Eileen Rocard
Ready for the Next Crisis? Investing in Health System Resilience

7. Strengthening resilience in long‑term care
Abstract
This chapter describes the impact of the COVID‑19 pandemic and the corresponding policy responses on the long-term care sector. It also presents policy avenues to make long-term care more resilient in the future. The chapter focuses on avoiding fragmentation of long-term care, financing and funding of the sector, preventive and rehabilitation services, and the critical role of long-term care workers and informal carers.
Key findings
The COVID‑19 pandemic has severely affected the long-term care (LTC) sector. This sector supports dependent people with the activities of daily living (such as eating and washing) alongside some types of medical care, or provides services (including cooking and cleaning) to assist people to live independently. Analysis of the impacts of the pandemic and the response to it found the following:
Around 34% of all cumulative COVID‑19 deaths were among residents in LTC facilities by April 2022. However, this share was down from 40% in early 2021, suggesting that efforts to contain and mitigate the spread of the virus among LTC recipients improved.
The vaccine rollout was a game changer. Residents in LTC facilities and staff were prioritised to receive COVID‑19 vaccinations in virtually all OECD countries from the end of 2020 to early 2021, and there was a decline in deaths shortly afterwards. However, the pandemic may still pose a threat to LTC residents due to the emergence of variants.
LTC was often delayed and cancelled. About 20% of older people who received personal care from people living outside their household regularly reported forgone or postponed care in 2021 across 23 OECD countries. LTC workers were also very exposed, and typically worked longer hours or became ill themselves. Informal carers generally reported an additional burden.
A range of policy actions can improve the readiness of the LTC sector to respond to future shocks, some of which OECD countries implemented once the pandemic began:
Infection prevention and control protocols, testing and personal protective equipment should remain updated/available. Maintaining high vaccination rates for LTC workers and residents is very important.
Countries need more LTC workers, and these additional workers must be well prepared and trained. Around 90% (20 of 22) of surveyed OECD countries implemented mobile teams to support rapid responses during outbreaks, especially in LTC facilities, according the 2021 OECD Survey on COVID‑19 and LTC. While many countries increased the workload of LTC workers, nearly all countries made efforts to recruit staff.
Efforts should be made to expand the use of digital technologies to ensure care continuity and maintain social contact between care recipients and their relatives in times of crisis. LTC facilities expanded the use of telehealth in 21 OECD countries after the pandemic began.
Task forces should include LTC experts, or LTC-specific task forces should be set up. Nearly 20% (5 of 26) of surveyed countries did not have COVID‑19 task forces that included an LTC expert.
Many of these actions taken by OECD countries, while valuable, were temporary and limited. OECD countries can and should make structural changes to better withstand population ageing and strengthen resilience:
Countries should further harmonise eligibility criteria and benefits in the LTC sector.
Countries should consider allocating additional permanent funding to long-term care, including to bolster the workforce. Over one‑third of people across OECD countries would be ready to pay an additional 2% of their income in taxes and social contributions to fund more public support for LTC. Avenues to fund more LTC may rely on broad-based funding routes.
Countries should develop further preventive, rehabilitation and end-of-life care services. These can improve quality of life and/or postpone LTC needs and related spending.
Ensuring that sufficient carers are available is vital. This requires policies to improve pay and working conditions that address structural workforce shortages in the sector. Countries can also provide better public support to informal (family) carers, including respite and leave entitlements.
7.1. The COVID‑19 pandemic and responses to it have impacted long-term care
The COVID‑19 pandemic was a shock that severely affected the long-term care (LTC) sector. Over one‑third of all cumulative COVID‑19 deaths were among residents in LTC facilities on average across OECD countries by April 2022. However, the share had decreased in virtually all countries with available data, suggesting that the vaccination rollout was a game changer. Care services were considerably disrupted at the beginning of the pandemic but resumed gradually. Providing adequate care nonetheless proved challenging during infection peaks when LTC workers were ill. Policy measures such as stringent visit restrictions impacted negatively on the well-being of LTC residents and their relatives, and a substantial share of care recipients at home felt low. Many LTC workers reported poor mental well-being.
7.1.1. Over one‑third of all COVID‑19 deaths were among long-term care residents
COVID‑19 disproportionately affects older people, who are at a higher risk of developing severe symptoms and dying because of underlying health conditions and frailty. More than 90% of all cumulative COVID‑19 deaths were among people aged 60 years and over, and over 50% were among those aged 80 years and over on average across 22 OECD countries by April 2022. These latter OECD averages have remained stable over the course of the pandemic. The rate of COVID‑19 deaths among the population aged 60 years and over was over 7 800 deaths per million people and among those aged 80 years and over was 24 000 deaths per million by mid-April 2022.
Residents of LTC facilities have been particularly affected. Older adults living in LTC facilities (including nursing homes, assisted living facilities, etc.) are at the highest risk because of both individual and group-level factors. At the individual level, they are typically in poorer physical and mental health; at the group level, they live in shared areas with group-based activities, and congregate during meals, facilitating the spread of the virus.
Over one‑third (34%) of total COVID‑19 deaths were among LTC residents across 25 OECD countries by April 2022 (Figure 7.1). While Finland and Norway had the highest shares of LTC resident deaths among all COVID‑19 deaths, they were also among the OECD countries with the lowest overall COVID‑19 mortality rates.
Figure 7.1. Proportion of LTC residents among all COVID‑19 deaths across OECD countries
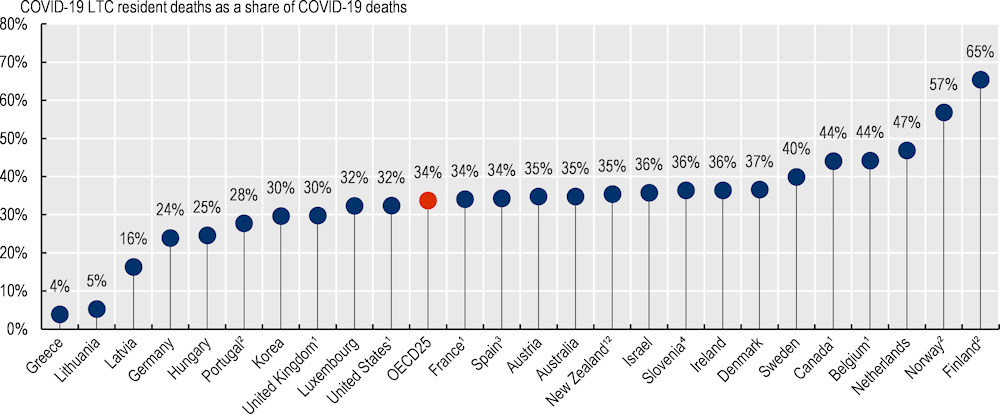
Note: Data on cumulative deaths covers different periods: data cover up to May 2022 for eight countries or else up to 2021 for the remaining countries, except for Israel (2020). 1. Includes confirmed and suspected COVID‑19 deaths. 2. Only includes deaths occurring within LTC facilities, not those occurring after transfer to hospitals. 3. Data come from regional governments using different methodologies, some including suspected deaths. 4. Slovenia includes deaths in nursing homes and social LTC facilities.
Source: LTC COVID‑19 website, complemented with European Centre for Disease Prevention and Control (ECDC) data and 2021 OECD Questionnaire on COVID‑19 in LTC.
Compared with the shares among all cumulative COVID‑19 deaths up to 2020 and up to 2021, the share of LTC resident deaths among all cumulative COVID‑19 deaths up to 2022 decreased in nearly all OECD countries with available data. The strongest reductions occurred in Australia and New Zealand – two countries with low COVID‑19 mortality rates compared to other OECD countries during the pandemic. This suggests that vaccination rollouts had a strong impact on the LTC sector.
7.1.2. Vaccines have been a game changer in long-term care
LTC residents and staff were prioritised to receive COVID‑19 vaccinations in most countries from the end of 2020 and early 2021, when many countries were hit by a COVID‑19 peak. There was a marked decline in deaths thereafter.
For example, in Canada, 95% of residents in most jurisdictions received their first dose of the vaccine between 15 January and 31 March 2021, compared with only 3% of the general population (Figure 7.2). This high vaccination rate reduced both infections and deaths among LTC residents by over 90%. The vaccine rollout for staff was slower. By 15 March 2021, 60% of staff had been vaccinated, and cases had declined by 63% (Canadian Institute for Health Information, 2021[1]). The number of COVID‑19 deaths in the community decreased at a slower pace in early 2021. By November 2021, the vaccination rate of LTC workers was above 95% in provinces with available data.
Figure 7.2. Reductions in COVID‑19 mortality in LTC facilities in Canada after vaccination rollout
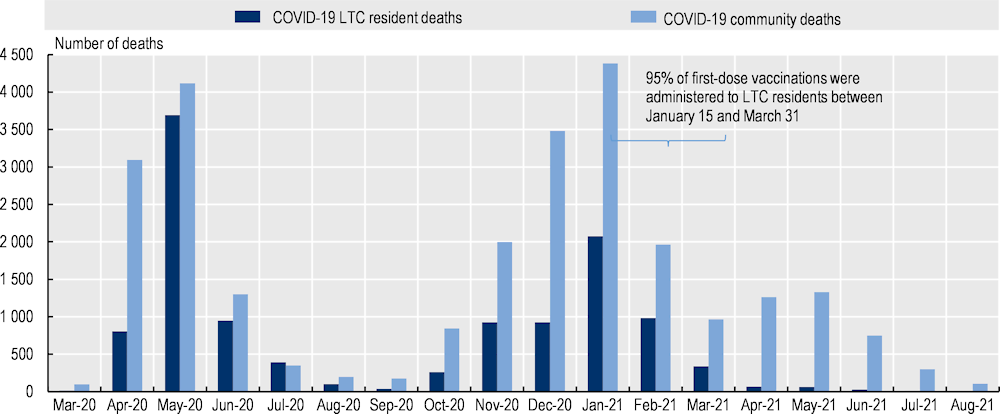
Source: Canadian Institute for Health Information (2021[1]), COVID‑19s impact on long-term care, https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/long-term-care.
Similarly, in Italy, the number of deaths of COVID‑19‑positive LTC residents decreased after vaccinations were rolled out. The share of COVID‑19 deaths among residents decreased from 0.4% in January and February 2021 to around 0.2% in April 2021. The share stabilised at around 0.1% or below afterwards, including during the winter’s infection peaks in Q4 2021 and Q1 2022 (Istituto Superiore di Sanità, 2022[2]).
7.2. The absorb stage of the pandemic was challenging in long-term care
The response to a shock comprises four stages (see the chapter on key findings and recommendations). These stages are prepare, absorb, recover and adapt. Prepare includes the steps taken to prepare critical functions to avoid and mitigate shocks. This occurs prior to the disruption. Absorb occurs after the shock commences, comprising the capability of the health system to maintain core functions and absorb the consequences without collapse. Thus, limiting the extent of the disruption and minimising the morbidity and mortality impact. Recover involves regaining the disrupted functions as quickly and efficiently as possible. Adapt is the capacity of the health system to “learn” and improve its capacity to absorb and recover from shocks, reducing the impact of similar threats in the future.
At the start of the COVID‑19 pandemic, when countries were absorbing its impacts, care was severely disrupted. Home‑based care was reduced. Day-care centres closed. LTC facilities were typically shielded when an outbreak occurred, with non-essential care delayed or deferred. However, care resumed progressively with appropriate infection prevention and control measures. The pandemic and the policy responses to absorb it came at a high cost for care recipients, LTC workers and informal carers.
7.2.1. Disruption was high during the absorb stage, but care resumed progressively
During the first months of the pandemic, home‑based care was reduced. Day-care centres also closed nationally in most OECD countries.
For example, in Germany, there was a slight reduction in available home‑based LTC and a considerable reduction in day care (Lorenz-Dant; Fischer and Hämel, 2022[3]). A survey among care providers in April/May 2020 showed that two‑thirds of day-care organisations closed completely or stopped accepting new clients. About 50% of home‑based care service providers also recorded a change in uptake of services – mostly a reduction (Wolf-Ostermann et al., 2020[4]). After these first months, day-care centre closures were typically decided based on the local epidemiological situation, and home care resumed, although over 40% (11 out of 26 surveyed countries, as part of the OECD Resilience of Health Systems Questionnaire 2022.) reported delays in accessing LTC in 2022, for various reasons.
In England (United Kingdom), a 2021 survey of adult social services (for disabled or older people) offers insight into the impact of the pandemic and its policy responses in the LTC sector. The survey found that an estimated 391 000 people were waiting for an assessment or overdue reassessment of their care needs, or for a service to be provided after assessment in November 2021. More than 41 million hours of care and support were provided for people in their homes from August to October 2021, an increase of 15% since May to July 2021.However, 1.5 million hours that had been commissioned could not be provided because of a lack of staff. Between June and November 2021, 48% of directors of adult social services needed to respond to a care home closure or a home provider going out of business, compared with 25% before the pandemic (Association of Directors of Adult Social Services, 2021[5]).
Many older people receiving home care also had to forgo health care for fear of infection, or were asked to postpone it. About 20% of older people who regularly received personal care from professionals or relatives living outside their household reported forgone or postponed care in 2021, based on the Survey of Health Retirement and Ageing (SHARE) data in 23 European countries and Israel.
LTC facilities were typically shielded when an outbreak occurred, discontinuing non-essential care such as some general practitioner (GP) visits. For example, in Canada, physician visits to LTC residents declined by 22% in April 2020, although they had returned to near pre‑pandemic levels by June 2021 (Canadian Institute for Health Information, 2021[1]). However, teleconsultations helped to maintain care continuity with primary care professionals to a certain extent.
One particular concern was related to the lack of access to physiotherapy and physical activity among recipients in LTC facilities, even though some countries took action. In France, there is evidence of the impact on physical health due to the disruption of physiotherapy support, with considerably higher numbers of older people losing autonomy, and requiring support with walking and other activities of daily living (Mission d'information sur l’impact, la gestion et les conséquences dans toutes ses dimensions de l’épidémie de Covid 19, 2020[6]). Similarly, in Germany, lockdowns of nursing homes during the first wave of the pandemic led to disruption of physical activity programmes. There were attempts to promote physical activity in LTC facilities, but the staff were not trained for this (Lorenz-Dant; Fischer and Hämel, 2022[3]). Some countries implemented targeted efforts to maintain a certain level of physical activity. For instance, in Navarre, Spain, 85% of nursing homes organised physical activity exercises and emotion management (Fresno, 2020[7]). In Chile, special isolation facilities for those infected with COVID‑19 were coupled with an additional budget for rehabilitation.
Transfers from LTC facilities to hospitals also decreased during the pandemic, although the reduction varied across countries. Reductions were more likely when hospitals were at full capacity. In Canada, there was an overall drop of 25% in transfers from LTC facilities to hospitals between March 2020 and June 2021 compared with the pre‑pandemic period, following changes in transfer protocols (Canadian Institute for Health Information, 2021[1]).
Countries also initially banned or heavily restricted visits from relatives in LTC facilities, and restricted activities. However, the most stringent restrictions were generally lifted after the first wave in 2020 because of important concerns about care recipients’ mental well-being. Visits were allowed with appropriate physical distancing and restrictions on the number of visits. Large group activities such as recreational activities were heavily restricted. In 17 OECD countries, it was also recommended that meals be eaten in bedrooms on a regular basis. Other countries kept such activities but encouraged physical distancing among residents. As countries have moved to the recover stage, communal activities face restrictions contingent on the epidemiological situation of the facility.
7.2.2. The pandemic had substantial impacts on LTC workers, care recipients and informal carers
LTC workers were particularly exposed to infections in LTC facilities. Available data on incidence among LTC residents and LTC workers show that the trends among LTC residents and LTC workers mirrored each other (including in the Czech Republic, Latvia and the United States).
LTC workers were put under pressure – particularly during outbreaks. They had to implement infection prevention and control protocols that required more work, while more of their colleagues were on sick leave or self-isolating. For example, in the United Kingdom a small survey undertaken after the first wave in 2020 found that over half of social care workers reported increased working hours, and 18% had had to self-isolate (and nearly one‑fifth of those who had self-isolated had not received pay when self-isolating) by July-August 2020. Nearly 90% of care workers working in LTC facilities reported increased feelings of tension, uneasiness and worry (Hussein et al., 2020[8]).
LTC workers who provide 24‑hour home‑based care were particularly affected. They faced greater financial precariousness and increased dependence on their employers and/or brokers. Undeclared workers experienced worse conditions as they were excluded from bonus payments, relief funds and travel facilitation. They generally lacked key employment law protections that safeguards workers in most other employment fields, as even where regulations exist, they are not always enforced in private households.
In addition, poor mental well-being among care recipients became a source of concern. About 27% of older people receiving personal care at home could not name anything to be hopeful or happy about or to look forward to across 23 OECD countries in 2021, based on SHARE data (Figure 7.3). In comparison, the share was 12% among older people who were not receiving personal care at home.
Figure 7.3. Proportion of older people who could not name anything to be hopeful or happy about or to look forward to
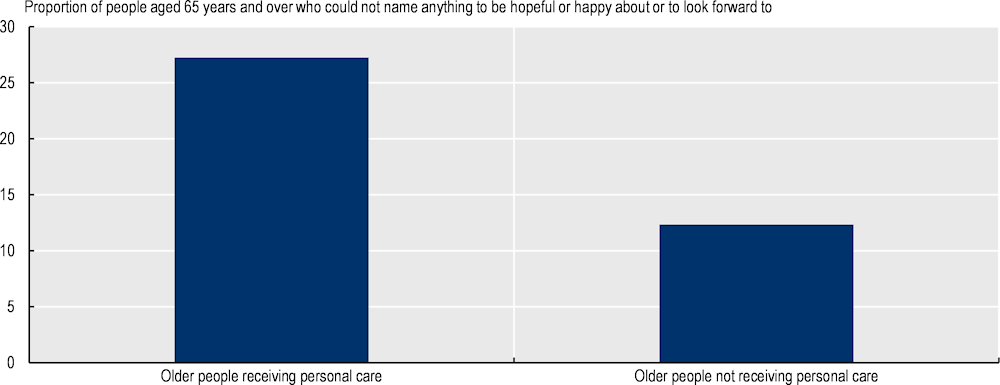
Note: questions were “What was your most uplifting experience since the outbreak of COVID‑19 – in other words, something that inspired hope or happiness?” and “What is it that you are looking most forward to doing once COVID‑19 abates?”. Personal care refers to care provided by anyone living outside the household, and care recipients in LTC facilities are excluded. Weighted data cover 23 OECD countries and refer to those aged 65 years and over.
Source: SHARE wave 9 (SHARE Corona Survey 2).
Similarly, 15 surveyed OECD countries reported that the COVID‑19 pandemic had a substantial negative impact on the mental health of LTC recipients, and 14 reported that it had exacerbated mental health issues for LTC recipients with dementia in particular (Box 7.1). Care recipients suffered particularly from the strictest isolation measures (e.g. remaining isolated in a bedroom).
Box 7.1. The challenge of containment strategies for patients affected by dementia
People affected by dementia require particular attention, as they face serious difficulties in understanding, accepting and remembering rules and restrictions, and they usually belong to the category of patients most at risk of dying from COVID‑19. Moreover, prolonged isolation tends to cause or exacerbate feelings of loneliness, depression and stress (Korczyn, 2020[9]). Worsening of cognitive symptoms and lower independence also emerged in some cases, following periods of prolonged isolation (Canevelli et al., 2020[10]). Being isolated and/or treated in intensive care units by unfamiliar doctors often triggered restless reactions in dementia patients, sometimes requiring sedation and causing post-traumatic stress disorder (Korczyn, 2020[9]).
Some OECD countries implemented special programmes for dementia patients, but decisions on this type of measure were often left to facilities and doctors. For example, in the Czech Republic and Greece, decisions were taken by individual doctors. Conversely, Korea set up nationwide programmes for patients with cognitive impairment during the pandemic. Korean LTC residents with dementia could take part in cognitive enhancement programmes, and outdoor activities replaced indoor group activities.
Countries should strive to find the right balance between sheltering dementia patients at risk of developing severe COVID‑19 symptoms and ensuring a good quality of life, taking into account the specificities of dementia symptoms. Implementing telehealth services can facilitate communication both with health care workers and with relatives.
With reduced formal services, the pandemic and its corresponding policy responses (such as closure of day centres and reduced home‑based care) created an additional burden on informal carers. In 23 OECD countries, 12% of people aged 50 years and over reported providing personal care to their own parents (outside their household), and 61% reported that they provided as much care in 2021 as during the first wave of the pandemic in 2020, based on SHARE data. In the United Kingdom, as part of a small survey of carers of people affected by dementia, 83% of carers said they had fewer opportunities to take a break from caring, and 86% said there had been a negative impact on their own physical, mental or social well-being (Dementia UK, 2020[11]). Similarly, in Germany, a survey found that more than half of respondents reported that their perceived health and quality of life had worsened since the beginning of the pandemic. Over two‑thirds of informal carers reported that reconciliation of work and care had become more difficult due to the pandemic (Rothgang et al., 2020[12]).
7.3. Policies are needed to make long-term care ready for future disruptions
The LTC sector was generally poorly prepared to tackle a health emergency: just over half of OECD countries had guidelines on infection controls in LTC facilities before the pandemic.
A range of policies can ensure that LTC systems are better prepared for – and can more effectively absorb, recover from and adapt to – shocks. LTC experts should be included in crisis planning and preparedness, including for future pandemics (but not limited to this type of large‑scale disruption). Infection prevention and control, and vaccination, are important avenues to contain and mitigate the impacts of newly emerging infectious diseases and/or future pandemics (see the chapter on containment and mitigation). Countries also need more LTC workers to strengthen the sector’s agility and responsiveness to future disruption. Expanded use of digital technology in the sector will also help to ensure care continuity and maintain social contact between care recipients and relatives, including in circumstances of crisis.
7.3.1. Infection prevention and control, and sufficient supplies, will better prepare the long-term care sector
Well before the COVID‑19 pandemic, a body of evidence showed that outbreaks of infectious diseases occurred in the LTC sector because of suboptimal infection prevention and control practices (Eze, Cecchini and Oliveira Hashiguchi, 2022[13]).
LTC systems with suboptimal practices put care recipients and LTC workers at a higher risk, and countries with stronger practices coped far better with the pandemic. For example, in Belgium, a non-representative survey showed that virucidal products were in short supply in about 15% of nursing homes, and medical devices were not disinfected appropriately in 19% of nursing homes that received support from the non-governmental organisation Médecins Sans Frontières at the beginning of the pandemic (Médecins Sans Frontières, 2020[14]). Belgium was one of the countries hardest hit during the first wave in March 2020. Conversely, Japan had stronger routine protocols of infection prevention and control after the severe acute respiratory syndrome (SARS) outbreak in 2002‑03, and was well prepared.
The pandemic highlighted the importance of adequate supplies of PPE, testing capacities, hand sanitisers, gloves and virucidal products to implement infection prevention and control protocols (see the chapter on securing supply chains). Support from line managers contributes to adequate availability and proper use of supplies.
While the LTC sector was typically not prioritised for PPE distribution at the onset of the pandemic, a couple of countries stood out as well prepared, and all OECD countries had sufficient PPE by mid‑2020. Korea took particularly swift measures. In March 2020 the country established a working group to manage supplies and an information technology (IT) system to distribute 5.46 million face masks for 770 000 employees swiftly via LTC providers.
Insufficient testing in nursing homes also hampered effective detection and isolation of confirmed cases at the early absorb stage of the pandemic, but countries took a range of measures to increase testing capacity. These included increasing training and equipment in LTC facilities, setting up mobile teams and providing extra funding. By March 2021, most OECD countries had policies to test LTC workers and residents with COVID-like symptoms, and to notify them when they have been in contact with a confirmed or suspected COVID‑19 case.
Following the vaccine rollout, and as countries moved to recover from the pandemic, testing strategies were generally maintained with more flexible arrangements. Nearly 85% (19 out of 23) of surveyed countries reported that they had testing requirements in place. Austria, France, Lithuania and Spain did not require regular testing for vaccinated workers, although they recommended it in the event of outbreaks. Regular testing remained required or highly recommended for vaccinated and non-vaccinated workers in the Czech Republic, Finland and Switzerland. In Korea, regular tests were recommended, and all LTC workers who tested received a monthly benefit of KRW 100 000 (EUR 74) per month between February and April 2022.
7.3.2. Pandemic task forces should include long-term care experts
The pandemic also demonstrated that task forces on pandemic preparedness and management should include LTC experts. Task forces consist of groups of experts organised at the national, local or facility level, with the aim of managing and co‑ordinating responses to the COVID‑19 pandemic. They are usually temporary, but Japan and Korea have permanent task forces in place to respond quickly to a crisis. While nearly half of the OECD countries surveyed created an LTC-specific task force, about 20% of countries did not include at least one LTC expert in COVID‑19 task forces (Figure 7.4).
Figure 7.4. COVID‑19 task forces that included a LTC expert
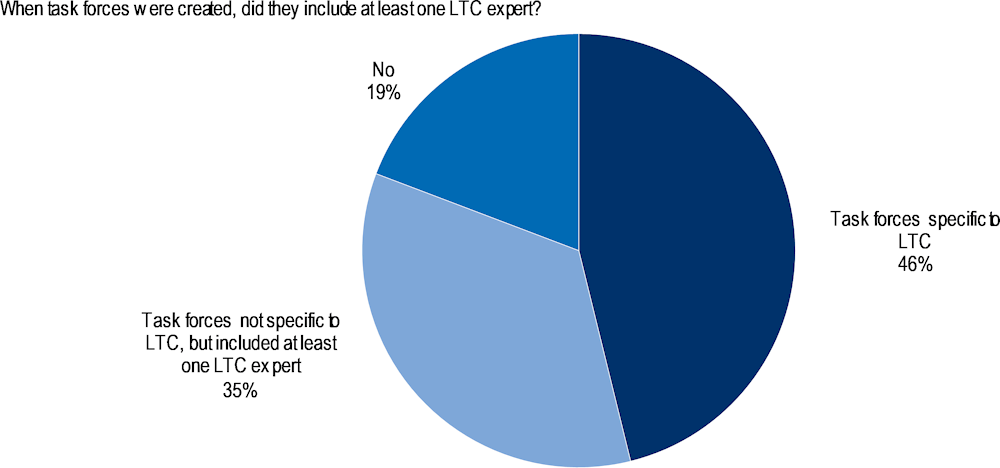
Note: Data collected in 2021 from the OECD Questionnaire on COVID‑19 and LTC.
Source: Rocard, Sillitti and Llena-Nozal (2021[15]), “COVID‑19 in long-term care: Impact, policy responses and challenges”, https://doi.org/10.1787/b966f837-en.
Task forces are particularly useful given that LTC systems are fragmented across stakeholders. A lack of co‑ordination with the health care system negatively affected LTC residents (Box 7.2).
Box 7.2. Impacts of the pandemic on LTC residents from a lack of co‑ordination with the health care system
There is evidence that the lack of co‑ordination with hospitals and primary care hampered swift reactions in many countries, including France, Italy and the United Kingdom. In France, the division of LTC responsibilities between the regional health authorities and departments was a possible source of confusion in responding to the COVID‑19 pandemic. Some regional health authorities did not possess sufficient information regarding home‑based LTC workers in their territories to be proactive, while others were able to contact them to propose, for example, a specific point of contact and help them to secure PPE (Commission d’Enquête Évaluation des politiques publiques face aux pandémies, 2020[16]). In Italy, nine regions left hospitals and LTC facilities responsible for transfers between them. In some cases, transfers were hampered or blocked (Berloto et al., 2020[17]). In north-west England (United Kingdom), there was an apparent reluctance among some LTC facilities to accept discharged hospital patients in a context of testing and PPE shortages during the first wave, and in the absence of a clear division of responsibilities (Comas-Herrera et al., 2020[18]).
The lack of primary care within nursing homes created particular difficulties – especially in places where transfer to hospital was not forthcoming. Since the pandemic, eight OECD countries have introduced new measures to foster multi-disciplinary teams, with the aim of integrating more primary care into LTC facilities. A few countries have also encouraged GP visits. In France, a new financial incentive is provided to primary care doctors to visit LTC residents. In Korea, an initiative is currently being tested to ensure that LTC facilities receive at least one GP visit twice a week.
In Israel, policy makers created a task force dedicated to outbreaks in LTC facilities one month after the start of the pandemic. At that time, LTC residents accounted for more than 50% of all COVID‑19 deaths, even though they made up less than 0.5% of the total population. The share of LTC residents had dropped to 36% of all COVID‑19 deaths in Israel by the end of April 2020 (Tsadok-Rosenbluth et al., 2021[19]).
Another example is Bavaria, Germany, which introduced a specific task force to support residential care settings in December 2020, after creating a broader task force on infectious disease in March 2020. The task force is called in as soon as one confirmed case has been established in a care home to prevent, advise on and control infections (Lorenz-Dant; Fischer and Hämel, 2022[3]).
Countries should review LTC infection prevention and control protocols and training regularly. Policy makers could identify LTC experts who could be involved in permanent or temporary task forces on infectious diseases. They could also ensure that LTC facilities conduct regular pandemic preparedness drills with the appropriate level of granularity (WHO, 2022[20]).
In addition, data related to infections and mortality should be generated to be useful for decision making in the absorb stage. Data on the share of LTC deaths among COVID‑19 deaths were challenging to collect in the early stages of the pandemic, hampering swift reactions. Meanwhile, prioritisation of resources towards the health system and not the LTC system exacerbated the pandemic’s impact on LTC residents. Data on infections and mortality became available later, although they were sometimes not sufficiently updated to be useful for decision making. It is important that countries keep monitoring key indicators, such as the number of COVID‑19 deaths in LTC facilities, and disseminate the findings in a timely manner.
7.3.3. A high vaccination rate among care recipients and LTC workers is crucial
Almost all OECD countries prioritised care recipients and LTC workers during the vaccine rollout, and this strategy was successful in reducing COVID‑19 case numbers and deaths (see Section 7.1).
Vaccinations rates among LTC workers were high in virtually all countries with available data. The rate was 90% or above in 2022 in Australia, Costa Rica, Germany, Israel, Italy, Latvia, Luxembourg, Mexico, Portugal and the United Kingdom. The rate was between 80% and 90% in Korea and the United States. It was at 70% in early 2021 in Slovenia, where LTC workers were not required to be vaccinated.
About 60% of surveyed countries required LTC workers to be vaccinated against COVID‑19. Vaccine hesitancy could have limited the success of vaccination programmes. Nonetheless, the overwhelming majority of OECD countries reported that achieving vaccination among LTC workers was not a concern or was a relatively low concern for policy makers.
In the future, it will be important to update vaccination requirements for possible boosters and, more generally, to promote confidence in vaccines.
7.4. Countries need rapid recruitment strategies to be better prepared
LTC workers are essential to implement any effective response to a crisis or large‑scale shock, such as a future pandemic, in LTC facilities.
In response to the COVID‑19 pandemic, countries implemented mobile teams and increased recruitment and retention efforts, although most measures were temporary. Reducing staff mobility was key to helping prevent and limit outbreaks. Evidence shows, however, that higher staffing was associated with fewer deaths, even though greater staff numbers were associated with a higher probability of an outbreak (Konetzka et al., 2021[21]). Bolstering the workforce was, and continues to be, very important to strengthening resilience in the LTC sector (see the chapter on investing in resilience).
7.4.1. Mobile teams supported rapid responses during outbreaks
Along with visitors, LTC workers represent potential transmission vectors, and countries implemented a range of policies to reduce staff mobility. For example, a study estimated that 49% of COVID‑19 cases in residential aged care facilities could be attributed to staff movement between facilities in the United States (Jepsen and Barker, 2020[22]). Policies to reduce staff mobility included reduced staff rotation within LTC facilities, reduction of multiple‑site work and single‑site policies. While these policies had some success (Jones et al., 2021[23]), restricting the movement of LTC workers between facilities is difficult to implement when many have multiple part-time jobs. Across OECD countries, 42% of LTC workers held part-time jobs in 2019 (OECD, 2021[24]). Asking LTC workers providing care at home to limit their mobility also led to reductions in wages that were already low. Some countries, such as Canada and the United Kingdom, provided time‑limited financial support to address the financial implications of such measures.
In the context of staff shortages, countries typically implemented mobile teams. Around 90% of surveyed countries prepared rapid response teams – at either the national or subnational level – to counteract staff shortages in overwhelmed facilities (Rocard, Sillitti and Llena-Nozal, 2021[15]). Workers came from different sectors or from geographical areas that were less hit by the pandemic. For example, in Australia, interstate staff recruited included registered nurses, enrolled nurses, personal care workers and cleaners. Workers could be deployed to care facilities for a four‑week period, followed by two weeks of quarantine. They were supplied with uniforms and PPE, regular COVID‑19 tests during their placement, and access to pastoral and mental health support (Low et al., 2022[25]). In at least five countries (Canada, the Czech Republic, Estonia, Germany and Israel) the army also deployed staff in facilities.
However, rapid response teams are not a panacea. In Australia, an independent review found that some of the additional workforce did not have appropriate skills and experience, had insufficient training in infection prevention and control, or did not speak English well enough. Many care homes preferred to avoid using workers they did not know (Low et al., 2022[25]).
7.4.2. Nearly all OECD countries boosted the recruitment of long-term care workers, and many increased the workload of existing staff
Nearly all the OECD countries surveyed took temporary actions to recruit staff – particularly nurses and personal carers – in 2020 and 2021 (Rocard, Sillitti and Llena-Nozal, 2021[15]). These recruitment efforts were in line with those taken in the health system (see the chapter on workforce).
Action focused on recruitment of former and unemployed LTC workers, LTC students and volunteers. A few initiatives were put in place to recruit foreign workers (as in Israel, which brought in 2 500 foreign workers) or to implement fast-track training programmes. For example, Canada committed CAD 23.2 million in 2020 to support training of up to 4 000 personal support worker interns through an accelerated six‑week online training programme combined with a four‑month work placement, to address acute labour shortages in the LTC and home care sectors. Countries that had a “sanitary reserve” force, such as France and Luxembourg, activated it. In Luxembourg, nearly 200 health professionals were deployed in LTC facilities during the first wave of the pandemic in 2020, but the recruitment efforts were still insufficient to address staff shortages.
As at 2022, the evidence about the short-term and long-term effects on turnover of LTC workers is scarce, although ten countries reported a perceived increased turnover since the beginning of the pandemic. At the same time, in Japan, survey data showed that the turnover rate was on a downward trend, and the total turnover rate of LTC workers in October 2019 to September 2020 was the lowest since fiscal year 2005. In the United Kingdom, Skills for Care reported that between 2019/20 and 2020/21 the turnover rate for care workers decreased from 38% to 34%. However, unweighted updates reported by Skills for Care in 2021/22 suggest that the number of staff in the sector has been falling.
In addition, seven OECD countries reported increasing the responsibilities and workload of existing LTC workers, but many also recognised LTC workers for their particularly heavy workload during the pandemic. For example, at the absorb stage of the pandemic, Finland allowed deviations from statutory annual leave to ensure sufficient staff availability. Exceptionally, France moved the maximum legal daily work time from 10 hours to 12 hours in April 2020. In Slovenia, health and social care providers also worked prolonged working hours (overtime). Germany suspended regular quality controls in LTC facilities at the beginning of the pandemic. About 50% of the 26 OECD countries surveyed in the 2021 OECD Survey on COVID‑19 and LTC provided one‑off bonuses to LTC workers for their exceptional efforts in 2020 (Rocard, Sillitti and Llena-Nozal, 2021[15]).
Task shifting was another strategy used to respond to workforce shortages, although this is not new. In the United Kingdom, care workers have increasingly taken on responsibility for more clinical tasks delegated from nurses in recent years. There is no information on specific tasks that can or cannot be delegated in the code of practice of nurses, nor a national framework or process for delegation of health care tasks to care staff such as care workers. In addition, decisions on responsibility increases and the workload of LTC workers during the pandemic were generally made at a local level, depending on the specific context and needs of local authorities and care providers.
It is thus incumbent on OECD countries to prepare avenues for rapid recruitment of LTC workers in the event of crises such as pandemics. Recruiting former and unemployed LTC workers, LTC students and volunteers, and increasing LTC workers’ workload enabled countries to address LTC worker shortages rapidly. Timely investment in these measures will enable countries to be well prepared for – and better able to absorb and recover from – workforce shortages in the future.
7.4.3. Digital technologies were scaled up, especially in long-term care facilities
The pandemic highlighted the importance of digital technologies to ensure LTC continuity (see the chapter on digital foundations).
Greater use of fit-for-purpose technology in LTC facilities has demonstrated its potential to enhance co‑ordination with the health care system, increase productivity, improve working conditions and enhance care quality (OECD, 2020[26]). This can free up professionals’ time from tasks that can be automated, allowing them to focus on the activities that are most important for people in need of care. Recording of data on older people is a laborious task that is still done by hand in many countries. Electronic devices can help to automate registration of user data for monitoring and to enhance communication across teams (e.g. between a nursing home and a hospital). For example, digital needs assessments facilitate collection of multi‑use data relevant to key questions from providers and policy makers (see Box 7.3).
Box 7.3. Digital needs assessments
With a digital needs assessment, the data collected are likely to meet the data needs of a broad group of stakeholders, including those covering:
eligibility to public support
care planning for providers (provided the assessment takes place on a regular basis)
evaluation of care effectiveness (people are followed at different points in time)
monitoring of providers’ care quality indicators
monitoring of care quality at municipal and national levels
international comparisons of care quality, if using standardised needs assessment instruments already implemented in many countries (e.g. InterRAI instruments).
While digital needs assessments are extremely useful, there are two pre‑requisites: an excellent IT system and trained staff.
While over half of surveyed OECD countries did not have programmes or guidelines on development of telehealth services in LTC before the outbreak, 21 OECD countries expanded the use of telehealth services to allow remote consultations between patients and the health care sector, and to keep LTC residents in touch with their relatives outside the facilities. Scaling up digital technologies includes setting up coverage rates or fee‑for-services, remote management, data sharing and monitoring technologies (see the chapter on care continuity for other examples).
For example, Portugal developed a digital platform to help residential facilities monitor the health status of COVID‑19‑positive residents. It generated alerts if situations arose in which it was necessary to intervene; facilitated recording and monitoring of users’ measurements; and supported institutions in active surveillance of symptoms associated with COVID‑19, as well as early identification of other respiratory diseases (Rocard, Sillitti and Llena-Nozal, 2021[15]).
Digital technologies were also useful to maintain social contact between LTC residents and their relatives, especially when facilities experienced outbreaks. Pre‑requisites for this include enough skilled staff, allowing staff to support contact, access to technologies and good internet connections. There is no “best” way to stay in touch for LTC residents and their relatives. While the pandemic led to new methods of contact (such as tablets), other ways were also used, such as phone calls and mail. Preferred options could be part of residents’ care plans, which should be updated regularly.
7.5. More resilient long-term care systems need to be built
There are many options available to OECD countries to improve LTC resilience in response to future shocks. Many OECD countries could harmonise their LTC governance and needs assessments to develop one coherent LTC system. As financial sustainability is crucial to more resilient LTC, avenues to fund better and more LTC could be considered. In addition, many countries could develop further preventive and rehabilitation services, as well as end-of-life care at home, to improve quality of life and potentially limit spending increases. They could also build on current recruitment and retention measures to expand the LTC workforce and offer better support for informal carers to help them continue to provide care.
7.5.1. Fragmentation of care in long-term care needs to be eliminated
At the onset of the pandemic, early responses were key to limiting and absorbing the health impact of infections. However, this was challenging because LTC systems tend to be very fragmented. Harmonising LTC governance and needs assessments for LTC cash benefits and services are necessary to create coherent LTC systems, rather than aggregations of cash and in-kind benefits with overlaps and gaps. More coherent systems would be better prepared to cope with external shocks such as COVID‑19, and resilient enough to withstand population ageing.
LTC governance would improve integration of LTC systems
Many countries in the OECD lack coherent LTC systems. LTC systems are sometimes spread out across health and social sectors, and incoherent frameworks result in overlaps and gaps in access and coverage, and possible cost shifting. Fragmentation also makes it difficult for users to get the support they need, considering the complexity of the system they must navigate. Harmonising LTC governance would foster integration in the sector. Single legislative frameworks and stronger public organisations dedicated to LTC are key methods to achieve coherent and stronger LTC governance. Ensuring a single entry-point to provision of cash benefits and services based on one standardised needs assessment would help with building more resilient LTC systems.
In Estonia, Latvia, Lithuania and the Slovak Republic, for example, separate legislative frameworks specify the division of responsibilities between the health care and the social care sector. These frameworks do not necessarily seek to harmonise provision of public support across the health and social sectors to form one coherent LTC system. The lack of co‑ordination with hospitals and other parts of the health care system does not help (Box 7.4; see also Box 7.2).
Box 7.4. Unnecessary hospital admissions resulting from a lack of co‑ordination with the health care system
The fragmentation of LTC systems leads to a lack of co‑ordination between LTC workers, primary care professionals, hospitals and social workers. Poor co‑ordination increases the risk of unnecessary hospitalisation, long hospital stays and readmissions. For example, a study of six areas of England (United Kingdom) found that care home residents experienced 0.78 emergency admissions each per year on average, compared with around 0.11 for England as a whole (although the areas were not representative of England overall). Even though residents have higher needs, the authors estimated that 40% of admissions from care homes were for conditions that could potentially be managed outside the hospital setting or avoided altogether – such as pneumonia or urinary tract infections (Steventon et al., 2018[27]; Lloyd et al., 2017[28]).
However, there are exceptions. In Portugal, LTC is provided jointly, as the Ministry of Health and the Ministry of Labour and Social Solidarity (responsible for social services) agreed on joint assessments and services in 2006 (Lopes, Mateus and Hernández-Quevedo, 2018[29]), and the pandemic reinforced this co‑ordination. In Scotland (United Kingdom), the government unified health and social care in 2016 to enhance services for LTC users. Slovenia passed a law in 2021 that defines LTC and outlines integration of health and social services for adults, after longstanding discussions. In Finland, a landmark law passed in 2021 will integrate health care and social services, including LTC, in 2023. In Lithuania, an ongoing reform process aims to integrate health and social services for older people (OECD, 2022[30]).
While there is no one‑size‑fits-all approach for a single LTC-related legislative framework, essential elements typically include definition of LTC (including a possible age threshold1), roles and responsibilities, needs assessments (except in some Scandinavian countries), cash benefits, services and financing schemes. Other laws related to finance typically set out funding routes, except in countries that have LTC insurance (such as Germany).
Single legislative frameworks are relatively recent – they were typically implemented within the last 30 years or so in Austria, France, Germany, Japan and the Netherlands. Austria has had one legislative framework since 1993, and Germany since 1995. In Japan, LTC insurance and the current LTC system were adopted in 2000.
In a number of OECD countries, a specific public organisation is in charge of a least one element of the LTC system, and often serves as the basis on which countries’ LTC systems are built. In countries with LTC insurance, like Germany and Japan, the LTC insurance fund is usually a public organisation. France, Scotland (United Kingdom) and Slovenia recently decided to strengthen the role of these LTC-related public organisations to build better integrated LTC systems. France is gradually expanding the role of one public organisation (CNSA) over a 10‑year period by transferring or giving more responsibilities for funding, financing and care provision, to ensure full integration and development of LTC. A 2020 law started the expansion by transferring the current funding schemes to this organisation and developing a roadmap. The CNSA will become the organisation in charge of a new branch called “autonomy”, which covers the majority of LTC for disabled adults and older people. It should be fully operational in 2030. Scotland passed a law in 2022 to create a new body – the National Care Service. It will be formed to set standards and commissioning priorities for delivery by newly established local care boards by 2026. In doing so, it will take away responsibility for social care from local authorities and centralise it. Slovenia’s 2021 reform has given an important role and new responsibilities to a new branch of the health insurance fund to assess LTC needs and manage the distribution of funds.
Harmonising cash benefits and services would reduce fragmentation
The current body of evidence suggests that well-structured and developed LTC benefits and services reduce use of emergency care (Rapp; Chauvin and Sirven, 2015[31]), and hospital admissions and utilisation. In Spain, a study showed that the structural LTC reform of 2007 reduced hospital admissions and use among both those receiving a caregiving allowance and beneficiaries of publicly funded home care, which amounted to 11% of total health care costs. Regions that had an operative regional health and social care co‑ordination plan saw stronger declines. This reform introduced a new structure of care benefits and expanded the availability of publicly funded home care (Costa-Font; Jimenez-Martin and Vilaplana, 2018[32]). However, the evidence remains mixed, and effect on hospital admissions and use is not always clear.
Nationwide standardised needs assessments are in place in Austria, Belgium, the Czech Republic, France, Germany, Japan, Latvia, Lithuania, the Netherlands, Portugal and Spain to ensure equal access and to reduce incidence of cost shifting. Ireland and Slovenia are introducing nationwide standardised needs assessments as part of ongoing LTC reforms. However, some countries have more than one LTC needs assessment, because they target different benefits (e.g. a specific cash benefit) or because they are designed by and for subnational areas, such as municipalities. For example, Swedish municipalities set their own needs assessments. Lithuania has one needs assessment for social services at home or in care institutions, and one for home care provided by the health care system, but none to access nursing hospitals (where a doctor’s referral is needed), although nursing hospitals overlap with care institutions. This fragmentation leads to overlaps and gaps in services, and more coherent frameworks for needs assessment might improve efficiency (OECD, 2022[30]).
Needs assessments typically evaluate a wide range of physical and mental capacities (see Figure 7.5). A gradation ladder of LTC needs is identified. Users of LTC are placed into tiers on the ladder depending on the severity of their condition, and receive higher or lower benefits accordingly. This can ensure that access to LTC cash benefits and services is identical across a country, and the approach tends to be easier to navigate for LTC recipients and their relatives. Such ladders exist in OECD countries, such as France, Germany and soon Slovenia. Each care grade can be related to a type of support – whether formal services, a cash benefit to LTC users, or direct or indirect cash benefits for informal caregivers. One advantage is that this can ensure that eligible people receive coherent benefits. It can also help operationalise a transition towards a more community-based care model that would reserve LTC facility space for those who need it the most. In addition, it can empower LTC users to choose the form of LTC care that works for them, whether formal or informal – which may help in part to address staff shortages.
Figure 7.5. A needs assessment linked to a gradation ladder of LTC needs
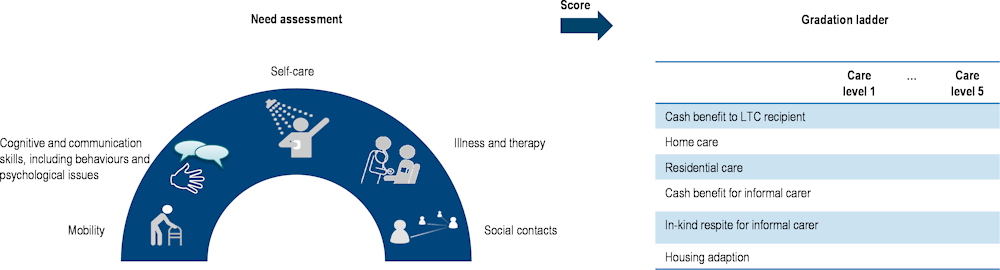
Note: This diagram builds on several needs assessments and gradation ladders, but does not represent any specifically.
7.5.2. Long-term care systems need further financing to be more resilient and meet more people’s needs
Provision of LTC for people with limitations in activities of daily living or instrumental activities of daily living can be very costly, but the generosity and coverage of the LTC system can be very limited (Oliveira Hashiguchi and Llena-Nozal, 2020[33]), in part because of insufficient funds. As a result, either the costs are borne elsewhere by families, civil society and other informal caregivers, or LTC needs are left unmet. About 30% of older people with at least one limitation in activities of daily living reported unmet LTC needs across 22 OECD countries in 2019‑20, based on SHARE data.
During the COVID‑19 pandemic, about 89% (17 out of 19 surveyed countries) of surveyed OECD countries reported that substantial temporary additional financing was made available to bolster LTC services (Box 7.5). However, many countries would need to increase funding permanently to increase the number of LTC workers.
Even without aiming to increase the LTC workforce and reduce unmet needs, countries should consider further additional permanent funding to factor in population ageing and to build resilience to future disruptions, including climate change. The share of people aged 65 years and over will reach 27% by 2050 across the 38 OECD countries, compared with 17% in 2019. About 11% of older people received LTC in 2019 across the 23 OECD countries with available data. Older care recipients depend on carers and medications that may be unavailable when absorbing and responding to future disruptions. They are also more likely to be isolated, making them more difficult to reach. With climate change disruptions, older people are at elevated risk for various reasons; for example, they are especially vulnerable to extreme temperatures since capacity to maintain core body temperature becomes compromised with age.
Box 7.5. Temporary funding provided to LTC systems in response to the pandemic across OECD countries
Canada committed up to CAN 1 billion through the Safe Long-Term Care Fund to help provinces and territories improve infection prevention and control in LTC (for example, via hiring additional staff, wage top-ups, new or renovated infrastructure including ventilation, and readiness assessments). In addition, the Safe Restart Agreement included CAN 740 million in funding to improve infection prevention and control measures to protect those in LTC, home care and palliative care. Canada also provided CAN 3 billion in emergency federal funding to its provinces and territories to increase the wages of low-income essential workers, including workers in LTC facilities and in the home care sector. In addition, it announced a further CAN 3 billion investment, starting in 2022‑23, to support provinces and territories in their efforts to ensure that standards for LTC are applied, and permanent changes are made. Provinces and territories have also invested substantially to improve LTC services.
In Germany, expenditure on LTC insurance for pandemic-related expenses in LTC facilities (nursing homes, day care and care services) and for family carers totalled EUR 4.87 billion in 2021.
In Japan, the budget to cover the costs of emergency hiring of LTC staff and disinfection and other measures reached JPY 6.8 billion in fiscal year 2020 (government expenditure basis). This was covered as part of a budget of JPY 13.7 billion for LTC facilities with outbreaks. Japan also supported thorough countermeasures against infectious diseases in LTC facilities and provided benefits to LTC staff as part of a budget of JPY 491.8 billion for fiscal year 2020 (government expenditure basis).
The United Kingdom supported LTC services for disabled adults and older people with funding of GBP 1.81 billion for infection prevention and control and GBP 523 million for testing. In addition, GBP 583 million was provided to support workforce capacity, recruitment and retention through the Workforce Capacity Fund in 2021 and two Workforce Recruitment and Retention Funds in 2021‑22. The United Kingdom made available an additional GBP 60 million to local authorities through the Omicron Support Fund in January 2021.
The United States provided additional financing through the Coronavirus Aid, Relief, and Economic Security (CARES) Act. Nursing homes and assisted living communities received about USD 14 billion from the Provider Relief Fund established by the CARES Act. The American Rescue Plan includes USD 200 million to support infection control and vaccine uptake at skilled nursing facilities. In addition, USD 337.5 million was appropriated to extend the existing Money Follows the Person Programme, which provides support to Medicaid beneficiaries requiring LTC moving from institutions to the community. The federal government also provided additional funding to states, including to help them address existing home and community-based workforce and structural issues, expand the capacity of critical services, and begin to meet the needs of people on waiting lists and family caregivers. Some states increased Medicaid reimbursement to nursing homes.
Pooling existing funding can be a step towards better funding. Combining funds into one well-defined budget can also improve transparency and facilitate distribution of existing funds in a more effective and efficient manner. It can help to reduce unnecessary activities, overuse of services, duplication of effort and cost shifting. For example, France has pooled the majority of its LTC funding schemes for the CNSA since 2020 to facilitate collection and the distribution of funds. An important next step is that the organisation should receive additional funds collected via the “generalised social contribution tax” to fund LTC services currently covered by statutory health insurance by 2024.
Many citizens reportedly support greater spending on LTC services, even if this would mean increasing taxes and social contributions. In 2020, between about 45% and 90% of people reported that they were concerned about not being able to access good-quality LTC, according to the OECD Risks That Matter Survey. In addition, around 20‑50% of people would be ready to pay an additional 2% of their income in taxes and social contributions to fund more public support for LTC (see Figure 7.6).
Figure 7.6. Proportion of people willing to pay more taxes to fund LTC across 25 OECD countries
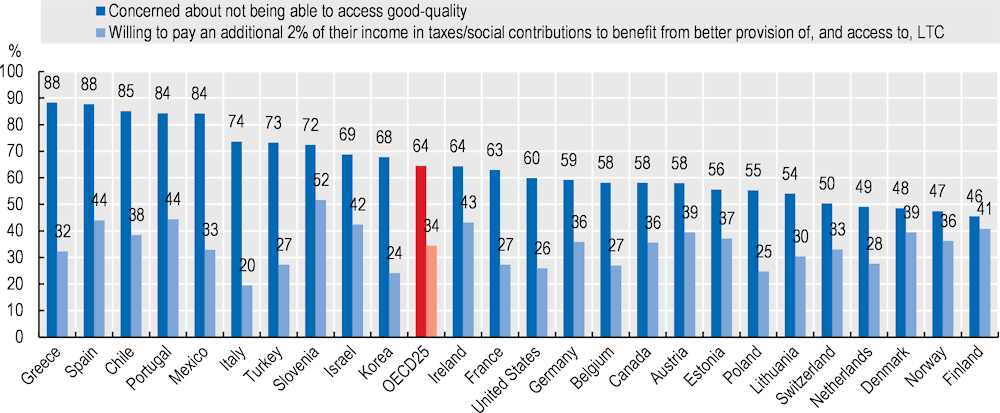
Source: OECD Risks That Matter Survey (data refer to 2020).
Avenues to fund more LTC services may rely on diverse and broad-based funding routes. These comprise LTC insurance, taxes and social contributions on incomes and assets. Diverse sources of funds might also make LTC systems more resilient to individual shocks.
LTC insurance may be one approach to ensure more funding. Belgium, Germany, Japan, Korea, Luxembourg and the Netherlands have implemented a public form of LTC insurance. In Japan, about half of funding comes from LTC insurance and the other half from national and subnational taxes. The Japanese LTC insurance fund spent JPY 11.1 trillion in 2018 (over EUR 79 billion in nominal euros of 2022). Slovenia passed an LTC law in 2021 that defines the broad future funding routes of the future LTC system – a mixture of a new LTC insurance borne by workers, current pension and health insurance funds reallocated to LTC and the state budget (OECD, 2022[30]). In accordance with the LTC Act, funding for LTC will be provided from existing funds and the state budget until mid‑2025, and adoption of a specific law on compulsory insurance for LTC is planned during this timeline.
Advantages of LTC insurance include greater transparency in managing funds and horizontal justice. Transparency is improved because the introduction of LTC insurance links funds to specific policies. Horizontal justice means that the services are the same for everyone, independent of the incomes of people in need, while contribution levels increase with the incomes of contributors. However, LTC insurance can create the expectation that anyone should access LTC, meaning that people might expect to be entitled to the benefit even if demand were to increase. If the LTC insurance fund were insufficient, countries would need to complement it with taxes and social contributions, and/or borrow to meet citizens’ expectations.
The main advantages of tax-based funding for LTC systems are that taxes can be broad-based, and citizens can expect benefit expenditure to align with public financial resources. However, there are sometimes concerns about fluctuations in funding – especially during an economic recession – as well as a lack of transparency in allocation of funds. Tax-based funding for LTC systems exists in many OECD countries, including in Austria, Scandinavian countries and Spain.
Funding can also come from a mixture of social contributions and taxes; in this case, countries typically levy money on a base broader than labour incomes. For example, in France, funding stems mostly from social contributions and taxes that cover a base that goes well beyond labour income.2 In many central and eastern European countries, LTC funding from the social sector is more tax-based, while LTC funding from the health care sector is more mixed.
Improving funding for LTC services is vital to address the needs of older people. It represents a substantial investment in the lives of future LTC recipients and the LTC workforce. This is imperative at a time when many OECD countries are experiencing ageing populations in a context of high inflation and budgetary pressure. There is a tension between improving LTC resilience and short-term budgetary sustainability, which should be addressed.
7.5.3. Further preventive and rehabilitation services and end-of-life care need to be developed
OECD countries could consider developing preventive and rehabilitation services at home to improve quality of life and potentially limit cost increases while improving resilience. Developing end-of-life care may be another cost-efficient means to improve quality of life. Increasing preventive care and rehabilitation decreases the vulnerabilities of the population. In turn, this improves resilience by reducing requirements on health and LTC systems in times of stress.
Preventive and rehabilitation services can improve quality of life and be cost-efficient
Scandinavian countries and some other OECD countries have well-developed preventive and rehabilitation services that can contribute to improving quality of life and potentially be cost-efficient. Preventive and rehabilitation services can help to postpone LTC needs, thereby potentially containing LTC expenditure.
In Denmark, municipalities provide preventive services, including preventive home visits and activities. Everyone aged over 75 years must be offered a home visit. The offer is also extended to people aged 65‑75 years who are in a special risk group, including widows, people who live in a secluded area and those recently discharged from hospital. Finally, those aged 80 years and over are offered a visit every year. Municipalities can organise group visits for those who usually decline home visits. Municipalities also carry out preventive activities of varying scope and type, such as workshops, education, talks and physical activity (Kvist, 2018[34]).
In Norway, introduction of the Preventive Home Visit Programme significantly lowered residential care in LTC facilities while increasing home care. A study found that care in nursing homes was reduced by 1.4 percentage points among people aged 80 years and over, from a baseline of 19%. This decline was partly matched by an increase in home‑based care, from a baseline of 35%. In addition, hospital admissions were reduced by about 7%, and mortality rates declined by nearly 5% in the years following the introduction of preventive home visits (Bannenberg et al., 2021[35]). Overall, evidence indicates that many preventive programmes are cost-effective (Scheckel, Stock and Müller, 2021[36]), and that preventive services can support LTC resilience.
Denmark has also put strong emphasis on rehabilitation services. Municipalities must offer a short and intensive (4‑10 weeks) rehabilitation programme prior to assessing the need for home help. The programme comprises one or more of the following elements: training in everyday activities (personal care), physical training, assistive devices and adaptation of the home (Kvist, 2018[34]). In 2018, 4.3% of people aged 65 years and over received rehabilitation services instead of – or alongside – home help (Rostgaard, 2021[37]). Danish evidence shows improvements in functional ability, a reduction in home care use and higher work motivation among staff. While there are no studies on the cost-effectiveness of these rehabilitation services, a decrease in home care use suggests possible savings (Rostgaard, n.d.[38]). More generally, a body of evidence shows that many specific rehabilitation programmes (e.g. for stroke) are cost-effective (Allen et al., 2018[39]).
End-of-life care at home can also improve quality of life and be cost-efficient
Countries could also strengthen end-of-life care for LTC recipients to respect their preferences. In addition, evidence from several countries shows that introduction of better access to palliative care can result in more cost-effective outcomes (Public Health England, 2017[40]). The effectiveness of palliative care stems mainly from reducing the length of hospital stays, readmissions and visits to intensive care units, thereby reducing the strain on health systems – including during times of disruption and stress. Hospital palliative care teams can be cost-effective, for instance, especially with early introduction and when integrated with other treatments (KMPG, 2020[41]).
When nearing the end of life, older people generally have a preference about their place of death. However, the actual place of death often does not align with these preferences. Home is often indicated as the patients’ preferred place of death (Calanzani et al., 2014[42]). However, 50% of all deaths occurs in hospitals across 22 OECD countries, although the share decreased slightly in the last decade (2009‑19) in over half of OECD countries (see Figure 7.7).
Figure 7.7. Deaths occurring in hospitals in 2019 across OECD countries
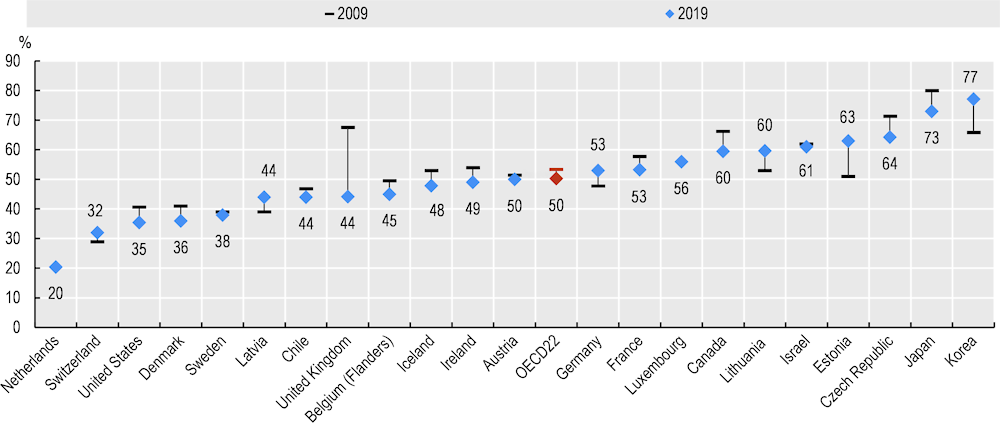
Source: OECD (2021[43]), Health at a Glance 2021: OECD Indicators, https://doi.org/10.1787/ae3016b9-en.
Some OECD countries reported that the pandemic and its policy responses negatively affected palliative care (Canada, France, Israel, Mexico, Slovenia, the United Kingdom and the United States), although evidence is lacking or anecdotal. For example, a report noted that many LTC workers administered medical and palliative care in the absence of GPs (Oung, 2022[44]). In Luxembourg, primary care doctors were permitted in April 2020 to retrieve “COVID‑19 kits”, which contained end-of-life care medication – including for pain management and relief, from specific pharmacies.
The availability of staff with end-of-life care knowledge is important to ensure both early identification of needs and adequate access to end-of-life care services at home and in institutions. In OECD countries, primary care professionals are not necessarily sufficiently trained and palliative care training could also be more common in nursing school education. Residency programmes for GPs/primary care doctors incorporates some palliative care training in 22 OECD countries (65%) and in less than half (44%) of 25 OECD countries medical schools include mandatory palliative care education in undergraduate curricula. Nearly three‑fifths (58%) of 24 OECD countries include mandatory palliative care training in nursing school curricula, and a further 21% report that palliative care training in undergraduate nursing programmes is mandatory in at least some regions of their country (OECD, 2023[45]).
Some countries have recently developed guidelines and training programmes to improve knowledge around end-of-life care among LTC workers. In Australia, the End of Life Direction for Aged Care toolkits aim at providing LTC workers with better knowledge and understanding of end-of-life care. England (United Kingdom) has piloted a training model for care homes, where LTC workers receive training from hospital teams on recognising dying, advance care planning, co‑ordination of care, symptom control, and bereavement care. Results from the pilot showed an increase in the share of people dying in their preferred place. Nevertheless, care guidance on end-of-life care is more common in hospital settings (90%) than in LTC facilities (62%) (OECD, 2023[45]).
7.5.4. Efforts are needed to ensure that sufficient carers are available in the long term
Providing LTC is labour-intensive. The pandemic has exacerbated workforce shortages, while informal carers have had to ensure care continuity, adding more pressure on them. Strengthening recruitment and retention policies for formal LTC workers is key to building LTC resilience and avoiding shifting the burden to health systems under stress (see the chapter on workforce). In addition, better public support for informal carers will help them continue to care.
Recruitment and retention policies are needed to tackle staff shortages
Poor working conditions contribute to structural staff shortages. Even though OECD countries have been implementing recruitment and retention policies, additional measures are needed. Non-standard working conditions contribute to low attraction and retention in the sector. About 42% of LTC workers worked part time in OECD countries in 2019. Temporary employment is also common. About 17% of LTC workers held a temporary contract in OECD countries in 2019. In addition, pay is often low. In more than half of OECD countries, population ageing has been outpacing the growth of LTC supply in the last decade (OECD, 2021[43]). In response, countries have implemented three main types of policies over the last decade. These aim to widen recruitment efforts to attract workers; to improve retention by enhancing working conditions, job quality and training for career progression; and to increase the effectiveness of the services provided (OECD, 2020[26]).
Following the start of the pandemic, the Czech Republic, France, Germany, Korea and other countries improved wages permanently to attract and retain more workers (more in the forthcoming Beyond Applause OECD publication).
Another option that emerged during the pandemic was increasing the minimum staff ratio recommendations or requirements. Four countries introduced guidelines on staff ratios (Japan, Lithuania, the Netherlands and Slovenia). In Ontario, Canada, in November 2020 the provincial government announced a commitment to increase the minimum number of hours of direct care to an average of four hours per resident by 2024‑25. In Finland, under the Older Person’s Care Act, the nurse‑client staffing ratio will be increased gradually from 5:10 to 7:10 by 2023, and will vary according to needs assessments.
Rising minimum staffing levels can be associated with better care quality, but higher requirements come at a cost. In the United States, a study examined the effect of a proposal to raise minimum staffing levels (presented in Congress in 2019) in skilled nursing facilities – for the three American categories of nurses and in total (4.1 total nursing hours per resident day). In 2019, only 5% of skilled nursing facilities met all four categories of minimum staffing levels; 25% met the minimum 4.1 total nursing hours per resident day, while 31% met the threshold for registered nurses, 85% met the threshold for licensed practical nurses, and 11% met the threshold for certified nursing assistants. Achieving the proposed federal minimums nationwide would require an estimated additional 35 804 registered nurses, 3 509 licensed practical nurses and 116 929 certified nursing assistants (full-time equivalent), at an annual salary cost of USD 7.25 billion (Hawk et al., 2022[46]).
At the same time, high rates of staff turnover generate not only a poorer quality of care but also higher costs. Turnover means that replacement staff need to be hired, which entails recruitment costs and generates periods of understaffing. In addition, newly hired personnel require training in the facility’s policies and work procedures (OECD, 2020[26]).
Factoring in these needs in short-term and medium-term workforce projections and budget allocation decisions is essential for a sustainable recovery from the pandemic, while avoiding over-reliance on redeployment and minimising disruptions to provision of LTC services (WHO, 2022[20]).
Better public support for informal carers would help them continue to provide care
Over recent decades, community-based LTC has been encouraged for various reasons – it respects people’s preference to stay at home and it can be seen as a less costly option than LTC facilities. It is typically used when LTC needs are moderate, and when older people do not have strong cognitive limitations or aggressive behaviour towards LTC workers. Over 50% of care recipients at home reported a combination of formal and informal care across 28 OECD countries in 2021, based on SHARE data.
Informal carers make a substantial contribution to societies and to broader societal resilience to address future shocks. A European Commission-funded study estimated that the value of the number of hours spent on informal care of older people and disabled adults probably ranged between 2.4% and 2.7% of EU GDP in 2018, depending on the methodology and assumptions used. In comparison, public expenditure on LTC was estimated at 1.7% of EU GDP in 2019 (European Commission, Directorate-General for Employment, Social Affairs and Inclusion, 2021[47]).
While informal carers may provide the bulk of care, and may be the preferred option of older people, they can suffer from negative consequences of care. Informal carers report negative impacts on their labour-force participation, finances, and physical and mental health, especially if they provide intensive care (more than 20 hours per week) or care for someone with strong cognitive limitations (e.g. dementia) (Rocard, E; Llena-Nozal, A, 2022[48]).
The participation of informal carers is not guaranteed in the future. Demographic changes are at play, including higher labour-force participation of women (who represent most carers, especially among the working-age population), smaller families and greater geographical distances between family members.
A comprehensive set of policy measures would make care more manageable for informal carers, including provision of information on support, counselling and training, respite, cash benefits, leave and other flexible work arrangements. While governments have improved access to information for carers in the past decade, provision of counselling and training continues to depend heavily on the voluntary sector. Moreover, respite measures typically remain insufficient, with low rates of uptake due to low compensation, low availability of services and organisational challenges. About two‑thirds of the OECD countries provide cash benefits to informal carers, either paid directly through a carer’s allowance or paid to those in need of care, at least part of which is then used to compensate registered informal carers formally. Nearly two‑thirds of OECD countries also mandate paid or unpaid leave entitlements to provide care for a family member (Rocard, E; Llena-Nozal, A, 2022[48]).
7.6. Conclusions: Preparation reduces the impact of crises in long-term care
The COVID‑19 pandemic has severely affected the LTC sector, with substantial infection and mortality rates among LTC residents, and delayed and cancelled care. Over one‑third of all COVID‑19 deaths were among LTC recipients. LTC workers were also very exposed – falling ill or working longer hours, and informal carers generally reported an additional burden.
The LTC sector was not sufficiently prepared to absorb the COVID‑19 pandemic initially, but infection prevention and control protocols, testing and PPE in long-term care became available. Countries implemented task forces to react promptly to outbreaks. They also sought to overcome temporary staff shortages by using mobile teams and recruiting additional workers. Countries generally expanded use of digital technologies to ensure care continuity and maintain social contacts.
While invaluable, most of these measures have been temporary and limited. Many OECD countries can – and should – make structural changes to build stronger LTC systems to withstand population ageing, transition further towards a community-based model and strengthen resilience to future shocks. Eliminating fragmentation of care by harmonising LTC governance, needs assessments, and cash benefits and services are important avenues to build resilient long-term care systems. Countries could also consider additional permanent funding of LTC based on diverse and broad-based funding routes.
Countries could develop further preventive and rehabilitation services and end-of-life care for LTC recipients. These services can improve quality of life while potentially being cost-efficient.
Finally, countries can ensure that sufficient carers are available by strengthening recruitment and retention policies for LTC workers (see chapters on workforce and investing in resilience), and providing better public support to informal carers.
References
[39] Allen, L. et al. (2018), “Assessing the impact of a home-based stroke rehabilitation programme: a cost-effectiveness study”, Disability and Rehabilitation, Vol. 41/17, pp. 2060-2065, https://doi.org/10.1080/09638288.2018.1459879.
[5] Association of Directors of Adult Social Services (2021), ADASS Snap Survey 21 - rapidly deteriorating picture of Social Care Services, https://www.adass.org.uk/snap-survey-nov21-rapidly-deteriorating-social-services.
[35] Bannenberg, N. et al. (2021), “Preventive Home Visits”, American Journal of Health Economics, Vol. 7/4, pp. 457-496, https://doi.org/10.1086/714988.
[17] Berloto, S. et al. (2020), Italy and the COVID-19 long-term care situation, International long-term care policy network, https://lab.gedidigital.it/gedi-visual/2020/coronavirus-i-contagi-in-italia/?ref=RHPPRB-BS-I254751933-C4-P1-S1.4- (accessed on 9 December 2020).
[42] Calanzani, N. et al. (2014), “Choosing care homes as the least preferred place to die: a cross-national survey of public preferences in seven European countries”, BMC Palliative Care, Vol. 13/1, https://doi.org/10.1186/1472-684x-13-48.
[1] Canadian Institute for Health Information (2021), COVID-19’s impact on long-term care, https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/long-term-care (accessed on 12 July 2022).
[10] Canevelli, M. et al. (2020), “Facing Dementia During the COVID ‐19 Outbreak”, Journal of the American Geriatrics Society, Vol. 68/8, pp. 1673-1676, https://doi.org/10.1111/jgs.16644.
[18] Comas-Herrera, A. et al. (2020), “COVID-19: Implications for the Support of People with Social Care Needs in England”, Journal of Aging & Social Policy, Vol. 32/4-5, pp. 365-372, https://doi.org/10.1080/08959420.2020.1759759.
[16] Commission d’Enquête Évaluation des politiques publiques face aux pandémies (2020), Santé publique : pour un nouveau départ - Leçons de l’épidémie de covid-19, http://www.senat.fr/rap/r20-199-1/r20-199-1.html.
[32] Costa-Font; Jimenez-Martin and Vilaplana (2018), “Does long-term care subsidization reduce hospital admissions and utilization?”, Journal of Health Economics, Vol. 58, pp. 43-66, https://doi.org/10.1016/j.jhealeco.2018.01.002.
[11] Dementia UK (2020), Facing it alone: experiences of dementia support A report from Dementia UK Facing it alone: experiences of dementia support, Dementia UK, https://www.dementiauk.org/wp-content/uploads/2020/11/Facing-It-Alone.pdf.
[47] European Commission, Directorate-General for Employment, Social Affairs and Inclusion (2021), Study on exploring the incidence and costs of informal long-term care in the EU, https://data.europa.eu/doi/10.2767/06382.
[13] Eze, N., M. Cecchini and T. Oliveira Hashiguchi (2022), “Antimicrobial resistance in long-term care facilities”, OECD Health Working Papers, No. 136, OECD Publishing, Paris, https://doi.org/10.1787/e450a835-en.
[7] Fresno, J. (2020), Estudios propios, Auditoría de los centros residenciales en Navarra ante la crisis de la Covid-19. Observatorio de la Realidad Social de Navarra, Observatorio de la Realidad Social,, https://www.observatoriorealidadsocial.es/es/estudios/auditoria-de-los-centrosresidenciales-en-navarra-ante-la-crisis-de-la-covid-19/es-556293/#.
[46] Hawk, T. et al. (2022), “Facility characteristics and costs associated with meeting proposed minimum staffing levels in skilled nursing facilities”, Journal of the American Geriatrics Society, Vol. 70/4, pp. 1198-1207, https://doi.org/10.1111/jgs.17678.
[8] Hussein, S. et al. (2020), COVID-19 and the Wellbeing of the Adult Social Care Workforce: Evidence from the UK, https://www.pssru.ac.uk/resscw/files/2020/12/COVID19-and-the-UK-Care-Workers_FINAL_01dec20.pdf.
[2] Istituto Superiore di Sanità (2022), SORVEGLIANZA STRUTTURE RESIDENZIALI SOCIO-SANITARIE NELL’EMERGENZA COVID-19, Istituto Superiore di Sanità, https://www.epicentro.iss.it/coronavirus/pdf/REPORT_STRUTTURE_dic2020_gen2022_08022022.pdf.
[22] Jepsen, D. and T. Barker (2020), “COVID-19 reveals: Multi-stakeholder perspectives on single site employment Guiding Principles in Residential Aged Care Facilities,”, Discussion and Roadmap, Aged & Community Services Association, https://ltccovid.org/wp-content/uploads/formidable/3/Jepsen-Barker-MQ-Covid-Residential-Aged-Care-Single-Site-Employment-final-report-210606-1.pdf.
[23] Jones, A. et al. (2021), “Impact of a Public Policy Restricting Staff Mobility Between Nursing Homes in Ontario, Canada During the COVID-19 Pandemic”, Journal of the American Medical Directors Association, Vol. 22/3, pp. 494-497, https://doi.org/10.1016/j.jamda.2021.01.068.
[41] KMPG (2020), Investing to Save: The economics of increased investment in palliative care in Australia.
[21] Konetzka, R. et al. (2021), “A systematic review of long‐term care facility characteristics associated with <scp>COVID</scp> ‐19 outcomes”, Journal of the American Geriatrics Society, Vol. 69/10, pp. 2766-2777, https://doi.org/10.1111/jgs.17434.
[9] Korczyn, A. (2020), “Dementia in the COVID-19 Period”, Journal of Alzheimer’s Disease, Vol. 75/4, pp. 1071-1072, https://doi.org/10.3233/jad-200609.
[34] Kvist, J. (2018), ESPN Thematic Report on Challenges in long-term care in Denmark.
[28] Lloyd, T. et al. (2017), Effect on secondary care of providing enhanced support to residential and nursing home residents: A subgroup analysis of a retrospective matched cohort study, The Health Foundation, https://doi.org/10.1136/BMJQS-2018-009130.
[29] Lopes, H., C. Mateus and C. Hernández-Quevedo (2018), “Ten Years after the Creation of the Portuguese National Network for Long-Term Care in 2006: Achievements and Challenges”, Health Policy, Vol. 122/3, pp. 210-216, https://doi.org/10.1016/j.healthpol.2018.01.001.
[3] Lorenz-Dant; Fischer and Hämel (2022), COVID-19 and the Long-Term Care system in Germany, In: Comas-Herrera A., Marczak J., Byrd W., Lorenz-Dant K., Pharoah D. (editors), https://ltccovid.org/ltccovid-country-profile-germany/ (accessed on 12 July 2022).
[25] Low, L. et al. (2022), COVID-19 and the Long-Term Care system in Australia, In: Comas-Herrera A., Marczak J., Byrd W., Lorenz-Dant K., Pharoah D.(editors), https://ltccovid.org/country-page-australia/ (accessed on 12 July 2022).
[14] Médecins Sans Frontières (2020), Les laissés pour compte de la réponse au Covid-19, Partage d’expérience sur l’intervention de Médecins Sans Frontières dans les maisons de repos de Belgique,, https://www.msf-azg.be/sites/default/files/imce/Rapport_MaisonsDeRepos/MSF_lessons%20l.
[6] Mission d’information sur l’impact, la gestion et les conséquences dans toutes ses dimensions de l’épidémie de Covid 19 (2020), Rapport d’information, Assemblée Nationale, Paris, https://www2.assemblee-nationale.fr/static/15/pdf/rapport/i3633.pdf.
[45] OECD (2023), Time for Better Care at the End of Life, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/722b927a-en.
[30] OECD (2022), Integrating Services for Older People in Lithuania, OECD Publishing, Paris, https://doi.org/10.1787/c74c44be-en.
[43] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[24] OECD (2021), “Long-term care workers”, in Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/c8078fff-en.
[26] OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/92c0ef68-en.
[33] Oliveira Hashiguchi, T. and A. Llena-Nozal (2020), “The effectiveness of social protection for long-term care in old age: Is social protection reducing the risk of poverty associated with care needs?”, OECD Health Working Papers, No. 117, OECD Publishing, Paris, https://doi.org/10.1787/2592f06e-en.
[44] Oung, C. (2022), COVID-19 and the Long-Term Care system in France, https://ltccovid.org/covid-19-and-the-long-term-care-system-in-france/ (accessed on 12 July 2022).
[40] Public Health England (2017), Cost-effective commissioning of end of life care: Understanding the health economics of palliative and end of life care.
[31] Rapp; Chauvin and Sirven (2015), “Are public subsidies effective to reduce emergency care? Evidence from the PLASA study”, Social Science & Medicine, Vol. 138, pp. 31-37, https://doi.org/10.1016/j.socscimed.2015.05.035.
[48] Rocard, E; Llena-Nozal, A (2022), “Supporting informal carers of older people: Policies to leave no carer behind”, OECD Health Working Papers, No. 140, OECD Publishing, Paris, https://doi.org/10.1787/0f0c0d52-en.
[15] Rocard, E., P. Sillitti and A. Llena-Nozal (2021), “COVID-19 in long-term care: Impact, policy responses and challenges”, OECD Health Working Papers, No. 131, OECD Publishing, Paris, https://doi.org/10.1787/b966f837-en.
[37] Rostgaard, T. (2021), Long-term care for older people living at home – Danish experiences in a Nordic context.
[38] Rostgaard, T. (n.d.), Reablement as a mechanism for sustainability and active long-term care, http://www.transforming-care.net/thematic-panel-3-reablement-as-a-mechanism-for-sustainability-and-active-long-term-care/ (accessed on 10 April 2022).
[12] Rothgang, H. et al. (2020), How Covid-19 has affected informal caregivers and their lives in Germany, https://ltccovid.org/2020/09/20/how-covid-19-has-affected-informal-caregivers-and-their-lives-in-germany/.
[36] Scheckel, B., S. Stock and D. Müller (2021), “Cost-effectiveness of group-based exercise to prevent falls in elderly community-dwelling people”, BMC Geriatrics, Vol. 21/1, https://doi.org/10.1186/s12877-021-02329-0.
[27] Steventon, A. et al. (2018), Briefing: Emergency hospital admissions in England: which may be avoidable and how?, The Health Foundation.
[19] Tsadok-Rosenbluth, S. et al. (2021), “Centralized Management of the Covid-19 Pandemic in Long-Term Care Facilities in Israel”, Journal of Long Term Care, pp. 92-99, https://doi.org/10.31389/jltc.75.
[20] WHO (2022), Strategic preparedness, readiness and response plan to end the global COVID-19 emergency in 2022, World Health Organization, Geneva, https://www.who.int/publications/i/item/WHO-WHE-SPP-2022.1 (accessed on 12 July 2022).
[4] Wolf-Ostermann, K. et al. (2020), “Pflege in Zeiten von Corona: Ergebnisse einer deutschlandweiten Querschnittbefragung von ambulanten Pflegediensten und teilstationären Einrichtungen”, Pflege, Vol. 33/5, pp. 277-288, https://doi.org/10.1024/1012-5302/a000761.
Notes
← 1. This element is crucial to ensuring that LTC benefits are coherent with disability benefits.
← 2. France’s Generalised Social Contribution relies on a very broad base (capital income, pensions, unemployment benefits, etc.) and has a relatively low rate. It levies over EUR 100 billion every year, which is more than the personal income tax.