Gaétan Lafortune
Noémie Levy

Gaétan Lafortune
Noémie Levy
The COVID‑19 pandemic has exacerbated pre‑existing health workforce issues in OECD countries, including shortages of doctors and nurses, insufficient investment in education and training, and retention challenges. These shortages have increased workloads and pressures. Many health workers have emerged from the pandemic exhausted and intending to leave their positions. This chapter reviews the health workforce capacity of OECD countries going into the pandemic and strategies used to mobilise additional health workers (surge capacity) to respond to peaks in demand during the absorb stage of the pandemic. It also reviews new strategies implemented by countries to increase health workforce capacity and flexibility in the recovery stage of the pandemic, to avoid future shortages and increase preparedness for future shocks. Addressing health workforce shortages calls for greater investment in education and training, increased staff recruitment to reduce the workload and pressure on existing staff, and increased retention rates by improving working conditions and pay rates for categories of workers that have traditionally been undervalued. At least half of all new investments needed to make health systems more resilient should be directed towards workforce training, recruitment, and retention.
Health workers have shown remarkable dedication and resilience, serving at the front line in the fight against the COVID‑19 pandemic. The commitment of individual workers needs to be backed by system-level actions to support the resilience of the health workforce overall.
The pandemic exposed serious weaknesses in the health workforce in many OECD countries, revealing that it was understaffed, under pressure and undervalued:
The health worker shortages faced by many countries were arguably the biggest capacity constraint faced – even more so than the availability of equipment or hospital beds. Shortages of specialised doctors and nurses were particularly acute in hospital intensive care units (ICUs). Many countries also reported scarcities of nurses in other hospital units, of general practitioners outside hospitals and of health care assistants in nursing homes as important constraints in absorbing the effects of the pandemic.
Pre‑existing health workforce shortages meant that the burden of responding to the pandemic fell on already understaffed health systems. Asking staff to work overtime under extreme pressure can only work for a limited time or it results in burnouts and resignations.
Valuing frontline health care staff – particularly nurses and health care assistants – is vital to avoid a large exodus of health and long-term care workers. A silver lining of the pandemic is that it has shown the potential for greater task sharing and teamwork between doctors, nurses and other health care providers. However, expanded roles and responsibilities need to be financially recognised and rewarded.
Greater investments are needed to strengthen health workforce capacity and flexibility and avoid the risk of entering another public health crisis or other global disruption with these critical structural weaknesses. At least half of the investments to strengthen health systems across OECD countries should be allocated to training and recruitment; improving working conditions; and increasing the flexibility of the workforce to respond to shocks and strains.
Training more health workers: Several OECD countries have increased the number of students in medical and nursing education programmes in recent years to address shortages, although it takes years for these training decisions to take effect. It is heartening that the interest of young people in pursuing a career as a doctor or nurse does not appear to have lessened since the pandemic. In many countries (such as Italy, Spain, the United Kingdom and the United States), the number of applications and admissions to nursing education programmes rose in 2020/21 and 2021/22. However, attracting more male students remains a challenge: over 80% of nursing students in many countries are female, reflecting what is still perceived as “women’s work”.
Improving working conditions to increase retention: After three years of the pandemic, many health workers are exhausted and demotivated by what they consider to be a lack of recognition for their work. In several countries, about 20% of nurses reported in 2021 that they were considering leaving the profession in the short term. Evidence of high resignation rates among health workers has emerged in the United Kingdom and the United States. Improving working conditions requires reducing the workload and pressure on staff; supporting their health, well-being and safety at work; and reviewing their pay rates. Improved working conditions are particularly necessary for categories of workers that have traditionally been undervalued, such as nurses and health care assistants. They are also especially urgent in countries experiencing significant losses of doctors and nurses because of early retirement or emigration to other countries.
Increasing flexibility to respond to shocks and strains on health systems: The pandemic highlighted the need to mobilise additional health workers quickly to cope with a surge in demand for certain types of care. Most countries were able to mobilise such human resources by reallocating current staff to clinical areas with the greatest need (such as ICUs) and by drawing on retired or other inactive doctors and nurses, medical and nursing students nearing the end of their studies, and military health staff. The pandemic provided an opportunity to expand the scope of practice of many categories of health workers, such as nurses and pharmacists, to contribute to COVID‑19 testing and vaccination campaigns and other pandemic responses. These strategies to address staff shortages should be maintained and expanded to respond to growing demands for care – including the evolving implications of “long COVID”– and contribute to a more resilient workforce.
Frontline health workers are the heart of health systems and are thus pivotal to any effort to increase health system resilience (Box 10.1 provides a general description of the various stages of resilience to a shock). Even before the pandemic, many categories of health workers in OECD countries were in short supply and working at full capacity, causing systems to become overloaded quickly when the COVID‑19 pandemic hit. Many health workers are exhausted, several years after the pandemic began. They are contemplating whether they still have the energy and motivation to continue working in the health sector. Health systems will only be able to fully recover from the pandemic if they can support staff to recover from the burnout many have experienced, and if they can increase the capacity and flexibility of the workforce for the future.
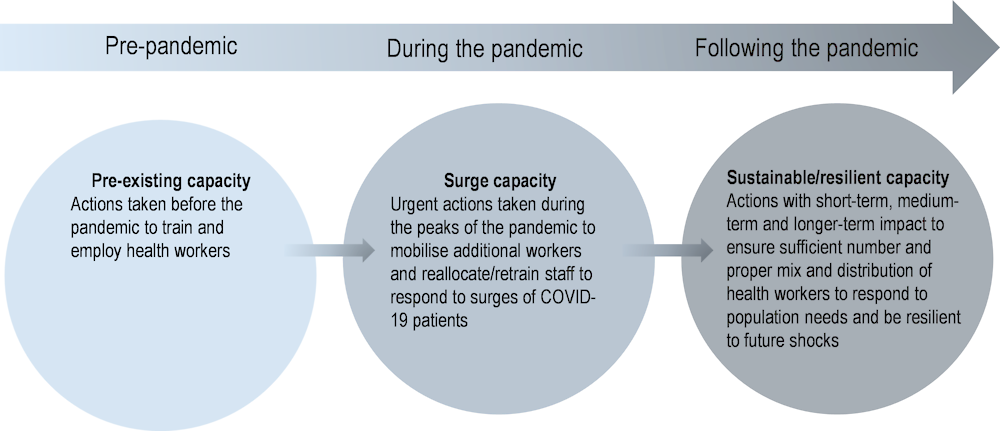
The response to a shock, such as a pandemic, comprises four stages (see the chapter on key findings and recommendations). These stages are prepare, absorb, recover and adapt. Prepare includes the steps taken to prepare critical functions to avoid and mitigate shocks. This occurs prior to the disruption. Absorb occurs after the shock commences, comprising of the capability of the health system to maintain core functions and absorb the consequences without collapse, thus limiting the extent of the disruption and minimising the morbidity and mortality impact. Recover involves regaining the disrupted functions as quickly and efficiently as possible. Adapt is the capacity of the health system to “learn” and improve its capacity to absorb and recover from shocks, reducing the impact of similar threats in the future.
Source: Chapter on key findings and recommendations.
Health workforce shortages may be exacerbated by a vicious cycle whereby shortages result in greater pressures and resignations, further exacerbating the underlying shortages. Health worker shortages can have real impacts on both access to care and the quality and safety of delivered care. In addition to the human costs, countries may end up paying significant financial penalties for shortages in the future. These include higher health care costs to manage conditions that have worsened due to poor access to and quality of care, and the significant (and avoidable) economic costs of safety lapses, which increase as workforces become overstretched.
As of 2022, available evidence of high levels of resignations among health workers was limited to a few countries only (e.g. the United Kingdom and the United States). However, many national surveys of nurses and other health workers show a reduction in motivation and an increase in intention to leave current jobs or the profession altogether. One of the key priorities is therefore to increase retention rates of existing staff by boosting recruitment and improving working conditions, while at the same time increasing the flexibility of health systems to respond both to strains arising from population ageing and to future shocks.
Many OECD countries have taken actions to improve the working conditions and remuneration of health workers to increase recruitment and retention rates – particularly for those categories of workers whose remuneration has been relatively low. In many countries, efforts to improve working conditions (for example through more flexible working hours and less requirement for overtime work or night shifts) and pay have focused on nurses and health care assistants working in public hospitals, as well as those working in nursing homes (see the chapter on long-term care).
Many OECD countries have also scaled up their efforts to train more doctors, nurses and other health workers. However, such decisions will only have an impact in the medium to long term, as it takes about 3‑5 years to train new nurses and about 8‑12 years to train new doctors. Increasing the number of students admitted in medicine, nursing and other health education programmes is key to avoid future shortages. Policy decisions on student intakes need to be based on robust and regular health workforce planning and forecasting, going beyond the traditional silo approach of looking at each profession in isolation.
This chapter follows a chronological assessment of some of the main health workforce issues that OECD countries faced going into the pandemic, experienced through the absorption and recovery stages, and confront as health systems adapt from the pandemic (Figure 10.1). It first reviews the pre‑existing health workforce capacity in OECD countries before the pandemic to provide important contextual information about each country’s starting point. Section 10.3 explores the health workforce issues that arose after the pandemic began and the strategies used to mobilise additional health workforce capacity to absorb and respond to peaks in demand (surge capacity). Section 10.4 reviews the strategies countries have started to implement to ensure sufficient health workforce capacity and flexibility to respond to growing health care needs arising from future shocks and population ageing. The chapter concludes with policy recommendations for smart investments in the health workforce to drive recovery and make health systems more resilient in the future.
This chapter focuses mainly on health workers in primary care and hospitals. The chapter on long-term care discusses issues related to long-term care workers in nursing homes and in patients’ homes.
The number of doctors and nurses per 1 000 population increased in nearly all countries in the two decades before the pandemic (OECD, 2021[1]), but in many countries the increase was insufficient to meet the growing demand for health care driven by population ageing. In addition, the composition of the medical workforce evolved towards a greater number of specialists and fewer GPs, resulting in growing shortages of primary care doctors – particularly in some rural and other underserved areas. This issue is often referred as “medical deserts” in France and other European countries (DREES, 2021[2])).
At the beginning of the pandemic, OECD countries had vastly different health workforce capacities. Several OECD countries in Central and South America (e.g. Chile, Colombia, Costa Rica and Mexico) and in Central and Eastern Europe (e.g. Latvia, Poland and the Slovak Republic), as well as Israel and Türkiye, had particularly low numbers of doctors and nurses (Figure 10.2). Low numbers of health professionals led to increased pressure on a smaller pool of staff to absorb and respond to growing demands during the different waves of the pandemic.
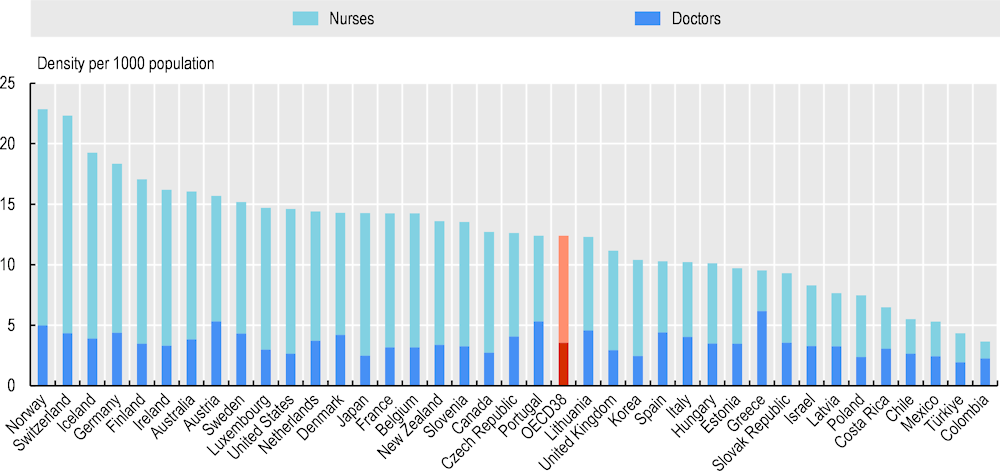
Note: In Greece and Portugal, the number of doctors refers to all doctors licensed to practise, resulting in a large overestimation of the number of practising doctors (of around 30% in Portugal). In Greece, the number of nurses is underestimated as it only includes those working in hospital.
Source: OECD Health Statistics 2022 (data refer to 2019).
A range of factors affected COVID‑19 infection rates and deaths during the first two years of the pandemic (see the chapter on COVID‑19 outcomes). The most important factor in mitigating the mortality impact was the capacity of countries to contain virus transmission effectively during the first year of the pandemic, and then to vaccinate the population at risk during the second year. Nonetheless, other associations can also be found between the number of health and social workers going into the pandemic and COVID‑19 mortality rate or all-cause excess mortality rate in 2020 and 2021 across OECD countries (see Box 10.2).
A wide range of factors can explain why some countries performed better than others in managing the impact of the pandemic and avoiding deaths. As discussed in the chapter on containment and mitigation, many studies have shown the importance of rapid and strong government interventions to contain the spread of the virus to reduce deaths from COVID‑19 (Dergiades et al., 2022[3]).
Basic descriptive data suggest an association between the number of people working in the health and social sector per 1 000 population just before the pandemic and COVID‑19 death rates across OECD countries, not controlling for other factors. Countries that had higher rates of health and social sector workers in 2019 generally had lower mortality rates from COVID‑19 in 2020 and 2021 (Figure 10.3). This was also the case for cumulative excess mortality.
However, these cross-tabulations also show wide variations in COVID‑19 mortality and excess mortality among countries that had the same number of health and social sector workers in 2019. For example, Spain and Italy had about the same number of workers in 2019 as Hungary and the Czech Republic, but lower death rates from COVID‑19 in 2020 and 2021. Similarly, Australia, Iceland and Japan had about the same number of workers as the United States in 2019, but much lower excess mortality in 2020 and 2021. This indicates that other factors played an important role in COVID‑19 deaths, including the strictness of public health interventions to contain the spread of the virus and vaccination coverage in 2021 (Meslé et al., 2021[4]).
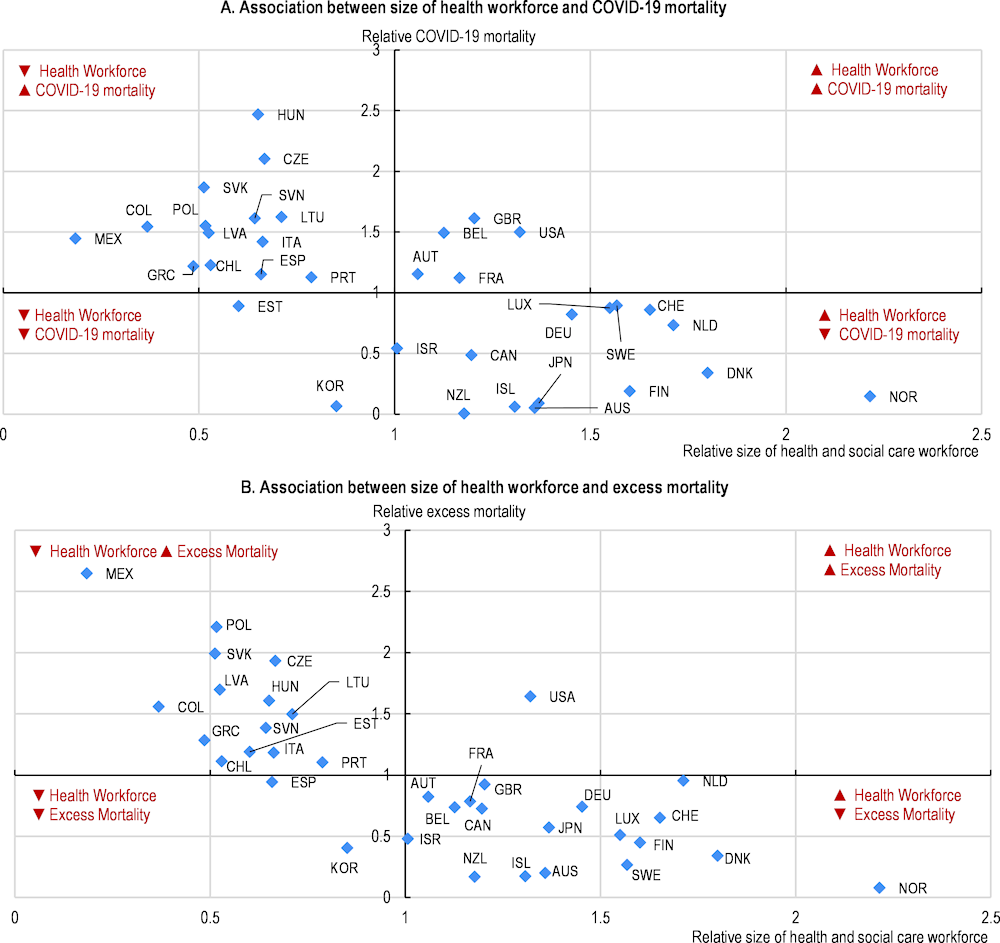
Note: The quadrant chart shows the association between the health workforce and COVID‑19 mortality (Panel A), and excess mortality (Panel B). The x-axis shows how much a country is above or below the OECD average for total health and social employment in 2019 (per 1 000 population); the y-axis shows how much a country is above or below the OECD average on COVID‑19 mortality in Panel A and excess mortality in Panel B in 2020 and 2021 (OECD average normalised to 1). This analysis does not adjust for other factors affecting COVID‑19 mortality or excess mortality; nor does it necessarily infer causality.
Source: OECD Health Statistics 2022, https://doi.org/10.1787/health-data-en.
The first wave of the pandemic triggered an abrupt new demand for care for COVID‑19 patients in hospital emergency departments and intensive care units (ICUs) (see chapter on critical care surge for further discussion), as well as new needs for human resources to deliver testing, tracing and isolation services (see chapter on containment and mitigation). From the end of 2020 through much of 2021, there was also a need to mobilise the health workforce to implement new population-wide vaccination campaigns.
About half of the countries responding to the OECD Resilience of Health Systems Questionnaire 2022 reported that health workforce shortages had an important impact on their capacity to deal with the pandemic (Figure 10.4). Canada, Japan, Latvia, the United Kingdom and the United States considered that health workforce shortages had a high impact. Conversely, Finland, Germany, Luxembourg and Switzerland considered that health workforce shortages had only a low-medium impact. In the case of Finland, this was associated with better containment of the pandemic than in most other OECD countries in 2020 and 2021, resulting in far fewer cases. Switzerland and Germany were among the countries with the highest numbers of doctors and nurses per 1 000 population going into the pandemic, meaning that they had a greater pool of health workers to absorb its consequences.
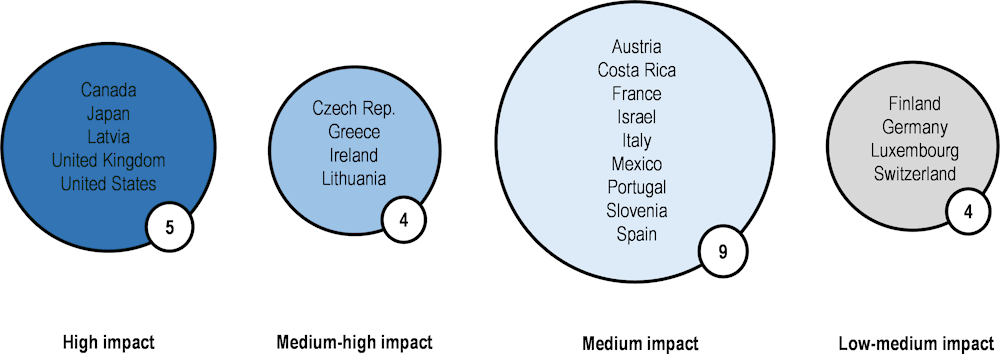
Note: This figure shows country responses to the question: “On a scale of 1 to 5, please indicate the impact of health workforce shortages in dealing with the pandemic: 1 (low), 2 (low-medium), 3 (medium), 4 (medium-high) or 5 (high)”.
Source: OECD Resilience of Health Systems Questionnaire, 2022 (based on 22 country responses).
In Austria, Canada, Italy, Latvia, Portugal, Spain, the United Kingdom and the United States, health workforce shortages were a widespread issue covering a range of health worker categories, including hospital doctors and GPs, nurses in hospitals and nursing homes, and health care assistants (Figure 10.5). In most countries, the shortages of nurses and doctors were particularly acute in ICUs. The vast majority of countries reported that the low supply of nurses in hospitals – those working in both ICUs and other wards – had been an issue in dealing with the pandemic. Two-thirds of countries reported that the lack of health care assistants in nursing homes had also been an issue (see the chapter on long-term care).
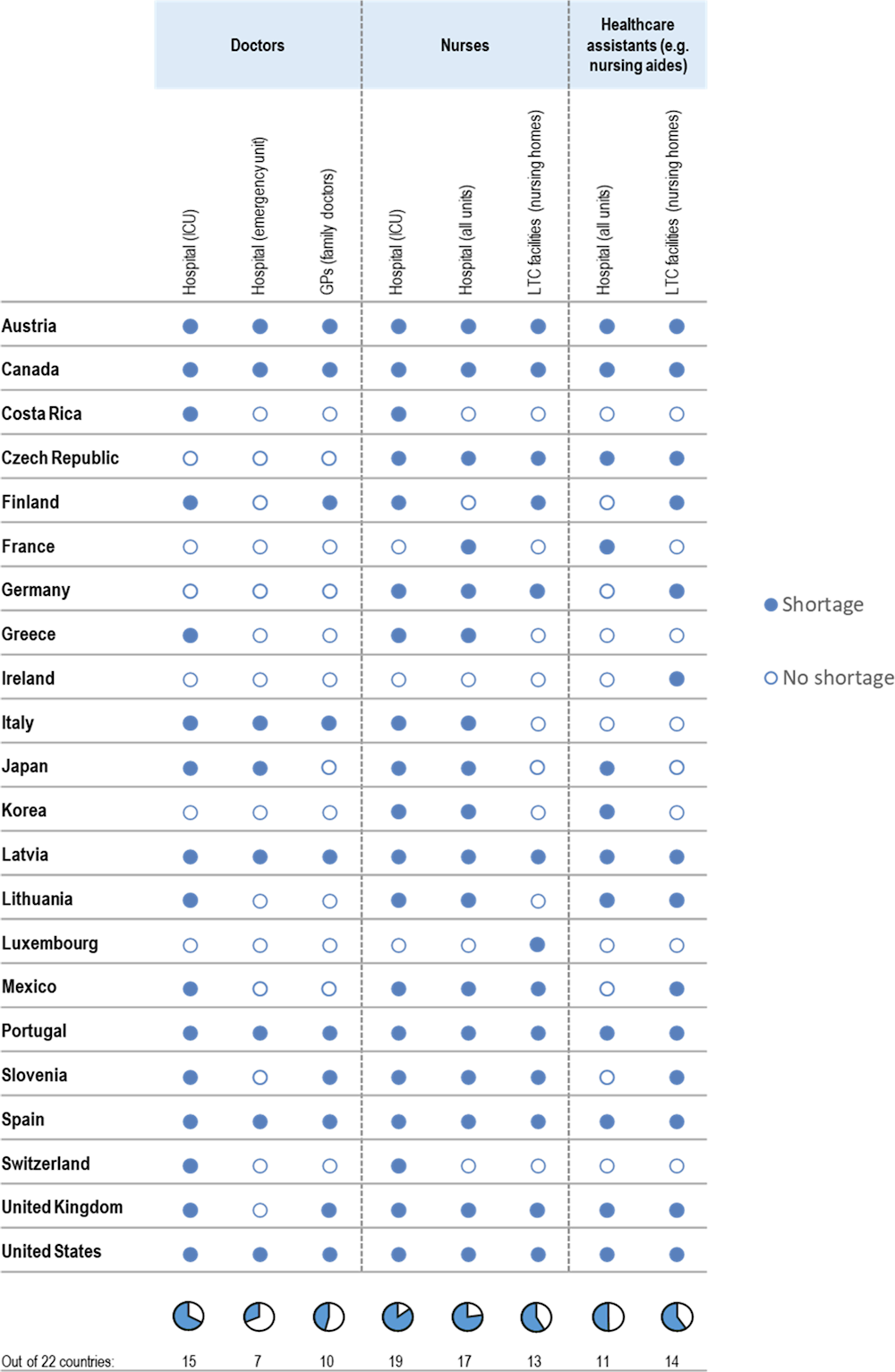
Note: This figure shows country responses to the question: “Which categories of health and long-term care workers were particularly in short supply during the COVID‑19 pandemic?”
Source: OECD Resilience of Health Systems Questionnaire, 2022 (based on 22 country responses).
Health workers were over-represented in terms of COVID‑19 infections at the beginning of the pandemic. The shortage of personal protective equipment (PPE), including basic equipment like face masks, was a key issue in many countries during the first few months of the pandemic, resulting in many health workers becoming infected. In the first few months of the pandemic, over 30 000 health workers were infected by the virus in France, the same number were infected in Italy, over 50 000 in Spain and about 200 000 in the United States (Santé Publique France, 2022[5]; CDC, 2022[6]; Instituto Superiore di Sanità, 2022[7]; Ministerio de Sanidad, 2020[8]).1 After a few months of acute shortages, countries were able to purchase and stockpile a sufficient quantity of PPE and prioritise distribution to health workers (see chapters on critical care surge and securing supply chains).
The scale, severity and duration of the outbreak became a more lasting issue, taking its toll on the mental health of many health workers. While health workers are generally trained to deal with health emergencies, the pandemic brought unprecedented and acute challenges. A large proportion of nurses and other health workers reported having been affected by mental health issues since the pandemic began, with symptoms of anxiety, depression, burnout and post-traumatic stress disorder (see subsection 10.3.6 for the potential implications of this issue). Some factors seem to have had a particular influence on the mental health of health workers, including working for long hours in a hospital ward and caring for COVID‑19 patients (Muller et al., 2020[9]). Family factors, such as having dependent children or infected family members, may also have had a negative impact on health workers’ mental health (Awano et al., 2020[10]; Aiyer et al., 2020[11]).
Many OECD countries introduced new services for health care staff (Table 10.1). At least two‑thirds of countries reported providing mental health support to health workers through access to mobile applications or websites, dedicated phone lines (hotlines) or consultations with specialists (psychologists or other mental health providers). However, past experience of virus outbreaks – such as severe acute respiratory syndrome (SARS) – showed that mental health problems such as anxiety and depressive symptoms can be detected among health workers more than a year following the event (Kisely et al., 2020[12]). This indicates that long-term support should be provided to all health workers who may need it.
|
Country |
Access to apps or web-based support sites |
Access to free phone line |
Access to consultation with a specialist |
|
Austria |
✓ |
||
|
Belgium |
✓ |
✓ |
✓ |
|
Canada |
✓ |
✓ |
✓ |
|
Costa Rica |
✓ |
✓ |
✓ |
|
Czech Republic |
✓ |
✓ |
✓ |
|
Finland |
✓ |
✓ |
|
|
France |
✓ |
✓ |
✓ |
|
Greece |
✓ |
✓ |
|
|
Israel |
✓ |
✓ |
✓ |
|
Italy |
✓ |
|
✓ |
|
Japan |
✓ |
✓ |
|
|
Korea |
✓ |
✓ |
✓ |
|
Lithuania |
✓ |
✓ |
✓ |
|
Luxembourg |
✓ |
|
✓ |
|
Mexico |
✓ |
✓ |
|
|
Portugal |
✓ |
✓ |
|
|
Slovenia |
✓ |
||
|
Spain |
✓ |
✓ |
|
|
Türkiye |
✓ |
✓ |
✓ |
|
United Kingdom |
✓ |
✓ |
✓ |
|
United States |
✓ |
✓ |
|
|
Total (out of 21 countries) |
17 |
16 |
17 |
Source: OECD Resilience of Health Systems Questionnaire, 2022 (based on 21 country responses).
Regardless of how many health workers they had when the pandemic started, virtually all OECD countries took measures to mobilise additional workforce resources in response to COVID‑19. Three broad types of strategies were used to scale up the health workforce capacity and flexibility to meet the surge of COVID‑19 patients in hospitals and to contain and manage the pandemic (Table 10.2).
Working harder: the first strategy was to increase the working time of existing staff by asking them to work overtime, asking part-time workers to work full time, cancelling or postponing leave, and providing staff with day care or school for their children during periods of lockdowns and school closures. However, this strategy has limitations. Prolonged periods of overtime can lead to burnout and a vicious cycle of relying increasingly on a shrinking pool of health workers.
Reallocating staff and retraining staff to work in hospitals and units with the greatest needs: the second strategy was to reallocate and reskill health workers to meet critical needs in ICUs in hospitals that were overburdened with COVID‑19 patients in certain parts of the country. This involved cancelling elective surgical procedures and other non-urgent care in hospitals, and bringing private sector workers into public hospitals or using ICU staff in private hospitals.
Mobilising additional staff: the third strategy was to mobilise additional workers – notably to support testing, tracing and isolating activities and vaccination campaigns – and to provide information and advice to the general population. The scope of practice of pharmacists, nurses and other health workers was expanded to respond to the huge demands for these services (see the chapter on care continuity). Most countries also mobilised medical and nursing students nearing the end of their studies; inactive health workers, including retired doctors and nurses; and others who had moved away from providing direct care. Some countries such as France used pre‑existing reserves of health workers, and some complementary mechanisms were also rapidly deployed to match the urgent demands from hospitals with people with the required skills and experience in different regions (Box 10.3). Many other countries also set up reserve lists quickly at the beginning of the pandemic.
|
Country |
Working harder |
Reallocating and retraining |
Mobilising additional workers |
||||||
|
Prolonging working hours |
Increasing workload |
Reallocating health workers to localities/ facilities with greater needs |
Reallocating health staff to key clinical areas and reducing non-COVID‑19 activities |
Providing rapid training in key clinical areas |
Reorganising clinical teams to spread expertise |
Mobilising medical and nursing students |
Calling in retired doctors and nurses |
Relying on national reserves of health professionals |
|
|
Austria |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|||
|
Belgium |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
Canada |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
Costa Rica |
✓ |
✓ |
✓ |
✓ |
✓ |
||||
|
Czech Republic |
✓ |
✓ |
✓ |
✓ |
✓ |
||||
|
Finland |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
France |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
Germany |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
||
|
Greece |
✓ |
✓ |
✓ |
✓ |
✓ |
||||
|
Israel |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|||
|
Italy |
✓ |
✓ |
✓ |
✓ |
|||||
|
Japan |
✓ |
✓ |
✓ |
✓ |
|||||
|
Korea |
✓ |
✓ |
✓ |
||||||
|
Latvia |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
Lithuania |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
Luxembourg |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
Mexico |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|||
|
Portugal |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
Slovenia |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
Spain |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
|
Switzerland¹ |
✓ |
✓ |
✓ |
✓ |
✓ |
||||
|
United Kingdom |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
United States² |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
✓ |
|
Total (out of 23 countries) |
18 |
18 |
16 |
21 |
18 |
13 |
19 |
19 |
15 |
Note: 1. In Switzerland, the policies ticked are those known to the Federal Office. The list is non-exhaustive, as the Swiss health system is decentralised and the cantons are responsible for health care provision. 2. Due to the decentralised structure of the US health system, policy responses regarding the workforce varied among the 50 states. There was no single, uniform policy response.
Source: OECD Resilience of Health Systems Questionnaire, 2022 (based on 23 country responses).
More than a decade before the COVID‑19 pandemic, France established a health reserve in response to the avian influenza pandemic in 2007. Its mandate was to support health workers in the event of exceptional public health emergencies. When the COVID‑19 pandemic started, the reserve was mobilised, but only a small proportion of the inactive doctors, nurses and other volunteers registered on the reserve list were called on to provide support during the first wave of the pandemic in 2020 (about 1 500 doctors and other health workers out of the 42 000 registered between March and July 2020).
This reserve, managed at the national level, proved to be less fit to respond to the massive urgent needs of the pandemic than other more decentralised and often informal mechanisms that were designed specifically to respond to the COVID‑19 crisis (Pittet et al., 2021[13]). Other mechanisms were quickly put in place by hospitals and long-term care facilities, together with regional health agencies to match their needs with the offer of services from volunteers. For example, in the Ile‑de‑France region (the national capital region), the platform “#Renforts COVID‑19” (#Backup COVID‑19) dispatched over 16 000 people to hospitals and long-term care facilities during the first few months of the pandemic. At the national level, more than 60 000 volunteers were mobilised between March and July 2020, bringing support to 6 000 hospitals and long-term care facilities.
As OECD countries emerge from the pandemic but health systems continue to face multiple pressures, a key priority is to increase the supply of doctors, nurses and health workers by increasing training capacity, recruitment and retention rates. Around 80% of OECD countries reported in November 2021 that workforce shortages in health and long-term care had become more severe since the COVID‑19 pandemic (OECD, 2022[14]). However, recruitment may be difficult in the short term if there is no spare capacity as it takes time to train new doctors, nurses and other skilled health workers. Several countries have actively recruited foreign doctors and nurses to fill needs in the short term (Box 10.4), but this may exacerbate shortages in origin countries.
While it takes many years to train new doctors and nurses, recruiting them from abroad can provide a quicker solution to address immediate shortages. It is also less expensive, as the costs of education and training are borne by other countries. Several OECD countries, including Australia, Canada, Ireland, Israel, New Zealand, Switzerland, the United Kingdom and the United States, have traditionally relied on international recruitment of doctors and nurses. In some countries, this reliance has increased since the pandemic began.
The United Kingdom is one example. In 2021/22, international recruitment of nurses reached an all-time high, and international recruitment of doctors reached a nearly 20‑year high. Over 12 000 new doctors and over 23 000 new nurses were foreign-trained in 2021/22. The countries of origin of foreign-trained nurses in the United Kingdom have changed greatly over the past decade (Figure 10.6). Between 2010 and 2016, growth in recruitment of nurses trained in European Union or European Economic Area (EU/EEA) countries was rapid. However, since the Brexit vote in 2016 and the introduction of new English language test requirements for nurses, international nurse recruitment has fallen from EU/EEA countries but grown substantially from others. In recent years, recruitment has increased rapidly from the Philippines and India, but also from Nigeria, Ghana and Zimbabwe.
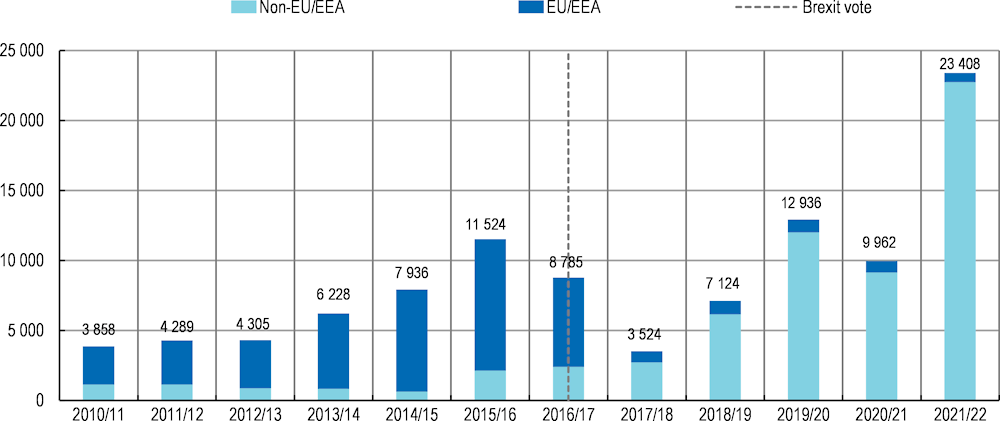
Note: The numbers refer to new nurse and midwifery registrants.
Source: Shembavnekar and Buchan (2022[15]), “How reliant is the NHS in England on international nurse recruitment?”, https://www.health.org.uk/news-and-comment/charts-and-infographics/how-reliant-is-the-nhs-in-england-on-international-nurse-recruitment, based on data from the UK Nursing and Midwifery Council.
International recruitment of foreign-trained nurses also reached an all-time high in Canada in 2020. This number is expected to continue to rise in 2021 and 2022 as the federal and provincial governments are encouraging more foreign nurses to come to the country to work. In early 2022, the Government of Ontario (the largest province) announced a plan to hire more than 1 000 foreign-trained nurses quickly (Government of Ontario, 2022[16]). Similarly, the Government of Quebec (the second largest province) is investing CAD 65 million to recruit and train nearly 1 000 nurses from francophone countries (Government of Quebec, 2021[17]). Most foreign-trained nurses in Canada come from the Philippines and India, although a growing number of francophone nurses are also recruited from France.
OECD countries are using a range of policies to increase the supply of doctors and nurses and promote a better skill mix in the future. Most countries (80%) who responded to the OECD Resilience of Health Systems Questionnaire 2022 recently increased student intakes in medical education and training programmes, and a similar proportion of countries provide some incentives to encourage more new doctors to choose general practice to address shortages of GPs. Most countries (60%) have or are planning to introduce or expand the roles of other health professionals like nurses to reduce the workload and pressures on doctors. Many countries also indicated that they have introduced or are planning to introduce new financial incentives to improve the geographic distribution of doctors (Figure 10.7).
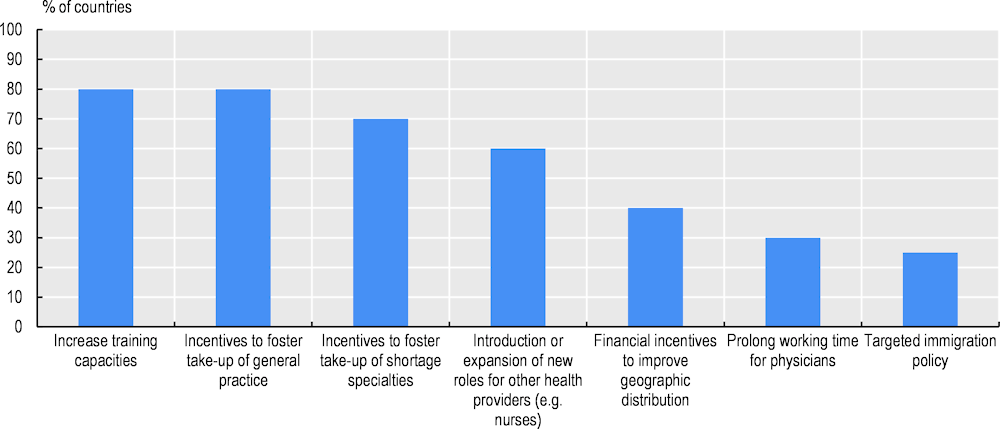
Source: OECD Resilience of Health Systems Questionnaire, 2022 (based on 20 country responses).
Figure 10.8 shows that over 80% of countries have increased or are planning to increase training capacities in nursing education programmes. More than two‑thirds are planning to introduce or expand the scope of practice to more advanced roles to provide greater career progression. The majority are planning to improve the working conditions of nurses and their pay rates to increase recruitment and retention.
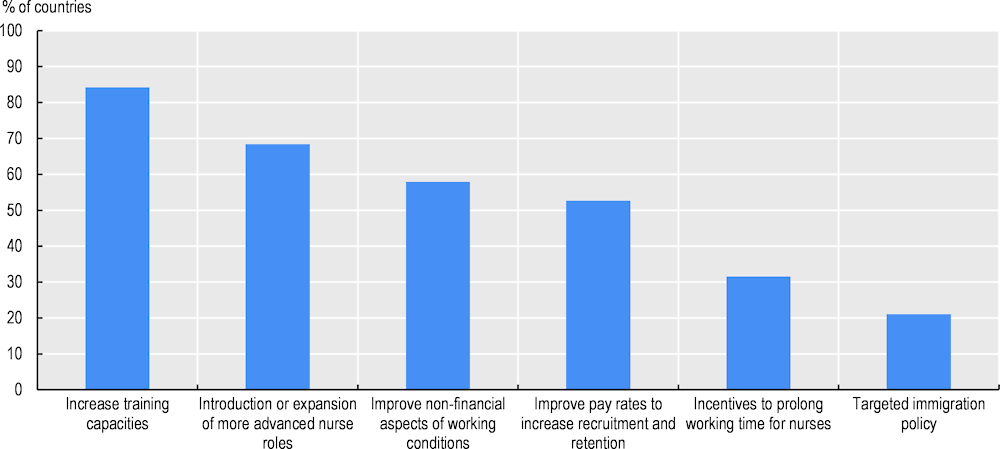
Source: OECD Resilience of Health Systems Questionnaire, 2022 (based on 19 country responses).
Many OECD countries have recently increased the number of students in medical and nursing education programmes to boost the supply of doctors and nurses, although there is a time lag between such decisions to increase student intakes and when students complete their training (about 8‑12 years for doctors and 3‑5 years for nurses).
In many countries, decisions to increase domestic training capacity preceded the COVID‑19 pandemic. For example, in the United Kingdom, the number of students admitted to medical education programmes started to increase markedly in 2018 to increase the supply of doctors and provide more opportunities for students with the talent and ambition to train as doctors (UK Department of Health, 2017[18]). Between 2017 and 2021, the number of new medical students admitted increased by 35%, from 7 765 in 2017 to more than 10 500 in 2021 (Figure 10.9).
Similarly, France has seen a rapid expansion in the number of new medical students since 2017 to address projected shortages of doctors. Furthermore, in 2021, the French Government adopted a five‑year plan for medical student admissions that provides for a further increase of 20% over the period 2021‑25 compared with 2016‑20 (Ministère des Solidarités et de la Santé, 2021[19]). The new “numerus apartus” also includes an element of flexibility compared with the previous “numerus clausus” policy, as it provides a recommended range for student admissions rather than a fixed number. On average between 2021 and 2025, over 10 000 medical students are expected to be admitted each year, reaching a new all-time high.
The number of students admitted to medical schools in many other countries (e.g. Germany and the United States) also continued to increase before and since the pandemic, although at a less rapid rate.
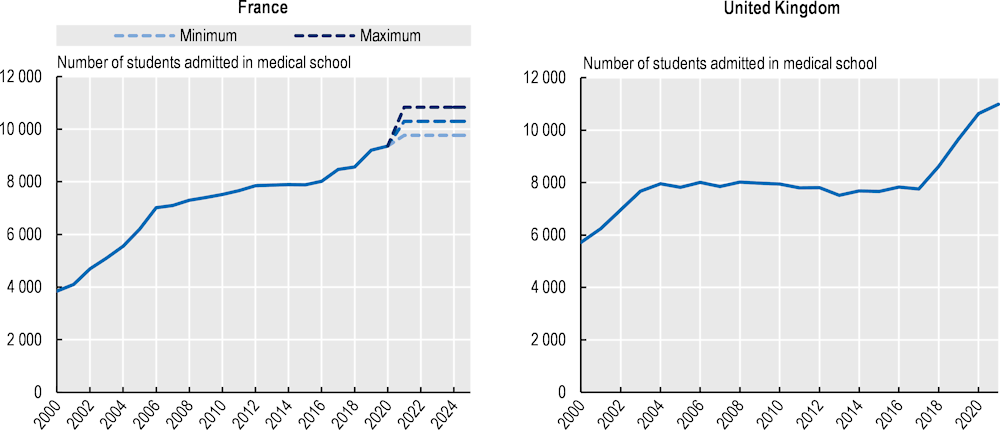
Sources: France: DREES (2021), https://drees.solidarites-sante.gouv.fr/publications/les-dossiers-de-la-drees/quelle-demographie-recente-et-venir-pour-les-professions; United Kingdom: Universities and Colleges Admissions Service (UCAS) (2021), https://www.ucas.com/data-and-analysis/undergraduate-statistics-and-reports/ucas-undergraduate-sector-level-end-cycle-data-resources-2021.
Many countries have also increased the number of students in nursing programmes to increase future supply and avoid shortages. The most recent evidence from several countries shows that young people’s interest in pursuing a career in nursing has increased following the pandemic as illustrated by the growing number of applications and admissions (Figure 10.10), despite concerns that fewer might be interested given the work pressure and relatively low pay.
In Italy, the number of applicants to nursing programmes increased by 7% between 2019 and 2020, and by another 14% in 2021 (total increase of 22% over this two‑year period). The number of students admitted also increased albeit at a slightly lower rate (15% over two years) (Mastrillo, 2021[20]).
In Spain, the number of applications to nursing programmes increased by over 50% between 2019 and 2021, although the number of students admitted only increased marginally (by 6%). This indicates persistent educational capacity constraints (Ministry of Education and Professional Training, 2022[21]).
In the United Kingdom, the number of applications to nursing education programmes increased steadily in 2020 and 2021, with an overall increase of over 33% during this two‑year period. The number of applicants increased across all ages, but the rise was particularly strong among 18‑year‑olds (39%). The pandemic was a significant factor behind this increase: 69% of applicants said that the pandemic inspired them to apply to study to become a nurse. In addition, the introduction in September 2020 of the NHS Learning Support Fund Programme that provides financial support to students in nursing and other health-related programmes; the promotion of nursing careers through the “We are the NHS” Campaign; and increased investment in practice placements contributed to the application increase (UCAS and HEE, 2021[22]). The sharp increase in applications in 2020 was accompanied by an even greater increase in student admissions (up by 24% compared with 2019), but the number of admissions stabilised in 2021 (with only a modest increase of 0.5% compared with 2020).
In the United States, the number of student applications in nursing increased by 14% between 2019 and 2021, signalling strong interest in nursing careers. The number of students admitted increased slightly less, by about 8% (AACN, 2022[23]).
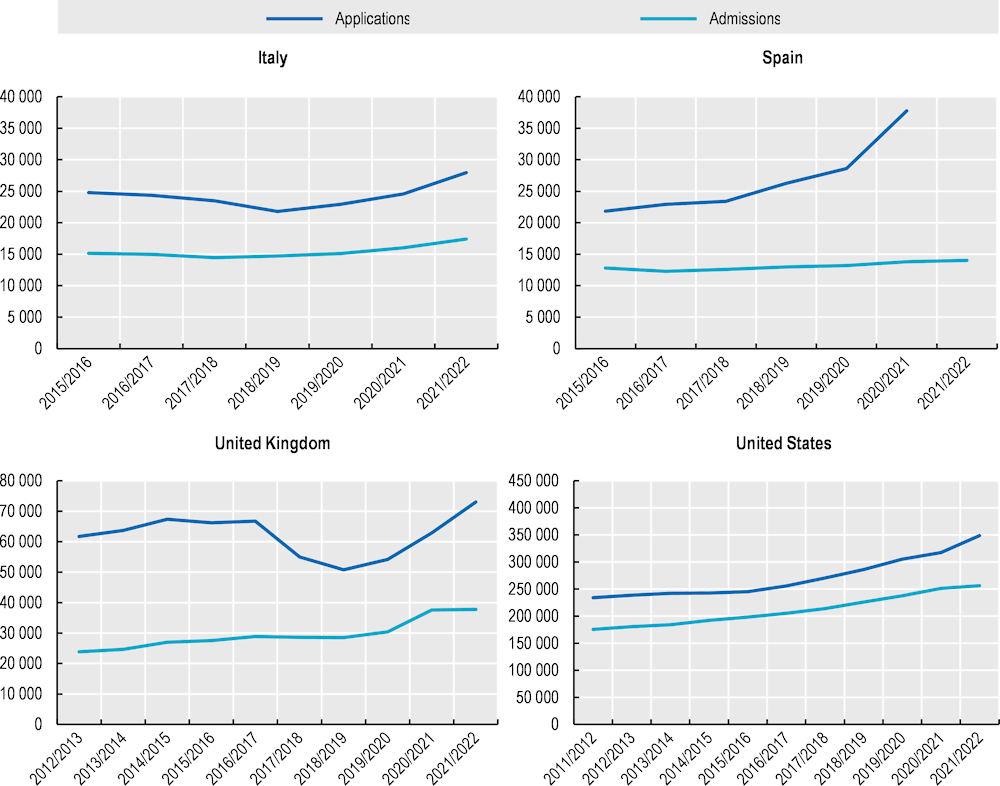
Note: For the United Kingdom, the data relate to applicants who have applied to at least one nursing course (not necessarily their first choice). For the United States, the data relate to entry-level nursing baccalaureate programmes (not graduate programmes).
Source: Italy: Mastrillo (2021), https://www.fioto.it/altreimg/Report%20Mastrillo%202021.pdf; Spain: Ministry of Education and Professional Training (2022), http://estadisticas.mecd.gob.es/EducaJaxiPx/Datos.htm?path=/Universitaria/Alumnado/EEU_2021/GradoCiclo/NuevoIngreso//l0/&file=NI_Grad_Sex_Edad(1)_Amb_Tot.px&type=pcaxis; United Kingdom: UCAS (2022), https://www.ucas.com/data-and-analysis/undergraduate-statistics-and-reports/ucas-undergraduate-sector-level-end-cycle-data-resources-2021; United States: AACN (2022), https://www.aacnnursing.org/News-Information/Press-Releases/View/ArticleId/25183/Nursing-Schools-See-Enrollment-Increases-in-Entry-Level-Programs.
One persistent challenge across most OECD countries is the need to attract more male students to nursing. The general perception remains that nursing is “women’s work”, and that the occupation has a low professional status and autonomy, along with limited career progression opportunities (Mann and Denis, 2020[24]). In most countries, at least 80% of students applying and admitted to nursing programmes continue to be female, reflecting the traditional gender composition of the nursing workforce. In the United Kingdom, nearly all the increase in student applications and admissions in the past few years has come from female students (Figure 10.11). This has also been the case in many other countries.
While increasing training capacity is crucial to increasing supply in the medium to long term, another key priority is to increase retention rates of doctors, nurses and other health workers to avoid exacerbating shortages. The combination of pre‑existing shortages of health workers before the pandemic and more than two years of COVID‑19 has led to many health workers feeling demotivated. Some are reporting an intention to leave their job to find work in other sectors and occupations or to retire early. This has been particularly the case for nurses and health care assistants, who often feel undervalued and underpaid for the work they do, and perceive that there is an imbalance between effort and reward.
Table 10.3 shows selected results from surveys of nurses and other health workers carried out in some OECD countries in 2020 and 2021, highlighting the perceived degradation of working conditions during the pandemic and intentions to leave jobs.
In Belgium, a survey from March 2021 found that close to a third of nurses, caregivers and other health workers reported feeling tired, and over half reported being under pressure or stress. Nearly 40% of respondents reported mental health issues and 19% were intending to leave the profession (Sciensano, 2021[25]).
In Canada, a survey from late 2021 found that 94% of nurses were experiencing symptoms of burnout and 45% screened positive for severe burnout. Half (50%) of the nurses who responded to this survey reported that they were considering leaving their job over the coming year and 20% were considering leaving the profession altogether (CFNU, 2022[26]).
In France, about three‑quarters of nurses reported in April-May 2021 that they did not feel better recognised than before the pandemic, and 40% said that the pandemic had made them consider changing their profession (an increase of 3% compared with a previous survey in October 2020) (Ordre National des Infirmiers, 2021[27]). A more recent survey from December 2021 found that over 80% of nurses thought that their working conditions had worsened since the pandemic began, and 15% of all nurses said they wish to change professions over the coming year (Ordre National des Infirmiers, 2022[28]).
In the United Kingdom, 57% of nurses reported in October 2021 that they were considering or planning to leave their job in the coming year, up from 36% a year earlier. The main reasons for thinking about leaving were feeling undervalued, feeling under too much pressure, feeling exhausted, insufficient staffing levels and insufficient pay (Royal College of Nursing, 2021[29]).
In the United States, 11% of nurses and nurse managers reported in 2021 that they intended to leave their job, and another 20% were undecided about keeping their job. The proportion of nurses and nurse managers intending to leave their job was particularly high among the most experienced (those with over 25 years of experience) (Raso, Fitzpatrick and Masick, 2021[30]).
|
Country |
Survey coverage and timing |
Key findings |
|---|---|---|
|
Belgium |
Survey of 2 530 health workers and caregivers (including 698 nurses and health care assistants), March 2021 |
|
|
Canada |
Survey of 3 676 nurses, June‑July 2020 |
|
|
Survey of 4 467 nurses, Nov-Dec 2021 |
|
|
|
France |
Survey of 30 000 nurses, April-May 2021 |
|
|
Survey of 60 000 nurses, December 2021 |
|
|
|
United Kingdom |
Survey of 9 577 members of the Royal College of Nursing, October 2021 |
|
|
United States |
Survey of 20 665 health care workers (incl. 2 301 nurses) at 124 institutions, 2020 |
|
|
Survey of 400 frontline nurses, 2021 |
|
|
|
Survey of 5 000 nurses and nurse managers, 2021 |
|
Sources: Belgium: Sciensano (2021), https://www.sciensano.be/en/biblio/power-care-lenquete-sur-le-bien-etre-des-personnes-et-professionnels-daide-et-de-soin-principaux, Canada: Havaei et al. (2021), https://pubmed.ncbi.nlm.nih.gov/33467080/; CFNU (2022), https://nursesunions.ca/wp-content/uploads/2022/02/Viewpoints_Survey_Results_2022_January_EN_FINAL-1.pdf, France: Ordre National des Infirmiers (2021), https://www.ordre-infirmiers.fr/actualites-presse/articles/les-infirmiers-sinterrogent-sur-leur-avenir-et-souhaitent-des-evolutions-profondes-de-leur-metier.html; Ordre National des Infirmiers (2022), https://www.ordre-infirmiers.fr/actualites-presse/articles/resultats-consultation-infirmiere-lordre-national-infirmiers-alerte-de-nouveau-sur-la-situation-de-la-profession.html, United Kingdom: Royal College of Nursing (2021), https://www.rcn.org.uk/professional-development/publications/employment-survey-2021-uk-pub-010-075, United States: Sinsky et al. (2021), https://pubmed.ncbi.nlm.nih.gov/34901752/; Gretchen et al. (2021), https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/nursing-in-2021-retaining-the-healthcare-workforce-when-we-need-it-most; Raso, Fitzpatrick and Masick (2021), https://pubmed.ncbi.nlm.nih.gov/34519700/.
Concerns about a possible “great resignation” of workers in the health sector (and in other sectors) emerged in the United States in early 2021, and a little later (2021 and 2022) in the United Kingdom. The term “great resignation” has been used to refer to the massive numbers of employee resignations from their jobs, because of long-lasting job dissatisfaction, wage stagnation (in a context of rising inflation) and safety concerns in the context of the COVID‑19 pandemic.
Since early 2021, the percentage of workers in the health and social sector in the United States who have resigned from their jobs increased to about 2.5% of all workers per month in the second half of 2021 and 2022, up from about 2.0% per month before the pandemic (Figure 10.12). American workers in the health and social sector and in other sectors who left their jobs in 2021 reported as the main reasons that they were dissatisfied with their pay, with opportunities for advancement and career progression, and with the flexibility of their working conditions.
However, the number of workers who were recruited in the health and social sector increased faster than the number who resigned, so the overall number of workers increased.2 The peak in hiring rates in the sector occurred after the first wave of the pandemic in summer 2020 (following a period of slowdown in hiring during the first wave and strong demand for health and social assistance workers), and remained higher in 2021 and 2022 than before the pandemic. The high resignation and hiring rates since early 2021 reflect a very dynamic job market, with many workers changing jobs to take advantage of better opportunities in a context of a tight labour market and very low unemployment rate. Despite all the job turnover, at the end of 2021, about 500 000 more people were working in the health and social assistance sector in the United States compared with 2020 (BLS, 2022[31]).
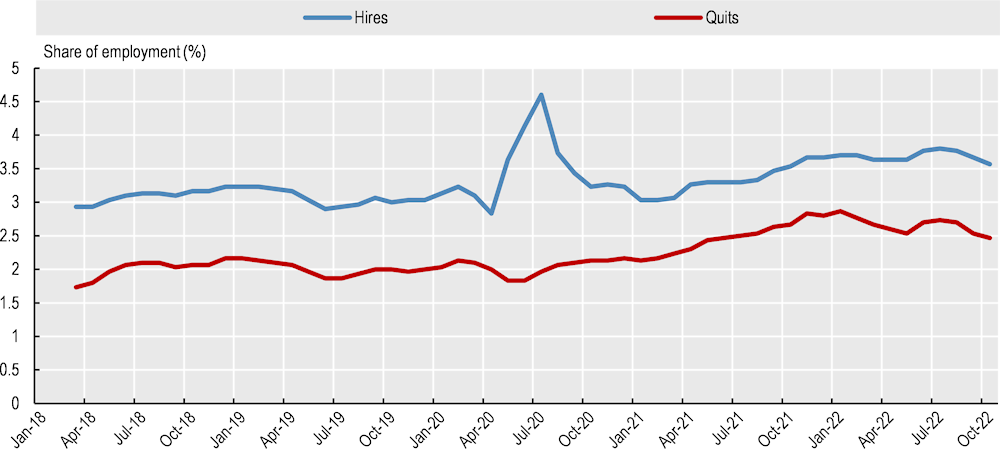
Note: Data are seasonally adjusted. They have been calculated as three‑month moving averages to reduce some of the monthly variation.
Source: Bureau of Labor Statistics, Job Openings and Labor Turnover Survey, https://www.bls.gov/jlt/data.htm.
In England (United Kingdom), the number of nurses who have left the NHS reached an all-time high in 2021/22, with over 40 000 leaving active service between June 2021 and June 2022. More than half of leavers were less than 40 years old and therefore still many years away from retirement age (King’s Fund, 2022[32]). At the same time, a record number of nurses joined NHS England in 2021/22 (Figure 10.13), driven largely by the international recruitment of nurses that also reached record levels in 2021/22.
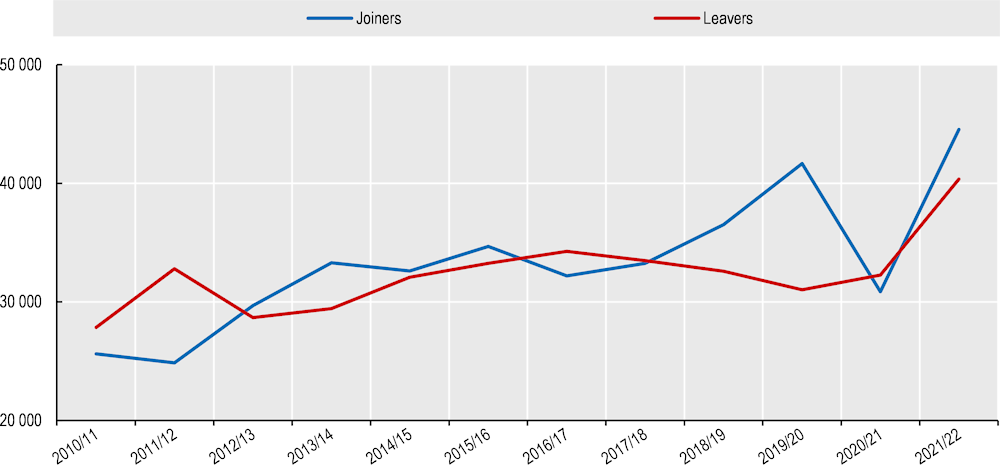
Note: The growth rate covers the period from June each year to June the following year. The data also include health visitors. Leavers include not only those permanently leaving the NHS but also those going on maternity leave or taking a temporary career break.
Source: Nuffield Trust based on NHS Digital data, https://www.nuffieldtrust.org.uk/resource/peak-leaving-a-spotlight-on-nurse-leaver-rates-in-the-uk.
Taking account of both entries into and exits from NHS England, staff numbers increased slightly during the pandemic. The number of hospital doctors was 5.6% higher in March 2022 than in March 2020, while the number of nurses was 1.6% higher. Focusing only on changes during 2021, the number of hospital doctors and nurses was 3.4% higher in December 2021 than a year earlier, but this growth may not have been sufficient to respond to greater demand (Figure 10.14).
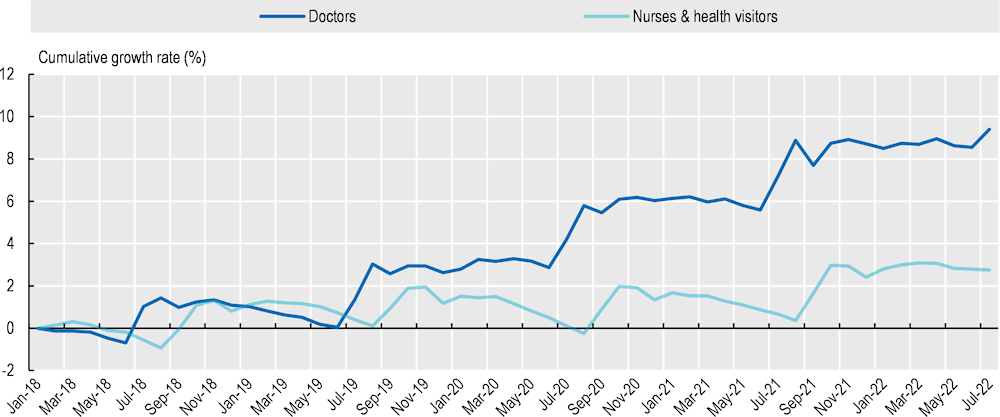
Source: NHS Digital, 2022 Hospital & Community Health Service monthly workforce statistics, https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics.
Many countries provided one‑off COVID‑19 rewards (or bonuses) to frontline workers following the first wave of the pandemic in 2020, in recognition of their elevated health risks, additional workload and commitment. Rewards were especially common for health workers (reported in about 75% of the OECD countries surveyed through the OECD Questionnaire on Policy Responses to the COVID‑19 Crisis in November 2021) and long-term care workers (about 50%). However, the value of the rewards and the coverage of health and long-term care workers varied across countries.
Permanently higher pay, rather than one‑time bonuses, is an even more powerful way to recognise the value of different categories of health and long-term care workers. Up to November 2021, there had been fewer government-led initiatives of this kind, although about 40% of the OECD countries surveyed reported such permanent pay increases for health workers and about 30% for long-term care workers (Figure 10.15). Countries like Belgium, Chile and Slovenia reported initiatives to promote pay increases for health and long-term care workers; Hungary, Latvia and Switzerland for health workers; and the Czech Republic for long-term care workers.
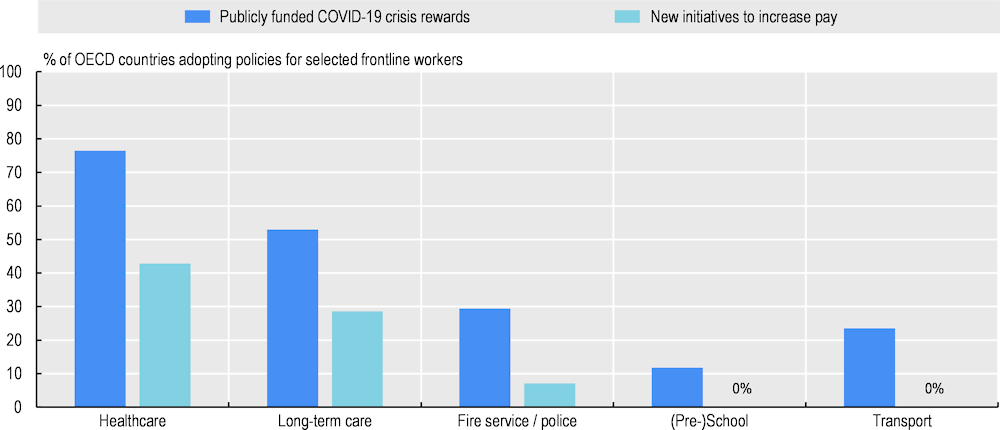
Note: For new initiatives to increase pay, data based on 14 country responses (AUT, BEL, CHE, CHL, CZE, FIN, HUN, ITA, JPN, LUX, LVA, NLD, SVN, SWE); for publicly funded crisis rewards, data based on 17 country responses (in addition: DNK, ISL, PRT). Several countries are not included, as these policy areas are the competence of subnational jurisdictions due to the country’s federal structure.
Source: OECD Questionnaire on Policy Responses to the COVID‑19 Crisis (November 2021).
In many countries, one‑off bonuses and pay increases focused on nurses and health care assistants in hospitals and nursing homes. In Germany, bonuses were provided in 2020 for nurses and other employees working in long-term care, and for nurses in hospitals with a minimum number of COVID‑19 patients (nearly one‑quarter of all hospitals qualified). An additional bonus was provided for nurses in about half of all hospitals in 2021. The national bonuses were in most cases between EUR 500 and EUR 1 500. Some federal states also provided additional bonuses of approximately EUR 500.
In France, payment for overtime work of nurses and other workers in hospitals and nursing homes was increased during the first wave of the pandemic in 2020. In addition, most hospital workers, including nurses and nursing aides, received a COVID‑19 bonus after the first wave, ranging from EUR 1 000 to EUR 1 500, depending on the intensity of the pandemic in each region. To improve recruitment and retention, all health workers in hospitals and nursing homes received a permanent pay rise of EUR 183 per month in 2020, followed by another of between EUR 45 and EUR 450 per month, depending on professional categories and years of experience (OECD/European Observatory on Health Systems and Policies, 2021[33]). However, these pay increases have not prevented a growing number of nurses in France preferring temporary jobs from interim companies rather than permanent jobs from hospitals, as they can often earn more as interim staff than regular staff. This is also the case in Belgium (Box 10.5).
The increased use of interim staff to address staff shortages in hospitals in countries like France and Belgium has had serious consequences. It has increased costs for hospitals and generated tensions in the workplace, as workers doing the same jobs are often paid more when employed by an interim company than if they are directly employed by the hospital. The growing use of interim staff has increased costs for hospitals because they must pay more for the same employees and must also pay additional fees to interim companies.
In France, hospitals increasingly relied on interim doctors and nurses to fill vacant posts in emergency departments and other hospital units in the first half of 2022. Interim doctors can earn 2‑3 times more than their counterparts who have a regular contract with the hospital, while interim nurses can earn about 30% more. Interim staff also have much more flexibility to choose their working hours than regular staff. Some hospitals have offered financial incentives (such as one‑off bonuses) to encourage interim nurses to accept longer-term contracts, but the take‑up of these more regular posts has been very limited and has not reduced sufficiently the advantages of working as interim staff.
In Belgium, hospitals and long-term care providers in the Flanders region also increasingly relied on interim staff to fill gaps in their nursing and care workforce in 2022. As interim agencies are not bound by the agreements in the health and long-term care sector, nurses and care workers employed as interim staff can bargain for better working conditions (e.g. higher wages, flexible working hours and extra advantages such as a company car). Thus, hospitals and nursing homes increasingly saw their staff leave to join these interim agencies, which find them positions back in hospitals and care institutions – in some instances, even in the same institutions from which they resigned.
In the United Kingdom, nurses in Scotland, Northern Ireland and Wales received a bonus payment in 2020/21 in recognition of their contributions during the pandemic, but those in England did not. NHS nurses and other staff in England received a 3% pay increase in 2021/22, but this was below the inflation rate, which meant a reduction in wages in real terms. In 2022/23, the British Government proposed another pay increase for NHS employees of 3%, but this is expected to be well below the inflation rate, meaning a further reduction in real wages (Shembavnekar and Buchan, 2022[15]).
In some countries, including Denmark, nurses have not been satisfied by the pay increases received since the pandemic. Members of the Danish Nurses Union went on strike for 10 weeks during summer 2021, demanding higher wages and increased staffing. An emergency law ended the strike at the end of August 2021, providing a 5% wage increase over three years, falling short of union members’ demands.
Rapid increases in the consumer price inflation rate in 2022 and 2023 can be expected to increase demand for higher pay increases from nurses and other health workers to avoid losses in purchasing power. If the pay increase in the health sector falls short of what workers in other sectors receive, this can be expected to incentivise health workers to consider changing jobs. However, the current situation of health worker shortages should be conducive to wage increases.
Health workforce shortages during the pandemic have sparked renewed interest among professional associations and other stakeholders in setting required minimum staffing ratios. Calls have been made to set such ratios, focusing either on specific hospital units (such as ICUs and maternity wards) or more broadly at a health system-wide level.
For example, the Belgian Health Care Knowledge Centre (KCE) has recommended that Belgian authorities (and possibly also European-level authorities) define minimum safe patient-to-nurse ratios, adapted to the patient acuity levels in specific hospital units (such as ICUs), based on international standards. The KCE recognises, however, that it is not yet possible to formulate precise recommendations because of differences in the definition of ICUs across countries, and differences in patient case mixes (Van den Heede Koen et al., 2022[34]).
At a broader system-wide level, the Standing Committee of European Doctors suggested in November 2021 that the European Commission might issue benchmarks for minimum ratios of health professionals per patient. These would support countries in meeting safe staffing levels – both for baseline universal health coverage and for health emergencies (CPME, 2021[35]).
Experiences of minimum staffing levels date back at least 20 years. In 2001, the state of Victoria in Australia adopted a law making it mandatory for large public hospitals to have minimum nurse‑to-patient ratios. These were set at five nurses to 20 patients in acute medical and surgical wards. In 2004, California became the first state in the United States to implement similar nurse‑to-patient ratios, depending on the hospital unit (for example, the ratio in paediatric and emergency departments was set at one nurse to four patients, while the minimum in a psychiatric ward was set at one nurse to six patients). More recently, Germany imposed minimum staffing requirements in hospitals in 2019 to increase the number of practising nurses. A maximum number of patients per nurse was defined for hospital units where nursing staff are especially needed, such as in intensive care, geriatric care and cardiac care. A distinction was also made between day and night shifts. For example, in cardiac surgery units, the ratio was set at a maximum of seven patients per nurse on a day shift and a maximum of 15 patients per nurse on a night shift.
The advantages and disadvantages of setting such minimum staffing requirements have been debated since they were first implemented (Buchan, 2005[36]). The main advantages are that this is an effective instrument to increase staffing levels, reduce the workload of existing staff, and improve quality of care and patient safety. As such, minimum staffing requirements increase job satisfaction for nurses and can also increase retention rates. The main disadvantages are that minimum staffing ratios are inflexible, are inefficient if not set at a proper level and raise staffing costs. In Germany, the newly set minimum staffing requirements were lifted temporarily in 2020 to provide greater flexibility to allocate more nurses for COVID‑19‑related activities.
One practical challenge to implementing minimum staffing ratios is to define precisely what constitutes a “safe” and “minimum” staffing level required in different parts of hospitals or outside hospitals. Different categories of health workers (doctors, pharmacists, nurses and health care assistants) can play various roles in delivering the same health services, and the possibilities of substitutions and complementarities are numerous. As the pandemic experience showed, the implementation of minimum staffing requirements may also need to be adapted under special circumstances, such as public health emergencies, to provide sufficient flexibility to respond to abrupt surges in demand for certain types of care.
The pandemic provided opportunities to expand the roles of some health care providers like pharmacists and nurses to respond to the surge in demand for COVID‑19‑related care and to maintain continuity of care for the rest of the population. Beyond contributing to the massive effort of COVID‑19 testing and vaccination, pharmacists and nurses (particularly those in advanced practice) in several countries were given new or additional authorisations. These workers were permitted to renew or extend prescriptions for people with stable conditions; to provide advice, treatment and referral of people with common health issues to avoid unnecessary visits to emergency departments in hospitals; and to vaccinate people against other infectious diseases like influenza.
Community pharmacists were granted the opportunity to renew repeat prescriptions in countries including Canada, France, Ireland, Italy, Portugal and the United States. In Belgium, Ireland, Italy, Norway and Portugal, community pharmacists were given expanded roles in dispensing and administering influenza vaccinations for people aged 65 years and over and other at-risk groups. In Belgium, Germany, the Netherlands, Portugal and the United Kingdom, community pharmacists were also granted the opportunity to provide alternative solutions when medicine shortages occurred (PGEU, 2021[37]).
Several countries also expanded the traditional roles of nurses to respond to the surge in demand for care in response to the pandemic. In Italy, the government formalised the role of “family and community nurses” in May 2020 as a new type of advanced practice nurse to strengthen home‑based care and support the activity of new special units for continuity of care. The Italian Government allocated EUR 480 million to hire an estimated 9 600 of these nurses in 2021 (Government of Italy, 2020[38]). Most countries who responded to the OECD Resilience of Health Systems Questionnaire 2022 reported that they were introducing or expanding more advanced roles for nurses to tackle persistent shortages of GPs and other doctors, and to make nursing a more attractive profession (Figure 10.7 and Figure 10.8). These included countries with long experience with advanced practice nursing (such as Canada, Finland, the United Kingdom and the United States) and other countries with more recent experience (such as France, Greece and Italy).
In countries like Canada and the United States, where advanced practice nursing has existed for several decades, nurse practitioners represent a sizeable and growing proportion of primary care providers, along with GPs and pharmacists (Figure 10.16). However, in most other countries, they still represent only a very tiny proportion of all primary care providers.
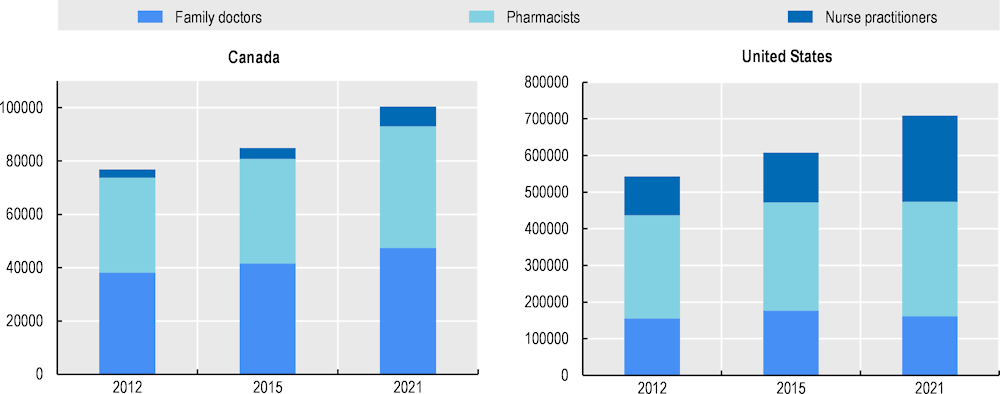
Note: In Canada, only about half of all nurse practitioners work in primary care, while this proportion is about 70% in the United States. A small proportion of pharmacists in Canada and the United States work in hospitals (not in the community). In the United States, family doctors include both family medicine and general internal medicine doctors.
Source: Canada: CIHI, https://www.cihi.ca/en/health-workforce; United States: Bureau of Labor Statistics, Occupational Employment and Wage Statistics data, https://www.bls.gov/oes/tables.htm.
A powerful lesson from the COVID‑19 pandemic is the crucial importance of the health workforce – and particularly frontline health workers – in treating patients, while often putting their own health and safety at risk. Although countries faced many resource constraints in absorbing the pandemic, the biggest constraint was a lack of health workers to respond to the surge in demand for care.
Greater investments are needed to strengthen health workforce capacity and flexibility, both to achieve universal health coverage and to avoid the risk of another public health crisis occurring with these critical structural weaknesses. Investing in the health workforce is an investment in health system resilience. At least half of investments to strengthen health systems and improve their readiness to address future shocks should be allocated to increasing training and recruitment; improving working conditions; and increasing the flexibility of the health workforce to respond to shocks and strains (see the chapter on investing in resilience).
Increasing training capacity is key to increasing the supply of doctors, nurses and other health workers to foster health system resilience in the medium and long term, especially in those countries where training capacity was low before the pandemic. Increasing retention rates of existing health workers and promoting more optimal skill mix and skill use are crucial to address workforce shortages in the short term, as countries seek to boost their recovery from the pandemic.
Many OECD countries have increased the number of students in medical and nursing education programmes in recent years to address shortages in the medium to long term. In many countries, decisions to increase student intakes preceded the pandemic, but the number of students has continued to increase. Domestic education and training should be designed to train enough new doctors, nurses and other health workers without having to rely unduly on international recruitment to fill domestic needs.
Policy decisions and guidance on student intakes in medical, nursing and other health education programmes need to be based on more robust and sophisticated health workforce planning and forecasting models. Planning should take into account demographic factors, as well as economic factors and innovations in health service delivery that may affect future demands for different types of doctors, nurses and other health workers.
Attracting enough young people into nursing is an important priority to address current and future shortages. It is heartening to see that the interest of young people in pursuing a career in nursing does not appear to have lessened since the pandemic. The number of student applications and admissions in nursing education programmes rose in 2020 and 2021 in many countries (e.g. Italy, Spain, the United Kingdom and the United States). However, the proportion of male students continues to be very low: over 80% of nursing students in many countries are female.
Increasing retention rates of existing doctors, nurses and other health workers is a key short-term priority to avoid a vicious cycle of growing shortages. Although evidence of a high level of resignations of health workers remains limited thus far, improvements in working conditions are needed to increase worker satisfaction, motivation and retention. These may require reducing workloads and pressure on staff; supporting their health, well-being and safety at work; and reviewing their pay rates. Such improvements in working conditions are particularly necessary for categories of workers that have traditionally been undervalued, such as nurses and health care assistants. They are also particularly urgent in countries experiencing significant losses of doctors and nurses through early retirement or emigration to other countries. While some of these measures may be implemented at a national level, several others need to be tailored at a more local level.
Many countries launched surveys to monitor health workforce safety and well-being during the pandemic. It will be important to continue to measure and address the safety and well-being of health workers regularly as these issues will not go away.
A key factor in resilience is how quickly and effectively health systems are able to use current health workers and any additional workers to respond to shocks and strains. The pandemic highlighted the need to mobilise additional health workers quickly to cope with a surge in demand for certain types of care. Most countries were able to mobilise such human resources by providing quick training and reallocating current staff to clinical areas with the greatest need (such as ICUs) and by drawing on retired or other inactive doctors and nurses, and medical and nursing students nearing the end of their studies, to support testing, tracing and isolating activities, and vaccination campaigns.
Health systems not only need to be better prepared to face unpredictable shocks in the future but also to adapt continuously to respond to predictable strains arising from population ageing and the growing burden of chronic diseases, including long COVID. The pandemic accelerated the development of new roles for some health care providers, such as pharmacists and advanced practice nurses, in prevention, testing and management of COVID‑19 and other chronic and communicable diseases. However, strategies used to address health workforce shortages during the pandemic were often adopted on a temporary basis. Countries need to assess whether these strategies should become a more permanent feature of their health service delivery models, contributing to a more resilient and flexible workforce in the future.
[23] AACN (2022), Nursing Schools See Enrollment Increases in Entry-Level Programs, Signaling Strong Interest in Nursing Careers, https://www.aacnnursing.org/News-Information/Press-Releases/View/ArticleId/25183/Nursing-Schools-See-Enrollment-Increases-in-Entry-Level-Programs.
[11] Aiyer, A. et al. (2020), “Mental Health Impact of COVID-19 on Healthcare Workers in the USA: A Cross-Sectional Web-Based Survey”, Journal of Depression and Anxiety, Vol. 9/4, pp. 1-8, https://doi.org/10.35248/2167-1044.20.9.373.
[10] Awano, N. et al. (2020), “Anxiety, Depression, and Resilience of Healthcare Workers in Japan During the Coronavirus Disease 2019 Outbreak”, Internal medicine (Tokyo, Japan), Vol. 59/21, pp. 2693-2699, https://doi.org/10.2169/INTERNALMEDICINE.5694-20.
[31] BLS (2022), Over 16 million women worked in health care and social assistance in 2021 : The Economics Daily: U.S. Bureau of Labor Statistics, https://www.bls.gov/opub/ted/2022/over-16-million-women-worked-in-health-care-and-social-assistance-in-2021.htm.
[36] Buchan, J. (2005), “A certain ratio? The policy implications of minimum staffing ratios in nursing”, Journal of Health Services Research and Policy, Vol. 10/4, pp. 239-244, https://doi.org/10.1258/135581905774414204.
[6] CDC (2022), COVID Data Tracker, https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
[26] CFNU (2022), Canadian Federation of Nurses Unions Member Survey Summary Report, CFNU.
[35] CPME (2021), CPME Policy on Health Workforce, https://www.cpme.eu/api/documents/adopted/2021/11/CPME_AD_27112021_096.-FINAL.CPME_.health.workforce.policy.pdf.
[3] Dergiades, T. et al. (2022), “Effectiveness of government policies in response to the first COVID-19 outbreak”, PLOS Global Public Health, Vol. 2/4, p. e0000242, https://doi.org/10.1371/JOURNAL.PGPH.0000242.
[2] DREES (2021), “Quelle démographie récente et à venir pour les professions médicales et pharmaceutique ? Constat et projections démographiques”.
[38] Government of Italy (2020), Relaunch decree, https://www.fnopi.it/wp-content/uploads/2020/05/Decreto-Rilancio-ore-17.30-13-maggio-2020-1.pdf.
[16] Government of Ontario (2022), Ontario Continues to Add Hospital Beds and Build Up Health Workforce | Ontario Newsroom, https://news.ontario.ca/en/release/1001411/ontario-continues-to-add-hospital-beds-and-build-up-health-workforce.
[17] Government of Quebec (2021), Programme d’aide à la reconnaissance des compétences (PARC) — Skill recognition assistance program (SRAP), https://www.immigration-quebec.gouv.qc.ca/en/partners/integration-programs/acces-ordres/index.html.
[7] Instituto Superiore di Sanità (2022), COVID-19 integrated surveillance data in Italy, https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-dashboard.
[32] King’s Fund (2022), “The NHS nursing workforce – have the floodgates opened?”, The King’s Fund, https://www.kingsfund.org.uk/blog/2022/10/nhs-nursing-workforce#vacancies-have-always-been-high.
[12] Kisely, S. et al. (2020), “Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis”, BMJ (Clinical research ed.), Vol. 369, p. m1642, https://doi.org/10.1136/BMJ.M1642.
[24] Mann, A. and V. Denis (2020), Can nursing thrive in the age of the coronavirus? What young people think about the profession | The OECD Forum Network, https://www.oecd-forum.org/posts/can-nursing-thrive-in-the-age-of-the-coronavirus-what-young-people-think-about-the-profession-dce5a659-cc6d-4914-b412-42e994be8197.
[20] Mastrillo, A. (2021), “CORSI DI LAUREA DELLE PROFESSIONI SANITARIE Dati sull’accesso ai corsi e programmazione posti nell’ A.A. 2021-22”, https://www.fioto.it/altreimg/Report%20Mastrillo%202021.pdf.
[4] Meslé, M. et al. (2021), “Estimated number of deaths directly averted in people 60 years and older as a result of COVID-19 vaccination in the WHO European Region, December 2020 to November 2021”, Eurosurveillance, Vol. 26/47, https://doi.org/10.2807/1560-7917.ES.2021.26.47.2101021.
[19] Ministère des Solidarités et de la Santé (2021), Arrêté du 13 septembre 2021 définissant les objectifs nationaux pluriannuels de professionnels de santé à former pour la période 2021-2025 - Légifrance, https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000044053576.
[8] Ministerio de Sanidad (2020), Actualización nº 194. Enfermedad por el coronavirus (COVID-19), https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_194_COVID-19.pdf.
[21] Ministry of Education and Professional Training (2022), Estadísticas de Educación - EDUCAbase, http://estadisticas.mecd.gob.es/EducaJaxiPx/Datos.htm?path=/Universitaria/Alumnado/EEU_2021/GradoCiclo/NuevoIngreso//l0/&file=NI_Grad_Sex_Edad(1)_Amb_Tot.px&type=pcaxis.
[9] Muller, A. et al. (2020), “The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review”, Psychiatry research, Vol. 293, https://doi.org/10.1016/J.PSYCHRES.2020.113441.
[14] OECD (2022), OECD Employment Outlook 2022: Building Back More Inclusive Labour Markets, OECD Publishing, Paris, https://doi.org/10.1787/1bb305a6-en.
[1] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[33] OECD/European Observatory on Health Systems and Policies (2021), State of Health in the EU, OECD Publishing, Paris, https://doi.org/10.1787/25227041.
[28] Ordre National des Infirmiers (2022), “L’Ordre National des Infirmiers alerte de nouveau sur la situation de la profession et appelle à l’organisation d’Etats-généraux de l’attractivité des professions de santé”, https://www.ordre-infirmiers.fr/actualites-presse/articles/resultats-consultation-infirmiere-lordre-national-infirmiers-alerte-de-nouveau-sur-la-situation-de-la-profession.html (accessed on 27 July 2022).
[27] Ordre National des Infirmiers (2021), “Enquête sur l’avenir de la profession infirmière auprès de plus 30 000 infirmiers”, https://www.ordre-infirmiers.fr/actualites-presse/articles/les-infirmiers-sinterrogent-sur-leur-avenir-et-souhaitent-des-evolutions-profondes-de-leur-metier.html (accessed on 16 December 2022).
[37] PGEU (2021), “Position Paper on the Role of Community Pharmacists in COVID-19-Lessons Learned from the Pandemic”.
[13] Pittet, L. et al. (2021), “Rapport Final: Mission indépendante nationale sur l’évaluation de la gestion de la crise Covid-19 et sur l’anticipation des risques pandémiques”.
[30] Raso, R., J. Fitzpatrick and K. Masick (2021), “Nurses’ Intent to Leave their Position and the Profession During the COVID-19 Pandemic”, The Journal of nursing administration, Vol. 51/10, pp. 488-494, https://doi.org/10.1097/NNA.0000000000001052.
[29] Royal College of Nursing (2021), Employment Survey 2021, Royal College of Nursing, https://www.rcn.org.uk/Professional-Development/publications/employment-survey-2021-uk-pub-010-075.
[5] Santé Publique France (2022), Recensement national des cas de COVID-19 chez les professionnels en établissements de santé, https://www.santepubliquefrance.fr/etudes-et-enquetes/recensement-national-des-cas-de-covid-19-chez-les-professionnels-en-etablissements-de-sante.
[25] Sciensano (2021), Power to Care: L’enquête sur le bien-être des personnes et professionnels d’aide et de soin. Principaux résultats de la deuxième enquête nationale, mars 2021., Sciensano, Bruxelles, https://www.sciensano.be/en/biblio/power-care-lenquete-sur-le-bien-etre-des-personnes-et-professionnels-daide-et-de-soin-principaux.
[15] Shembavnekar, N. and J. Buchan (2022), How reliant is the NHS in England on international nurse recruitment?, https://www.health.org.uk/news-and-comment/charts-and-infographics/how-reliant-is-the-nhs-in-england-on-international-nurse-recruitment.
[22] UCAS and HEE (2021), “Next Steps: Who are the ’Future Nurses’?”, https://www.ucas.com/next-steps-who-are-future-nurses?hash=ZlHV4VFctNT5WdPg4V1yq45O7rXDGjcnHZDmv-KjIxE.
[18] UK Department of Health (2017), “Expansion of undergraduate medical education - Government response to consultation”, http://www.nationalarchives.gov.uk/doc/open-government-licence/.
[34] Van den Heede Koen et al. (2022), Nurse staffing on Belgian intensive care units: the impact of two years of COVID-19 pandemic | KCE, https://kce.fgov.be/en/nurse-staffing-on-belgian-intensive-care-units-the-impact-of-two-years-of-covid-19-pandemic.
← 1. The data for France cover the period from 1 March to end of June 2020, while the data for Italy, Spain and the United States extends to the end of August 2020.
← 2. A full account of recruitment to and exits from the sector should also take into account layoffs by employers. However, layoffs from the health care and social assistance sector in the United States were relatively low and stable in 2021 and early 2022, at a rate of about 0.5% of total employment each month, according to data from the Job Openings and Labor Turnover Survey.