This chapter covers the case study of Physical Activity on Prescription (PAP), a programme in Sweden where health professionals write individualised prescriptions for physical activity to patients. The case study includes an assessment of PAP against the five best practice criteria, policy options to enhance performance and an assessment of its transferability to other OECD and EU27 countries.
Healthy Eating and Active Lifestyles

4. Physical Activity on Prescription
Abstract
Physical Activity on Prescription (PAP): Case study overview
Description: Under the Swedish PAP programme, health professionals write individualised prescriptions for physical activity based on the patient’s health status, motivation, prior experiences and preferences. A handbook is available detailing the latest evidence on physical activity and its impact on specific diseases. After the prescription, a follow-up meeting is used to adjust the prescription and foster motivation.
Best practice assessment:
Table 4.1. OECD best practice assessment of Physical Activity on Prescription
|
Criteria |
Assessment |
|---|---|
|
Effectiveness |
The implementation of PAP with a coverage rate of 2.39% in Sweden is estimated to result in a cumulative gain of 10 995 LYs and 13 113 DALY by 2050. |
|
Efficiency |
Due to its low cost, the PAP intervention is cost saving, with a net saving of approximately SEK 91 000 (EUR 9 000) per DALY gained. |
|
Equity |
Data from the region of Stockholm suggest that PAP reaches people across socio‑economic groups. However, as implementation of the intervention is decentralised, variation across the regions risks creating inequalities. |
|
Evidence‑base |
The RCT upon which the effectiveness modelling parameters are based is rated as strong, and there are a large number of other RCTs and observational studies of the PAP programme. An evidence‑based handbook with physical activity recommendations was developed and is regularly being updated. |
|
Extent of coverage |
In 2019, 45 000 prescriptions for physical activity were prescribed in primary care, equating to 5.6 prescriptions per 1 000 population. However, in some regions the coverage rate was considerably higher. |
Enhancement options: Evidence suggests that there are a number of factors that can enhance the effectiveness of the intervention, such as prescribing a higher frequency of physical activity rather than intensity. To enhance the equity of the intervention, a national register can help provide the information needed to ensure that the programme is implemented effectively and equitably in all regions. A high population coverage is crucial for this intervention, and can be enhanced by increasing knowledge and affirmative attitude among the health care professionals, clear and supportive management for the intervention, putting in place supporting structures, and potentially through incentives.
Transferability: Transfer of the Swedish PAP intervention to nine other European countries has already started under the EU-funded “European Physical Activity on Prescription Model” project (EUPAP). Based on publically available indicators, many countries have structures and policies in place to support PAP.
Conclusion: PAP is a cost-effective, evidence‑based intervention which can help increase physical activity, prevent disease and reduce health care expenditures.
Intervention description
For almost 20 years, Sweden has used the physical activity on prescription (PAP) intervention to address low levels of physical activity in the adult population (Onerup et al., 2019[1]). The intervention is currently being transferred to nine other EU countries as part of EUPAP – a three‑year project co-funded by the European Commission (EUPAP.org, n.d.[2]).
The intervention consists of five key components (EUPAP, 2020[3]):
Person-centred individualised counselling
Written prescription
Evidence based physical activity recommendation
Follow-up
Supporting environment, community-based network.
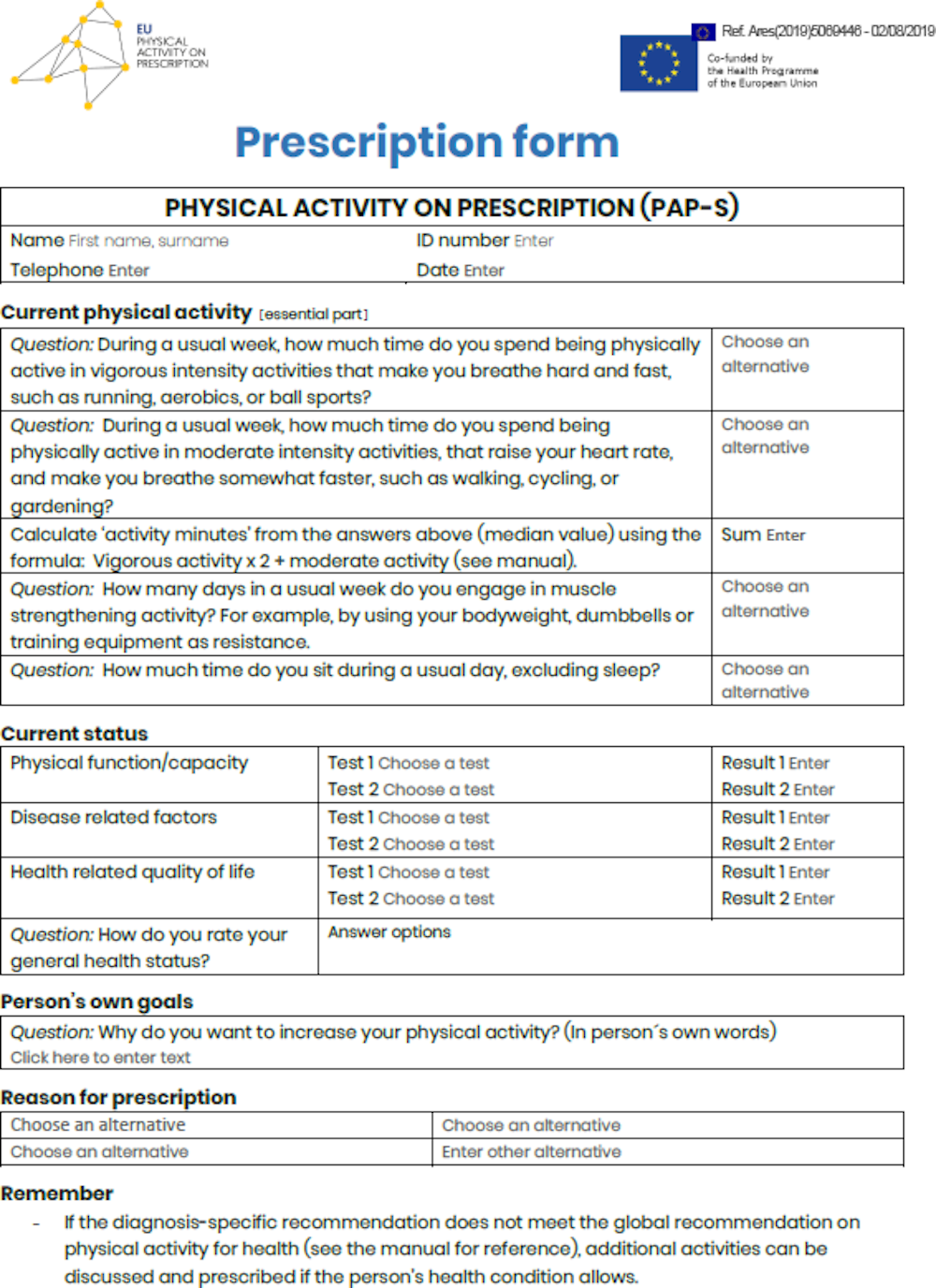
The person-centred individualised counselling is central to the intervention, providing patients with a personalised advice that takes into account their health status, motivation, prior experiences and preferences (EUPAP, 2020[3]). This advice is given as a written prescription (see Annex 4.A) and documented in the patient’s medical file. It includes the recommended type and dose of physical activity, possible contraindications and a plan for follow-up. To ensure that the prescription is evidence‑based, a handbook is available to prescribers (Box 4.1). Follow-up, in person or via phone, letter or email, is used to adjust the prescription and foster motivation. This generally takes place once after six months. Finally, the patient can be referred to structured exercise through a community-based network of activity organisers, such as NGOs, public or private facilities. However, it is important to note that in most cases the physical activity agreed upon in the prescription is handled and paid for by the patient, outside the health care system.
While there are no formal referral criteria, prescriptions are generally written for people who are insufficiently physically active, have overweight or who have chronic conditions that would benefit from increased physical activity.
The execution of the PAP intervention differs across regions in Sweden. While many prescriptions come from primary health care providers, all licensed Swedish health care professionals may prescribe PAP (Onerup et al. (2019[1]) and EUPAP (2020[3])). This includes for example community nurses, physiotherapists, midwifes, dietitians, specialist doctors and psychologists. In some cases, specific PAP coaches or PAP-co‑ordinators are available. Moreover, local collaborations between health care services and activity organisers can be set up. There are no requirements or incentives to prescribers to participate in the programme.
While there is no central funding for the PAP programme, in some cases funding is available from specific projects or for certain diagnoses, or through agreements between regions and sports federations or facilities. Resources made available for the programme include a prescription form (see Annex 4.A) and the handbook (see Box 4.1). These are updated regularly, as the PAP programme in general is continuously under development.
Box 4.1. The FYSS (Physical activity in Disease Prevention and Treatment) handbook
The FYSS (Physical activity in Disease Prevention and Treatment) handbook consists of 53 chapters, each providing an overview of the evidence of how physical activity can help prevent or manage a specific condition.
The production of the book has taken place more or less non-stop for the last 20 years. The first edition was published in 2003, while the second edition came out 2008 and the third in 2017. The fourth edition is to be published later in 2021. The work is performed by a steering committee (YFA) which is a working group within the Swedish Society of Exercise and Sports Medicine (part of the Swedish Medical Association). The steering committee, consisting of 7‑10 specialists (medical doctors, professors, personal trainers) co‑ordinate the work, with more than 100 experts writing the different chapters.
The process has been supported by grants from the Swedish Bureau of Health and Welfare, and also by the Norwegian Public Health Agency. The book has a budget of around SEK 6‑8 million (EUR 600 000) for each version, covering writers fees and administration.
An online version is available on the website www.fyss.se, and a paperback version can be ordered from the website of the YFA. For copyright reasons, currently 33 of 53 FYSS chapters are available on the website, but in the long run all chapters will be freely available.
For the EUPAP programme, which aims to transfer the Swedish PAP model to other European countries, a concise, English-language version was created: the FYSS-short. This version covers 32 diagnoses and has been systematically compiled with uniform terminology and evidence‑based recommendations. All of the diagnosis chapters in FYSS-short are organised into five sections:
Prevention: this section presents any evidence to suggest that physical activity can prevent the condition.
Indication: this section notes whether physical activity is indicated or recommended for someone with this particular diagnosis.
Effects of physical activity: this section provides evidence of the effects of physical activity on the condition, covering both “acute effects” (during and directly after exercising) and the effects of regular physical activity over a longer period of time.
Recommended physical activity: this section provides specific recommendations in terms of doses and types of physical activity for each specific diagnosis.
Diagnosis-specific advice: this section provides disease‑specific advice that is particularly important to follow, such as intensity, medical supervision (e.g. cardiac monitoring), instructor-led exercise, managed by a physiotherapist or exercise scientist, warm up/cool down, progress, medication, pain, motivational issues, equipment and dietary issues.
Source: YFA (2022[4]), “FYSS – vägen till bättre folkhälsa”, https://www.yfa.se/fyss/vad-ar-fyss/; FYSS (2022[5]), “FYSS – EVIDENSBASERAD KUNSKAPSBAS”, https://www.fyss.se/.
OECD Best Practices Framework assessment
This section analyses PAP against the five criteria within OECD’s Best Practice Identification Framework – Effectiveness, Efficiency, Equity, Evidence‑base and Extent of coverage (see Box 4.2 for a high-level assessment of PAP). Further details on the OECD Framework can be found in Annex A.
Box 4.2. Assessment of PAP, Sweden
Effectiveness
The implementation of PAP with the current coverage rate of 0.56% in Sweden is estimated to result in a cumulative total gain of 737 life years (LY) and 979 disability-adjusted life years (DALYs) by 2050
At a higher coverage rate of 2.39%, PAP is estimated to result in a cumulative gain of 10 995 LYs and 13 113 DALY by 2050
Efficiency
At a coverage rate of 2.39%, PAP would lead to cumulative health expenditure savings of EUR 19.37 (SEK 205.06) per person by 2050 or EUR 1.03 on average per person, per year, in Sweden
At a net saving of approximately SEK 91 000 (EUR 9 000) per DALY gained, the PAP intervention is cost-saving
Equity
Data from the region of Stockholm suggest that PAP reaches people across socio‑economic groups
However, as implementation of the programme is decentralised, there is large variation across the regions, which risks creating inequalities
Evidence‑base
The randomised control trial (RCT) upon which the effectiveness modelling parameters are based in rated as strong by the Quality Assessment Tool for Quantitative Studies
A large number of other RCTs and observational studies of the PAP intervention exist, and a five‑year follow-up study is currently underway to understand the long-term impact
To ensure that the prescribed PA is evidence‑based, a handbook with physical activity recommendations was developed and is regularly updated
Extent of coverage
In 2019, 45 000 prescriptions for physical activity were prescribed in primary care, equating to 5.6 prescriptions per 1 000 population, or approximately 14.1 prescriptions per 1 000 eligible people
In some regions the coverage rate is up to eight times higher than the national average
Effectiveness
A randomised controlled trial (RCT) of the PAP programme found that individuals who received the PAP intervention increased their physical activity level by 159 minutes of (at least) moderate‑intensity activity per week, from a baseline of 120 minutes, compared to no change in the control group. Using a weight of four METs for moderate intensity activities (WHO, n.d.[6]), this equates to an increase of 636 MET-minutes per week (approximately one hour of running per week, at 10 kilometres per hour). In addition, they report that body-mass index (BMI) decreased by 0.6 in the intervention group, compared to 0.2 in the controls. A decrease of 0.4 BMI points can therefore be attributed to the intervention (Kallings et al., 2009[7]) (Sjögren et al., 2012[8]).
These results were used to estimate the potential impact of the PAP programme on population health and the economy if scaled-up and transferred to all OECD and EU27 countries up until year 2050, using the OECD SPHeP-NCDs model. This microsimulation model compared a “business-as-usual” scenario, to a scenario where all countries implement the PAP programme, to be able to measure the difference in health and economic outcomes. The results presented in this section (Effectiveness) and the next (Efficiency) are based on this modelling exercise (see Annex 4.B for more details on modelling assumptions).
The coverage rate of the intervention in Sweden is about 5.6 prescriptions per 1 000 population (0.56%). Assuming 40% of the adult population is eligible for the PAP scheme, the exposure would be 14.1 prescriptions per 1 000 of eligible people. This uptake is relatively low. Therefore, a higher coverage rate was also explored. In the region of Norrbotten, overall population coverage rate was 23.9 per 1 000 population (2.39%), or 59.7 per 1 000 eligible population. The scenario with a 0.56% coverage rate was modelled only for Sweden, to show the current impact the programme has. The scenario with a 2.39% coverage rate was used for Sweden and all other countries to compare the potential impact the programme could have. (Note that the 2.39% scenario is considered the main scenario, and that any results refer to this scenario unless specifically stated that the coverage rate is 0.56%.)
Sweden
With the current coverage rate of 0.56%, the PAP programme is estimated to result in a cumulative gain of 737 life years (LY) and 979 disability-adjusted life years (DALYs) by 2050 (Figure 4.1). The implementation of PAP with a coverage rate of 2.39% in Sweden is estimated to gain a cumulative total of 10 995 LYs and 13 113 DALYs by 2050 (Figure 4.2). This translates into a rate of 5.62 and 6.61 DALYs gained per 100 000 people, on average, per year over the period 2021‑50.
Figure 4.1. Cumulative number of LYs and DALYs gained (2021‑50) – PAP, Sweden (0.56% coverage rate)
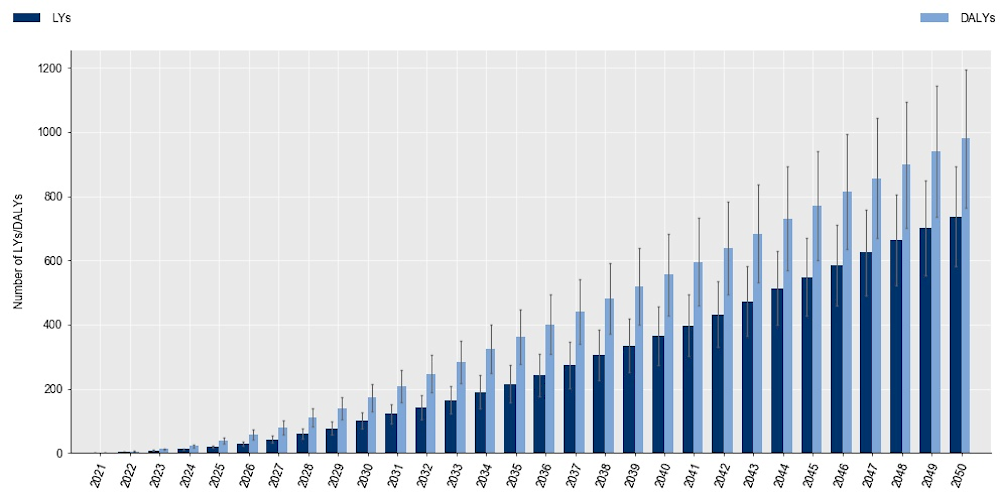
Note: The black lines represent 95% confidence intervals.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
Figure 4.2. Cumulative number of LYs and DALYs gained (2021‑50) – PAP, Sweden (2.39% coverage rate)
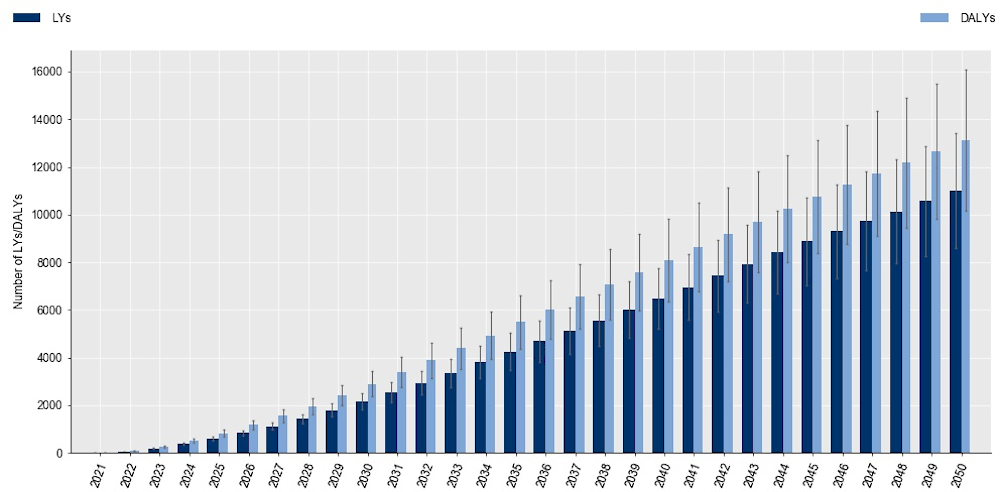
Note: The black lines represent 95% confidence intervals. Figures are discounted at a rate of 3%.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
In gross terms, PAP is expected to have the greatest impact on cardiovascular diseases (CVDs), mental health conditions and musculoskeletal disorders (MSDs) (Figure 4.3). Between 2021 and 2050, the number of CVD cases is estimated to be reduced by 7 316 cases due to the PAP intervention. Other diseases affected include diabetes, dementia and several cancers.
Figure 4.3. Cumulative number of disease cases avoided by 2050 – PAP, Sweden (2.39% coverage rate)
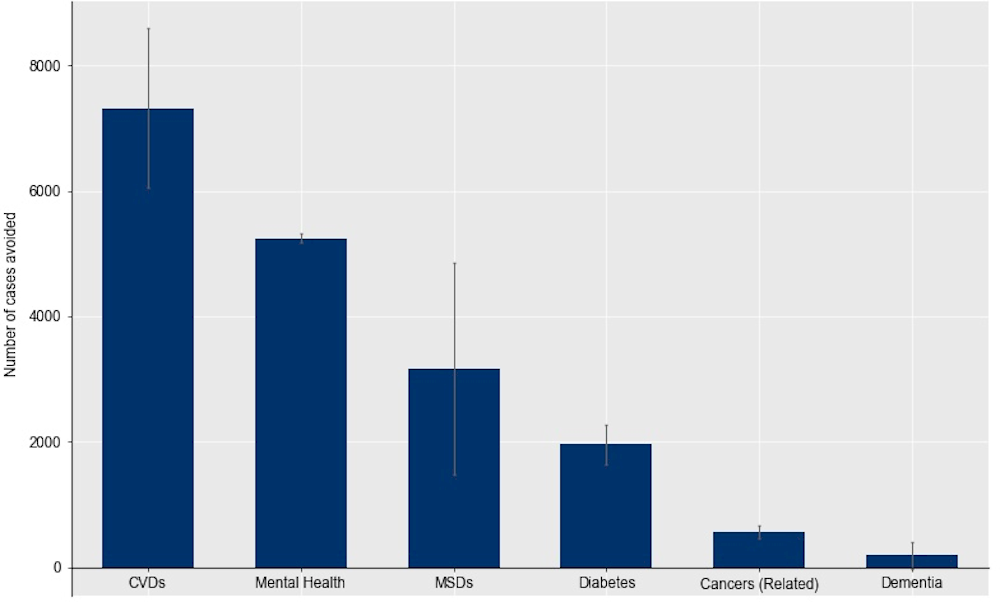
Note: MSDs = musculoskeletal disorders, CVDs = cardiovascular diseases. Related cancers include colorectal, breast, oesophageal and liver cancer. The black lines represent 95% confidence intervals.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
OECD and non-OECD European countries
Transferring PAP to all OECD and EU27 countries, with a coverage rate of 2.39%, is estimated to result in 9.90 and 8.76 LYs gained per 100 000 people, respectively, on average per year between 2021 and 2050 (Figure 4.4). For DALYs, gains are even higher at 12.10 for OECD and 10.01 for EU27 countries. The impact is as high as 51.55 DALYs per 100 000 in the United States. On the other hand, in some smaller countries like Malta, Iceland, Cyprus, Latvia and Luxembourg, the low coverage rate means that the effects of the intervention were not significant.
Figure 4.4. LYs and DALYs gained annually per 100 000 people, 2021‑50 – PAP, all countries (2.39% coverage rate)
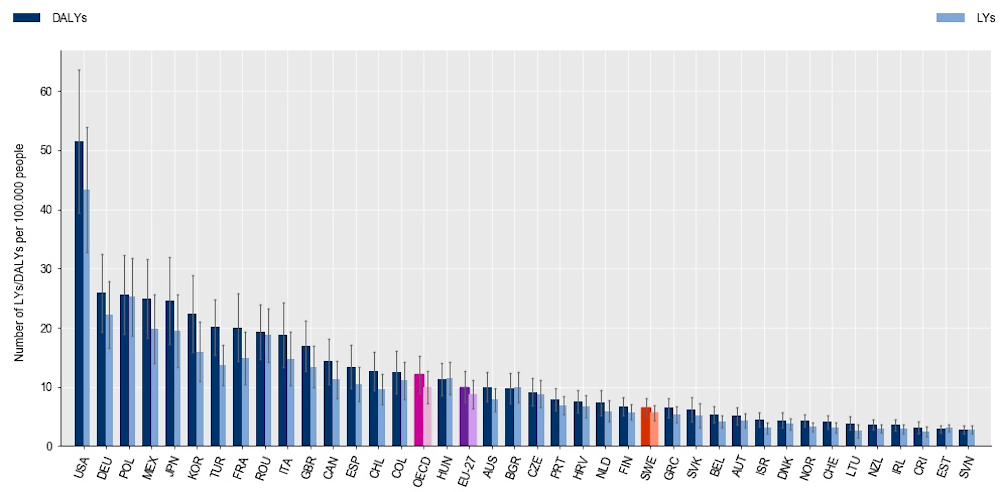
Note: The black lines represent 95% confidence intervals. Results for Cyprus, Iceland, Malta, Latvia and Luxembourg were not significant.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
In gross terms, in OECD countries, PAP would have the greatest impact on cardiovascular diseases (CVD), reducing the number of cases by 1.5 million between 2021 and 2050 (Figure 4.5). The OECD total is considerably higher than the EU27, as the OECD includes a number of large countries with high impacts, such as Mexico, the United States, and Japan. In the EU27, PAP is estimate to prevent 0.39 million cases of CVDs over 2021 to 2050.
Figure 4.5. Total disease cases avoided, between 2021 and 2050 – PAP, OECD and EU27 countries (2.39% coverage rate)
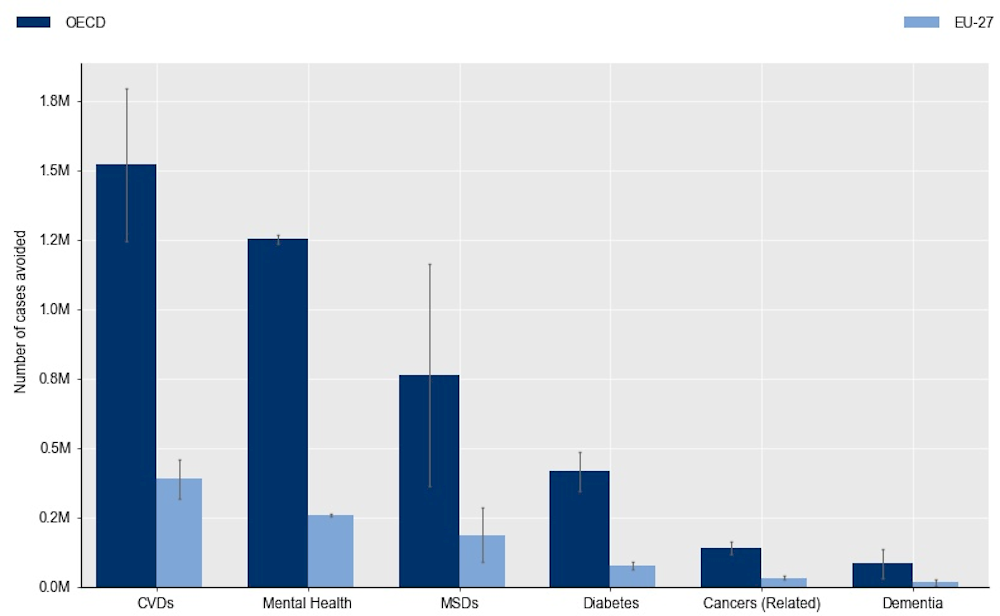
Note: MSDs = musculoskeletal disorders, CVDs = cardiovascular diseases. The black lines represent 95% confidence intervals.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
Efficiency
Similar to “Effectiveness”, this section presents results for the Sweden followed by remaining OECD and non-OECD European countries.
Sweden
By improving levels of physical activity, PAP can reduce health care costs. At the current coverage rate of 0.56%, over the modelled period of 2021‑50, the OECD-SPHeP NCD model estimates that PAP would lead to cumulative health expenditure savings of EUR 2.02 (SEK 21.42) per person by 2050 (Figure 4.6). A coverage rate of 2.39% would lead to considerably higher cumulative health expenditure savings, of EUR 19.37 (SEK 205.06) per person by 2050 (Figure 4.7) or EUR 1.03 on average per person, per year. Cost savings however are to an extent offset by intervention operating costs (see Table 4.2).
Figure 4.6. Cumulative health expenditure savings per person, EUR, 2021‑50 – PAP, Sweden (0.56% coverage rate)
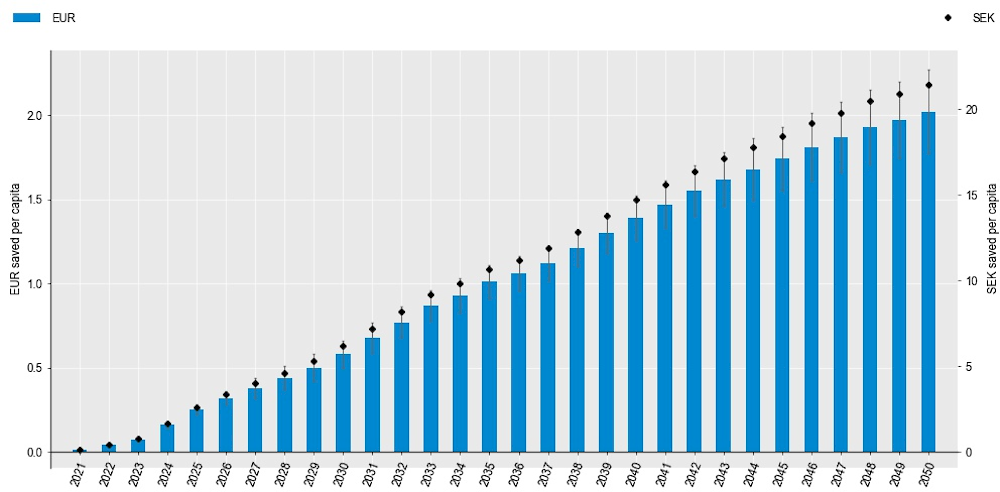
Note: The black lines represent 95% confidence intervals; values are discounted at 3% annually.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
Figure 4.7. Cumulative health expenditure savings per person, EUR, 2021‑50 – PAP, Sweden (2.39% coverage rate)
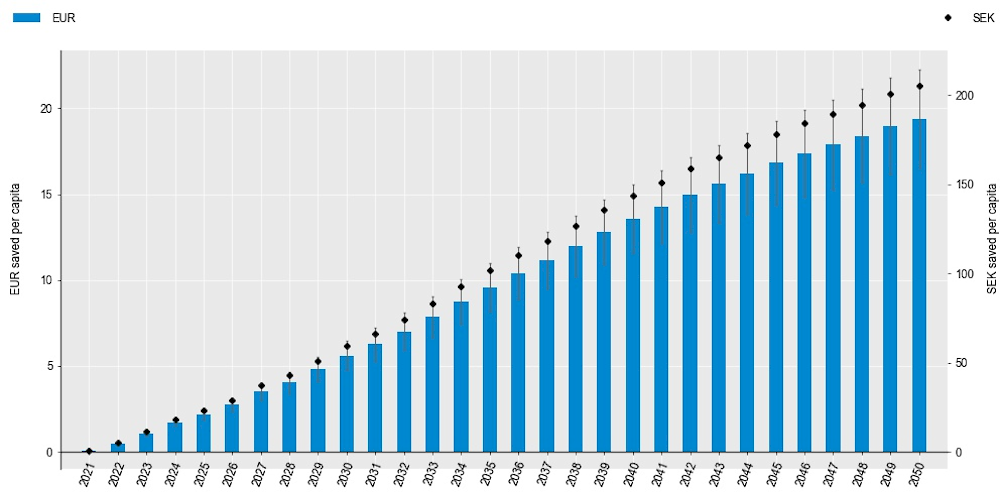
Note: The black lines represent 95% confidence intervals; values are discounted at 3% annually.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
OECD and non-OECD European countries
Average annual health expenditure (HE) savings as a proportion of total HE is around 0.03% for EU27 countries, and 0.05% for OECD countries, at a coverage rate of 2.39% (Figure 4.8). On a per capita basis, this translates into average annual savings of EUR 0.67 and EUR 1.16 for EU27 and OECD countries, respectively. The impact on health care expenditure in the United States is considerably larger than in other countries, which is driven both by the large impact on health and high health care cost.
Figure 4.8. Health expenditure (HE) savings as a percentage of total HE and per capita (EUR), average 2021‑50 – PAP, all countries (2.39% coverage rate)
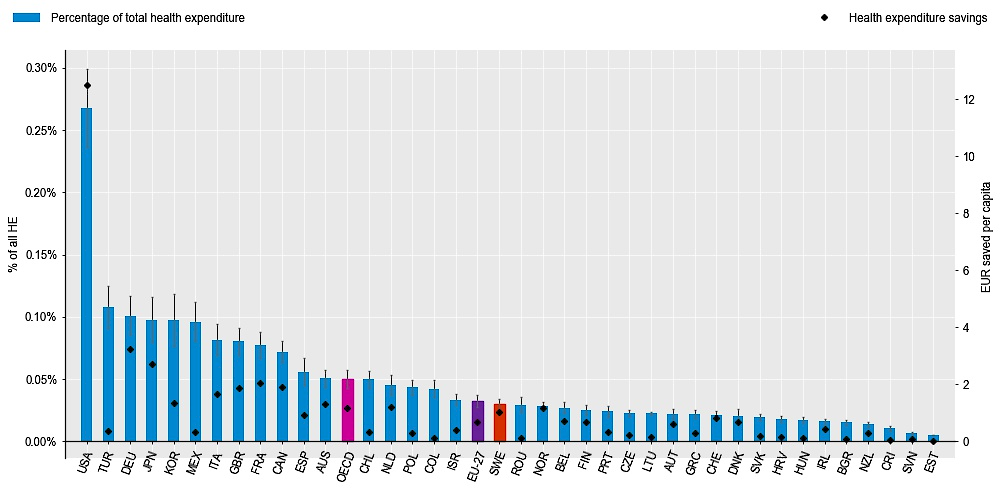
Note: The black lines represent 95% confidence intervals. Results for Cyprus, Iceland, Malta, Latvia and Luxembourg were not significant.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
Table 4.2 provides information on intervention costs, total health expenditure savings and the cost per DALY gained in local currency for OECD and non-OECD European countries. In most countries, PAP is cost-saving (i.e. there is a negative cost per DALY gained). In all countries PAP is considered cost-effective with the cost per DALY far below the average cost-effectiveness threshold applied in European countries (i.e. EUR 50 000 based on (Vallejo-Torres et al., 2016[9]). This is largely due to the low cost of the intervention.
Table 4.2. Cost effectiveness figures in local currency – PAP, all countries (2.39% coverage rate)
|
Country |
Local currency |
Intervention costs per capita, average per year |
Total health expenditure savings, 2021‑50 |
Cost per DALY gained* |
|---|---|---|---|---|
|
Australia |
AUD |
1.48 |
62 646 363 |
Cost saving |
|
Austria |
EUR |
0.44 |
5 509 234 |
Cost saving |
|
Belgium |
EUR |
0.45 |
8 856 137 |
Cost saving |
|
Bulgaria |
BGN |
0.22 |
1 067 921 |
411 |
|
Canada |
CAD |
1.37 |
116 464 815 |
Cost saving |
|
Chile |
CLF |
245.08 |
5 314 162 395 |
Cost saving |
|
Colombia |
COP |
632.3 |
25 429 120 003 |
1 239 432 |
|
Costa Rica |
CRC |
103.19 |
197 430 561 |
2 116 606 |
|
Croatia |
HRK |
1.17 |
4 024 441 |
1 591 |
|
Czech Republic |
CZK |
5.23 |
62 726 895 |
Cost saving |
|
Denmark |
DKK |
3.8 |
30 391 196 |
Cost saving |
|
Estonia |
EUR |
0.15 |
32 125 |
4 120 |
|
Finland |
EUR |
0.46 |
3 844 272 |
Cost saving |
|
France |
EUR |
1.19 |
140 174 902 |
Cost saving |
|
Germany |
EUR |
1.15 |
257 243 029 |
Cost saving |
|
Greece |
EUR |
0.31 |
2 906 213 |
464 |
|
Hungary |
HUF |
50.88 |
392 154 086 |
66 079 |
|
Ireland |
EUR |
0.37 |
2 231 457 |
Cost saving |
|
Israel |
ILS |
1.86 |
17 338 079 |
6 496 |
|
Italy |
EUR |
0.91 |
95 979 662 |
Cost saving |
|
Japan |
JPY |
115.43 |
38 048 054 235 |
Cost saving |
|
Korea |
KRW |
842.54 |
89 851 794 792 |
Cost saving |
|
Lithuania |
EUR |
0.14 |
438 553 |
Cost saving |
|
Mexico |
MXN |
9.53 |
1 083 401 157 |
9 278 |
|
Netherlands |
EUR |
0.56 |
21 389 850 |
Cost saving |
|
New Zealand |
NZD |
0.58 |
2 517 493 |
2 883 |
|
Norway |
NOK |
5.78 |
69 603 206 |
Cost saving |
|
Poland |
PLN |
1.05 |
45 261 027 |
Cost saving |
|
Portugal |
EUR |
0.3 |
3 290 442 |
Cost saving |
|
Romania |
RON |
0.73 |
10 730 606 |
518 |
|
Slovak Republic |
EUR |
0.17 |
908 205 |
Cost saving |
|
Slovenia |
EUR |
0.17 |
165 225 |
3 215 |
|
Spain |
EUR |
0.7 |
42 493 946 |
Cost saving |
|
Sweden |
SEK |
4.91 |
120 193 131 |
Cost saving |
|
Switzerland |
CHE |
0.64 |
8 550 738 |
Cost saving |
|
Turkey |
TRY |
1.68 |
213 713 413 |
Cost saving |
|
United Kingdom |
GBP |
0.93 |
117 403 932 |
Cost saving |
|
United States |
USD |
3.92 |
5 137 720 257 |
Cost saving |
* Cost per DALY (disability-adjusted life year) gained is measured using total intervention costs less total health expenditure savings divided by total DALYs gained over the period 2021‑50. Results for Cyprus, Iceland, Malta, Latvia and Luxembourg were not significant and therefore not included in the table above.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
The reduction in chronic diseases resulting from PAP has, in turn, an impact on labour market participation and productivity. By reducing chronic disease incidence, PAP is expected to lead to increases in employment and reductions in absenteeism, presenteeism, and early retirement. Converting these labour market outputs into full-time equivalent (FTE) workers, it is estimated that OECD and EU27 countries will gain 8.50 and 3.97 FTE per 100 000 working age people per year between 2021 and 2050, respectively. The high rate in OECD countries as compared to EU27 countries is driven by the high impact in non-EU countries such as the United States, Mexico, Japan and Korea. In monetary terms, this translates into average per capita increase in labour market production of EUR 1.02 for OECD and EUR 0.56 for EU27 countries (Figure 4.9).
Figure 4.9. Labour market impacts, average per year, 2021‑50 – PAP, all countries (2.39% coverage rate)
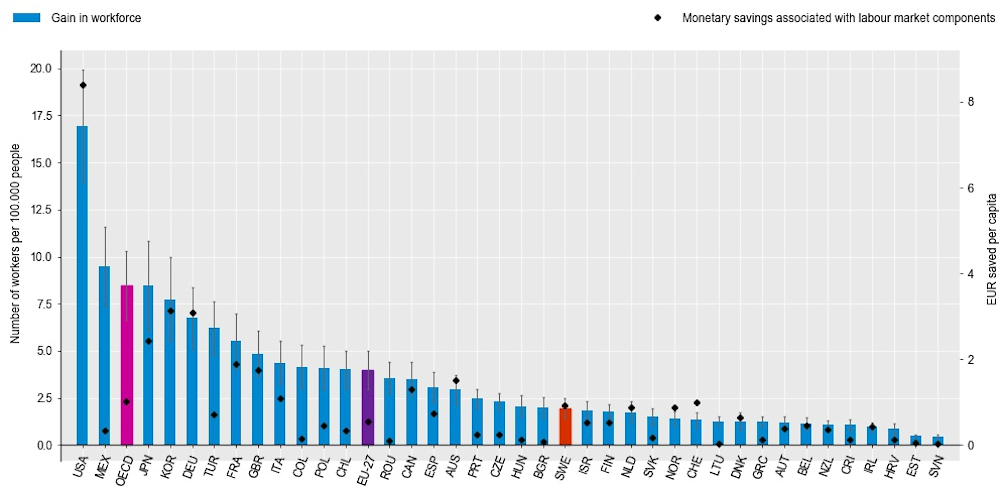
Note: The black lines represent 95% confidence intervals. Results for Cyprus, Iceland, Malta, Latvia and Luxembourg were not significant.
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2021.
Equity
The Swedish health care system is based on 21 autonomous regions, and each is in charge of the implementation of PAP in their region. As a result, there is large variation across the regions in the number of prescriptions for physical activity (see also section on the “Extent of the coverage”). While this approach allows regions to tailor the intervention to local resources and population needs (e.g. working with local sports facilities, focusing on specific diagnoses), it risks creating regional inequalities in access to the programme.
Data on PA prescriptions in the region of Stockholm shows that people of the high socio‑economic group (SEG) made up 21% of individuals receiving a PAP, the middle group accounted for 36% of prescriptions and 42% went to people in the low SEG. This distribution is similar to the population distribution of the main diagnoses for which PAP is given (e.g. the prevalence of overweight and obesity is 20% in highest SEG, 30% in middle SEG and 50% in lowest SEG), suggesting that different SEGs benefit equally from the intervention in the Stockholm region.
Evidence‑base
Evidence‑base of the modelling exercise
The data used to model effectiveness and efficiency is based on a randomised controlled trial (RCT) (Kallings et al., 2009[7]) (Kallings, 2008[10]). The Quality Assessment Tool for Quantitative Studies rates this study as “strong” (Table 4.3) (Effective Public Health Practice Project, 1998[11]). The study design, randomisation of participants and low drop-out rate all contribute to reliable estimates of the true effect of the intervention. The main limitation of the study is the representativeness of the study population. The trial focused on people aged 67 or 68 years old, with obesity but without heart disease, hypertension, diabetes, cancer or other serious conditions. In reality PAP targets people of all ages, and in particular those with chronic conditions that may benefit from physical activity.
Table 4.3. Evidence‑based assessment, PAP
|
Assessment category |
Question |
Rating |
|---|---|---|
|
Selection bias |
Are the individuals selected to participate in the study likely to be representative of the target population? |
Representative of target population of the study: very likely Representative of target population of the intervention: not likely |
|
What percentage of selected individuals agreed to participate? |
60‑79% |
|
|
Selection bias score: Moderate |
||
|
Study design |
Indicate the study design |
RCT |
|
Was the study described as randomised? |
Yes |
|
|
If Yes, was the method of randomisation described? |
Yes |
|
|
If Yes, was the method appropriate? |
Yes |
|
|
Study design score: Strong |
||
|
Confounders |
Were there important differences between groups prior to the intervention? |
No |
|
Confounders score: Strong |
||
|
Blinding |
Was the outcome assessor aware of the intervention or exposure status of participants? |
Not specified |
|
Were the study participants aware of the research question? |
Not specified |
|
|
Blinding score: Poor |
||
|
Data collection methods |
Were data collection tools shown to be valid? |
Yes |
|
Were data collection tools shown to be reliable? |
Yes |
|
|
Data collection methods score: Strong |
||
|
Withdrawals and dropouts |
Were withdrawals and dropouts reported in terms of numbers and/or reasons per group? |
Yes |
|
Indicate the percentage of participants who completed the study? |
80 ‑100% |
|
|
Withdrawals and dropouts score: Strong |
||
Source: Effective Public Health Practice Project (1998[11]), “Quality assessment tool for quantitative studies”, https://www.nccmt.ca/knowledge-repositories/search/14.
The RCT by Kallings was chosen to use in the OECD SPHeP-NCDs model because of its strong design and because it measured physical activity in MET-minutes (see Annex 4.B). However, a large number of other RCTs and observational studies of the PAP programme exist (Onerup et al., 2019[1]). Moreover, a five‑year follow-up study is currently underway to understand the long-term impact of the intervention. The overall evidence base of the evaluation of this intervention is therefore robust.
Evidence‑base of the individual prescriptions
To ensure that the prescribed PA is evidence‑based, a handbook with physical activity recommendations was developed. The FYSS handbook is regularly updated with input from a large number of experts and based on a systematic literature review. Grading of Recommendations, Assessment, Development and Evaluations (GRADE) has been used to rate the quality of evidence underpinning the clinical practice recommendations in the handbook (BMJ Best Practice, n.d.[12]).
Extent of coverage
The extent of coverage criterion measures two key measures – the participation rate and the dropout rate. For the participation rate, data on the number of PA prescriptions can be used. The Swedish Board of Health and Welfare has collected data on the number of PA prescriptions from the regions during the years 2014‑19. In 2019, the regions reported that approximately 45 000 prescriptions for physical activity were prescribed in primary care. As the Swedish adult population in 2019 was around 8 million, this is roughly 5.6 prescriptions per 1 000 people. Looking only at the adult population with insufficient physical activity (around 40%), the coverage would be 14.1 prescriptions per 1 000 eligible people. This number has been relatively constant over time, though some regions decreased their numbers while others increased their prescriptions. The number of prescriptions per capita more than doubles when examining the eligible population only – i.e. those living with overweight or obese, who make up 56% of the adult population in Sweden (WHO Global Health Observatory, 2018[13]).
There is considerable variation in coverage across regions (Figure 4.10). While in some regions less than one prescription is written per 1 000 inhabitants, in others it is four to eight times higher than the national average. In the region of Västernorrland there are approximately 40 prescriptions for physical activity per 1 000 inhabitants – but this number also includes other types counselling on physical activity.
Figure 4.10. Prescription rate per region
Number of prescriptions for physical activity per year as compared to the relevant population
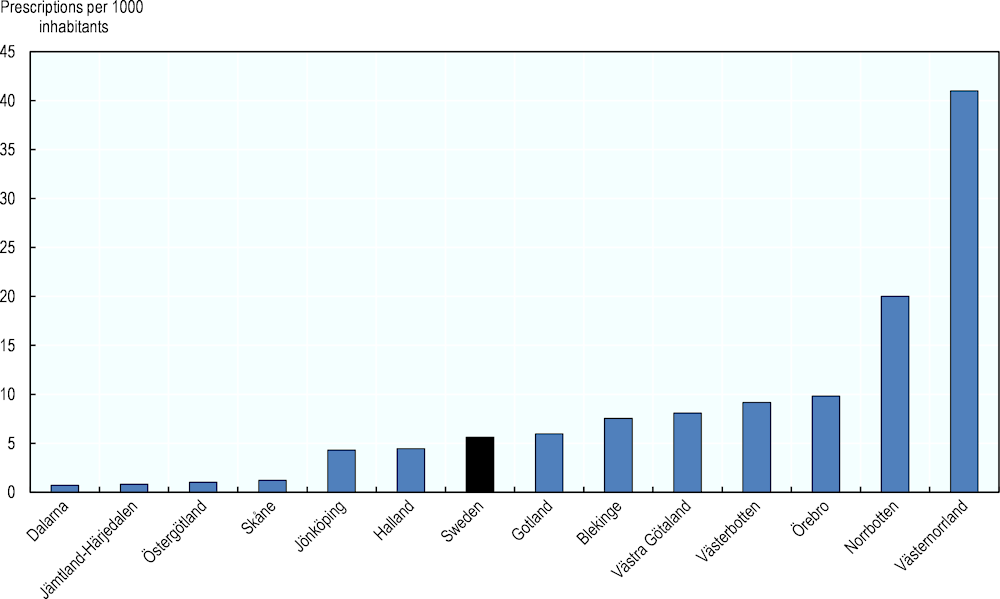
Source: OECD analysis on data from SVT News (2019[14]), “Stor skillnad på hur mycket motion på recept som skrivs ut i riket [Large difference in how much exercise on prescription is prescribed in the country]”, https://www.svt.se/nyheter/lokalt/orebro/regioner-anser-att-motion-pa-recept-borde-oka.
Besides PAP, there are other types of counselling in primary care on physical activity in Sweden. For example, health care professionals are recommended to use a Brief Intervention, for instance motivational interviewing or counselling, to promote physical activity. Furthermore, sometimes PAP is registered under Brief Intervention and therefore not included in the PAP count. In 2019, a total of 426 571 interventions were performed to promote physical activity in primary care. The majority of interventions were brief advice. Out of all the reported interventions in primary care, approximately 10% were reported to be PAP.
The dropout rate for this intervention is difficult to determine, as the physical activity takes place on the participant’s own initiative and is not monitored. However, as a proxy the percentage of people who do not have their follow-up meeting with the prescriber can be used. Data shows that in the region of Norrbotten, over the period 2013 to 2020, approximately 50 to 65% of prescriptions were followed up after six months. In the region of Stockholm, this figure was approximately 50%.
Policy options to enhance performance
This section summarises policy options available to policy makers in settings where PAP is implemented (or being transferred) to further enhance the performance of this intervention.
Enhancing effectiveness
While a written prescription with a follow-up meeting sometime later form the basis of the PAP model, the intervention can be adjusted and expanded to include counselling from physiotherapists or personal trainers, structured exercise groups, or subsidised access to sports facilities. A number of factors have been identified as increasing the effectiveness of the PAP intervention:
Two systematic reviews found that a longer intervention duration, as well as a longer follow-up period, are associated with a greater impact (Goryakin, Suhlrie and Cecchini, 2018[15]) (Arsenijevic and Groot, 2017[16]).
A study of adherence to physical activity prescriptions found that non-adherence was more frequent among subjects who were issued with referrals for facility-based activities rather than home‑based activities. However, low motivation was often cited as the reason for non-adherence to home‑based activities, suggesting that facility-based activities may be preferred for participants with a lower motivation (Leijon et al., 2011[17]).
An RCT looking at intensity and frequency found that prescribing a higher frequency of physical activity increased the accumulation of exercise without a decline in adherence, while a higher intensity decreased adherence (Duncan et al., 2005[18]) (Perri et al., 2002[19]).
Prescriptions need to be carefully tailored to the participant’s capability (e.g. physical capacity), opportunity (e.g. having access to appropriate activities) and motivation (e.g. finding activities that encouraged continuation) to undertake physical activity (Andersen et al., 2019[20]).
Enhancing efficiency
PAP is a low-cost intervention, taking place within the existing health system and with minimal overhead or per-capita cost. Measures to enhance efficiency have therefore not been identified.
Enhancing equity
The PAP intervention is available nationally, but in practice access varies by region, as implementation is done locally by the health boards. This may create inequalities across regions. Moreover, while the data from the Stockholm region suggests that the intervention reaches people in different socio‑economic groups equally, it is unclear whether this applies to other regions and other population groups.
In addition to prescribing physical activity to all population groups, it is also important that all have access to physical activity resources. Since the PAP programme does not include provision or financing of the actual physical activities, this might create barriers for lower-income population groups. Linking the PAP programme to existing or new policies aimed at increasing access to sport facilities for disadvantaged groups might increase adherence and equity.
To ensure an equitable intervention, providing access and quality to everyone, more data is needed on who receives a prescription, and what their outcomes are. Currently, there is no national register for PAP programme in Sweden. Sweden could therefore looked to the Netherlands who are in the process of establishing a national register to monitor a similar lifestyle intervention (see Box 4.3). This would also support the evidence base of the programme, as it would provide detailed impact data by population group.
Box 4.3. Monitoring of the Combined Lifestyle Intervention in the Netherlands
Since January 2019, participation in a Combined Lifestyle Intervention (CLI) to combat overweight is reimbursed by health insurers in the Netherlands under the base health insurance package. Under the CLI, participants receive individual or group counselling on healthy diet, physical activity and other factors contributing to a healthy lifestyle.
Similar to the PAP in Sweden, CLI, in practice is delivered locally, following different programmes and by different care providers. To ensure the effectiveness, cost-effectiveness and equity of the programme, monitoring is undertaken centrally by the national public health organisation RIVM. Twice a year, RIVM analyses claims data collected from health insurers. The data is published in a factsheet which includes information on the number of reimbursements, the age, sex, education, health and regional distribution of participants, as well as the type of programmes and providers.
In addition to the monitor based on insurance claims data, RIVM is in the process of setting up a register to capture intervention outcomes. This register will record information such as weight, BMI, waist circumference and quality of life among participants before and after CLI. Analysing this data for different population groups and regions can identify potential inequalities, and highlight areas where additional resources or efforts are needed.
Enhancing the evidence‑base
PAP is based on a robust evidence base – both the prescriptions and the evaluation of the intervention itself. Of note will be the results of the ongoing trial looking at the longer-term effect of PAP. A register of participations, as described above could also provide additional insights into the effectiveness of the programme across different population groups.
Enhancing extent of coverage
Compared to the large potential target population of the intervention, the uptake of the intervention is relatively low. For a low-cost, low-intensity intervention such as PAP, a higher population coverage is needed to produce desired effects.
In an interview study with primary health care staff and management, Gustavsson et al. (2018[21]) identified the following elements that could facilitate implementation and increased uptake of PAP:
Increased knowledge and affirmative attitude among the health care professionals. This includes knowledge on how to talk about health behaviours in patient consultations, and knowledge of and belief in the PAP method. A study in New York City found that a two‑session practitioner education and a toolbox of resources significantly increased prescriber confidence and the number of prescriptions written (Kyei-Frimpong et al., 2021[22]).
Clear and supportive management. Policies and clinical guidelines need to be developed, shared and approved at all levels, central management needs to show clear support for the intervention and earmark time and resources for PAP consultations.
Supporting structures. This includes a centralised or local support function, such as a central PAP-co‑ordinator or PAP-educator, tailored written routines at health care centres on how to provide PAP, and co‑operation with external physical activity organisers through for example a contact list.
These elements correspond with the barriers to uptake identified in a different study, which include difficulties in finding time for PAP, uncertainty about the effectiveness, and a lack of procedures and clear guidelines (Persson et al., 2013[23]).
In addition to removing barriers to uptake, incentives could be explored. Financial incentives to prescribers or their practice can encourage uptake, especially when combined with efforts to simplify the prescription routine (Persson, Ovhed and Hansson, 2010[24]). Non-economic incentives such a public reporting of prescription data by provider or region, or personalised letters to prescribers comparing their prescribing rate to their peers, could provide a “nudge” to increase the number of prescriptions (Hallsworth et al., 2016[25]) (Wang and Groene, 2020[26]). Other nudges that could be explored include automatic prompts and programmes to encourage public commitment (Wang and Groene, 2020[26]).
Transferability
This section explores the transferability of PAP and is broken into three components: 1) an examination of existing transfers; 2) a transferability assessment using publically available data; and 3) additional considerations for policy makers interested in transferring PAP.
Existing transfers of PAP
Transfer of the Swedish PAP intervention to other European countries has begun under the EU-funded “European Physical Activity on Prescription Model” project (EUPAP). This three‑year project (2019‑22), co‑ordinated by the Public Health Agency of Sweden, will transfer the Swedish PAP to a further nine countries: Portugal, Romania, Lithuania, Spain, Germany, Denmark, Belgium, Italy and Malta.
EUPAP will provide education and training initiatives according to the needs of different partner countries, targeting both health care professionals responsible for prescribing as well as trainers or educators. In addition, several tools will be developed in English, which countries can translate into their local language, including:
An electronic version of the FYSS handbook
Concise guidelines on the PAP methodology
A sample prescription form.
Another important part of the EUPAP project is the feasibility study (EUPAP, 2020[3]). Each of the target countries was analysed to understand the context in which PAP would operate and how this compares to the Swedish situation. At the macro level, the feasibility study looked at the political context, past experiences with PAP schemes, relevant regulations and budget. At the micro level, the study assessed the preparedness for implementation among four groups: stakeholders (e.g. whether agreements were in place between the health and the sports sector), health care settings (e.g. which health care settings confirmed participation in the intervention), prescribers (e.g. who will be prescribing physical activity), and end-users/patients (e.g. what the target population would be, mostly based on age, conditions and/or use of specific health care services). Finally, the proposed plan in the target country was compared to the Swedish model following the five key components of the PAP programme.
An evaluation of these transfers is not yet possible as the intervention is ongoing and has experienced some delays due to the COVID‑19 pandemic.
Transferability assessment
The following section outlines the methodological framework to assess transferability and results from the assessment.
Methodological framework
Details on the methodological framework to assess transferability can be found in Annex A.
Indicators from publically available datasets to assess the transferability of PAP are listed in Table 4.4. These cover indicators related to the population, sector, political and economic contexts. Please note, the assessment is intentionally high level given the availability of public data covering OECD and non-OECD European countries.
Table 4.4. Indicators to assess the transferability of PAP
|
Indicator |
Reasoning |
Interpretation |
|---|---|---|
|
Population context |
||
|
% of the population with access to recreational green space within 10min walking distance |
PAP participants are responsible for undertaking prescribed physical activity. Given the link between green space and physical activity, PAP may be more successful in countries with better access to green space. |
🡹 value = more transferable |
|
Sector specific context (primary care) |
||
|
Health professionals are trained in health-enhancing physical activity |
PAP requires health professionals to make recommendations on physical activity, and is therefore more likely to be successful if health professionals have been trained on this topic |
“Implemented” or “Foreseen” = more transferable |
|
General practitioners density per 1 000 people |
General practitioners are one of the main prescribers. If there are few GPs per population, it is less likely they will have time to commit to PAP |
🡹 value = more transferable |
|
% people who visited a GP in the last 12 months at least once |
PAP candidates are identified during routine primary care. The more often people see their GP, the more likely PAP reaches the right people |
🡹 value = more transferable |
|
Implementation of specific framework to support access to recreational or exercise facilities for socially disadvantaged groups |
Participants are required to cover access to exercise facilities themselves. In countries where such access is supported to target population groups, PAP is more likely to be successful. |
“Implemented” or “Foreseen” = more transferable |
|
Political context |
||
|
Programme or scheme to promote counselling on physical activity by health professionals |
PAP is more likely to have political support in a country that already supports counselling on physical activity by health professionals |
“Implemented” or “Foreseen” = more transferable |
|
Operational strategy/action plan/policy to reduce physical inactivity |
PAP is more likely to have political support in a country that explicitly aims to reduce physical inactivity |
“Yes” = more transferable |
|
Economic context |
||
|
Gross domestic product per capita (purchasing power parity, international dollars) |
As participants need to cover any cost associated with the physical activities themselves PAP will have a greater reach in wealthier countries |
🡹 value = more transferable |
Source: WHO Regional Office for Europe (2021[27]), “2021 Physical Activity Factsheets for the European Union Member States in the WHO European Region”, https://apps.who.int/iris/bitstream/handle/10665/345335/WHO-EURO-2021-3409-43168-60449-eng.pdf; Eurostat (2021[28]), “Persons visiting a doctor in the last 12 months by medical speciality, number of visits, educational attainment level, sex and age”, http://eurostat.ec.europa.eu/; WHO (n.d.[29]), “Global Health Observatory”, https://www.who.int/data/gho’; World Bank (2020[30]), “GDP, PPP (current international $)”, https://data.worldbank.org/indicator/NY.GDP.MKTP.PP.CD.
Results
Results from the transferability assessment using publically available data are available in Table 4.5. The analysis shows number of GPs as well as the number of visits per year are similar or higher in most countries. Moreover, while Sweden does not have a national strategy on physical activity, a specific framework to support access to recreational or exercise facilities for socially disadvantaged groups, nor is physical activity included in the curriculum of health professionals, these enablers are in place in several potential transfer countries. The main limitation to the transfer of PAP to other countries is the cost for the participant. Since organised exercise classes or access to sports facilities is not covered by the intervention, PAP is more likely to be successful in wealthier countries.
Table 4.5. Transferability assessment by country, PAP (OECD and non-OECD European countries)
Darker shades indicate PAP is more transferable to that particular country
|
Access to green space (%) |
Healthy lifestyle curriculum for health professionals |
General practitioners: density per 1 000 people |
% people who visited a GP in the last 12 months at least once |
Access to exercise facilities for disadvantaged groups |
Programs to support PA counselling by health professionals |
Physical activity strategy |
GNI per capita (Int $ PPP) |
|
|---|---|---|---|---|---|---|---|---|
|
Sweden |
99 |
Implemented |
0.6 |
62 |
Not implemented |
Implemented |
Yes |
53 928 |
|
Australia |
90* |
n/a |
1.2 |
83 |
n/a |
n/a |
Yes |
48 007 |
|
Austria |
98 |
Implemented |
0.8 |
84 |
Not implemented |
Implemented |
Yes |
56 304 |
|
Belgium |
95 |
Implemented |
1.2 |
87 |
Implemented |
Implemented |
Yes |
52 562 |
|
Bulgaria |
n/a |
Foreseen |
0.6 |
47 |
Not implemented |
Foreseen |
Yes |
22 883 |
|
Canada |
n/a |
n/a |
1.3 |
n/a |
n/a |
n/a |
Yes |
48 384 |
|
Chile |
n/a |
n/a |
1.3 |
n/a |
n/a |
n/a |
Yes |
24 131 |
|
Colombia |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
Yes |
14 163 |
|
Costa Rica |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
Yes |
19 094 |
|
Croatia |
n/a |
Not implemented |
0.6 |
68 |
Not implemented |
Implemented |
Yes |
28 388 |
|
Cyprus |
n/a |
Not implemented |
n/a |
68 |
Not implemented |
Foreseen |
No |
38 207 |
|
Czech Republic |
98 |
Implemented |
0.7 |
86 |
Foreseen |
Foreseen |
Yes |
38 326 |
|
Denmark |
89 |
Implemented |
n/a |
86 |
Implemented |
Foreseen |
Yes |
57 449 |
|
Estonia |
97 |
Implemented |
0.7 |
73 |
Not implemented |
Foreseen |
Yes |
36 123 |
|
Finland |
100 |
Implemented |
n/a |
68 |
Implemented |
Implemented |
Yes |
49 050 |
|
France |
93 |
Implemented |
0.9 |
85 |
Foreseen |
Implemented |
Yes |
47 065 |
|
Germany |
96 |
Implemented |
0.7 |
89 |
Implemented |
Implemented |
Yes |
54 878 |
|
Greece |
94 |
Not implemented |
0.3 |
40 |
n/a |
n/a |
Yes |
29 708 |
|
Hungary |
91 |
Implemented |
0.5 |
71 |
Implemented |
Implemented |
Yes |
31 771 |
|
Iceland |
61 |
n/a |
0.6 |
n/a |
n/a |
n/a |
Yes |
54 095 |
|
Ireland |
94 |
Implemented |
0.8 |
76 |
Implemented |
Implemented |
Yes |
65 698 |
|
Israel |
n/a |
n/a |
0.3 |
n/a |
n/a |
n/a |
Yes |
39 946 |
|
Italy |
88 |
Not implemented |
0.7 |
71 |
Implemented |
Implemented |
Yes |
42 784 |
|
Japan |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
Yes |
42 808 |
|
Latvia |
95 |
Implemented |
0.7 |
80 |
Not implemented |
Implemented |
Yes |
30 528 |
|
Lithuania |
95 |
Implemented |
0.9 |
76 |
Not implemented |
Implemented |
Yes |
35 989 |
|
Luxembourg |
99 |
Implemented |
n/a.. |
89 |
Not implemented |
Not implemented |
Yes |
72 376 |
|
Malta |
n/a |
Implemented |
0.8 |
83 |
Not implemented |
Foreseen |
Yes |
40 372 |
|
Mexico |
n/a |
n/a |
0.6 |
n/a |
n/a |
n/a |
Yes |
19 189 |
|
Netherlands |
97 |
Implemented |
0.9 |
71 |
Implemented |
Implemented |
Yes |
57 072 |
|
New Zealand |
n/a |
n/a |
1.0 |
n/a |
n/a |
n/a |
Yes |
41 672 |
|
Norway |
95 |
n/a |
0.8 |
79 |
n/a |
n/a |
Yes |
67 563 |
|
Poland |
93 |
Implemented |
0.2 |
64 |
Not implemented |
Not implemented |
Yes |
31 913 |
|
Portugal |
83 |
Implemented |
2.4 |
81 |
Implemented |
Implemented |
Yes |
34 154 |
|
Republic of Korea |
n/a |
n/a |
0.1 |
n/a |
n/a |
n/a |
Yes |
43 240 |
|
Romania |
n/a |
Implemented |
0.6 |
57 |
Not implemented |
Foreseen |
Yes |
29 549 |
|
Slovak Republic |
96 |
Not implemented |
n/a |
82 |
Not implemented |
Implemented |
Yes |
29 622 |
|
Slovenia |
94 |
Implemented |
0.6 |
76 |
Implemented |
Implemented |
Yes |
38 411 |
|
Spain |
93 |
Not implemented |
0.8 |
80 |
Not implemented |
Implemented |
Yes |
41 046 |
|
Switzerland |
97 |
n/a |
n/a |
n/a |
n/a |
n/a |
Yes |
65 821 |
|
Turkey |
n/a |
n/a |
0.6 |
n/a |
n/a |
n/a |
Yes |
27 814 |
|
United Kingdom |
91 |
Implemented |
0.8 |
74 |
Implemented |
Implemented |
Yes |
45 851 |
|
United States |
n/a |
n/a |
0.3 |
n/a |
n/a |
n/a |
Yes |
62 513 |
Note:*The figure for Australia represents the average cross each major city and refer to access to green space within 400m. n/a = no data available; GNI = gross national income; PPP = purchasing power parity. The shades of blue represent the distance each country is from the country in which the intervention currently operates, with a darker shade indicating greater transfer potential based on that particular indicator (see Annex A for further methodological details).
Source: WHO Regional Office for Europe (2021[27]), “2021 Physical Activity Factsheets for the European Union Member States in the WHO European Region”, https://apps.who.int/iris/bitstream/handle/10665/345335/WHO-EURO-2021-3409-43168-60449-eng.pdf; Eurostat (2021[28]), “Persons visiting a doctor in the last 12 months by medical speciality, number of visits, educational attainment level, sex and age”, http://eurostat.ec.europa.eu/; WHO (n.d.[29]), “Global Health Observatory”, https://www.who.int/data/gho’; World Bank (2020[30]), “GDP, PPP (current international $)”, https://data.worldbank.org/indicator/NY.GDP.MKTP.PP.CD.
To help consolidate findings from the transferability assessment above, countries have been clustered into one of three groups (see Figure 4.11 and Table 4.6). Countries in clusters with more positive values have the greatest transfer potential. Findings from the each of the clusters are below:
Countries in cluster one have population, political, economic and sector specific arrangements in place to transfer PAP and are therefore good transfer candidates. The original of the intervention is in this cluster: Sweden.
Countries in cluster two have policies in place that would support PAP. However, certain countries would benefit from assessing whether PAP is affordable among the population, as well as ensuring health professionals are properly trained, for example.
Countries in cluster three may want to consider the overall affordability of PAP as well as whether the sector is ready for such an intervention (e.g. such as an appropriately trained workforce).
Figure 4.11. Transferability assessment using clustering, PAP
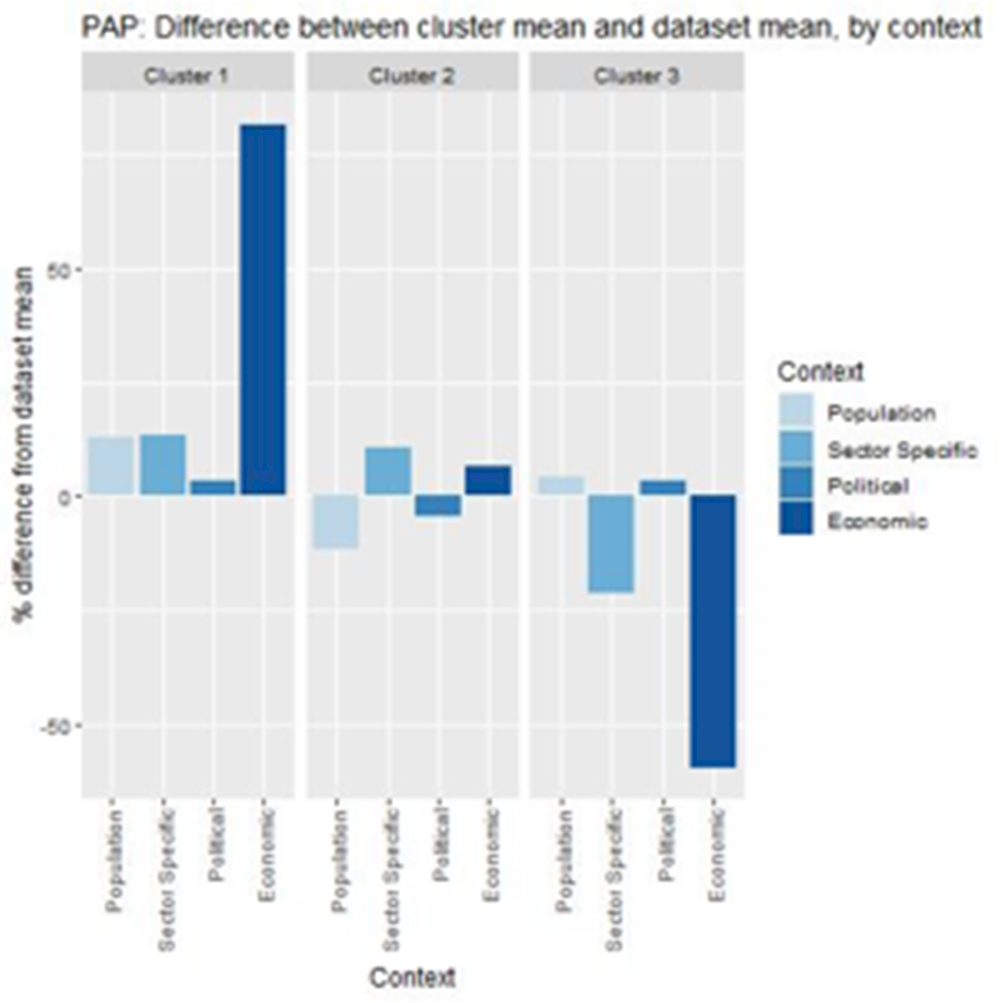
Note: Bar charts show percentage difference between cluster mean and dataset mean, for each indicator.
Source: WHO Regional Office for Europe (2021[27]), “2021 Physical Activity Factsheets for the European Union Member States in the WHO European Region”, https://apps.who.int/iris/bitstream/handle/10665/345335/WHO-EURO-2021-3409-43168-60449-eng.pdf; Eurostat (2021[28]), “Persons visiting a doctor in the last 12 months by medical speciality, number of visits, educational attainment level, sex and age”, http://eurostat.ec.europa.eu/; WHO (n.d.[29]), “Global Health Observatory”, https://www.who.int/data/gho’; World Bank (2020[30]), “GDP, PPP (current international $)”, https://data.worldbank.org/indicator/NY.GDP.MKTP.PP.CD.
Table 4.6. Countries by cluster, PAP
|
Cluster 1 |
Cluster 2 |
Cluster 3 |
|---|---|---|
|
Austria Germany Ireland Luxembourg Netherlands Norway Sweden |
Australia Belgium Cyprus Czech Republic Denmark Finland France Iceland Italy Malta Portugal Spain United Kingdom |
Bulgaria Croatia Estonia Greece Hungary Latvia Lithuania Poland Romania Slovak Republic Slovenia |
Note: Due to high levels of missing data, the following countries were omitted from the analysis: Australia, Canada, Chile, Colombia, Costa Rica, Israel, Japan, Mexico, New Zealand, Republic of Korea, Switzerland, Turkey and the United States.
New indicators to assess transferability
Data from publically available datasets is not sufficient to assess the transferability of PAP. Box 4.4 outlines several new indicators policy makers should consider before transferring PAP.
Box 4.4. New indicators to assess transferability
In addition to the indicators within the transferability assessment, policy makers are encouraged to collect information on the following questions:
Population context
Who are the target population groups for this intervention?
What is the population’s attitude towards physical exercise?
What is the level of health literacy in the population?
Sector specific context (primary care)
What, if any, compatible interventions exist?
What, if any, competing interventions exist?
Which health care professionals are best placed to prescribe physical activity? Do these health care professionals have the appropriate skills?
What is the level of access to structured physical activity or sporting facilities?
Is there a culture of health promotion and disease prevention in the health system?
Political context
Has the intervention received political support from key decision-makers?
Has the intervention received commitment from key decision-makers?
Economic context
What is the cost of implementing the intervention?
Does the intervention reach lower-income population groups?
Do lower-income groups have access to sporting facilities?
Conclusion and next steps
In Sweden, the PAP intervention provides people with personalised and evidence‑based advice on how to increase their physical activity. Using OECD’s SPHeP-NCD model, it is estimated that the resulting reduction in disease incidence leads to annual health expenditure savings of SEK 205.06 (EUR 19.37) per person by 2050. At a net saving of around SEK 91 000 (approximately EUR 9 000) per DALY, the PAP programme is cost saving.
Various factors have been identified to increase the effectiveness of the PAP intervention, including a longer duration and a high frequency of physical activity. To ensure an equitable intervention, providing access and quality to everyone, more data is needed on who receives a prescription, and what their outcomes are. For a low-cost, low-intensity intervention such as PAP, it is important to ensure a higher population coverage.
Transfer of the Swedish PAP intervention to nine other European countries has already started under the EU-funded “European Physical Activity on Prescription Model” project (EUPAP). Data from publically available sources indicates many potential transfer countries have policies in place to support PAP such as the inclusion of healthy lifestyle in the curriculum for health professionals.
Box 4.5 outlines next steps for policy makers and funding agencies regarding PAP.
Box 4.5. Next steps for policy makers and funding agencies
Next steps for policy makers and funding agencies to enhance PAP are listed below:
To understand the differences in uptake across the regions, and potentially even differences in outcomes, policy makers should consider setting up a register to follow participants and their outcomes
To enhance the uptake of the intervention, policy makers are advised to explore whether and how health care professionals can be encouraged and enabled to prescribe more.
References
[34] Aittasalo, M. et al. (2006), “A randomized intervention of physical activity promotion and patient self-monitoring in primary health care”, Preventive Medicine, Vol. 42/1, pp. 40-46, https://doi.org/10.1016/j.ypmed.2005.10.003.
[20] Andersen, P. et al. (2019), “Patients’ experiences of physical activity on prescription with access to counsellors in routine care: A qualitative study in Sweden”, BMC Public Health, Vol. 19/1, pp. 1-11, https://doi.org/10.1186/s12889-019-6535-5.
[16] Arsenijevic, J. and W. Groot (2017), “Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses”, BMJ Open, Vol. 7/2, p. 12156, https://doi.org/10.1136/bmjopen-2016-012156.
[12] BMJ Best Practice (n.d.), What is GRADE?, https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/ (accessed on 10 November 2021).
[18] Duncan, G. et al. (2005), “Prescribing exercise at varied levels of intensity and frequency: A randomized trial”, Archives of Internal Medicine, Vol. 165/20, pp. 2362-2369, https://doi.org/10.1001/archinte.165.20.2362.
[11] Effective Public Health Practice Project (1998), Quality assessment tool for quantitative studies, https://www.nccmt.ca/knowledge-repositories/search/14.
[3] EUPAP (2020), EUPAP Feasibility Study - Final Report, https://www.eupap.org/storage/app/media/WP4%20Feasibility%20Study.pdf (accessed on 4 February 2021).
[2] EUPAP.org (n.d.), EUPAP leaflet, https://www.eupap.org/storage/app/media/EUPAP_skrajute_atvartas.pdf (accessed on 4 February 2021).
[28] Eurostat (2021), Persons visiting a doctor in the last 12 months by medical speciality, number of visits, educational attainment level, sex and age, http://eurostat.ec.europa.eu/ (accessed on 25 August 2021).
[5] FYSS (2022), FYSS – Evidensbaserad Kunskapsbas, https://www.fyss.se/.
[15] Goryakin, Y., L. Suhlrie and M. Cecchini (2018), Impact of primary care-initiated interventions promoting physical activity on body mass index: systematic review and meta-analysis, Blackwell Publishing Ltd, https://doi.org/10.1111/obr.12654.
[21] Gustavsson, C. et al. (2018), “What is required to facilitate implementation of Swedish physical activity on prescription? - Interview study with primary healthcare staff and management”, BMC Health Services Research, Vol. 18/1, https://doi.org/10.1186/s12913-018-3021-1.
[25] Hallsworth, M. et al. (2016), “Provision of social norm feedback to high prescribers of antibiotics in general practice: a pragmatic national randomised controlled trial”, The Lancet, Vol. 387/10029, pp. 1743-1752, https://doi.org/10.1016/s0140-6736(16)00215-4.
[33] Hellgren, M. et al. (2016), “A lifestyle intervention in primary care prevents deterioration of insulin resistance in patients with impaired glucose tolerance: A randomised controlled trial”, Scandinavian Journal of Public Health, Vol. 44/7, pp. 718-725, https://doi.org/10.1177/1403494816663539.
[32] Hemmingsson, E. et al. (2009), “Increased physical activity in abdominally obese women through support for changed commuting habits: A randomized clinical trial”, International Journal of Obesity, Vol. 33/6, pp. 645-652, https://doi.org/10.1038/ijo.2009.77.
[10] Kallings, L. (2008), Physical activity on prescription: Studies on physical activity level, adherence and cardiovascular risk factors, Karolinska Institutet, Stockholm.
[7] Kallings, L. et al. (2009), “Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: results from a randomized controlled trial”, European Journal of Cardiovascular Prevention & Rehabilitation, Vol. 16/1, pp. 80-84, https://doi.org/10.1097/HJR.0b013e32831e953a.
[22] Kyei-Frimpong, J. et al. (2021), “Exercise as medicine: Providing practitioner guidance on exercise prescription”, Preventive Medicine Reports, Vol. 22, p. 101323, https://doi.org/10.1016/j.pmedr.2021.101323.
[35] Leijon, M. et al. (2008), “Physical activity referrals in Swedish primary health care - Prescriber and patient characteristics, reasons for prescriptions, and prescribed activities”, BMC Health Services Research, Vol. 8, p. 201, https://doi.org/10.1186/1472-6963-8-201.
[36] Leijon, M. et al. (2010), “Factors associated with patients self-reported adherence to prescribed physical activity in routine primary health care”, BMC Family Practice, Vol. 11, p. 38, https://doi.org/10.1186/1471-2296-11-38.
[17] Leijon, M. et al. (2011), “Who is not adhering to physical activity referrals, and why?”, Scandinavian Journal of Primary Health Care, Vol. 29/4, pp. 234-240, https://doi.org/10.3109/02813432.2011.628238.
[31] Morén, C. et al. (2016), “The Effects of “Physical Activity on Prescription” in Persons With Transient Ischemic Attack: A Randomized Controlled Study”, Journal of Neurologic Physical Therapy, Vol. 40/3, pp. 176-183, https://doi.org/10.1097/NPT.0000000000000134.
[38] OECD (2019), SPHeP-NCDs documentation, http://oecdpublichealthexplorer.org/ncd-doc/ (accessed on 16 December 2019).
[1] Onerup, A. et al. (2019), Physical activity on prescription in accordance with the Swedish model increases physical activity: A systematic review, BMJ Publishing Group, https://doi.org/10.1136/bjsports-2018-099598.
[19] Perri, M. et al. (2002), “Adherence to exercise prescriptions: Effects of prescribing moderate versus higher levels of intensity and frequency”, Health Psychology, Vol. 21/5, pp. 452-458, https://doi.org/10.1037/0278-6133.21.5.452.
[23] Persson, G. et al. (2013), “Physical activity on prescription (PAP) from the general practitioner’s perspective - A qualitative study”, BMC Family Practice, Vol. 14/1, p. 128, https://doi.org/10.1186/1471-2296-14-128.
[24] Persson, G., I. Ovhed and E. Hansson (2010), “Simplified routines in prescribing physical activity can increase the amount of prescriptions by doctors, more than economic incentives only: an observational intervention study”, BMC Research Notes, Vol. 3/1, https://doi.org/10.1186/1756-0500-3-304.
[37] Romé, Å. et al. (2009), “Physical activity on prescription (PAP): Costs and consequences of a randomized, controlled trial in primary healthcare”, Scandinavian Journal of Primary Health Care, Vol. 27/4, pp. 216-222, https://doi.org/10.3109/02813430903438734.
[8] Sjögren, P. et al. (2012), “Functional changes in adipose tissue in a randomised controlled trial of physical activity”, Lipids in Health and Disease, Vol. 11/1, p. 80, https://doi.org/10.1186/1476-511X-11-80.
[14] SVT Nyheter (2019), Stor skillnad på hur mycket motion på recept som skrivs ut i riket [Large difference in how much exercise on prescription is prescribed in the country], https://www.svt.se/nyheter/lokalt/orebro/regioner-anser-att-motion-pa-recept-borde-oka (accessed on 6 October 2021).
[26] Triberti, S. (ed.) (2020), “The effectiveness of behavioral economics-informed interventions on physician behavioral change: A systematic literature review”, PLOS ONE, Vol. 15/6, p. e0234149, https://doi.org/10.1371/journal.pone.0234149.
[9] Vallejo-Torres, L. et al. (2016), “On the Estimation of the Cost-Effectiveness Threshold: Why, What, How?”, Value in Health, Vol. 19/5, pp. 558-566, https://doi.org/10.1016/j.jval.2016.02.020.
[29] WHO (n.d.), Global Health Observatory, https://www.who.int/data/gho (accessed on 25 August 2021).
[6] WHO (n.d.), Global Physical Activity Questionnaire (GPAQ) Analysis Guide, http://www.who.int/chp/steps/GPAQ/en/index.html (accessed on 29 January 2021).
[13] WHO Global Health Observatory (2018), Mean body mass index (BMI) trends among adults, https://apps.who.int/gho/data/view.main.CTRY12461.
[27] WHO Regional Office for Europe (2021), 2021 Physical Activity Factsheets for the European Union Member States in the WHO European Region, https://apps.who.int/iris/bitstream/handle/10665/345335/WHO-EURO-2021-3409-43168-60449-eng.pdf.
[30] World Bank (2020), GDP, PPP (current international $), https://data.worldbank.org/indicator/NY.GDP.MKTP.PP.CD (accessed on 25 August 2021).
[4] YFA (2022), FYSS – vägen till bättre folkhälsa, https://www.yfa.se/fyss/vad-ar-fyss/.
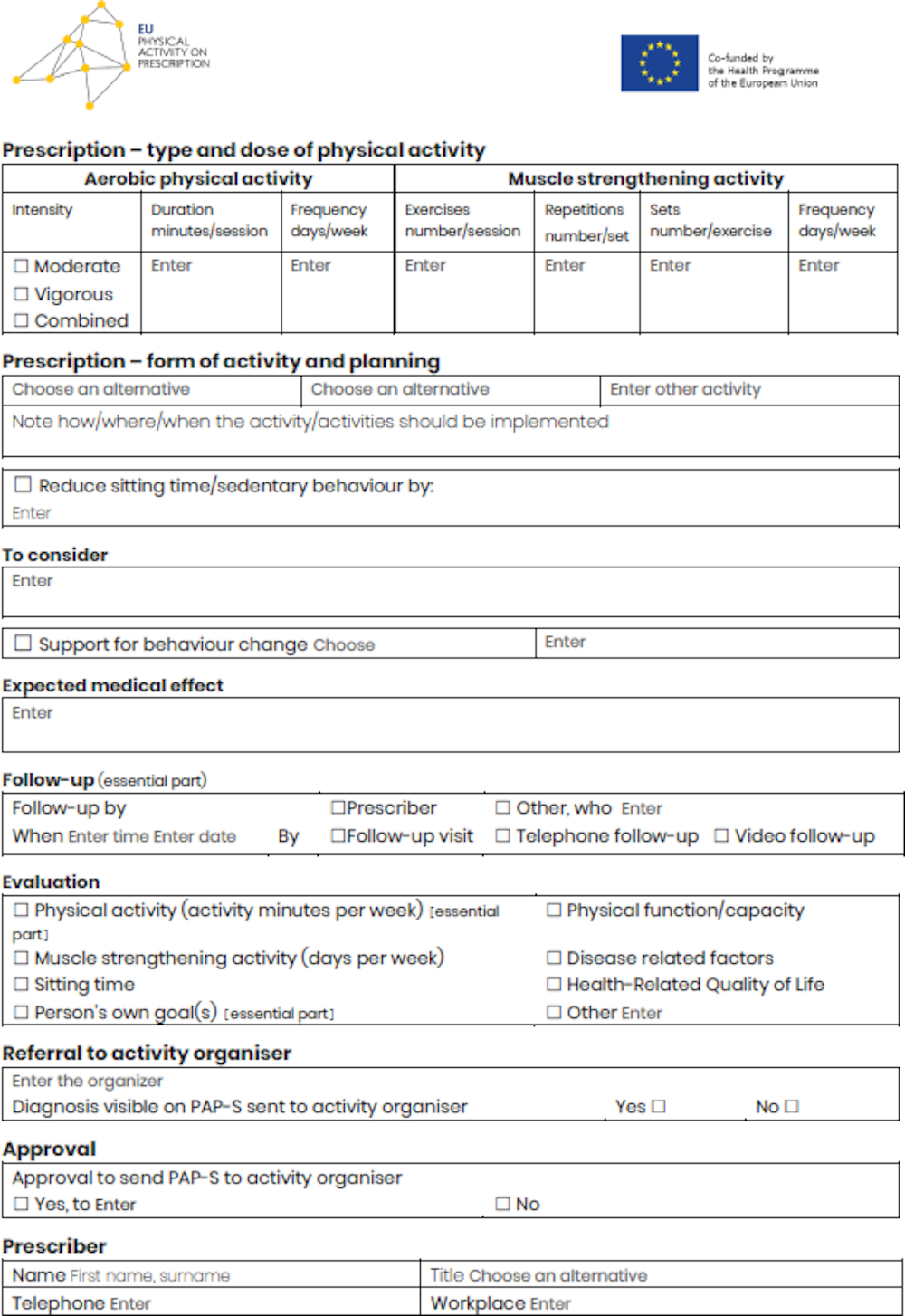
Annex 4.A. Sample of the PAP prescription form
Annex 4.B. Modelling assumptions for PAP
Annex Table 4.B.1. Parameters to model the impact of PAP
|
Physical Activity on Prescription model inputs |
|
|---|---|
|
Effectiveness |
BMI: ‑0.4 kg/m2 MET min / week: +636 |
|
Time to maximum effectiveness |
6 months to maximum effectiveness, after which the effect stays stable for 1 year, and then reverts to zero after another 6 months All changes are modelled as a linear increase/decrease |
|
Target population |
People of both sexes, over the age of 18, who do less than 600 MET min/week; and have overweight (BMI >25), high blood pressure, diabetes, COPD, asthma, depression, cardiovascular disease or musculoskeletal disorders |
|
Exposure |
Base scenario: Overall participation rate = 0.56% of the total adult population Dropout rate: 50% Higher scenario: Overall participation rate = 2.39% of the total adult population Dropout rate: 50% |
|
Per capita cost, SEK and EUR |
SEK 2.08 (EUR 0.21) per capita SEK 532.77 (EUR 53.26) per treated person |
Effectiveness
As the Swedish PAP model has been in use for over 20 years, a number of studies exist on its effectiveness. In 2019, Onerup et al. conducted a systematic review to evaluate the existing scientific evidence for the efficacy of the Swedish PAP model, focusing on studies that have a control group (Onerup et al., 2019[1]). However, as many of the studies included in the review used different measures for the level of PA, often with different follow-up times, no meta‑analysis was performed. Moreover, some studies looked at specific subpopulations (e.g. people with transient ischemic attack (Morén et al., 2016[31])), considered a broader set of interventions besides PAP (e.g. group counselling and free bicycles (Hemmingsson et al., 2009[32])), did not measure physical activity in a way that can be included in the OECD SPHeP-NCDs model (e.g. a four level scale (Hellgren et al., 2016[33])) or not based in Sweden (e.g. Finland (Aittasalo et al., 2006[34]))
A number of the studies included in the review were based on data from the same randomised controlled trial (RCT) (Kallings et al., 2009[7]) (Sjögren et al., 2012[8]). In this RCT, 101 healthy but insufficiently physically active 67 to 68‑year‑olds with overweight either received a 6‑month intervention of PAP or a low-intensity intervention, with one page of written general information about the importance of PA for health. Individuals who received the PAP intervention were found to have increased their physical activity level by 159 minutes of (at least) moderate‑intensity activity per week, from a baseline of 120 minutes, compared to no change in the control group. Using a weight of 4 METs for moderate intensity activities (WHO, n.d.[6]), this equates to an increase of 636 MET-minutes per week.
In addition, they report that BMI decreased by 0.6 in the intervention group, compared to 0.2 in the controls. A decrease of 0.4 BMI points (95% CI 0.1 to 0.8) can therefore be attributed to the intervention.
Time to maximum effectiveness
The follow-up time of the RCT by (Kallings et al., 2009[7]) was 6 months, coinciding with the 6‑month follow-up counselling session. After reaching a maximum impact at 6 months, the effect is expected to remain at its maximum level for 12 months, after which it wears off over another 6 months. Any increase or decrease is modelled linearly (Goryakin, Suhlrie and Cecchini, 2018[15]).
Target population
Anyone over the age of 18 can receive a prescription for physical activity, regardless of their health status. However, in practice the intervention is prescribed to people whom health care professionals believe would benefit from increased physical activity, due to sedentary lifestyles and diagnoses such as high blood pressure, diabetes, overweight, COPD, asthma, depression, cardiovascular disease and musculoskeletal disorders (Leijon et al., 2008[35]) (Morén et al., 2016[31]). Therefore, people doing less than 600 MET-minutes per week (the WHO guidelines for physical activity) who also have high BMI or other NCDs are considered to be the target population.
Exposure
One study found that 1.3% of primary health care (PHC) patients visiting a PHC centre in the study area was prescribed physical activity annually (Leijon et al., 2008[35]). However, these rates were observed more than 15 years ago. In 2019, a total of 45 000 prescriptions were made across all regions. As the Swedish adult population in 2019 was around 8 million, this amounts to 5.6 prescriptions per 1 000 population. Assuming 40% of the adult population is eligible for the PAP scheme, the exposure would be 14.1 prescriptions per 1000.
As this exposure is relatively low, the coverage rate of one of the better preforming regions was also modelled. In Norrbotten in 2019, 4 776 patients received PAP, out of a population of approximately 200 000. This equated to an overall population coverage rate of 23.9 per 1 000 population, or 59.7 per 1 000 eligible population.
Self-reported adherence to the prescribed PA was 56% at 3 months and 50% at 12 months (Leijon et al., 2010[36]). An RCT looking at the PAP programme has a dropout rate of 53% at 4 months (Romé et al., 2009[37]). Data from practice shows that in the region of Norrbotten over the period 2013 to 2020, approximately 50 to 65% of prescriptions was followed up six months later. In the region of Stockholm this figure was approximately 50%. Overall, a 50% drop out rate was therefore assumed for the model. For people who drop out, no effect was assumed. This is a conservative assumption, as some might have increased their physical activity level despite not coming in for a follow-up meeting, but there is no data to confirm this.
Eligible persons can participate again in the future.
Cost of implementation and delivery
Cost are estimated using the WHO Costing Tool (see section 7.4 of the SPHeP-NCD documentation (OECD, 2019[38]), and consider the base PAP programme only, and no potential additional cost associated with providing exercise classes or access to facilities. In the RCT, the individualised patient-centred counselling based on which the prescription was written took approximately 30 minutes (Kallings et al., 2009[7]). The follow-up meeting is assumed to take 10 minutes. To calculate the cost of these two meetings, both the initial and follow-up appointments are assumed to be provided by an equal mix of GPs, physiotherapists and nurses. In Sweden, this mix varies by region and it will also differ per country. Actual cost may be higher if PAP is mostly delivered by GPs, or lower if it is mostly done by nurses. Moreover, under the EUPAP programme, a number of EU countries have implemented PAP but with a longer length of consultations, or with more follow-up meetings, both of which would also increase the cost of the programme. The cost of the initial meeting for people who drop out of the intervention is included in the cost of treated people. Per treated person, the cost were estimated to be SEK 532.77 (EUR 53.26).
In addition to these treatment cost, central cost were calculated. These include a charge for providing GPs with a copy of the handbook. While there are cost associated with the development and maintenance of the handbook, this is already covered by the Swedish programme and translation/adaptation cost for other countries is expected to be minimal. There are however some overheads associated with the central planning of the programme. In all, the central cost of the programme were estimated at SEK 2.08 (EUR 0.21) per capita.
