Rishub Keelara
Philip Haywood

Rishub Keelara
Philip Haywood
This chapter discusses the digital and data context in which OECD countries entered the COVID‑19 pandemic and their responses, common challenges and lessons learnt. The pandemic accelerated the digitisation of health systems. Improvements in data, data governance, analytics, and digital foundations were required to manage health systems effectively in response to the pandemic. OECD countries improved data reporting and almost all enhanced data timeliness. The chapter outlines how increasing the availability of integrated digital information, underpinned by appropriate governance frameworks, would strengthen health system resilience. Beyond building resilience to address future shocks, improving the use of health data and its governance would aid the functioning of health systems between crises.
Modern health systems are built around data and information. These are required during crises, such as the COVID‑19 pandemic, and to ensure that health systems are sustainable, effective and efficient over the longer term.
Prior to the COVID‑19 pandemic, less than two‑thirds of OECD countries (13 of 22) responding to the 2019‑20 OECD survey of National Health Data Infrastructure and Governance could link data across multiple health care settings. Half of 22 responding OECD countries had data from any key national dataset available within a week of record creation. Only four OECD countries had data available from five or more key national datasets within a week of record creation.
These data deficits limited early absorption of the impacts of the pandemic. Information was needed at multiple levels across the health system. Countries that lacked basic timely data – on hospitalisations, health care workforce, resources and mortality – risked unintended consequences. Not having sufficient information on vulnerable and marginalised groups was also a weakness. For example, poor data measurement and evaluation in long-term care facilities hampered the early response to COVID‑19.
The pandemic accelerated health digitalisation. All countries responding to the OECD Health Data and Governance Changes during the COVID-19 Pandemic Questionnaire 2021 reported improved data reporting and almost all (over 90%) enhanced the timeliness of data. These positive changes facilitated the effective use of resources (for example, supporting co‑ordination of intensive care capacity), improved mitigation efforts (for example, through vaccine passports) and protected the public and health care workers (for example, through use of telehealth). Information was used beyond the health system to improve containment and mitigation efforts (for example, daily updates of dashboards were commonly used to communicate with the public). International co‑operation and data sharing increased (for example, clinical trials were conducted across national boundaries).
While OECD countries have sought to mitigate data deficits, countries need to build further on the gains made to deliver an information-rich future:
In 2022, most countries still could not link important markers of vulnerability to health outcomes, benefits and harms.
Resources and training are required to improve the use of information across health systems, fortifying the evidence base for appropriate action.
Health data governance frameworks need to preserve trust of populations in how their health data is collected, stored, and used (for example, for contact tracing and vaccine certificates). Preserving trust is vital to responding effectively to large‑scale crises.
Increasing the reliance of health systems on digitalisation also brings risks that need to be mitigated. In 2022, cyber threats and disasters restricted access to digital information in health systems. Furthermore, the benefits of digitalisation may not be spread across the population, entrenching inequality.
Health system resilience would benefit from high-quality timely data, facilitating a speedier and more agile response to shocks. Data from outside the health system will need to be linked to health system data for whole‑of-society responses. For example, health data may need to be combined with meteorological data to identify early and mitigate future heat waves.
Updating governance frameworks, ensuring interoperability and enhancing the use of existing data are important to building more resilience into health systems. Policies should both foster the development of data and artificial intelligence‑driven tools and sharing of these innovations equitably across the health system.
Health systems continue to be built around data and information in the 21st century. An integrated health information system enables secure exchange and movement of data used to create information and knowledge that advance health systems and broader policy objectives. Integrated health information systems require strong data infrastructure, comprising the assets, technology, agencies and institutions needed to collect, store, maintain, distribute and (re)use data by different end users (OECD, 2022[1]).
An integrated health information system helps countries improve their capacity to get the best performance and value out of their health systems between and during crises in three ways. First, it improves care quality (including safety, effectiveness and efficiency). Second, it improves patient empowerment by enabling people to access their own health information, and for this information to “follow the patient” wherever they seek care in the health system. Finally, it increases the capacity to use health and other data for important secondary purposes, such as informing continuous assessment of health system performance and facilitating learning, from the national level to the clinician’s office. Integrated health information systems enable more effective and efficient:
public health monitoring and surveillance
resource allocation and reimbursement to reward value
biomedical research and development
innovation, such as big data analytics and artificial intelligence (AI) to enhance knowledge‑based decisions for patient care and health system governance.
These features make health systems more sustainable as well as more resilient (OECD, 2022[1]). Improved information facilitates improvements in care, which in turn reduce demand on the health care system in times of crisis.
This chapter is divided into five sections. Section 12.1 reviews the crucial role of data and information in shaping modern and robust health systems. Section 12.2 discusses the situation within OECD countries prior to the COVID‑19 pandemic. Sections 12.3 and 12.4 outline some of the policies and interventions undertaken within the absorb stage of the pandemic, and some of the adaptations that countries have implemented since or intend to implement. The final section concludes with considerations relevant to building the data and digital foundation of health systems, and how this would improve the resilience of these systems. Box 12.1 outlines some of the common terms and definitions used in this chapter.
It is necessary to distinguish between data and information. Data are raw figures and facts and – in and of themselves – may not be very valuable. Information, on the other hand, is meaning and insights obtained from analysis of data. An information system includes the capacity to convert data into usable information and knowledge. An integrated information system has the capacity to move information around the system to those who require it, supporting decision making.
A useful analogy is an integrated transportation network, which allows passengers to move safely and securely across boundaries within a country, using various transport types. While the physical and technical infrastructure is essential, this system also requires people and institutions to operate it effectively, efficiently, safely and predictably (OECD, 2022[1]).
Data can also be public goods (see the chapter on global public goods) because their use by one actor does not prevent their use by others (i.e. they are non-rival). As multiple actors in the health system (and potentially beyond) can generate valuable information from data, gaps in data and fragmentation limit their potential as a public good. Therefore, investment is required to maximise the usefulness and provision of data (see the chapter on investing in resilience).
Health systems may contain many different types of data and data collections. Digitised information about patients – including electronic health records (EHRs) and electronic medical records (EMRs) – was particularly relevant during the COVID‑19 pandemic (Oderkirk et al., forthcoming[2]).
This chapter uses the following definitions:
Digitalisation is the use of digital technologies and data, as well as the interconnection, that results in new activities, or in changes or adaptation to existing activities.
An EHR refers to the longitudinal electronic record of an individual patient that contains or virtually links records together from multiple EMRs, which can be shared across health care settings (making it interoperable). It aims to contain a history of contact with the health care system for individual patients from multiple organisations that deliver care.
An EMR refers to a computerised medical record created in an organisation that delivers care, such as a hospital or physician’s office, for a patient of that organisation. EMRs are provider- or organisation-centric, and allow storage, retrieval and modification of patient records.
Health data comprise individual personal health and other individual level data. They also include data related to the administration and running of health care and the health system, including operational and financial data.
Interoperability is the ability of two or more systems to exchange information and to make use of exchanged information. It is an essential pre‑condition to developing EHRs from EMRs.
The response to a shock comprises four stages (see the chapter on key findings and recommendations). These stages are prepare, absorb, recover and adapt. Prepare includes the steps taken to prepare critical functions to avoid and mitigate shocks. This occurs prior to the disruption. Absorb occurs after the shock commences, comprising the capability of the health system to maintain core functions and absorb the consequences without collapse. Thus, limiting the extent of the disruption and minimising the morbidity and mortality impact. Recover involves regaining the disrupted functions as quickly and efficiently as possible. Adapt is the capacity of the health system to “learn” and improve its capacity to absorb and recover from shocks, reducing the impact of similar threats in the future.
Responding to large, fast-moving shocks requires accurate and current information that gives all users the best chance of pursuing action that maximises the functioning of the health system and minimises harm. Such harm can arise from the shock itself, or from the direct and indirect effects of the policies used to respond to it. The COVID‑19 pandemic demonstrated these requirements.
In the context of the pandemic, decision makers at institutional, regional and national levels required integration of diverse data collections to provide real-time information to inform their assessments and co‑ordinate the health system and actions beyond the system. The impact of the pandemic spread well beyond the health system, with the burden falling heavily on the social care and long-term care sectors (see the chapter on long-term care).
At the individual patient and provider levels, availability of information that follows the patient was useful, given the pandemic’s widespread disruption of health care – including rapid changes in how and where health care was provided, and by whom. To target care to those who need it most, information about such needs must be provided to the health system (see the chapter on care continuity). This was a requirement not only in absorbing the pandemic but also in recovering from it, including to address delayed and deferred care (see the chapter on waiting times).
Novel pathogens like SARS‑CoV‑2 or new threats require knowledge to be generated about vulnerabilities, effective treatments and outcomes. This process is aided by data moving to those who can analyse them to produce information. Integrated data were also critical to the public health response to the pandemic: surveillance of infections and early detection were crucial to limiting spread during the pandemic’s absorb stage (see the chapter on containment and mitigation). Later in the pandemic, the ability to gather information from multiple sources contributed to monitoring implementation of policies, their unintended consequences and relative effectiveness in driving recovery.
These issues exist for all shocks: early detection of problems can lead to policy interventions that limit and better absorb disruptions, foster a quicker and less burdensome recovery, and promote adaptability to address future shocks. Surveillance can ensure appropriate deployment of resources and excess capacity to mitigate against cascading failure.
For this to occur, information needs to be timely, comprehensive, appropriate, interpretable and tied to responsibilities for decision making. The response to large shocks, like the pandemic, can involve transformation of the health system (e.g. the move to telehealth), new collaborations (e.g. integration of private and public critical care facilities) and learning feedback loops to address novel and new situations. It is important that data infrastructure facilitates these activities and is not a barrier to using data when needed. The ability to have the information on which to base a decision is fundamental to a resilient health system (Hanefeld et al., 2018[3]).
Just months before the start of the COVID‑19 pandemic, the OECD released a flagship report entitled Health in the 21st Century (2019[4]). This assessed the state of digitalisation in the health sector and the opportunities to bring health systems into the 21st century. The main finding of this work was that, in most cases, the health sector in OECD countries remained “data rich but information poor”. The report noted that, despite some promising indications and successes, the health sector was lagging behind other sectors and had yet to harness the full potential of digital opportunities. To gain the benefits of these opportunities, data need to be available, and an appropriate governance structure needs to be in place.
The COVID‑19 pandemic highlighted this lag. In many OECD countries, key national health data were kept in silos, fragmented, unstandardised and inaccessible, with a wide range of distinct governance frameworks for sharing and implementing data insights. The decentralisation of data was an impediment to quick and co‑ordinated responses to the pandemic.
According to the 2019‑20 OECD survey of National Health Data Infrastructure and Governance, prior to the pandemic only 13 of 22 responding OECD countries were able to link data across multiple settings within health care (Figure 12.1), and few had real-time data available for some data collections (Oderkirk, 2021[5]). Differences in data linkage capability between countries also grew over time. The survey results suggest that between 2013 and 2020, half of all responding countries (i.e. 22 OECD countries and Singapore) reported improvements in dataset availability, maturity and use, while half reported a drop in capability.
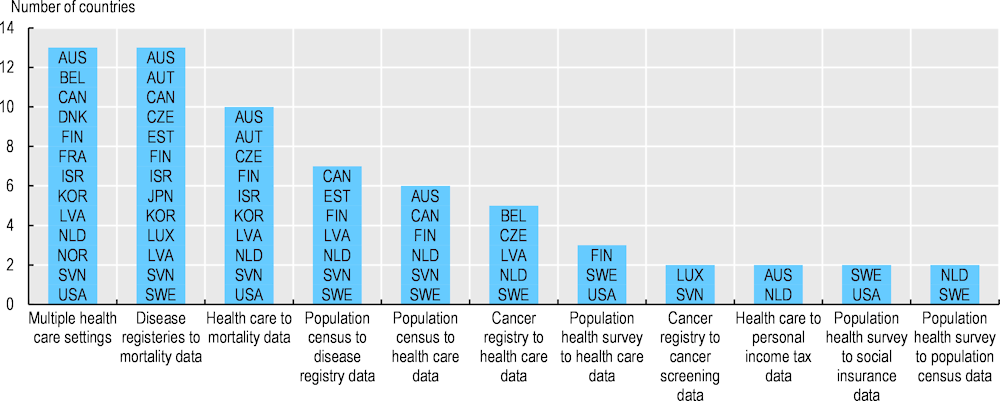
Source: Adapted from Oderkirk (2021[5]), “Survey results: National health data infrastructure and governance”, https://doi.org/10.1787/55d24b5d-en.
Few responding OECD countries had real-time data availability before the pandemic. Half (11 of 22) of responding OECD countries had data from any of 13 key national datasets available within a week of record creation. Only four OECD countries had data available from 5 or more of the 13 key national datasets within a week of record creation.
Multiple challenges were experienced when developing national health datasets. These included limitations in data quality (e.g. in content, gaps in population coverage, lack of unique patient identifiers, exclusion of non-reimbursed services, data coding problems, lack of digitisation and lack of timeliness), challenges in policies and data governance, high costs of data access, lack of resources and barriers to linkages and sharing within countries. Two-thirds of OECD countries (14 of 22) responding to the survey reported concerns about the quality of national data that limited their usefulness (Oderkirk, 2021[5]).
Fragmentation of data and information make it more difficult to integrate care around patients. Without systematic data linkages at the individual patient level, health systems lack the ability to monitor poor performance (Barrenho et al., 2022[6]). In 2019, data from the Commonwealth Fund survey of primary care physicians showed that hospitals failed to notify primary health care about patient emergency admissions in up to 86% of cases, and failed to send critical clinical information within 48 hours after discharge in up to 88% of cases (Doty et al., 2020[7]). This situation had worsened since 2012.
The lack of real-time data was not limited to discharge information from hospitals to primary care physicians. Key information for health system management was not available in real-time or near real-time. For example, prior to the pandemic, only two countries reported having weekly mortality data (OECD, 2022[8]). Similar limitations existed for hospitalisation and intensive care data.
OECD research (2019[4]) found that the main barriers to building digital health systems are not technological but rather institutional and organisational. Developing an overarching digital strategy, strengthening governance of health data, and building institutional and operational capacity would reduce these barriers.
It is important for systems to implement clear, comprehensive and consistent health data governance frameworks to facilitate sharing of information and degradation of silos. An integrated health information system does not require all data of a certain type to be kept in a single location. It is quite possible to achieve the three objectives outlined above without central storage or even aggregation.
Capacity building is required in digital skills among health workers. One of the major drivers of adopting digital technologies is the ability to use them. Increased digital capacity in the workforce would aid this, as would engaging end users in the design process to ensure that technologies meet the needs of health workers and patients. Deficits in specialist skills, such as informatics, need to be addressed (Socha-Dietrich, 2021[9]).
A unified and co‑ordinated approach to national data governance can enable smooth information exchange and use for a range of purposes without compromising privacy, security and ownership of data. An integrated health information system requires a data governance framework that avoids overuse of consent to authorise data exchange, in favour of legal authorisation and an approach that protects privacy and ensures data security while enabling data to be exchanged and used for legitimate purposes. The OECD Council Recommendation on Health Data Governance sets out the elements for a national health data governance framework (OECD, 2016[10]; OECD, 2022[1]).
The 2019‑20 OECD survey of National Health Data Infrastructure and Governance reported challenges and difficulties in developing health data governance. Virtually all respondents experienced some challenges. Those most commonly experienced were: legal restrictions or policy barriers to public authorities undertaking data linkages (16 respondents); concerns with the quality of data that limit their usefulness (15 respondents); and legal restrictions or policy barriers to sharing data among public authorities (13 respondents) (Oderkirk, 2021[5]).
According to the 2019‑20 OECD survey of National Health Data Infrastructure and Governance, countries varied in the maturity of their dataset availability and governance. Figure 12.2 demonstrates the relative maturity in Demark, Finland and Korea compared to other reporting OECD countries.
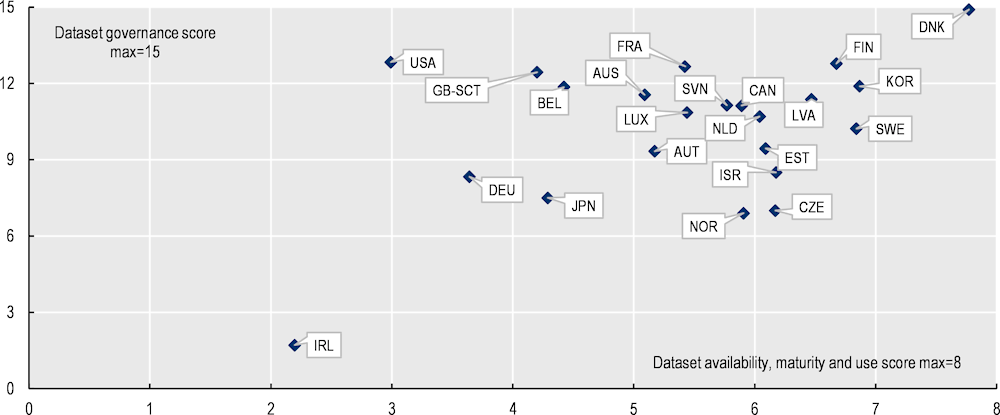
Note: The dataset governance score is the sum or the proportion of health care datasets meeting 15 dataset governance elements. The dataset availability, maturity and use score is the sum of the proportion of health datasets meeting 8 elements of dataset availability, maturity and use.
Source: Oderkirk (2021[5]), “Survey results: National health data infrastructure and governance”, https://doi.org/10.1787/55d24b5d-en: see Annex B Tables A B.1 and A B.2 in that report for further detail.
Many country respondents to the survey reported policy-relevant projects involving multiple countries in the linkage of their datasets or in the extraction of data from clinical record systems. These projects included parallel studies, where researchers in each country follow a common study protocol, and studies where data were shared across borders. In some OECD countries, data localisation regimes either explicitly prohibited approving the sharing of data with an organisation located outside their country or created obstacles to such sharing, such as a lack of clarity about how data sharing beyond the border might be approved (Svantesson, 2020[11]). Seven respondents reported that de‑identified data from all health care datasets could be shared for approved research to take place outside their country. Another six respondents reported that sharing data outside their country was possible for the majority of health care datasets. Cancer registry data were the national data most likely to be shared internationally: 14 countries reported that they could share de‑identified national cancer registry data with approved foreign researchers in academic and non-profit organisations.
Countries with federal systems also noted the difficulties in transferring information between states or provinces. Canada reported that such sharing is possible at the national level, but only if it is not prohibited by provincial law or by the terms of data sharing agreements with data suppliers. Germany also indicated that, owing to its federal structure, state data protection laws and laws governing hospitals may prohibit data sharing with entities within, and outside, national borders. This illustrates how harmonisation of policy frameworks within countries is also critical.
As the COVID‑19 pandemic continued, countries improved data collections and reformed governance to manage population health and inform decisions to respond effectively to the pandemic’s impacts, as discussed in Sections 12.3 and 12.4 below. To support health system resilience in the face of future shocks, however, countries can still do more to develop systems to provide the “right information at the right time”, both nationally and beyond.
Once the COVID‑19 pandemic began, many activities undertaken in the health system and beyond benefited from digital transformation and leveraged the value of digitised health information systems. Face‑to-face consultations were replaced with virtual alternatives, many processes were automated, new tools and information were provided to the public, real-time data were used to manage the health system, and some barriers to research were lowered. Countries with more developed digital governance and datasets had an advantage. The benefits of digitalisation become reinforcing as the infrastructure can be used for many different applications (Figure 12.3).

Note: ICT stands for information and communication technology.
Source: OECD (2023[12]), The COVID‑19 Pandemic and the Future of Telemedicine, https://doi.org/10.1787/ac8b0a27-en, compilation building on glossaries from the American and German telemedicine associations, and from ISO/TS 13131:2014.
The pandemic required transformation of health systems, with the ability to deliver services in a safe and physically distanced environment. For example, there was significant expansion in delivery of services using telehealth (see the chapter on care continuity). While changes in financing, physical infrastructure and training were important in expanding the use of telehealth, the digital and data foundation of the health system was essential to its success. Eighteen of 25 OECD1 countries surveyed in the 2021 OECD Survey on Electronic Health Record System Development, Use and Governance expect the number of telemedicine consultations to increase in the future. Another four countries (Canada, Czech Republic, Denmark and Sweden) expect the number of telemedicine consultations to decrease compared to the peak of the pandemic but still be much higher than before the pandemic began (Oderkirk et al., forthcoming[2]).
E‑prescribing was another example of digital transformation of the health system that reduced exposure to the risks of COVID‑19. Other examples of digitisation of previously analogue activities included: online booking systems; vaccination appointments; tracking, tracing and allocating COVID‑19 tests; sick leave and vaccination certificates; and reporting of test results. New digital tools and information were also provided to the public and patients, and development of public-facing applications that aided COVID‑19 tracking was widespread (de Bienassis et al., 2022[13]).
The pandemic demonstrated the wide variety of actors in the health system who need access to appropriate information to make informed and timely decisions, beyond high-level decision makers. These included those making decisions about resourcing at a local level, and researchers and others evaluating the effectiveness of interventions – both medical and societal. A substantially wider group of actors beyond the health system were also using this information, from the social care sector to employers. The public need for information was also critical to promoting trust, and to the effectiveness of containment and mitigation measures (see the chapter on containment and mitigation).
The onset of the pandemic made apparent the need for solutions to address deficits in information and communication that were vital for system monitoring and policy action. Many countries found that they lacked basic timely data for decision making within the health system – such as information on health workforce, resources, hospitalisations and mortality. Linking data across multiple datasets and providing information to those who needed it was essential to successful responses. Data from separate silos were required to assess and respond to different requirements across the health system.
A lack of real-time data on resources was a limitation in the early critical care surge, which needed to be remedied to implement effective strategies (see the chapter on critical care surge). Utilising “surge capacity” requires access and integration of data so that resources can be matched to needs. For example, information was required on available and used critical care resources across regions so that patients could be transferred from regions without capacity to those with capacity (load-balancing). In response to this issue, for example, the Australian Government established the Hospital Capacity and Activity Data Sharing System. This ensured availability of real-time patient flow data to monitor public hospital capacity and activity across state borders, collating daily data from every Australian public hospital. Canada also developed a Health System Capacity Planning Tool to support decision makers in understanding expected health resource demands and supply shortfalls related to the pandemic (de Bienassis et al., 2022[13]).
Beyond critical care, linkages of data within the health system improved countries’ ability to prioritise resources for those who needed them most and to ensure completeness of treatment. This facilitated implementation of public health monitoring, test reporting and contract tracing systems. In Belgium, for example, linked databases included test results and vaccinations. The linked data were used to: identify priority groups for vaccination and evaluate vaccination coverage in certain target groups; monitor infections in certain professional categories; find contact details to facilitate contact tracing; and adapt contact tracing procedures automatically to the health status (in terms of previous infection or vaccination) of the high-risk contacts identified. Costa Rica also used linked data to underpin its COVID‑19 response (Box 12.2).
Prior to 2012, medical records in Costa Rica were fragmented, which was an impediment to delivering high-quality health care. Since 2012, a unified digital health records system (EDUS) has been a priority for the Caja Costarricense de Seguro Social – the national social insurance fund that provides universal health services for the population. The aim was to have an information system to link all public hospitals and the primary health services network. Since 2014, there was marked improvement in the information infrastructure supporting providers across Costa Rica. In 2018, it was legally mandated that all levels of health care should be compliant and should have implemented the EDUS.
The health care actions of every provider within the Caja Costarricense de Seguro Social are included in the EDUS. The completeness of the information and the full coverage of the EDUS meant that it was a practical tool in Costa Rica’s pandemic response – especially in providing telehealth, remote patient monitoring and home follow-up of COVID‑19 patients.
Primary care in Costa Rica is delivered by more than 1 000 multi-disciplinary teams integrated into the community, who use the EDUS remotely. All citizens within Costa Rica are assigned to a team, based on geographical location. Using the information in the EDUS, which is available in both clinics and the community, the teams were responsive to the COVID‑19 pandemic. The inclusion of clinical pathways within the EDUS facilitated regular updating of the protocols used by teams, thereby ensuring the most up-to-date evidence‑informed health care.
Multiple initiatives aimed at caring for individuals were implemented in response to the pandemic, using the information and functionality in the EDUS. These included:
a rapid move to telehealth provision
expansion of the EDUS app to include COVID‑19 risk assessment and prioritisation
identification and follow-up of at-risk families
virtual visits by families for hospitalised patients
specialist follow-up of patients
implementation of vaccination programmes
home delivery of medicines.
Complementing these initiatives, the data within the EDUS were used for system level organisation, with real-time data and dashboards generating a better understanding of available resources (Figure 12.4). The EDUS also provided the framework for effective use of dedicated facilities for COVID‑19, allowing other facilities to continue non-COVID‑19 health care.
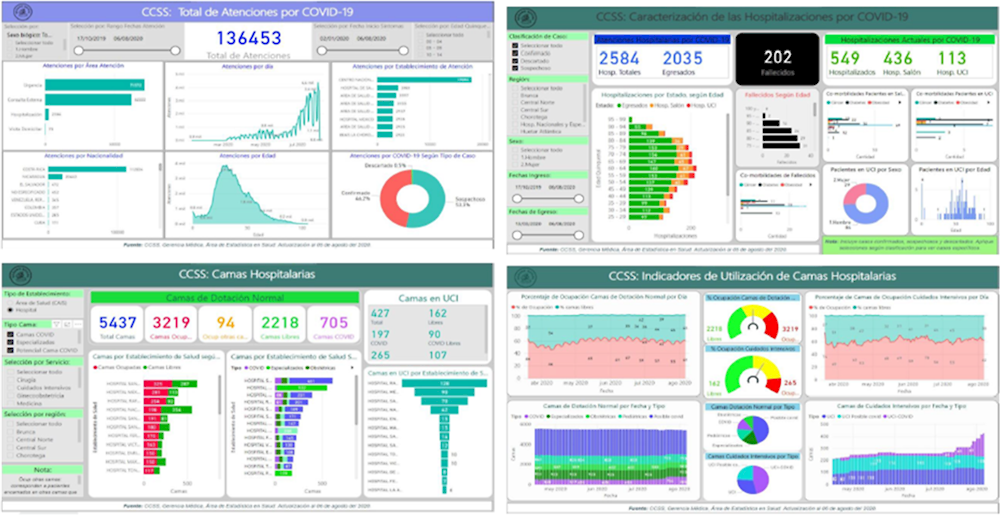
Source: Provided by Caja Costarricense de Seguro Social.
Comprehensive population level information systems, combined with population level coverage, facilitate agile real-time responses to threats. This requires technological infrastructure to be built and used by health care providers and the community prior to a threat occurring. However, such infrastructure and the data it generates need to be fortified against other risks. For example, in 2022, Costa Rica – like several other countries – was subject to cyber attacks, a key vulnerability of a digital system, leaving patients and providers at risk of data exposure or disrupting care.
Costa Rica demonstrated the benefits of extending information systems beyond simply recording health care. Household and social information are beneficial in such situations because it facilitates efficient management of resources and effective community care and treatment.
Source: Information provided by the Costa Rican Ministry of Health and Caja Costarricense de Seguro Social.
While the impact of the pandemic was predictable on some parts of health systems – such as critical care demand – it was less clear in others, including measuring the impact on non-COVID‑19 patients. This gap in accessible information affected planning and co‑ordination. When information was required across silos, governance frameworks were often insufficient to co‑ordinate sharing and utilisation of data: while COVID‑19 and the response to it crossed borders, locally collected data could not always do so. Furthermore, with data siloed, so too were practices and timeliness of inputting and maintaining data. Inconsistencies across different data systems affected the immediate use and reliability of information.
EHRs – or real-time, patient-centred medical records most often used in direct care settings – provided a robust information system for managing acute symptoms and treatments for SARS‑CoV‑2, and mitigating further spread of the disease. For example, EHRs supported disease surveillance and contact tracing by linking patient outcomes with contact information and communication channels. This was a key functionality for patient health. It supported broader efforts to model disease transmission and identify pockets of higher incidence. EHRs also enabled mapping of comorbidities and successful treatments to patient subgroups, enhancing care for future patients (Satterfield, Dikilitas and Kullo, 2021[14]).
Of the 25 countries responding to the 2021 OECD Survey on Electronic Health Record System Development, Use and Governance, 14 reported that EHR data were used to facilitate tracking and tracing of patients infected with Sars-CoV‑2. For example, in Iceland, a system developed for COVID‑19 screening at borders was expanded to be used for all COVID‑19 testing in the country. The system is highly automated and fully integrated with the national EHR system and the national patient portal, meaning that all health care providers can see instantly whether a patient has a positive COVID‑19 test. Furthermore, the system is integrated with the Department of Civil Protection and Emergency Management and is used to manage the national COVID‑19 vaccination programme (Oderkirk et al., forthcoming[2]).
A connection between or integration of EHRs and issuing of COVID‑19 vaccination certificates was reported in 16 of the 25 respondents to the 2021 survey. Iceland, for example, was again able to integrate this functionality into national EHRs, the COVID‑19 testing system and the national patient portal. Seven days after a person has been completed the initial vaccination schedule with a second shot they can download a valid e‑Certificate for proof of COVID‑19 vaccination that complies with EU standards and includes a QR code. In Lithuania, all vaccination records (including for COVID‑19) are stored in the central e‑health system, and the plan is to have electronic/paper vaccination certificates with easy proof of validity compatible with World Health Organization and European Commission recommendations. In some countries, EHRs are used not only to store and communicate vaccination data but also for post-market surveillance of COVID‑19 vaccine efficacy and/or adverse effects. Of the 25 responding countries, 11 reported that they are using or planning to use EHR data for this purpose (Oderkirk et al., forthcoming[2]).
Linkages made beyond the health system to other data also improved the performance of the health system response to COVID‑19. For example, tracking and tracing was aided by linkages to other data information systems in Korea, including those related to international travellers (Box 12.3Box 12.3).
Information about socio‑economic characteristics linked to health information allowed evidence to be generated about the risks of COVID‑19 for different groups (see the chapter on COVID‑19 outcomes). Some countries promoted linkages between health information and other socio‑economic information. For example, Wales (United Kingdom) added linkages to COVID‑19 testing, sequencing, tracking and vaccination data to its existing Linkage Databank, and Canada integrated provisional data on long-term care to understand the impact of COVID‑19 on long-term care facilities (de Bienassis et al., 2022[13]).
During the first year of the pandemic, the Korean health system’s management of the COVID‑19 pandemic achieved case numbers and deaths that were among the lowest in the world. This was accomplished through unprecedented collaboration across agencies and sectors, which enabled standardisation and integration (linkage) of data, and use of a secure mechanism to make these data accessible to a range of actors for pandemic management and research.
Prior to the pandemic, Korea had built an epidemiological investigation support system that integrated information from a wide range of sectors to identify cases and trace contacts quickly. Several elements of this system built on Korea’s review of experience with the Middle East Respiratory Syndrome (MERS) outbreak of 2015. For example, Korea developed an International Traveller Information System to provide real-time data to health providers about travellers entering from higher-risk countries. This facilitated prioritisation for testing. The 2015 MERS outbreak also triggered amendments to existing legislation so that public agencies could, at the outbreak of a serious infectious disease, collect and share several categories of data, including data outside the health system.
The system was activated in response to the COVID‑19 pandemic. It offered the potential to link the data on patients who were infected with SARS‑CoV‑2 to data outside the health system, such as location data from mobile phone carriers and transactions from credit card companies (Park, Choi and Ko, 2020[15]).
Source: OECD (2022[1]), Towards an Integrated Health Information System in Korea, https://doi.org/10.1787/c4e6c88d-en.
Information was used beyond the health system in several different ways: to be published; to be integrated with mitigation activities taking place outside the health system; and for research.
Dashboards were used in most OECD countries. Dashboards were a key communication tool for sharing COVID‑19‑related data with the public. Generally, they were publicly accessible and updated daily. Countries usually reported number of COVID-19 tests, cases and deaths. Some countries also reported other indicators. For example, Canada included information on excess mortality and cases by country for international benchmarking (de Bienassis et al., 2022[13]).
Information on the impact of mitigation efforts needed to be integrated with information on available resources and predictions of future cases (see the chapter on critical care surge). High-level decision makers relied on this integrated information to balance the benefits and risks of their whole‑of-society approaches to COVID‑19 (see the chapter on containment and mitigation).
The pandemic also required rapid generation of research. At the onset, many aspects were unknown (see chapters on critical care surge, and containment and mitigation). Many countries made data accessible to researchers, producing one‑stop data depositories, and improved access to patient-level data (de Bienassis et al., 2022[13]). For example, Ireland developed the COVID‑19 Data-hub and introduced the COVID‑19 Biobank, standardising collection and making data available for research (University College Dublin, 2021[16]).
Beyond national improvements in access to data, international co‑operation and data sharing increased. European countries submitted data systematically to the European Centre for Disease Prevention and Control, and participated in the European Health Data Space, which began in February 2021. There was also a push towards decentralised clinical trials across national boundaries (de Bienassis et al., 2022[13]; De Brouwer et al., 2021[17]).
Nonetheless, fragmentation of information – especially early in the COVID‑19 pandemic – resulted in disproportionate impacts on vulnerable populations and services, and particularly on those with poor data accessibility. For example, long-term care had sparse data on outcomes, and a lack of data on infections and mortality hampered early absorption and response to the pandemic (see the chapter on long-term care). These consequences emphasise the importance of an integrated health information system that breaks down silos beyond the traditional health care system to include the most vulnerable sectors of care.
When responding to the COVID‑19 pandemic, some countries found their existing health data infrastructure inadequate to meet their needs – including systems for public health monitoring, assessment of resource use and availability, and data to monitor the status of non-COVID‑19 health needs. These information gaps, some of which were highlighted in Section 12.3, served as a catalyst for new investments to strengthen health data infrastructure. The pandemic also saw countries leverage COVID‑19‑related reforms in a way that may address longstanding barriers in the structures, policies and institutions that have prevented OECD countries from making full use of health-related data (de Bienassis et al., 2022[13]).
The pandemic changed the landscape of data required to respond effectively. Countries needed more regular access to more health data, while still protecting the privacy and security of this information. Accordingly, countries instituted a wide range of initiatives to improve health data availability, accessibility, sharing, privacy, and security (Figure 12.5).
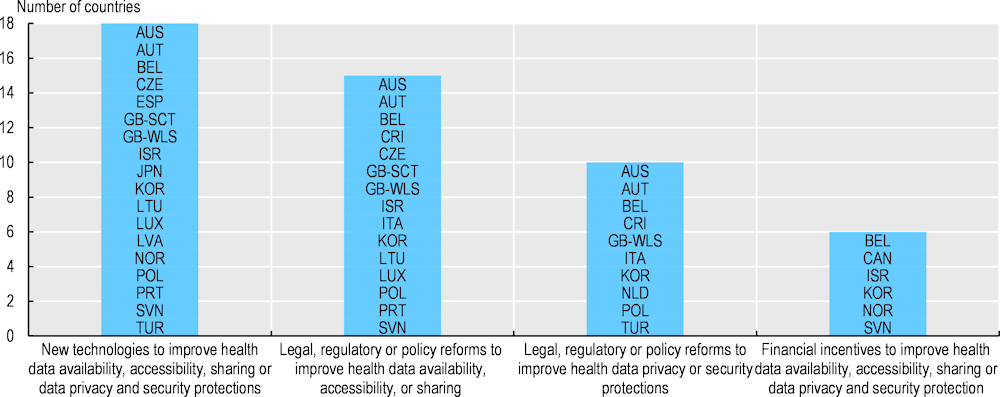
Note: For the purposes of this figure, Scotland (United Kingdom) (GB-SCT) and Wales (United Kingdom) (GB-WLS) are represented independently.
Source: OECD Questionnaire on Health Data and Governance Developments in relation to COVID‑19 2021.
For many countries, comprehensive legislative action was required to share and use health data to inform policy responses to the pandemic. In Australia, for example, the Office of the National Data Commissioner pursued a range of legislative priorities to support nationally co‑ordinated health data systems that were accessible and could be shared between government agencies to expedite use in emergencies.
The Data Availability and Transparency Act, which came into effect on 1 April 2022, established a scheme to share government data safely. Its implementation was supported by the addition of digital services to assist in accreditation, submission of data requests and data sharing agreements, among others.
The Data Inventories Pilot Program developed individual data inventories for different agencies, with common standards, which could be aggregated into a central Data Catalogue to support transparency and quick response in emergencies.
An Intergovernmental Agreement (2021) on data sharing reflected a commitment for public sector data to be shared securely, safely, lawfully and ethically, where possible. This was an important step in recognising the role of data as a national asset.
An Addendum to the National Health Reform Agreement (2020‑25) specified national actions to enable health data to contribute to long-term health reform and drive health system improvements.
In Lithuania, a new State Data Governance System was implemented to permit each state institution to prepare their data and make it publicly accessible – as such, regulations regarding the right to receive information from state and municipal institutions and bodies were updated. This encouraged state institutions to prepare, merge and analyse their data, and to create a platform to facilitate data sharing for public use. This reform related to ongoing efforts to establish the legal basis for data sharing, and for creating incentives and systems for data owners to share information.
Belgium also experienced challenges related to its existing legal framework to collect and use data for public health crisis management. In response, it created new frameworks, with the approval of many different stakeholders, and new working groups, taskforces and committees were set up to inform decision making. Similarly, in the Netherlands, legal changes were made so that the National Institute for Public Health and the Environment had access to complete and validated data from health care and long-term care (de Bienassis et al., 2022[13]).
Wales (United Kingdom) also recognised that regulatory and policy barriers were hampering timely access to data, and that the expiry of emergency regulations would make access contingent on satisfying the common law duty of confidentiality. Accordingly, Wales (United Kingdom) is monitoring the proposed changes to the legal and regulatory framework that governs the use of personal and confidential data in the United Kingdom to determine if, when and how to use its devolved powers.
Italy also progressed its legislative efforts to facilitate the use of EHRs. These included extending the types of health and social care data that can flow into EHRs, especially those related to: providing services outside the national health system; securing the ability to update and activate health data by giving citizens more ownership of their data; and guaranteeing the “right to know” who has accessed a patient’s EHR.
In addition, many countries introduced financial incentives to encourage sharing of data efficiently and to improve data quality. For example, the United States established the Strengthening the Technical Advancement and Readiness of Public Health via Health Information Exchange Program to reward public health agencies for improving health information exchange for communities disproportionately affected by the pandemic. Korea also encouraged exchange of information for policy purposes by reducing or fully exempting data usage fees for COVID‑19‑related research.
Real-time (or near real-time) data were key to informing decision making during the pandemic. Despite limitations in real-time information at the onset of the pandemic (as outlined in Section 12.2), almost all countries (over 90%) improved the timeliness of their data. Specific improvements occurred in mortality data, with many countries moving from an annual release to more rapid updating (de Bienassis et al., 2022[13]).
Some countries also developed new infrastructure to monitor public health. For example, Norway developed Bered’C19 in April 2020 to collect daily data on hospitalisations, primary care and emergency care. This system acts as a “data lake” to link all data sources in real-time at the patient level; this supports public health monitoring and fosters research and preparedness. Implementation of Bered’C19 was supported by existing legislation (the Health Preparedness Act) and development of infrastructure at the individual data source level. As a further example, Australia is replacing its National Notifiable Diseases Surveillance System with a secure cloud-based system that will process data in near real-time.
Change was not only legislative; technical ability and the landscape to facilitate data sharing were also improved in some OECD countries. Managing cases, contact tracing and post-market surveillance of vaccinations were examples of extensions made to existing health data infrastructure, both to monitor public health and to co‑ordinate the pandemic response (see the chapter on containment and mitigation).
Timely, comprehensive population wide data are required for an effective response to crises. Such data were missing within numerous jurisdictions at the start of the pandemic. This information may need to be broader than health data and include social and other aspects, so that decision makers can understand where vulnerabilities exist and thus where resources should be prioritised. This is especially important when crises have implications well beyond the health sector and disproportionately affect disadvantaged groups. More mature data infrastructure and governance give countries an advantage when responding to new and novel threats.
In responding to the OECD Health Data and Governance Changes during the COVID-19 Pandemic Questionnaire 2021, OECD countries with the greatest capacity to leverage health information for policy planning, decision making and research during the pandemic were those that already had a digital strategy with three key elements:
Mature health information systems with key national health data across the health care continuum that are timely and of high quality, and that can be linked with one another and with contextual information.
Standardised, coherent and accessible national electronic clinical record systems, including EHRs, that address fragmentation of data across health care silos and enable “one patient, one record” for a complete view of health care and long-term care trajectories and outcomes.
Comprehensive health data governance frameworks with legislation and policies that protect privacy and data security while enabling data about health and health care to be developed, linked, accessed and analysed for uses in the public interest, including cross-border collaborations (de Bienassis et al., 2022[13]).
Fortifying the foundations of the health system (see the chapter on investing in resilience) will require investment in an information-rich future. This means investment in both equipment (information technology infrastructure) and ensuring that the information is developed and used well (via software, operational processes, data scientists and technological skills). It is estimated that this may require an investment of over 0.28% of GDP compared to a 2019 baseline. As discussed in Section 12.4, some of this investment has occurred since the pandemic began. Prior OECD work estimated a three‑fold return on this investment (OECD, 2019[4]).
The OECD Council Recommendation on Health Data Governance set principles for national health data governance frameworks and called on governments to address unnecessary barriers to the efficient exchange and interoperability of health data (Box 12.4Box 12.4). The pandemic challenged countries to progress data governance reforms, which should adhere to the Council Recommendation. Steps undertaken to track and trace COVID‑19 cases may generate concern about violating privacy, and balancing transparently the public health benefits with privacy is important (Park et al., 2020[18]). A policy environment in which respect for privacy and trust is maintained is a key reason for having a health data governance framework (OECD, 2019[4]).
The OECD recommends that governments establish and implement a national health data governance framework to encourage availability and use of personal health data to serve the health-related public interest, while promoting the protection of privacy, personal health data and data security. Below are the 12 key elements to develop and implement national health data governance frameworks.
1. Engagement and participation, notably through public consultation, of a wide range of stakeholders to ensure the framework serves the public interest and is consistent with societal values
2. Government co‑ordination and promotion of co‑operation among organisations processing personal health data, whether in the public or private sectors, to encourage common data terminology and interoperability standards, and common procedures to minimise barriers to sharing data
3. Review of the capacity of the public sector to process personal health data for research, statistical and other uses within the public interest – including data availability, quality, accessibility and privacy protection
4. Clear provision of information to individuals about the processing of their personal health data and timely notification of a data breach
5. Processing of personal health data by informed consent or a lawful alternative; and, when processing is not based on consent, the ability for individuals to object to the processing (to opt out), or if opt-out is not possible then to be provided with the reason why and the legal authorisation for the processing
6. Review and approval procedures for the uses of personal health data that assess whether the uses are within the public interest, which should be objective, fair, timely and transparent to the public
7. Provision of public information about the purpose of processing of personal health data, the public interest served, the procedure and criteria to approve data processing and a summary of approval decisions taken
8. Maximising the potential of new technologies to support data use and re‑use, protect privacy and manage digital security risks, and support individuals’ control of the uses of their own data
9. Monitoring and evaluating whether the uses of personal health data have served the public interest and brought the benefits that were expected
10. Providing training and skills development in privacy and security measures to those processing personal health data
11. Implementing controls and safeguards to:
a. provide accountability for personal health data processing and mechanisms for audit
b. provide privacy, data protection and security training for staff members processing personal health data
c. designate a data protection officer to be accountable for the organisation’s information security programme
d. undertake risk assessment processes that include the risk of unauthorised data linkages and breaches
e. take technical, physical and organisational measures to protect privacy and data security, including:
i. mechanisms that limit the identification of individuals while allowing data re‑use (linkage)
ii. data sharing agreements that specify data security requirements and sanction non-compliance
iii. alternatives to data transfers, such as secure data access centres and remote data access
iv. identity verification and authentication of individuals accessing personal health data
12. Requiring organisations processing personal health data to demonstrate that they meet national expectations for health data governance, which can include certification or accreditation.
Source: OECD (2016[10]), “OECD Recommendation on Health Data Governance”, https://legalinstruments.oecd.org/en/instruments/OECD-LEGAL-0433.
In many countries, pandemic experiences have influenced national EHR and e‑health strategies that will allow greater use of information to support health systems resilience. Two-thirds of responding countries (16 of 25) to the 2021 OECD Survey on Electronic Health Record System Development, Use and Governance reported that the COVID‑19 pandemic had changed their EHR system or their plans for further development and use of the EHR system.
For example, based on its pandemic experience, Canada is developing a Pan-Canadian Health Data Strategy that will modernise how health data are managed so that EHR data can flow more easily between health data systems. This will help to ensure that decision makers have the information they need to respond to public health situations.
OECD countries are also considering afresh the potential value of EHRs.
Italy reported that its COVID‑19 experience increased awareness of the strategic role of EHRs for health care and governance, and that an early warning and response system requires EHR data to be linked with other available sources. Thus, the Italian recovery plan contains a project to enhance and accelerate EHR system functionalities and usage.
Lithuania reported that improvements have been made to the quality of EHR data, the collection of health data and the integration of EHR systems to enable the sharing and publication of COVID‑19 information, with the possibility of creating open datasets. This practice is expected to facilitate further improvements related to data used for statistics, research and health care planning.
In Portugal, the Recovery and Resilience Plan and the pandemic accelerated the digital transformation and use of digital tools in the context of health care and treatment. The Plan aims to respond to current and future weaknesses of the health system by reinforcing the current levels of evolution and standardisation of the information systems of the national health service.
In Slovenia, the pandemic raised national awareness of the benefits of EHR exchange. As a result, use of the national EHR platform has increased significantly, dedicated financial resources have been provided, and new services and programmes have been implemented.
In the 2021 OECD Survey on Electronic Health Record System Development, Use and Governance, OECD countries also reported several levers to improve the spread and interoperability of their electronic clinical data, as highlighted below (Oderkirk et al., forthcoming[2]):
A legal requirement for health care providers to meet national standards for EHR interoperability: 13 countries reported having a legal requirement for health care providers to adopt an EHR system (software) that conformed with national standards for both clinical terminology and electronic messaging (exchange).
Certification of EHR system (software) vendors that requires them to adopt national standards for both clinical terminology and electronic messaging.
Financial incentives for health care providers to install an EHR system that meets national standards and meets the requirements for national EHR interoperability.
The pandemic brought about a rapid change in the digital landscape. It is of the utmost importance to understand the political, technological, legal, regulatory and financial implications that result from this.
Increasing digitalisation of the health system has advantages, but it also potentially increases the risks from natural and malicious sources. For example, heat stress resulted in cancellation of operations associated with the failure of servers during 2022 (Building Better Healthcare, 2022[19]). The COVID‑19 pandemic also underlined the vulnerability of the health system to malicious actors, including Distributed Denial of Service and ransomware attacks on hospitals in the Czech Republic, France, Germany and Spain. Increasing vulnerability to cyber threats must be mitigated, and the OECD has distilled lessons and made recommendations to strengthen digital security, drawing from the pandemic context (OECD, 2020[20]; OECD, 2022[21]).
Another risk is that the benefits of digitisation may not be evenly spread across the population and may favour advantaged groups. New tools and digital solutions should be accelerated, designed, and tested with vulnerable groups including those living with disabilities. Making use of these tools and solutions also requires OECD countries to continue to promote health and digital literacy (OECD, 2019[4]).
The potential of AI in health is profound but the risks of unintended and negative consequences associated with its use are commensurately high in both crisis and non-crisis contexts, as highlighted in Box 12.5.
Artificial Intelligence (AI) – technology to simulate intelligent behaviour and critical thinking – has profound potential applications in health (Huang et al., 2022[22]). This is because of the growing volume of health data, the reliance by health systems on quality, timely information to solve problems, and the variability and complexity of how diseases interact with individuals and populations (OECD, 2020[23]). AI applications in health may be physical (e.g. a robotic system for telepresence, enabling a health worker to perform actions remotely from a patient) or virtual (e.g. machine or deep learning, represented by mathematical algorithms that improve learning through experience and may enable “systems thinking” about health care) (Huang et al., 2022[22]).
Several systematic reviews analysed the impact of AI in the context of the COVID‑19 pandemic (Isgut et al., 2022[24]). These reviews show the promise of AI, including the use of robots to disinfect remotely to reduce the exposure of health workers to the virus (Teng, Ding and See, 2022[25]) and to assist with medical image screening for COVID‑19 diagnosis (Ozsahin, Isa and Uzun, 2022[26]).
These reviews, however, underscore AI’s successful validation and deployment was limited in practice. The limitations reported include poor data quality, the challenges of scaling up projects and ensuring proper controls (without which AI could reinforce biases), and the lack of interpretability of the results (with the potential for AI to generate noise instead of real, clinically meaningful signals) (Giuste et al., 2022[27]; Huang et al., 2022[22]; Isgut et al., 2022[24]).
Many of these limitations have been noted beyond the pandemic context – poor health data governance means AI still needs human curation. In this context, governments and other stakeholders may wish to be guided by the 2019 OECD Recommendation on AI, which outlines the principles for responsible stewardship of AI and the policy requirements for trustworthy AI. This Recommendation focuses on ensuring transparency of AI, accountability for the outputs of AI models, regulatory oversight, building capacity among health workers (and the public), and long-term investment. Strong policy frameworks based on inclusive and extensive dialogue among all stakeholders are needed to ensure AI adds value to patients and to society (OECD, 2020[23]).
A final risk to be managed when increasing digitalisation is to recognise its benefits will not occur merely by digitising current processes. A key part of digital transformation relates to how new attitudes and thinking are taken on and adopted. It is important to establish national consensus on digital strategy as well as standards, policy, governance, and social license to take advantage of an integrated health system. Success and improved resilience will depend on ensuring that patients, the health workforce, institutions within the health system and decision makers use information for tangible public benefit.
Adequate data on healthcare needs, prioritisation, waiting times and healthcare delivery are required for countries to move from pandemic response to recovery. Some countries have implemented approaches to co-ordinate this information. For example, in England (United Kingdom), the Clinical Prioritisation Programme has published prioritisation frameworks for surgery, diagnostics and endoscopy to help manage waiting lists, promote their accuracy and ensure that priority is based on clinical need. These frameworks outline the steps for clinicians to check a patient’s condition, establish additional risk factors and understand treatment options (NHS, n.d.[28]).
Data needs for future shocks and to address the longer-term implications of the COVID-19 pandemic will differ from those needs identified and addressed to date. For example, understanding the health and economic implications of “long COVID” will require more high-quality data, and potentially more linkage between health and employment data (see the chapter on key findings and recommendations).
The field of health is yet to realise the full potential of big data analytics, that is, tools and methods to extract and analyse high volume, high variety and high velocity data to produce valuable insights which cannot be obtained from traditional data sources ( (OECD, 2019[4]). Big data sources can include data from EMRs and EHRs, data from health monitoring devices and wearable technologies, and genomic, spatial/geographic, environmental, behavioural and economic data sets. In 2021, eight respondents to an OECD survey reported applying data mining to find or extract data within their EHR systems, eight reported applying machine learning/AI algorithms to EHR systems data for patient care or decision making, and six reported national projects to link EHR data with the types of non-health data sets outlined (OECD, 2022[8]).
Nonetheless, “bigger is not always better” when it comes to promoting high-quality data use and linkage. Big data is not necessarily “whole data”: the large size of a data set does not necessarily mean it is a representative of a certain population. Therefore, big data requires robust methodologies in place to interpret it and account for biases (OECD, 2019[4]).
Availability of high-quality linked data will help to mitigate future shocks and their impacts on the health system. Co-ordination of data integration can facilitate better disease management through contact tracing, and support research into potential treatments and risk factors. Where these cross-cutting high-quality data are available, and governance frameworks for sharing and protection are in place, health systems can be more resilient and have more information available to prevent long-term consequences.
This is true of the shock that was the COVID-19 pandemic, and it will be true for others. For example, high-quality linked data will aid responses to climate events and disasters. Accordingly, stronger digital foundations may be required to support additional linkages to non-health data, such as meteorological information. Importantly, these linkages will not only support an enhanced response to shocks but improve the functioning of the health system between crises. Building the data and digital future of health systems will benefit their resilience, efficiency and sustainability.
[6] Barrenho, E. et al. (2022), “International comparisons of the quality and outcomes of integrated care: Findings of the OECD pilot on stroke and chronic heart failure”, OECD Health Working Papers, No. 142, OECD Publishing, Paris, https://doi.org/10.1787/480cf8a0-en.
[19] Building Better Healthcare (2022), Heatwave spells disaster for data servers, https://www.buildingbetterhealthcare.com/news/article_page/Heatwave_spells_disaster_for_data_servers/202652 (accessed on 26 September 2022).
[13] de Bienassis, K. et al. (2022), “Health data and governance developments in relation to COVID-19: How OECD countries are adjusting health data systems for the new normal”, OECD Health Working Papers 138, https://doi.org/10.1787/18152015.
[17] De Brouwer, W. et al. (2021), “Empowering clinical research in a decentralized world”, npj Digital Medicine, Vol. 4/1, https://doi.org/10.1038/s41746-021-00473-w.
[7] Doty, M. et al. (2020), “Primary Care Physicians’ Role In Coordinating Medical And Health-Related Social Needs In Eleven Countries”, Health Affairs, Vol. 39/1, pp. 115-123, https://doi.org/10.1377/hlthaff.2019.01088.
[27] Giuste, F. et al. (2022), “Explainable Artificial Intelligence Methods in Combating Pandemics: A Systematic Review”, IEEE Reviews in Biomedical Engineering, https://doi.org/10.1109/RBME.2022.3185953.
[3] Hanefeld, J. et al. (2018), “Towards an understanding of resilience: Responding to health systems shocks”, Health Policy and Planning, Vol. 33/3, pp. 355-367, https://doi.org/10.1093/heapol/czx183.
[22] Huang, J. et al. (2022), Telemedicine and artificial intelligence to support self-isolation of COVID-19 patients: Recent updates and challenges, SAGE Publications Inc., https://doi.org/10.1177/20552076221100634.
[24] Isgut, M. et al. (2022), “Systematic Review of Advanced AI Methods for Improving Healthcare Data Quality In Post COVID-19 Era”, IEEE Reviews in Biomedical Engineering, https://doi.org/10.1109/RBME.2022.3216531.
[28] NHS (n.d.), Clinical Prioritisation Programme, https://www.england.nhs.uk/coronavirus/secondary-care/other-resources/clinical-prioritisation-programme/ (accessed on 15 June 2022).
[5] Oderkirk, J. (2021), “Survey results: National health data infrastructure and governance”, OECD Health Working Papers, No. 127, OECD Publishing, Paris, https://doi.org/10.1787/55d24b5d-en.
[2] Oderkirk, J. et al. (forthcoming), “Stocktaking of country level advancements in implementing and utilizing EHR systems”, OECD Health Working Papers, OECD Publishing, Paris.
[12] OECD (2023), The COVID-19 Pandemic and the Future of Telemedicine, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/ac8b0a27-en.
[8] OECD (2022), Health Data Governance for the Digital Age: Implementing the OECD Recommendation on Health Data Governance, OECD Publishing, Paris, https://doi.org/10.1787/68b60796-en.
[21] OECD (2022), OECD Policy Framework on Digital Security: Cybersecurity for Prosperity, OECD Publishing, Paris, https://doi.org/10.1787/a69df866-en.
[1] OECD (2022), Towards an Integrated Health Information System in Korea, OECD Publishing, Paris, https://doi.org/10.1787/c4e6c88d-en.
[20] OECD (2020), “Seven lessons learned about digital security during the COVID-19 crisis”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/e55a6b9a-en.
[23] OECD (2020), Trustworthy AI in Health, OECD, Paris, https://www.oecd.org/health/trustworthy-artificial-intelligence-in-health.pdf (accessed on 21 January 2023).
[4] OECD (2019), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/e3b23f8e-en.
[10] OECD (2016), OECD Recommendation on Health Data Governance, https://legalinstruments.oecd.org/en/instruments/OECD-LEGAL-0433 (accessed on 23 September 2022).
[26] Ozsahin, D., N. Isa and B. Uzun (2022), The Capacity of Artificial Intelligence in COVID-19 Response: A Review in Context of COVID-19 Screening and Diagnosis, MDPI, https://doi.org/10.3390/diagnostics12122943.
[18] Park, O. et al. (2020), “Contact transmission of Covid-19 in South Korea: Novel investigation techniques for tracing contacts”, Osong Public Health and Research Perspectives 1, pp. 60-63, https://doi.org/10.24171/j.phrp.2020.11.1.09.
[15] Park, S., G. Choi and H. Ko (2020), “Information Technology-Based Tracing Strategy in Response to COVID-19 in South Korea - Privacy Controversies”, JAMA - Journal of the American Medical Association, Vol. 323/21, pp. 2129-2130, https://doi.org/10.1001/jama.2020.6602.
[14] Satterfield, B., O. Dikilitas and I. Kullo (2021), “Leveraging the Electronic Health Record to Address the COVID-19 Pandemic”, Mayo Clinic Proceedings, Vol. 96/6, pp. 1592-1608, https://doi.org/10.1016/j.mayocp.2021.04.008.
[9] Socha-Dietrich, K. (2021), “Empowering the health workforce to make the most of the digital revolution”, OECD Health Working Papers, No. 129, OECD Publishing, Paris, https://doi.org/10.1787/37ff0eaa-en.
[11] Svantesson, D. (2020), “Data localisation trends and challenges: Considerations for the review of the Privacy Guidelines”, OECD Digital Economy Papers, No. 301, OECD Publishing, Paris, https://doi.org/10.1787/7fbaed62-en.
[25] Teng, R., Y. Ding and K. See (2022), Use of Robots in Critical Care: Systematic Review, JMIR Publications Inc., https://doi.org/10.2196/33380.
[16] University College Dublin (2021), UCD co-lead in National Irish COVID-19 Biobank, https://www.ucd.ie/research/news/2021/ucdco-leadinnationalirishcovid-19biobank/body,563207,en.html (accessed on 16 November 2022).
← 1. Excluding Norway.