belgium COVID-19 Epidemiological Situation Mental Health Studies (database).
The mental health impact of the pandemic on young people in Belgium reflects the experience of young adults in a number of OECD countries. Across seven OECD countries with available data, the share of young people with symptoms of depression increased everywhere in 2020-2021 compared with 2019, more than doubling in all but one country, including in Belgium.
Figure 4.6. Share of young people with symptoms of depression
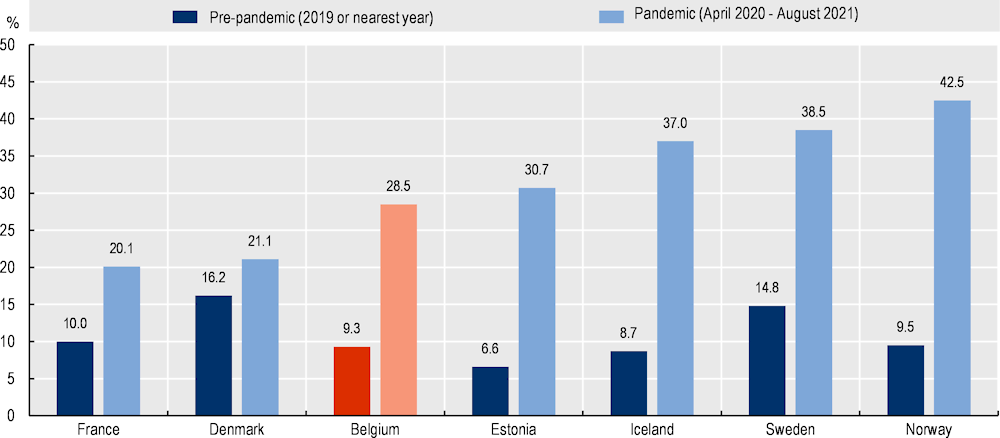
Note: Given the prevalence of symptoms of depression has fluctuated within countries over the course of the pandemic, prevalence estimates are pooled from longitudinal or repeated cross-sectional surveys within countries up to 12 August 2021. However, not all surveys are representative and the number and timing of surveys has varied across countries which hampers cross-country comparability. Symptoms of depression have been measured using PHQ-8 and PHQ-9 in all countries except France and Estonia. Some pre-pandemic and pandemic data are not strictly comparable due to differences in scoring methods, which could understate the increase in symptoms to some extent. Symptoms of depression in France during the pandemic have been measured using HADS-D which could lead to lower estimates of the share of young people with symptoms of depression compared to other countries using PHQ-8 and PHQ-9.
Source: OECD/European Union (2022[42]). Health at a Glance: Europe 2022: State of Health in the EU Cycle, OECD Publishing, Paris, https://doi.org/10.1787/507433b0-en.
Data on hospital admissions and waiting times for child psychiatric services further suggests that the relatively higher mental health toll of the pandemic on young adults also applies to children and adolescents. In Flanders, waiting times for residential care for eating disorders were reported to be four times as high in October 2021 as they had been prior to the pandemic (Godderis, 2021[40]). Both outpatient and residential child psychiatry services were also reported to have been heavily oversubscribed, with two to three month waiting times for child psychiatric appointments and hospitalisations, and a shortage of child psychiatric beds (Godderis, 2021[40]).
The well-being and mental health of the healthcare workforce was also strongly impacted during the pandemic. Results from the OECD Survey of General Practitioners indicated that of the 17% of survey respondents who reported seeking mental health support during the pandemic, four-fifths (81%) had not previously sought mental health support prior to the pandemic, or had not received mental health support for a long time prior to the pandemic (OECD, 2023[43]). Across Belgium, more than three-fifths of general practitioners (hereafter, GP) respondents to the PRICOV-19 study, conducted during the pandemic, reported that they had felt burned out from their work during the past month, with the proportion of general practitioners at risk of distress (based on the Mayo Clinic scale) rising by 15% in comparison to before the pandemic, from 60% to 69% (Fomenko, 2023[44]). Another large-scale study of nurses during the first COVID-19 peak in Belgium found that 70% were at risk of burnout (Khan, Bruyneel and Smith, 2022[45]).
4.2.3. The COVID-19 pandemic led to disruptions in routine care
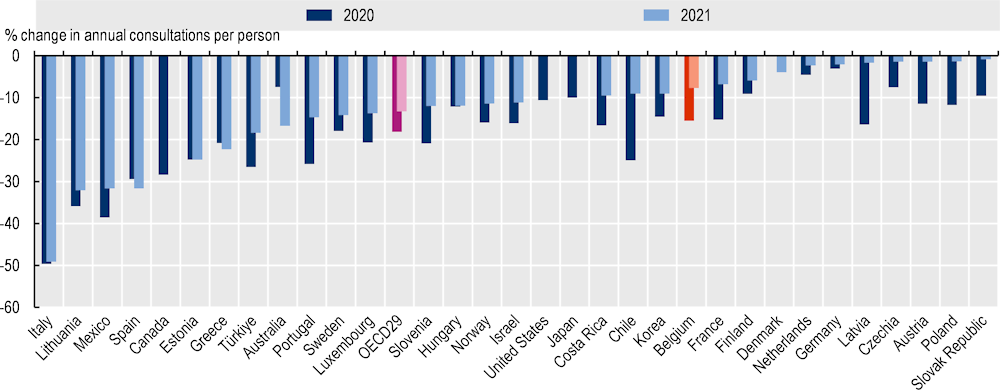
Making space for the needs of COVID-19 patients led to delays and postponements in care across the health system. As the scale of the pandemic became clearer, health authorities moved to free up space in hospitals and the health sector in part by postponing and delaying routine and elective care to the greatest extent possible, beginning in March 2020. This approach – which was broadly adopted across OECD countries – led to a decline in the number of physician consultations, particularly during the initial waves of the pandemic, with the number of consultations for many specialties remaining below pre-pandemic (2019) levels at the end of 2021.
Compared with other OECD countries for which data was available, the drop in consultations in Belgium following the onset of the pandemic was relatively modest (Figure 4.7). Consultations fell by 15.5% in 2020 compared to 2019 and by 7.7% in 2021 compared with 2019. In comparison, the average number of in-person consultations dropped by 18.1% across 28 OECD countries on average in 2020, and by 13.2% in 2021 compared to 2019. The reduction was smaller in Germany (-3.1% in 2020, -2.0% in 2021) and the Netherlands (-4.5% in 2020, -2.3% in 2021), roughly similar in France (-15.3% in 2020, -6.8% in 2021), and slightly more severe in Luxembourg, especially in 2020 (-20.7% in 2020, -13.7% in 2021).
Figure 4.7. Percentage change in number of in-person doctor consultations compared to 2019
Looking at more disaggregated data available for Belgium, between 2019 and 2020, the number of consultations fell across a range of specialties, with a particularly large decline recorded during the first wave of the pandemic. Geriatric consultations, which experienced the biggest fall during the first wave (a 63%-decrease compared to the same period in 2019), also recorded the biggest fall over the course of the entire year in 2020 and remained 15% lower than pre-pandemic levels through 2021. In contrast, both cardiology and oncology fell in 2020 – by 12% and 5%, respectively – but recorded increases in the number of consultations in 2021 compared to 2019 (1% and 4%).
Figure 4.8. Percentage change in number of doctor consultations compared to 2019
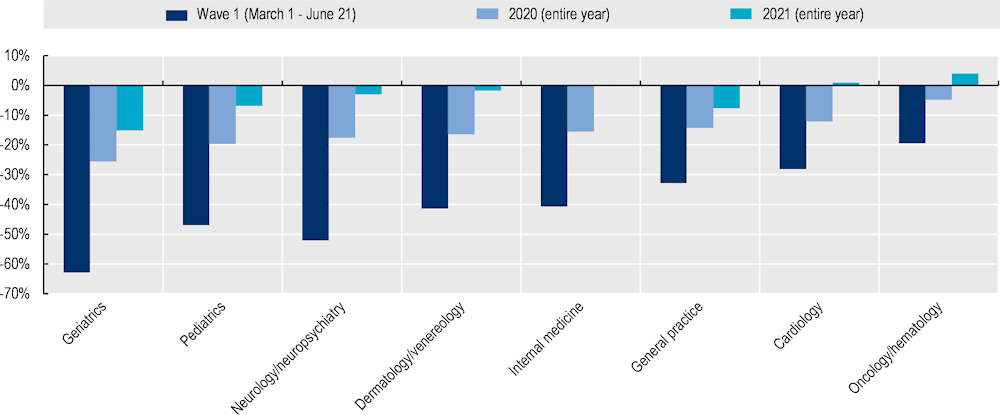
Note: Year refers to December of the previous year – November of the referenced year. For wave 1, estimates based on assumption that consultations are evenly distributed across the month.
Source: INAMI (2022[46]), Monitoring COVID-19: L'impact de la COVID-19 sur le remboursement des soins de santé, https://www.inami.fgov.be/SiteCollectionDocuments/monitoring_COVID19_update_fevrier_2022.pdf.
The activation of emergency plans and measures taken to make space for COVID-19 patients in hospitals by the Hospital Transport and Surge Capacity Committee (HTSC), the advisory body set up to manage hospital and transport control measures during the pandemic, led to reductions in hospitalisations for routine and elective services. During the first and second waves of the pandemic in Belgium, the total number of hospital stays fell to 52% and 75% of the median of the four years prior to the COVID-19 pandemic, respectively (FPS Public Health, 2023[47]). Surgical day hospitalisations fell the most: during the first wave, the number of hospitalisations for ambulatory surgeries fell to 11% of the previous four-year median (FPS Public Health, 2023[47]). Some routine surgeries, including hip replacements and total knee replacements, fell in the first year of the pandemic compared to pre-pandemic levels. Total knee replacements, for example, fell by 55% in Belgium between 2019 and 2020 – more than twice the OECD average reduction of 23%, and higher than neighbouring France (-28%), Germany (-12%), and Luxembourg (-31%) – and remained 23% below their 2019 levels in 2021. Hip replacements similarly fell during the pandemic, by 19% in 2020 compared to 2019, and remained below pre-pandemic levels into 2021 (OECD, 2023[33]). Despite these drops, however, hip and total knee replacements in Belgium remain well above the OECD average, with 271 hip replacements performed per 100 000 population in 2021 (compared to 172 on average across 33 OECD countries), and 164 total knee replacements per 100 000 population in 2021 (compared to 119 across 32 OECD countries) (OECD, 2023[15]).
4.2.4. Some declines in cancer screening and diagnosis were reported in Belgium
As in other OECD countries, Belgium experienced declines in the number of new cancer diagnoses made during the pandemic. Diagnoses for breast and colorectal cancers plummeted during the first wave of the pandemic, with breast cancer diagnoses among women in the age group for screening (aged 50-69) falling by 56% in April 2020 compared with April 2019, and colorectal cancer diagnoses for men and women in the screening age group (aged 50-74) falling by 54% over the same period (Belgian Cancer Registry, 2022[48]). While still slightly below 2019 levels, diagnosis rates have largely recovered over the course of the pandemic, with breast cancer diagnosis among women of screening age being 2% lower between January 2020-December 2021 compared with the previous period, and colorectal cancer diagnosis among people of screening age being 8% lower (-10% among men and -5% among women) (Belgian Cancer Registry, 2022[48]). Overall, the Belgian Cancer Registry has estimated that about 2 700 diagnoses of cancer were missing over the first two years of the pandemic (Belgian Cancer Registry, 2022[48]).
The decline in screening rates and cancer diagnoses across many countries over the course of the pandemic has led to concerns about the implications of delayed diagnosis and treatment for the stage at diagnosis and ultimately mortality. There is some evidence to suggest that the delays in cancer diagnoses have more negative impacts on cancers that progress more quickly, such as head and neck cancer. The incidence of head and neck cancers in Belgium was nearly 10% (9.5%) lower in 2020 than what would have been predicted based on the trend from 2017-2019, but with an increased stage at diagnosis among both men and women for oropharynx and larynx tumours, though not all head and neck tumours overall (Peacock et al., 2023[49]).
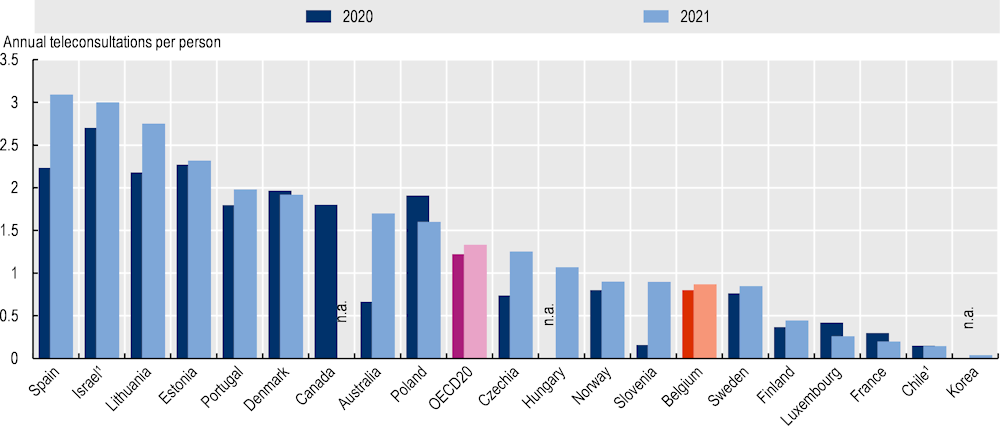
4.2.5. Belgium introduced teleconsultations to help ensure access to care, but uptake remains below that of other OECD countries
As in many countries, the scale-up of telemedicine served as a crucial tool to maintain a measure of access to, and continuity of, care during the pandemic. In Belgium, reimbursement for teleconsultation services was adopted at the beginning of March 2020. Prior to the pandemic, no reimbursements were possible for remote consultations. Starting from 14 March, the INAMI-RIZIV approved three new billing codes for physicians providing remote medical services – by telephone and with or without video – to support both COVID-19-related triage (code 101990), COVID-19 care and triage organised by general practitioners (code 101835), as well as continuity of care (code 101135). For all three types of care, physicians billed health insurers EUR 20, with no additional charges or fees for the patient (Institut national d'assurance maladie-invalidité, 2022[50]).
In addition to making teleconsultations available for non-COVID-19 related continuity of care, many COVID-19 patients also received telemedical services to monitor the progression of their illness. Nonetheless, while access to teleconsultation services increased compared to prior to the pandemic (when such care was not reimbursed), the take-up of telemedicine in Belgium remained comparatively low, averaging just 0.8 consultations per capita in 2020 and 0.9 per capita in 2021, lower than the OECD average of 1.2 consultations per person in 2020 and 1.3 consultations in 2021 (Figure 4.9). The share of teleconsultations as a proportion of overall doctor consultations is also lower than in other OECD countries. In 2021, teleconsultations made up 11% of overall consultations, compared with 19% on average across 20 OECD countries (OECD, 2023[15]).
Figure 4.9. Doctor teleconsultations per person, 2020 and 2021 (or nearest year)
The results of a survey conducted by the INAMI-RIZIV following the first six months of their COVID-19 telemedicine reimbursement policy found that the majority of teleconsultations were conducted with a general practitioner (78%), with specialists representing 11% of remote consultations and mental health specialists (psychiatrists and psychologists) representing a further 7% of remote consultations (CIN-NIC, 2020[51]). Notably, patients were far more likely to report that specialists and mental health professionals (psychiatrists and psychologists) had taken the initiative to organise the teleconsultation than the patients themselves, with the majority of patients reporting that teleconsultations replaced a specialist or mental health appointment planned in advance. In contrast, nearly three-quarters of appointments with general practitioners were not organised as a replacement for a previously organised consultation (CIN-NIC, 2020[51]).
An analysis of the use of teleconsultations during the first year of the pandemic suggests that access to telemedicine and teleconsultations was fairly evenly distributed across the population. Throughout the year, the proportion of the population accessing telemedical services was largely similar between people living in regions considered to be among the poorest quartile, compared with those living in the wealthiest quartile regions (Vrancken et al., 2022[52]). For the majority of the year, access to telemedicine services was slightly higher among people living in the poorest quartile regions (Vrancken et al., 2022[52]). While this may in part be related to a comparatively higher risk of poor health and COVID-19, the lack of a significant difference in access to telemedicine services suggests that overall, full reimbursement from the INAMI-RIZIV and the ability to engage in teleconsultations with and without video may have helped to address some challenges of the digital divide.
4.3. How effective was the health response to the pandemic in Belgium?
4.3.1. The complex governance and crisis response structures of Belgium complicated the initial pandemic response
Belgium activated the “federal phase” of its crisis management system on 12 March 2020 (see Chapter 3). While the emergency nature of the pandemic was understood, the response to the pandemic in the initial months was complicated by some lack of institutional and personal leadership, as well as the complexity and number of structures set up to co-ordinate the response. Two major bodies responsible for managing the crisis – the National Crisis Center (NCCN) and the Federal Public Service Public Health (hereafter, FPS Public Health) – did not have a strong leadership role from the onset of pandemic. In many cases, the crisis structures set up by NCCN were bypassed in favour of ad hoc bodies formed to address the pandemic, while a lack of familiarity between NCCN and the public health community further complicated its ability to lead. In the FPS Public Health, its main advisory body, the Risk Management Group (RMG), grew to a size that made it difficult to issue advice, and became instead largely a forum for discussion and debate. Moreover, the crisis management capacity within the FPS Public Health was limited, with the existing unit focused primarily on emergency response, rather than risk anticipation and preparedness. Some of these co-ordination challenges were alleviated by the creation of the COVID Commissariat in October 2020. Ensuring crisis management capacities in the FPS Public Health are strengthened will be essential for addressing future health emergencies.
4.3.2. Belgium encountered a severe shortage of personal protective equipment (PPE) in the first weeks of the pandemic.
The destruction of the federal strategic stockpile (see Chapter 2) and fragmented competencies for emergency stocks meant that many key sectors faced acute PPE shortages at the start of the pandemic. In the initial weeks, similar to most OECD countries, Belgium encountered a severe shortage of PPE, such as masks, gowns, and other protective gear across all sectors. Indeed, Belgium’s strategic stock of PPE had expired prior to the pandemic, was subsequently destroyed, and had not been replaced at the onset of the pandemic.
Healthcare providers received PPE from different sources, which reflects the governance structure of the country. Hospitals are largely a federal competency. Subsequently, the federal level was in charge of providing PPE to hospitals. It set up a joint Task Force in mid-March 2020 to take an inventory of PPE and to alleviate the shortage, for example by confiscating existing mask stocks, by procuring masks on the national and international market, and by restricting the sale of masks and other PPE to individuals with a prescription from a healthcare professional. The federal government also procured masks from Doctors Without Borders (Médecins sans frontières). Long-term care facilities, on the other hand, are a competency of federated entities, and thus received PPE from the subnational governments. They reported encountering substantial difficulties sourcing PPE at the start of the pandemic. While creating a task force charged with co-ordinating the pandemic response in long-term care facilities was briefly considered, concerns related to overstepping competencies meant that the idea was quickly abandoned. In general, efforts to procure and equip providers with PPE were hampered by debates on how competencies are divided among different government levels in the first weeks.
The situation across regions was very heterogeneous and depended on the success of each regional authority to procure PPE, as well as long-term facilities’ own connections with local hospitals. When the sub-national entities learned in March that the strategic stock had been destroyed, they tried to procure masks on the international market themselves. For example, the German-speaking Community successfully procured masks from German manufacturers in the early phase of the pandemic, and also built its own storage facility and network. Providers in that part of the country could post an order on a weekly basis. The Brussels-Capital region organised and received PPE from NGOs, such as Doctors of the World (Médecins du Monde). In the Flanders region, nursing homes with ties to hospitals or first-line structures sometimes received masks through these networks. Efforts to engage with national manufacturers such as the clothing industry to produce masks were of limited success, for example due to shortages in supply material. Health providers also reused masks, for example by alternating masks in weekly turns, and improvised using alternative devices, such as diving gear (OECD, 2023[53]).
Assessments of providers on the availability of PPE suggest that shortages were most acute in the initial two waves of the pandemic. In August 2020, an observational study of Belgian GPs found that a quarter of GPs still faced major shortages of FFP2 masks (Vaes et al., 2022[54]). Survey responses from the OECD Survey of General Practitioners in Belgium indicated that of the 64% (264) of GPs who reported experiencing PPE shortages in their practice, 96% (254) experienced shortages during the first wave and 19% (49) during the second wave (OECD, 2023[43]). In contrast, just 3% reported shortages in the third wave, while a further 3% reported that shortages lasted throughout the pandemic (OECD, 2023[43]). All responding hospitals in the OECD Survey of Hospitals reported experiencing shortages of PPE (n=27), with three facilities reporting that these shortages continued to be problematic throughout the pandemic (OECD, 2023[55]).
Belgium’s experience with severe shortages of PPE have underscored the importance of improving transparency on PPE procurement and stocks to facilitate the response, and to building strategic stockpiles for future crises. In the public procurement of PPE, well-functioning structures were largely absent at the beginning of the pandemic, leading to an insufficient preparedness in the first year. Belgium could learn from other OECD countries in developing more responsive systems for PPE allocation and distribution. Norway, for example, introduced a centralised system to report, allocate and distribute PPE (OECD/European Observatory on Health Systems and Policies, 2021[56]). National authorities could trace PPE orders of municipalities via a web calculator (OECD, 2021[57]). This allowed Norway to monitor the demand and supply of PPE and helped to improve access for health providers. Similarly, Luxembourg set up a daily stock management to track the delivery and use of PPE of hospitals and care facilities on a daily basis (OECD, 2022[11]).
Belgium would have also benefitted from greater co-ordination capacity between the federal government and federated entities. Some countries have mandated the stockpile quantity by type of service. In Lithuania, for example, the national government has to uphold a stockpile for 60 days, and long-term care facilities for 30 days (OECD, 2021[57]). New regulations by federated entities requiring nursing homes to have a stock of PPE are a welcome development. Stockpiles should be assured for essential health and social care services, as well as relevant operators of critical infrastructure, regardless of whether they are the responsibility of the federal government or federated entities.
4.3.3. Many nursing homes lacked the appropriate information, supplies, and expertise to respond effectively to the COVID-19 pandemic
Residents of nursing homes were among the hardest hit during the pandemic, particularly during its initial waves, with a significant proportion of all COVID-19 mortality occurring in and among residents of nursing homes (see Section 4.1.3). With much of the initial pandemic response driven by images of the overwhelmed hospitals in Wuhan and in Northern Italy, planning for the pandemic was initially focused on preparing hospitals to respond – an understandable and necessary step, but one that may have contributed to comparatively less attention being given to other key sectors, including nursing homes.
While hospital capacity in Belgium remained relatively solid throughout the pandemic and age was not considered the leading factor in directives issued related to hospital transfers during the pandemic, data from the HTSC indicates that transfers from nursing homes were notably lower during the first wave of the pandemic than in the second wave during the fall and winter of 2020-2021 (Figure 4.10).
Figure 4.10. Sum of total transfers from nursing homes by week
As the pandemic spread quickly through nursing homes, the limited ability of many nursing homes to control the virus became clear. In many cases, while nursing homes had healthcare professionals – including nurses and doctors – on staff, facilities were designed as a living environment, rather than for infection control and management. Features such as communal living spaces and ventilation systems connected across multiple rooms severely complicated efforts to contain the spread of the virus once it had entered a facility. In response to the pandemic, a range of measures were implemented to strengthen infection control and limit outbreaks in long-term care facilities. These included:
The use of outbreak support teams: All federated entities employed mobile outbreak support teams to help support nursing homes experiencing clusters of cases or bigger outbreaks with infection control. In Brussels, for example, outbreak support teams comprised one doctor and three nurses, with teams created to support outbreaks among collective institutions (including nursing homes), schools, and homeless populations.
The development of other mobile teams for infection control and mental health support: In addition to teams that could support nursing homes in-person and at a distance in the context of outbreaks, mobile teams were deployed to reinforce knowledge on infection control, hygiene and isolation measures among health and care workers in long-term care facilities. Mobile teams also provided psychological support. In Wallonia, for example, the mobile psychological care support teams (SPAD) also provided support for first-line healthcare workers, including those working in care facilities, while in Flanders, mobile teams could actively help identify nursing homes’ employees who could benefit from psychological support. In Flanders, mobile teams visited three-quarters of the region’s nursing homes to provide information and training on PPE, hand hygiene, and provide general support.
The deployment of the military to provide additional personnel support: In cases where nursing homes were overwhelmed, support from the military and the Belgian Civil Protection was called in to provide additional personnel support. In Wallonia, for example, the Civil Protection was brought into nursing homes when clusters grew too large and exceeded 10 people.
During the crisis, all long-term care facilities were asked to report daily on the number of COVID-19 patients (suspected and confirmed) and COVID-19-related deaths that had occurred in their facilities. Prior to the pandemic, nursing homes had been included in epidemiological surveillance systems set up by Sciensano in only a limited (convenience sample) way, alongside a small but representative sample of hospitals and general practitioners. The general lack of previous data infrastructure and experience with data reporting meant that these requests in some cases added substantial pressures on nursing home staff, particularly when combined with the burdens placed on nursing homes in dealing with the pandemic itself. Moreover, unlike the data collected by Sciensano and the Incident Crisis Management System and used by the HTSC, data collected from nursing homes was primarily not collected to help manage the response in nursing homes, but focused on informing health authorities of the progression of the pandemic.
Good working relationships with nearby hospitals were considered critical at the beginning of the pandemic with regard to access, testing and receiving test results quickly, as well as to procure PPE (OECD, 2023[53]). Some nursing homes were able to leverage their good working relationships with virologists in local hospitals for further clinical advice on treating patients with COVID-19 in nursing homes. Proactively strengthening co-ordination and relationships between nursing homes and local health facilities, including hospitals, is necessary to help the long-term care sector better respond to future crises. During the pandemic, Belgium was already able to benefit from the co-operation of hospitals and long-term care facilities that exchanged knowledge, equipment, and staff and made use of their local hospital networks (loco-hospital networks) to organise patient transports (Rocard, Sillitti and Llena-Nozal, 2021[14]; Van de Voorde et al., 2020[58]). Other countries operated with similar measures, such as guidelines for better integration of long-term care facilities with hospitals, as in Canada, Estonia, Finland, Portugal, and Slovenia (Rocard, Sillitti and Llena-Nozal, 2021[14]). France profited from a central government strategy that was translated into regional measures, such as a hospital COVID-19 support platform for long-term care facilities (Rocard, Sillitti and Llena-Nozal, 2021[14]; Rolland et al., 2020[59]).
Belgium can build on preexisting structures and move towards a more integrated and co-ordinated approach to long-term care than was possible during the pandemic. For example, Belgium should integrate long-term care facilities into locally co-ordinated structures to give them as much weight as other healthcare facilities, and to strengthen timely infection prevention and control to outbreaks. Belgium could look to other OECD countries to strengthen the integration of nursing homes with the clinical system: Czechia, Denmark, Finland, France, Germany, Japan, Luxembourg, Portugal, Slovenia and the United States all reported having had legislation or guidelines on integrating primary and long-term care prior to the pandemic, while in Ireland, the National Integrated Care Progamme for Older Persons is developing a co-ordinated care pathway for older people, particularly those with complex needs, across primary, secondary and tertiary care (Rocard, Sillitti and Llena-Nozal, 2021[14]). Hospitals could strengthen their relationships with local long-term care facilities to improve co-ordination and infection control expertise and make use of their loco-hospital hospital networks to organise patient transports. Belgium should also consider how the inter-federal response to long-term care can be strengthened, including whether interministerial conferences could be used to improve the long-term care response in future events.
Following the gradual easing from the peak of the pandemic, the data infrastructure that was developed to collect information from long-term care facilities has been largely wound down. Data collection and monitoring challenges related to long-term care and nursing homes are well established in Belgium. While the monitoring set up during the pandemic was built quickly and intended to serve a specific pandemic-related purpose, authorities should consider how its legacy could be used to improve data collection efforts and surveillance in nursing homes, both during acute crises and as part of a broader agenda of care quality improvement.
4.3.4. Pandemic-specific data and information systems needed to be set up at the start of the pandemic to channel information and quickly proved crucial to informing decisions
The Belgian government managed to quickly set up the necessary infrastructure to monitor data on the spread of the pandemic to inform decision making. To some extent, it built on already existing structures that had been set up in past crises, although these were often less systematic than necessary to meet the COVID-19 challenge, had longer reporting horizons, and mostly relied on voluntary participation. This data infrastructure was built in the first few weeks and months of the pandemic. The time required to scale up a new data infrastructure, combined with challenges related to testing capacity at the start of the pandemic, meant that Belgium was only able to properly monitor the spread of the virus several weeks after the start of the COVID-19 outbreak.
The COVID-19 pandemic marks the first time all hospitals and long-term care facilities reported daily data to health authorities. Hospitals and long-term care facilities were initially surveilled on death rates only as large-scale testing was not available yet. An established reporting pathway of mortality data from hospitals was fully operational from 15 March 2020 onwards and was rolled out in the two subsequent weeks for long-term care facilities (Renard et al., 2021[1]). Information from hospitals was directly collected by the federal government, whereas information from medical doctors and long-term care facilities was collected by the regional authorities, and subsequently forwarded to federal authorities. Mass testing in long-term care facilities was only launched on 15 April, which finally allowed long-term care facilities to move towards more tailored strategies, for example by isolating individual cases. In other OECD countries, a limited availability of tests in long-term care facilities at the start of the pandemic also hampered a good response (OECD, 2021[57]). The United Kingdom launched a mass testing strategy in early April 2020 and introduced additional measures to increase testing rates over the course of that month (Rough, 2020[60]). South Korea, which was one of the first countries affected, moved earlier than many other OECD countries by introducing local testing in mid-February and drive-through testing in early March (Dighe et al., 2020[61])
In one case, the authorities responsible for infection control during the pandemic were initially unable to receive data for the population they were responsible for. Prior to the pandemic, the German-speaking Community had delegated the responsibility for infection control to Wallonia. Shortly after the start of the pandemic, in March 2020, this responsibility was transferred back from Wallonia to the German-speaking Community. While policies made within the German-speaking Community sometimes differed from the rest of Wallonia as a result, most data (with the notable exception of vaccination data and surveillance in long-term care facilities) were not available in public reports for this sub-population before November 2020, which complicated monitoring the effectiveness of measures taken to combat the virus.
Belgium operated three additional surveys to monitor the situation in hospitals (Van Goethem et al., 2020[62]). From early March 2020 onwards, hospitals were surveyed daily on their surge capacity via the Incident Crisis Management System, the hospital surge capacity survey, and the Clinical Survey. These surveys recorded structural hospital information, such as the available beds in intensive care units (ICUs), the number of available ventilators and extracorporeal membrane oxygenation devices (ECMOs), and patient information (such as on risk parameters and patient outcomes), and informed the daily meetings of the HTSC. They were adapted several times over the course of the pandemic to respond to the need for additional information. Following a data migration of the Clinical Survey in mid-September and extensions of the data collection, such as the social security number, data linkages became possible and these allowed for a more comprehensive analysis (Van de Voorde et al., 2020[58]). Data was also collected directly from electronic medical records used by GPs to monitor both the pandemic and the needs of general practitioners, including their access to PPE, workload, and support needs, and helped to inform decision making of the Risk Assessment Group (RAG) (Vaes et al., 2022[54]).
These additional surveys and an extensive data collection in general have allowed Belgium to better monitor the outbreak and to introduce corresponding adjustments to its health system. Belgium is encouraged to save this knowledge for future pandemics, to maintain an infrastructure that could be quickly reactivated in future health emergencies, to work torwards a structure that records data from different health sectors, and to ensure that actors which are in charge of organising the health system response are equipped with the necessary information to successfully fulfil their role. Building on its experiences during the COVID-19 pandemic, Belgium could proactively anticipate how its formidable electronic data infrastructure could be even more quickly employed to monitor the pandemic and its impacts on the population and mount a rapid response that takes into account the needs of vulnerable populations. In Costa Rica, for example, the digital integration of its multi-disciplinary teams allowed health authorities to use the data in electronic medical records to help in risk assessments and prioritisation, the identification of vulnerable patients, delivery of medicines to people’s homes, and arranging virtual visits for hospitalised patients (OECD, 2023[63]).
Overall, Belgium managed to quickly set up a data infrastructure and to successfully integrate it into the organisation of the pandemic response. For example, the collection of hospital data allowed the HTSC to co-ordinate capacities, to monitor the effect of their decisions on patient outcomes, and to adjust its decisions accordingly. Similarly, the Task Force Vaccination and regional entities used vaccination data to monitor the progress of the vaccination campaign and to identify where additional, tailored approaches were needed. Belgium is strongly encouraged to maintain its data infrastructure, and to systematically include means to monitor infection outbreaks.
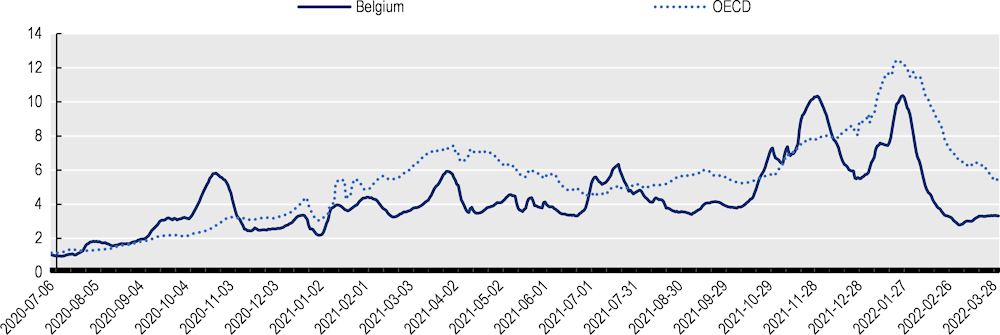
4.3.5. Belgium rapidly increased testing capacities in the first months of the pandemic
Following a slow start, Belgium managed to increase testing capacities and to reduce turnaround times, and testing and tracing played an important part in the mitigation of the virus and the deconfinement of the country (Willem et al., 2021[64]). Within the first weeks of the pandemic, the number of tests performed per 1 000 inhabitants in Belgium increased from below to considerably above OECD average. Over the period from 1 March 2020 to 31 March 2022, nearly 33 million tests were recorded on the national testing platform (Sciensano, 2023[65]). Daily reporting to a national database (healthdata.be) was mandatory. Overall, Belgium’s testing rates were close to the OECD average (Figure 4.11) (ECDC, 2022[66]).
Figure 4.11. Tests performed per 1 000 inhabitants in Belgium and the OECD
At the beginning of the pandemic, Belgium had very low testing capacities with only one laboratory, the National Reference Centre of the University Hospital of Leuven, performing tests against COVID-19. The country also faced a shortage in testing material and long turnaround times of several days. In addition, the testing protocol was initially very restrictive, with only symptomatic people returning from high-risk destinations eligible for COVID-19 tests, though this was broadened over the period from mid-March to June (Meurisse et al., 2021[67]). This limited Belgium’s initial capacity to understand and monitor the evolution of the pandemic in its country.
Belgium managed to increase the number of tests and turnaround times by increasing the number of laboratories, scaling up the workforce, and setting up effective financial incentives. In March and April 2020 alone, Belgium issued licenses to test against COVID-19 to 73 clinical microbiology laboratories. This was complemented by the federal testing platform, which was introduced in April 2020 to add additional test capacities. Pharmacists were allowed to perform rapid antigen tests from 12 July onwards, and beginning on 21 September 2021, Belgium granted the right to carry out laboratory tests to individuals without medical degrees. Different financing schemes helped to incentivise laboratories to increase capacities and reduce the turnaround time. Laboratories first received a financial guarantee to quickly set up and increase their capacities. Later, the payment was made conditional on reporting test results within 12 hours after performing the test, which managed to reduce the time between the sampling and reporting of the test result. As a result, average waiting times reduced from close to a week to less than one day within several weeks of the pandemic (INAMI, 2023[68]; Meurisse et al., 2021[67]).
The availability of self-tests greatly increased the total test coverage. It allowed individuals to quickly obtain a test result, to self-isolate, and to alert others in case of a positive test. From April 2021 onwards, self-tests were available in pharmacies at EUR 8 (later around EUR 5) per test, with a reduced price of EUR 1 for vulnerable groups. From July onwards, they were available in supermarkets for around EUR 2-6. Sales particularly increased around certain events such as the start of the Delta wave in October 2021 and the Christmas period (Lafort et al., 2023[69]).
Tracking and tracing efforts were further supported by the introduction of an app for contract tracing, and the availability of self-tests. The app Coronalert was launched on 30 September 2020 and alerted users of a potential high-risk contact after more than 15 minutes of exposure to a positive COVID-19 case within 2 meters or less using Bluetooth. From January 2021 onwards, the app was linked to COVID-19 apps of 10 other European countries, including France, Germany, and the Netherlands. The app was later retired in November 2022. Studies from Belgium about its effectiveness are lacking and it is not clear yet whether the benefits of the app justified its high costs. Evaluations from other OECD countries are mixed, with an evaluation from England and Wales showing that their app played a significant role in reducing the spread of the virus and helped prevent hospitalisations and deaths, whereas evaluations from Australia indicate limited effectiveness (Vogt et al., 2022[70]; Wymant et al., 2021[71]; Kendall et al., 2023[72]). Evaluations from Belgium identified limitations due to losses of information in the communication and time lags between the test results and the digital alert (Raymenants et al., 2022[73]; Geenen et al., 2023[74]). As in many other countries, concerns about privacy and data security in using the app were raised, with privacy concerns identified as a key driving factor among people who chose not to use or to discontinue use of the app (Jacob and Lawarée, 2020[75]; Walrave, Waeterloos and Ponnet, 2022[76]).
Box 4.1. Regional responses to testing and tracing
The testing and tracing itself was organised on the regional level, with the Interfederal Committee on Testing and Tracing serving as an advisory body to co-ordinate and harmonise the regions’ different testing and tracing strategies. Regions set up COVID-19 test centres and contracted with different providers to organise and perform these tests, such as hospitals and the Red Cross. Financing was shared by the federal and regional level. Costs for setting up test centres were borne by the regions, whereas the federal level covered costs for personnel and laboratories. “Testing villages” were set up to test a particularly high volume of people. For example, Wallonia converted the airport of Liège, the city of Antwerp in Flanders used a festival area, and Brussels set up a centre next to the Atomium. Following a positive test, call centres traced positive cases and their contacts by phone or home visits. These were set up by the regions and became operational in mid-May 2020 with the loosening of the first lockdown. They used outreach teams to visit people at their homes, particularly in vulnerable and hard-to-reach communities.
Across Belgium, some communities faced barriers of access to information and testing and turned to information from their home countries or social networks, which sometimes deviated from what was reported by Belgium (Nöstlinger et al., 2022[77]). Regions and municipalities introduced additional means to respond to these needs and to reach out communities with low testing rates and higher risks of transmission. In Brussels, for example, the contact centre operated in 15 languages during the peak of their activity. Antwerp set up a local contact tracing system where general practitioners reported index cases with complex need, such as limited language skills) to a network of Arabic and Berber-speaking volunteers following alerts by family physicians of outbreaks in certain communities (Verdonck et al., 2023[78]). In September 2020, this volunteer system was integrated in the Flemish structure of primary care (first line) zones. Antwerp also recorded outbreaks in the orthodox Jewish Community and sent out individual invitations for them to get tested. The co-operation with leading figures of the Jewish Community, such as rabbis and physicians, was essential in reaching out to the Jewish Community (Vanhamel et al., 2021[79]).
Despite Belgium’s success in quickly setting up and expanding testing capacities, some factors hampered the testing strategy. First, there were technical obstacles, such as a time lag between the infection and outbreak of symptoms, delays in the reporting of the test result, and a potential underreporting of high-risk contacts that might have limited the effect of the testing strategy (Proesmans et al., 2022[80]). Second, for some populations, difficult socioeconomic circumstances complicated complying with measures, such as isolation, even where testing and tracing policies may have been correctly implemented (Nöstlinger et al., 2022[77]). Third, parts of the population had privacy concerns. They opposed sharing private information, and / or reported false information, such as wrong addresses and phone numbers during contact tracing (Verdonck et al., 2023[78]). Similar privacy concerns presented a barrier to using the app (Walrave, Waeterloos and Ponnet, 2020[81]). Finally, parts of the population were not convinced of some of the measures. A lack of perceived benefits was identified to be the most important factor of not using the app Coronalert and increased with age (Walrave, Waeterloos and Ponnet, 2022[76]; Walrave, Waeterloos and Ponnet, 2020[81]).
Belgium’s initial difficulties with limited testing capacities hold vital lessons learned for future pandemics. Its focus on a single laboratory and the narrow case definition restricted the country’s ability to perform tests on a large scale and trace transmissions. Other countries, such as Germany , benefitted from a wide network of laboratories (Stoto et al., 2023[82]). Germany had already introduced a billing number for COVID-19 tests on 1 February 2020, allowing physicians to perform and bill tests from the very beginning of the pandemic.
4.3.6. Belgium’s COVID-19 vaccination campaign was largely successful and incorporated lessons learned from the first year of the pandemic
Belgium launched its vaccination campaign in early January 2021. Overall, the government managed a quick roll-out of the vaccination campaign and achieved a population coverage that ranks considerably above the OECD average. Vaccination also led to a drastic reduction in outbreaks, hospitalisation rates, and mortality rates in 2021, including in nursing homes (Crèvecoeur et al., 2022[83]; Catteau et al., 2021[84]).
By March 2022, the share of people vaccinated against COVID-19 was above the OECD average as well as the rates of its neighboring countries France, Germany, Luxembourg, and the Netherlands. 78% of the population, or a total of 9.14 million inhabitants, had completed the initial vaccination protocol compared to an OECD average of 73%. 63%, or 7.33 million inhabitants, had received a booster vaccination, positioning Belgium slightly above OECD average. Belgium has historically ranged above the OECD and EU average for routine vaccinations, such as seasonal influenza (OECD, 2021[85]).
Figure 4.12. Percentage of population having completed the initial vaccination protocol, as of March 2022
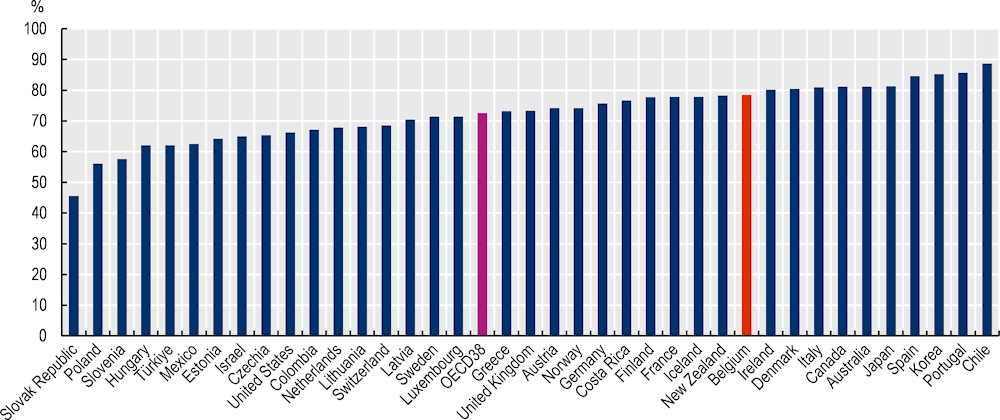
Note: The percentage represents the total number of people who received all doses prescribed by the initial vaccination protocol, divided by the total population of the country. Data are considered up to and including week 13 of the 2022 calendar year except for Luxembourg where data refer to mid-March 2023.
Source: Our World in Data (database accessed in May 2023).
Vaccination rates differ within Belgium, with the region of Flanders having the highest rate of people having received their first booster, with 84% of the population aged 18 and above having received a booster shot compared to 67% in Wallonia, 65% in Ostbelgien, and 48% in Brussels by the end of March 2022 (Sciensano, 2023[65]). This is in line with general vaccination patterns, with the population in Flanders historically displaying higher vaccination rates than Wallonia and Brussels for selected types of vaccination, such as against seasonal influenza for people aged 65 and above (KCE, 2022[86]).
COVID-19 vaccines were rolled out in three phases, first concentrating on high-risk populations, who were vaccinated in mass vaccination centres or nursing homes via mobile teams. Individuals were prioritised based on their exposure to COVID-19, risk of transmission, and risk of contracting severe COVID-19. Following greater availability of vaccinations and successful vaccination of high-risk groups, vaccinations shifted towards the wider population, and from mass vaccination centres to general practitioners and pharmacists.
This stepwise approach was very similar to other European countries (van Kessel et al., 2023[87]).
Phase Ia began in January-February 2021 and covered residents and staff in long-term care facilities, healthcare professionals working in the in- and outpatient sector, and other health professionals working in other parts of the healthcare sector.
Phase Ib, which began in April 2021, was aimed at individuals aged 65 and above, people aged 45-64 with risk factors, essential workers, and pregnant women. People with medical risk factors were identified by their general practitioners.
Phase II, which started in June 2021, addressed everyone aged 18 and above (Catteau et al., 2021[84]).
Boosters were offered to priority groups starting in September 2021, and to the entire population from November 2021.
The vaccination campaign was designed and co-ordinated by the Task Force Vaccination, which operated within the Corona Commissariat. Its main role consisted of designing and advising on the vaccination strategy, co-ordinating federal and federated authorities, defining priority rules and eligibility criteria, advising the Interministerial Conference on Public Health, and communicating the joint vaccination strategy to the public. Competencies were shared between the federal government, which managed the procurement of vaccines and participated in the joint procurement of the European Union, and the federated entities, which organised the roll-out of the vaccination in their given region. Regions had substantial flexibility in the implementation of the vaccination campaign and introduced tailored strategies to reach out to specific population groups. In the German-speaking Community, for example, personal invitations were organised by email and letter to targeted groups, with reservations possible both online and by telephone.
Box 4.2. Regional strategies to vaccinate vulnerable groups
In Belgium, a migrant background, being a single parent, and a low socio-economic status were negatively associated with being vaccinated (Cavillot et al., 2022[88]; Faes et al., 2022[89]). To improve vaccination rates among hard-to-reach communities, the federated entities introduced a set of outreach strategies and moved towards a more decentralised approach over time. All federated entities used “vaccination buses” that toured through their region to offer vaccinations in highly populated areas, such as public places, sports clubs, and cultural and religious venues. Brussels offered vaccinations at Ikea, Primark, Action, and Carrefour in areas with low vaccination rates, such as Molenbeek, and the city of Antwerp initiated a vaccination campaign in their zoo. Over the period from January to December 2021, Brussels complemented its 10 vaccination centres with 384 additional vaccination initiatives.
Additionally, Belgium employed mobile vaccination teams for the homeless (an estimated 17 000 individuals) and people without residency permit (sans-papiers, an estimated 85 000 to 160 000 individuals) (Task Force Vaccination, 2021[90]). These groups were identified by the federated entities in co-operation with regional actors, such as humanitarian organisations and charities. These actors played an important role in reaching out to vulnerable populations. For example, from May to September 2021, the team Mobivax from the Belgian Red Cross, Doctors Without Borders, and Samusocial performed 2 000 vaccinations of individuals who were otherwise unable to obtain a vaccination.
Mobile vaccination clinics and teams were widely used across the OECD to vaccinate individuals in vulnerable communities (Gupta et al., 2022[91]; ECDC, 2021[92]). In Belgium, they had already been successfully employed by Flanders during past measles outbreaks in hard-to-reach communities, such as orthodox Jewish Communities, the homeless and Roma people (Cornelissen et al., 2020[93]; Wyndham-Thomas, Boon and Van Damme, 2018[94]).
In addition, Belgium co-operated with religious leaders, who can play a key role in building trust and reaching communities that are otherwise hard to reach. For example, vaccinations were offered in Mosques and imams shared information about the vaccine on social media or during religious services.
A number of factors help to explain the relative success of Belgium’s vaccination campaign. First, it successfully mobilised and integrated healthcare workers. General practitioners played a key role in identifying individuals eligible for vaccination based on their medical records. Belgium successfully used medical records and claims data to identify high-risk individuals that qualified for prioritised access to vaccinations. Pharmacists were given access to information of the vaccination codes database, received a notification when an unvaccinated individual purchased from them, and could inform them about the vaccination. From mid-March 2022 onwards, pharmacists were allowed to perform vaccinations.
Second, it set up a comprehensive data set that allowed the country to monitor the vaccination campaign. All vaccinations had to be registered in a national registry (Vaccinnet+), which was originally initiated by the Flemish government in 2004 as a dedicated platform for health professionals to order vaccines (Vaccinnet). The database collects personal information on the vaccinated person, the vaccine, and the vaccinating entity (Catteau et al., 2021[84]). This data was linked with five additional sources of personal, demographic, and clinical data under the programme LINK-VACC, which allowed healthcare professionals to target specific people for vaccination (Catteau et al., 2021[84]).
Third, it successfully built on already established structures, for example by converting testing centres into vaccination centres in many municipalities. OECD data indicates that just over half of municipalities (52%) reported feeling sufficiently prepared to implement the “test and trace” COVID-19 case strategy, in terms of human resources, space, distribution of PPE, and other considerations (OECD, 2023[95]). In contrast, 68% of municipalities reported feeling sufficiently prepared to implement the vaccination strategy (OECD, 2023[95]).
Fourth, Belgium has historically performed well in vaccinations and could build on this for the COVID-19 vaccination campaign (Turner et al., 2022[96]). The willingness to get vaccinated was considerably higher than in some other European countries, such as Italy and France (de Meijere et al., 2023[97]). As a result, it did not need additional policy interventions, such as large financial incentives and performance targets for physicians (Milstein et al., 2022[98]).
Despite the broad success of the vaccination campaign, some indicators unveil further room for improvement. Vaccination rates of some groups of healthcare workers missed the target of the European Commission of 80% by May 2021, and regional differences persisted over the course of the vaccination campaign (Boukaert, Devrise and Van den Heede, 2021[99]; Catteau et al., 2021[84]). On 31 October 2021, the national average of 89.5% of health workers having completed the initial vaccination protocol varied by federated entity and ranged from 72.9% in Brussels to 94.7% in Flanders (Catteau et al., 2021[84]).
Moreover, vaccine hesitancy remains an important concern. In Belgium, the willingness to get vaccinated was generally lower in French-speaking parts of the population and among the younger and the less educated, and those that felt less at risk (Kessels, Luyten and Tubeuf, 2021[100]; Gbenonsi et al., 2022[101]). Distrust in the vaccine, such as its safety and effectiveness, was a large contributing factor to vaccine hesitancy among both the general population and healthcare workers (Schmitz et al., 2022[102]; Verger et al., 2021[103]). Regions reached out with letters and information campaigns to certain workforce groups, and the federal government considered following some other OECD countries, such as France and Germany, with the introduction of a vaccine mandate for healthcare workers. Plans for a mandate were eventually dropped due to higher vaccination rates among healthcare workers and the surge of the omicron variant.
In July 2021, Belgium introduced a Covid Safe Ticket, which aimed to reduce the spread of the virus, and offered access to certain activities, such as restaurants and bars, based on the COVID-19 status of the individual. It was later expanded to include the vaccination status and might have provided an incentive to get vaccinated. Belgium followed other countries, who had introduced similar policies before (van Kessel et al., 2023[87]), such as Italy with its Super Green Pass (January 2021), and Denmark with its Coronapas (since May 2021). Germany had started easing regulations for vaccinated individuals since May 2021, while France launched the Pass sanitaire in June 2021 as part of its deconfinement strategy. The Covid Safe Ticket was contested and the magnitude of its effect on reducing the spread and increasing vaccination rates in Belgium is unclear. Individuals did report getting vaccinated to travel more easily, regain some of their freedom, and avoid multiple tests for the Covid Safe Ticket, so a positive effect of the Covid Safe Ticket is possible. However, there were concerns that the Covid Safe Ticket could promote a sense of false security, increase social division, stigmatise certain population groups, and increase resistance against public health measures (Gbenonsi et al., 2022[101]). Those with a positive attitude towards the ticket were largely more risk-sensitive and more likely to be vaccinated to begin with, and were disappointed by the limited effect of the ticket on reintroducing pre-Covid activities (Vermeulen et al., 2023[104]). Evidence from other countries indicates a positive effect of certificates on vaccinations prior to and shortly after the introduction of the policy, but they might not have reduced vaccine hesitancy as such, and its long-term effects are unclear (Mills and Rüttenauer, 2022[105]; Karaivanov et al., 2022[106]; Gbenonsi et al., 2022[101]; Oliu-Barton et al., 2022[107]; Ward et al., 2022[108]).
Belgium’s vaccination campaign consisted of some successful policies while at the same time holding lessons learned for future pandemics. As in other countries, such as France, Germany, and the Netherlands, Belgium prioritised individuals at high risk of infection and severe COVID-19 (van Kessel et al., 2023[87]). The innovative use of claims data, medical records and additional data, and the co-operation with GPs has greatly helped to identify these groups. Additional attention could have been devoted to approaching and building trust among hard-to-reach communities, for example through an earlier roll-out of vaccinations to GPs and even stronger co-operation with on-the-ground services and spokespersons of hard-to-reach communities, such as religious and other local community leaders, as happened in Italy and the United States (van Kessel et al., 2023[87]; Evans, Webster and Flores, 2021[109]). Several regions in Belgium launched initiatives in this regard (see Box 4.2), providing a good starting point to launch these initiatives in a more intensive and timely way in future pandemics.
4.3.7. A high number of beds and rapidly organised response prevented hospitals from being overwhelmed for most of the pandemic
Belgium was able to build on a relatively high supply of acute care beds with a quickly organised hospital response that was informed by daily reports from every acute care hospital in the country. These factors allowed Belgium to avoid overwhelming hospitals in the way some countries experienced during the pandemic, particularly at its start. Compared with other OECD countries, the number of hospital beds per capita is relatively high in Belgium, at 5.5 per 1 000 population, compared to 4.3 per 1 000 population across 37 OECD countries on average (OECD, 2023[15]). At 17.2 beds per 100 000 population in 2021, the number of ICU beds per capita in Belgium is largely in line with the average across 29 OECD countries (16.9 beds per 100 000 population) (OECD, 2023[15]).
While half of hospitals reported having a pandemic preparedness plan in place prior to the COVID-19 pandemic (13 of 26 reporting), the majority – nearly two-thirds – reported that no pandemic preparedness exercises had been undertaken at their hospital prior to COVID-19 (17 of 26 reporting), with only one of 26 hospitals reporting that exercises specifically in anticipation of the arrival of COVID-19 in Belgium had been undertaken (OECD, 2023[55]).
Experts affiliated with the government’s pandemic response began informally assessing the capacity of the hospital system to absorb COVID-19 patients in late January 2020, and a decision was taken at the end of February 2020 to establish the Hospital Transport and Surge Capacity Committee (HTSC), which would report to the RMG (see Chapter 3). The HTSC was tasked by the RMG with monitoring the number of COVID-19-patients across Belgian hospitals, discussing issues related to hospital capacity and patient flow, and proposing policy decisions to the RMG that would allow the best implementation of capacity and transport planning in the hospital sector. Members comprised policymakers from the Federal Public Service Public Health (FPS Public Health), academic experts, representatives of healthcare institutions, representatives from federated entity administrations, the Ministry of Defense, and French and Flemish emergency hospital planning co-ordinators. Beginning on 14 March, all hospitals were also required to activate their emergency plans, while general, university and rehabilitation hospitals, as well as private clinics, were required to postpone all elective services.
Box 4.3. The Hospital and Transport Surge Capacity Committee
The Hospital & Transport Surge Capacity Committee (HTSC) was set up as an advisory body within FPS Public Health to ensure sufficient hospital capacities and to co-ordinate patient transfers where necessary. It officially became operational on 6 March 2020. The committee designed a hospital contingency plan, which defined three distinct phases to monitor the situation in Belgium’s Intensive Care Units (ICUs) and to act accordingly. It distinguished between three phases. Depending on the phase, 15% to 60% of ICU beds should have been reserved to COVID-19 patients. In phase 2, hospitals would need to activate additional ICU capacities within seven days.
The committee undertook several measures to ensure sufficient capacities to COVID-19 patients while maintaining routine delivery of care. These included the postponement of all elective procedures and discharge of patients where possible, capacity increases, for example by re-training non-ICU personnel for ICUs, and the transfer and reallocation of patients to hospitals with sufficient capacities. In most cases, transfers took place within a hospital network (loco-regional hospital network). Hospitals could either reach out directly to other hospitals or the province or request a transfer from the Patient Evacuation Centre. The number of transfers varied a lot. For example, from 1 March to 30 June, only 629 transfers took place, in contrast to 1 178 transfers from 1 October to 15 November 2020.
The HTSC successfully operated thanks to a strong leadership in the committee, and a common agreement on and adherence to the confidentiality and communication strategy (OECD, 2022[110]; Van de Voorde et al., 2020[58]). The data that was collected by Sciensano and discussed by the HTSC offered a rich data base that allowed to introduce tailored policy interventions, to understand their effects on patient outcomes, and to adjust them if necessary. The extensive data reporting requirements put in place by the HTSC also allowed the Committee to monitor the impact of the policies they were adopting, with a number of policy changes, notably around patient discharge and transfer, implemented between waves as a result. For example, it allowed the HTSC to revise transfer recommendations after inspecting patient outcomes post transfer (Taccone et al., 2021[111]).
4.3.8. The pandemic has underlined the need for a hospital payment and funding reform
Hospitals are largely a federal competency. In 2022, Belgium had 103 hospitals (excluding mental health hospitals), with the majority being private non-profit (72%) and the remainder public. Capital and investment costs are covered by federated entities, whereas running costs are covered by the federal state. The payment system depends on the type of service. Nursing and non-medical costs are covered by an annual budget, whereas medical and paramedical activities are largely paid on a fee-for-service basis.
The Belgian hospital payment scheme, where an annual budget represents a significant share of a hospital’s total annual income, offers more financial stability and resilience to shocks than payment schemes which are based almost exclusively on activity, but the budget share of the total hospital income was likely too low to be financially sufficient to cover fixed costs and to buffer sudden changes in volume. In addition, hospitals were tasked with capacity increases. As a result, the government offered financial support to hospitals. In April 2020, it distributed a total of EUR 1 billion to general hospitals, and another EUR 500 million in July and October each to general and psychiatric hospitals (FPS Public Health, 2023[47]). Costs were covered by the FPS Health and the INAMI-RIZIV. Furthermore, hospitals received additional financial support of a bit more than EUR 2 million annually for patient transports.
Belgium is reforming its hospital payment system, joining a group of countries, such as Denmark, France, Germany and the United Kingdom (England) in order to move from paying for volume, to paying for value. The country had already recognised the need for a reform prior to the crisis to reduce the fragmentation and the pandemic has only further underlined the need for this reform. It is moving towards payment systems that aim at moving from volume to value, at improving continuity, patient-centeredness, and quality of care. First, it intends to reduce fragmentation and unnecessary interventions by integrating cost components into diagnosis-related group (DRG) tariffs that were previously paid separately (all-in) and intends to move towards bundled payments in the longer run. At the same time, the schedule of fees for medical acts will be revised. Second, it aims at shifting the delivery of care from the in- to the outpatient sector by making the outpatient treatment the default option for a set of surgical treatments and by recalculating payments.
These reforms are in line with payment reforms in other OECD countries. For example, Canada (Ontario), France, Norway, and the United States are experimenting with bundled payments, and Austria, Denmark, France, and Norway, are using financial incentives to shift care from the in- to the outpatient sector. Several countries, such as Denmark, England, France, and the United States are moving towards a combination of diagnosis-related groups and global budgets to improve the financial stability of hospitals and make them less vulnerable to volume changes. Some of these payments are adjusted based on quality indicators to incentivise quality improvements (Milstein and Schreyögg, 2024[112]). Belgium should continue its reform process, and to make use of the experiences of other OECD countries where necessary.
4.3.9. Increasing workforce shortages are a pressing concern
The pandemic had severe effects on the health workforce, and the effects are likely to be long-lasting. Prior to the pandemic, Belgium ranked below OECD average for practicing doctors per capita, and above average for practicing nurses per capita. In 2021, it recorded a rate of 3.3 practicing doctors per 1 000 population compared to an OECD average of 3.7, and 11.1 nurses per 1 000 population against an OECD average of 9.2 (OECD, 2023[15]).
The pandemic negatively affected the healthcare workforce due to an increased workload, shortage of PPE, public pressure, and constant exposure to emotionally challenging tasks. The work dissatisfaction among nurses increased from about one in four (27%) in 2019 to more than a third (39%) in 2021/22. Subsequently, the intention to quit increased among nurses by about 12 percentage points from around 32% in 2009 and 2019 on general wards to 43.9% in late 2021 to early 2022 on ICU wards (KCE, 2019, 2022). Nurses reported an increasing workload and shortages of PPE as major obstacles in their daily work (Vaes et al., 2022[54]). The mental health of healthcare workers was also heavily affected by the pandemic, with nurses and younger healthcare workers being particularly affected (Tiete et al., 2021[113]; Vanhaecht et al., 2020[114]).
The intention to quit appears not to be limited to nurses. Health care workers in long-term care facilities and hospitals have left the workforce, most notably after the second wave. The disagreement with some measures, such as isolating residents in long-term care facilities, may have in part fueled the decision to quit, as did the intensity of working through the first waves of the pandemic.
As in other OECD countries, Belgium offered financial premiums to compensate for additional tasks over the pandemic (Waitzberg et al., 2022[115]). Personnel in hospitals and home care, general practitioners and those in training working in the in- or outpatient sector, and medical specialists in training in the inpatient sector during the period from 1 September to 30 November 2020 were eligible for a bonus of up to EUR 985 gross (INAMI, 2022). Nurses received a voucher of EUR 300.
The role of certain healthcare professionals was also expanded to meet the needs of the pandemic. Pharmacists were allowed to perform rapid antigen tests beginning in July 2020, while lab tests were allowed to be conducted by professionals without a medical degree beginning in September 2021.
For mental health, healthcare workers largely relied on support from their peers (Vanhaecht et al., 2020[114]). Some of them indicated the need for more professional support and leadership. In a survey among 4 509 healthcare workers in Flanders, 18% mentioned the need for more professional support from a psychologist, and 27% wished for more support from their leadership (Vanhaecht et al., 2020[114]). In some instances, they received additional psychological support from the regions.
The health workforce represents one of the most critical areas of investment to strengthen health systems resilience across countries (OECD, 2023[63]). The COVID-19 pandemic has likely only further exacerbated existing workforce challenges in the health sector in Belgium. Continuing to invest in policies to encourage recruitment and retention, including changes to remuneration schemes and promoting task-sharing – as were pursued by Belgium even prior to the pandemic – remain important to address both pre-existing workforce shortages and those exacerbated by the pandemic.
4.3.10. Primary care played a strong role in the pandemic response, with some variation across federated entities
Primary care is a competency of the federated entities, leading to regional differences in how the pandemic response was organised in primary care. However, in all entities primary care played an important role in the health system’s response to COVID-19.
In Flanders, for example, the newly created 60 primary care / first line zones, covering roughly 100 000 inhabitants each, which had come into effect only shortly before the pandemic to co-ordinate the activities of local authorities and health providers, played an important role in connecting what was happening on the ground to decisions made at the federal and regional level. Each first line zone included a COVID co-ordinator who was able to communicate to the Flemish government the needs in their zones and were in some cases able to co-ordinate the pandemic response across different actors in the area – including not only primary care physicians but also schools and nursing homes. Such locally co-ordinated efforts helped to strengthen the pandemic response at the local level and can be built on both for strengthening primary care and for responding resiliently to crises.
Following the establishment of the HTSC at the beginning of March, the recognition of possible challenges in co-ordination at the primary care level led to the proposal and development of the Primary and Outpatient Surge Capacity Committee (POSC) in mid-March (Primary Care and Outpatient Surge Capacity Committee, 2020[116]). As with the HTSC, the POSC was co-ordinated through FPS Public Health and made recommendations to the RMG. It comprised of representatives from the federated entities, hospital federations, general practitioners, the COVID-19 scientific committee, and policymakers from FPS Public Health. Policymakers, recognising that many local initiatives had been undertaken to improve triage, crisis management and nursing homes, and other local responses, aimed to streamline and co-ordinate practices through the Committee to facilitate a clearer and more uniform front line response (Primary Care and Outpatient Surge Capacity Committee, 2020[116]).
However, while the HTSC played an indispensable role in co-ordinating the hospital response and mitigating capacity challenges in the sector, the POSC’s role in streamlining the primary care response was weaker. This may in part have been related to the governance and relative fragmentation of the primary care sector, given the different organisation of primary care across federated entities. There were also challenges in communication and consensus-building across practitioners, with a high number of associations and syndicates representing general practitioners, some of whom did not always agree upon the role primary care should be expected to take during the pandemic (OECD, 2023[43]).
Indeed, results from the OECD Survey of General Practitioners on COVID-19 management underscores the divergent views of general practitioners in their role during the pandemic. 48% of survey respondents reported feeling sufficiently involved by health authorities in the COVID-19 response, with 52% responding that they felt they had not been sufficiently included. Overall, some 40% of survey respondents reported that they wished they had been given a greater role in supporting the care continuity of patients during the pandemic, with about one-fifth also reporting that they would have liked to have had a bigger role as a source of information for patients and the public (21%), and in vaccination campaigns (20%).
The majority of GPs responding to the OECD Survey of General Practitioners reported that they did not receive any training on caring for patients with COVID-19, with just three in ten reporting they had received training for caring for people with COVID-19, though others may have been offered training they did not accept.
General practitioners were nearly evenly divided in whether they felt they had been kept sufficiently informed about changes to care delivery that were implemented during the pandemic, with 49% (n=198) reporting they had felt sufficiently informed, and 51% (n=208) reporting they did not feel they had been kept sufficiently informed of changes to care delivery over the course of the pandemic (OECD, 2023[43]).
Even as many general practitioners reported feeling insufficiently included in the pandemic response, the majority of respondents to the OECD Survey of General Practitioners reported that they involved themselves in outreach to their most vulnerable patients during the pandemic, with the majority of responding general practitioners reported that they had engaged in outreach. The majority of general practitioners provided additional information during consultations to medically or socially vulnerable populations. More proactive engagement, including reaching out personally or sharing information with the Vaccination Task Force to enable priority targeting during the initial vaccination roll-out, was less frequently practiced during the pandemic (Figure 4.13).
Figure 4.13. Proportion of general practitioners reporting they engaged in outreach to vulnerable groups
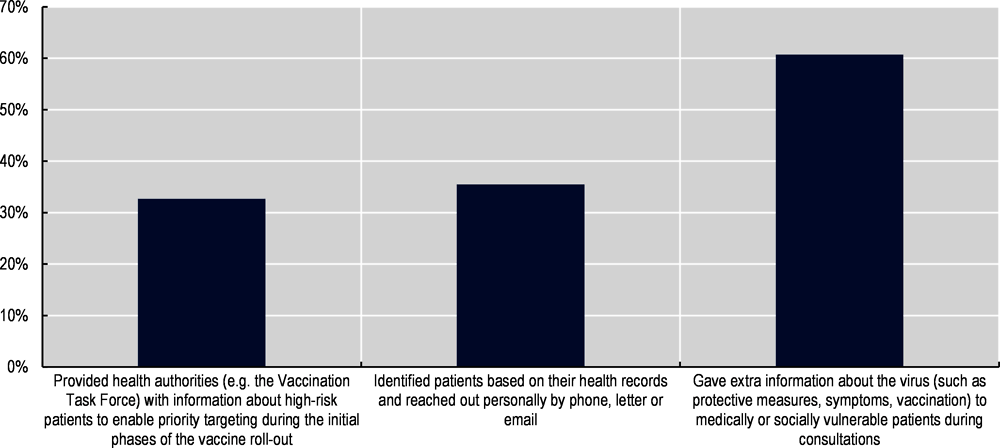
Note: n=392.
Source: OECD (2023[43]), OECD Survey of General Practitioners in the Context of OECD’s Evaluation of Belgium’s COVID-19 response.
In some cases, existing roles for primary care in surveillance were severely impacted during the crisis. Prior to the pandemic, Sciensano had in place a network of hospitals and general practitioners (“lookout doctors”) who registered acute respiratory infections, flu outbreaks, diarrheal outbreaks and other infectious diseases. Approximately 120 general practice cabinets participate in the network (Sciensano, 2023[117]). While the surveillance network of hospitals was rapidly scaled up to include mandatory reporting from all hospitals, the functioning of the sentinel network of general practitioners was disrupted in the first year of the pandemic.
Belgium benefitted from local structures in its pandemic response, including the employment of first-line zones and health roundtables in some federated entities. Other countries undertook similar efforts to strengthen local structures and expand the role of primary care to reach vulnerable groups. For example, Canada, France, and the United States have built multidisciplinary approaches, such as multi-professional health centres (Centres de Santé) in France (OECD, 2021[118]).
4.3.11. Organisations close to the ground helped to reach vulnerable groups, while lack of data and competing priorities sometimes hampered a more effective government response
Policymakers recognised early on the particularly harmful effects the pandemic could have on vulnerable groups, and took steps to try to protect the most vulnerable populations from both the virus itself and from the social and economic impacts of the protective measures adopted. In Brussels, for example, the Fédération des Services Sociaux was engaged in mid-March 2020 to help create a plan of action for how to reach vulnerable populations, such as people living on the streets, to ensure they would still receive needed services should a shutdown occur. Homeless and undocumented populations were the initial focus of such efforts, which included temporarily housing homeless populations in empty hotels. In Flanders, first line zones created locally organised outreach teams to help reach particularly vulnerable populations and explain lockdown and other policies to vulnerable groups affected by these changes. In Wallonia, a working group on vulnerable groups was quickly set up, focusing initially on victims of domestic violence, homeless populations, and people with severe mental illness. Similar outreach efforts that aimed to ensure care would be accessible where vulnerable people were located were made in other OECD countries, such as through the creation of Community Assessment Hubs in Ireland and the establishment of “Schnupfen-Boxen” multidisciplinary primary care teams in Austria (Berchet, Bijlholt and Ando, 2023[18]).
At the same time, the results of efforts to integrate representatives of marginalised and vulnerable groups into more formalised response structures, such as the GEMS, were mixed. While the presence of such voices on expert groups can help to raise the attention given to more vulnerable populations, the wide scope of considerations under the mandate of GEMS and the many groups and interests represented meant that the needs of vulnerable groups were not necessarily prioritised.
Throughout the pandemic and particularly in its initial months, a lack of data on vulnerable groups hampered a more systematic response. Certain measures taken – in some cases effectively – to target vulnerable groups, such as identifying vulnerable populations through their medical records to identify priority vaccination groups, were predicated on having relationships with general practitioners and being at least marginally connected to parts of the Belgian health and social security system. For the most deprived populations, including homeless populations and undocumented persons, the almost entire lack of available data made it difficult to target measures or monitor their progress among these populations. Here, the knowledge of on-the-ground community services is particularly indispensable in ensuring the needs of vulnerable populations are not overlooked or deprioritised during crises. Belgium should use the experience of the pandemic to expand the data collection and strengthen the co-operation with on-the-ground services.
Belgium enjoys a strong civil society and on-the-ground social services. Their insights were integrated to some extent, for example through the Task Force Vulnerables, the activities of Médecins Sans Frontières and the Belgian Red Cross in organising and managing the pandemic response. Belgium can strengthen and formalise this approach by systematically integrating them, by using a more comprehensive definition of vulnerable groups beyond the directly visible ones, such as the homeless, and by giving them the same (political) weight as other actors.
4.4. Summary of main recommendations
The COVID-19 pandemic severely affected the health system in Belgium. Beyond the immediate health impacts of the virus, the pandemic has laid bare weaknesses in the healthcare system that have been further stressed by ongoing needs linked to COVID-19, including delays in care, demands for care for long COVID, and an increase in demand for mental health services. At the same time, there is an important opportunity for Belgium to learn from the challenges of the pandemic to improve its healthcare system and increase its resilience and preparedness for future health emergencies.
4.4.1. Build structural and organisational capacities to quickly respond to crises
Define clear responsibilities for health crisis response by ensuring that support structures are articulated in advance and fit for purpose, actors are equipped with the information and authority they need to make informed decisions, and crisis management in the FPS Public Health is reinforced.
Set up and strengthen co-ordination mechanisms between health actors at the local level, including between hospitals, long-term care facilities and primary care to strengthen primary and long-term care responses.
Reform the way providers are paid to move from volume to value, to improve continuity of care, and to improve the resilience towards external shocks by expanding the budget component.
Improve the long-term care response, including strengthening inter-federal co-ordination and investing in measures to improve infection control in nursing homes.
Systematically prioritise vulnerable groups, including by proactively integrating them into decision making, and improve evidence-based responses for vulnerable populations, including through further data disaggregation.
4.4.2. Further strengthen innovative responses and structures set up during the pandemic
Ensure that innovative data infrastructures developed during the pandemic, such as the hospital data collection under the HTSC, are maintained and can be used to improve performance and outcomes in the longer term.
Take advantage of Belgium’s strong linked data architecture by advancing data linkage capabilities across data sets, including making more use of data from the Crossroads Bank for Social Security.
Monitor the long-term effects of the pandemic on the population, including by evaluating the impacts of long COVID on health outcomes and labour market participation.
Continue to invest in strengthening the health workforce and respond the long-term effects of the pandemic on the well-being and workforce participation of healthcare professionals.
References
[17] Aburto, J. et al. (2022), “Significant impacts of the COVID-19 pandemic on race/ethnic differences in US mortality”, Proceedings of the National Academy of Sciences, Vol. 119/35, https://doi.org/10.1073/pnas.2205813119.
[48] Belgian Cancer Registry (2022), Approximately 2700 missing cancer diagnoses in first two years of the COVID-19 pandemic in Belgium, https://kankerregister.org/media/docs/cijfersoverkanker/March2022-COVID-v6_ENG.pdf.
[18] Berchet, C., J. Bijlholt and M. Ando (2023), “Socio-economic and ethnic health inequalities in COVID-19 outcomes across OECD countries”, OECD Health Working Papers, No. 153, OECD Publishing, Paris, https://doi.org/10.1787/6c2a96c9-en.
[99] Boukaert, N., S. Devrise and K. Van den Heede (2021), Couverture vaccinale du personnel des hôpitaux et maisons de repos et de soins contre le COVID-19. Une analyse cross-sectionelle. D//2020/10.2733/27., KCE.
[30] Bruggeman, H. et al. (2022), “Anxiety and Depression in Belgium during the First 15 Months of the COVID-19 Pandemic: A Longitudinal Study”, Behavioral Sciences, Vol. 12/5, p. 141, https://doi.org/10.3390/bs12050141.
[3] Bustos Sierra, N. et al. (2021), Excess Mortality During the First and Second Waves of the COVID-19 Epidemic in Belgium: Data from 10 March 2020 to 14 February 2021, https://www.sciensano.be/sites/default/files/be-momo_report_excess_mortality_during_the_covid-19_epidemic_in_belgium.pdf.
[7] Bustos Sierra, N. et al. (2020), “All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century”, Archives of Public Health, Vol. 78/1, https://doi.org/10.1186/s13690-020-00496-x.
[25] Castanares-Zapatero, D. et al. (2021), Long COVID: Pathophysiology - epidemiology and patient needs, https://doi.org/10.57598/R344C.
[84] Catteau, L. et al. (2021), Couverture vaccinale et impact épidémiologique de la campagne de vaccination COVID-19 en Belgique. Données jusqu’au 31 octobre 2021 inclus, Sciensano, https://www.sciensano.be/fr/biblio/couverture-vaccinale-et-impact-epidemiologique-de-la-campagne-de-vaccination-covid-19-en-belgique.
[88] Cavillot, L. et al. (2022), “COVID-19 vaccination uptake in Belgium: socioeconomic and sociodemographic disparities”, European Journal of Public Health, Vol. 32/Supplement_3, https://doi.org/10.1093/eurpub/ckac129.046.
[51] CIN-NIC (2020), Enquete Intermutualiste: Téléconsultations, https://gcm.rmnet.be/clients/rmnet/content/medias/rapport_intermut_enquete_teleconsultations.pdf.
[93] Cornelissen, L. et al. (2020), “High number of hospitalisations and non-classical presentations: lessons learned from a measles outbreak in 2017, Belgium”, Epidemiology and Infection, Vol. 148, https://doi.org/10.1017/s0950268820000278.
[83] Crèvecoeur, J. et al. (2022), “Change in COVID19 outbreak pattern following vaccination in long-term care facilities in Flanders, Belgium”, Vaccine, Vol. 40/43, pp. 6218-6224, https://doi.org/10.1016/j.vaccine.2022.09.028.
[29] Daly, M., A. Sutin and E. Robinson (2020), “Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study”, Psychological Medicine, Vol. 52/13, pp. 2549-2558, https://doi.org/10.1017/s0033291720004432.
[97] de Meijere, G. et al. (2023), “Attitudes towards booster, testing and isolation, and their impact on COVID-19 response in winter 2022/2023 in France, Belgium, and Italy: a cross-sectional survey and modelling study”, The Lancet Regional Health - Europe, Vol. 28, p. 100614, https://doi.org/10.1016/j.lanepe.2023.100614.
[21] Decoster, A., T. Minten and J. Spinnewijn (2021), “The Income Gradient in Mortality during the Covid-19 Crisis: Evidence from Belgium”, The Journal of Economic Inequality, Vol. 19/3, pp. 551-570, https://doi.org/10.1007/s10888-021-09505-7.
[61] Dighe, A. et al. (2020), “Response to COVID-19 in South Korea and implications for lifting stringent interventions”, BMC Medicine, Vol. 18/1, https://doi.org/10.1186/s12916-020-01791-8.
[66] ECDC (2022), Evaluation of the SARS-CoV-2 testing policy in Belgium from June to December 2021, European Centre for Disease Prevention and Control.
[92] ECDC (2021), Overview of the implementation of COVID-19 vaccination strategies and deployment plans in the EU/EEA, European Centre for Disease Prevention and Control.
[10] Eurostat (2023), Excess mortality - statistics, https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Excess_mortality_-_statistics#Excess_mortality_in_the_EU_during_COVID-19_pandemic.
[109] Evans, A., J. Webster and G. Flores (2021), “Partnering With the Faith-Based Community to Address Disparities in COVID-19 Vaccination Rates and Outcomes Among US Black and Latino Populations”, JAMA, Vol. 326/7, p. 609, https://doi.org/10.1001/jama.2021.12652.
[89] Faes, C. et al. (2022), “Geographical variation of COVID-19 vaccination coverage, ethnic diversity and population composition in Flanders”, Vaccine: X, Vol. 11, p. 100194, https://doi.org/10.1016/j.jvacx.2022.100194.
[44] Fomenko, L. (2023), OECD analysis using data from PRICOV-19 Study: Quality and safety in primary care in times of COVID-19.
[47] FPS Public Health (2023), Key data in healthcare: COVID-19 - period March 2020-October 2022, https://www.health.belgium.be/sites/default/files/uploads/fields/fpshealth_theme_file/blikvanger_covid-ii_en_23.02.02.pdf.
[101] Gbenonsi, G. et al. (2022), “Factors Associated With COVID-19 Vaccination Among Individuals With Vaccine Hesitancy in French-Speaking Belgium”, JAMA Network Open, Vol. 5/9, p. e2234433, https://doi.org/10.1001/jamanetworkopen.2022.34433.
[74] Geenen, C. et al. (2023), “Individual level analysis of digital proximity tracing for COVID-19 in Belgium highlights major bottlenecks”, Nature Communications, Vol. 14/1, https://doi.org/10.1038/s41467-023-42518-6.
[40] Godderis, L. (2021), Mental health of Belgian population: update 18/12/2021, https://www.brain-helicon.be/evidence/indirect-effects/54-mental-assessment-group-reports (accessed on 2023).
[91] Gupta, P. et al. (2022), “Mobile Health Services for COVID-19: Counseling, Testing, and Vaccination for Medically Underserved Populations”, American Journal of Public Health, Vol. 112/11, pp. 1556-1559, https://doi.org/10.2105/ajph.2022.307021.
[38] Healthy Belgium (2023), Key data in healthcare: Funding for psychological support, https://www.healthybelgium.be/en/key-data-in-healthcare/covid-19/funding/funding-for-psychosocial-support.
[68] INAMI (2023), Note d’évaluation concernant la Plateforme fédérale de testing COVID-19, INAMI, https://www.riziv.fgov.be/SiteCollectionDocuments/note_evaluation_plateforme_federale.pdf.
[46] INAMI (2022), Monitoring COVID-19: L’impact de la COVID-19 sur le remboursement des soins de santé, Rapport 2021, Mise à jour février 2022, Institut national d’assurance maladie-invalidité, https://www.inami.fgov.be/SiteCollectionDocuments/monitoring_COVID19_update_fevrier_2022.pdf.
[50] Institut national d’assurance maladie-invalidité (2022), Continuité et sécurité des soins: avis médicaux à distance par les maisons médicales et les postes de garde, https://www.inami.fgov.be/fr/covid19/Pages/continuite-securite-soins-avis-medicaux-telephone-postes-garde-mg.aspx#:~:text=postes%20de%20garde-,Continuit%C3%A9%20et%20s%C3%A9curit%C3%A9%20des%20soins%20%3A%20avis%20m%C3%A9dicaux%20%C3%A0%20distance%20par,l.
[26] Institut national d’assurance maladie-invalidité (2022), COVID long : Remboursement des soins en cas de symptômes COVID-19 persistants, https://www.inami.fgov.be/fr/themes/cout-remboursement/maladies/Pages/post-covid-remboursement-soins-1re-ligne-symptomes-persistants.aspx.
[75] Jacob, S. and J. Lawarée (2020), “The adoption of contact tracing applications of COVID-19 by European governments”, Policy Design and Practice, pp. 1-15, https://doi.org/10.1080/25741292.2020.1850404.
[4] Jurcevic, J. et al. (2023), Epidemiology of COVID-19 mortality in Belgium from wave 1 to wave 7 (March 2020 – 11 September 2022), Sciensano, https://www.sciensano.be/en/biblio/epidemiology-covid-19-mortality-belgium-wave-1-wave-7-march-2020-11-september-2022.
[106] Karaivanov, A. et al. (2022), “COVID-19 vaccination mandates and vaccine uptake”, Nature Human Behaviour, Vol. 6/12, pp. 1615-1624, https://doi.org/10.1038/s41562-022-01363-1.
[86] KCE (2022), Health System Performance Assessment: care for people with chronic conditions, https://www.healthybelgium.be/metadata/hspa/P4.pdf.
[72] Kendall, M. et al. (2023), “Epidemiological impacts of the NHS COVID-19 app in England and Wales throughout its first year”, Nature Communications, Vol. 14/1, https://doi.org/10.1038/s41467-023-36495-z.
[100] Kessels, R., J. Luyten and S. Tubeuf (2021), “Willingness to get vaccinated against Covid-19 and attitudes toward vaccination in general”, Vaccine, Vol. 39/33, pp. 4716-4722, https://doi.org/10.1016/j.vaccine.2021.05.069.
[45] Khan, Y., A. Bruyneel and P. Smith (2022), “Determinants of the risk of burnout among nurses during the first wave of the COVID‐19 pandemic in Belgium: A cross‐sectional study”, Journal of Nursing Management, Vol. 30/5, pp. 1125-1135, https://doi.org/10.1111/jonm.13624.
[69] Lafort, Y. et al. (2023), “Were SARS-CoV-2 self-tests used for their intended purpose? The experience in Belgium”, BMC Health Services Research, Vol. 23/1, https://doi.org/10.1186/s12913-023-09704-0.
[34] L’Agence InterMutualiste (2023), ATLAS IMA website, https://www.aim-ima.be/Atlas-AIM?lang=fr (accessed on 14 August 2023).
[37] Lasserre, S. and A. Misson (2021), Lieux de liens: Maillons essentiels dans les parcours de soins: Recensement, analyse et recommandations, https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwigsMypp8OBAxXyUKQEHbkVIvIQFnoECBYQAQ&url=https%3A%2F%2Ffedabxl.be%2Ffr%2F2021%2F06%2Flieux-de-liens-maillons-essentiels-dans-les-parcours-de-soins%2F&usg=AOvVaw3ykpmpC4orXQErMW5tqsK.
[6] Luyten, J. and E. Schokkaert (2021), “Belgium’s response to the COVID-19 pandemic”, Health Economics, Policy and Law, Vol. 17/1, pp. 37-47, https://doi.org/10.1017/s1744133121000232.
[16] McGowan, V. and C. Bambra (2022), “COVID-19 mortality and deprivation: pandemic, syndemic, and endemic health inequalities”, The Lancet Public Health, Vol. 7/11, pp. e966-e975, https://doi.org/10.1016/s2468-2667(22)00223-7.
[20] Meurisse, M. et al. (2022), “The association between area deprivation and COVID-19 incidence: a municipality-level spatio-temporal study in Belgium, 2020–2021”, Archives of Public Health, Vol. 80/1, https://doi.org/10.1186/s13690-022-00856-9.
[67] Meurisse, M. et al. (2021), “One year of laboratory-based COVID-19 surveillance system in Belgium: main indicators and performance of the laboratories (March 2020–21)”, Archives of Public Health, Vol. 79/1, https://doi.org/10.1186/s13690-021-00704-2.
[105] Mills, M. and T. Rüttenauer (2022), “The effect of mandatory COVID-19 certificates on vaccine uptake: synthetic-control modelling of six countries”, The Lancet Public Health, Vol. 7/1, pp. e15-e22, https://doi.org/10.1016/s2468-2667(21)00273-5.
[112] Milstein, R. and J. Schreyögg (2024), “The end of an era? Activity-based funding based on diagnosis-related groups: A review of payment reforms in the inpatient sector in 10 high-income countries”, Health Policy, Vol. 141, p. 104990, https://doi.org/10.1016/j.healthpol.2023.104990.
[98] Milstein, R. et al. (2022), “How to pay primary care physicians for SARS-CoV-2 vaccinations: An analysis of 43 EU and OECD countries”, Health Policy, Vol. 126/6, pp. 485-492, https://doi.org/10.1016/j.healthpol.2022.03.008.
[12] Morgan, D. et al. (2023), “Examining recent mortality trends: The impact of demographic change”, OECD Health Working Papers, No. 163, OECD Publishing, Paris, https://doi.org/10.1787/78f69783-en.
[28] Moron, L., K. Irimata and J. Parker (2023), Comparison of Mental Health Estimates by Sociodemographic Characteristics in the Research and Development Survey 3 and the 2019 National Health Interview Survey, U.S. Department of Health and Human Services.
[31] Moulin, F. et al. (2023), “Longitudinal impact of the COVID19 pandemic on mental health in a general population sample in France: Evidence from the COMET Study”, Journal of Affective Disorders, Vol. 320, pp. 275-283, https://doi.org/10.1016/j.jad.2022.09.142.
[27] NHS England (2021), Enhanced service specification: Long COVID 2021/22, https://www.england.nhs.uk/wp-content/uploads/2021/06/C1313-ess-long-covid-21-22.pdf.
[77] Nöstlinger, C. et al. (2022), “COVID-19 as a social disease: qualitative analysis of COVID-19 prevention needs, impact of control measures and community responses among racialized/ethnic minorities in Antwerp, Belgium”, International Journal for Equity in Health, Vol. 21/1, https://doi.org/10.1186/s12939-022-01672-x.
[15] OECD (2023), Health at a Glance 2023: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/7a7afb35-en.
[36] OECD (2023), OECD Belgium COVID-19 Health Systems Questionnaire.
[53] OECD (2023), OECD COVID-19 Belgium Expert Interviews.
[33] OECD (2023), OECD Health Statistics.
[95] OECD (2023), OECD Survey of Belgian municipalities in the context of teh OECD Evaluation of Belgium’s COVID-19 responses.
[43] OECD (2023), OECD Survey of General Practitioners in Belgium.
[55] OECD (2023), OECD Survey of Hospitals in the context of the OECD Evaluation of Belgium’s COVID-19 Response.
[63] OECD (2023), Ready for the Next Crisis? Investing in Health System Resilience, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/1e53cf80-en.
[11] OECD (2022), Evaluation of Luxembourg’s COVID-19 Response: Learning from the Crisis to Increase Resilience, OECD Publishing, Paris, https://doi.org/10.1787/2c78c89f-en.
[110] OECD (2022), “First lessons from government evaluations of COVID-19 responses: A synthesis”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/483507d6-en.
[85] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[57] OECD (2021), “Rising from the COVID 19 crisis: Policy responses in the long-term care sector”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/34d9e049-en.
[118] OECD (2021), “Strengthening the frontline: How primary health care helps health systems adapt during the COVID 19 pandemic”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/9a5ae6da-en.
[32] OECD (2021), “Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/0ccafa0b-en.
[56] OECD/European Observatory on Health Systems and Policies (2021), Norway: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris, https://doi.org/10.1787/6871e6c4-en.
[42] OECD/European Union (2022), Health at a Glance: Europe 2022: State of Health in the EU Cycle, OECD Publishing, Paris, https://doi.org/10.1787/507433b0-en.
[9] Office for National Statistics (2022), Comparisons of all-cause mortality between European countries and regions: 28 December 2019 to week ending 1 July 2022, https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/comparisonsofallcausemortalitybetweeneuropeancountriesandregions/28december2019toweekending1july2022.
[39] Office of Frank Vandenbroucke (2022), Dossier de presse: Réforme des soins psychologiques de première ligne - état de la situation: Investissements dans les soins de santé mentale - aperçu (press release), https://vandenbroucke.belgium.be/fr/dossier-de-presse-r%C3%A9forme-des-soins-psychologiques-de-premi%C3%A8re-ligne-%E2%80%93-%C3%A9tat-de-la-situation.
[107] Oliu-Barton, M. et al. (2022), “The effect of COVID certificates on vaccine uptake, health outcomes, and the economy”, Nature Communications, Vol. 13/1, https://doi.org/10.1038/s41467-022-31394-1.
[49] Peacock, H. et al. (2023), “Stage shift and relative survival for head and neck cancer during the 2020 COVID-19 pandemic: a population-based study of temporal trends”, Frontiers in Oncology, Vol. 13, https://doi.org/10.3389/fonc.2023.1253968.
[2] Peeters, I. et al. (2021), Surveillance of COVID-19 Mortality in Belgium: Epidemiology and methodology during 1st and 2nd wave (March 2020 - 14 February 2021), https://www.sciensano.be/sites/default/files/surveillance_of_covid-19_mortality_in_belgium.pdf.
[116] Primary Care and Outpatient Surge Capacity Committee (2020), Comité Primary and Outpatient Care Surge Capacity: Proposition au RMG concernant le pre-triage.
[80] Proesmans, K. et al. (2022), “COVID-19 contact tracing in Belgium: main indicators and performance, January – September 2021”, Archives of Public Health, Vol. 80/1, https://doi.org/10.1186/s13690-022-00875-6.
[73] Raymenants, J. et al. (2022), “Empirical evidence on the efficiency of backward contact tracing in COVID-19”, Nature Communications, Vol. 13/1, https://doi.org/10.1038/s41467-022-32531-6.
[94] Rechel, B., E. Ricardson and M. McKee (eds.) (2018), Belgium, European Observatory on Health Systems and Policies.
[1] Renard, F. et al. (2021), “Establishing an ad hoc COVID-19 mortality surveillance during the first epidemic wave in Belgium, 1 March to 21 June 2020”, Eurosurveillance, Vol. 26/48, https://doi.org/10.2807/1560-7917.es.2021.26.48.2001402.
[14] Rocard, E., P. Sillitti and A. Llena-Nozal (2021), “COVID-19 in long-term care: Impact, policy responses and challenges”, OECD Health Working Papers, No. 131, OECD Publishing, Paris, https://doi.org/10.1787/b966f837-en.
[59] Rolland, Y. et al. (2020), “A COVID-19 Support Platform for Long Term Care Facilities”, The journal of nutrition, health & aging, Vol. 24/5, pp. 461-462, https://doi.org/10.1007/s12603-020-1364-x.
[60] Rough, E. (2020), Coronavirus: Testing for COVID-19. Briefing paper. Number CBP 8897, 14 October 2020, House of Commons Library.
[102] Schmitz, M. et al. (2022), “Predicting vaccine uptake during COVID-19 crisis: A motivational approach”, Vaccine, Vol. 40/2, pp. 288-297, https://doi.org/10.1016/j.vaccine.2021.11.068.
[13] Schöley, J. et al. (2022), “Life expectancy changes since COVID-19”, Nature Human Behaviour, Vol. 6/12, pp. 1649-1659, https://doi.org/10.1038/s41562-022-01450-3.
[8] Schöley, J. et al. (2023), “Conflicting COVID-19 excess mortality estimates”, The Lancet, Vol. 401/10375, pp. 431-432, https://doi.org/10.1016/s0140-6736(23)00116-2.
[65] Sciensano (2023), Belgium COVID-19 Dashboard, https://lookerstudio.google.com/embed/u/0/reporting/c14a5cfc-cab7-4812-848c-0369173148ab/page/cUWaB.
[41] Sciensano (2023), Belgium COVID-19 Epidemiological Situation: Mental Health Studies (database), https://lookerstudio.google.com/embed/u/0/reporting/7e11980c-3350-4ee3-8291-3065cc4e90c2/page/ykUGC (accessed on 14 August 2023).
[5] Sciensano (2023), COVID-19 epidemiological situation, https://epistat.sciensano.be/covid/ (accessed on October 2023).
[23] Sciensano (2023), COVIMPACT - Long COVID and its physical, mental and social implications, https://www.sciensano.be/en/projects/long-covid-and-its-physical-mental-and-social-implications.
[117] Sciensano (2023), Le résau des Médecins Vigies, https://www.sciensano.be/fr/reseau-des-medecins-vigies#l-enregistrement-activit-infections-respiratoires-aigu-s-syndromes-grippaux-et-diarrh-e-aigu-.
[24] Smith, P. et al. (2022), Etude COVIMPACT: Infection COVID-19 et ses implications physiques, mentales et sociales à long terme - Résultats du suivi à 3 et 6 mois suivant l’infection, https://doi.org/10.25608/gyzc-w673.
[82] Stoto, M. et al. (2023), “The European experience with testing and surveillance during the first phase of the COVID-19 pandemic”, Globalization and Health, Vol. 19/1, https://doi.org/10.1186/s12992-023-00950-9.
[111] Taccone, F. et al. (2021), “The role of organizational characteristics on the outcome of COVID-19 patients admitted to the ICU in Belgium”, The Lancet Regional Health - Europe, Vol. 2, p. 100019, https://doi.org/10.1016/j.lanepe.2020.100019.
[90] Task Force Vaccination (2021), COVID-19 Programme de vaccination. Standard Operating Procedures - Mobile vaccination. Version 1.1 (06/04/21).
[113] Tiete, J. et al. (2021), “Mental Health Outcomes in Healthcare Workers in COVID-19 and Non-COVID-19 Care Units: A Cross-Sectional Survey in Belgium”, Frontiers in Psychology, Vol. 11, https://doi.org/10.3389/fpsyg.2020.612241.
[96] Turner, D. et al. (2022), “Understanding differences in vaccination uptake among OECD countries”, OECD Economics Department Working Papers, No. 1704, OECD Publishing, Paris, https://doi.org/10.1787/76482043-en.
[54] Vaes, B. et al. (2022), “Burden of COVID-19 on primary care in Belgium: a prospective nationwide observational study from March to August 2020”, Archives of Public Health, Vol. 80/1, https://doi.org/10.1186/s13690-022-01003-0.
[58] Van de Voorde, C. et al. (2020), Assessing the management of hospital surge capacity in the first wave of the COVID-19 pandemic in Belgium. KCE Reports 335, Belgian Health Care Knowledge Centre (KCE), https://doi.org/10.57598/R335C.
[62] Van Goethem, N. et al. (2020), “Rapid establishment of a national surveillance of COVID-19 hospitalizations in Belgium”, Archives of Public Health, Vol. 78/1, https://doi.org/10.1186/s13690-020-00505-z.
[87] van Kessel, R. et al. (2023), “Divergent COVID-19 vaccine policies: Policy mapping of ten European countries”, Vaccine, Vol. 41/17, pp. 2804-2810, https://doi.org/10.1016/j.vaccine.2023.03.036.
[35] Vandamme, J. et al. (2023), “The Impact of the COVID-19 Pandemic on the Registration and Care Provision of Mental Health Problems in General Practice: Registry-Based Study”, JMIR Public Health and Surveillance, Vol. 9, p. e43049, https://doi.org/10.2196/43049.
[114] Vanhaecht, K. et al. (2020), “COVID-19 is having a destructive impact on health-care workers’ mental well-being”, International Journal for Quality in Health Care, Vol. 33/1, https://doi.org/10.1093/intqhc/mzaa158.
[79] Vanhamel, J. et al. (2021), “Understanding how communities respond to COVID-19: experiences from the Orthodox Jewish communities of Antwerp city”, International Journal for Equity in Health, Vol. 20/1, https://doi.org/10.1186/s12939-021-01417-2.
[19] Vanthomme, K. et al. (2021), “A population-based study on mortality among Belgian immigrants during the first COVID-19 wave in Belgium. Can demographic and socioeconomic indicators explain differential mortality?”, SSM - Population Health, Vol. 14, p. 100797, https://doi.org/10.1016/j.ssmph.2021.100797.
[22] Verbeeck, J. et al. (2021), “Confirmed COVID-19 Cases per Economic Activity during Autumn Wave in Belgium”, International Journal of Environmental Research and Public Health, Vol. 18/23, p. 12489, https://doi.org/10.3390/ijerph182312489.
[78] Verdonck, K. et al. (2023), “Local initiative supports case isolation and contact tracing during a SARS-CoV-2 surge in summer 2020: a community case study in Antwerp, Belgium”, Frontiers in Public Health, Vol. 11, https://doi.org/10.3389/fpubh.2023.1000617.
[103] Verger, P. et al. (2021), “Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020”, Eurosurveillance, Vol. 26/3, https://doi.org/10.2807/1560-7917.es.2021.26.3.2002047.
[104] Vermeulen, N. et al. (2023), “Expectations and disappointments relative to COVID-19 passes: results from a voluntary mixed-methods study in French-speaking Belgium”, IJID Regions, Vol. 6, pp. 146-151, https://doi.org/10.1016/j.ijregi.2023.01.010.
[70] Vogt, F. et al. (2022), “Effectiveness evaluation of digital contact tracing for COVID-19 in New South Wales, Australia”, The Lancet Public Health, Vol. 7/3, pp. e250-e258, https://doi.org/10.1016/s2468-2667(22)00010-x.
[52] Vrancken, J. et al. (2022), Les téléconsultations durant la pandémie de COVID-19: Par qui ? Pour qui ?, https://aim-ima.be/IMG/pdf/teleconsultations_durant_la_pandemie_de_covid-19_-_def_-_newtemp.pdf.
[115] Waitzberg, R. et al. (2022), “Balancing financial incentives during COVID-19: A comparison of provider payment adjustments across 20 countries”, Health Policy, Vol. 126/5, pp. 398-407, https://doi.org/10.1016/j.healthpol.2021.09.015.
[76] Walrave, M., C. Waeterloos and K. Ponnet (2022), “Reasons for Nonuse, Discontinuation of Use, and Acceptance of Additional Functionalities of a COVID-19 Contact Tracing App: Cross-sectional Survey Study”, JMIR Public Health and Surveillance, Vol. 8/1, p. e22113, https://doi.org/10.2196/22113.
[81] Walrave, M., C. Waeterloos and K. Ponnet (2020), “Adoption of a Contact Tracing App for Containing COVID-19: A Health Belief Model Approach”, JMIR Public Health and Surveillance, Vol. 6/3, p. e20572, https://doi.org/10.2196/20572.
[108] Ward, J. et al. (2022), “The French health pass holds lessons for mandatory COVID-19 vaccination”, Nature Medicine, Vol. 28/2, pp. 232-235, https://doi.org/10.1038/s41591-021-01661-7.
[64] Willem, L. et al. (2021), “The impact of contact tracing and household bubbles on deconfinement strategies for COVID-19”, Nature Communications, Vol. 12/1, https://doi.org/10.1038/s41467-021-21747-7.
[71] Wymant, C. et al. (2021), “The epidemiological impact of the NHS COVID-19 app”, Nature, Vol. 594/7863, pp. 408-412, https://doi.org/10.1038/s41586-021-03606-z.
Note
← 1. Mortality rates are Age-Standardised Mortality Rates (ASMR) based on three age bands: 0-44, 45-64 and 65+.