Sofia Astorga-Pinto
Emily Hewlett
Philip Haywood

Sofia Astorga-Pinto
Emily Hewlett
Philip Haywood
This chapter focuses on the impact of shocks and systemic disruptions on people’s mental health, with a focus on the COVID‑19 pandemic. It presents information about the prevalence of anxiety and depression in OECD countries, and about the disruption to mental health services. In response to the pandemic, the chapter reviews measures taken by OECD countries to protect and promote mental health, and improve mental health support. It concludes by offering recommendations to strengthen mental health and mental health support at individual and societal levels to build resilience and readiness to face future challenges.
Shocks such as pandemics, large‑scale displacements of people, natural and climate‑related disasters, and financial crises can affect people’s mental health profoundly. They can increase the prevalence of mental health issues and disrupt mental health services.
The COVID‑19 pandemic had a sizeable and negative impact on population mental health across OECD countries. There was a substantial increase in the prevalence of anxiety and depression symptoms associated with rises in COVID‑19 deaths and increased stringency of confinement policies in several OECD countries. Since the pandemic began, young people (aged up to 29 years) have consistently reported a higher prevalence of mental health issues than other age groups.
The pandemic disrupted mental health service referrals and delivery. Countries responded with a rapid shift to telehealth and other ways of delivering mental health support. All 26 OECD countries responding to the OECD Resilience of Health Systems Questionnaire 2022 introduced emergency mental health services and almost all (25 of 26) reported introducing permanent increases in services. Over two‑thirds of responding OECD countries (20 of 26) undertook mental health prevalence surveys, or tracked the impact of COVID‑19 on mental health service use (19 of 26).
While OECD countries made efforts to support mental health during the pandemic, it exposed a lack of capacity in mental health services and underinvestment in prevention. As the mental health legacy of COVID‑19 persists, a higher risk exists of key groups (including young people, women and people who are unemployed) presenting with mental health conditions and having unmet needs, generating or deepening inequalities in mental health.
Given the challenges the COVID‑19 pandemic presented for people’s mental health, and the potential opportunities for reform, it is recommended that OECD countries:
use the momentum gained during the pandemic to transform short-term measures into long-term changes to improve population mental health
include mental health considerations in crisis planning, developing mechanisms to understand the impact of public policies on population mental health in a crisis and improving mental health information systems
ensure the availability of valuable real-time information on the prevalence of mental health symptoms or issues and the knock-on effects of mental health service disruption to make evidence‑based decisions
implement interventions at an individual and population level to promote well-being and prevent mental health issues from arising, appreciating the interconnectivity of mental health with other systems and services requiring a whole‑of-society approach
improve access to and use of mental health services, especially for vulnerable populations.
Crises have a negative impact on mental health (WHO, 2014[1]; Lund et al., 2018[2]). The population affected by a sufficiently large shock will experience a degree of psychological distress that will usually improve over time. Some individuals will, however, develop a mental health issue, such as a depressive, anxiety and/or post-traumatic stress disorder (WHO, 2022[3]).
Shocks such as disasters, accidents, wars and economic crises affect not only individuals but also communities, institutions and systems. They can also deepen social inequities (WHO, 2014[1]). Disruptions to the health system also affect delivery of mental health services, worsening the impact of a crisis on people’s mental health.
The response to a crisis comprises four stages (see the key findings and recommendations chapter): prepare, absorb, recover and adapt. The prepare stage includes the steps taken to prepare critical functions to avoid and mitigate shocks. This occurs prior to the crisis. The absorb stage occurs after the shock commences. It comprises the capability of the health system to maintain core functions and absorb the consequences without collapse, limiting the extent of the disruption and minimising the morbidity and mortality impact. The recover stage involves regaining the disrupted functions as quickly and efficiently as possible. The adapt stage is the capacity of the health system to “learn” and improve its ability to absorb and recover from shocks, reducing the impact of similar threats in the future.
If mental health issues in a crisis are addressed promptly and effectively during the absorb stage, people will suffer fewer long-term effects as the response unfolds (WHO, 2022[3]). Analysing and implementing the lessons of the short-term interventions undertaken during the COVID‑19 pandemic – for example, the increased use of telehealth during the absorb and recover stages – could lead to beneficial long-term changes in mental health services during the adapt stage (WHO, 2020[4]). It is relevant, therefore, to understand the impact of shocks on people’s mental health, to promote more resilient health systems.
The following sections examine the impact of crises on people’s mental health (Section 8.1), the disruption to mental health services following the COVID‑19 pandemic, and measures taken by OECD countries to protect and promote mental health, and improve mental health support (Section 8.2). The final section (8.3) offers recommendations to strengthen mental health and mental health support to build resilience and readiness for future crises. Box 8.1 outlines the terminology, data and scope of this chapter.
The terms “mental health conditions” and “mental health issues” are used in this chapter. This is to align the language with ongoing efforts to raise awareness and address stigma, and to ensure – where possible – that language is person-centred, strengths-based and recovery-focused, reflecting the differing experiences of mental health issues from individual to individual.
This OECD report uses LGBTQI+ to refer to lesbian, gay, bisexual, transgender, queer (or questioning), intersex and gender fluid populations. However, other institutions, organisations, country policies and researchers use many variations on this term (McBrien, Rutigliano and Sticca, 2022[5]). This chapter includes the terminology in the original research or citation. This includes LGBTQ2S+: lesbian; gay; bisexual; transgender; queer or questioning; and two-spirit (Mental Health Research Canada, 2022[6]).
Population mental health data (especially age‑stratified data) remain limited in coverage. This chapter primarily uses prevalence of symptoms of anxiety and depression, estimated through surveys, as a proxy for mental health issues. Where possible, it uses validated instruments – such as the 7‑item General Anxiety Disorder scale (GAD‑7) for anxiety and the 9‑item Patient Health Questionnaire (PHQ‑9) for depression. Samples are not necessarily nationally representative (especially for rapid surveys undertaken during the COVID‑19 pandemic), and survey methods differ between studies, limiting the opportunity for cross-country comparisons. As symptoms are self-reported, increasing prevalence may reflect changes in levels of awareness or stigma about mental health, which can influence trends across countries and over time.
The very limited discussion of mental health issues beyond anxiety and depression in this chapter does not reflect their importance. These areas require further investigation and inclusion in plans to improve health systems resilience. Further data and information would benefit and nuance the findings made and the recommendations offered.
This chapter focuses on specific populations and highlights several issues for specific groups. Some of the mental health implications for specific populations are covered in other chapters. For instance, the impact on carers and on those in long-term care is discussed in the chapter on long-term care. The impact on health care workers is discussed in the chapter on the health workforce. More comprehensive information can also be found in other OECD publications (OECD, 2021[7]), including a focus on the mental health of young people (OECD/European Union, 2022[8]; OECD, 2021[9]).
Box 8.2 focuses on examples from Chile (2010 earthquake) and Australia (2019‑20 bushfires). Another example was the global financial crisis (2007‑08), which was linked to an increase in suicide rates in Greece (Kentikelenis et al., 2011[10]),the United Kingdom (Barr et al., 2012[11]), United States (Reeves et al., 2012[12]) and ten European countries (Stuckler et al., 2011[13]).
In 2010, Chile suffered a magnitude 8.8 earthquake followed by a tsunami. Hundreds of people died, and thousands lost their homes. This led to an increase in prevalence of mental health issues, including psychological distress, post-traumatic stress disorder, anxiety and depression (Leiva-Bianchi, 2011[14]; Díaz, Quintana and Vogel, 2012[15]; Fernandez et al., 2020[16]; Dutta et al., 2022[17]). Female adolescents (compared to male adolescents) and people exposed to multiple stressors were more at risk of developing mental health issues (Díaz, Quintana and Vogel, 2012[15]; Fernandez et al., 2020[16]). After two years, those with risk factors still had a higher prevalence of mental health conditions (Andrades, García and Kilmer, 2021[18]).
The quick response of the health system in some cities avoided heavy disruption of mental health care. The Hospital of Curicó was destroyed during the earthquake, but mental health services were rapidly relocated, and care continued to be provided two days after the earthquake (Vitriol G et al., 2013[19]). However, coverage of mental health services during the crisis was distributed unequally. Mental health interventions were implemented in affected areas, but only covered 35% of the affected population and focused mainly on areas that were geographically accessible and where people of high socio‑economic status lived (Vitriol et al., 2014[20]).
The bushfire season in Australia lasted over nine months between 2019 and 2020. There were 33 direct deaths, over 400 excess deaths, millions of hectares were burnt, and thousands of homes were destroyed. Studies showed an increase in mental health issues, including anxiety, depression, stress and sleep disturbances (Rodney et al., 2021[21]; Podubinski and Glenister, 2021[22]; Isaac et al., 2021[23]). Women and people with pre‑existing medical conditions were more vulnerable to this crisis.
Podubinski and Glenister (2021[22]) also studied the cumulative impacts of multiple crises on mental health by analysing the interaction of fire exposure and COVID‑19, and their effects on mental health in Australia. They found that people who had experienced prior crises or disruptions (such as exposure to fires or another form of shock) required additional support to protect their mental health during the pandemic. This demonstrates the compounding nature of stresses.
The COVID‑19 pandemic was very disruptive. Its health impact was compounded by the social and economic consequences, such as lockdowns and other containment and mitigation measures, schooling disruption and changing employment status.
Previous OECD publications have highlighted the significant initial impact the pandemic had on population mental health (OECD, 2021[24]; 2021[9]; 2021[7]). These studies also found that population mental health is worse than before the pandemic, with the prevalence of mental health symptoms having doubled in some OECD countries. For example, the share of young people (aged 18‑29 years) with symptoms of depression more than doubled in seven European countries for which broadly comparable pre‑pandemic and pandemic data are available (OECD/European Union, 2022[8]).
Recent evidence provides a more comprehensive view of the impact of the pandemic on population mental health, especially over the longer absorb and recover stages of the response to it (see the chapter on key findings and recommendations).
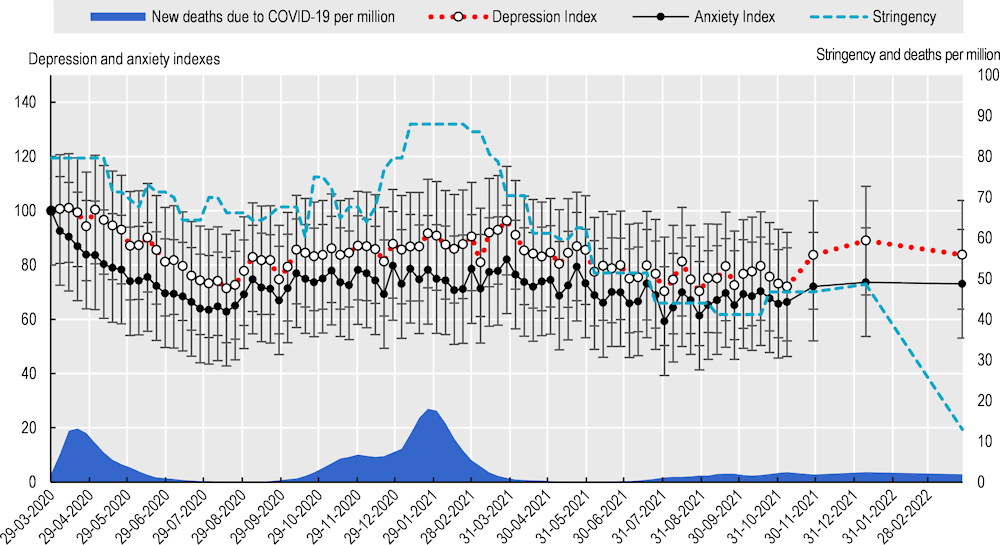
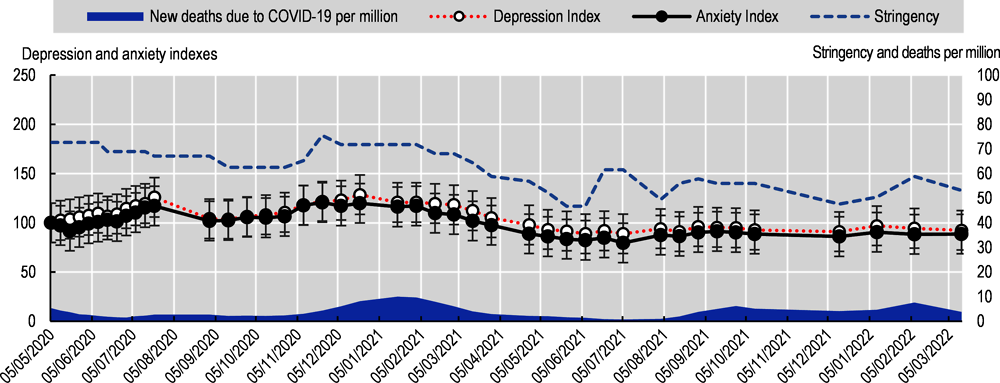
Figure 8.1 to Figure 8.6 present data on prevalence of depression and anxiety from the first two years of the pandemic for six countries. Available data from selected OECD countries were analysed to identify some points of comparison (Box 8.3).
In general, the mental health status of populations in these six countries in late 2021 and early 2022 was better than during the first and second lockdown periods, but it was worse than at the beginning of the pandemic in some countries. For example, in Canada (Figure 8.2), the depression and anxiety point estimates were above the 100 baseline during the remainder of the data presented. On the other hand, data from populations in countries like Switzerland (Figure 8.4) and the United Kingdom ( Figure 8.5) suggest a lower burden of mental health symptoms in late 2021 and early 2022 than earlier.
Additionally, Figure 8.1 to Figure 8.6 show that, in general, anxiety and depression followed a similar trend to numbers of deaths due to COVID‑19 and the stringency of government responses (Table 8.1). Thus, when the stringency of measures and deaths increased, the prevalence of anxiety and depression symptoms also increased. These relationships varied, however, depending on the country, the mental health symptoms examined and other pandemic variables.
The countries assessed depression and anxiety differently (see the footnotes for each figure), and began collecting data at different time‑points, impeding direct comparisons between countries. To understand the variation in these mental health issues better, an index was calculated using the first time‑point with available data as a baseline. The baseline was transformed into a 100 value, and the rest of the data points were converted by calculating their variation from the 100 baseline. Thus, the data can be interpreted as how much the prevalence of anxiety and depression symptoms varied from the point at which the relevant country started collecting data (usually at the beginning of the pandemic).
The values for COVID‑19 deaths are based on the daily reports of new deaths due to COVID‑19 per million people (smoothed values) (Mathieu et al., 2020[25]). A 7‑day mean of new cases was calculated for this chapter, from 21 January 2020 until March 2022. Finally, the Stringency Index was calculated by the Oxford Coronavirus Government Response Tracker (Mathieu et al., 2020[25]). The data were extracted on 11 April 2022.
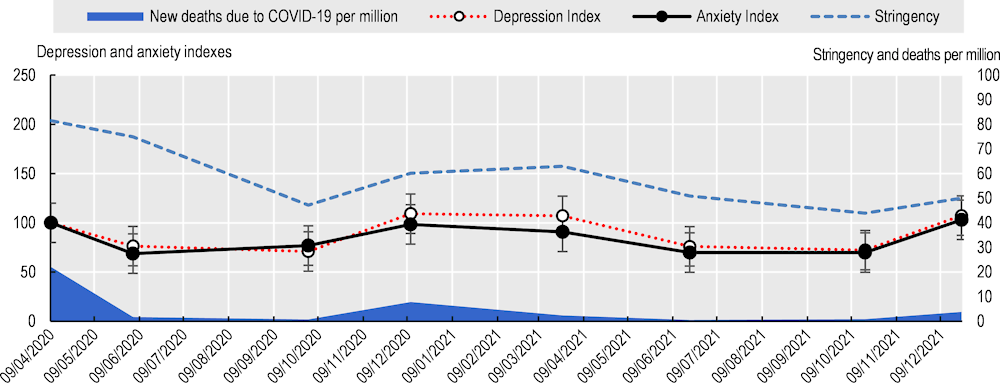
Note: PHQ‑9 was used to assess depressive symptoms and GAD‑7 to assess anxiety symptoms.
Source: Superior Health Council of Belgium (n.d.[26]), Belgium COVID‑19 Epidemiological Situation: Mental Health Studies, https://datastudio.google.com/embed/reporting/7e11980c-3350-4ee3-8291-3065cc4e90c2/page/ykUGC.
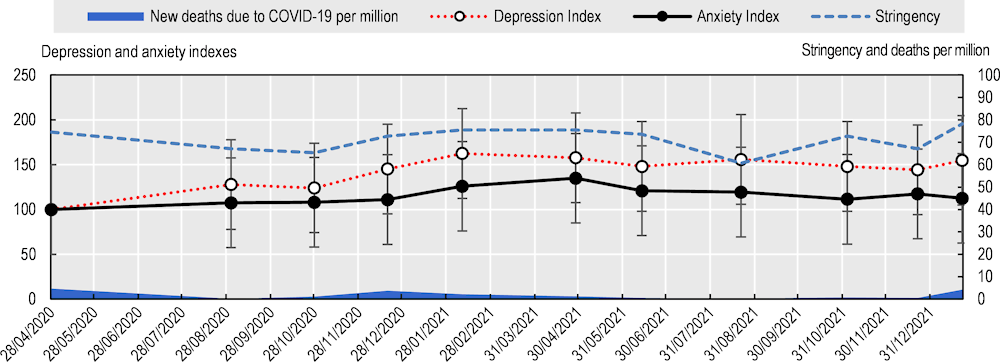
Note: Anxiety and depression indexes were calculated based on the self-rated levels of anxiety and depression in answer to the question: “Your level of anxiety/depression since the coronavirus (COVID‑19) outbreak in Canada”, on a 0 to 10 scale, where “10” is extremely high and “0” is none. Categories were low (0‑4), medium (5‑7) and high (8‑10). The chart presents the high results. The data do not include Canada’s territories (Yukon, Northwest Territories and Nunavut).
Source: Mental Health Research Canada, (2022[6]), Mental Health in Crisis: How COVID‑19 Is Impacting Canadians National Poll (Poll 12), https://www.mhrc.ca/national-polling-covid.
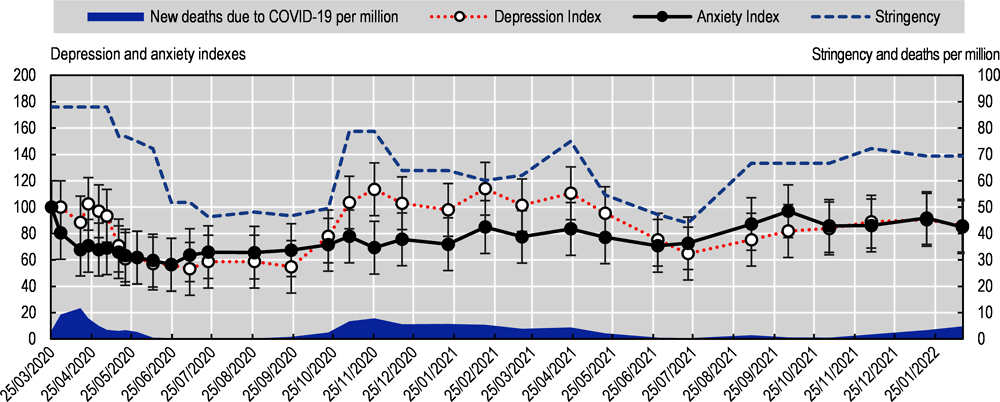
Note: The Hospital Anxiety and Depression scale (scores of >10) was used to assess anxiety and depression symptoms.
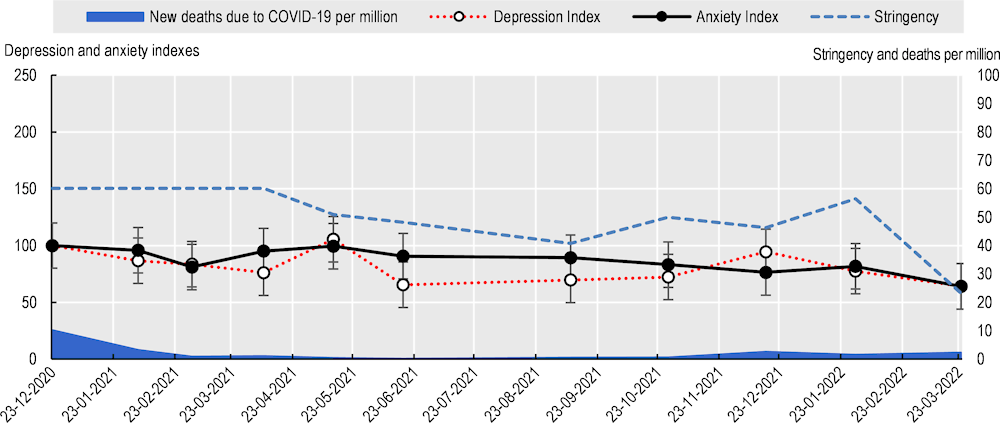
Note: The PHQ‑4 anxiety subscale 0‑6 was used to assess anxiety symptoms and the PHQ‑4 depression subscale 0‑6 to assess depression symptoms. The data present results categorised as “red flag for depression/anxiety disorder” (≥5 is a red flag, while ≥3 is a yellow flag). Please note the first time point is December 2020.
Source: Höglinger et al. (n.d.[28]), COVID‑19 Social Monitor: Mental Health, https://covid19.ctu.unibe.ch.
Note: PHQ‑9 was used to assess depressive symptoms and GAD‑7 to assess anxiety symptoms. The size of the graph has been increased to show the number of time points clearly.
Source: UCL (2022[29]), UCL COVID‑19 Social Study Reports, https://www.covidsocialstudy.org/results.
Note: The modified PHQ‑2 was used to assess depressive symptoms and modified GAD‑2 to assess anxiety symptoms.
Source: CDC (2022[30]) Household Pulse Survey, https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm.
|
|
Mean |
Standard deviation |
Correlation with Stringency |
Correlations with COVID‑19 deaths* |
Correlation of Anxiety and Depression indices |
|
|---|---|---|---|---|---|---|
|
Belgium |
Depression index |
89.97 |
17.42 |
0.33 |
0.47 |
1 |
|
Anxiety index |
84.70 |
14.87 |
0.28 |
0.62 |
0.92 |
|
|
Canada |
Depression index |
142.57 |
18.42 |
0.14 |
‑0.28 |
1 |
|
Anxiety index |
115.33 |
9.68 |
0.16 |
‑0.36 |
0.80 |
|
|
France |
Depression index |
83.17 |
19.23 |
0.50 |
0.70 |
1 |
|
Anxiety index |
74.73 |
10.88 |
0.20 |
0.07 |
0.52 |
|
|
Switzerland |
Depression index |
81.43 |
13.97 |
0.48 |
0.47 |
1 |
|
Anxiety index |
86.98 |
10.97 |
0.68 |
0.26 |
0.49 |
|
|
United Kingdom |
Depression index |
83.44 |
7.55 |
0.62 |
0.55 |
1 |
|
Anxiety index |
72.79 |
6.74 |
0.53 |
0.47 |
0.93 |
|
|
United States |
Depression index |
105.48 |
11.55 |
0.75 |
0.38 |
1 |
|
Anxiety index |
99.57 |
11.87 |
0.72 |
0.39 |
0.97 |
|
*Mean 7 days of new deaths due to COVID‑19 per million population.
Note: Care must be taken when comparing data across countries because they assessed mental health with different screening tools.
Strength of the correlation coefficients can be interpreted with the following rule of thumb (for positive or negative correlations): 0.90‑1.00 = very high correlation; 0.70‑0.90 = high correlation; 0.50‑0.70 = moderate correlation; 0.30‑0.50 = low correlation; 0.00‑0.30 = very low correlation.
Source: Mukaka (2012[31]), Statistics Corner: A guide to appropriate use of correlation coefficient in medical research, https://pubmed.ncbi.nlm.nih.gov/23638278/
Evidence on suicide rates is currently inconsistent, showing increases and decreases depending on the country and stage of the pandemic. Although suicide rates did not increase significantly across populations in 2021, suicidal ideation increased during the COVID‑19 pandemic, especially among young people (WHO, 2022[32]; OECD, 2021[24]). For example, the increase was around five‑fold in reported rates of suicidal ideation in Belgium (among those aged 18‑29 years) and in France (among those aged 18‑24 years), compared to pre‑pandemic prevalence (OECD/European Union, 2022[8]). It is therefore critically important that suicide prevention measures are strengthened and that rates of death by suicide are monitored closely as the pandemic continues.
The mental health impact of the COVID‑19 crisis was borne inequitably across the population of OECD countries. Some of the key population groups affected disproportionately were those with pre‑existing health conditions, people infected with COVID‑19, unemployed people, people with lower socio‑economic status and education levels, women, transgender people, members of the LGBT2Q+ community and young people. These groups have a higher risk of poor mental health and greater unmet mental health needs. However, this list is not exhaustive. Other vulnerable populations’ needs should also be considered in some countries – for example, indigenous peoples in Canada (Jenkins et al., 2021[33]).
People with pre‑existing health and mental health conditions were at a higher risk of experiencing mental health issues during the COVID‑19 pandemic (WHO, 2022[32]). For example, in Finland, the effects were more severe for people with previous mental health conditions – especially children and adolescents (Kestilä et al., 2022[34]). In Canada, people with pre‑existing mental health issues (due to health, social and/or structural vulnerabilities) were also more likely to report worse mental health (Jenkins et al., 2021[33]).
People infected with COVID‑19 reported a higher prevalence of mental health issues than non-COVID‑19 patients (WHO, 2022[32]). Studies into mental health and post-COVID‑19 syndrome or “long COVID” patients have some limitations – including the lack of a clear definition of long COVID, and inconsistent criteria for selecting participants. However, the evidence is accumulating as OECD countries transition into the recovery stage of the pandemic. A study from Hungary in 2022 found that higher levels of depressive and anxiety symptoms were associated with a higher number of long COVID symptoms, and that depression was a predictor of a higher number of long COVID symptoms (Ocsovszky et al., 2022[35]). Life satisfaction and social support are also negatively associated with long COVID symptoms. A longitudinal study in the People’s Republic of China found that, even though COVID‑19 survivors’ mental health had improved after two years, they still had a higher prevalence of anxiety and depression than people without long COVID symptoms (Huang et al., 2022[36]). Further research is needed to study the relationship between long COVID and mental health outcomes.
Unemployment is commonly related to poorer mental health outcomes (OECD, 2021[37]). The pandemic exacerbated this situation: people who were unemployed reported more symptoms of depression and anxiety (OECD, 2021[24]). In France, unemployed people were more likely to report depression and anxiety symptoms than those in employment. In the United Kingdom, workers who were in long-term insecure jobs before and after the start of the pandemic without furlough reported a significant increase in mental distress during the pandemic (OECD, 2021[24]; Smith, Taylor and Kolbas, 2020[38]). A Finnish study found an increase in psychological stress for unemployed people, and especially unemployed women, in 2020 compared to 2018 data (Kestilä et al., 2022[34]). This study also found that retired women experienced a higher increase in psychological stress during the pandemic. In 2021 and early 2022, self-rated levels of anxiety and depression continued to be worse for unemployed people in Canada (Mental Health Research Canada, 2022[6]).
It was well known before the COVID‑19 pandemic that socio‑economic status and education are determinants of mental health: people with lower socio‑economic status and education levels tend to have poorer mental health outcomes (WHO, 2014[1]). These determinants were a factor during the pandemic, but data supporting the association were not consistent across countries. For example, in the United Kingdom, people with lower education and income levels presented with higher anxiety scores (Fancourt, Steptoe and Bu, 2021[39]). The United States had similar findings: the group with the lowest education levels consistently presented with a higher prevalence of depressive symptoms compared to groups with higher education levels (CDC, 2022[30]). In Finland, however, psychological stress was found to have increased among highly educated women, as well as among less-educated men and women (Kestilä et al., 2022[34]; CDC, 2022[30]).
Similar inconsistencies according to socio‑economic status and education level were reported for unmet mental health needs. The US Household Pulse Survey 2022 found that the population with a medium education level was the group with the highest unmet mental health needs – they needed counselling or therapy but did not receive it (Figure 8.7) (CDC, 2022[30]). The survey also found, however, that the group with high education levels used counselling or therapy more. Therefore, the groups with a higher prevalence of depressive symptoms and higher unmet needs were not the groups using more counselling or therapy services, meaning that the delivery of care was potentially inequitable. This is an ongoing challenge for many OECD countries as countries seek to recover from the pandemic.
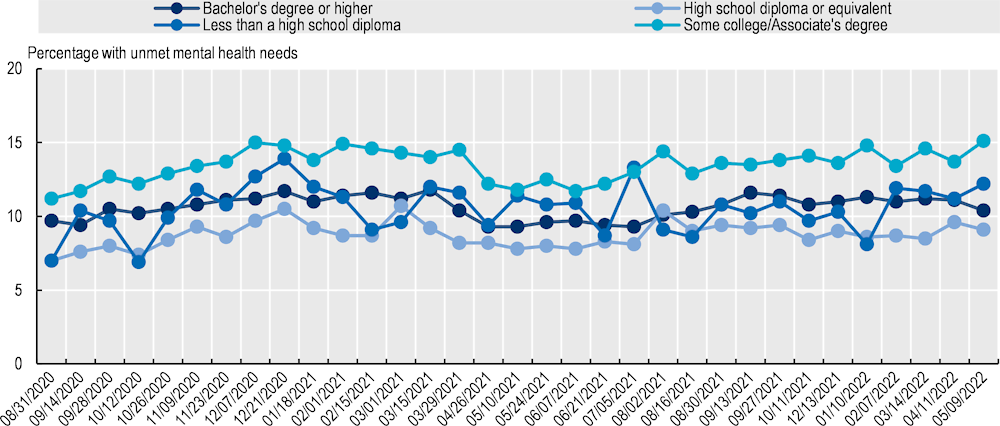
Note: Unmet mental health needs refer to the number of people that needed counselling or therapy but did not receive it.
Source: CDC (2022[30]) Household Pulse Survey, https://www.cdc.gov/nchs/covid19/pulse/mental-health-care.htm.
Before the pandemic, women were already more likely to report and be diagnosed with depression and anxiety symptoms than men, but the pandemic increased the gap in mental well-being between women and men (WHO, 2022[32]; OECD, 2021[24]). In the first months of the pandemic, the gap widened by 66% in the United States (Adams-Prassl et al., 2020[40]). This trend then continued. For example, in Canada, women had a higher prevalence of self-reported anxiety than men (25% vs. 16%) in 2022 (Mental Health Research Canada, 2022[6]). In Finland, highly educated and retired women presented with increased psychological stress during the pandemic (Kestilä et al., 2022[34]). Women also had higher unmet needs than men, at least in some countries. In the United States, women reported higher unmet mental health needs than men, and this was consistent during the first two years of the pandemic (CDC, 2022[30]).
The US Household Pulse Survey 2022 found that transgender people had a higher prevalence of unmet mental health needs compared to cisgender females and males (CDC, 2022[30]) (Figure 8.8). Also, members of the LGBTQI+ community in general (LGBTQ2S+) presented with higher levels of self-reported anxiety and depression than the adult population in Canada in 2022 (Mental Health Research Canada, 2022[6]).
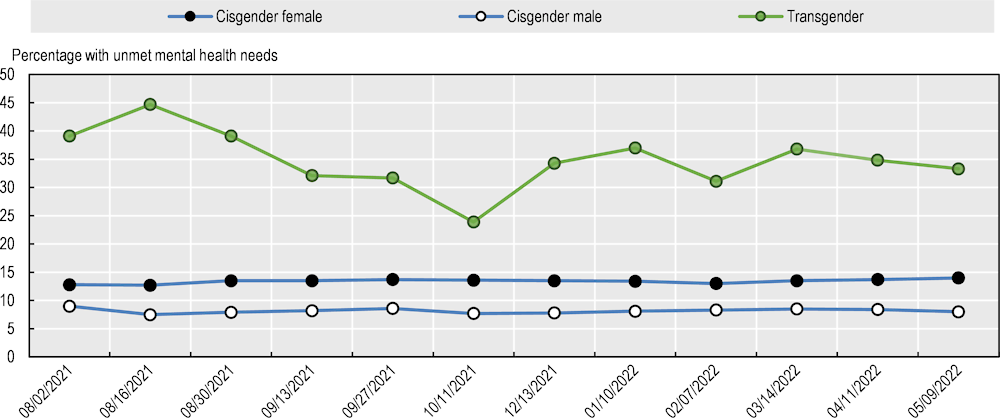
Note: Unmet mental health needs refer to the number of people that needed counselling or therapy but did not receive it.
Source: CDC (2022[30]) Household Pulse Survey, https://www.cdc.gov/nchs/covid19/pulse/mental-health-care.htm.
Young people (aged up to 29 years) consistently reported a higher prevalence of mental health issues compared to other age groups since the pandemic began. In OECD countries, the increase in prevalence of anxiety and depression symptoms in this group was significant (OECD/European Union, 2022[8]). Additionally, the prevalence of symptoms has not returned to pre‑pandemic levels, despite the lifting of containment and mitigation measures (OECD, 2021[9]). A WHO report found that younger age was reportedly a risk factor for mental health issues in several studies and countries during the pandemic (WHO, 2022[32]). A global meta‑analysis of studies reporting on symptoms of anxiety and depression in people aged up to 18 years found that prevalence of symptoms was double pre‑pandemic levels, with one in four experiencing symptoms of depression, and one in five experiencing symptoms of anxiety (Racine et al., 2021[41]).
In Japan, 31% of people aged 20‑29 years presented with depression symptoms compared to 18% of older adults in mid‑2020 (Fukase et al., 2021[42]). In 2021, young people (aged 18‑29 years) in Belgium, France and the United States showed a 30‑80% higher prevalence of anxiety and depression symptoms than the general population, and this was twice the prevalence they experienced before the pandemic (OECD, 2021[9]).
This situation continued into 2022. Younger groups in Canada showed a higher prevalence of self-reported anxiety than older groups (24% of people aged 16‑17 years and 31% of people aged 18‑34 years, compared to 14% of people aged 55 years and over) (Mental Health Research Canada, 2022[6]). In Finland, mood problems among children and young people have reportedly increased, albeit with no large differences between girls and boys. People aged 15‑29 years reported experiencing more stress during the pandemic compared to older age groups (Kestilä et al., 2022[34]).
Younger people also presented with higher unmet mental health needs compared to older age groups. The US Household Pulse Survey 2022 found that a higher number of people aged 18‑29 years reported needing counselling or therapy, but fewer received it compared to older age groups (Figure 8.9) (CDC, 2022[30]).
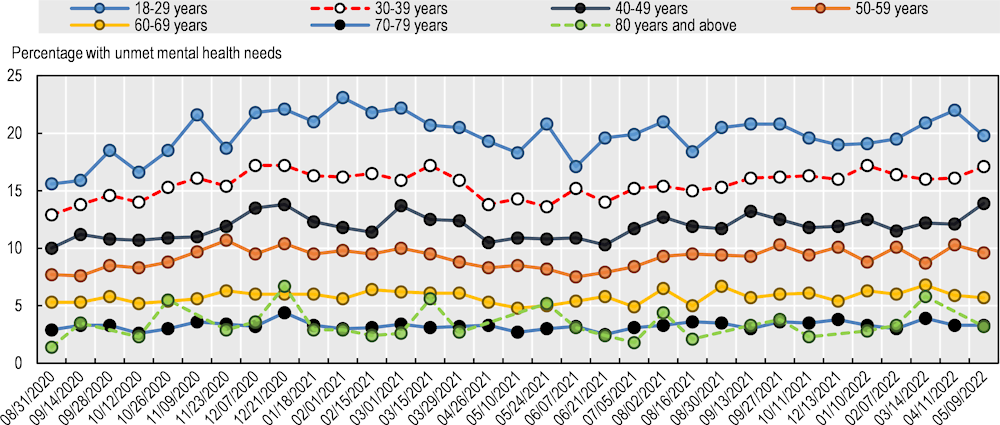
Note: Unmet mental health needs refer to the number of people that needed counselling or therapy but did not receive it.
Source: CDC (2022[30]) Household Pulse Survey, https://www.cdc.gov/nchs/covid19/pulse/mental-health-care.htm.
Data from Finland showed an increase in the number of children and adolescents who waited more than 90 days for mental health treatment during the pandemic (Terveyden ja hyvinvoinnin laitos, 2022[43]). A large increase occurred at the end of 2020 (Figure 8.10). Another Finnish study found that only 39% of children and adolescents received help with learning during the pandemic, and there was an association between not receiving support and higher anxiety levels. This association was strong for both girls and boys; however, more girls needed learning support but did not receive it (Kestilä et al., 2022[34]).
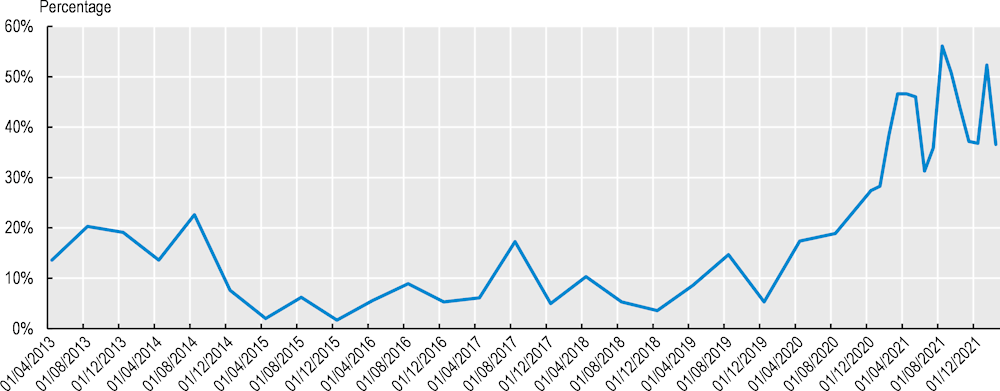
Source: Terveyden ja hyvinvoinnin laitos (2022[43]),Mental health services for children and adolescents – Queue situation in specialised medical care, psychiatry – THL cube and sealing interface.
The pandemic disrupted the delivery of mental health services globally, including across OECD countries (OECD, 2021[7]). Worldwide, 93% of countries reported interruptions in their mental health services (WHO, 2020[4]). In the Netherlands, there was a drop of 25‑80% in the number of referrals to mental health providers and a drop of 10‑40% in treatment demand during the first wave of the pandemic (OECD, 2021[24]). In Switzerland, access to mental health care was also reduced owing to containment and mitigation measures (Stocker et al., 2021[44]). Effective and timely delivery of mental health care was already challenged before the pandemic began. Containment measures during the early months of the pandemic magnified these challenges in many OECD countries.
The reasons for the disruption are well understood. The absorb stage of the pandemic response focused on tackling the critical care requirements of the crisis (see the chapter on critical care surge). Elective care was cancelled (including mental health care), and hospital beds typically reserved for mental health patients were instead used for COVID‑19 patients (WHO, 2020[4]; OECD, 2021[7]). Additionally, patients did not attend in-person mental health consultations because of fears of contracting the virus, and travel restrictions also affected access. Altruism and concern for freeing up health resources also played a role. For example, in Switzerland, some patients withdrew from telephone mental health consultations because they considered themselves non-urgent cases. Also, people declined to attend day clinics because they were (or could be) high-risk COVID‑19 patients (Stocker et al., 2021[44]).
Community-based services were among the most affected mental health services (OECD, 2021[24]). Worldwide, 40% of countries closed their community-based mental health services entirely or in part (WHO, 2020[4]). In Italy, 14% of community mental health centres closed, and 25% reduced their hours in April 2020 (Carpiniello et al., 2020[45]). England (United Kingdom) also reduced primary care contacts for mental health conditions (Mansfield et al., 2021[46]).
Outpatient and emergency mental health services in hospitals were also disrupted heavily (OECD, 2021[24]). Approximately 78% of day hospitals closed in Italy in April 2020 (Carpiniello et al., 2020[45]). In Lombardy (Italy), emergency department psychiatric visits suffered a 43% reduction (Stein et al., 2020[47]). Three hospitals in Paris (France) sustained a 54.8% drop in the number of emergency psychiatric consultations during the first weeks of the pandemic (Pignon et al., 2020[48]). On the other hand, psychiatric services in Swiss hospitals stayed almost entirely open and were available during the first lockdown. Only a few day clinics closed for some weeks or continued operating on a reduced scale (Stocker et al., 2021[44]).
Other mental health services also experienced disruptions. Services focused on prevention and promotion – which were already struggling before the pandemic – were affected profoundly (WHO, 2020[4]). Home care and day services were closed completely or partly in 60‑70% of countries surveyed by WHO. In England (United Kingdom), referrals to the Increasing Access to Psychological Therapies Programme fell by 61% between February and April 2020 (Johnson et al., 2021[49]). In Switzerland, psychiatric rehabilitation services were inaccessible or had limited accessibility during and after the first lockdown.
Mental health support in schools, workplaces and broader community settings is a critical part of overall delivery of mental health services (OECD, 2021[50]; 2021[37]). Extensive evidence is available on the relevance of integrating mental health treatment with employment support to improve work and mental health outcomes. These services were also disrupted significantly during the absorb stage of the pandemic, with closed schools and workplaces. In 2020, around 75% of school or workplace mental health services were disrupted fully or partly (WHO, 2020[4]). In early 2021, school-based mental health programmes were still highly interrupted (WHO, 2021[51]).
In response to the COVID‑19 pandemic, several OECD countries rapidly included mental health in their plans to address the crisis. By mid‑2020, 89% of the countries surveyed by WHO reported that mental health and psychosocial support were included in their COVID‑19 response plans (WHO, 2020[4]).
As countries move further into recovering from the pandemic, mental health support has broadened and deepened. Among respondents to the OECD Resilience of Health Systems Questionnaire 2022, 100% of countries (26 of 26) reported having introduced emergency mental health support measures for the public during the pandemic. Additionally, 96% (25 of 26) reported having permanently increased mental health support or capacity since the start of the crisis. This said, only 58% of countries (15 of 26) reported having new or temporary mental health services or including service entitlement in emergency mental health support.
As OECD countries began addressing the disruptions, the use of mental health services increased in 2020 and 2021 compared to previous years. For example, in Australia, the number of mental health services provided in 2021 was higher than in 2019 and 2020 (Figure 8.11) (Australian Institute of Health and Welfare, 2022[52]). The total number of weekly mental health services increased by 25% from March 2020 to December 2020. It then decreased by 41% in January 2021 and peaked in August 2021 – an 83% increase. Figure 8.11 also shows that 2019, 2020 and 2021 had similar seasonal patterns in the number of mental health services provided, defined as consultations provided by mental health workers. The steeper decrease in December-January is explained by holiday leave arrangements.
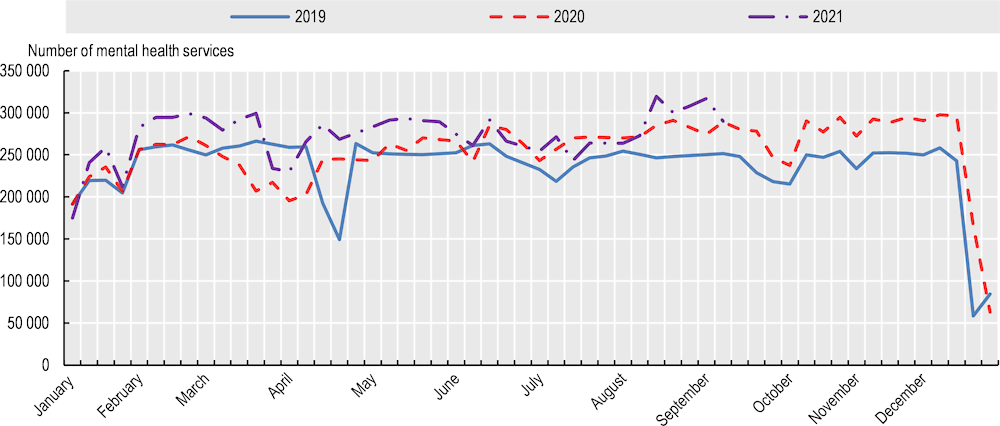
Note: These are services billed via the Medical Benefits Schedule by a recognised practitioner; data exclude services that are not billed under these arrangements (including, for example, some public hospital services and some crisis support services).
Source: Australian Institute of Health and Welfare (2022[52]), Mental health impact of COVID‑19, https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/covid-19-impact-on-mental-health.
In Lithuania, like Australia, the number of people who sought treatment for depression, anxiety and high-stress disorders was higher in 2020 than 2019, according to responses to the OECD Resilience of Health Systems Questionnaire 2022 (Figure 8.12).
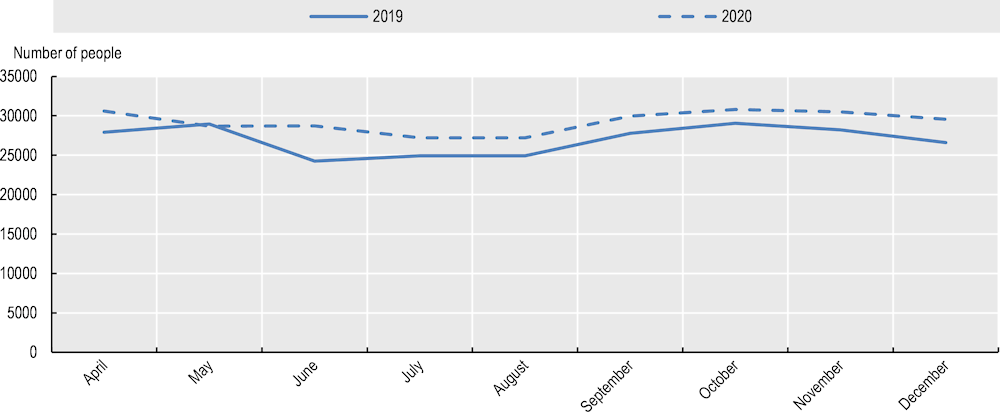
Source: Data provided by the Ministry of Health of Lithuania in response to the OECD Resilience of Health Systems Questionnaire 2022.
Canada also saw an increase in the number of people accessing mental health services once the pandemic began. According to a national survey of mental health and COVID‑19, 10% of participants accessed mental health support in 2019, whereas 22% of participants accessed this support after the pandemic began (Mental Health Research Canada, 2022[6]). In terms of age distribution, 35% of the group aged 18‑34 years accessed support, compared to 25% of the group aged 35‑54 years and 10% of the group aged 55 years and over. The number of people who decided not to attend mental health services due to an inability to pay also fell (from 37% in 2019 to 16% in 2020) (Mental Health Research Canada, n.d.[53]).
In Switzerland, the use of mental health services was on an upward trend before the pandemic. It then increased markedly once the pandemic began (Stocker et al., 2021[44]). This research found that women sought and received more mental health services, and that children, adolescents and young people were important groups seeking mental health services. However, the report also found that people with a migrant background did not access mental health services often. In Finland, children and adolescents showed an increase in mental health symptoms, but their use of services also increased (Kestilä et al., 2022[34]). Similarly, England (United Kingdom) saw an upswing in mental health service referrals and contacts for children and adolescents aged 0‑18 years (Figure 8.13).
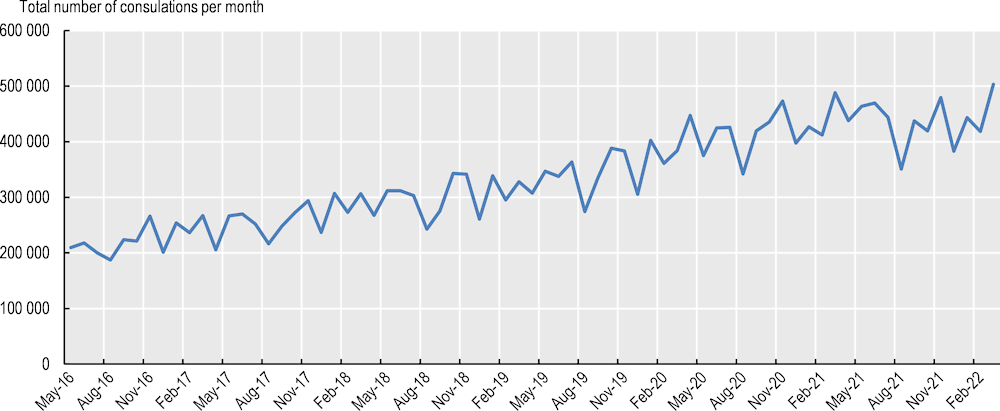
Note: Total variable includes all consultation mediums for mental health care (email, face‑to-face communication, SMS text messaging, telehealth web camera, telephone, talk type for a person unable to speak, instant messaging, message board, text message, video consultation, chat room, face‑to-face communication, other, other not listed, missing and invalid). The data are from May 2016 to March 2022.
Source: NHS digital (2021[54]), Mental health services referrals and care contacts for children and young people aged 0 to 18 years, NHS digital, https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/mental-health-data-hub/dashboards/mental-health-services-monthly-statistics#mental-health-services-referrals-and-care-contacts-for-children-and-young-people-aged-0-to-18.
The COVID‑19 pandemic accelerated the delivery of mental health services via telehealth (online or by phone), and catalysed the availability and use of virtual mental health tools. Worldwide, 70% of countries replaced in-person attendance with telehealth and 68% introduced mental health helplines (WHO, 2020[4]).
OECD countries observed a substantial increase in the delivery of mental health services through telehealth (OECD, 2021[7]; 2021[24]). Digital mental health support services offered included screening, self-management and treatment, as well as information. In Canada, the reduction in in-person mental health care in 2020 was complemented by telehealth (Mental Health Research Canada, n.d.[53]).
Responses to the OECD Resilience of Health Systems Questionnaire 2022 revealed that 88% of countries (23 of 26) introduced new phone support lines as emergency mental health support for the public once the pandemic began (Box 8.4). These countries included Australia, Austria, Canada, Costa Rica, the Czech Republic, Finland, France, Germany, Greece, Ireland, Israel, Italy, Korea, Latvia, Lithuania, Luxembourg, Mexico, Portugal, Slovenia, Spain, Türkiye, the United Kingdom and the United States (Box 8.4).
Costa Rica implemented a mental health support line for families who lost members due to COVID‑19 or for other reasons. The country also introduced helplines for students and suicide prevention helplines.
Finland offered support for students via phone, email or other digital platforms.
Latvia introduced two phone lines for psycho‑emotional support for adults and adolescents.
Lithuania implemented a free phone line for emotional support, including specific helplines for children, young people, women and parents.
Source: Examples provided by countries in response to the OECD Resilience of Health Systems Questionnaire 2022.
In England (United Kingdom), in-person consultations for children and adolescents (aged 0‑18 years) also suffered a drop in 2020 when the pandemic started, but this was complemented by telehealth appointments (Figure 8.14). Numbers of face‑to-face sessions were, however, still higher than those of online sessions up to the end of the reporting window in August 2021 (NHS digital, 2021[54]).
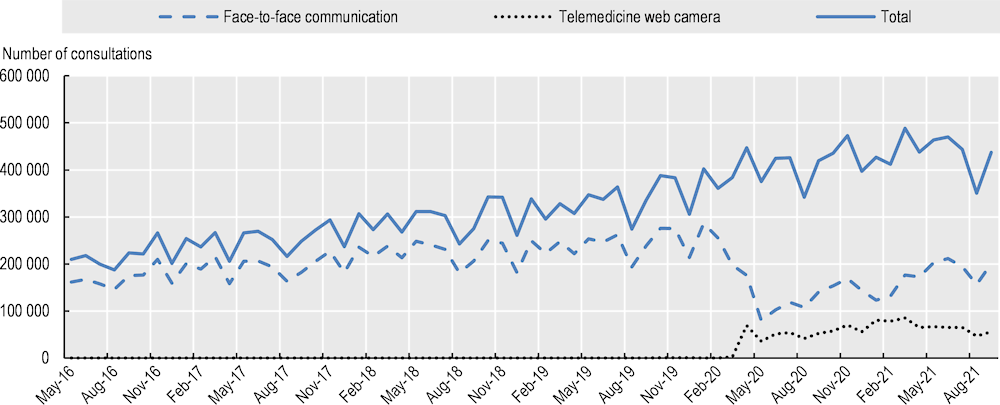
Note: Total includes all consultation mediums for mental health care (email, face‑to-face communication, SMS text messaging, telehealth web camera, telephone, talk type for a person unable to speak, instant messaging, message board, text message, video consultation, chat room, face‑to-face communication, other, other not listed, missing and invalid).
Source: NHS digital (2021[54]) Mental health services referrals and care contacts for children and young people aged 0 to 18 years, https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/mental-health-data-hub/dashboards/mental-health-services-monthly-statistics#mental-health-services-referrals-and-care-contacts-for-children-and-young-people-aged-0-to-18.
Increasing evidence supports the use of telehealth for therapy, showing that treatment efficacy is not sacrificed with mental telehealth (Bean et al., 2022[55]; Feijt et al., 2020[56]; Wilczewski et al., 2022[57]). For example, cognitive behavioural therapy via telehealth shows similar efficacy levels to in-person treatment, and there are no significant differences in symptom reduction between the modes of delivery. Mental health providers in the United States agree that it is possible to form a therapeutic relationship with patients, which was an initial concern with mental telehealth. Telehealth is also more affordable than in-person therapy (considering the costs and time of transportation as well) and it can reach patients who would usually not access these services. In Canada, 84% of the participants in the Canadian Digital Health Survey reported being satisfied with the care received through mental telehealth (Canada Health Infoway, 2021[58]).
The increased use of telehealth for mental health support does, however, have limitations. One relevant concern is data security and how institutions use this information. In Canada, some people opt not to use virtual mental health support because of concerns about security and privacy of personal information (Mental Health Research Canada, n.d.[53]). Another issue is the number of people who can access telehealth services, given that not everyone has access to electronic devices (Fisk, Livingstone and Pit, 2020[59]). Issues including poor Internet connection, lack of digital knowledge and patients’ perceptions of telehealth also affect delivery (Wilczewski et al., 2022[57]).
Countries are increasing economic and legal support for delivery of mental health services through telehealth (OECD, 2021[24]). For example, the United States changed legal regulations and funding so that telehealth is covered by Medicaid and third-party payer reimbursement (Bartels et al., 2020[60]). Australia provided additional funding to improve access to mental telehealth services, and increased the entitlement to reimburse psychological therapies under the Medicare Benefits Scheme (Australian Institute of Health and Welfare, 2022[52]). Canada responded to the OECD Resilience of Health Systems Questionnaire 2022 that it had implemented measures to ensure that practitioners are reimbursed for telehealth.
The disruption to mental health services was not only at the health system level; it was also experienced in schools and workplaces, as highlighted in Section 8.2.1. In response, several countries adopted a multi-sectoral approach to support mental health – a combined effort of different public and private organisations, providing local, regional and/or national support – in line with OECD recommendations of an integrated and multi-sectoral approach (OECD, 2021[24]).
According to the World Health Organization (2020), 65% of countries used multi-sectoral partnerships to address the impact of the pandemic on mental health (WHO, 2020[4]). These partnerships often involved ministries of health, social affairs and education, as well as non-governmental organisations (Hyun et al., 2020[61]). Responses to the OECD Resilience of Health Systems Questionnaire 2022 show, for example, that the Ministry of Health and Welfare of Korea, along with other ministries and 17 provinces, set up a COVID‑19 Depression Consultative Group to discuss the policy direction for mental health support. This Group co‑operates with private societies of psychiatry, social welfare and psychology to provide professional and in-depth psychological support. Australia, Canada and France also used multi-sectoral partnerships to help address the impact of the pandemic on mental health, reaching school students and/or employees (OECD, 2021[24]). Luxembourg provided financial support to encourage children and families to participate in sports clubs in the context of the pandemic (OECD, 2022[62]).
Many OECD countries used new ways to communicate online and delivered new mental health information during the pandemic (OECD, 2021[24]). The OECD Resilience of Health Systems Questionnaire 2022 found that 85% of country respondents (22 of 26) introduced new online information as an emergency mental health support measure. For example, Canada created a new webpage about staying mentally healthy during the pandemic (https://www.canada.ca/en/public-health/services/mental-health-services/mental-health-get-help.html). Germany implemented an information portal called “Mind Your Mental Health” in April 2020 to improve coping mechanisms and share information about mental health services (https://www.zusammengegencorona.de/corona-im-alltag/psychisch-stabil-bleiben/). Other Questionnaire respondents reporting similar initiatives were Australia, Austria, Costa Rica, the Czech Republic, Finland, France, Greece, Ireland, Korea, Latvia, Lithuania, Luxembourg, Mexico, Portugal, Slovenia, Spain, Switzerland, Türkiye, the United Kingdom and the United States.
International agencies including the WHO, the Inter-Agency Standing Committee (IASC) and the European Commission also produced digital guidelines on coping during the COVID‑19 crisis (OECD, 2021[24]). For example, the IASC developed an illustrated book for children about coping during the pandemic (IASC, 2020[63]).
Responses to the OECD Resilience of Health Systems Questionnaire 2022 showed that some countries have taken significant steps to increase funding for mental health. OECD countries, including Australia, Austria, Canada, Chile, Latvia, Lithuania and the United Kingdom, announced new mental health care funding in response to the pandemic (OECD, 2021[24]). For example, the United Kingdom provided an additional GBP 500 million in the financial year 2021/2022 to increase access to mental health support, reduce the waiting time for mental health services and invest in NHS workers. In Lithuania, funding for mental health support helplines was increased by 80%. Austria launched the Healthy Out of the Crisis Project in March 2022 to strengthen the mental health of children and adolescents, with funding of EUR 13 million. In 2020, Australia increased the budget and services for mental health support, allocating more than AUD 1 billion (more than USD 700 million). This budgetary support was maintained in 2021 (Australian Institute of Health and Welfare, 2022[52]). However, this was not the case for most countries. According to the WHO, the increase in mental health support during the first year of the pandemic was not always related to a rise in investment: only 17% of countries reported additional funding to cover additional mental health support (WHO, 2020[4]).
Some countries also offered training in basic psychosocial skills for health workers during the pandemic (WHO, 2020[4]). According to responses to the OECD Resilience of Health Systems Questionnaire 2022, the Portuguese Society for Traumatic Stress Studies offered training in trauma prevention and crisis intervention strategies for frontline staff to promote psychological resilience. There was also an increase in training of mental health workers – for example, Spain increased training for psychiatry by 19% and clinical psychology by 45%.
Among countries responding to a WHO survey, 53% reported collecting data on mental health issues or symptoms in people infected with COVID‑19, and 66% mentioned having ongoing or planned studies on the impact of COVID‑19 on mental health (WHO, 2020[4]).
Most OECD countries collected data on mental health issues. The OECD Resilience of Health Systems Questionnaire 2022 found that 77% of respondents undertook mental health prevalence surveys in 2020‑21. These included national longitudinal surveys and repeated cross-sectional studies with several time‑points to collect up-to-date data on mental health issues, including anxiety and depression symptoms, and psychological distress. Many of these surveys included information about age, sex and gender, occupation and other relevant demographic variables. Additionally, 73% of respondents reported tracking the impact of COVID‑19 on mental health service use and delivery.
The following recommendations are designed to offer a non-exhaustive suite of options for improved mental health support and service delivery within the lens of health system resilience. It is vital that OECD countries continue to examine and share evidence of mental health initiatives that work well (and those that do not), and to analyse the outcomes. These data can be used to inform longer-term reforms that will help to buffer population mental health and mental health service delivery against future crises and systemic disruptions.
Crises reinforce the importance of resilience in population mental health and in mental health service delivery. Historically, mental health has suffered from a lack of resources and attention from governments, called the “treatment gap” – a gap between the mental health needs of populations and the resources available to address these needs (WHO, 2022[64]; OECD, 2021[50]). Worldwide, the treatment gap exceeds 50% (WHO, 2022[64]). Previous work estimated that 63.7% of working age people in OECD countries indicated they have difficulty accessing mental health for financial or geographical reasons, or because of long waiting times (OECD, 2021[50]).
The COVID‑19 pandemic has exacerbated this situation, generating an increase in the prevalence of mental health conditions, unmet needs and disruption of mental health services. The higher burden has fallen heavily on some groups, including (but not limited to) the younger population, women and unemployed people.
Despite countries having taken measures (mental telehealth, increased investment, improved information access and so on), mental health is now an even larger public health concern. Mental health in 2022 has not reduced to levels seen before the pandemic (OECD/European Union, 2022[8]). This suggests that mental health support and the scale‑up of mental health services during the pandemic’s recovery stage, while commendable, remain insufficient to cover growing needs, including for people whose mental health is affected by long COVID (CHNP, 2021[65]). The situation requires concerted efforts by countries and other stakeholders to embed and implement long-term reforms and improvements to population mental health and mental health support.
Including mental health in crisis planning will help to build more resilient health systems. This involves addressing mental health needs in planning, absorbing and recovering from crises, and ensuring that systems learn so that they adapt in the future.
According to responses to the OECD Resilience of Health Systems Questionnaire 2022, 77% of countries included, or planned to include, mental health considerations in routine crisis preparedness and planning. Countries gave different examples of how mental health is considered in crisis planning, including integration into general health system planning and independent action. For example, Australia developed a specific National Mental Health and Well-being Pandemic Response Plan in May 2020. On the other hand, Austria included mental health in the country’s overall health plan for pandemics. Similarly, Slovenia developed an action plan to provide psychological assistance in epidemic or pandemic situations in October 2020, which forms part of the National Plan for Protection and Rescue in the Outbreak of Human Infectious Diseases or Pandemics.
Improving health system resilience requires an appreciation of the interconnectivity between systems and services, including mental health services. Mental health cannot be separated from broader systems, given that it is affected not only by individual factors but also by socio‑economic determinants (WHO, 2014[1]). One example is the relationship between mental health and employment presented in Fitter Minds, Fitter Jobs (OECD, 2021[37]), which recommends integrating health (and mental health), education and employment services to strengthen the positive impact of mental health policies. Therefore, to avoid potential cascading failure, it is critical that mental health crisis planning appreciates the connectivity with other systems and services.
When including mental health in crisis planning, countries should have mechanisms to understand the impact of public policies on mental health in a crisis – such as containment or public health policies, limits on movement, school closures and measures that have economic impacts – and the potential to adapt policies in the light of mental health concerns. Plans should consider potential disruptions to mental health services and the implication of such disruptions. For example, if countries need to use mental health beds or staff for other health services during a crisis, they should implement measures to address this challenge. Disruption of systems might be unavoidable, but it is relevant to consider how this can affect people’s mental health, especially among vulnerable groups and more severely ill patients.
Decision making during crises can be difficult. Countries should be able to understand when there is a need to protect the general population’s mental health and/or the mental health of specific groups. Valuable real-time data inform good decisions in this challenging context. Having high-quality mental health data on the prevalence of mental health symptoms or issues and information about mental health service disruption should help policy makers to understand:
people’s needs, and the groups affected unequally by the crisis
how mental health services can still be delivered during and in response to the crisis
the capacity of countries to provide immediate responses during the crisis.
Being able to quantify the resilience of mental health services is helpful during a crisis. It will aid decision making, including any necessary trade‑offs between systemic efficiency and resilience. Australia is an example of an OECD country that focused on mental health planning to respond to disasters (Box 8.5).
Australia was one of the first countries in the world to recognise the mental health impacts of the pandemic and to develop a specific National Mental Health and Well-being Pandemic Response Plan, announced on 15 May 2020. In addition to the COVID‑19 pandemic, droughts, cyclones, floods and bushfires are among the many crises Australia has experienced in recent decades. The National Mental Health Commission is leading the development of a national framework to guide a co‑ordinated approach to psychosocial and mental health issues in the context of disasters (Australian Goverment, 2022[66]). This will aim to improve how state governments work together to respond to and support people’s mental health before, during and after disasters.
Having timely available data on mental health is crucial to identifying needs and allocating funding for mental health support (OECD, 2021[50]). OECD countries made valuable efforts to continue collecting data and tracking the mental health status of the population during the pandemic. It is important to retain this momentum to improve the information systems for mental health and to integrate mental health into routinely collected data, subject to appropriate privacy and other safeguards.
Different types of information on mental health can be collected. However, countries need to collect data that leads to implementation of interventions and policies that will tackle mental health issues and needs at a population level. Data on prevalence of mental health conditions and disruption of mental health services are crucial because countries need to understand their population’s mental health situation. In the context of the COVID‑19 pandemic, it has been recommended (Kestilä et al., 2022[34]) that governments should be able to assess:
the extent to which mental strain is alleviated by the removal of restrictions on everyday life and the reduction of COVID‑19 infections
which mental health symptoms remain more persistent, requiring treatment and rehabilitation
the most effective ways to combat the adverse mental health effects of the pandemic.
Screening for symptoms is accessible and inexpensive; compared to the use of diagnostic tools, it can be self-assessed and undertaken more frequently (Regier et al., 1998[67]; Schmitz et al., 1999[68]). It is recommended, however, that countries also assess the prevalence of mental health conditions through diagnostic tools. This is usually done with less frequency because it needs to be undertaken by a mental health professional (so it requires more time and resources), but it delivers high-quality data to inform policies and interventions. While use of diagnostic/screening tools to assess the prevalence of depression and anxiety is more common, it may be worthwhile to consider post-traumatic stress disorder prevalence, given the accumulative effect of stressors (Fernandez et al., 2020[16]; Podubinski and Glenister, 2021[22]). Maintaining surveillance of mental health conditions requires collaboration among institutions in the health sector – whether data are collected routinely in mental health services or through national health or mental health surveys.
Additionally, countries should track disruption to mental health services. During a crisis or large‑scale shock, it is helpful to track the services that have been interrupted and evaluate the need to offer alternatives. It is recommended that countries should also monitor the number of people using mental health services (for example, via admission and discharge numbers) outside crisis periods to assess potential disruptions in access to and use of services.
Countries should also collect data on socio-demographic variables to identify possible vulnerable groups in the population. These could include age, sex, gender identity, socio‑economic status, employment status, ethnicity, and migration background. This information will help policy makers to identify groups at higher risk of having mental health issues who are not accessing mental health services. Identifying risk factors from the data will also help to inform future mental health protections and address potential inequalities in mental health.
Independently of the type of data countries decide to collect and analyse, they should use the same tool consistently. Having one screening/diagnostic tool facilitates comparison of different time periods and observation of changes in trends, which are especially useful for understanding the impact of crises. The tools must be validated for the national context. Examples of good screening tools are Patient Health Questionnaire‑9 (PHQ‑9) to assess depressive symptoms and General Anxiety Disorder‑7 for anxiety symptoms (Box 8.1). PHQ‑9 is considered one of the most reliable screening tools for depressive symptoms and depression. It has been used across many different countries and settings (Costantini et al., 2021[69]).
The frequency of data collection can be monthly or even weekly, depending on the stage of a shock. It would, however, be useful to track the data in all stages of a shock and afterwards, to have comparison points and to understand how mental health is affected over time. This will help policy makers to understand the short and longer-term impacts of a shock better, and thus to design and implement more effective policy responses.
Reducing vulnerabilities in the population will reduce demand on the health system during crises and systemic disruption. To strengthen mental health, countries should implement measures aimed at both populations and individuals to promote well-being and to prevent mental health issues from arising.
Governments should implement strategies to increase the capacity of individuals and populations to protect their mental health as much as possible before future crises. In this sense, engaging early with people with vulnerabilities is pivotal to addressing the individual barriers and stigma around mental health during all stages of the disruption cycle. Additionally, countries should implement population-scale public mental health interventions. These types of measures not only improve mental health and well-being but also lead to economic savings in the short- and long-term (Campion and Knapp, 2018[70]). Reducing the vulnerability of populations prior to a crisis will reduce the demand during a crisis. This action during the prepare stage of the disruption cycle will limit the impact of the disruption during the absorb stage and speed up recovery.
The focus of mental health should be on the whole population, including vulnerable groups. This includes groups that have historically been in vulnerable situations for mental health issues (such as women and unemployed people) but also “new” groups that arise from specific crises – for example, in the context of the pandemic, the younger population and those with long-COVID. Having timely and high-quality data on mental health helps policy makers to identify high-risk groups. Without this information, mitigation strategies cannot be implemented effectively.
It is also necessary to improve access to and use of mental health services, especially for vulnerable populations. While mental health service use increased as the COVID‑19 pandemic continued, access to services was not equal for all groups. People with higher prevalence of mental health conditions also presented with higher unmet needs; therefore, they were unable to access or use the mental health services they needed, worsening their situation. Countries should consider hard-to-reach populations (for example, migrants, asylum seekers, people who are homeless and indigenous people) and geographical areas (such as remote and rural areas, islands etc.).
Countries should also continue to offer alternatives to in-person consultations. Offering mental health support through different mediums and at different times (especially outside business hours) is essential to improve access to and use of such services (Stocker et al., 2021[44]). It is recommended that countries consider training in mental telehealth for future crises, as well as improve the quality of mental health care in non-crisis times (Wilczewski et al., 2022[57]).
Mental health services are only part of what countries need to consider when addressing the lingering impact of the pandemic on people’s mental health (Kestilä et al., 2022[34]). An inter-disciplinary and inter-system approach is relevant for designing mental health public policies, and this will help to address inequalities in mental health (WHO, 2014[1]; Lund et al., 2018[2]). A whole‑of-society approach is required.
Countries should continue to implement measures to move beyond hospital-based mental health care and incorporate and/or strengthen mental health in primary health care. In some cases, mitigating disruptions to employment, schooling, sporting and community activities will also improve people’s mental health (OECD, 2021[24]). For example, an Australian study found that measures to promote employment, invest in childcare and expand mental telehealth services were among the most effective in addressing the negative impact of the COVID‑19 pandemic on mental health (Occhipinti et al., 2020[71]). The OECD has also found that measures to protect jobs play an essential role in mitigating the pandemic’s impact on mental health (OECD, 2021[24]).
The decline in people’s mental health seen in the COVID‑19 pandemic is not immutable. The adaptions suggested in this chapter are designed to improve the resilience of health systems by strengthening mental health prior to and during crises.
[40] Adams-Prassl, A. et al. (2020), The Impact of the Coronavirus Lockdown on Mental Health: Evidence from the US, https://doi.org/10.17863/CAM.57997.
[18] Andrades, M., F. García and R. Kilmer (2021), “Post‐traumatic stress symptoms and post‐traumatic growth in children and adolescents 12 months and 24 months after the earthquake and tsunamis in Chile in 2010: A longitudinal study”, International Journal of Psychology, Vol. 56/1, pp. 48-55, https://doi.org/10.1002/ijop.12718.
[66] Australian Goverment (2022), National COVID and Disaster Response, National Mental Health Comission, https://www.mentalhealthcommission.gov.au/projects/national-disaster-response (accessed on 25 July 2022).
[52] Australian Institute of Health and Welfare (2022), Mental health impact of COVID-19, https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/covid-19-impact-on-mental-health (accessed on 3 June 2022).
[11] Barr, B. et al. (2012), “Suicides associated with the 2008-10 economic recession in England: time trend analysis”, BMJ, Vol. 345/aug13 2, pp. e5142-e5142, https://doi.org/10.1136/bmj.e5142.
[60] Bartels, S. et al. (2020), “COVID-19 Emergency Reforms in Massachusetts to Support Behavioral Health Care and Reduce Mortality of People With Serious Mental Illness”, Psychiatric Services, Vol. 71/10, pp. 1078-1081, https://doi.org/10.1176/appi.ps.202000244.
[55] Bean, C. et al. (2022), “A comparison of telehealth versus in‐person group therapy: Results from a DBT‐based dual diagnosis IOP”, Journal of Clinical Psychology, https://doi.org/10.1002/jclp.23374.
[70] Campion, J. and M. Knapp (2018), “The economic case for improved coverage of public mental health interventions”, The Lancet Psychiatry, Vol. 5/2, pp. 103-105, https://doi.org/10.1016/S2215-0366(17)30433-9.
[58] Canada Health Infoway (2021), Canadian Digital Health Survey 2021: What Canadians Think, https://www.infoway-inforoute.ca/en/component/edocman/4011-canadian-digital-health-survey-2021-what-canadians-think/view-document (accessed on 15 December 2022).
[45] Carpiniello, B. et al. (2020), “Mental health services in Italy during the COVID-19 pandemic”, Psychiatry and Clinical Neurosciences, Vol. 74/8, pp. 442-443, https://doi.org/10.1111/pcn.13082.
[30] CDC (2022), Household Pulse Survey - Anxiety and Depression, Centers for Disease Control and Prevention, https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm (accessed on 23 June 2022).
[65] CHNP (2021), Nehmen Sie an unserer internationalen Psy-Long-COVID Studie teil, https://www.chnp.lu/blog/2021/09/24/participez-a-notre-etude-internationale-psy-long-covid/?lang=de (accessed on 7 February 2023).
[69] Costantini, L. et al. (2021), Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): A systematic review, Elsevier B.V., https://doi.org/10.1016/j.jad.2020.09.131.
[15] Díaz, C., G. Quintana and E. Vogel (2012), “Síntomas de depresión, ansiedad y estrés post-traumático en adolescentes siete meses después del terremoto del 27 de febrero de 2010 en Chile”, Terapia psicológica, Vol. 30/1, pp. 37-43, https://doi.org/10.4067/S0718-48082012000100004.
[17] Dutta, A. et al. (2022), “Earthquake exposure, adverse childhood experiences, and psychosocial functioning in Chilean children: A longitudinal study”, Journal of Traumatic Stress, https://doi.org/10.1002/jts.22826.
[39] Fancourt, D., A. Steptoe and F. Bu (2021), “Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study”, The Lancet Psychiatry, Vol. 8/2, pp. 141-149, https://doi.org/10.1016/S2215-0366(20)30482-X.
[56] Feijt, M. et al. (2020), “Mental Health Care Goes Online: Practitioners’ Experiences of Providing Mental Health Care During the COVID-19 Pandemic”, Cyberpsychology, Behavior, and Social Networking, Vol. 23/12, pp. 860-864, https://doi.org/10.1089/cyber.2020.0370.
[16] Fernandez, C. et al. (2020), “Assessing the relationship between psychosocial stressors and psychiatric resilience among Chilean disaster survivors”, The British Journal of Psychiatry, Vol. 217/5, pp. 630-637, https://doi.org/10.1192/bjp.2020.88.
[59] Fisk, M., A. Livingstone and S. Pit (2020), “Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States”, Journal of Medical Internet Research, Vol. 22/6, p. e19264, https://doi.org/10.2196/19264.
[42] Fukase, Y. et al. (2021), “Depression, risk factors, and coping strategies in the context of social dislocations resulting from the second wave of COVID-19 in Japan”, BMC Psychiatry, Vol. 21/1, p. 33, https://doi.org/10.1186/s12888-021-03047-y.
[28] Höglinger, M. et al. (n.d.), COVID-19 Social Monitor, https://covid19.ctu.unibe.ch/ (accessed on 12 April 2022).
[36] Huang, L. et al. (2022), “Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study”, The Lancet Respiratory Medicine, https://doi.org/10.1016/S2213-2600(22)00126-6.
[61] Hyun, J. et al. (2020), “Psychosocial Support during the COVID-19 Outbreak in Korea: Activities of Multidisciplinary Mental Health Professionals”, Journal of Korean Medical Science, Vol. 35/22, https://doi.org/10.3346/jkms.2020.35.e211.
[63] IASC (2020), My Hero is You, Storybook for Children on COVID-19, Inter-Agency Standing Committee Reference Group on Mental Health and Psychosocial Support in Emergency Settings (IASC MHPSS RG), https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/my-hero-you-storybook-children-covid-19 (accessed on 18 May 2022).
[23] Isaac, F. et al. (2021), “A Systematic Review of the Impact of Wildfires on Sleep Disturbances”, International Journal of Environmental Research and Public Health, Vol. 18/19, p. 10152, https://doi.org/10.3390/ijerph181910152.
[33] Jenkins, E. et al. (2021), “A portrait of the early and differential mental health impacts of the COVID-19 pandemic in Canada: Findings from the first wave of a nationally representative cross-sectional survey”, Preventive Medicine, Vol. 145, p. 106333, https://doi.org/10.1016/j.ypmed.2020.106333.
[49] Johnson, S. et al. (2021), “Impact on mental health care and on mental health service users of the COVID-19 pandemic: a mixed methods survey of UK mental health care staff”, Social Psychiatry and Psychiatric Epidemiology, Vol. 56/1, pp. 25-37, https://doi.org/10.1007/s00127-020-01927-4.
[10] Kentikelenis, A. et al. (2011), “Health effects of financial crisis: omens of a Greek tragedy”, The Lancet, Vol. 378, pp. 1457-1458, https://doi.org/10.1016/S0140.
[34] Kestilä, L. et al. (2022), Covid-19-epidemian vaikutukset hyvinvointiin, palvelujärjestelmään ja kansantalouteen, Terveyden ja hyvinvoinnin laitos, https://www.julkari.fi/bitstream/handle/10024/144268/THL_Rap4_2022_Covid-seuranta_kevat_2022_web.pdf?sequence=4&isAllowed=y (accessed on 23 March 2022).
[14] Leiva-Bianchi, M. (2011), “Relevancia y prevalencia del estrés post-traumático post-terremoto como problema de salud pública en Constitución, Chile”, Rev. salud pública, Vol. 12/4, pp. 551-559.
[2] Lund, C. et al. (2018), Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews, Elsevier Ltd, https://doi.org/10.1016/S2215-0366(18)30060-9.
[46] Mansfield, K. et al. (2021), “Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study”, The Lancet Digital Health, Vol. 3/4, pp. e217-e230, https://doi.org/10.1016/S2589-7500(21)00017-0.
[25] Mathieu, E. et al. (2020), Coronavirus Pandemic (COVID-19), https://ourworldindata.org/coronavirus (accessed on 18 January 2023).
[5] McBrien, J., A. Rutigliano and A. Sticca (2022), “The Inclusion of LGBTQI+ students across education systems: An overview”, OECD Education Working Papers, No. 273, OECD Publishing, Paris, https://doi.org/10.1787/91775206-en.
[6] Mental Health Research Canada (2022), Mental Health in Crisis: How COVID-19 Is Impacting Canadians (Poll 12), https://www.mhrc.ca/findings-of-poll-12 (accessed on 30 March 2022).
[53] Mental Health Research Canada (n.d.), A Summary of Canadian’s Access to Mental Health Care Pre and Post COVID-19, https://static1.squarespace.com/static/5f31a311d93d0f2e28aaf04a/t/615db4a2708dfa7b91f226bd/1633531043202/A+Summary+of+Canadian%27s+Acces+to+Care+Pre-+and+Post+COVID+19.pdf (accessed on 14 December 2022).
[31] Mukaka, M. (2012), “Statistics Corner: A guide to appropriate use of correlation coefficient in medical research”, Malawi Medical Journal, Vol. 24/3, pp. 69-71, http://www.mmj.medcol.mw.
[54] NHS digital (2021), Mental health services referrals and care contacts for children and young people aged 0 to 18, https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/mental-health-data-hub/dashboards/mental-health-services-monthly-statistics#mental-health-services-referrals-and-care-contacts-for-children-and-young-people-aged-0-to-18 (accessed on 12 April 2022).
[71] Occhipinti, J. et al. (2020), “Mental health: build predictive models to steer policy”, Frontiers in Psychiatry, Vol. 11, https://doi.org/10.3389/fpsyt.2022.815904.
[35] Ocsovszky, Z. et al. (2022), “The associations of long-COVID symptoms, clinical characteristics and affective psychological constructs in a non-hospitalized cohort”, Physiology International, https://doi.org/10.1556/2060.2022.00030.
[62] OECD (2022), Evaluation of Luxembourg’s COVID-19 Response, OECD Publishing, Paris, https://doi.org/10.1787/2c78c89f-en.
[50] OECD (2021), A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill-Health, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/4ed890f6-en.
[7] OECD (2021), COVID-19 and Well-being: Life in the Pandemic, OECD Publishing, Paris, https://doi.org/10.1787/1e1ecb53-en.
[37] OECD (2021), Fitter Minds, Fitter Jobs: From Awareness to Change in Integrated Mental Health, Skills and Work Policies, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/a0815d0f-en.
[9] OECD (2021), Supporting young people’s mental health through the COVID-19 crisis, OECD, Paris, https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquete-pour-suivre-.
[24] OECD (2021), “Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/0ccafa0b-en.
[8] OECD/European Union (2022), Health at a Glance: Europe 2022: State of Health in the EU Cycle, OECD Publishing, Paris, https://doi.org/10.1787/507433b0-en.
[48] Pignon, B. et al. (2020), “Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID‐19 in Paris and suburbs”, Psychiatry and Clinical Neurosciences, Vol. 74/10, pp. 557-559, https://doi.org/10.1111/pcn.13104.
[22] Podubinski, T. and K. Glenister (2021), “The Pandemic Is Not Occurring in a Vacuum: The Impact of COVID-19 and Other Disasters on Workforce Mental Health in Australia”, Disaster Medicine and Public Health Preparedness, pp. 1-7, https://doi.org/10.1017/dmp.2021.238.
[41] Racine, N. et al. (2021), “Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19”, JAMA Pediatrics, Vol. 175/11, p. 1142, https://doi.org/10.1001/jamapediatrics.2021.2482.
[12] Reeves, A. et al. (2012), “Increase in state suicide rates in the USA during economic recession”, The Lancet, Vol. 380/9856, pp. 1813-1814, https://doi.org/10.1016/S0140-6736(12)61910-2.
[67] Regier, D. et al. (1998), “Limitations of Diagnostic Criteria and Assessment Instruments for Mental Disorders Implications for Research and Policy”, Archives of General Psychiatry (JAMA Psychiatry), Vol. 55, pp. 109-115, http://www.ama-assn.org/psych.
[21] Rodney, R. et al. (2021), “Physical and Mental Health Effects of Bushfire and Smoke in the Australian Capital Territory 2019–20”, Frontiers in Public Health, Vol. 9, https://doi.org/10.3389/fpubh.2021.682402.
[27] Santé publique France (2022), CoviPrev: une enquête pour suivre l’évolution des comportements et de la santé mentale pendant l’épidémie de COVID-19, https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-covid-19 (accessed on 22 March 2022).
[68] Schmitz, N. et al. (1999), “Diagnosing mental disorders in primary care: the General Health Questionnaire (GHQ) and the Symptom Check List (SCL-90-R) as screening instruments”, Social Psychiatry and Psychiatric Epidemiology, Vol. 34, pp. 360-366.
[38] Smith, N., I. Taylor and V. Kolbas (2020), Exploring the relationship between economic security, furlough and mental distress, NatCen Social Research, https://dera.ioe.ac.uk/38381/1/Exploring-the-relationship-between-economic-security-furlough-and-mental-distress.pdf (accessed on 17 June 2022).
[47] Stein, H. et al. (2020), “Pre/post comparison study of emergency mental health visits during the COVID‐19 lockdown in Lombardy, Italy”, Psychiatry and Clinical Neurosciences, Vol. 74/11, pp. 605-607, https://doi.org/10.1111/pcn.13126.
[44] Stocker, D. et al. (2021), Der Einfluss der COVID-19-Pandemie auf die psychische Gesund-heit der Schweizer Bevölkerung und die psychiatrisch-psychothera-peutische Versorgung in der Schweiz, Bundesamt für Gesundheit, Bern.
[13] Stuckler, D. et al. (2011), “Effects of the 2008 recession on health: a a first look at European data”, The Lancet, Vol. 378, pp. 124-125, https://doi.org/10.1016/S0140-6736(11)61079-9.
[26] Superior Health Council of Belgium (n.d.), Belgium COVID-19 Epidemiological Situation - Mental Health Studies, https://datastudio.google.com/embed/reporting/7e11980c-3350-4ee3-8291-3065cc4e90c2/page/ykUGC (accessed on 4 April 2022).
[43] Terveyden ja hyvinvoinnin laitos (2022), Access to specialised medical care - Mental health services for children and adolescents, https://sampo.thl.fi/pivot/prod/fi/eshjono/psyk2/summary_psykiatria?aika_0=51052&paltu_0=516079&paltu_1=&eala_0=527878&mittarit_0=18684 (accessed on 30 March 2022).
[29] UCL (2022), COVID-19 Social Study Reports (Report Week 94), https://www.covidsocialstudy.org/results (accessed on 4 April 2022).
[19] Vitriol G, V. et al. (2013), “Terremoto en Chile: estrés agudo y estrés post-traumático en mujeres en tratamiento por depresión grave”, Revista médica de Chile, Vol. 141/3, pp. 338-344, https://doi.org/10.4067/S0034-98872013000300009.
[20] Vitriol, V. et al. (2014), “Respuesta de los centros de atención primaria en salud mental después del terremoto y tsunami del 2010 en la Región del Maule”, Revista médica de Chile, Vol. 142/9, pp. 1120-1127, https://doi.org/10.4067/S0034-98872014000900005.
[32] WHO (2022), Mental Health and COVID-19: Early evidence of the pandemic’s impact, World Health Organization, https://apps.who.int/iris/handle/10665/352189.
[64] WHO (2022), Mental health gap action programme (mhGAP), World Health Organization, http://www.emro.who.int/mnh/mental-health-gap-action-programme/index.html (accessed on 11 July 2022).
[3] WHO (2022), Mental health in emergencies, https://www.who.int/news-room/fact-sheets/detail/mental-health-in-emergencies (accessed on 31 May 2022).
[51] WHO (2021), Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic, World Health Organization, https://apps.who.int/iris/handle/10665/340937.
[4] WHO (2020), The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment, World Health Organization, https://apps.who.int/iris/handle/10665/335838.
[1] WHO (2014), Social determinants of mental health, World Health Organization, https://apps.who.int/iris/handle/10665/112828.
[57] Wilczewski, H. et al. (2022), “Perceptions of Telemental Health Care Delivery During COVID-19: A Cross-Sectional Study With Providers, February-March 2021”, Frontiers in Psychiatry, Vol. 13, https://doi.org/10.3389/fpsyt.2022.855138.