This chapter covers the case study of ToyBox, a school-based healthy lifestyle intervention operating in several European countries targeting children aged 3‑4 years of age. The case study includes an assessment of ToyBox against the five best practice criteria, policy options to enhance performance and an assessment of its transferability to other OECD and EU27 countries.
Healthy Eating and Active Lifestyles

8. ToyBox
Abstract
ToyBox: Case study overview
Description: ToyBox is an intervention delivered in schools to children aged 3‑4 years of age (i.e. in Kindergarten) with the aim of promoting health lifestyles to prevent obesity. It is a 24‑week, multi-component intervention targeting four key behaviours namely: drinking water when thirsty; consuming healthy snacks; increasing physical activity; and prolong periods of sedentary behaviour.
Selected kindergartens in European countries including Belgium, Bulgaria, Greece, Germany, Malta, Poland and Spain have implemented ToyBox.
Best practice assessment:
Table 8.1. OECD best practice assessment, ToyBox
|
Criteria |
Assessment |
|---|---|
|
Effectiveness |
ToyBox has been shown to reduce sedentary behaviour, increase physical activity and improve eating behaviours, however, evaluation results are not conclusive. |
|
Efficiency |
Available economic evaluations indicate ToyBox is cost-effective, however, results are limited in scope |
|
Equity |
ToyBox aims to address inequalities by addressing a health issue that disproportionality affects children with a low socio‑economic status (SES) Evidence on impact indicate ToyBox is more effective for children attending high-SES kindergartens |
|
Evidence‑base |
Evidence to evaluate ToyBox is strong in many areas including study design and the data collection methods used However, as in many public health studies, neither researchers nor participants were blinded. |
|
Extent of coverage |
In kindergartens offering ToyBox, between 63‑74% of children participate |
Enhancement options: to enhance effectiveness, ToyBox administrators could enhance interactive engagement with parents and the community, as well as extend the duration of the intervention beyond 24 weeks. To ensure staff have the appropriate skills to deliver the intervention, additional support for teachers as well as integrating obesity prevention topics into formal qualifications required to become a kindergarten teacher could prove beneficial. To enhance the evidence‑base, reporting the impact of ToyBox on BMI in addition to secondary outcome measures (e.g. physical activity) is needed. To the extent possible, authors are encouraged to report results by different population groups with a particular focus on those who are disadvantaged. To enhance the extent of coverage, a multi-pronged approach to recruit parents (and therefore their children) may prove beneficial in boosting participation rates, for example, by promoting ToyBox with support from government organisations to enhance trust.
Transferability: ToyBox operates in several European and non-European countries indicating it is a transferable intervention. In countries where it does not operate, publically available data indicate that ToyBox is likely to receive political support, a key pillar of transferability, as it targets a prominent public health issue – childhood obesity.
Conclusion: a review of ToyBox across several European countries found the intervention performed well against most criteria within the OECD Best Practices Framework and is transferable. For example, ToyBox reduces sedentary behaviour and improves eating habits, and has been shown to be cost-effective. However, results indicate it is more effective among high socio‑economic status kindergartens, which is a key limitation. To improve the performance of ToyBox, policy makers could increase parental and community engagement as well as extend the duration of the programme beyond 24 weeks.
Intervention description
Overweight and obesity amongst young children is a key concern across many developed and developing countries. In the EU, for example, approximately one in eight children (12%) aged 7‑8 are obese with this figure increasing to 17% for children in Malta (OECD/European Union, 2018[1]; WHO, 2018[2]). Childhood obesity is particularly concerning given its link to psychosocial problems including low self-esteem, bullying, underachievement in schools, and depression (OECD/European Union, 2018[1]). Further, it is a key determinant of obesity in adulthood, which is associated with various health issues including higher probability of developing diabetes, certain cancers and cardiovascular diseases (CVDs) (OECD, 2019[3]).
To reduce the rate of overweight and obesity amongst young schoolchildren, seven EU countries have implemented the ToyBox intervention.1 ToyBox is a Kindergarten‑based intervention (i.e. for children aged between 3‑4 years) aimed at promoting healthy lifestyles to prevent overweight and obesity rates among children. The intervention is run by teachers over a 24‑week period, which concentrates on the four main energy balance‑related behaviours (EBRBs) among young children (Manios et al., 2014[4]; ToyBox, 2020[5]):2
Water consumption (encouraging children to drink water when thirsty)
Healthy snacking
Physical activity
Sedentary behaviour (breaking up periods of sitting).3
Teachers are encouraged to introduce each of the EBRBs to students in a fun, interactive environment for example through interactive stories, experiments and games.
Countries such as Germany, Greece and Spain implemented ToyBox 2012‑13 (ToyBox, 2020[5]), while Malta implemented the intervention in 2019. Teachers who deliver ToyBox receive a once‑off 1.5 hour training session (with follow-up at six months), in addition, teachers receive a guidebook and classroom activity guides to help structure lessons.
To encourage children to maintain healthy behaviours in the home environment, the intervention also aims to engage parents. Specifically, parents are provided newsletters, tip cards (e.g. tips on how to motivate your child to move and decrease screen time) and posters on how good EBRBs learnt in school can be transferred into the home (Manios et al., 2014[4]; ToyBox, 2020[5]).
OECD Best Practices Framework assessment
This section analyses ToyBox against the five criteria within OECD’s Best Practice Identification Framework – Effectiveness, Efficiency, Equity, Evidence‑base and Extent of coverage (see Box 8.1 for a high-level assessment of ToyBox). Further details on the OECD Framework can be found in Annex A.
Box 8.1. Assessment of ToyBox
Effectiveness
ToyBox is an effective intervention for reducing sedentary behaviour, increasing physical activity and improving diet. However, results were not statistically significant across the total sample for the majority of indicators.
There is no evidence to support the direct impact of ToyBox on childhood rates of overweight and obesity, however, previous studies indicate interventions combining nutrition and physical activity can reduce BMI amongst children aged 0‑5 years.
Efficiency
There is limited information on the cost-effectiveness of the ToyBox intervention with only publically available results for the intervention’s impact through changes in sedentary behaviour
The estimated incremental cost-effectiveness ratio (ICER) (cost per QALY gained) of ToyBox is estimated between EUR 1 703 and EUR 28 080 depending on gender and country
Equity
ToyBox targets obesity which disproportionately affects children from lower socio‑economic status (SES) families, however, it is unclear whether specific efforts were made to address the needs of priority population groups.
In Belgium, ToyBox was more effective at changing the behaviours of children from high-SES kindergartens, which is a key limitation of this intervention.
School-based interventions are generally considered to decrease inequalities when attendance is compulsory.
Evidence‑base
Randomised trials were used to assess the impact of ToyBox on outcomes such as sedentary behaviour, physical activity and eating behaviours
The evidence to support ToyBox is particularly strong in regards to the study design and the data collection methods used, however, like many public health studies, researchers and participants were not blinded
Extent of coverage
Participation by children ranges between 63‑74% amongst eligible kindergartens in European sites
Data on dropout rates is not available, however, this is expected to be low to none given the intervention is delivered within schools
Effectiveness
ToyBox has been shown to reduce sedentary behaviour, increase physical activity and improve eating behaviours, however, evaluation results are not conclusive
Several peer-reviewed studies evaluating the impact of ToyBox on several EBRBs are available. These include studies on:4
Sedentary behaviours:
Latomme et al. (2017[6]) found across six European countries, participation in ToyBox led to a statistically significant smaller increase in daily use of computer/video games. Specifically, children in the intervention group, on average, increased computer/video games use on weekdays by +5.48 min/day (versus +8.89 min/day in the control Group) and on weekends by +9.47 min/day (versus 15.43 min/day).
De Craemer et al. (2016[7]) analysed results in Belgium and concludes participation in ToyBox did not lead to statistically significant reductions in sedentary behaviour when examining the total sample. However, statistically significantly results for certain student groups:
Children in the intervention group among high SES kindergartens reduced sedentary behaviour on weekdays by 0.42% compared to an increase of 3.24% for the control group (p = 0.03). The same intervention group also recorded a reduction in sedentary behaviour during schools hours by ‑2%, whereas in the control group it increased by +0.47% (p = 0.04).
Among low SES kindergartens, children in the intervention group recorded a smaller increase in computer time during the weekend compared to the control group (+6.06min/day versus +12.49min/day, respectively) (p = 0.03).
Physical activity:
De Craemer et al. (2014[8]) measured the impact of ToyBox on objectively collected measures of physical activity in Belgium. Results from the study found children in the intervention group increased their moderate to vigorous and vigorous only levels of physical activity during after school hours while the opposite occurred for those in the control group (with results being statistically significant). When stratified for SES and gender, results found ToyBox was more effective in improving physical activity for boys and children in high SES kindergartens. For example, among low SES kindergartens, the intervention group only saw a small increase in vigorous physical activity after school hours compared to the intervention group in high SES kindergartens, which recorded improvements in light and moderate physical activity as well as total physical activity across the whole week.
De Craemer et al. (2017[9]) analysed the impact of ToyBox on physical activity levels across six European countries, which found no statistically significant differences in the intervention and control group across the whole sample. When analysed at the country level, the authors found average steps per day increased in the intervention group for children in Bulgaria (+542 steps/day versus ‑634 steps/day) (p = 0.03).
Eating behaviours:
Pinket et al. (2016[10]) found across six European countries studied that children in the intervention group experienced a statistically significant reduction in pre‑packed fruit juice when compared to the control group. Specifically, consumption of pre‑packaged juice fell by ‑33ml compared to ‑10ml for the control group (p < 0.001). However, results for other beverages such as water, soft drinks, sugared and chocolate milk were not statistically significant.
Lambrinou et al. (2019[11]) found ToyBox did not have a statistically significant impact on unhealthy snack consumption, however, it was shown to have a positive impact on parental rules and knowledge regarding snacking (e.g. restriction while watching television).
The impact of ToyBox on BMI is not available, however, a systematic review of the wider literature concluded that interventions targeting diet and physical activity “can reduce the risk of obesity in young children aged 0 to 5 years” (Brown et al., 2019[12]).
The long-term impact of ToyBox is not known given it was first implemented in 2012. Previous analysis by OECD, however, can shed light on the potential health and economic impact of school-based obesity prevention schemes (OECD, 2019[3]). Specifically, OECD estimated that school-based obesity prevention programs will reduce the number of cardiovascular disease (CVD) and diabetes cases by 48 154 and 136 586 each year, respectively, between 2020 and 2050 for the 36 countries analysed (which includes all ToyBox country sites) (OECD, 2019[3]).
Finally, in addition to the evidence outlined above, the WHO within its “Best Buys” guidelines for tackling NCDs recommended school-based programme to reduce unhealthy diets as well as increase physical activity (WHO, 2017[13]).
Efficiency
Available economic evaluations indicate ToyBox is cost-effective, however, publically available results are limited in their scope
Publically available studies regarding the efficiency of ToyBox focus on the impact of changes to sedentary behaviour. To calculate the effect, sedentary behaviour data was used to estimate the probability of a child being obese or not (i.e. the relative risk (RR) of being obese is 1.86 when a child engages in more than 1 hour of computer games / weekday) (Annemans and Pil, n.d.[14]). Second, to calculate obesity into adulthood, RRs were used which differ based on gender (overweight girls are at 5 times greater risk of being obese in adulthood compared to 4.4. times at risk for boys). Thirdly, the RR of developing certain NCDs (e.g. diabetes, certain cancers and stroke) for obese adults was estimated used RRs. Finally, results from step 3 were transformed into QALYs using EQ‑5D results from the published literature (Annemans and Pil, n.d.[14]).
Costs for the intervention covered several inputs including materials, training and transport with final figures estimating the cost between EUR 5 248 (USD PPP 7 672) (Poland) and EUR 28 840 (USD PPP 42 161) (Germany) per 1 000 children, depending on the country (Annemans and Pil, n.d.[14]).
Results of the cost-effectiveness analysis (CEA) are publically available for Greece and Poland. For Greece, the incremental cost-effectiveness ratio (ICER) (cost per QALY gained) was estimated at EUR 14 587 for men and EUR 28 080 for women (USD PPP 21 324 and USD PPP 41 050), assuming investment every five years (i.e. it costs between EUR 14 587 and EUR 28 080 to gain one year in full health). In Poland these figures are markedly less at EUR 3 149 and EUR 1 703 (USD PPP 4 603 and 2 490), respectively (Annemans and Pil, n.d.[14]).
Equity
ToyBox targets overweight and obesity, which disproportionately affects children from low-SES backgrounds
The literature on childhood and adult obesity indicate those from lower socio‑economic status (SES) groups are more likely to be overweight or obese. For example, an analysis of preschool-aged children in countries where ToyBox has been implemented found 17.8% of children whose mothers have a low level of education were overweight or obese compared to 12.1% for mothers with a medium/high level of education (Manios et al., 2018[15]). OECD analysis of HBSC (Heath Behaviour in School-Aged Children) data support these findings by estimating that across 26 European countries, overweight and obesity rates are 8 percentage points higher for children in the lowest income quintile compared to those in the highest income quintile (25% versus 17%) (OECD/European Union, 2018[1]).
Previous OECD analyses on the impact of obesity interventions indicate those delivered at schools are effective at tackling socio‑economic inequalities, particularly when attendance is compulsory. School-based interventions are particularly effective amongst OECD countries given high attendance levels amongst children with a low-SES.
By addressing a health issue that disproportionally affects children from lower-SES groups, ToyBox aims to reduce health inequalities. However, it is unclear whether specific efforts were made to address other disadvantaged groups such as children from different ethnic backgrounds and/or who live in remote/regional areas.
Finally, results from (De Craemer et al., 2016[7]) and (De Craemer et al., 2014[8]) indicate the intervention (as implemented in Belgium) has been more successful in changing the behaviours of children from high SES kindergartens (see “Effectiveness” results for further details). This is a key limitation of the intervention.
Evidence‑base
The quality of evidence to evaluate the intervention is strong in many areas
Several studies evaluating ToyBox are available, most of which use RCTs to assess impact. For the purpose of this case study, the study undertaken by Latomme et al. (2017[6]) has been used to assess the evidence‑base. This study was chosen given: it includes data from six European countries; it recorded statistically significant results; and the outcome of interest (i.e. sedentary behaviour) was used to evaluate efficiency.
Latomme et al. (2017[6]) utilised a randomised cluster (pre‑test/post-test) design to evaluate the impact of ToyBox on sedentary behaviours across six countries. Kindergartens were randomised using a sophisticated approach to ensure equal representation of pre‑schoolers across different socio‑economic contexts. Sedentary behaviour was measured using the Primary Caregivers’ Questionnaire (PCQ), which included questions such as “How much time does your child spend on TV-viewing?” PCQ is a valid and reliable tool for measuring sedentary behaviour in children.
Using the Quality Assessment Tool for Quantitative Studies from the Effective Public Health Practice Project, the quality of Latomme et al.’s (2017[6]) study is rated as “strong” in two areas (study design and data collection methods); “moderate” in three areas (selection bias, confounders, and withdrawals and dropouts); and “weak” in one area (blinding) (Effective Public Health Practice Project, 1998[16]). Details of the assessment are in Table 8.2.
Table 8.2. Evidence‑based assessment, ToyBox
|
Assessment category |
Question |
Score |
|---|---|---|
|
Selection bias |
Are the individuals selected to participate in the study likely to be representative of the target population? |
Very likely |
|
What percentage of selected individuals agreed to participate? |
Can’t tell |
|
|
Selection bias score: Moderate |
||
|
Study design |
Indicate the study design |
RCT |
|
Was the study described as randomised? |
Yes |
|
|
Was the method of randomisation described? |
Yes |
|
|
Was the method of randomisation appropriate? |
Yes |
|
|
Study design score: Strong |
||
|
Confounders |
Were there important differences between groups prior to the intervention? |
Can’t tell |
|
What percentage of potential confounders were controlled for? |
Most (80‑100%) |
|
|
Confounders score: Moderate |
||
|
Blinding |
Was the outcome assessor aware of the intervention or exposure status of participants? |
Yes |
|
Were the study participants aware of the research question? |
Yes |
|
|
Blinding score: Weak |
||
|
Data collection methods |
Were data collection tools shown to be valid? |
Yes |
|
Were data collection tools shown to be reliable? |
Yes |
|
|
Data collection methods score: Strong |
||
|
Withdrawals and dropouts |
Were withdrawals and dropouts reported in terms of numbers and/or reasons per group? |
Yes |
|
Indicate the percentage of participants who completed the study? |
60‑70% |
|
|
Withdrawals and dropouts score: Moderate |
||
Source: Effective Public Health Practice Project (1998[16]), “Quality assessment tool for quantitative studies”, https://www.nccmt.ca/knowledge-repositories/search/14.
Extent of coverage
In kindergartens offering ToyBox, between 63‑74% of children participate
Participation rates in ToyBox differ depending on the country. In Malta, of the 37 schools who were invited to participate, 27 (14 who were independents and 13 church schools) chose to participate (organisation participation rate of 73%). Of the 991 children eligible to participate in these schools, 733 parents gave consent for their children to participate (individual level participation rate of 74%). Comparatively, across the six other European sites (i.e. Belgium, Bulgaria, Germany, Greece, Poland and Spain) the individual participation rate was lower at 63.3% (Manios et al., 2014[4]).
Policy options to enhance performance
Enhancing effectiveness
A review of various school-based childhood obesity interventions identified a range of factors associated with success including parental and community involvement as well as appropriate training and support for teachers (see Box 8.2). Based on a gap analysis comparing these factors against the design of ToyBox, several policy options to enhance effectiveness are outlined below.
Increase parental involvement
The importance of involving parents in school-based nutrition intervention is reflected in WHO’s Nutrition-Friendly Schools Initiative (NFSI) (WHO, 2021[17]). Specifically, a review of the available evidence found parental involvement was positively associated with better health outcomes (e.g. BMI and dietary outcomes), particularly for younger age groups. Further, direct methods of involving parents in school-based interventions (e.g. face‑to-face as opposed to newsletters) is associated with better health outcomes (WHO, 2021[17]).
At present, ToyBox engages parents through the provision of tip cards and posters to encourage healthy behaviours in the home. To further boost parental involvement, administrators could consider more interactive strategies such as school information sessions with parents; joint child-school-parent activities; school-led family cooking workshops; family activity nights; and child-parent goal setting (Lloyd et al., 2018[18]; Waters et al., 2011[19]; National Cancer Institute, 2020[20]). Given lack of time is a key barrier for parental involvement (e.g. due to work commitments or over-saturation of school activities), other more accessible activities could also be considered, for example, phone and internet-based services and support (Wolfenden et al., 2012[21]). Further, staff could use the opportunity at events with high attendance from parents to further promote the ToyBox intervention (e.g. school carnivals, fetes, and fundraisers) as opposed to relying on attendance at separate information sessions (Jones et al., 2014[22]).
Create an holistic approach involving all key stakeholders
Community involvement in nutrition action in schools is recommended by the WHO – NFSI essential criteria 2.2 (“Activities for families and community, community involvement and outreach in the area of nutrition and health related issue”) (WHO, 2021[17]). Example policies to boost community involvement in ToyBox include procuring healthy fruit and vegetables from local suppliers (in line with EU’s Farm to Fork Strategy) (European Commission, 2019[23]), and collaborating with community providers with relevant facilities (e.g. kitchens for preparing and cooking healthy meals, edible community gardens, gyms) (Gerritsen, 2016[24]).
Ensure appropriate training for teachers
One of the essential criteria within WHO’s NFSI is to ensure “school staff training in nutrition and health related issues” (WHO, 2021[17]). A review of the available evidence found the provision of ongoing training, support and communication positively affects child health outcomes such as BMI, physical activity levels and diet (WHO, 2021[17]).
ToyBox provides teachers with an initial 1.5‑hour training session in addition to a guidebook and classroom activity guides to help structure lessons. Given the complexity of obesity, expanding the amount of training teachers receive could improve health outcomes particularly if confidence in delivering nutrition and activity based activities is low amongst teachers. At a wider, systematic level, obesity prevention topics could be added to the curriculum to become a kindergarten teacher (CDC, 2017[25]).
Increase the duration of the intervention
Reviews of school-based obesity interventions found those that last longer than one year were more likely to achieve their objectives (Silveira et al., 2011[26]; Gonzalez-Suarez et al., 2009[27]; WHO, 2021[17]). Extending ToyBox beyond 24 weeks may therefore yield better outcomes.
Box 8.2. Example success factors for school-based obesity interventions
This box lists several success factors related to obesity interventions in schools. The list draws upon the WHO’s Nutrition Friendly Schools Initiative, however, it is not exhaustive. For further details on WHO’s Nutrition Friendly Schools Initiative, see: https://apps.who.int/iris/handle/10665/338781
Longer duration: a systematic review of school-based nutrition education programs found interventions that last longer than one year were more likely to demonstrate effectiveness (Silveira et al., 2011[26]). These results are supported by an earlier meta‑analysis which found school-based obesity interventions implemented for longer than a year reduced obesity levels (Gonzalez-Suarez et al., 2009[27]).
Holistic approach involving the community: given the complexity of childhood obesity, schools are increasingly moving towards holistic approaches to reducing BMI (often referred to as “comprehensive school health” or “health promoting schools”) (Okely and Hammersley, 2018[28]). Holistic approaches to reducing obesity aim to change the school and community environment in order for the easy choice to be the healthy choice.
Parental involvement: obesity is a complex health issue and requires initiatives implemented in both the school and home environment. The importance of transferring knowledge and skills regarding healthy eating and exercise in schools to the home is supported by a recent article which found nearly all successful school-based obesity interventions promoted family involvement (Waters et al., 2011[19]; Okely and Hammersley, 2018[28]; Ash et al., 2017[29]).
Training and support for teachers: to successfully implement school-based obesity interventions all staff involved must receive the appropriate training and professional development support and as well as ongoing capacity building and support (Jones et al., 2014[22]).
Enhancing efficiency
Efficiency is calculated by obtaining information on effectiveness and expressing it in relation to inputs used. Therefore policies to boost effectiveness without significant increases in costs will have a positive impact on efficiency.
Enhancing equity
The impact of ToyBox on different outcome indicators of interest indicate the intervention is more effective among children in high-SES kindergartens (see “Effectiveness”). Possible reasons for this disparity include:
Lower levels of access to outdoor space – e.g. private gardens or nearby parks – for children living in low-SES areas thereby making it difficult for parents/caregivers to implement ToyBox recommendations on physical activity (De Craemer et al., 2014[8])
Lower levels of health literacy among parents/caregivers in low-SES areas
Less funding among schools in low-SES areas to implement and deliver ToyBox as intended.
The points outlined above represent possible explanations only – therefore, future studies should explore this topic in further detail to understand why ToyBox affects SES groups differently. Findings from this research can be used to adapt ToyBox to ensure it reduces, as opposed to exacerbates, existing health inequalities.
Without this information, specific recommendations on how to enhance equity for ToyBox is not possible. Nevertheless, previous research on school-based obesity interventions in low SES areas can shed light on effective strategies (Box 8.3).
Box 8.3. Effective school-based obesity strategies in low-SES areas
Research by Lambrinous et al. (2020[30]) identified several strategies to increase the effectiveness of school-based obesity interventions in low-SES areas. At a high level, these include:
Undertaking a situational analysis and formative research to guide the implementation and delivery of school-based obesity interventions.
Focusing less on education and more on changing the environment to promote healthy lifestyles, parental engagement and interactive activities.
Adapting the programme so that it culturally aligns with the community.
Collaborating with community stakeholders.
Enhancing the evidence‑base
Several RCTs evaluating ToyBox across multiple European sites are available (see assessment of “Effectiveness”). These studies focus on intermediate outcomes namely changes in sedentary behaviour, physical activity and eating behaviours. Given ToyBox is ultimately interested in reducing rates of overweight and obesity in children, further studies are encouraged to include objectively measured BMI as an outcome.
To assist policy makers compare the performance of ToyBox against similar school-based interventions, programme administrators may wish to convert data into indicators that are universally recognised (and therefore frequently reported). For example:
Percentage of children who consume fruits at least once per day
Percentage of children who consume vegetables at least once per day
Percentage of children whose weight‑for-height is greater than 2 standard deviations above WHO Child Growth Standards median5
Percentage of children whose weight‑for-height is greater than 3 standard deviations above WHO Child Growth Standards median6
Percentage of adults (i.e. parents) who consume recommended amount of fruits and vegetables everyday (i.e. 400 grammes)
To better understand the impact of ToyBox across different groups of children, a breakdown of evaluation results by priority population groups is encouraged. Previous studies have done this by presenting results by SES status and gender, however, it is also important to understand how ToyBox affects children from different ethnic backgrounds as well as by location (e.g. rural versus urban kindergartens, if possible). A breakdown of results by ethnicity, for example, would be an important contributor to the wider literature on school-based obesity interventions given the current paucity of available studies (Amini et al., 2015[31]).
To evaluate the long-term impact of ToyBox on rates of obesity, it is important to collect data frequently using the same measures, and, ideally, the same individuals (i.e. panel data). Longitudinal panel data is considered the “gold standard” as it reduces bias by taking into account differences across individuals. Given this policy requires long-term funding and support, responsibility for this policy option lies with higher-level policy makers as opposed to ToyBox administrators.
Enhancing extent of coverage
Implementation of ToyBox in Malta recorded a participation rate of around 70% at the both kindergarten and individual level. These figures are higher than those recorded in other ToyBox European sites yet lower than the 85% figure considered high for school-based obesity interventions (Fung et al., 2012[32]). In future rounds of student recruitment, a multi-pronged approach for boosting participation could be considered. Example strategies include (Jones et al., 2014[22]):
Promoting the intervention with support from government organisations to enhance trust among parents. For example, the Good for Kids, Good for Life intervention in New South Wales (Australia) was promoted using a support letter from the State’s Chief Health Officer. Policy makers however should first consider if messaging from government organisations may in fact reduce uptake among disadvantaged groups. For example, there is evidence showing those with a low SES and/or lower level of education are more anxious and suspicious of prevention messaging from public health authorities (Peretti-Watel and Constance, 2009[33]).
Promoting ToyBox as a healthy behaviour intervention that aims to boost enjoyable physical activity and healthy eating as opposed to obesity prevention. By framing ToyBox in a positive light, this may reduce stigma associated with participation.
Increasing efforts to recruit students whose parents are from culturally or linguistically diverse backgrounds given consent may be harder to obtain (for example, by including staff members who are knowledgeable about relevant cultural characteristics).
Promoting the intervention over a sufficiently long time period using colourful, “eye‑grabbing” material in conjunction with frequent digital and face‑to-face follow-up with parents.
Transferability
This section explores the transferability of ToyBox and is broken into three components: 1) an examination of previous transfers; 2) a transferability assessment using publically available data; and 3) additional considerations for policy makers interested in transferring ToyBox.
Previous transfers
ToyBox operates in six EU countries – Belgium, Bulgaria, Germany, Greece, Malta, Poland and Spain. As outlined under “Effectiveness”, ToyBox has led to positive outcomes across these countries, such as reducing the level of sedentary behaviour. Following the success of ToyBox, two non-EU countries, Scotland and Malaysia, transferred the intervention to their own country. The impact of ToyBox in these countries is not publically available.
A full list of reports and publications produced by the ToyBox EU study are at: http://www.toybox-study.eu/.
Transferability assessment
The following section outlines the methodological framework to assess transferability and results from the assessment.
Methodological framework
Details on the methodological framework to assess transferability can be found in Annex A.
Several indicators to assess the transferability of ToyBox were identified (see Table 8.2). Indicators were drawn from international databases and surveys to maximise coverage across OECD and non-OECD European countries. Please note the assessment is intentionally high level given the availability of public data covering OECD and non-OECD European countries.
The owner setting for the transferability assessment of ToyBox is Spain given this was the only country where ToyBox operates and where data for all indicators was available.
Table 8.3. Indicators to assess the transferability of ToyBox
|
Indicator |
Reasoning |
Interpretation |
|---|---|---|
|
Sector specific context (early childhood education) |
||
|
Enrolment rate in early childhood education (children aged 3‑5 years) |
ToyBox targets children aged 3‑4 who attend early childhood education (i.e. kindergarten). Therefore, ToyBox will have a greater extent of coverage in countries with higher enrolment rates. |
🡹 = “more transferable” |
|
Student to teacher ratio in early childhood education |
ToyBox will be more transferable to countries with a low student to teacher ratios given a reduced workload. |
🡻 = “more transferable” |
|
% of teachers who are highly motivated* |
ToyBox will be more transferable to countries whose teachers are highly motivated |
🡹 = “more transferable” |
|
Political context |
||
|
Childhood obesity strategy |
ToyBox will be more transferable to countries that prioritise childhood obesity |
“Yes” = more transferable |
|
Economic context |
||
|
Annual expenditure on early childhood education and care per child in USD, converted to purchasing power parities (PPP) |
ToyBox will be more successful in countries who spend more on early childhood education and care |
🡹 = “more transferable” |
* This indicator represents the proportion of teacher who report that influencing the development of children and young people is of moderate or high importance in deciding to become a better teacher.
Source: OECD Health Statistics 2021, https://doi.org/10.1787/health-data-en; WHO (n.d.[34]), “Global Health Observatory”, https://www.who.int/data/gho; OECD (2022[35]), “OECD data: Education”, https://data.oecd.org/education.htm; OECD (2019[3]), The Heavy Burden of Obesity: The Economics of Prevention, https://dx.doi.org/10.1787/67450d67-en.
Results
Results from the transfer assessment show ToyBox is likely to have political support given it targets childhood obesity, which is a political priority in most countries (see Table 8.3). Further, in countries where data is available, teacher motivation levels and spending on early childhood education and care (ECEC) are on average higher than the owner setting, Spain. For example, Spain spends USD PPP 7 759 on ECEC compared to USD PPP 9 729, which is the average spend across OECD and non-OECD EU countries. Nevertheless, ToyBox may have a lower extent of coverage in other countries given enrolment rates in ECEC are relatively high in Spain (97% versus 83%, which is the OECD and non-OECD EU average).
Table 8.4. Transferability assessment by country, ToyBox (OECD and non-OECD European countries)
A darker shade indicates ToyBox is more suitable for transferral in that particular country
|
Enrolment rate by age – 3‑5 years (%) |
Ratio of students to teaching staff in educational institutions, primary |
Teacher motivation level (%)* |
Childhood obesity strategy |
Funding for early childhood education, USD PPP |
|
|---|---|---|---|---|---|
|
Spain |
97 |
14 |
89 |
Yes |
7 759 |
|
Australia |
57 |
15 |
96 |
No** |
7 863 |
|
Austria |
90 |
12 |
96 |
Yes |
11 009 |
|
Belgium † |
98 |
13 |
95 |
Yes |
n/a |
|
Bulgaria † |
n/a |
n/a |
95 |
Yes |
n/a |
|
Canada |
n/a |
17 |
99 |
Yes |
n/a |
|
Chile |
79 |
19 |
97 |
Yes |
6 727 |
|
Colombia |
64 |
23 |
98 |
Yes |
n/a |
|
Costa Rica |
60 |
12 |
n/a |
No |
n/a |
|
Croatia |
n/a |
n/a |
95 |
No |
n/a |
|
Cyprus |
n/a |
n/a |
n/a |
Yes |
n/a |
|
Czech Republic |
87 |
19 |
93 |
Yes |
6 109 |
|
Denmark |
99 |
12 |
94 |
Yes |
18 502 |
|
Estonia |
91 |
13 |
88 |
Yes |
8 137 |
|
Finland |
82 |
14 |
83 |
Yes |
13 186 |
|
France |
1.00 |
19 |
92 |
No |
8 894 |
|
Germany † |
94 |
15 |
n/a |
Yes |
12 817 |
|
Greece † |
n/a |
9 |
n/a |
No |
n/a |
|
Hungary |
92 |
10 |
93 |
Yes |
7 401 |
|
Iceland |
97 |
11 |
79 |
Yes |
17 310 |
|
Ireland |
60 |
15 |
n/a |
Yes |
4 568 |
|
Israel |
1.00 |
15 |
97 |
Yes |
5 049 |
|
Italy |
91 |
12 |
79 |
Yes |
8 780 |
|
Japan |
n/a |
16 |
89 |
Yes |
7 609 |
|
Latvia |
93 |
12 |
93 |
Yes |
6 222 |
|
Lithuania |
86 |
11 |
91 |
Yes |
6 677 |
|
Luxembourg |
85 |
9 |
n/a |
Yes |
19 326 |
|
Malta † |
n/a |
n/a |
96 |
Yes |
n/a |
|
Mexico |
73 |
26 |
99 |
Yes |
2 570 |
|
Netherlands |
89 |
16 |
86 |
Yes |
6 959 |
|
New Zealand |
n/a |
17 |
96 |
Yes |
9 599 |
|
Norway |
97 |
10 |
89 |
Yes |
19 663 |
|
Poland † |
n/a |
10 |
n/a |
Yes |
7 164 |
|
Portugal |
91 |
12 |
94 |
No |
n/a |
|
Republic of Korea |
n/a |
17 |
n/a |
Yes |
n/a |
|
Romania |
n/a |
n/a |
98 |
Yes |
n/a |
|
Slovak Republic |
78 |
18 |
93 |
Yes |
6 123 |
|
Slovenia |
91 |
10 |
89 |
Yes |
9 329 |
|
Sweden |
94 |
14 |
94 |
Yes |
15 442 |
|
Turkey |
38 |
17 |
98 |
Yes |
n/a |
|
United Kingdom |
72 |
20 |
n/a |
Yes |
5 971 |
|
United States |
n/a |
15 |
99 |
Yes |
n/a |
Note: The shades of blue represent the distance each country is from the country in which the intervention currently operates, with a darker shade indicating greater transfer potential based on that particular indicator (see Annex A for further methodological details). *Results in Canada and the United Kingdom represents Alberta and England only, respectively. Further, results for Belgium are an average of the Belgium Flemish and Belgium French teachers. **There are a number of strategies focusing on children and young people within the proposed National Obesity Prevention Strategy (2022‑2032). † = countries that have already transferred ToyBox to their country. n/a = data not available; PPP = purchasing power parity.
Source: OECD Health Statistics 2021, https://doi.org/10.1787/health-data-en; WHO (n.d.[34]), “Global Health Observatory”, https://www.who.int/data/gho; OECD (2022[35]), “OECD data: Education”, https://data.oecd.org/education.htm; OECD (2019[3]), The Heavy Burden of Obesity: The Economics of Prevention, https://dx.doi.org/10.1787/67450d67-en.
To help consolidate findings from the transferability assessment above, countries have been clustered into one of three groups, based on indicators reported in Table 8.3. Countries in clusters with more positive values have the greatest transfer potential. For further details on the methodological approach used, please refer to Annex A.
Key findings from each of the clusters are below with further details in Figure 8.2 and Table 8.4:
Countries in cluster one have political, economic and sector specific arrangements in place to transfer ToyBox. Countries in this cluster are therefore less likely to experience issues in implementing and operating ToyBox in their local context.
Countries in cluster two also have political and sector specific arrangements in place to transfer ToyBox, but would benefit from increasing spending on early childhood education and care (ECEC) to ensure affordability.
Countries in cluster three would benefit from undertaking further analyses to ensure ToyBox is affordable (given relatively low levels of funding for early childhood education) and that it aligns with overarching political priorities.
It is important to note that Spain and Greece, which operate ToyBox, fall under clusters two and three, respectively, meaning conditions in which these clusters could improve on, although ideal, are not pre‑requisites.
Figure 8.1. Transferability assessment using clustering, ToyBox
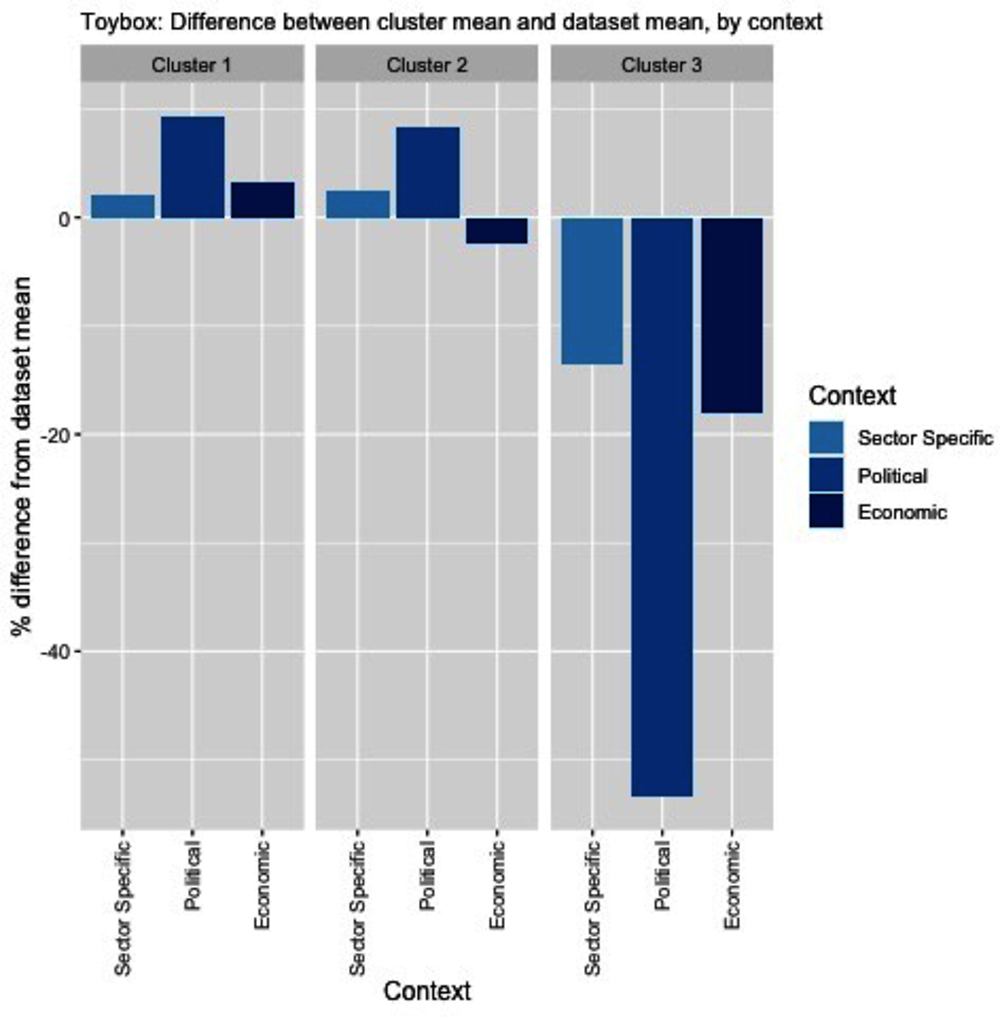
Note: Bar charts show percentage difference between cluster mean and dataset mean, for each indicator.
Source: OECD Health Statistics 2021, https://doi.org/10.1787/health-data-en; WHO (n.d.[34]), “Global Health Observatory”, https://www.who.int/data/gho; OECD (2022[35]), “OECD data: Education”, https://data.oecd.org/education.htm; OECD (2019[3]), The Heavy Burden of Obesity: The Economics of Prevention, https://dx.doi.org/10.1787/67450d67-en.
Table 8.5. Countries by cluster, ToyBox
|
Cluster 1 |
Cluster 2 |
Cluster 3 |
|---|---|---|
|
Austria Belgium Bulgaria Chile Colombia Czech Republic Denmark Germany Hungary Ireland Israel Latvia Lithuania Luxembourg Mexico Norway Poland Slovenia Sweden Switzerland United Kingdom |
Canada Estonia Finland Iceland Italy Japan Malta Netherlands New Zealand Republic of Korea Romania Slovak Republic Spain Turkey United States |
Australia Costa Rica Croatia France Greece Portugal |
Note: Due to high levels of missing data, Cyprus is not included in the analysis.
New indicators to assess transferability
Data from publically available datasets is not ideal to assess the transferability of ToyBox. For example, there is no international data measuring the level of parental engagement in schools. Therefore, Box 8.4 outlines several new indicators policy makers should consider before transferring ToyBox.
Box 8.4. New indicators to assess transferability
In addition to the indicators within the transferability assessment, policy makers are encouraged to collect data for the following indicators, as well as those outlined within WHO’s “Making every school a health-promoting school” report (WHO, 2021[36]).
Population context
What is the ethnicity and cultural diversity of the target population?
What is the level of acceptability of ToyBox amongst parents?*
What is the level of health literacy amongst parents? (e.g. knowledge regarding what constitutes health eating, and the impact of healthy eating and exercise on overall health and well-being)
What is the level of parental engagement with schools and teachers?
What is the level of physical inactivity amongst children?
Sector specific context (early childhood education)
What is the level of acceptability of ToyBox amongst teachers and the Head of School?*
Does the school have an overarching policy/framework in place to promote healthy lifestyles amongst students?
What is the level of health literacy amongst teachers? (How comfortable do teachers feel activities part of ToyBox?)
Does the school already include healthy lifestyle lessons in the formal curricula?
What infrastructure is available in schools for children to be active? (e.g. playgrounds)
How much greenspace is there for children to be physically active in the school environment?
Do kindergartens have access to a canteen on site? Or is food provided by parents?
What are the regulations/legislation regarding data collection from young children?
Political context
Has the intervention received political support from key decision-makers?
Has the intervention received commitment from key decision-makers?
Economic context
What is the cost of implementing the intervention in the target setting?
* Research into acceptability of ToyBox among teachers and parents has previously been undertaken in Scotland. See Malden et al. (2020[37]) for further details.
Conclusion and next steps
ToyBox is a school-based childhood obesity intervention targeting children aged 3‑4 years. The intervention aims to alter four energy-related behaviours with the greatest impact on weight, as identified within the academic literature. The intervention operates in several European countries and two non-EU countries.
ToyBox has led to statistically significant improvements in intermediate outcomes related to obesity including reductions in sedentary behaviour. However, statistically significant results typically do not apply to the whole population being studied or for all indicators being measured – for example, results from ToyBox in Belgium indicate the intervention is more effective among high SES kindergartens. Further, there is limited evidence on the impact of ToyBox on BMI directly (a final health outcome). Regarding efficiency, economic evaluations of ToyBox found it is cost-effective, however, these results are limited in scope (i.e. by focusing on sedentary behaviour only).
An assessment of ToyBox against the OECD Framework as well as a review of the literature on school-based obesity prevention programs identified several policy options to enhance implementation. These include, but are not limited to: boosting parental and community engagement; increasing duration beyond 24 weeks; integrating obesity prevention into the curriculum for kindergarten teachers; and boosting participation by using government supported promotional material. In addition, researchers are encouraged to report the impact of ToyBox on BMI directly, and, to the extent possible, provide results by different population groups beyond SES and gender (e.g. by ethnicity and location (urban versus regional)).
Box 8.5 outlines next steps for policy makers and funding agencies regarding ToyBox.
Box 8.5. Next steps for policy makers and funding agencies
Next steps for policy makers and funding agencies to enhance ToyBox are listed below:
Support policy efforts to provide teachers with appropriate training to deliver nutrition and physical activity lessons, for example, by including these topics in the curriculum to become a kindergarten teacher
Support policy efforts to boost population health literacy in order to motivate parental involvement school-based obesity programs
Ensure funding for future scale‑up and transfer efforts
Promote findings from the ToyBox case study to better understand what countries/regions are interested in transferring the intervention
Promote “lessons learnt” from regions that have transferred ToyBox to their local setting.
References
[31] Amini, M. et al. (2015), Effect of school-based interventions to control childhood obesity: A review of reviews, Isfahan University of Medical Sciences(IUMS), https://doi.org/10.4103/2008-7802.162059.
[14] Annemans, L. and L. Pil (n.d.), Building a framework for long-term nutrition economic evaluations of interventions to address childhood obesity: The ToyBox study, Ghent University, https://ec.europa.eu/jrc/sites/jrcsh/files/20151112-13-health-nutrition-economics-pil_en.pdf.
[29] Ash, T. et al. (2017), Family-based childhood obesity prevention interventions: A systematic review and quantitative content analysis, BioMed Central Ltd., https://doi.org/10.1186/s12966-017-0571-2.
[12] Brown, T. et al. (2019), “Interventions for preventing obesity in children”, Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.cd001871.pub4.
[25] CDC (2017), Acting Early to Prevent Obesity, CDC Division of Nutrition, Physical Activity and Obesity, https://www.cdc.gov/obesity/downloads/acting-early-to-prevent-obesity.pdf.
[7] De Craemer, M. et al. (2016), “The effect of a cluster randomised control trial on objectively measured sedentary time and parental reports of time spent in sedentary activities in Belgian preschoolers: The ToyBox-study”, International Journal of Behavioral Nutrition and Physical Activity, Vol. 13/1, https://doi.org/10.1186/s12966-015-0325-y.
[8] De Craemer, M. et al. (2014), “The effect of a kindergarten-based, family-involved intervention on objectively measured physical activity in Belgian preschool boys and girls of high and low SES: The ToyBox-study”, International Journal of Behavioral Nutrition and Physical Activity, Vol. 11/1, https://doi.org/10.1186/1479-5868-11-38.
[9] De Craemer, M. et al. (2017), “Effect and process evaluation of a kindergarten-based, family-involved cluster randomised controlled trial in six European countries on four- to six-year-old children’s steps per day: The ToyBox-study”, International Journal of Behavioral Nutrition and Physical Activity, Vol. 14/1, https://doi.org/10.1186/s12966-017-0574-z.
[16] Effective Public Health Practice Project (1998), Quality assessment tool for quantitative studies, https://www.nccmt.ca/knowledge-repositories/search/14.
[23] European Commission (2019), Farm to Fork Strategy: For a fair, healthy and environmentally-friendly food system, https://ec.europa.eu/food/sites/food/files/safety/docs/f2f_action-plan_2020_strategy-info_en.pdf.
[32] Fung, C. et al. (2012), “From “best practice” to “next practice”: the effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity”, International Journal of Behavioral Nutrition and Physical Activity, Vol. 9/1, p. 27, https://doi.org/10.1186/1479-5868-9-27.
[24] Gerritsen, S. (2016), “Nutrition education for early childhood managers, teachers and nursery cooks: a prerequisite for effective obesity prevention”, Public Health, Vol. 140, pp. 56-58, https://doi.org/10.1016/j.puhe.2016.05.025.
[27] Gonzalez-Suarez, C. et al. (2009), “School-Based Interventions on Childhood Obesity. A Meta-Analysis”, American Journal of Preventive Medicine, Vol. 37/5, pp. 418-427, https://doi.org/10.1016/j.amepre.2009.07.012.
[22] Jones, R. et al. (2014), “School-based obesity prevention interventions: Practicalities and considerations”, Obesity Research and Clinical Practice, Vol. 8/5, pp. e497-e510, https://doi.org/10.1016/j.orcp.2013.10.004.
[11] Lambrinou, C. et al. (2019), “Mediators of the effectiveness of a kindergarten-based, family-involved intervention on pre-schoolers’ snacking behaviour: The ToyBox-study”, Public Health Nutrition, Vol. 22/1, pp. 157-163, https://doi.org/10.1017/S1368980018002653.
[6] Latomme, J. et al. (2017), “Effect and process evaluation of a kindergarten-based, family-involved intervention with a randomized cluster design on sedentary behaviour in 4- to 6-year old European preschool children: The ToyBoxstudy”, PLoS ONE, Vol. 12/4, https://doi.org/10.1371/journal.pone.0172730.
[18] Lloyd, J. et al. (2018), “Effectiveness of the Healthy Lifestyles Programme (HeLP) to prevent obesity in UK primary-school children: a cluster randomised controlled trial”, The Lancet Child and Adolescent Health, Vol. 2/1, pp. 35-45, https://doi.org/10.1016/S2352-4642(17)30151-7.
[37] Malden, S. et al. (2020), “Assessing the acceptability of an adapted preschool obesity prevention programme: ToyBox‐Scotland”, Child: Care, Health and Development, Vol. 46/2, pp. 213-222, https://doi.org/10.1111/cch.12736.
[4] Manios, Y. et al. (2014), “Designing and implementing a kindergarten-based, family-involved intervention to prevent obesity in early childhood: the ToyBox-study.”, Obesity reviews : an official journal of the International Association for the Study of Obesity, Vol. 15 Suppl 3/SUPPL.3, pp. 5-13, https://doi.org/10.1111/obr.12175.
[15] Manios, Y. et al. (2018), “Prevalence and sociodemographic correlates of overweight and obesity in a large Pan-European cohort of preschool children and their families: The ToyBox-study”, Nutrition, Vol. 55-56, pp. 192-198, https://doi.org/10.1016/j.nut.2018.05.007.
[20] National Cancer Institute (2020), Alberta Project Promoting active Living and healthy Eating (APPLE Schools), https://rtips.cancer.gov/rtips/programDetails.do?programId=3624004.
[35] OECD (2022), OECD data: Education, https://data.oecd.org/education.htm.
[3] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/67450d67-en.
[1] OECD/European Union (2018), Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris/European Union, Brussels, https://doi.org/10.1787/health_glance_eur-2018-en.
[28] Okely, A. and M. Hammersley (2018), School–home partnerships: the missing piece in obesity prevention?, Elsevier B.V., https://doi.org/10.1016/S2352-4642(17)30154-2.
[30] on behalf of the Feel4Diabetes-study group (2020), “Effective strategies for childhood obesity prevention via school based, family involved interventions: a critical review for the development of the Feel4Diabetes-study school based component”, BMC Endocrine Disorders, Vol. 20/S2, https://doi.org/10.1186/s12902-020-0526-5.
[33] Peretti-Watel, P. and J. Constance (2009), “Comment les fumeurs pauvres justifient-ils leur pratique et jugent-ils la prévention ?”, Déviance et Société, Vol. 33/2, p. 205, https://doi.org/10.3917/ds.332.0205.
[10] Pinket, A. et al. (2016), “Effect and process evaluation of a cluster randomized control trial on water intake and beverage consumption in preschoolers from six European countries: The ToyBox-study”, PLoS ONE, Vol. 11/4, https://doi.org/10.1371/journal.pone.0152928.
[26] Silveira, J. et al. (2011), Effectiveness of school-based nutrition education interventions to prevent and reduce excessive weight gain in children and adolescents: A systematic review, J Pediatr (Rio J), https://doi.org/10.2223/JPED.2123.
[5] ToyBox (2020), ToyBox – a European multi-country study to develop an obesity prevention programme specifically for pre-school children, http://www.toybox-study.eu/?q=en/node/1.
[19] Waters, E. et al. (2011), Interventions for preventing obesity in children, John Wiley and Sons Ltd, https://doi.org/10.1002/14651858.CD001871.pub3.
[36] WHO (2021), Making every school a health-promoting school: Global standards and indicators, World Health Organization and the United Nations Educational, Scientific and Cultural Organization, https://www.who.int/publications/i/item/9789240025059.
[17] WHO (2021), Nutrition action in schools: a review of evidence related to the nutrition-friendly schools initiative, https://www.who.int/publications/i/item/9789241516969.
[2] WHO (2018), WHO European Childhood Obesity Surveillance Initiative (COSI).
[13] WHO (2017), Best buys and other recommended interventions for the prevention and control of noncommunicable diseases, WHO, Geneva, https://apps.who.int/iris/bitstream/handle/10665/259232/WHO-NMH-NVI-17.9-eng.pdf;jsessionid=3E76AC01272E9377F8382B8BC19545AF?sequence=1 (accessed on 10 September 2019).
[34] WHO (n.d.), Global Health Observatory, https://www.who.int/data/gho (accessed on 25 August 2021).
[21] Wolfenden, L. et al. (2012), “Engaging parents in child obesity prevention: Support preferences of parents”, Journal of Paediatrics and Child Health, Vol. 48/2, https://doi.org/10.1111/j.1440-1754.2010.01776.x.
Notes
← 1. Participating countries include Belgium, Bulgaria, Germany, Greece, Malta, Spain and Poland.
← 2. The intervention concentrates on each EBRBs for four weeks (16 weeks) which is then repeated, however, for only two weeks (eight weeks).
← 3. In addition, the importance of good oral health is also being emphasised in Malta.
← 4. An evaluation of the ToyBox (Malta) was planned for year 2020, however, due to unforeseen barriers caused by COVID‑19, the evaluation was put on hold indefinitely.
← 5. See following link for WHO Child Growth Standards: https://www.who.int/childgrowth/standards/weight_for_height/en/ (indicator designed for children under five years of age)
← 6. Ibid.
